You are using an outdated browser. Please upgrade your browser to improve your experience.
Skip to Site Navigation Skip to Page Content
- Physician Referrals
- Patient Resources
- Why UT Southwestern
Refine your search: Find a Doctor Search Conditions & Treatments Find a Location

Appointment New Patient Appointment or Call 214-645-8300
Your Pregnancy Matters

4 common pregnancy-related GI issues, and when to call the doctor
October 9, 2018
Gastrointestinal (GI) issues are common during pregnancy. As your baby grows, you’ll have less available real estate in your abdomen for your intestines, stomach, and esophagus to function. Additionally, hormonal changes can affect digestion and other GI functions.
Most GI symptoms pass relatively quickly during pregnancy and can be treated with over-the-counter remedies at home. However, to avoid potential complications, women should be aware of what’s normal and when to call the doctor when it comes to GI health during pregnancy.
1. Nausea and vomiting
During the first 16 weeks of pregnancy , we expect some mild to moderate nausea and vomiting – the infamous period of morning sickness . In fact, for many women, nausea is one of the earliest symptoms of pregnancy .
If you have severe symptoms, a doctor can recommend medication to reduce dehydration and discomfort. For mild symptoms, or if you prefer not to take medication, you can usually manage symptoms with dietary changes or vitamin therapy under the care of your doctor.
After 16 weeks of pregnancy , vomiting typically is not pregnancy-related and might be due to a bug or infection. In rare cases, vomiting can be caused by more serious medical concerns, such as hepatitis, pancreatitis, or ulcers. If you experience nausea or vomiting past the first trimester of pregnancy, don’t assume it’s pregnancy-related, and don’t let your doctor assume so, either, without checking for underlying causes.
2. Heartburn
Heartburn, or gastroesophageal reflux, affects three of five people in the general population. By the time women reach the third trimester, as many as half will experience heartburn at one point or another. During pregnancy, the muscle between the esophagus and stomach relaxes due to hormonal changes related to pregnancy. At the same time, the growing uterus puts increased pressure on the stomach. The combination is a perfect storm for heartburn.
Eating smaller, more frequent meals can help stave off heartburn. Standard treatments – antacids, proton pump inhibitors (Prevacid), or H2 blockers (Tagamet or Pepcid) – are generally safe during pregnancy.
However, if you experience pain below the ribs in your upper abdomen, call your doctor. Although rare, epigastric pain can be a sign of fatty liver disease or preeclampsia , a serious blood pressure disease that can arise suddenly during pregnancy.
3. Diarrhea
Let’s face it – diarrhea is the worst. When it lasts just a few days, diarrhea typically is related to an infection (usually gastroenteritis ) or eating something that upsets your stomach. Check in with your doctor to determine the best treatment option to reduce dehydration and duration of illness.
Diarrhea that develops without an identifiable trigger or in combination with low back pain and increased vaginal discharge or mucus can be symptoms of preterm labor. Call your doctor immediately if you experience this combination of symptoms.
4. Constipation
Pregnancy hormones affect the lower GI tract, effectively slowing down the transit of stool through the bowels. This slow-motion process allows more water to be absorbed in the stools, which makes them hard to pass. Certain prenatal vitamins and iron therapy also can contribute to constipation. Later in pregnancy, pressure from the growing uterus can also make it harder to pass stools, which increases the risk of hemorrhoids.
Drinking more fluids and eating more fiber is effective in reducing and preventing constipation. Stool softeners are safe to use as well, and some iron supplements actually contain them. More severe constipation might require a mild laxative. Talk to your doctor about additional treatments if you experience abdominal pain, bloody stools, or painful hemorrhoids.
Most women will experience GI concerns at some point during pregnancy. If your symptoms are serious or if you are concerned, talk to your doctor. It’s better to be safe, and we’re here to help your pregnancy – and GI tract – flow smoothly.
Stay on top of health care news. Subscribe to our blog today.
More in: Your Pregnancy Matters

Next Article RhoGAM shortage: Managing Rh incompatibility in pregnancy
More from Your Pregnancy Matters
Rhogam shortage: managing rh incompatibility in pregnancy.
- Robyn Horsager-Boehrer, M.D.
April 2, 2024

Closing gaps in postpartum care: the IMPACT study
- Elaine Duryea, M.D.
- David Nelson, M.D.
March 22, 2024

Congenital syphilis is on the rise: What pregnant women need to know
- Emily Adhikari, M.D.
March 12, 2024

Women's Health; Your Pregnancy Matters
Breaking the silence about endometriosis
- Kimberly Kho, M.D.
February 22, 2024

Is genetic screening recommended during pregnancy if you’ve had IVF?
- Ashley Zink, M.D.
- Heather Fisher, M.S.
February 20, 2024

Mental Health; Your Pregnancy Matters
Studying the connection between anxiety and preterm birth
February 9, 2024

Why pregnant women should resist ‘vaccine fatigue’
January 9, 2024

Aging; Men's Health; Your Pregnancy Matters
How does a father’s age affect fertility and a baby’s health?
- Leen Al-Hafez, M.D.
October 13, 2023

Can genetic testing explain the cause of recurrent miscarriages?
September 19, 2023
More Articles
Appointment New Patient Appointment or 214-645-8300 or 817-882-2400
- Share via Facebook facebook
- Share via Twitter twitter
- Share via LinkedIn linkedin
- Share via Email email
- Print this page print
Download Pathkind Labs App

Enter your mobile no. An OTP will be sent to this no.
Other Cities
- { window.location.reload(); }, 1000);"> Mumbai
- { window.location.reload(); }, 1000);"> Delhi
- { window.location.reload(); }, 1000);"> Bangalore
- { window.location.reload(); }, 1000);"> Hyderabad
- { window.location.reload(); }, 1000);"> Ahmedabad
- { window.location.reload(); }, 1000);"> Chennai
- { window.location.reload(); }, 1000);"> Kolkata
- { window.location.reload(); }, 1000);"> Surat
- { window.location.reload(); }, 1000);"> Pune
- { window.location.reload(); }, 1000);"> Jaipur
- { window.location.reload(); }, 1000);"> Lucknow
- { window.location.reload(); }, 1000);"> Kanpur
- { window.location.reload(); }, 1000);"> Nagpur
- { window.location.reload(); }, 1000);"> Indore
- { window.location.reload(); }, 1000);"> Thane
- { window.location.reload(); }, 1000);"> Bhopal
- { window.location.reload(); }, 1000);"> Visakhapatnam
- { window.location.reload(); }, 1000);"> Pimpri-Chinchwad
- { window.location.reload(); }, 1000);"> Patna
- { window.location.reload(); }, 1000);"> Vadodara
- { window.location.reload(); }, 1000);"> Ghaziabad
- { window.location.reload(); }, 1000);"> Ludhiana
- { window.location.reload(); }, 1000);"> Agra
- { window.location.reload(); }, 1000);"> Nashik
Steps You Can Take to Avoid Stomach Problems During Pregnancy

During pregnancy, several physical and emotional aspects happen in your body. While awaiting your new baby brings numerous joys, other experiences make the pregnancy process daunting and uncomfortable, such as early pregnancy stomach pain. It includes multiple complications like:
- Indigestion
- Constipation
These problems occur due to hormonal imbalance , extra pressure on the abdomen, and changes in diet, among others. Fortunately, you can take some steps to facilitate better digestive health during your pregnancy.
10 Steps You Can Take to Avoid Stomach Problems During Pregnancy
Here are 10 actionable steps you can employ to prevent stomach problems during pregnancy:
- Eat Small, Regular Meals - During pregnancy, your stomach produces more acid and may become more sensitive. When you eat large meals, you put pressure on your stomach and intestines, raising the risk of early pregnancy stomach pain. To avoid combatting your sensitive digestion, eat small meals regularly. You should have something every couple of hours to ensure your blood sugar levels remain stable and that you and your baby receive a constant supply of nutrients.
- Eat Foods High in Nutrients - Certain foods are high in vitamins and minerals and fibrous foods that help support your baby’s growth and digestion. Eat plenty of fresh fruits and vegetables, whole grains, and plant-based proteins with healthy fats. Whole grain foods help nourish beneficial bacteria while also supporting your food waste. Pass up sugary snacks or refined carbohydrates.
- Stay Hydrated - Sufficient hydration is essential not only for proper digestion but also for preventing constipation during pregnancy. You should aim to drink approximately eight to ten glasses of water daily and consume hydrating foods such as fruits and vegetables. Proper hydration can also help to soften stool, facilitating regular bowel movements and reducing the risk of constipation. If you dislike the flavour of plain water, you can infuse it with fresh fruit or enjoy herbal teas, such as peppermint or ginger, which can aid digestion.
- Avoid Trigger Foods - Certain foods and beverages may aggravate stomach issues during pregnancy. Spicy, greasy, and acidic dishes, as well as caffeinated and carbonated drinks, may contribute to heartburn, indigestion, and nausea. Avoid food that causes complications with your body. Consider learning how to keep a food diary to keep track of your symptoms and speaking with a registered dietitian for individualised dietary recommendations.
- Mindful Eating - Mindful eating requires paying attention to the body’s hunger and fullness cues while savouring each bite. Eating slowly and mindfully reduces the risk of overeating. Eating too quickly places a strain on your digestive system, leading to an increased risk of stomach problems. Therefore, eat slowly and remember to chew your food as much as possible to relish the experience without any diversion. Similarly, avoid eating while looking at your smartphone or watching TV.
- Manage Stress - Pregnancy is an exciting period but also quite stressful. High-stress levels may significantly affect digestive health. They may further deteriorate conditions like indigestion or irritable bowel syndrome. To reduce stress and ensure proper digestion, adopt stress-reduction behaviours, such as deep breathing, prenatal yoga, meditation, or any gentle exercise. Choose the exercises that make you relaxed and happy and practise them daily. Also, engage in self-care activities you like and enjoy, and seek personal support from your partner, relatives, or friends.
- Stay Active - Regular physical activity can facilitate digestion and eliminate constipation during pregnancy. Perform low-impact exercise, such as walking, swimming, or yoga, to move your body and increase bowel function. Consult your physician before starting physical activity during pregnancy, listen to your body, and never overburden yourself. Strive for at least 30 minutes of exercise at moderate intensity most days of the week. Incorporate physical activities that you like and feel comfortable doing.
- Consider Probiotics - Probiotics as health-friendly bacteria can help keep a balanced environment in your gut flora and may assist in alleviating digestive issues, including constipation or diarrhoea. Discuss taking a probiotic supplement with your prenatal care provider or consume natural probiotic-rich food, such as yoghourt, kefir, sauerkraut, or miso.
- Sleep on Your Left Side - You may experience better digestion when you sleep on your left side while pregnant. Sleeping on your left side also reduces the risk of heartburn and acid reflux. That is because gravity prevents stomach acid from flowing back into the oesophagus. This might decrease night time discomfort and improve sleep quality. While sleeping on your side, use pillows to raise your belly and legs. You may want to experiment with different sleeping positions to figure out which one is most comfortable for you.
- Consult Your Healthcare Provider - Speak with your healthcare provider immediately if you believe you have severe gastrointestinal problems. Your healthcare provider can provide personal recommendations and treatment to improve your quality of life and your child’s health. Certain specialised measures they recommend include treatments. You can get over the counter or prescribed medications to manage certain digestive problems or be directed to other physicians. Discussing your misconceptions or questioning your health team is necessary to address your digestion issues during pregnancy.
Final Thoughts
Stomach problems are almost inevitable during pregnancy, but by adhering to the above steps and adopting proactive measures, you can minimise the inconvenience associated with them and take care of the health of your digestive system. Navigating digestive health challenges during pregnancy becomes smoother and more bearable by doing so.
However, remember to keep in touch with your doctor to figure out what may work for you and prioritise your overall well-being. Preventing digestive discomfort helps you focus on preparing for and connecting with your new baby.
If you’re a pregnant mother and want to give your baby the healthiest life possible, then get screened for potential problems early on! Book a full-body test at Pathkind today and secure your baby’s future!
Most viewed

Omicron Variant - How to Deal with the New Scare?

How Covid-19 Mutates and How It Affects Vaccines?

Essential Blood Tests for Ageing Gracefully

When and Why You Should Go for the Lipid-Profile Test?

Most Frequently Asked Questions About Exercise

The Ergonomics of Working from Home during Coronavirus

Hormones and Hair Fall: Understanding the Hormonal Imbalance

How Can You Help Others During This COVID-19 Crisis?

Diabetes Test Packages: Your Comprehensive Guide to Patholog...

Thyroid Troubles? Don't Panic! Find Out How to Restore Balan...

5 Best Medicines You Can Take in Fever to Prevent Body Pain ...

How to beat bad breath?

All you need to know about Dengue fever is here!

Celebrating International Yoga Day with Mindful Movement

What Food to Avoid Eating While Having a Kidney Stone?
Related blog.

Should I Go for Blood Tests During my Menstrual Cycle?
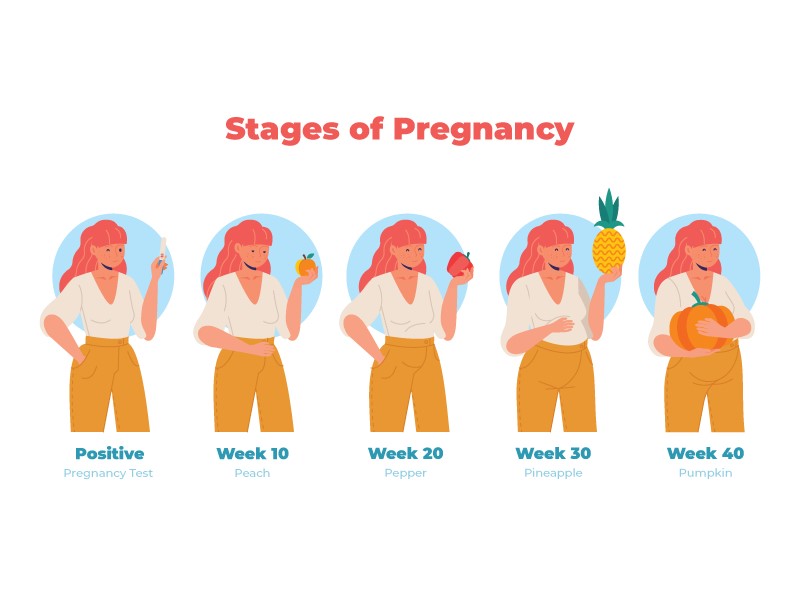
Navigating Pregnancy Stages: Understanding the Significance ...

Recurrent Pregnancy Loss- Current Scenario and Causes
A Path to Parenthood: Exploring the Diversity of Assisted Te...

Embracing the Journey of Motherhood: Pregnancy Symptoms and ...

Navigating Pregnancy Comfort: A Comprehensive Guide to Manag...

Kegels and Pregnancy: A Comprehensive Guide for Expecting Mo...
Get a call back from our health advisor.
and get the best benefits out of special packages for thyroid
Related Test
RPL Panel (Recurrent Pregnancy Loss)
Pregnancy Associated Plasma Protein-A(PAPP-A)
Urine Pregnancy Test (UPT)
Lipid Profile
Recent Blog

What Are the 5 Serious Viral Infections You Can Encounter?

How Low Your Blood Pressure Can Go in Hypotension? Take Precautions Now !!
5 best medicines you can take in fever to prevent body pain and muscle ache.

7 Food Items You Can Avoid During Loose Motion Sickness

5 Home Remedies for Relief from Swollen Veins Caused Due to Piles Disease

Unmasking the Stealth Symptoms - Recognizing Uncommon Signs of Urinary Tract Inf...
.webp)
Strategies for Managing Polycystic Ovarian Syndrome (PCOS)
Blood tests near you.
- Blood Test in Ace City
- Blood Test in Alpha 2
- Blood Test in ECO Village
- Blood Test in Sector 120, Noida
- Blood Test in Sector 76, Noida
- Blood Test in Sector 74, Noida
- Blood Test in Chi 4
- Blood Test in P 1
- Blood Test in Beta I
- Blood Test in Evergreen Complex
- Blood Test in Gaur City
- Blood Test in Greater Noida
- Blood Test in Bahlolpur
- Blood Test in Sector 44, Noida
- Blood Test in Sector 50, Noida
- Blood Test in Alpha Ii
- Blood Test in Sector 150, Noida
- Blood Test in Noida Extension
- Blood Test in Noida
- Blood Test in Paras Tierea
- Blood Test in Sector 1, Noida
- Blood Test in Sector 100, Noida
- Blood Test in Sector 93a, Noida
- Blood Test in Sector 30, Noida
- Blood Test in Sector 79, Noida
- Blood Test in Sector 45, Noida
- Blood Test in Sector 52, Noida
- Blood Test in Sector 104, Noida
- Blood Test in Sector 110, Noida
- Blood Test in Sector 119, Noida
- Blood Test in Sector 47, Noida
- Blood Test in Sector 107, Noida
- Blood Test in Sector 61, Noida
- Blood Test in Adrash Nagar
- Blood Test in Air Force
- Blood Test in Alaknanda
- Blood Test in Indraprastha
- Blood Test in Saket
- Blood Test in Safdarjung Enclave
- Blood Test in Alipur
- Blood Test in Babarpury
- Blood Test in Bakhtawar Pur
- Blood Test in Vasant Vihar
- Blood Test in Kalkaji Extension
- Blood Test in Karol Bagh
- Blood Test in Bakhtawarpur
- Blood Test in Baprola
- Blood Test in Burari
- Blood Test in Uttam Nagar
- Blood Test in New Friends Colony
- Blood Test in CR Park
- Blood Test in Chattarpur
- Blood Test in Civil Line
- Blood Test in Mumbai
- Blood Test in Select
- Blood Test in Borivali
- Blood Test in Andheri
- Blood Test in Bandra
- Blood Test in Jogeshwari 74, Noida
- Blood Test in Juhu
- Blood Test in Kandivali
- Blood Test in Prabhadevi
- Blood Test in Santacruz
- Blood Test in Thane
- Blood Test in Ulhasnagar
- Blood Test in Hiranandani Estate
- Blood Test in Oshiwara
- Blood Test in Bhandup
- Blood Test in Byculla
- Blood Test in Chembur
- Blood Test in Khar
- Blood Test in Kurla
- Blood Test in Lal Baug
- Blood Test in Vikhroli
- Blood Test in Vile Parle
- Blood Test in Wadala
- Blood Test in CBD Belapur
- Blood Test in Nerul
- Blood Test in Miraroad
- Blood Test in Churchgate
- Blood Test in Colaba
- Blood Test in Dadar
- Blood Test in Mahim
- Blood Test in Malad
- Blood Test in Matunga
- Blood Test in Worli
- Blood Test in Tardeo
- Blood Test in Marine Lines
- Blood Test in Versova
- Blood Test in Parel
- Blood Test in Virar
- Blood Test in Dahisar
- Blood Test in Ghatkopar
- Blood Test in Goregaon
- Blood Test in Mulund
- Blood Test in Mumbai Central
- Blood Test in Powai
- Blood Test in Kharghar
- Blood Test in Lokhandwalla
- Blood Test in Sion
- Blood Test in Vashi
- Blood Test in Airoli
- Blood Test in Sanpada
- Blood Test in Sector 42, Gurgaon
- Blood Test in Sector 3, Gurgaon
- Blood Test in Sector 14, Gurgaon
- Blood Test in Sector 10 A, Gurgaon
- Blood Test in Sector 23, Gurgaon
- Blood Test in Sector 37c, Gurgaon
- Blood Test in Sector 104, Gurgaon
- Blood Test in Sector 107, Gurgaon
- Blood Test in Sector 33, Gurgaon
- Blood Test in Sector 91, Gurgaon
- Blood Test in Sector 53, Gurgaon
- Blood Test in Sushant Lok 2
- Blood Test in Sector 15, Gurgaon
- Blood Test in Sector 17 A, Gurgaon
- Blood Test in Sector 40, Gurgaon
- Blood Test in Dlf Phase 3
- Blood Test in Dlf Phase 2
- Blood Test in New Railway Rd
- Blood Test in Sector 52, Gurgaon
- Blood Test in Sector 69, Gurgaon
- Blood Test in Sector 70 A, Gurgaon
- Blood Test in Sector 39, Gurgaon
- Blood Test in Sector 45, Gurgaon
- Blood Test in Sector 46, Gurgaon
- Blood Test in Rajiv Nagar
- Blood Test in Sohna
- Blood Test in South City 2
- Blood Test in Sector 47, Gurgaon
- Blood Test in Sector 50, Gurgaon
- Blood Test in Manesar
- Blood Test in Sector 8, Gurgaon
- Blood Test in Maruti Kunj
- Blood Test in Sector 38, Gurgaon
- Blood Test in Sector 86, Gurgaon
- Blood Test in Sector 94, Gurgaon
- Blood Test in Sector 57, Gurgaon
- Blood Test in Sector 48, Gurgaon
- Blood Test in Sector 49, Gurgaon
- Blood Test in Sector 56, Gurgaon
- Blood Test in South City 1
- Blood Test in Sushant Lok 1
- Blood Test in Sector 66, Gurgaon
- Blood Test in Palam Vihar
- Blood Test in Sector 78, Gurgaon
- Blood Test in Sector 83, Gurgaon
- Blood Test in Sector 63, Gurgaon
- Blood Test in Sector 10, Gurgaon
- Blood Test in Sector 102, Gurgaon
- Blood Test in Sector 65, Gurgaon
- Blood Test in Sector 71, Gurgaon
- Blood Test in Sector 84, Gurgaon
- Blood Test in Wazirpur
- Blood Test in Sector 43, Gurgaon
- Blood Test in Sector 109, Gurgaon
About Pathkind Labs
Discover precision diagnostics with Pathkind Labs, a trusted name in diagnostic services in India. Our NABL accredited labs, equipped with advanced technology, are staffed by a certified team of over 200 senior pathologists and 2000 technicians. From tailored health check-ups to specialized tests in Oncology, Neurology, Gynaecology, Nephrology, and more, we've got your health covered. Skip the hassle with online booking for tests or check-ups, available for both lab visits and at-home blood collection. For a seamless experience and early detection, choose Pathkind Labs in Gurugram. Book your appointment today and experience diagnostics made easy.
Popular Health Tests
- Adenosine Deaminase (ADA) | SGPT / ALT | Albumin | Alkaline Phosphatase (ALP) | Amylase | SGOT / AST | Bilirubin Total (Direct & Indirect) | Bilirubin Total | Blood Urea Nitrogen (BUN) | Calcium | Creatine Phosphokinase (CPK) | Creatinine | Sodium, Potassium, Chloride | Estimated Glomerulus Filtration Rate | Gamma-Glutamyl Transferase (GGT) | Glucose Challenge Test (GCT) | Fasting Plasma Glucose | Creatine Kinase MB | Glucose Post Prandial | Glucose Random | Glucose Tolerance Test (GTT-2) | HbA1C (Glycosylated Hemoglobin) | Iron Studies | Lactate Dehydrogenase (LDH) | Lipase | Microalbuminuria, Spot Urine | Phosphorus | Blood Urea Nitrogen (BUN), Urea | Potassium | Protein / Creatinine Ratio | Sodium | Sodium | Total Cholesterol | Uric Acid | Alpha-Fetoprotein (AFP) | Anti Cyclic Citrullinated PeptideAntibodies (Anti CCP) | Progesterone | Prolactin (PRL) | Prostate Specific Antigen (PSA) Total | Parathyroid Hormone (PTH) | QUADRUPLE MARKER TEST | Testosterone Total | Thyroid Profile | Anti Mullerian Hormone (AMH) | TSH 3rd Generation | Vitamin B12 | Vitamin D 25 - Hydroxy | LF, FSH | Anti Thyroid Peroxidase Antibodies (TPO) | CA 125 | Carcinoembryonic Antigen (CEA) | Serum Cortisol | DOUBLE MARKER | Vitamin Check | Estradiol (E2) | Ferritin | Folic Acid | Follicle-Simulating Hormone (FSH) | Thyroid Profile Free | FT4, TSH 3rd Gen | FT4 (Free Thyroxine 4) | Homocysteine | LH + FSH + PRL | IgE Total | Insulin Fasting | Luteinizing Hormone (LH) | APTT | BT, CT Time | Prothrombin Time | D-Dimer(Quantitative) | Cerebrospinal Fluid (CSF) Analysis | Pleural Fluid Analysis | Semen Analysis | Stool Occult Blood | Stool Routine & Microscopic Examination | Urine Pregnancy Test (UPT) | Urine Routine & Microscopy | Fine Needle Aspiration Cytology (FNAC) | PAP (Papanicolaou) Smear | Liquid Based Cytology (LBC),Sure path Cytology | Cytology For Malignant Cells | HLA B27, Flowcytometry | Absolute Eosinophil Count (AEC) | Blood Grouping, Rh (D) Typing | Haemogram with PS | Complete Blood Count (CBC) | Erythrocyte Sedimentation Rate (ESR) | Haemoglobin (Hb) | Indirect Coombs Test (ICT) Serum | Malaria Antigen detection, Rapid | Malaria Parasite (MP) Smear | Peripheral Blood Smear Examination | Platelet Count | Reticulocyte Count | TLC, DLC (Differential Leucocyte Count) | Hemoglobin Variant (Hb Electrophoresis) | CBC, ESR | TLC (Total Leucocyte Count) | DLC (Differential Leucocyte Count) | Histopathology: Large Tissue Biopsy | Histopathology:Medium tissue biopsy | Histopathology: Small Tissue Biopsy | Return Of Paraffin Block / Slide | COVID-19 Virus Qualitative RT PCR | Hepatitis B (HBV) Viral Load By Real Time PCR | Hepatitis C (HCV) Viral Load By Real Time PCR | Acid Fast Bacilli (AFB) Smear | Gram Stain | Mantoux / Tuberculin Sensitivity Test | Culture -Aerobic Paediatric Blood-Bactec | Culture, Sputum | Culture, Urine | Culture, Aerobic Blood -Bactec | Genexpert Ultra MTB/RIF | Culture, Semen | Culture Aerobic, Pus | Ante Natal Profile Basic | Diabescreen | Fever Panel- 1 | Renal Profile | Lipid Profile Direct | Healthkind Advance | Healthkind Platinum | Liver & Kidney Profile | Liver Function Extended Panel | Basic Liver Panel | Lipid Profile | Fever Panel | Fever Panel Basic | Kidney Profile (KFT) | ANC Panel | Pre Operative Panel | Vitamin D Panel | LBC + HPV | Fertikind Complete | Healthkind Complete | Lipid Screen | Healthkind Lite | Healthkind Active | Fever Screen | Ante Natal Profile 1 | Healthkind Total | Healthkind Screen | Fertikind Total | Liver Function Test (LFT) | Surgical Profile | Anti Streptolysin O (ASO), Quantitative | C-Reactive Protein (CRP), Quantitative | Dengue Duo Rapid Test |
- Book a Test
- Upload Prescription
- Download Report
- Health Packages
- Lab Locator
Partner with us
- Franchise Opportunities
- Corporate Wellness
- Hospital Lab Management
- Organise Camps
- National Reference Lab
- Research and Development
- Download Forms
- Scientific Literature
- Mission & Vision
- Disclosures
- Get in touch
- Share Your Feedback
Download App

- Terms of Use
- Franchising Opportunities
- Privacy Policy
Get in Touch
- Call Us: 75000 75111
- Mail Us: [email protected]
© 2024 Pathkind Diagnostics Pvt. Ltd. All Rights Reserved | Unsubscribe
- Radiology Test Available only in Kolkata & Gurgaon
Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Health Encyclopedia
Pregnancy: how your digestion changes, what is digestion.
Food and drink must be changed into smaller molecules of nutrients to be absorbed into the blood and carried to cells throughout the body. Digestion is the process of breaking down food and drink into smaller parts so that the body can use them to build and nourish cells, and to provide energy.
How does the digestive process work?
Digestion involves:
The mixing of food with digestive juices
The movement of food through the digestive tract
A chemical breakdown of large molecules of food into smaller molecules. The body can then use them to nourish cells and provide energy. This happens by a process called absorption. It occurs mostly in the small intestine.
Digestion begins in the mouth, where food and drink are taken in. It ends in the small intestine.
What makes up the digestive system?
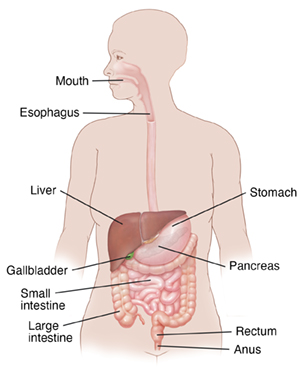
The digestive tract is a series of organs joined in a long, twisting tube from the mouth to the anus. It consists of:
Small intestine
Large intestine
Organs that help with digestion but are not part of the digestive tract include:
Glands in the mouth that make saliva
Gallbladder
Parts of other organ systems, such as nerves and blood, also play a major role in the digestive process.
How does food move through the digestive system?
Muscles move food and liquid along the digestive tract in a wave-like movement called peristalsis.
What changes occur in the digestive system during pregnancy?
Pregnancy hormones can affect the digestive system. The hormone progesterone, which causes smooth muscle relaxation, often causes relaxation and slowing of digestion in the stomach and the small and large intestines. The gallbladder is also affected with delayed emptying. That can increase the chances of gallstone formation. Many of the digestive discomforts of pregnancy, such as morning sickness (nausea or vomiting), constipation, and heartburn, are all related to the relaxed tone and slowed action of the digestive system.
The growing uterus itself can affect the digestive system. As the uterus grows, it can press on or even block parts of the digestive tract. This can lead to slowed movement of food and constipation. Increasing fluids, regular exercise, and increasing the fiber in your diet are some of the ways to prevent constipation. Always ask your healthcare provider before taking any medicine for this condition.
Many women have appetite changes in pregnancy, such as:
Increased hunger
Decreased appetite
Nausea and vomiting
A few women develop pica, a rare craving to eat things other than food. This includes things like dirt, clay, ice, raw rice, flour, starch, or coal. The craving may mean there is a nutritional deficiency, such as not enough iron in the body.
Medical Reviewers:
- Donna Freeborn PhD CNM FNP
- Heather M Trevino BSN RNC
- Irina Burd MD PhD
- Ask a Medical Librarian Make an Appointment Physicians & Services Physicians who provide Maternal Fetal Care
Managing GERD During Pregnancy: Causes, Symptoms, and Solutions

Pregnancy is a remarkable journey filled with various physical and emotional changes. Among these changes, some women may experience a common yet uncomfortable condition known as Gastroesophageal Reflux Disease (GERD). In this blog article, we'll explore why GERD is common during pregnancy, its potential impact on pregnancy, when symptoms typically appear, how it progresses through trimesters, and what you can do to manage it safely. We'll also discuss the safety of GERD medications during pregnancy, alternative ways to alleviate symptoms, dietary adjustments, nighttime GERD management, when to seek medical advice, and whether GERD goes away after pregnancy.
Why is GERD Common During Pregnancy?
Gastroesophageal Reflux Disease, or GERD, is a digestive disorder characterized by the backflow of stomach acid into the esophagus. During pregnancy, several factors contribute to the prevalence of GERD:
1. Hormonal Changes: One of the primary reasons for GERD during pregnancy is hormonal fluctuations. Increased levels of the hormone progesterone cause the muscles that control the lower esophageal sphincter (LES) to relax. When this happens, it becomes easier for stomach acid to flow back into the esophagus, leading to heartburn and other GERD symptoms.
2. Pressure on the Abdomen: As the baby grows, the uterus exerts pressure on the stomach, pushing its contents upwards. This pressure can force stomach acid into the esophagus, causing discomfort.
3. Relaxation of Digestive Muscles: In addition to the LES, the muscles responsible for propelling food through the digestive tract may also become more relaxed due to pregnancy hormones. This can slow down digestion and increase the likelihood of acid reflux.
Can GERD Affect Pregnancy?
GERD itself typically doesn't directly affect the pregnancy or the developing fetus. However, it can cause significant discomfort and disrupt sleep, which may indirectly impact a pregnant woman's overall well-being and quality of life. Severe and untreated GERD can lead to complications like esophagitis or Barrett's esophagus, but these are relatively rare during pregnancy.
When Do GERD Symptoms Typically Appear During Pregnancy?
GERD symptoms can appear at any time during pregnancy, but they are most common in the second and third trimesters. This is when the uterus expands significantly, exerting more pressure on the stomach and promoting the relaxation of the LES.
Will GERD Get Worse During the Second or Third Trimester?
For many pregnant women, GERD symptoms tend to worsen as pregnancy progresses, especially during the second and third trimesters. The combination of hormonal changes, increased abdominal pressure, and slower digestion can intensify symptoms. However, the severity of GERD can vary widely among individuals, and not all pregnant women experience worsening symptoms.
If I Had GERD Before, Will It Get Worse During Pregnancy?
If you had GERD before becoming pregnant, you may be at a higher risk of experiencing more pronounced symptoms during pregnancy. However, the severity of GERD during pregnancy can still vary from woman to woman. It's essential to communicate with your healthcare provider about your pre-existing condition, as they can guide managing GERD while pregnant.
Are GERD Drugs Safe to Take During Pregnancy?
Managing GERD during pregnancy often involves lifestyle modifications and dietary changes as the first line of defense. However, in some cases, your healthcare provider may recommend medications to relieve severe symptoms. While the safety of any medication during pregnancy should be discussed with a healthcare professional, certain medications for GERD, like antacids and H2 blockers, are generally considered safe for short-term use during pregnancy. Proton pump inhibitors (PPIs) should be used with caution and only under the guidance of a healthcare provider due to potential concerns about long-term use and fetal development.
Can GERD Medications Cause Birth Defects?
The safety of medications during pregnancy is a crucial concern. Studies on the use of antacids and H2 blockers in pregnancy have not shown a significantly increased risk of birth defects. However, as with any medication during pregnancy, it's essential to consult your healthcare provider before starting or continuing any treatment.
What Are Other Ways to Reduce GERD During Pregnancy?
Managing GERD during pregnancy often involves a combination of lifestyle changes and home remedies. Here are some effective strategies to reduce GERD symptoms:
1. Elevate Your Upper Body: Sleeping with your upper body elevated can help prevent nighttime reflux. Consider using extra pillows or a wedge pillow to prop yourself up.
2. Eat Smaller, Frequent Meals: Large meals can put more pressure on your stomach, leading to acid reflux. Opt for smaller, more frequent meals throughout the day.
3. Avoid Trigger Foods: Identify foods that trigger your GERD symptoms and avoid them. Common triggers include spicy foods, citrus fruits, caffeine, and fatty or fried foods.
4. Stay Upright After Meals: Don't lie down immediately after eating. Instead, remain upright for at least two hours to allow your food to digest properly.
5. Maintain a Healthy Weight: Excess weight can exacerbate GERD symptoms. Maintaining a healthy weight through regular exercise can help alleviate symptoms.
6. Chew Gum: Chewing sugarless gum after meals can stimulate saliva production, which can help neutralize stomach acid.
7. Consider Herbal Remedies: Some herbal remedies, such as ginger or chamomile tea, may provide relief from GERD symptoms. Consult with your healthcare provider before using herbal supplements during pregnancy.
What Foods Help with Acid Reflux During Pregnancy?
While certain foods can trigger GERD symptoms, others may help alleviate them. Consider incorporating these GERD-friendly foods into your pregnancy diet:
1. Oatmeal: Oatmeal is a low-acid, high-fiber option that can soothe the stomach.
2. Ginger: Ginger, in various forms such as ginger tea or ginger candies, may help relieve nausea and indigestion.
3. Bananas: Bananas are low in acid and can provide a soothing effect on the esophagus.
4. Yogurt: Opt for plain, low-fat yogurt to help balance stomach acid.
5. Vegetables: Non-acidic vegetables like broccoli, carrots, and green beans are gentle on the stomach.
6. Lean Proteins: Skinless poultry, fish, and lean cuts of meat are less likely to trigger GERD symptoms.
7. Whole Grains: Whole grains like brown rice and whole wheat bread can be less irritating to the esophagus.
How to Reduce GERD at Night During Pregnancy
Nighttime GERD can be particularly disruptive to sleep. To minimize nighttime symptoms, try these tips:
1. Elevate Your Upper Body: As mentioned earlier, use pillows or a wedge pillow to raise your upper body while sleeping.
2. Sleep on Your Left Side: Sleeping on your left side can help prevent stomach acid from flowing back into the esophagus.
3. Avoid Late-Night Eating: Finish your meals at least two to three hours before bedtime to allow for digestion.
4. Stay Hydrated During the Day: Sip fluids throughout the day to stay hydrated, but limit your intake in the evening to reduce the risk of nighttime reflux.
5. Relaxation Techniques: Practice relaxation exercises like deep breathing or meditation to reduce stress, which can exacerbate GERD symptoms.
When to See a Doctor
While many pregnant women experience mild GERD symptoms that can be managed with lifestyle changes, it's essential to seek medical advice if:
1. Your symptoms are severe or persistent.
2. You're losing weight unintentionally.
3. You have difficulty swallowing or experience pain when swallowing.
4. You notice blood in your vomit or stool.
5. You have asthma or other respiratory problems alongside GERD symptoms.
6. Over-the-counter antacids or lifestyle changes don't provide relief.
Your healthcare provider can evaluate your condition and recommend appropriate treatment options, including safe medications if necessary.
Does GERD Go Away After Pregnancy?
The good news is that GERD symptoms often improve or resolve after pregnancy. As your hormonal levels return to normal and your uterus shrinks back to its pre-pregnancy size, the factors contributing to GERD during pregnancy diminish. However, if you continue to experience GERD symptoms postpartum, it's advisable to consult with a healthcare provider for further evaluation and guidance on long-term management.
Managing GERD during pregnancy involves understanding why it occurs, recognizing its potential impact on pregnancy, and adopting strategies to alleviate symptoms safely. While GERD can be uncomfortable, it's usually a temporary condition that improves after childbirth. By making lifestyle modifications, watching your diet, and consulting with your healthcare provider when needed, you can navigate your pregnancy journey with greater comfort and ease. Remember that every pregnancy is unique, so it's essential to tailor your GERD management plan to your specific needs and circumstances.
Complete Healthcare for Women - Obstetrics and Gynecology
509-392-6700
Richard Lorenzo, D.O.
Kortney Jones ARNP

You Might Also Enjoy...

Ensuring Women's Health and Well-being: The Role of Complete Healthcare for Women in Richland, WA

Hysterectomy for Treatment of Heavy Vaginal Bleeding

Fertility and Pregnancy After 35


Prevention is Key: Managing Vaginitis in Women's Health

Long Term Birth Control Options for Women

Heavy menstrual bleeding is a common problem that affects many women.
- Set your location
- Change your location
- to see results near you
- Set Your Location
- Clear Location
- Set my preferred location
- Change my preferred location
- to show options closest to me
- Set Your location
Suggested Searches
- Online Bill Pay
- Weight Control
- Maternity Tours
- Nursing Jobs
Common Digestive Issues that Occur During Pregnancy

Pregnancy is a time when a woman’s body goes through many physical and physiological changes. Not only does her anatomy change to accommodate the growing fetus, but her hormone levels shift as well. In many cases, these changes produce digestive issues. While they typically aren’t dangerous to the mother or her unborn baby, they can be very unpleasant. Fortunately, there are steps a woman can take to prevent, minimize or eliminate the symptoms.
If you’re pregnant, it’s likely that you’ll encounter one or more of the gastrointestinal (GI) conditions below.
Nausea and vomiting
In the first trimester of pregnancy, 50-80 percent of women experience nausea and vomiting. Also known as “morning sickness,” the condition is very common early in a pregnancy but typically subsides by the second trimester. If it doesn’t, you should talk with your doctor. A rare but more serious condition called hyperemesis gravidarum can cause severe nausea and vomiting that affects your electrolytes. It may require medical treatment.
With common morning sickness, typically no treatment is needed. You can minimize your symptoms by:
- Eating smaller meals more often
- Cutting back on fatty foods and fresh vegetables, as they slow the rate at which food leaves the stomach
- Drinking plenty of water
- Getting adequate amounts of vitamin B1 and vitamin B6
Also known as gastroesophageal reflux disease (GERD), heartburn affects approximately half of women by the time they reach the third trimester. The burning sensation in the chest that occurs after eating is the result of stomach acid backing up into the esophagus. Hormonal changes that relax the sphincter at the top of the stomach and pressure from the growing fetus make GERD more common in pregnancy.
To prevent or decrease heartburn symptoms:
- Eat smaller meals more often
- Don’t recline soon after eating
- Use antacids
- Use over-the-counter medications like H2 blockers or proton pump inhibitors, as directed by your doctor
Constipation
Approximately 40 percent of women experience constipation during their pregnancy. This occurs because hormonal changes slow the movement of food through the lower GI tract, allowing the body to absorb more water from the stool and making it more difficult to pass.
To prevent or relieve constipation, you can:
- Increase your water intake
- Eat foods high in fiber
- Take an over-the-counter stool softener
- Take an over-the-counter laxative, if constipation is severe
Diarrhea is defined as three or more bowel movements per day. Approximately 35 percent of women will experience this condition at some point in their pregnancy. It’s typically related to an infection and resolves on its own in a few days.
If you develop diarrhea, be sure to:
- Consume plenty of water to prevent dehydration
- Contact your doctor if it’s accompanied by increased vaginal discharge of mucus or low back pain, as these can be indicators of preterm labor
GI issues can take some of the joy out of being pregnant. But by taking steps to address any issues that arise, and getting advice from your doctor as needed, you can spend more of your time free of symptoms.
Baptist’s Patient-Centered Maternity Care Focuses on You . Baptist Health has a passion for helping moms live out the positive labor and delivery experience they imagine. Across eight locations in Kentucky and southern Indiana, each of our facilities offers unique innovations that help the families in our care realize that reality.
Learn More.
- Digestive Health
- Mother Baby Care
- Digestive Problems
- Digestive System
Related Blog Articles

Why Is My Poop Green?

Early Pregnancy: Diet Tips and Managing Symptoms in the First Trimester

Is Getting COVID-19 While Pregnant Harmful to Baby?
Let's Stay in Touch
Sign up to receive Baptist Health emails to learn more about your health from our blog, e-newsletter, and Flourish. Or follow one of our social media accounts.
- The Clinic at Christie
- The Clinic at Ossington

5 Ways To Deal With Digestive Issues During Pregnancy
Have you been experiencing constipation, nausea, or heartburn since becoming pregnant?
That is a normal experience as digestive issues are very common during pregnancy. Thankfully, there are ways to mitigate an upset digestive system. Here are 5 go to tips to help with your new symptoms:
1. Eat smaller, more frequent meals
Instead of eating three big meals a day, try eating smaller amounts frequently. This can help prevent you from being overly full at each meal, which can exacerbate nausea.
2. Prioritize movement
Movement is important during pregnancy for many reasons, but it can also be really helpful in managing constipation. Doing a couple of brisk walks a day, even for just 20 minutes or so can help improve your digestion.
3. Focus on fiber-rich foods
It’s okay to eat refined carbohydrates such as crackers, white bread, and pasta in moderation during pregnancy, but they are quite low in dietary fiber and can make constipation worse. Try including fiber-rich sources of carbohydrates such as oats, quinoa, whole grain crackers, brown rice, sweet potatoes, and fresh fruit instead.
4. Swap leafy greens for root vegetables
During pregnancy, leafy greens and raw vegetables are no longer appealing due to nausea and food aversions. Instead, opt for root vegetables, as these are generally easier to tolerate when nauseous.
6. Slow down at meal time
Slowing down at meals and thoroughly chewing your food can help your food digest more efficiently.
Experiencing digestive issues or other pregnancy concerns? Book a complimentary session with one of our dietitians or Naturopathic doctors at The Clinic .
Indigestion and heartburn in pregnancy
Indigestion, also called heartburn or acid reflux , is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach.
You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
Symptoms of indigestion and heartburn
Symptoms of indigestion and heartburn include:
- a burning sensation or pain in the chest
- feeling full, heavy or bloated
- burping or belching
- feeling or being sick
- bringing up food
Symptoms usually come on soon after eating or drinking, but there can sometimes be a delay between eating and getting indigestion.
You can get symptoms at any point during your pregnancy, but they are more common from 12 weeks onwards.
Things you can do to help with indigestion and heartburn
Changes to your diet and lifestyle may be enough to control your symptoms, particularly if they are mild.
Eat healthily
You're more likely to get indigestion if you're very full.
If you're pregnant, it may be tempting to eat more than you would normally, but this may not be good for you or your baby.
Find out more about a healthy diet in pregnancy and foods to avoid in pregnancy .
Change your eating and drinking habits
You may be able to control your indigestion with changes to your eating habits.
It can help to eat small meals often, rather than larger meals 3 times a day, and to not eat within 3 hours of going to bed at night.
Sit up straight when you eat and just after eating. This will take the pressure off your stomach.
Cutting down on drinks containing caffeine, and foods that are rich, spicy or fatty, can also ease symptoms.
Sleeping position
Propping your head and shoulders up when you go to bed can stop stomach acid coming up while you sleep.
Sleeping on your left side can also help.
Stop smoking
Smoking when pregnant can cause indigestion, and can seriously affect the health of you and your unborn baby.
When you smoke, the chemicals you inhale can contribute to your indigestion. These chemicals can cause the ring of muscle at the lower end of your gullet to relax, which allows stomach acid to come back up more easily. This is known as acid reflux.
Smoking also increases the risk of:
- your baby being born prematurely (before week 37 of your pregnancy)
- your baby being born with a low birthweight
- sudden infant death syndrome (SIDS) , or "cot death"
There's lots of help available to stop smoking. Talk to your midwife or call the NHS Smokefree helpline on 0300 123 1044.
Find out more about stopping smoking in pregnancy
Avoid alcohol
Drinking alcohol can cause indigestion. During pregnancy, it can also lead to long-term harm to the baby. It's safest to not drink alcohol at all in pregnancy.
Find out more about alcohol and pregnancy
When to get medical help
See your midwife or GP if you need help managing your symptoms or if changes to your diet and lifestyle do not work. They may recommend medicine to ease your symptoms.
You should also see your midwife or GP if you have any of the following:
- difficulty swallowing
- a hoarse voice
- a cough that does not get better or keeps coming back
- swollen glands on each side of your neck
- weight loss
- pain or swelling in your stomach
Your midwife or GP may ask about your symptoms and examine you by pressing gently on different areas of your chest and stomach to see whether it's painful.
If you're taking prescription medicines
Speak to your GP if you're taking medicine for another condition, such as antidepressants, and you think it may be making your indigestion worse. They may be able to prescribe an alternative medicine.
Never stop taking a prescribed medicine unless you're advised to do so by your GP or another qualified healthcare professional who's responsible for your care.
Medicines for indigestion and heartburn
Medicines for indigestion and heartburn during pregnancy include:
- antacids to neutralise the acid in your stomach – you can get some types from a pharmacist (tell them you're pregnant as some antacids are not suitable during pregnancy)
- alginates to relieve indigestion caused by acid reflux by stopping the acid in your stomach coming back up your gullet
You may only need to take antacids and alginates when you start getting symptoms. However, your GP may recommend taking them before symptoms come on – for example, before a meal or before bed.
Do not take antacids within 2 hours of taking folic acid or iron supplements. Antacids can stop these supplements from being absorbed by your body.
If antacids and alginates do not improve your symptoms, your GP may prescribe another medicine to reduce the amount of acid in your stomach.
Causes of indigestion in pregnancy
You get symptoms of indigestion when the acid in your stomach irritates your stomach lining or gullet. This causes pain and a burning feeling.
When you're pregnant, you're more likely to have indigestion because of:
- hormonal changes
- the growing baby pressing on your stomach
- the muscles between your stomach and gullet relaxing, allowing stomach acid to come back up
You may be more likely to get indigestion in pregnancy if:
- you had indigestion before you were pregnant
- you've been pregnant before
- you're in the later stages of pregnancy
Video: Eating well on a budget
In this video, a dietitian gives advice on how to eat healthily on a budget.
Page last reviewed: 14 November 2023 Next review due: 14 November 2026
- Conditionally
- Newsletter Signup
Health Conditions Chevron
Sexual and Reproductive Health Chevron
Pregnancy Chevron
- Constipation
6 Gastrointestinal Issues That Can Affect You During Pregnancy
By Korin Miller

Pregnancy can make your body feel like a foreign landscape, including when it comes to gastrointestinal issues ...oh, the gastrointestinal issues. Where do we even begin?
If you want to have a baby, these changes can feel totally worth it. Still, it’s nice to have a heads up about what’s in store and whether or not what you’re going through is considered normal. Here are the gastrointestinal issues you might develop during pregnancy, plus what you can do about them.
1. Nausea and vomiting
Shocker, we know. These are probably the most common gastrointestinal issues people experience during the earlier stages of pregnancy, Heather Beall, M.D., an ob/gyn at Northwestern Medicine McHenry Hospital, tells SELF. This is usually not harmful to the pregnancy , but isn’t exactly a delightful experience.
You’ve probably heard this referred to as “ morning sickness ,” but the American College of Obstetricians and Gynecologists (ACOG) points out that it can happen during any part of the day (or night). And, while nausea and vomiting usually start before the 9th week of pregnancy and go away by 14 weeks, for some people, they last the whole pregnancy.
Nausea and vomiting in pregnancy seem to happen thanks to pregnancy hormones like human chorionic gonadotropin (hCG), which rises sharply in the first few weeks of pregnancy , Jennifer Aquino, M.D., an ob/gyn at NYU Langone Health, tells SELF. “High hCG levels can contribute to the process of nausea and vomiting,” she says. Estrogen, another hormone that increases during pregnancy, may also cause morning sickness, the Mayo Clinic says.
If you’re dealing with this, there are a few things you can do. Eating bland foods like dry toast or crackers can help, along with drinking plenty of fluids, avoiding smells that bother you, and having small, frequent meals instead of larger ones, ACOG says. If lifestyle tweaks don’t work, your doctor may recommend taking vitamin B6, vitamin B6 with doxylamine (a medication found in OTC sleep aids), or a drug that combines both. (Both drugs—taken together or apart—have been found to be safe during pregnancy, ACOG says, though experts aren’t sure exactly how they may prevent morning sickness.)
If your nausea and vomiting are bad enough to cause severe dehydration or make you lose more than 5 percent of your pre-pregnancy body weight, you may have hyperemesis gravidarum , which is essentially an extreme, potentially debilitating version of morning sickness. If your nausea and vomiting are really impacting your life, see your doctor. They may prescribe antiemetic drugs to control your symptoms.
2. Constipation
Constipation can certainly be an issue during pregnancy. This is due to the hormone progesterone , Kyle Staller, M.D., a gastroenterologist at Massachusetts General, tells SELF. “That changes how the colon contracts and, as a result, people get slower colonic motility,” he says. Basically, food moves through your colon at a slower rate than usual, which can lead to build-up, harder-than-usual poops, and trouble going as often as you used to.

By Jenna Ryu

By Maressa Brown
By Julia Sullivan
Later in your pregnancy, the pressure from your uterus and growing baby can press on your rectum, also making it harder than usual to poop, Daniela Jodorkovsky, M.D., a gastroenterologist at NewYork-Presbyterian/Columbia University Irving Medical Center, tells SELF.
If you’re pregnant and are having way too much trouble pooping, dietary tweaks like increasing your fiber intake may help, Dr. Staller says. This nutrient makes your poop softer and easier to expel. You should work your way up to the recommended daily grams for your age over a few weeks, according to the Mayo Clinic . (That’ll likely be between 25 and 28 grams.) Going all in too quickly can result in issues like gas and cramping. Drinking plenty of fluids like water (it helps fiber do its job) and prune juice (it’s fiber-rich , but only try it if you can stomach it) can help, Dr. Jodorkovsky says.
If that doesn’t do the trick, talk to your doctor. Stool softeners are generally considered OK to use during pregnancy —just get your doctor’s OK first.
3. Hemorrhoids
Hemorrhoids are swollen veins in your anus and lower rectum, and you can get them during pregnancy from increased pressure on those areas, the Mayo Clinic says. Straining when you poop (like when you’re constipated) can increase the pressure even more, Dr. Jodorkovsky says.
Hemorrhoids aren’t fun to deal with: They can cause bleeding when you poop, anal swelling, itching, irritation, and pain down there, the Mayo Clinic says.
For relief, you can try methods like soaking in a warm tub or using an OTC hemorrhoid cream, according to the Mayo Clinic . Talk to your doctor before using any medication to make sure the one you’re interested in is safe during pregnancy.
Since constipation can also contribute to hemorrhoids, having more fiber in your diet and drinking plenty of fluids may also help you get relief, Dr. Jodorkovsky says
4. Anal fissures
We hate to put this mental image in your head, but anal fissures are small tears in the thin, delicate lining of your anus, as the Mayo Clinic explains. These can cause pain and bleeding when you poop. This health issue, which should honestly be illegal, can also cause pain that lasts several hours after you poop. Or after you try to, anyway, because you probably won’t be surprised to hear that anal fissures can be a complication of constipation. All that pushing can rip your fragile skin.
If you happen to develop an anal fissure during pregnancy, at least know that it will likely heal in a few days or weeks . Keeping your poop soft enough that you don’t need to strain and irritate the area even further should help, Dr. Staller says. The best ways to do that? Drum roll...try to drink more fluids and increase your fiber intake. Soaking in a warm tub for 10 to 20 minutes can help relax your sphincter (the ring of muscle around the opening of your anus) and may help you to heal faster, the Mayo Clinic says.
5. Acid reflux
Acid reflux happens when acid that should stay put in your stomach goes rogue and flows back into your esophagus, the tube that connects your mouth and stomach, the Mayo Clinic says. This backwash can irritate the lining of your esophagus and cause symptoms like heartburn , chest pain, difficulty swallowing, feeling like there’s a lump in your throat, a chronic cough, laryngitis, and disrupted sleep . As a not-at-all-welcome bonus, heartburn can also cause excessive burping .
This issue progresses into gastroesophageal reflux disease (GERD) if you have mild acid reflux at least twice a week, or if your acid reflux is moderate to severe and happens at least once every seven days, according to the Mayo Clinic .
Acid reflux can happen more frequently during pregnancy because the hormone progesterone causes your esophageal sphincter (which is supposed to keep acid and food in your stomach) to relax, the Mayo Clinic explains. “The growing baby also pushes on the stomach, putting pressure on it, and making acid more likely to go out,” Dr. Staller says.
To help combat this, the Mayo Clinic recommends that you eat small, frequent meals and avoid foods you’ve noticed make your reflux worse. (Common items include spicy or fried foods, citrus fruits, and chocolate, the Mayo Clinic says. Sorry.) Trying not to eat in the three hours before bedtime can also help, because lying down makes it easier for that acid to creep up.
6. Gallstones
Gallstones are hardened deposits of digestive fluid that can form in your gallbladder, a small, pear-shaped organ on the right side of your abdomen just beneath your liver, the Mayo Clinic says. Your gallbladder holds a digestive fluid called bile that's released into your small intestine to help with the crucial task of breaking down your food.
You can have gallstones and not know it, or you can have intense symptoms like sudden and severe pain in the upper right or center portion of your abdomen, pain between your shoulder blades, pain in your right shoulder, or nausea and vomiting. The pain can last anywhere from several minutes to a few hours, the Mayo Clinic says.
There are a few reasons why you might have gallstones during pregnancy. One is that estrogen tends to increase the production of HDL cholesterol , which is a component of bile, Dr. Aquino says. At the same time, progesterone slows the rate at which your gallbladder empties , she says. “This combination can ultimately cause changes in bile consistency, resulting in gallstones in pregnancy,” she says.
If you’re having pain or any other symptoms that you suspect are due to gallstones, talk to your doctor as soon as possible. They may give you medication to try to manage the pain, Dr. Staller says. Surgery to remove the gallbladder is also a common treatment for this issue and is generally safe during pregnancy .
Your body can do weird things when you’re pregnant. If your gut is quite literally telling you something is off, don’t hesitate to call your doctor, Dr. Beall says. They’re there to help.
- Gastroenterologists Share 7 Things to Do When You Have Painful Gas
- This Is How You’ll Know It’s Time to See a Doctor for Constipation
- 7 Fascinating Ways Your Boobs Can Change During Pregnancy

SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional.

For Appointments Call : +91 - 8081998800
Smiles Gastroenterology
Best Fissure, Fistula & Piles Treatment in Bangalore
Common Gastrointestinal Issues During Pregnancy
Published On - 26/04/2021
Are you experiencing Gastrointestinal issues?
Gastrointestinal (GI) issues are the most frequent problems during pregnancy. This is due to GI problems affecting the gastrointestinal tract, primarily the esophagus, stomach, and intestines. Additionally, hormonal changes during pregnancy can also contribute to digestive problems and other GI functions.
Some women may experience GI disorders that develop after becoming pregnant. Others have chronic gastrointestinal diseases prior to pregnancy that requires special consideration during pregnancy. Understanding the prevalence of various GI issues during pregnancy is necessary to optimize care.
Therefore, SMILES, in this article focuses on the most common symptoms of GI disorders during pregnancy, its causes, and the ways to manage them.
What are the symptoms of Gastrointestinal issues during pregnancy?
Because there is a wide range of gastrointestinal disorders, the symptoms may vary. Some of them include:
1. Nausea and Vomiting
In fact, nausea is one of the earliest symptoms of pregnancy in the first semester that can often be accompanied by vomiting . In rare cases, it is referred to as morning sickness, however, it can become severe and require immediate treatment to manage.
2. Diarrhoea
Diarrhoea is a common condition during pregnancy that causes loose or watery stools caused by viruses or bacteria. This can also be caused by certain medications. While diarrhoea is common and generally not serious, the patient should consult a doctor if experiencing blood of mucus in stool.
3. Constipation
Constipation is having an infrequent bowel movement or having hard to pass bowel movements. It is generally described as having fewer than three bowel movements a week. The pressure from the enlarging uterus on the rectum and lower part of the intestines may cause constipation.
4. Heartburn
Heartburn affects many pregnant women due to increased progesterone, the hormone that relaxes muscles, also relaxes the stomach valve that keeps acid out of the esophagus. Moreover, the growing uterus crowds the stomach, forcing acid into the esophagus.
5. Bloating
Bloating, a build-up of gas in the stomach and intestines may occur during early pregnancy. This is due to the excess gas production and hormonal changes that occur during pregnancy, which slows down the digestive system. Bloating can cause pain, discomfort, and a stuffed feeling in the upper abdomen.
6. Gallstones
A gallstone is a collection of extra cholesterol and bile acids that form a stone in the gallbladder. Pregnant women are at increased risk of gallstones due to the increased estrogen levels – says Dr. Parameshwara, one of the best gastroenterologists in Bangalore. Gallstones, if left untreated can cause the gallbladder to become infected.
What causes GI issues during pregnancy?
While many gastrointestinal problems are very common during pregnancy, women may not have experienced any before. Some of the common causes of gastrointestinal conditions during pregnancy can include:
- ● Changes in hormones
- ● Obesity or overweight
- ● Certain medications
- ● Poor nutrition
- ● Thyroid problems
- ● Lack of physical exercise
- ● Ove usage of laxatives
- ● Viral or bacterial infections
- ● Food intolerance or allergies
How GI disorders during pregnancy be treated?
Gastrointestinal diseases are very common during pregnancy, but they do not cause serious health complications. Most gastrointestinal infections caused by virus or bacteria normally resolves in a few days.
The experts of gastroenterology at SMILES recommend some home remedies that help manage GI issues.
1. Eat a healthy diet
Increase the amount of fiber in your diet. Avoid sugary foods and processed foods. Limit caffeine and dairy products in your daily intake.
2. Drink lots of fluids
Certain GI issues can cause dehydration and so increase the amount of fluids you take in, including water and juices. It helps improves digestion and keeps your GI tract moving regularly.
3. Exercise
Regular exercise boosts blood circulation to the internal organs which help bowels to move smoothly. So, aim for at least 30 minutes of moderate exercise a day. Speak to your doctor and find the best workouts that are safe during pregnancy.
4. Medication
If your symptoms of GI diseases are persistent and unmanageable, you may be recommended medications which include antacids, digestive enzymes, antidiarrheals, and GI stimulants, etc.
When to see a doctor?
You should consult with your gastrointestinal specialist and seek immediate medical care if you have any of the following digestive symptoms.
- ● Heartburn that persists and/or becomes more severe.
- ● A sensation of food caught in your chest or throat
- ● The discomfort that interferes with daily activities
- ● Unusual abdominal pain
- ● Extreme fatigue
- ● Dramatic weight loss
- ● Persistent diarrhea or constipation
Need more information about gastrointestinal diseases during pregnancy?
Schedule an appointment with our top gastroenterologists at SMILES.
Digestive Problems During Pregnancy

Constipation, hemorrhoids, indigestion, heartburn, flatulence and belching are all part of the fun of pregnancy. There's nothing to be embarrassed about here—it's a fact of life. Here's a breakdown of some of the issues you might experience.
More: Pooping and Pregnancy: a Step-by-Step Guide
Constipation
Most of the digestive problems of pregnancy begin with constipation . This condition is universally common in pregnant women for many reasons:
- The high level of certain hormones during pregnancy relaxes the muscles of the bowels and makes it hard for them to work efficiently.
- The growing uterus presses on the bowel and disrupts normal function.
- The iron in your vitamin supplement is known to make stools dry and difficult to pass.
Just because constipation is common in pregnancy, doesn't mean you have to accept it. You can do many things to avoid constipation, including the following:
- Drink lots of fluids. Water and fruit juices soften stools and keep digested waste passing through the bowel. (Prune juice is a powerful constipation zapper!)
- Eat fiber-rich foods . Certain foods are especially good at keeping stools soft and at making sure they pass easily through the bowel. These foods include many of the highly nutritious foods recommended for a healthy diet during pregnancy: fruits, vegetables, whole grains and legumes (beans and peas).
- Limit sugary, processed foods. They are binding.
- Exercise. Not only does exercise keep your muscles in shape, it boosts blood circulation and brings more oxygen to all organs (including the bowels) to help them do their jobs more efficiently.
When you are constipated, don't take a laxative. Not only can it wash necessary nutrients out of your system, it might be harmful to your baby. Talk to your doctor before taking any medicated remedy for constipation.
More: The Benefits of Exercise During Pregnancy
Hemorrhoids are a mass of swollen tissue at the opening of the rectum (where stools exit the body).

Hemorrhoids
Straining during a bowel movement to pass hard stools can cause hemorrhoids. These are varicose veins of the rectum that are sometimes called "piles" because they look like piles of small peas.
If you see blood on your tissue when you wipe after a bowel movement, or if you have pain or excessive itching at the opening of the rectum, ask your doctor to check for hemorrhoids. (This might seem embarrassing, but it's nothing he or she hasn't seen before.) If you have hemorrhoids, they will accompany you through the pregnancy and will probably get worse during the pushing stage of delivery. If you take good care of them, however, they might disappear after the birth.
The following tips should help keep these piles from piling up, and if you don't have them yet, these tips will help you prevent them:
- Avoid constipation. Use all the tips mentioned above to keep your stools soft and moving easily through your bowel.
- Try not to strain during bowel movements.
- Put your feet up on a small stool during bowel movements to make the movement easier.
- Don't read on the toilet. If you get into a good story, you'll sit there longer than necessary; this puts unnecessary strain on the anus.
- Avoid standing still or sitting for very long periods of time. Move around, change position.
If you are bothered by the pain or itching of hemorrhoids, take action. You can use topical creams that are sold in pharmacies to ease the pain and itching. You might also try applying a compress of witch hazel or ice to the hemorrhoids. If the pain is so bad you can't sit comfortably in a chair, go to your pharmacy and buy a doughnut pillow (this is an inflatable pillow with a hole in the middle so your buttocks don't touch the chair!).
When all else fails, get off your feet and lie down; this relieves the pressure and the pain.
Flatulence and Belching
The problem of flatulence (also known as "passing gas" or "blowing wind") is caused by a buildup of gases in the large intestine. Belching (also called burping) is the sudden expulsion of gases from the stomach. These are common problems during pregnancy that cause more embarrassment than pain or discomfort. Constipation can cause these problems, and so can certain foods .
More: 9 Foods and Beverages to Avoid While Pregnant
If you've been clearing out the room lately with odorous flatulence or belching, avoid constipation and steer clear of known gas producers, such as beans, onions, fried foods, cabbage, broccoli and Brussels sprouts.
Join the Family
Your partner in parenting from baby name inspiration to college planning.

- Pregnancy Week By Week
- Ovulation Calculator
Digestion During Pregnancy

Digestion issues such as diarrhea , constipation , or other issues are very common during pregnancy, though occasionally diarrhea could be a sign of something more serious like food poisoning . As the uterus expands, the pressure moves outward and this causes pressure on the wall of the stomach as well as the pelvic veins. Pressure is also felt on the rib cage and the stomach. While the female body will open up the rib cage to house the new growing fetus, this is not enough to keep the baby from pressing right up against the stomach.
3 stages of digestion during pregnancy
There are three stages of digestion are mouth, stomach, and colon. Each of these three stages is affected by the pregnancy hormones and the weight of the fetus.
In the mouth, an increase in saliva will begin to break down the food much more quickly than before the female was pregnant. The increase in mouth acids is often the cause of bleeding gums and pain in the mouth during pregnancy.
Of all the bodily processes that change during pregnancy, digestion during pregnancy is the only one affected on all three levels.
As the food passes into the stomach, you may notice there is less room than before. This is a common problem in the third trimester of pregnancy. Less room means eating smaller meals more frequently to consume all the calories needed to grow a healthy baby.
The colon is the last stop in digestion. The pregnancy hormone is one reason constipation occurs. The muscles of the body are all relaxed and this includes the muscles of the intestines. Food will move slowly through the last phase of digestion during pregnancy causing some constipation.
Another reason for a slower final step in digestion during pregnancy is the weight of the fetus on the colon. Extra weight means the colon may not be able to empty its contents all the way.
Eating more means more digestion
Despite all of the issues with digestion during pregnancy, the mother's body and the baby will need huge amounts of calories, vitamins, and nutrients. Metabolism will also increase, so mom needs to eat more than she did before she was pregnant to keep development on track for the fetus. Taking a prenatal vitamin at least once a day is important. If digestion during pregnancy is a problem during a specific time of day (like morning sickness), take the prenatal vitamin at another time. It is important to keep the supplement down so the body can use the extra vitamins and nutrients for the baby's growth.
Of all the bodily processes that change during pregnancy, digestion during pregnancy is the only one affected on all three levels. Many digestion problems during pregnancy are common and easily avoidable, but all should be discussed with your doctor.
Read More: Diarrhea Causes and Treatment During Pregnancy Probiotics and Prebiotics During Pregnancy

Pregnancy is an engineering challenge − diagnosing and treating preterm birth requires understanding its mechanics
Professor of Biomedical Engineering, University of Wisconsin-Madison
Professor of Mechanical Engineering, Columbia University
Associate Professor of Biomedical Engineering, Arts & Sciences at Washington University in St. Louis
Disclosure statement
Melissa Skala receives funding from the National Institutes of Health and the National Science Foundation.
Kristin Myers receives funding from the National Institutes of Health, the National Science Foundation, and The Iris Fund.
Michelle L. Oyen receives funding from Wellcome Leap as part of the In Utero program, and from the National Institutes of Health. Michelle is an Associate Fellow of Homerton College, Cambridge.
Arts & Sciences at Washington University in St. Louis and University of Wisconsin–Madison provide funding as members of The Conversation US.
View all partners
Why are babies born prematurely? Researchers still don’t really know.
Obstetricians are very good at managing the process of birth. But when it comes to predicting whether a baby will be born in a timely manner, the science is still catching up . Research on the causes of preterm birth is decades behind that of other conditions such as cancer. That means nurses, doctors, midwives and doulas don’t have the tools and resources they need to do the best job possible when babies are born before 37 weeks of pregnancy .
One of the few known risk factors of preterm birth is whether a pregnant person has previously given birth to a preterm baby. Others include being pregnant with twins, triplets or more, and certain medical conditions such as urinary tract infections, high blood pressure or diabetes. Knowing these risk factors, however, does not always pinpoint the cause of preterm birth.
Progress has been slow in part because much of the research to date on preterm birth has approached pregnancy from the perspective of reproductive biology . That includes the enormous physiological changes across the reproductive, cardiovascular and endocrine systems of the pregnant person, and the influence of hormones and genetics on both parent and fetus.
Yet pregnancy is also an engineering challenge because it involves physical forces. Clinicians are dealing with an average 7-pound (3.2 kg) baby in around 1 liter of amniotic fluid held in place with a membrane less than 1 millimeter thick – all within a uterus that started out the size of a fist. That involves forces, pressures and mechanical loads that all can contribute to maternal, fetal and placental conditions that can trigger preterm birth.
In a paper published over 150 years ago , a physician recognized that birth is a mechanical event. But he was using 19th-century technology to measure the pressure per area on membranes that support pregnancy. Only now do researchers have the mechanical, electrical and computational engineering expertise to address the challenges of preterm birth.
But research on preterm birth is still so early that scientists first must build the tools to study it before they can diagnose and treat it. Our team of researchers is working to do just that.
Many complications can cause preterm birth
It’s hard to narrow down who is at risk of preterm birth because there is no single cause. Preterm birth can be triggered by multiple factors involving the pregnant person, the fetus, the placenta or the fetal membranes attached to the placenta that connect fetus and parent.
Globally, 1 in 10 live births are preterm, or born before 37 weeks of pregnancy. Of these preterm births, about 30% to 40% are caused by premature rupture of the fetal membranes, and another 1% to 9% by the cervix dilating prematurely.
With current technology, preterm births are rarely preventable. Current screening tools to measure the risk of preterm birth are fairly primitive. Doctors use ultrasound to monitor the size and position of the baby, and they touch the cervix to feel whether it is softening, a normal process prior to labor but problematic if it is happening too soon.
If the baby isn’t growing, perhaps because of insufficient blood supply to the placenta, doctors perform preterm C-sections to prevent stillbirth. Preemptive C-sections are also sometimes used to prevent or treat preeclampsia, or dangerously high blood pressure during pregnancy.
In both cases, patients and doctors balance the benefit of an early C-section for the fetus and the parent against the risks associated with preterm birth, including a lifetime of breathing, vision, cardiovascular or other health issues for the child.
The wide variety of factors that play a role in preterm birth make early diagnosis a challenge. But a better core understanding of the biomechanical forces at work during pregnancy can give researchers new places to look for diagnostic clues.
Tackling the challenge from multiple angles
Pregnancy is essentially a physical process , from the uterus stretching to accommodate the baby to the cervix dilating when labor contractions begin and it’s time for the parent to push. And when something mechanical goes wrong, it can lead to tragic results.
For example, maternal risk factors for preterm birth include rupture of the uterus or preeclampsia. The placenta could also detach from the wall of the uterus, causing the parent to bleed to death. Carrying twins comes with additional amniotic fluid and blood volume that adds an extra load to the placenta, which can trigger preterm labor.
Our team of biomechanical and biomedical engineers is working to understand the underlying causes of preterm birth from different angles, all with a view toward diagnosis and intervention.
One of us, Kristin Myers , studies the biology of tissue remodeling to quantify the biomechanics of pregnancy. Her lab creates computer models to measure how the uterus, cervix and fetal membranes work to carry the mechanical loads that pregnancy generates. She and her team use ultrasound to look at how the uterus grows and stretches and how much mechanical load is on the cervix, predicting whether it will fail too soon. Using the uterus as a pressure gauge for the mechanical environment of pregnancy could help identify problems before they occur.
Another of us, Michelle Oyen , studies the physics and materials science of soft tissues focusing on the mechanical properties of the fetal membranes and nutrient transport in the placenta. Her lab, along with Myers’ team, is applying big data and machine learning to anonymized medical records to create digital twins – or computational models of a given patient’s health data – that could help predict how a pregnancy will unfold. This may help physicians treat or avoid pregnancy complications.
Finally, Melissa Skala uses a noninvasive technique called optical coherence tomography . This imaging method produces 3D images of tissues that can’t be captured by ultrasound or MRI, such as extremely thin fetal membranes. Her lab used this technique to study how fetal membranes rupture under different pressures, providing a baseline of information that can be used to build better digital models of fetal membrane stress. Improved imaging of the fetal membranes and cervix can alert physicians to when these structures are at risk of failing.
Better imaging and better models
The Holy Grail of preterm birth prevention is early diagnosis. An early warning checklist for preterm birth risk could help protect the health of both baby and mother.
This checklist could look like your doctor ordering an imaging scan as soon as you find out you’re pregnant to understand the size of your uterus and cervix. Then they might take a swab of vaginal fluid to analyze biological changes in your cervix.
Better modeling techniques would be able to assess how your pregnancy will progress, and more precise imaging tools could measure changes over time. With a better prediction for when labor will start, doctors and patients can make a more informed decision on whether a C-section is necessary.

An accurate early warning checklist for preterm birth is still years away. But researchers in reproductive biology, epidemiology, bioinformatics and engineering are working hard to better understand in greater detail how babies are born and the many complications that can arise along the way, including preterm birth.
We believe that engineering – creative problem-solving using technology – is a critical addition to the multidisciplinary approach needed to address the complexity of preterm birth.
- Biomechanics
- Engineering
- Maternal health
- Bioengineering
- Mechanical engineering
- Preterm birth
- Disease modeling
- Developmental biology
- Childbirth complications

Head of School, School of Arts & Social Sciences, Monash University Malaysia

Chief Operating Officer (COO)

Clinical Teaching Fellow

Data Manager

Director, Social Policy

IMAGES
VIDEO
COMMENTS
3. Diarrhea. Let's face it - diarrhea is the worst. When it lasts just a few days, diarrhea typically is related to an infection (usually gastroenteritis) or eating something that upsets your stomach.Check in with your doctor to determine the best treatment option to reduce dehydration and duration of illness.
Keep crackers, dried fruit or cereal handy for snacking throughout the day. 4. Hydrate. Drinking water is a must to help prevent constipation (as well as hemorrhoids and excessive swelling) during pregnancy, since waste moves through the body more slowly than usual, and needs plenty of water to help keep bowel movements soft.
Nausea and vomiting are common pregnancy digestion issues women face, usually during the first trimester. Traditionally, the medical profession refers to these episodes as "morning sickness," though it can occur at any time of the day. Researchers believe hormonal changes produce these unpleasant sensations. You can treat this condition by:
10 Steps You Can Take to Avoid Stomach Problems During Pregnancy. Here are 10 actionable steps you can employ to prevent stomach problems during pregnancy: Eat Small, Regular Meals -. During pregnancy, your stomach produces more acid and may become more sensitive. When you eat large meals, you put pressure on your stomach and intestines ...
Add prune juice to your diet. Eat more whole-grain foods, fresh fruits, and vegetables. Ask us to recommend a stool softener. Eat 5 or 6 small meals a day instead of 3 big ones. Eat slowly and chew your food well. Steer clear of carbonated beverages. Skip foods that give you trouble. Beans, broccoli, and lettuce are common culprits. Eat 5 or 6 ...
Learn More. Some of the most common gastrointestinal issues women experience during pregnancy are nausea and vomiting, hyperemesis gravidarum, gastroesophageal reflux disease, gallstones, diarrhea, and constipation. Some women may have been diagnosed prior to pregnancy with GI disorders such as Crohn's disease or ulcerative colitis.
Pregnancy hormones can affect the digestive system. The hormone progesterone, which causes smooth muscle relaxation, often causes relaxation and slowing of digestion in the stomach and the small and large intestines. The gallbladder is also affected with delayed emptying. That can increase the chances of gallstone formation.
Relaxation of Digestive Muscles: In addition to the LES, the muscles responsible for propelling food through the digestive tract may also become more relaxed due to pregnancy hormones. This can slow down digestion and increase the likelihood of acid reflux.
Some of the many surprises you might experience during your pregnancy. You can blame a variety of pregnancy hormones for many of these annoying, sometimes embarrassing, symptoms. Here's how to get some relief: Constipation. Drink plenty of water. So important! Add prune juice to your diet. Eat more whole-grain foods, fresh fruits, and vegetables.
Nausea and vomiting. In the first trimester of pregnancy, 50-80 percent of women experience nausea and vomiting. Also known as "morning sickness," the condition is very common early in a pregnancy but typically subsides by the second trimester. If it doesn't, you should talk with your doctor. A rare but more serious condition called ...
That is a normal experience as digestive issues are very common during pregnancy. Thankfully, there are ways to mitigate an upset digestive system. Here are 5 go to tips to help with your new symptoms: 1. Eat smaller, more frequent meals . Instead of eating three big meals a day, try eating smaller amounts frequently.
Indigestion, also called heartburn or acid reflux , is common in pregnancy. It can be caused by hormonal changes and the growing baby pressing against your stomach. You can help ease indigestion and heartburn by making changes to your diet and lifestyle, and there are medicines that are safe to take in pregnancy.
1. Nausea and vomiting. Shocker, we know. These are probably the most common gastrointestinal issues people experience during the earlier stages of pregnancy, Heather Beall, M.D., an ob/gyn at ...
1. Nausea and Vomiting. In fact, nausea is one of the earliest symptoms of pregnancy in the first semester that can often be accompanied by vomiting. In rare cases, it is referred to as morning sickness, however, it can become severe and require immediate treatment to manage. 2.
Causes. Early in pregnancy, the pregnancy hormones interact with hormones that control other body systems, particularly those involved with blood sugar regulation, and this results in feelings of nausea and vomiting. Late in pregnancy, problems with digestion may occur because the uterus takes up most of the space in your abdomen, displacing ...
More: Pooping and Pregnancy: a Step-by-Step Guide. Constipation. Most of the digestive problems of pregnancy begin with constipation. This condition is universally common in pregnant women for many reasons: The high level of certain hormones during pregnancy relaxes the muscles of the bowels and makes it hard for them to work efficiently.
Eat at least 28 grams of fiber every day to improve digestion. Reach for foods that are high in fiber, including beans, whole grains, fruits and vegetables. Consume more probiotic-rich foods, such as yogurt, kefir and sauerkraut. Probiotics are a type of "good" bacteria in the gut that helps fight off the harmful bacteria that contributes ...
Foods to avoid for gastritis during pregnancy. Changes should be made to your dietary habits. Cut out foods that are spicy, fried, acidic, and high in fat content as these can cause gastritis flare-ups. Caffeinated drinks are also culprits, so swap your coffees and sodas with herbal teas and flavored water. Certain dishes like red meat, pork ...
This is because being upright during the initial stages of digestion means that gravity is helping your food move south where it should be going, instead of back up. 3. Focus on fiber-rich foods It can be tempting during pregnancy (especially when you're nauseous) to mostly eat refined carbohydrates such as crackers, white bread, and pasta.
There are three stages of digestion are mouth, stomach, and colon. Each of these three stages is affected by the pregnancy hormones and the weight of the fetus. In the mouth, an increase in saliva will begin to break down the food much more quickly than before the female was pregnant. The increase in mouth acids is often the cause of bleeding ...
Your digestive tract experiences some significant changes during pregnancy. Perhaps the most dramatic occur late in pregnancy when your developing baby compresses your stomach and intestine. Your first trimester, however, isn't without its own share of digestive changes. These are mostly due to hormones, and can lead to a number of symptoms.
HG is a severe form of nausea and vomiting associated with weight loss of more than 5% of pre-pregnant weight, dehydration and electrolyte imbalances. HG usually starts before the 22 nd week of gestation, affects 0.3-2.0% of pregnancies and sometimes requires hospital admission [ 22, 23 ].
Dental problems (Trimesters 1,2,3) fluoridated toothpaste. Your body builds more capillaries (tiny blood vessels) to handle the higher blood volume of pregnancy. These delicate vessels in your gums may bleed when you brush or floss. The pregnancy hormone progesterone dilates blood vessels, which can make gums swell and bleed more than normal.
Yet pregnancy is also an engineering challenge because it involves physical forces. Clinicians are dealing with an average 7-pound (3.2 kg) baby in around 1 liter of amniotic fluid held in place ...