- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Effectiveness of...
Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials
- Related content
- Peer review
- Claire D Madigan , senior research associate 1 ,
- Henrietta E Graham , doctoral candidate 1 ,
- Elizabeth Sturgiss , NHMRC investigator 2 ,
- Victoria E Kettle , research associate 1 ,
- Kajal Gokal , senior research associate 1 ,
- Greg Biddle , research associate 1 ,
- Gemma M J Taylor , reader 3 ,
- Amanda J Daley , professor of behavioural medicine 1
- 1 Centre for Lifestyle Medicine and Behaviour (CLiMB), The School of Sport, Exercise and Health Sciences, Loughborough University, Loughborough LE11 3TU, UK
- 2 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
- 3 Department of Psychology, Addiction and Mental Health Group, University of Bath, Bath, UK
- Correspondence to: C D Madigan c.madigan{at}lboro.ac.uk (or @claire_wm and @lboroclimb on Twitter)
- Accepted 26 April 2022
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care.
Design Systematic review and meta-analysis of randomised controlled trials.
Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary care compared with no treatment, attention control, or minimal intervention and weight change at ≥12 months follow-up.
Data sources Trials from a previous systematic review were extracted and the search completed using the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021.
Data extraction and synthesis Two reviewers independently identified eligible studies, extracted data, and assessed risk of bias using the Cochrane risk of bias tool. Meta-analyses were conducted with random effects models, and a pooled mean difference for both weight (kg) and waist circumference (cm) were calculated.
Main outcome measures Primary outcome was weight change from baseline to 12 months. Secondary outcome was weight change from baseline to ≥24 months. Change in waist circumference was assessed at 12 months.
Results 34 trials were included: 14 were additional, from a previous review. 27 trials (n=8000) were included in the primary outcome of weight change at 12 month follow-up. The mean difference between the intervention and comparator groups at 12 months was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, P<0.001), favouring the intervention group. At ≥24 months (13 trials, n=5011) the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, P<0.001) favouring the intervention. The mean difference in waist circumference (18 trials, n=5288) was −2.5 cm (−3.2 to −1.8 cm, I 2 =69%, P<0.001) in favour of the intervention at 12 months.
Conclusions Behavioural weight management interventions for adults with obesity delivered in primary care are effective for weight loss and could be offered to members of the public.
Systematic review registration PROSPERO CRD42021275529.
Introduction
Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality. 1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19. 4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight. 6
Primary care is an ideal setting for delivering weight management services, and international guidelines recommend that doctors should opportunistically screen and encourage patients to lose weight. 7 8 On average, most people consult a primary care doctor four times yearly, providing opportunities for weight management interventions. 9 10 A systematic review of randomised controlled trials by LeBlanc et al identified behavioural interventions that could potentially be delivered in primary care, or involved referral of patients by primary care professionals, were effective for weight loss at 12-18 months follow-up (−2.4 kg, 95% confidence interval −2.9 to−1.9 kg). 11 However, this review included trials with interventions that the review authors considered directly transferrable to primary care, but not all interventions involved primary care practitioners. The review included interventions that were entirely delivered by university research employees, meaning implementation of these interventions might differ if offered in primary care, as has been the case in other implementation research of weight management interventions, where effects were smaller. 12 As many similar trials have been published after this review, an updated review would be useful to guide health policy.
We examined the effectiveness of weight loss interventions delivered in primary care on measures of body composition (weight and waist circumference). We also identified characteristics of effective weight management programmes for policy makers to consider.
This systematic review was registered on PROSPERO and is reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. 13 14
Eligibility criteria
We considered studies to be eligible for inclusion if they were randomised controlled trials, comprised adult participants (≥18 years), and evaluated behavioural weight management interventions delivered in primary care that focused on weight loss. A primary care setting was broadly defined as the first point of contact with the healthcare system, providing accessible, continued, comprehensive, and coordinated care, focused on long term health. 15 Delivery in primary care was defined as the majority of the intervention being delivered by medical and non-medical clinicians within the primary care setting. Table 1 lists the inclusion and exclusion criteria.
Study inclusion and exclusion criteria
- View inline
We extracted studies from the systematic review by LeBlanc et al that met our inclusion criteria. 11 We also searched the exclusions in this review because the researchers excluded interventions specifically for diabetes management, low quality trials, and only included studies from an Organisation for Economic Co-operation and Development country, limiting the scope of the findings.
We searched for studies in the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021 (see supplementary file 1). Reference lists of previous reviews 16 17 18 19 20 21 and included trials were hand searched.
Data extraction
Results were uploaded to Covidence, 22 a software platform used for screening, and duplicates removed. Two independent reviewers screened study titles, abstracts, and full texts. Disagreements were discussed and resolved by a third reviewer. All decisions were recorded in Covidence, and reviewers were blinded to each other’s decisions. Covidence calculates proportionate agreement as a measure of inter-rater reliability, and data are reported separately by title or abstract screening and full text screening. One reviewer extracted data on study characteristics (see supplementary table 1) and two authors independently extracted data on weight outcomes. We contacted the authors of four included trials (from the updated search) for further information. 23 24 25 26
Outcomes, summary measures, and synthesis of results
The primary outcome was weight change from baseline to 12 months. Secondary outcomes were weight change from baseline to ≥24 months and from baseline to last follow-up (to include as many trials as possible), and waist circumference from baseline to 12 months. Supplementary file 2 details the prespecified subgroup analysis that we were unable to complete. The prespecified subgroup analyses that could be completed were type of healthcare professional who delivered the intervention, country, intensity of the intervention, and risk of bias rating.
Healthcare professional delivering intervention —From the data we were able to compare subgroups by type of healthcare professional: nurses, 24 26 27 28 general practitioners, 23 29 30 31 and non-medical practitioners (eg, health coaches). 32 33 34 35 36 37 38 39 Some of the interventions delivered by non-medical practitioners were supported, but not predominantly delivered, by GPs. Other interventions were delivered by a combination of several different practitioners—for example, it was not possible to determine whether a nurse or dietitian delivered the intervention. In the subgroup analysis of practitioner delivery, we refer to this group as “other.”
Country —We explored the effectiveness of interventions by country. Only countries with three or more trials were included in subgroup analyses (United Kingdom, United States, and Spain).
Intensity of interventions —As the median number of contacts was 12, we categorised intervention groups according to whether ≤11 or ≥12 contacts were required.
Risk of bias rating —Studies were classified as being at low, unclear, and high risk of bias. Risk of bias was explored as a potential influence on the results.
Meta-analyses
Meta-analyses were conducted using Review Manager 5.4. 40 As we expected the treatment effects to differ because of the diversity of intervention components and comparator conditions, we used random effects models. A pooled mean difference was calculated for each analysis, and variance in heterogeneity between studies was compared using the I 2 and τ 2 statistics. We generated funnel plots to evaluate small study effects. If more than two intervention groups existed, we divided the number of participants in the comparator group by the number of intervention groups and analysed each individually. Nine trials were cluster randomised controlled trials. The trials had adjusted their results for clustering, or adjustment had been made in the previous systematic review by LeBlanc et al. 11 One trial did not report change in weight by group. 26 We calculated the mean weight change and standard deviation using a standard formula, which imputes a correlation for the baseline and follow-up weights. 41 42 In a non-prespecified analysis, we conducted univariate and multivariable metaregression (in Stata) using a random effects model to examine the association between number of sessions and type of interventionalist on study effect estimates.
Risk of bias
Two authors independently assessed the risk of bias using the Cochrane risk of bias tool v2. 43 For incomplete outcome data we defined a high risk of bias as ≥20% attrition. Disagreements were resolved by discussion or consultation with a third author.
Patient and public involvement
The study idea was discussed with patients and members of the public. They were not, however, included in discussions about the design or conduct of the study.
The search identified 11 609 unique study titles or abstracts after duplicates were removed ( fig 1 ). After screening, 97 full text articles were assessed for eligibility. The proportionate agreement ranged from 0.94 to 1.0 for screening of titles or abstracts and was 0.84 for full text screening. Fourteen new trials met the inclusion criteria. Twenty one studies from the review by LeBlanc et al met our eligibility criteria and one study from another systematic review was considered eligible and included. 44 Some studies had follow-up studies (ie, two publications) that were found in both the second and the first search; hence the total number of trials was 34 and not 36. Of the 34 trials, 27 (n=8000 participants) were included in the primary outcome meta-analysis of weight change from baseline to 12 months, 13 (n=5011) in the secondary outcome from baseline to ≥24 months, and 30 (n=8938) in the secondary outcome for weight change from baseline to last follow-up. Baseline weight was accounted for in 18 of these trials, but in 14 24 26 29 30 31 32 44 45 46 47 48 49 50 51 it was unclear or the trials did not consider baseline weight. Eighteen trials (n=5288) were included in the analysis of change in waist circumference at 12 months.

Studies included in systematic review of effectiveness of behavioural weight management interventions in primary care. *Studies were merged in Covidence if they were from same trial
- Download figure
- Open in new tab
- Download powerpoint
Study characteristics
Included trials (see supplementary table 1) were individual randomised controlled trials (n=25) 24 25 26 27 28 29 32 33 34 35 38 39 41 44 45 46 47 50 51 52 53 54 55 56 59 or cluster randomised controlled trials (n=9). 23 30 31 36 37 48 49 57 58 Most were conducted in the US (n=14), 29 30 31 32 33 34 35 36 37 45 48 51 54 55 UK (n=7), 27 28 38 41 47 57 58 and Spain (n=4). 25 44 46 49 The median number of participants was 276 (range 50-864).
Four trials included only women (average 65.9% of women). 31 48 51 59 The mean BMI at baseline was 35.2 (SD 4.2) and mean age was 48 (SD 9.7) years. The interventions lasted between one session (with participants subsequently following the programme unassisted for three months) and several sessions over three years (median 12 months). The follow-up period ranged from 12 months to three years (median 12 months). Most trials excluded participants who had lost weight in the past six months and were taking drugs that affected weight.
Meta-analysis
Overall, 27 trials were included in the primary meta-analysis of weight change from baseline to 12 months. Three trials could not be included in the primary analysis as data on weight were only available at two and three years and not 12 months follow-up, but we included these trials in the secondary analyses of last follow-up and ≥24 months follow-up. 26 44 50 Four trials could not be included in the meta-analysis as they did not present data in a way that could be synthesised (ie, measures of dispersion). 25 52 53 58 The mean difference was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, τ 2 =3.38; P<0.001) in favour of the intervention group ( fig 2 ). We found no evidence of publication bias (see supplementary fig 1). Absolute weight change was −3.7 (SD 6.1) kg in the intervention group and −1.4 (SD 5.5) kg in the comparator group.

Mean difference in weight at 12 months by weight management programme in primary care (intervention) or no treatment, different content, or minimal intervention (control). SD=standard deviation
Supplementary file 2 provides a summary of the main subgroup analyses.
Weight change
The mean difference in weight change at the last follow-up was −1.9 kg (95% confidence interval −2.5 to −1.3 kg, I 2 =81%, τ 2 =2.15; P<0.001). Absolute weight change was −3.2 (SD 6.4) kg in the intervention group and −1.2 (SD 6.0) kg in the comparator group (see supplementary figs 2 and 3).
At the 24 month follow-up the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, τ 2 =3.13; P<0.001) (see supplementary fig 4). As the weight change data did not differ between the last follow-up and ≥24 months, we used the weight data from the last follow-up in subgroup analyses.
In subgroup analyses of type of interventionalist, differences were significant (P=0.005) between non-medical practitioners, GPs, nurses, and other people who delivered interventions (see supplementary fig 2).
Participants who had ≥12 contacts during interventions lost significantly more weight than those with fewer contacts (see supplementary fig 6). The association remained after adjustment for type of interventionalist.
Waist circumference
The mean difference in waist circumference was −2.5 cm (95% confidence interval −3.2 to −1.8 cm, I 2 =69%, τ 2 =1.73; P<0.001) in favour of the intervention at 12 months ( fig 3 ). Absolute changes were −3.7 cm (SD 7.8 cm) in the intervention group and −1.3 cm (SD 7.3) in the comparator group.

Mean difference in waist circumference at 12 months. SD=standard deviation
Risk of bias was considered to be low in nine trials, 24 33 34 35 39 41 47 55 56 unclear in 12 trials, 25 27 28 29 32 45 46 50 51 52 54 59 and high in 13 trials 23 26 30 31 36 37 38 44 48 49 53 57 58 ( fig 4 ). No significant (P=0.65) differences were found in subgroup analyses according to level of risk of bias from baseline to 12 months (see supplementary fig 7).

Risk of bias in included studies
Worldwide, governments are trying to find the most effective services to help people lose weight to improve the health of populations. We found weight management interventions delivered by primary care practitioners result in effective weight loss and reduction in waist circumference and these interventions should be considered part of the services offered to help people manage their weight. A greater number of contacts between patients and healthcare professionals led to more weight loss, and interventions should be designed to include at least 12 contacts (face-to-face or by telephone, or both). Evidence suggests that interventions delivered by non-medical practitioners were as effective as those delivered by GPs (both showed statistically significant weight loss). It is also possible that more contacts were made with non-medical interventionalists, which might partially explain this result, although the metaregression analysis suggested the effect remained after adjustment for type of interventionalist. Because most comparator groups had fewer contacts than intervention groups, it is not known whether the effects of the interventions are related to contact with interventionalists or to the content of the intervention itself.
Although we did not determine the costs of the programme, it is likely that interventions delivered by non-medical practitioners would be cheaper than GP and nurse led programmes. 41 Most of the interventions delivered by non-medical practitioners involved endorsement and supervision from GPs (ie, a recommendation or checking in to see how patients were progressing), and these should be considered when implementing these types of weight management interventions in primary care settings. Our findings suggest that a combination of practitioners would be most effective because GPs might not have the time for 12 consultations to support weight management.
Although the 2.3 kg greater weight loss in the intervention group may seem modest, just 2-5% in weight loss is associated with improvements in systolic blood pressure and glucose and triglyceride levels. 60 The confidence intervals suggest a potential range of weight loss and that these interventions might not provide as much benefit to those with a higher BMI. Patients might not find an average weight loss of 3.7 kg attractive, as many would prefer to lose more weight; explaining to patients the benefits of small weight losses to health would be important.
Strengths and limitations of this review
Our conclusions are based on a large sample of about 8000 participants, and 12 of these trials were published since 2018. It was occasionally difficult to distinguish who delivered the interventions and how they were implemented. We therefore made some assumptions at the screening stage about whether the interventionalists were primary care practitioners or if most of the interventions were delivered in primary care. These discussions were resolved by consensus. All included trials measured weight, and we excluded those that used self-reported data. Dropout rates are important in weight management interventions as those who do less well are less likely to be followed-up. We found that participants in trials with an attrition rate of 20% or more lost less weight and we are confident that those with high attrition rates have not inflated the results. Trials were mainly conducted in socially economic developed countries, so our findings might not be applicable to all countries. The meta-analyses showed statistically significant heterogeneity, and our prespecified subgroups analysis explained some, but not all, of the variance.
Comparison with other studies
The mean difference of −2.3 kg in favour of the intervention group at 12 months is similar to the findings in the review by LeBlanc et al, who reported a reduction of −2.4 kg in participants who received a weight management intervention in a range of settings, including primary care, universities, and the community. 11 61 This is important because the review by LeBlanc et al included interventions that were not exclusively conducted in primary care or by primary care practitioners. Trials conducted in university or hospital settings are not typically representative of primary care populations and are often more intensive than trials conducted in primary care as a result of less constraints on time. Thus, our review provides encouraging findings for the implementation of weight management interventions delivered in primary care. The findings are of a similar magnitude to those found in a trial by Ahern et al that tested primary care referral to a commercial programme, with a difference of −2.7 kg (95% confidence interval −3.9 to −1.5 kg) reported at 12 month follow-up. 62 The trial by Ahern et al also found a difference in waist circumference of −4.1 cm (95% confidence interval −5.5 to −2.3 cm) in favour of the intervention group at 12 months. Our finding was smaller at −2.5 cm (95% confidence interval −3.2 to −1.8 cm). Some evidence suggests clinical benefits from a reduction of 3 cm in waist circumference, particularly in decreased glucose levels, and the intervention groups showed a 3.7 cm absolute change in waist circumference. 63
Policy implications and conclusions
Weight management interventions delivered in primary care are effective and should be part of services offered to members of the public to help them manage weight. As about 39% of the world’s population is living with obesity, helping people to manage their weight is an enormous task. 64 Primary care offers good reach into the community as the first point of contact in the healthcare system and the remit to provide whole person care across the life course. 65 When developing weight management interventions, it is important to reflect on resource availability within primary care settings to ensure patients’ needs can be met within existing healthcare systems. 66
We did not examine the equity of interventions, but primary care interventions may offer an additional service and potentially help those who would not attend a programme delivered outside of primary care. Interventions should consist of 12 or more contacts, and these findings are based on a mixture of telephone and face-to-face sessions. Previous evidence suggests that GPs find it difficult to raise the issue of weight with patients and are pessimistic about the success of weight loss interventions. 67 Therefore, interventions should be implemented with appropriate training for primary care practitioners so that they feel confident about helping patients to manage their weight. 68
Unanswered questions and future research
A range of effective interventions are available in primary care settings to help people manage their weight, but we found substantial heterogeneity. It was beyond the scope of this systematic review to examine the specific components of the interventions that may be associated with greater weight loss, but this could be investigated by future research. We do not know whether these interventions are universally suitable and will decrease or increase health inequalities. As the data are most likely collected in trials, an individual patient meta-analysis is now needed to explore characteristics or factors that might explain the variance. Most of the interventions excluded people prescribed drugs that affect weight gain, such as antipsychotics, glucocorticoids, and some antidepressants. This population might benefit from help with managing their weight owing to the side effects of these drug classes on weight gain, although we do not know whether the weight management interventions we investigated would be effective in this population. 69
What is already known on this topic
Referral by primary care to behavioural weight management programmes is effective, but the effectiveness of weight management interventions delivered by primary care is not known
Systematic reviews have provided evidence for weight management interventions, but the latest review of primary care delivered interventions was published in 2014
Factors such as intensity and delivery mechanisms have not been investigated and could influence the effectiveness of weight management interventions delivered by primary care
What this study adds
Weight management interventions delivered by primary care are effective and can help patients to better manage their weight
At least 12 contacts (telephone or face to face) are needed to deliver weight management programmes in primary care
Some evidence suggests that weight loss after weight management interventions delivered by non-medical practitioners in primary care (often endorsed and supervised by doctors) is similar to that delivered by clinician led programmes
Ethics statements
Ethical approval.
Not required.
Data availability statement
Additional data are available in the supplementary files.
Contributors: CDM and AJD conceived the study, with support from ES. CDM conducted the search with support from HEG. CDM, AJD, ES, HEG, KG, GB, and VEK completed the screening and full text identification. CDM and VEK completed the risk of bias assessment. CDM extracted data for the primary outcome and study characteristics. HEJ, GB, and KG extracted primary outcome data. CDM completed the analysis in RevMan, and GMJT completed the metaregression analysis in Stata. CDM drafted the paper with AJD. All authors provided comments on the paper. CDM acts as guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: AJD is supported by a National Institute for Health and Care Research (NIHR) research professorship award. This research was supported by the NIHR Leicester Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. ES’s salary is supported by an investigator grant (National Health and Medical Research Council, Australia). GT is supported by a Cancer Research UK fellowship. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: This research was supported by the National Institute for Health and Care Research Leicester Biomedical Research Centre; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
The lead author (CDM) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported, and that no important aspects of the study have been omitted.
Dissemination to participants and related patient and public communities: We plan to disseminate these research findings to a wider community through press releases, featuring on the Centre for Lifestyle Medicine and Behaviour website ( www.lboro.ac.uk/research/climb/ ) via our policy networks, through social media platforms, and presentation at conferences.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- Renehan AG ,
- Heller RF ,
- Bansback N ,
- Birmingham CL ,
- Abdullah A ,
- Peeters A ,
- de Courten M ,
- Stoelwinder J
- Aghili SMM ,
- Ebrahimpur M ,
- Arjmand B ,
- KETLAK Study Group
- ↵ Department of Health and Social Care. New specialised support to help those living with obesity to lose weight UK2021. www.gov.uk/government/news/new-specialised-support-to-help-those-living-with-obesity-to-lose-weight [accessed 08/02/2021].
- U.S. Preventive Services Task Force
- ↵ National Institute for Health and Care Excellence. Maintaining a Healthy Weight and Preventing Excess Weight Gain in Children and Adults. Cost Effectiveness Considerations from a Population Modelling Viewpoint. 2014, NICE. www.nice.org.uk/guidance/ng7/evidence/evidence-review-2-qualitative-evidence-review-of-the-most-acceptable-ways-to-communicate-information-about-individually-modifiable-behaviours-to-help-maintain-a-healthy-weight-or-prevent-excess-weigh-8733713.
- ↵ The Health Foundation. Use of primary care during the COVID-19 pandemic. 17/09/2020: The Health Foundation, 2020.
- ↵ Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings, 2017-18. 2019 ed. Canberra, Australia, 2018. www.abs.gov.au/AUSSTATS/[email protected]/Lookup/4839.0Main+Features12017-18?OpenDocument.
- LeBlanc ES ,
- Patnode CD ,
- Webber EM ,
- Redmond N ,
- Rushkin M ,
- O’Connor EA
- Damschroder LJ ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- McKenzie JE ,
- Bossuyt PM ,
- ↵ WHO. Main terminology: World Health Organization; 2004. www.euro.who.int/en/health-topics/Health-systems/primary-health-care/main-terminology [accessed 09.12.21].
- Aceves-Martins M ,
- Robertson C ,
- REBALANCE team
- Glasziou P ,
- Isenring E ,
- Chisholm A ,
- Wakayama LN ,
- Kettle VE ,
- Madigan CD ,
- ↵ Covidence [program]. Melbourne, 2021.
- Welzel FD ,
- Carrington MJ ,
- Fernández-Ruiz VE ,
- Ramos-Morcillo AJ ,
- Solé-Agustí M ,
- Paniagua-Urbano JA ,
- Armero-Barranco D
- Bräutigam-Ewe M ,
- Hildingh C ,
- Yardley L ,
- Christian JG ,
- Bessesen DH ,
- Christian KK ,
- Goldstein MG ,
- Martin PD ,
- Dutton GR ,
- Horswell RL ,
- Brantley PJ
- Wadden TA ,
- Rogers MA ,
- Berkowitz RI ,
- Kumanyika SK ,
- Morales KH ,
- Allison KC ,
- Rozenblum R ,
- De La Cruz BA ,
- Katzmarzyk PT ,
- Martin CK ,
- Newton RL Jr . ,
- Nanchahal K ,
- Holdsworth E ,
- ↵ RevMan [program]. 5.4 version: Copenhagen, 2014.
- Sterne JAC ,
- Savović J ,
- Gomez-Huelgas R ,
- Jansen-Chaparro S ,
- Baca-Osorio AJ ,
- Mancera-Romero J ,
- Tinahones FJ ,
- Bernal-López MR
- Delahanty LM ,
- Tárraga Marcos ML ,
- Panisello Royo JM ,
- Carbayo Herencia JA ,
- Beeken RJ ,
- Leurent B ,
- Vickerstaff V ,
- Hagobian T ,
- Brannen A ,
- Rodriguez-Cristobal JJ ,
- Alonso-Villaverde C ,
- Panisello JM ,
- Conroy MB ,
- Spadaro KC ,
- Takasawa N ,
- Mashiyama Y ,
- Pritchard DA ,
- Hyndman J ,
- Jarjoura D ,
- Smucker W ,
- Baughman K ,
- Bennett GG ,
- Steinberg D ,
- Zaghloul H ,
- Chagoury O ,
- Leslie WS ,
- Barnes AC ,
- Summerbell CD ,
- Greenwood DC ,
- Huseinovic E ,
- Leu Agelii M ,
- Hellebö Johansson E ,
- Winkvist A ,
- Look AHEAD Research Group
- LeBlanc EL ,
- Wheeler GM ,
- Aveyard P ,
- de Koning L ,
- Chiuve SE ,
- Willett WC ,
- ↵ World Health Organization. Obesity and Overweight, 2021, www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Starfield B ,
- Sturgiss E ,
- Dewhurst A ,
- Devereux-Fitzgerald A ,
- Haesler E ,
- van Weel C ,
- Gulliford MC
- Fassbender JE ,
- Sarwer DB ,
- Brekke HK ,

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Health Topics
Managing Overweight and Obesity in Adults: Systematic Evidence Review from the Obesity Expert Panel

Expert Panel Members - Managing Overweight and Obesity in Adults: Systematic Evidence Review from the Obesity Expert Panel
Co-Chair (Voting)
Michael Jensen, M.D. Mayo Clinic Rochester, Minnesota
Donna Ryan, M.D. Pennington Biomedical Research Center Baton Rouge, Louisiana
Members (Voting)
Caroline M. Apovian, M.D. Boston University School of Medicine Boston, Massachusetts
Jamy Ard, M.D. Wake Forest University Baptist Medical Center Winston-Salem, NC
Anthony G. Comuzzie, Ph.D. Southwest Foundation for Biomedical Research San Antonio, Texas
Frank Hu, M.D., Ph.D. Harvard University Boston, Massachusetts
John M. Jakicic, Ph.D. University of Pittsburgh Pittsburgh, Pennsylvania
Robert Kushner, M.D. Northwestern University Chicago, Illinois
Barbara Millen, Dr.P.H., R.D. Boston University School of Medicine Boston, Massachusetts
Cathy Nonas, M.S., R.D. New York City Department of Health and Mental Hygiene New York, New York
F. Xavier Pi-Sunyer, M.D., M.P.H. Columbia University St. Luke's-Roosevelt Hospital New York, New York
June Stevens, Ph.D. University of North Carolina at Chapel Hill Chapel Hill, North Carolina 27599-7461
Victor J. Stevens, Ph.D. Kaiser Permanente Center for Health Research Portland, Oregon
Thomas A. Wadden, Ph.D. University of Pennsylvania Philadelphia, Pennsylvania
Bruce Wolfe, M.D. Oregon Health and Science University Portland, Oregon
Ex-Officio Members (Voting)
Van Hubbard, M.D., Ph.D. National Institute of Diabetes and Digestive and Kidney Diseases Bethesda, MD
Catherine Loria, Ph.D. National Heart, Lung, and Blood Institute Bethesda, MD
Susan Z. Yanovski, M.D. National Institute of Diabetes and Digestive and Kidney Diseases Bethesda, MD
NHLBI Program Coordinator (Non-voting)
Karen Donato, S.M., R.D. National Heart, Lung, and Blood Institute Bethesda, MD
Related Health Topics
Additional support.
- Open access
- Published: 21 June 2021
The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies
- Emma Farrell ORCID: orcid.org/0000-0002-7780-9428 1 ,
- Marta Bustillo 2 ,
- Carel W. le Roux 3 ,
- Joe Nadglowski 4 ,
- Eva Hollmann 1 &
- Deirdre McGillicuddy 1
Systematic Reviews volume 10 , Article number: 181 ( 2021 ) Cite this article
6331 Accesses
9 Altmetric
Metrics details
Obesity is a prevalent, complex, progressive and relapsing chronic disease characterised by abnormal or excessive body fat that impairs health and quality of life. It affects more than 650 million adults worldwide and is associated with a range of health complications. Qualitative research plays a key role in understanding patient experiences and the factors that facilitate or hinder the effectiveness of health interventions. This review aims to systematically locate, assess and synthesise qualitative studies in order to develop a more comprehensive understanding of the lived experience of people with obesity.
This is a protocol for a qualitative evidence synthesis of the lived experience of people with obesity. A defined search strategy will be employed in conducting a comprehensive literature search of the following databases: PubMed, Embase, PsycInfo, PsycArticles and Dimensions (from 2011 onwards). Qualitative studies focusing on the lived experience of adults with obesity (BMI >30) will be included. Two reviewers will independently screen all citations, abstracts and full-text articles and abstract data. The quality of included studies will be appraised using the critical appraisal skills programme (CASP) criteria. Thematic synthesis will be conducted on all of the included studies. Confidence in the review findings will be assessed using GRADE CERQual.
The findings from this synthesis will be used to inform the EU Innovative Medicines Initiative (IMI)-funded SOPHIA (Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy) study. The objective of SOPHIA is to optimise future obesity treatment and stimulate a new narrative, understanding and vocabulary around obesity as a set of complex and chronic diseases. The findings will also be useful to health care providers and policy makers who seek to understand the experience of those with obesity.
Systematic review registration
PROSPERO CRD42020214560 .
Peer Review reports
Obesity is a complex chronic disease in which abnormal or excess body fat (adiposity) impairs health and quality of life, increases the risk of long-term medical complications and reduces lifespan [ 1 ]. Operationally defined in epidemiological and population studies as a body mass index (BMI) greater than or equal to 30, obesity affects more than 650 million adults worldwide [ 2 ]. Its prevalence has almost tripled between 1975 and 2016, and, globally, there are now more people with obesity than people classified as underweight [ 2 ].
Obesity is caused by the complex interplay of multiple genetic, metabolic, behavioural and environmental factors, with the latter thought to be the proximate factor which enabled the substantial rise in the prevalence of obesity in recent decades [ 3 , 4 ]. This increased prevalence has resulted in obesity becoming a major public health issue with a resulting growth in health care and economic costs [ 5 , 6 ]. At a population level, health complications from excess body fat increase as BMI increases [ 7 ]. At the individual level, health complications occur due to a variety of factors such as distribution of adiposity, environment, genetic, biologic and socioeconomic factors [ 8 ]. These health complications include type 2 diabetes [ 9 ], gallbladder disease [ 10 ] and non-alcoholic fatty liver disease [ 11 ]. Excess body fat can also place an individual at increased cardiometabolic and cancer risk [ 12 , 13 , 14 ] with an estimated 20% of all cancers attributed to obesity [ 15 ].
Although first recognised as a disease by the American Medical Association in 2013 [ 16 ], the dominant cultural narrative continues to present obesity as a failure of willpower. People with obesity are positioned as personally responsible for their weight. This, combined with the moralisation of health behaviours and the widespread association between thinness, self-control and success, has resulted in those who fail to live up to this cultural ideal being subject to weight bias, stigma and discrimination [ 17 , 18 , 19 ]. Weight bias, stigma and discrimination have been found to contribute, independent of weight or BMI, to increased morbidity or mortality [ 20 ].
Thomas et al. [ 21 ] highlighted, more than a decade ago, the need to rethink how we approach obesity so as not to perpetuate damaging stereotypes at a societal level. Obesity research then, as now, largely focused on measurable outcomes and quantifiable terms such as body mass index [ 22 , 23 ]. Qualitative research approaches play a key role in understanding patient experiences, how factors facilitate or hinder the effectiveness of interventions and how the processes of interventions are perceived and implemented by users [ 24 ]. Studies adopting qualitative approaches have been shown to deliver a greater depth of understanding of complex and socially mediated diseases such as obesity [ 25 ]. In spite of an increasing recognition of the integral role of patient experience in health research [ 25 , 26 ], the voices of patients remain largely underrepresented in obesity research [ 27 , 28 ].
Systematic reviews and syntheses of qualitative studies are recognised as a useful contribution to evidence and policy development [ 29 ]. To the best of the authors’ knowledge, this will be the first systematic review and synthesis of qualitative studies focusing on the lived experience of people with obesity. While systematic reviews have been carried out on patient experiences of treatments such as behavioural management [ 30 ] and bariatric surgery [ 31 ], this review and synthesis will be the first to focus on the experience of living with obesity rather than patient experiences of particular treatments or interventions. This focus represents a growing awareness that ‘patients have a specific expertise and knowledge derived from lived experience’ and that understanding lived experience can help ‘make healthcare both effective and more efficient’ [ 32 ].
This paper outlines a protocol for the systematic review of qualitative studies based on the lived experience of people with obesity. The findings of this review will be synthesised in order to develop an overview of the lived experience of patients with obesity. It will look, in particular, at patient concerns around the risks of obesity and their aspirations for response to obesity treatment.
The review protocol has been registered within the PROSPERO database (registration number: CRD42020214560) and is being reported in accordance with the reporting guidance provided in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement [ 33 , 34 ] (see checklist in Additional file 1 ).
Information sources and search strategy
The primary source of literature will be a structured search of the following electronic databases (from January 2011 onwards—to encompass the increase in research focused on patient experience observed over the last 10 years): PubMed, Embase, PsycInfo, PsycArticles and Dimensions. There is no methodological agreement as to how many search terms or databases out to be searched as part of a ‘good’ qualitative synthesis (Toye et al. [ 35 ]). However, the breadth and depth of the search terms, the inclusion of clinical and personal language and the variety within the selected databases, which cover areas such as medicine, nursing, psychology and sociology, will position this qualitative synthesis as comprehensive. Grey literature will not be included in this study as its purpose is to conduct a comprehensive review of peer-reviewed primary research. The study’s patient advisory board will be consulted at each stage of the review process, and content experts and authors who are prolific in the field will be contacted. The literature searches will be designed and conducted by the review team which includes an experienced university librarian (MB) following the methodological guidance of chapter two of the JBI Manual for Evidence Synthesis [ 36 ]. The search will include a broad range of terms and keywords related to obesity and qualitative research. A full draft search strategy for PubMed is provided in Additional file 2 .
Eligibility criteria
Studies based on primary data generated with adults with obesity (operationally defined as BMI >30) and focusing on their lived experience will be eligible for inclusion in this synthesis (Table 1 ). The context can include any country and all three levels of care provision (primary, secondary and tertiary). Only peer-reviewed, English language, articles will be included. Studies adopting a qualitative design, such as phenomenology, grounded theory or ethnography, and employing qualitative methods of data collection and analysis, such as interviews, focus groups, life histories and thematic analysis, will be included. Publications with a specific focus, for example, patient’s experience of bariatric surgery, will be included, as well as studies adopting a more general view of the experience of obesity.
Screening and study selection process
Search results will be imported to Endnote X9, and duplicate entries will be removed. Covidence [ 38 ] will be used to screen references with two reviewers (EF and EH) removing entries that are clearly unrelated to the research question. Titles and abstracts will then be independently screened by two reviewers (EF and EH) according to the inclusion criteria (Table 1 ). Any disagreements will be resolved through a third reviewer (DMcG). This layer of screening will determine which publications will be eligible for independent full-text review by two reviewers (EF and EH) with disagreements again being resolved by a third reviewer (DMcG).
Data extraction
Data will be extracted independently by two researchers (EF and EH) and combined in table format using the following headings: author, year, title, country, research aims, participant characteristics, method of data collection, method of data analysis, author conclusions and qualitative themes. In the case of insufficient or unclear information in a potentially eligible article, the authors will be contacted by email to obtain or confirm data, and a timeframe of 3 weeks to reply will be offered before article exclusion.
Quality appraisal of included studies
This qualitative synthesis will facilitate the development of a conceptual understanding of obesity and will be used to inform the development of policy and practice. As such, it is important that the studies included are themselves of suitable quality. The methodological quality of all included studies will be assessed using the critical appraisal skills programme (CASP) checklist, and studies that are deemed of insufficient quality will be excluded. The CASP checklist for qualitative research comprises ten questions that cover three main issues: Are the results of the study under review valid? What are the results? Will the results help locally? Two reviewers (EF and EH) will independently evaluate each study using the checklist with a third and fourth reviewer (DMcG and MB) available for consultation in the event of disagreement.
Data synthesis
The data generated through the systematic review outlined above will be synthesised using thematic synthesis as described by Thomas and Harden [ 39 ]. Thematic synthesis enables researchers to stay ‘close’ to the data of primary studies, synthesise them in a transparent way and produce new concepts and hypotheses. This inductive approach is useful for drawing inference based on common themes from studies with different designs and perspectives. Thematic synthesis is made up of a three-step process. Step one consists of line by line coding of the findings of primary studies. The second step involves organising these ‘free codes’ into related areas to construct ‘descriptive’ themes. In step three, the descriptive themes that emerged will be iteratively examined and compared to ‘go beyond’ the descriptive themes and the content of the initial studies. This step will generate analytical themes that will provide new insights related to the topic under review.
Data will be coded using NVivo 12. In order to increase the confirmability of the analysis, studies will be reviewed independently by two reviewers (EF and EH) following the three-step process outlined above. This process will be overseen by a third reviewer (DMcG). In order to increase the credibility of the findings, an overview of the results will be brought to a panel of patient representatives for discussion. Direct quotations from participants in the primary studies will be italicised and indented to distinguish them from author interpretations.
Assessment of confidence in the review findings
Confidence in the evidence generated as a result of this qualitative synthesis will be assessed using the Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research (GRADE CERQual) [ 40 ] approach. Four components contribute to the assessment of confidence in the evidence: methodological limitations, relevance, coherence and adequacy of data. The methodological limitations of included studies will be examined using the CASP tool. Relevance assesses the degree to which the evidence from the primary studies applies to the synthesis question while coherence assesses how well the findings are supported by the primary studies. Adequacy of data assesses how much data supports a finding and how rich this data is. Confidence in the evidence will be independently assessed by two reviewers (EF and EH), graded as high, moderate or low, and discussed collectively amongst the research team.
Reflexivity
For the purposes of transparency and reflexivity, it will be important to consider the findings of the qualitative synthesis and how these are reached, in the context of researchers’ worldviews and experiences (Larkin et al, 2019). Authors have backgrounds in health science (EF and EH), education (DMcG and EF), nursing (EH), sociology (DMcG), philosophy (EF) and information science (MB). Prior to conducting the qualitative synthesis, the authors will examine and discuss their preconceptions and beliefs surrounding the subject under study and consider the relevance of these preconceptions during each stage of analysis.
Dissemination of findings
Findings from the qualitative synthesis will be disseminated through publications in peer-reviewed journals, a comprehensive and in-depth project report and presentation at peer-reviewed academic conferences (such as EASO) within the field of obesity research. It is also envisaged that the qualitative synthesis will contribute to the shared value analysis to be undertaken with key stakeholders (including patients, clinicians, payers, policy makers, regulators and industry) within the broader study which seeks to create a new narrative around obesity diagnosis and treatment by foregrounding patient experiences and voice(s). This synthesis will be disseminated to the 29 project partners through oral presentations at management board meetings and at the general assembly. It will also be presented as an educational resource for clinicians to contribute to an improved understanding of patient experience of living with obesity.
Obesity is a complex chronic disease which increases the risk of long-term medical complications and a reduced quality of life. It affects a significant proportion of the world’s population and is a major public health concern. Obesity is the result of a complex interplay of multiple factors including genetic, metabolic, behavioural and environmental factors. In spite of this complexity, obesity is often construed in simple terms as a failure of willpower. People with obesity are subject to weight bias, stigma and discrimination which in themselves result in increased risk of mobility or mortality. Research in the area of obesity has tended towards measurable outcomes and quantitative variables that fail to capture the complexity associated with the experience of obesity. A need to rethink how we approach obesity has been identified—one that represents the voices and experiences of people living with obesity. This paper outlines a protocol for the systematic review of available literature on the lived experience of people with obesity and the synthesis of these findings in order to develop an understanding of patient experiences, their concerns regarding the risks associated with obesity and their aspirations for response to obesity treatment. Its main strengths will be the breadth of its search remit—focusing on the experiences of people with obesity rather than their experience of a particular treatment or intervention. It will also involve people living with obesity and its findings disseminated amongst the 29 international partners SOPHIA research consortium, in peer reviewed journals and at academic conferences. Just as the study’s broad remit is its strength, it is also a potential challenge as it is anticipated that searchers will generate many thousands of results owing to the breadth of the search terms. However, to the best of the authors’ knowledge, this will be the first systematic review and synthesis of its kind, and its findings will contribute to shaping the optimisation of future obesity understanding and treatment.
Availability of data and materials
Not applicable.
Abbreviations
Body mass index
Critical appraisal skills programme
Grading of Recommendations Assessment, Development and Evaluation Confidence in Evidence from Reviews of Qualitative Research
Innovative Medicines Initiative
Medical Subject Headings
Population, phenomenon of interest, context, study type
Stratification of Obesity Phenotypes to Optimize Future Obesity Therapy
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D, et al. Obesity in adults: a clinical practice guideline. Can Med Assoc J. 2020;192(31):E875–91. https://doi.org/10.1503/cmaj.191707 .
Article Google Scholar
World Health Organisation. Fact sheet: obesity and overweight. Geneva: World Health Organisation; 2020.
Google Scholar
Mechanick J, Hurley D, Garvey W. Adiposity-based chronic disease as a new diagnostic term: the American Association of Clinical Endocrinologists and American College Of Endocrinology position statement. Endocrine Pract. 2017;23(3):372–8. https://doi.org/10.4158/EP161688.PS .
Garvey W, Mechanick J. Proposal for a scientifically correct and medically actionable disease classification system (ICD) for obesity. Obesity. 2020;28(3):484–92. https://doi.org/10.1002/oby.22727 .
Article PubMed Google Scholar
Biener A, Cawley J, Meyerhoefer C. The high and rising costs of obesity to the US health care system. J Gen Intern Med. 2017;32(Suppl 1):6–8. https://doi.org/10.1007/s11606-016-3968-8 .
Article PubMed PubMed Central Google Scholar
Department of Health and Social Care. Healthy lives, healthy people: a call to action on obesity in England. London: Department of Health and Social Care; 2011.
Di Angelantonio E, Bhupathiraju SN, Wormser D, Gao P, Kaptoge S, de Gonzalez AB, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388(10046):776–86. https://doi.org/10.1016/S0140-6736(16)30175-1 .
Sharma AM. M, M, M & M: a mnemonic for assessing obesity. Obesity Reviews. 2010;11(11):808–9. https://doi.org/10.1111/j.1467-789X.2010.00766.x .
Article PubMed CAS Google Scholar
Asnawi A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract 2010;89:309-19. Diab Res Clin Pract. 2010;89:309–19.
Dagfinn A, Teresa N, Lars JV. Body mass index, abdominal fatness and the risk of gallbladder disease. 2015;30(9):1009.
Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20(9).
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. 2003;289(2):187-193.
Grover SA, Kaouache M, Rempel P, Joseph L, Dawes M, Lau DCW, et al. Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: a modelling study. 2015;3(2):114-122.
Ackerman S, Blackburn O, Marchildon F, Cohen P. Insights into the link between obesity and cancer. Curr Obes Rep. 2017;6(2):195–203. https://doi.org/10.1007/s13679-017-0263-x .
Wolin K, Carson K, Colditz G. Obesity and cancer. Oncol. 2010;15(6):556–65. https://doi.org/10.1634/theoncologist.2009-0285 .
Resolution 420: Recognition of obesity as a disease [press release]. 05/16/13 2013.
Brownell KD. Personal responsibility and control over our bodies: when expectation exceeds reality. 1991;10(5):303-10.
Puhl RM, Latner JD, O'Brien K, Luedicke J, Danielsdottir S, Forhan M. A multinational examination of weight bias: predictors of anti-fat attitudes across four countries. 2015;39(7):1166-1173.
Browne NT. Weight bias, stigmatization, and bullying of obese youth. 2012;7(3):107-15.
Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. 2015;26(11):1803-11.
Thomas SL, Hyde J, Karunaratne A, Herbert D, Komesaroff PA. Being “fat” in today’s world: a qualitative study of the lived experiences of people with obesity in Australia. 2008;11(4):321-30.
Ogden K, Barr J, Rossetto G, Mercer J. A “messy ball of wool”: a qualitative study of the dimensions of the lived experience of obesity. 2020;8(1):1-14.
Ueland V, Furnes B, Dysvik E, R¯rtveit K. Living with obesity-existential experiences. 2019;14(1):1-12.
Avenell A, Robertson C, Skea Z, Jacobsen E, Boyers D, Cooper D, et al. Bariatric surgery, lifestyle interventions and orlistat for severe obesity: the REBALANCE mixed-methods systematic review and economic evaluation. 2018;22(68).
The PLoS Medicine Editors. Qualitative research: understanding patients’ needs and experiences. Plos Med. 2007;4(8):1283–4.
Boulton M, Fitzpatrick R. Qualitative methods for assessing health care doi:10.1136/qshc.3.2.107. Qual Health Care. 1994;3:107–13.
Johnstone J, Herredsberg C, Lacy L, Bayles P, Dierking L, Houck A, et al. What I wish my doctor really knew: the voices of patients with obesity. Ann Fam Med. 2020;18(2):169–71. https://doi.org/10.1370/afm.2494 .
Brown I, Thompson J, Tod A, Jones G. Primary care support for tackling obesity: a qualitative study of the perceptions of obese patients. Br J Gen Pract. 2006;56(530):666–72.
PubMed PubMed Central Google Scholar
Brown I, Gould J. Qualitative studies of obesity: a review of methodology. Health. 2013;5(8A3):69–80.
Garip G, Yardley L. A synthesis of qualitative research on overweight and obese people’s views and experiences of weight management. Clin Obes. 2011;1(2-3):10–126.
Coulman K, MacKichan F, Blazeby J, Owen-Smith A. Patient experiences of outcomes of bariatric surgery: a systematic review and qualitative synthesis. Obes Rev. 2017;18(5):547–59. https://doi.org/10.1111/obr.12518 .
European Patients’ Forum. “Patients’ Perceptions of Quality in Healthcare”: Report of a survey conducted by EPF in 2016 Brussels: European Patients’ Forum; 2017.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. https://doi.org/10.1186/2046-4053-4-1 .
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349(jan02 1):g7647. https://doi.org/10.1136/bmj.g7647 .
Toye F, et al. Meta-ethnography 25 years on: challenges and insights for synthesising a large number of qualitative studies. BMC Med Res Methodol. 2014;14(80).
Lockwood C, Porrit K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, et al. Chapter 2: Systematic reviews of qualitative evidence. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis: JBI; 2020, doi: https://doi.org/10.46658/JBIMES-20-03 .
Methley AM, et al. PICO, PICOS and SPIDER: a comparison study of spcificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Services Res. 2014;14.
Covidence. Cochrane Community; 2020. Available from: https://www.covidence.org .
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45. https://doi.org/10.1186/1471-2288-8-45 .
Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci. 2018;13(1):2. https://doi.org/10.1186/s13012-017-0688-3 .
Download references
Acknowledgements
Any amendments made to this protocol when conducting the study will be outlined in PROSPERO and reported in the final manuscript.
This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking (JU) under grant agreement No 875534. The JU receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA and T1D Exchange, JDRF and Obesity Action Coalition. The funding body had no role in the design of the study and will not have a role in collection, analysis and interpretation of data or in writing the manuscript.
Author information
Authors and affiliations.
School of Education, University College Dublin, Belfield, Dublin 4, Ireland
Emma Farrell, Eva Hollmann & Deirdre McGillicuddy
University College Dublin Library, Dublin, Ireland
Marta Bustillo
Diabetes Complications Research Centre, University College Dublin, Dublin, Ireland
Carel W. le Roux
Obesity Action Coalition, Tampa, USA
Joe Nadglowski
You can also search for this author in PubMed Google Scholar
Contributions
EF conceptualised and designed the protocol with input from DMcG and MB. EF drafted the initial manuscript. EF and MB defined the concepts and search items with input from DmcG, CleR and JN. MB and EF designed and executed the search strategy. DMcG, CleR, JN and EH provided critical insights and reviewed and revised the protocol. All authors have approved and contributed to the final written manuscript.
Corresponding author
Correspondence to Emma Farrell .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:..
PRISMA-P (Preferred Reporting Items for Systematic review and Meta-Analysis Protocols) 2015 checklist: recommended items to address in a systematic review protocol*.
Additional file 2: Table 1
. Search PubMed search string.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Farrell, E., Bustillo, M., le Roux, C.W. et al. The lived experience of people with obesity: study protocol for a systematic review and synthesis of qualitative studies. Syst Rev 10 , 181 (2021). https://doi.org/10.1186/s13643-021-01706-5
Download citation
Received : 28 October 2020
Accepted : 14 May 2021
Published : 21 June 2021
DOI : https://doi.org/10.1186/s13643-021-01706-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lived experience
- Patient experience
- Obesity treatment
- Qualitative
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Systematic review and meta-analysis of short-term outcomes: robot-assisted versus laparoscopic surgery for gastric cancer patients with visceral obesity
- Published: 04 June 2024
- Volume 18 , article number 238 , ( 2024 )
Cite this article

- Lin-Wen Yang 1 na1 ,
- Xiang-Yu Bai 1 na1 &
- Guo-Min Jing 2
The objective of this meta-analysis was to assess the comparative efficacy of robot-assisted and laparoscopic surgery in treating gastric cancer among patients characterized by a high visceral fat area (VFA). In April 2024, we conducted a comprehensive literature review using major international databases, such as PubMed, Embase, and Google Scholar. We restricted our selection to articles written in English, excluding reviews, protocols without published data, conference abstracts, and irrelevant content. Our analysis focused on continuous data using 95% confidence intervals (CIs) and standard mean differences (SMDs), while dichotomous data were assessed with odds ratios (ORs) and 95% CIs. We set the threshold for statistical significance at P < 0.05. Data extraction included baseline characteristics, primary outcomes (such as operative time, major complications, lymph node yield, and anastomotic leakage), and secondary outcomes. The meta-analysis included three cohort studies totaling 970 patients. The robotic-assisted group demonstrated a significantly longer operative time compared to the laparoscopic group, with a weighted mean difference (WMD) of − 55.76 min (95% CI − 74.03 to − 37.50; P < 0.00001). This group also showed a reduction in major complications, with an odds ratio (OR) of 2.48 (95% CI 1.09–5.66; P = 0.03) and fewer occurrences of abdominal infections (OR 3.17, 95% CI 1.41–7.14; P = 0.005), abdominal abscesses (OR 3.83, 95% CI 1.53–9.57; P = 0.004), anastomotic leaks (OR 4.09, 95% CI 1.73–9.65; P = 0.001), and pancreatic leaks (OR 8.93, 95% CI 2.33–34.13; P = 0.001). However, no significant differences were observed between the groups regarding length of hospital stay, overall complications, estimated blood loss, or lymph node yield. Based on our findings, robot-assisted gastric cancer surgery in obese patients with visceral fat appears to be correlated with fewer major complications compared to laparoscopic surgery, while maintaining similar outcomes in other surgical aspects. However, it is important to note that robot-assisted procedures do tend to have longer operative times.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Data availability
The original contributions detailed in the study are encompassed within the article material. For additional inquiries, please contact the corresponding author/s directly.
Abbreviations
Newcastle ottawa scale
Confidence intervals
Odds ratios
Weighted mean difference
Visceral fat area
Standard deviation
Body mass index
Robot-assisted gastrectomy
Laparoscopic gastrectomy
- Gastric cancer
Medical subject headings
Population intervention comparison outcomes study type
Randomized controlled trials
Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F (2020) Gastric cancer. Lancet 396(10251):635–648. https://doi.org/10.1016/S0140-6736(20)31288-5
Article CAS PubMed Google Scholar
Park SH, Lim DH, Sohn TS et al (2021) A randomized phase III trial comparing adjuvant single-agent S1, S-1 with oxaliplatin, and postoperative chemoradiation with S-1 and oxaliplatin in patients with node-positive gastric cancer after D2 resection: the ARTIST 2 trial☆. Ann Oncol 32(3):368–374. https://doi.org/10.1016/j.annonc.2020.11.017
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4(2):146–148
CAS PubMed Google Scholar
Sugimoto M, Kinoshita T, Shibasaki H et al (2013) Short-term outcome of total laparoscopic distal gastrectomy for overweight and obese patients with gastric cancer. Surg Endosc 27(11):4291–4296. https://doi.org/10.1007/s00464-013-3045-x
Article PubMed Google Scholar
Kim YW, Baik YH, Yun YH et al (2008) Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg 248(5):721–727. https://doi.org/10.1097/SLA.0b013e318185e62e
Ma J, Li X, Zhao S, Zhang R, Yang D (2020) Robotic versus laparoscopic gastrectomy for gastric cancer: a systematic review and meta-analysis. World J Surg Oncol 18(1):306. https://doi.org/10.1186/s12957-020-02080-7
Article PubMed PubMed Central Google Scholar
Jung JH, Ryu SY, Jung MR, Park YK, Jeong O (2014) Laparoscopic distal gastrectomy for gastric cancer in morbidly obese patients in South Korea. J Gastric Cancer 14(3):187–195. https://doi.org/10.5230/jgc.2014.14.3.187
Hashizume M, Sugimachi K (2003) Robot-assisted gastric surgery. Surg Clin North Am 83(6):1429–1444. https://doi.org/10.1016/S0039-6109(03)00158-0
Dalsgaard T, Jensen MD, Hartwell D, Mosgaard BJ, Jørgensen A, Jensen BR (2020) Robotic surgery is less physically demanding than laparoscopic surgery: paired cross sectional study. Ann Surg 271(1):106–113. https://doi.org/10.1097/SLA.0000000000002845
Yang K, Cho M, Roh CK et al (2019) Robotic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. Surg Endosc 33(7):2357–2363. https://doi.org/10.1007/s00464-019-06772-4
Gehrig PA, Cantrell LA, Shafer A, Abaid LN, Mendivil A, Boggess JF (2008) What is the optimal minimally invasive surgical procedure for endometrial cancer staging in the obese and morbidly obese woman? Gynecol Oncol 111(1):41–45. https://doi.org/10.1016/j.ygyno.2008.06.030
Bernardini MQ, Gien LT, Tipping H, Murphy J, Rosen BP (2012) Surgical outcome of robotic surgery in morbidly obese patient with endometrial cancer compared to laparotomy. Int J Gynecol Cancer 22(1):76–81. https://doi.org/10.1097/IGC.0b013e3182353371
Moskovic DJ, Lavery HJ, Rehman J, Nabizada-Pace F, Brajtbord J, Samadi DB (2010) High body mass index does not affect outcomes following robotic assisted laparoscopic prostatectomy. Can J Urol 17(4):5291–5298
PubMed Google Scholar
Yu X, Zhu L, Zhang Y, Feng Q (2023) Robotic versus laparoscopic gastrectomy for gastric cancer in patients with obesity: systematic review and meta-analysis. Front Oncol 13:1158804. https://doi.org/10.3389/fonc.2023.1158804
Xu F, Earp JE, Adami A et al (2022) The sex and race/ethnicity-specific relationships of abdominal fat distribution and anthropometric indices in US adults. Int J Environ Res Public Health 19(23):15521. https://doi.org/10.3390/ijerph192315521
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27(6):1785–1805. https://doi.org/10.1177/0962280216669183
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Lau J, Ioannidis JPA, Terrin N, Schmid CH, Olkin I (2006) The case of the misleading funnel plot. BMJ 333(7568):597–600. https://doi.org/10.1136/bmj.333.7568.597
Sterne JA, Gavaghan D, Egger M (2000) Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol 53(11):1119–1129. https://doi.org/10.1016/s0895-4356(00)00242-0
Hikage M, Fujiya K, Waki Y et al (2022) Advantages of a robotic approach compared with laparoscopy gastrectomy for patients with high visceral fat area. Surg Endosc 36(8):6181–6193. https://doi.org/10.1007/s00464-022-09178-x
Kubo N, Sakurai K, Hasegawa T et al (2024) Impact of a robotic system on intra-abdominal infectious complications after minimally invasive gastrectomy in patients with gastric cancer: a propensity score matching analysis regarding visceral obesity. Ann Gastroenterol Surg 8(2):221–233. https://doi.org/10.1002/ags3.12748
Park JY, Ryu KW, Reim D et al (2015) Robot-assisted gastrectomy for early gastric cancer: is it beneficial in viscerally obese patients compared to laparoscopic gastrectomy? World J Surg 39(7):1789–1797. https://doi.org/10.1007/s00268-015-2998-4
Kandil EH, Noureldine SI, Yao L, Slakey DP (2012) Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg 214(4):558–564. https://doi.org/10.1016/j.jamcollsurg.2012.01.002
Song J, Kang WH, Oh SJ, Hyung WJ, Choi SH, Noh SH (2009) Role of robotic gastrectomy using da Vinci system compared with laparoscopic gastrectomy: initial experience of 20 consecutive cases. Surg Endosc 23(6):1204–1211. https://doi.org/10.1007/s00464-009-0351-4
Woo Y, Hyung WJ, Pak KH et al (2011) Robotic gastrectomy as an oncologically sound alternative to laparoscopic resections for the treatment of early-stage gastric cancers. Arch Surg 146(9):1086–1092. https://doi.org/10.1001/archsurg.2011.114
Shibasaki S, Suda K, Obama K, Yoshida M, Uyama I (2020) Should robotic gastrectomy become a standard surgical treatment option for gastric cancer? Surg Today 50(9):955–965. https://doi.org/10.1007/s00595-019-01875-w
Fujiya K, Tokunaga M, Mori K et al (2016) Long-term survival in patients with postoperative intra-abdominal infectious complications after curative gastrectomy for gastric cancer: a propensity score matching analysis. Ann Surg Oncol 23(Suppl 5):809–816. https://doi.org/10.1245/s10434-016-5577-5
Kinoshita T, Sato R, Akimoto E, Tanaka Y, Okayama T, Habu T (2022) Reduction in postoperative complications by robotic surgery: a case-control study of robotic versus conventional laparoscopic surgery for gastric cancer. Surg Endosc 36(3):1989–1998. https://doi.org/10.1007/s00464-021-08483-1
Hikage M, Fujiya K, Kamiya S et al (2021) Robotic gastrectomy compared with laparoscopic gastrectomy for clinical stage I/II gastric cancer patients: a propensity score-matched analysis. World J Surg 45(5):1483–1494. https://doi.org/10.1007/s00268-020-05939-8
Zhang Z, Zhang X, Liu Y et al (2021) Meta-analysis of the efficacy of Da Vinci robotic or laparoscopic distal subtotal gastrectomy in patients with gastric cancer. Med Baltim 100(34):e27012. https://doi.org/10.1097/MD.0000000000027012
Article Google Scholar
Park JY, Jo MJ, Nam BH et al (2012) Surgical stress after robot-assisted distal gastrectomy and its economic implications. Br J Surg 99(11):1554–1561. https://doi.org/10.1002/bjs.8887
Guerrini GP, Esposito G, Magistri P et al (2020) Robotic versus laparoscopic gastrectomy for gastric cancer: the largest meta-analysis. Int J Surg 82:210–228. https://doi.org/10.1016/j.ijsu.2020.07.053
Hyun MH, Lee CH, Kwon YJ et al (2013) Robot versus laparoscopic gastrectomy for cancer by an experienced surgeon: comparisons of surgery, complications, and surgical stress. Ann Surg Oncol 20(4):1258–1265. https://doi.org/10.1245/s10434-012-2679-6
Mogal H, Fields R, Maithel SK, Votanopoulos K (2019) In patients with localized and resectable gastric cancer, what is the optimal extent of lymph node dissection-D1 versus D2 versus D3? Ann Surg Oncol 26(9):2912–2932. https://doi.org/10.1245/s10434-019-07417-5
Smith DD, Schwarz RR, Schwarz RE (2005) Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database. J Clin Oncol 23(28):7114–7124. https://doi.org/10.1200/JCO.2005.14.621
Schwarz RE, Smith DD (2007) Clinical impact of lymphadenectomy extent in resectable gastric cancer of advanced stage. Ann Surg Oncol 14(2):317–328. https://doi.org/10.1245/s10434-006-9218-2
Download references
Author information
Lin-Wen Yang and Xiang-Yu Bai contributed equally.
Authors and Affiliations
Department of Gastrointestinal Surgery, Affiliated Hospital of North Sichuan Medical College, Nanchong, Sichuan Province, China
Lin-Wen Yang & Xiang-Yu Bai
Clinical Medicine Department of North Sichuan Medical College, Nanchong, Sichuan Province, China
Guo-Min Jing
You can also search for this author in PubMed Google Scholar
Contributions
Every author contributed to the conceptualization and design of the study. YLW and BXY were tasked with data collection and analysis. YLW authored the initial draft of the manuscript, while JGM performed critical revisions, significantly enriching the intellectual content. All authors reviewed preliminary versions, provided feedback, and approved the final manuscript, ensuring a collaborative and thorough development process.
Corresponding author
Correspondence to Guo-Min Jing .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethical approval and consent to participate
Not applicable.

Consent for publication
Additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Yang, LW., Bai, XY. & Jing, GM. Systematic review and meta-analysis of short-term outcomes: robot-assisted versus laparoscopic surgery for gastric cancer patients with visceral obesity. J Robotic Surg 18 , 238 (2024). https://doi.org/10.1007/s11701-024-02002-9
Download citation
Received : 25 April 2024
Accepted : 27 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1007/s11701-024-02002-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Robot-assisted
- Laparoscopic
- Visceral obesity
- Meta-analysis
- Find a journal
- Publish with us
- Track your research
Association of air pollution exposure with overweight or obesity in children and adolescents: A systematic review and meta-analysis
Affiliations.
- 1 School of Public Health, Jilin University, Changchun 130021, China.
- 2 School of Public Health, Xinjiang Medical University, Xinjiang 834000, China.
- 3 School of Public Health, Jilin University, Changchun 130021, China. Electronic address: [email protected].
- PMID: 37984657
- DOI: 10.1016/j.scitotenv.2023.168589
Childhood overweight and obesity is a global problem. 38 million children under five years old were reported as being overweight/obese in 2019. However, current evidence regarding the effects of air pollution on children weight status remains scarce and inconsistent. This study aimed to determine the association between air pollutants and the weight status of children and adolescents. Four databases were searched up to August 9, 2023. Adjusted merged odds ratios (ORs), regression coefficients (β), and their 95 % confidence intervals (95 % CIs) were calculated and pooled. A total of 27 studies were included. The results showed that air pollutants had adverse effects on the body weight of children and adolescents. Exposure to PM 1 , PM 2.5 , PM coarse , and PM 10 were associated with increased risk of overweight/obesity, with pooled ORs (95 % CI) of 1.23 (1.09, 1.40), 1.18 (1.10, 1.28), 1.04 (1.03, 1.05) and 1.11 (1.06, 1.17) per 10 μg/m 3 increment, respectively. Individuals with higher exposure levels to NO X , O 3 , SO 2 and CO (per 10 μg/m 3 increment) were associated with 12 %, 6 %, 28 % and 1 % increased odds of being overweight/obese, respectively. With respect to the level of body mass index, the pooled β (95 % CIs) for each 10 μg/m 3 increase in PM 1 , PM 2.5 , PM 10 , and NO X exposure were 0.15 (0.12, 0.18), 0.11 (0.06, 0.16), 0.07 (0.03, 0.10), and 0.03 (0.01, 0.04), respectively. PM 1 has relatively strong adverse effects on body weight status. The subgroup analysis revealed a significantly increase in the risk of overweight/obesity when the concentrations of PM 2.5 , PM 10 , and NO 2 exceeded 35 μg/m 3 , 50 μg/m 3 , and 40 μg/m 3 , respectively. Exposure to PM 2.5 , PM 10 and NO X increased the risk of overweight/obesity, especially in Asia. This study provides evidence of the association between air pollution and being overweight/obese in children and adolescents.
Keywords: Adolescent; Air pollution; Body mass index; Children; Obesity; Overweight.
Copyright © 2023 Elsevier B.V. All rights reserved.
Publication types
- Meta-Analysis
- Systematic Review
- Air Pollutants* / analysis
- Air Pollution* / analysis
- Child, Preschool
- Environmental Exposure / analysis
- Nitrogen Dioxide / analysis
- Overweight / chemically induced
- Overweight / epidemiology
- Particulate Matter / adverse effects
- Particulate Matter / analysis
- Pediatric Obesity* / chemically induced
- Pediatric Obesity* / epidemiology
- Air Pollutants
- Particulate Matter
- Nitrogen Dioxide
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Systematic Review
- Open access
- Published: 04 June 2024
Techniques and Methods
A systematic review of recruitment and retention of ethnic minorities and migrants in obesity prevention randomised controlled trials
- Nidhi Wali ORCID: orcid.org/0000-0003-3667-9476 1 ,
- Md. Nazmul Huda ORCID: orcid.org/0000-0001-7048-1266 2 ,
- Timothy Gill 3 ,
- Julie Green 4 , 5 , 6 &
- Andre M. N. Renzaho ORCID: orcid.org/0000-0002-6844-0833 7
International Journal of Obesity ( 2024 ) Cite this article
Metrics details
- Epidemiology
- Risk factors
Participants’ recruitment and retention into community-based interventions can be challenging, especially in research involving ethnic minorities and migrants. Despite known challenges, there are limited reviews that probe recruitment and retention strategies involving ethnic minorities and migrants in the Organisation for Economic Cooperation and Development (OECD) countries. This systematic review aimed to measure recruitment and retention rates and identify the barriers and facilitators to effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention Randomised Control Trials (RCTs) in OECD countries.
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Five databases (CINAHL, Cochrane, Embase, Medline and PsychInfo) were searched from January 2000 to March 2022, in addition to Google and Google Scholar. Methodological quality and risk of bias were assessed, and pooled analysis and meta-ethnographic analysis were conducted on the included studies.
Twenty-five studies were included in the review. The pooled analysis found a 64% rate of recruitment of ethnic minorities in RCTs, with a retention rate of 71%. Key facilitators identified were—use of multiple communication channels, incentives, recruiting community champions, participant convenience and employing culturally sensitive strategies. Key barriers to participation were limited access to study sites, time constraints, limited trust, perceived fear, and anxiety.
Findings suggest the importance of undertaking culturally appropriate recruitment and retention strategies to minimise barriers and facilitate effective recruitment and retention of low-income ethnic minorities and migrants in community-based research.
Similar content being viewed by others

A toolkit for capturing a representative and equitable sample in health research
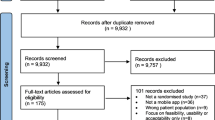
Development features and study characteristics of mobile health apps in the management of chronic conditions: a systematic review of randomised trials
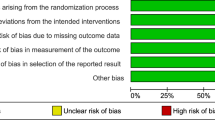
Culturally adapting internet- and mobile-based health promotion interventions might not be worth the effort: a systematic review and meta-analysis
Introduction.
Recruitment and retention of ethnic minorities and migrant populations into community-based obesity prevention trials continues to be a challenge [ 1 , 2 ]. This is due to multiple factors, including work-and family-related barriers, limited awareness of existing programmes [ 3 ], competing priorities, fear, mistrust [ 4 , 5 ], participants’ time constraints, inadequate transport facilities, and increased mobility of participants [ 6 ]. Moreover, a culturally incongruent discussion about informed consent to participate and limited recruitment of investigators and staff from similar ethnic backgrounds can hinder the effective recruitment and retention of participants in community-based obesity prevention trials [ 5 ]. Approximately 50–70% of community-based obesity prevention trials are unable to meet the target estimated sample size because of low recruitment and retention of participants [ 7 ]. Such poor and slow recruitment and participant retention in community-based obesity prevention trials may generate inconclusive findings, affect the delivery of interventions, and increase a trial’s cost [ 1 ].
To overcome these barriers some strategies have shown successful recruitment and retention of participants from ethnic minorities into community-based obesity prevention trials. Evidence suggests that community outreach and in-person on-site recruitment at recreational centres, schools, and faith-based organisations such as churches, temples and mosques, are successful strategies for including participants in interventions [ 2 ]. Furthermore, a combination of strategies involving consistent follow-up and frequent communications by, for example distributing flyers and posters in multiple languages, radio messaging, texting, phone calls, emailing and sending letters and reminders, are required to enhance participants’ recruitment and retention in interventions [ 8 , 9 ]. Gaining support from community leaders [ 10 ], community-based recruitment, recruitment of additional bilingual staff, contacting eligible potential participants with trained staff, flexible timings (weekends and evenings), and a suitable study site are also reported as important recruitment and retention strategies [ 8 ]. Moreover, building trust with participants [ 11 ], collaborating and developing relationships with communities [ 4 , 12 ], and friend referral [ 9 ] may play a critical role in facilitating recruitment and retention of participants into studies. Additionally, funding community-based interventions [ 12 ], providing financial incentives to assist with the costs of participation, for example, travel [ 9 , 13 ] and keeping study participants engaged through newsletters and social gatherings [ 3 ] may demonstrate commitment in increasing participants’ recruitment and retention into interventions. These strategies may guide researchers and staff towards effective recruitment and retention of study participants into community-based obesity prevention interventions.
To date, there are limited systematic reviews that brings together evidence to understand common barriers and facilitators of recruitment and retention of participants from ethnic minorities and migrant populations in community-based obesity prevention trials. A 2021 systematic review identified barriers (e.g., time constraints, limited understanding of clinical trials, consent complexity, inadequate transportation and limited childcare benefits) and facilitators (e.g. benefits for participants and others, financial incentives, friend referral, support, and recommendations from medical practitioners) to children’s participation in obesity interventions in the United States, Australia, Europe, and Canada [ 7 ]. Other reviews on the barriers and facilitators to ethnic and migrant populations’ participation in interventions were conducted in the United Kingdom [ 14 ] and the US [ 5 , 15 , 16 ]. However, these systematic reviews did not include ethnic minorities and migrants from most countries of the Organisation of Economic Cooperation and Development (OECD) and did not explore the barriers and facilitators of their effective recruitment and retention specifically in community-based obesity prevention trials. Therefore, there is limited understanding about the barriers and facilitators of recruitment and retention of ethnic minorities in community-based obesity prevention randomised control trials (RCTs). This systematic review aims to address the gaps in previous research through identifying, collating, appraising, and synthesising available literature on the recruitment and retention rates of ethnic minorities and migrants, and the related barriers and facilitators to effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention RCTs in OECD countries. Our findings will inform practice and support the development of empirical studies and programme evaluations, and the execution of community-based obesity prevention RCTs designed for ethnic minorities and migrants in OECD countries.
A systematic review was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [ 17 ]. The protocol was registered with The International Prospective Register of Systematic Reviews (PROSPERO: ID: CRD42022326690).
Search strategy
A comprehensive search of peer-reviewed articles from five computerised bibliographic databases using relevant MeSH terms or subheadings of key words was conducted. The databases searched were CINAHL, Cochrane, Embase, Medline and PsychInfo. Google and Google Scholar were searched to identify any additional studies. Search terms were adapted to meet the requirements of different databases. Supplementary Table 1 provides the search terms used.
Inclusion criteria
The Participants, Intervention, Comparison, and Outcomes (PICO) framework was used to guide our eligibility criteria, provided below [ 18 ]. This review included randomised controlled trials (RCTs), cluster randomised trials or quasi-experimental study designs for obesity interventions for minority communities, including adults, adolescents, and children in OECD countries [ 19 ]. Studies published in English from January 2000 to March 2022 were included in this review. The year 2000 was chosen as the base year due to the rapid rise in migration globally [ 20 ]. Studies were included if they were peer-reviewed and explored the barriers and/or facilitators of recruitment and/or retention of ethnic minorities, migrants and/or indigenous populations in community-based obesity prevention RCTs. This study defined recruitment as a process of finding and enrolling eligible participants in an RCT. Retention is defined as an RCT’s capacity to keep participants enrolled and engaged during its entire duration [ 21 ]. Ethnic minorities are groups of individuals who are distinct from majority populations regarding race, ethnicity, nationality, culture, language, and religion. Migrants are any individuals who changed his/her usual country of residence for various reasons, including work, education, family reunification, or seeking asylum [ 22 ].
Study eligibility criteria using the PICO framework.
Exclusion criteria
Studies that did not highlight the barriers and/or facilitators of recruitment and/or retention of ethnic minorities, migrants and/or indigenous populations in community-based obesity prevention RCTs were excluded. Studies that met the inclusion criteria but provided scant data were excluded, determined via discussion between two researchers (MNH and NW). This review also excluded grey literature documents, review papers, conference presentations, protocols and studies not published in English.
The retrieved articles were imported from each database into an Endnote library. Duplicates were removed in Endnote before screening in MS Excel. Title and abstract of the identified studies were screened by two authors in MS Excel (MNH and NW). Reasons for exclusion were recorded at the full-text stage (i.e. no information on outcomes, barriers and facilitators of effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention programmes in industrialised countries). Full texts of all studies were reviewed by the second author (MNH) and a sample of 30% were reviewed by the primary author (NW). Any discrepancies between two reviewers were resolved through discussion with a third reviewer (AR).
Data extraction
MNH and NW conducted the data extraction of included studies in MS Excel. Quantitative and qualitative data from mixed methods studies were extracted separately (see Table 1 ). Data extracted from studies included general information (authors, publication year, country, research design, data analysis, participants’ ethnicity, sample size, and main findings on barriers and facilitators of effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention programmes). Two authors (MNH and NW) reviewed the entire data extraction file to ensure accuracy and consistency.
Methodological quality and risk of bias
Methodological quality and risk of bias were independently assessed by two authors (MNH and NW) using the CASP tool for RCTs [ 23 ] and the Cochrane risk of bias tool [ 24 ]. Nine criteria of the CASP tool were used to assess the methodological quality [ 23 ]. Studies with scores from 7 to 9 were considered ‘high’ quality, scores from 4–6 were ‘medium’ quality and 0–3 were classified as ‘low’ quality (Supplementary Table 2 ). The Cochrane risk of bias tool determines how well a study has addressed potential biases in its design and analysis [ 24 ]. The risk of bias of included studies was assessed using six domains of the Cochrane risk of bias tool (Supplementary Table 3 ). Discrepancies were discussed by both reviewers (MNH and NW), with a third reviewer (AR) brought in to reach a consensus for any disagreements.
Data synthesis
Quantitative studies included in the review varied in study design, methods, definitions and measurement of outcomes and explanatory variables. Although a pooled analysis of proportions was performed to combine the results of included studies on participants’ recruitment and retention in obesity prevention RCTs, a meta-regression was not possible due to inconsistent reporting or marked clinical heterogeneity in study populations, interventions, and the outcomes studied [ 25 ]. The “metaprop” Stata 9 (version 16.0, StataCorp, College Station, TX, USA) command was used to generate forest plots for the ethnic minority and migrant share of the sample size and the proportion of retention (those in the intervention who completed it). Each forest plot shows the proportion and associated 95% confidence intervals (CI), and corresponding weight. A test of heterogeneity showed a high level of inconsistency ( I 2 > 50%), hence a random-effect model was used for the pooled analysis [ 26 ]. Sensitivity analyses were conducted to examine the effect of outliers comparing the pooled prevalence before and after removal of one study at a time [ 27 ].
Additionally, a meta-ethnographic approach was used to synthesis evidence of included studies [ 28 ], this approach is increasingly being recognised to synthesise data in reviews [ 29 ]. The meta-ethnographic approach involved four stages: (1) identifying metaphors and common findings by re-reading the studies to gain familiarity within the data and identify themes and patterns in each study; (2) determining how the study findings were related by comparing the thematic analysis of all studies: (3) reciprocal translation of studies by comparing the themes of all studies, this included comparison and matching of themes across papers to ensure that the key themes across studies are captured; and lastly (4) synthesising translations which form a line of argument for the description of findings. This approach allowed to identify relationships between studies, which led to a better understanding of effective recruitment and retention strategies of ethnic minorities and migrants in community-based obesity prevention trials. It allowed to identify common factors across studies and reciprocal translation of studies to inform findings around recruitment and retention strategies of ethnic minorities and migrants.
In total 772 records were identified from five databases, Google, and Google Scholar searches. After removing duplicates and conducting the screening of titles, abstracts, and full texts, 25 studies were identified for inclusion in this systematic review. The reasons for excluding studies were: (1) not conducted in OECD countries, (2) not peer-reviewed, (3) not an RCT, and (4) full-text not available. Search results at each stage of the review process are illustrated in Fig. 1 , using the PRISMA diagram.

Systematic search results in PRISMA flow chart.
Characteristics of included studies
This review included 25 studies on recruitment and retention of ethnic minorities in obesity prevention RCTs. Of the 25 studies, majority of the studies were conducted in the USA ( N = 23) [ 2 , 3 , 8 , 9 , 10 , 13 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ] except 1 that was conducted in UK [ 46 ] and 1 in Australia [ 47 ]. Seven RCTs were exclusively conducted among Latino Americans [ 30 , 34 , 38 , 39 , 40 , 41 , 44 ], 4 among African Americans [ 31 , 35 , 37 , 45 ], and 1 among Mexican descent immigrants in the USA [ 43 ] and 1 among Brazilian immigrants in the USA [ 11 ]; 3 RCTs combined Latino and African American population [ 8 , 33 , 36 ], 1 combined Hispanic and Latino population [ 32 ] and 1 combined Hispanic and non-Hispanic black population [ 3 ]. The remaining studies were a combination of populations from different ethnic backgrounds [ 2 , 9 , 10 , 13 , 42 , 46 ]. The studies used various statistical techniques for data analysis, including descriptive statistics (proportion, percentage, mean, interquartile range, standard deviation), inferential statistics (Chi-square, Fisher’s exact tests, t -test, ANOVA, Wilcoxon and Kruskal–Wallis tests, regression analysis). Few studies did not mention any analytical techniques.
Recruitment and retention of ethnic minorities in obesity prevention RCTs
This review found that the pooled proportion of recruitment of ethnic minorities in obesity prevention programmes and trials was 64% (Fig. 2 ). Of those recruited, the pooled proportion of retention of ethnic minorities in obesity prevention programmes and trials was 71% (Fig. 3 ).

Pooled analysis of the proportion of the sample that is ethnic minorities and migrants.

Proportion of ethnic minority and migrants who completed the programme.
Barriers to effective recruitment and retention
The meta-ethnographic analysis of studies included in this review provide a range of barriers to the effective recruitment and retention of ethnic minorities and migrants in community-based interventions in OECD countries. These findings are summarised below.
Barriers related to study characteristics
Studies reported study characteristics contributing to the recruitment and retention of ethnic minorities in RCTs, including intervention types, dose (duration, frequency), and involvement types. For example, studies discussed the different types of interventions aimed at recruiting and retaining participants, such as lifestyle and behavioural interventions [ 30 , 34 , 41 , 46 ], interactive group classes on lifestyles [ 44 ], nutrition education and counselling by a dietitian [ 31 ], curriculum on nutrition and physical activity [ 9 ], bicycling [ 33 , 36 ], exercise [ 37 ], behavioural weight management intervention [ 39 ], and weight-loss interventions [ 40 ]. Types of involvement (physical, face-to-face delivery of interventions [ 37 , 44 ] telephone and online delivery of intervention [ 44 , 46 ], also affected participants’ recruitment and retention in RCTs. The duration of the RCTs varied; one for 3 years [ 2 ], one for 2 years and 7 months [ 41 ], three ran for 2 years [ 3 , 9 , 40 ], one for 18 months [ 45 ], and three for 1 year [ 31 , 33 , 36 ]. The rest lasted for less than 6 months [ 36 , 43 , 48 ]. Limited duration of intervention of less than 6 months contributed to decreased participants’ recruitment and retention [ 46 ].
Limited access to study sites
Three studies with ethnic minorities, such as, American Indians [ 10 ], Latinos [ 30 ], and African Americans [ 31 ], highlighted the limited access to study site as a reason to not to be part of the recruitment process. Their participation was impacted by long travel distances [ 10 ] and transportation problems [ 2 ], including limited transport, problems with cars and high travel costs [ 11 , 31 , 41 ].
Time constraints
Time conflict was commonly reported across several ethnic minorities and migrant communities (e.g. Latinos, Brazilian immigrants, African Americans, etc.) [ 2 , 11 , 31 , 46 , 47 ]. These time conflicts were due to participants’ commitments to family activities, jobs [ 2 , 46 ], childcare, housing and limited personal time [ 47 ], affecting their participation [ 31 ]. Participants’ limited availability of time in the afternoon and evening due to children’s after-school activities, work commitments and children’s meals and bedtimes also impacted their participation [ 46 ].
Lack of trust
Four studies mentioned a lack of trust as a barrier to effective recruitment and retention of ethnic and migrant communities [ 2 , 10 , 30 , 35 ]. According to these studies, participants had a history of distrust with researchers particularly medical care and research, including previous experience of disrespect, poor quality of medical care and researchers not following through commitments. These studies established trust with communities through repeated contacts, listening, shared learning, bi-directional communication, following through on commitments and mutual respect.
Perceived fear and anxiety
Perceived fear and anxiety were a barrier reported in three US studies conducted among Latinos [ 38 ], Spanish-speaking adults of Mexican origin [ 43 ], and Brazilian immigrants [ 11 ]. Many ethnic migrants, such as Mexican Americans [ 43 ] and Latinos [ 38 ], were afraid of participating in interventions due to fear and anxiety produced by strict anti-illegal immigration laws [ 43 ]. Fear of revealing information to researchers also discouraged the participants from taking part in the programmes [ 11 ].
Other barriers to recruitment and retention
Other barriers to recruitment and retention included a lack of safety for participants with special needs such as walking difficulty [ 30 ], language barriers, low levels of health and intervention literacy [ 43 ], and perceived stigma [ 38 ]. The current review also found other barriers of participation-associated costs [ 11 ], difficulty in maintaining a large pool of potential participants for contact, and prolonged waits in receipt of provider approval [ 3 ].
Facilitators of effective recruitment and retention
Facilitators of effective recruitment and retention of ethnic minorities and migrants in RCTs are summarised below. Figures 4 and 5 outline the most effective recruitment and retention strategies, study wise description of these is provided in Supplementary Table 4 .

Facilitators of effective recruitment.

Facilitators of effective retention.
Using multiple communication channels
The use of multiple communication channels, including emails, flyers, frequent contacts with participants and sending weekly reminders via telephone and mobile text, etc., were reported as essential to facilitate participants’ recruitment and retention. Twelve studies highlighted communication as a facilitator, these study participants included low-income Latino [ 30 , 34 , 41 ] and African Americans [ 13 , 33 , 36 ], Hispanic immigrants [ 3 , 32 ], non-Hispanic/Latino Americans [ 39 ], mothers and children from Brazil, Latin America, and Haiti [ 9 ], Spanish-speaking adults of Mexican origin [ 43 ], rural American Indian and Hispanic children [ 10 ], and Brazilian immigrants in the US [ 11 ]. Moreover, university communication channels (e-mail lists) helped disseminate study information among potential study participants and facilitated their recruitment in research [ 43 ].
Employing culturally sensitive strategies
Eight of the 25 studies conducted with low-income ethnic minorities and migrants living in the US [ 2 , 10 , 11 , 33 , 35 , 40 , 43 ] and Australia [ 47 ] documented culturally sensitive strategies (e.g. cultural competency, recruiting bilingual and culturally sensitive staff, translating recruitment and study materials into participants’ languages) as a critical facilitator of recruitment and retention of participants. For example, a study with Brazilian immigrants in the US found that staff member’s understanding of participants’ sociocultural context and the application of linguistically and culturally sensitive recruitment strategies helped meet the needs of participants and facilitated their successful recruitment and enrolment [ 11 ]. Bilingual staff who were culturally competent and sensitive to participants were able to effectively deliver study materials and presentations in the participant’s languages [ 2 , 10 , 33 , 35 , 40 , 43 ]. Such culturally sensitive strategies increased participants’ recruitment and retention, in particular when bilingual and bicultural staff were provided with in-depth training before recruiting participants in health research [ 40 ].
Incentives and compensation for participants
Monetary incentives (gift cards, recipe books, cash, reimbursements for transportation, parking, childcare) and compensation for participants after data collection helped reduce barriers to participants’ recruitment and retention with low-income and multi-ethnic communities [ 2 ], including African-American women [ 13 , 37 ], children from Hispanic and Latino communities [ 32 , 44 ] and rural American Indian and Hispanic children [ 10 ]. A US bases RCT reported that having an adequate budget helped provide a financial base for financial incentives to the participants [ 2 ]. For example, providing participants with $25 for the completion of the baseline assessment, $50 for the completion of assessments at weeks 12 and 24, and $25 for the completion of mini-assessments kept participants engaged in childhood obesity prevention and prevention studies [ 2 ].
Participant convenience
As described in Table 1 , participants’ convenience was one of the most common facilitators, appearing in 7 of the 25 included studies. The use of a dedicated phone [ 13 ], the time [ 10 ] and locations convenient to participants [ 2 ] and providing scheduling flexibility outside participants’ regular work for completing studies, addressed barriers to participants’ recruitment and retention in studies [ 7 , 32 , 36 ].
Recruiting community leaders/local champions
Three RCTs, all conducted in the USA, reported recruiting local champions to contact potential participants, schedule interviews with them and recruit them for studies [ 2 , 10 , 30 ]. The largest study, which recruited rural American Indian and Hispanic children, found that recruiting community leaders, who hold a strong position in the community, can serve as a primary contact to assist with the project, including advocating the project and promoting its benefits [ 10 ]. The second RCT included participants from low-income, racially diverse parent–child dyads, reported that strengthening connections with the local community leaders and soliciting information from them helped retain the participants [ 2 ]. Building trust with the community leaders and strengthening relationships with them helped disseminate study materials and sustained their participation in the interventions [ 30 ].
On-site/in-person recruitment
Studies with low-income African Americans [ 35 ], Brazilian immigrants born in the US [ 11 ], and rural American Indian and Hispanic children [ 10 ] that had on-site/in-person recruitment enhanced participant engagement. For instance, Lindsay et al. [ 11 ] found that on-site in-person recruitment at church (e.g., mass and other church events), and private social and community events (e.g., health and cultural fairs), were effective recruitment strategies in health research.
Summary of key findings
This systematic review reported on the recruitment and retention of ethnic minorities in community-based obesity prevention RCTS with the pooled proportions of recruitment and retention at 64% and 71% respectively. Evidence on recruitment and retention rates is limited and varied across literature. For instance a systematic review reports considerable variability in recruitment rates (median 66.4%; interquartile range = 42.7–85.2) and retention rates (median 80.5%; IQR = 68.5–89.5) [ 49 ]. While our findings indicate a high pooled proportion of recruitment of 64%, this could be due to successful strategies that are culturally sensitive and based on participants convenience. Our findings suggest of those recruited, the pooled proportion of retention of ethnic minorities in obesity prevention programmes and trials was 71%, which further indicates the success of strategies employed for retention of participants.
Our findings revealed multiple barriers to effective recruitment of ethnic minority and migrants into obesity prevention programmes, including African Americans, American Indians, Mexican Americans, Hispanic Latinos, and Brazilian immigrants in the US, Arabic- and Chinese Australian and young adults living in UK, Australia, and Ireland. These included limited access to study sites, time constraints, limited trust, perceived fear, and anxiety. The identified barriers in this systematic review are consistent with those identified previously. For instance, Clayton et al. found lack of transportation made accessing the study sites difficult to access and time constraints to get to the clinic amidst other commitments [ 7 ]. Similarly, George et al. revealed mistrust and consequent fear of participation as a key barrier of recruitment and participation of migrants and ethnic minorities in the US in clinical research [ 5 ].
Our review findings highlight facilitators of effective recruitment and retention of ethnic minorities in community-based obesity prevention programmes. These included use of multiple communication channels, incentives, recruiting community champions, participant convenience and employing culturally sensitive strategies. Research suggests community outreach and in-person on-site recruitment at recreational centres, schools, and faith-based organisations such as churches, temples and mosques, as proven strategies for successful recruitment and ongoing participation in clinical research [ 2 ]. Similarly, convenience to participants such as flexible timings (weekends and evening), and a suitable study site also contributed to successful recruitment and retention of African American and Latino youth participants in research [ 8 ]. Our findings concur with research that highlights a combination of communication tools such as involving consistent follow-up and frequent communications by tools such as distributing flyers and posters in multiple languages, radio messaging, texting, phoning, emailing and sending letters and reminders, are required to enhance participants’ recruitment and retention [ 8 , 9 ]. Financial incentives for participants is also an effective tool to improve retention of participants in research [ 5 , 49 ].
Application of multiple strategies together can facilitate effective recruitment and retention
Review findings suggest that using multiple strategies can help reduce barriers to participants’ recruitment and retention in studies and facilitate effective recruitment and retention of ethnic minorities and migrants in obesity prevention programmes, consistent with previous research [ 50 ]. Further our findings suggest that multiple strategies need to embed culturally competent and safe recruitment practices to attract and recruit ethnic minorities. Culturally competent recruitment practices promote a research environment that allows researchers to recruit effectively in cross-cultural situations [ 51 ], while culturally safe recruitment practices prioritise shared respects, knowledge reciprocity, and experience in a research environment that makes research participants feel socially, emotionally, and spiritually safe [ 52 ]. Israel et al. indicate that such practices should meet 8 criteria: (1) recognise the collective nature of ethnic minorities’ communities as a unit of identity (e.g. membership in a family, friendship network, or geographic neighbourhood); (2) build on strengths, resources, and relationships that exist within communities of identity (e.g. recognising, supporting, and expanding skills, assets, and social structures and social processes that enable community members to work together); (3) facilitate collaborative partnerships in all phases of the research implementation; (4) Integrate knowledge and action for mutual benefit of all partners; (5) promote a co-learning and empowering process that attends to social inequalities; (6) involve a cyclical and iterative process; (7) Address health from both positive and ecological perspectives; and (8) Disseminate findings and knowledge gained to all partners [ 53 ]. Implicit in these criteria is that ethnic minorities need to be well informed research participants and have the agency to make decision. This is why our findings emphasise the importance of multiple field‐based strategy and snowballing strategies that can work at different levels and help reduce participants’ barriers to participation in health research such as community mistrust of the research process, the need to culturally appropriate compensation, and overcoming language barrier and low level of literacy. Recruitment strategies might include use of flyers, newspaper advertisements, community outreach, snowball, and social media [ 54 ]. Retention strategies might include rapport with ongoing engagement, post-visit phone calls, fair compensation, flexibility, frequent reminders, and being respectful and sensitive [ 54 ]. Therefore, researchers can effectively recruit and retain participants by reducing barriers if they build rapport with participants via multiple communication channels, addressing their needs (e.g. flexibility in schedules and techniques, incentives) and recruiting them in person [ 55 ]. Employing bi-cultural staff and investing in the their training may further enhance their skills in recruitment [ 40 ] and increase recruitment and retention rates [ 55 ], thus increasing generalisability [ 56 ].
Implications of recruitment and retention
Given that the success of a project largely depends on the effective recruitment and retention of participants, addressing the barriers whilst promoting facilitators can enhance ethnic minorities and migrants’ participation and retention in community-based obesity prevention programmes. As multiple social factors, including stigma [ 38 ], distrust [ 35 ], and limited health literacy [ 43 ], can hinder participants’ enrolment in research, providing staff with appropriate training on cultural sensitivity may enhance the participation of diverse ethnic and migrant communities. It is also equally important to provide ethnic minorities with relevant education and brief them about concerns. For example, an education session for African Americans may include a historical context of distrust and its related causes. During these sessions, participants can openly discuss the issues [ 5 ]. Moreover, allowing participants to ask questions about any concerns about the research process and protective measures for participants may address their fear and anxiety associated with their participation in the studies. Furthermore, when a clinical trial involves populations from low-income ethnic minorities and migrants, there may be a requirement to approach participants using various communication channels [ 43 ] and community champions [ 10 ], with scheduling flexibility [ 32 ] and incentives [ 37 ]. These efforts may help recruit and retention participants from low-income multi-cultural communities living in high-income countries in a culturally appropriate manner [ 5 ]. Such approaches may reduce the barriers to recruitment and retention and facilitate their effective participation in health research.
Strengths and limitations
Our study has several strengths. First, to the best of our knowledge, this is the first study to systematically review the barriers and facilitators of effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention trials in OECD countries. Second, the application of a systematic approach [ 17 ] to search data from relevant scientific databases enabled the revealing most available papers on the subject. Third, we used a comprehensive list of search terms covering many ethnic minorities and migrants in OECD countries and conducted these searches across five electronic databases, Google and Google Scholar. Finally, we used rigorous and objective measures to assess for eligibility and evaluate for risk of bias. However, our review does have a few limitations. The review only included studies written in English due to time and resource constraints. Thus, this review may have missed some relevant papers published in other languages. Another limitation is that the review was limited to articles focusing on the barriers and facilitators of effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention trials in OECD countries. As a result, valuable accounts on the barriers and facilitators of effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention trials beyond OECD countries were excluded. Lastly, majority of the studies were conducted in the US, potentially limiting their representativeness for recruitment and retention practices across all OECD countries.
Our systematic review of the peer-reviewed literature found a low recruitment rate and identified many barriers and facilitators of effective recruitment and retention of ethnic minorities and migrants in community-based obesity prevention programmes. However, most studies we reviewed were conducted with ethnic minorities and migrants living in the US. Our review points to the urgent need to conduct more research focusing on multicultural ethnic minorities living in other OECD countries. Our review suggests the importance of undertaking culturally appropriate multiple recruitments and retention strategies to minimise barriers and facilitate the effective recruitment and retention of ethnic minorities and migrants in community-based research.
Data availability
All data generated or analysed during this study are included in this published article.
Fleming J, Kamal A, Harrison E, Hamborg T, Stewart-Brown S, Thorogood M, et al. Evaluation of recruitment methods for a trial targeting childhood obesity: families for Health randomised controlled trial. Trials. 2015;16:1–10.
Article Google Scholar
Cui Z, Truesdale KP, Robinson TN, Pemberton V, French SA, Escarfuller J, et al. Recruitment strategies for predominantly low-income, multi-racial/ethnic children and parents to 3-year community-based intervention trials: Childhood Obesity Prevention and Treatment Research (COPTR) Consortium. Trials. 2019;20:1–10.
Article CAS PubMed PubMed Central Google Scholar
Warner ET, Glasgow RE, Emmons KM, Bennett GG, Askew S, Rosner B, et al. Recruitment and retention of participants in a pragmatic randomized intervention trial at three community health clinics: results and lessons learned. BMC Public Health. 2013;13:1–12.
Stockton MB, McClanahan BS, Lanctot JQ, Klesges RC, Beech BM. Identification of facilitators and barriers to participation in weight gain prevention research by African American girls. Contemp Clin Trials. 2012;33:38–45.
Article PubMed Google Scholar
George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104:e16–31.
Article PubMed PubMed Central Google Scholar
Nagler RH, Ramanadhan S, Minsky S, Viswanath K. Recruitment and retention for community-based eHealth interventions with populations of low socioeconomic position: strategies and challenges. J Commun. 2013;63:201–20.
Clayton P, Connelly J, Ellington M, Rojas V, Lorenzo Y, Trak‐Fellermeier MA, et al. Facilitators and barriers of children’s participation in nutrition, physical activity, and obesity interventions: a systematic review. Obes Rev. 2021;22:e13335.
DeFrank G, Singh S, Mateo KF, Harrison L, Rosenthal A, Gorman A, et al. Key recruitment and retention strategies for a pilot web-based intervention to decrease obesity risk among minority youth. Pilot Feasibility Stud. 2019;5:1–13.
Metayer N, Boulos R, Tovar A, Gervis J, Abreu J, Hval E, et al. Recruitment of new immigrants into a randomized controlled prevention trial: the live well experience. J Prim Prev. 2018;39:453–68.
Cruz TH, Davis SM, FitzGerald CA, Canaca GF, Keane PC. Engagement, recruitment, and retention in a trans-community, randomized controlled trial for the prevention of obesity in rural American Indian and Hispanic children. J Prim Prev. 2014;35:135–49.
Lindsay AC, Wallington SF, Rabello LM, Alves ADSM, Arruda CAM, Rocha TC, et al. Faith, family, and social networks: effective strategies for recruiting Brazilian immigrants in maternal and child health research. J Racial Ethn Health Disparities. 2021;8:47–59.
Holston D, Stroope J, Cater M. Facilitators and barriers to implementation of community-based socio-ecological approaches to obesity prevention among Cooperative Extension Agents. J Hum Sci Ext. 2021;9:139–55.
Google Scholar
Nicholson LM, Schwirian PM, Klein EG, Skybo T, Murray-Johnson L, Eneli I, et al. Recruitment and retention strategies in longitudinal clinical studies with low-income populations. Contemp Clin Trials. 2011;32:353–62.
Quay TA, Frimer L, Janssen PA, Lamers Y. Barriers and facilitators to recruitment of South Asians to health research: a scoping review. BMJ Open. 2017;7:e014889.
Hughes TB, Varma VR, Pettigrew C, Albert MS. African Americans and clinical research: evidence concerning barriers and facilitators to participation and recruitment recommendations. Gerontologist. 2017;57:348–58.
Nicholson LM, Schwirian PM, Groner JA. Recruitment and retention strategies in clinical studies with low-income and minority populations: progress from 2004–2014. Contemp Clin Trials. 2015;45:34–40.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7:1–6.
Organisation for Economic Co-operation and Development. Our global reach. 2022. https://www.oecd.org/about/members-and-partners/ .
Akombi-Inyang B, Huda MN, Schutte AE, Macniven R, Lin S, Rawstorne P, et al. The association between post-migration nutrition and lifestyle transition and the risk of developing chronic diseases among Sub-Saharan African migrants: a mixed method systematic review protocol. Int J Environ Res Public Health. 2021;18:4706.
Robinson L, Adair P, Coffey M, Harris R, Burnside G. Identifying the participant characteristics that predict recruitment and retention of participants to randomised controlled trials involving children: a systematic review. Trials. 2016;17:1–17.
Hannigan A, O’Donnell P, O’Keeffe M, MacFarlane A. How do variations in definitions of “migrant” and their application influence the access of migrants to health care services? World Health Organization. Regional Office for Europe; 2016.
Critical Appraisal Skills Programme. CASP checklist: 11 questions to help you make sense of a Randomised Controlled Trial. 2018. https://casp-uk.net/wp-content/uploads/2018/01/CASP-Randomised-Controlled-Trial-Checklist-2018.pdf .
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Hartling L, Shaik MS, Tjosvold L, Leicht R, Liang Y, Kumar M. Music for medical indications in the neonatal period: a systematic review of randomised controlled trials. Arch Dis Child Fetal Neonatal Ed. 2009;94:F349–54.
Article CAS PubMed Google Scholar
Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72:1–10.
Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37:1148–57.
George N, Hare R. Meta-ethnography. Thousand Oaks: SAGE Publications, Inc; 1988.
Feast A, Orrell M, Charlesworth G, Poland F, Featherstone K, Melunsky N, et al. Using meta-ethnography to synthesise relevant studies: capturing the bigger picture in dementia with challenging behaviour within families. London: SAGE Publications. Sage research methods cases psychology. 2018.
Marquez DX, Aguinaga S, Castillo A, Hughes SL, Der Ananian C, Whitt-Glover MC. Ojo! What to expect in recruiting and retaining older Latinos in physical activity programs. Transl Behav Med. 2019;19:1566–1572.
Srivastava G, Palmer KD, Ireland KA, McCarthy AC, Donovan KE, Manders AJ, et al. Shape-up and eat right families pilot program: feasibility of a weight management shared medical appointment model in African-Americans with obesity at an urban academic medical center. Front Pediatr. 2018;6:101.
Heerman WJ, Burgess LE, Escarfuller J, Teeters L, Slesur L, Liu J, et al. Competency Based Approach to Community Health (COACH): the methods of a family-centered, community-based, individually adaptive obesity randomized trial for pre-school child-parent pairs. Contemp Clin trials. 2018;73:1–7.
Dressel A, Schneider R, DeNomie M, Kusch J, Welch W, Sosa M, et al. Assessing health promotion interventions: limitations of traditional research methods in community-based studies. Health Promot Pract. 2018;19:573–80.
Crespo NC, Talavera GA, Campbell NR, Shadron LM, Behar AI, Slymen D, et al. A randomized controlled trial to prevent obesity among Latino paediatric patients. Pediatr Obes. 2018;13:697–704.
Lynch E, Mack LJ, Karavolos K, Avery E, Liebman R, Keim KS, et al. Recruitment and baseline characteristics of participants in the lifestyle improvement through food and exercise (LIFE) study. J Health Care Poor Underserved. 2017;28:463–86.
Bernstein R, Schneider R, Welch W, Dressel A, DeNomie M, Kusch J, et al. Biking for health: results of a pilot randomized controlled trial examining the impact of a bicycling intervention on lower-income adults. WMJ. 2017;116:154–60.
PubMed PubMed Central Google Scholar
Pekmezi D, Ainsworth C, Joseph R, Bray MS, Kvale E, Isaac S, et al. Rationale, design, and baseline findings from HIPP: a randomized controlled trial testing a home-based, individually-tailored physical activity print intervention for African American women in the Deep South. Contemp Clin Trials. 2016;47:340–8.
Daly P, Pace T, Berg J, Menon U, Szalacha LA. A mindful eating intervention: a theory-guided randomized anti-obesity feasibility study with adolescent Latino females. Complement Ther Med. 2016;28:22–8.
Coday M, Richey P, Thomas F, Tran QT, Terrell SB, Tylavsky F, et al. The recruitment experience of a randomized clinical trial to aid young adult smokers to stop smoking without weight gain with interactive technology. Contemp Clin Trials Commun. 2016;2:61–8.
Rosas LG, Thiyagarajan S, Goldstein BA, Drieling RL, Romero PP, Ma J, et al. The effectiveness of two community-based weight loss strategies among obese, low-income US Latinos. J Acad Nutr Diet. 2015;115:537–50.e2.
Koniak-Griffin D, Brecht ML, Takayanagi S, Villegas J, Melendrez M, Balcazar H. A community health worker-led lifestyle behavior intervention for Latina (Hispanic) women: feasibility and outcomes of a randomized controlled trial. Int J Nurs Stud. 2015;52:75–87.
Anderson LM, Symoniak ED, Epstein LH. A randomized pilot trial of an integrated school-worksite weight control program. Health Psychol. 2014;33:1421–5.
Vincent D, McEwen MM, Hepworth JT, Stump CS. Challenges and success of recruiting and retention for a culturally tailored diabetes prevention program for adults of Mexican descent. Diabetes Educ. 2013;39:222–30.
Arauz Boudreau AD, Kurowski DS, Gonzalez WI, Dimond MA, Oreskovic NM. Latino families, primary care, and childhood obesity: a randomized controlled trial. Am J Prev Med. 2013;44:S247–57.
Kumanyika SK, Shults J, Fassbender J, Whitt MC, Brake V, Kallan MJ, et al. Outpatient weight management in African-Americans: the Healthy Eating and Lifestyle Program (HELP) study. Prev Med. 2005;41:488–502.
Griffin T, Sun Y, Sidhu M, Adab P, Burgess A, Collins C, et al. Healthy Dads, Healthy Kids UK, a weight management programme for fathers: feasibility RCT. BMJ Open. 2019;9:e033534.
Marshall S, Taki S, Love P, Laird Y, Kearney M, Tam N, et al. Feasibility of a culturally adapted early childhood obesity prevention program among migrant mothers in Australia: a mixed methods evaluation. BMC Public Health. 2021;21:1–18.
Heerman WJ, Cole J, Teeters L, Lane T, Burgess LE, Escarfuller J, et al. Qualitative analysis of COACH: a community-based behavioral intervention to reduce obesity health disparities within a marginalized community. Contemp Clin Trials Commun. 2019;16:100452.
Bricca A, Swithenbank Z, Scott N, Treweek S, Johnston M, Black N, et al. Predictors of recruitment and retention in randomized controlled trials of behavioural smoking cessation interventions: a systematic review and meta-regression analysis. Addiction. 2022;117:299–311.
Preston NJ, Farquhar MC, Walshe CE, Stevinson C, Ewing G, Calman LA, et al. Strategies designed to help healthcare professionals to recruit participants to research studies. Cochrane Database Syst Rev. 2016;2:MR000036.
PubMed Google Scholar
Hughson J-A, Woodward-Kron R, Parker A, Hajek J, Bresin A, Knoch U, et al. A review of approaches to improve participation of culturally and linguistically diverse populations in clinical trials. Trials. 2016;17:263.
Williams R. Cultural safety-what does it mean for our work practice? Aust N Z J Public Health. 1999;23:213–4.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202.
Otado J, Kwagyan J, Edwards D, Ukaegbu A, Rockcliffe F, Osafo N. Culturally competent strategies for recruitment and retention of African American populations into clinical trials. Clin Transl Sci. 2015;8:460–6.
Felsen CB, Shaw EK, Ferrante JM, Lacroix LJ, Crabtree BF. Strategies for in-person recruitment: lessons learned from a New Jersey primary care research network (NJPCRN) study. J Am Board Fam Med. 2010;23:523–33.
Badr H, Krebs P. A systematic review and meta‐analysis of psychosocial interventions for couples coping with cancer. Psychooncology. 2013;22:1688–704.
Download references
Acknowledgements
This review is part of a study externally funded by the National Health and Medical Research Council (NHMRC) of Australia.
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and affiliations.
School of Social Sciences, Humanitarian and Development Research Initiative (HADRI), Western Sydney University, Sydney, NSW, 2751, Australia
Discipline of Psychiatry and Mental Health, School of Clinical Medicine, University of New South Wales, Sydney, NSW, 2052, Australia
Md. Nazmul Huda
Charles Perkins Centre, University of Sydney, Sydney, NSW, 2050, Australia
Timothy Gill
Murdoch Children’s Research Institute, Parkville, VIC, 3052, Australia
Julie Green
Department of Paediatric, University of Melbourne, Parkville, VIC, 3052, Australia
School of Medicine, Western Sydney University, Campbelltown, NSW, 2560, Australia
Translational Health Research Institute (THRI), Western Sydney University, Campbelltown, NSW, 2560, Australia
Andre M. N. Renzaho
You can also search for this author in PubMed Google Scholar
Contributions
AMNR and NH conceptualised the manuscript; NH and NW developed the methodology and conducted the research; AMNR validated the methodology; NH and NW undertook the formal analysis and wrote the original draft. All authors reviewed the results and edited the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Nidhi Wali .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Search terms, quality assessment, risk of bias assessment, factors for effective recruitment and retention, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wali, N., Huda, M.N., Gill, T. et al. A systematic review of recruitment and retention of ethnic minorities and migrants in obesity prevention randomised controlled trials. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01545-z
Download citation
Received : 14 November 2023
Revised : 13 May 2024
Accepted : 13 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1038/s41366-024-01545-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Res Med Sci
- v.19(10); 2014 Oct
Controlling childhood obesity: A systematic review on strategies and challenges
Roya kelishadi.
Department of Pediatrics, Child Growth and Development Research Center, Research Institute for Primary Prevention of Non-communicable Disease, Isfahan University of Medical Sciences, Isfahan, Iran
Fatemeh Azizi-Soleiman
1 School of Nutrition and Food Sciences, Isfahan University of Medical Sciences, Isfahan, Iran
Background:
Childhood obesity is a global health problem with short- and long-term health consequences. This systematic review presents a summary of the experiences on different family-, school-, and clinic-based interventions.
Materials and Methods:
Electronic search was conducted in MEDLINE, PubMed, ISI Web of Science, and Scopus scientific databases. We included those studies conducted among obese individuals aged up to 18 years. Our search yielded 105 relevant papers, 70 of them were conducted as high quality clinical trials.
Our findings propose that school-based programs can have long-term effects in a large target group. This can be related to this fact that children spend a considerable part of their time in school, and adopt some parts of lifestyle there. They have remarkable consequences on health behaviors, but as there are some common limitations, their effects on anthropometric measures are not clear. Due to the crucial role of parents in development of children's behaviors, family-based interventions are reported to have successful effects in some aspects; but selection bias and high dropout rate can confound their results. Clinic-based interventions revealed favorable effects. They include dietary or other lifestyle changes like increasing physical activity or behavior therapy. It seems that a comprehensive intervention including diet and exercise are more practical. When they have different designs, results are controversial.
Conclusion:
We suggest that among different types of interventional programs, a multidisciplinary approach in schools in which children's family are involved, can be the best and most sustainable approach for management of childhood obesity.
INTRODUCTION
The epidemic of childhood obesity is no more limited to high-income countries,[ 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 ] and has become as one of the most important global health problems of the 21 th century.[ 9 ] The World Health Organization (WHO) experts have estimated that there are 43 million overweight children under the age of 5 and by 2020 more than 60% of global disease burden will be the result of obesity related disorders.[ 2 , 10 ] Childhood obesity is associated with several short term and long-term health hazards as cardiovascular diseases, hypertension, type 2 diabetes, fatty liver disease, orthopedic problems, low self-esteem, etc.[ 11 , 12 ] Childhood obesity can reduce life expectancy by 2-5 years.[ 2 ] Moreover, the increasing trend of obesity has enormous economic outcomes.[ 13 ] Two main underlying causes of excess weight are genes and environment.[ 14 , 15 ] Although both genes and environment have a role in an obesity epidemic, gene defects needs to time to show their phenotype; so obesogenic environment is responsible for obesity.[ 11 ]
Primordial/primary prevention of pediatrics obesity and establishment of a healthy lifestyle behaviors from early life are the favored against the epidemic of obesity at the global level.[ 16 ]
Effective interventions for prevention and control of childhood obesity should be considered for different aspects.[ 11 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ] Experts recommend specific eating and physical activity (PA) behaviors through counseling.[ 14 ] Along with clinic-based interventions, researchers have attempted to manage obesity by virtue of family, community, school, and after school programs. Based on Cochrane review of obesity prevention programs in children, most of the well-designed interventions had positive results especially in 6-12-year-old children.[ 25 ] Clearly targeted interventions for children and population-based approach for adolescents may be useful and make economic sense. The purpose of this investigation was to systematically review the effects of various clinical-, family-, and community-based interventions targeting the control of childhood obesity and make a suggestion for future interventions.
MATERIALS AND METHODS
Literature search.
Relevant literature reporting the interventions for controlling excess weight in children and adolescents was identified through electronic search of papers published from 2000 to 2012 in MEDLINE, PubMed, ISI Web of Science, and Scopus. Keywords such as “childhood obesity”, “overweight,” “weight disorder,” “intervention,” “treatment,” “management,” “control,” “PA,” “nutrition,” “behavior therapy,” and “diet therapy” were used. The searches yielded 1768 articles.
Study selection and eligibility criteria
Having removed duplicates, the relevant papers were selected in three phases. In the first and second phases, titles and abstracts of papers were screened and irrelevant papers were excluded. In the last phase, the full text of recruited papers was explored deeply to select only relevant papers. All these three screening phases were done by two independent reviewers (RK and FA). Discrepancies were resolved by consultation and consensus.
Studies were included if they met the following criteria: Studies on 2-18-year-old children; community, family, school, and clinic interventions or a combination of them; English language; and conducted among obese or overweight children and adolescents. Systematic reviews, meta-analysis, and editorials were excluded. Articles were firstly assessed on their abstracts and 234 were removed.
Data extraction and abstraction
The required information that was extracted from all eligible papers was as follow:
- (i) General characteristics of the study (first author's name, publication year, study year, study design, sampling method,
- (ii) Characteristics of the study population (age and sex of studied participants and sample size, follow-up),
- (iii) Type and duration of the intervention, measure(s) used to assess child weight, and
- (iv) Main finding. One reviewer (FA) extracted the data while another (RK) randomly selected 10% of them and checked their extracted data.
The selection process of our systematic review is presented in Figure 1 .

Flow chart of study selection process
The interventions were categorized as school-based, family-based, and clinic-based programs as described below:
School-based programs
A summary of the school-based obesity prevention and control programs is presented in Table 1 . In brief, such interventions are suggested to be feasible and effective;[ 26 ] because students spend a considerable part of their time in school,[ 27 ] moreover teachers and peers can be engaged in such programs.[ 28 ] These kinds of programs can improve health behaviors in a large target group. They are characterized by nutritional education and changes in dietary habits, as well as increase in PA through structured programs.[ 29 ] Findings of various studies proposed that the effects of such interventions will be preserved for several years after intervention.[ 30 , 31 , 32 ] This effect has been of special concern about consuming fruits and vegetables, and healthy snacks, as well as increased PA. Nevertheless, the impact of school-based programs on obesity prevention is controversial and remains to be determined by large studies with long-term follow-up research. Some studies have not evaluated the effect of intervention on anthropometric measures,[ 27 , 33 , 34 ] but they have shown positive impacts on eating and activity behaviors. The most common limitation of these studies is presenting self-reported data, non-randomized selection of schools, short duration of study, and not masking the interventional groups.
School-based weight control studies

Family-based programs
Reaching a healthy weight is not successful unless children have support for making healthy behavior choices; obviously, providers of this support are families. Family is an applicable target for health promoting interventions. Family-based intervention programs are considered as one of the most successful methods for obesity treatment or prevention.[ 59 ] Engaging parents in childhood obesity prevention programs may make weight loss easier for children; because they can provide confirmatory conditions to help their children to choose healthy behaviors, furthermore they are important role models for their children.[ 60 ] It is difficult for parents to know and accept that their child has excess weight, and that recommended diets would not have adverse health effect for their children;[ 61 ] therefore, they often do not comprehend the necessity of obesity prevention. Families are able to construct children's lifestyle habits, perhaps through their “parenting style” and management of “family functioning.”[ 62 ] Table 2 shows family-based interventions for management of childhood obesity. As it demonstrates, most of these programs were successful in decreasing body mass index (BMI) z-score and some health consequences of overweight. After participation of parents in these kinds of programs, their children consumed more fiber and were less sedentary. In some cases, significant decrease in fat mass is documented, as well.[ 63 , 64 ] It has shown that low parental confidence predicts dropout rate from family-based behavioral treatment.[ 65 ] The main limitation of family-based studies is the small sample size, high dropout rate, no follow-up data, and selection of motivated families.
Family-based studies for controlling childhood obesity

Clinic-based programs
Table 3 presents a summary of clinic-based weight management programs conducted in the pediatric age group. Although most researchers have tried low calorie-low fat diets for treating obesity, experts have recommended to consider a diet with balanced macronutrients.[ 14 ] Nevertheless, different dietary changes have been tried to control excess weight in children and adolescents. High protein (HP) diets seems to make more satiety, but two studies did not confirm their advantage versus standard diets.[ 90 , 91 ]
Clinic-based weight control studies for children and adolescents

In studies in which diet, exercise or both of them were taken into account, nutrition plus PA had more effect on anthropometric indices.[ 99 , 103 , 124 ] One study showed that combination of aerobic and strength training along with diet therapy results in BMI decrease in comparison with strength training plus diet recommendation.[ 127 ] A successful experience is reported about the favorable effects of zinc supplementation on anthropometric and metabolic indices.[ 102 , 133 ]
Obesity behavioral therapy has different parts such as motivational interviewing, goal setting, positive reinforcement, monitoring, and cognitive restructuring.[ 134 ] Most of behavioral therapies had positive consequences on weight, BMI, or dietary and PA habits.[ 92 , 98 , 107 , 108 , 116 ]
All interventions that consisted of nutrition, exercise, and counseling had significant effects on body weight or other obesity-related factors[ 84 , 93 , 96 , 100 , 101 , 105 , 109 , 111 , 112 , 113 , 114 , 115 , 117 , 118 , 120 , 128 , 135 ] except for a study, which had beneficial effects only on obesity related behaviors.[ 97 ] The main limitation of some of these studies is lack of comparison with the control group, and short-term follow-up of participants, and the uncertain sustainability of such kinds of interventions.
This review evaluated three different approaches in childhood obesity management. As the design of most studies is a clinical trial, it makes their comparison easier. Schools are a safe place for learning healthy skills and continuing them during life. Most (29/32) of the papers reported a positive effect of school-based intervention on dietary habits or anthropometric measures. One of negative effects of this kind intervention is discrimination resulted from stigmatization. This may persuade them to get involved in healthier lifestyle or might have opposite results. All of the studies conducted in the family setting ( n = 26), had favorable results on obesity criteria. Although some of them had negligible effects. Clinic-based intervention had different methods but almost the same results.
Some studies had no effects on anthropometric index. However, they had resulted in dietary habits or physical fitness improvement.[ 35 , 36 , 46 , 55 , 72 , 97 , 78 , 132 ] One explanation for this can be self-reported dietary intake and PA data. On the other words, children may not pay attention to the instruction they were given.
Teachers can train students how to choose nutritious and low-calorie foods. In addition, exercise training can be reinforced in the school curriculum.[ 14 ] Most students with excess weight prefer to eat fatty, sweetened, and salty snacks; they also choose fast foods as their first meal preference. If attendants get involved in obesity prevention programs, they can provide an environment for children to purchase healthy snacks and foods. Families can also make a circumstance which facilitates dietary and behavioral changes. Furthermore, if parents recognize the importance of weight control, they will be motivated to persuade their children for weight control. Families, especially mothers, are the best paradigm for children to learn a healthful eating pattern and activity habits.[ 136 ] Through family meals, children can eat more whole grains, fruits, vegetables, low fat milk, and consume less sweets and unhealthy fats. Parents should involve kids in preparing food to make a positive effect on their attitudes toward obesity prevention. It seems that the family has a key role in long-term weight control.[ 71 ] It has been shown that if family confidence is low, rate of dropout from weight loss programs will increase.[ 65 ] In this regard, providing parenting styles and skills as well as child management strategies are really critical.[ 81 , 137 ] Principally clinic-setting programs have brought nutrition, PA, and education or counseling together to achieve their goals and they have demonstrated long lasting results.[ 138 ] Most experts advise a low calorie low fat diet for obesity management; but they may have side-effects such as binge eating.[ 139 ] Actually weight loss is allowed in severe obesity and in other cases weight maintenance is an appropriate policy.[ 114 ] Some studies recommend HP or low carbohydrate diets because they cause more satiety.[ 140 ] A review article revealed that low carbohydrate ad libitum diets are as effective as calorie restricted diets.[ 140 ] In addition, a Cochrane review showed that low fat diets have no extra advantages in comparison with other diets with calorie restriction.[ 141 ] Another review article revealed moderate effect of exercise on adiposity and not on BMI.[ 142 ] Clearly, PA is efficient when lasts for more than 60 min, is moderate to vigorous, and is done in all weekdays.[ 134 ] As low calorie diets are harmful for growth, and complying with them is difficult, some studies suggested that vigorous exercise can be a suitable substitute for diet therapy.[ 137 , 139 ] As always emphasized, to be effective, PA should be considered as an enjoyable fun, and should be integrated into daily lifestyle. Obesity causes mental problems in children and adolescents,[ 118 ] so behavior therapy seems to be vital. It sounds that group treatment is more successful than individual ones;[ 75 , 79 ] specifically when parents are engaged. Counselors should persuade children and adolescents to eat breakfast, to have structured meal plan to increase consumption of fruits, vegetables, and family meals, as well as to decrease the intake of sweetened beverages, calorie-dense foods, and eating out, as well as reducing the sedentary behaviors and the screen time.[ 14 , 91 ] Counselors also need to teach families about healthy shopping and cooking habits. Unfortunately, most studies did not show favorable effects, many of them had small sample sizes or had short-term follow-up or lacked of the control group. Managing extra group support sessions or using technologies such as E-mail or SMS for monitoring weight losers can be a good idea.[ 63 , 92 , 143 ]
The findings suggest that among different types of interventional programs for management of childhood obesity, a multidisciplinary approach in schools in which children's family are involved, can be the most feasible and effective approach. As teachers and parents are the best role models, it will be easier to accustom children with healthy dietary, PA, and behavioral habits. Future studies are needed to determine the long-term effects and sustainability of different programs.
AUTHORS’ CONTRIBUTION
FAS contributed in the conception of the work, conducting the review, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. RK contributed in the conception and design of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
Source of Support: Nil
Conflict of Interest: None declared.

IMAGES
VIDEO
COMMENTS
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
The present study conducted a systematic literature review to examine obesity research and machine learning techniques for the prevention and treatment of obesity from 2010 to 2020. Accordingly, 93 papers are identified from the review articles as primary studies from an initial pool of over 700 papers addressing obesity.
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care. Design Systematic review and meta-analysis of randomised controlled trials. Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary ...
Khera, R, Murad, MH, Chandar, AK, et al. Association of pharmacological treatments for obesity with weight loss and adverse events: a systematic review and meta-analysis. JAMA 2016;315:2424-2434 ...
A systematic review by Bagnall et al. (2019) reported a range of positive health outcomes resulting from the adoption of WSA in the context of obesity and related public health issues in multiple countries; these include improvements in BMI, awareness and health behaviors among others . Such findings highlight the importance of addressing the ...
A systematic review of 26 obesity prevention studies focused on the same age group (7-12 years) as WHOSTOPS found that interventions lasting 12 months or less were most effective in preventing obesity . Future research should pay attention to potential interactions between intervention length and impact.
Methods. This systematic review and network meta-analysis included searches of PubMed, Embase, and Cochrane Library (CENTRAL) from inception to March 23, 2021, for randomised controlled trials of weight-lowering drugs in adults with overweight and obesity.
Systematic search strategy and COVID-19 outcomes reported in association with obesity. (A) PRISMA Flow Diagram showing the numbers of articles per stage of review, resulting in n = 22 full text ...
To date, systematic reviews and clinical trials have reported positive impacts of obesity treatment on body size, weight, body composition, cardiometabolic health, functional capacity, musculoskeletal pain, neuromusculoskeletal fitness (72-85) and cardiovascular health . Future research is needed to ensure that clinical trials and evaluation ...
Childhood overweight and obesity is a global public health issue. Although there is evidence of a reduced prevalence in some countries, there is still much controversy about the efficacy of health interventions that aim to prevent and treat obesity in this specific population. The objective of the present study is to develop an overview of systematic reviews (OSRs) that assesses the effects of ...
The current systematic review considered research published within the 10 years preceding June 2019, dealing with the topic of obesity and pain. Within the context of the complex biological and ...
While several systematic reviews on the economic burden of obesity were identified [10,11,12,13,14,15], it is important to update such evidence on a regular basis.
We searched MEDLINE using the keywords "childhood obesity", "prevention", "systematic review" from Jan 1, 2017 to Feb 28, 2022, for any recent systematic reviews that aimed to synthesize international childhood obesity prevention interventions, using a randomized controlled design, conducted in any setting, targeting school-aged ...
- Managing Overweight and Obesity in Adults: Systematic Evidence Review from the Obesity Expert Panel Co-Chair (Voting) Michael Jensen, M.D. Mayo Clinic Rochester, Minnesota. Donna Ryan, M.D. Pennington Biomedical Research Center ...
The objective of SOPHIA is to optimise future obesity treatment and stimulate a new narrative, understanding and vocabulary around obesity as a set of complex and chronic diseases. The findings will also be useful to health care providers and policy makers who seek to understand the experience of those with obesity. Systematic review registration
A systematic review and meta‐analysis combing adolescent and adult data to evaluate weight loss and the effect of age following the laparoscopic sleeve gastrectomy. Danielle Karakso, ... Below is a list of the most read articles published in Obesity Reviews. Open access.
Strategies to promote health behaviors in parents with small children—A systematic review and realist synthesis of behavioral interventions. Anne Timm, Karoline Kragelund Nielsen, Larke Joenck, Nanna Husted Jensen, Dorte Moeller Jensen, Ole Norgaard, Helle Terkildsen Maindal, e13359. First Published: 03 November 2021. Abstract.
Obesity has been proven to increase the susceptibility of an individual to infections, but the relationship between obesity and COVID-19 is still unclear. This study aimed to conduct a systematic review and meta-analysis of the prevalence of obesity and its effects in patients with COVID-19.
Background: Obesity and depression co-occur in a significant proportion of the population. Mechanisms linking the two disorders include the immune and the endocrine system, psychological and social mechanisms. The aim of this systematic review was to ...
Potent incretin‐based therapy for obesity: A systematic review and meta‐analysis of the efficacy of semaglutide and tirzepatide on body weight and waist circumference, and safety. Alberte Laura Oest Müllertz, Rasmus Michael Sandsdal, Simon Birk Kjær Jensen, Signe Sørensen Torekov. ,
This article aims to conduct the first systematic review and meta-analysis of the short-term outcomes between robot-assisted and laparoscopic surgeries for GC patients with visceral obesity, addressing this critical gap in the literature. ... (2023) Robotic versus laparoscopic gastrectomy for gastric cancer in patients with obesity: systematic ...
The following research question was developed using a modified Population, Intervention, Comparison, Outcome and Study type (PICOS) framework: "What are the lived experiences of people living with obesity and chronic pain?". One review author will conduct a systematic search based on keywords and Medical Subject Headings (MeSH) terms for ...
A recent systematic review article in this regard also proposed that artificial sweeteners, sugar alcohols, and fructose may cause obesity and metabolic dysfunctions by altering the gut microbiota ...
The subgroup analysis revealed a significantly increase in the risk of overweight/obesity when the concentrations of PM 2.5, PM 10, and NO 2 exceeded 35 μg/m 3, 50 μg/m 3, and 40 μg/m 3, respectively. Exposure to PM 2.5, PM 10 and NO X increased the risk of overweight/obesity, especially in Asia. This study provides evidence of the ...
Background: The rising prevalence of obesity represents an important public health issue.An assessment of its costs may be useful in providing recommendations for policy and decision makers. This systematic review aimed to assess the economic burden of obesity and to identify, measure and describe the different obesity-related diseases included in the selected studies.
Obesity, a public health problem and a risk factor for numerous comorbidities, has stimulated a growing interest in bioactive-rich foods, such as guarana (Paullinia cupana).This systematic review examined the impact of guarana on obesity-related diseases using animal models from January 1990 and November 2023.
This systematic review reported on the recruitment and retention of ethnic minorities in community-based obesity prevention RCTS with the pooled proportions of recruitment and retention at 64% and ...
Along with clinic-based interventions, researchers have attempted to manage obesity by virtue of family, community, school, and after school programs. Based on Cochrane review of obesity prevention programs in children, most of the well-designed interventions had positive results especially in 6-12-year-old children. [ 25]
More than 40% of U.S. adults live with obesity, a major risk factor for heart disease and stroke, according to the Centers for Disease Control and Prevention. Recent advances in research have led to a deeper understanding of the complex causes of obesity, including the role of sociological and physiological determinants of health.
The range of outcomes and outcome measurement instruments collected in multisectoral community‐based obesity prevention interventions in children: A systematic review. Marufa Sultana, Melanie Nichols, Jane Jacobs, Derin Karacabeyli, Steven Allender, Rachel Novotny, Vicki Brown. , First Published: 3 March 2024. Abstract. Full text. PDF ...