
- Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Ther Adv Urol . 2019;11:1756287219832172.
- Schaeffer AJ, Nicolle LE. Urinary tract infections in older men. N Engl J Med . 2016;374:562-571.
- Öztürk R, Murt A. Epidemiology of urological infections: a global burden. World J Urol . 2020;38:2669-2679.
- Sabih A, Leslie SW. Complicated urinary tract infections. In: Abai A, Abu-Ghosh A, Archarya AB, et al. StatPearls . StatsPearls Publishing; 2020. Updated February 2021. Accessed July 1, 2021. https://www.ncbi.nlm.nih.gov/books/NBK436013/
- Colgan R, Williams M. Diagnosis and treatment of acute uncomplicated cystitis. Am Fam Physician . 2011;84:771-776.
- Tamma PD, Aitken L, Bonomo RA, et al. Infectious Diseases Society of America guidance on the treatment of antimicrobial resistant gram-negative infections. Published September 8, 2020. Accessed July 1, 2021. https://www.idsociety.org/globalassets/idsa/practice-guidelines/amr-guidance/idsa-amr-guidance.pdf
- Kudinha T. The pathogenesis of Escherichia coli urinary tract infection. In: Samie A, ed. Escherichia coli - Recent Advances on Physiology, Pathogenesis and Biotechnological Applications. IntechOpen Limited; 2017. Accessed July 1, 2021. https://www.intechopen.com/books/-i-escherichia-coli-i-recent-advances-on-physiology-pathogenesis-and-biotechnological-applications/the-pathogenesis-of-i-escherichia-coli-i-urinary-tract-infection
- Moore EE, Hawes SE, Scholes D, et al. Sexual intercourse and risk of symptomatic urinary tract infection in post-menopausal women. J Gen Intern Med . 2008;23:595-599.
- Belyayeva M, Jeong JM. Acute pyelonephritis. In: Abai A, Abu-Ghosh A, Acharya AB, et al. StatPearls . StatsPearls Publishing; 2020. Updated July 2020. Accessed July 1, 2021. https://www.ncbi.nlm.nih.gov/books/NBK519537/
- Mertz D, Duława J, Drabczyk R. Uncomplicated acute pyelonephritis. In: McMaster Textbook of Internal Medicine . Medycyna Praktyczna; 2019. Accessed July 3, 2021. https://empendium.com/mcmtextbook/chapter/B31.II.14.8.3
- National Cancer Institute (NCI) Seer Training Modules. Normal Blood Values. Accessed July 16, 2021. https://training.seer.cancer.gov/abstracting/procedures/clinical/hematologic/blood.html
- Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis . 2011;52:e103-e120.
- Arena F, Giani T, Pollini S, et al. Molecular antibiogram in diagnostic clinical microbiology: advantages and challenges. Future Microbiol . 2017;12:361-364.
- Wagenlehner FM, Cek M, Naber KG, et al. Epidemiology, treatment and prevention of healthcare-associated urinary tract infections. World J Urol . 2012;30:59-67.
- Gharbi M, Drysdale JH, Lishman H, et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all cause mortality: population based cohort study. BMJ . 2019;364:1525.
- Lentz GM. Urinary tract infections in obstetrics and gynecology. Global Library of Women's Medicine. Updated May 2009. Accessed July 1, 2021. https://www.glowm.com/section-view/heading/Urinary%20Tract%20Infections%20in%20Obstetrics%20and%20Gynecology/item/118#.YN8TjehKhBA
- Ehlers S, Merrill SA. Staphylococcus saprophyticus . In: Abai A, Abu-Ghosh A, Acharya AB, et al. StatPearls . StatsPearls Publishing; 2020. Updated June 2020. Accessed July 2, 2021. https://www.ncbi.nlm.nih.gov/books/NBK482367/
- Katouli M. Population structure of gut Escherichia coli and its role in development of extra-intestinal infections. Iran J Microbiol . 2010;2:59-72.
- Mobley HL, Donnenberg MS, Hagan EC. Uropathogenic Escherichia coli . EcoSal Plus . 2009;3:10.1128/ecosalplus.8.6.1.3.
- Tamma PD, Aitken SL, Bonomo RA, et al. Infectious Diseases Society of America guidance on the treatment of extended-spectrum β-lactamase producing enterobacterales (ESBL-E), carbapenem-resistant enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR- aeruginosa ). Clin Infect Dis . 2021;72:e169-e183.
- Doi Y, Park YS, Rivera JI, et al. Community-associated extended-spectrum β-lactamase-producing Escherichia coli infection in the United States. Clin Infect Dis . 2013;56:641-648.
- Jernigan JA, Hatfield KM, Wolford H, et al. Multidrug-resistant bacterial infections in US hospitalized patients, 2012-2017. N Engl J Med . 2020;382:1309-1319.
- van Duin D, Paterson DL. Multidrug-resistant bacteria in the community: trends and lessons learned. Infect Dis Clin North Am . 2016;30:377-390.
- Rawat D, Nair D. Extended-spectrum β-lactamases in gram negative bacteria. J Glob Infect Dis . 2010;2:263-274.
- Karanika S, Karantanos T, Arvanitis M, et al. Fecal colonization with extended-spectrum beta-lactamase-producing Enterobacteriaceae and risk factors among healthy individuals: a systematic review and metaanalysis. Clin Infect Dis . 2016;63:310-318.
- Gutiérrez-Gutiérrez B, Rodríguez-Baño J. Current options for the treatment of infections due to extended-spectrum beta-lactamase-producing Enterobacteriaceae in different groups of patients. Clin Microbiol Infect . 2019;25:932-942.
- Centers for Disease Control and Prevention (CDC). Antibiotic Resistance Threats in the United States - 2019. Updated December 2019. Accessed July 2, 2021. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
- Karaiskos I, Giamarellou H. Carbapenem-sparing strategies for ESBL producers: when and how. Antibiotics (Basel) . 2020;9:61.
- Larramendy S, Deglaire V, Dusollier P, et al. Risk factors of extended-spectrum beta-lactamases-producing Escherichia coli community acquired urinary tract infections: a systematic review. Infect Drug Resist . 2020;13:3945-3955.
- Goyal D, Dean N, Neill S, et al. Risk factors for community-acquired extended-spectrum beta-lactamase-producing Enterobacteriaceae infections-a retrospective study of symptomatic urinary tract infections. Open Forum Infect Dis . 2019;6:ofy357.
- Koksal E, Tulek N, Sonmezer MC, et al. Investigation of risk factors for community-acquired urinary tract infections caused by extended-spectrum beta-lactamase Escherichia coli and Klebsiella Investig Clin Urol . 2019;60:46-53.
- Augustine MR, Testerman TL, Justo JA, et al. Clinical risk score for prediction of extended-spectrum β-lactamase-producing Enterobacteriaceae in bloodstream isolates. Infect Control Hosp Epidemiol . 2017;38:266-272.
- Goodman KE, Lessler J, Cosgrove SE, et al. A clinical decision tree to predict whether a bacteremic patient is infected with an extended-spectrum β-lactamase-producing organism. Clin Infect Dis . 2016;63:896-903.
- Tumbarello M, Trecarichi EM, Bassetti M, et al. Identifying patients harboring extended-spectrum-beta-lactamase-producing Enterobacteriaceae on hospital admission: derivation and validation of a scoring system. Antimicrob Agents Chemother . 2011;55:3485-3490.
- Nicolle LE, Gupta K, Bradley SF, et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis . 2019;68:e83-e110.
- Givler DN, Givler A. Asymptomatic bacteriuria. In: Abai A, Abu-Ghosh A, Acharya AB, et al. StatPearls . StatsPearls Publishing; 2020. Updated January 2021. Accessed July 3, 2021. https://www.ncbi.nlm.nih.gov/books/NBK441848/
- Hooton TM, Gupta K. Acute Complicated Urinary Tract Infection (Including Pyelonephritis) in Adults. UpToDate. Updated March 19, 2021. Accessed July 3, 2021. https://www.uptodate.com/contents/acute-complicated-urinary-tract-infection-including-pyelonephritis-in-adults
- Cai T, Mazzoli S, Mondaini N, et al. The role of asymptomatic bacteriuria in young women with recurrent urinary tract infections: to treat or not to treat? Clin Infect Dis . 2012;55:771-777.
- Habak PJ, Griggs, Jr RP. Urinary tract infection in pregnancy. In: Abai A, Abu-Ghosh A, Acharya AB, et al. StatPearls . StatsPearls Publishing; 2020. Updated November 2020. Accessed July 3, 2021. https://www.ncbi.nlm.nih.gov/books/NBK537047/
- Kazemier BM, Koningstein FN, Schneeberger C, et al. Maternal and neonatal consequences of treated and untreated asymptomatic bacteriuria in pregnancy: a prospective cohort study with an embedded randomised controlled trial. Lancet Infect Dis . 2015;15:1324-1333.
- Centers for Disease Control and Prevention (CDC). Multidrug-resistant Pseudomonas aeruginosa . Published 2019. Accessed July 4, 2021. https://www.cdc.gov/drugresistance/pdf/threats-report/pseudomonas-aeruginosa-508.pdf
- Döring G, Ulrich M, Müller W, et al. Generation of Pseudomonas aeruginosa aerosols during handwashing from contaminated sink drains, transmission to hands of hospital personnel, and its prevention by use of a new heating device. Zentralbl Hyg Umweltmed . 1991;191:494-505.
- Aloush V, Navon-Venezia S, Seigman-Igra Y, et al. Multidrug-resistant Pseudomonas aeruginosa : risk factors and clinical impact. Antimicrob Agents Chemother . 2006;50:43-48.
- Pang Z, Raudonis R, Glick BR, et al. Antibiotic resistance in Pseudomonas aeruginosa : mechanisms and alternative therapeutic strategies. Biotechnol Adv . 2019;37:177-192.
- Cole SJ, Records AR, Orr MW, et al. Catheter-associated urinary tract infection by Pseudomonas aeruginosa is mediated by exopolysaccharide-independent biofilms. Infect Immun . 2014;82:2048-2058.
- Raman G, Avendano EE, Chan J, et al. Risk factors for hospitalized patients with resistant or multidrug-resistant Pseudomonas aeruginosa infections: a systematic review and meta-analysis. Antimicrob Resist Infect Control . 2018;7:79.
- Gomila A, Carratalà J, Eliakim-Raz N, et al. Risk factors and prognosis of complicated urinary tract infections caused by Pseudomonas aeruginosa in hospitalized patients: a retrospective multicenter cohort study. Infect Drug Resist . 2018;11:2571-2581.
- Lamas Ferreiro JL, Álvarez Otero J, González González L, et al. Pseudomonas aeruginosa urinary tract infections in hospitalized patients: mortality and prognostic factors. PLoS One . 2017;12:e0178178.
- Zerbraxa® (ceftolozane and tazobactam) [prescribing information]. Merck & Co, Inc; Approved 2014. Revised September 2020.
- Haidar G, Philips NJ, Shields RK, et al. Ceftolozane-tazobactam for the treatment of multidrug-resistant Pseudomonas aeruginosa infections: clinical effectiveness and evolution of resistance. Clin Infect Dis . 2017;65:110-120.
- Lob SH, Hoban DJ, Young K, et al. Activity of ceftolozane-tazobactam and comparators against Pseudomonas aeruginosa from patients in different risk strata - SMART United States 2016-2017. J Glob Antimicrob Resist . 2020;20:209-213.
- Shirley M. Ceftazidime-avibactam: a review in the treatment of serious gram-negative bacterial infections. Drugs . 2018;78:675-692.
- Avycaz® (ceftazidime and avibactam) [prescribing information]. Allergan USA, Inc; Approved 2015. Revised December 2020.
- Stone GG, Newell P, Gasink LB, et al. Clinical activity of ceftazidime/avibactam against MDR Enterobacteriaceae and Pseudomonas aeruginosa: pooled data from the ceftazidime/avibactam phase III clinical trial programme. J Antimicrob Chemother . 2018;73:2519-2523.
- Recarbrio™ (imipenem, cilastatin, and relebactam) [prescribing information] Merck & Co, Inc; Approved 2019. Revised June 2020.
- Heo YA. Imipenem/cilastatin/relebactam: a review in gram-negative bacterial infections. Drugs . 2021;81:377-388.
- US Food & Drug Administration (FDA). FDA approves new antibacterial drug to treat complicated urinary tract infections as part of ongoing efforts to address antimicrobial resistance. News release. November 14, 2019. Accessed July 5, 2021. https://www.fda.gov/news-events/press-announcements/fda-approves-new-antibacterial-drug-treat-complicated-urinary-tract-infections-part-ongoing-efforts
- Fetroja® (cefiderocol) [prescribing information]. Shionogi Inc; Approved 2019. Revised September 2020.
- El-Lababidi RM, Rizk JG. Cefiderocol: a siderophore cephalosporin. Ann Pharmacother . 2020;54:1215-1231.
- Stevens RW, Clancy M. Compassionate use of cefiderocol in the treatment of an intraabdominal infection due to multidrug-resistant Pseudomonas aeruginosa : a case report. Pharmacotherapy . 2019;39:1113-1118.
- Krause KM, Serio AW, Kane TR, et al. Aminoglycosides: an overview. Cold Spring Harb Perspect Med . 2016;6:a027029.
- Gonzalez LS 3rd, Spencer JP. Aminoglycosides: a practical review. Am Fam Physician . 1998;58:1811-1820.
- Teixeira B, Rodulfo H, Carreño N, et al. Aminoglycoside resistance genes in Pseudomonas aeruginosa isolates from Cumana, Venezuela. Rev Inst Med Trop Sao Paulo . 2016;58:13.
- Amikacin sulfate injection, USP [prescribing information]. SAGENT Pharmaceuticals. Revised February 2018. https://www.sagentpharma.com/wp-content/uploads/2021/02/Amikacin-Sulfate-Inj-USP_PI_Feb-2018.pdf
- Gentamicin injection, USP [prescribing information]. APP Fresenius Kabi, USA, LLC. Revised October 2013.
- Zemdri® (plazomicin) [prescribing information]. Cipla USA, Inc; Approved 2018. Revised January 2020.
- Tobramycin injection, USP [prescribing information]. APP Fresenius Kabi USA, LLC. Revised October 2013.
- Eljaaly K, Alharbi A, Alshehri S, et al. Plazomicin: a novel aminoglycoside for the treatment of resistant gram-negative bacterial infections. Drugs . 2019;79:243-269.
- Wagenlehner FME, Cloutier DJ, Komirenko AS, et al. Once-daily plazomicin for complicated urinary tract infections. N Engl J Med . 2019;380:729-740.
- McKinnell JA, Dwyer JP, Talbot GH, et al. Plazomicin for infections caused by carbapenem-resistant Enterobacteriaceae. N Engl J Med . 2019;380:791-793.

Faculty and Disclosures
As an organization accredited by the ACCME, Medscape, LLC requires everyone who is in a position to control the content of an education activity to disclose all relevant financial relationships with any commercial interest. The ACCME defines "relevant financial relationships" as financial relationships in any amount, occurring within the past 12 months, including financial relationships of a spouse or life partner, that could create a conflict of interest.
Medscape, LLC encourages Authors to identify investigational products or off-label uses of products regulated by the US Food and Drug Administration, at first mention and where appropriate in the content.

Neil Clancy, MD
Associate Chief of VA Pittsburgh Health System (VAPHS) and Opportunistic Pathogens Associate Professor of Medicine Director, Mycology Program Chief, Infectious Diseases Section VA Pittsburgh Health Care System Pittsburgh, Pennsylvania
Disclosure: Neil Clancy, MD, has the following relevant financial relationships: Advisor or consultant for: Astellas; Cidara; Merck; Needham & Company; Qpex; Scynexis; Shionogi; The Medicines Company Speaker or a member of a speakers bureau for: Merck; T2 Biosystems Grants for clinical research from: Astellas; Cidara; Melinta; Merck
Christina T. Loguidice
Medical Writer and Medical Education Director, Medscape, LLC
Disclosure: Christina T. Loguidice has disclosed no relevant financial relationships.
CME Reviewer
Amanda Jett, PharmD, BCACP
Disclosure: Amanda Jett, PharmD, BCACP, has disclosed no relevant financial relationships.
None of the nonfaculty planners for this educational activity have relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
Peer Reviewer
This activity has been peer reviewed and the reviewer has disclosed no relevant financial relationships.

CME / ABIM MOC / CE
Clinical challenge: case studies in recurrent complicated utis.
- Authors: Neil Clancy, MD
CME / ABIM MOC / CE Released: 8/20/2021
- THIS ACTIVITY HAS EXPIRED FOR CREDIT
Valid for credit through: 8/20/2022 , 11:59 PM EST
Target Audience and Goal Statement
This activity is intended for infectious disease specialists, urologists, primary care physicians, pharmacists, and other healthcare providers involved in the management of recurrent complicated urinary tract infections (UTIs).
The goal of this activity is to improve clinicians' ability to evaluate the role of newer antibiotic agents for the treatment of recurrent, complicated UTIs caused by multidrug-resistant organisms.
Upon completion of this activity, participants will:
- Risk factors for multidrug-resistant infection in UTIs
- The use of an antibiogram to guide antibiotic selection
- The selection of appropriate therapies for the treatment of recurrent complicated UTIs
Disclosures
Accreditation statements.

For Physicians
Medscape, LLC designates this enduring material for a maximum of 1.0 AMA PRA Category 1 Credit(s)™ . Physicians should claim only the credit commensurate with the extent of their participation in the activity. Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) program. Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit. Aggregate participant data will be shared with commercial supporters of this activity.
Contact This Provider
For Pharmacists
Medscape, LLC designates this continuing education activity for 1.0 contact hour(s) (0.100 CEUs) (Universal Activity Number JA0007105-0000-21-450-H01-P).
For questions regarding the content of this activity, contact the accredited provider for this CME/CE activity noted above. For technical assistance, contact [email protected]
Instructions for Participation and Credit
There are no fees for participating in or receiving credit for this online educational activity. For information on applicability and acceptance of continuing education credit for this activity, please consult your professional licensing board. This activity is designed to be completed within the time designated on the title page; physicians should claim only those credits that reflect the time actually spent in the activity. To successfully earn credit, participants must complete the activity online during the valid credit period that is noted on the title page. To receive AMA PRA Category 1 Credit™ , you must receive a minimum score of 70% on the post-test. Follow these steps to earn CME/CE credit*:
- Read about the target audience, learning objectives, and author disclosures.
- Study the educational content online or print it out.
- Online, choose the best answer to each test question. To receive a certificate, you must receive a passing score as designated at the top of the test. We encourage you to complete the Activity Evaluation to provide feedback for future programming.
You may now view or print the certificate from your CME/CE Tracker. You may print the certificate, but you cannot alter it. Credits will be tallied in your CME/CE Tracker and archived for 6 years; at any point within this time period, you can print out the tally as well as the certificates from the CME/CE Tracker. *The credit that you receive is based on your user profile.
CASE 1: PATIENT HISTORY AND PRESENTATION
Tara is a 26-year-old Korean American woman who presents to the emergency department (ED) with fevers, chills, and right-sided flank pain, which developed acutely during the previous night. After she telephoned her healthcare provider in the morning about these symptoms, she was told to go directly to the ED. She is sexually active in a jointly monogamous relationship with her boyfriend of 2 years. Her only standing medication is an oral contraceptive, which she takes regularly. Her medical history is significant for an asymptomatic horseshoe kidney that was found incidentally and approximately 1 episode of cystitis per year, characterized by dysuria. After developing symptoms of cystitis, she telephones her healthcare provider and receives a prescription for ciprofloxacin or trimethoprim-sulfamethoxazole. She does not recall providing a urine sample for urinalysis or culture in the past. Her last episode of dysuria was 2 weeks ago, for which she took ciprofloxacin "for a couple of days." Her symptoms resolved without apparent incident. Since the onset of her presenting symptoms, she took 2 doses of ciprofloxacin that were left over from her previous prescription.

- Abbreviations
The educational activity presented above may involve simulated, case-based scenarios. The patients depicted in these scenarios are fictitious and no association with any actual patient, whether living or deceased, is intended or should be inferred. The material presented here does not necessarily reflect the views of Medscape, LLC, or any individuals or commercial entities that support companies that support educational programming on medscape.org. These materials may include discussion of therapeutic products that have not been approved by the US Food and Drug Administration, off-label uses of approved products, or data that were presented in abstract form. These data should be considered preliminary until published in a peer-reviewed journal. Readers should verify all information and data before treating patients or employing any therapies described in this or any educational activity. A qualified healthcare professional should be consulted before using any therapeutic product discussed herein.
Medscape Education © 2021 Medscape, LLC

This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Ahmed H, Farewell D, Francis NA, Paranjothy S, Butler CC. Risk of adverse outcomes following urinary tract infection in older people with renal impairment: Retrospective cohort study using linked health record data. PLoS Med. 2018; 15:(9) https://doi.org/10.1371/journal.pmed.1002652
Bardsley A. Diagnosis, prevention and treatment of urinary tract infections in older people. Nurs Older People. 2017; 29:(2)32-38 https://doi.org/10.7748/nop.2017.e884
Barnsley Hospital NHS FT/The Rotherham NHS FT. Adult antimicrobial guide. 2022. https://viewer.microguide.global/BHRNFT/ADULT (accessed 13 March 2023)
Bradley S, Sheeran S. Optimal use of Antibiotics for urinary tract infections in long-term care facilities: Successful strategies prevent resident harm. Patient Safety Authority. 2017; 14:(3) http://patientsafety.pa.gov/ADVISORIES/pages/201709_UTI.aspx
Chardavoyne PC, Kasmire KE. Appropriateness of Antibiotic Prescriptions for Urinary Tract Infections. West J Emerg Med. 2020; 21:(3)633-639 https://doi.org/10.5811/westjem.2020.1.45944
Deresinski S. Fosfomycin or nitrofurantoin for cystitis?. Infectious Disease Alert: Atlanta. 2018; 37:(9) http://www.proquest.com/trade-journals/fosfomycin-nitrofurantoin-cystitis/docview/2045191847
Doogue MP, Polasek TM. The ABCD of clinical pharmacokinetics. Ther Adv Drug Saf. 2013; 4:(1)5-7 https://doi.org/10.1177/2042098612469335
Doyle JF, Schortgen F. Should we treat pyrexia? And how do we do it?. Crit Care. 2016; 20:(1) https://doi.org/10.1186/s13054-016-1467-2
Fransen F, Melchers MJ, Meletiadis J, Mouton JW. Pharmacodynamics and differential activity of nitrofurantoin against ESBL-positive pathogens involved in urinary tract infections. J Antimicrob Chemother. 2016; 71:(10)2883-2889 https://doi.org/10.1093/jac/dkw212
Geerts AF, Eppenga WL, Heerdink R Ineffectiveness and adverse events of nitrofurantoin in women with urinary tract infection and renal impairment in primary care. Eur J Clin Pharmacol. 2013; 69:(9)1701-1707 https://doi.org/10.1007/s00228-013-1520-x
Greener M. Modified release nitrofurantoin in uncomplicated urinary tract infection. Nurse Prescribing. 2011; 9:(1)19-24 https://doi.org/10.12968/npre.2011.9.1.19
Confusion in the older patient: a diagnostic approach. 2019. https://www.gmjournal.co.uk/confusion-in-the-older-patient-a-diagnostic-approach (accessed 13 March 2023)
Haasum Y, Fastbom J, Johnell K. Different patterns in use of antibiotics for lower urinary tract infection in institutionalized and home-dwelling elderly: a register-based study. Eur J Clin Pharmacol. 2013; 69:(3)665-671 https://doi.org/10.1007/s00228-012-1374-7
Health Education England. The Core Capabilities Framework for Advanced Clinical Practice (Nurses) Working in General Practice/Primary Care in England. 2020. https://www.hee.nhs.uk/sites/default/files/documents/ACP%20Primary%20Care%20Nurse%20Fwk%202020.pdf (accessed 13 March 2023)
Hoang P, Salbu RL. Updated nitrofurantoin recommendation in the elderly: A closer look at the evidence. Consult Pharm. 2016; 31:(7)381-384 https://doi.org/10.4140/TCP.n.2016.381
Langner JL, Chiang KF, Stafford RS. Current prescribing practices and guideline concordance for the treatment of uncomplicated urinary tract infections in women. Am J Obstet Gynecol. 2021; 225:(3)272.e1-272.e11 https://doi.org/10.1016/j.ajog.2021.04.218
Lajiness R, Lajiness MJ. 50 years on urinary tract infections and treatment-Has much changed?. Urol Nurs. 2019; 39:(5)235-239 https://doi.org/10.7257/1053-816X.2019.39.5.235
Komp Lindgren P, Klockars O, Malmberg C, Cars O. Pharmacodynamic studies of nitrofurantoin against common uropathogens. J Antimicrob Chemother. 2015; 70:(4)1076-1082 https://doi.org/10.1093/jac/dku494
Lovatt P. Legal and ethical implications of non-medical prescribing. Nurse Prescribing. 2010; 8:(7)340-343 https://doi.org/10.12968/npre.2010.8.7.48941
Malcolm W, Fletcher E, Kavanagh K, Deshpande A, Wiuff C, Marwick C, Bennie M. Risk factors for resistance and MDR in community urine isolates: population-level analysis using the NHS Scotland Infection Intelligence Platform. J Antimicrob Chemother. 2018; 73:(1)223-230 https://doi.org/10.1093/jac/dkx363
McKinnell JA, Stollenwerk NS, Jung CW, Miller LG. Nitrofurantoin compares favorably to recommended agents as empirical treatment of uncomplicated urinary tract infections in a decision and cost analysis. Mayo Clin Proc. 2011; 86:(6)480-488 https://doi.org/10.4065/mcp.2010.0800
Medicines.org. Nitrofurantoin. 2022. https://www.medicines.org.uk/emc/search?q=Nitrofurantoin (accessed 13 March 2023)
NHS England, NHS Improvement. Online library of Quality Service Improvement and Redesign tools. SBAR communication tool – situation, background, assessment, recommendation. 2021. https://www.england.nhs.uk/wp-content/uploads/2021/03/qsir-sbar-communication-tool.pdf (accessed 13 March 2023)
National Institute for Health and Care Excellence. NG5: Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes. 2015. https://www.nice.org.uk/guidance/ng5 (accessed 13 March 2023)
National Institute for Health and Care Excellence. Urinary tract infection (lower) – women. 2021. https://cks.nice.org.uk/topics/urinary-tract-infection-lower-women/ (accessed 13 March 2023)
Nursing and Midwifery Council. The Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates. 2021. https://www.nmc.org.uk/standards/code/ (accessed 13 March 2023)
O'Grady MC, Barry L, Corcoran GD, Hooton C, Sleator RD, Lucey B. Empirical treatment of urinary tract infections: how rational are our guidelines?. J Antimicrob Chemother. 2019; 74:(1)214-217 https://doi.org/10.1093/jac/dky405
O'Neill D, Branham S, Reimer A, Fitzpatrick J. Prescriptive practice differences between nurse practitioners and physicians in the treatment of uncomplicated urinary tract infections in the emergency department setting. J Am Assoc Nurse Pract. 2021; 33:(3)194-199 https://doi.org/10.1097/JXX.0000000000000472
Royal Pharmaceutical Society. A competency framework for designated prescribing practitioners. 2019. https://www.rpharms.com/resources/frameworks (accessed 13 March 2023)
Singh N, Gandhi S, McArthur E Kidney function and the use of nitrofurantoin to treat urinary tract infections in older women. CMAJ. 2015; 187:(9)648-656 https://doi.org/10.1503/cmaj.150067
Stamatakos M, Sargedi C, Stasinou T, Kontzoglou K. Vesicovaginal fistula: diagnosis and management. Indian J Surg. 2014; 76:(2)131-136 https://doi.org/10.1007/s12262-012-0787-y
Swift A. Understanding the effects of pain and how human body responds. Nurs Times. 2018; 114:(3)22-26 https://www.nursingtimes.net/clinical-archive/pain-management/understanding-the-effect-of-pain-and-how-the-human-body-responds-26-02-2018/
Taylor K. Non-medical prescribing in urinary tract infections in the community setting. Nurse Prescribing. 2016; 14:(11)566-569 https://doi.org/10.12968/npre.2016.14.11.566
Wijma RA, Huttner A, Koch BCP, Mouton JW, Muller AE. Review of the pharmacokinetic properties of nitrofurantoin and nitroxoline. J Antimicrob Chemother. 2018; 73:(11)2916-2926 https://doi.org/10.1093/jac/dky255
Wijma RA, Curtis SJ, Cairns KA, Peleg AY, Stewardson AJ. An audit of nitrofurantoin use in three Australian hospitals. Infect Dis Health. 2020; 25:(2)124-129 https://doi.org/10.1016/j.idh.2020.01.001
Urinary tract infection in an older patient: a case study and review
Advanced Nurse Practitioner, Primary Care
View articles
Gerri Mortimore
Senior lecturer in advanced practice, department of health and social care, University of Derby
View articles · Email Gerri

This article will discuss and reflect on a case study involving the prescribing of nitrofurantoin, by a non-medical prescriber, for a suspected symptomatic uncomplicated urinary tract infection in a patient living in a care home. The focus will be around the consultation and decision-making process of prescribing and the difficulties faced when dealing with frail, uncommunicative patients. This article will explore and critique the evidence-base, local and national guidelines, and primary research around the pharmacokinetics and pharmacodynamics of nitrofurantoin, a commonly prescribed medication. Consideration of the legal, ethical and professional issues when prescribing in a non-medical capacity will also be sought, concluding with a review of the continuing professional development required to influence future prescribing decisions relating to the case study.
Urinary tract infections are common in older people. Haley Read and Gerri Mortimore describe the decision making process in the case of an older patient with a UTI
One of the growing community healthcare delivery agendas is that of the advanced nurse practitioner (ANP) role to improve access to timely, appropriate assessment and treatment of patients, in an attempt to avoid unnecessary health deterioration and/or hospitalisation ( O'Neill et al, 2021 ). The Core Capabilities Framework for Advanced Clinical Practice (Nurses) Working in General Practice/Primary Care in England recognises the application of essential skills, including sound consultation and clinical decision making for prescribing appropriate treatment ( Health Education England [HEE], 2020 ). This article will discuss and reflect on a case study involving the prescribing of nitrofurantoin by a ANP for a suspected symptomatic uncomplicated urinary tract infection (UTI), in a patient living in a care home. Focus will be around the consultation and decision-making process of non-medical prescribing and will explore and critique the evidence-base, examining the local and national guidelines and primary research around the pharmacokinetics and pharmacodynamics of nitrofurantoin. Consideration of the legal, ethical and professional issues when prescribing in a non-medical capacity will also be sought, concluding with review of the continuing professional development required to influence future prescribing decisions relating to the case study.
Mrs M, an 87-year-old lady living in a nursing home, was referred to the community ANP by the senior carer. The presenting complaint was reported as dark, cloudy, foul-smelling urine, with new confusion and night-time hallucinations. The carer reported a history of disturbed night sleep, with hallucinations of spiders crawling in bed, followed by agitation, lethargy and poor oral intake the next morning. The SBAR (situation, background, assessment, recommendation) tool was adopted, ensuring structured and relevant communication was obtained ( NHS England and NHS Improvement, 2021 ). The National Institute for Health and Care Excellence ( NICE, 2021 ) recognises that cloudy, foul-smelling urine may indicate UTI. Other symptoms include increased frequency or pressure to pass urine, dysuria, haematuria or dark coloured urine, mild fever, night-time urination, and increased sweats or chills, with lower abdominal/loin pain suggesting severe infection. NICE (2021) highlight that patients with confusion may not report UTI symptoms. This is supported by Gupta and Gupta (2019) , who recognise new confusion as hyper-delirium, which can be attributed to several causative factors including infection, dehydration, constipation and medication, among others.
UTIs are one of the most common infections worldwide ( O'Grady et al, 2019 ). Lajiness and Lajiness (2019) define UTI as a presence of colonising bacteria that cause a multitude of symptoms affecting either the upper or lower urinary tract. NICE (2021) further classifies UTIs as either uncomplicated or complicated, with complicated involving other systemic conditions or pre-existing diseases. Geerts et al (2013) postulate around 30% of females will develop a UTI at least once in their life. The incidence increases with age, with those over 65 years of age being five times more likely to develop a UTI at any point. Further increased prevalence is found in patients who live in a care home, with up to 60% of all infections caused by UTI ( Bardsley, 2017 ).
Greener (2011) reported that symptoms of UTIs are often underestimated by clinicians. A study cited by Greener (2011) found over half of GPs did not record the UTI symptoms that the patient had reported. It is, therefore, essential during the consultation to use open-ended questions, listening to the terminology of the patient or carers to clarify the symptoms and creating an objective history ( Taylor, 2016 ).
In this case, the carer highlighted that Mrs M had been treated for suspected UTI twice in the last 12 months. Greener (2011) , in their literature review of 8 Cochrane review papers and 1 systematic review, which looked at recurrent UTI incidences in general practice, found 48% of women went on to have a further episode within 12 months.
Mrs M's past medical history reviewed via the GP electronic notes included:
- Hypertension
- Diverticular disease
- Basal cell carcinoma of scalp
- Retinal vein occlusion
- Severe frailty
- Fracture of proximal end of femur
- Total left hip replacement
- Previous indwelling urinary catheter
- Chronic kidney disease (CKD) stage 2
- Urinary and faecal incontinence
- And, most recently, vesicovaginal fistula.
Bardsley (2017) identified further UTI risk factors including postmenopausal females, frailty, co-morbidity, incontinence and use of urethral catheterisation. Vesicovaginal fistulas also predispose to recurrent UTIs, due to the increase in urinary incontinence ( Stamatokos et al, 2014 ). Moreover, UTIs are common in older females living in a care home ( Bradley and Sheeran, 2017 ). They can cause severe risks to the patient if left untreated, leading to complications such as pyelonephritis or sepsis ( Ahmed et al, 2018 ).
Mrs M's medication included:
- Paracetamol 1 g as required
- Lactulose 10 ml twice daily
- Docusate 200 mg twice daily
- Epimax cream
- Colecalciferol 400 units daily
- Alendronic acid 70 mg weekly.
She did not take any herbal or over the counter preparations. Her records reported no known drug allergies; however, she was allergic to Elastoplast. A vital part of clinical history involves reviewing current prescribed and non-prescribed medications, herbal remedies and drug allergies, to prevent contraindications or reactions with potential prescribed medication ( Royal Pharmaceutical Society, 2019 ). Several authors, including Malcolm et al (2018) , indicate polypharmacy as a common cause of adverse drug reactions (ADRs), worsening health and affecting a person's quality of life. NICE (2015) only recommends review of patients who are on four or more medications on each new clinical intervention, not taking into account individual drug interactions.
Due to Mrs M's lack of capacity, her social history was obtained via the electronic record and the carer. She moved to the care home 3 years ago, following respite care after her fall and hip replacement. She had never smoked or drank alcohol. Documented family history revealed stroke, ischaemic heart disease and breast cancer. Taylor (2016) reports a good thorough clinical history can equate to 90% of the working diagnosis before examination, potentially reducing unnecessary tests and investigations. This can prove challenging when the patient has confusion. It takes a more investigative approach, gaining access to medical/nursing care notes, and using family or carers to provide further collateral history ( Gupta and Gupta, 2019 ).
As per NICE (2021) guidelines, a physical examination of Mrs M was carried out. On examination it was noted that Mrs M had mild pallor with normal capillary refill time, no signs of peripheral or central cyanosis, and no clinical stigmata to note. Her heart rate was elevated at 112 beats per minute and regular, she had a normal respiration rate of 17 breaths per minute, oxygen saturations (SpO 2 ) were 98% on room air and blood pressure was 116/70 mm/Hg. Her temperature was 37.3oC. According to Doyle and Schortgen (2016) , there is no agreed level of fever; however, it becomes significant when above 38.3oC. Bardsley (2017) adds that older patients do not always present with pyrexia in UTI because of an impaired immune response.
Heart and chest sounds were normal, with no peripheral oedema. The abdomen was non-distended, soft and non-tender on palpation, with no reports of nausea, vomiting, supra-pubic tenderness or loin pain. Loin pain or suprapubic tenderness can indicate pyelonephritis ( Bardsley, 2017 ). Tachycardia, fever, confusion, drowsiness, nausea/vomiting or tachypnoea are strong predictive signs of sepsis ( NICE, 2021 ).
During the consultation, confusion and restlessness were evident. Therefore, it was difficult to ask direct questions to Mrs M regarding pain, nausea and dizziness. Non-verbal cues were considered, as changes in behaviour and restlessness can potentially highlight discomfort or pain ( Swift, 2018 ).
Mrs M's most recent blood tests indicated CKD stage 2, based on an estimated glomerular filtration rate (eGFR) of 82 ml/minute/1.73m 2 . The degree of renal function is vital to establish prior to any prescribing decision, because of the potential increased risk of drug toxicity ( Doogue and Polasek, 2013 ). The agreed level of mild renal impairment is when eGFR is <60 ml/minute/1.73 m 2 , with chronic renal impairment established when eGFR levels are sustained over a 3-month period ( Ahmed et al, 2018 ).
Previous urine samples of Mrs M grew Escherichia coli bacteria, sensitive to nitrofurantoin but resistant to trimethoprim. A consensus of papers, including Lajiness and Lajiness (2019) , highlight the most common pathogen for UTI as E. coli. Fransen et al (2016) indicates that increased use of empirical antibiotics has led to a prevalence of extended spectrum beta lactamase positive (ESBL+) bacteria that are resistant to many current antibiotics. This is not taken into account by the NICE guidelines (2021) ; however, it is discussed in local guidelines ( Barnsley Hospital NHS FT/Rotherham NHS FT, 2022 ).
Mrs M was unable to provide an uncontaminated urine sample due to incontinence. NICE (2021) advocate urine culture as a definitive diagnostic tool for UTIs; however, do not highlight how to objectively obtain this. Bardsley (2017) recognises the benefit of an uncontaminated urinalysis in symptomatic patients, stating that alongside other clinical signs, nitrates and leucocytes strongly predict the possibility of UTI. O'Grady et al (2019) points out that although NICE emphasise urine culture collection, it omits the use of urinalysis as part of the assessment.
Based on Ms M's clinical history and physical examination, a working diagnosis of suspected symptomatic uncomplicated UTI was hypothesised. A decision was made, based on the local antibiotic prescribing guidelines, as well as the NICE (2021) guidelines, to treat empirically with nitrofurantoin modified release (MR), 100 mg twice daily for 3 days, to avoid further health or systemic complications. The use of electronic prescribing was adopted as per local organisational policy and the Royal Pharmaceutical Society (2019) . Electronic prescribing is essential for legibility and sharing of prescribing information. It also acts as an audit on prescribing practices, providing a contemporaneous history for any potential litigation ( Lovatt, 2010 ).
Pharmacokinetics and pharmacodynamics
Lajiness and Lajiness (2019) reflect on the origins of nitrofurantoin back to the 1950s, following high penicillin usage leading to resistance of Gram-negative bacteria. Nitrofurantoin has been the first-line empirical treatment for UTIs internationally since 2010, despite other antibacterial agents being discovered ( Wijma et al, 2020 ). Mckinell et al (2011) highlight that a surge in bacterial resistance brought about interest in nitrofurantoin as a first-line option. Their systematic review of the literature indicated through a cost and efficacy decision analysis that nitrofurantoin was a low resistance and low cost risk; therefore, an effective alternative to trimethoprim or fluoroquinolones. The weakness of this paper is the lack of data on nitrofurantoin cure rates and resistance studies, demonstrating an inability to predict complete superiority of nitrofurantoin over other antibiotics. This could be down to the reduced use of nitrofurantoin treatment at the time.
Fransen et al (2016) reported that minimal pharmacodynamic knowledge of nitrofurantoin exists, despite its strong evidence-based results against most common urinary pathogens, and being around for the last 70 years. Wijma et al (2018) hypothesised this was because of the lack of drug approval requirements in the era when nitrofurantoin was first produced, and the growing incidence of antibiotic resistance. Pharmacokinetics and pharmacodynamics are clinically important to guide effective drug therapy and avoid potential ADRs. Focus on the absorption, distribution, metabolism and excretion (ADME) of nitrofurantoin is needed to evaluate the correct choice for an individual patient, based on a holistic assessment ( Doogue and Polasek, 2013 ).
Nitrofurantoin is structurally made up of 4 carbon and 1 oxygen atoms forming a furan ring, connected to a nitrogroup (–NO 2 ). Its mode of action is predominantly bacteriostatic, with some bactericidal tendencies in high concentration levels ( Wijma et al, 2018 ). It works by inhibiting bacterial cell growth, breaking down its strands of DNA ( Komp Lindgren et al, 2015 ). Hoang and Salbu (2016) add that nitrofurantoin causes bacterial flavoproteins to create reactive medians that halt bacterial ribosomal proteins, rendering DNA/RNA cell wall synthesis inactive.
Nitrofurantoin is administered orally via capsules or liquid. Greener (2011) highlights the different formulations, which originally included microcrystalline tablets and now include macro-crystalline capsules. The increased size of crystals was found to slow absorption rates down ( Hoang and Salbu, 2016 ). Nitrofurantoin is predominantly absorbed via the gastro-intestinal tract, enhanced by an acidic environment. It is advised to take nitrofurantoin with food, to slow down gastric emptying ( Wijma et al, 2018 ). The maximum blood concentration of nitrofurantoin is said to be <0.6 mg/l. Lower plasma concentration equates to lower toxicity risk; therefore, nitrofurantoin is favourable over fluoroquinolones ( Komp Lindgren et al, 2015 ). Wijma et al (2020) found a reduced effect on gut flora compared to fluoroquinolones.
Distribution of nitrofurantoin is mainly via the renal medulla, with a renal bioavailability of 38.8–44%; therefore, it is specific for urinary action ( Hoang and Salbu, 2016 ). Haasum et al (2013) highlight the inability for nitrofurantoin to penetrate the prostate where bacteria concentration levels can be present. Therefore, they do not advocate the use of nitrofurantoin to treat males with UTIs, because of the risk of treatment failure and further complications of systemic infection. This did not appear to be addressed by local guidelines.
The metabolism of nitrofurantoin is not completely understood; however, Wijma et al (2018) indicate several potential metabolic antibacterial actions. Around 0.8–1.8% is metabolised into aminofurantoin, with 80.9% other unknown metabolites ( medicines.org, 2022 ). Wijma et al (2020) calls for further study into the metabolism of nitrofurantoin to aid understanding of the pharmacodynamics.
Excretion of nitrofurantoin is predominantly via urine, with a peak time of 4–5 hours, and 27–50% excreted unchanged in urine ( medicines.org, 2022 ). Komp Lindgren et al (2015) equates the fast rates of renal availability and excretion to lower toxicity risks and targeted treatment for UTI pathogens. Wijma et al (2018) found high plasma concentration levels of nitrofurantoin in renal impairment. Singh et al (2015) indicate that nitrofurantoin is mainly eliminated via glomerular filtration; therefore, its impairment presents the potential risks of treatment failure and increased ADRs. Early guidelines stipulated the need to avoid nitrofurantoin in patients with mild renal impairment, indicating the need for an eGFR of >60 ml/min due to this toxicity risk. This was based on several small studies, cited by Hoang and Salbu (2016) , looking at concentration levels rather than focused on patient treatment outcomes.
Primary research by Geerts et al (2013) involving treatment outcomes in a large cohort study, led to guidelines changing the limit to mild to moderate impairment or eGFR >45 ml/min. However, the risk of ADRs, including pulmonary fibrosis and hepatic changes, were increased in renal insufficiency with prolonged use. The study participants had a mean age of 47.8 years; therefore, the study did not indicate the effects on older patients. Singh et al (2015) presented a Canadian study, looking at treatment success with nitrofurantoin in older females, with a mean age of 79 years. It indicated effective treatment despite mild/moderate renal impairment. It did not address the levels of ADRs or hospitalisation. Ahmed et al (2018) conducted a large, UK-based, retrospective cohort study favouring use of empirical nitrofurantoin in the older population with increased risk of UTI-related hospitalisation and mild/moderate renal impairment. It concluded not treating could increase mortality and morbidity. This led to guidelines to support empirical treatment of symptomatic older patients with nitrofurantoin.
Dosing is highly variable between the local and national guidelines. Greener (2011) highlights that product information for the macro-crystalline capsules recommends 50–100 mg 4 times a day for 7 days when treating acute uncomplicated UTI. Local guidelines from Barnsley Hospital NHS FT/Rotherham NHS FT Adult antimicrobial guide (2022) stipulate 50–100 mg 4 times daily for 3 days for women, whereas NICE (2021) recommends a MR version of 100 mg twice daily for 3 days.
In a systematic literature review on the pharmacokinetics of nitrofurantoin, Wijma et al (2018) found that use of a 5–7 day course had similar strong efficacy rates, whereas 3 days did not, potentially causing treatment failure, equating to poor patient outcomes and resistant behaviour. Deresinski (2018) conducted a small, randomised controlled trial involving 377 patients either on nitrofurantoin MR 100 mg three times a day for 5 days or fosfomycin single dose treatment after urinalysis and culture. It looked at response to treatment after 28 days. Nitrofurantoin was found to have a 78% cure rate compared to 50% with fosfomycin. Therefore, these studies directly contradict current NICE and local guidelines on treatment dosing of UTI in women. More robust studies on dosing regimens are therefore required.
Fransen et al (2016) conducted a non-human pharmacodynamics study looking at time of action to treat on 11 strains of common UTI bacteria including two ESBL+. It demonstrated the kill rate for E. coli was 16–24 hours, slower than Enterobacter cloacae (6–8 hours) and Klebsiella pneumoniae (8 hours). The findings also indicated that nitrofurantoin appeared effective against ESBL+. Dosing and urine concentrations were measured, and found that 100 mg every 6 hours kept the urine concentration levels significant enough to reach peak levels. This study directly contradicted the findings of Lindgren et al (2015) , who conducted similar non-human kinetic style kill rate studies, and found nitrofurantoin's dynamic action to be within 6 hours for E. coli. Both studies have limitations in that they did not take into account human immune response effects.
Wijma et al (2020) highlighted inconsistent dosing regimens in their retrospective audit involving 150 patients treated for UTIs across three Australian secondary care facilities. The predominant dosing of nitrofurantoin was 100 mg twice daily for 5 days for women and 7 days for males. Although a small audit-based paper, it creates debate regarding the lack of clarity around the correct dosing, leaving it open to error. It therefore requires primary research into the follow up of cure rates on guideline prescribing regimens. Dose and timing remains an important issue to reduce treatment failure. It indicates the need for bacteria-dependant dosing, which currently NICE (2021) does not discuss.
Haasum et al (2013) found poor adherence to guidelines for choice and dosing in elderly patients in their Swedish register-based large population study. It highlighted high use of trimethoprim in frail older care home residents, despite guidelines recommending nitrofurantoin as first-line. A recent retrospective, observational, quantitative study by Langner et al (2021) involving 44.9 million women treated for a UTI in the USA across primary and secondary care, found an overuse of fluoroquinolones and underuse of nitrofurantoin and trimethoprim, especially by primary care physicians for older Asian and socio-economically deprived patients. Both these studies did not seek a true qualitative rationale for choices of antibiotics; therefore, limiting the findings.
Legal and ethical considerations
NMP regulation of best practice is set by the Royal Pharmaceutical Society framework (2019) , incorporating several acts of law including the medicines act 1968, and medicinal products prescribed by the Nurses Act (1992). As per Nursing Midwifery Council (2021) Code of Conduct and Health Education England (2020), ANPs have a duty of care to patients, ensuring that they work within their area of competence and recognise any limitations, demonstrating accountability for decisions made ( Lovatt, 2010 ).
Empirical treatment of UTIs is debated in the literature. O'Grady et al (2019) summarises that empirical treatment can reduce further UTI complications that can lead to acute health needs and hospitalisation, without increased risk of antibiotic resistance. Greener (2011) states that uncomplicated UTIs can be self-limiting; therefore, not always warranting antibiotic treatment if sound self-care advice is adopted. Chardavoyne and Kasmire (2020) discuss delayed prescribing, involving putting the onus on the patient and carers, which was not advisable in the case of Mrs M. Bradley and Sheeran (2017) found that three quarters of antibiotics in care home residents were prescribed inaccurately, hence recommended a watch and wait approach to treatment in the older care home resident, following implementation of a risk reduction strategy.
Taylor (2016) recommended an individual, holistic approach, incorporating ethical considerations such as choice, level of concordance, understanding and agreement of treatment choice. This can prove difficult in a case such as Mrs M. If a patient is deemed to lack capacity, a decision to act in the patient's best interest should be applied ( Gupta and Gupta, 2019 ). Therefore, understanding a patient's beliefs and values via family or carers should be explored, balancing the needs and possible outcomes. The principle of non-maleficence should be adopted, looking at risks versus benefits on prescribing the antibiotic to the individual patient ( Royal Pharmaceutical Society, 2019 ).
Non-pharmacological advice was provided to the carers to ensure that Mrs M maintained good fluid intake of 2 litres in 24 hours. NICE (2021) advocates the use of written self-care advice leaflets that have been produced to educate patients and/or carers on non-pharmacological actions, supporting recovery and improving outcomes. The use of paracetamol for symptoms of fever and/or pain was also recommended for Mrs M. Prevention strategies proposed by Lajiness and Lajiness (2019) included looking at the benefits of oestrogen cream in post-menopausal women in reducing the incidence of UTIs. Cranberry juice, probiotics and vitamin C ingestion are not supported by any strong evidence base.
There is a duty of care to ensure that follow up of the patient during and after treatment is delivered by the NMP ( Chardavoyne and Kasmire, 2020 ). Clinical safety netting advice was discussed with the carers to monitor Mrs M for any deterioration, and to seek further clinical review urgently. Particular attention to signs of ADRs and sepsis, and the need for 999 response if these occurred, was advocated. A treatment plan was also sent to the GP to ensure sound communication and continuation of safe care ( Taylor, 2016 ).
Professional development issues
The extended role of prescribing brings additional responsibility, with onus on both the NMP and the employer vicariously, to ensure key skills are updated. This is where continued professional development involving research, training and knowledge is sought and applied, using evidence-based, up-to-date practice ( HEE, 2020 ). Adoption of antibiotic stewardship is highlighted by several papers including Lajiness and Lajiness (2019) . They advise nine points to consider, to increase knowledge around the actions and consequences of the drug by the prescriber. Despite no acknowledgment in NICE (2021) guidance, previous results of infections and sensitivities are also proposed as vital in antibiotic stewardship.
The use of decision support tools, proposed by Malcolm et al (2018) , involves an audit approach looking at antibiograms, that highlight local microbiology resistance patterns to aid antibiotic choices, alongside a risk reduction team strategy. Bradley and Sheeran (2017) looked at improving antibiotic use for UTI treatment in a care home in Pennsylvania. They employed a programme of monitoring and educating clinical staff, patients, carers and relatives in evidence-based self-care and clinical assessment skills over a 30-month period. It demonstrated a reduction in inappropriate antibiotic prescribing, and an improvement in monitoring symptoms and self-care practices, creating better patient outcomes. It was evaluated highly by nursing staff, who reported a sense of autonomy and confidence involving team work. Langner et al (2021) calls for further education and feedback to prescribers, involving pharmacists and microbiology data to identify and understand patterns of prescribing.
UTIs can be misdiagnosed and under- or over-treated, despite the presence of local and national guidelines. Continued monitoring of nitrofurantoin use requires priority, due to its first-line treatment status internationally, as this may increase reliance and overuse of the drug, with potential for resistant strains of bacteria becoming prevalent.
Diligent clinical assessment skills and prescribing of appropriate treatment is paramount to ensure risk of serious complications, hospitalisation and mortality are reduced, while quality of life is maintained. The use of competent clinical practice, up-to-date evidence-based knowledge, good communication and understanding of individual patient needs, and concordance are essential to make sound prescribing choices to avoid harm. As well as the prescribing of medications, the education, monitoring and follow-up of the patient and prescribing practices are equally a vital part of the autonomous role of the NMP.
KEY POINTS:
- Urinary tract infections (UTIs) can be misdiagnosed and under- or over-treated, despite the presence of local and national guidelines
- The incidence of UTI increases with age, with those over 65 years of age being five times more likely to develop a UTI at any point
- Nitrofurantoin has been the first-line empirical treatment for UTIs internationally since 2010. Its mode of action is predominantly bacteriostatic, with some bactericidal tendencies in high concentration levels
- Diligent clinical assessment skills and prescribing of appropriate treatment is paramount to ensure risk of serious complications, hospitalisation and mortality are reduced, while quality of life is maintained
CPD REFLECTIVE PRACTICE:
- How can a good clinical history be gained if the patient lacks capacity?
- What factors need to be considered when safety netting in cases like this?
- What non-pharmacological advice would you give to a patient with a urinary tract infection (or their carers)?
- How will this article change your clinical practice?
A Practical Guideline on Sampling and Analysis of Urine and Blood Specimens in Urinary Tract Infections
- First Online: 08 June 2024
Cite this chapter

- Tommaso Cai 3 , 4 , 5 &
- Truls E. Bjerklund Johansen 4 , 5 , 6
18 Accesses
A urine specimen for culture should be collected prior to the initiation of antimicrobial therapy in all cases of UTI, except for uncomplicated cystitis where an empirical treatment can be administered without a urine culture. The universally accepted diagnostic criterion for a urinary tract infection based on a voided specimen is ≥10 5 CFU/mL of a single Gram-negative organism. A urine culture sample should be taken after catheter replacement in case of CAUTI. In uncomplicated infections of the upper urinary tract, urine analysis and urine culture are strongly recommended. In all patients with fever or suspected sepsis, a blood culture is strongly recommended. The aim of this chapter is to provide practical guidelines on sampling of urine and blood specimens in urinary tract infections and to give an introduction to the diagnostic verification of urinary tract infection by culture tests and urinalysis.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
European Association of Urology Guidelines on urological infections. https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Urological-Infections-2022.pdf .
ICUD book on urogenital infections. http://www.icud.info/urogenitalinfections.html .
Nicolle LE. Urinary tract infection. Crit Care Clin. 2013;29(3):699–715. https://doi.org/10.1016/j.ccc.2013.03.014 .
Article PubMed Google Scholar
McCarter YS, Sharp SE. Laboratory diagnosis of urinary tract infections. Washington, DC: ASM Press; 2009. p. 25.
Google Scholar
Platt R. Quantitative definition of bacteriuria. Am J Med. 1983;75(1B):44–52.
Article CAS PubMed Google Scholar
Kunin CM. Bacteriuria, pyuria, proteinuria, hematuria, and pneumaturia. In: Kunin CM, editor. Urinary tract infections: detection, prevention, and management. Baltimore: Williams & Wilkins; 1997. p. 9.
Hooton TM, Stapleton AE, Roberts PL, and Stamm WE, Comparison of microbiologic findings in paired midstream and catheter urine specimens from women with acute uncomplicated cystitis. Abstract L-609 48th annual ICAAC, Washington DC, 2008
Kass EH. Chemotherapeutic and antibiotic drugs in the management of infections of the urinary tract. Am J Med. 1955;18(5):764–81.
Stamm WE, Counts GW, Running KR, Fihn S, Turck M, Holmes KK. Diagnosis of coliform infection in acutely dysuric women. N Engl J Med. 1982;307(8):463–8.
Rubin RH, Shapiro ED, Andriole VT, Davis RJ, Stamm WE. Evaluation of new anti-infective drugs for the treatment of urinary tract infection. Infectious Diseases Society of America and the Food and Drug Administration. Clin Infect Dis. 1992;15(Suppl 1):S216–27.
Opota O, Croxatto A, Prod'hom G, Greub G. Blood culture-based diagnosis of bacteraemia: state of the art. Clin Microbiol Infect. 2015;21(4):313–22. https://doi.org/10.1016/j.cmi.2015.01.003 .
Lala V, Minter DA. Acute cystitis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022.
Download references
Author information
Authors and affiliations.
Department of Urology, Santa Chiara Regional Hospital, Trento, Italy
Tommaso Cai
Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Tommaso Cai & Truls E. Bjerklund Johansen
Department of Urology, Oslo University Hospital, Oslo, Norway
Institute of Clinical Medicine, University of Aarhus, Aarhus, Denmark
Truls E. Bjerklund Johansen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Tommaso Cai .
Editor information
Editors and affiliations.
Department of Urology, Santa Chiara Regional Hospital, Trento, Trento, Italy
Rights and permissions
Reprints and permissions
Copyright information
© 2024 Springer Nature Switzerland AG
About this chapter
Cai, T., Bjerklund Johansen, T.E. (2024). A Practical Guideline on Sampling and Analysis of Urine and Blood Specimens in Urinary Tract Infections. In: Bjerklund Johansen, T.E., Cai, T. (eds) Guide to Antibiotics in Urology. Springer, Cham. https://doi.org/10.1007/978-3-319-92366-6_3
Download citation
DOI : https://doi.org/10.1007/978-3-319-92366-6_3
Published : 08 June 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-319-92365-9
Online ISBN : 978-3-319-92366-6
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Patient Care & Health Information
- Diseases & Conditions
- Urinary tract infection (UTI)
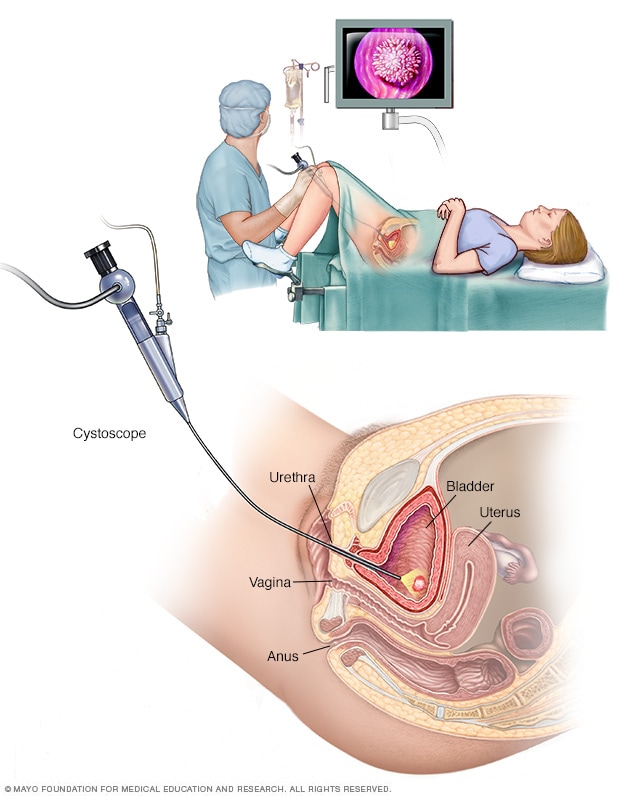
Female cystoscopy
Cystoscopy allows a health care provider to view the lower urinary tract to look for problems, such as a bladder stone. Surgical tools can be passed through the cystoscope to treat certain urinary tract conditions.
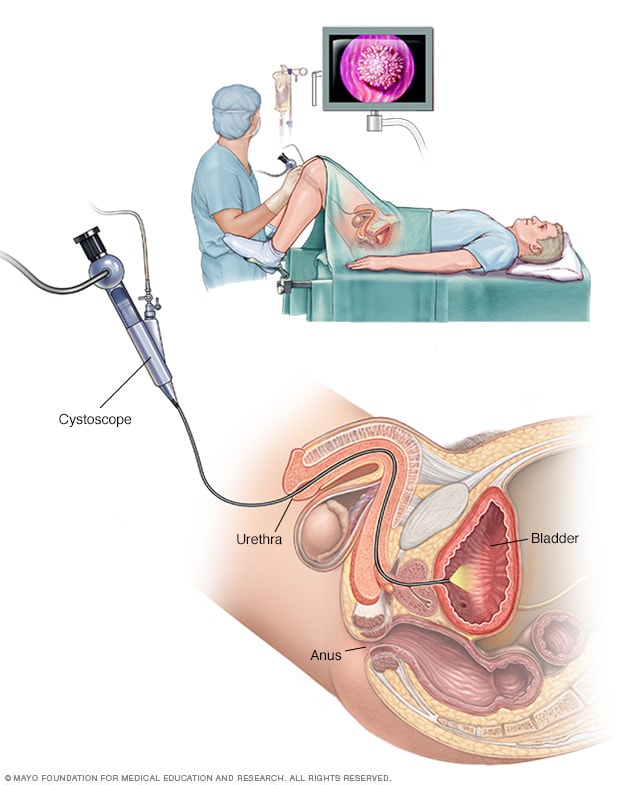
Male cystoscopy
Cystoscopy allows a health care provider to view the lower urinary tract to look for problems in the urethra and bladder. Surgical tools can be passed through the cystoscope to treat certain urinary tract conditions.
Tests and procedures used to diagnose urinary tract infections include:
- Analyzing a urine sample. Your health care provider may ask for a urine sample. The urine will be looked at in a lab to check for white blood cells, red blood cells or bacteria. You may be told to first wipe your genital area with an antiseptic pad and to collect the urine midstream. The process helps prevent the sample from being contaminated.
- Growing urinary tract bacteria in a lab. Lab analysis of the urine is sometimes followed by a urine culture. This test tells your provider what bacteria are causing the infection. It can let your provider know which medications will be most effective.
- Creating images of the urinary tract. Recurrent UTI s may be caused by a structural problem in the urinary tract. Your health care provider may order an ultrasound, a CT scan or MRI to look for this issue. A contrast dye may be used to highlight structures in your urinary tract.
- Using a scope to see inside the bladder. If you have recurrent UTI s, your health care provider may perform a cystoscopy. The test involves using a long, thin tube with a lens, called a cystoscope, to see inside the urethra and bladder. The cystoscope is inserted in the urethra and passed through to the bladder.
- Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your Urinary tract infection (UTI)-related health concerns Start Here
Antibiotics usually are the first treatment for urinary tract infections. Your health and the type of bacteria found in your urine determine which medicine is used and how long you need to take it.
Simple infection
Medicines commonly used for simple UTI s include:
- Trimethoprim and sulfamethoxazole (Bactrim, Bactrim DS)
- Fosfomycin (Monurol)
- Nitrofurantoin (Macrodantin, Macrobid, Furadantin)
- Ceftriaxone
The group of antibiotics known as fluoroquinolones isn't commonly recommended for simple UTI s. These drugs include ciprofloxacin (Cipro), levofloxacin and others. The risks of these drugs generally outweigh the benefits for treating uncomplicated UTI s.
In cases of a complicated UTI or kidney infection, your health care provider might prescribe a fluoroquinolone medicine if there are no other treatment options.
Often, UTI symptoms clear up within a few days of starting treatment. But you may need to continue antibiotics for a week or more. Take all of the medicine as prescribed.
For an uncomplicated UTI that occurs when you're otherwise healthy, your health care provider may recommend a shorter course of treatment. That may mean taking an antibiotic for 1 to 3 days. Whether a short course of treatment is enough to treat your infection depends on your symptoms and medical history.
Your health care provider also may give you a pain reliever to take that can ease burning while urinating. But pain usually goes away soon after starting an antibiotic.
Frequent infections
If you have frequent UTI s, your health care provider may recommend:
- Low-dose antibiotics. You might take them for six months or longer.
- Diagnosing and treating yourself when symptoms occur. You'll also be asked to stay in touch with your provider.
- Taking a single dose of antibiotic after sex if UTI s are related to sexual activity.
- Vaginal estrogen therapy if you've reached menopause.
Severe infection
For a severe UTI , you may need IV antibiotics in a hospital.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Urinary tract infections can be painful, but you can take steps to ease discomfort until antibiotics treat the infection. Follow these tips:
- Drink plenty of water. Water helps to dilute your urine and flush out bacteria.
- Avoid drinks that may irritate your bladder. Avoid coffee, alcohol, and soft drinks containing citrus juices or caffeine until the infection has cleared. They can irritate your bladder and tend to increase the need to urinate.
- Use a heating pad. Apply a warm, but not hot, heating pad to your belly to help with bladder pressure or discomfort.
Alternative medicine
Many people drink cranberry juice to prevent UTI s. There's some indication that cranberry products, in either juice or tablet form, may have properties that fight an infection. Researchers continue to study the ability of cranberry juice to prevent UTI s, but results aren't final.
There's little harm in drinking cranberry juice if you feel it helps you prevent UTI s, but watch the calories. For most people, drinking cranberry juice is safe. However, some people report an upset stomach or diarrhea.
But don't drink cranberry juice if you're taking blood-thinning medication, such as warfarin (Jantovin).
Preparing for your appointment
Your primary care provider, nurse practitioner or other health care provider can treat most UTI s. If you have frequent UTI s or a chronic kidney infection, you may be referred to a health care provider who specializes in urinary disorders. This type of doctor is called a urologist. Or you may see a health care provider who specializes in kidney disorders. This type of doctor is called a nephrologist.
What you can do
To get ready for your appointment:
- Ask if there's anything you need to do in advance, such as collect a urine sample.
- Take note of your symptoms, even if you're not sure they're related to a UTI .
- Make a list of all the medicines, vitamins or other supplements that you take.
- Write down questions to ask your health care provider.
For a UTI , basic questions to ask your provider include:
- What's the most likely cause of my symptoms?
- Are there any other possible causes?
- Do I need any tests to confirm the diagnosis?
- What factors do you think may have contributed to my UTI ?
- What treatment approach do you recommend?
- If the first treatment doesn't work, what will you recommend next?
- Am I at risk of complications from this condition?
- What is the risk that this problem will come back?
- What steps can I take to lower the risk of the infection coming back?
- Should I see a specialist?
Don't hesitate to ask other questions as they occur to you during your appointment.
What to expect from your doctor
Your health care provider will likely ask you several questions, including:
- When did you first notice your symptoms?
- Have you ever been treated for a bladder or kidney infection?
- How severe is your discomfort?
- How often do you urinate?
- Are your symptoms relieved by urinating?
- Do you have low back pain?
- Have you had a fever?
- Have you noticed vaginal discharge or blood in your urine?
- Are you sexually active?
- Do you use contraception? What kind?
- Could you be pregnant?
- Are you being treated for any other medical conditions?
- Have you ever used a catheter?
Urinary tract infection (UTI) care at Mayo Clinic
- Partin AW, et al., eds. Infections of the urinary tract. In: Campbell-Walsh-Wein Urology. 12th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed June 13, 2022.
- Ferri FF. Urinary tract infection. In: Ferri's Clinical Advisor 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed June 13, 2022.
- Bladder infection (urinary tract infection) in adults. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/bladder-infection-uti-in-adults. Accessed June 13, 2022.
- Urinary tract infections (UTIs). The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/urinary-tract-infections. Accessed June 13, 2022.
- Cai T. Recurrent uncomplicated urinary tract infections: Definitions and risk factors. GMS Infectious Diseases. 2021; doi:10.3205/id000072.
- Hooton TM, et al. Acute simple cystitis in women. https://www.uptodate.com/contents/search. Accessed June 14, 2022.
- Pasternack MS. Approach to the adult with recurrent infections. https://www.uptodate.com/contents/search. Accessed June 14, 2022.
- Cranberry. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/cranberry. Accessed June 13, 2022.
- Goebel MC, et al. The five Ds of outpatient antibiotic stewardship for urinary tract infections. Clinical Microbiology Reviews. 2021; doi:10.1128/CMR.00003-20.
- Overactive bladder (OAB): Lifestyle changes. Urology Care Foundation. https://urologyhealth.org/urologic-conditions/overactive-bladder-(oab)/treatment/lifestyle-changes. Accessed June 13, 2022.
- Nguyen H. Allscripts EPSi. Mayo Clinic. May 5, 2022.
- AskMayoExpert. Urinary tract infection (adult). Mayo Clinic; 2022.

News from Mayo Clinic
- UTI: This common infection can be serious Jan. 12, 2024, 04:24 p.m. CDT
- Mayo Clinic Q and A: 6 UTI myths and facts Feb. 02, 2023, 01:42 p.m. CDT
- 5 tips to prevent a urinary tract infection July 12, 2022, 04:41 p.m. CDT
Products & Services
- A Book: Mayo Clinic Guide to Home Remedies
- A Book: Taking Care of You
- Assortment of Health Products from Mayo Clinic Store
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
Is It a Urinary Tract Infection (UTI)? What Women Should Know
BY Lisa Fields June 7, 2024

People usually feel relief when they empty their bladders—unless they have a urinary tract infection (UTI) . Instead of comfort, they may experience a burning sensation or other symptoms when they urinate, prompting them to visit the doctor.
A UTI is a bacterial infection that affects the urinary tract. Most are caused by Escherichia coli ( E. coli ), although other bacteria are sometimes responsible.
UTIs occur when bacteria enter the urinary tract through the urethra, the thin tube that runs from your bladder to the opening where urine exits your body. UTIs may affect the urethra, bladder, kidneys, or ureters, which are thin tubes that connect the kidneys to the bladder.
Urinary tract infections are much more common among women than men. “UTIs tend to increase in frequency when women enter the postmenopausal stage, but it certainly can happen across the lifespan,” says Yale Medicine urogynecologist Leslie Rickey, MD, MPH . “UTIs are impactful on people’s quality of life. They are more than just an annoyance; they can really affect people’s ability to participate in social, work, and travel activities.”
Below, Dr. Rickey shares information on how to know if you have a UTI.
1. What are the symptoms of UTIs?
People with UTIs often experience one or more of the following symptoms:
- Pain or burning during urination
- More frequent urination than usual
- Increased feelings of urinary urgency
- Releasing only a small amount of urine, despite a strong urgency
- Discomfort in the lower abdomen
- Sensation of an inability to completely empty the bladder
- Blood in the urine (if you have visible blood in your urine, you should let your doctor know as soon as possible)
It’s important to note that just having bacteria in your urine doesn’t mean you have a UTI. With a few exceptions (noted below), the presence of bacteria doesn’t automatically mean that you need antibiotics.
“If someone has bacteria in their urine and no urinary symptoms, that’s called asymptomatic bacteriuria, and it does not need to be treated in most people,” Dr. Rickey says. “In special circumstances, women may be screened for bacteriuria, such as during pregnancy and prior to undergoing certain urologic procedures.”
2. Why are UTIs more common in women?
Women likely experience UTIs significantly more often than men because of the anatomical differences between males and females.
A female has a short urethra, which starts at the bladder and ends near the vaginal opening, where urine exits the body, so the bacteria don’t have as far to travel to reach the bladder. Also, in women, the opening to the urethra is closer to the rectum, where fecal matter (stool) leaves the body. Bacteria in the anorectal area may enter the urethra, causing infection.
“It’s thought that the rectum—and the stool—is a reservoir for uropathogens, which are bacteria that can cause infections in the urinary tract,” Dr. Rickey says.
Males have a much longer urethra than females. The male urethra runs from the bladder through the length of the penis. For males, the opening to the urethra is at the end of the penis, which isn’t as close to the rectum. This makes it less likely for bacterial contamination from the anorectal area to occur. Men, however, are more likely to get UTIs if they have enlarged prostates. (When a man has an enlarged prostate and has trouble emptying his bladder, bacteria are more likely to build up in the urine. That urine remains for longer periods within the bladder, leading to a urinary tract infection.)
Certain conditions increase the risk of UTIs in females, such as being sexually active (bacteria may be introduced to the vaginal area during sexual activity), using spermicides (which can affect the vaginal biome), or being postmenopausal. “Getting UTIs during menopause probably has to do with changes in the vaginal microbiome associated with changes in estrogen levels,” Dr. Rickey says. “There may be some changes in the bladder lining as well.”
3. How are UTIs diagnosed?
Many people who experience UTI-like symptoms go to their primary care physician or an urgent care facility for care. At the appointment, your doctor should ask you to leave a urine sample.
“Having a urinary tract infection diagnosis requires both symptoms and a positive urine test,” Dr. Rickey says. “Therefore, it’s helpful to have the urine test to determine whether urinary bacteria are causing the symptoms.”
A urine sample is analyzed in a laboratory to determine whether or not you have a urinary tract infection and, if you do, which bacteria are causing it.
Sometimes, doctors will treat a UTI before getting the patient’s urinalysis results back.
“If someone has very clear symptoms of a UTI, and it’s maybe their first one or they get a UTI infrequently, there’s a decent chance their health care provider might just treat them,” Dr. Rickey says. “But if a woman is having frequent or repeated UTI episodes, then a urine specimen should be obtained for testing.” Recurrent UTIs are defined as having more than two infections in six months or more than three infections in a year.
Some people check to see if they have a UTI from the privacy of their own homes, since there are over-the-counter tests to screen for UTIs. At-home tests are used by some patients as a screening tool, but sometimes the results provide false positives or negatives.
“Additional lab testing may be necessary before a provider will prescribe antibiotics,” Dr. Rickey says.
4. How are UTIs treated?
Because UTIs are bacterial infections, they are most often treated with antibiotics.
“Macrobid, bactrim, and fosfomycin are the first-line antibiotics recommended,” Dr. Rickey says. “We’re usually going to start with these, unless a patient has an allergy to the medication or has had a recent UTI that was resistant to these antibiotics.”
Resistant bacteria can create a problem as there are fewer antibiotic options for treatment. “This is one of the reasons why we try to avoid the unnecessary use of antibiotics, because you can create resistant bacteria that have less available treatment options in terms of effective antibiotics,” Dr. Rickey says.
For women getting frequent infections, there are various options for trying to prevent UTIs.
“There are some common nonantibiotic prevention strategies. There is very good evidence of the effectiveness of vaginal estrogen therapy in preventing UTIs and also increasing evidence of how cranberry supplements can help. Another popular option is an over-the-counter [OTC] supplement called D-mannose,” Dr. Rickey says.
Vaginal estrogen therapy includes creams or tablets that are used in the vagina a few times a week, says Dr. Rickey. The vaginal estrogen cream requires a prescription from a medical provider.
Vaginal estrogen likely works by restoring the vaginal pH and microbiome, Dr. Rickey says, while cranberry and D-mannose help prevent certain bacteria, including E. coli bacteria, from attaching to surfaces within the urinary tract. Because most UTIs are caused by E. coli , these supplements may be helpful for controlling UTIs. However, more research is needed to determine the mechanism of action and effectiveness. Because D-mannose is a type of sugar, people with diabetes should not take this supplement unless they talk to their doctor.
If women continue to have recurrent UTIs despite these treatments, they may be prescribed a low-dose antibiotic to take daily in order to reduce the number of UTIs that occur.
5. How can you help prevent UTIs?
Certain habits may help to decrease the risk of getting UTIs. These suggestions may help:
- Stay hydrated. Drink enough water throughout the day; six to eight glasses daily may be effective. “The increased fluid intake recommendation is evidence-based—it has been shown in a study to help reduce UTIs in women getting frequent UTIs,” Dr. Rickey says.
- Go to the bathroom at appropriate intervals. “The act of voiding flushes out the bladder and helps to decrease the risk of bacterial numbers building up,” Dr. Rickey says. A healthy voiding interval is not well defined, but is probably at least every three to four hours, depending on your fluid intake. Holding urine in your bladder for a very long time may increase the risk of a UTI.
- Urinate after having sex. Women who are sexually active are at an increased risk of UTIs, but using the bathroom before and after sex may decrease that risk.
- Take cranberry tablets. This OTC product works by preventing bacteria from sticking to the bladder wall. OTC tablets are better than cranberry-based beverages. “We’ve tried to get people away from drinking the cranberry juice cocktail, which can have a lot of sugar or artificial sweetener and probably doesn’t have the concentration of the active cranberry metabolite,” Dr. Rickey says. Look for a dietary supplement with 36 mg of proanthocyanidins (PACs).
- Practice good hygiene. When using the bathroom, women getting frequent UTIs may want to practice wiping front to back instead of back to front. “I’m not sure there’s a lot of evidence behind that, but I think it may help, and it certainly doesn’t hurt,” Dr. Rickey says.
- See a bladder specialist. If you’re a woman who gets frequent UTIs, your doctor may refer you to a urologist or urogynecologist. It’s uncommon for women to have an anatomic cause for recurrent UTIs, but sometimes additional tests may be helpful. Most importantly, they can work with you to reduce your risk of future UTIs.
More news from Yale Medicine


VICTORIA J. SHARP, MD, DANIEL K. LEE, MD, AND ERIC J. ASKELAND, MD
A more recent article on office-based urinalysis is available.
Am Fam Physician. 2014;90(8):542-547
Author disclosure: No relevant financial affiliations.
Urinalysis is useful in diagnosing systemic and genitourinary conditions. In patients with suspected microscopic hematuria, urine dipstick testing may suggest the presence of blood, but results should be confirmed with a microscopic examination. In the absence of obvious causes, the evaluation of microscopic hematuria should include renal function testing, urinary tract imaging, and cystoscopy. In a patient with a ureteral stent, urinalysis alone cannot establish the diagnosis of urinary tract infection. Plain radiography of the kidneys, ureters, and bladder can identify a stent and is preferred over computed tomography. Asymptomatic bacteriuria is the isolation of bacteria in an appropriately collected urine specimen obtained from a person without symptoms of a urinary tract infection. Treatment of asymptomatic bacteriuria is not recommended in nonpregnant adults, including those with prolonged urinary catheter use.
Urinalysis with microscopy has proven to be an invaluable tool for the clinician. Urine dipstick testing and microscopy are useful for the diagnosis of several genitourinary and systemic conditions. 1 , 2 In 2005, a comprehensive review of urinalysis was published in this journal. 3 This article presents a series of case scenarios that illustrate how primary care physicians can utilize the urinalysis in common clinical situations.
| Microscopic confirmation of a positive urine dipstick test is required to diagnose microscopic hematuria. | C | |
| The initial evaluation of patients with asymptomatic microscopic hematuria should include renal function testing, urinary tract imaging, and cystoscopy. | C | |
| Computed tomographic urography is the preferred imaging modality for the evaluation of patients with asymptomatic microscopic hematuria. | C | , |
| Treatment of asymptomatic bacteriuria is not recommended in nonpregnant adults, including those with prolonged urinary catheter use. | C |
Microscopic Hematuria: Case 1
Microscopic hematuria is common and has a broad differential diagnosis, ranging from completely benign causes to potentially invasive malignancy. Causes of hematuria can be classified as glomerular, renal, or urologic 3 – 5 ( Table 1 6 ) . The prevalence of asymptomatic microscopic hematuria varies among populations from 0.18% to 16.1%. 4 The American Urological Association (AUA) defines asymptomatic microscopic hematuria as three or more red blood cells per high-power field in a properly collected specimen in the absence of obvious causes such as infection, menstruation, vigorous exercise, medical renal disease, viral illness, trauma, or a recent urologic procedure. 5 Microscopic confirmation of a positive dipstick test for microscopic hematuria is required. 5 , 7
| Familial causes | |
| Fabry disease | |
| Hereditary nephritis (Alport syndrome) | |
| Nail-patella syndrome | |
| Thin basement membrane nephropathy | |
| Primary glomerulonephritis | |
| Focal segmental glomerulosclerosis | |
| Goodpasture syndrome | |
| Henoch-Schönlein purpura | |
| Immunoglobulin A nephropathy (Berger disease) | |
| Mesangial proliferative glomerulonephritis | |
| Postinfectious glomerulonephritis | |
| Rapidly progressive glomerulonephritis | |
| Secondary glomerulonephritis | |
| Hemolytic uremic syndrome | |
| Systemic lupus nephritis | |
| Thrombotic thrombocytopenic purpura | |
| Vasculitis | |
| Polycystic kidney disease | |
| Renal artery embolism | |
| Renal papillary necrosis | |
| Renal vein thrombosis | |
| Sickle cell disease or trait | |
| Arteriovenous malformation | |
| Hypercalciuria | |
| Hyperuricosuria | |
| Loin pain–hematuria syndrome | |
| Malignant hypertension | |
| Medullary sponge kidney | |
| Benign prostatic hyperplasia | |
| Cancer (kidney, ureteral, bladder, prostate, or urethral) | |
| Cystitis/pyelonephritis | |
| Nephrolithiasis | |
| Prostatitis | |
| infection | |
| Tuberculosis | |
| Drugs (e.g., nonsteroidal anti-inflammatory drugs, heparin, warfarin [Coumadin], cyclophosphamide) | |
| Trauma (e.g., contact sports, running, Foley catheter) | |
DIAGNOSTIC APPROACH
Case 1: microscopic hematuria.
A 58-year-old truck driver with a 30-year history of smoking one pack of cigarettes per day presents for a physical examination. He reports increased frequency of urination and nocturia, but does not have gross hematuria. Physical examination reveals an enlarged prostate. Results of his urinalysis with microscopy are shown in Table 2 .
Based on this patient's history, symptoms, and urinalysis findings, which one of the following is the most appropriate next step?
A. Repeat urinalysis in six months.
B. Obtain blood urea nitrogen and creatinine levels, perform computed tomographic urography, and refer for cystoscopy.
C. Treat with an antibiotic and repeat the urinalysis with microscopy.
D. Inform him that his enlarged prostate is causing microscopic hematuria, and that he can follow up as needed.
E. Perform urine cytology to evaluate for bladder cancer.
The correct answer is B .
| Color | Pale yellow | — |
| Clarity | Clear | — |
| pH | 6.5 | — |
| Specific gravity | 1.010 | — |
| Glucose | Negative | Negative |
| Blood | 1+ | Negative |
| Ketones | Negative | Negative |
| Protein | Negative | Negative |
| Urobilinogen | Negative | Negative |
| Bilirubin | Negative | Negative |
| Leukocyte esterase | Negative | Negative |
| Nitrite | Negative | Negative |
| White blood cells | 1 per high-power field | 0 to 5 per high-power field |
| Red blood cells | 7 per high-power field | 0 to 4 per high-power field |
| Squamous epithelial cells | None | None |
For the patient in case 1 , because of his age, clinical history, and lack of other clear causes, the most appropriate course of action is to obtain blood urea nitrogen and creatinine levels, perform computed tomographic urography, and refer the patient for cystoscopy. 5 An algorithm for diagnosis, evaluation, and follow-up of patients with asymptomatic microscopic hematuria is presented in Figure 1 . 5 The AUA does not recommend repeating urinalysis with microscopy before the workup, especially in patients who smoke, because tobacco use is a risk factor for urothelial cancer ( Table 3 ) . 5
| Analgesic abuse |
| Exposure to chemicals or dyes (benzenes or aromatic amines) |
| History of chronic indwelling foreign body |
| History of chronic urinary tract infection |
| History of exposure to carcinogenic agents or chemotherapy (e.g., alkylating agents) |
| History of gross hematuria |
| History of irritative voiding symptoms |
| History of pelvic irradiation |
| History of urologic disorder or disease |
| Male sex |
| Older than 35 years |
| Smoking (past or current) |
A previous article in American Family Physician reviewed the American College of Radiology's Appropriateness Criteria for radiologic evaluation of microscopic hematuria. 8 Computed tomographic urography is the preferred imaging modality for the evaluation of patients with asymptomatic microscopic hematuria. 5 , 8 It has three phases that can detect various causes of hematuria. The non–contrast-enhanced phase is optimal for detecting stones in the urinary tract; the nephrographic phase is useful for detecting renal masses, such as renal cell carcinoma; and the delayed phase outlines the collecting system of the urinary tract and can help detect urothelial malignancies of the upper urinary tract. 9 Although the delayed phase can detect some bladder masses, it should not replace cystoscopy in the evaluation for bladder malignancy. 9 After a negative microscopic hematuria workup, the patient should continue to be followed with yearly urinalysis until at least two consecutive normal results are obtained. 5
In patients with microscopic hematuria, repeating urinalysis in six months or treating empirically with antibiotics could delay treatment of potentially curable diseases. It is unwise to assume that benign prostatic hyperplasia is the explanation for hematuria, particularly because patients with this condition typically have risk factors for malignancy. Although urine cytology is typically part of the urologic workup, it should be performed at the time of cystoscopy; the AUA does not recommend urine cytology as the initial test. 5
Dysuria and Flank Pain After Lithotripsy: Case 2
After ureteroscopy with lithotripsy, a ureteral stent is often placed to maintain adequate urinary drainage. 10 The stent has one coil that lies in the bladder and another that lies in the renal pelvis. Patients with ureteral stents may experience urinary frequency, urgency, dysuria, flank pain, and hematuria. 10 They may have dull flank pain that becomes sharp with voiding. This phenomenon occurs because the ureteral stent bypasses the normal nonrefluxing uretero-vesical junction, resulting in transmission of pressure to the renal pelvis with voiding. Approximately 80% of patients with a ureteral stent experience stent-related pain that affects their daily activities. 11
POTENTIALLY MISLEADING URINALYSIS
Case 2: dysuria and flank pain after lithotripsy.
A 33-year-old woman with a history of nephrolithiasis presents with a four-week history of urinary frequency, urgency, urge incontinence, and dysuria. She recently had ureteroscopy with lithotripsy of a 9-mm obstructing left ureteral stone; she does not know if a ureteral stent was placed. She has constant dull left flank pain that becomes sharp with voiding. Results of her urinalysis with microscopy are shown in Table 4 .
A. Treat with three days of ciprofloxacin (Cipro), and tailor further antibiotic therapy according to culture results.
B. Treat with 14 days of ciprofloxacin, and tailor further antibiotic therapy according to culture results.
C. Obtain a urine culture and perform plain radiography of the kidneys, ureters, and bladder.
D. Perform a 24-hour urine collection for a metabolic stone workup.
E. Perform computed tomography.
The correct answer is C .
| Color | Yellow | — |
| Clarity | Clear | — |
| pH | 6.0 | — |
| Specific gravity | 1.010 | — |
| Glucose | Negative | Negative |
| Blood | 2+ | Negative |
| Ketones | Negative | Negative |
| Protein | Negative | Negative |
| Urobilinogen | Negative | Negative |
| Bilirubin | Negative | Negative |
| Leukocyte esterase | 2+ | Negative |
| Nitrite | Negative | Negative |
| White blood cells | 15 per high-power field | 0 to 5 per high-power field |
| Red blood cells | 6 per high-power field | 0 to 4 per high-power field |
| Squamous epithelial cells | None | None |
The presence of a ureteral stent causes mucosal irritation and inflammation; thus, findings of leukocyte esterase with white and red blood cells are not diagnostic for urinary tract infection, and a urine culture is required. In this setting, plain radiography of the kidneys, ureters, and bladder would be useful to determine the presence of a stent. If a primary care physician identifies a neglected ureteral stent, prompt urologic referral is indicated for removal. Retained ureteral stents may become encrusted, and resultant stone formation may lead to obstruction. 10
Flank discomfort and recent history of urinary tract manipulation suggest that this is not an uncomplicated urinary tract infection; therefore, a three-day course of antibiotics is inadequate. Although flank pain and urinalysis suggest possible pyelonephritis, this patient should not be treated for simple pyelonephritis in the absence of radiography to identify a stent. A metabolic stone workup may be useful for prevention of future kidney stones, but it is not indicated in the acute setting. Finally, although computed tomography would detect a ureteral stent, it is not preferred over radiography because it exposes the patient to unnecessary radiation. Typically, microscopic hematuria requires follow-up to ensure that there is not an underlying treatable etiology. In this case , the patient's recent ureteroscopy with lithotripsy is likely the etiology.
Urinalysis in a Patient Performing Clean Intermittent Catheterization: Case 3
Case 3: urinalysis in a patient performing clean intermittent catheterization.
A 49-year-old man who has a history of neurogenic bladder due to a spinal cord injury and who performs clean intermittent catheterization visits your clinic for evaluation. He reports that he often has strong-smelling urine, but has no dysuria, urge incontinence, fever, or suprapubic pain. Results of his urinalysis with microscopy are shown in Table 5 .
A. Inform the patient that he has a urinary tract infection, obtain a urine culture, and treat with antibiotics.
B. Refer him to a urologist for evaluation of a complicated urinary tract infection.
C. Perform computed tomography of the abdomen and pelvis to evaluate for kidney or bladder stones.
D. Inform him that no treatment is needed.
E. Obtain a serum creatinine level to evaluate for chronic kidney disease.
The correct answer is D .
| Color | Dark yellow | — |
| Clarity | Turbid | — |
| pH | 7.0 | — |
| Specific gravity | 1.010 | — |
| Glucose | Negative | Negative |
| Blood | Negative | Negative |
| Ketones | Negative | Negative |
| Protein | Negative | Negative |
| Urobilinogen | Negative | Negative |
| Bilirubin | Negative | Negative |
| Leukocyte esterase | Positive | Negative |
| Nitrite | Positive | Negative |
| White blood cells | 20 per high-power field | 0 to 5 per high-power field |
| Red blood cells | 2 per high-power field | 0 to 4 per high-power field |
| Squamous epithelial cells | None | None |
| Bacteria | Many | — |
Although the urinalysis results are consistent with a urinary tract infection, the clinical history suggests asymptomatic bacteriuria. Asymptomatic bacteriuria is the isolation of bacteria in an appropriately collected urine specimen obtained from a person without symptoms of a urinary tract infection. 12 The presence of bacteria in the urine after prolonged catheterization has been well described; one study of 605 consecutive weekly urine specimens from 20 chronically catheterized patients found that 98% contained high concentrations of bacteria, and 77% were polymicrobial. 13
Similar results have been reported in patients who perform clean intermittent catheterization; another study of 1,413 urine cultures obtained from 407 patients undergoing clean intermittent catheterization found that 50.6% contained bacteria. 14 Guidelines from the Infectious Diseases Society of America recommend against treatment of asymptomatic bacteriuria in nonpregnant patients with spinal cord injury who are undergoing clean intermittent catheterization or in those using a chronic indwelling catheter. 12
In the absence of symptoms of a urinary tract infection or nephrolithiasis, there is no need to culture the urine, treat with antibiotics, refer to a urologist, or perform imaging of the abdomen and pelvis. There is no reason to suspect acute kidney injury in this setting; thus, measurement of the serum creatinine level is also unnecessary.
Data Sources : Literature searches were performed in PubMed using the terms urinalysis review, urinalysis interpretation, microscopic hematuria, CT urogram, urinary crystals, indwelling ureteral stent, asymptomatic bacteriuria, and bacteriuria with catheterization. Guidelines from the American Urological Association were also reviewed. Search dates: October 2012 and June 2013.
Wu X. Urinalysis: a review of methods and procedures. Crit Care Nurs Clin North Am. 2010;22(1):121-128.
Hardy PE. Urinalysis interpretation. Neonatal Netw. 2010;29(1):45-49.
Simerville JA, Maxted WC, Pahira JJ. Urinalysis: a comprehensive review [published correction appears in Am Fam Physician . 2006;74(7):1096]. Am Fam Physician. 2005;71(6):1153-1162.
Cohen RA, Brown RS. Clinical practice. Microscopic hematuria. N Engl J Med. 2003;348(23):2330-2338.
American Urological Association. Diagnosis, evaluation and follow-up of asymptomatic microhematuria (AMH) in adults. http://www.auanet.org/education/asymptomatic-microhematuria.cfm . Accessed June 6, 2014.
Ahmed Z, Lee J. Asymptomatic urinary abnormalities. Hematuria and proteinuria. Med Clin North Am. 1997;81(3):641-652.
Rao PK, Jones JS. How to evaluate ‘dipstick hematuria’: what to do before you refer. Cleve Clin J Med. 2008;75(3):227-233.
Choyke PL. Radiologic evaluation of hematuria: guidelines from the American College of Radiology's Appropriateness Criteria. Am Fam Physician. 2008;78(3):347-352.
Sadow CA, Wheeler SC, Kim J, Ohno-Machado L, Silverman SG. Positive predictive value of CT urography in the evaluation of upper tract urothelial cancer. AJR Am J Roentgenol. 2010;195(5):W337-W343.
Haleblian G, Kijvikai K, de la Rosette J, Preminger G. Ureteral stenting and urinary stone management: a systematic review. J Urol. 2008;179(2):424-430.
Joshi HB, Stainthorpe A, MacDonagh RP, Keeley FX, Timoney AG, Barry MJ. Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol. 2003;169(3):1065-1069.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults [published correction appears in Clin Infect Dis . 2005;40(10):1556]. Clin Infect Dis. 2005;40(5):643-654.
Warren JW, Tenney JH, Hoopes JM, Muncie HL, Anthony WC. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982;146(6):719-723.
Bakke A, Digranes A. Bacteriuria in patients treated with clean intermittent catheterization. Scand J Infect Dis. 1991;23(5):577-582.
Continue Reading
More in AFP
More in pubmed.
Copyright © 2014 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
INFECTIONS OF THE URINARY TRACT (Case Study)
Students also viewed
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Urol Assoc J
- v.7(9-10 Suppl 4); Sep-Oct 2013
Painful bladder: Case studies
As part of the program at the 3 rd Annual Canadian Urology Forum (2013), participants engaged in interactive discussions of difficult cases throughout the event. The following is a summary of discussions pertaining to two cases illustrating the difficulties in diagnosis and management of bladder pain symptoms.
An 18-year-old female with recurrent “urinary tract infection”/cystitis
The patient is an 18-year-old female, with a two-year history of “recurrent urinary tract infection” (UTI)/cystitis. She has had two positive cultures and 10 negative. Courses of antibiotics have provided some relief at times, but other times have had no effect.
She presents for an ongoing episode over the past two weeks in which she has been experiencing frequency (every 30–60 minutes during the day), a constant urge, voiding five times prior to falling asleep and waking three times each night. She experiences significant dysuria and suprapubic (SP) pain with bladder fullness. She has not experienced any episodes of incontinence. Although she describes this as a “flare,” she has had similar but slightly less intense symptoms on a daily basis for the past two years. She is accompanied at this visit by her mother, who is demanding answers about what is wrong with her daughter.
She has been sexually active for the past two years and says that she finds sexual activity uncomfortable. She is a smoker (approximately two packs per week), but has no other chronic conditions or remarkable medical history.
Physical examination finds a tender SP region and anterior vaginal wall.
Urinalysis shows 1 to 3 red blood cells and 5 to 10 white blood cells per high-power field. Culture and sensitivity are negative.
The participants at the 2013 Urology Forum made several observations and recommendations with respect to the diagnosis and management of this patient. The opinions regarding appropriate investigations and interventions at this point were varied.
Smoking cessation was deemed to be of paramount importance, and should be a major focus of patient education initiatives. It was agreed that education in general (about painful bladder syndrome, how it is treated) is a critical component of care, particularly with such a young patient.
In a situation like this, much will depend on the patient’s level of awareness and knowledge of their condition. Many patients will already have researched their condition on the Internet and have already tried conservative measures (e.g., avoiding irritants, dietary modification, exercise, stress reduction). Such patients may be ready to move on to other treatment options such as pelvic-floor physiotherapy, oral or intravesical therapy, or cystoscopy with hydrodistention (note that if the patient had not yet been sexually active, cystoscopy may be less appropriate). Other participants advocated further work-up with local cystoscopy and pelvic examination to investigate for potential causes of her pain and, if negative, to reassure the patient that the bladder is normal, at least in the anatomical aspect.
The discussion of treatment options in this session seemed to reflect the nature of the evidence available for interventions for painful bladder syndrome. There is no clear, compelling evidence that any therapy is superior to others. Among the participants, there were advocates of every different potential therapeutic approach to this patient, including hydrodistention, oral therapy, intravesical therapy or combinations of these approaches.
The possibility of an extended course of antibiotics (e.g., nitro-furantoin + pyridium for 2–3 weeks) therapy was also discussed as a means of ruling out an infectious etiology (given that her symptoms are episodic). Participants also felt that multimodality (addressing the LUTS, pain, emotional health, etc) management was recommended but is not always feasible given local resources.
A 32-year-old woman with a seven-year history of severe suprapubic pain
This patient has a seven-year history of severe suprapubic pain, with urethral burning, and urinary frequency. She describes her pain as “achy, burny and gripping.” Her daytime frequency is 14 to 18, with nocturia averaging four voids. She says she has constant urgency, hesitancy, slow flow, and experiences significant dyspareunia. Cultures have always been negative.
Before this referral, she had already been to see two different urologists and two different gynecologists. Her treatment history includes seven hydrodistentions, which have provided some benefit lasting anywhere from two weeks to three months.
She has failed courses of therapy with antimuscarinics, tricyclic antidepressants, pentosan polysulfate, intravesical lidocaine, and heparin therapy. She is currently using oxycodone as needed to manage her pain. She is highly distressed and frustrated about the inability to manage her symptoms.
Cystoscopy, which the patient has trouble tolerating due to pain, shows a small capacity (150 mL) and normal mucosa. Urodynamics show early sensation, maximum cystometric capacity of 90 mL, no detrusor overactivity, poor bladder contraction, slow flow and complete emptying.
The participants agreed that this is a very challenging case, for which there is no easy and standard answer. Prior to embarking on surgical intervention, it was agreed that all means of conservative management modalities be exhausted, in particular achieving better pain management. This patient might benefit from involvement by a pain specialist, physiotherapist and psychologist. It was, however, mentioned that there are substantial practical barriers to implementing this strategy, including access to therapists who are trained in this sub-specialty and cost.
This patient has not yet been offered a trial of sacral nerve stimulation or botulinum toxin injection. These would also be reasonable options to try at this point. Bladder augmentation is not advised given the significant vaginal and urethral pain, and potential self-catheterization may not be successful for that reason. Urinary diversion would be the absolute last option and is not recommended at this point in time.
Competing interests: This article is part of a CUAJ supplement sponsored by Astellas Pharma Canada, Inc. Dr. Bailly has received speaker fees, educational grants, and/or travel assistance from Allergan, Astellas, Eli Lilly, and Pfizer.

An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- U.S. Department of Health & Human Services

Call the OWH HELPLINE: 1-800-994-9662 9 a.m. — 6 p.m. ET, Monday — Friday OWH and the OWH helpline do not see patients and are unable to: diagnose your medical condition; provide treatment; prescribe medication; or refer you to specialists. The OWH helpline is a resource line. The OWH helpline does not provide medical advice.
Please call 911 or go to the nearest emergency room if you are experiencing a medical emergency.
Urinary tract infections

Urinary tract infections (UTIs) are most often caused by bacteria (germs) that get into the bladder, which is part of the urinary tract. UTIs are also called bladder infections. UTIs are common, especially in women. More than half of women will have at least one UTI at some point in life. 1 UTIs are serious and often painful. But most UTIs are easy to treat with antibiotics.
What is a urinary tract infection (UTI)?
UTIs can happen anywhere in the urinary system (which includes the kidneys, ureters, bladder, and urethra). UTIs are most common in the bladder. A UTI in the bladder is called cystitis. Infections in the bladder can spread to the upper part of the urinary tract or the kidneys. A UTI in the kidneys is called pyelonephritis or "pyelo."
Who gets UTIs?
Women get UTIs up to 30 times more often than men do. 2 Also, as many as 4 in 10 women who get a UTI will get at least one more within six months. 3
Women get UTIs more often because a woman's urethra (the tube from the bladder to where the urine comes out of the body) is shorter than a man's. This makes it easier for bacteria to get into the bladder. A woman's urethral opening is also closer to both the vagina and the anus , the main source of germs such as Escherichia coli ( E. coli ) that cause UTIs. 4
Are some women more at risk for UTIs?
Yes. You may be at greater risk for a UTI if you: 1 , 5
- Are sexually active. Sexual activity can move germs that cause UTIs from other areas, such as the vagina, to the urethra.
- Use a diaphragm for birth control or use spermicides (creams that kill sperm) with a diaphragm or with condoms. Spermicides can kill good bacteria that protect you from UTIs.
- Are pregnant. Pregnancy hormones can change the bacteria in the urinary tract, making UTIs more likely. Also, many pregnant women have trouble completely emptying the bladder, because the uterus (womb) with the developing baby sits on top of the bladder during pregnancy. Leftover urine with bacteria in it can cause a UTI.
- Have gone through menopause . After menopause, loss of the hormone estrogen causes vaginal tissue to become thin and dry. This can make it easier for harmful bacteria to grow and cause a UTI.
- Have diabetes, which can lower your immune (defense) system and cause nerve damage that makes it hard to completely empty your bladder
- Have any condition, like a kidney stone, that may block the flow of urine between your kidneys and bladder
- Have or recently had a catheter in place. A catheter is a thin tube put through the urethra into the bladder. Catheters drain urine when you cannot pass urine on your own, such as during surgery.
What are the symptoms of a UTI?
If you have a UTI, you may have some or all of these symptoms: 6 , 7
- Pain or burning when urinating
- An urge to urinate often, but not much comes out when you go
- Pressure in your lower abdomen
- Urine that smells bad or looks milky or cloudy
- Blood in the urine. This is more common in younger women. If you see blood in your urine, tell a doctor or nurse right away.
- Feeling tired, shaky, confused, or weak. This is more common in older women.
- Having a fever, which may mean the infection has reached your kidneys
What causes UTIs?
UTIs are caused by bacteria or, rarely, yeast getting into your urinary tract. Once there, they multiply and cause inflammation (swelling) and pain. You can help prevent UTIs by wiping from front to back after using the bathroom. Learn other ways to help prevent UTIs.
How is a UTI diagnosed?
To find out whether you have a UTI, your doctor or nurse will test a clean sample of your urine. This means you will first wipe your genital area with a special wipe. Then you will collect your urine in midstream in a cup. Your doctor or nurse may then test your urine for bacteria to see whether you have a UTI, which can take a few days.
If you have had a UTI before, your doctor may order more tests to rule out other problems. These tests may include:
- A cystogram. This is a special type of x-ray of your urinary tract. These x-rays can show any problems, including swelling or kidney stones.
- A cystoscopic exam. The cystoscope is a small tube the doctor puts into the urethra to see inside of the urethra and bladder for any problems.
How is a UTI treated?
UTIs are treated with antibiotics prescribed by your doctor. You may feel better in one or two days. Make sure to finish taking all of the antibiotics as prescribed, even if you feel better after a day or two.
What can happen if a UTI is not treated?
If treated right away, a UTI is not likely to damage your urinary tract. But if your UTI is not treated, the infection can spread to the kidneys and other parts of your body. The most common symptoms of kidney infection are fever and pain in the back where the kidneys are located. Antibiotics can also treat kidney infections.
Sometimes the infection can get in the bloodstream. This is rare but life-threatening.
How do UTIs affect pregnancy?
Changes in hormone levels during pregnancy raise your risk for UTIs. UTIs during pregnancy are more likely to spread to the kidneys.
If you're pregnant and have symptoms of a UTI, see your doctor or nurse right away. Your doctor will give you an antibiotic that is safe to take during pregnancy.
If left untreated, UTIs could lead to kidney infections and problems during pregnancy, including:
- Premature birth (birth of the baby before 39 to 40 weeks)
- Low birth weight (smaller than 5 1/2 pounds at birth)
- High blood pressure, which can lead to a more serious condition called preeclampsia 8
How can I prevent UTIs?
You can take steps to help prevent a UTI. But you may follow these steps and still get a UTI.
- Urinate when you need to. Don't go without urinating for longer than three or four hours. The longer urine stays in the bladder, the more time bacteria have to grow.
- Try to urinate before and after sex.
- Always wipe from front to back.
- Try to drink six to eight glasses of fluid per day.
- Clean the anus and the outer lips of your genitals each day.
- Do not douche or use feminine hygiene sprays.
- If you get a lot of UTIs and use creams that kill sperm (spermicides), talk to your doctor or nurse about using a different form of birth control instead.
- Wear underpants with a cotton crotch. Avoid tight-fitting pants, which trap moisture, and change out of wet bathing suits and workout clothes quickly.
- Take showers, or limit baths to 30 minutes or less.
Can cranberry juice help prevent UTIs?
Maybe. Studies on whether cranberry juice or products prevent or treat UTIs show mixed results.
Cranberries may help prevent bacteria from attaching to cells in the wall of the urinary tract and causing infection. If you get recurrent UTIs, talk to your doctor or nurse about taking cranberry products to prevent UTIs.
What should I do if I keep getting UTIs?
Women who get two UTIs in six months or three in a year have recurrent UTIs. 3 Your doctor or nurse might do tests to find out why. If the test results are normal, you may need to take a small dose of antibiotics every day to prevent infection. Your doctor may also give you a supply of antibiotics to take after sex or at the first sign of infection. 9
Did we answer your question about UTIs?
For more information about UTIs, call the OWH Helpline at 1-800-994-9662 or contact the following organizations:
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), NIH, HHS Phone Number: 1-800-891-5390
- American College of Obstetricians and Gynecologists (ACOG) Phone Number: 1-800-673-8444
- American Urogynecologic Society Phone Number: 301-273-0570
- National Kidney Foundation Phone Number: 1-800-622-9010
- Bergamin, P.A., Kiosoglous, A.J. (2017). Non-surgical management of recurrent urinary tract infections in women. Translational Andrology and Urology; 6(Suppl 2): S142-S152.
- Foxman, B. (2002). Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. American Journal of Medicine; 113(Suppl. 1A): 5S-13S.
- Arnold, J.J., Hehn, L.E., Klein, D.A. (2016). Common questions about recurrent urinary tract infections in women. American Family Physician; 93(7): 560-569.
- Najar, M.S., Saldanha, C.L., Banday, K.A. (2009). Approach to urinary tract infections. Indian Journal of Nephrology; 19(4): 129-139.
- Minardi, D., d'Anzeo, G., Cantoro, D., Conti, A., Muzzonigro, G. (2011). Urinary tract infections in women: etiology and treatment options. International Journal of General Medicine; 4: 333-343.
- National Institute of Diabetes and Digestive and Kidney Diseases. (2017). What are the symptoms of a bladder infection?
- Pallett, A., Hand, K. (2010). Complicated urinary tract infections: practical solutions for the treatment of multiresistant Gram-negative bacteria. Journal of Antimicrobial Chemotherapy; 65(Suppl. 3): iii25-iii33.
- Karmon, A., Sheiner, E. (2008). The relationship between urinary tract infection during pregnancy and preeclampsia: causal, confounded or spurious? Archives of Gynecology and Obstetrics; 277(6): 479-481.
- Dason, S., Dason, J.T., Kapoor, A. (2011). Guidelines for the diagnosis and management of recurrent urinary tract infection in women. Canadian Urological Association Journal; 5(5): 316-322.
- Tamara G. Bavendam, M.D., M.S., Senior Scientific Officer and Program Director, Division of Kidney, Urologic, and Hematologic Diseases, National Institute of Diabetes and Digestive and Kidney Diseases
- Andrew Hundley, M.D., Division Director of the Female Pelvic Medicine and Reconstructive Surgery Division of the Department of Obstetrics and Gynecology at The Ohio State University Wexner Medical Center
- HHS Non-Discrimination Notice
- Language Assistance Available
- Accessibility
- Privacy Policy
- Disclaimers
- Freedom of Information Act (FOIA)
- Use Our Content
- Vulnerability Disclosure Policy
- Kreyòl Ayisyen
A federal government website managed by the Office on Women's Health in the Office of the Assistant Secretary for Health at the U.S. Department of Health and Human Services.
1101 Wootton Pkwy, Rockville, MD 20852 1-800-994-9662 • Monday through Friday, 9 a.m. to 6 p.m. ET (closed on federal holidays).


An official website of the United States government
Here's how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
What Is Menopause?
On this page:
Understanding the menopausal transition
Is it menopause, what are the signs and symptoms of menopause, treating menopause symptoms: what's right for me.
Larissa is experiencing the menopausal transition, a normal part of aging for women. Menopause is not a disease or disorder. This time in a woman's life is often full of other transitions in addition to physical ones: Women may be caring for aging parents or relatives, supporting their children as they move into adulthood, or taking on new responsibilities at work.

Some women don't have any trouble with menopausal symptoms and may even feel relieved when they no longer need to worry about painful periods or getting pregnant. For other women, the menopausal transition can bring hot flashes , trouble sleeping , pain during sex , moodiness and irritability, depression , or a combination of these symptoms. Some may decide to talk with their doctor about lifestyle changes or medications to treat their symptoms.
Menopause is a point in time 12 months after a woman's last period. The years leading up to that point, when women may have changes in their monthly cycles, hot flashes, or other symptoms, are called the menopausal transition or perimenopause.
The menopausal transition most often begins between ages 45 and 55. It usually lasts about seven years but can be as long as 14 years. The duration can depend on lifestyle factors such as smoking, age it begins, and race and ethnicity. During perimenopause, the body's production of estrogen and progesterone, two hormones made by the ovaries, varies greatly.
The menopausal transition affects each woman uniquely and in various ways. The body begins to use energy differently, fat cells change, and women may gain weight more easily. You may experience changes in your bone or heart health, your body shape and composition, or your physical function.
If you are having symptoms that are common during menopause, your doctor may ask questions about your age, symptoms, and family history to determine if it really is the menopausal transition causing your problems. In some cases, your doctor may suggest a blood test to check your follicle-stimulating hormone (FSH) and estradiol (E2) levels to rule out any other causes for the changes you're experiencing.
While the menopausal transition may commonly be referred to as "menopause," true menopause doesn't happen until one year after a woman’s final menstrual period. For that reason, a woman who does not want to get pregnant should continue to use birth control for at least a full 12 months after her last period.
Menopause can also be triggered by a hysterectomy or surgical removal of the ovaries, which produce hormones. If you have surgery to remove your uterus or ovaries and are not taking hormones, you will experience symptoms of menopause immediately.
After menopause, women enter postmenopause. Postmenopausal women are more vulnerable to heart disease and osteoporosis . During this time, it is important to continue to eat a healthy diet , be active , and make sure you get enough calcium for optimal bone health.

Estrogen is used by many parts of a woman’s body. As levels of estrogen decrease, you could have various symptoms. Many women experience mild symptoms that can be treated by lifestyle changes such as avoiding caffeine or carrying a portable fan. Some women don’t require any treatment at all, but for others, symptoms can be more severe. The severity of symptoms varies greatly around the world and by race and ethnicity.
Here are the most common changes you might notice at midlife. Some may be part of aging rather than directly related to menopause.
Change in your period. This might be what you notice first. Your periods may no longer be regular. They may be shorter or last longer. You might bleed more or less than usual. These are all normal changes, but to make sure there isn’t a problem, see your doctor if:
- Your periods happen very close together.
- You have heavy bleeding.
- You have spotting.
- Your periods last more than a week.
- Your periods resume after no bleeding for more than a year.
Hot flashes. Many women have hot flashes, which can last for many years after menopause. They may be related to changing estrogen levels. A hot flash is a sudden feeling of heat in the upper part or all of your body. Your face and neck may become flushed. Red blotches may appear on your chest, back, and arms. Heavy sweating and cold shivering can follow. Hot flashes can be very mild or strong enough to wake you up (called night sweats). Most hot flashes last between 30 seconds and 10 minutes. They can happen several times an hour, a few times a day, or just once or twice a week. Find information on managing hot flashes in Hot Flashes: What Can I Do?
Bladder control. A loss of bladder control is called incontinence . You may have a sudden urge to urinate, or urine may leak during exercise, sneezing, or laughing. The first step in treating incontinence is to see a doctor. Bladder infections also can occur in midlife.
Sleep. Around midlife, some women start having trouble getting a good night’s sleep . Maybe you can’t fall asleep easily, or you wake too early. Night sweats might wake you up. And if you wake up during the night, you might have trouble falling back to sleep. Learn how to improve your sleep during the menopausal transition and beyond in Sleep Problems and Menopause: What Can I Do?
Vaginal health and sexuality. After menopause, the vagina may become drier, which can make sexual intercourse uncomfortable. Read about options for addressing vaginal pain during sex in Sex and Menopause: Treatment for Symptoms . You may also find that your feelings about sex are changing. You could be less interested, or you could feel freer and sexier because after one full year without a period, you can no longer become pregnant. However, you could still be at risk for sexually transmitted diseases (STDs), such as gonorrhea or HIV/AIDS . Your risk for an STD increases if you have sex with more than one person or with someone who has sex with others. If so, make sure your partner uses a condom each time you have sex.
Mood changes. You might feel moodier or more irritable around the time of menopause. Scientists don’t know why this happens. It’s possible that stress, family changes such as growing children or aging parents, a history of depression , or feeling tired could be causing these mood changes. Talk with your primary care provider or a mental health professional about what you’re experiencing. There are treatments available to help.
Your body seems different. Your waist could get larger. You could lose muscle and gain fat. Your skin could become thinner. You might have memory problems , and your joints and muscles could feel stiff and achy. Researchers are exploring such changes and how they relate to hormones and growing older.
In addition, for some women, symptoms may include aches and pains , headaches, and heart palpitations. Follow up with a doctor. Because menopausal symptoms may be caused by changing hormone levels, it is unpredictable how often women will experience symptoms and how severe they will be.
My Menoplan Tool
My Menoplan is an evidence-based online resource developed by NIA-funded researchers to help people learn about the symptoms and treatments of menopause and create a personalized plan. Learn more on the My Menoplan website.
Deciding whether and how to treat the symptoms of menopausal transition can be complicated and personal. Discuss your symptoms, family and medical history, and preferences with your doctor. No matter what you decide, see your doctor every year to talk about your treatment plan and discuss any changes you want to make.
Learn about options to help you manage hot flashes , sleep problems , and sex problems during the menopausal transition.
You may also be interested in
- Viewing an infographic on staying healthy during and after menopause
- Reading about sexuality and intimacy in older adults
- Learning about osteoporosis
Sign up for email updates on healthy aging
For more information on menopause.
Office on Women's Health Department of Health and Human Services 800-994-9662 www.womenshealth.gov
American College of Obstetricians and Gynecologists 800-673-8444 [email protected] www.acog.org
North American Menopause Society 440-442-7550 [email protected] www.menopause.org
This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
Content reviewed: September 30, 2021
nia.nih.gov
An official website of the National Institutes of Health
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Urinary Tract Infection Case Study
- Jordan Bittengle
- Kellie Berry
- Kristina Hickman
- Leslie Starkey
Our rationale for choosing this condition:
We chose urinary tract infection as our case study because we all have experience taking care of patients that have had urinary tract infections. Our group thought this was a good topic because we know that moving forward in our careers, we will take part in treating patients with urinary tract infections no matter what setting we work in.
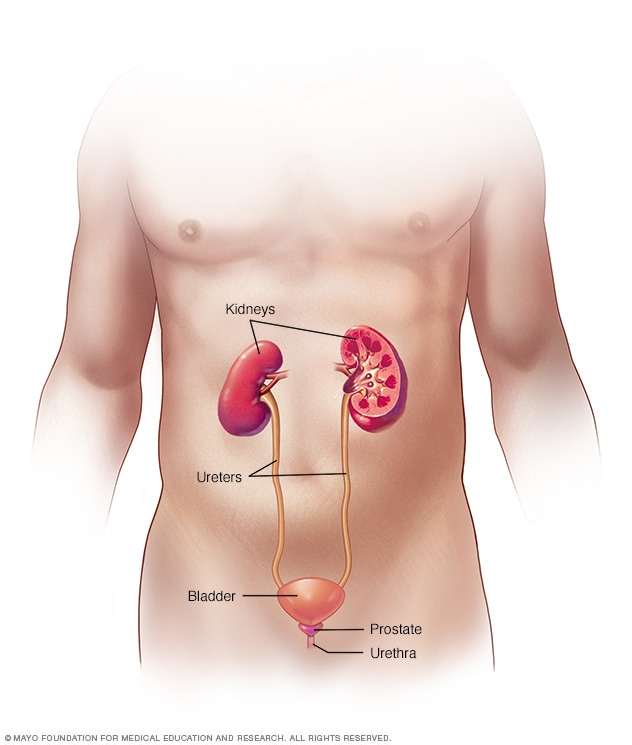
https://www.mayoclinic.org/diseases-conditions/urinary-tract-infection/symptoms-causes/syc-20353447

IMAGES
VIDEO
COMMENTS
Patient Presentation. Ms. Smith is a 27-year-old woman who presents to her PCP after just finishing a course of antibiotics for an upper respiratory infection with complaints of dysuria and foul-smelling urine. She also complains of frequency to void, but only able to get out a few drops at a time. She has had 4/10 abdominal discomfort for the ...
Urinary tract infection (UTI) is the most common bacterial infection encountered in the ambulatory care setting in the United States, accounting for 8.6 million visits (84% by women) in 2007. 1 Acute cystitis is more common than acute pyelonephritis, with an estimated ratio of 28 cases of cystitis to 1 case of pyelonephritis. 2
Urinary tract infections are due to the colonization of the urinary tract by microbes. Certain populations are at higher risk of infections of the urinary tract. Women are among those most affected by UTIs, with a lifetime incidence rate of almost 50%. 3 The difference between the sexes is attributed to women's shorter urethral length. Women ...
Target Audience and Goal Statement. This activity is intended for infectious disease specialists, urologists, primary care physicians, pharmacists, and other healthcare providers involved in the management of recurrent complicated urinary tract infections (UTIs). The goal of this activity is to improve clinicians' ability to evaluate the role ...
Recent large, international studies of the in vitro susceptibility of E. coli strains that cause uncomplicated urinary tract infection 28 have revealed rates of resistance to amoxicillin of 20% or ...
Introduction. Urinary tract infection (UTI) is one of the most common indications for which antimicrobials are initiated. 1-3 UTIs cause symptoms that are often distressing for patients and can lead to serious complications. They are also often overscreened by means of obtaining urine cultures when not clinically indicated and, especially in the case of asymptomatic bacteriuria (ASB ...
Urinary tract infections (UTIs) are among the most common bacterial infections worldwide, occurring in both community and healthcare settings. Although the clinical symptoms of UTIs are heterogeneous and range from uncomplicated (uUTIs) to complicated (cUTIs), most UTIs are usually treated empirically. Bacteria are the main causative agents of ...
Dysuria, urinary urgency and frequency, bladder fullness/discomfort. Hemorrhagic cystitis (bloody urine) reported in as many as 10% of cases of UTI in otherwise healthy women. Pyelonephritis (upper UTI) in the adult: Fever, sweating. Nausea, vomiting, flank pain, dysuria. Signs and symptoms of dehydration, hypotension.
Abstract. This article will discuss and reflect on a case study involving the prescribing of nitrofurantoin, by a non-medical prescriber, for a suspected symptomatic uncomplicated urinary tract infection in a patient living in a care home. The focus will be around the consultation and decision-making process of prescribing and the difficulties ...
From the microbiologist's point of view, a urinary tract infection (UTI) is defined as the presence of bacteria in an individual with symptoms related to the urinary tract [].A correct approach to UTI starts from a correct microbiological diagnosis [].International guidelines suggest basing antimicrobial therapy on antibiograms [].The only clinical situation where an empirical approach is ...
Differential Diagnosis for UTI. Rationale: Mrs. Smith's presentation of symptoms such as abdominal pain, back pain, urinary frequency with little urine being made, dysuria, and foul-smelling urine provide rationale that this could be a Urinary Tract Infection. A UTI is an infection of the urinary tract infection that can happen when bacteria ...
Types of Urinary Tract Infection: Urinary tract infections are caused by bacterium that invade the urinary epithelium cells causing irritation and inflammation of these cells. The infection can start in the urethra and can progress its way up to the bladder, ureters, or kidney. Infection of the urethra or bladder is known as a lower urinary ...
Tests and procedures used to diagnose urinary tract infections include: Analyzing a urine sample. Your health care provider may ask for a urine sample. The urine will be looked at in a lab to check for white blood cells, red blood cells or bacteria. You may be told to first wipe your genital area with an antiseptic pad and to collect the urine ...
Keith RN Case study urinary tract primary concept infection interrelated concepts (in order of emphasis) perfusion fluid and electrolyte balance ... Case Study Urinary Tract Infection/Urosepsis; Respiratory Syncytial Virus (RSV) Bronchiolitis; 9 HIV Case Study; ... Glucose 184 Bun 35 Creatinine 1. NA, K WNL
View Case Study 35 Urinary Tract Infection.odt from NURSING 420 at West Coast University. Daniel Alvarez 06/03/2020 Case Study 35 Urinary Tract Infection Patient Case Question 1. List a minimum of
UTI is defined as a kidney infection that can lead to systemic symptoms such as fever and weakness and can cause discomfort and difficulty with daily activities [ 1 ]. UTI ranges in severity from mild self-limitation to severe sepsis, with a mortality rate of 20-40% [ 1 ]. Specifically, in this case we will discuss a common UTI in an elderly ...
View Case Study 35.docx from NUR MISC at American Career College, Long Beach. Peter Canepa Park Ave clinical Ms. Shertick March 18, 2020 Case Study # 35 1. ... View Urinary Tract Infection case study.docx from LVN 191104-3 at American Career Colle... UTI DB.docx. California State University, East Bay. NURS 316. urinary tract infection. UTI.
View Urinary Tract Infection case study.docx from LVN 191104-3 at American Career College, Ontario. Case Study 35 - Urinary Tract Infection Patient case questions: 1. List a minimum of 8 appropriate
A UTI is a bacterial infection that affects the urinary tract. Most are caused by Escherichia coli ( E. coli ), although other bacteria are sometimes responsible. UTIs occur when bacteria enter the urinary tract through the urethra, the thin tube that runs from your bladder to the opening where urine exits your body.
In a patient with a ureteral stent, urinalysis alone cannot establish the diagnosis of urinary tract infection. Plain radiography of the kidneys, ureters, and bladder can identify a stent and is ...
Creators: Our rationale for choosing this condition: We chose urinary tract infection as our case study because we all have experience taking care of patients that have had urinary tract infections. Our group thought this was a good topic because we know that moving forward in our careers, we will take part in treating patients with urinary ...
An uncomplicated urinary tract infection (UTI) is a bacterial infection of the bladder and associated structures. Patients with uncomplicated UTIs have no structural abnormality of the urinary tract and no comorbidities such as diabetes, an immunocompromised state, recent urologic surgery, or pregnancy. An uncomplicated UTI is also known as cystitis or a lower tract UTI.
Fever, chills, flank pains, and positive kidney punch are suggestive of: - Pyelonephritis. What is the correct about urinary tract infections? - Infections are always the result of trauma to the urinary tract. Case: A 28-year-old housewife consulted a physician because of scanty urine, increased frequency of urination and burning sensation at ...
Acute dysuria or pain, swelling, or tenderness of testes, epididymis, or prostate. Fever or leukocytosis and ≥1 of the following: • Acute costovertebral angle pain or tenderness. • Suprapubic pain. • Gross hematuria. • New or marked increase in incontinence. • New or marked increase in urgency. • New or marked increase in frequency.
Urinary Tract Infection Case Study 35 Summary-An infection in any part of the urinary system, the kidneys, bladder, or urethra. Urinary tract infections are more common in women. They usually occur in the bladder or urethra, but more serious infections involve the kidney. A bladder infection may cause pelvic pain, increased urge to urinate, pain with urination, and blood in the urine.
Diagnostic tests; On 30-11-2017 Test for (MP antigen) : negative Widal = negative Urine Microscopic examination- 30-11-17 Pus cells- 6-10cells/hpf (occasional clumf) Epithelial cells- 2-3/hpf. 14. 15. Based on the reports of routine urine examination and microscopy, the present case was diagnosed as that of Urinary tract infection on 31/05/13.
An 18-year-old female with recurrent "urinary tract infection"/cystitis. The patient is an 18-year-old female, with a two-year history of "recurrent urinary tract infection" (UTI)/cystitis. She has had two positive cultures and 10 negative. Courses of antibiotics have provided some relief at times, but other times have had no effect.
Urinary tract infections (UTIs) are most often caused by bacteria (germs) that get into the bladder, which is part of the urinary tract. UTIs are also called bladder infections. UTIs are common, especially in women. More than half of women will have at least one UTI at some point in life. 1 UTIs are serious and often painful.
Menopause is a point in time 12 months after a woman's last period. The years leading up to that point, when women may have changes in their monthly cycles, hot flashes, or other symptoms, are called the menopausal transition or perimenopause. The menopausal transition most often begins between ages 45 and 55.
Urinary Tract Infection Case Study. Creators: Our rationale for choosing this condition: We chose urinary tract infection as our case study because we all have experience taking care of patients that have had urinary tract infections. Our group thought this was a good topic because we know that moving forward in our careers, we will take part ...