Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 November 2021

A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data
- Shobhit Srivastava ORCID: orcid.org/0000-0002-7138-4916 1 ,
- Shekhar Chauhan ORCID: orcid.org/0000-0002-6926-7649 2 ,
- Ratna Patel ORCID: orcid.org/0000-0002-5371-7369 3 &
- Pradeep Kumar ORCID: orcid.org/0000-0003-4259-820X 1
Scientific Reports volume 11 , Article number: 22841 ( 2021 ) Cite this article
11k Accesses
7 Citations
11 Altmetric
Metrics details
- Health care
- Health services
- Public health
Acquired Immunodeficiency Syndrome caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. This study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with the change in awareness level on HIV-related information among adolescents over the period. Data used for this study were drawn from Understanding the lives of adolescents and young adults, a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh. The present study utilized a sample of 4421 and 7587 unmarried adolescent boys and girls, respectively aged 10–19 years in wave-1 and wave-2. Descriptive analysis and t-test and proportion test were done to observe changes in certain selected variables from wave-1 (2015–2016) to wave-2 (2018–2019). Moreover, random effect regression analysis was used to estimate the association of change in HIV awareness among unmarried adolescents with household and individual factors. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2 to 39.1% between wave-1 & wave-2. With the increase in age and years of schooling, the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV. Adolescent boys' paid work status was inversely associated with HIV awareness [Coef: − 0.01; p < 0.10]. Use of internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness with reference to their counterparts. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups, as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents.
Similar content being viewed by others

Predictors of never testing for HIV among sexually active individuals aged 15–56 years in Rwanda
Awareness and use of HIV pre-exposure prophylaxis and factors associated with awareness among MSM in Beijing, China

Identification of adolescent girls and young women for targeted HIV prevention: a new risk scoring tool in KwaZulu Natal, South Africa
Introduction.
Acquired Immunodeficiency Syndrome (AIDS) caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. So far, HIV has claimed almost 33 million lives; however, off lately, increasing access to HIV prevention, diagnosis, treatment, and care has enabled people living with HIV to lead a long and healthy life 1 . By the end of 2019, an estimated 38 million people were living with HIV 1 . More so, new infections fell by 39 percent, and HIV-related deaths fell by almost 51 percent between 2000 and 2019 1 . Despite all the positive news related to HIV, the success story is not the same everywhere; HIV varies between region, country, and population, where not everyone is able to access HIV testing and treatment and care 1 . HIV/AIDS holds back economic growth by destroying human capital by predominantly affecting adolescents and young adults 2 .
There are nearly 1.2 billion adolescents (10–19 years) worldwide, which constitute 18 percent of the world’s population, and in some countries, adolescents make up as much as one-fourth of the population 3 . In India, adolescents comprise more than one-fifth (21.8%) of the total population 4 . Despite a decline projection for the adolescent population in India 5 , there is a critical need to hold adolescents as adolescence is characterized as a period when peer victimization/pressure on psychosocial development is noteworthy 6 . Peer victimization/pressure is further linked to risky sexual behaviours among adolescents 7 , 8 . A higher proportion of low literacy in the Indian population leads to a low level of awareness of HIV/AIDS 9 . Furthermore, the awareness of HIV among adolescents is quite alarming 10 , 11 , 12 .
Unfortunately, there is a shortage of evidence on what predicts awareness of HIV among adolescents. Almost all the research in India is based on beliefs, attitudes, and awareness of HIV among adolescents 2 , 12 . However, few other studies worldwide have examined mass media as a strong predictor of HIV awareness among adolescents 13 . Mass media is an effective channel to increase an individuals’ knowledge about sexual health and improve understanding of facilities related to HIV prevention 14 , 15 . Various studies have outlined other factors associated with the increasing awareness of HIV among adolescents, including; age 16 , 17 , 18 , occupation 18 , education 16 , 17 , 18 , 19 , sex 16 , place of residence 16 , marital status 16 , and household wealth index 16 .
Several community-based studies have examined awareness of HIV among Indian adolescents 2 , 10 , 12 , 20 , 21 , 22 . However, studies investigating awareness of HIV among adolescents in a larger sample size remained elusive to date, courtesy of the unavailability of relevant data. Furthermore, no study in India had ever examined awareness of HIV among adolescents utilizing information on longitudinal data. To the author’s best knowledge, this is the first study in the Indian context with a large sample size that examines awareness of HIV among adolescents and combines information from a longitudinal survey. Therefore, this study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with a change in awareness level on HIV-related information among adolescents over the period.
Data and methods
Data used for this study were drawn from Understanding the lives of adolescents and young adults (UDAYA), a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh 23 . The first wave was conducted in 2015–2016, and the follow-up survey was conducted after three years in 2018–2019 23 . The survey provides the estimates for state and the sample of unmarried boys and girls aged 10–19 and married girls aged 15–19. The study adopted a systematic, multi-stage stratified sampling design to draw sample areas independently for rural and urban areas. 150 primary sampling units (PSUs)—villages in rural areas and census wards in urban areas—were selected in each state, using the 2011 census list of villages and wards as the sampling frame. In each primary sampling unit (PSU), households to be interviewed were selected by systematic sampling. More details about the study design and sampling procedure have been published elsewhere 23 . Written consent was obtained from the respondents in both waves. In wave 1 (2015–2016), 20,594 adolescents were interviewed using the structured questionnaire with a response rate of 92%.
Moreover, in wave 2 (2018–2019), the study interviewed the participants who were successfully interviewed in 2015–2016 and who consented to be re-interviewed 23 . Of the 20,594 eligible for the re-interview, the survey re-interviewed 4567 boys and 12,251 girls (married and unmarried). After excluding the respondents who gave an inconsistent response to age and education at the follow-up survey (3%), the final follow-up sample covered 4428 boys and 11,864 girls with the follow-up rate of 74% for boys and 81% for girls. The effective sample size for the present study was 4421 unmarried adolescent boys aged 10–19 years in wave-1 and wave-2. Additionally, 7587 unmarried adolescent girls aged 10–19 years were interviewed in wave-1 and wave-2 23 . The cases whose follow-up was lost were excluded from the sample to strongly balance the dataset and set it for longitudinal analysis using xtset command in STATA 15. The survey questionnaire is available at https://dataverse.harvard.edu/file.xhtml?fileId=4163718&version=2.0 & https://dataverse.harvard.edu/file.xhtml?fileId=4163720&version=2.0 .
Outcome variable
HIV awareness was the outcome variable for this study, which is dichotomous. The question was asked to the adolescents ‘Have you heard of HIV/AIDS?’ The response was recorded as yes and no.
Exposure variables
The predictors for this study were selected based on previous literature. These were age (10–19 years at wave 1, continuous variable), schooling (continuous), any mass media exposure (no and yes), paid work in the last 12 months (no and yes), internet use (no and yes), wealth index (poorest, poorer, middle, richer, and richest), religion (Hindu and Non-Hindu), caste (Scheduled Caste/Scheduled Tribe, Other Backward Class, and others), place of residence (urban and rural), and states (Uttar Pradesh and Bihar).
Exposure to mass media (how often they read newspapers, listened to the radio, and watched television; responses on the frequencies were: almost every day, at least once a week, at least once a month, rarely or not at all; adolescents were considered to have any exposure to mass media if they had exposure to any of these sources and as having no exposure if they responded with ‘not at all’ for all three sources of media) 24 . Household wealth index based on ownership of selected durable goods and amenities with possible scores ranging from 0 to 57; households were then divided into quintiles, with the first quintile representing households of the poorest wealth status and the fifth quintile representing households with the wealthiest status 25 .
Statistical analysis
Descriptive analysis was done to observe the characteristics of unmarried adolescent boys and girls at wave-1 (2015–2016). In addition, the changes in certain selected variables were observed from wave-1 (2015–2016) to wave-2 (2018–2019), and the significance was tested using t-test and proportion test 26 , 27 . Moreover, random effect regression analysis 28 , 29 was used to estimate the association of change in HIV awareness among unmarried adolescents with household factors and individual factors. The random effect model has a specific benefit for the present paper's analysis: its ability to estimate the effect of any variable that does not vary within clusters, which holds for household variables, e.g., wealth status, which is assumed to be constant for wave-1 and wave-2 30 .
Table 1 represents the socio-economic profile of adolescent boys and girls. The estimates are from the baseline dataset, and it was assumed that none of the household characteristics changed over time among adolescent boys and girls.
Figure 1 represents the change in HIV awareness among adolescent boys and girls. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2% in wave-1 to 39.1% in wave-2.
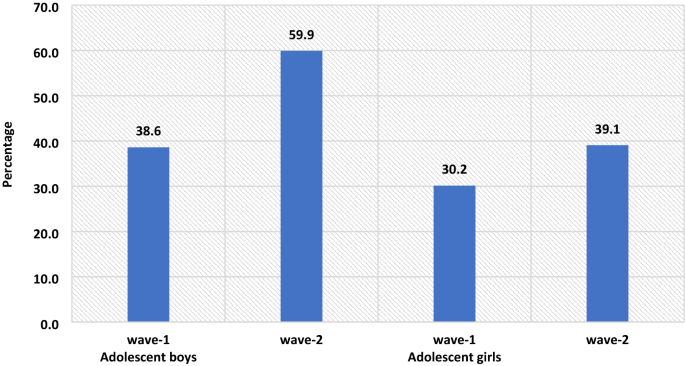
The percenate of HIV awareness among adolescent boys and girls, wave-1 (2015–2016) and wave-2 (2018–2019).
Table 2 represents the summary statistics for explanatory variables used in the analysis of UDAYA wave-1 and wave-2. The exposure to mass media is almost universal for adolescent boys, while for adolescent girls, it increases to 93% in wave-2 from 89.8% in wave-1. About 35.3% of adolescent boys were engaged in paid work during wave-1, whereas in wave-II, the share dropped to 33.5%, while in the case of adolescent girls, the estimates are almost unchanged. In wave-1, about 27.8% of adolescent boys were using the internet, while in wave-2, there is a steep increase of nearly 46.2%. Similarly, in adolescent girls, the use of the internet increased from 7.6% in wave-1 to 39.3% in wave-2.
Table 3 represents the estimates from random effects for awareness of HIV among adolescent boys and girls. It was found that with the increases in age and years of schooling the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV in comparison to those who had no exposure to mass media. Adolescent boys' paid work status was inversely associated with HIV awareness about adolescent boys who did not do paid work [Coef: − 0.01; p < 0.10]. Use of the internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness in reference to their counterparts.
The awareness regarding HIV increases with the increase in household wealth index among both adolescent boys and girls. The adolescent girls from the non-Hindu household had a lower likelihood to be aware of HIV in reference to adolescent girls from Hindu households [Coef: − 0.09; p < 0.01]. Adolescent girls from non-SC/ST households had a higher likelihood of being aware of HIV in reference to adolescent girls from other caste households [Coef: 0.04; p < 0.01]. Adolescent boys [Coef: − 0.03; p < 0.01] and girls [Coef: − 0.09; p < 0.01] from a rural place of residence had a lower likelihood to be aware about HIV in reference to those from the urban place of residence. Adolescent boys [Coef: 0.04; p < 0.01] and girls [Coef: 0.02; p < 0.01] from Bihar had a higher likelihood to be aware about HIV in reference to those from Uttar Pradesh.
This is the first study of its kind to address awareness of HIV among adolescents utilizing longitudinal data in two indian states. Our study demonstrated that the awareness of HIV has increased over the period; however, it was more prominent among adolescent boys than in adolescent girls. Overall, the knowledge on HIV was relatively low, even during wave-II. Almost three-fifths (59.9%) of the boys and two-fifths (39.1%) of the girls were aware of HIV. The prevalence of awareness on HIV among adolescents in this study was lower than almost all of the community-based studies conducted in India 10 , 11 , 22 . A study conducted in slums in Delhi has found almost similar prevalence (40% compared to 39.1% during wave-II in this study) of awareness of HIV among adolescent girls 31 . The difference in prevalence could be attributed to the difference in methodology, study population, and study area.
The study found that the awareness of HIV among adolescent boys has increased from 38.6 percent in wave-I to 59.9 percent in wave-II; similarly, only 30.2 percent of the girls had an awareness of HIV during wave-I, which had increased to 39.1 percent. Several previous studies corroborated the finding and noticed a higher prevalence of awareness on HIV among adolescent boys than in adolescent girls 16 , 32 , 33 , 34 . However, a study conducted in a different setting noticed a higher awareness among girls than in boys 35 . Also, a study in the Indian context failed to notice any statistical differences in HIV knowledge between boys and girls 18 . Gender seems to be one of the significant determinants of comprehensive knowledge of HIV among adolescents. There is a wide gap in educational attainment among male and female adolescents, which could be attributed to lower awareness of HIV among girls in this study. Higher peer victimization among adolescent boys could be another reason for higher awareness of HIV among them 36 . Also, cultural double standards placed on males and females that encourage males to discuss HIV/AIDS and related sexual matters more openly and discourage or even restrict females from discussing sexual-related issues could be another pertinent factor of higher awareness among male adolescents 33 . Behavioural interventions among girls could be an effective way to improving knowledge HIV related information, as seen in previous study 37 . Furthermore, strengthening school-community accountability for girls' education would augment school retention among girls and deliver HIV awareness to girls 38 .
Similar to other studies 2 , 10 , 17 , 18 , 39 , 40 , 41 , age was another significant determinant observed in this study. Increasing age could be attributed to higher education which could explain better awareness with increasing age. As in other studies 18 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , education was noted as a significant driver of awareness of HIV among adolescents in this study. Higher education might be associated with increased probability of mass media and internet exposure leading to higher awareness of HIV among adolescents. A study noted that school is one of the important factors in raising the awareness of HIV among adolescents, which could be linked to higher awareness among those with higher education 47 , 48 . Also, schooling provides adolescents an opportunity to improve their social capital, leading to increased awareness of HIV.
Following previous studies 18 , 40 , 46 , the current study also outlines a higher awareness among urban adolescents than their rural counterparts. One plausible reason for lower awareness among adolescents in rural areas could be limited access to HIV prevention information 16 . Moreover, rural–urban differences in awareness of HIV could also be due to differences in schooling, exposure to mass media, and wealth 44 , 45 . The household's wealth status was also noted as a significant predictor of awareness of HIV among adolescents. Corroborating with previous findings 16 , 33 , 42 , 49 , this study reported a higher awareness among adolescents from richer households than their counterparts from poor households. This could be because wealthier families can afford mass-media items like televisions and radios for their children, which, in turn, improves awareness of HIV among adolescents 33 .
Exposure to mass media and internet access were also significant predictors of higher awareness of HIV among adolescents. This finding agrees with several previous research, and almost all the research found a positive relationship between mass-media exposure and awareness of HIV among adolescents 10 . Mass media addresses such topics more openly and in a way that could attract adolescents’ attention is the plausible reason for higher awareness of HIV among those having access to mass media and the internet 33 . Improving mass media and internet usage, specifically among rural and uneducated masses, would bring required changes. Integrating sexual education into school curricula would be an important means of imparting awareness on HIV among adolescents; however, this is debatable as to which standard to include the required sexual education in the Indian schooling system. Glick (2009) thinks that the syllabus on sexual education might be included during secondary schooling 44 . Another study in the Indian context confirms the need for sex education for adolescents 50 , 51 .
Limitations and strengths of the study
The study has several limitations. At first, the awareness of HIV was measured with one question only. Given that no study has examined awareness of HIV among adolescents using longitudinal data, this limitation is not a concern. Second, the study findings cannot be generalized to the whole Indian population as the study was conducted in only two states of India. However, the two states selected in this study (Uttar Pradesh and Bihar) constitute almost one-fourth of India’s total population. Thirdly, the estimates were provided separately for boys and girls and could not be presented combined. However, the data is designed to provide estimates separately for girls and boys. The data had information on unmarried boys and girls and married girls; however, data did not collect information on married boys. Fourthly, the study estimates might have been affected by the recall bias. Since HIV is a sensitive topic, the possibility of respondents modifying their responses could not be ruled out. Hawthorne effect, respondents, modifying aspect of their behaviour in response, has a role to play in HIV related study 52 . Despite several limitations, the study has specific strengths too. This is the first study examining awareness of HIV among adolescent boys and girls utilizing longitudinal data. The study was conducted with a large sample size as several previous studies were conducted in a community setting with a minimal sample size 10 , 12 , 18 , 20 , 53 .
The study noted a higher awareness among adolescent boys than in adolescent girls. Specific predictors of high awareness were also noted in the study, including; higher age, higher education, exposure to mass media, internet use, household wealth, and urban residence. Based on the study findings, this study has specific suggestions to improve awareness of HIV among adolescents. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents. Investment in education will help, but it would be a long-term solution; therefore, public information campaigns could be more useful in the short term.
WHO. HIV/AIDS . https://www.who.int/news-room/fact-sheets/detail/hiv-aids (2020).
Singh, A. & Jain, S. Awareness of HIV/AIDS among school adolescents in Banaskantha district of Gujarat. Health Popul.: Perspect. Issues 32 , 59–65 (2009).
Google Scholar
WHO & UNICEF. adolescents Health: The Missing Population in Universal Health Coverage . 1–31 https://www.google.com/search?q=adolescents+population+WHO+report&rlz=1C1CHBF_enIN904IN904&oq=adolescents+population+WHO+report&aqs=chrome..69i57.7888j1j7&sourceid=chrome&ie=UTF-8 (2018).
Chauhan, S. & Arokiasamy, P. India’s demographic dividend: state-wise perspective. J. Soc. Econ. Dev. 20 , 1–23 (2018).
Tiwari, A. K., Singh, B. P. & Patel, V. Population projection of India: an application of dynamic demographic projection model. JCR 7 , 547–555 (2020).
Troop-Gordon, W. Peer victimization in adolescence: the nature, progression, and consequences of being bullied within a developmental context. J. Adolesc. 55 , 116–128 (2017).
PubMed Google Scholar
Dermody, S. S., Friedman, M., Chisolm, D. J., Burton, C. M. & Marshal, M. P. Elevated risky sexual behaviors among sexual minority girls: indirect risk pathways through peer victimization and heavy drinking. J. Interpers. Violence 35 , 2236–2253 (2020).
Lee, R. L. T., Loke, A. Y., Hung, T. T. M. & Sobel, H. A systematic review on identifying risk factors associated with early sexual debut and coerced sex among adolescents and young people in communities. J. Clin. Nurs. 27 , 478–501 (2018).
Gurram, S. & Bollampalli, B. A study on awareness of human immunodeficiency virus among adolescent girls in urban and rural field practice areas of Osmania Medical College, Hyderabad, Telangana, India. (2020).
Jain, R., Anand, P., Dhyani, A. & Bansal, D. Knowledge and awareness regarding menstruation and HIV/AIDS among schoolgoing adolescent girls. J. Fam. Med. Prim Care 6 , 47–51 (2017).
Kawale, S., Sharma, V., Thaware, P. & Mohankar, A. A study to assess awareness about HIV/AIDS among rural population of central India. Int. J. Commun. Med. Public Health 5 , 373–376 (2017).
Lal, P., Nath, A., Badhan, S. & Ingle, G. K. A study of awareness about HIV/AIDS among senior secondary school Children of Delhi. Indian J. Commun. Med. 33 , 190–192 (2008).
CAS Google Scholar
Bago, J.-L. & Lompo, M. L. Exploring the linkage between exposure to mass media and HIV awareness among adolescents in Uganda. Sex. Reprod. Healthcare 21 , 1–8 (2019).
McCombie, S., Hornik, R. C. & Anarfi, J. K. Effects of a mass media campaign to prevent AIDS among young people in Ghana . Public Health Commun. 163–178 (Routledge, 2002). https://doi.org/10.4324/9781410603029-17 .
Sano, Y. et al. Exploring the linkage between exposure to mass media and HIV testing among married women and men in Ghana. AIDS Care 28 , 684–688 (2016).
Oginni, A. B., Adebajo, S. B. & Ahonsi, B. A. Trends and determinants of comprehensive knowledge of HIV among adolescents and young adults in Nigeria: 2003–2013. Afr. J. Reprod. Health 21 , 26–34 (2017).
Rahman, M. M., Kabir, M. & Shahidullah, M. Adolescent knowledge and awareness about AIDS/HIV and factors affecting them in Bangladesh. J. Ayub. Med. Coll. Abbottabad 21 , 3–6 (2009).
Yadav, S. B., Makwana, N. R., Vadera, B. N., Dhaduk, K. M. & Gandha, K. M. Awareness of HIV/AIDS among rural youth in India: a community based cross-sectional study. J. Infect. Dev. Countries 5 , 711–716 (2011).
Alhasawi, A. et al. Assessing HIV/AIDS knowledge, awareness, and attitudes among senior high school students in Kuwait. MPP 28 , 470–476 (2019).
Chakrovarty, A. et al. A study of awareness on HIV/AIDS among higher secondary school students in Central Kolkata. Indian J. Commun. Med. 32 , 228 (2007).
Katoch, D. K. S. & Kumar, A. HIV/AIDS awareness among students of tribal and non-tribal area of Himachal Pradesh. J. Educ. 5 , 1–9 (2017).
Shinde, M., Trivedi, A., Shinde, A. & Mishra, S. A study of awareness regarding HIV/AIDS among secondary school students. Int. J. Commun. Med. Public Health https://doi.org/10.18203/2394-6040.ijcmph20161611 (2016).
Article Google Scholar
Council, P. UDAYA, adolescent survey, Bihar and Uttar Pradesh, 2015–16. Harvard Dataverse https://doi.org/10.7910/DVN/RRXQNT (2018).
Kumar, P. & Dhillon, P. Household- and community-level determinants of low-risk Caesarean deliveries among women in India. J. Biosoc. Sci. 53 , 55–70 (2021).
Patel, S. K., Santhya, K. G. & Haberland, N. What shapes gender attitudes among adolescent girls and boys? Evidence from the UDAYA Longitudinal Study in India. PLoS ONE 16 , e0248766 (2021).
CAS PubMed PubMed Central Google Scholar
Fan, C., Wang, L. & Wei, L. Comparing two tests for two rates. Am. Stat. 71 , 275–281 (2017).
MathSciNet Google Scholar
Kim, T. K. T test as a parametric statistic. Korean J. Anesthesiol. 68 , 540–546 (2015).
PubMed PubMed Central Google Scholar
Bell, A., Fairbrother, M. & Jones, K. Fixed and random effects models: making an informed choice. Qual. Quant. 53 , 1051–1074 (2019).
Jarrett, R., Farewell, V. & Herzberg, A. Random effects models for complex designs. Stat. Methods Med. Res. 29 , 3695–3706 (2020).
MathSciNet CAS PubMed PubMed Central Google Scholar
Neuhaus, J. M. & Kalbfleisch, J. D. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 54 , 638–645 (1998).
CAS PubMed MATH Google Scholar
Kaur, G. Factors influencing HIV awareness amongst adolescent women: a study of slums in Delhi. Demogr. India 47 , 100–111 (2018).
Alene, G. D., Wheeler, J. G. & Grosskurth, H. Adolescent reproductive health and awareness of HIV among rural high school students, North Western Ethiopia. AIDS Care 16 , 57–68 (2004).
CAS PubMed Google Scholar
Oljira, L., Berhane, Y. & Worku, A. Assessment of comprehensive HIV/AIDS knowledge level among in-school adolescents in eastern Ethiopia. J. Int. AIDS Soc. 16 , 17349 (2013).
Samkange-Zeeb, F. N., Spallek, L. & Zeeb, H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: a systematic review of published literature. BMC Public Health 11 , 727 (2011).
Laguna, E. P. Knowledge of HIV/AIDS and unsafe sex practices among Filipino youth. in 15 (PAA, 2004).
Teitelman, A. M. et al. Partner violence, power, and gender differences in South African adolescents’ HIV/sexually transmitted infections risk behaviors. Health Psychol. 35 , 751–760 (2016).
Oberth, G. et al. Effectiveness of the Sista2Sista programme in improving HIV and other sexual and reproductive health outcomes among vulnerable adolescent girls and young women in Zimbabwe. Afr. J. AIDS Res. 20 , 158–164 (2021).
DeSoto, J. et al. Using school-based early warning systems as a social and behavioral approach for HIV prevention among adolescent girls. Preventing HIV Among Young People in Southern and Eastern Africa 280 (2020).
Ochako, R., Ulwodi, D., Njagi, P., Kimetu, S. & Onyango, A. Trends and determinants of Comprehensive HIV and AIDS knowledge among urban young women in Kenya. AIDS Res. Ther. 8 , 11 (2011).
Peltzer, K. & Supa, P. HIV/AIDS knowledge and sexual behavior among junior secondary school students in South Africa. J. Soc. Sci. 1 , 1–8 (2005).
Shweta, C., Mundkur, S. & Chaitanya, V. Knowledge and beliefs about HIV/AIDS among adolescents. WebMed Cent. 2 , 1–9 (2011).
Anwar, M., Sulaiman, S. A. S., Ahmadi, K. & Khan, T. M. Awareness of school students on sexually transmitted infections (STIs) and their sexual behavior: a cross-sectional study conducted in Pulau Pinang, Malaysia. BMC Public Health 10 , 47 (2010).
Cicciò, L. & Sera, D. Assessing the knowledge and behavior towards HIV/AIDS among youth in Northern Uganda: a cross-sectional survey. Giornale Italiano di Medicina Tropicale 15 , 29–34 (2010).
Glick, P., Randriamamonjy, J. & Sahn, D. E. Determinants of HIV knowledge and condom use among women in madagascar: an analysis using matched household and community data. Afr. Dev. Rev. 21 , 147–179 (2009).
Rahman, M. Determinants of knowledge and awareness about AIDS: Urban-rural differentials in Bangladesh. JPHE 1 , 014–021 (2009).
Siziya, S., Muula, A. S. & Rudatsikira, E. HIV and AIDS-related knowledge among women in Iraq. BMC. Res. Notes 1 , 123 (2008).
Gao, X. et al. Effectiveness of school-based education on HIV/AIDS knowledge, attitude, and behavior among secondary school students in Wuhan, China. PLoS ONE 7 , e44881 (2012).
ADS CAS PubMed PubMed Central Google Scholar
Kotecha, P. V. et al. Reproductive health awareness among urban school going adolescents in Vadodara city. Indian J. Psychiatry 54 , 344–348 (2012).
Dimbuene, T. Z. & Defo, K. B. Fostering accurate HIV/AIDS knowledge among unmarried youths in Cameroon: do family environment and peers matter?. BMC Public Health 11 , 348 (2011).
Kumar, R. et al. Knowledge attitude and perception of sex education among school going adolescents in Ambala District, Haryana, India: a cross-sectional study. J. Clin. Diagn. Res. 11 , LC01–LC04 (2017).
ADS PubMed PubMed Central Google Scholar
Tripathi, N. & Sekher, T. V. Youth in India ready for sex education? Emerging evidence from national surveys. PLoS ONE 8 , e71584 (2013).
Rosenberg, M. et al. Evidence for sample selection effect and Hawthorne effect in behavioural HIV prevention trial among young women in a rural South African community. BMJ Open 8 , e019167 (2018).
Gupta, P., Anjum, F., Bhardwaj, P., Srivastav, J. & Zaidi, Z. H. Knowledge about HIV/AIDS among secondary school students. N. Am. J. Med. Sci. 5 , 119–123 (2013).
Download references
This paper was written using data collected as part of Population Council’s UDAYA study, which is funded by the Bill and Melinda Gates Foundation and the David and Lucile Packard Foundation. No additional funds were received for the preparation of the paper.
Author information
Authors and affiliations.
Ph.D. Research Scholar, Department of Survey Research & Data Analytics, International Institute for Population Sciences, Mumbai, India
Shobhit Srivastava & Pradeep Kumar
Ph.D. Research Scholar, Department of Family and Generations, International Institute for Population Sciences, Mumbai, India
Shekhar Chauhan
Ph.D. Research Scholar, Department of Public Health and Mortality Studies, International Institute for Population Sciences, Mumbai, India
Ratna Patel
You can also search for this author in PubMed Google Scholar
Contributions
Conception and design of the study: S.S. and P.K.; analysis and/or interpretation of data: P.K. and S.S.; drafting the manuscript: S.C., and R.P.; reading and approving the manuscript: S.S., P.K., S.C. and R.P.
Corresponding author
Correspondence to Pradeep Kumar .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Srivastava, S., Chauhan, S., Patel, R. et al. A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data. Sci Rep 11 , 22841 (2021). https://doi.org/10.1038/s41598-021-02090-9
Download citation
Received : 05 June 2021
Accepted : 29 September 2021
Published : 24 November 2021
DOI : https://doi.org/10.1038/s41598-021-02090-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Advances in HIV Prevention and Treatment: A Literature Review
Joseph N. Inungu1*, Daudet Ilunga Tshiswaka2, Daryn Papenfuse1
1 School of Health Sciences, Central Michigan University, Mount Pleasant, MI, USA
2 Department of Public Health, University of West Florida, Pensacola, FL, USA
* Corresponding author: Joseph N Inungu, School of Health Sciences, Central Michigan University, Mt Pleasant, MI, USA. Tel: +1-9897744476, Fax: +19897742908; Email: [email protected]
Received Date: March 25, 2017; Accepted Date: 25 April, 2017; Published Date: 02 May, 2017
Citation: Inungu JN, Tshiswaka DI, Papenfuse D (2017) Advances in HIV Prevention and Treatment: A Literature Review. Curr Res HIV 2017: CRHA-111. DOI: 10.29011/2575-7105. 100011
Background: The last decade has witnessed several advances in the management of HIV/AIDS with the development of potent and safe antiretroviral drugs and new HIV prevention technologies.
Objective: This review summarizes the recent advances in the management of the HIV infection .
Methods: Medline via PubMed and Google search engine were searched for articles dealing with antiretroviral therapy and new prevention technologies.
Results: The understanding of the lifecycle of the HIV was a turning point that provided researchers with the knowledge and tools needed to prosecute drug discovery efforts focused on targeted inhibition with specific pharmacological agents. New prevention technologies continue to expand the current toolbox, transforming HIV/AIDS from an inevitable lethal disease into a manageable condition. The integration of behavioral, biomedical and structural interventions will likely reduce the incidence of HIV while promising new leads for an effective HIV vaccine keep the hope of a world free of HIV alive.
Conclusion: Although the fight against HIV has been long and arduous, many signs seem to suggest that ending HIV epidemic is not only possible; it is well in our reach.
Keywords: Antiretroviral Therapy; HIV/AIDS; HIV Prevention Technology;Lifecycle
Introduction
Three decades following the report about a cluster of Kaposi’s sarcoma and Pneumocystis pneumonia among homosexual men in Los Angeles and New York, [1] HIV/AIDS remains a global public health challenge. Approximately 36.7 million people were living with HIV/AIDS (PLH) worldwide at the end of 2015. An estimated 2.1 million people became newly infected with HIV and 1.1 million died from AIDS-related illnesses during the same year. The vast majority of people living with HIV are in low and middle income countries. Sub-Saharan Africa is the most affected region, with an estimated 25.6 million people living with HIV in 2015. About 66% of new HIV infections in 2015 occurred in sub-Saharan Africa [2]. Unprecedented efforts of the last thirty years have turned human immunodeficiency virus infections from terrifying lethal diseases to manageable conditions [3]. Combination antiretroviral therapy dramatically reduces the viral load to an undetectable level (
The impact of the HIV pandemic on women is rising, even in countries where other routes of transmission are more prevalent [5]. Women have few options to protect themselves from acquiring HIV. Efforts to promote abstinence, monogamy and the use of condoms have not been enough to stop the epidemic nor are these approaches practical in many settings [6]. Women face difficulties convincing their male partners, especially husbands and regular partners, to use condoms or to be monogamous or faithful. Female condoms, developed as an alternative to give more control to women to protect themselves, are not widely accepted. Structural issues and high cost have hampered their use. HIV Pre-Exposure Prophylaxis (PrEP) provides a promising new approach for slowing the spread of HIV in the United States [7].However, Prep is not widely available globally [8], limiting the number of options to women to protect themselves against HIV. The development of products applied inside the vagina or rectum to protect against HIV commonly called microbicides provide great potential for a female-controlled, preventive option, which would not require negotiation, consent or even knowledge of the partners [9]. Microbicides could benefit both men and women. The successful utilization of this preventive method depends on its efficacy and its acceptability.
The discovery of an effective vaccine remains the goal of HIV research. Vaccine technologies have evolved significantly in the last decade. Reports that the prime/boost combination of two vaccines (ALVAC (R) HIV and AIDSVAX(R) B/E) lowered the rate of HIV infection by 31.2 percent in more than 16,000 volunteers in Thailand demonstrated that the development of an effective preventive HIV vaccine is scientifically possible. This discovery has reinvigorated and raised hope among researchers. This review was undertaken to describe promising new initiatives in our continued efforts to fight the HIV epidemic. This update will keep knowledge about HIV/AIDS current among community organizers, health educators and policy makers.
1. Methods Search strategy Medline via PubMed and Google search engine were searched for relevant articles published between January 2007 and April 2017. The key search terms applied included: “Lifecycle” or “Antiretroviral therapy” or “New Prevention technologies” or “HIV Vaccines” and "HIV”. The formal review process was further informed by searches of published research and technical reports from peer-reviewed journals presented at scientific conferences and reference lists from publications of interest. Some grey literature including conference presentations, project reports, government reports, and released by international organizations such as UNAIDS and the World Health Organization were also considered.
1.1 Inclusion Criteria
Original articles published in English and covering any of the above-mentioned keywords regardless of the country were considered for this review. Articles published in any language other than English were excluded. Methods of assessment of documents Citations were examined, titles and abstracts were screened for eligibility. Selected citations were classified as either:
- Primary citations qualifying for inclusion in the synthesis or
- Not relevant citations not included in this study.
Full texts were reviewed in greater detail if deemed relevant, and findings pertinent to this literature review were included in this article.
2.1 HIV/AIDS Treatment
2.1.1 Mechanisms of Action of Antiretroviral Drugs
The discovery of the causative agent of AIDS together with the understanding of the virus replication cycle were instrumental in assisting researchers to prosecute drug discovery efforts focused on targeted inhibition with specific pharmacological agents [10]. ( Figure 1) summarizes the HIV life cycle. To multiply, the HIV virus infects only cells that carry CD4 receptors on their surface, such as T4-lymphocytes, monocytes and macrophages, glial cells in the brain, chromaffin cells in the intestines and Langerhans' cells in the skin [11]. TheCCR5 or CXCR4 antagonists are antiretroviral drugs that can prevent the viral attachment to the CD4 T-cells.
Once the HIV binds to a CD4+ surface receptor, it activates other proteins on the surface of the human cell known as CCR5 and CXCR4 to allow the HIV envelope and CD4 cell membrane to fuse. A second group of drugs can interfere with the fusion process (Fusion inhibitors). Once inside the cell, the viral capsid that contains the RNA and important enzymes is released into the host cell (Uncoating). A viral enzyme called reverse transcriptase converts its genetic material, HIV RNA into HIV DNA, allowing HIV to enter the CD4 cell nucleus. Reverse transcription can be blocked by NucleosideReverse Transcriptase Inhibitors(NRTIs) and Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs). The newly formed viral DNA is then integrated with the DNA of the human host cell using a viral enzyme called integrase (Integration). The Integrase inhibitors can block the integration phase. Once integrated into the CD4 cell, the CD4 machinery produces long chains of HIV proteins (replication). A viral enzyme called protease cuts these long chains of proteins into smaller proteins to form the structure of the new HIV particle, including each of the enzymes and proteins needed to repeat the reproductive process [12].
Once the new viral particles are assembled, they bud off the host cell and can infect other cells. Protease inhibitors can block viral assembly.
2.1.2 Classes of A ntiretroviral Drugs
The FDA approved the first antiretroviral drug, zidovudine (AZT), to treat people infected with HIV/AIDS on March 19, 1987 [13]. Since the advent of the first HIV-1 specific antiviral drugs given as monotherapy, significant progress has led to the development of more than 25 FDA-approved antiretroviral drugs. The 6 classes of ARVs include: The Nucleoside/Nucleotide Reverse Transcriptase Inhibitors (NRTIs), Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs), Protease Inhibitors (PIs), a Fusion Inhibitor (FI), a CCR5 antagonist, and Integrase Strand Transfer Inhibitors (INSTIs). Other drugs including Ritonavir (RTV) and Cobicistat (COBI) are used to improve the Pharmacokinetic (PK) profiles of some ARV drugs (e.g., PIs and The INSTI Elvitegravir (EVG) [14]. (Table 1) presents the antiretroviral drugs used in the treatment of HIV infection. The description of individual drug is beyond the scope of this paper.
HIV Clinicians and patients may select a regimen based on several considerations including antiviral potency, short- and long-term adverse effects, ease of administration, drug interactions, risk of resistance and cost [15].To address the complexity in HIV management in terms of initiating, switching and discontinuing the Anti-Retroviral Treatment (ART), a panel of experts in HIV research and patient care recommended that all HIV-infected individuals with detectable viremia, regardless of their CD4 cell count, should begin ART as soon as possible after diagnosis to prevent disease progression, improve clinical outcomes and limit transmission [16]. They recommended that the initial regimen should consist of 2 Nucleoside Reverse Transcriptase Inhibitors (NRTIs) plus an Integrase Strand Transfer Inhibitor (InSTI). They also made recommendations for special populations (e.g. pregnant women, hepatitis B/C virus coinfection) and for context of acute opportunistic infections [15]. Study data supports switching therapy in some patients because of virologic failure, drug resistance or more adverse or toxic effects [17]. For the good management of PLH, the panel of experts in HIV research and patient care recommend that CD4 cell count, plasma HIV RNA, serum chemistries and estimated creatinine clearance be done as close to the time of HIV diagnosis as possible and prior to beginning ART. Strict adherence to antiretroviral therapy is key to sustained HIV suppression, reduced risk of drug resistance, improved overall quality of life, and survival, [18] as well as decreased risk of HIV transmission [19].
2.2 HIV/AIDS Prevention
Effective HIV prevention requires a combination of behavioral, biomedical and structural intervention strategies [20]. The early initiation of antiretroviral therapy has been shown to reduce rates of sexual transmission of HIV-1 and clinical events, indicating both personal and public health benefits from such therapy[19].The evidence to support the use of Antiretroviral Therapy (ART) for prevention of new HIV infection in the form of Pre-exposure Prophylaxis (PrEP) among men who have sex with men, transgender, people who inject drugs, heterosexual men and women and HIV-1 serodiscordant couples, or Treatment as Prevention (TasP) for sero
Discordant couples have also grown [21].
2.2.1 Biomedical Intervention
2.2.1.1 Prevention of Mother-to-Child Transmission
The first success of ART has been in preventing mother-to-child transmission of HIV Prevention of Mother-To-Child Transmission (PMTCT) of HIV in the United States and Europe has been a tremendous success, such that transmission rates of less than 2% have been achieved [22].
2.2.1.2 therapy as prevention.
Though long suspected that treatment reduces an individual’s viral load resulting in decreased risk of HIV transmission, the HIV Prevention Trials Network 052 (HPTN 052) study was the first to conclusively prove this theory. Early initiation of ART (when cell counts are greater than 350) by HIV-infected individuals reduced the
risk of HIV transmission to the uninfected sexual partners by 96 percent compared to initiation when CD4 counts were
2.2.1.3 Pre-Exposure and Post Exposure Prophylaxis
Pre-Exposure Prophylaxis (PrEP), is the concept of HIV-negative individuals taking HIV ART to prevent the acquisition of HIV. The use of an ART for PrEP was approved by the United States Food and Drug Administration (FDA) in July 2012 and has been shown to be safe and effective through the Global iPrEx and Partners Prep studies [25].
There is evidence that Post Exposure Prophylaxis (PEP) can reduce the risk of HIV transmission [26]. PEP is an emergency intervention designed to abort HIV acquisition in the event of occupational (i.e., needle stick or mucous membrane splash) or no occupational (i.e., sexual or injecting drug use) exposure to HIV-infected blood or potentially infectious bodily fluids [27].
2.2.1.4 HIV Testing and Counseling
Early knowledge of one’s positive HIV sero status maximizes opportunities for the person to access care, thereby greatly reducing HIV-related morbidity and mortality, and/or preventing transmission of HIV. Meta-analyses find that PLH who are aware of their sero status are at least half as likely to engage in risky sexual behaviors compared to those unaware PLH [28]. HIV testing is the cornerstone for HIV prevention.
2.2.1.5 Male and Female Condoms
When used consistently and correctly, male condoms can be highly effective in preventing Sexually Transmitted Diseases (STDs) including HIV [29]. However, they provide less protection against STDs spread through skin-to-skin contact like human papillomavirus (genital warts), genital herpes, and syphilis. Although the female condom has been on the market for more than ten years, adoption by end-users, providers, national governments, and donors has remained low. The high price and certain technical characteristics are often cited as the primary obstacles for end-user adoption [30].
2.2.1.6 Diaphragmes
There is considerable interest in developing new multipurpose prevention technologies to address women's reproductive health needs. Dapivirine-releasing diaphragm with daily release quantities potentially can prevent HIV transmission [31].
2.2.1.7 Male Circumcision
Three large Randomized Controlled Clinical Trials (RCTs) conducted in South Africa, Kenya and Uganda showed that medical circumcision significantly reduced male participants’ HIV infection risk, ranging from 48% to 61% [32-35]. In addition, circumcision was shown to be associated with a significantly reduced risk of urinary tract infection [35]. Circumcision, however, has not shown a significant protective effect against HIV acquisition among Men Who Have Sex with Men (MSM).
2.2.1.8 Microbicides
After several disappointing microbicide trials that failed to show protection against HIV infection, [36,37] the results of the Centre for the AIDS Program of Research in South Africa - the CAPRISA 004 trial - demonstrated that a vaginal microbicide gel containing tenofovir reduced the risk of HIV infection for women by 39% (95% CI: 6, 60) [38]. Building on that experience, the NIH-ASPIRE study, also known as MTN-020, showed that a vaginal ring that continuously releases the experimental antiretroviral drug Dapivirine provided a modest level of protection against HIV infection in women with an overall effectiveness of 31 percent [39]. Microbicides may also be preferable to condoms as an HIV prevention option for some women because women would not have to negotiate their use, as they often must do with condoms.
2.2.2 Behavioral Interventions
Given the challenges of further reducing HIV infection rates and developing an effective vaccine, it is critical to focus on behavioral prevention efforts that are based on the best available scientific evidence [40]. Behavioral interventions have been shown to decrease sexual risk behaviors [41] and increase condom use [42]. The compendium of effective HIV prevention interventions exists [43]. Sister-to-Sister is a brief (20-minute), one-on-one, skill-based HIV/STD risk-reduction behavioral intervention for sexually active African American women 18 to 45 years old that is delivered during a routine medical visit. Sister-to-Sister is designed to provide intensive, culturally sensitive health information to empower and educate women in a clinical setting; help women understand HIV/STD risk behaviors; and enhance women’s knowledge, beliefs, motivation, confidence, and skills to help them make behavioral changes that will reduce their risk [44].
2.2.3 Structural Interventions
Macroeconomic and social forces such as poverty, racism, sexism and homophobia, help fuel HIV epidemics, although the pathways between these forces and HIV infection are complex and not always clear [45,46]. Structural interventions seek to address social, economic, political or environmental factors that make individuals or groups vulnerable to HIV infection. For example, laws that criminalize same-sex relationships often hinder men who have sex with men from accessing condoms. A lack of infrastructure, such as transport, prevents many people from accessing health clinics. By successfully addressing these structural barriers, individuals are empowered and able to access HIV prevention services [47].
One example of structural intervention is the Needle and Syringe Programs (NSPs). NSPs are a type of harm reduction initiative that provide clean needles and syringes to people who inject drugs (sometimes referred to as PWID). NSPs are offered at fixed or mobile sites. Fixed sites are typically located where the drugs are bought and sold openly. At fixed sites, additional services such as healthcare services alongside testing and counselling for HIV and other blood-borne viruses [48]. Outreach programs may include mobile units (such as a van or bus), backpacking services on the street or even home deliveries. NSPs substantially and cost effectively reduce the spread of HIV among PWID and do so without evidence of exacerbating injecting drug use at either the individual or societal level [49].
Despite the promise of structural interventions and donor enthusiasm for additional efforts in their implementation and evaluation, less data has been collected on structural interventions than on biomedical and behavioral interventions. Few currently existing programs have been rigorously evaluated against biological outcomes, such as HIV biomarkers [50].
2.3 HIV Vaccine
The discovery of an effective vaccine remains the ultimate goal of HIV research. However, several factors have contributed to slowing the international efforts to develop an effective HIV vaccine. The number of circulating viral strains is one of the most intractable obstacles to vaccine development. Extremely rapid and error-prone replication yields a large number of mutant genomes, some of which are able to escape immune control [51]. Another major obstacle is the lack of clear immune correlates of protection in humans.
Hard fought advances in basic and clinical research are raising new hope. First, vaccine technology has evolved significantly in the last decade, profoundly changing the future of vaccine development. Reports that the prime/boost combination of two vaccines (ALVAC (R) HIV and AIDSVAX(R) B/E) lowered the rate of HIV infection by 31.2 percent in more than 16,000 volunteers in Thailand demonstrating that the development of an effective preventive HIV vaccine is scientifically possible. Recent advances in isolating broadly neutralizing antibodies and designing new tools and technologies for vaccine delivery have enhanced hope and reinvigorated vaccine discovery efforts [52]. Investigation into additional therapeutic approaches led to the use of gene therapy aimed at a diverse list of disorders including arthritis, HIV infection, dozens of different types of cancers and extremely rare genetic diseases [53].
2.4 The Future of HIV/AIDS
2.4.1 Long Lasting Antiretroviral therapy
Although antiretroviral drugs provide durable control of virus replication in many patients, they are not devoid of unwanted secondary effects including long-term side effects, the emergence of multidrug resistance and transmission of drug-resistant HIV strains. Further simplification of treatment and identification of more effective drug combinations are needed to improve patient adherence, the most significant cause of treatment failure. New mechanisms to deliver long-acting ART are being studied and present the potential to improving adherence to treatment and optimizing HIV care [54].
2.4.2 Shock and Kill
Combinatory antiretroviral therapy increases the survival and quality of life of HIV-1-infected patients. However, interruption of therapy almost invariably leads to the re-emergence of detectable viral replication because HIV-1 persists in viral latent reservoirs. Improved understanding of the molecular mechanisms involved in HIV-1 latency has paved the way for innovative strategies that attempt to purge the latent virus[55].One strategy termed “shock and kill” is aimed at decreasing the numbers of latently infected cells after the activation of HIV transcription in order for host cells to produce HIV-1 proteins (shock); this will presumably allow the cells to be cleared by virus-associated cell death or by a host response (kill) [54].A wide variety of compounds are under investigation as candidate Latency-Reversing Agents (LRAs) for the shock step. Latency-Reversing Agent (LRA) combinations exhibit such a potent effect and represent a proof-of-concept for the co-administration of two different types of latency-reversing agents as a potential strategy to reduce the size of the latent HIV-1 reservoirs [56]. The ongoing BCN02 trial adds three doses of R omidepsin between the initial and the final vaccine boosts. This cancer drug can activate hidden HIV reservoirs, making it easier for the immune system to eliminate latent viruses [54].
2.4.3 New Tools and Technologies for Vaccine Delivery
Developing safe, effective and affordable HIV vaccines is the best hope for ending the HIV/AIDS pandemic. Advances in HIV vaccine development-including the design of new tools and technologies for vaccine delivery-have boosted optimism in the field about the prospects for the development of a safe and effective HIV vaccine. The identification of dozens of broad spectrum antibodies that neutralize a wide spectrum of HIV variants circulating around the world is a major step against the constant ability of the virus to mutate. The cell immunity can be stimulated using a new antigen delivery mechanism. Recombinant vaccines rely on the capacity of one or multiple defined antigens to induce immunity against the pathogen, when administered in the presence of adjuvants or when expressed by plasmids or harmless bacterial/viral vectors [57].
This study was undertaken to advances in the management of the HIV infection. This review showed how unprecedented efforts in the fields of biology, pharmacology, and clinical care led to the development of several antiretroviral agents. As a result, the HIV/AIDS causing retrovirus has gone from being an untreatable infectious agent to one eminently susceptible to a range of approved therapies. Approximately thirty antiretroviral agents with different mechanisms of action, formulated either singly or in combination, are available today to treat patients with Human Immunodeficiency Virus (HIV-1).
Despite the impressive results of antiretroviral drugs, HIV-1/AIDS pandemic remains a challenge. While antiretroviral drugs are widely accessible in rich-country, they are not accessible by every PLH, especially those living in developing countries. Current coverage shortfalls, combined with the relentless expansion of the epidemic, underscore the need for effective prevention interventions to control HIV epidemic. Promoting the utilization of condoms, performing male circumcision in poor communities, and making clean needles available to injecting drug users are few interventions known to be effective. They can be easily integrated to curb the spread of HIV in poor countries.
People living with HIV are expected to take antiretroviral therapy for the rest of their lives in order to prevent viral replication and hopefully prevent opportunistic infections. However, long term ARV therapy increases the risk for cardiac and metabolic side-effects, including dyslipidemias, insulin resistance, and abnormal body fat re-distribution (lipodystrophy, which can lead to increased risk for heart disease and type 2 diabetes. Treatment of these chronic health conditions will require additional resources in an already financially challenged health system.
Integrated provirus in memory T cells, dendritic cells, macrophages, and microglia, that persists for long periods, makes true HIV-1 eradication difficult with available technologies. However, Latency-Reversing Agent (LRA) combinations is a promising strategy to reduce the size of the latent HIV-1 reservoirs.
This review found that when the viral load becomes and stays undetectable with successful treatment, the risk for sexual transmission of HIV is negligible. The public health implication of this knowledge underscores the needs for governments in countries hit hard by the HIV epidemic to do every effort to make antiretroviral therapy available to as many HIV-infected people as possible. A concern that low educated people may not adhere to the regimen and give rise to virus resistance has not materialized in sub-Saharan Africa.
Several approaches have been tried to fight HIV epidemic. Gene therapy and viral mediated therapy are few methods that have been used. Regardless of their outcome relative to HIV infection, knowledge gained in the fight against HIV epidemic could have indirect benefit. Lessons learned could be applied to treat other conditions. For example, knowledge in the development gained in the development of an HIV vaccine contributed to the rapid development of the Ebola vaccine. Other techniques are now being used to treat cancer.
This review is by no means a daily account of events that occurred from the discovery of the new disease till today. It highlighted what the authors considered important to provide a broad picture of the important achievement in the fight against HIV/AIDS. The fact that only papers published in English were reviewed, other important events may have been overlooked.
The fight against HIV epidemic has been hard, long and expensive. Yet, progress has been made and the end of the tunnel is perceptible. The HIV prevention toolbox continues to grow steadily, allowing clinicians to safely prevent and treat HIV infection. While waiting for the advent of the magic bullet to cure HIV infection, the combination of behavioral, structural and biomedical interventions can prevent the incidence of new HIV cases, but also prevent the occurrence of opportunistic infections and improve the quality of life for people living with HIV. Efforts are currently being made to address disparities that persist for the attainment of the 90-90-90 targets, which are that 90% of people living with HIV know their HIV status, 90% of people who know their HIV-positive status are accessing treatment and 90% of people on treatment have suppressed viral loads by 2020 [58].
Conflict of Interest
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgements
We are immensely grateful to Robert Brown for designing the HIV life cycle for this manuscript. We also thank Jennifer Rundles, the librarian from Central Michigan University, for assisting the authors in the database search.

Figure1: HIV Lifecycle.
Table 1: FDA-Approved Antiretroviral Drugs. Adapted From: Antiretroviral Drugs Used in the Treatment of HIV Infection , U.S. FDA.
- Friedman-Kien A, Laubenstein L, Marmor M, Hymes K, Green J, et al. (1981) Kaposissarcoma and Pneumo cystis pneumonia among homosexual men--New York City and California. MMWR Morbidity and mortality weekly report 30: 305-308.
- HIV/AIDS Basics : Global Statistics.
- Farooq T, Hameed A, Rehman K, Ibrahim M, Qadir MI, et al. (2016) Antiretroviral Agents : Looking for the Best Possible Chemotherapeutic Options to Conquer HIV. Critical Reviews in Eukaryotic Gene Expression 26: 363-381.
- Al-Harthi L, Siegel J, Spritzler J, Pottage J, Agnoli M, et al. (2000) Maximum suppression of HIV replication leads to the restoration of HIV-specific responses in early HIV disease. AIDS 14: 761-770.
- Nicoll A, Gill O (1999) Global impact of HIV infection and disease. Communicable Disease and Public Health 2: 85-95.
- Bender J (2012) Microbicides as an HIV Prevention Tool: A Review of the Literature. University of Pittsburgh.
- McMahon JM, Myers JE, Kurth AE, Cohen SE, Mannheimer SB, et al. (2014) Oral pre-exposureprophylaxis (PrEP) for prevention of HIV in serodiscordant hetero sexual couples in the United States :opportunities and challenges. AIDS patient care and STD s28: 462-474 .
- Dawson L, Garner S, Anude C, Ndebele P, Karuna S, et al. (2015) Testing the waters: ethical considerations for including PrEP in a phase IIb HIV vaccine efficacy trial. Clinical trials 12: 394-402.
- Gupta SK, Nutan (2013) Clinical use of vaginal or rectally applied microbicides in patients suffering from HIV/AIDS. HIV/AIDS 5:295-307.
- Rajarapu G (2013) Genes and Genome of HIV-1. Journal of Phylogenetics & Evolutionary Biology 2: 1-7.
- Hughes JR (2002) HIV- Structure, Life Cycle and Pathogenecity.
- Kirchhoff F (2013) HIV life cycle :Overview. Encyclopedia of AIDS, New York, Springer : 1-9.
- Staff Ag (1987) Approval of AZT.
- AIDS info (2013) A Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents.
- Gunthard HF, Saag MS, Benson CA, Del Rio C, Eron JJ, et al. (2016) Antiretroviral drugs for treatment and prevention of HIV infection in adults: 2016 recommendations of the International Antiviral Society-USA panel. Jama 316: 191-210.
- Group ISS (2015) Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Eng J Med 373: 795-807.
- Trottier B, Lake J, Logue K (2015) Switching to Abacavir/Dolutegravir/Lamivudine combination (ABC/DTG/3TC FDC) from a PI, INI or NNRTI based regimen maintains HIV suppression. Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC) : 17-21.
- Chesney MA (2006) The elusive gold standard :future perspective for HIV adherenceassessment and intervention. J Acqui Immune DeficSyn d 43: 149-155.
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, et al. (2011) Prevention of HIV-1 infection with early anti retro viral therapy. New Eng J Medi 365: 493-505.
- Rotheram-Borus MJ, Swendeman D, Chovnick G (2009) The past, present, and future of HIV prevention: integratingbehavioral, biomedical, and structural intervention strategies for the next generation of HIV prevention. Annual review of clinical psychology 5: 143-167.
- Idoko J, Folayan MO (2014) The use of antiretroviral therapy for the prevention of new HIV infection in populations at high risk for HIV sero-conversion in Nigeria : perspectives paper. African J Reprod Health 18: 127-134.
- Fowler MG, Lampe MA, Jamieson DJ, Kourtis AP, Rogers MF (2007) Reducing the risk of mother-to-child human immuno deficiency virus transmission :past successes, current progress and challenges and future direction. American Journal of Obstetrics and Gynecology197: 3-9.
- Organization WH (2012) Programmatic update : Antiretroviral Treatment As Prevention (TASP) of HIV and TB :Executive Summary.
- Turner BJ (2002) Adherence to Antiretroviral therapy by human immuno deficiency virus-infected patients. Journal of Infectious Diseases 185: S143-S151.
- Hankins CA, Dybul MR (2013) The promise of pre-exposurepro phylaxiswithanti retro viral drugs to prevent HIV transmission : Areview. Current opinion in HIV and AIDS 8: 50-58.
- Mackie N, Coker R (2000) Post-exposureprophylaxis following non-occupational exposure to HIV :risks, uncertainties, and ethics. International journal of STD & AIDS 11: 424-427.
- Marrazzo JM, Del Rio C, Holtgrave DR, Cohen MS, Kalichman SC, et al. (2014) HIV prevention in clinical care settings : 2014 recommendations of the International Antiviral Society-USA Panel. JAMA 312 : 390-409.
- Marks G, Crepaz N, Senterfitt JW, Janssen RS (2005) Meta-analysis of high-risk sexual behavior in personsaware and unaware they are infected with HIV in the United States : implications for HIV prevention programs. J Acquir Immune Defic Syndromes 39: 446-453.
- Anderson JE (2003) Condom use and HIV riskamong US adults. Am J Public Health93 :912-914.
- Dias PRT, Souto K, Page-Shafer K (2006) Long-term female condom use among vulnerable populations in Brazil. AIDS and Behavior10: 67-75.
- Major I, Boyd P, Kilbourne-Brook M, Saxon G, Cohen J, et al. (2013) A modified SILCS contraceptive diaphragm for long-termcontrolled release of the HIV microbicide dapivirine. Contraception 88: 58-66.
- Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, SittaR,et al. (2005) Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS medicine 2: e298.
- Bailey RC, Moses S, Parker CB, Agot K, Maclean I, et al. (2007) Male circumcision for HIV prevention in young men in Kisumu, Kenya : Arandomised controlled trial. The Lancet 369: 643-656.
- Gray RH, Kigozi G, Serwadda D, Makumbi F, Watya S, et al. (2007) Male circumcision for HIV prevention in men in Rakai, Uganda : Arandomised trial. The Lancet 369: 657-666.
- Singh-Grewal D, Macdessi J, Craig J (2005) Circumcision for the prevention of urinary tract infection in boys : Asystematic review of randomised trials and observational studies. Arch Dis Child 90: 853-858.
- Halpern V, Ogunsola F, Obunge O, Wang C-H, Onyejepu N, et al. (2008) Effectiveness of cellulose sulfate vaginal gel for the prevention of HIV infection :results of a Phase III trial in Nigeria. PloS one 3: e3784.
- McCormack S, Ramjee G, Kamali A, Rees H, Crook AM, et al. (2010) PRO2000 vaginal gel for prevention of HIV-1 infection (Microbicides Development Programme 301) : A phase 3, randomised, double-blind, parallel-group trial. The Lancet 376: 1329-1337.
- Abdool Karim Q, Abdool Karim SS, Frohlich JA, Grobler AC, Baxter C,et al. (2010) Effectiveness and safety of tenofovir gel, an antiretro viral microbicide, for the prevention of HIV infection in women. Science 329: 1168-1174.
- Baeten JM, Palanee-Phillips T, Brown ER, Schwartz K, Soto-Torres LE, et al. (2016) Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. New Eng J Med 375: 2121-2132.
- Lyles CM, Kay LS, Crepaz N, Herbst JH, Passin WF, et al. (2007) Best-Evidence Interventions: Findings From a Systematic Review of HIV Behavioral Interventions for US Populations at High Risk, 2000-2004. Am J Public Health 97: 133-143.
- von Sadovszky V (2014) Pilot Test of a Web-Based Decisional Support Intervention called Strong Women Stay Safe to Promote Safer Sex Behaviors in Young Women. In: 142nd APHA Annual Meeting and Exposition: APHA.
- Scott-Sheldon LA, Huedo-Medina TB, Warren MR, Johnson BT, Carey MP (2011) Efficacy of behavioral interventions to increase condom use and reduce sexually transmitted infections: a meta-analysis, 1991 to 2010. J Acquir Immune Defici Syndromes 58: 489-498.
- Control CfD (2010) Prevention: HIV/AIDS Prevention Research Synthesis Project. Compendium of HIV Prevention Interventions with Evidence of Effectiveness.
- Jemmott LS, Jemmott III JB, O’Leary A (2007) Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. Am J Public Health 97: 1034-1040.
- Lane SD, Rubinstein RA, Keefe RH, Webster N, Cibula DA, et al. (2004) Structural violence and racial disparity in HIV transmission. J Health Care Poor Underserved 15: 319-335.
- Blankenship KM, Friedman SR, Dworkin S, Mantell JE (2006) Structural interventions : concepts, challenges and opportunities for research. J Urban Health83: 59-72.
- Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A (2008) Structural approaches to HIV prevention. The Lancet 372: 764-775.
- Organization WH (2007) Guide to starting and managing needle and syringe programmes.
- Alex W, Annie C (2004) Organization WH: Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. Evidence for action technical papers.
- Pronyk P, Lutz B (2013) Policy and programme responses for addressing the structural determinants of HIV. USAID’s AIDS Support and Technical Assistance Resources, AIDSTAR-One. Task Order : 1.
- O’Connell RJ, Kim JH, Corey L, Michael NL (2012) Human Immunodeficiency Virus Vaccine Trials. Cold SpringHarb Perspect Med 2: 7351.
- Koff WC, Burton DR, Johnson PR, Walker BD, King CR, et al. (2013) Accelerating next-generation vaccine development for global disease prevention. Science 340: 1232910.
- Cermakova K, Weydert C, Christ F, De Rijck J, Debyser Z (2016) Lessons Learned: HIV Points the Way Towards Precision Treatment of Mixed-Lineage Leukemia. Trends Pharmacol Sci 37: 660-671.
- Delagrèverie HM, Delaugerre C, Lewin SR, Deeks SG, Li JZ (2016) Ongoing Clinical Trials of Human Immunodeficiency Virus Latency-Reversing and Immuno modulatory Agents. Open Forum Infectious Dise 3: 189.
- Darcis G, Van Driessche B, Van Lint C (2017) HIV Latency: Should We Shock or Lock?Trends Immunol 38: 217-228.
- Darcis G, Kula A, Bouchat S, Fujinaga K, Corazza F, et al (2015) An In-Depth Comparison of Latency-Reversing Agent Combinations in Various In Vitro and Ex Vivo HIV-1 Latency Models Identified Bryostatin-1+JQ1 and Ingenol-B+JQ1 to Potently Reactivate Viral Gene Expression. PLoS pathogens 11: e1005063.
- Nascimento I, Leite L (2012) Recombinant vaccines and the development of new vaccine strategies. Braz J Med Bio Res 45: 1102-1111.
- Isbell MT, Kilonzo N, Mugurungi O, Bekker LG (2016)We neglect primary HIV prevention at our peril. The Lancet HIV 3: e284-e285.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA : Creative Commons Attribution-Share Alike 4.0 International License. With this license, readers can share, distribute, download, even commercially, as long as the original source is properly cited. Read More .
Current Research on HIV/AIDS
- About Journal
- Aims and Scope
- Board Members
- Article in Press
- Recent Articles
- Articles Search
- Current Issue
We use cookies for a better experience. Read privacy policy . Manage your consent settings:
Manage Your Consent:
- Open access
- Published: 01 June 2024
Comprehensive knowledge of mother-to-child HIV/AIDS transmission, prevention, and associated factors among reproductive-age women in East Africa: insights from recent demographic and national health surveys
- Bewuketu Terefe 1 ,
- Mahlet Moges Jembere 2 &
- Bikis Liyew 2
BMC Women's Health volume 24 , Article number: 318 ( 2024 ) Cite this article
159 Accesses
1 Altmetric
Metrics details
More than 90% of babies acquire HIV/AIDS through vertical transmission, primarily due to low maternal comprehensive knowledge about Mother-To-Child Transmission (MTCT) of HIV/AIDS and its prevention, which is a cornerstone for eliminating MTCT of HIV/AIDS. However, there are limitations in terms of population data and literature evidence based on recent Demographic and Health Surveys (DHS) reports in East Africa. Therefore, this study aims to assess the comprehensive knowledge and PMTCT of HIV/AIDS among women, as well as the associated factors in East Africa.
Our data was obtained from the most recent DHS conducted in East African countries between 2011 and 2022. For our research, we included DHS data from ten nations, resulting in a total weighted sample of 133,724 women for our investigation. A generalized linear model (GLM) with a log link and binomial family to directly estimate prevalence ratios (PR) and 95% confidence intervals (CI) for the association between the independent variables, and the outcome variable. Finally, we reported the adjusted prevalence ratios along with their corresponding 95% CIs. Factors with p-values ≤ 0.2 for univariate logistic regression and < 0.05 were considered statistically significant factors of HIV/AIDS knowledge and prevention in the final model.
In this study, 59.41% (95% CI: 59.15–59.67) of respondents had a comprehensive knowledge about MTCT of HIV/AIDS and its prevention among reproductive-age women in East Africa. Being in the older age group, better education level, being from a rich household, employment status, having ANC follow up, institutional delivery, and modern contraception usage were associated with higher prevalence ratios of comprehensive knowledge about MTCT of HIV/AIDS and its prevention. However, being single in marital status, rural women, and traditional contraception utilization were associated with lower ratios of comprehensive knowledge about MTCT of HIV/AIDS and its prevention.
Our findings indicate a significant deficiency in comprehensive knowledge and prevention of HIV/AIDS MTCT among women in East Africa. These results emphasize the need for significant improvements in maternal-related health services. It is crucial to effectively target high-risk populations during interventions, raise awareness about this critical public health issue, and address the catastrophic consequences associated with MTCT. By implementing these measures, we can make substantial progress in reducing the transmission of HIV/AIDS from mother to child and ensuring better health outcomes for both mothers and their children.
Peer Review reports
Introduction
Vertical transmission of Human Immunodeficiency Virus (HIV) from mother to child during pregnancy, birth, and breast feeding remains a serious public health concern and is the leading source of HIV infection in children under the age of 15 worldwide [ 1 , 2 ]. Morbidity and mortality from HIV infection have declined globally over the last decade as a result of preventive measures such as greater coverage of Antiretroviral Therapy (ART) and prevention of HIV/AIDS transmission from mother to child (PMTCT) [ 3 , 4 ]. However, over 90% of new infections of HIV in babies and young children are transmitted from mother to child still [ 5 ]. In 2022, there was around 39 million HIV-positive people worldwide [ 6 ]. Among these, about 37.5 million, and 1.5 million were adults and children (15 and under), 53% were women and girls [ 6 , 7 ]. Similarly, the USAIDS, in 2023 estimated, more than 39 million individuals were infected with HIV, and lived with the virus [ 8 ]. Additionally, AIDS-related illnesses claimed the lives of almost 630 thousand people this year [ 8 ]. However, Eastern and Southern Africa making over half of that number [ 9 , 10 ]. Using the above references, it is obvious that the number of people getting infected with HIV is increasing over time, and rigorous research related to it is expected from various individuals and organizations [ 6 ].
According to the UNAIDS 2023 report, in terms of women and girls in 2022, women and girls of all ages accounted for 46% of all new HIV infections worldwide [ 11 ]. Women and girls (of all ages) accounted for 63% of all new HIV infections in Sub-Saharan Africa (SSA) [ 6 , 11 ]. In all other geographical regions, men and boys accounted for more than 70% of new HIV infections in 2022. In 2022, 4000 adolescent girls and young women aged 15–24 years would be infected with HIV per week over the world. SSA was responsible for 3100 of these illnesses [ 12 ].
In 2017, approximately 50% of the 180,000 new pediatric HIV infections occurred during breastfeeding, and it is estimated that in the absence of any intervention to prevent MTCT, the risk of transmission ranges from 15 to 45% (5–10% during pregnancy, 10–20% during childbirth, and 10–20% via mixed infant feeding) [ 13 ]. This rate, however, can be reduced to less than 5% with appropriate interventions [ 13 ]. The recent 2023 UNAIDS reports indicated that, each day, HIV infection affects 4,000 individuals, including 1,100 young people aged 15 to 24. If present patterns persist, it is projected that 1.2 million individuals will acquire HIV in 2025, which is three times higher than the targeted number of 370,000 new infections for that year [ 14 ].
Knowledge of MTCT and PMTCT for HIV/AIDS is associated with characteristics such as maternal age, maternal education, wealth level, occupation, marital status, media exposure, and domicile [ 15 , 16 , 17 , 18 , 19 , 20 ]. Maternal awareness of HIV/AIDS MTCT and prevention is essential for HIV MTCT elimination. Despite the fact that the majority of the population in SSA lives in rural areas with limited availability and accessibility of health facilities, the majority of studies on HIV/AIDS knowledge and prevention were conducted among available women, such as those who came to the health facility for their antenatal care follow up [ 17 , 21 , 22 , 23 , 24 , 25 ]. Since East Africa is the second most affected region by HIV/AIDS, women are the primary vulnerable group among the population in the region, and no current study has revealed the situation utilizing nationally representative data from recent DHS surveys that this study aims to investigate. Hence, studying women’s comprehensive knowledge about HIV/AIDS will help reduce stigma and discrimination, improve health outcomes for mothers and children, and decrease MTCT [ 26 ]. Furthermore, by understanding the factors involved, the findings of this study can provide valuable insights for policymakers, healthcare providers, and public health practitioners in East Africa. Therefore, using the recent national demographic health survey data, this study aimed to assess the comprehensive knowledge and PMTCT of HIV/AIDS among women, as well as its associated factors in East Africa.
Data sources and study population
Our data was obtained from the most recent Demographic and Health Surveys (DHS) conducted in East African countries between 2011 and 2022. This study included DHS data from 10 countries as shown in Table 1 . To conduct our research, we incorporated DHS data from these 10 nations using the corresponding Stata command. The survey utilized stratified, two-stage cluster sampling. In the first step, enumeration areas (EAs) were selected with a probability proportional to their size within each sampling stratum. Subsequently, households were sampled in the second step. The source population consisted of mothers of reproductive age. Consequently, classical logistic regression was deemed more appropriate. Ultimately, our study utilized a weighted sample of 133,724 women of reproductive age.
Data management and statistical analysis
Stata version 17 is used to extract, recode, and analyze data. Weighting was used throughout the study to ensure representativeness and non-response rate, as well as to obtain a suitable statistical estimate (robust standard error) [ 27 ]. In the univariate analysis, variables with a p-value of ≤ 0.2 were considered for the multivariable analysis. The multivariable logistic model provided the adjusted prevalence ratio (APR) with a 95% confidence interval to identify the associated factors of knowledge of PMTCT use. We used generalized linear models (GLM) with a log link and binomial family to directly estimate prevalence ratios (PR) and 95% confidence intervals (CI) for the association between the independent variables and the binary outcome of comprehensive knowledge of PMTCT. This approach allows for the estimation of PRs without the common issue of overestimation that can occur when using logistic regression to estimate odds ratios for common outcomes. We specified robust standard errors to account for potential heteroscedasticity in the model. The log-binomial GLM allowed us to directly estimate prevalence ratios, which are more readily interpretable than odds ratios for this cross-sectional study with a relatively common outcome. The use of robust standard errors ensures valid statistical inferences in the presence of any violation of model assumptions.
Since the data had a potential hierarchical structure, we assessed it to determine if multilevel model analysis could be conducted by calculating the intra-class correlation (ICC) coefficient. However, the ICC coefficient was found to be only approximately 1.7%, which did not meet the minimum criterion for conducting multilevel analysis. Descriptive data were summarized using measures such as frequency count and proportion for categorical variables. To examine multicollinearity among the independent variables, a logistic regression was fitted using the variance inflation factor. The Hosmer and Lemeshow test were also used to evaluate the overall fitness of the final regression model. The statistical significance for the final model was set at p < 0.05.
Variables of the study
The outcome variable.
The outcome variable of this study was the comprehensive knowledge of PMTCT among women of reproductive age. This outcome was measured using two percentages: the percentage of women who were aware that HIV can be transmitted from mother to child during pregnancy, delivery, and breastfeeding, and in all three ways; and the percentage of women who knew that the risk of mother-to-child transmission can be reduced by the mother taking special drugs. Women who responded “Yes” to both questions were considered knowledgeable about PMTCT, whereas those who missed either of them were classified as not knowledgeable. The study population included all women of reproductive age, specifically those aged 15–49 years old, as determined by the IR file, and the time period was defined by the current status at the time of the survey interview. The outcome variable was subsequently recategorized as “Yes = 1” if the women knew the correct answers to both questions, and “No = 0” if they missed either of them. All classifications and analyses were conducted following the guidelines provided in the DHS statistics book [ 28 ].
The independent variables
Independent variables: Various maternal-related factors were included, such as maternal age, educational status, types of places of residence, marital status, household wealth index, current employment status, mass media exposure, ANC follow-up, place of delivery, number of health visits in the past 12 months, under-five children, contraceptive utilization, distance to the health facility, knowledge of HIV/AIDS, sex of the household head, country, and breastfeeding status.
Sociodemographic characteristics of the study participant
In this study, a total weighted sample of 133,724 women of reproductive age were enrolled in East African countries. Nearly half of them, 53,712 (40.17%), fell within the 15–24 years age group. In terms of marital status, approximately half of the mothers, 66,037 (49.38%), were married. Regarding place of residence, educational status, wealth index, place of delivery, and ANC follow-up, the majority of mothers, 97,636 (73.01%), 97,637 (46.81%), 34,309 (25.66%), 120,494 (90.11%), and 129,855 (97.11%), respectively, were from rural areas, had primary educational status, belonged to the richest households, opted for institutional delivery, and had at least one ANC follow-up during their pregnancies. Similarly, approximately 67,551 (50.52%) and 79,879 (59.73%) of women did not have access to any form of mass media exposure (such as radio, television, or magazines/newspapers) and were unemployed, respectively. However, more than half of the mothers, 88,376 (66.09%), and 51,509 (38.52%), did not utilize any contraceptive methods and reported facing challenges related to the distance to the health facility. Furthermore, around 107,992 (80.76%) participants had only one health facility visit per year, and 93,094 (69.62%) reported having male household heads (Table 2 ).
Knowledge of women about PMTCT of HIV/AIDS
The overall comprehensive knowledge of PMTCT of HIV/AIDS was about 79,447(59.41%). The transmission of HIV/AIDS during pregnancy 110,349(82.52%), during delivery 120,735(90.29%), during breastfeeding 119,955(89.70%), and about a special drug to avoid HIV during pregnancy 108,782(81.35%) was replied correctly (Table 3 ).
Factors associated with comprehensive knowledge of PMTCT of HIV/AIDS among women in East Africa
The adjusted prevalence ratio (APR) of having comprehensive knowledge about PMTCT of HIV increased by 1.09 times (APR = 1.09, 95% CI: 1.07, 1.11) and 1.05 times (APR = 1.05, 95% CI: 1.03, 1.08) among women aged 25–34 years and 35–49 years, respectively, compared to women aged 15–24 years. Similarly, compared to participants with no education, mothers who had completed primary education and secondary/higher education had higher prevalence ratios of being knowledgeable about PMTCT of HIV, with prevalence ratios of 1.08 (APR = 1.08, 95% CI: 1.05, 1.10) and 1.06 (APR = 1.06, 95% CI: 1.03, 1.13) respectively. Regarding the household wealth index, mothers from middle, richer, and richest households showed higher ratios of having comprehensive knowledge of PMTCT of HIV compared to mothers from the poorest households, with prevalence ratios of 1.06 (APR = 1.06, 95% CI: 1.02, 1.11), (APR = 1.09, 95% CI: 1.04, 1.13), and (APR = 1.08, 95% CI: 1.05, 1.11) respectively. The prevalence ratio of comprehensive knowledge about HIV were 1.04 times higher among employed mothers (APR = 1.04, 95% CI: 1.03, 1.06) compared to unemployed mothers. The ratios of knowledge about HIV among married and divorced/widowed women were (APR = 1.19, 95% CI: 1.15, 1.26) and (APR = 1.16, 95% CI: 1.14, 1.19) times higher, respectively, when compared to never married women. Women who gave birth at health institutions had 1.25 times higher ratios of (APR = 1.25, 95% CI: 1.23, 1.28) of being knowledgeable about PMTCT of HIV compared to those who gave birth at home. Moreover, women who had at least one ANC visit showed more comprehensive knowledge about PMTCT, with a prevalence ratio of 1.22 (95% CI: 1.17, 1.27) compared to those who did not have an ANC visit. On the other hand, regarding contraceptive method types, mothers who utilized traditional methods had 0.13 times lower ratios (APR = 0.87, 95% CI: 0.84, 0.91), while those who used modern methods had 1.09 times higher ratios (APR = 1.09, 95% CI: 1.07, 1.10), of being knowledgeable about PMTCT of HIV compared to mothers who did not use any type of contraceptives. Finally, women from rural areas showed less comprehensive knowledge about PMTCT, with a prevalence ratio of 0.98 (95% CI: 0.97, 0.99) compared to urban residential women (Table 4 ).
The purpose of this study was to examine comprehensive knowledge regarding HIV/AIDS transmission from mother to child, as well as its prevention and associated factors, among reproductive-age women in East Africa using recent DHS data. In this survey, about 59.41% of respondents were comprehensively knowledgeable with HIV/AIDS MTCT and its prevention. This result is lower than in previous studies conducted in Zimbabwe [ 16 ], Tanzania [ 29 ], and Nigeria [ 30 ]. However, our study’s findings are slightly higher than those of research conducted in SSA [ 19 ], Ethiopia [ 17 ], and Uganda [ 31 ]. Firstly, the disparity may be due to the fact that the study conducted a pooled analysis that included data from multiple East African countries. Since each country may have different contexts, healthcare systems, and population characteristics, the combined analysis might have introduced variations in the results. Secondly, differences in the study time, sample size, outcome ascertainment criteria, approach of analysis, and the study population could contribute to the observed disparity. These methodological variations can influence the findings and interpretations. For example, if the studies were conducted at different time points, there could have been changes in healthcare policies, interventions, or awareness campaigns that could impact the knowledge levels about the specific topic being studied. Additionally, differences in sample sizes, criteria for determining the outcome, analytical approaches, and characteristics of the study population (e.g., age groups, socioeconomic status) can all introduce variations in the results. Overall, the observed disparity in the findings may be due to a combination of factors related to the diverse nature of the pooled analysis, as well as differences in study methodology and population characteristics. These factors need to be considered when interpreting and comparing the results of studies conducted in different settings or at different time points. In the multiple logistic regression analysis, older age, attendance at primary and secondary school, coming from a wealthy family, marital status, at least one ANC follow-up, institutional delivery, and contraception use were associated with a higher likelihood of knowing about HIV/AIDS MTCT and prevention.
The study found that older age groups had higher ratios of knowing about MTCT of HIV/AIDS and its prophylaxis than younger age groups (women aged 15–24 years). This is consistent with research conducted in SSA, Ethiopia, and Zimbabwe [ 16 , 19 , 20 ]. This could be linked to older women’s proximity to various maternal health services during each consecutive pregnancy. Furthermore, this could imply that initiatives to support younger women (adolescents) in raising HIV awareness, reducing MTCT, and promoting ART adherence and viral suppression are insufficient [ 13 ]. As a result, more attention should be placed on HIV/AIDS and MTCT ideas for those young moms in order to prevent HIV transmission from mother to child. The study’s findings regarding the association between age groups and knowledge about MTCT of HIV/AIDS align with the Social Cognitive Theory (SCT) proposed by Bandura (1986) [ 32 ]. According to SCT, individuals acquire knowledge and behavior through observational learning and social interactions. In this context, older women’s higher ratios of knowing about MTCT and its prophylaxis could be attributed to their increased exposure to maternal health services, which provide opportunities for information exchange and learning from healthcare professionals. This finding supports the notion that access to healthcare services and exposure to educational interventions play a crucial role in knowledge acquisition and behavior change. Furthermore, the paragraph suggests that the lack of sufficient initiatives targeting younger women, particularly adolescents, raises questions about the effectiveness of current interventions based on the Theory of Planned Behavior (TPB). According to TPB, individuals’ attitudes, subjective norms, and perceived behavioral control influence their intentions and subsequent behaviors [ 33 ].
Similarly, when compared to uneducated participants, women with primary and secondary/higher educational attainment had significantly higher likelihood of being knowledgeable about HIV PMTCT. This is consistent with prior research done elsewhere SSA [ 19 ], and Ethiopia [ 15 , 20 , 34 ]. This could be because educated women have better access to health-related information and can grasp HIV/AIDS and associated MTCT. The findings regarding the association between educational attainment and knowledge about HIV PMTCT align with several theoretical perspectives. One such framework is the Health Belief Model (HBM), which suggests that individuals’ health-related beliefs and perceptions influence their adoption of preventive behaviors. In this context, educated women may have a higher level of perceived susceptibility to HIV/AIDS and recognize the significance of PMTCT knowledge in protecting their own health and that of their children [ 35 , 36 , 37 ]. Education can also enhance their perceived benefits of adopting preventive measures, such as adhering to antiretroviral therapy and practicing safe delivery methods, leading to a higher likelihood of being knowledgeable about PMTCT [ 35 ]. Furthermore, the findings resonate with the Diffusion of Innovations theory, which posits that knowledge and new ideas are more readily adopted by individuals with higher education levels [ 36 , 38 ].
In terms of the household wealth index, and employment status, the current study discovered that mothers from the middle, richer, and richest households were more likely to have comprehensive knowledge of HIV PMTCT than mothers from the worst household wealth index, and unemployed mothers respectively. This is consistent with research undertaken in SSA [ 19 ], Ethiopia [ 15 ], and Tanzania [ 39 ]. The higher degree of awareness among women from well-off households could be attributed to their easy access to maternal health services such as PMTCT programs and mass media exposure. Employed mothers may have more social interaction and independence than unemployed mothers.
In terms of marital status, married and divorced/widowed women were more educated about HIV PMTCT than never married women. Women who were married or divorced were more likely to have comprehensive understanding about MTCT and its eradication. This conclusion is similar with findings from Rwanda [ 40 ], Nigeria [ 41 , 42 ], and Ethiopia [ 15 , 43 ]. The most obvious explanation is that married and divorced women obtain health information at health care centers during ANC visits and related family planning services [ 15 ]. Women who gave birth in health facilities, those who used modern contraception, and those who had ANC follow-up during their pregnancy periods had a higher likelihood of understanding HIV PMTCT than their counterparts. This could be because women who have a history of ANC follow-up may have the opportunity to learn from health experts, and this information may improve women’s knowledge of PMTCT. Similarly, women with a history of institutional delivery and contemporary contraception use may be eligible for PMTCT services from health experts at a health facility. This finding is similar to the findings of an Ethiopian investigation [ 18 , 44 ].
Women from rural areas in developing countries and Sub-Saharan Africa tend to exhibit lower comprehensive knowledge about Prevention of Mother-to-Child Transmission (PMTCT) of HIV compared to urban residential women. Research indicates that various factors influence this disparity in PMTCT knowledge among women in different settings. Studies have shown that women with access to mass media, formal education, and occupation are more likely to have correct knowledge of MTCT and PMTCT [ 15 , 45 ]. Urban areas often provide better access to health information and education through media and workplaces, contributing to higher knowledge levels among urban women. Women’s decision-making power, wealth index, and occupation type play a significant role in their PMTCT knowledge [ 46 , 47 ]. Women with decision-making power, manual occupations, and higher wealth status are more likely to have better PMTCT knowledge.
Factors like ANC follow-up and utilization of maternal health services are associated with higher PMTCT knowledge among women [ 45 , 48 ]. Women who engage in ANC services have increased opportunities to learn about PMTCT from health professionals. Rural residents face challenges in accessing PMTCT services due to limited infrastructure and media coverage, contributing to lower knowledge levels compared to urban areas [ 45 , 48 ]. Efforts are needed to intensify health education and PMTCT services in rural and emerging regions.
This study relied on nationally representative data, as well as adequate statistical analysis and a large number of factors. As a result, it can assist policymakers, as well as governmental and non-governmental groups, in making appropriate actions. However, the study had certain shortcomings. First, because it was based on survey data, some characteristics that may be related with the outcome variable, such as the quality and availability of health care and knowledge about HIV/AIDS, were not addressed. Second, because it is based on survey data, we are unable to demonstrate the temporal relationship between the result variable and the independent variables that were included. Furthermore, we used DHS from the preceding ten years, and there may have been changes in MTCT and ART regimen awareness, as well as ART uptake before to and during pregnancy (Option B+) over time. As a result, due to time constraints, caution is advised when interpreting study findings.
Conclusions, and implications
The study findings reveal that HIV/AIDS MTCT and preventive knowledge among reproductive-age women in East Africa is rated as low. However, certain factors were identified to be associated with a higher likelihood of knowledge about MTCT of HIV/AIDS and its prevention. These factors include older age, attending primary and secondary school, coming from a wealthy family and rural areas, being married, having at least one antenatal care (ANC) follow-up, opting for institutional delivery, and using contraception.
These findings have important implications for addressing the knowledge gap and improving the prevention of HIV/AIDS MTCT among reproductive-age women in East Africa. The study highlights the need for targeted interventions and educational programs that focus on improving knowledge and awareness of HIV/AIDS transmission and prevention methods. Specifically, efforts should be directed towards younger women, those with limited education, and those from lower socioeconomic backgrounds, as they are more likely to have lower levels of knowledge.
Furthermore, the study underscores the importance of ANC utilization and institutional delivery, as these factors were associated with higher knowledge levels. Strengthening and expanding ANC services, particularly in terms of HIV/AIDS education and counseling, can enhance women’s understanding of MTCT and its prevention. Similarly, promoting contraception use among reproductive-age women can serve as an additional avenue to disseminate information on MTCT prevention.
Policy makers, healthcare providers, and public health practitioners in East Africa should consider incorporating these findings into their strategies and interventions. By addressing the identified factors and tailoring interventions to the specific needs of different subgroups, it is possible to improve knowledge levels, reduce stigma and discrimination, enhance health outcomes for mothers and children, and ultimately reduce the incidence of HIV/AIDS MTCT in the region. As a result, it is preferable to prioritize high-risk populations during the intervention in order to raise awareness about this critical public health issue and address its catastrophic consequences. Improving maternal-related services such as ANC, institutional delivery, and family planning are examples of good possibilities for women to have a more thorough understanding of HIV/AIDS vertical transmission.
Data availability
All data concerning this study are accommodated and presented in this document. The detailed data set can be freely accessible from the www.dhsprogram.com website.
HIV/AIDS JUNPo. UNAIDS Report on the Global AIDS Epidemic. Geneva. World Health Organization; 2012.
Piot P, Quinn TC. Response to the AIDS pandemic—a global health model. N Engl J Med. 2013;368(23):2210–8.
Article CAS PubMed PubMed Central Google Scholar
Granich R, Gupta S, Hersh B, Williams B, Montaner J, Young B, Zuniga JM. Trends in AIDS deaths, new infections and ART coverage in the top 30 countries with the highest AIDS mortality burden; 1990–2013. PLoS ONE. 2015;10(7):e0131353.
Article PubMed PubMed Central Google Scholar
Organization WH. United Nations Programe on HIV/AIDS. Initiating second generation HIV surveillance systems: practical guidelines Ginebra. WHOS/UNAIDS; 2006.
Schouten EJ, Jahn A, Midiani D, Makombe SD, Mnthambala A, Chirwa Z, et al. Prevention of mother-to-child transmission of HIV and the health-related Millennium Development Goals: time for a public health approach. Lancet. 2011;378(9787):282–4.
Article PubMed Google Scholar
HIV JUNPo. World AIDS Day Report 2022: dangerous inequalities. UN; 2022.
Services UDHH. HIV and AIDS global statistics:The Global HIV and AIDS Epidemic: https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics/ . 2023.
USAIDS, THE PATH THAT ENDS. AIDS 2023 USAIDS Global AIDS Update: https://www.unaids.org/en . 2023.
Gelaw YA, Magalhães RJS, Assefa Y, Williams G. Spatial clustering and socio-demographic determinants of HIV infection in Ethiopia, 2015–2017. Int J Infect Dis. 2019;82:33–9.
Safer WHODMP, Organization WH. Counselling for maternal and newborn health care: a handbook for building skills. World Health Organization; 2010.
UNAIDS, Global HIV. & AIDS statistics — Fact sheet: https://www.unaids.org/en/resources/fact-sheet . 2023.
UNAIDS, Global HIV. & AIDS statistics — Fact sheet 2023: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf . 2023.
UNAIDS. Start Free stay free AIDS Free—2017 progress report. Switzerland: UNAIDS Geneva; 2017.
Google Scholar
UNAIDS G. IN DANGER: Global AIDS Update 2022: Joint United Nations Programme on HIV/ AIDS. 2022: https://www.unaids.org/en/resources/documents/2022/in-danger-global-aids-update . 2022.
Luba TR, Feng Z, Gebremedhin SA, Erena AN, Nasser AM, Bishwajit G, Tang S. Knowledge about mother–to–child transmission of HIV, its prevention and associated factors among Ethiopian women. J Global Health. 2017;7(2).
Masaka A, Dikeleko P, Moleta K, David M, Kaisara T, Rampheletswe F, Rwegerera GM. Determinants of comprehensive knowledge of mother to child transmission (MTCT) of HIV and its prevention among Zimbabwean women: analysis of 2015 Zimbabwe demographic and Health Survey. Alexandria J Med. 2019;55(1):68–75.
Article Google Scholar
Alemu YM, Habtewold TD, Alemu SM. Mother’s knowledge on prevention of mother-to-child transmission of HIV, Ethiopia: a cross sectional study. PLoS ONE. 2018;13(9):e0203043.
Liyeh TM, Cherkose EA, Limenih MA, Yimer TS, Tebeje HD. Knowledge of prevention of mother to child transmission of HIV among women of reproductive age group and associated factors at Mecha district, Northwest Ethiopia. BMC Res Notes. 2020;13(1):1–6.
Teshale AB, Tessema ZT, Alem AZ, Yeshaw Y, Liyew AM, Alamneh TS, et al. Knowledge about mother to child transmission of HIV/AIDS, its prevention and associated factors among reproductive-age women in sub-saharan Africa: evidence from 33 countries recent demographic and health surveys. PLoS ONE. 2021;16(6):e0253164.
Terefe B, Techane MA, Assimamaw NT. Comprehensive knowledge, attitudes, behaviors, and associated factors of HIV/AIDS in Gondar City Public Health Facilities Among HIV Testing and Counselling Service Users, Northwest Ethiopia, 2022; an ordinal logistic regression analysis. HIV/AIDS-Research and Palliative Care. 2023:713 – 26.
Nyarko V, Pencille L, Akoku DA, Tarkang EE. Knowledge, attitudes and practices regarding the prevention of mother-to-child transmission of HIV among pregnant women in the Bosome Freho District in the Ashanti region of Ghana: a descriptive cross-sectional design. PAMJ-Clinical Med. 2019;1(69).
Mukhtar M, Quansar R, Bhat SN, Khan S. Knowledge, attitude and practice regarding mother-to-child transmission of HIV, its prevention, and associated factors among antenatal women attending a health care facility in district Srinagar, North India: a cross sectional study. Int J Community Med Public Health. 2020;7(7):2622.
Abebe AM, Kassaw MW, Shewangashaw NE. Level of knowledge about prevention of mother-to-child transmission of HIV option B + and associated factors among ANC clients in Kombolcha Town, South Wollo Amhara Regional State, Ethiopia, 2017. HIV/AIDS-Research and Palliative Care. 2020:79–86.
Abiodun MO, Munir’deen AI, Aboyeji PA. Awareness and knowledge of mother-to-child transmission of HIV among pregnant women. J Natl Med Assoc. 2007;99(7):758.
PubMed PubMed Central Google Scholar
Terefe B, Mekonnen BA, Tamir TT, Assimamaw NT, Limenih MA. Evaluation of Quality of Prevention of Mother to Child Transmission of HIV Service Provision and its determinants: the case of Health Facility readiness and mothers’ perspectives. J Multidisciplinary Healthc. 2024:93–110.
Terefe B, Jembere MM. Discrimination against HIV/AIDS patients and associated factors among women in east African countries: using the most recent DHS data (2015–2022). J Health Popul Nutr. 2024;43(1):3.
Elkasabi M. Sampling and Weighting with DHS Data: https://blog.dhsprogram.com/sampling-weighting-at-dhs/ . 2015.
Croft T, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S, et al. Guide to DHS statistics: DHS-7 (version 2). Rockville, MD: ICF; 2020.
Wangwe P, Nyasinde M, Charles D. Counselling at primary health facilities and level of knowledge of antenatal attendees and their attitude on prevention of mother to child transmission of HIV in Dar-Es Salaam, Tanzania. Afr Health Sci. 2013;13(4):914–9.
Ashimi A, Omole-Ohonsi A, Amole T, Ugwa E. Pregnant women’s knowledge and attitude to mother to child transmission of human immuno-deficiency virus in a rural community in Northwest Nigeria. West Afr J Med. 2014;33(1):68–73.
CAS PubMed Google Scholar
Byamugisha R, Tumwine JK, Ndeezi G, Karamagi CA, Tylleskär T. Attitudes to routine HIV counselling and testing, and knowledge about prevention of mother to child transmission of HIV in eastern Uganda: a cross-sectional survey among antenatal attendees. J Int AIDS Soc. 2010;13(1):1–11.
Bandura A. Social foundations of thought and action. Englewood Cliffs NJ. 1986;1986:23–8.
Conner M, Armitage CJ. Extending the theory of planned behavior: a review and avenues for further research. J Appl Soc Psychol. 1998;28(15):1429–64.
Malaju MT, Alene GD. Determinant factors of pregnant mothers’ knowledge on mother to child transmission of HIV and its prevention in Gondar town, North West Ethiopia. BMC Pregnancy Childbirth. 2012;12(1):1–7.
Strecher VJ, Champion VL, Rosenstock IM. The health belief model and health behavior. 1997.
Jeihooni AK, Arameshfard S, Hatami M, Mansourian M, Kashfi SH, Rastegarimehr B, et al. The effect of educational program based on health belief model about HIV/AIDS among high school students. Int J Pediatrics-Mashhad. 2018;6(3):7285–96.
Tarkang EE, Zotor FB. Application of the health belief model (HBM) in HIV prevention: a literature review. Cent Afr J Public Health. 2015;1(1):1–8.
Bertrand JT. Diffusion of innovations and HIV/AIDS. J Health Communication. 2004;9(S1):113–21.
Haile ZT, Teweldeberhan AK, Chertok IR. Correlates of women’s knowledge of mother-to-child transmission of HIV and its prevention in Tanzania: a population-based study. AIDS Care. 2016;28(1):70–8.
Deynu M, Nutor JJ. Determinants of comprehensive knowledge on mother-to-child transmission of HIV and its prevention among childbearing women in Rwanda: insights from the 2020 Rwandan demographic and Health Survey. BMC Public Health. 2023;23(1):1–14.
Olopha PO, Fasoranbaku AO, Gayawan E. Spatial pattern and determinants of sufficient knowledge of mother to child transmission of HIV and its prevention among Nigerian women. PLoS ONE. 2021;16(6):e0253705.
Olugbenga-Bello A, Adebimpe W, Osundina F, Abdulsalam S. Perception on prevention of mother-to-child-transmission (PMTCT) of HIV among women of reproductive age group in Osogbo, Southwestern Nigeria. Int J Women’s Health. 2013:399–405.
Abtew S, Awoke W, Asrat A. Knowledge of pregnant women on mother-to-child transmission of HIV, its prevention, and associated factors in Assosa town, Northwest Ethiopia. HIV/AIDS-Research and Palliative Care. 2016:101-7.
Abajobir AA, Zeleke AB. Knowledge, attitude, practice and factors associated with prevention of mother-to-child transmission of HIV/AIDS among pregnant mothers attending antenatal clinic in Hawassa referral hospital, South Ethiopia. J Aids Clin Res. 2013;4(6):2–7.
Liyeh TM, Cherkose EA, Limenih MA, Yimer TS, Tebeje HD. Knowledge of prevention of mother to child transmission of HIV among women of reproductive age group and associated factors at Mecha district, Northwest Ethiopia. BMC Res Notes. 2020;13:1–6.
Zegeye B, Ahinkorah BO, Ameyaw EK, Seidu A-A, Olorunsaiye CZ, Yaya S. Women’s decision-making power and knowledge of prevention of mother to child transmission of HIV in sub-saharan Africa. BMC Womens Health. 2022;22(1):115.
Sama C-B, Feteh VF, Tindong M, Tanyi JT, Bihle NM, Angwafo FF III. Prevalence of maternal HIV infection and knowledge on mother–to–child transmission of HIV and its prevention among antenatal care attendees in a rural area in northwest Cameroon. PLoS ONE. 2017;12(2):e0172102.
Deynu M, Nutor JJ. Determinants of comprehensive knowledge on mother-to-child transmission of HIV and its prevention among childbearing women in Rwanda: insights from the 2020 Rwandan demographic and Health Survey. BMC Public Health. 2023;23(1):5.
Download references
Acknowledgements
We would like to acknowledge the DHS program for providing permission for this study following research ethics.
This study was not supported financially by anyone.
Author information
Authors and affiliations.
Department of Community Health Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Bewuketu Terefe
Department of Emergency and Critical Care Nursing, School of Nursing, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Mahlet Moges Jembere & Bikis Liyew
You can also search for this author in PubMed Google Scholar
Contributions
BT was involved in conceptualization, design, data extraction, statistical analysis, language editing, and original manuscript writing. MMJ reviewed the study’s design and the draft manuscript, checked the analysis, and made a significant contribution. BL data interpretation, data curation, article review, and validation, critical revision for intellectual substance, and article review. The authors approved the final version of the manuscript.
Corresponding author
Correspondence to Bewuketu Terefe .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted after obtaining a permission letter from www.dhsprogram.com on an online request to access East African DHS data after reviewing the submitted brief descriptions of the survey to the DHS program. The datasets were treated with the utmost confidence. This study was done based on secondary data from East Africa DHS. Issues related to informed consent, confidentiality, anonymity, and privacy of the study participants are already done ethically by the DHS office. We did not manipulate and apply the microdata other than in this study. There was no patient or public involvement in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Terefe, B., Jembere, M.M. & Liyew, B. Comprehensive knowledge of mother-to-child HIV/AIDS transmission, prevention, and associated factors among reproductive-age women in East Africa: insights from recent demographic and national health surveys. BMC Women's Health 24 , 318 (2024). https://doi.org/10.1186/s12905-024-03173-1
Download citation
Received : 26 August 2023
Accepted : 29 May 2024
Published : 01 June 2024
DOI : https://doi.org/10.1186/s12905-024-03173-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Comprehensive knowledge
- Mother-to-child transmission
- HIV/AIDS prevention
- Reproductive-age women
- East Africa
- Associated factors
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Systematic Review
- Open access
- Published: 03 June 2024
Precancerous cervical lesion and associated factors among HIV-infected women in Ethiopia: systematic review and meta- analysis
- Yeshiwas Ayale Ferede 1 ,
- Worku Chekol Tassew 2 &
- Agerie Mengistie Zeleke 3
BMC Cancer volume 24 , Article number: 678 ( 2024 ) Cite this article
74 Accesses
Metrics details
Despite several preventative and control measures Ethiopia continues to see an increase in cervical cancer. Comprehensive evidence is very important to suggest ministry of health. Therefore, the aim of this study is to estimate the pooled violence of Precancerous Cervical Lesion and to identify associated factors among women living with HIV AIDS in Ethiopia.
From February 15, 2024 to March 17, 2024, systematic and methodical search of the literature was conducted using electronic databases such as PubMed, HINARI, Global Health, Scopus, EMBASE, Web of Science, African Journal online (AJOL), and Google Scholar. Quality appraisal was assessed based on Joanna Briggs Institute (JBI) critical appraisal checklist for analytical cross-sectional study using 9 criteria. The Cochrane Q and I2 test statistics were used to verify the heterogeneity of the studies. Using a fixed effect model, the pooled estimate prevalence of precancerous cervical lesion among women living with HIV was calculated.
After reviewing 9,470 studies, 9 studies involving 2,910 women with HIV were included. The pooled estimate of precancerous cervical cancer among women living with HIV in Ethiopia was 15.34% (95% CI: 8.97, 21.72). Having history of sexual infection (POR = 3.12; 95% CI: 1.38, 7.05), having multiple sexual partner (POR = 3.14; 95% CI: 2.29, 4.30), and parity greater than two (POR = 4.97; 95% CI: 3.17, 7.78) were identified factors associated with precancerous cervical lesion.
This study found that about one-six of HIV-positive women developed precancerous cervical lesion. According to this study, there was a substantial correlation between precancerous cervical lesion among HIV-positive women and having history of sexually transmitted infection, having multiple sexual partners, and being multipara. In order to reduce precancerous cervical lesion, FMOH, policy makers, and interested parties should pay particular attention to this issue.
Peer Review reports
Keywords prevalence, cervical lesion, associated factors, HIV –positive women, Ethiopia, systematic review and meta-analysis.
Cervical cancer is the fourth most common cancer in women globally with around 660 000 new cases and around 350 000 deaths in 2022 [ 1 ]. Nonetheless, approximately 90% of cervical cancer deaths occur in poorer nations, making it the fourth most common cause of cancer-related deaths among women worldwide. Approximately 22% of cervical cancer cases worldwide are in sub-Saharan Africa [ 2 , 3 , 4 ]. By 2030, 443,000 deaths are predicted, a 67% increase in the current number of deaths [ 5 ]. An estimated 5000 people in Ethiopia pass away from cervical cancer each year, along with 7000 new cases [ 6 ].
A disproportionate lack of screening is the main cause of the high incidence of cervical cancer in sub-Saharan Africa, some regions of Latin America and the Caribbean, and other medically underserved groups [ 4 ]. Sexually transmitted infections such as human papillomavirus (HPV) are linked to a higher prevalence of HIV infection, particularly in sub-Saharan Africa [ 7 , 8 , 9 , 10 ]. Women who are HIV-positive face an increased risk of acquiring human papillomavirus (HPV), especially when their CD4 + cell count is low. The use of antiretroviral therapy (ART) has been shown to decrease the likelihood of HPV acquisition, increase the body’s ability to clear the virus, and decrease the progression to precancerous stages. This effect is likely due to the restoration of the immune system’s functionality [ 11 ]. In Ethiopia, HPV-related risk factors for cervical cancer include cultural factors, poverty, coinfection, and lack of awareness [ 12 ]. Moreover, Ethiopian women usually seek cancer care at a late stage of the disease, when therapy is probably ineffective, and there is no uniform strategy or methodology for cervical cancer screening; instead, it is patchy or inconsistent [ 6 ].
Cervical cancer-related morbidities and deaths are considerably reduced when high-risk and vulnerable groups are screened for asymptomatic precancerous cervical lesions [ 13 ]. In Ethiopia, cervical cancer is a serious concern, especially since 99% of HIV + women undergo a Visual Inspection Acetic acid(VIA) test [ 14 ]. To fulfill the 2020 aim of screening at least 80% of women aged 30–49 years, a precancerous cervical lesion (PCCL) screening program has been established [ 15 ]. Despite several preventative and control measures, there is a continuing increase in the incidence of Ethiopia among patients with cervical cancer. The 2016 Ethiopian Demographic Health Survey (EDHS) revealed that 1.2% of women between the ages of 15 and 49 had HIV/AIDS [ 16 ]. A total of 534,000 Ethiopian women who were 15 years of age or older with HIV were included. Due to their tenfold increased risk of precancerous lesions and increased likelihood of developing invasive cervical cancer compared to those of uninfected women, these women are among the most susceptible to the disease [ 10 , 14 ]. According to WHO guidelines, all sexually active women between the ages of 30 and 49 years should undergo cervical cancer screening at least once every five years. However, HIV-positive women of any age should undergo screening every three years [ 2 ]. Ethiopia embraced the WHO recommendation in 2015, advising HIV-positive women to start screening as soon as they receive their diagnosis, regardless of age, and to rescreen every five years [ 14 ]. The government of Ethiopia has increased its focus on early detection programs. Various stakeholders, including professionals, academics, the media, and development partners, have launched several advocacy campaigns to combat cervical cancer [ 14 ].
In this study, the literature on precancerous cervical lesions among women living with HIV AIDS in Ethiopia was reviewed. However, studies have shown differences in precancerous cervical lesions and associated factors, and to the knowledge of the investigator concerned, the literature has not been systematically examined. Therefore, this systematic review and meta-analysis aimed to estimate the pooled incidence of cancer involving cervical lesions and to identify associated factors among women living with HIV-AIDS in Ethiopia. The findings of this meta-analysis will help policy makers and other stakeholders effectively implement the prevention and control of precancerous cervical lesions.
Materials and methods
This systematic review and meta-analysis was performed based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [ 17 ].

Search strategy
A thorough and methodical review of the literature was conducted across various electronic databases, such as PubMed, HINARI, Global Health, Scopus, EMBASE, Web of Science, African Journal Online (AJOL), and Google Scholar, spanning from February 15, 2024, to March 17, 2024. Additionally, manual searches were performed across different repositories to identify unpublished studies and gray literature. The search utilized a combination of keywords and Medical Subject Headings (MeSH) terms. Specifically, the search strategy included the following terms: “precancerous” (MeSH), “cervical lesion”, “Cervical Intraepithelial Neoplasia” (MeSH), “factors”, “Determinants” (MeSH), “HIV-positive”, “HIV Seropositivity” (MeSH), “women” (MeSH), and “Ethiopia” (MeSH). Boolean operators (AND, OR), truncation, and appropriate application of MeSH terms were employed in the systematic search. The focus was on identifying epidemiological studies concerning precancerous cervical lesions and their associated factors among HIV-positive women in Ethiopia.
Inclusion and exclusion criteria
Original research studies reporting on precancerous cervical lesions and/or associated factors among HIV-positive women in Ethiopia were included in the study. Both published and unpublished articles written only in the English language were considered for inclusion. All publications reported up to March 17, 2024, were considered. Studies that did not clearly report precancerous cervical lesions among HIV-positive women in Ethiopia were excluded. In addition, articles without full texts, abstracts, editorial reports, letters, reviews, and commentaries were excluded from the study.
Data extraction
Following the screening of titles, abstracts, and full texts of each selected original study, data extraction was carried out using a standardized tool adapted from the Joanna Briggs Institute (JBI). Two independent reviewers (YAF & AMZ) performed the data extraction process and thoroughly reviewed all included articles. Any disagreements between the reviewers were resolved through discussion. Various study characteristics, including the first author’s name, study region, publication year, study design, participants, sampling technique, and sample size, were extracted. Additionally, the prevalence of precancerous cervical lesions and associated risk factors, along with their corresponding 95% confidence intervals, were also extracted.
Risk of bias (quality) assessment
The assessment of study quality was conducted using the Joanna Briggs Institute (JBI) critical appraisal checklist for analytical cross-sectional studies, which comprises nine criteria [ 18 ]. These criteria included [ 1 ] appropriateness of the sample frame for addressing the target population [ 2 ], appropriateness of participant sampling [ 3 ], adequacy of sample size [ 4 ], detailed description of study subjects and setting [ 5 ], thoroughness of data analysis covering the identified sample [ 6 ], utilization of valid methods for condition identification [ 7 ], measurement of the condition in a standardized and reliable manner for all participants [ 8 ], appropriate statistical analysis, and [ 9 ] adequacy of response rate. Each criterion was scored as 0 for ‘not reported or not appropriate’ and 1 for ‘yes’. The scores across these items were then aggregated to obtain a total quality score ranging from 0 to 9. Subsequently, studies were categorized as low, medium, or high quality based on the total points awarded: 0–4 for low quality, 5–7 for medium quality, and 7–9 for high quality.
Outcome measurement
This review focused on two main outcomes. The primary outcome addressed in this systematic review and meta-analysis pertains to precancerous cervical lesions. These lesions are characterized by dense acetowite areas with well-defined margins observed in proximity to the transformation zone or if the entire cervix or cervical growth turns white during VIA. Classification as negative, positive, or suspicious for invasive cervical cancer (ICC) followed the guidelines outlined in the International Agency for Research on Cancer (IARC) training manual [ 19 ].
The second outcome variable of interest in the study was the identification of factors associated with precancerous cervical lesions among HIV-positive women in Ethiopia, assessed in terms of the odds ratio (AOR). The odds ratio for each identified factor was calculated based on the binary outcome data reported in each primary study.
Data synthesis and analysis
The data extraction process involved utilizing a Microsoft Excel spreadsheet, followed by importing the data into STATA version 11 for subsequent analysis. To describe and summarize the primary studies, tables, figures, and forest plots were used. The pooled estimate of precancerous cervical lesions was calculated using a fixed-effects model, along with a 95% confidence interval (CI). For the assessment of factors associated with precancerous cervical lesions among HIV-positive women, associations were estimated using odds ratios with corresponding 95% CIs. A fixed-effects model was employed during the meta-analysis due to the demonstrated homogeneity among the included studies. The assessment of heterogeneity among the included studies was conducted using Cochran’s Q statistic and I² statistics. Additionally, visual inspection of asymmetry in funnel plots and Egger regression tests were performed, with a p value of less than 0.05 serving as the cutoff point to indicate the presence of publication bias.
Study selection
Out of a total of 9,470 articles retrieved regarding precancerous cervical lesions and/or associated factors among women living with HIV/AIDS in Ethiopia, 125 duplicates were identified and removed. Subsequently, 9,282 articles were excluded after their titles and abstracts were evaluated based on predetermined criteria. After the evaluation of the full texts of the remaining 63 articles against the qualifying criteria, 54 studies were further excluded, primarily because they were published outside of Ethiopia or because of differences in the study population. Consequently, nine studies met the inclusion criteria and were included in the final meta-analysis (Fig 1 ).

Flow chart of study selection for systematic review and meta-analysis of precancerous cervical lesion and associated factors among HIV-positive women in Ethiopia, 2024
Characteristics of the included studies
Of the included studies, eight were institutional-based and cross-sectional, and the remaining study was a case‒control study. All studies that were included in this evaluation were published between 2013 and 2023. Among the papers included in this review, four involved systematic sampling, one involved simple random sampling, one involved consecutive sampling, and the remaining three studies did not report the sampling technique used. There were 2,910 participants from an estimated 2,969 HIV-positive women, with an estimated sample size ranging from 129 [ 20 ] to 458 [ 21 ]. According to the included research, the prevalence of precancerous cervical lesions ranged from 7.5% [ 15 ] to 22.1% [ 21 ]. The Amhara area was the focus of five of the studies included in this review [ 9 , 20 , 22 , 23 , 24 ]; two investigations were conducted in the Southern Nations, Nationalities, and People’s Region (SNNPR) [ 21 , 25 ], and the remaining two were conducted in the Addis Ababa and Oromia Regions[ 15 , 26 ] Table 1 .
Meta-analysis
Risk of bias assessment for the included studies.
The critical evaluation checklist developed by the Joanna Briggs Institute (JBI) and adjusted for cross-sectional studies. The quality evaluation summary showed two-third ( n = 6, 66.66%) of the included studies had high quality while the remaining one-third ( n = 3, 33.33%) of studies had medium quality.
Precancerous cervical lesion
In this study, the pooled estimate of Precancerous cervical lesion among HIV-positive women was 15.34% (95% CI: 8.97, 21.72). In estimating the pooled prevalence of Precancerous cervical lesion among HIV-positive women homogeneity through the included studies was exhibited (I2 = 0.00%; p = 0.931). Therefore, a fixed effects model was used in the meta-analysis to calculate the pooled prevalence of Precancerous cervical lesion (Fig. 2 ).
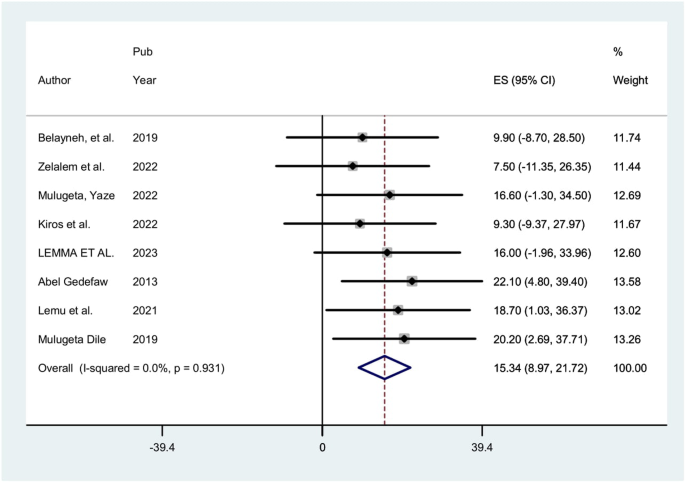
Forest plot of the pooled prevalence of precancerous cervical lesion among HIV-positive women in Ethiopia, 2024
Publication bias
To determine if publication bias existed, a visual examination of the asymmetry in funnel plots and Egger regression tests were used. As a consequence, the results of Egger’s tests and funnel plots indicated that publication bias existed in the included papers. Egger’s test revealed the existence of publication bias with a statistically significant result ( p = 0.000). Additionally, an examination of the funnel plots visually revealed an uneven distribution of the study (Fig. 3 ).

Showing publication bias using funnel plot, 2024
Trim and fill analysis
Because there is publication bias, Trim and fill analysis was done. Trim and fill analysis findings showed that one study was removed.
Associated factors
In this study, certain factors associated to precancerous cervical lesion were statistically pooled, but some weren’t since the independent variables were not evenly classified or grouped about the outcome, which is precancerous cervical lesion.
Eight studies indicated that having history sexually transmitted infection has a substantial correlation with precancerous cervical lesion. The odds of precancerous cervical lesion were 3.12 times (POR = 3.12; 95% CI: 1.38, 7.05) higher among Womens who had history sexually transmitted infection when compared with those who hadn’t history sexually transmitted infection. This meta-analysis revealed considerable heterogeneity among the included studies (I2 = 92.4%, P = 0.000). Thus, an analysis using a random effect model was employed (Fig. 4 ).

Showing the forest plot of the association between sexual transmitted infection and precancerous cervical lesion in Ethiopia, 2024
Four studies indicated that sexual partner has a substantial correlation with precancerous cervical lesion. The odds of precancerous cervical lesion were 3.14 times (POR = 3.14; 95% CI: 2.29, 4.30) higher among HIV positive women who had multiple sexual partner when compared with those hadn’t multiple sexual partner. The homogeneity of the included studies in this analysis was noted (I2 = 0.0%, P = 0.931). Thus, a fixed effect model analysis was applied (Fig. 5 ).

Showing the forest plot of the association life time sexual partner and precancerous cervical lesion in Ethiopia, 2024
Furthermore: Two studies indicated that parity has a substantial correlation with precancerous cervical lesion. The odds of precancerous cervical lesion were 4.97 times (POR = 4.97; 95% CI: 3.17, 7.78) higher among women whose parity greater than two when compared with those whose parity less than or equal two. Homogeneity was found in the analysis of the included studies (I2 = 0.0%, P = 0.973). Thus, an analysis using a fixed effect model was employed (Fig. 6 ).

Showing the forest plot of the association between parity and precancerous cervical lesion in Ethiopia, 2024
The purpose of this meta-analysis was to estimate the prevalence of precancerous cervical lesion nationwide and its associated factors. This meta-analysis, to the best of our knowledge, is the first of its type to calculate the pooled prevalence of precancerous cervical lesion and associated factors among women living with HIV in Ethiopian. According to this analysis, there is a broad range of precancerous cervical lesion among HIV-positive women from 7.5 to 22.1%. In Ethiopia, the pooled prevalence of precancerous cervical lesion among women living with HIV was 15.34% (95% CI: 8.97, 21.72). This finding strongly showed that being HIV-positive means at risk for developing a precancerous cervical lesion. The current study’s findings on precancerous cervical lesion among women living with HIV are in line with other Studies recently conducted in Côte d’Ivoire(11%) [ 27 ], however higher than the study conducted in Nigeria found that the prevalence of precancerous cervical cancer lesion to be 6% [ 28 ]. On the other hand, this study was lower than the studies conducted in Kenya (26.7%), Rwanda (24.3%), Uganda (73%), and Zambia (76%), in Sub-Saharan Africa.
25.6% [ 29 ], and South Africa (66.3%) [ 30 , 31 , 32 , 33 , 34 ], .
According to this study, women who had higher parity had a higher risk of precancerous cervical lesions. This finding is in line with the findings of earlier research carried out in Tanzania(33 and Côte d’Ivoire [ 35 ]. This is because frequent vaginal deliveries put the woman at risk of HPV infection by tearing of the vaginal wall, which allows for cross-contamination. On the other hand, study done in Rwandan found that the likelihood of getting a cervical cancer lesion declined as party number increased [ 36 ].
According to this study, women with a history of sexually transmitted infections (STIs) were 3.12 times more likely to develop a precancerous cervical lesion than women without a history of STIs. This finding is consistent with research from Uganda, which found that women without a history of STIs had a 76% lower risk of developing precancerous cervical lesions [ 37 ]. Most of the available data pointed to a viral infection as the primary cause of cervical cancer and suggested that the virus is transmitted through sex. For example, there is evidence linking the severity of aberrant cervical cytology and HPV infection to chlamydia trachomatis infection.
Furthermore, the current study discovered that women who had several sexual partners throughout the course of their lifetimes were 2.53 times more likely than women who had only one partner to acquire precancerous cervical lesions. This is because unprotected sexual contact is one method that HPV may spread, which could explain why women who have several sexual partners may be at a higher risk of contracting the virus [ 38 ]. Therefore, health practitioners who routinely care for HIV-positive women should prescribe the VIA test in addition to advising women to limit the number of sexual partners to lower the prevalence of PCCL.
This study showed that women with higher parity were more likely to have precancerous cervical lesion compared. This finding is consistent with the results from the previous studies conducted in Tanzania [ 39 ] and Côte d’Ivoire [ 35 ] This is due to repeated vaginal delivery might be exposed to human papillo virus strains (HPVs) infection due to vaginal wall laceration which is conducive for cross contamination. However, in contrast, another study done in Rwanda indicated the risk of developing any cervical cancerous lesion decreased with increasing party [ 36 ].
Despite being the first systematic review and meta-analysis on precancerous cervical lesion among Ethiopian women living with HIV, this study has many shortcomings. This meta-analysis includes full-text articles that were published only in English. The pooled odds ratio for all variables associated to precancerous cervical lesion among women living with HIV was not examined as the included studies had varying definitions of the variables. The facility-based nature of the cross-sectional research seen in all of the included articles that were considered may restrict the generalizability of the findings. Additionally, this analysis only included studies from four regions, which may affect the generalizability of the findings at the national level. Furthermore, the presence of publication bias is also another limitation of this meta-analysis.
Data availability
All relevant data generated and analyzed is included in this article.
Abbreviations
Pooled odd ratio
Adjusted odd ratio
Confidence intervals
Preferred Reporting Items for Systematic review and Meta-analysis
South Nation and Nationality Peoples Regional
Federal, Ministry, of Health
International Agency for Research on Cancer
Visual Inspection Acetic acid
Organization WH. Regional Office for the Western Pacific. Strategic framework for the comprehensive prevention and control of cervical cancer in the Western Pacific Region 2023–2030. WHO Regional Office for the Western Pacific; 2023.
Organization WH. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention: supplemental material: GRADE evidence-to-recommendation tables and evidence profiles for each recommendation. World Health Organization; 2013.
Begoihn M, Mathewos A, Aynalem A, Wondemagegnehu T, Moelle U, Gizaw M, et al. Cervical cancer in Ethiopia–predictors of advanced stage and prolonged time to diagnosis. Infect Agents cancer. 2019;14:1–7.
Article Google Scholar
Cecilia NC, Rosliza A, Suriani I. Global burden of cervical cancer: a literature review. Int J Public Health Clin Sci. 2017;4(2):10–8.
Google Scholar
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68(6):394–424.
Asseffa NA. Cervical cancer: Ethiopia’s outlook. J Gynecol Womens Health. 2017;5(2):555660.
Organization WH. Alcohol… use and abuse. What you should know. WHO Regional Office for South-East Asia; 2006. p. 9290222751.
Kassa RT. Risk factors associated with precancerous cervical lesion among women screened at Marie Stops Ethiopia, Adama town, Ethiopia 2017: a case control study. BMC Res Notes. 2018;11:1–5.
Belayneh T, Mitiku H, Weldegebreal F. Precancerous cervical lesion and associated factors among HIV-infected women on ART in Amhara Regional State, Ethiopia: a hospital-based cross-sectional study. Int J Health Sci. 2019;13(3):4.
Hailemariam T, Yohannes B, Aschenaki H, Mamaye E, Orkaido G, Seta M. Prevalence of cervical cancer and associated risk factors among women attending cervical cancer screening and diagnosis center at Yirgalem General Hospital, Southern Ethiopia. J Cancer Sci Ther. 2017;9(11):730–5.
Liu G, Sharma M, Tan N, Barnabas RV. HIV-positive women have higher risk of human papilloma virus infection, precancerous lesions, and cervical cancer. AIDS. 2018;32(6):795–808.
Article PubMed Google Scholar
Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Global Health. 2020;8(2):e191–203.
Organization WH. Strategic framework for the comprehensive prevention and control of cervical cancer in the Western Pacific Region 2023–2030. 2023.
Gelibo T, Roets L, Getachew T, Bekele A. Coverage and factors associated with cervical cancer screening: results from a population-based WHO steps study in Ethiopia. Adv Oncol Res Treat. 2017;1(115):2.
Zelalem W, Weldegebreal F, Ayele BH, Deressa A, Debella A, Eyeberu A, et al. Precancerous cervical lesion among adult women with human immune deficiency virus on anti retroviral therapy at Saint Peter specialized hospital, Ethiopia: a hospital-based cross-sectional study. Front Oncol. 2022;12:910915.
Article PubMed PubMed Central Google Scholar
CSA I. Ethiopia demographic and health survey: key indicators report. Ethiopia: Central Statistical Agency, Addis Ababa; 2016.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Omura M, Maguire J, Levett-Jones T, Stone TE. The effectiveness of assertiveness communication training programs for healthcare professionals and students: a systematic review. Int J Nurs Stud. 2017;76:120–8.
Chamot E, Kristensen S, Stringer JS, Mwanahamuntu MH. Are treatments for cervical precancerous lesions in less-developed countries safe enough to promote scaling-up of cervical screening programs? A systematic review. BMC Womens Health. 2010;10:1–11.
Kiros M, Mesfin Belay D, Getu S, Hailemichael W, Esmael A, Andualem H et al. Prevalence and Determinants of Pre-Cancerous Cervical Lesion and Human Papillomavirus Among HIV-Infected and HIV-Uninfected Women in North-West Ethiopia: A Comparative Retrospective Cross-Sectional Study. HIV/AIDS-Research and Palliative Care. 2021:719 – 25.
Gedefaw A, Astatkie A, Tessema GA. The prevalence of precancerous cervical cancer lesion among HIV-infected women in southern Ethiopia: a cross-sectional study. PLoS ONE. 2013;8(12):e84519.
Mulugeta Y. Prevalance and Associated factors of pre-cancerous cervical lesion among hiv-infected and hiv-uninfected women at Health institutions in Bahir Dar City, North West, Ethiopia/2022 2022.
Dessie TM, Kassaw AT, Alen GD. Determinants of precancerous cervical lesion among HIV infected women on ART in Woldia comprehensive specialized hospital NorthEast Ethiopia. BMC Womens Health. 2023;23(1):458.
Bagriansky J, Champa N, Pak K, Whitney S, Laillou A. The economic consequences of malnutrition in Cambodia, more than 400 million US dollar lost annually. Asia Pac J Clin Nutr. 2014;23(4):524–31.
PubMed Google Scholar
Lemu LG, Woldu BF, Teke NE, Bogale ND, Wondimenew EA. Precancerous cervical lesions among HIV-Infected women attending HIV Care and Treatment clinics in Southwest Ethiopia: a cross-sectional study. Int J Women’s Health. 2021:297–303.
Lemma TM, Bala ET, Hordofa MA, Solbana LK. Precancerous cervical lesions and associated factors among women on antiretroviral therapy at Dukem Health Center, Central Ethiopia: a cross-sectional study. Health Sci Rep. 2024;7(3):e1972.
Anderson J, Lu E, Harris M, Kibwana S, Estep D, Varallo J, et al. editors. Initial Results from a Multi-country Cervical Cancer Screening Program for HIV + Women. Proceedings of the 18th Conference on Retroviruses and Opportunistic Infections: 27 February-2 March 2011 Boston, MA; 2011.
Ononogbu U, Almujtaba M, Modibbo F, Lawal I, Offiong R, Olaniyan O, et al. Cervical cancer risk factors among HIV-infected Nigerian women. BMC Public Health. 2013;13:1–10.
Weldegebreal F, Worku T. Precancerous cervical lesion among HIV-positive women in Sub-saharan Africa: a systematic review and meta-analysis. Cancer Control. 2019;26(1):1073274819845872.
Moodley JR, Constant D, Hoffman M, Salimo A, Allan B, Rybicki E, et al. Human papillomavirus prevalence, viral load and pre-cancerous lesions of the cervix in women initiating highly active antiretroviral therapy in South Africa: a cross-sectional study. BMC Cancer. 2009;9:1–8.
Blossom D, Beigi R, Farrell J, Mackay W, Qadadri B, Brown D, et al. Human papillomavirus genotypes associated with cervical cytologic abnormalities and HIV infection in Ugandan women. J Med Virol. 2007;79(6):758–65.
Article CAS PubMed PubMed Central Google Scholar
Parham GP, Sahasrabuddhe VV, Mwanahamuntu MH, Shepherd BE, Hicks ML, Stringer EM, et al. Prevalence and predictors of squamous intraepithelial lesions of the cervix in HIV-infected women in Lusaka, Zambia. Gynecol Oncol. 2006;103(3):1017–22.
Memiah P, Mbuthia W, Kiiru G, Agbor S, Odhiambo F, Ojoo S et al. Prevalence and risk factors associated with precancerous cervical cancer lesions among HIV-infected women in resource-limited settings. AIDS research and treatment. 2012;2012.
Leroy V, Ladner J, De Clercq A, Meheus A, Nyiraziraje M, Karita E, et al. Cervical dysplasia and HIV type 1 infection in African pregnant women: a cross sectional study, Kigali, Rwanda. The pregnancy and HIV Study Group (EGE). Sex Transm Infect. 1999;75(2):103–6.
Adjorlolo-Johnson G, Unger ER, Boni-Ouattara E, Touré-Coulibaly K, Maurice C, Vernon SD, et al. Assessing the relationship between HIV infection and cervical cancer in Cote d’Ivoire: a case-control study. BMC Infect Dis. 2010;10:1–8.
Makuza JD, Nsanzimana S, Muhimpundu MA, Pace LE, Ntaganira J, Riedel DJ. Prevalence and risk factors for cervical cancer and pre-cancerous lesions in Rwanda. Pan Afr Med J. 2015;22(1).
Izudi J, Adrawa N, Amongin D. Precancerous cervix in human immunodeficiency virus infected women thirty years old and above in Northern Uganda. Journal of oncology. 2016;2016.
Megersa T, Dango S, Kumsa K, Lemma K, Lencha B. Prevalence of high-risk human papillomavirus infections and associated factors among women living with HIV in Shashemene town public health facilities, Southern Ethiopia. BMC Womens Health. 2023;23(1):125.
Liu E, McCree R, Mtisi E, Fawzi WW, Aris E, Lema IA, et al. Prevalence and risk factors of cervical squamous intraepithelial lesions among HIV-infected women in Dar Es Salaam, Tanzania. Int J STD AIDS. 2016;27(3):219–25.
Article CAS PubMed Google Scholar
Download references
Acknowledgements
The authors would like to thank the authors of the included primary studies, which used as source of information to conduct this study.
The authors received no specific funding for this work.
Author information
Authors and affiliations.
Department of Reproductive Health, Teda Health Science College, Gondar, Ethiopia
Yeshiwas Ayale Ferede
Department of Medical Nursing, Teda Health Science College, Gondar, Ethiopia
Worku Chekol Tassew
Department of Clinical Midwifery, Teda Health Science College, Gondar, Ethiopia
Agerie Mengistie Zeleke
You can also search for this author in PubMed Google Scholar
Contributions
YAF: Conceptualization, Formal analysis, Investigation, Methodology, Visualization. WCT: Methodology, Supervision, Writing – original draft, Writing – review & editing AMZ: Formal analysis, Supervision, Writing – original draft, Writing – review & editing.
Corresponding author
Correspondence to Yeshiwas Ayale Ferede .
Ethics declarations
Ethical approval and consent to participate.
Ethical approval not applicable.
Consent for publication
Not applicable.
Informed consent
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ferede, Y.A., Tassew, W.C. & Zeleke, A.M. Precancerous cervical lesion and associated factors among HIV-infected women in Ethiopia: systematic review and meta- analysis. BMC Cancer 24 , 678 (2024). https://doi.org/10.1186/s12885-024-12462-9
Download citation
Received : 22 March 2024
Accepted : 31 May 2024
Published : 03 June 2024
DOI : https://doi.org/10.1186/s12885-024-12462-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10612072

Prevention and Control Are Not a Regional Matter: A Spatial Correlation and Molecular Linkage Analysis Based on Newly Reported HIV/AIDS Patients in 2021 in Jiangsu, China
1 Key Laboratory of Environmental Medicine Engineering of Ministry of Education, Department of Epidemiology and Health Statistics, School of Public Health, Southeast University, Nanjing 210009, China; nc.ude.ues@380932032 (D.Y.); nc.ude.ues@307322022 (S.L.); nc.ude.ues@169312022 (F.O.)
Shanshan Liu
2 School of Public Health, Nanjing Medical University, Nanjing 211166, China; nc.ude.umjn.uts@7630111202
3 Department of HIV/STD Control and Prevention, Jiangsu Provincial Center for Disease Control and Prevention, Nanjing 210009, China; nc.cdcsj@negnilihs (L.S.); nc.cdcsj@yxuil (X.L.); nc.cdcsj@oatuiq (T.Q.)
Xiaoyan Liu
Associated data.
All publicly available data for this study are included in the content, and some data are provided in the Supplementary Materials .
HIV-related spatial analysis studies in China are relatively few, and Jiangsu Province has not reported the relevant data in recent years. To describe the spatial distribution and molecular linkage characteristics of HIV-infected patients, this article combined descriptive epidemiology, spatial analysis, and molecular epidemiology methods to analyze patient reporting, patient mobility information, and HIV sequence information simultaneously. The results showed that HIV reporting profiles differed among Jiangsu cities, with the reporting rate in southern Jiangsu being above average. There was a spatial autocorrelation (Global Moran I = 0.5426, p < 0.05), with Chang Zhou showing a High–High aggregation pattern. Chang Zhou and Wu Xi were identified as hotspots for HIV reporting and access to molecular transmission networks. Some infected individuals still showed cross-city or even cross-province mobility after diagnosis, and three were linked with individuals in the destination cities within the largest molecular transmission cluster, involving 196 patients. The cross-city or cross-province mobility of patients may result in a potential HIV transmission risk, suggesting that combining timely social network surveys, building an extensive transmission network across cities and provinces, and taking critical regions and key populations as entry points could contribute to improved prevention and control efficiency and promote achievement of the 95-95-95 target and cascade.
1. Introduction
In 2022, there were around 1.3 million new HIV infections globally. The 95-95-95 testing and treatment cascade, which aims to ensure that 95% of people living with HIV know their HIV status, 95% of all people living with HIV are accessing treatment, and 95% of all people living with HIV have suppressed viral loads, had been achieved at rates of 86%, 76%, and 71% [ 1 ]. These rates were slightly lower in Asia and the Pacific region, including China, at 78%, 65%, and 62% [ 2 ], respectively. Despite previous surveys indicating that Yunnan, Sichuan, and Chongqing were the areas most severely affected by the HIV epidemic in China [ 3 ], Jiangsu Province, which is located in the eastern region of China, has reported a high level of new cases due to its developed economy, convenient transportation, large jurisdictional span, proximity to several neighboring provinces, and frequent movement of people. From January to October 2022, Jiangsu reported 3677 new HIV cases [ 4 ], a decrease of only 2.1% compared with the same period in the previous year [ 5 ], and lower than the 16.7% national decline reported at the 8th National Academic AIDS Conference.
HIV, similar to other infectious diseases, exhibits spatial distribution characteristics that are closely related to geographical factors, affecting both its transmission and prevalence. However, previous studies have mainly focused on descriptive analysis of epidemic trends or infection characteristics from a temporal perspective, neglecting the spatial information and failing to comprehensively understand the disease and its impact on different regions and populations. Spatial analysis can fully utilize the spatial information in disease data, so it is widely used in describing the spatial distribution characteristics and changing trends of diseases, and in disease surveillance, evaluation of intervention effects, and exploratory analysis of influencing factors [ 6 , 7 , 8 ].
The HIV transmission network can be categorized into social and molecular networks. The social network includes confirmed HIV-infected persons, undiagnosed HIV-infected persons, and high-risk contacts without HIV infection. However, constructing a social network can be challenging because identifying the core members is difficult and the individuals and locations where high-risk behaviors occur are relatively concealed. Using the genetic similarity of HIV sequences, a molecular transmission network can be built to investigate transmission patterns, accurately determine potential transmission, and identify active transmission clusters [ 9 ]. However, it should be noted that the molecular network only contains HIV-infected individuals and the linkage obtained by genetic distance calculation does not represent the closeness of the transmission relationship and the direction of virus transmission. Therefore, it must be judged in conjunction with the contact history between hosts.
Reports of HIV-related spatial analysis in China are relatively few and mainly focus on a single province, city, or population in the southwestern region of China; insufficient attention has been paid to reporting differences among cities under the same province and the flow of patients during treatment under sub-jurisdictions. Jiangsu Province has also not reported the relevant data in recent years. This paper combined descriptive epidemiology, spatial analysis, and molecular epidemiology methods to analyze the patient reporting data, patient flow information, and HIV sequence information of Jiangsu Province in 2021 to further dissect the spatial distribution characteristics of HIV-infected patients, identify critical areas, and detect molecular linkage of strains between regions. This provided ideas and a scientific basis for developing targeted prevention and control strategies, precise containment of the local HIV epidemic, optimal allocation of health resources, and achieving the 95-95-95 target and cascade.
2. Materials and Methods
2.1. data sources.
The data used in this study consisted of two main parts: one from the database of newly reported patients with HIV/AIDS in Jiangsu Province, which included information on the patient’s reporting area and the patient’s address at the first treatment follow up, in addition to essential sociodemographic characteristics; the other part was the HIV sequence information from patients newly reported in 2021 obtained from the laboratory. In addition, information such as the number of residents in each city in Jiangsu Province was obtained from the websites of the provincial and municipal statistical bureaus ( Supplementary Material ); the maps used were obtained from the website DataV.GeoAtlas ( http://datav.aliyun.com/portal/school/atlas/area_selector , accessed on 10 May 2023).
2.2. Spatial Analysis
In the spatial analysis, the Moran I index and the Getis-Ord Gi index were calculated using the spdep package, and the local indicators of spatial association (LISA) clustering and cold–hot spot maps were drawn using the ggplot2 package in R. The global Moran I index takes values ranging from −1 to 1 (α = 0.05). When the global Moran I is positive, it indicates a positive correlation in spatial data, which means similar values are more likely to cluster together in space. When the global Moran I index is negative, there is a negative correlation in spatial data, which means that similar values are more likely to be scattered in various regions in space. When the global Moran I index is 0, it indicates no autocorrelation in the spatial data, and the distribution of the spatial data is random. Based on the local Moran I index, regions can be classified into five states: Insignificant, HH (High–High), LL (Low–Low), HL (High–Low), and LH (Low–High), and plotted in the LISA clustering maps. For example, if the value for a region is higher than the values for all the surrounding regions, and the surrounding regions are also all high value regions, this region will be classified as an HH region, and the other states are similarly assigned. The local Getis-Ord Gi* index depends on the difference between the observed and expected values of the spatial data. Hot and cold spots with different confidence intervals (CI) can be identified and marked on the maps. Hot spots indicate that the region has high observed and low expected values, so the disease exhibits significant aggregation in this region, and cold spots represent the opposite.
2.3. Laboratory Examination and Molecular Transmission Network Construction
Sample collection, experimental manipulation, and sequence processing have been described in a previous study [ 10 ]. According to the Technical Guide for HIV Transmission Networks Monitoring and Intervention (2021 trial version) published by the Chinese Center for Disease Control and Prevention, the phylogenetic tree was first constructed using Fasttree (version: 1.4.3), and the number of clusters and edges under different thresholds was calculated using ClusterPicker (version: 1.2.5) and Hyphy (version: 2.2.4) software, respectively, combining the information from both to select the optimal gene distance threshold ( Supplementary Material Figure S1 ) and complete the visualization of the molecular transmission network using Cytoscape software (version: 3.9.1).
2.4. Statistical Analysis
Statistical analysis in this study was mainly performed using R software (version: 4.2.3), including the data frequency and percentage calculations, and image plots.
3.1. Characterization of Newly Reported HIV/AIDS Patient Profiles in 2021
The numbers of newly reported patients with HIV/AIDS in Jiangsu Province ( Figure 1 ), listed by city name from high to low, were Su Zhou, Nan Jing, Wu Xi, Nan Tong, Chang Zhou, Xu Zhou, Yan Cheng, Yang Zhou, Tai Zhou, Huai An, Zhen Jiang, Lian Yungang, and Su Qian. After calculating the standardized reporting rate by combining the number of residents, the standardized rates were ranked Wu Xi, Chang Zhou, Su Zhou, Nan Jing, Zhen Jiang, Nan Tong, Yang Zhou, Tai Zhou, Yan Cheng, Huai An, Xu Zhou, Lian Yungang, and Su Qian from highest to lowest.

Disease map of the number of newly reported HIV/AIDS patients ( A ) and the standardized reporting rate ( B ) in Jiangsu Province in 2021.
The composition of the top five HIV-1 subtypes in each city was almost the same ( Figure 2 ), involving eight subtypes, among which Nan Tong, Tai Zhou, Wu Xi, Yang Zhou, Lian Yungang, and Zhen Jiang were dominated by CRF (Circulating Recombinant Form) 01_AE, 07_BC, 08_BC, 55_01B and 67_01B; B, 01_AE, 07_BC, 08_BC and 55_01B dominated in Chang Zhou and Su Zhou. The top five subtypes in Nan Jing and Xu Zhou also included (Unique Recombinant Form) URF_107, while 68_01B reached the top five in Huai An and Yan Cheng.

Composition of the top five HIV-1 subtypes in 13 cities in Jiangsu Province.
3.2. Spatial Analysis of New Reporting of Patients with HIV/AIDS in 2021
To identify whether new HIV/AIDS reporting in Jiangsu Province was spatially linked among regions, a spatial analysis was performed using each region’s standardized reporting rate, and a global Moran I = 0.5426 ( p < 0.05) was obtained, suggesting a spatial correlation. However, this result only suggested the existence of spatial aggregation and did not account for the specific situation of each region, so the local Moran I index and local Gi* index were further calculated. The LISA clustering map ( Figure 3 A) and the cold–hot spots map ( Figure 3 B) were drawn based on the corresponding results.

LISA clusters map ( A ) and cold–hot spots map ( B ) of standardized HIV/AIDS reporting rate in Jiangsu Province in 2021.
As can be seen from Figure 3 , Chang Zhou showed a High–High clustering pattern, Tai Zhou showed a Low–Low clustering pattern, and Xu Zhou, Su Qian, Huai An, and Lian Yungang showed a Low–High clustering pattern. At the 99% CI, only one cold spot was identified in Lian Yungang; at the 95% CI, Chang Zhou and Wu Xi were identified as hot spots, while Xu Zhou, Su Qian, and Huai An were identified as cold spots; at the 90% CI, Tai Zhou and Yan Cheng were identified as hot and cold spots, respectively.
3.3. Flow Profiles of Patients between Different Regions in Jiangsu Province at the Time of Reporting and Follow Up
The spatial analysis provided autocorrelation within the spatial data and correlation between a region and adjacent regions. However, it could not determine the correlation between non-adjacent regions, yet patient mobility was not limited to adjacent regions. Although cross-regional mobility of patients before reporting of HIV infection was not available, we conducted a mobility analysis using patients’ address areas at the time of reporting and first follow up after antiretroviral therapy (ART) as patient coordinates ( Figure 4 ). The results showed that Su Zhou had the highest number of “destination cities” for patients, with destinations including all 12 cities except Su Zhou. Meanwhile, 116 patients in Su Zhou were reported to have moved to other areas, mainly outside Jiangsu province, while Chang Zhou, Wu Xi, and Su Qian dominated Jiangsu Province. Nan Jing, Wu Xi, Nan Tong, and Tai Zhou each had one patient moving to Su Zhou.

Sankey diagram of permanent address mobility of newly reported HIV/AIDS patients in Jiangsu Province, 2021. Note: Sankey diagrams were constructed using the address of the patient at the time of reporting (first column) and the address of the patient’s usual residence at the first follow up visit after receiving ART (second column) as the coordinates before and after the cross-regional flow of patients, where “others 192” indicates all patients moving outside Jiangsu Province, and the third column shows the top 10 provinces in “others 192”.
Although patients from Chang Zhou moved to only six cities, Chang Zhou had the highest outflow (thirty patients), among whom twenty went to Nan Tong, four went to Su Qian, three went to Wu Xi, and one each went to Yan Chen, Huai An, and Lian Yungang; meanwhile, Chang Zhou had the highest number of source cities for inflow patients, with five and three patients from Su Zhou and Wu Xi, and the remaining three patients from Xu Zhou, Huai An, and Zhen Jiang, respectively.
Besides Su Zhou and Chang Zhou, Wu Xi, Nan Jing, Xu Zhou, Zhen Jiang, and Lian Yungang also had fewer patients than originally reported because the outflow patients exceeded the inflow patients. In contrast, the treated patients in the remaining six cities were more numerous than the reported patients, with Yang Zhou and Su Qian having only one outflow patient who moved outside the province, and treated patients increased due to the inflow of patients from Su Zhou and Nan Jing, and four patients moving from Chang Zhou to Su Qian.
Except for Huai An, from which only 1 patient went to Chang Zhou after diagnosis, the remaining 12 cities reported 192 patients moving out of the province, involving 28 of the 32 provincial administrative regions in mainland China, and the main destination provinces were Anhui, Henan, Sichuan, Guangzhou, and Yunnan.
3.4. Spatial Analysis Based on the Molecular Transmission Network
The mobility analysis provided clues to the spread of HIV strains between regions. To determine whether there were linkages between the prevalent HIV strains in the regions in which people moved around each other, a molecular transmission network was established based on 3579 pol sequences ( Figure 5 a). Of these, 501 sequences formed a transmission association with at least one other sequence, based on the criteria of gene distance ≤ 0.02 and Bootstraps ≥ 95%, and were entered into the transmission network analysis, accounting for 14.00% (501/3579) of all sequences. The 501 sequences formed 79 transmission clusters, and the number of sequences included in the clusters ranged from 2 to 196.

Molecular transmission network of newly reported HIV/AIDS patients in Jiangsu Province in 2021. Note: ( a ): Molecular transmission network based on 3579 pol sequences; the colors of the nodes in the figure corresponds to different regions. ( b ): A patient reported by Chang Zhou, whose usual residence at the first follow up was reported as Huai An. ( c ): A patient reported by Huai An, whose usual residence at the first follow up was reported as Chang Zhou. ( d ): A patient reported by Su Zhou, whose usual residence at the first follow up was reported as Chang Zhou.
The distribution of different regions is shown in Figure 5 a. The molecular transmission networks contained sequences from all 13 cities in Jiangsu Province, with sequences from Chang Zhou accounting for the highest proportion of the transmission network (37.33%, 187/501), followed by Wu Xi (14.37%, 72/501) and Su Zhou (8.78%, 44/501), which were also the top three cities in terms of the outflow of newly reported HIV/AIDS patients after diagnosis in Jiangsu Province in 2021.
Most of the molecular transmission networks contained fewer than 10 sequences, mainly formed by sequences from one or two cities. However, 7 of the 79 networks contained more than 10 sequences, and the largest network contained 196 sequences from all 13 cities, with Chang Zhou (22.96%, 45/196) predominating, followed by Wu Xi (12.76%, 25/196), and Nan Tong and Su Zhou tied for third in terms of sequence number (10.20%, 20/196). Of the remaining six networks, five contained sequences at least from Chang Zhou and Wu Xi, and one network consisted of 11 sequences from Chang Zhou, Su Zhou, Tai Zhou, Yan Cheng, and Zhen Jiang.
Eight patients moved between cities during ART in the largest cluster, and three of whom were linked to patients in the destination cities in the largest network. The first patient, reported by Chang Zhou, whose usual residence at the first follow up was reported as Huai An, was linked to 30 other sequences (3 sequences from Huai An) in the molecular transmission network ( Figure 5 b). The second patient, reported by Huai An, whose usual residence at the first follow up was reported as Chang Zhou, was linked to 12 other sequences (11 sequences from Chang Zhou) in the molecular transmission network ( Figure 5 c). The third patient, reported by Su Zhou, whose usual residence at the first follow up was reported as Chang Zhou, was linked to 10 other sequences (9 sequences from Chang Zhou) in the molecular transmission network ( Figure 5 d).
Spatial analysis was performed after calculating the standardized network entry rate using the number of entries in each region, and the results showed a global Moran I = 0.5617 ( p < 0.05), suggesting the existence of spatial autocorrelation, which meant that two adjacent cities in Jiangsu Province tended to have similar network entry rates. LISA clustering maps ( Figure 6 A) and cold–hot spot maps ( Figure 6 B) were also drawn using the local Moran I index and local Gi* index. Wu Xi showed a High–High clustering pattern, Chang Zhou showed a High–Low clustering pattern, and Nan Jing showed a Low–Low clustering pattern. Chang Zhou and Wu Xi were identified as hot spots at 90% CI, and no cold spots were identified.

LISA clustering map ( A ) and cold–hot spots map ( B ) of standardized molecular transmission network entry rate in Jiangsu Province in 2021.
4. Discussion
In previous epidemiological studies, the absolute number of HIV infections did not correctly indicate the local HIV infection level. After calculating the standardized reporting rate, this study found that HIV/AIDS patients were unevenly distributed in different cities in Jiangsu, and southern Jiangsu had a higher rate than the average. Spatial analysis revealed that Chang Zhou showed a High–High aggregation pattern and was identified as a hot spot at 95% CI. Patient mobility information also suggested that Chang Zhou ranked first in Jiangsu regarding the number of outflow patients and inflow cities. Meanwhile, the molecular transmission network also showed that some patients who moved between cities were linked with patients from destination cities.
A study in southwestern China noted that urbanization and population density were positively associated with HIV infection [ 11 ]. Southern Jiangsu, including Chang Zhou and Wu Xi, occupies the top position in both urbanization and population density in Jiangsu ( Table S1 in Supplementary Material ), which may be one reason why HIV reporting rates in southern Jiangsu are generally higher than average, and the two adjacent areas of Chang Zhou and Wu Xi are identified as hot spots at 95% CI. However, Su Zhou and Nan Jing, which also have high population density and urbanization rates, were not identified as hot spots. Some studies have pointed out that gross domestic product (GDP) was a protective factor for HIV infection [ 12 , 13 ], and GDP in Su Zhou and Nan Jing far exceeded that of other cities in Jiangsu ( Table S1 in Supplementary Material ), which may have influenced the occurrence of HIV infection, but further analysis combined with more information is needed.
The survey results in Jiangsu Province from 2009 to 2011 showed that more than half of the HIV-1 genotypes of infected patients were 01_AE, and the main transmission route had changed from heterosexual to homosexual [ 14 ]. The survey also reported that 01_AE and 07_BC dominated, and besides subtype B, the rest of the subtypes with a composition ratio of more than 1% were CRFs and URFs in men who have sex with men (MSM) in 2017 and 2018. This study showed that the main subtype composition of newly reported HIV/AIDS patients in 2021 was similar to previous studies but with increased CRFs and URFs. Meanwhile, the proportion of 07_BC exceeded that of 01_AE, which previously ranked first, and the proportion of 08_BC increased from fourth to third [ 15 ], suggesting that both the number of HIV-1 subtypes and their proportions in Jiangsu Province were changing. It is necessary to investigate the situation through close and comprehensive surveillance and combine this with monitoring of prevalent HIV-1 strain characteristics to allow timely adjustments of prevention and treatment policies.
Previous studies have shown that the highest prevalence of HIV in Jiangsu Province gradually shifted from Xu Zhou in northern Jiangsu to southern Jiangsu, with Nan Jing, Su Zhou, Wu Xi, Chang Zhou, and other southern areas dominating since 2008, and showing a tendency to radiate to central and northern Jiangsu [ 16 ]. This study also found clusters in Chang Zhou and Su Zhou but not in Nan Jing and Wu Xi; it also found clusters in Tai Zhou, which belongs to central Jiangsu, which may be related to the strategies adopted in recent years to strengthen publicity and education, expand the coverage of sentinel sites, and improve the accuracy of counseling and testing in the whole province [ 4 ]. The findings suggested that the HIV clustering profiles in Jiangsu changed to a certain extent, and it was necessary to combine the monitoring results in order to direct resources toward high aggregation regions, to carry out prevention and treatment measures such as increasing the frequency of testing for high-risk groups, promote the application of pre-exposure prophylaxis (PrEP), expand the scope of ART, and improve the effectiveness of ART to interrupt the transmission of HIV. This will gradually reduce the number of new HIV infections and ultimately achieve the UNAIDS 2030 GOALS.
The results of this study showed clustering of patients of reported HIV/AIDS in Su Zhou and Chang Zhou, the frequent patient mobility between these two cities, and the widespread presence of sequences from Chang Zhou in different molecular transmission networks, suggesting that HIV-1 strains prevalent in Jiangsu Province were not only spreading within the same city but also spreading among different cities. It is important to note that although three patients in this study had a change of address after diagnosis, and molecular transmission network analysis also revealed that these three patients were linked molecularly to some of the newly reported patients in the destination cities, it was uncertain whether these patients’ movements and molecular linkages were related to the cross-transmission of HIV-1 strains between these cities owing to the lack of information on the patients’ addresses before diagnosis, as well as their mobility characteristics and social transmission networks after infection. Jiangsu Province mainly detects HIV-infected patients through voluntary counseling testing (VCT) clinics [ 4 ]. However, active testing based on the perceived HIV infection risk may be more effective than widespread screening methods [ 17 , 18 ]. A study in Jiangsu surveyed the acceptance of smartphone applications for self-testing of HIV infection status among MSM and found that 71.2% of respondents were willing to use this application to increase the testing frequency [ 19 ], so multiple testing modes such as self-testing should be developed in addition to testing at health care facilities. Some researchers have pointed out intensive intervention programs in high-risk groups were more efficient in reducing new HIV infections than interventions aimed at the general population [ 20 ]. Jiangsu Province has been conducting drug resistance monitoring of all newly reported HIV/AIDS patients since 2017 while continuously expanding the scope of monitoring and improving the monitoring network, as well as cooperating with social organizations to carry out publicity and testing work on high-risk populations to provide conditions for promoting early detection, diagnosis, and treatment of infected patients. At present, Jiangsu is also working on constructing a dynamic molecular transmission network covering all HIV/AIDS patients in the province, hoping to provide critical information for the timely detection of new networks, clarify the transmission characteristics of strains, and deploy prevention and control resources rationally. As a preliminary exploration of network construction, this study needs to be combined with information from epidemiological surveys and social transmission networks to provide directions for further construction.
About 5% of patients moved to other provinces with severe HIV epidemics after diagnosis; they were mainly concentrated in Anhui, Henan, Sichuan, Guizhou, and Yunnan [ 21 ]. 85_BC was relatively frequent in Sichuan, in addition to the major subtypes like 07_BC, 01_AE, and 08_BC [ 22 ]. The subtype composition was more complex in Yunnan, which borders Myanmar, Vietnam, and Laos, owing to frequent cross-border HIV transmission [ 23 ], and the new subtype numbers were significantly higher in Yunnan [ 24 ], explaining the difference in HIV-1 subtype composition from Jiangsu. Previous studies have shown that the antibodies produced after HIV infection are insufficient to resist re-infection with other HIV strains [ 25 ], and re-infection leads to many adverse outcomes due to the virologic rebound [ 26 ]. Movement of patients between cities, and especially across provinces, and failure to maintain optimal ART outcomes and reduce their high-risk behavior, may lead to recombination of different subtypes and new subtypes emerging [ 27 ], bringing more challenges to HIV prevention and control. Therefore, realizing timely communication and cooperation among different provinces, focusing on vital mobile populations, jointly improving prevention and control effects, reducing cross-province HIV transmission, and avoiding generation of new CRFs should be the focus of intervention.
This study combined three aspects: patient reporting, patient mobility, and HIV sequence information for the first time in Jiangsu Province to identify cities of high aggregation and mobility as well as active transmission clusters, using spatial and molecular linkages of patients. It has provided reliable information for targeted regional surveillance efforts to strengthen and promote precise interventions. However, there were some limitations of this study: First, this study only included the sequences collected in 2021, and therefore could not identify the changes and linkages of HIV/AIDS patients in each region over time, and only provided clues rather than complete evidence of HIV transmission. Second, although this study identified highly aggregated and high-mobility cities such as Chang Zhou and Wu Xi, and also identified several inter-city flows of patients in the molecular transmission network, further models such as social transmission networks are needed to analyze the role of this frequent mobility of diagnosed patients in HIV transmission, owing to the lack of more information including social, economic, cultural and patient behavioral factors.
5. Conclusions
There was a spatial aggregation of newly reported HIV infections in Jiangsu Province in 2021, and there was inter-city mobility of infected individuals after diagnosis. The cities in southern Jiangsu, represented by Chang Zhou and Wu Xi, were critical for epidemic prevention and control. Future studies should combine molecular and social transmission networks to construct a larger transmission network model, taking key regions and key populations as entry points, enhancing prevention and control efforts, improving prevention and control timeliness and efficiency under limited resources, and contributing to achieving the 95-95-95 target and cascade.
Acknowledgments
We want to thank all the staff who helped collect samples, gather information, and perform experimental operations. We are also grateful to all patients who cooperated with us and provided us with information. We would also like to express our sincere gratitude to all the experts who provided advice and assistance during this article’s writing, review, and publication.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/v15102053/s1 , Figure S1 Clusters and edges number line graph under different thresholds; Table S1 Characteristics of 13 cities in Jiangsu Province
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, B.W., Y.Z., D.Y., S.L. and L.S.; data curation, D.Y., S.L., L.S., X.L. and T.Q.; formal analysis, D.Y.; investigation, D.Y., S.L. and L.S.; methodology, D.Y.; project administration, B.W. and Y.Z.; resources, X.L. and T.Q.; software, D.Y.; supervision, B.W. and Y.Z.; validation, B.W., Y.Z. and D.Y.; visualization, D.Y., F.O. and W.A.; writing—original draft preparation, B.W., Y.Z., D.Y. and S.L.; writing—review and editing, B.W., D.Y., S.L., F.O., W.A. and L.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The studies involving human participants were reviewed and approved by the Ethics Review Committee of Jiangsu Provincial Center for Disease Control and Prevention (Approval No: JSJK2021-B017-01. Approval Date: 23 December 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

IMAGES
VIDEO
COMMENTS
In this systematic review of stigma and the HIV/AIDS epidemic, we examined the existing literature on how H/A stigma is conceptualized, the methodologies for measuring stigma, the available data on the relationship of stigma to the effectiveness of HIV prevention and treatment programs, and interventions and programs for reducing stigma.
AIDS is a. condition in humans in which p rogressive failure of the immune s ystem allows life-threatening. infections and cancers to thrive. Infection with HIV occurs by t he transfer of blood ...
1.2Young people, HIV/AIDS and the global goals During the past 20 years, and despite the continued lack of an effective vac-cine, the armamentarium for preventing the transmission and decreasing the impact of HIV and AIDS has slowly grown (9, 10) (see also chapter 3). HIV/AIDS has its roots in a range of problems that undermine people's health
1 The new consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations bring together all existing World Health Organization (WHO) guidance relevant to five key populations: men who have sex with men, people who inject drugs, people in prisons and other closed settings, sex workers and transgender people.It includes a number of new recommendations and updates ...
The objective of this review is to carry out a review of published and grey literature on the evidence of injecting and non-injecting stimulant use (particularly crack, cocaine and ATS) and their possible link to HIV, HCV & HBV vulnerability and transmission. To identify: • The extent of HIV, HCV and HBC infection among stimulant users
Keywords: HIV/AIDS; systematic review; qualitative approaches 1. Introduction HIV is one of the main problems with regard to public health, with greater representation in developing countries [1]. The most a ected region is Africa, where almost two thirds of new HIV infections can be found [2].
In this Review, Landovitz, Scott and Deeks explore the current state of the art for HIV prevention and treatment, including unmet needs and emerging tools. They describe how researchers are ...
Twenty-eight million people in Africa are living with HIV/AIDS and Southern Africa has the highest HIV adult prevalence in the world. Well over two thirds of the HIV/AIDS related deaths (18 million, or 72%) are from Africa (World Bank, 2002) and almost one in every ten adults in sub-Saharan Africa are HIV positive (UNESCO, 2002), although ...
In a meeting with members of the GMR Team in February 2009, the following areas of input were suggested: Children affected and infected by HIV and AIDS as a significant group of the most marginalized; Examination of the education policy, teaching and learning processes and curricula - their marginalizing and de-marginalizing impact on learners ...
2. This literature review summarizes empirical literature examining the prevalence of HIV stigma and discrimination and the relationship between stigma and HIV prevention, treatment and care, as well as evaluations of programs to reduce HIV-related stigma and discrimination. Publications in this literature review were published between mid-2005 ...
AIDS is now 30 years old. Joint United Nations Programme on HIV/AIDS (UNAIDS) reported that in 2010 more than 34 million people were living with HIV/AIDS (PLHA), of which 22.5 million were from sub-Saharan Africa, which recorded 30 million deaths from the time AIDS was first identified on June 5, 1981. 2 Undoubtedly, over the past 3 decades, huge efforts to combat HIV/AIDS have been faithfully ...
HIV/AIDS-related stigma has been recognised as a key problem that needs to be addressed in HIV/AIDS interventions with adults (for a review, see Deacon et al. 2005). The literature on children and HIV/AIDS is extensive, as is the literature on HIV/AIDS-related stigma, but specific research on HIV/AIDS-related stigma and children is relatively
The status of older adults in Africa occupies a small but rapidly expanding share of the global literature on ageing. The human immunodeficiency virus (HIV) and acquired immune deficiency syndrome ...
Acquired Immunodeficiency Syndrome caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. This study intends to ...
Gcina Kheswa. Medicine, Sociology. 2014. TLDR. The findings show that stigmatisation remains a pervasive experience in the lives of the children of PLWHA, and suggests that more research should be conducted on how HIV stigma affects the life of children whose parents are affected by HIV and AIDS in South Africa.
The literature relating to children and HIV/AIDS. stigma in regions with a type 1 epidemic, where predominant risk groups include gay. men and drug users, is of variable applicability in high ...
Curr Res HIV 2017: CRHA-111. DOI: 10.29011/2575-7105. 100011. Background: The last decade has witnessed several advances in the management of HIV/AIDS with the development of potent and safe antiretroviral drugs and new HIV prevention technologies. Objective: This review summarizes the recent advances in the management of the HIV infection.
of HIV progression in humans. We included two strategies of search with and without MeSH terms. We classified the models by their mathematical structure and research question. We created a checklist of desirable features of the models, reviewed and classified the articles to inform our conclusions. Results: Among 3491 articles found, 93 met the inclusion criteria. Among the selected articles ...
More than 90% of babies acquire HIV/AIDS through vertical transmission, primarily due to low maternal comprehensive knowledge about Mother-To-Child Transmission (MTCT) of HIV/AIDS and its prevention, which is a cornerstone for eliminating MTCT of HIV/AIDS. However, there are limitations in terms of population data and literature evidence based on recent Demographic and Health Surveys (DHS ...
In this study, the literature on precancerous cervical lesions among women living with HIV AIDS in Ethiopia was reviewed. However, studies have shown differences in precancerous cervical lesions and associated factors, and to the knowledge of the investigator concerned, the literature has not been systematically examined.
From January to October 2022, Jiangsu reported 3677 new HIV cases [ 4 ], a decrease of only 2.1% compared with the same period in the previous year [ 5 ], and lower than the 16.7% national decline reported at the 8th National Academic AIDS Conference. HIV, similar to other infectious diseases, exhibits spatial distribution characteristics that ...