License for Use of "Physicians' Current Procedural Terminology", (CPT) Fourth Edition
End User/Point and Click Agreement: CPT codes, descriptions and other data only are copyright 2009 American Medical Association (AMA). All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the AMA.
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials including but not limited to CGS fee schedules, general communications, Medicare Bulletin , and related materials internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2)(June 1995) and/or subject to the restrictions of DFARS 227.7202-1(a)(June 1995) and DFARS 227.7202-3(a)June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provisions of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department Federal procurements.

AMA Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CGS or the CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
CMS Disclaimer
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT must be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
This license will terminate upon notice to you if you violate the terms of this license. The AMA is a third party beneficiary to this license.
POINT AND CLICK LICENSE FOR USE OF "CURRENT DENTAL TERMINOLOGY", ("CDT")
End User License Agreement
These materials contain Current Dental Terminology, Fourth Edition (CDT), copyright © 2002, 2004 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED "I ACCEPT", YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED "I DO NOT ACCEPT" AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, "YOU" AND "YOUR" REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
- Subject to the terms and conditions contained in this Agreement, you, your employees, and agents are authorized to use CDT-4 only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT-4 is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT-4. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
- Applicable Federal Acquisition Regulation Clauses (FARS)\Department of Defense Federal Acquisition Regulation Supplement (DFARS) Restrictions Apply to Government use. Please click here to see all U.S. Government Rights Provisions .
- ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT-4 is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT-4. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for the software, including any CDT-4 and other content contained therein, is with (insert name of applicable entity) or the CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third-party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT-4 should be addressed to the ADA. End users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CDT-4. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL COVERED BY THIS LICENSE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. If the foregoing terms and conditions are acceptable to you, please indicate your agreement by clicking below on the button labeled "I ACCEPT". If you do not agree to the terms and conditions, you may not access or use the software. Instead, you must click below on the button labeled "I DO NOT ACCEPT" and exit from this computer screen.

| | | |
| | | ">Email | Font Size: | | | | | | The Provider Statistical and Reimbursement (PS&R) reports are generated by a system maintained by the Centers for Medicare and Medicaid Services (CMS). The PS&R system accumulates Medicare Part A data processed by the standard claims processing system. The primary PS&R report is the Provider Summary report, which includes a summary of Medicare charges, patient days, deductibles, coinsurance, payments, etc. for each provider for a specified period of time. The Provider Summary reports should be used by a provider when preparing the Medicare cost report. CMS has implemented the new redesigned PS&R system effective for cost reporting periods ending on or after January 31, 2009. Providers with cost reports ending after this will obtain the PS&R reports needed to file the Medicare cost report by accessing the Enterprise Identity Management (EIDM) system. A provider must first register for an EIDM account to allow access to PS&R data specific to their organization. With the implementation of the redesigned PS&R, you will not be sent a summary PS&R to use in filing a cost report. Providers will be expected to obtain PS&R reports from the redesigned PS&R website. Detail PS&R requests will continue to be made through the J15 MAC. For additional information about the redesigned PS&R refer to the Overview section of the Web page. Additional information about accessing EIDM is also available under the Provider Community and FI/MAC Community sections of that same page. CGS Home Health and Hospice providers may contact us at 1.615.660.5562 for questions regarding their PS&R.
|
Stay Connected
People With Medicare
| 26 Century Blvd Ste ST610, Nashville, TN 37214-3685 | © CGS Administrators, LLC. All Rights Reserved |
- Audit and Reimbursement
- Provider Statistical and Reimbursement System
Provider Statistical and Reimbursement System: Order Summary Report

The Provider Statistical and Reimbursement (PS&R) System contains various report features. The following describes how to order the Summary Report which is used in preparing the Medicare cost report.
An approved PS&R User can order reports. Access to the PS&R is controlled through the Identity Management (IDM) system. If access is needed, refer to the article Provider Statistical and Reimbursement: Obtain Access via IDM ( JJ Part A , JM Part A , HHH ) for instructions.
A. Login to PS&R
Use the following link to login to the PS&R: https://psr-ui.cms.hhs.gov/psr-ui
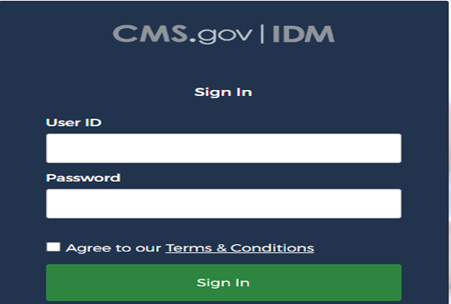
To sign in, enter ID and Password, select "Agree to Terms and Conditions" and selet Sign In .
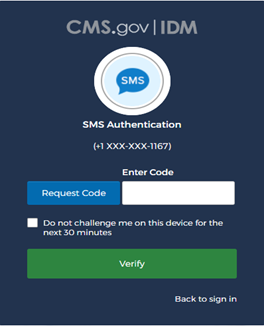
At SMS Authentication, select Request Code , enter the code received via Test message or email, and select Verify .
Select Log In .
B. Order Summary Report
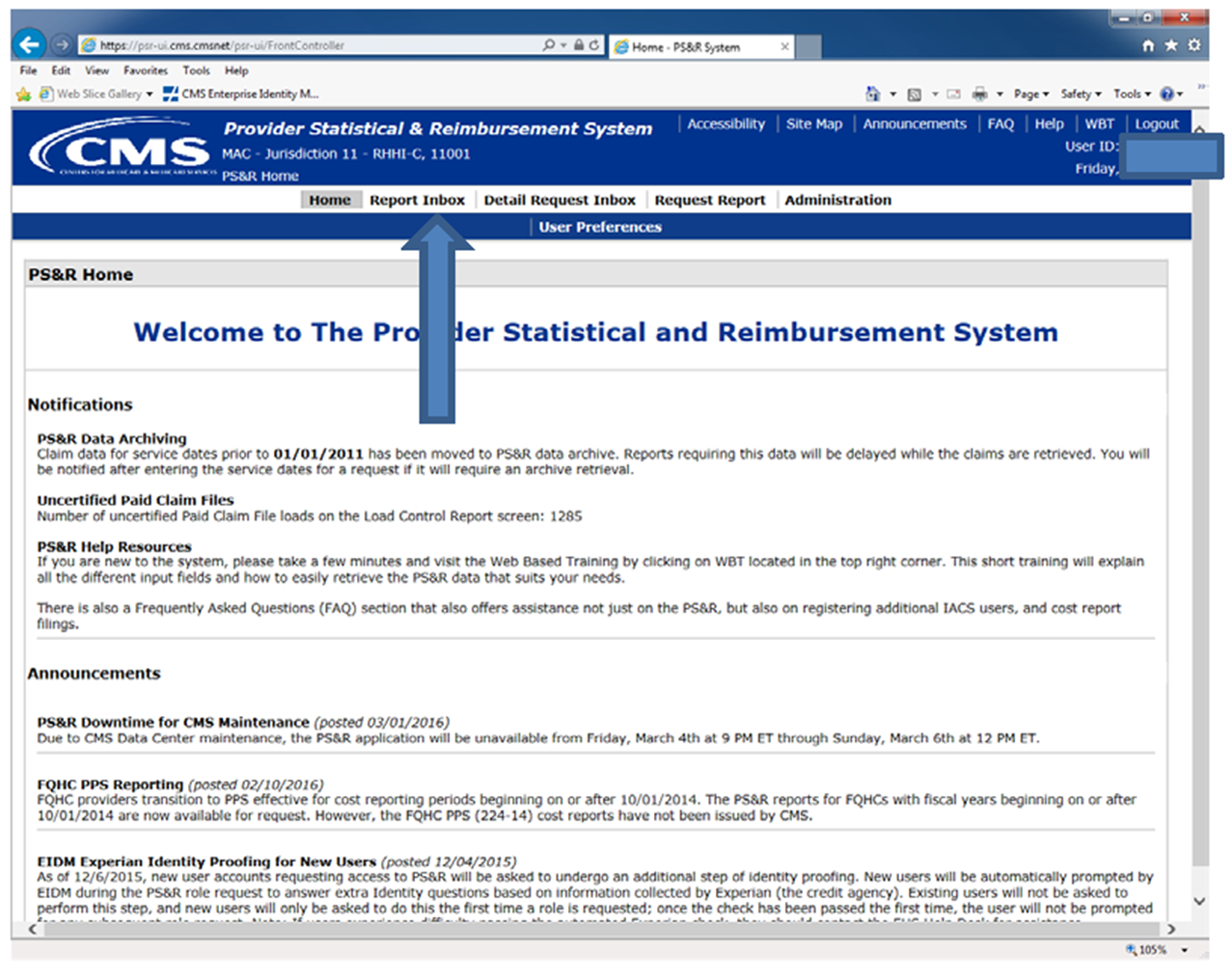
After logging in, the Welcome to The Provider Statistical and Reimbursement System screen will appear.
In the banner line at the top of the screen select Request Report .
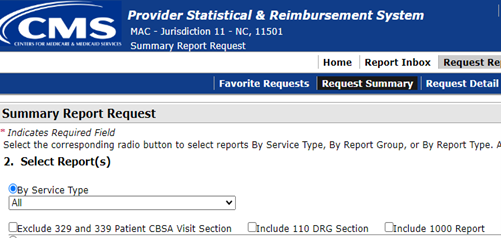
On the next screen, select Request Summary .
The Summary Report Request screen will appear. Perform the following steps to complete the request.
- Select Provider(s) Select the provider number/name and click >> button to select the provider. Select Continue at the bottom of the screen.
- Select Report(s) Select the first option, By Service Type , by clicking the round button. All will be displayed on the next line. Scroll to the end of the screen and select Continue .
- Enter Service Periods (Format: MM/DD/YYYY) Four periods may be listed. If only one period is needed, exclude the other periods by clicking the box beside Exclude . If a different period is desired, enter the dates in the above section and select Apply.
- Enter Paid Dates (Format: MM/DD/YYYY) The default setting is all paid dates and is typically used. If different dates are desired, choose those below. Scroll down to the end of the screen and select Continue .
- Select Report Format The PDF option will produce the PS&R in a report format. The CSV option will produce a file that can be loaded into the cost report software. If in doubt, order both. Select Continue .
- Confirm Report Request This presents information on the request. Scroll down to the end of the screen and select Submit to complete the request (or select Back to modify).
Note : The PS&R System may take a few minutes to a few hours to process the report. The next section will explain how to obtain the completed report.
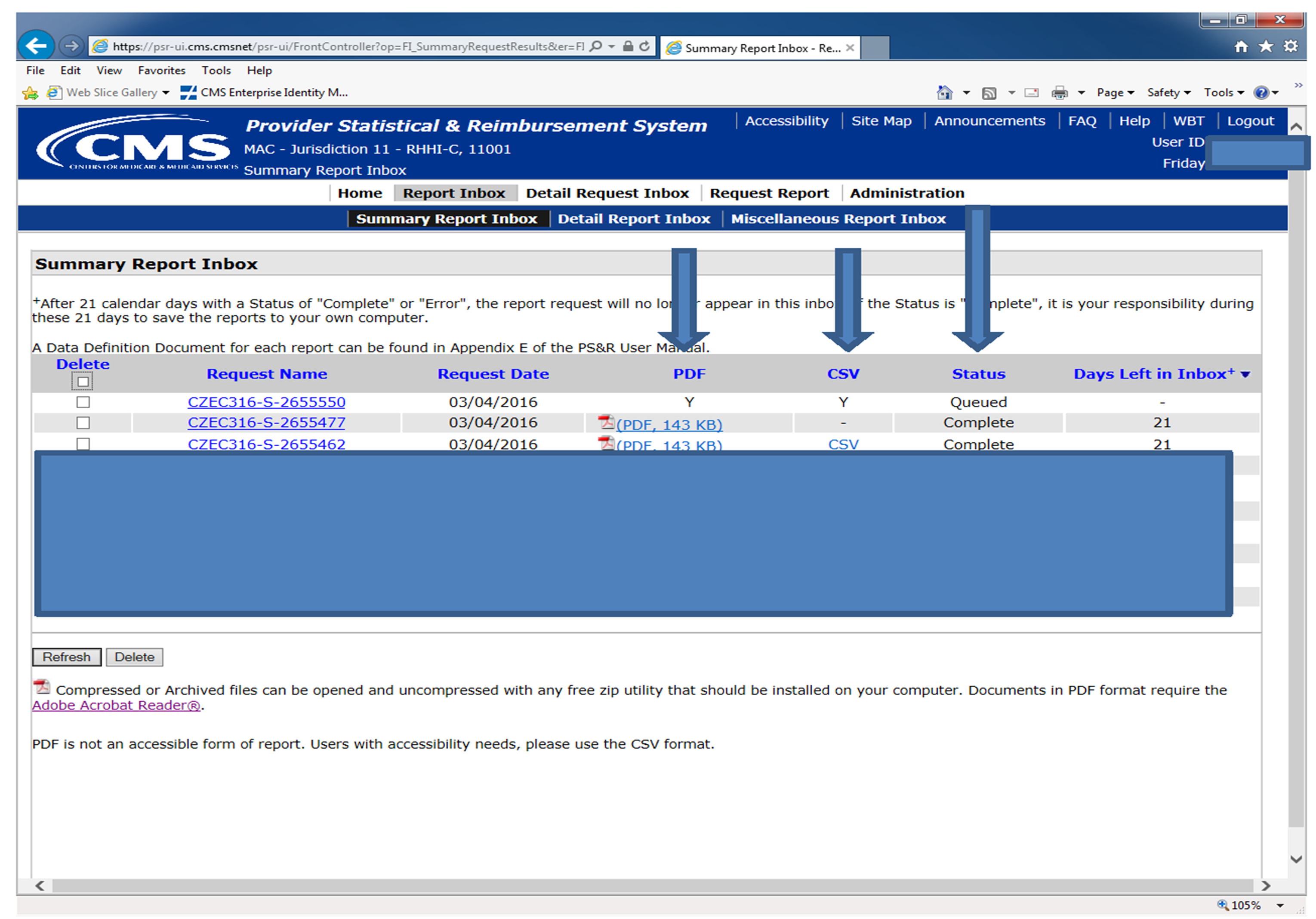
C. Print or Save the Summary Report
To obtain the completed report, Select Report Inbox in the banner at top of the screen.
On the following screen please note the following:
- If status is Queued — the reporting is waiting to process
- If status is Processing — the report should be complete in a few minutes
- If status is Complete — the report is available
- Click on the item in the PDF or CSV column to open the file
- After opening the file — print the report or save the file containing the report
Auto Launching . . .
We are attempting to open this content in a new window. You can also access it here: Open Content in New Window
Was this article helpful?
Similar articles that you may find useful:
- Enroll in Medicare
- Provider Enrollment Training Modules
- Enroll in Electronic Claims Submission
- Register for eServices
- Register for Provider Statistical and Reimbursement Access
- Become a Medicare Expert
An official website of the United States government
Here’s how you know
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

U.S. Dept. of Health & Human Services
CMS Provider Statistical & Reimbursement Report (PS&R)
Guidance for provider statistical and reimbursement report data summarized in various reports, which are used by providers to prepare Medicare cost reports, and by MACs during the audit and settlement process.
Issued by: Centers for Medicare & Medicaid Services (CMS)
Issue Date: August 27, 2018
The Provider and Statistical Reimbursement (PS&R) System is a key tool for institutional healthcare providers, Medicare Administrative Contractors (MACs) and CMS. The system accumulates statistical and reimbursement data applicable to the processed and finalized Medicare Part A claims. This data is summarized in various reports, which are used by providers to prepare Medicare cost reports, and by MACs during the audit and settlement process.
Follow the link below for additional information.
HHS is committed to making its websites and documents accessible to the widest possible audience, including individuals with disabilities. We are in the process of retroactively making some documents accessible. If you need assistance accessing an accessible version of this document, please reach out to the [email protected] .
DISCLAIMER: The contents of this database lack the force and effect of law, except as authorized by law (including Medicare Advantage Rate Announcements and Advance Notices) or as specifically incorporated into a contract. The Department may not cite, use, or rely on any guidance that is not posted on the guidance repository, except to establish historical facts.
The independent source for health policy research, polling, and news.
What to Know about Medicare Spending and Financing
Juliette Cubanski and Tricia Neuman Published: Jan 19, 2023
Medicare, the federal health insurance program for 65 million people ages 65 and older and younger people with long-term disabilities, helps to pay for hospital and physician visits, prescription drugs, and other acute and post-acute care services. This brief provides an overview of Medicare spending and financing, based on the most recent historical and projected data published in the 2022 annual report of the Board of Medicare Trustees and the 2022 Medicare baseline and projections from the Congressional Budget Office (CBO). The brief highlights trends in Medicare spending and key drivers of spending growth, including higher enrollment, growth in health care costs, and increases in payments to Medicare Advantage plans.
| Key Facts about Medicare Spending and Financing |
Overview of Medicare Spending
Medicare accounts for 21% of national health spending and 10% of the federal budget.
Medicare plays a major role in the health care system, accounting for 21% of total national health spending in 2021, 26% of spending on both hospital care and physician and clinical services, and 32% of spending on retail prescription drug sales (Figure 1).
In 2021, Medicare spending, net of income from premiums and other offsetting receipts, totaled $689 billion and accounted for 10% of the federal budget—a similar share as spending on Medicaid, the Affordable Care Act (ACA), and the Children’s Health Insurance Program combined, and defense spending (Figure 2).
Historical and Projected Medicare Spending
Medicare spending on Part A, Part B, and Part D benefits in 2021 totaled $829 billion, up from $541 billion in 2011, according to the Medicare Trustees (Figure 3). These amounts reflect gross spending, not subtracting premiums or other offsetting receipts, and include spending on beneficiaries in both traditional Medicare and Medicare Advantage. Medicare benefit spending is expected to grow to $1.8 trillion in 2031 (Figure 3).
CBO projects that between 2021 and 2032, net Medicare spending—after subtracting premiums and other offsetting receipts—will grow as a share of both the federal budget, from 10.1% to 17.8%, and the nation’s economy, from 3.1% to 4.3% of gross domestic product (GDP). Projected spending growth for Medicare is due in part to growing enrollment in Medicare related to the aging of the population, increased use of services and intensity of care, and rising health care costs.
Over the longer term, net Medicare spending will increase to 5.9% of GDP in 2052, according to CBO’s most recent long-term projections . CBO projects that rising health care costs per person will account for two-thirds of the increase in spending on the nation’s major health care programs (Medicare, Medicaid, and subsidies for ACA Marketplace coverage) over the next 30 years, and the aging of the population will account for one-third.
Spending on Physician and Other Outpatient Services Accounts for a Growing Share of Medicare Spending
Spending on benefits under each part of Medicare (A, B, and D) increased in dollar terms between 2011 and 2021, but the distribution of total benefit payments by part has changed over time. Spending on Part B benefits, including physician services, hospital outpatient services, physician-administered drugs, and other outpatient services, increased from 41% in 2011 to 48% in 2021, and now accounts for the largest share of total spending on Medicare benefits (Figure 4). The share of total spending on Part A benefits (mainly hospital inpatient services) decreased from 47% to 39%, reflecting a shift from inpatient to outpatient services. Moving forward, Medicare spending on physician services and other services covered under Part B is expected to grow to just over half of total Medicare spending by 2031, while spending on hospital care and other services covered under Part A is projected to decrease further as a share of the total.
Spending on Part D prescription drug benefits has been a roughly constant share of total Medicare spending since the drug benefit began in 2006 (around 12-13%) and is expected to account for a similar share in the coming decade (11% in 2031). This projection does not take into account any savings to Medicare associated with implementation of the prescription drug provisions in the Inflation Reduction Act , which CBO projects will reduce the federal deficit by $237 billion between 2022 and 2031.
Spending on Medicare Advantage Has Grown as a Share of Total Medicare Spending
Another notable change in Medicare spending over the past decade is the increase in payments to Medicare Advantage plans, which are private health plans, such as HMOs and PPOs, that cover all Part A and Part B benefits and typically also Part D benefits. Medicare payments to Medicare Advantage plans for benefits covered under Part A and Part B nearly tripled between 2011 and 2021, from $124 billion to $361 billion—increasing from 26% of total Part A and Part B spending to 47% over this period. These payments are expected to increase to $943 billion in 2031, accounting for nearly 60% of total Part A and B spending that year (Figure 5). Beginning in 2023, Medicare spending on Part A and Part B benefits for beneficiaries in Medicare Advantage will exceed Part A and Part B benefits spending for beneficiaries in traditional Medicare.
Historically, growth in spending on Medicare Advantage is due in large part to steady growth in private plan enrollment. In 2022, 48% of eligible Medicare beneficiaries are enrolled in Medicare Advantage plans, up from 26% in 2011. Based on CBO’s latest Medicare enrollment projections , Medicare Advantage enrollment will increase to 61% of eligible Medicare beneficiaries by 2031.
In addition, Medicare pays more to private Medicare Advantage plans for enrollees than their costs would be in traditional Medicare, on average, and these higher payments have contributed to growth in spending on Medicare Advantage and overall Medicare spending. In 2022, payments to Medicare Advantage plans are estimated to be 104% of what traditional Medicare would have spent on these beneficiaries, on average, according to MedPAC. This percentage is lower than in 2010, when Congress made changes to how Medicare Advantage plans are paid, but it has been trending higher since 2017.
According to the Congressional Budget Office, higher payments to Medicare Advantage plans, relative to traditional Medicare spending, are due to three factors . First, the payment methodology is based on benchmarks that are higher than traditional Medicare spending in half of all U.S. counties. Second, Medicare Advantage enrollees have higher “risk scores” than traditional Medicare beneficiaries in part because plans have a financial incentive to code for diagnoses, which increases the amount they are paid per enrollee. Third, Medicare Advantage plans typically receive higher payments based on their quality-based star ratings ( $10 billion in 2022 , according to KFF analysis), but these bonus payments do not apply to traditional Medicare.
Administrative Expenses in Traditional Medicare Are Relatively Low, But Higher for Medicare Part D and Medicare Advantage Plans
The overall cost of administering benefits for traditional Medicare is relatively low. In 2021, administrative expenses for traditional Medicare (plus CMS administration and oversight of Part D) totaled $10.8 billion, or 1.3% of total program spending , according to the Medicare Trustees; this includes expenses for the contractors that process claims submitted by beneficiaries in traditional Medicare and their providers.
This estimate does not include insurers’ costs of administering private Medicare Advantage and Part D drug plans, which are considerably higher. Medicare’s actuaries estimate that insurers’ administrative expenses and profits for Part D plans were 8% of total net plan benefit payments in 2021 . The actuaries have not provided a comparable estimate for Medicare Advantage plans, but according to KFF analysis , medical loss ratios (medical claims covered by insurers as a share of total premiums income) averaged 83% for Medicare Advantage plans in 2020, which means that administrative expenses, including profits, were 17% for Medicare Advantage plans.

Medicare Spending Grew More Slowly in the Past Decade than in Decades Prior but Faster Growth Is Projected in the Coming Years
Looking at the average annual rate of growth in Medicare spending, both overall and per beneficiary, growth was notably slower in the most recent decade (2010-2020) than in prior decades, and somewhat slower than growth in private health insurance (PHI) per capita spending. For 2020-2030, the Medicare Trustees project that Medicare per capita spending growth will be higher than in the past decade, but on par with growth in private health insurance (PHI) per capita spending (Figure 6).
Growth in Total Medicare Spending
- Between 2010 and 2020, average annual growth in total Medicare spending was 5.9%, down from 9.0% between 2000 and 2010. The influx of younger, healthier beneficiaries since 2011, when the baby boom generation started becoming eligible for Medicare, was a contributing factor in the slower rate of growth in overall Medicare spending in the 2010s. Slower growth in Medicare spending can also be attributed to policy changes made by the ACA, including reductions in Medicare payments to plans and providers and increased revenues, and the Budget Control Act of 2011, which lowered Medicare spending through sequestration that reduced payments to providers and plans by 2%, beginning in 2013 and since extended through 2031.
- Between 2020 and 2030, average annual growth in total Medicare spending is projected to be somewhat higher than between 2010 and 2020 (6.5% vs. 5.9%).
Growth in Medicare Spending Per Person
Prior to 2010, per enrollee spending growth rates were comparable for Medicare and private health insurance. With the recent slowdown in the growth of Medicare spending and the recent expansion of private health insurance through the ACA, the difference in growth rates between Medicare and private health insurance spending per enrollee widened but is expected to be roughly the same over the next decade.
- In the 1990s and 2000s, Medicare spending per enrollee grew at a similar rate to per enrollee spending among people with private insurance: 5.8% and 5.9%, respectively, in the 1990s and 7.4% and 7.0% in the 2000s.
- Between 2010 and 2020, Medicare per capita spending was relatively low, and grew more slowly than private insurance spending, increasing at an average annual rate of 1.9% over these years, while average annual private health insurance spending per capita grew at a rate of 2.8%.
- Between 2020 and 2030, Medicare per capita spending is projected to grow at a faster rate than between 2010 and 2020, on par with average annual growth in per capita private health insurance spending (5.4% vs. 5.3%).
Growth in Per Capita Medicare Spending on Parts A, B, and D
- Between 2010 and 2020, per capita spending on each of the three parts of Medicare (A, B, and D) grew more slowly than in previous decades (Figure 7). For Part D, estimates are based on spending starting in 2006, the first year of the Part D benefit. For example, the average annual growth rate for Part A was 0.5% between 2010 and 2020, down from 4.5% between 2000 and 2010. For Part B, average annual spending grew at 3.2% between 2010 and 2020, down from 7.0% between 2000 and 2010.
- Between 2020 and 2030, Medicare’s actuaries project a higher per capita growth rate for each part of Medicare, compared to growth between 2010 and 2020: 4.5% for Part A (up from 0.5%), 7.2% for Part B (up from 3.2%), and 3.7% for Part D (up from 2.0%). The Medicare Trustees project faster growth in Part B per capita spending due to higher spending on outpatient hospital services and physician-administered drugs, while the projected increase in Part D per capita spending growth is driven by a slowdown in the generic dispensing rate and increased specialty drug use, offset somewhat but not completely by higher manufacturer rebates negotiated by private plans. The projections for Part B and Part D do not take into account any savings associated with implementation of the prescription drug provisions in the Inflation Reduction Act . The Medicare Trustees have not yet updated spending projections to reflect these changes.
How is Medicare Financed?
Funding for medicare comes primarily from general revenues, payroll taxes, and premiums.
Funding for Medicare, which totaled $888 billion in 2021, comes primarily from general revenues (46%), payroll tax revenues (34%), and premiums paid by beneficiaries (15%) (Figure 8). Other sources include taxes on Social Security benefits, payments from states, and interest. The different parts of Medicare are funded in varying ways, and revenue sources dedicated to one part of the program cannot be used to pay for another part.
- Part A, which covers inpatient hospital stays, skilled nursing facility (SNF) stays, some home health visits, and hospice care, is financed primarily through a 2.9% tax on earnings paid by employers and employees (1.45% each). Higher-income taxpayers (more than $200,000 per individual and $250,000 per couple) pay a higher payroll tax on earnings (2.35%). Payroll taxes accounted for 90% of Part A revenue in 2021.
- Part B, which covers physician visits, outpatient services, preventive services, and some home health visits, is financed primarily through a combination of general revenues (73% in 2021) and beneficiary premiums (25%) (and 2% from interest and other sources). Beneficiaries with annual incomes over $97,000 per individual or $194,000 per couple pay a higher, income-related Part B premium reflecting a larger share of total Part B spending, ranging from 35% to 85% (Figure 9).
- Part D, which covers outpatient prescription drugs , is financed primarily by general revenues (74%) and beneficiary premiums (15%), with an additional 11% of revenues coming from state payments for beneficiaries enrolled in both Medicare and Medicaid. Higher-income enrollees pay a larger share of the cost of Part D coverage, as they do for Part B.
Medicare Advantage Is Not Separately Financed
The Medicare Advantage program (sometimes referred to as Part C) does not have its own separate revenue sources. Funds for Part A benefits provided by Medicare Advantage plans are drawn from the Medicare HI trust fund (accounting for 42% of Medicare Advantage spending on Part A and B benefits in 2021). Funds for Part B and Part D benefits are drawn from the Supplementary Medical Insurance (SMI) trust fund. Beneficiaries enrolled in Medicare Advantage plans pay the Part B premium and may pay an additional premium if required by their plan. In 2022, 69% of Medicare Advantage enrollees pay no additional premium.
Assessing Medicare’s Financial Condition
Medicare’s financial condition can be assessed in different ways, including comparing various measures of Medicare spending—overall or per capita—to other spending measures, such as Medicare spending as a share of the federal budget or as a share of GDP, as discussed above, and estimating the solvency of the Medicare Hospital Insurance (Part A) trust fund.
The Medicare Hospital Insurance Trust Fund Faces Solvency Challenges
The solvency of the Medicare Hospital Insurance trust fund, out of which Part A benefits are paid, is one way of measuring Medicare’s financial status, though because it only focuses on the status of Part A, it does not present a complete picture of total program spending. The solvency of Medicare in this context is measured by the level of assets in the Part A trust fund. In years when annual income to the trust fund exceeds benefits spending, the asset level increases, and when annual spending exceeds income, the asset level decreases. When spending exceeds income and the assets are fully depleted, Medicare will not have sufficient funds to pay all Part A benefits for the full year.
Each year, Medicare’s actuaries provide an estimate of the year when the asset level is projected to be fully depleted. In the 2022 Medicare Trustees report, the actuaries projected that the Part A trust fund will be depleted in 2028 , six years from now. This is a modest improvement from the projection in the 2021 Medicare Trustees report, when the depletion date was projected to be 2026 , based primarily on projections of higher revenues from payroll taxes resulting from higher employment and wage growth. Since 1990, the Trustees have projected that the Medicare Part A trust fund will come within six years of depletion six times (Figure 10).
The actuaries estimate that in 2028, Medicare will be able to cover almost all of Part A benefits spending with revenues plus the small amount of assets remaining at the beginning of the year, and just under 90% with revenues alone in 2029 through 2031, once the assets are depleted. Over a longer 75-year timeframe, the Medicare Trustees estimate that it would take either an increase of 0.70% of taxable payroll (from 2.9% to 3.6%) or a 15% reduction in benefit payments to bring the Part A trust fund into balance.
The Solvency of the Part A Trust Fund Is Affected by Several Factors
In addition to legislative and regulatory changes that affect Part A spending (including utilization of services and payments for services provided by hospitals, skilled nursing facilities, and other providers, and for Part A services covered by Medicare Advantage plans) and revenues, Part A trust fund solvency is affected by:
- The level of growth in the economy , which affects Medicare’s revenue from payroll tax contributions: economic growth that leads to higher employment and wages boosts revenue to the trust fund, while an economic downturn can have the opposite effect.
- Overall health care spending trends : higher health care price and cost growth can lead to higher spending for services covered under Medicare Part A, which could hasten the depletion date, while moderation in the growth of prices and costs could slow spending growth.
- Demographic trends : this includes the aging of the population, which is leading to increased Medicare enrollment , especially between 2010 and 2030 when the baby boom generation reaches Medicare eligibility age; a declining ratio of workers per beneficiary making payroll tax contributions, which means lower revenue; and other factors, such as fertility rates and immigration.
While Part A is funded primarily by payroll taxes, benefits for Part B physician and other outpatient services and Part D prescription drugs are funded by general revenues and premiums paid for out of separate accounts in the Supplementary Medical Insurance (SMI) trust fund. The revenues for Medicare Part B and Part D are determined annually to meet expected spending obligations, meaning that the SMI trust fund does not face a funding shortfall, in contrast to the HI trust fund. But higher projected spending for benefits covered under Part B and Part D will increase the amount of general revenue funding and beneficiary premiums required to cover costs for these parts of the program in the future.
Impact of COVID-19 on Medicare Spending and Financing
According to the Medicare Trustees, the COVID-19 pandemic has had a significant impact on Medicare spending and financing , and some effects are expected to continue for several years. In terms of revenues, the pandemic initially resulted in a substantial increase in unemployment that caused a drop in payroll tax revenue to the HI trust fund. Spending was affected by new outlays for COVID-19 treatment, testing , and vaccine administration , plus accelerated and advance payments to providers, but this higher spending was more than offset by a steep reduction in spending on non-COVID services, as utilization dropped sharply in 2020. While utilization picked up again in 2021, it remained lower than expected that year. In addition, beneficiaries who died of COVID-19 had higher costs pre-pandemic than the average Medicare beneficiary, and the lower morbidity among the surviving Medicare population contributed to modestly lower costs in 2020 and 2021, according to the Medicare Trustees.
Moving forward, the Trustees project that the spending effects of the pandemic will not have a large effect on the financial status of the Medicare program beyond 2028. Accelerated and advance payments are expected to be fully repaid by the end of 2022. A rebound in employment since the early days of the pandemic has bolstered payroll tax revenue in the short term, while Medicare spending trends are expected to return to pre-pandemic levels in 2024 as beneficiaries seek care that was deferred in 2020 and 2021, which in fact may lead to more intensive and costly services. The morbidity effect associated with deaths due to COVID-19 is expected to decrease over time and end in 2028.
The Future Outlook
Over the longer term, the Medicare program faces financial pressures associated with higher health care costs, growing enrollment, and an aging population. Growth in Medicare spending places pressure on the federal budget, contributes to the depletion of the Part A trust fund, and results in higher Medicare premiums, deductibles, and cost sharing paid by beneficiaries.
A number of changes to Medicare have been proposed in the past to address Medicare’s fiscal challenges, including options such as raising the age of Medicare eligibility and transitioning Medicare to a premium support system. More recently, Congress passed the Inflation Reduction Act of 2022 , which aims to control the growth in Medicare prescription drug spending by requiring the federal government to negotiate drug prices in Medicare and requiring drug manufacturers to pay rebates for drug price increases faster than inflation, among other changes. To sustain Medicare for the long run, policymakers may consider adopting broader changes to the program that could include both changes in payments to health care providers and Medicare Advantage plans or reductions in benefits, and additional revenues, such as payroll tax increases or new sources of tax revenue.
At the same time, proposals that could increase Medicare spending are also being discussed, or have been adopted, including policies related to provider payments and Medicare benefit improvements. For example, the recently-enacted Consolidated Appropriations Act, 2023 includes several Medicare spending provisions, such as a reduction in the scheduled physician payment cut for 2023 from 4.5% to 2%, increases in payments to certain hospitals, an extension of Medicare telehealth coverage through 2024, and improvements in Medicare coverage of mental health services. Spending on these provisions will be offset in part by extending the 2% Medicare payment sequestration, currently set to expire in 2031, partway into fiscal year 2032. In addition, policymakers have expressed interest in other policies that could increase Medicare spending, such as enhancing Medicare’s benefit package by adding coverage of vision, hearing, and dental care, adding an out-of-pocket spending cap to traditional Medicare, making permanent Medicare coverage of telehealth, and strengthening financial protections for low-income beneficiaries.
While the prospects for proposals that would affect Medicare spending and financing over the long term are unknown, evaluating such changes will involve a consideration of their effects on federal expenditures, the Medicare program’s finances, and beneficiaries, health care providers, and taxpayers.
This work was supported in part by Arnold Ventures. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.
- Medicare's Future
- Medicare Advantage
- Federal Budget
- Medicare Part D
Also of Interest
- FAQs on Medicare Financing and Trust Fund Solvency
- Medicare Advantage 2023 Spotlight: First Look
- An Overview of the Medicare Part D Prescription Drug Benefit
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CMS Newsroom
Search cms.gov.
- Physician Fee Schedule
- Local Coverage Determination
- Medically Unlikely Edits
- Overview of rules & fact sheets
- Provider resources and requirements
- Providers: submit a billing complaint
- Providers: payment resolution with patients
- Plans and issuers resources and requirements
- Independent Dispute Resolution Reports
- Privacy policies
- About independent dispute resolution
- Tips for disputing parties
- Apply to be certified
- List of certified organizations
- Submit petition to deny entity certification
- Submit petition to revoke entity certification
- Consumer Advocate Toolkit
- Know your rights
Ending Surprise Medical Bills
Learn how providers, facilities, plans and issuers can comply with surprise billing protections and resolve out-of-network payment disputes
No Surprises Act
Policies & resources.
Review rules and fact sheets on what No Surprises rules cover, and get additional resources with more information.
Resolving out-of-network payment disputes
Learn about out-of-network payment disputes between providers and health plans and how to start the independent dispute resolution (IDR) process, apply to become a certified independent dispute resolution entity, or submit a petition on an applicant or to revoke certification of a current IDR entity.
Learn about or start a payment dispute Tips for disputing parties Become a dispute resolution organization List of certified organizations
Submit petition to deny IDRE certification
Submit petition to revoke IDRE certification
Consumers and consumer advocates
Learn about rights and protections for consumers to end surprise bills and remove consumers from payment disagreements between their providers, health care facilities and health plans.

IMAGES
VIDEO
COMMENTS
The Provider and Statistical Reimbursement (PS&R) System is a key tool for institutional healthcare providers, Medicare Administrative Contractors (MACs) and CMS. The system accumulates statistical and reimbursement data applicable to the processed and finalized Medicare Part A claims. This data is summarized in various reports, which are used ...
The PS&R Redesign is now available. Providers that file cost reports are required to register for the PS&R system through Individuals Authorized Access to the Centers for Medicare & Medicaid Services (CMS) Computer Services (IDM) to obtain the PS&R reports. The PS&R Redesign will be utilized for all cost reports with fiscal years ending January ...
PS&R Quick Guide - Provider Page: 1 Version 3.0 Last Update: 11/18/2016 . Provider Statistical and Reimbursement System (PS&R) Quick Guide - Providers V3.0 . You must produce the Summary PS&R reports needed to file your cost report ending on or after January 31, 2009. There are many variations of report requests that can be made in
organization for access to the PS&R system. Note -The SO will delegate PS&R access to the "PS&R Users". Once the SO is approved, the PS&R Users should complete the following in order to access the PS&R system: EIDM - In the EIDM website, https://portal.cms.gov/, select New User Registration and complete the questions.
The PS&R system is comprised of many web pages that allow Medicare Part A providers to request the generation of summary and detail reports for inpatient and outpatient services. The reports that can be generated by a specific user are determined by the user's access authority assigned to the user ID. The PS&R system provides the following:
The Provider Summary reports should be used by a provider when preparing the Medicare cost report. CMS has implemented the new redesigned PS&R system effective for cost reporting periods ending on or after January 31, 2009. Providers with cost reports ending after this will obtain the PS&R reports needed to file the Medicare cost report by ...
An approved PS&R User can order reports. Access to the PS&R is controlled through the Enterprise Identity Management (EIDM) website. If access i s needed, refer to the article, PS&R - Obtain Access through EIDM, for instructions. A.Login to PS&R Use the following link to login to the PS&R: https://psr-ui.cms.hhs.gov/psr-ui
The Provider and Statistical Reimbursement (PS&R) System is a key tool for institutional healthcare providers, Medicare Administrative Contractors (MACs) and CMS. The system accumulates statistical and reimbursement data applicable to the processed and finalized Medicare Part A claims. This data is summarized in various reports, which are used ...
The Enterprise Portal is a gateway that provides access to different Centers for Medicare & Medicaid Services (CMS) healthcare-based applications. ... CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore,Maryland 21244-1850. OK Updated ... PS&R/STAR Close. Provider Statistical and Reimbursement/System ...
PS&R Reports (cont.) PS&R system is Web-based, accessed through IDM Allows all users to access data specific to their organization, at any time Providers are responsible for obtaining PS&R reports needed to file Medicare cost report directly from CMS PS&R System • MACs should not be supplying providers PS&Rs
The PDF option will produce the PS&R in a report format. The CSV option will produce a file that can be loaded into the cost report software. If in doubt, order both. ... Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ...
How to Pull the PS&R for your Medicare Cost Report PS&R stands for Provider Statistical and Reimbursement System. It's wise to pull a PS&R report when you submit information for your Medicare Cost Report. For cost reports submitted for fiscal years beginning on or after October 2014, the PS&R report will be required. Here's how to pull it: 1.
A9: The on-screen registration process should take no more than 10 minutes for the initial registration of an organization and a security official. The remainder of the time is taken up by postal delays (documents being mailed), followed by the amount of time it takes for external user services (EUS) to process the application (which itself varies based on the number of applications being ...
Provider Statistical & Reimbursement (PS&R) Report; If a submitted cost report is considered unacceptable, Noridian (we) will return it to the provider with a letter detailing the reasons for rejection. If the cost report due date has expired, we will institute withholding of the interim payments and/or assessment of interest and penalties and ...
Medicare CAP report. An approved PS&R User can order reports. Access to the PS&R is controlled through the Enterprise Identity Management (EIDM) website. If access is needed, refer to the article, PS&R - Obtain Access through EIDM, for instructions. A. Login to PS&R Use the following link to login to the PS&R: https://psr-ui.cms.hhs.gov/psr-ui
The Provider and Statistical Reimbursement (PS&R) System is a key tool for institutional healthcare providers, Medicare Administrative Contractors (MACs) and CMS. The system accumulates statistical and reimbursement data applicable to the processed and finalized Medicare Part A claims. This data is summarized in various reports, which are used ...
You can produce all PS&R summary reports using the following steps: • Enter Service Dates -- the system will default to your cost report period. If one full cost report period is needed, you will not need to change these amounts. However, you may change the date ranges if needed. Note: If period "splits" are needed for cost reporting, you ...
Units/Census. Cost Report Reference Deduct & Charges Coins Net Reimb. 11A INPATIENT - PART A (MSP-LCC) 11K INPATIENT REHABILIATION - PPS INTERIM BILLS 11R INPATIENT REHABILIATION - PART A 11U INPATIENT PSYCHIATRIC - PART A 110 INPATIENT - PART A 118 INPATIENT - PART A MANAGED CARE. 119 INPATIENT - PPS INTERIM BILLS 12A INPATIENT - PART B (MSP ...
The Provider and Statistical Reimbursement (PS&R) System is a key tool for institutional healthcare providers, Medicare Administrative Contractors (MACs) and CMS. The system accumulates statistical and reimbursement data applicable to the processed and finalized Medicare Part A claims. This data is summarized in various reports, which are used ...
Instructions for obtaining & downloading the PS&R: Download CMS Quick Guide. Visit: https://psr-ui.cms.hhs.gov/psr-ui. Login using your userid and password. Select All Providers. Select All Reports available. Select Service dates - using cost report begin and end dates.
The PS&R provides the following: • All providers can request their own summary reports directly in the system. • Users can define report selection criteria such as the report types, report numbers, service types and date ranges to include in the reports. • Providers can submit online requests for detail reports.
Medicare spending on Part A, Part B, and Part D benefits in 2021 totaled $829 billion, up from $541 billion in 2011, according to the Medicare Trustees (Figure 3). These amounts reflect gross ...
You can use this tool to find and compare different types of Medicare providers (like physicians, hospitals, nursing homes, and others). Use our maps and filters to help you identify providers that are right for you. Find Medicare-approved providers near you & compare care quality for nursing homes, doctors, hospitals, hospice centers, more.
This report shows in detail claims accepted by the PS&R system with totals by provider within report type. All claims processed by the PS&R system will be reflected on this report. It can serve as an audit trail for claims activities and for comparison to the summary report. FREQUENCY: Upon request.
Sponsor: Rep. Kelly, Mike [R-PA-16] (Introduced 06/12/2024) Committees: House - Ways and Means; Energy and Commerce: Latest Action: House - 06/12/2024 Referred to the Committee on Ways and Means, and in addition to the Committee on Energy and Commerce, for a period to be subsequently determined by the Speaker, in each case for consideration of such provisions as fall within the jurisdiction of ...
The five Ps. The five Ps are product, price, place, promotion, and people . Today, many marketers use the five Ps over the four Ps because they center the experiences of customers and staff in the marketing process. Typical considerations include how a customer behaves, their product experience, and overall satisfaction with the business.
The Medicare Cost Report e-Filing system (MCReF) provides all Medicare Part A providers the ability to electronically file 100% of their MCR package, including all supporting documentation, directly to their MAC for Fiscal Year Ends on or after 12/31/2017. Successful MCReF submissions will immediately be received by the provider's MAC to ...
04/09/2024 12:19 PM. Help with File Formats and Plug-Ins. Policies & resourcesReview rules and fact sheets on what No Surprises rules cover, and get additional resources with more information.