- Skip to content

State Resources
National Resources
Nursing Organizations
- MNWC Initiatives

Maryland Nursing Workforce Center
- NextGen NCLEX
Faculty Case Studies
The purpose of this project was to develop a repository of NextGen NCLEX case studies that can be accessed by all faculty members in Maryland.
Detailed information about how faculty members can use these case students is in this PowerPoint document .
The case studies are in a Word document and can be modified by faculty members as they determine.
NOTE: The answers to the questions found in the NextGen NCLEX Test Bank are only available in these faculty case studies. When students take the Test Bank questions, they will not get feedback on correct answers. Students and faculty should review test results and correct answers together.
The case studies are contained in 4 categories: Family (13 case studies), Fundamentals and Mental Health (14 case studies) and Medical Surgical (20 case studies). In addition the folder labeled minireviews contains PowerPoint sessions with combinations of case studies and standalone items.
Family ▾
- Attention Deficit Hyperactivity Disorder - Pediatric
- Ectopic Pregnancy
- Febrile Seizures
- Gestational Diabetes
- Intimate Partner Violence
- Neonatal Jaundice
- Neonatal Respiratory Distress Syndrome
- Pediatric Hypoglycemia
- Pediatric Anaphylaxis
- Pediatric Diarrhea and Dehydration
- Pediatric Intussusception
- Pediatric Sickle Cell
- Postpartum Hemmorhage
- Poststreptococcal Glomerulonephritis Pediatric
- Preeclampsia
Fundamentals and Mental Health ▾
- Abdominal Surgery Postoperative Care
- Anorexia with Dehydration
- Catheter Related Urinary Tract Infection
- Deep Vein Thrombosis
- Dehydration Alzheimers
- Electroconvulsive Therapy
- Home Safety I
- Home Safety II
- Neuroleptic Maligant Syndrome
- Opioid Overdose
- Post Operative Atelectasis
- Post-traumatic Stress
- Pressure Injury
- Substance Use Withdrawal and Pain Control
- Suicide Prevention
- Tardive Dyskinesia
- Transfusion Reaction
- Urinary Tract infection
Medical Surgical ▾
- Acute Asthma
- Acute Respiratory Distress
- Breast Cancer
- Chest Pain (MI)
- Compartment Syndrome
- Deep Vein Thrombosis II
- End Stage Renal Disease and Dialysis
- Gastroesphageal Reflux
- Heart Failure
- HIV with Opportunistic Infection
- Ketoacidosis
- Liver Failure
- Prostate Cancer
- Spine Surgery
- Tension Pneumothorax
- Thyroid Storm
- Tuberculosis
Community Based ▾
Mini Review ▾
- Comprehensive Review
- Fundamentals
- Maternal Newborn Review
- Medical Surgical Nursing
- Mental Health Review
- Mini Review Faculty Summaries
- Mini Review Training for Website
- Mini Reviews Student Worksheets
- Pediatric Review
- OJIN Homepage
- Table of Contents
- Volume 23 - 2018
- Number 2: May 2018
- Evidence Psychiatric Mental Health Interventions
Evidence for Psychiatric and Mental Health Nursing Interventions: An Update (2011 through 2015)
Dr. Bekhet is an Associate Professor at Marquette University College of Nursing in Milwaukee, WI. She received aBSN and MSN from Alexandria University in Alexandria, Egypt. She received a PhD from Case Western Reserve University (CWRU) in Cleveland, OH. Her clinical experience in psychiatric nursing is with persons having schizophrenia, bipolar disorders, obsessive-compulsive disorders, and depressive disorders. She has taught psychiatric mental health nursing to undergraduate and direct entry students. She has also advised PhD students. Dr. Bekhet’s program of research focuses on the effects of positive cognitions and resourcefulness in overcoming adversity in vulnerable populations. Her research has been funded by Sigma Theta Tau International; American Psychiatric Nursing Foundation; International Society of Psychiatric Mental Health Nurses; and Marquette University. She is a past recipient of a Midwest Nursing Research Society Mentorship Grant Award, and has received the Award for Excellence from the CWRU Nursing Alumni Association in 2011 and the Way-Klinger Young Scholar Award from Marquette University in 2012. More recently, she was awarded the 2014 research award from the International Society of Psychiatric Mental Health Nurses. Dr. Bekhet has published numerous articles and presented numerous papers and posters at regional, national, and international conferences.
Dr. Zauszniewski is the Kate Hanna Harvey Professor in Community Health Nursing, and Director of the PhD in Nursing Program at the Case Western Reserve University (CWRU), Cleveland, OH. She received a PhD and MSN from CWRU, Cleveland, OH; a MA in Counseling and Human Services from John Carroll University, Cleveland, OH; a BA in psychology from Cleveland State University, Cleveland, OH; and a diploma in nursing from St. Alexis Hospital School of Nursing, Cleveland, OH. She has practiced nursing for 42 years, including 33 years in the field of psychiatric-mental health nursing; she has experience as a staff nurse, clinical preceptor, head nurse, supervisor, patient care coordinator, nurse educator, and nurse researcher, and is board certified by the American Nurses Credentialing Center (ANCC). Her program of research focuses on the identification of factors and strategies to prevent depression and to preserve healthy functioning across the lifespan. She is best known for her research examining the development and testing of nursing interventions to teach resourcefulness skills to family caregivers. She has received research funding from the National Institutes of Nursing Research and Aging; the National Institutes of Health; Sigma Theta Tau International; the American Nurses Foundation; Midwest Nursing Research Society; and the State of Ohio Board of Regents.
Denise Matel-Anderson is a doctoral student at Marquette University College of Nursing in Milwaukee, WI. She holds an Advanced Practice Nurse Prescriber license, and is currently working on a PhD in nursing with a focus on mental health. She has three publications in mental health nursing journals. Ms. Matel-Anderson currently lectures at Carroll University, Waukesha, WI, in the undergraduate mental health nursing theory course, and serves as a nurse practitioner on the medical team at an acute mental health facility.
Jane Suresky is an Adjunct Assistant Professor at the Frances Payne Bolton School of Nursing of Case Western Reserve University (CWRU) in Cleveland, OH. She has received DNP and MSN degrees from CWRU, and a BSN degree from Cleveland State University, Cleveland, OH. Her clinical experience in psychiatric nursing covers the areas of psychobiological research, adolescent dual diagnosis, and mood disorders. She has taught psychiatric mental health nursing to undergraduate and graduate students. In addition, she has been involved in nursing research that focuses on the stress of the female family members of the severely mentally ill.
Mallory Stonehouse recently graduated with a Master of Science in Nursing degree from Marquette University in Milwaukee, WI, where she completed the adult-older adult, primary care, nurse practitioner program. She is a registered nurse at Froedtert Community Memorial Hospital in Wisconsin, where she works on the Behavioral Health Unit. Ms. Stonehouse holds a Bachelor of Arts degree in psychology.
- Figures/Tables
This state-of-the-evidence review summarizes characteristics of intervention studies published from January 2011 through December 2015, in five psychiatric nursing journals. Of the 115 intervention studies, 23 tested interventions for mental health staff, while 92 focused on interventions to promote the well-being of clients. Analysis of published intervention studies revealed 92 intervention studies from 2011 through 2015, compared with 71 from 2006 through 2010, and 77 from 2000 through 2005. This systematic review identified a somewhat lower number of studies from outside the United States; a slightly greater focus on studies of mental health professionals compared with clients; and a continued trend for testing interventions capturing more than one dimension. Though substantial progress has been made through these years, room to grow remains. In this article, the authors discuss the background and significance of tracking the progress of intervention research disseminated within the specialty journals, present the study methods used , share their findings , describe the intervention domains and nature of the studies , discuss their findings , consider the implications of these studies , and conclude that continued track of psychiatric and mental health nursing intervention research is essential.
Key Words: best practices, evidence-based practice, psychiatric nursing journals, psychiatric nursing research, published research, research dissemination, research utilization, systematic review, tradition, intervention research
Implementation science is concerned with the translation of research into practice... The past five years have seen a rapidly growing interest in the field of implementation science ( Sorensen & Kosten, 2011 ). Implementation science is concerned with the translation of research into practice; it involves the examination of the challenges and the opportunities for successful, evidence-based changes in practice ( Nilsen, 2015 ). Translating research into practice depends heavily on the dissemination of findings from intervention research to those most likely to use those findings in clinical or community settings. In contrast to implementation, dissemination involves the spread of information about an intervention, for example, through publication of the intervention in professional journals. Dissemination strategies that are actively targeted toward spreading evidence-based findings concerning an intervention may prompt future implementation in clinical practice ( Proctor et al., 2009 ).
Translating research into practice depends heavily on the dissemination of findings from intervention research... Important for psychiatric and mental health nurses, it is critical that implementation of evidence-based findings occurs across multiple settings (i.e., beyond specialty mental healthcare units) to medical settings, such as primary care areas in which mental health services are provided, and to non-specialized settings, such as criminal justice and school systems and community social service agencies, where mental healthcare is delivered (Proctor et al., 2009). However, before implementation can happen, dissemination of findings from well-designed intervention studies that can inform psychiatric and mental health nursing practice is needed.
One of the best mediums for disseminating evidence-based findings in psychiatric and mental health nursing is the professional nursing journals that are most available to practicing psychiatric and mental health nurses. Nursing journals that are specifically designed a specialty are more likely to be read by persons in the given specialty area than are other nursing research journals. Nurses in practice settings, including those at an advanced practice level, may not have access to scientific research journals or may choose not to read them if the research does not appear meaningful for their practice. The goal of this review was to describe the findings from intervention studies disseminated through publication in one of the five psychiatric and mental health nursing specialty journals published from 2011 through 2015.
Background and Significance
Through the years, more psychiatric and mental health nurse researchers have been targeting specialty journals for disseminating findings from intervention research. For example, in previous reviews of intervention studies published in the five major psychiatric and mental health specialty journals, there was a higher percentage of quantitative intervention studies conducted from 2006 through 2010 (84%) than in a similar review conducted from 2000-2005 (64%) ( Zauszniewski, Suresky, Bekhet, & Kidd, 2007 ; Zauszniewski, Bekhet, & Haberlein, 2012 ), indicating increased use of more rigorous, statistical analytic methods in published intervention research over time ( Zauszniewski et al., 2007 ; Zauszniewski et al., 2012 ).
Tracking the progress of intervention research disseminated within the specialty journals in psychiatric and mental health nursing is important for two reasons. First, it provides data to show improvements in dissemination efforts of psychiatric and mental health nurse researchers. Second, it calls attention to the importance for continued dissemination of intervention research to practicing psychiatric and mental health nurses who are in the best positions to implement the findings in practice. Therefore, the purpose of this review of the same, five, peer-reviewed psychiatric and mental health nursing journals, covering 2011 through 2015, was to determine the number and types of intervention studies within the specified review period. For consistency, the same criteria for selecting the intervention studies that were described in the previous review ( Zauszniewski et al., 2012 ) were applied: A study was determined to be an intervention study if nursing strategies, procedures, or practices were examined for effectiveness in enhancing or promoting health or preventing disability or dysfunction ( Kane, 2015 ).
Five peer-reviewed nursing journals, regarded as the most frequently read in the mental health nursing profession, were analyzed for the years 2011 through 2015. The journals included in the analysis were Archives of Psychiatric Nursing ; Issues in Mental Health Nursing ; Journal of the American Psychiatric Nurses Associatio n; Journal of Psychosocial and Mental Health Services; and Perspectives in Psychiatric Care .
Journals were reviewed for the type of intervention study (qualitative or quantitative); the study domain (biological, psychological, or social); and the number of intervention studies found within the journals. After review, the agreed upon intervention studies were extracted and individually analyzed by the co-authors.
There were 832 databased articles published from January 2011 through December 2015. However, only 115 (14%) evaluated or tested psychiatric nursing interventions. Of these 115 intervention studies, 14 tested interventions with nursing students, nine involved nurses and mental health professionals, while 92 focused on interventions to promote mental health in clients of care.
This section describes the findings from the 115 intervention studies included in the review. The 23 studies that included nursing students, nurses, and mental health professional, and the 92 that involved recipients of mental health services or care are presented in this section. First, the research settings in which the 115 studies were conducted, and descriptions of the targeted populations are described. Next, the 23 studies’ designs, purposes, and findings are discussed in detail. Third, the 92 studies that involved recipients of mental health services or care are presented using the categories of the bio-psycho-social framework. Finally, the type of data (quantitative, qualitative, or mixed) are discussed and presented in the table.
Research Settings Sixty-six of the 115 intervention studies were completed in the United States. Five studies each were done in Australia and United Kingdom. Four each were completed in Korea, China, and Turkey; three each in Norway, Canada, and Iran; and two each in Taiwan, Mexico, Sweden, France, and Netherlands. One study each was conducted in Jordan, Europe, Iceland, Pacific Islands, Thailand, Spain, Greece, and Singapore
Targeted Populations Fourteen of the 115 intervention studies involved interventions with nursing students, while nine studies focused on nurses and mental health professionals. Ninety-two of the studies examined the effect of the intervention on the client. Examples of the studies describing each of these groups are described below.
Fourteen of the 23 nursing intervention studies involved undergraduate nursing students. Nursing students . Fourteen of the 23 nursing intervention studies involved undergraduate nursing students. One study was conducted in Australia regarding consumer participation ( Happell, Moxham, & Plantain-Phung, 2011 ). In this study, researchers investigated whether education programs introducing nursing students to mental health nursing lead to more favorable attitudes towards consumer participation in the mental health setting after completing the mental health component of the nursing program. Study participants were in the first semester of the final year of the Bachelor of Nursing program. The study used a within-subject design using two points (pre-and post-educational program implementation). Results indicated that students demonstrated positive attitudes toward consumer participation even before completing the mental health component. Only marginal and non-significant changes were noted at the post-test stage. The authors concluded that the findings were not surprising given the positive scores recorded at baseline (ceiling effect) ( Happell et al., 2011 ). Another study investigated the effect of pedagogy of curriculum infusion on nursing students’ well-being and the improvement of quality of patients’ care ( Riley & Yearwood, 2012 ).
Pedagogy of curriculum infusion involves instilling the university values and mission with a focus on educating the whole person, and encouraging faculty to translate the core mission of the university into practice in the classroom. this can be accomplished through a variety of courses that provide students with opportunities for contemplation, reflective engagement, and also action through volunteerism, service, and study abroad. The ultimate goal of the study was to encourage critical thinking through reflective exercises and group discussion. Results indicated that students who have experienced the curriculum infusion showed an ability to be self-advocates when discussing their work challenges. Also, they were able to identify specific nursing actions for patient safety; to recognize the patient as a partner in care; and to demonstrate respect for patients' uniqueness, values, and desires as evidenced by case analysis and personal reflections ( Riley & Yearwood, 2012 ).
Three intervention studies explored simulation to see its impact on improving the learning experiences of the nursing students. Three intervention studies explored simulation to see its impact on improving the learning experiences of the nursing students ( Kameg, Englert, Howard, & Perozzi, 2013 ; Kidd, Knisley & Morgan, 2012 ; Masters, Kane, & Pike, 2014 ). Different simulations were used in the three studies; all of them were deemed effective. For example, the results of the study conducted by Kidd and colleagues indicated that undergraduate, mental health nursing students perceived that Second Life® virtual simulation was moderately effective as an educational strategy and slightly difficult as a technical program ( Kidd et al., 2012 ). Also, second degree and traditional BSN students found that a tabletop simulation, which was developed as a patient safety activity and involved checking-in a patient admitted to a psychiatric care unit, was a good learning experience and helpful to prepare students for situations they may experience in the workplace ( Masters et al., 2014 ). The third study used a high-fidelity, patient simulation (HFPS) to assess senior level nursing student knowledge and retention of knowledge utilizing three parallel, 30-item Elsevier Health Education Systems, Inc. (HESITM) Custom Exams. Although students’ knowledge did not improve following the HFPS experiences, the findings provided evidence that HFPS may improve knowledge in students who are at risk (defined as those earning less than 850 on HESI exam). Students reported that they viewed this simulation as a positive learning experience ( Kameg et al., 2013 ).
An additional intervention study used a quasi-experimental design to explore perceptions of student nurses toward nurses who are chemically dependent, using a two-group, pretest–posttest design (prior to formal education and after receiving substance abuse education). Results indicated that the student nurses in this study had positive perceptions about nurses who are chemically dependent before the intervention; and the education program appeared to reinforce their existing attitudes. ( Boulton & Nosek, 2014 ).
Mitchell et al. ( 2013 ) investigated the impact of an addiction training program for nurses consisting of Screening, Brief Intervention, and Referral to Treatment (SBIRT), and embedded within an undergraduate nursing curriculum, on students’ abilities to apply an evidence-based screening and brief intervention approach for risky alcohol and drug use in their nursing practice. Results indicated that the SBIRT program was effective in changing the undergraduate nursing students’ self-perceptions of their knowledge, skills, and effectiveness in screening and intervening for hazardous alcohol and drug use. Furthermore, this positive perception was maintained at 30-day follow-up ( Mitchell et al., 2013 ).
Luebbert and Popkess ( 2015 ) investigated the impact of an innovative, active-learning strategy using simulated, standardized patients on suicide assessment skills in a sample of 34 junior and senior baccalaureate nursing students. Additionally, Schwindt, McNelis, and Sharp ( 2014 ) evaluated a theory-based educational program to motivate nursing students to intervene with persons having serious mental illness. Other intervention studies among nursing students focused on improving students' interpersonal relationships; communication competence; empathetic skills; and confidence in performing mental health nursing skills among nursing students ( Choi, Song, & Oh, 2015 ; Choi & Won, 2013 ; Fiedler, Breitenstein, & Delaney 2012 ; Ozcan, Bilgin, & Eracar, 2011 ; Stiberg, Holand, Ostad, & Lorem, 2012 ).
Nursing staff and mental health professionals . Interventions among the nursing staff and mental health professionals accounted for nine of the nursing intervention studies. The majority of these studies were nursing interventions to educate the nursing staff. Educational interventions included: training videos ( Irvine et al., 2012 ); a continuing education course on suicide awareness ( Tsai, Lin, Chang, Yu,& Chou, 2011 ); an education program using simulation ( Usher et al., 2014 ; Wynn, 2011 ); an educational workshop ( White, Hemingway, & Stephenson, 2014 ); training on family-centered care ( Wong, 2014 ); and the impact of the completion of a 26-week trial on nursing staff’s experience for working as a cardio-metabolic health nurse ( Happell et al., 2014 ).
Terry and Cutter ( 2013 ) used a mixed methods pilot study to evaluate the effect of education on confidence in assessing and addressing physical health needs following attendance at a module titled “Physical Health Issues in Adult Mental Health Practice.” The majority of the participants had studied at the university during the previous five years, at either the diploma or the degree level. Results showed improvement in confidence scores for all study participants following the module; participants were able to identify new knowledge and perspectives for practice change.
Results indicated that care zoning increased the nursing team’s capacity to share information and to communicate patients’ clinical needs... Finally, the study conducted by Taylor and colleagues ( 2011 ) used a pragmatic approach to increase understanding of the clinical-risks needs in acute in-patient unit settings. Each patient was classified according to three zoning levels using a traffic light system: red (high level of risk), amber (medium/moderate level of risk), and green (low level of risk). The level of risk was based on multiple factors including clinical judgment and team discussion ( Taylor et al., 2011 ). Results indicated that care zoning increased the nursing team’s capacity to share information and to communicate patients’ clinical needs, as well as to enhance their abilities to address complex clinical presentation and to seek support when needed.
Intervention Domains
Ninety-two of the studies examined the effect of an intervention for the client. In the following section, we will describe the intervention domains of these 92 articles and provided examples. Additional detail is included in the Table .
Interventions in the Biological Domain Eight interventions were in the biological domain. Study interventions included yoga, dancing, diet, medication, electroconvulsive therapy (ECT), exercise, walking, and educational intervention on metabolic syndrome. Four interventions used various kinds of exercises, including walking ( Beebe, Smith, Davis, Roman, & Burke, 2012 ); dancing ( Emory, Silva, Christopher, Edwards, & Wahl, 2011 ); yoga ( Kinser, Bourguigion, Whaley, Hauenstein, & Taylor, 2013 ); and group exercise program ( Stanton, Donohue, Garnon, & Happell, 2015 ). Diet was also used as an intervention. For example, Lindseth, Helland, and Caspers ( 2015 ) used dietary intake of a high or low tryptophan diet as an intervention. Results indicated improvement in patients’ mood, depression, and anxiety for those consuming a high tryptophan diet as compared to those who consumed a low tryptophan diet ( Lindseth et al. 2015 ). A third category within the biological domain was the use of medications as an intervention. One study tested the use of different psychotropic medications for patients diagnosed with schizophrenia ( Zhou et al., 2014 ). A second used ECT as a treatment modality and measured scores on the Montgomery Asberg (MA) Depression Rating Scale before and after the course of treatment ( Pulia, Vaidya, Jayaram, Hayat, & Reti, 2013 ). A final category was an educational program on metabolic syndrome provided to mental health counselors who performed intake assessments on patients newly admitted to two outpatient mental health facilities. ( Arms, Bostic, & Cunningham, 2014 ). Prior to the intervention, neither facility screened for metabolic syndrome at intake or referred patients with a body mass index (BMI) >25 for medical evaluation. Following the intervention, 53 of 132 patients had a documented BMI >25, and 47 of 53 patients were referred to a primary care provider for evaluation. These findings suggested that screening for metabolic syndrome and associated illnesses will increase the rate of detection of chronic conditions ( Arms et al., 2014 ).
Interventions in the Psychological Domain ...the psychological domain had the largest number of intervention studies. Compared to the other domains, the psychological domain had the largest number of intervention studies. Twenty-four of the 92 total intervention studies extracted were in the psychological domain. The intervention studies in the psychological domain included emotion, behavior, and cognition (e.g., counseling) in addition to studies that focused on behavior therapy and psychoeducational programs. Examples of psychological domains studies included: counseling regarding tobacco cessation treatment ( Battaglia, Benson, Cook, & Prochazka, 2013 ); counseling regarding sexual assault ( Lawson, Munoz-Rojas, Gutman, & Siman, 2012 ); resourcefulness training intervention for relocated older adults ( Bekhet, Zauszniewski, & Matel-Anderson, 2012 ); and resilience training and cognitive therapy in women with symptoms of depression aged 18-22 years of age ( Zamirinejad, Hojjat, Golzari, Borjali, & Akaberi, 2014 ) Please see the Table for further details.
One study utilizing an intervention from the psychological domain examined a brief, six- session, cognitive-behavioral intervention among patients with alcohol dependence and depression. The researchers used a quasi-experimental design with a control group and pretest, posttest, and follow-up assessments. Results indicated that the mean depression scores decreased significantly in both the experimental (n = 33) and control groups (n = 27) at the one-month follow-up (Week 7). However, only the experimental group showed significant differences in their mean depression scores between pre- and posttest. At Week 7, the experimental group showed significantly lower mean depression scores than the control group ( Thapinta, Skulphan, & Kittrattanapaiboon, 2014 ).
Interventions in the Social Domain The social domain considers the patients’ environment and its impact on patients’ adjustment and responses to stress. Nine studies involved use of the social domain in their interventions. The social domain considers the patients’ environment and its impact on patients’ adjustment and responses to stress. Interventions in this domain included family, friends, and social support, as well as community interactions ( Zauszniewski et al., 2012 ). One example of an intervention in the social domain involved studying the long-term impact of safe shelter and justice services on abused women’s ability to function after receiving services ( Koci, 2014 ). Another example of an intervention study in the social domain was a pilot, randomized, controlled trial study by Simpson, Quigley, Henry, and Hall ( 2014 ). In this study, the researchers evaluated the selection, training, and support of a group of peer workers recruited to provide support to service users discharged from acute psychiatric unites in London, comparing peer support with usual care ( Simpson et al., 2014 ) (see Table ). A third example in the social domain was designed to help participants successfully transfer from hospitals to the community by enhancing staff participation, creating/maintaining supportive ward milieus, and supporting managers throughout the implementation process ( Forchuk et al., 2012 ).
The study conducted by Horgan, McCarthy, and Sweeny ( 2013 ) was another example of research in the social domain. This study included designing a website for people ages 18-24 who were experiencing depressive symptoms. The website provided a forum to allow participants to offer peer support to each other; it also provided information on depression and links to other supports ( Horgan et al., 2013 ).
Combinations of the Domains Many studies used more than one domain as interventions. Many studies used more than one domain as interventions (see Figure ). Almost half (49%) of the 92 reviewed studies (n = 45) tested an intervention that included two domains. Thirty studies were psychosocial, twelve were biopsychological, and three were biosocial. In addition, six studies (7%) tested intervention with all three domains (biopsychosocial). In the following section, one study from each combination will be described. Again, additional information is provided in the Table .
Figure. Psychiatric Nursing Interventions: Examples of Domains and Their Total Numbers

Iskhandar Shah and colleagues ( 2015 ) studied and tested an intervention from the biopsychological domain using a single-group, pretest–posttest, quasi-experimental research design. Their intervention program included three daily, one-hour sessions incorporating psychoeducation and virtual-reality-based relaxation practice in a convenience sample of twenty-two people with mental disorders. Results indicated that those who completed the program had significantly lowered subjective stress, depression, and anxiety, along with increased skin temperature, perceived relaxation, and knowledge ( Iskhandar Shah et al., 2015 ).
Pedersen, Nordaunet, Martinsen, Berget, and Braastad ( 2011 ) studied an intervention from the biosocial domain. Their intervention program tested the impact of a 12-week, farm-animal-assisted intervention consisting of work and contact with dairy cattle, on levels of anxiety and depression in a sample of fourteen adults diagnosed with clinical depression. The twice-a-week program involved video recording each participant twice during the intervention. Participants were given the choice of either choosing their work tasks with animals (e.g., milking, feeding, hand feeding, moving animals) or the choice of spending their time in contact with farm animals (e.g., patting, stroking, and other non-work-related physical contact). Results indicated that levels of anxiety and depression decreased, and self-efficacy increased during the intervention. Interaction with farm animals (social) via work tasks showed a greater potential for improved mental health than merely animal contact, but only when progress in working skills (biological aspect) was achieved, indicating the role of coping experiences for a successful intervention. ( Pedersen et al., 2011 ).
The NP often accompanied the participant to medical and mental health appointments... Chandler, Roberts, and Chiodo ( 2015 ) conducted a study in the psychosocial domain that examined the feasibility and potential efficacy of implementing a four-week, empower-resilience intervention (ERI) to build resilience capacity with young adults who have identified adverse childhood experiences. The intervention included using mindfulness-based stress reduction (psychological domain) and social support with guided peer and facilitator interaction (social domain). The study randomly assigned a purposive sample of female undergraduate students between the ages of 18 and 24 years of age into two groups: intervention (n = 17) and control (n = 11), and used a pretest–posttest design to compare symptoms, health behaviors, and resilience before and after the intervention program. Results indicated that subjects in the intervention group reported greater building of strengths, reframing resilience, and creating support connections as compared with the control group ( Chandler et al., 2015 ).
Interventions in the biopsychosocial domain include all three components (biological, psychological, and social). There were six studies that included all three domains in their interventions. Hanrahan, Solomon, and Hurford ( 2014 ) used a randomized controlled design to deliver a transitional care model (TCM) intervention to patients with serious mental illness who were transferring from hospital care to home. The intervention group (n = 20) received the TCM intervention delivered by a psychiatric nurse practitioner (NP) for 90 days post hospitalization and the control group (n = 20) received the usual care. The intervention by the nurse practitioner included helping the patients adapt to the home by focusing on managing problem behaviors and physical problems, managing risk factors to prevent further cognitive or emotional decline, promoting adherence to therapies, and integrating physical and mental care approaches. The NP often accompanied the participant to medical and mental health appointments to facilitate communication, translate information to specialty providers, and advocate for the participant ( Hanrahan et al., 2014 ).
Table. Research Classifications by Domains, Design, and Type of Data Used
|
|
|
|
|
|
|
| Beebe et al. ( ) | Walking program | Self-efficacy for exercise was significantly higher in experimental participants than in controls after intervention. | Random assignment, researchers blinded, pre-/ posttest | Quantitative | Biological |
| Emory et al. ( ) | Line dancing program | The fall rate post intervention was 2.8% compared with 3.2% before intervention. | Pretest-posttest | Quantitative | Biological |
| Kinser, Bourguignon, Taylor, & Steeves ( ) | 8-week yoga intervention | Yoga served as a self-care technique for the stress and ruminative aspects of depression. Yoga facilitated connectedness and helped in sharing experiences in a safe environment. | Qualitative data through daily logs in which participants documented their feelings before and after daily home yoga practice. | Qualitative | Biological |
| Stanton et al. ( ) | Evaluate satisfaction with inpatient group activities designed to assist with recovery, including cognitive behavioral therapy, creative expression, relaxation, reflection/ discussion, and exercise. | More inpatients (50%) rated exercise as “excellent” compared with all other activities. Nonattendance rates were lowest for cognitive behavioral therapy (6.3%), highest for the relaxation group (18.8%), and for the group exercise program (12.5%). | Site evaluation upon discharge; evaluation survey was completed anonymously. | Quantitative | Biological |
| Lindseth et al. ( ) | Dietary intake of high or low tryptophan diet. | Improvement in patients’ mood, depression, and anxiety for those consuming a high tryptophan diet as compared to those who consumed a low Tryptophan. | Within-subjects crossover-designed study, random assignment to control /experimental | Quantitative | Biological |
| Zhou et al. ( ) | Examine the predictive value of time-based prospective memory (TBPM) and other cognitive components for remission of positive symptoms in first episode of schizophrenia. | Higher scores, reflecting better TBPM, at baseline were more likely to achieve remission after 8 weeks of optimized antipsychotic treatment. | Random assignment, pretest-posttest | Quantitative | Biological |
| Pulia et al. ( ) | ECT technique. Two changes were introduced: (a) switching the anesthetic agent from propofol to methohexital, and (b) using a more aggressive ECT charge dosing regimen for right unilateral (RUL) electrode placement. | Compared with patients receiving ECT with RUL placement prior to the changes, patients who received RUL ECT after the changes had a significantly shorter inpatient Length of stay (27.4 versus 18 days, p = 0.028). | A retrospective analysis was performed on two inpatient groups treated on Mood Disorders Unit. | Quantitative | Biological |
| Arms et al. ( ) | Education session about metabolic syndrome for clinicians. | No difference in educational pre-posttest scores. Clinicians increased referral to Primary Care Provider for BMI >25. | Pretest/posttest, chart audit | Quantitative | Biological |
| Battaglia et al. ( ) | Counseling regarding tobacco cessation treatment designed to increase patient engagement while hospitalized. | The intervention had minimal impacts on internalized stigma and personal recovery. Peer support demonstrated positive effects on internalized stigma and personal recovery. | Pilot study, single group, unblinded intervention trial | Quantitative and Qualitative | Psychological |
| Lawson et al. ( ) | “Men's Program”- rape prevention intervention. | Promising change in attitudes about rape beliefs and bystander behaviors in Hispanic males exposed to the educational intervention. | Exploratory study, mixed methods design, pre- and post-test, focus group transcription thematic coding | Quantitative and Qualitative | Psychological |
| Bekhet, Zauszniewski, & Matel-Anderson ( ) | Resourcefulness training (RT) for relocated older adults assessing necessity, acceptability, feasibility, safety and effectiveness of RT. | 76.3% of the older adults scoring below 120, indicating a strong need for RT. Participants indicated acceptability, feasibility, safety, and effectiveness with recommendations for intervention improvement. | Pilot study, random assignment, convenience sample | Quantitative and Qualitative | Psychological |
| Zamirinejad, Hojjat, Golzari, Borjali, & Akaberi ( ) | Resilience training and cognitive therapy for young women with depression | The resilience training group and cognitive therapy group showed a signiï¬cant decrease in the average depression score from pretest to posttest and from pretest to follow-up. There was no signiï¬cant difference between effectiveness of resilience training and cognitive therapy on depression but there was a signiï¬cant difference between these two treatment groups and the control group. | Three-group design with control, pretest- posttest | Quantitative | Psychological |
| Thapinta, Skulphan, & Kittrattanapaiboon ( ) | Brief Cognitive Behavioral Therapy intervention to reduce depression among alcohol-dependent individuals | The mean depression scores decreased signiï¬cantly in both the experimental and control groups at the one-month follow-up. However, only the experimental group showed signiï¬cant differences in their mean depression scores between pre-and posttest. At Week 7, the experimental group showed signiï¬cantly lower mean depression scores than the control group. | Quasi-experimental, control group, pretest/ posttest design | Quantitative | Psychological |
| Koci et al. ( ) | shelter and justice services for abused women | At 4 months following a shelter stay or justice services, improvement in all mental health measures; however, improvement was the lowest for PTSD. minimum further improvement at 12 months. | Prospective study | Quantitative | Social |
| Simpson et al. ( ) | peer support workers for inpatient aftercare | Participants indicated that the training was valuable, challenging, yet positive experience that provided them with a good preparation for the role. | Pilot randomized controlled trial (RCT), focus groups | Quantitative and Qualitative | Social |
| Forchuk et al. ( ) | Transitional Relational Model (TRM) was used to help mental health clients transitioning from a psychiatric hospital setting to the community. Strategies included enhancing staff participation, creating/ maintaining supportive ward milieus. | Group C implemented the TRM model significantly quicker than the other groups. | Randomized controlled trial; compared three groups of hospital wards; Group A wards had already adopted the TRM, Group B wards implemented the TRM in Year 1, and Group C wards implemented the TRM in Year 2. | Quantitative | Social |
| Horgan, McCarthy, & Sweeney ( ) | online peer support for young adults experiencing depressive symptoms | No statistical significance difference pre- and post-test. The forum posts revealed that the participants' main difficulties were loneliness and perceived lack of socialization skills. The website provided a place for emotional support. | Mixed method, involving quantitative descriptive, pre- and post-test and qualitative descriptive designs | Quantitative and Qualitative | Social |
| Iskhandar Shah et al. ( ) | Virtual reality (VR)-based stress management (VR DE-STRESS) program for people with mood disorders | Those who completed the program had significantly lowered stress, depression, anxiety. | Single-group, pretest–posttest, quasi-experimental research design and convenience sample | Quantitative and Qualitative | Bio-psychological |
| Pedersen et al. ( ) | Farm animal-assisted intervention consisting of work and contact with dairy cattle | Levels of anxiety and depression decreased, and self-efficacy increased during the intervention. | Pretest-posttest, video recording thematic coding | Quantitative and Qualitative | Bio-Social |
| Chandler et al ( ) | Empower resilience intervention (ERI) to build resilience | Subjects in the intervention group reported building strengths, reframing resilience, and creating support connections. | Purposive sampling, random assignment, intervention and control, pretest-posttest design | Quantitative and Qualitative | Psychosocial |
| Hanrahan et al. ( ) | Transitional care model (TCM) intervention to patients with serious mental illness transferring from hospital care to home | Emergency room use was lower for intervention group but not statistically significant. Continuity of care with primary care appointments were significantly higher for the intervention group. The intervention group's general health improved but was not statistically significant compared with controls. | Randomized controlled trial | Quantitative | Bio-psychosocial |
Discussion
Although substantial progress is being made to develop and test interventions for persons with psychiatric and mental health challenges and their families, there remains much work to be done. Nurse scientists and practitioners share a professional obligation to persons entrusted to their care, which includes providing the highest quality care grounded in solid empirical evidence ( Willis, Beeber, Mahoney, & Sharp, 2010 ). This review yields evidence for the continued dissemination of findings from intervention studies from 2011 through 2015. To perform the analysis reported here, we employed methods that were similar to those used for amassing information from the intervention studies in two previous reviews ( Zauszniewski et al., 2007 ; Zauszniewski et al., 2012 ) in order to facilitate comparisons over time.
... the continued publication of evidence from countries outside the United States remains important... During the review period (2011-2015), 57% of the published intervention studies took place in the United States (U.S.) while 43% were conducted outside the U.S. (i.e., internationally). These percentages compare with 72% and 54% of published U.S. intervention studies and 28% and 46% published international intervention studies in the 2000-2005 and 2006-2010 reviews, respectively. The somewhat lower percentages (28% and 46%) of international intervention studies within the current time frame (2011-2015) may indicate a need for more descriptive research to identify distinguishing characteristics of international populations and important phenomena that may be amenable to intervention prior to the systematic testing of interventions. However, the continued publication of evidence from countries outside the United States remains important for developing globally relevant interventions for psychiatric nursing practice.
...there have been dramatic increases through the years in the overall number of studies that have tested interventions that tap more than one domain. Of the 115 intervention studies from 2011 through 2015 found in the five journals, nurses, student nurses, nursing staff, or other mental health professionals were the intervention recipients in 23, representing 20% of the intervention studies. This percent is higher than the 14% reported in the previous review conducted from 2006 through 2010, indicating a slightly greater focus on testing interventions in mental health care professionals in recent years. Although the interventions tested in these populations are not focused directly on outcomes for clients with mental health issues, promoting or preserving the mental health of professional caregivers most certainly affects those for whom they provide care.
Analysis of published intervention studies in the 5-year interval from 2011 through 2015 revealed an increase in the number of studies of psychiatric patients or clients in the five selected journals. For this time frame, we found 92 intervention studies in comparison with 71 from 2006 through 2010 and 77 from 2000 through 2005, which reflect 5 and 6-year intervals respectively.
We also noted fewer intervention studies where all three domains were integrated within the intervention... Moreover, there have been dramatic increases through the years in the overall number of studies that have tested interventions that tap more than one domain. For example, 33% of intervention studies from 2011 through 2015 tested psychosocial interventions, compared to 17% in the previous review (2006-2010) and 12% in the one prior to that (2000-2005). In addition, 13% of the studies from 2011 through 2015 tested biopsychological interventions compared with 4% and 5% in the previous two reviews. However, there was a slightly lower percent of biosocial intervention studies, specifically 3% in comparison with 4% from 2000-2005 and 6% from 2006-2010. We also noted fewer intervention studies where all three domains were integrated within the intervention, specifically only 6% in comparison with 17% in the previous time frame (2006-2010). Yet, our review revealed a larger percent of biopsychosocial intervention studies than from the review conducted from 2000-2005 (1%). Despite the lower number of studies that integrated all three intervention domains, there was an overall trend toward testing interventions that were not restricted only to one domain, indicating increased attention toward more holistic interventions.
... the overall trend shows a lesser focus on testing interventions within a single domain over time... There were 41 intervention studies between 2011 and 2015 that focused solely on one domain. With the exception of the biological domain (9%), interventions within the psychological (26%) and social (10%) domains were fewer than in previous reviews. For example, there has been a clear downward trend in the percent of psychological intervention studies over time with 57% from 2000-2005 to 38% from 2006-2010 and 26% in this current review. Intervention studies within the social domain decreased from 17% in 2006-2010 to 10% in this review. Studies of interventions in the biological domain have fluctuated over time from 11% in 2000-2005 down to 1% from 2005-2010 and up to 9% in the review reported here. However, the overall trend shows a lesser focus on testing interventions within a single domain over time, pointing perhaps to a growing interest in determining effective interventions that are multifaceted and target multiple factors that affect a person’s health.
Implications: Research Needed
The mind and body do not function independently of each other; therefore, when considering the focus of nursing research, we need to target both systems. Nursing has as its foundation a holistic approach to patient care. At this point in our history as we build a knowledge base, a multifaceted approach is needed when planning nursing research. This study of nursing interventions in our research has explored the biological, psychological, and social domains. Studies in the biopsychosocial domain would benefit our knowledge base and improve the criteria for more accurate, evidence-based nursing interventions.
Medicine has increasingly focused on the mental health component of medical illnesses. Nursing research would be strengthened by focusing on the possibility of medical illness and its relationship to mental illness. This nursing research approach'‹ would support our holistic philosophy of care and increase our knowledge of the whole person. It would provide the best evidence-based approach to planning treatment. In addition, it would serve to increase the sphere of psychiatric nursing beyond the psychiatric unit in health care settings.
...an increase in multicultural studies is needed to further strengthen our evidenced based practice. Finally, an increase in multicultural studies is needed to further strengthen our evidenced based practice. The individual person is complex. Identified culture provides important information as to how patients view health and illness. This information is an important component when planning our evidenced based care and should not be isolated from the patient presentation.
Tracking the progress in intervention research relevant for psychiatric and mental health nursing practice is essential to identify evidence gaps. This current, systematic review of intervention studies published in the most accessible psychiatric and mental health nursing journals for practicing nurses, educators, and researchers in the United States has revealed a somewhat lower number of studies from outside the United States; a slightly greater focus on studies of nurses, nursing students, or other mental health professionals as compared with clients who receive their care or services; and a continued trend for testing interventions that captured more than one dimension. Tracking the progress in intervention research relevant for psychiatric and mental health nursing practice is essential to identify evidence gaps. Though substantial progress has been made through the years, there is still room to grow.
Abir K. Bekhet, PhD, RN, HSMI Email: [email protected]
Jaclene A. Zauszniewski, PhD, RN-BC, FAAN Email: [email protected]
Denise M. Matel-Anderson, APNP, RN Email: [email protected]
Jane Suresky, DNP, MSN Email: [email protected]
Mallory Stonehouse, MSN, RN Email: [email protected]
Arms, T., Bostic, T., & Cunningham, P. (2014). Educational intervention to increase detection of metabolic syndrome in patients at community mental health centers. Journal of Psychosocial Nursing & Mental Health Services, 52 (9), 32-36. doi:10.3928/02793695-20140703-01
Battaglia, C., Benson, S.L., Cook, P.F., & Prochazka, A. (2013). Building a tobacco cessation telehealth care management for veterans with posttraumatic stress disorder. Journal of the American Psychiatric Nurses Association , 19 (2), 78-91. doi:10.1177/1078390313483314
Beebe, L.H., Smith, K., Davis, J., Roman, M., & Burke, R. (2012). Meet me at the crossroads: Clinical research engages practitioners, educators, students, and patients. Perspectives in Psychiatric Care, 48 (2), 76-82. doi: 10.1111%2Fj.1744-6163.2011.00306.x
Bekhet, A.K., Zauszniewski, J.A., & Matel-Anderson, D.M. (2012). Resourcefulness training intervention: Assessing critical parameters from relocated older adults’ perspectives. Issues in Mental Health Nursing, 33 (7), 430-435. doi:10.3109/01612840.2012.664802
Boulton, M.A., & Nosek, L. (2014). How do nursing students perceive substance abusing nurses? Archives of Psychiatric Nursing, 28 (1), 29-34. doi:10.1016/j.apnu.2013.10.005
Chandler, G.E., Roberts, S.J., & Chiodo, L. (2015). Resilience intervention for young adults with adverse childhood experiences. The Journal of Psychiatric Nurses Association, 21 (6), 406-416. doi:10.1177/1078390315620609
Choi, Y., Song, E., & Oh, E. (2015). Effects of teaching communication skills using a video clip on a smart phone on communication competence and emotional intelligence in nursing students. Archives of Psychiatric Nursing, 29 (2), 90-95. doi:10.1016/j.apnu.2014.11.003
Choi, Y-J., & Won, M-R. (2013). A pilot study on effects of a group program using recreational therapy to improve interpersonal relationships for undergraduate nursing students. Archives of Psychiatric Nursing, 27 (1), 54-55. doi:10.1016/j.apnu.2012.08.002
Emory, S.L., Silva, S.G., Edwards, P.B., & Wahl, L.E. (2011). Stepping to stability and fall prevention in adult psychiatric patients. Issues in Mental Health Nursing, 49 (12), 30-36 doi:10.3928/02793695-20111102-01
Fiedler, R.A., Breitenstein, S., & Delaney, K. (2012). An assessment of students’ confidence in performing psychiatric mental health nursing skills: The impact of the clinical practicum experience. Journal of the American Psychiatric Nurses Association, 18 (4), 244-250. doi:10.1177/1078390312455218
Forchuk, C., Martin, M-L., Jensen, E., Ouseley, S., Sealy, P., Beal, G., … Sharkey, S. (2012). Integrating the transitional relationship model into clinical practice. Archives in Psychiatric Nursing, 26 (5), 374-381. doi:10.1111/j.1365-2850.2012.01956.x
Hanrahan, N.P., Solomon, P., & Hurford, M.O. (2014). A pilot randomized control trial: Testing a transitional care model for acute psychiatric conditions. Journal of the American Psychiatric Nurses Association , 20 (5), 315-327. doi:10.1177/1078390314552190
Happell, B., Hodgetts, D., Stanton, R., Millar, F., Phung, C.P., & Scott, D. (2014). Lessons learned from the trial of a cardiometabolic health nurse. Perspectives in Psychiatric Care, 50 (4), 1-9. doi:10.1111/ppc.12091
Happell, B., Moxham, L., &Platania-Phung, C. (2011). The impact of mental health nursing education on undergraduate nursing students’ attitudes to consumer participation. Issues in Mental Health Nursing, 32 (2), 108-113. doi:10.3109/01612840.2010.531519
Horgan, A., McCarthy, G., & Sweeny, J. (2013). An evaluation of an online peer support forum for university students with depressive symptoms. Archives of Psychiatric Nursing, 27 (2), 54-55. doi:10.1016/j.apnu.2012.12.00
Irvine, A.B., Billow, M.B., Eberhage, M.G., Seeley, J.R., McMahon, E., & Bourgeois, M. (2012). Mental illness training for licensed staff in long-term care. Issues in Mental Health Nursing, 33 (3), 181-194. doi: 10.3109/01612840.2011.639482
Iskhandar Shah, L.B., Torres, S., Kannusamy, P., Lee Chng, C.M., He, H-G., Klainin-Yobas, P. (2015). Efficacy of the virtual reality-based stress management program on stree-related variables in people with mood disorders: The feasibility of the study. Archives of Psychiatric Nursing, 29 (1), 6-13. doi:10.1016/j.apnu.2014.09.003
Kameg, K.M., Englert, N.C., Howard, V.M., & Perozzi, K.J. (2013). Fusion of psychiatric and medical high-fidelity patient simulation scenarios: Effect on nursing student knowledge, retention of knowledge, and perception. Issues in Mental Health Nursing, 34 (12), 892-900. doi:10.3109/01612840.2013.854543
Kane, C. (2015). The 2014 Scope and Standards of Practice for psychiatric mental health nursing: Key Updates. OJIN: The Online Journal of Issues in Nursing, 20 (1), Manuscript 1. doi:10.3912/OJIN.Vol20No01Man01
Kidd, L.I., Knisley, S.J. & Morgan, K.I. (2012). Effectiveness of a Second Life® simulation as a teaching strategy for undergraduate mental health nursing students. Journal of Psychosocial & Mental Health Services, 50 (7), 3-5. doi:10.3928/02793695-20120605-04
Kinser, P.A., Bourgugnon, C. Taylor, A.G., Steeves, R. (2013). "A feeling of connectedness": Perspectives on a gentle yoga interenvention for women with major depression. Issues in Mental Health Nursing, 34 (6), 402-211. doi:10.3109/01612840.2012.762959
Kinser, P.A., Bourguigion, C., Whaley, D., Hauenstein, E., & Taylor, A.G. (2013). Feasibility, acceptability, and effects of gentle Hatha yoga for women with major depression: Findings from a randomized controlled mixed-methods study. Archives of Psychiatric Nursing, 27 (3), 137-147. doi:10.1016/j.apnu.2013.01.003
Koci, A.F., Cesario, S., Nava, A., Liu, F., Montalvo-Liendo, N., & Zahed, H. (2014). Women’s functioning following an intervention for partner violence: New knowledge for clinical practice from a 7-year study. Issues in Mental Health Nursing, 35 (10), 745-755. doi:10.3109/01612840.2014.901450
Lawson, S.L., Munoz-Rojas, D., & Siman, M.N. (2012). Changing attitudes and perceptions of Hispanic men ages 18-25 about rape and rape prevention. Issues in Mental Health Nursing, 22 (12), 864-70. doi:10.3109/01612840.2012.728279
Lindseth, G., Helland, B., & Caspers, J. (2015). The effects of dietary tryptophan on affective disorders. Archives of Psychiatric Nursing, 29 (3), 102-107. doi:10.1016/j.apnu.2014.11.008
Luebbert, R., & Popkess, A. (2015). The influence of teaching method on performance of suicide assessment in baccalaureate nursing students. The Journal of American Psychiatric Nurses Association, 21 (2), 126-133. doi:10.1177/1078390315580096
Masters, J.C., Kane, M.G., & Pike, M.E. (2014). The suitcase simulation: An effective and inexpensive psychiatric nursing teaching activity. Journal of Psychosocial Nursing, 52 (8), 39-44. doi:10.3928/02793695-20140619-01
Mitchell, A.M., Puskar, K., Hagle, H., Gotham, H.J., Talcott, K.S., Terhorst, L., … Burns, H.K. (2013). Screening, brief intervention, and referral to treatment: Overview of and student satisfaction with an undergraduate addiction training program for nurses. Journal of Psychosocial Nursing & Mental Health Services, 51 (10), 29-37. doi:10.3928/02793695-20130628-01
Nilsen, P. (2015). Making sense of implementation theories, models and frameworks. Implementation Science : IS , 10 , 53. doi:10.1186/s13012-015-0242-0
Ozcan, N.D., Bilgin, H., & Eracar, N. (2011). The use of expressive methods for developing empathetic skills. Issues in Mental Health Nursing, 32 (2), 131-136. doi:10.3109/01612840.2010.534575
Pedersen, I., Nordaunet, T., Martinsen, E.W., Berget, B., & Braastad, B.O. (2011). Farm animal-assisted intervention: Relationship between work and contact with farm animals and change in depression, anxiety, and self-efficacy among persons with clinical depression. Issues in Mental Health Nursing, 32 (8), 493-500. doi:10.3109/01612840.2011.566982
Proctor, E.K., Landsverk, J., Aarons, G., Chambers, D., Glisson, C., & Mittman, B. (2009). Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Administration and Policy in Mental Health, 36 (1), 24-34 doi:10.1007/s10488-008-0197-4
Pulia, K., Vaidya, P., Jayaram, G., Hayat, M., & Reti, I.M. (2013). ECT treatment outcomes following performance improvement changes. Journal of Psychosocial and Mental Health Services, 51 (11), 20-25. doi:10.3928/02793695-20130628-02
Riley, J.B., & Yearwood, E.L. (2012). The effect of a pedagogy of curriculum infusion on nursing student well-being and intent to improve the quality of nursing care. Achieves in Psychiatric Nursing, 26 (5), 364-63. doi:10.1016/j.apnu.2012.06.004
Schwindt, R.G., McNelis, A.M., & Sharp, D. (2014). Evaluation of a theory-based educational program to motivate nursing students to intervene with their seriously mentally ill clients who use tobacco. Archives of Psychiatric Nursing, 28 (4), 277-283. doi:10.1016/j.apnu.2014.04.003
Simpson, A., Quigley, J., Henry, S.J., & Hall, C. (2014). Evaluating the selection, training, and support of peer support workers in the United Kingdom. Journal of Psychosocial Nursing and Mental Health Services, 52 (1), 31-40. doi:10.3928/02793695-20131126-03
Sorensen, J. L., & Kosten, T. (2011). Developing the tools of implementation science in substance use disorders treatment: applications of the consolidated framework for implementation research. Psychology of Addictive Behaviors, 25 (2), 262-268. doi:10.1037/a0022765
Stanton, R., Donohue, T., Garnon, M., & Happell, B. (2015). Participation in and satisfaction with an exercise program for inpatient mental health consumers. Perspectives in Psychiatric Care, 52 (1), 62-67. doi:10.1111/ppc.12108
Stiberg, E., Holand, U., Olstad, R., & Lorem, G. (2012). Teaching care and cooperation with relatives: Video as a learning tool in mental health work . Issues in Mental Health Nursing, 33 (8). doi:10.3109/01612840.2012.687804
Taylor. K., Guy, S., Stewart, L., Ayling, M., Miller, G., Anthony, A., … Thomas, M. (2011). Care zoning a pragmatic approach to enhance the understanding of clinical needs as it relates to clinical risks in acute in-patient unit settings. Issues in Mental Health Nursing, 32 (5), 318-326. doi:10.3109/01612840.2011.559570
Terry, J. & Cutter, J. (2013). Does education improve mental health practitioners’ confidence in meeting the physical health needs of mental health service users? A mixed method pilot study. Issues in Mental Health , 34(4), 249-255. doi:10.3109/01612840.2012.740768
Thapinta, D., Skulphan, S., & Kittrattanapaiboon, P. (2014). Brief cognitive behavioral therapy for depression among patients with alcohol dependence in Thailand. Issues in Mental Health Nursing, 35( 9), 689-693. doi:10.3109/01612840.2014.917751
Tsai, W-P., Lin, L-Y., Chang, H-C., Yu, L-S., & Chou, M-C. (2011). The effects of the gatekeeper suicide-awareness program for nursing personnel. Perspectives in Psychiatric Care, 47 (3), 117-125. doi:10.1111/j.1744-6163.2010.00278
Usher, K., Park, T., Trueman, S., Redman-MacLaren, M., Casella, E., & Woods, C. (2014). An educational program for mental health nurses and community health workers from Pacific Island countries: Results from a pilot study . Issues in Mental Health Nursing, 35 (5), 337-343. doi:10.3109%2F01612840.2013.868963
White, J., Hemingway, S., & Stephenson, J. (2014). Training mental health nurses to assess the physical health needs of mental health service users: A pre- and post-test analysis. Perspectives in Psychiatric Care, 50( 4), 243-250. doi:10.1111/ppc.12048
Willis, D.G., Beeber, L., Mahoney, J., & Sharp, D. (2010). Strategies for advancing psychiatric-mental health nursing science relevant to practice. Perspectives from the American Psychiatric Nurses Association research council co-chairs. Contemporary Nurse, 34 (2), 135-139
Wong, O.L. (2014). Contextual barriers to the successful implementation of family-centered practice in mental health care: A Hong Kong study. Archives of Psychiatric Nursing, 28 (3), 197-199. doi:10.1016/j.apnu.2014.02.001
Wynn, S.D. (2011). Improving the quality of care of veterans with diabetes. Journal of Psychosocial Nursing & Mental Health Services, 49 (2), 38-43. doi:10.3928/02793695-20110111-01
Zamirinejad, S., Hojjat, SK., Golzari, M., Borjali, A., &Akaberi, A. (2014). Effectiveness of resilience training versus cognitive therapy on reduction of depression in female Iranian college students. Issues in Mental Health Nursing, 36 (6), 480-488. doi:10.3109/01612840.2013.879628
Zauszniewski, J.A, Bekhet, A., &Haberlein, S. (2012). A decade of published evidence for psychiatric and mental health nursing interventions. OJIN: The Online Journal of Issues in Nursing, 17 (3), doi:10.3912/OJIN.Vol17No03HirshPsy01
Zauszniewski, J., Suresky M.J., Bekhet, A., & Kidd, L. (May 14, 2007). Moving from Tradition to Evidence: A Review of Psychiatric Nursing Intervention Studies . Online Journal of Issues in Nursing 12 (2) doi:10.3912/OJIN.Vol12No02HirshPsy01
Zhou, F-C., Xiang, Y-T., Wang, C-Y., Dickerson, F., Kryenbuhl, J., Ungari, G.S., … Chiu, H.F.K. (2014). Predictive value of prospective memory for remission in first-episode schizophrenia. Perspectives in Psychiatric Care, 50 (2), 102-110. doi:10.1111/ppc.12027
May 31, 2018
DOI : 10.3912/OJIN.Vol23No02Man04
https://doi.org/10.3912/OJIN.Vol23No02Man04
Citation: Bekhet, A.K., Zauszniewski, J.A., Matel-Anderson, D.M., Suresky, M.J., Stonehouse, M., (May 31, 2018) "Evidence for Psychiatric and Mental Health Nursing Interventions: An Update (2011 through 2015)" OJIN: The Online Journal of Issues in Nursing Vol. 23, No. 2, Manuscript 4.
- Article May 31, 2018 Advancing Scholarship through Translational Research: The Role of PhD and DNP Prepared Nurses Deborah E. Trautman, PhD, RN, FAAN; Shannon Idzik, DNP, CRNP, FAANP, FAAN; Margaret Hammersla, PhD, CRNP-A; Robert Rosseter, MBA, MS
- Article May 31, 2018 Connecting Translational Nurse Scientists Across the Nation—The Nurse Scientist-Translational Research Interest Group Elizabeth Gross Cohn, RN, NP, PhD, FAAN; Donna Jo McCloskey, RN, PhD, FAAN; Christine Tassone Kovner, PhD, RN, FAAN; Rachel Schiffman, RN, PhD, FAAN; Pamela H. Mitchell, RN, PhD, FAAN
- Article May 31, 2018 Translation Research in Practice: An Introduction Marita G. Titler, PhD, RN, FAAN
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Mental health in nursing
A student's perspective.
Halsted, Candis DNP-PMHNP, RN; Hart, Virginia T. DNP, RN, PMHNP-BC
At Radford University School of Nursing in Radford, Va., Candis Halsted recently earned her DNP and Virginia T. Hart is an assistant professor and interim psychiatric mental health NP program coordinator.
The authors have disclosed no financial relationships related to this article.
A stigma around mental health issues within healthcare and nursing itself has created a culture of perfectionism in the workplace, and nurses struggle to live up to the expectations while pushing aside their feelings, thoughts, and needs. Inspired by one author's personal experiences, this article explores mental health issues many nurses confront today.
Inspired by one author's personal experiences, this article explores mental health issues many nurses confront today.

I DECIDED TO RETURN to school in 2015 after practicing as a nurse in various settings for 7 years. I subscribe to the adage that knowledge is power. My drive for additional education and experience was based on my desire to achieve a higher status, assume more control over my practice, and to garner more respect from other healthcare professionals. As I immersed myself in my graduate studies, however, I found my desires, self-image, and professional viewpoint had changed.
I have always endeavored to be the best student, greatest employee, and most dependable teammate. Those efforts took on a feverish intensity during periods of transition—student to nurse, nurse to working mother, mother and nurse to professional student. Good was not good enough, and my drive to be the best and greatest was an integral part of my self-worth. Unfortunately, it led to anxiety, depression, hopelessness, and isolation that negatively impacted my education, practice, and personal life.
It was not until my clinical rotations as a psychiatric-mental health NP student that I came to realize the magnitude of the situation. There I was, taking courses on trauma-informed care and giving my patients tools for building self-efficacy, self-compassion, and coping skills while simultaneously ignoring my own needs.
Having left the workplace to focus on my online studies, I was isolated, lacking confidence, feeling overwhelmed, and overcompensating for some perceived shortcoming that I could not even define. I felt hopeless and defeated. I experienced bouts of anxiety and depression so intense I lost my sense of purpose. I considered dropping out of school many times, but I gave in to the expectations of others. I forced myself to continue pushing aside my own needs, persisting despite my growing depression and anxiety.
Looking back, I had so many chances to speak up and reach out for help. I could have spoken with nurse managers, coworkers, fellow students, and faculty a hundred different ways on so many occasions. Instead, I allowed the culture of silence and my own perfectionism to rule.
At my lowest point, I made the life-altering decision to reach out for help—first to my husband, then a therapist, a fellow student, and finally my school faculty. With their assistance, some serious self-reflection, and a lot of self-help reading, I am working to address my mental illness and establish a sense of well-being.
That is not to say that I have it all figured out. I still struggle many days to keep faith in my strengths and abilities. The things I have learned and witnessed, the obstacles I have encountered and overcome, whether academic, professional, or personal, have humbled me and restored my desire to return to the love, service, and justice at the core of my professional drive and practice. I am once again prioritizing my values and making sure my actions reflect them. Among those values is the desire to work toward the unification of our profession and to advocate for policy changes that support the mental health of all nurses. Inspired by my personal experiences, this article explores mental health issues many nurses confront today.
A pervasive problem
Although mental health and suicide among nurses have emerged as areas of professional concern in recent years, little research or literature exists regarding profession-specific risk factors, prevalence of mental illness, and suicide rates. With little to no concrete statistics to draw from, the true incidence of mental illness within the nursing profession is unknown. Furthermore, little has been done to bring these problems to the attention of the general public or to acquire the recognition and support of the professional community. 1-3
What can be found are decades of research stating that nursing is psychologically demanding and can contribute to poor mental health in a variety of ways, such as depression, anxiety, secondary trauma, compassion fatigue, and burnout. 1-7 The occupational hazards of nursing can also compromise work-life balance. Add to this various individual risk factors such as genetic predisposition or history of personal trauma, as well as the fact that academic standards for the profession favor those who are exacting and high-performing. It stands to reason that nurses are in jeopardy of significantly elevated levels of stress and maladaptive coping. 5,8 When ongoing, this can lead to impaired functioning. In the professional setting, impairment has been correlated with increased risk for errors, patient harm, and clinical ineffectiveness. 9
Mental illness can be defined as clinically significant impairment in social, conceptual, and practical functioning. 9,10 Although very common, mental illness is often untreated. 11 One in five adults will have some experience with mental illness each year, but less than half will receive treatment. 11
Nursing has a hidden culture of stigma and silence regarding mental illness, which serves to minimize and overshadow those experiencing clinically significant distress. 6,12 Competition, intimidation, and bullying among nurses are pervasive across practice and in academic settings. 13,14 These behaviors can breed psychologically hazardous and hostile environments. Fear of becoming a target may result in blame, shame, self-stigmatization, isolation, and suffering in any individual with potentially undesirable characteristics in such settings, regardless of his or her mental health status. Such abuses and fear can promote conformity and negatively impact disclosure and help-seeking behaviors in stressed, distressed, and impaired individuals. 1,2,5,13
The issue is exacerbated by a lack of respect and recognition for nursing that is still present within the healthcare culture at large. The traditional hierarchy holds physicians as experts, not nurses. Even advanced practice nurses are diminished, often referred to as “mid-level providers” and “physician extenders.” 15 These attitudes undermine the autonomy and dignity of nurses, especially when they collaborate with other healthcare disciplines. 14
In addition, while healthcare entities and societies champion the rights of the patient, the need to protect the basic human dignity and professional image of nurses is often overlooked. 14 Fundamental protections and rights for nurses are being compromised every day when we are expected to tolerate long hours, interrupted (or nonexistent) breaks, heavy patient caseloads, incivility, and even violence in the workplace. Nurse unions across the country are threatening walkouts and going on strike because of the failure of hospitals to address these issues. 16,17 The situation is not helped by the fact that guiding and governing bodies for nursing practice are numerous yet, in my opinion, self-segregated.
Systemic change
Although some organizations have created emotional wellness programs, a cohesive or public effort to address systemic problems is lacking. 1-3 Until employers, boards of nursing, and nursing organizations place the same importance on the well-being of nurses and risk mitigation, nurses may continue to suffer in silence. Within the currently disjointed system, we cannot hope to make substantive changes without offering our passion and expertise as well as identifying and supporting means for promoting self-care and wellness among the thousands of practicing nurses and preprofessionals experiencing distress or symptoms of mental illness.
Pressures and barriers to mental health and help-seeking extend to the academic setting. 4-5 For professional nurses returning to school, the pressure associated with practice and professional expectations may be exacerbated by their increased need to balance a variety of personal and/or family responsibilities, deadlines, financial obligations, leisure time, and peer competitiveness. Despite these contributory risk factors, I have seen few—if any—educational programs for health and helping disciplines, such as nursing, medicine, and social work, place value on assessing students' stress and distress. In commiserative discussions with others doing graduate work in nursing, social work, occupational therapy, and physical therapy, I have yet to meet anyone who felt the faculty took action to address the genuine difficulties many of them faced in balancing their lives. In short, students (myself included) feel devalued by the lack of respect, holistic consideration, and mentorship they encounter. Academic learning environments have a great need to support improvement of the emotional well-being and psychological resiliency of students and for improving the accessibility of support, counseling, and mental health resources. 4,5
I encourage you to take a long, hard look at yourself and those around you. If you are struggling, please reach out to someone you trust and let them know you are not okay. If you are not sure that what you are experiencing is normal or cause for concern, there are many websites that provide education and information on how to identify mental health problems, as well as hotline crisis intervention services and referrals to local counseling. These websites often have articles and tips on how to improve your mental health through physical, spiritual, and psychological self-care. (See Mental health resources .)
No mental health concern is too big or too small. If you are not well, talk to a friend, family member, professional, or help hotline. If you suspect a coworker, colleague, or student needs help, please reach out. Something as simple as asking if they are okay and giving them the space and time to express their feelings can make all the difference. As Edward Everett Hale once said, “I am only one, but still I am one. I cannot do everything, but still I can do something. And because I cannot do everything, I will not refuse to do the something that I can do.” 18 We owe it to ourselves, our profession, our patients, and their families to seek help and to offer help to our fellow nurses in need.
For anyone requiring immediate crisis intervention or assistance finding a local mental health provider, the following resources are available:
- Mental Health America: 1-866-400-6428 for referrals, 1-800-273-8255 for crisis
- National Alliance on Mental Illness HelpLine 1-800-950-6264
- National Suicide Prevention Helpline 1-800-273-8255
Crisis Text Line available 24 hours a day, text “HOME” to 741741
Mental health resources
- American Psychological Association
- www.apa.org
- American Psychiatric Nurses Association (APNA)
- www.apna.org
- MentalHealth.gov
- www.mentalhealth.gov
- National Alliance on Mental Illness
- www.nami.org
- National Suicide Prevention Lifeline
- https://suicidepreventionlifeline.org
- Crisis Text Line
- www.crisistextline.org
anxiety; compassion fatigue; depression; emotional wellness; mental health; nursing; suicide prevention
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Assessing mental health in vulnerable adolescents, managing loneliness and chronic illness in older adults, destigmatizing alcohol use disorder among nurses, can nurses trust nurses in recovery reentering the workplace, new drugs 2019, part 3.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Nursing intervention in mental health: a case study in a home setting †.

1. Introduction
2. material and methods, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Associação Portuguesa de Familiares e Amigos dos Doentes de Alzheimer. Available online: https://alzheimerportugal.org/prevalencia-da-demencia/ (accessed on 29 April 2022).
- Nunes, B.; Pais, J. Doença de alzheimer exercícios de estimulação ; Lidel: Lisboa, Portugal, 2021. [ Google Scholar ]
- Ordem dos Enfermeiros. Regulamento dos Padrões de Qualidade dos Cuidados Especializados em Enfermagem de Saúde Mental ; Ordem dos Enfermeiros: Lisboa, Portugal, 2015. [ Google Scholar ]
- Ferreira, A. Contributo da visita domiciliária: Perceção dos cuidadores informais dos doentes com demência de Alzheimer. Master’s Thesis, Escola Superior de Enfermagem do Porto, Porto, Portugal, 2014. [ Google Scholar ]
- Silva, R. Estimulação cognitiva em pessoas idosas: Intervenção individual na fragilidade cognitiva. Ph.D. Thesis, Universidade Católica Portuguesa, Porto, Portugal, 2020. [ Google Scholar ]
- Sequeira, C. Cuidar de idosos com dependência física e mental , 2nd ed.; Lidel: Lisboa, Portugal, 2021. [ Google Scholar ]
- Galdeano, L.E.; Rossi, L.A.; Zago, M.M.F. Roteiro instrucional para a elaboração de um estudo de caso clínico. Rev. Lat.-Am. Enferm. 2003 , 11 , 371–375. [ Google Scholar ] [ CrossRef ]
- Coelho, J.; Ribeiro, A.R.; Sampaio, F.; Sequeira, C.; Lleixà Fortuño, M.; Roldán Merino, J. Cultural adaptation and psychometric properties assessment of the NOC outcome “Cognition” in a sample of Portuguese adults with mental illness. Int. J. Nurs. Knowl. 2019 , 31 , 180–187. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moorhead, S.; Johnson, M.; Maas, M.L.; Swanson, E. Classificação dos Resultados de Enfermagem (NOC) , 5th ed.; Elsevier: Rio de Janeiro, Brazil, 2016. [ Google Scholar ]
- Meleis, A. Theorical Nursing: Development e Progress , 4th ed.; Lippincott: Philadelphia, PA, USA, 2007. [ Google Scholar ]
- Ordem dos Enfermeiros. Regulamento de Competências Específicas do Enfermeiro Especialista em Enfermagem de Saúde Mental e Psiquiátrica ; Ordem dos Enfermeiros: Lisboa, Portugal, 2018. [ Google Scholar ]
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Oliveira, P.; Figueiredo, S.; Martinho, J.; Pires, R.; Pinto, C.B. Nursing Intervention in Mental Health: A Case Study in a Home Setting. Med. Sci. Forum 2022 , 16 , 3. https://doi.org/10.3390/msf2022016003
Oliveira P, Figueiredo S, Martinho J, Pires R, Pinto CB. Nursing Intervention in Mental Health: A Case Study in a Home Setting. Medical Sciences Forum . 2022; 16(1):3. https://doi.org/10.3390/msf2022016003
Oliveira, Palmira, Sofia Figueiredo, Júlia Martinho, Regina Pires, and Cristina Barroso Pinto. 2022. "Nursing Intervention in Mental Health: A Case Study in a Home Setting" Medical Sciences Forum 16, no. 1: 3. https://doi.org/10.3390/msf2022016003
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- Reasons to publish with us
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, research design and method, opening of the encounter: developing a reciprocal relationship, active listening: power sharing, vision of the future: emphasizing the positive, conclusions.
- < Previous
Empowering counseling—a case study: nurse–patient encounter in a hospital
- Article contents
- Figures & tables
- Supplementary Data
Tarja Kettunen, Marita Poskiparta, Leena Liimatainen, Empowering counseling—a case study: nurse–patient encounter in a hospital , Health Education Research , Volume 16, Issue 2, April 2001, Pages 227–238, https://doi.org/10.1093/her/16.2.227
- Permissions Icon Permissions
This study illustrates practices that a nurse uses in order to empower patients. The emphasis is on speech formulae that encourage patients to discuss their concerns and to solicit information about impending surgery. The study is a part of a larger research project and a single case was selected for presentation in this article because it differed from the rest of the data by manifesting empowering practice. A videotaped nurse–patient health counseling session was conducted in a hospital and transcribed verbatim. The investigator interviewed the nurse and the patient after the conversation, and these interviews were transcribed as well. The encounter that is presented here as a case study is a concrete example of a counseling session during which the patient is free to discuss with the nurse. The empowering practices that the nurse employed were as follows: encouraging the patient to speak out, tactfully sounding out the patient's concerns and knowledge of impending surgery, listening to feedback, and building a positive vision of the future for the patient. We suggest that nurses should pay attention to verbal expression and forms of language. This enables them to gain self-awareness and discover new tools to work with.
In recent literature, empowerment has become an important concept of health education ( Feste and Anderson, 1995 ; van Ryn and Heaney, 1997 ), health promotion ( Labonte, 1994 ; Tones, 1994 , 1995 ; Williams, 1995 ; McWilliam et al. , 1997 ) and health counseling ( Poskiparta et al. , 2000 ). The process of empowerment has been related more to community and organizational levels than to micro levels of practice ( van Ryn and Heaney, 1997 ) where it is constantly crucial ( Tones, 1994 ). In addition, operationalization of the concept of empowerment has been relatively vague. According to Tones ( Tones, 1994 ), empowerment is a major goal of health promotion. This article focuses on health counseling as a means of interpersonal health education practice and uses health promotion as an umbrella term.
Empowerment is as much a process as an outcome of developing the skills and perceptions of clients. It is not only something that happens but a process that is facilitated. In interpersonal health counseling, the primary goal is not to change clients' behavior and seek their compliance with the presented message but rather to raise critical awareness through learning and support, to give clients tools for making changes on their own. The aim is personal empowerment, control and choice, which means that patients become aware of changes in their knowledge and understanding, decision-making skills, enhanced self-esteem/sense of personal control, and development of various social, health and life skills ( Labonte, 1994 ; Tones 1994 ; Anderson et al. , 1995 ; Feste and Anderson, 1995 ; van Ryn and Heaney, 1997 ; Kar et al. , 1999 ).
The basic point of departure for empowerment is taking into consideration the interactive nature of the individual and the environment: people are not completely controlled by their environment nor can they fully control their physical, social or economic circumstances ( Tones, 1994 ). Empowering health counseling is based on recognizing clients' competence, resources, explanations of action styles of coping and support networks. Client initiative, clients' realizations and clients' expressions of their opinions and interpretations are the basis on which clients can approach health issues in collaboration with professionals. They are of crucial importance for their decisions on future action ( Anderson, 1996 ). All this supports the notion that empowering health counseling is significant.
Because learning about personal health is complex, the key issue of empowering health counseling is partnership and reciprocal conversation in a confidential relationship. This means that clients not only analyze their situation but also have an opportunity to plan what to do next, and how to go on and to construct their own solutions to health issues. In this type of hospital health counseling, either patients raise the issues (i.e. determine the topics) or the nurses do so in a sensitive and non-threatening manner ( Poskiparta et al. , 2000 ). Nurses recognize and respect patients' experiences, knowledge and skills, and make their own professional knowledge and expertise available to them ( Williams, 1995 ; McWilliam, et al. , 1997 ), which are important aspects of nurse–patient relationships that are also reported by patients ( Häggman-Laitila and Åstedt-Kurki, 1994 ; Lindsey and Hartrick, 1996 ; Wiles 1997 ). The emphasis is placed on patient-driven [see ( Lindsey and Hartrick, 1996 )] health counseling, where patients' life situations are respected, patient-initiated actions are supported, and shared knowledge and deep understanding are nurtured.
The nurse's institutional task is not only to facilitate patient participation but also to promote patients' awareness of their routines and preconceptions as they are revealed to both interlocutors. This should lead to the aim of interaction, which is to activate self-reflection and re-evaluation and reorganization of patients' activities. The assumption is that new knowledge is gained in this process as a result of empirical realization and deliberation ( Feste and Anderson, 1995 ), which means that both patients and nurses have linked new knowledge to existing knowledge. Thus, patients learn to interpret and outline even familiar health problems in new ways that conform to their worldview [ cf . ( Mattus, 1994 )]. As for nurses, empowerment calls for not only sensitivity but also an ability to accurately perceive patients' messages.
From this point on, the focus is on the content of the interactive process. Tones ( Tones, 1994 ) discusses empowerment theoretically, Labonte ( Labonte, 1994 ) expresses ideas for practice in general, while Feste and Anderson ( Feste and Anderson, 1995 ) provide three empowerment tools for facilitating patients' empowering process: using questions, behavioral language and storytelling. According to them, questions maintain the process of pursuing wisdom, i.e. exploring the meaning of health problems in the context of everyday life. This kind of questioning involves broad questions that relate to one's personal philosophy and lifelong dreams. In addition, it includes practical, day-to-day issues of successfully integrating into one's personal, family, social and professional life. Behavioral language means using words such as `list', `describe', `identify', `decide', etc., in order to encourage patients to act and make choices instead of being satisfied with receiving information. Stories help to facilitate the process of self-discovery because diseases affect all areas of life and each individual's health status is unique.
Van Ryn and Heaney ( Van Ryn and Heaney, 1997 ) pay attention to interpersonal relations by suggesting concrete strategies and examples for empowering practice. In their article, they demonstrate two principles of interaction: (1) provide clients with unconditional positive regard and acceptance, and (2) facilitate client participation. Both principles include several practical strategies (Table I ).
However, the authors pay less attention to empirical findings ( Northouse, 1997 ). The present article describes some linguistic realizations of empowering practice. This article describes a nurse's empowering speech formulae during her efforts to give a patient information about an impending surgical operation and to strengthen her feelings of security by providing her with an opportunity to discuss her concerns. This study adopts a holistic approach to interaction and does not focus on isolated sentences or dialogue structure. The relationship of language and context in comprehension, as well as non-verbal communication, are also discussed.
This article describes a single case derived from qualitative data collected from a total of 38 counseling sessions in a Finnish hospital. Nurse–patient encounters were videotaped and transcribed verbatim. Interviews with the nurses and the patients after the sessions were transcribed as well. All participants volunteered to take part in the research, signed a research license and granted permission for the transcribed data to be used in publications. Nineteen nurses participated in this study. Each nurse conducted two videotaped counseling sessions with different patients. There was only one male nurse while the patient group consisted of 24 female and 14 male patients. The research material took shape as nurses volunteered in the hospital and it was found to be adequate for qualitative analysis. The length of the nurses' careers varied from 1 to 25 years. The ages of the nurses were between 24 and 50 years (mean age 36.9 years) while the patients' ages ranged from 18 to 70 years (mean age 47.9 years). The researcher did not attend the counseling sessions, which lasted from 5 to 45 min. The participating patients were experiencing diverse health problems. Various surgical problems, e.g. knee surgery, hernia operation, breast surgery, hip operation, back operation, post status of brain bleeding and post care of bypass surgery, were among the most representative. In addition to the health problems that had led to hospitalization, many patients also suffered from chronic diseases, such as hypertension, asthma, rheumatic illnesses or diabetes. Many patients also found themselves in an insecure situation when a chronic disease had suddenly been manifested or they were undergoing examinations. There were also some mothers in the group who had delivered recently and had no health problems.
The health counseling sessions were genuine counseling situations that were related to the patients' treatment. A single video camera was used, which meant that the observation of non-verbal communication was limited to examining the session as a whole, including only eye contact, smiles, laughter, tone of voice, gestures and, to some extent, facial expressions. Consequently, the emphasis of this study was examining verbal communication. Separate interviews with the nurses and the patients where both parties were encouraged to express their evaluations of the health counseling were used for partial support of the interpretations, e.g. when describing the patients' opinions about health counseling. We also checked if there were any nurses or patients who were nervous about the videotaping.
This article concentrates on videotaped data. When we examined all of the data we found many encounters that involved some empowering features from time to time, but there were none that were consistently empowering. In this article, we present a single case from the data. This particular encounter was selected because it differed from the rest of the data ( Stake, 1994 ) by manifesting empowering practice most widely. In order to study the interactive nature of communication, the coding and analysis of the videotaped data was based on principles of Conversation Analysis ( Drew and Heritage, 1998 ). The videotapes were transcribed word by word, including stammering, etc. At the same time, additional data were added to the transcriptions, such as pauses during and between turns, onset and termination of overlapping talk, intonation information, and some non-verbal communication. The following transcription symbols were used to indicate this information:
ha+ hands support speech
vo+ rising voice
vo– falling voice
[ ] at the beginning and end of overlapping speech, words enclosed
(( )) transcriber's comments, e.g. smile, laughter, body movements
(.) small but detectable pause
underlining emphasis
… omission of text
=no interval between the end of prior and start of next speech unit
°speech° speech in low volume, words enclosed
`speech'pitch change, words enclosed
The analysis was carried out on a turn-by-turn basis. The principle behind this analysis was to examine how turns were taken with regard to other participants' speech and what sequential implications each turn had for the next. After reading the transcript and watching the recording several times, we discovered a number of empowering expressions in the nurse's speech and concluded that this case was the one which best manifested empowering action in the data.
The particular case describes at the individual level information about the patient's situation, the nurse's interview after the encounter, an in-depth description of the nurse–patient conversation and the observational data derived from it. Pearson ( Pearson, 1991 ) and Patton ( Patton, 1990 ) indicate that a case study can be used, for example, for examining how different concepts emerge or change in particular contexts. However, an even more important question is what can be learned from a single case. Stake ( Stake, 1994 ) suggests that one should select a case that seems to offer an opportunity to learn and contributes to our understanding of specific phenomena. Here, a detailed single case analysis illustrates how empowerment may be practiced during health counseling and demonstrates how new working tools for empowerment can be developed on the basis of a single encounter ( Laitakari, 1998 ). The present study describes the speech of a nurse when she helped a patient to deal with anxiety and to receive information about surgery in an empowering way.
The nurse anesthetist has come to see a patient who is scheduled to have surgery the next day. The encounter involves, besides interviewing, producing a lot of information about the operation, counseling on the preparations for the surgery and advising how to manage after the surgery. The encounter takes place at a table, with the nurse and the patient facing each other. Both are women; the nurse is 50 and the patient 41 years old. The patient had had problems with her back for 10 years and was suddenly admitted to the hospital because of these problems. The patient has recently been examined and a decision has been made to operate on her the next morning. The interviewing session lasted 14 min.
At the beginning of a conversation the participants evaluate each others aims and concerns, and the communication situation as a whole, and this evaluation directs the entire discussion because the participants base their actions on it (Goffman, 1982). In a hospital, it is typical that nurses initiate a discussion ( Leino-Kilpi, 1991 ) and that is what happened in this case ( Extract 1 ). Professional dominance common in medical encounters ( Fairclough, 1992 ) is not so obvious in this conversation. After greeting the patient, the nurse refers to the goal of the discussion and individualizes it by using familiar `you' (line 1) instead of the formal, plural form of `you'. This form of address can be viewed as an act of communicating an appropriate degree of informality. It implies intimacy and mutual respect when a relationship is established ( van Ryn and Heaney, 1997 ).
1 N: Hello, Rose (.) you are going to have surgery 2 tomorrow…but now I would like to ask you 3 you well about the operation tomorrow if 4 there is (.) something that would influence 5 the preparations for your operation (.) and 6 then you ((ha+)) can bring things up ask well 7 er if something is unclear to you ((nod+)) If 8 you want to know anything about what's 9 going to happen to you tomorrow ((vo–))
((at first the nurse looks at papers on the table, while she speaks she turns her eyes to the patient and nods))
This opening was not typical of the other interviews in the data set, because in the data these encounters were usually initiated with the nurses' brief statements about the impending operation. They explained that they interviewed patients in advance in order to get information and that they could provide information to the patients as well. Nurses usually used formal, plural forms of address when speaking. When referring to the preoperative encounter, they used the plural, institutionalized form `we' [see ( Drew and Heritage, 1998 )], instead of first person singular `I', and plural `you', instead of the singular, when addressing the patient. Other nurses did not individualize their speech. On the contrary, they maintained a distance from the patients. In this particular case, a familiar mode of address reduces social distance, which is very important in health education practice [ cf . ( van Ryn and Heaney, 1997 )]. We explain our interpretations in more detail below.
The nurse uses the verb `ask' (line 2), but her remark further on (line 6–9) `then you can bring up ask well er if you were unclear about something if you want to know something about what's going to happen to you tomorrow' introduces a context for the discussion. Even though the nurse goes on to ask a question about previous operations, the interview becomes an interactive dialogue, with the patient actively participating. On her own initiative the patient discloses symptoms that she has experienced during the last few months, what happened when she needed to come to the hospital and the doctor's decision to perform surgery.
Thus, the nurse introduces the context of the discussion with her opening words [ cf . ( Peräkylä, 1995 )]. She expresses her acceptance by offering collaboration [ cf . ( van Ryn and Heaney, 1997 )] when asking questions. The verb form `would like to' (line 2) gives the discussion an air of voluntariness. The conditional form softens the notion of the necessity of the questions, and the verbal mode implies respect for the patient. At the beginning of the session (lines 1–9), the nurse combines two topics into a single long sentence, which also encourages (lines 6–9) the patient to clarify matters that are unclear to her. The nurse's words leave room for the patient's own thoughts and invites her to look for a personally meaningful way to connect the nurse's questions about the preparations (line 5) for the operation to her lack of information (lines 7–9). Encouraging statements can stimulate the patient to think in a way that is personally meaningful to her and to participate in the conversation ( van Ryn and Heaney, 1997 ; Tomm, 1988). Here, encouragement takes a form that is different from what Feste and Anderson ( Feste and Anderson, 1995 ) suggested; it is given in a more sophisticated manner. The opening words ( Extract 1 ) correspond with the goal that the nurse states later during the interview: `that the patient would receive the information she needs, what she wants to know and that she would feel safe to come, that at least those worst fears would be like forgotten. That she would feel safe'.
An encounter can threaten a patient's need for autonomy and freedom because it gives the nurse the legitimate power to request information about the patient's private life ( van Ryn and Heaney, 1997 ). Here, the nurse is mitigating her power by avoiding threatening terms and using tentative formulations (`would like to, well er, you you'), the emphasis being on the patient's needs. The opening of the interview by the nurse plays an important role in the development of the atmosphere. The act has been planned in advance but is not thoroughly thought out. In addition to conveying information, the main consideration in setting the goal for the discussion is to help the patient deal with her concerns. These are issues that have also been stressed in earlier studies ( Häggman-Laitila and Åstedt-Kurki, 1994 ; Breemhaar et al. , 1996 ; Leinonen et al. , 1996 ; Lindsey and Hartrick, 1996 ; Otte, 1996 ).
Tactful exploration: activation of reflection
Later during the interview, the patient mentions having thought about the impending surgery, which the nurse interprets as an indication of fear for the operation ( Extract 2 ). She indirectly gives the patient an opportunity to deal with her fears. The patient's words (lines 1, 3, 5 and 7) are related to the previous topic and her status during the operation and conclude the discussion. The nurse changes the subject (line 9) by praising the doctor's skill. The nurse and the patient look at each other.
1 P:mmm[think about during the day]= 2 N:[of] course ((nod+)) 3 P:=what's going to happen and (.) 4 N:right ((nod+)) 5 P:°like[that]° (.) 6 N:[mmm] 7 P:°it's[okay]° ((nod+, vo–)) 8 N: [that's] right (.) ((glance at papers: doctor's 9 name)) is is an excellent surgeon so in that 10 respect you can definitely (.) ((vo–)) feel 11 safe ((nod+)) that 12 P:yes of course I am 13 N:mmm 14 P: and and absolutely 110% (.) I trust that (.) 15 the thing is that (.) this is small case for 16 him but this is a horribly big thing for me…
The nurse's comment about the operating surgeon contains an allusion to fear of surgery. Instead of soothing the patient by telling her not to be afraid or asking if the patient is scared, the nurse indirectly comments on the doctor's professional skill (line 9) and emphasizes the expertise as a guarantee of success (line 10 and 11). Thus, the nurse allows the patient to save face when she leaves her to interpret her words. Her indirectness implies politeness and gives the patient options: if she does not want to deal with her fear, she may choose not to take the hint [see ( Brown and Levinson, 1987 )]. Here, politeness can also be linked to and interpreted through empowering practice, where the nurse holds the patient in high regard [ cf . ( van Ryn and Heaney, 1997 )].
The extract might have been interpreted as an example of the nurse cutting the patient off if one had not seen the videotape. Our interpretation is supported by a number of factors. First of all, the entire conversation until this extract has been tranquil and calm, the nurse has spoken and asked questions at a gentle pace, with pauses, and she has explored the patient's experiences. In this extract, the situation is similar, and she looks at the patient and nods. She speaks quite slowly, and her voice is low, friendly, and convincing ( van Ryn and Heaney, 1997 ). We can also see that the patient completes her speech by pausing (lines 3 and 5) and lowering her voice (lines 5 and 7). Therefore, after the nurse's words (lines 8–11), the patient presents her fear for discussion (lines 15 and 16) and also returns to the matter later during the interview. The extract shows how the issue has been constructed together by the nurse and the patient. The nurse raises the theme in a sensitive and non-threatening manner, and the patient continues the same topic. It also shows that the relationship is confidential enough for the patient to disclose her concerns and become aware of her own understanding, and thus contributes to empowerment. Salmon ( Salmon, 1993 ) has stressed that the main goal in the discussions between nurses and patients before surgery is not to reduce the patients' fears but to help them to deal with them.
Indirectness is a polite feature of discourse. There is `strategic indefiniteness' in indirectness that offers patients an opportunity to continue a discussion according to their own wishes ( Brown and Levinson, 1987 ). In general, nurses' empowering acts are mostly manifested in the form of questions ( Poskiparta et al. , 2000 ). In some cases, an indirect comment by a nurse, instead of a question, may encourage patients to talk about topics that they fear. Here it generates reflection in the patient. After disclosing her concerns, the patient analyzes the situation and recounts the conversation that she had with the doctor who explained the reason for her back surgery ( Extract 3 ).
Extract 3 .
1 P:this morning ((doctor's name)) said that 2 N:`this morning' ((surprised)) 3 P:this morning 4 N:that's recent for sure 4 P:yes 5 N:well it happened so 6 P: so it happened suddenly because yesterday 7 it became evident that (.) there was in the 8 X-ray ((doctor's name)) said that there was 9 a cause when I asked if there was anything 10 that caused the pain or if I was just imagining 11 it (.) so he said that yes there was a 12 genuine cause…
The amount of information given always depends on the situation and the nurse needs to continually evaluate the patient's needs: what it is that the patient knows, wants to know and how much she does want to know. This is also important because there are several persons that the patient sees before surgery ( Breemhaar et al. , 1996 ). Furthermore, nurses and doctors may deal with the same issues in their counseling. In Finland, the doctors, the surgeon and the consultant anaesthetist inform patients about the medical facts, risks, and benefits of operations. The patient also has an interview with a nurse on the surgical ward and, in addition to these encounters, there will occasionally be an encounter with a nurse anesthetist.
The nurse's empowering approach is manifested in how she raises issues or questions from time to time as if with hesitation. A pause precedes questions [`I don't have any (.) questions to ask you any more but do you—you have anything to ask from me like such things about tomorrow that worry you') ((looks at the patient))]. She asks the questions more quietly than normal and looks at the patient. According to Beck and Ragan's ( Beck and Ragan, 1992 ) study, nurses' softening words and their hesitant and tentative manner of speaking indicate discretion and tact and are aimed at not embarrassing patients. In our data, slow and hesitant speech also encourages the patients to comment more than nurses' more usual and brief question does: `Do you have any questions?'.
The nurse's tentative manner of asking questions makes it easier for the patient to start dealing with her concerns. She repeatedly pauses briefly and, in addition to the closed questions in the medical history questionnaire, she asks open-ended questions that explore the patient's experiences: `What kind of memories do you have of previous operations?' `Is there anything else you remember (.) is there something?'. Open-ended questions encourage the patient to speak and participate, e.g. in the naming and solving of a problem [ cf . ( Feste and Anderson, 1995 ; van Ryn and Heaney, 1997 )]. In this particular case, indirectness and hesitation are polite speech formulae that help the patient to save face ( Fairclough, 1992 ). They can also serve as empowering strategies that provide unconditional positive regard and acceptance for patients.
Despite these quite extensive empowering acts, the nurse subsequently evaluated her information skills only. She indicated how difficult it was for her to decide what kind of information to give to the patient:
I wondered if I should have maintained a more professional role, I mean more facts, if the patient got all that she wanted. Because this is not really medical science, you know, that's up to the doctor. It has to happen on the patient's terms, what she wants to know. I tried to check the patient's needs several times.
The content of the session satisfied the patient as well:
I got enough information about the operation, things that occupied my mind, so I didn't, she even told me before I asked. There's nothing to find out any more. As I said to her, I'm terribly afraid but I'll go ahead with confidence.
The nurse's way of posing questions builds up interaction. With her questions she steers the discussion thematically. This is how she controls the conversation. On the other hand, it is the patient who determines the content of the discussion. Her answers are reflective and bring up new issues. When the patient speaks, the nurse supports her with various feedback (e.g. Extracts 2 and 3) `mmm, right, of course, yes, exactly' and sometimes by paraphrasing. She nods a lot, bends toward the patient and looks at her. The feedback also occasionally includes completing the patient's sentences. According to van Ryn and Heaney ( van Ryn and Heaney, 1997 ), such non-verbal cues signal acceptance and, according to Caris-Verhallen et al. ( Caris-Verhallen et al. , 1999 ), they are patient-centered. With her feedback the nurse shows that she is there to listen to the patient, that she does not want to interrupt. Her feedback encourages the patient to speak in a similar way as in the doctor–patient conversation of an alternative medical interview described by Fairclough ( Fairclough, 1992 ). The patient interprets the feedback as encouragement, goes on to discuss the matter, and indicates her intention to continue by using the expressions `What I have been wondering…', `I did that when…' and `on the other hand, it's…'. This is how the nurse supports the patient's right to speak, which is not necessarily typical of a medical conversation ( Fairclough, 1992 ). The nurse's multi-facetted listening feedback is empowering, and this can be seen here and there in the data [see also ( Poskiparta et al. , 2000 )]. In this encounter, the feedback is exceptional because it disregards the participant's status. Generally, this type of feedback is directed to the dominant person ( Hakulinen, 1989 ). In a medically oriented environment, the hospital staff are viewed as superior to patients in knowledge ( van Ryn and Heaney, 1997 ; Tones, 1994 ). In this particular case, the nurse's listening feedback manifests power sharing.
When the patient discusses the reason for her admission to the hospital, the nurse builds up a positive, healthier vision of the future through other patients' experiences ( Extract 4 ). She makes her professional knowledge and expertise available to the patient ( Williams, 1995 ; McWilliam et al. , 1997 ). This lends a touch of reality and possibly builds on the patient's strengths ( van Ryn and Heaney, 1997 ) in this situation. The nurse attempts to dispel the patient's concerns about the risks of the operation. Her tone is convincing, and her non-verbal messages also inspire confidence: she looks at the patient, reinforces her message by nodding her head and gestures with her hands. Encouraged by the nurse, the patient can have a vision of her postoperative future.
Extract 4 .
1 N:these these ((ha+)) back operations are 2 like such that patients in them are usually 3 really grateful ((nod+)) after the operation 4 because if the operation like succeeds and 5 something is found (.) then the pain will be 6left in the operating room (.) ((ha+)) and 7 in that in that this is like like different from 8 other operations (.) and then because the 9 woundpainisinthebacksomehowit's 10 different than in here if the wound was here 11 inthestomach(ha+))andit'snotthatthat 12bad when it is if[you]= 13 P:[yeah] 14 N:=afterthosestomachoperationsyouoften 15 often hear that these patients who have had 16their back operated are such fortunate 17((nod+)) cases in the sense [that]= 18 P:[yeah] ((nod+)) 19 N:= because the pain will be left in the 20 operating room and and that's it then 21 ((nod+/ha+))
The nurse encourages the patient to examine her life at some hypothetical future point of time when the operation will have succeeded. Hypothetical questions encourage patients to discuss issues that they fear [ cf . ( Peräkylä, 1995 ; Tomm, 1987 )], while a hypothetical positive situation encourages patients indirectly. In this case, discussing the past would not calm the patient but rather lead her thoughts to the incident that caused her hospitalization. The vision of the future that the nurse provides to the patient with may help relieve her. A positive example is an empowering message and displays the nurse's understanding of the patient's anxiety. This vision can tap new resources in the patient for facing the future that is suddenly uncertain [ cf . ( van Ryn and Heaney, 1997 )]. Some manifestations of this can be seen in the patient's words: `…I'm very happy that if it's going to be over (.) yes I'm ready though I feel nervous' or `…I'm going ahead with confidence…'. A skilful use of future focus by the nurse helps the patient to find new solutions to her problems [ cf . ( Tomm, 1987 )]. As Atwood ( Atwood, 1995 ) suggests, confining the clients' thoughts to their problems is not sufficient in therapy work (focus on the past). In addition, we need to assist clients to expand their outlook by re-visioning their lives (future focus).
The encounter that is presented here as a case study demonstrates empowering nursing practice in hospital. It is a concrete example of a discussion during which the official and formal nature that characterizes the role of an institutional nurse is not emphasized. It actually emphasizes partnership and reciprocal conversation [ cf . ( van Ryn and Heaney, 1997 ; Poskiparta et al. , 2000 )], with the nurse's social interaction skills at the heart of the encounter [ cf . ( Wiles, 1997 )]. The patient is free to discuss her thoughts, concerns, experiences and even fears with the nurse, and the nurse adopts an empowerment strategy in order to facilitate the patient's participation. This encounter included the following empowering practices: (1) opening the session in an encouraging and constructive manner, which improves the atmosphere, (2) tactful exploration when examining the patient's need for information and concerns for surgery, (3) active, power sharing listening, and (4) building up a positive vision of the future.
The descriptions of empowerment strategies reported by van Ryn and Heaney ( van Ryn and Heaney, 1997 ) support our findings. However, we agree with Northouse's ( Northouse, 1997 ) criticism that the reported strategies are not completely separated. In our study, empowerment was manifested through intimacy and mutual respect. The nurse's encouragement of the patient's participation and her attempt to share power signaled acceptance, and perhaps gave the patient new insights for controlling her feelings about the impending surgery. Furthermore, the perceptions of active listening feedback and questioning are consistent with our previous studies ( Poskiparta et al. , 1998 , 2000 ; Kettunen et al. , 2000 ), where we found them to be a means of activating patients' self-evaluation and self-determination. In this study, we did not find evidence for empowering stories or questions that relate to patients' personal philosophy, as mentioned by Feste and Anderson ( Feste and Anderson, 1995 ). In addition, the nurse's encouragement was more sophisticated than what Feste and Anderson suggest with their empowering tools.
Our research data consisted of only one videotaped session per patient. Thus we have no evidence about how patients' decision-making skills develop or their self-esteem improves. During the interviews we did not ask the patients' opinion on the effects of counseling and that is why the patients evaluated conversations at a quite general level. In this particular case, the patient said that an encounter was ` illuminating ' for her. She mentioned that she received enough information and again spoke about her fears but used the same words as the nurse did when she emphasized a positive vision of future (see Extract 4 , lines 5, 6, 19 and 20): `if it's a fact that the pain will be left in the operating room, if it really is possible…that there's going to be an operation and they'll do it tomorrow, then that's how it's going to be'. This could, perhaps, signify some kind of relief or new resources to face an uncertain future. During the interview it also became evident that the patient's fears had not been diminished, but she talked about them and stressed a strong reliance on the professionals and on the operation as a whole: `I believe what I'm told'. This is in line with the perspective of Salmon ( Salmon, 1993 ), who emphasized that patients' anxiety about surgery should not be seen as a problem but rather as a normal phenomenon, a sign of patients' emotional balance, of an ability to feel fear. Thus, the nurse's task is not to diminish the patient's fears but to facilitate the patient's disclosure and offer help for dealing with fear.
With caution, we can speculate on the factors behind this kind of empowering practice, which became evident during the subsequent interviews. There was no evidence that nurses' or patients' age, education or work experience influenced the format of the counseling. What makes this case different from traditional rigid counseling sessions is that the nurse had a goal that she had planned in advance and pursued flexibly. This indicates that she had reflected on the significance of this situation from the patient's perspective. In most cases, nurses approached counseling without any goal or the hospital provided a detailed agenda based on professional knowledge of diseases, their care and prevention. Then, different kinds of institutionalized health counseling packages seemed to restrict nurses' communication, and health counseling often followed the standard institutional order of phases mentioned by Drew and Heritage ( Drew and Heritage 1998 ).
This study highlights empowering opportunities that arise in actual situations and that nurses can consciously use in their work. The results of this study can be applied to other health counseling practices and we would argue that every nurse should consider how (s)he initiates discussion. The analysis of the encounter shows that a tentative discussion style gives the patient a chance to deal with her concerns and to absorb the information that she needs. Thus, the patient has an opportunity to participate more actively in the discussion from the beginning than she could in the case of filling out a questionnaire in a strict predetermined order.
Clearly there are limitations to the generalizability of these findings. For example, both interlocutors were women, and this could in part explain the nature of the conversation since the highest levels of empathic and positive behavior occur between females [see ( Coates, 1986 ; Roter and Hall, 1993 ), p. 63]. There is also some concern whether the nurse may have been subject to a performance bias because she was aware of being videotaped and possibly behaved differently. However, we think that this was limited because only two nurses discussed this type of bias in the interviews afterwards and other nurses did not even notice the camera or did so only briefly at the beginning of counseling [see also ( Caris-Verhallen et al. , 1998 )]. Techniques to enhance the credibility of the findings included data and methodological triangulation of research data ( Patton, 1990 ; Stake, 1994 ; Begley, 1996 ), and acquiring data that included both verbal and non-verbal communication from the videotaped health counseling sessions and the subsequent interviews. In addition, team analysis sessions (investigator triangulation) ensured the accuracy of data interpretation (Polit and Hunger 1995). Different expertise helped us to get more complete picture from this case and empowerment philosophy when we discussed interpretations together.
However, in the last analysis, the effect of an empowering encounter could be checked after the operation by checking the patient's perspective, e.g. her satisfaction, recovery rate, etc. Evidence from nursing and medical staff might also be offered as additional evidence. Further research from larger numbers of patients is needed and more evidence from different settings will be required for a more extensive description of empowering practice. We will continue our research, and, for example, present qualitative analysis of interaction by describing how power features and patients' taciturnity are manifested in nurse–patient counseling. In addition, we will investigate how student nurses make progress in empowering counseling.
We suggest that nurses should pay attention to verbal expression and forms of language, in addition to non-verbal messages, because then they can empower patients by opening new and important perspectives for them. Nurses' every question, remark or piece of advice leads to individualized understanding and interpretation by the patient. It is important to remember that each communication situation is a unique, dynamic and transforming process. Nurses should observe what figures of speech they use and thus gain self-awareness and discover new tools to work with. We suggest a training program where the development of health care professionals' empowering skills can occur in practical, dynamic communication situations, be videotaped and transcribed for later theoretical, conscious and instructive evaluation. Analyzing the transcripts of video or tape-recorded counseling sessions opens up the possibility of an exact evaluation of empowering skills.
In health counseling, it is important that patients are able to maintain and strengthen a positive image of themselves as communicators. Positive experiences build up patients' self-esteem and increase their confidence in their ability to influence their care. The mere opportunity to discuss one's opinions and interpretations or different health concerns with a nurse may have the effect of unlocking patients' mental resources. This article demonstrates particularly how unconditional acceptance and facilitation of participation can be used in interpersonal counseling [see ( van Ryn and Heaney, 1997 )]. The empowering practices that are presented in this article should not be regarded as rigid and formalistic, rather they should be adapted to one's personal style.
Empowering principles of interpersonal practice ( van Ryn and Heaney, 1997 )
| Provide clients with unconditional positive regard and acceptance . | Facilitate client participation . |
|---|---|
| Make empathic acceptance statements | Ask open-ended questions |
| Use non-verbal cues that signal acceptance | Meet client statements with acceptance |
| Avoid criticizing or blaming clients | Develop active listening skills |
| Avoid engaging in psychological interpretations or psychoanalysis of clients' motives, conflicts or defenses | Reduce social distance between health educator by highlighting similarities |
| Use active listening processes to identify, to reflect back and to build on clients' strengths | Share all information and resources relevant to thethemes that are raised as part of the participatory process |
| Examine self and setting for barriers to providing unconditional positive regard and acceptance, and generate and implement methods for overcoming such barriers |
| Provide clients with unconditional positive regard and acceptance . | Facilitate client participation . |
|---|---|
| Make empathic acceptance statements | Ask open-ended questions |
| Use non-verbal cues that signal acceptance | Meet client statements with acceptance |
| Avoid criticizing or blaming clients | Develop active listening skills |
| Avoid engaging in psychological interpretations or psychoanalysis of clients' motives, conflicts or defenses | Reduce social distance between health educator by highlighting similarities |
| Use active listening processes to identify, to reflect back and to build on clients' strengths | Share all information and resources relevant to thethemes that are raised as part of the participatory process |
| Examine self and setting for barriers to providing unconditional positive regard and acceptance, and generate and implement methods for overcoming such barriers |
This study was supported by the Ministry of Health and Social Affairs of Finland and by the Finnish Cultural Foundation. We are sincerely grateful to all that participated in this study.
Anderson, J. M. ( 1996 ) Empowering patients: issues and strategies. Social Science and Medicine , 43 , 697 –705.
Anderson, R. M., Funnell, M. M., Butler, P. M., Arnold, M. S., Fitzgerald, J. T. and Feste, C. C. ( 1995 ) Patient empowerment. Results of randomized controlled trial. Diabetes Care , 18 , 943 –949.
Atwood, J. D. ( 1995 ) A social constructionist approach to counseling the single parent family. Journal of Family Psychotherapy , 6 , 1 –32.
Beck, C. S. and Ragan, S. L. ( 1992 ) Negotiating interpersonal and medical talk: frame shifts in the gynaecologic exam. Journal of Language and Social Psychology , 11 , 47 –61.
Begley, C. M. ( 1996 ) Using triangulation in nursing research. Journal of Advanced Nursing , 24 , 122 –128.
Breemhaar, B., van den Born, H. W. and Mullen, P. D. ( 1996 ) Inadequacies of surgical patient education. Patient Education and Counseling , 28 , 31 –44.
Brown, P. and Levinson, S. C. (1987) Politeness. Some Universals in Language Usage. Cambridge University Press, Cambridge.
Caris-Verhallen, W. M. C. M., Kerkstra, A., van der Heijden, P. G. M. and Bensing, J. M. ( 1998 ) Nurse–elderly patient communication in home care and institutional care: an explorative study. International Journal of Nursing Studies , 35 , 95 –108.
Caris-Verhallen, W. M. C. M., Kerkstra, A. and Bensing, J. M. ( 1999 ) Non-verbal behaviour in nurse–elderly patient communication. Journal of Advanced Nursing , 29 , 808 –818.
Coates, J. (1986) Women , Men and Language. A Sociolinguistic Account of Sex Differences in Language. Longman, New York.
Drew, P. and Heritage, J. (1998) Analyzing talk at work: an introduction. In Drew, P. and Heritage, J. (eds), Talk at Work. Interaction in Institutional Settings. Cambridge University Press, Cambridge, pp. 3–65.
Fairclough, N. (1992) Discourse and Social Change. Polity Press, Cambridge, pp. 134–168.
Feste, C. and Anderson, R. M. ( 1995 ) Empowerment: from philosophy to practice. Patient Education and Counseling , 26 , 139 –144.
Goffman, E. (1967/1982) Interaction Ritual. Doubleday, New York, pp. 5–45.
Hakulinen, A. (1989) Keskustelun luonnehtimisesta konteksti- ja funktionaalisten tekijöiden nojalla. [Characterizing the conversation according to contextual and functional factors]. In Hakulinen, A. (eds), Kieli 4 Suomalaisen Keskustelun Keinoja I. Helsingin Yliopiston Suomen Kielen Laitos, Helsinki, pp. 41–72.
Häggman-Laitila, A. and Åstedt-Kurki, P. ( 1994 ) What is expected of nurse–client interaction and how these expectations are realized in Finnish health care. International Journal of Nursing Studies , 31 , 253 –261.
Kar, S. B., Pascual, C. A. and Chickering, K. L. ( 1999 ) Empowerment of women for health promotion: a meta-analysis. Social Science and Medicine , 49 , 1431 –1460.
Kettunen, T., Poskiparta M. and Liimatainen, L. (2000) Communicator styles of hospital patients during nurse–patient counseling. Patient Education and Counseling , in press.
Labonte, R. ( 1994 ) Health promotion and empowerment: reflections on professional practice. Health education quarterly , 21 , 253 –268.
Laitakari, J. ( 1998 ) How to develop one's counseling—demonstration of the use of single-case studies as a practical tool for evaluating the outcomes of counseling. Patient Education and Counseling , 33 , S39 –S46.
Leino-Kilpi, H. ( 1991 ) Good nursing care—the relationship between client and nurse. Hoitotiede , 3 , 200 –206.
Leinonen, T., Leino-Kilpi, H. and Katajisto, J. ( 1996 ) The quality of intraoperative nursing care: the patient's perspective. Journal of Advanced Nursing , 24 , 843 –852.
Lindsey, E. and Hartrick, G. ( 1996 ) Health-promoting nursing practice: the demise of the nursing process? Journal of Advanced Nursing , 23 , 106 –112.
Mattus, M.-R. (1994) Interview as intervention: strategies to empower families of children with disabilities. In Leskinen, M. (ed.), Family in Focus. New Perspectives on Early Childhood Special Education. Jyväskylä Studies in Education, Psychology and Social Research 108. Jyväskylä University Printing House, Jyväskylä, pp. 87–107.
McWilliam, C. L., Stewart, M., Brown, J. B., McNair, S., Desai K., Patterson, M. L., Del Maestro, N. and Pittman, B. J. ( 1997 ) Creating empowering meaning: an interactive process of promoting health with chronically ill older Canadians. Health Promotion International , 12 , 111 –123.
Northouse P. G. 1997 . Effective helping relationships: the role of power and control. Health Education and Behavior , 24 , 703 –706.
Otte, D. I. ( 1996 ) Patients' perspectives and experiences of day case surgery. Journal of Advanced Nursing , 23 1226 –1237.
Patton, M. G. (1990) Qualitative Evaluation and Research Methods. Sage, Newbury Park, CA, pp. 388–390.
Pearson, P. ( 1991 ) Clients' perceptions: the use of case studies in developing theory. Journal of Advanced Nursing , 16 , 521 –528.
Peräkylä, A. (1995) AIDS Counselling. Institutional Interaction and Clinical Practice . Cambridge University Press, Cambridge.
Polit, D. F. and Hungler, B. P. (1995) Nursing Research. Principles and Methods. Lippincott, Philadelphia, PA.
Poskiparta, M., Kettunen, T. and Liimatainen, L. ( 1998 ) Reflective questions in health counseling. Qualitative Health Research , 8 , 682 –693.
Poskiparta, M., Kettunen, T. and Liimatainen, L. ( 2000 ) Questioning and advising in health counseling. Results from a study of Finnish nurse counselors. Health Education Journal , 95 , 47 –67.
Roter, D. L. and Hall, J. A. (1993) Doctors Talking with Patients/Patients Talking with Doctors . Greenwood, Westport, CT.
van Ryn, M. and Heaney, C. A. ( 1997 ) Developing effective helping relationships in health education practice. Health Education and Behavior , 24 , 683 –702.
Salmon, P. ( 1993 ) The reduction of anxiety in surgical patients: an important nursing task or the medicalization of preparatory worry? International Journal of Nursing Studies , 30 , 323 –330.
Stake, R. E. (1994) Case studies. In Denzin, N. K. and Lincoln, Y. S. (eds), Handbook of Qualitative Research. Sage, Newbury Park, CA, pp. 236–247.
Tomm, K. ( 1987 ) Interventive interviewing: part II. Reflexive questioning as a means to enable self-healing. Family Process , 26 , 197 –183.
Tones, K. (1994) Health promotion, empowerment and action competence. In Jensen B. B and Schnack, K. (eds), Action and Action Competence as Key Concepts in Critical Pedagogy. Studies in Educational Theory and Curriculum . Royal Danish School of Educational Studies, vol. 12, pp. 163–183.
Tones, K. ( 1995 ) Editorial. Health Education Research , 10 , i –v.
Wiles, R. ( 1997 ) Empowering practice nurses in the follow-up of patients with established heart disease: lessons from patients' experiences. Journal of Advanced Nursing , 26 , 729 –735.
Williams, J. ( 1995 ) Education for empowerment: implications for professional development and training in health promotion. Health Education Journal , 54 , 37 –47.
| Month: | Total Views: |
|---|---|
| November 2016 | 13 |
| December 2016 | 9 |
| January 2017 | 17 |
| February 2017 | 44 |
| March 2017 | 41 |
| April 2017 | 61 |
| May 2017 | 30 |
| June 2017 | 14 |
| July 2017 | 7 |
| August 2017 | 10 |
| September 2017 | 14 |
| October 2017 | 39 |
| November 2017 | 86 |
| December 2017 | 351 |
| January 2018 | 396 |
| February 2018 | 436 |
| March 2018 | 654 |
| April 2018 | 425 |
| May 2018 | 276 |
| June 2018 | 225 |
| July 2018 | 300 |
| August 2018 | 345 |
| September 2018 | 354 |
| October 2018 | 369 |
| November 2018 | 452 |
| December 2018 | 412 |
| January 2019 | 271 |
| February 2019 | 264 |
| March 2019 | 552 |
| April 2019 | 913 |
| May 2019 | 570 |
| June 2019 | 414 |
| July 2019 | 438 |
| August 2019 | 430 |
| September 2019 | 337 |
| October 2019 | 407 |
| November 2019 | 338 |
| December 2019 | 246 |
| January 2020 | 274 |
| February 2020 | 245 |
| March 2020 | 312 |
| April 2020 | 275 |
| May 2020 | 165 |
| June 2020 | 217 |
| July 2020 | 208 |
| August 2020 | 182 |
| September 2020 | 276 |
| October 2020 | 232 |
| November 2020 | 187 |
| December 2020 | 138 |
| January 2021 | 157 |
| February 2021 | 207 |
| March 2021 | 261 |
| April 2021 | 232 |
| May 2021 | 198 |
| June 2021 | 139 |
| July 2021 | 134 |
| August 2021 | 153 |
| September 2021 | 231 |
| October 2021 | 204 |
| November 2021 | 204 |
| December 2021 | 140 |
| January 2022 | 152 |
| February 2022 | 229 |
| March 2022 | 268 |
| April 2022 | 218 |
| May 2022 | 254 |
| June 2022 | 148 |
| July 2022 | 134 |
| August 2022 | 95 |
| September 2022 | 173 |
| October 2022 | 189 |
| November 2022 | 247 |
| December 2022 | 163 |
| January 2023 | 131 |
| February 2023 | 125 |
| March 2023 | 124 |
| April 2023 | 134 |
| May 2023 | 94 |
| June 2023 | 89 |
| July 2023 | 96 |
| August 2023 | 118 |
| September 2023 | 98 |
| October 2023 | 132 |
| November 2023 | 170 |
| December 2023 | 121 |
| January 2024 | 96 |
| February 2024 | 78 |
| March 2024 | 127 |
| April 2024 | 142 |
| May 2024 | 130 |
| June 2024 | 49 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Case Examples
Examples of recommended interventions in the treatment of depression across the lifespan.

Children/Adolescents
A 15-year-old Puerto Rican female
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. Her more recent episodes related to her parents’ marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT).
Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety , 26, 98-103. https://doi.org/10.1002/da.20457
Sam, a 15-year-old adolescent
Sam was team captain of his soccer team, but an unexpected fight with another teammate prompted his parents to meet with a clinical psychologist. Sam was diagnosed with major depressive disorder after showing an increase in symptoms over the previous three months. Several recent challenges in his family and romantic life led the therapist to recommend interpersonal psychotherapy for adolescents (IPT-A).
Hall, E.B., & Mufson, L. (2009). Interpersonal Psychotherapy for Depressed Adolescents (IPT-A): A Case Illustration. Journal of Clinical Child & Adolescent Psychology, 38 (4), 582-593. https://doi.org/10.1080/15374410902976338
© Society of Clinical Child and Adolescent Psychology (Div. 53) APA, https://sccap53.org/, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Society of Clinical Child and Adolescent Psychology (Div. 53) APA.
General Adults
Mark, a 43-year-old male
Mark had a history of depression and sought treatment after his second marriage ended. His depression was characterized as being “controlled by a pattern of interpersonal avoidance.” The behavior/activation therapist asked Mark to complete an activity record to help steer the treatment sessions.
Dimidjian, S., Martell, C.R., Addis, M.E., & Herman-Dunn, R. (2008). Chapter 8: Behavioral activation for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 343-362). New York: Guilford Press.
Reprinted with permission from Guilford Press.
Denise, a 59-year-old widow
Denise is described as having “nonchronic depression” which appeared most recently at the onset of her husband’s diagnosis with brain cancer. Her symptoms were loneliness, difficulty coping with daily life, and sadness. Treatment included filling out a weekly activity log and identifying/reconstructing automatic thoughts.
Young, J.E., Rygh, J.L., Weinberger, A.D., & Beck, A.T. (2008). Chapter 6: Cognitive therapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 278-287). New York, NY: Guilford Press.
Nancy, a 25-year-old single, white female
Nancy described herself as being “trapped by her relationships.” Her intake interview confirmed symptoms of major depressive disorder and the clinician recommended cognitive-behavioral therapy.
Persons, J.B., Davidson, J. & Tompkins, M.A. (2001). A Case Example: Nancy. In Essential Components of Cognitive-Behavior Therapy For Depression (pp. 205-242). Washington, D.C.: American Psychological Association. http://dx.doi.org/10.1037/10389-007
While APA owns the rights to this text, some exhibits are property of the San Francisco Bay Area Center for Cognitive Therapy, which has granted the APA permission for use.
Luke, a 34-year-old male graduate student
Luke is described as having treatment-resistant depression and while not suicidal, hoped that a fatal illness would take his life or that he would just disappear. His treatment involved mindfulness-based cognitive therapy, which helps participants become aware of and recharacterize their overwhelming negative thoughts. It involves regular practice of mindfulness techniques and exercises as one component of therapy.
Sipe, W.E.B., & Eisendrath, S.J. (2014). Chapter 3 — Mindfulness-Based Cognitive Therapy For Treatment-Resistant Depression. In R.A. Baer (Ed.), Mindfulness-Based Treatment Approaches (2nd ed., pp. 66-70). San Diego: Academic Press.
Reprinted with permission from Elsevier.
Sara, a 35-year-old married female
Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks.
Bleiberg, K.L., & Markowitz, J.C. (2008). Chapter 7: Interpersonal psychotherapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: a treatment manual (4th ed., pp. 315-323). New York, NY: Guilford Press.
Peggy, a 52-year-old white, Italian-American widow
Peggy had a history of chronic depression, which flared during her husband’s illness and ultimate death. Guilt was a driving factor of her depressive symptoms, which lasted six months after his death. The clinician treated Peggy with psychodynamic therapy over a period of two years.
Bishop, J., & Lane , R.C. (2003). Psychodynamic Treatment of a Case of Grief Superimposed On Melancholia. Clinical Case Studies , 2(1), 3-19. https://doi.org/10.1177/1534650102239085
Several case examples of supportive therapy
Winston, A., Rosenthal, R.N., & Pinsker, H. (2004). Introduction to Supportive Psychotherapy . Arlington, VA : American Psychiatric Publishing.
Older Adults
Several case examples of interpersonal psychotherapy & pharmacotherapy
Miller, M. D., Wolfson, L., Frank, E., Cornes, C., Silberman, R., Ehrenpreis, L.…Reynolds, C. F., III. (1998). Using Interpersonal Psychotherapy (IPT) in a Combined Psychotherapy/Medication Research Protocol with Depressed Elders: A Descriptive Report With Case Vignettes. Journal of Psychotherapy Practice and Research , 7(1), 47-55.
- Section One: Introduction
- Section Two: Learning and Teaching Resources to Support Integration of Mental Health and Addiction in Curricula
- Section Three: Faculty Teaching Modalities and Reflective Practice
- Section Four: Student Reflective Practice and Self-Care in Mental Health and Addiction Nursing Education
- Section Five: Foundational Concepts and Mental Health Skills in Mental Health and Addiction Nursing
- Section Six: Legislation, Ethics and Advocacy in Mental Health and Addiction Nursing Practice
- Section Seven: Clinical Placements and Simulations in Mental Health and Addiction Nursing Education
- Section Eight: Reference and Bibliography
- Section Nine: Appendices and Case Studies
Section Nine
- Case Study 1
Also in this section
- Alignment between CASN/ CFMHN Entry-to-Practice Mental Health and Addiction Competencies and Sections in the Nurse Educator Mental Health and Addiction Resource
- Process Recording
- Criteria for Validation: Process Recording
- Criteria for Phase of Relationship: Process Recording
- Journaling Activity
- Safety and Comfort Plan Template
- Advocacy Groups for Mental Health in Canada
- Tips for Engaging Lived Experience
- Glossary of Terms
- Case Study 2
- Case Study 3
- Case Study 4
- Case Study 5
- Case Study 6
- Case Study 7
- Case Study 8
- Case Study 9
Teresa is a 32-year-old woman in your practice who frequently misses her appointments, and at other times shows up without an appointment, often in crisis. She currently uses alcohol and tobacco, and has started to use street drugs.
As you have developed a therapeutic relationship with Teresa, you learn that she grew up in a household with a violent father who frequently assaulted her mother, her siblings and herself. Although now estranged from her father, the impact of his violence presents itself on a daily basis as Teresa struggles to cope with the trauma she experienced.
Teresa left school early, has few marketable skills and has never been able to hold a job for more than three months. Teresa receives $606 per month from Ontario Works and has no money left for food or other essentials at the end of the month. She is currently in a relationship with a man whom you suspect may be violent
Student Questions
What are your next steps with Teresa? How do you go about providing trauma-informed care?
- Is a crisis intervention required?
- What are some other interventions you could take to improve Teresa’s health in this situation that include addressing health inequities and structural drivers of the conditions of daily life, such as the inequitable distribution of power, money and resources?
Educator elaborations
- Assess Teresa’s mental status and history of mental health care; explore her substance use and whether it places her at high risk for self medication and suicide; explore issues of violence in her life, income support and her housing situation.
Discussion Topics
- Cultural competency and mental illness
- Trauma informed care
- Crisis intervention
- Social determinants of health
- Printer-friendly version
Mental Health Nursing
At a glance, grahame smith.
- Your Feedback
- Become a reviewer
- More student books
- Student Apps
- Join an e-mail list

Buy now/find out more
Case Studies
Case 5: denise.
Denise, a 19-year-old woman, has been admitted informally to an acute mental health ward; this is Denise's first admission. Denise was being treated for depression by her GP; prior to her admission Denise attempted to kill herself by cutting her wrists. Subsequently a short admission was arranged with the aim of devising a comprehensive care package.
After speaking about the circumstances leading up to her suicide attempt Denise became increasingly tearful and distressed, and started demanding to see a doctor. After being told that the doctor was on their way and would arrive in about 10 minutes, Denise became angry demanding medication to calm her down; she then proceeded to run towards the ward's doors shouting that she wanted to go home. At that moment the doctor arrived on the ward and Denise also immediately calmed down.
During the assessment process Denise disclosed that being angry if she did not get her way was not unusual for her. She also mentioned that she felt awful after these bouts of anger. She described herself as a "terrible person who was out of control" and she just wanted to die. After assessing Denise the nurse started to formulate a plan of care.
(a) What type of psychological interventions would the nurse consider implementing?
Show Answer
- Build a collaborative and therapeutic relationship based on a person-centred approach.
- Normalise an individual's experiences of mental distress.
- Take a "strengths approach".
- Maintain safety and effectively manage challenging behaviours.
- Explore the individual's capacity to change.
- Modify thought processes – identify, challenge and replace negative thoughts.
- Focus on the individual controlling and regulating their behaviour – promoting and enhancing healthy ways of coping.
- Prevent social isolation and promote social functioning.
- Focus on relapse prevention – early warning signs and self-monitoring of symptoms.
- Signpost to self-help and relevant support groups.
- Therapeutically support recovery.
(b) Currently Denise has been admitted informally to the ward. Due to Denise's impulse control difficulties this may change. On this basis what does the nurse professionally need to know when managing Denise's legal status?
- Understand and apply current legislation in a way that protects Denise.
- Act in accordance with the law, relevant ethical and regulatory frameworks, and also take into account local protocols/policies.
- Respect and uphold Denise's rights
- Know when to actively share personal information with others when the interests of safety and protection override the need for confidentiality.
(c) Denise is subsequently diagnosed with a "borderline personality disorder". What other types of personality disorders are there?
- Cluster A – paranoid, schizoid and schizotypal.
- Cluster B – antisocial (type: dissocial), borderline (type: emotionally unstable), histrionic, and narcissistic (not included in types).
- Cluster C – avoidant (type: anxious), dependent, obsessive-compulsive (type: anankastic).
- paranoid – suspicious and excessively sensitive;
- schizoid – emotional coldness, little interest in other people;
- schizotypal – odd beliefs and unusual appearance;
- borderline – instability of mood, impulsive;
- histrionic – excessive attention seeking;
- narcissistic – grandiose and arrogant;
- antisocial – disregard of self and others;
- avoidant – feelings of inadequacy;
- dependent – submissive behaviour;
- 0bsessive-compulsive – a preoccupation with orderliness.
(d) What specific psychological interventions would the nurse deliver?
- boundary setting;
- promoting healthy ways of coping;
- motivational interviewing and pre-therapy work;
- delivering specific therapeutic approaches/therapies.
(e) How could the nurse learn from their experiences of working with Denise?
- identifying and describing the experiences;
- examining the experiences in depth and teasing out the key issues;
- critically processing the issues;
- learning from the experiences by implementing future actions that improve the nurse's practice.
Denise has now been on the ward for over 6 months. Each time discharge has been arranged Denise self-harms or threatens suicide. Denise has now agreed to go to a therapeutic community, a place has been secured and Denise is now engaging in pre-therapy work.
(a) What other treatments besides a therapeutic community are recommended for individuals diagnosed with a borderline personality disorder?
- cognitive behaviour therapy – group and individual;
- behavioural approaches;
- mentalisation-based approaches;
- dialectic behaviour therapy.
(b) While working with Denise the primary nurse has found the relationship at times to be quite stressful. What are the signs of stress?
- sleep problems;
- loss of appetite;
- difficulty concentrating;
- constantly feeling anxious;
- feeling irritable and/or angry;
- having repeating thoughts;
- avoiding certain situations and/or people;
- an increased use of alcohol;
- muscle tension.
(c) What strategies could the nurse use to manage their stress?
- engage in physical activity;
- engage in something that makes them laugh;
- learn relaxation and/or deep breathing techniques;
- take control of the situation;
- seek support and talk;
- problem solve;
- eat a healthily diet;
- drink plenty of water;
- be mindful.
(d) What process should be utilised as a way to support the primary nurse to improve their practice?
Correct answer: A common method of systematically reflecting on practice is through the clinical supervision, which is a formal activity where a clinical supervisor facilitates the nurse to reflect upon their practice and identify strategies that focus on improving their practice.
Consider Chapters 20, 34 and 37.
Print Answers | « Previous Case
A sample case study: Mrs Brown
On this page, social work report, social work report: background, social work report: social history, social work report: current function, social work report: the current risks, social work report: attempts to trial least restrictive options, social work report: recommendation, medical report, medical report: background information, medical report: financial and legal affairs, medical report: general living circumstances.
This is a fictitious case that has been designed for educative purposes.
Mrs Beryl Brown URN102030 20 Hume Road, Melbourne, 3000 DOB: 01/11/33
Date of application: 20 August 2019
Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke, which has left her with moderate weakness in her left arm and leg. A diagnosis of vascular dementia was also made, which is overlaid on a pre-existing diagnosis of Alzheimer’s disease (2016). Please refer to the attached medical report for further details.
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job. The eldest daughter Catherine lives on the Gold Coast with her family. Mrs Brown is a retired school teacher and she and both daughters describe her as a very private woman who has never enjoyed having visitors in her home. Mrs Brown took much encouragement to accept cleaning and shopping assistance once a week after her most recent admission; however, she does not agree to increase service provision. Jean has Enduring Power of Attorney (EPOA) paperwork that indicates that Mrs Brown appointed her under an EPOA two years ago. She does not appear to have appointed a medical treatment decision maker or any other decision-supporter.
I also understand from conversations with her daughters that Jean and Mrs Brown have always been very close and that there is a history of long-standing conflict between Catherine and Jean. This was exacerbated by the death of their father. Both daughters state they understand the impact of the stroke on their mother’s physical and cognitive functioning, but they do not agree on a discharge destination. Mrs Brown lacks insight into her care needs and says she will be fine once she gets back into her own home. Repeated attempts to discuss options with all parties in the same room have not resulted in a decision that is agreeable to all parties.
Mrs Brown has a history of Alzheimer’s disease; type II diabetes – insulin dependent; hypertension; high cholesterol and osteoarthritis. She has had two recent admissions to hospital for a urinary tract infection and a fall in the context of low blood sugars. She is currently requiring one to two people to assist her into and out of bed and one person with managing tasks associated with post-toilet hygiene. She can walk slowly for short distances with a four-wheel frame with one person to supervise. She benefits from prompting to use her frame; she needs someone to cut her food and to set her up to eat and drink regularly and to manage her medication routine. She requires one person to assist her to manage her insulin twice daily.
The team believe that Mrs Brown’s capacity for functional improvement has plateaued in the last ten days. They recommend that it is in her best interests to be discharged to a residential care setting due to her need for one to two people to provide assistance with the core tasks associated with daily living. Mrs Brown is adamant that she wants to return home to live with Jean who she states can look after her. Jean, who has a history of chronic back pain, has required several admissions to hospital over the past five years, and states she wants to be able to care for her mother at home. Jean states she is reluctant to agree to extra services as her mother would not want this. Her sister Catherine is concerned that Jean has not been coping and states that given this is the third admission to hospital in a period of few months, believes it is now time for her mother to enter residential care. Catherine states that she is very opposed to her mother being discharged home.
Mrs Brown is at high risk of experiencing falls. She has reduced awareness of the left side of her body and her ability to plan and process information has been affected by her stroke. She is now requiring one to two people to assist with all her tasks of daily living and she lacks insight into these deficits. Mrs Brown is also at risk of further significant functional decline which may exacerbate Jean’s back pain. Jean has stated she is very worried about where she will live if her mother is to enter residential care.
We have convened two family meetings with Mrs Brown, both her daughters and several members of the multi-disciplinary team. The outcome of the first meeting saw all parties agree for the ward to provide personalised carer training to Jean with the aim of trialling a discharge home. During this training Jean reported significant pain when transferring her mother from the bed and stated she would prefer to leave her mother in bed until she was well enough to get out with less support.
The team provided education to both Jean and Catherine about the progressive impact of their mother’s multiple conditions on her functioning. The occupational therapist completed a home visit and recommended that the downstairs shower be modified so that a commode can be placed in it safely and the existing dining room be converted into a bedroom for Mrs Brown. Mrs Brown stated she would not pay for these modifications and Jean stated she did not wish to go against her mother’s wishes. The team encouraged Mrs Brown to consider developing a back-up plan and explore residential care options close to her home so that Jean could visit often if the discharge home failed. Mrs Brown and Jean refused to consent to proceed with an Aged Care Assessment that would enable Catherine to waitlist her mother’s name at suitable aged care facilities. We proceeded with organising a trial overnight visit. Unfortunately, this visit was not successful as Jean and Catherine, who remained in Melbourne to provide assistance, found it very difficult to provide care without the use of an accessible bathroom. Mrs Brown remains adamant that she will remain at home. The team is continuing to work with the family to maximise Mrs Brown’s independence, but they believe that it is unlikely this will improve. I have spent time with Jean to explore her adjustment to the situation, and provided her with information on community support services and residential care services. I have provided her with information on the Transition Care Program which can assist families to work through all the logistics. I have provided her with more information on where she could access further counselling to explore her concerns. I have sought advice on the process and legislative requirements from the Office of the Public Advocate’s Advice Service. I discussed this process with the treating team and we decided that it was time to lodge an application for guardianship to VCAT.
The treating team believe they have exhausted all least restrictive alternatives and that a guardianship order is required to make a decision on Mrs Brown’s discharge destination and access to services. The team recommend that the Public Advocate be appointed as Mrs Brown’s guardian of last resort. We believe that this is the most suitable arrangement as her daughters are not in agreement about what is in their mother’s best interests. We also believe that there is a potential conflict of interest as Jean has expressed significant concern that her mother’s relocation to residential care will have an impact on her own living arrangements.
Mrs Brown’s medical history includes Alzheimer’s disease; type II diabetes; hypertension; high cholesterol and osteoarthritis. She was admitted to Hume Hospital on 3 March 2019 following a stroke that resulted in moderate left arm and leg weakness. This admission was the third hospital admission in the past year. Other admissions have been for a urinary tract infection, and a fall in the context hypoglycaemia (low blood sugars), both of which were complicated by episodes of delirium.
She was transferred to the subacute site under my care, a week post her admission, for slow-stream rehabilitation, cognitive assessment and discharge planning.
Mrs Brown was diagnosed with Alzheimer’s disease by Dr Joanne Winters, Geriatrician, in April 2016. At that time, Mrs Brown scored 21/30 on the Standardised Mini-Mental State Examination (SMMSE). During this admission, Mrs Brown scored 15/30. I have undertaken cognitive assessment and agree with the diagnosis; further cognitive decline has occurred in the context of the recent stroke. There are global cognitive deficits, but primarily affecting memory, attention and executive function (planning, problem solving, mental flexibility and abstract reasoning). The most recent CT-Brain scan shows generalised atrophy along with evidence of the new stroke affecting the right frontal lobe. My assessments suggest moderate to severe mixed Alzheimer’s and vascular dementia.
While able to recall some key aspects of her financial affairs, including the general monetary value of her pension and regular expenses, Mrs Brown was unable to account for recent expenditure (for repairs to her home) or provide an estimate of its value, and had difficulty describing her investments. In addition, I consider that she would be unable to make complex financial decisions due to her level of cognitive impairment. Accordingly, I am of the view that Mrs Brown now lacks capacity to make financial decisions.
Mrs Brown states that she previously made an Enduring Power of Attorney (EPOA) but could no longer recall aspects of the EPOA, such as when it would commence and the nature of the attorney’s powers. Moreover, she confused the EPOA with her will. Her understanding of these matters did not improve with education, and therefore I consider that she no longer has capacity to execute or revoke an EPOA.
Mrs Brown acknowledges that she needs some assistance but lacks insight into the type of assistance that she requires, apart from home help for cleaning and shopping. She does not appreciate her risk of falling. She is unable to get in and out of bed without at least one person assisting her. She frequently forgets to use her gait aid when mobilising and is not able to describe how she would seek help in the event of falling. She is not able to identify or describe how she would manage her blood sugar levels, and this has not improved with education. Accordingly, I consider that she lacks capacity to make decisions about accommodation arrangements and services.
Mrs Brown does not agree with the treating team’s recommendation to move into residential care and maintains her preference to return home. This is in spite of a failed overnight trial at home with both her daughters assisting her. Unfortunately, she was unable to get out of bed to get to the toilet and required two people to assist her to do so in the morning. In light of these matters, and in the context of family disagreement regarding the matter, the team recommends that the Office of the Public Advocate be appointed as a guardian of last resort.
Reviewed 22 July 2022
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Voluntary assisted dying
- Quality, safety and service improvement
- Planned surgery recovery and reform program
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Sustainability in Healthcare
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- Victorian Supercare Pharmacies
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public Dental and Community Health Program funding model review
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Inquiry into Women's Pain submissions
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Radiation newsletter
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Principles in the Mental Health and Wellbeing Act and the Chief Psychiatrist's guidelines
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Reporting obligations for clinical mental health and wellbeing services
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Office of the Chief Psychiatrist's reform activities and news
- Oversight of forensic mental health and wellbeing services
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Wellbeing and participation
- Age-friendly Victoria
- Healthy ageing
- Seniors participation
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Pathway to good health for children in care
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window
- NLN Certification
- Assessment Services
- CNEA Accreditation
- NLN Foundation
- Mission & Core Values
- History & Archives
- Board of Governors
- Senior Management
- Consultants & Speakers Bureau
- NLN Elections
- NLN Nominations
- Career Center

Henry and Ertha Williams
Julia morales and lucy grey, millie larsen.
- Developing Interprofessional Education and Practice in Oral Health
- Importance of Oral-Systemic Health in Older Adults
- Performing Oral Health Assessments on Aging Patients
- Oral Health for the Older Adult Living in the Community
- Elder Abuse in the United States
- Geriatric Syndromes
- Mental Health Needs of Older Adults
- Student-Led Geriatric Nursing Conference: Evidence in Practice
- Teaching Oral Health Care for Older Adults
- Using Case Study Betsy to Understand Down's Syndrome & Dementia
- Using Cinema to Enhance Teaching Issues Related to Older Adults
- Using the Monologue of Doris Smith to Understand Situational Decision-Making
- Caring for the Caregiver
- Caring for the Older Adult at Risk for Falling
- Coordinating and Managing Care During Transitions Among Care Settings
- End-of-Life Decision Making for Older Adults: Competent and Compassionate Care
- Myths of Aging
- Using Continuing Care Retirement Communities to Enhance a Better Understanding of Older Adults
- ACE.S Knowledge Domains
- ACE.S Essential Nursing Actions
- ACE.S Framework
- ACE.S Development & History
- ACE.S Additional Resources
- ACE.S Video Library
ACE.S Unfolding Cases
An unfolding case is one that evolves over time in a manner that is unpredictable to the learner. New situations develop and are revealed with each encounter. Every ACE unfolding case uses the highly regarded unfolding case model developed for Advancing Care Excellence for Seniors (ACE.S) . Each case includes the following:
- A first-person monologue that introduces the family and the complex problems they are facing.
- Simulation scenarios designed to help students practice assessing function and expectations of their patient(s), with links to appropriate evidence-based assessment tools. Suggestions for debriefing are included.
- An innovative final assignment that asks students to finish the story .
- Instructor toolkits with suggestions on how to use the various components of the unfolding cases and incorporate them into the curriculum.
These unfolding cases combine the power of storytelling with the experiential nature of simulation scenarios. They are intended to create a robust, meaningful experience for students, one that provides a simulated experience of continuity of care and that will help them integrate the Essential Knowledge Domains and Nursing Actions into their practice of nursing. We hope you will give them a try! Standardized/Simulated patients are recommended for all ACE simulations. If you are not already familiar with the Association for Standardized Patient Educators Standards of Best Practice, we encourage you to review them.
Learn more about unfolding cases by visiting the How to Use an Unfolding Case page.
Sherman "Red" Yoder
Nln leadership development program for simulation educators project mapping the ace.s unfolding cases to the aacn essentials.
Project Disclaimer: Simulation leadership projects are a requirement for the Leadership Development Program for Simulation Educators. All projects are then placed within SIRC for the benefit of the nursing education community. Inclusion of this specific project does not constitute an endorsement by the NLN of the AACN Essentials.
Unfolding Cases with Older Adults from Other ACE Programs
Butch sampson (ace.v), eugene shaw (ace.v), ertha williams (ace.z), george palo (ace.z), judy and karen jones (ace.z), mike walker (ace+).
Somatoform Disorder Case Study (30 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Access More! View the full outline and transcript with a FREE trial
A 22-year-old patient presents to the emergency room after a motor vehicle collision. The patient had airbag deployment and was wearing his seatbelt. The patient was hit on the passenger side by a vehicle going about 40 miles per hour. Extraction time was 5 minutes and the patient was ambulatory on the scene. No loss of consciousness was reported and the patient denies hitting their head. The patient is complaining of chest pain.
Which diagnostic tests should be performed for this patient?
- EKG and cardiac markers such as troponins.
- CBC to check for possible internal bleeding from the trauma
An EKG shows sinus tachycardia and the patients cardiac markers come back negative. The patient states, “I know what is happening to my body and I am having a heart attack! They hit me so hard that my heart stopped working! That is the only explanation for this pain in my chest! My grandfather died of a heart attack, so check again. Isn’t there another test we can do to make sure?” Despite reasoning with the patient and informing him his chest hurts from the seatbelt restraining him during the car accident, this patient is convinced he is having a heart attack.
What is the best therapeutic approach for this patient?
- This patient will not listen to science per-se so building a trusting relationship is key to help this patient listen to you.
- VALIDATE their concerns and feelings!!!! For example, “Being hit by another car is very jarring to the body, I have you on the cardiac monitor, so if anything shows up we will be able to intervene. Your heart is pumping at a fast rate so we will keep monitoring you.”
- Never tell the patient that they are being ridiculous/overly worrisome or that they are making it up.
- Comfort them by letting them know you are concerned and will be monitoring them.
What medication could help this patient calm down?
- Potentially a benzodiazepine such as Ativan or Xanax.
- This patient likely has a lot of adrenaline on board due to the intensity of being hit by another car, making their heart rate high.
- Don’t forget to always have the antidote on hand just in case: Flumazenil!)
You administer 2 mg IV Ativan and the patient is calming down, they report that they are still having a heart attack and want to go to cath-lab to be checked out. You explain to the patient that cath-lab is used for people having blockages in their cardiovascular system and would not be indicated for them since they are not having any ischemia in the heart. The patient insists that there has to be something wrong with their heart and that something needs to be done.
What is this patient likely suffering from?
- Somatoform disorder
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10661295

Breaking the Stigma in Mental Health Nursing through High-Fidelity Simulation Training
Agustín javier simonelli-muñoz.
1 Department of Nursing, Physiotherapy and Medicine, University of Almeria, 04120 Almería, Spain; se.lau@741ams (A.J.S.-M.); se.lau@932rjd (D.J.-R.); se.lau@ianauj (J.I.G.-G.)
Diana Jiménez-Rodríguez
Oscar arrogante.
2 Department of Nursing, Faculty of Nursing, Physiotherapy and Podology, University Complutense of Madrid, 28040 Madrid, Spain; se.mcu@nagorrao
Fernando Jesús Plaza del Pino
Juana inés gallego-gómez, associated data.
The data presented in this study are available on request from the corresponding author.
The social stigma toward individuals with mental health problems is habitual among nursing students, which can lead to poor quality of health care services for patients with mental illnesses. The purpose of the present study was to learn about nursing students’ perceptions of providing care to patients with severe mental disorders before and after participating in a simulated student clinical case. A descriptive qualitative study was conducted through 39 interviews. The difficulties expected by the students and their perceptions about patients were explored before the simulation training. Their perceptions about the use of clinical simulation for learning about the adequate management of these patients were analyzed afterwards. Results: Before the simulation training, the students assessed the case as being complicated, expressed their lack of specific training, and felt fear and insecurity, thus reproducing the stigma towards mental health patients. After this training, they positively valued the usefulness of the clinical simulation for gaining confidence and overcoming the stigma. Discussion: The use of high-fidelity simulation offers nursing students the opportunity to approach patients with mental health conditions, overcoming their fears and normalizing mental disorders. Simulation training allows nursing students to analyze the reasoning of clinical judgment and to detect the influence of previous prejudices about mental illness in their clinical decision. This study was not registered.
1. Introduction
Mental disorders are presently one of the major problems in public health [ 1 ]. In the last decade, an increase of 13% has been observed in mental disorders and substance abuse. These disorders result in living with a disability for 1 to 5 years, with depression being one of the main causes of this disability. Also, the fourth cause of death in individuals aged between 15 and 29 years old is suicide [ 2 ]. Despite the advancements in some countries, patients with mental health problems suffer severe violations of human rights, discrimination, and stigma [ 2 ].
According to theorists such as Goffman [ 3 ], the concept of stigma has a double connotation. On the one hand, it is an attribute that turns the other into a different individual which relates them to a series of undesirable characteristics or negative stereotypes of the person. On the other hand, it is considered a socially constructed product of rejection or disapproval by the social environment with its corresponding negative responses or unwanted effects in terms of behavior that person [ 3 ].
Mental health-related stigma is often grounded in stereotypes that persons with mental health issues are dangerous (unpredictable, violent), responsible for their mental health issue, cannot be controlled nor recover, and should be ashamed [ 4 ]. The phenomenon of stigma towards mental health patients is not restricted to specific communities or countries [ 5 ], and it is common among primary care professionals [ 6 ]. Consequently, this phenomenon can therefore negatively affect the care provided to the mentally ill user [ 7 ].
1.1. Background
Many nursing students hold negative assumptions about mental health practice, with fearful stigma and stereotypes [ 8 ]. They can often lack confidence in communicating with people with mental disorders and may be afraid to do or say something harmful [ 9 ]. However, discriminatory and negative attitudes can be addressed in specific anti-stigma interventions and ideally incorporated into mental health nursing education among undergraduate nursing students from the beginning of professional training [ 10 ]. In this sense, a systematic review concludes that mental health-specific training seems to improve nursing students’ perceptions toward mental health, highlighting that clinical placement underpins theory, leading to a decrease in negative attitudes and stigma regarding mental health [ 11 ]. Specifically, a recent review and meta-analysis support the effectiveness of simulation training in mental health nursing education [ 12 ].
Modern stereotypes still present the mentally ill as at fault, unpredictable, and violent [ 13 ], and observational studies have indicated that health professionals, including nurses, are often part of the stigma [ 6 , 13 ]. However, many people who suffer from mental health problems will receive care and attention from nurses at different stages of care throughout their lives. For this reason, there is a strong need to re-enforce education programs [ 14 ]. These programs will allow nursing students to tend to the needs of these patients and to offer a comprehensive approach to the care of mentally ill patients [ 15 ].
Nursing departments at many Spanish universities now include a specific course about psychiatry and mental health. However, some nurses believe that greater exposure to problems associated with mental health is needed, not only in communities but also in health sciences faculties [ 5 , 16 ]. However, a general psychiatry course during the nursing degree may not, by itself, change the biased point of view about mental health [ 7 ]. Therefore, they propose re-enforcement through exposure and interaction with patients with mental disorders [ 7 , 17 ].
In this sense, nursing students enrolled in the mental health course and practical sessions have a diversity of pre-conceived ideas. Professors play a central role in the identification and development of psychoeducational strategies to address the concerns of the students and to increase their interest in the mental health speciality [ 18 ]. Clinical simulation is an excellent medium for learning and evaluating skills, both technical as well as non-technical, and in the field of nursing, the use of this approach has been increasing to help students acquire basic competences [ 19 ]. Specifically, our university added training activities to its study plan, in which clinical simulation scenarios play a relevant role in the teaching and evaluation of competencies, thus ensuring the acquisition and practical application of the professional qualities required in nursing [ 20 ].
Consequently, it is necessary to train nursing students on mental health through clinical simulation sessions. The objective for their use is for the students to acquire specific skills and competences which will allow them to improve their view of mental health patients, minimizing their suspicions and fears and thus allowing them to improve the nursing attention and care of individuals with mental disorders.
1.2. Rationale and Aim
Although specific anti-stigma interventions are recommended in undergraduate nursing students [ 10 ] and simulation training is effective in mental health nursing education [ 12 ], most previous studies have mainly adopted a quantitative approach, and the few qualitative studies available have mainly the nursing students’ perceptions only after simulation training, without their pre-conceived ideas about mental illness. Moreover, few studies have included standardized patients who played the role of severely mentally ill patients.
Therefore, the main aim of our study is to learn about nursing students’ perceptions of providing care to patients with severe mental disorders before and after participating in high-fidelity simulation training using standardized patients.
2. Materials and Methods
2.1. study design.
We conducted a descriptive qualitative study in order to explore the experiences and perceptions of our participants [ 21 ], considering their circumstances and their own points of view [ 22 ]. Moreover, in our case, we aimed to explore the perceptions of nursing students before and after participating in a simulated case of a patient with a mental disorder. The recommendations of the COREQ guide for qualitative research reporting [ 23 ] were followed.
2.2. Sample and Environment
This study involved students in the last year of their nursing degree at a public university in southern Spain. According to the European Qualification Framework, the 4-year nursing degree in Spain meets level 6. These students had taken the third-year course, nursing in mental health, and took part in clinical simulation scenarios related to mental health within the context of the Practicum IV-V course in their last (4th) year. Voluntary participation was offered to all of the students (56 students). The study was conducted between October and November 2021.
2.3. High-Fidelity Simulation Procedure
A high-fidelity clinical simulation scenario was developed about a patient diagnosed with borderline personality disorder, according to DSM-5-TR [ 24 ], and admitted to a long-term hospital residency unit; the patient’s name has been changed ( Table 1 ). This clinical case represented in the simulated scenario was designed by three registered nurses specialized in mental health with more than ten years of experience in patient care for the mentally ill. The participation of students during the simulation was evaluated according to the nursing activities associated with the appropriate Nursing Interventions Classification (NIC) [ 25 ]. See Table 1 for the resolution of this simulated clinical case.
Simulated scenario, appropriate NIC (Nursing Interventions Classification) interventions, and related nursing activities for its resolution.
| Simulated Scenario | NIC Intervention | Nursing Activities |
|---|---|---|
| Juan. A 32-year-old man diagnosed with borderline personality disorder was admitted to the therapeutic community of mental health (a long-term hospital residency unit) 3 days ago. He does not want to get up and does not want to shower or eat because he does not want to be admitted. He feels sad, nervous, and angry because of the situation, and he is especially angry with his parents, whom he blames for the admittance. | (5270) Emotional support | Favor conversation over crying as a way to decrease emotional tension. |
| Remain with the patient and provide safety during periods of higher anxiety. | ||
| Comment on the emotional experience with the patient. | ||
| Provide help in the making of decisions. | ||
| Encourage the patient to express his feelings of anxiety, anger, or sadness. | ||
| (4640) Anger control assistance | Support the patient in the practice of anger control strategies and their adequate manifestation. | |
| Instruct the patient about measures that provide calmness (resting and deep breathing). | ||
| Identify the consequences of the inadequate expression of anger. | ||
| Use an approach that is serene and safe. | ||
| Comment on the changes in lifestyle that could be necessary to avoid future complications and/or control the disease process. |
Both the NIC interventions and the nursing activities served as a guide to discuss the performance of the students during the debriefing phase. Even though the students were familiarized with the NIC interventions and the nursing activities related to subjects covered in their previous courses about the theme, they were not previously informed that their performance would be evaluated based on them.
The main learning objective of the simulation scenario was for students to learn how to provide good nursing care to a patient with a mental disorder by utilizing nursing competences associated with emotional support and relaxation through the teaching methodology of clinical simulation. To achieve this objective, a total of 21 clinical simulation sessions were conducted. The students were divided into work teams composed of 2–3 nursing students for each simulated clinical case. Thus, all the students were able to participate in the simulated scenario designed. All the clinical simulation sessions followed the Best Practices Standards proposed by the International Nursing Association of Clinical and Simulation Learning (INACSL) during its four phases [ 26 ]: pre-briefing, briefing, development of the simulated scenario, and debriefing. Two university professors, with more than ten years of experience in clinical simulation methodology, carried out and supervised the four phases of this methodology recommended by the INACSL. It must be pointed out that in the pre-briefing phase, a psychologically safe context was promoted, following the recommendations by Rudolph et al. [ 27 ]. Also, in the debriefing phase [ 28 ], the tool used was the GAS (gather, analyze, and summarize) technique proposed by Phrampus and O′Donnell [ 29 ].
Below is a description of the phases developed during the high-fidelity clinical simulation sessions:
- Pre-briefing: Two weeks before the simulated scenario sessions, the students were provided with information to establish a psychologically safe environment and to consolidate the learning process [ 27 ]. Thus, a document with a brief description of the simulated scenario was provided to each student so that they could search and plan its resolution through an evidence-based approach. This information included details such as medical history and state of health (young man who was recently admitted due to a mental disorder and who was angry for his admission).
- Briefing: the clinical scenario was put into context through a brief presentation of the clinical case background.
- Simulation scenario: The clinical scenario was as real as possible. This scenario aimed to provide emotional support and to use relaxation techniques with a young patient who had just been admitted due to a mental disorder. For this, 5 main nursing activities were related to the corresponding Nurse Interventions Classifications (NIC). These NICs were only used as a guide, as the evaluation of the students’ performance was broader. During the clinical simulation session, video cameras and microphones installed in the simulation room were utilized.
- Debriefing: After the end of the simulation scenario, it was analyzed and discussed [ 28 ], with this phase structured with the debriefing tool GAS (gather, analyze, and summarize). Following this, the nursing students discussed and analyzed the practices based on the best available evidence related to the clinical case, promoting anin-depth reflection and analysis of the nursing activities that were well conducted, the mistakes, and those that needed to be improved during the clinical simulation session. The nursing professors trained in the clinical simulation methodology provided feedback to the students about their clinical performance.
2.4. Data Collection
Semi-structured interviews with open-ended questions were given to each participant in two phases: the first phase before taking part in the high-fidelity clinical simulation (pre-CS) and the second phase after the last simulation session (post-CS). The interview guide was designed and validated by the study researchers in agreement with the theoretical categories related to the theoretical foundations of the debriefing phase in the clinical simulation methodology [ 29 ].
The pre-CS phase was centered on delving into the expected difficulties with the case according to the students and the perceptions of the students concerning the patients with mental health disorders. The post-CS interview phase was oriented toward the use of high-fidelity clinical simulation for learning how to manage patients with mental disorders. Below, Table 2 shows the interview guide.
Interview guide.
| Pre-clinical simulation phase | Explain what difficulties you expect to find when you address the case. |
| According to you, what features or characteristics define patients with mental disorders? | |
| What perceptions and feelings or emotions do you feel when you have to care for a patient with a mental disorder? | |
| Post-clinical simulation | What knowledge and/or skills do you think you have acquired after this experience? |
| What usefulness do you see in the use of clinical simulation in mental health nursing? |
All of the interviews were conducted in a room that was set up for this at the university, seven days before the start of the first simulation session (pre-CS phase) and seven days after the last session (post-CS phase). The interviews lasted an average of 25 min per phase. The interviewer was a member of the research team who did not participate in the simulation sessions, thus avoiding possible biases. All of the interviews were recorded with the verbal consent of the participants.
2.5. Data Analysis
The interview recordings were transcribed and reviewed by two researchers to ensure that the transcription was correct. The data were stored, managed, classified, and organized with help from the qualitative data analysis software ATLAS-ti 8.0 (Scientific Software Development GmbH, Berlin, Germany). We followed the steps for adequate descriptive qualitative analysis [ 30 ]: (1) transcribing and sorting the data, (2) giving codes to the initial data obtained from interviews, (3) adding comments/reflections (memos), etc., (4) trying to identify similar phrases, patterns, themes, relationships, and sequences, (5) taking these patterns and themes to help focus the next wave of data collection, and (6) gradually elaborating a small set of generalizations that cover the consistencies you discern in the data. Thus, an explicit description of the perceptions of the students about the experience was obtained. The categories identified were initially aligned with the subjects of study proposed in the two phases of the interview. Two researchers, who are experts in qualitative research, developed the entire process of obtaining categories and subcategories independently, ending the process with the sharing of both and a consensus on the final decisions of the analysis.
2.6. Ethical Considerations
The research protocol was approved by the Research Ethics Committee from the Department of Nursing, Physiotherapy, and Medicine at the University of Almería (EFM 75/2020). To guarantee anonymity and confidentiality, a code was assigned to each participant. In all of the cases, an informed consent form was read aloud and explained to the students, which detailed the aim of the study and the acceptance of the student to participate in the study, with the students who wanted to participate signing the form.
2.7. Qualitative Rigor
The quality of our study was evaluated according to the criteria of Lincoln and Guba [ 31 ]. They assessed the credibility, transferability, and confirmability of the research. Data were triangulated between the researchers involved in the analysis, and independent researchers reviewed the analysis process to ensure credibility. Transferability was guaranteed by describing the research setting, as well as the participants, context, and method. Confirmability was achieved through the presence of variability in participants’ experiences; reading and analysis were conducted by each researcher independently, contrasting and then agreeing on emerging themes and subthemes.
A total of fifty-six students in the last year of their nursing degree attended the high-fidelity clinical simulation sessions, of which thirty-nine accepted to participate in the study (response rate of 67.5%). Those who did not participate were due to disinterest, lack of time, or other reasons. Most of the participants were women (76%), with a mean age of 23 years old (mean = 23.30; SD = 6.932).
As a preliminary exercise, at the start of the pre-CS interview, the participants were asked to order various simulation scenarios centered on patients from different medical specialities, including the scenario to be analyzed, according to their participation preference; more than half of the informants placed the mental health patient case in the last place. The reasoning behind this decision appears in the presentation below of the different categories and subcategories. Regardless of where they placed the mental health patient case in terms of their preference, all thirty-nine participants completed the two interviews.
Table 3 presents a summary of the subcategories identified, according to the different questions asked to the students.
List of categories and subcategories identified.
| Interview | Category | Sub-Category |
|---|---|---|
| Pre-clinical simulation | What difficulties I will find. | Complex case Not knowing |
| Perceptions of patients with a mental disorder. | The prejudices; the stigma Like another patient | |
| Emotions felt with regard to a patient with a mental disorder. | Fear Insecurity | |
| What is lacking in my training. | Communication skills Clinical experience Unspecified training | |
| Post-clinical simulation | Knowledge acquired. | Negotiation and relaxation techniques Management of mental health patient |
| How does CS help in the care of patients with mental disorders? | Breaking the stigma Provides confidence |
The six main categories that appeared from the open-ended question and their corresponding categories, supported by the narratives of the participants, are described below, differentiating the pre-CS and post-CS categories. It should be noted that all the interviews were performed in Spanish and the quotes were translated into English by a bilingual native speaker, thus avoiding the loss of important semantic details.

3.1. Pre-CS Categories
During the pre-CS interview phase (before entering the simulated scenario), the students pointed out the difficulties that they thought they may encounter; they believed the case to be complicated and did not think they had sufficient training. We can find the social stigma suffered by these patients with mental health conditions in the perceptions of the majority of the students, although, for other students, they were considered as just another patient. In general, before taking part in the simulation, they started feeling fear and insecurity.
3.1.1. What Difficulties I Will Find
Together with the previous exercise in which they arranged the possible scenarios according to their participation preference, among which we find a pediatric scenario, another with a patient under hemodialysis, and one involving surgery, they were asked to justify their answer and to express the difficulties they believed they would find in this specific scenario. Most of the students placed the case addressed in the present study in last place, as they perceived that this scenario included diverse difficulties, which will be described below.
- Complex case:
Many informants mentioned the complexity they perceived in the case due to the protagonist being a mental health patient. It was noted that their comments were strongly determined by their own beliefs and/or prejudice against these patients.
Treating a patient with a mental illness is difficult in many aspects, some of them are more susceptible to the usual and could think that it hurts them instead of helping them . (S9)
It is difficult to make patients with personality disorders collaborate, it is quite a challenge . (S18)
Communication with this type of patient can be complicated . (S31)
In my opinion, it is complicated, as you are never 100% sure about how the patient will react . (S3)
- Not knowing:
Students frequently expressed their lack of competences/skills for addressing a mental health patient, despite having taken a specific course during their nursing studies. They fundamentally referred to non-technical or socio-emotional skills such as communication skills and emotional management.
Not knowing how to address the situation when Juan loses it (S1)
Knowing how to interact with him and be part of the negotiation . (S16)
Knowing how to address a patient with a mental illness is foreign to me, and I think that a lot of professional experience is needed for addressing this type of patient . (S18)
Not knowing how to address or calm the patient due to a lack of knowledge or expression techniques for talking with patients with mental illnesses . (S30)
3.1.2. Perception of the Patients with a Mental Disorder
Among the nursing students’ perceptions about mentally ill patients, we found that some students had pre-conceived ideas (such as prejudices and social stigma), while others perceived these patients as any other, without pre-conceived or prejudiced assessments.
- The prejudices; the stigma:
Within the comments from our informants, we observed some pre-conceived ideas, and in some cases, the social stigma suffered by people with mental health problems is very present. This is an important finding, as the beliefs or perceptions determine the possible future behavior toward these patients.
Emotionally-unstable individuals, if I could define them with a single word, it would be ‘unpredictable’ . (S22)
Non-collaborative, non-communicative . (S11)
Emotional liability, extreme behavioural changes… (S8)
Abnormal beliefs, difficulty in thinking clearly, sadness, anxiety, mood changes … (S17)
On the other hand, despite stating that they were not wellversed in these individuals, many of the participants talked about a theory or analysis of these patients (pre-conceived ideas).
They are unique, they are scared about their true nature or they fear things that other people, depending on their past, would not fear, they have difficulties we are not able to see and/or be empathetic with … (S5)
They have very defined routines in their head and it is very difficult to change them . (S12)
People who have suffered and need a lot of support. They are warm and grateful . (S32)
They do not recognize their illness, they live in a reality that does not exist and believe that everyone else is trying to harm them and do not care about them . (S18)
Also, many students believed that these patients are found outside of the established norms, cataloguing them as strange individuals.
Those who are outside of what is considered in society to be normal . (S8)
They are people who live in the fringes of society, they are different from the rest . (S9)
The typically strange and extravagant person who lives in his or her own world . (S29)
- Like another patient:
However, we also found a minority of students who perceived these individuals as any other patient, without pre-conceived notions or prejudiced assessments; they are Please confirm if the bold is unnecessary and can be removed. The following highlights are the same. Simply another patient to provide care for.
It depends on the disorder, you cannot define a person with a characteristic if you do not know his or her history . (S2)
As any other normal person who has an illness, and needs someone to listen to them, to feel comfortable . (S19)
For me, there is nothing that defines them, they are just like the other people with an illness, another patient . (S25)
People with a pathology, just as others have hyperthyroidism. I believe that we should not have prejudices because they are like any other person with or without a pathology . (S30)
3.1.3. Emotions Felt with Regard to a Patient with a Mental Disorder
Among our informants, we found a predominance of negative emotions regarding contact with a person with a mental disorder, such as fear or insecurity, which could make approaching the patient more difficult, as well as determining the therapeutic relationship that could be established.
The students expressed that they felt fear when they were told they would have to interact with a patient with a mental disorder, and this emotion was associated with the lack of knowledge about these individuals, as well as their lack of experience.
As we are dealing with a mental health patient, we always feel more fear and insecurities . (S5)
I have never provided care for them but maybe fear that they will not like what you say and challenge me . (S18)
Fear of not knowing how to communicate so that he understands everything you explain and does not misinterpret anything . (S22)
- Insecurity:
Strongly associated with the previous feeling, the students felt insecure about the relationship with these patients, in many cases due to the perception of lack of skills and specific training in mental health.
The uncertainty of dealing with a person with non-controlled mental problems . (S25)
Uncertainty about how he will react when you have to perform a technique with him, I see them as unpredictable individuals, and I feel unsure, in case I don’t know how to deal with them . (S10)
Distress for wanting to help but lacking the necessary tools for it . (S28)
I don’t think they are aggressive, but they seem to be unpredictable, and I’m unsure in case I don’t know how to deal with them . (S36)
3.1.4. What Is Lacking in My Training
Among the deficits in their training, the students highlighted both the communication skills as well as the lack of clinical experience and in other cases, did not clearly identify their training needs.
- Communication skills:
The students highlighted the need to be able to maintain adequate communication with their patients and considered the lack of this ability.
I need to know how to communicate, I don’t think I’ll be able to connect . (S28)
Communication is the main problem that he doesn’t understand what I say, and despite understanding it, he does not agree . (S39)
- Clinical experiences:
Despite being enrolled in the final stage of their nursing degree education, the students recognized their lack of clinical experience in mental health as one of their main handicaps.
The main difficulty is borderline personality disorder, as you have to know how to deal with it at all times, and I’ve never done that . (S18)
I lack the necessary experience to know how to address it correctly . (S32)
- Unspecified training:
In some cases, our informants were aware of their lack of training in this field, although they were not able to define their deficiencies.
He is patient with mental health condition, with them, you have to have certain skills to be able to manage them . (S4)
With patients with a physical illness, it’s easier, you learn a technique, and that’s it, but with mental illnesses, you need other, more complicated things, but I don’t know how to explain them . (S27)
3.2. Post-CS Categories
Once the simulated scenario had ended, the nursing students focused on identifying the main knowledge and skills provided by this simulation experience and aspects of the high-fidelity clinical simulation that could be useful for improving the care provided to patients with mental illnesses.
3.2.1. Knowledge Acquired
When the students discussed what they had learned, they all agreed on two aspects: the management of these patients and relaxation and negotiation techniques.
- Management of mental health patients:
Experiencing a simulated situation with a mental health patient allowed the students to gain confidence in their interaction with these patients.
Be calm with a severe patient. Know how to create a relationship of trust . (S8)
I acquired more experience in these types of cases; how to talk to the patient and the presence of the nurses . (S21)
Thanks to this scenario, we were able to discover the most effective way to deal with a mental health patient, and how to create a therapeutic relationship . (S26)
- Negotiation and relaxation techniques:
To successfully resolve the simulation scenario, the students had to delve into the knowledge and application of negotiation and relaxation techniques, which they valued positively.
Knowing how to negotiate and knowing tools to manage emotions . (S4)
Help the patient control his anger and impulses . (S13)
3.2.2. How Does CS Help in the Care of Patients with Mental Disorders?
For students, the main potential benefit of high-fidelity clinical simulation in mental health is its ability to break down prejudices against these individuals; they also pointed out the confidence it provides them for their future clinical practice when facing scenarios that are very real life-like.
- Breaking down the stigma:
The social stigma of patients with mental disorders is one of the main barriers to their relationship with health professionals. Our students recognized that this simulation experience made them change their point of view about these individuals.
In the beginning, I thought I would be more afraid, but in the end, you get to know them, and they would be unable to hurt a fly . (S19)
Now I have good feelings, it feels as if I had dealt with them in the past . (S23)
It normalizes mental health . (S27)
It helps to end the stigma we find with mental health patients, as on many occasions, they see these patients as ‘impossible cases’ . (S32)
- Provides confidence:
The students mentioned feeling more confident going into the simulated scenario when evaluating this experience as very useful for its application in clinical practice.
As it was so real, the simulation helped us to prepare for situations that we will very likely find someday . (S22)
It is very necessary knowledge for students, as it strengthens us and gives us the confidence needed for the development of emotional skills, which are fundamental in this field. In this scenario, we learn about what we do well, and what we could improve, and it is a very enriching experience . (S15)
4. Discussion
The need for the present study arose from the observation that during their education, a systematic tendency of nursing students was found to select clinical cases of patients with physical problems during the Practicum IV and V courses, associated with hospitalization, excluding the cases of patients with mental disorders. This led us to question if the opinions of the students could be marked by a certain social stigma toward these individuals or their lack of knowledge about their care. With this in mind, we designed a qualitative study to discover the attitudes, limitations, and conflicts of the students toward mental health patients and work on specific skills and competences through the use of clinical simulation sessions, which would allow them to improve their view of mental health by promoting changes in their attitudes and in the intention of working with mental health patients (treat, specialize, or work in the field) and by optimizing the attention and care given by nurses.
In general, the results obtained in the pre-CS interview confirm that many nursing students hold negative assumptions about mentally ill patients, with pre-conceived ideas, prejudices, and social stigmas [ 8 ]. In addition, these results also are coherent with other studies that have found nursing students can often lack confidence in communicating with these patients [ 9 ]. However, our participants changed and improved their perceptions toward mental health in the post-CS interview after the high-fidelity simulation training. This result is coherent with recent systematic reviews and meta-analyses which found that mental health-specific training may improve these perceptions [ 11 ], highlighting the usefulness of simulation training in mental health nursing education [ 12 ].
Specifically, below, we carry out a more detailed comparative analysis of the previous scientific evidence in this field. For this purpose, the discussion is structured according to the main categories that emerged from the participants’ discourses.
In the pre-CS interview, we observed that the nursing students’ opinions were marked by the social stigma of these individuals, qualifying the clinical cases with mental disorder patients as ‘complex, unstable, unpredictable, and little communicative’ and expressing training deficits in communication skills and a lack of clinical experience. Previous studies have also found attitudes of rejection and stigmatization among nursing professionals [ 6 ] and a fear of contact with the patient from students during their clinical practices [ 32 ], thus observing the need to promote inclusive education and to develop specific curricular interventions against the stigma [ 33 ]. In this sense, Carrara et al. [ 34 ] consider that anti-stigma interventions that involve social contact between primary health providers and patients with mental illnesses seem to be more efficient for reducing this stigma. However, our results and previous studies support education strategies without direct social contact, such as discussion groups or clinical simulation [ 35 , 36 ].
Moreover, our nursing students stated that they did not have sufficient knowledge to deal with the care of the patient with a mental illness. In this way, they created the dichotomy of mental versus physical health, since they understood that the physical is objectifiable and may be solved by knowing what to do, while for managing a mentally ill patient, some unspecified skills are needed, for which the biomedical model seems to be insufficient [ 37 ]. Even a strong academic curriculum is not enough to change stigmatized perceptions about mental illness, psychiatric care, and mental health nursing as a profession. In this sense, Martin et al. [ 7 ] consider that a general psychiatry course during nursing school is, by itself, unlikely to change biased views and should be enhanced by exposure to and interaction with people with lived experiences of mental illness.
After the high-fidelity simulation training, we found that the nursing students’ perceptions about mentally ill patients changed and improved in the post-CS interview. In this sense, previous studies have highlighted the usefulness of clinical simulation for the development of psychosocial evaluation skills, allowing the students to develop the necessary principles to offer safe and effective care to patients [ 35 ]. Specifically, the report after the simulation session is the cornerstone of the learning experience in a clinical simulation environment [ 27 ]. It allows both professors and students to re-examine the simulated case experience, share their mental model, and promote the rationale behind the clinical judgement [ 38 ].
In our study, once the simulation experience was completed, students focused on identifying the main knowledge skills provided by this simulation experience and aspects of the high-fidelity clinical simulation that could be useful for improving the care provided to patients with mental illnesses. In addition, our nursing students indicated that the simulation provided them with a realistic environment in which they were able to develop skills and manage clinical situations more independently, minimizing their feelings of insecurity and initial stigmatizing ideas, and to improve their learning deficiencies associated with communication skills. All of these findings confirm the results obtained in previous studies related to the use of clinical simulation methodology in mental health nursing education [ 8 , 9 , 12 ].
Finally, and from the point of view of educators, we believe that simulation-based education, when it is utilized in adequate conditions following the international best practices standards [ 26 ], correlates with significant effects on the knowledge, skills, and behaviors toward the patient with a mental illness [ 38 ]. In our case, the learning was based on the management of asevere mental health patient, using negotiation and relaxation techniques. In this sense, our nursing students highlighted the potential of high-fidelity simulation training in mental health education to break down their initial pre-conceived ideas (such as prejudices and social stigma) and provide them with confidence for facing their future clinical practice in real scenarios, aside from allowing them to delve into and acquire new knowledge [ 39 ].
Limitations
Although the study reflects the perceptions of nursing students after staging a high-fidelity simulation case based on a mental health patient, it would be important to delve into these perceptions through a qualitative study at a greater scale, through the design of new simulated clinical cases with patients with other mental disorders, and through a larger sample of nursing students, as well as other studies with quantitative methodology to evaluate the effectiveness of this education intervention. Likewise, future studies based on the clinical simulation methodology should be conducted with nursing professionals. Thus, the clinical simulation teaching methodology should not only be expanded to education centers but also health centers, placing value on the acquisition of nursing competences needed for the adequate care of patients with mental disorders by nursing professionals and not only of students.
5. Conclusions
Considering the findings from our study, at first, the participants were insecure and reticent about working with mental health patients, classifying them as ‘complex and unpredictable patients’. However, after taking part in clinical simulation sessions, the students reported high levels of satisfaction with the simulation experience, stating that the simulation approach to these patients normalized mental health and helped them to be more prepared for clinical rotations.
In conclusion, experiences of active learning are necessary and efficient for the development of skills, provide participants with the confidence necessary for caring for patients with a mental disorder, and help break down the stigma of nursing professionals toward mental health patients.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, F.J.P.d.P. and A.J.S.-M.; methodology, D.J.-R., F.J.P.d.P. and O.A.; formal analysis, F.J.P.d.P., D.J.-R. and O.A.; investigation, F.J.P.d.P. and J.I.G.-G.; data curation, F.J.P.d.P. and J.I.G.-G.; writing—original draft preparation, F.J.P.d.P., D.J.-R., O.A., A.J.S.-M. and J.I.G.-G.; writing—review and editing, F.J.P.d.P., D.J.-R., O.A., A.J.S.-M. and J.I.G.-G.; supervision, F.J.P.d.P., D.J.-R. and O.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Research and Ethics Board of the Department of Nursing, Physiotherapy, and Medicine of the A. University (Approval no. EFM-75/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Public involvement statement.
No public involvement in any aspect of this research.
Guidelines and Standards Statement
QOREQ: (Consolidated criteria for Reporting Qualitative research) checklist. The use of high-fidelity simulation lets nursing students become closer to mental health patients, overcoming their fears, and normalizing mental disorders. This training gave students the necessary confidence when caring for individuals with mental disorders, breaking away from the stigma toward these patients. Therefore, it is considered that the realization of clinical simulation sessions in mental health nursing education has a positive effect on their future healthcare practice, since it allows students to share their mental model, analyze the reasoning behind clinical judgment, and detect the possible influence of previous prejudices about mental illness in their clinical decision.
Conflicts of Interest
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
The mental and behavioral health crisis in youth: Strategic solutions post COVID-19 pandemic: An American Academy of Nuring consensus paper
Affiliations.
- 1 Psychiatric, Mental Health, and Substance Use Expert Panel. Electronic address: [email protected].
- 2 Psychiatric, Mental Health, and Substance Use Expert Panel; Health Equity Expert Panel.
- 3 Child, Adolescent, and Family Expert Panel.
- 4 Psychiatric, Mental Health, and Substance Use Expert Panel.
- 5 Trauma and Violence Expert Panel.
- PMID: 38901064
- DOI: 10.1016/j.outlook.2024.102177
The COVID-19 pandemic wrought significant negative impacts on youth well-being, particularly among Black, Hispanic, American Indian, Alaska Native, and LGBTQ+ (Lesbian, gay, bisexual, transgender, queer or questioning) youth. The pandemic disrupted connections to family, school, and community, which are essential supports for youth mental health. Lessons learned from the pandemic suggest the role of stress and windows of opportunity to build resiliency. Drawing from a policy dialog on the youth mental health crisis conducted by 4 American Academy of Nursing Expert Panels, we present approaches to the current increase in youth mental health problems. Included is emerging literature on building youth resilience, particularly via re-establishing school and community connections. The role of families, schools, and community support is emphasized, particularly by creating a healing school environment and the pivotal role of school nurses. Recommendations include increased support for families, engaging the school nurse role, and developing school-based innovative programs to build connections and youth wellness.
Keywords: Adolescent; Behavioral health; Child; Mental health; Resiliency; School nursing.
Copyright © 2024 Elsevier Inc. All rights reserved.
PubMed Disclaimer
Conflict of interest statement
Declaration of Competing Interest The authors declare no conflicts of interest.
Similar articles
- Latinx LGBTQ Youth, COVID-19, and Psychological Well-Being: A Systematic Review. Abreu RL, Barrita AM, Martin JA, Sostre J, Gonzalez KA. Abreu RL, et al. J Clin Child Adolesc Psychol. 2024 Jan-Feb;53(1):98-113. doi: 10.1080/15374416.2022.2158839. Epub 2023 Jan 23. J Clin Child Adolesc Psychol. 2024. PMID: 36689641
- The Role of School and Community Involvement in the Psychosocial Health Outcomes of Black and Latinx LGBTQ Youth. Heath RD, Keene L. Heath RD, et al. J Adolesc Health. 2023 May;72(5):650-657. doi: 10.1016/j.jadohealth.2022.11.010. Epub 2023 Jan 3. J Adolesc Health. 2023. PMID: 36599760
- Teen, Queer, and Asian: Lesbian, Gay, Bisexual, Transgender, Queer, Plus Asian American Students' Experiences in Schools. Gorse MM, Bacolores JP, Cheung J, De Pedro KT. Gorse MM, et al. J Sch Health. 2021 Nov;91(11):906-914. doi: 10.1111/josh.13077. Epub 2021 Sep 5. J Sch Health. 2021. PMID: 34486117
- A National Analysis of State Policies on Lesbian, Gay, Bisexual, Transgender, and Questioning/Queer Inclusive Sex Education. Garg N, Volerman A. Garg N, et al. J Sch Health. 2021 Feb;91(2):164-175. doi: 10.1111/josh.12987. Epub 2020 Dec 13. J Sch Health. 2021. PMID: 33314223 Review.
- Strengthening Our Schools to Promote Resilience and Health Among LGBTQ Youth: Emerging Evidence and Research Priorities from The State of LGBTQ Youth Health and Wellbeing Symposium. Johns MM, Poteat VP, Horn SS, Kosciw J. Johns MM, et al. LGBT Health. 2019 May/Jun;6(4):146-155. doi: 10.1089/lgbt.2018.0109. Epub 2019 Apr 8. LGBT Health. 2019. PMID: 30958731 Free PMC article. Review.
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Counseling and Mental Health Center
Providing mental health support through assessment and referral, group and individual counseling, psychiatry, and well-being services to the students of UT Austin.
Student Services Building, 5th floor 100 West Dean Keeton Street
8 a.m. - 5 p.m.
Monday - Friday
Main Line: 512-471-3515
24/7 Crisis Line: 512-471-2255
We're Here For You
We are located in the Services Building on the 5th floor at 100 West Dean Keeton Street.
8 a.m.-5 p.m. Monday-Friday
512-471-3515
24/7 Crisis Line
If you need immediate help call 512-471-2255 (CALL) to speak with a crisis counselor anytime.
24/7 Online Support
TimelyCare is a virtual mental health and well-being platform for currently enrolled UT Austin students. It provides 24/7, on-demand non-crisis emotional support as well as health coaching and counseling.
Clinical Services
Our comprehensive services cater to a variety of needs, ensuring students feel supported and empowered.
Well-Being Resources
Empowering holistic well-being through accessible resources and innovative tools.
Supporting Others
Mental health resources for faculty, staff and parents.
How May We Help you?
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Sed ante tellus, dictum vitae leo et, lobortis fringilla lorem. Nam sodales magna sed magna hendrerit semper.
Frequently Asked Questions
- When is the CMHC open?
- I’m a new client. How do I make an appointment for clinical and or psychiatric services?
- How much will this cost?
- Do I only receive a certain amount of clinical and or psychiatric sessions?
- Will CMHC refer me to an external clinician?
- Can my parents access my CMHC records?
- How do I complete my paperwork for my appointment?
- How long does it take to get an appointment?
- When is UHS open?
CMHC is open from 8 a.m. to 5 p.m. from Monday-Friday.
Additionally, the CMHC offers various 24/7 services. This includes the 24/7 Crisis Line (512-471-2255), which offers immediate crisis counseling and TimelyCare, a virtual mental health and well-being platform offering round-the-clock support through TalkNow.
Making an Appointment
New clients must first complete the Brief Assessment and Referral Process, which involves a 15-minute phone call to ensure you are matched with the most suitable service for your needs. Returning clients will work with their clinician to book future appointments after their initial session. Appointments are scheduled through the MyUHS/CMHC portal.
Cost of Services
CMHC services are free. Psychiatry services are $10/visit.
The CMHC does not bill insurance.
Number of Clinical or Psychiatric Sessions
The number of sessions provided varies for each client. Clients receive the number of sessions that are most appropriate for their current mental health needs and resources, including transportation, health insurance, and other factors. For more information on receiving clinical or psychiatric services, call 512-471-3515, Monday-Friday from 8 a.m. to 5 p.m.
External Clinicians
You may be referred to an external clinician after completing the Brief Assessment and Referral process. Our case management team will assist you with referrals to external providers.
Parents Accessing CMHC Records
Anyone who has access to your UT EID and password will have access to your mental health records. See the mental health records page for information on important privacy considerations.
Completing Paperwork
See the information regarding appointment preparation .
Appointment Wait Time
Same-day crisis appointments are available. For non-crisis appointments, the wait time depends on your needs and the current workload of the clinical team. On average, scheduled appointments take place within 1-2 weeks of booking.
UHS is open from 8 a.m. to 5 p.m. Monday-Friday.
Many of our clinics have specific operating hours. For more information on all of our clinic hours, visit the services page.
CMHC services are free. Psychiatry services are $10/visit. The CMHC does not bill insurance.
CMHC offers a wide variety of groups which address a range of concerns. Visit the groups pages for more information.
Groups offered this summer:
Black Voices: Drop-in Mental Health Support Group for Black Students
Coping through art: mental health support through creative exploration, latine voices: drop-in mental health support for latine students, yoga for mental wellness: mental health support through mindful movement, vav drop-in support hour: mental health support for survivors of interpersonal trauma, vav trauma informed yoga: mental health support through mindful movement, dissertation support group: addressing stuckness, balance and mental health, summer associates support circle: drop-in mental health support for navigating legal beginnings, roots of resilience: existential therapy for mental health, understanding self and others counseling group, groups and workshops.
CMHC offers a wide variety of groups and workshops which address a range of issues.
Updates and Events
No Additional Summer Fee and Summer 2024 Usage and Eligibility
Whether you're taking summer classes or just taking a break before the Fall 2024 semester, you can still use the Counseling and Mental Health Center without any additional summer fee. Your eligibility to use these services depends on your enrollment status and where you currently live.
A free 3rd party virtual mental health and well-being platform for currently enrolled UT Austin students. Through either the mobile app or desktop, receive 24/7 access to virtual care through phone or secure video visits from anywhere in the United States.
Healthcare Products Delivered
Get over-the-counter medications prescriptions, first-aid supplies, period products, contraception and more delivered.
Summer 2024 Counseling Groups
Options include drop-in support groups, yoga groups for mental health support, mindful eating groups, other support and skill-building groups and more.
- Open access
- Published: 28 June 2024
An organizational working time reduction and its impact on three domains of mental well-being of employees: a panel study
- Francisca Mullens 1 &
- Ilse Laurijssen 1 , 2
BMC Public Health volume 24 , Article number: 1727 ( 2024 ) Cite this article
44 Accesses
Metrics details
Work hours are an important aspect of one’s job and these in turn have the potential to impact people’s well-being. Much research investigating the link between working hours and well-being uses cross-sectional data. Longitudinal studies, especially those studying the same subjects changing their working time, can study the impact of work time more clearly. Using panel data, this study aims to explore the impact of a reduction in working time on three domains of well-being: general well-being, job-related well-being (positive work experience) and work-family well-being (work-family conflict). In addition, our study offers insights into the role of concomitant changes in work and private circumstances of employees as we investigate whether the impact of shorter working hours for well-being is mediated by changes in the participants’ and circumstances related to paid and unpaid work resources.
An organization of about 60 (female) employees trialed a shorter workweek for one calendar year in 2019. All full-time employees reduced their hours. The part-time working employees can be used as a control group. Panel data (survey and time-use diary data) of a 30-h workweek trial in Belgium was collected in four waves over two years in a pre- and post-intervention design. Change over time (waves) was analyzed through multilevel growth models.
A decrease in work-family conflict was observed during the shorter workweek. Part of this decrease is explained by concomitant changes in work and private circumstances, such as sufficiency in free time, schedule control, and satisfaction with work pressure. Positive work experience and general well-being tend to have decreased during the shorter workweek, although this could partly be explained by other organizational changes and not by the reduction in working hours per se. Schedule control helped suppress these somewhat negative effects of organizational changes on positive work experience.
Reduced working hours have the largest and most positive impact on work-family conflict. The feeling of having enough leisure time contributes to this increased well-being. Especially for women, who were the majority in this study, a reduction in working time might be beneficial as they often bear more responsibility for household work and care tasks. Next to the duration of working time, schedule control/autonomy has an important impact on well-being.
Peer Review reports
Introduction
Work hours are an important aspect of one’s job and these in turn have the potential to impact people’s well-being. Reductions in working time have often been introduced with the (partial) aim of improving workers’ well-being [ 21 ]. However, most research on working hours and their impact on well-being uses cross-sectional data, comparing people with different amounts of working hours. While some of these studies find lower well-being when working longer hours (e.g., [ 4 , 27 ]), review studies show rather weak or inconsistent support for the negative association between long hours (and overtime) and mental health [ 16 , 48 ]. The inconsistent findings could be due to different conceptualizations of mental health but could also be related to the cross-sectional design of these studies in which other work-related and personal conditions might impact subjective well-being. Longitudinal studies into the well-being of the same people over time might help to overcome the latter issue, and in particular cases studying the consequences of collective work time reductions. Even though trials and large-scale reductions in the last decades are still rather scarce, the evidence available shows a positive impact of work time reduction on workers’ well-being (e.g., [ 18 , 19 , 31 , 46 ]). Adding to that body of knowledge, we report on results from a 30-h workweek work time reduction trial conducted in a Belgian organization in 2019. A strength of our study is the dynamic perspective, as we have measured (the almost exclusively female) employees’ well-being both before and after the introduction of the working time reduction, and can compare changes in well-being between employees whose work time was reduced (more) and others whose work time did not reduce or reduced less. We look into the impact of this case of collective working time reduction on three domains of mental well-being, namely employees’ feelings of general (or context-free) well-being, job-related well-being and work-family well-being, corresponding to the three domains of well-being discerned in Fox’s et al. review study [ 14 ] on the impact of workplace interventions on worker well-being. In addition, our study offers insights into the role of concomitant changes in work and private circumstances of employees as we investigate whether the impact of shorter working hours for well-being is mediated by changes in time use, circumstances related to unpaid work, and (paid) work resources of respondents.
Background: the impact of work time reduction
Working time reduction might yield a ‘triple dividend’, impacting social, economic, and environmental dimensions [ 3 , 18 ]. These dimensions correspond to the three large motivations behind working time reductions historically [ 21 ]. While the environmental and economic dimensions primarily entail collective and societal impacts (although individual/employee productivity can also be part of the economic dimension), the social dividend encompasses mostly individual-level implications such as well-being. This paper investigates how a reduced workweek can contribute to individuals’ well-being.
There has been little research on the impact of working hours on mental health or well-being that uses a longitudinal design. In one example, using longitudinal data, Gash et al. [ 17 ] found that women who reduced their working hours while staying in the same job felt happier over time. The authors speculate that most of these women voluntarily reduced their hours from full-time to part-time and this might help explain the positive results. Their hours are more in line with their preferences and this work hours fit is known to impact well-being (e.g., [ 41 ]). When women switch from full-time to part-time this is often an individual choice based on gendered preferences. These working time preferences ‘are usually compromises between what is desirable and what is feasible’ ([ 8 ], p. 16). The individual’s decision to reduce working hours is influenced by their conditions, (gendered) norms and preferences. However, collective reductions are less dependent on these individual factors. By studying the effects of changing work hours in collective reductions on a national or organizational level, researchers can separate and analyze them more clearly. This also offers a more promising context to study the impact of working less on mental well-being and some examples of this type of research are already available. In Korea for example, Rudolf [ 37 ] studied the impact of a national working time reduction on overall life and job satisfaction. He concluded that the policy did not improve overall satisfaction with one’s life and job [ 37 ]. The author suggests that this could be due to an intensification of work and downward adjustments in leave [ 37 ]. Other country-wide reductions in working time such as those in France in the early 2000s (from 39 to 35 h) and Portugal in 1997 (from 44 to 40 h) did show an improvement in workers’ well-being: using the European Community Household Panel, Lepinteur [ 31 ] found that the reforms increased both the job satisfaction and leisure satisfaction of workers [ 31 ]. Investigating the impact in France, Fagnani and Letablier [ 12 ] find that parents of young children did have positive opinions on the impact of the shorter working hours, however, the reduction of hours was not large enough for all parents to improve work-family balance. The authors conclude that the context of these changes (the size of the organization, the form of reduction, e.g., weekly vs yearly reductions, etc.) should be considered.
Next to research on national work hours reductions, there are a few smaller-scale trials with reductions on an organizational level that have been studied. A review study [ 46 ] on 7 studies based in Northern Europe mainly in health care sectors, looked into the impact of organizational reductions in working hours on health outcomes. The study concludes that working time reduction improves working-life quality. Only three cases also evaluated the effect on the quality of life outside of work but did not find improvements in this area. However, [ 5 ] reported a decrease in work intrusion on private life, while [ 47 ] did not find any significant effects for work-home interference. Hanbury’s et al. [ 18 ] recent systematic review study showed that the strongest evidence and most pronounced effects of working time reduction can be found within the social dividend, meaning that it has the strongest impact on personal health and well-being (life satisfaction, quality of life, work-family conflict, etc.) of the employees. Similar findings were reported in the scoping review of Karhula et al. [ 26 ]. Other case studies, that were not included in either of the above-discussed review studies, such as the recent experiments in Iceland and the UK, preliminarily also show positive impacts on job-related well-being: increases in job satisfaction, feeling well at work, and job motivation [ 19 , 42 ].
Although review studies generally point to a rather positive impact of collective working time reductions on employees’ well-being, the overall evidence presented by the above-discussed studies seems somewhat inconsistent. This inconsistency might be due to deviations in the definition and measurement of (long) working hours (e.g., [ 20 ] as well as well-being [ 9 ]). Inconsistent findings can also be related to different conceptualizations and contexts in which the implementations took place [ 18 ]. These contexts relate to how the reduction is implemented (form), the extent and the level of implementation, what other changes took place (such as some organizations not reducing the workload, resulting in increased work intensity) (e.g., [ 37 ]), the work conditions and wage compensation, but also the broader (national) social and gender context [ 1 ]. We aim to emphasize in this study that it is not just concomitant changes in work and work context that are significant to changes in well-being in collective reduction of work hours, but also the concomitant changes that happen in the private realm and the household context related to this reduction.
Changes in work context
Working time reductions might change work conditions or the work context, which can in turn also affect well-being. Anttila et al. [ 1 ] found different impacts by socio-economic status: only manual and lower-level white-collar employees experienced a reduction in work-family conflict, while upper-level white-collar employees did not. Similarly, Hanbury et al. [ 18 ] found smaller reductions in work-life conflict for upper-level white-collar workers. The authors relate these differences to upper-level white-collar employees having to do the same tasks in less time and having less autonomy over their work timing than before, while on the other hand, blue-collar workers might in general have fewer other resources to cope with work stressors and therefore a reduction in work time might have a larger impact. Other research has shown that perceived control over time (time autonomy) can act as a moderator between working hours and occupational stress (e.g., [ 24 ]). Occupational stress might also be impacted by work intensity or work pressure. Especially when a reduction in working hours is not accompanied by a reduction in workload, (imposed) work intensity/pressure might rise [ 9 , 29 ]. The socio-economic aspect might also be important in our Belgian case study in that almost all workers (80%) are highly educated and are categorized as ‘knowledge workers’. These workers also have a lot of temporal autonomy over their work. We thus expect that changes in both work pressure and schedule control/autonomy over work will affect job-related well-being and general well-being as well.
Changes in the private realm and time use
How the extra time off is spent might also affect the experience of a working time reduction [ 46 ], yet this aspect is often absent from research. Having time for activities other than work might be of importance when it comes to workers’ well-being, as it makes room for recovery. Especially time spent on non-work activities [ 45 ], free time activities [ 28 , 30 ] and socialization activities and sports [ 15 ] are associated with higher levels of happiness and well-being. On the other hand, spending more time on childcare, spousal care activities and housework was found to be detrimental to mental health, especially for women [ 32 ]. Rather than actual time spent on housework, Thomas et al. [ 43 ] found that it was the perceived unfairness of the division of household labor that was associated with reduced health and well-being for women. Differential effects of work hours on well-being for women and men, such as more negative impacts of long hours on women’s depressive symptoms [ 49 ] or a better work-life balance for part-time working women [ 6 ] can be explained by gendered roles and expectations, with women more responsible for the family, while also taking up the work role (double burden/shift) (e.g., [ 7 , 22 ]). Anttila et al. [ 1 ] found that shorter daily hours reduced time-based work-family conflict for women, but only for those with children. Especially those well-being indicators related to the combination of both the family and the work role might thus be affected in women. Nevertheless, how the freed-up time is spent, might also impact more general well-being.
The Femma Wereldvrouwen case of work time reduction
This study reports results from a shorter workweek trial based in Belgium in 2019. As a non-profit women’s organization in the socio-cultural work sector, Femma Wereldvrouwen also supports a collective working time reduction on a societal level to reduce the inequalities in time use between women and men and to improve the often difficult combination of both paid and unpaid work for individual employees. Femma Wereldvrouwen opted to trial a shorter workweek themselves to see what the impact would be on their employees. For 12 months about 60 employees (varying over the years due to end of contracts and retirements) trialed a 30-h work week. All full-time employees reduced their working hours to 30 per week and retained their full-time salary. A normal full-time workweek before the 30-h workweek at Femma Wereldvrouwen comprised 36 h, yet some worked a full-time week of only 34 or 32 h. This already existing small reduction is not part of the trial and was based on age and agreed upon on a sectorial level. The age-based reduction is a union-acquired right for all end-of-career employees in specific sectors in Belgium and should be understood in the context of workable work. All employees over 50 could work 34 h full-time and those over 55 could work 32 h full-time. These groups thus reduced their working hours respectively by 4 or 2 h to 30/week in the 30-h workweek trial. Next to full-time workers, Femma Wereldvrouwen also had a group of part-time workers who did not reduce their hours but did receive a proportional wage increase. The part-time workers working 28 h/week before the trial had the option to increase their work hours to 30 and receive full-time pay. The employees at Femma Wereldvrouwen are fairly homogeneous: all but one were women and most (80%) were highly educated (with a college or university degree).
Organizational commitment and change to accommodate a shorter working week together with employee consultation seem important for successful implementation, especially regarding positive impacts on workers’ well-being (e.g.,[ 11 , 25 ]). Aware of this importance and committed to not increasing employees’ workload, Femma Wereldvrouwen sought support from organizational change consultants and installed a work group of employees who were co-responsible for the organizational changes in the run-up to the 30-h workweek. As part of this reorganizational plan, new employees were hired, and some tasks were outsourced during the trial to relieve pressure on employees. In addition, new self-managing teams were introduced several months before the start of the shorter workweek. Self-management, however, was not easy for all teams, and some struggled the first half year/year. A few teams (comprising 33% of employees) in particular deviated from other teams and management had to intervene in how they worked together and even started the resignation procedure for those employees who could not cope with the change. This affected the work atmosphere in these teams and might have impacted other teams as well.
Aim of our study and hypotheses
Using data on the effects of this collective reduction of working time trial, this study adds to the scarce evidence on the impact of collectively introduced shorter workweeks on mental well-being among female knowledge workers. This study will investigate changes in the three important domains of mental well-being: namely general (context-free) well-being, job-related well-being, and work-family well-being [ 14 ]. Our first hypothesis relates to work-family well-being. We hypothesize that a working time reduction will improve work-family well-being (H1a) because the burden of paid work is lowered in terms of duration which decreases the dual burden many women experience. Yet we expect that this might be mediated by how the extra time off is used. Extra time spent on leisure might be more beneficial (H1b). To the best of the authors’ knowledge, this will be the first paper including time-use data in the analysis of the impact of a collective shorter work week on mental well-being. Our second hypothesis relates to job-related well-being: following recent research on shorter workweek experiments discussed above, we expect job-related well-being to improve during the shorter workweek (H2a). However, changes in schedule control or work pressure will probably also affect this domain of well-being (H2b). Lastly, for our third hypothesis, we expect general well-being (like life satisfaction in Lepinteur’s study, [ 31 ]) to improve in the shorter workweek (H3a), which is also a consequence of the increase in job-related well-being and work-family well-being (H3b).
Data & methods
Research unit TOR at the BRISPO research group of the VUB was approached for its expertise in the study of time use and asked to study the impact of Femma Wereldvrouwen’s shorter workweek trial. Although some alignment was necessary, TOR conducted independent research and Femma Wereldvrouwen was not involved in the hypotheses, data analyses or discussion of results. We set up a panel study consisting of five waves of data collection both before, during, and after the 30-h workweek trial. In each wave, a 7-day time-use diary and survey (pre- and post-diary) data were collected from all employees. The first two waves took place in March and October of 2018, the year before the trial. These are the pre-measurements. The third and fourth waves took place during the trial, in March and October 2019. The last wave took place in March 2020, some months after the end of the trial. Unfortunately, the first Covid-19 lockdown started in the middle of March in Belgium and most of the employees were still in the process of keeping their time-use diary when everyone was told to stay home. We cannot compare this wave to earlier waves. We will thus only use the pre- and during the shortened workweek (also called pre- and post-intervention) measurements of 2018 and 2019 to study the impact of the working time reduction. Table 1 shows the total number of employees invited and participating in all stages of the included waves. In the pre-diary survey, respondents were asked about their work hours, socio-demographic background variables, their workplace experiences, experienced time use, and schedule control. In the time-use diary, respondents registered in detail all of their activities with timings during seven days. The post-diary survey included questions on their filled-in diary week (was this a normal week etc.), transport, the division of unpaid work, and questions on well-being. Table A1 in the appendix lists for each dependent and independent variable used in this article with which instrument the data were collected. All data was collected through the MOTUS software [ 35 ].
For the analyses, we use the sample of respondents with a valid response for (at least one of) the dependent variables (total n = 60, not all observed in every wave, 200 observations over the waves, see numbers in Table 1 ). The percentage of missing values in this sample varies by variable (see Table A1 in the appendix) and missings were imputed (see also further for the method of imputation).
Experimental and control groups
The impact of the shorter workweek can be studied by comparing the well-being scores in waves 3 and 4 (post-measurements) to their scores in wave 1 and wave 2 (pre-measurements). In addition, changes in well-being can be compared between what we might call experimental and control groups. The trial was not designed to have a randomly assigned control group to compare the experimental group with. Yet when 30 h became the new maximum number of work hours, some workers’ work time was reduced to a greater extent than others’. Thus, intervention effects can be expected to depend on workers’ initial work hours (as a proxy for the amount of change in work hours), as is explained in the variables section on work hours.
Table 2 shows the mean values and percentages of all dependent and independent variables for each wave.
Dependent variables
To address the multidimensional character of well-being, workers’ well-being was assessed in three domains: work-family well-being, job-related well-being, and general (or context-free) well-being.
Work-family conflict is used as a measure of the work-family well-being dimension. The work-family conflict scale is constructed as a sum score (rescaled to 0–10) of four items scored on a 4-point Likert-scale (ranging from 1 never or almost never to 4 always or almost always) with a Cronbachs α > 0.79. Items include [How often does it happen that…] ‘you feel less involved with your family/friends because of the requirements of your work?’ or ‘you feel that you lag behind the events at home?’. The higher the score, the higher the conflict experienced.
Positive work experience is the variable that we use as a proxy for job-related well-being. The scale measures the pleasure, meaningfulness and challenge in work and is a sum scale (rescaled to 0–10) based on five items scored on a 4-point Likert-scale (ranging from 1 never or almost never to 4 always or almost always) (Cronbachs α > 0.88). Items include ‘I find it pleasant to start the workday’ and ‘I love the challenge in my work’ (see appendix for full list). The higher the score on the scale, the better the subject’s work experience.
General (context-free) well-being was measured using 5 items from the short version of the Warwick-Edinburgh Mental Well-being Scale (SWEMWBS), all measured on a 5-point Likert scale ranging from never to always (Cronbachs α > 0.74) to construct a general well-being sum score (rescaled to 0–10). SWEMWBS represents mostly aspects of psychological and eudemonic well-being (as part of the full 14-item WEMWBS; [ 40 ]). Even though SWEMWBS construct validity was confirmed in diverse populations (e.g., [ 13 , 44 ]), in our study (longitudinal) confirmatory factor analyses led us to exclude two items (which improved model fit from poor to fair as RMSEA changed from 0.125 to 0.077 and CFI from 0.729 to 0.932), which also improved longitudinal measurement invariance (see further). Items include [in the last two weeks] ‘I’ve been feeling optimistic about the future’ and ‘I’ve been feeling relaxed’. Whereas the other measures were administered in each of the four waves, the SWEMWBS scale was only included in the surveys starting in wave 2.
In this study, employees were categorized into three groups: those working 26 h or less before the start of the trial (i.e., part-time employees), those working 28 to 34 h, and those working 36 h before the trial. The 36-h group makes up 41% to 49% of employees in our data, with exact numbers varying over the different waves. The 28–34-h group represents 28% to 31% over the waves and the 26-h or less group is between 20 and 30%. The fluctuations in numbers are due to non-response and the imposition of strict quality checks on the time diaries, as well as changes in the composition of employees at Femma Wereldvrouwen over time as some employees retired, resigned or new ones were hired. As stated above, all full-time employees (working 32, 34 or 36 h) reduced their working hours to 30 per week in 2019. The 36-h group is the most interesting here as they experienced the largest reduction in work time (6 h per week; see also Fig. 1 ). The 28 to 34 h group consists of employees with a smaller reduction in work time (4 or 2 h per week). A few employees even increased their work time (voluntarily, from 28 to 30 h), which we control for with a dummy variable (1 = increased work hours, 0 = not increased work hours). The part-time group that worked 26 h or less per week did not reduce their weekly working hours and as such can be considered as some sort of control group for the full-time workers. This group, similar to the 28–34 h group, differs from the 36-h intervention group as the workers are older, do not have children at home, and experienced less work-family conflict and household stress at baseline (see Table A3 in the appendix). As discussed further in this section, we control for these socio-demographic background characteristics as well as for (time-varying) work and private life-related variables, which is in line with JRC’s recommendations [ 10 ]. Regarding the effect of work time reduction, we expect to find the largest changes between waves among the 36-h group, followed by smaller changes in the 28–34 h group, and no effects in the 26-h or less group.
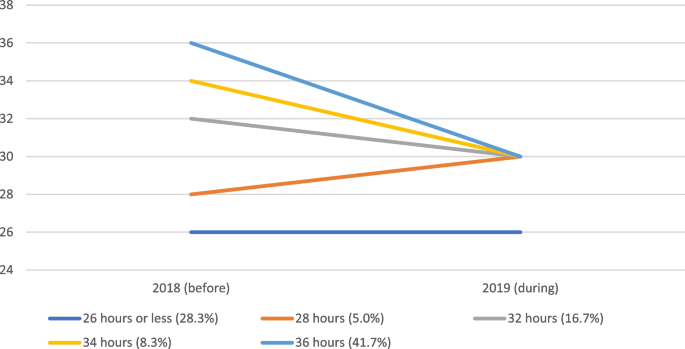
Reduction (or increase) of working time for different working time groups between 2018 (before the trial) and 2019 (during the trial) (research sample N = 60, same as used in further analyses)
Time-changing mediating variables
Time-use variables.
Most of the time-use-related variables are derived from the 7-day time diaries respondents kept and measured based on the total duration of time spent on activities during these 7 days (and rescaled to number of hours per day). Only the variable ‘sufficient free time’ is derived from the pre-diary survey.
Sufficient free time was measured by the question ‘To what extent do you feel you have sufficient free time?’, scored from 1 (too little) to 7 (more than enough). This measures the adequacy of free time experienced by the respondent.
Time spent on leisure activities (hobbies, games, TV and video, cultural participation, going out, sports, recreation, music, reading).
Time spent on social participation (talking, visiting family, friends, …).
Time spent on household work (cleaning, cooking, washing, …).
Work variables
Schedule control is a scale score calculated as the average on three items scored on a 5-point Likert-scale (ranging from 1 totally disagree to 5 totally agree). Items include: ‘I can decide for myself how I do my work’; ‘I can decide for myself how much work I do in a day’; ‘I can decide for myself what work I do in a day’.
Satisfaction with work pressure was measured by one item ‘Please indicate the extent to which you are currently satisfied with the following aspects of your work: work pressure’ on a 5-point Likert-scale (ranging from 1 not at all satisfied to 5 very satisfied).
Household variables
Household stress is a scale score calculated as the average of four items on a 5-point Likert-scale (ranging from 1 totally disagree to 5 totally agree). Items include ‘There are moments when I am short of hands in the household’; ‘I feel stressed when I think about the household tasks that still have to be done’; ‘I often postpone my household chores’; ‘The time for household work is planned and fixed in advance’ (reverse coded).
Satisfaction with division of housework is based on the question ‘To what extent are you satisfied with the division of housework between you and your partner?’. The question was answered with a 5-point Likert-scale (ranging from 1 not at all satisfied to 5 very satisfied).
Control variables
Socio-demographic variables.
Age of the respondent was measured based on their age in 2020. In our analyses, we centered the age variable at its mean (48). The mean age of the 36-h group in 2020 was 38,5. This is the youngest group. The mean age of the 28 to 34-h group was 54 and the mean age of the 26-h or less group was 58,2.
Living with children: We also controlled for the composition of the household, taking into account whether the respondent lived with children under 18 in their household or not (reference category). With this, we want to control for the extra care responsibilities in the household.
Living with partner: We discern those who live with their partner (reference category) from those who do not live with their partner or do not have a partner.
Work context
Transitioning teams: We control for membership of a teams that had difficulties dealing with the organizational changes and reorganization (see the context section). Being a member of a team that did not experience particular adjustment problems acts as the reference category.
Missing values were imputed using multiple imputations by chained equations (MICE), on the full set of the analyses variables, including the dependent variables, adapted to the measurement level of the variables, and using the original Likert items to derive (passively) imputed scale scores. We generated 10 complete datasets. Results of the repeated complete data analyses were combined by averaging estimates and with adjusted standard errors using Rubin’s rules (using the R-libraries mice, broom.mixed and mitml ).
Longitudinal measurement invariance of the Likert-item composed scale variables was checked (using sem and Lavaan libraries in R) to assess the psychometric equivalence of the constructs for individuals over time. The procedure is to specify confirmatory factor analysis structural models for each wave simultaneously (and allowing covariance over time both in latent constructs and in corresponding items) and compare this model with models with additional constraints to test measurement invariance over time (e.g. [ 36 ]). Full scalar measurement invariance was reached for schedule control, household stress and positive work experience (see also Table A2 in the appendix). For work-family conflict and the well-being scale, metric invariance is confirmed. Scalar measurement invariance can be accepted according to certain model fit criteria (i.e., model with the lowest BIC or change in RMSEA < 0.01), even though it would be rejected by the (overly strict) likelihood ratio model comparison tests (respectively 21, df 9, p = 0,012, and 169, df = 8, p = 0.031).
To analyze the effects of work time reduction, we model change over time (waves) using multilevel growth models (cf. [ 39 ]), with measurements at each of the waves as first-level observations, nested within the respondents as the second-level grouping variable. For the two context-specific well-being measures (work-family conflict and positive work experience), we specify a random slope (for wave) model, for the general well-being measure, we specify a random intercept model (as we only have three measurement occasions). In all these models, the wave is included as a predictor using dummy coding (reference: first wave), as well as the work hours group (36-h group as reference group), and the interaction terms for these two variables which allow detecting different changes over time by work hours group. These multilevel analyses were performed in R using the lme4 library. The number of observations in our sample exceeds the minimum recommendation by Hox and McNeish [ 23 ] for longitudinal samples to obtain adequate parameters from hierarchical linear modeling when using the REML method. Footnote 1
For each of the three well-being measures, we report on two models. Model 1 is the base model with the three working time groups, the four waves and their interaction terms, including controls for socio-demographic background and work context. In Model 2 we add the time-changing mediating variables to the Model 1 specification. Here we are interested in a) how concomitant changes in work and home/private circumstances might explain work time reduction effects and b) which of these changes are related to changes over time in well-being (longitudinal rather than cross-sectional effect estimations). By including workers’ initial levels in these time-changing characteristics, we control for person-level (between) differences and ensure that the effect parameters for the time changing work and household characteristics can be interpreted as the effects of changes over time (within differences). Finally, for general well-being we report on a third model, in which the time-changing variables for work-family conflict and positive work experience (as well as workers’ initial levels as control variables) are included as well.
Table 3 reports on the results from the multilevel growth models for the three well-being measures. To facilitate interpretation, in Fig. 2 we also visualize the growth curves for the three work hour groups, based on the estimates from Model 1 in Table 3 . These figures visualize the model-based estimated means for each work hour group in all waves. Apart from illustrating the differences between the groups, the figures show the changes over time for each of the work hour groups. The error bands illustrate the precision of estimated within-individual change and depict the standard error of the estimated wave effects in relation to the first wave.
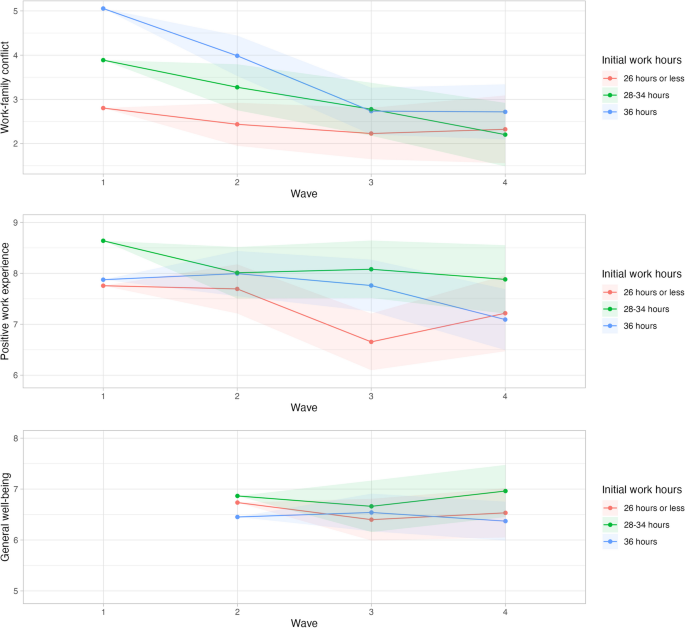
Growth curves for the three work hour groups of the three tested domains of well-being: work-family conflict, positive work experience and general well-being (based on the Model 1 parameters reported in Table 3 )
Note: Estimated means calculated at age 38, living with a partner and having children at home. Error bands represent the standard error of the estimated wave effects per work hours group with reference to the first wave (second wave for general well-being). To highlight the differences, the Y-axes in the figures do not cover the complete range. This scaling visually accentuates the differences between groups, which are not necessarily statistically significant
- Work-family conflict
Work-family conflict decreased significantly over the waves for the 36-h group (Model 1 in Table 3 , see also Fig. 2 ). Already in wave 2 (October 2018) when the shorter workweek trial had not even started, work-family conflict decreased (B = –1.07; 95% confidence interval: [–1.97, –0.17]) among the 36-h group. This decrease becomes even larger during the 30-h workweek trial in wave 3 (B = –2.32; [–3.36, –1.28]) and in wave 4 (B = –2.34; [–3.56, –1.12]), which is in line with hypothesis H1a. Among the less than 26-h group, this decrease in work-family conflict is much smaller as the time effects differ significantly from those in the 36-h group, (if summed, only small negative effect parameters remain over time for the less than 26-h group, and when used as the reference group in analyses not shown here we did not find significant changes over time). As mentioned in the data section, this group did experience a lower work-family conflict to start with (cf. main effect for work hours group), which is probably explained by their standard shorter working hours (before the experiment). The time effects for the in-between 28 to 34-h group do not differ significantly from those of the 36-h group, but the (positive) effect parameters for the time interaction terms (in combination) indicate that the decrease in work-family conflict over time for the 28–34 h group is smaller than the 36-h group’s and larger than the less than 26-h group’s. Those who reduced their working hours more thus reap the most benefits in work-family conflict. This beneficial effect of work time reduction, however, is much less clear for the members of the few teams that had difficulty in coping with the organizational changes. In particular, in wave four, work-family conflict started to increase among the (remaining) employees of these teams. The negative work-family effects for these team members were probably caused by the spill-over of negative work experiences (see further).
Model 2 allows us to look into the effects of concomitant changes in work and the private realm. Holding these time-changing characteristics constant, the decrease in work-family conflict over time for the 36-h group remains but is less pronounced. Slightly less than 30% of the decrease in work-family conflict during the shorter workweek (wave 3 and 4) among the 36-h group is explained by concomitant changes in work and private circumstances (e.g., B of –2.32 becomes –1.66 in wave 3; –1.66/–2.32 = 71.6% of the effect remains). The main changes over time that are related to changes in work-family conflict concern schedule control, satisfaction with work pressure and sufficient free time. Increases over time in schedule control, satisfaction with work pressure and sufficiency of free time, correlate with a decrease in work-family conflict. For hypothesis H1b we expected that if extra time was spent on leisure time this would impact work-family conflict. Yet we only find the subjective sufficiency of free time experienced by the employees, in addition to two work-related variables, to play a role in explaining some of the reduction in conflict between work and family.
Positive work experience
Although there is a negative tendency in all work hour groups (in particular in wave 4, and most strongly for members of the teams who struggled with the organizational changes), no significant general change is apparent in positive work experience over the waves (Model 1 in Table 3 , see also Fig. 2 ). This does not provide support for hypothesis H2a. We even see that among employees who were part of a team that had difficulties with the reorganizational changes, the positive work experience decreased strongly (and significantly) in wave 4 (October 2019) in comparison with wave 1 (March 2018) (B = –1.75; [-3.31, -0.19]).
Holding constant the time-changing work and home variables (Model 2), positive work experience does decrease strongly and significantly for employees in the 36-h group in wave 4 compared to wave 1 (B = –1.23; [-2.45, -0.01]). Nine months into the shorter workweek, these employees would have experienced a less positive work environment/experience but this negative effect is offset (in part) by some other (positive) concomitant changes. The most important time-changing variable affecting change in positive work experience is schedule control: an increase in schedule control leads to an increase in positive work experience (controlled for baseline differences). Schedule control acts as a suppressor variable: if it had not changed over the waves, the 36-h group would have had a lower positive work experience (B = –1.23). Schedule control can thus help alleviate negative experiences at work. This partly supports hypothesis H2b in which we expected (changes in) schedule control to affect job-related well-being.
General well-being
For general well-being, we only have data for the three last waves, so October 2018 (three months before the start of the trial) is the reference wave. There is no significant change in general well-being over the waves, for either of the three groups (Model 1 in Table 3 , see also Fig. 2 ), so hypothesis H3a is not confirmed. Holding the time-changing characteristics of work and home contexts constant (Model 2), general well-being tends to decrease over time, which is partly due to the decreased work enjoyment, particularly in wave 4 (Model 3), although effects are not statistically significant.
Among the changes in work and private context, having sufficient free time is an important predictor for general well-being. Increases over time in the experience of sufficient free time and satisfaction with the division of housework at home are related to increases in general well-being (B = 0.27 [0.01, 0.53]; B = 0.28 [-0.01, 0.57]). As positive work experience and work-family conflict might affect general (or context-free) well-being, we added these to Model 3. Indeed, a change in positive work experience impacts general well-being, more specifically an increase in positive work experience over time is related to improvements in general well-being (B = 0.14 [-0.03, 0.31]), partly supporting hypothesis H3b. The decrease in positive work experience however offset part of the potential positive effects of work-time reduction for general well-being. Work-family conflict, on the other hand, does not appear to be related to general well-being longitudinally.
Discussion and conclusion
In this quasi-experiment, the shorter workweek in itself did not seem to significantly impact general well-being. After nine months, employees whose weekly work hours were reduced with 6 h experienced lower job-related well-being (positive work experience), in particular if the increase in schedule control for this group was accounted for. This corresponds to some of the findings from the national working time reduction in Korea [ 37 ], yet is unlike findings from many other small-scale experiments [ 2 , 18 , 42 , 46 ] and from national implementations in France and Portugal [ 31 ] where job and life satisfaction did increase during the shorter workweek. However, we did find an improvement in work-family conflict over the waves for the women whose working hours were reduced. As of wave 2, in October 2018, the conflict between work and family started to decrease, even more so during the shorter workweek. This improvement was partly explained by increased schedule control, satisfaction with work pressure and perception of sufficient free time over time. When the shorter workweek led to more of these, work-family conflict decreased. Yet also without changes in these work and family context characteristics, the shorter workweek decreased the experienced work-family conflict. That we find an impact on work-family conflict could have been expected as a shorter workweek reduces the time spent on work and releases time for private pursuits such as family. This was also an important aim of the 30-h workweek at Femma Wereldvrouwen. Especially for women who often bear more responsibility over household work and care tasks, such a reduction might be beneficial [ 1 , 6 , 22 , 49 ]. However, in the case of this trial, not only the time spent at work was reduced, but the organization also put in efforts to decrease work pressure by outsourcing work and hiring new employees to take over tasks that could no longer be performed by the former employees due to reduced work time in the shorter workweek. This had a positive impact on work-family conflict (already at wave 2). Other research has shown that having to do the same work in a shorter workweek can lead to higher work intensity and increase stress among employees [ 11 , 29 , 37 ].
For both work-family conflict and positive work experience change over time in schedule control has a beneficial impact. Improving schedule control can thus be a good strategy to alleviate possible negative impacts of a shorter workweek (such as changes in teams or the organization of work) or increase positive impacts even more. This relates to Anttila’s finding [ 2 ] that the loss of some schedule control in the 6-h workday experiments in municipalities in Sweden led to some adverse effects concerning work and family.
Context is important to understand shorter workweek trials as they do not take place in a vacuum but in the real world. The same reorganization that helped outsource work to not increase work pressure also installed new self-managing teams four to three months before the start of the shorter workweek trial. Self-management is not easy for everyone and some teams did not handle it very well. In the middle of 2019, management had to intervene in these teams and some employees that could no longer ground in the new organizational set-up were laid off or decided to leave the organization themselves. Through in-depth interviews that were part of the broader research project, we know that this negatively impacted the atmosphere in some of the teams. This contextual info might help understand the findings for job-related well-being (and spill-over into general well-being) for the few teams that had a harder time. It also shows that a collective decrease in working time should go hand in hand with a careful rethinking of work practices, and this should be an ongoing concern. Allowing enough time for interventions such as new self-managing teams to settle before introducing other interventions is an important lesson as well. Femma Wereldvrouwen learned that the time between the reorganization and the introduction of the shorter workweek was too short as teams needed time to settle in their new ways of working. Both during and after the trial, Femma Wereldvrouwen made some adjustments in the teams such as merging some of the teams and reintroducing bilateral coaching.
We did not find any significant effects of any of our time use variables based on the 7-day diary. We had expected that increases in leisure time in the shorter workweek might have positively affected some well-being indicators. The only time-use-related variable that seemed to matter was the experience of sufficient free time. This variable is a subjective evaluation (originated from the surveys), which correlates significantly but weakly with time spent on leisure time (from the diaries) ( r = 0.265). The dependent variables are also subjective measures, and originate from the surveys as well. It could be a common method effect that these subjective measures correlate more strongly with each other than with the durations of time spent on activities from a random week, which are more objective measures. Additionally, the reference period of the dependent variables’ items is two weeks or ‘in general’ and thus differs from the reference period of the diary, which is 7 days.
The trial lasted one year, which is as long or longer than other recent trials with reduced work hours (e.g. [ 11 , 42 ]). For work-family conflict, we see the start of the positive impact of a shorter workweek already in wave 2, three months before the start of the trial. This might point to some sort of Hawthorne effect, where the fact of being part of a trial, here the fact of working for an employer that is involved with workers’ well-being and that will trial a shorter workweek (and concomitant preparations), in itself already impacts the experienced well-being of employees. Schor [ 38 ] mentioned a similar finding for job satisfaction in the recent experiments with the four-day workweek in the US. Lastly, the trial was limited to one organization, where partners of employees did not reduce working hours. Within the vision of Femma Wereldvrouwen, the aimed result of a better and fairer combination of paid and unpaid work and gender equality would only be attained if everyone worked less. In this case, it was only one organization with mostly female employees. For now, the shorter workweek at Femma Wereldvrouwen did improve women’s experiences of their work-family combination, which is an important step towards more gender equality as women still bear most of the burden of the double shift.
Despite the limitations of the non-randomized study design and the small sample of highly-educated female knowledge workers, our longitudinal design with two pre-measurements and two post-intervention-measurements including time-use data, as well as intervention and some sort of control groups, provided us with a unique dataset and broad set of measures to evaluate the impact of work time reduction. Although the results from this trial might not transfer to other contexts, it does provide compelling evidence that shorter workweeks can potentially lead to significant improvements in work-life balance, i.e. through reduced work-family conflict as evidenced in our longitudinal analysis. Although the other well-being impacts were variable, the marked benefits for female employees underscore the potential for tailored work time reductions to enhance the combination of work and family life. Our study can inform other trials, and organizations considering trialing a shorter workweek and furthers the limited scientific knowledge on the topic.
Availability of data and materials
The raw data on the employees of the organization that trialled the shorter workweek as well as the aggregated data are protected and shared only with researchers within our research group. The organization is very small and anonymity cannot be guaranteed. The organization only consented on the data being used by us. Upon request, our syntaxes of analyses can be made available. Please e-mail [email protected].
The use of small sample sizes is not uncommon in longitudinal studies. We analyze LGM within the HLM framework. Even in the case of small numbers, HLM seems to be a viable method of analysis with good performance to recover parameters and providing the least-biased method to account for clustering [ 33 , 50 ]. The number of respondents in our sample seems adequate, in particular as we use the REML method (instead of ML), whose performance is better for smaller samples. E.g. based on a review of studies, McNeish & Stapleton [ 34 ] recommend in the case of a continuous outcome a minimum of 15 to 30 clusters for unbiased fixed effects parameters and of at least 30 clusters for unbiased fixed effects standard errors. For longitudinal samples, Hox and McNeish [ 23 ] recommend a minimum of 20 clusters for adequate fixed effect parameters when using REML.
Anttila T, Nätti J, Väisänen M. The experiments of reduced working hours in Finland: impact on work-family interaction and the importance of the sociocultural setting. Community Work Fam. 2005;8(2):187–209. https://doi.org/10.1080/13668800500049704 .
Article Google Scholar
Anttila T. Reduced working hours: reshaping the duration, timing and tempo of work [Doctoral dissertation]. Jyväskylä: University of Jyväskylä; 2005.
Google Scholar
Bader C, Hanbury HA, Neubert SF, Moser S. Weniger ist Mehr–Der dreifache Gewinn einer Reduktion der Erwerbsarbeitszeit. Weniger arbeiten als Transformationsstrategie für eine ökologischere, gerechtere und zufriedenere Gesellschaft–Implikationen für die Schweiz [Internet]. 2020. Available from: https://boris.unibe.ch/144160/1/CDE_Working_Paper_6_Bader_2020.pdf
Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health. 2014;40(1):5–18. https://doi.org/10.5271/sjweh.3388 .
Article PubMed Google Scholar
Barck-Holst P, Nilsonne Å, Åkerstedt T, Hellgren C. Reduced working hours and stress in the Swedish social services: A longitudinal study. International Social Work. 2017;60(4):897–913. https://doi.org/10.1177/0020872815580045
Beham B, Drobnič S, Präg P, Baierl A, Eckner J. Part-time work and gender inequality in Europe: a comparative analysis of satisfaction with work–life balance. Eur Soc. 2019;21(3):378–402. https://doi.org/10.1080/14616696.2018.1473627 .
Bianchi SM, Milkie MA, Sayer LC, Robinson JP. Is anyone doing the housework? Trends in the gender division of household labor. Soc Forces. 2000;79(1):191–228. https://doi.org/10.1093/sf/79.1.191 .
Bielenski H, Bosch G, Wagner A. Working time preferences in sixteen European countries. Dublin: European Foundation for the Improvement of Living and Working Conditions; 2002.
Cooke PJ, Melchert TP, Connor K. Measuring well-being. Counsel Psychol. 2016;44(5):730–57.
Cuello H. Assessing the validity of four-day week pilots. Seville: European Commission, JRC; 2023.
Delaney H, Casey C. The promise of a four-day week? A critical appraisal of a management-led initiative. Empl Relat. 2021;44(1):176–90. https://doi.org/10.1108/er-02-2021-0056 .
Fagnani J, Letablier M-T. Work and family life balance: the impact of the 35-hour laws in France. Work Employ Soc. 2004;18(3):551–72. https://doi.org/10.1177/0950017004045550 .
Fat LN, Scholes S, Boniface S, Mindell J, Stewart-Brown S. Evaluating and establishing national norms for mental wellbeing using the short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS): findings from the Health Survey for England. Qual Life Res. 2017;26:1129–44.
Fox KE, Johnson ST, Berkman LF, Sianoja M, Soh Y, Kubzansky LD, et al. Organisational- and group-level workplace interventions and their effect on multiple domains of worker well-being: a systematic review. Work Stress. 2022;36(1):30–59. https://doi.org/10.1080/02678373.2021.1969476 .
Galay K. Time use and happiness. Thimphu: Centre for Buthan Studies; 2008.
Ganster DC, Rosen CC, Fisher GG. Long working hours and well-being: what we know, what we do not know, and what we need to know. J Bus Psychol. 2018;33(1):25–39. https://doi.org/10.1007/s10869-016-9478-1 .
Gash V, Mertens A, Romeu Gordo L. Women between part-time and full-time work: the influence of changing hours of work on happiness and life-satisfaction. SSRN Electron J. 2009. https://doi.org/10.2139/ssrn.1553702 .
Hanbury H, Illien P, Ming E, Moser S, Bader C, Neubert S. Working less for more? A systematic review of the social, economic, and ecological effects of working time reduction policies in the global North. Sustainability. 2023;19:2222595.
Haraldsson DG, Kellam J. Going public: Iceland’s journey to a shorter working week. Alda and Autonomy; 2021.
Härmä M, Ropponen A, Hakola T, Koskinen A, Vanttola P, Puttonen S, et al. Developing register-based measures for assessment of working time patterns for epidemiologic studies. Scand J Work Environ Health. 2015;41:268–79.
Hayden A. Well-being, suffiency, and work-time reduction. In: Costanza R, Kubiszewski I, editors. Creating a sustainable and desirable future - insights from 45 global thought leaders. Singapore: World Scientific Publishing; 2014. p. 249–53.
Chapter Google Scholar
Hochschild AR. The second shift: working parents and the revolution in the home. London: Piatkus Books; 1989.
Hox J, McNeish D. Small samples in multilevel modeling. In: Van de Schoot R, Miočević M, editors. Small sample size solutions a guide for applied researchers and practitioners. London: Routledge; 2020.
Hsu YY, Bai CH, Yang CM, Huang YC, Lin TT, Lin CH. Long hours’ effects on work-life balance and satisfaction. Biomed Res Int. 2019;2019(5046934):1–8.
Jahal T, Bardoel A, Hopkins JL. Could the 4-day week work? A scoping review. Asia Pac J Hum Res. 2023;62:e12395.
Karhula K, Anttila T, Vanttola P, Härmä M. Workplace-level interventions and trials of working time reduction: a scoping review. Helsinki: Finnish Institute of Occupational Health; 2023.
Kasser T, Brown KW. On time, happiness, and ecological footprints. In: De Graaf J, editor. Take back your time: fighting overwork and time poverty in America. San Francisco: Berrett-Koehler; 2003. p. 107–12.
Kasser T, Sheldon KM. Time affluence as a path toward personal happiness and ethical business practice: empirical evidence from four studies. J Bus Ethics. 2009;84(S2):243–55. https://doi.org/10.1007/s10551-008-9696-1 .
Kelliher C, Anderson D. Doing more with less? Flexible working practices and the intensification of work. Human Relations. 2010;63:83–106.
Knight K, Rosa EA, Schor JB. Reducing growth to achieve environmental sustainability: the role of work hours. In: Capitalism on trial. Cheltenham: Edward Elgar Publishing; 2013.
Lepinteur A. The shorter workweek and worker wellbeing: evidence from Portugal and France. Labour Econ. 2019;58:204–20. https://doi.org/10.1016/j.labeco.2018.05.010 .
MacDonald M, Phipps S, Lethbridge L. Taking its toll: the influence of paid and unpaid work on women’s well-being. Fem Econ. 2005;11(1):63–94. https://doi.org/10.1080/1354570042000332597 .
McNeish DM, Harring JR. Clustered data with small sample sizes: comparing the performance of model-based and design-based approaches. Commun Stat Simul Comput. 2017;46(2):855–69.
McNeish DM, Stapleton LM. The effect of small sample size on two-level model estimates: a review and illustration. Educ Psychol Rev. 2016;28(2):295–314.
Minnen J, Glorieux I, van Tienoven TP, Daniels S, Weenas D, Deyaert J, et al. Modular Online Time Use Survey (MOTUS) – translating an existing method in the 21st century. Electron Int J Time Use Res. 2014;11(1):73–93.
Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. https://doi.org/10.1016/j.dr.2016.06.004 .
Article PubMed PubMed Central Google Scholar
Rudolf R. Work shorter, be happier? Longitudinal evidence from the Korean five-day working policy. J Happiness Stud. 2014;15(5):1139–63. https://doi.org/10.1007/s10902-013-9468-1 .
Schor J. A Four-Day Work Week? Boston College Magazine. 2022. Available from: https://www.bc.edu/content/bc-web/sites/bc-magazine/fall-2022-issue/linden-lane/a-four-day-work-week-.html .
Singer JD, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. New York: Oxford University Press; 2003.
Book Google Scholar
Stewart-Brown S, Tennant A, Tennant R, Platt S, Parkinson J, Weich S. Internal construct validity of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS): a Rasch analysis using data from the Scottish Health Education Population Survey. Health Qual Life Outcomes. 2009;7(1):15. https://doi.org/10.1186/1477-7525-7-15 .
Sturman MC, Walsh K. Strengthening the employment relationships: the effects of work-hours fit on key employee attitudes. J Organ Behav. 2014;35(6):762–84.
Lewis K, Stronge W, Kellam J, Kikuchi L. The results are in: the UK’s four-day week pilot. 2023.
Thomas CL, Laguda E, Olufemi-Ayoola F, Netzley S, Yu J, Spitzmueller C. Linking job work hours to women’s physical health: the role of perceived unfairness and household work hours. Sex Roles. 2018;79(7–8):476–88. https://doi.org/10.1007/s11199-017-0888-y .
Thygesen LC, Møller SP, Ersbøll AK, Santini ZI, Nielsen MBD, Grønbæk MK, et al. Decreasing mental well-being during the COVID-19 pandemic: a longitudinal study among Danes before and during the pandemic. J Psychiatr Res. 2021;144:151–7. https://doi.org/10.1016/j.jpsychires.2021.09.035 .
Verbakel E, Diprete TA. value of non-work time in cross-national quality of life comparisons: the case of the United States vs. The Netherlands. Soc Forces. 2008;87(2):679–712.
Voglino G, Savatteri A, Gualano MR, Catozzi D, Rousset S, Boietti E, et al. How the reduction of working hours could influence health outcomes: a systematic review of published studies. BMJ Open. 2022;12(4):e051131. https://doi.org/10.1136/bmjopen-2021-051131 .
von Thiele Schwarz U, Lindfors P, Lundberg U. Health-related effects of worksite interventions involving physical exercise and reduced workhours. Scand J Work, Environ Health. 2008;34(3):179–88.
Watanabe K, Imamura K, Kawakami N. Working hours and the onset of depressive disorder: a systematic review and meta-analysis. Occup Environ Med. 2016;73(12):877–84. https://doi.org/10.1136/oemed-2016-103845 .
Weston G, Zilanawala A, Webb E, Carvalho LA, McMunn A. Long work hours, weekend working and depressive symptoms in men and women: findings from a UK population-based study. J Epidemiol Community Health. 2019;73(5):465–74. https://doi.org/10.1136/jech-2018-211309 .
Yamamoto Y, Miyazaki Y. Small sample methods in multilevel analysis. J Exp Educ. 2024;Online First:1–32.
Download references
Acknowledgements
The authors would like to thank the employees who participated in the study. FM would also like to thank William Fleming for the brainstorms in the beginning of the process of this paper and Brendan Burchell for providing some feedback on the literature study.
The research is part of a larger research project that was funded by FWO Vlaanderen (G019020N).
Author information
Authors and affiliations.
Research Group BRISPO, Vrije Universiteit Brussel, Pleinlaan 2, Brussel, 1050, Belgium
Francisca Mullens & Ilse Laurijssen
Research Group BRIO, Vrije Universiteit Brussel, Pleinlaan 2, Brussel, 1050, Belgium
Ilse Laurijssen
You can also search for this author in PubMed Google Scholar
Contributions
FM helped collect the data, clean the data, initiated the idea of the paper and wrote the literature background, performed some of the descriptive analyses and wrote the results and discussion. IL helped clean the data and performed most of the analytical work, the longitudinal measurement invariance analyses and the multilevel growth models in R. IL also made adjustments to the texts written by FM. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Francisca Mullens .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Ethics Committee of Human Sciences at the Vrije Universiteit Brussel (reference number ECHW_215). Every participant consented to use their data for academic purposes and analyses on aggregated level when starting the surveys and time-use diaries. Informed consent was obtained from all subjects. All experiments were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mullens, F., Laurijssen, I. An organizational working time reduction and its impact on three domains of mental well-being of employees: a panel study. BMC Public Health 24 , 1727 (2024). https://doi.org/10.1186/s12889-024-19161-x
Download citation
Received : 22 May 2023
Accepted : 14 June 2024
Published : 28 June 2024
DOI : https://doi.org/10.1186/s12889-024-19161-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Working hours
- Shorter workweek
- Working time reduction
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Thousands with disabilities subjected to segregation in these three states
A family wonders how a cousin “slipped through the cracks” and wound up in a state nursing facility not long after her 18th birthday; a mother wonders how she lost her daughter to the same system; and a woman in her late 50s longs to leave a state facility to see her family again.
These are among the findings of an extensive Department of Justice investigation into how three states – Missouri, Utah and Nebraska – illegally segregated people with mental health disabilities. Federal prosecutors found that the states are unnecessarily institutionalizing thousands of people in state facilities, cutting them off from family and the rest of society.
The investigations date back to March 2021 based on numerous complaints.
“I have a dream that one day I will be free. Free to live on my own, free to live within my community, free to have overnight visits with my grandchildren,” says Angela, the woman in her late 50s, in the Missouri report issued by the DOJ. The federal report quotes people by their first name only. “Free to not be told who I can associate with, free to not have someone place me in a nursing home and leave me, without any regard to my well-being mentally and physically, most of all just free to live my life.”
The investigations found widespread violations of the Americans with Disabilities Act, which says adults with disabilities must live in as integrated of settings as possible.
"This is about weaving people with disabilities into the tapestry of American life," Assistant Attorney General Kristen Clarke of the Justice Department’s Civil Rights Division told USA TODAY. "This is about bringing an end to the unnecessary segregation and isolation of people with disabilities in our country. And it's about recognizing their dignity, their autonomy and their independence."
The investigations were published around the 25th anniversary of the 1999 Olmstead v. L.C. Supreme Court decision which upheld the principle that public entities must provide community-based services to people with disabilities to prevent segregation.
"Our work is about breathing life into the ADA's integration mandate," Clarke said. "We hope that our enforcement work sends a loud message to jurisdictions about the steps that they must take to comply with the law, and specifically to comply with the ADA."
The office of Missouri Gov. Michael L. Parson did not respond to requests for comment. The state cooperated with the Justice Department’s investigation, according to the report.
The report from the DOJ is one in a slew of investigations that have also gone after Utah and Nebraska for similar practices.
A federal investigation into practices in Utah found that the state is segregating people with disabilities by placing them in isolated “warehouse-like” facilities for day programs; an investigation into Nebraska’s practices found the state was also placing people with disabilities into segregated day programs and segregated living facilities .
In a statement, Utah’s Department of Health and Human Services said it’s committed to improving state treatment of people with disabilities. Nebraska’s Department of Health and Human Services said it was disappointed with the Justice Department’s "allegations,” adding that Gov. Jim Pillen’s administration had already shown its commitment to improving care for people with disabilities.
'Highly restrictive and controlled' in Missouri
The 45-page DOJ report on Missouri’s treatment of people with mental disabilities details how the state systematically funneled people into state nursing facilities, even though almost none needed even short-term stays.
The facilities come with skilled caregivers and are commonly known as nursing homes. But more than half of the people covered in the report were under 65 and didn’t require the care offered. The people covered in the report had been inside them for at least three years on average, and around half were clustered at just 39 of the state’s 500 nursing facilities.
The people interviewed in the report describe prison-like conditions at the facilities.
“They are highly restrictive and controlled settings that isolate and segregate residents by severely limiting or entirely cutting off their relationships with loved ones and their community,” the report says, “preventing them from interacting with non-disabled people.”
The isolation inhibits residents from pursuing work or education, which the report called “hallmarks of a segregated institution.”
“My son had a life before they took him there and now, he has nothing,” the mother of a man named Kelvin is quoted in the report as saying.
The DOJ investigation was based on reviewing state documents, data and interviews with dozens of state officials and county officials who are appointed guardians for people with disabilities, plus 130 interviews with people directly impacted by the state’s practices. Investigators inspected over 60 sites, including psychiatric hospitals and sites housing people with mental health disabilities.
Rules, according to people who described the facilities as like jail, included no telephone use, mail, freedom to leave and just one hour outside per day.
How do people end up there?
Federal officials found Missouri relies on state institutions more than almost any other state. Nearly 3,300 people without Alzheimer’s or dementia have been in such institutions for over 100 days as of March 2023, according to the report. They hold an average of 95 residents but range in size from 47 to 225 people.
Missouri places people with bipolar disorder or schizophrenia in its facilities at one of the highest rates in the country. At 10 of the 39 facilities, adults with either bipolar or schizophrenia diagnoses account for 82% to 90% of the population in 2021.
The people covered in the report have “low care needs.” Nationally, low-care residents account for 9% of people in nursing facilities; in Missouri, they account for 25%. The rate of people under 65 is more than twice the national rate of 18%.
The report attributed the widespread practice to the state’s court-appointed guardianship system, which it called a “pipeline to a nursing facility.” The pattern in Missouri is that people with mental health disabilities cycle in and out of psychiatric hospitals; they get assigned a guardian, either family or a public administrator because they’re found to be unable to care for themselves; and then, frequently, the guardian places the person in state facilities.
Thousands have ended up in nursing facilities as a result of guardianship. One unnamed person cited in the report called the court-mandated oversight a “sentence to be locked in a (nursing facility).”
Guardians are also allowed to set limits beyond those set by the actual facilities.
“Prisoners have more rights than a person under guardianship has,” said a resident named Angela. “Anything I do or have pleasure in, like smoking, can be taken away (at) the whim of my guardian.”
Alternatives to institutions
The people in Missouri institutions instead need community-based services, according to the report, which allow them to live in their communities in compliance with the Americans with Disabilities Act. All are offered in the Midwestern state but not widely.
The alternatives, the report says, include:
◾ Assertive community treatment: an evidence-based model where people with mental health disabilities are treated by people trained in psychiatry, social work, nursing and other fields.
◾ Permanent supportive housing: another evidence-based model where the person with a disability is limited to spending up to 30% of their income on rent for housing that’s in a community or building not reserved for people with disabilities.
◾ Peer support service: A type of mental health care provided by people with experience with mental health issues.
◾ Mobile crisis services: Mental health providers respond to mental health emergencies like 911 intending to divert people from psychiatric hospitalization.
◾ Crisis stabilization services: These community settings serve as an alternative to emergency rooms for people experiencing mental health crises and aim to connect them to lasting care.
Utah investigation
The DOJ found Utah was “segregating” people with disabilities, a clear violation of the Americans with Disabilities Act.
The federal investigators found the state has a practice of funneling people with disabilities into programs in “warehouse-like” settings in isolation from people without disabilities. In such settings, they aren't allowed to choose how to spend their time and cannot partake in typical community activities, including shopping, exercising, or meeting friends.
At the warehouses, they perform repetitive tasks like sorting through recycling, shredding paper, or folding laundry, often for less than minimum wage, the report says. The programs tend to target young people with disabilities who are transitioning out of school.
The report found the wait for state vocational programs providing long-term job support for people with disabilities is over five years long.
The Utah investigation began in March 2021 and was published this week.
Joe Dougherty, a spokesperson for the state’s Department of Health and Human Services, issued a statement in response.
“While nobody likes hearing that their programs still have barriers for people to receive services, the state of Utah sees people with disabilities as critical citizens in our state and is committed to improving our service system,” he said. “The benefit is reciprocal, as people in the community benefit from the talents, perspectives and experiences of people with disabilities.”
Nebraska pushes back
The DOJ’s investigation in Nebraska focused on people with serious mental illness. It found the state was also funneling people into segregated day programs and living facilities, rather than programs aimed at promoting integration.
State law, according to the report, mandates there be enough community-based programs to ensure people with mental illness can work and live independently. But around 5,000 people live in nursing facilities, many exclusively for people with disabilities.
Nebraska’s Department of Health and Human Services pushed back against what it called “allegations.”
Spokesperson Jeff Powell touted the creation of Certified Community Behavioral Health Clinics where anyone can get mental health care; the development of better programs to help people get disability accommodations; and the fact that it already offered employment and supportive housing programs.
“Pointedly, the DOJ concedes that the programs desired by the federal government already exist in Nebraska today,” Powell said. “DHHS intends to resolve this matter as expeditiously as possible and in a manner consistent with law and the best interests of the people of Nebraska.”
Women who sued Texas after being denied abortions say reproductive rights are their top election issue
The summary.
- On the second anniversary of the Supreme Court’s Dobbs decision, women who sued the state of Texas over exceptions to its abortion ban say reproductive rights are a defining election issue for them.
- The Texas Supreme Court last month ruled against the plaintiffs in the case, Zurawski vs. State of Texas.
- Amanda Zurawski, the lead plaintiff, told NBC News that she plans to dedicate all of her time and energy to re-electing President Joe Biden.
On the second anniversary of the Supreme Court’s Dobbs decision, women who sued the state of Texas in a high-profile lawsuit over exceptions to its abortion ban say their experiences have made abortion a defining issue for them heading into the November election.
The Texas Supreme Court last month, in Zurawski v. State of Texas, ruled against a group of women who had sued after they were denied abortions despite serious health complications during pregnancy. The group, represented by the Center for Reproductive Rights, grew to include a total of 20 women and two obstetrician-gynecologists who sought more specific guidelines about what situations qualify for medical emergency exceptions to Texas’ strict ban.
The state Supreme Court rejected their challenge, however, saying that Texas law does not permit abortion even when a fetus has a severe abnormality, and that it is up to doctors to determine when terminating a pregnancy is warranted under the law.
Samantha Casiano, one of the plaintiffs, said the experience of being denied an abortion brought home the reality of how severe Texas’ restrictions are.
“Now, everyone in my family has to vote,” she said. “If you’ve never voted before, you’re going to vote this year. I will drive you there. It’s just so important to me.”
Casiano was pregnant and living in East Texas with her husband and four children when she learned in December 2022 that her fetus had anencephaly, a fatal condition in which the brain and skull do not fully develop. She did not have the finances or child care to travel out of state for an abortion, so she carried the pregnancy to term and gave birth, only to watch her baby die within hours.
“Waking up every morning, knowing that your child is going to die and planning your child’s funeral before your child’s even here is insane, and it’s unfair. There’s just a lot of suffering there,” she said.
Casiano said supporting abortion access is especially important to her because she has a 3-year-old daughter.
“Later on, she’s going to be a mother. I have nieces that are going to be mothers, and I want them to have the health care that they need,” she said. “If, God forbid, they need it, it should be there for them.”

One in 10 women say the right to abortion is the most important issue determining their vote , according to a survey published last week by KFF , a health care research and policy organization.
Five states — Colorado, Florida, Maryland, New York and South Dakota — have abortion rights on the November ballot, and similar measures are pending in six more. Organizers in Montana on Friday submitted the required number of signatures to get a constitutional amendment on the ballot there that would enshrine abortion access.
Texas — where abortions are prohibited unless a patient has a life-threatening emergency and where doctors risk fines of at least $100,000, up to 99 years in prison and the loss of their medical licenses for performing abortions — does not have an abortion measure on the ballot.
The state’s medical board on Friday issued updated guidance for doctors about its abortion ban but refused to provide a list of specific medical conditions that would qualify as an exception.
“Exceptions do not exist. They are a lie. They don’t exist in practice,” said Lauren Miller, another plaintiff in the Zurawski case.
“We just shouldn’t be in a situation where there is a defined point at which your bodily autonomy is forfeited to the state,” Miller added. “People’s lives are on the line.”
Miller, who is from Dallas, was excited when she learned she was pregnant with twins in September 2022. But at 12 weeks’ gestation, she found out that one twin had trisomy 18, a life-threatening condition that also threatened the health of Miller and the other fetus.
She ended up in the emergency room with severe vomiting and dehydration, which put her at risk of organ damage, but doctors would not perform an abortion to remove the affected twin. She traveled nearly 800 miles and spent thousands of dollars to get care in Colorado. In March 2023, she gave birth to her son, Henry.
“We’ve seen so many elections now that are decided on very thin margins, and every vote matters,” Miller said.
Amanda Zurawski, the lead plaintiff in the lawsuit, vowed that “from now until November, I am dedicating all of my time, all of my energy into re-electing President Biden and Vice President Harris.”
Zurawski quit her job to become a campaign surrogate for Biden.
“Frankly, I’m terrified at what would happen if Trump makes his way back to the White House,” she said.
Zurawski was denied an abortion after her water broke at 18 weeks — far too early for a baby to survive. Zurawski wanted to leave the state to end the pregnancy, but doctors warned her that she was likely to get an infection and should not be more than 15 minutes from a hospital.
After her condition deteriorated, doctors performed an emergency abortion. Zurawski then developed sepsis and spent three days in intensive care.
The Texas Supreme Court noted in its Zurawski ruling that abortions can be allowed in cases where a patient’s water breaks before the point of fetal viability, since that often leads to infection. That’s cold comfort to Zurawski now.
“I have to use a surrogate now because of what happened to me. The damage to my reproductive organs is permanent,” Zurawski said.
Now, she added, protecting reproductive rights “is the most important thing in the world to me.”
Laura Jarrett is a senior legal correspondent for NBC News.
Elysee Barakett is a health intern at NBC News.
Advertisement
Justices Limit Power of Federal Agencies, Imperiling an Array of Regulations
A foundational 1984 decision had required courts to defer to agencies’ reasonable interpretations of ambiguous statutes, underpinning regulations on health care, safety and the environment.
- Share full article

By Adam Liptak
Reporting from Washington
- June 28, 2024
The Supreme Court on Friday reduced the power of executive agencies by sweeping aside a longstanding legal precedent, endangering countless regulations and transferring power from the executive branch to Congress and the courts.
The precedent, Chevron v. Natural Resources Defense Council , one of the most cited in American law, requires courts to defer to agencies’ reasonable interpretations of ambiguous statutes. There have been 70 Supreme Court decisions relying on Chevron, along with 17,000 in the lower courts.
The decision is all but certain to prompt challenges to the actions of an array of federal agencies, including those regulating the environment, health care and consumer safety.
The vote was 6 to 3, dividing along ideological lines.
“Chevron is overruled,” Chief Justice John G. Roberts Jr. wrote for the majority. “Courts must exercise their independent judgment in deciding whether an agency has acted within its statutory authority.”
In dissent, Justice Elena Kagan said the ruling amounted to a judicial power grab. “A rule of judicial humility,” she wrote, “gives way to a rule of judicial hubris.”
Justice Kagan summarized her dissent from the bench, a rare move and a sign of profound disagreement. “Courts, in particular this court, will now play a commanding role” in setting national policy, she said.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

IMAGES
VIDEO
COMMENTS
The case studies are contained in 4 categories: Family (13 case studies), Fundamentals and Mental Health (14 case studies) and Medical Surgical (20 case studies). In addition the folder labeled minireviews contains PowerPoint sessions with combinations of case studies and standalone items. ... The MNWC was founded in July 2018 by a Nurse ...
Comparative multiple case study design: Adult borderline personality disorder services, community. Netherlands. Caseloads of nurses approached in random order. ... As per the inclusion criteria, all studies targeted the relationship between mental health nursing staff and service users, although there were a range of additional criteria. The ...
The case study is an effective teaching strategy that is used to facilitate learning, improve critical thinking, and enhance decision-making Sprang, (2010). Below are nine case studies that educators may employ when working with students on mental illness and addiction. The case studies provided cover major concepts contained in the RNAO Nurse ...
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
This state-of-the-evidence review summarizes characteristics of intervention studies published from January 2011 through December 2015, in five psychiatric nursing journals. Of the 115 intervention studies, 23 tested interventions for mental health staff, while 92 focused on interventions to promote the well-being of clients.
Mental illness can be defined as clinically significant impairment in social, conceptual, and practical functioning. 9,10 Although very common, mental illness is often untreated. 11 One in five adults will have some experience with mental illness each year, but less than half will receive treatment. 11. Nursing has a hidden culture of stigma ...
This case study aims to describe the implementation of the decision-making process in mental health nursing given the care needs identified in a person with Alzheimer's disease at home. The cognitive assessment, supported by the cognitive decision algorithm, revealed that the patient presented moderate dementia, with visuospatial disorganization, memory changes, orientation, evocation, and ...
1.1. Background. Based on Peplau's model of interpersonal relationships by (), which is the most widely held theory in the mental health nursing community, many authors have based their models on person‐centred mental health nursing (Barker & Buchanan‐Barker, 2010; O'Brien, 2001; Scanlon, 2006).All of them identify the therapeutic relationship as the foundation of nursing practice and the ...
Journal of Psychiatric and Mental Health Nursing is a bimonthly mental health journal publishing research relevant to psychiatric nursing and mental ... Case studies provide researchers with the opportunity to gain an intimate understanding of a person's conditions, thoughts, actions, interventions and environment (Stake, 2005; Yin, 2014). 2.1 ...
The mere opportunity to discuss one's opinions and interpretations or different health concerns with a nurse may have the effect of unlocking patients' mental resources. This article demonstrates particularly how unconditional acceptance and facilitation of participation can be used in interpersonal counseling [see ( van Ryn and Heaney, 1997 )].
Mental health nursing is acknowledged internationally as being a demanding profession due to workplace ... highlighted that 13.7% of MHN were at high risk of developing PTSD following a case of completed suicide among a large cohort (n = 292) of ... International Journal of Nursing Studies, 52, 1412-1422. [PMC free article ...
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
Chapter 1: Psychiatric-mental Health Nursing and Evidence-based Practice, Case Studies Chapter 2: Mental Health and Mental Disorders: Fighting Stigma and Promoting Recovery, Case Studies Chapter 3: Cultural and Spiritual Issues Related to Mental Health Care, Case Studies
nurse-patient relationship is one of the most important. a spects of mental health nursing, significantly improves. client outcomes, and can be developed by implementing. empathy, friendliness ...
Case Study 1. Teresa is a 32-year-old woman in your practice who frequently misses her appointments, and at other times shows up without an appointment, often in crisis. She currently uses alcohol and tobacco, and has started to use street drugs. As you have developed a therapeutic relationship with Teresa, you learn that she grew up in a ...
Case 5: Denise. Denise, a 19-year-old woman, has been admitted informally to an acute mental health ward; this is Denise's first admission. Denise was being treated for depression by her GP; prior to her admission Denise attempted to kill herself by cutting her wrists. Subsequently a short admission was arranged with the aim of devising a ...
OBJECTIVE. This study aimed to describe and analyze, from the perspective of human development, on-line. clinical case discussions among nursing students in. the Psychiatric Nursing course ...
Social work report: Background. Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke ...
ACE.S Unfolding Cases. An unfolding case is one that evolves over time in a manner that is unpredictable to the learner. New situations develop and are revealed with each encounter. Every ACE unfolding case uses the highly regarded unfolding case model developed for Advancing Care Excellence for Seniors (ACE.S). Each case includes the following:
Mental health nursing case study on Somatoform disorder with answers for nursing students to learn critical thinking. Somatoform Disorder Case Study (30 min) Watch More! Unlock the full videos with a FREE trial ... This nursing case study course is designed to help nursing students build critical thinking.
A Psychiatric Case Study. College of Nursing, Simmons University. NURS-335AC: Psychiatric and Mental Health Nursing. Professor Jennifer Livesley. March 28, 2022. The Psychiatric Assessment. This patient, an 83 year old white female was admitted on 3/04/2022. She is widowed and has one adult son who was appointed her guardian one month ago.
1.1. Background. Many nursing students hold negative assumptions about mental health practice, with fearful stigma and stereotypes [].They can often lack confidence in communicating with people with mental disorders and may be afraid to do or say something harmful [].However, discriminatory and negative attitudes can be addressed in specific anti-stigma interventions and ideally incorporated ...
Drawing from a policy dialog on the youth mental health crisis conducted by 4 American Academy of Nursing Expert Panels, we present approaches to the current increase in youth mental health problems. Included is emerging literature on building youth resilience, particularly via re-establishing school and community connections. ...
Counseling and Mental Health Center. Providing mental health support through assessment and referral, group and individual counseling, psychiatry, and well-being services to the students of UT Austin. Student Services Building, 5th floor 100 West Dean Keeton Street. 8 a.m. - 5 p.m. Monday - Friday Main Line: 512-471-3515. 24/7 Crisis Line: 512 ...
Background Work hours are an important aspect of one's job and these in turn have the potential to impact people's well-being. Much research investigating the link between working hours and well-being uses cross-sectional data. Longitudinal studies, especially those studying the same subjects changing their working time, can study the impact of work time more clearly. Using panel data ...
Assertive community treatment: an evidence-based model where people with mental health disabilities are treated by people trained in psychiatry, social work, nursing and other fields.
The Texas Supreme Court last month, in Zurawski v. State of Texas, ruled against a group of women who had sued after they were denied abortions despite serious health complications during ...
International Journal of Mental Health Nursing is a mental health journal examining trends and developments in mental ... highlighted that 13.7% of MHN were at high risk of developing PTSD following a case of completed suicide among a large cohort (n = 292 ... This study has implications for the attraction and retention of nurses in the MHN ...
The mental health crisis among young people is an emergency — and social media has emerged as an important contributor. ... Evidence from tobacco studies show that warning labels can increase ...
A foundational 1984 decision had required courts to defer to agencies' reasonable interpretations of ambiguous statutes, underpinning regulations on health care, safety and the environment.