
- Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130:1480-1491. Abstract
- Patient Reported Outcomes Measurement Information System (PROMIS). National Institutes of Health. http://www.nihpromis.org/ Accessed August 12, 2011.
- 3Brandt LJ, Chey WD, Foxx-Orenstein AE, et al. An evidence-based systematic review on the management of irritable bowel syndrome. Am J Gastroenterol. 2009;104:S1-S34.
- Bijkerk CJ, de Wit NJ, Muris JWM, Whorwell PJ, Knottnerus JA, Hoes AW. Soluble or insoluble fibre in irritable bowel syndrome in primary care? Randomised placebo controlled trial. BMJ. 2009;339:B3154-B3160. Abstract
- Atkinson W, Sheldon TA, Shaath N, Whorwell PJ. Food elimination based on IgG antibodies in irritable bowel syndrome: a randomised controlled trial. Gut. 2004;53:1459-1464. Abstract
- Shepherd SJ, Parker FC, Muir JG, et al. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence. Clin Gastroenterol Hepatol. 2008;6:765-771. Abstract
- Shah ED, Basseri RJ, Chong K, et al. Abnormal breath testing in IBS: a meta-analysis. Dig Dis Sci. 2010;55:2441-2449. Abstract
- Frissora CL, Cash BD. Review article: the role of antibiotics vs. conventional pharmacotherapy in treating symptoms of irritable bowel syndrome. Aliment Pharmacol Ther. 2007;25:1271-1281. Abstract
- Pimental M, Lembo A, Chey W, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22-32. Abstract
- Camilleri M, Chey WY, Mayer EA, et al. A randomized controlled clinical trial of the serotonin type 3 receptor antagonist alosetron in women with diarrhea, predominant irritable bowel syndrome. Arch Intern Med. 2001;161:1733-1740. Abstract
- Nyhlin H, Bang C, Elsborg L, et al. A double-blind, placebo-controlled, randomized study to evaluate the efficacy, safety, and tolerability of tegaserod in patients with irritable bowel syndrome. Scand J Gastroenterol. 2004;39:119-126. Abstract
- Drossman DA, Chey WD, Johanson JF, et al. Clinical trial: lubiprostone in patients with constipation-associated irritable bowel syndrome-results of two randomized, placebo-controlled studies. Aliment Pharmacol Ther. 2009;29:329-341. Abstract
- Pimentel M, Park S, Mirocha J, et al. The effect of a nonabsorbed oral antibiotic (rifaximin) on the symptoms of irritable bowel syndrome. Ann Intern Med. 2006;145:557-563. Abstract
- DuPont HL, Jiang ZD. Influence of rifaximin treatment on the susceptibility of intestinal gram-negative flora and enterococci. Clin Microbiol Infect. 2004;10:1009-1011. Abstract
- Yang J, Lee HR, Low K, et al. Rifaximin versus other antibiotics in the primary treatment and retreatment of bacterial overgrowth in IBS. Dig Dis Sci. 2008;53:169-174. Abstract
- Pimentel M, Morales W, Chua K, et al. Effects of rifaximin treatment and retreatment in nonconstipated IBS subjects. Dig Dis Sci. 2011;56:2067-2072. Abstract

Faculty and Disclosures
As an organization accredited by the ACCME, Medscape, LLC, requires everyone who is in a position to control the content of an education activity to disclose all relevant financial relationships with any commercial interest. The ACCME defines "relevant financial relationships" as financial relationships in any amount, occurring within the past 12 months, including financial relationships of a spouse or life partner, that could create a conflict of interest.
Medscape, LLC, encourages Authors to identify investigational products or off-label uses of products regulated by the US Food and Drug Administration, at first mention and where appropriate in the content.
Brooks D. Cash, MD
Professor, Uniformed Services University of the Health Sciences; Chief of Medicine, National Naval Medical Center, Bethesda, Maryland
Disclosure: Brooks D. Cash, MD, has disclosed the following relevant financial relationships: Served as an advisor or consultant for: Salix Pharmaceuticals, Inc.; Takeda Pharmaceuticals North America, Inc.; Ironwood Pharmaceuticals, Inc.; Prometheus Laboratories Inc. Served as a speaker or a member of a speakers bureau for: Salix Pharmaceuticals, Inc.; Takeda Pharmaceuticals North America, Inc.; Prometheus Laboratories Inc. Received grants for clinical research from: Salix Pharmaceuticals, Inc. Dr. Cash does intend to discuss investigational drugs, mechanical devices, biologics, or diagnostics not approved by the FDA for use in the United States. Dr. Cash does intend to discuss off-label uses of drugs, mechanical devices, biologics, or diagnostics approved by the FDA for use in the United States.
Shari Weisenfeld, MD
Scientific Director, Medscape, LLC
Disclosure: Shari Weisenfeld, MD, has disclosed no relevant financial relationships.

A 32-Year-Old Woman With IBS: Clinical Outcomes and the Use of Antibiotics
Case presentation.
SN is a 32-year-old white woman who presents with symptoms of recurrent abdominal pain and loose stools. She states that she has experienced these symptoms since adolescence, with periods of improvement and worsening over the years. She notes that her symptoms were most pronounced when she was in college, and they improved during her pregnancy with her first child 4 years ago. Over the past year, her symptoms have been occurring more frequently and with greater severity. She also has been increasingly bothered by bloating and distention over the past 6 months. The bloating seems to worsen with food intake, while the distention progresses throughout the day. When questioned about abdominal pain, she describes it as 7 (on a scale of 10) at its worst and seemingly related to defecation, with acute worsening immediately prior to defecation and significant improvement after defecation. She has loose stools approximately one third of the time and often will have 2-3 bowel movements per day.
Other than her gastrointestinal symptoms, she considers herself healthy. She has no chronic illnesses or prior surgeries. She had an uncomplicated pregnancy and a vaginal delivery 4 years ago (gravida 1, para 1). She has no family history of organic gastrointestinal diseases such as inflammatory bowel disease, malignancy, or celiac disease.
SN is employed part time at an accounting firm. She jogs 2-3 miles 3-4 times a week, tries to eat 4-6 servings of fruits and vegetables daily, and takes a daily multivitamin, which she has taken for many years.
Her weight and other vital signs are within normal limits: height 5'6", weight 120 lb, blood pressure 108/64 mm Hg, pulse 60 beats per minute, and respiratory rate 12 breaths per minute.
On physical examination, she is a well-developed, well-nourished woman in no acute distress. Her physical examination is notable for mild tenderness to palpation in the left lower quadrant, but there is no rebound tenderness, guarding, or other peritoneal signs. The remainder of the physical examination is unremarkable.
IBS Presentations
The hallmark symptoms of irritable bowel syndrome (IBS) are abdominal pain or discomfort associated with at least two of the following characteristics: (1) pain or discomfort associated with a change in the form of the stool; (2) pain or discomfort associated with a change in the stool frequency; and/or (3) the pain or discomfort is relieved with defecation. The above characteristics are a liberal translation of the Rome III criteria for IBS. [1] The reality of clinical practice is that IBS can have a wide variety of clinical presentations. In addition to the "classic" symptom complex mentioned above, patients will often complain of other abdominal or defecatory symptoms such as bloating, gas, a prominent gastrocolic reflex, flatulence, distention, mucous in bowel movements, a sense of incomplete evacuation, and straining required for defecation.
IBS typically can be classified into 1 of 3 major categories, defined by the predominant stool pattern: IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), and mixed IBS (IBS-M). Each subgroup accounts for about one third of IBS patient presentations, although the percentage of each subtype may vary depending upon geography and patient population. [1]
Treatments and Clinical Trials
Treatment for IBS is typically directed at improving individual symptoms. For IBS-C this usually involves laxative therapies, and for IBS-D this usually involves antidiarrheal medications. Antispasmodic medications have long been used to target the pain and discomfort that patients often experience with IBS; however, there is no compelling evidence from clinical trials performed in the United States to support their use. Other common pharmacologic therapies prescribed for IBS include antidepressants, probiotics, and antibiotics.
Just as therapy is often directed at specific symptoms, patient response in clinical practice is typically dependent on changes in those symptoms and can be highly variable. This is in contrast to the many clinical trials of therapies for IBS, where changes in composite or global symptom measures are used to assess therapeutic efficacy. It is important for clinicians to understand the differences between measures of efficacy in clinical trials and the individual responses seen in practice, while also recognizing the wide-ranging global effects of IBS on the lives of their patients so that they can move beyond simply asking about individual symptoms (Figure 1).
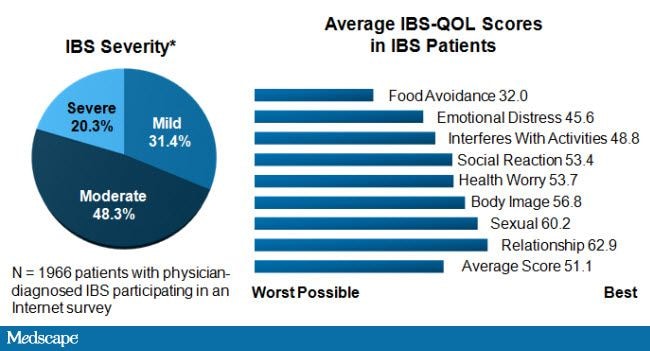
Figure 1. IBS profoundly affects QOL. Adapted from International Foundation for Functional Gastrointestinal Disorders; IBS patients: their illness experience and unmet need. Milwaukee, WI: International Foundation for Gastrointestinal Disorders; 2009.
IBS is a very subjective condition, without reliable biomarkers to help make the diagnosis or follow response to therapy, which has made developing clinical trial endpoints a difficult endeavor. Some trials evaluate the effects of therapy on individual IBS symptoms, while others use composite IBS scores or global IBS symptoms as their measure of efficacy. Still others use physiologic, rather than clinical, endpoints. Over the last decade, the US Food and Drug Administration (FDA) has favored a global endpoint for phase 3 clinical trials. It remains unclear if this is the optimal approach, especially because so much of the routine clinical practice surrounding IBS is directed at alleviating the individual symptoms patients experience.
In recent years, the National Institutes of Health has embarked on developing improved measures for patient-reported outcomes. The Patient Reported Outcome Measurement Information System (PROMIS®) aims to provide clinicians and researchers access to efficient, precise, valid, and responsive adult- and child-reported measures of health and well-being. [2] The stated strategic goals of this program are to (1) create and promulgate a set of qualitative and quantitative methodological standards for development and validation of instruments; (2) launch a sustainable entity that is able to promote the research, development, and dissemination activities for the network; (3) identify and prioritize a set of research and development opportunities that include clinical applications; and (4) disseminate information in order to forge strategic alliances to enhance the adoption of these standards in research, clinical practice, and policy. Currently, investigators from the University of California, Los Angeles, are working on a project under this program to develop and test a "gastrointestinal distress scale" that may have significant applicability for future IBS clinical trials.
Perhaps because IBS is such a heterogeneous disorder, there is no single therapeutic approach that has proven to be the de facto "first-line" treatment strategy. Generally, the aim of treatments for conditions that do not result in long-term health sequelae or impaired life expectancy, such as IBS, is to minimize the costs and possible adverse effects of therapies.
Multiple studies have considered the effects of nonpharmacologic therapies for IBS as well, including fiber supplementation or bulking agents, food-restriction diets, and psychological/cognitive behavior-based treatments. Among these 3 categories, psychological therapies have the best evidence supporting their use.
Bulking agents have traditionally been felt to be ineffective therapies for IBS. [3] However, Bijkerk and colleagues recently compared psyllium, bran, and a rice-flour placebo among patients with IBS and found that the percentage of patients responding, defined as adequate symptom relief, was significantly greater than placebo in the first (primary endpoint) and second months of therapy. Additionally, treatment with bran 10 g/day was also significantly better than placebo during the third month of treatment. [4]
Dietary restriction has been used by many patients with IBS in order to minimize gastrointestinal symptoms. Typically this includes limiting foods containing dairy sugars such as lactose, foods containing gluten, and most recently limiting fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs). Examples of FODMAPs include fructose and lactose, sorbitol, fructans, and raffinose, which humans do not express suitable hydrolases for and thus are always poorly absorbed. There are a number of studies that support FODMAP-restricted diets. In one study, 150 outpatients with IBS were randomly assigned to 3 months of a diet excluding all foods for which they had elevated immunoglobulin G antibodies (enzyme-linked immunosorbent assay test) or a sham diet excluding the same number of foods but not those to which they had antibodies. [5] After 12 weeks, the true diet resulted in a 10% greater reduction in symptom score than the sham diet (mean difference of 39.95% [95% confidence interval (CI), 5-72]; P = .024) and a 26% greater reduction in fully compliant patients (difference 98.95% [95% CI, 52-144]; P < .001). Global rating also significantly improved in the true-diet group as a whole ( P = .048, number needed to treat [NNT] = 9) and even more in compliant patients ( P = .006, NNT = 2.5). All other outcomes showed trends favoring the true diet, and relaxing the diet led to a 24% greater deterioration in symptoms in those on the true diet (difference 52 [95% CI, 18-88]; P = .003).
In another double-blinded, randomized, controlled trial, 25 patients who had responded to dietary change consisting of a FODMAP-restricted diet were rechallenged with reintroduction of fructose, fructans, alone or in combination, or glucose for a maximum test period of 2 weeks. [6] Approximately 70% of patients receiving fructose, 77% receiving fructans, and 79% receiving a mixture were not adequately controlled compared with 14% receiving glucose ( P ≤ .02). FODMAP-restricted diets can be difficult to adhere to; however, in patients with IBS and fructose malabsorption, dietary restriction of fructose and/or fructans may improve symptoms and is a reasonable treatment option.
Another therapeutic strategy for IBS has emerged from investigations on the origins of IBS symptoms from the interaction of enteric bacteria with ingested carbohydrates. This theory has been popularized by multiple reports demonstrating that patients with IBS are more likely than non-IBS controls to have abnormal breath tests after ingestion of fermentable carbohydrates. [7] Furthermore, studies have demonstrated that normalization of breath tests with antibiotic therapy may be accompanied by an improvement in IBS symptoms. These observations have led to multiple trials using antibiotic therapy for IBS. [8] This area of research recently culminated with the publication of the TARGET 1 and 2 trials in the New England Journal of Medicine . [9] This report of the effects of antibiotic therapy for IBS by Pimentel and colleagues represents a major addition to the IBS therapy literature and details the results of 2 identical trials for nonconstipated IBS. Both of these large studies (n = 623 for TARGET 1; n = 637 for TARGET 2) were conducted in multiple sites throughout the United States and Canada and enrolled patients with mild to moderate symptoms of nonconstipation IBS according to the Rome II IBS diagnostic criteria. After a 1- to 2-week screening phase to confirm eligibility requirements, patients were randomly assigned via concealed allocation to receive either rifaximin or placebo, in a 1:1 ratio. After completing the 14-day treatment period, patients were evaluated for 10 additional weeks, in order to monitor the short-term durability of treatment effects and symptoms. Efficacy assessments were obtained daily by means of an interactive voice-response system over the course of the entire study and a clearly defined endpoint, adequate relief of global IBS symptoms for at least 2 of the 4 weeks during the primary evaluation period based on a binary response to a yes/no question. A key secondary endpoint, satisfactory relief of bloating, was assessed in a similar fashion as the primary endpoint over the same period of time.
In both studies, patients consistently fulfilled the criteria for relief of global IBS symptoms and bloating (Figure 2). A statistically significant proportion of patients randomly assigned to the rifaximin group, compared with those who received placebo, had adequate relief of global IBS symptoms (41% vs 32% pooled data, P < .001) and bloating (40% vs 30% pooled data, P < .001) for at least 2 of the first 4 weeks of the treatment assessment period. Moreover, these results were durable, with statistically significant differences favoring rifaximin for the relief of global symptoms and bloating through the10-week post-treatment observation period. Other important individual symptoms of IBS were assessed, including abdominal pain and stool consistency, and these endpoints were also more likely to improve with rifaximin compared with placebo. No clinically significant differences were observed in terms of treatment-emergent adverse events between patients in either treatment arm.
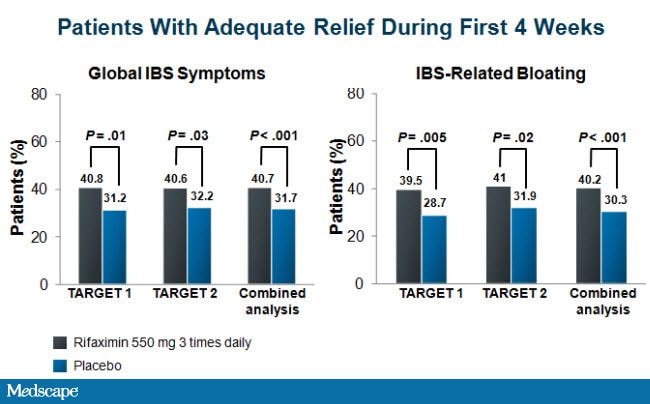
Figure 2. Efficacy of rifaximin in improving global IBS symptoms and IBS-related bloating. Adapted from Pimental M, et al. N Engl J Med . 2011;564:22-32. [9]
Clinical experience has demonstrated that rifaximin can significantly improve the gastrointestinal symptoms of some IBS patients. These results from the 2 large and well-designed clinical trials described offer convincing evidence that results that have been observed anecdotally for the last several years are in fact consistent and reproducible. The differences observed for the primary and secondary endpoints between rifaximin and placebo, while only 9%-10%, were similar to treatment differences observed in other phase 3 clinical trials of medications that have received FDA approval as therapies for IBS such as alosetron, tegaserod, and lubiprostone. [10-12]
The promising results of TARGET 1 and TARGET 2, however, do not completely resolve the issues surrounding the use of antibiotics for IBS. One of the most important questions remaining is the optimal means to identify probable responders. Some have suggested that breath test evidence of small intestinal bacterial overgrowth (SIBO) should be used as a treatment criterion, but previous studies of antibiotic therapy for IBS have not convincingly demonstrated a strong correlation between normalization of breath tests and clinical response. [13] As a practical matter, many clinicians have used positive breath tests to obtain third-party reimbursement for rifaximin, which is an expensive medication in the 1200- to 1650-mg doses used for IBS. Another question surrounding the use of antibiotics and probiotics for IBS is exactly how they are exerting an effect on the gastrointestinal tract of patients with IBS who respond to these therapies. Popular theories hold that these medications may decrease the density of fermenting bacteria in the small bowel, but there are other theories, such as anti-inflammatory effects that lead to alterations in enteric motility, secretion, and sensitivity, which have been put forth as possible explanations. Another concern surrounds the possibility of resistance, but there are abundant data in the literature demonstrating the safety of nonabsorbed antibiotics with respect to this issue. [14] Another issue, one that was raised by the FDA in their review of the clinical trial data during the approval deliberations for rifaximin, is the durability of response. While treatment differences between rifaximin and placebo persisted throughout the conclusion of the 12-week study period, a gradual diminution of the relief of global IBS symptoms and bloating was observed in both groups as the trial progressed. This observation mirrors community-based clinical experience. While there can be a dramatic response in some patients, symptom recurrence at a variable point after rifaximin appears to be common. Data on recurrence and retreatment effects with rifaximin, or any other antibiotic used for IBS, are crucial to obtain as there is very little guidance in the literature. What data that exist suggest that responders who experience recurrent IBS symptoms will respond to retreatment. [15,16]
Case Conclusion
Based on her long history of typical symptoms and lack of alarm features, SN is diagnosed with IBS. Her description allows for further categorization as IBS-D with prominent bloating. A complete blood count, thyroid studies, celiac sprue, and pregnancy testing are ordered. Based upon her age, lack of risk factors and alarm features, and intermittent loose stools, there was a discussion with the patient, and a decision was made not to perform colonoscopy at this time. SN is given educational material regarding IBS, including important Websites with IBS information like the International Foundation for Functional Gastrointestinal Disorders Website.
SN is anxious to avoid medications, and thus lifestyle modification with a FODMAP-restricted diet is prescribed. She returns 4 weeks later without symptom improvement, admitting that the diet was difficult to adhere to, particularly with other family members to consider. Her laboratory results are within normal limits. Rifaximin (550 mg 3 times a day for 14 days) is prescribed along with loperamide. SN is advised to begin with 2 mg of loperamide every morning and to increase by an additional 2 mg every week if her stool remains frequently soft and runny and to decrease to every other day should constipation occur.
SN returns after 4 weeks on this therapy and reports that her bloating and distention have almost completely resolved, her bowel habits are more predictable, and she has more solid stool. She reports occasional cramping and abdominal discomfort that signals the need to defecate, but this has been minimal and short lived. She does not want to pursue additional medical therapy at this time. She also has made some small changes to her diet like decreasing the amount and frequency of cruciferous vegetable and legumes she consumes, and she feels that this has helped her symptoms. She is advised about possible symptom recurrence over the next 6 months, especially bloating, and she has agreed to contact you for retreatment with rifaximin if she experiences a recurrence of symptoms.
Supported by an independent educational grant from Salix Pharmaceuticals.
The material presented here does not necessarily reflect the views of Medscape, LLC, or companies that support educational programming on www.medscape.org. These materials may discuss therapeutic products that have not been approved by the US Food and Drug Administration and off-label uses of approved products. A qualified healthcare professional should be consulted before using any therapeutic product discussed. Readers should verify all information and data before treating patients or employing any therapies described in this educational activity.
Medscape Education © 2011 Medscape, LLC

- Case report
- Open access
- Published: 03 August 2021
Pain and psyche in a patient with irritable bowel syndrome: chicken or egg? A time series case report
- Felicitas Engel 1 ,
- Tatjana Stadnitski 2 ,
- Esther Stroe-Kunold 1 ,
- Sabrina Berens 1 ,
- Rainer Schaefert 1 , 3 &
- Beate Wild ORCID: orcid.org/0000-0002-2279-8135 1
BMC Gastroenterology volume 21 , Article number: 309 ( 2021 ) Cite this article
2571 Accesses
3 Citations
1 Altmetric
Metrics details
Irritable bowel syndrome (IBS) appears to have a bidirectional interaction with both depressive and anxiety-related complaints. However, it remains unclear how exactly the psychological complaints, at the individual level, are related to somatic symptoms on a daily basis. This single case study investigates how somatic and psychological variables are temporally related in a patient with irritable bowel syndrome.
The patient was a woman in her mid-twenties with an IBS diagnosis. She reported frequent soft bowel movements (5–6 times per day), as well as flatulence and abdominal pain. She resembled a typical IBS patient; however, a marked feature of the patient was her high motivation for psychosomatic treatment as well as her willingness to try new strategies regarding the management of her symptoms. As an innovative approach this single case study used a longitudinal, observational, time series design. The patient answered questions regarding somatic and psychological variables daily over a period of twelve weeks with an online diary. The diary data was analysed using an autoregressive (VAR) modeling approach. Time series analyses showed that in most variables, strong same-day correlations between somatic (abdominal pain, daily impairment) and psychological time series (including coping strategies) were present. The day-lagged relationships indicated that higher values in abdominal pain on one day were predictive of higher values in the psychological variables on the following day (e.g. nervousness, tension, catastrophizing, hopelessness). The use of positive thinking as a coping strategy was helpful in reducing the pain on the following days.
In the presented case we found a high correlation between variables, with somatic symptoms temporally preceding psychological variables. In addition, for this patient, the use of positive thoughts as a coping strategy was helpful in reducing pain.
Peer Review reports
Irritable bowel syndrome (IBS) is characterized by recurrent abdominal pain that is associated with a change in frequency or form (appearance) of stool and can be related to defecation [ 1 ]. Currently, the symptom pattern is not sufficiently explained by peripheral organ pathology. IBS affects about 8% of the European population [ 2 ] and is most recently understood as a disorder of (microbiota-) gut-brain interaction [ 3 , 4 ] with a multifactorial origin that includes biological, psychological, and social factors [ 5 ]. Many patients who suffer from IBS also suffer from comorbid depressive or anxiety-related disorders [ 5 ]. Mood and anxiety disorders can precede or follow an IBS diagnosis due to the high discomfort caused by IBS [ 6 , 7 , 8 ]. By looking at specific psychological variables it was found that catastrophizing is directly associated with IBS symptom severity, while anxiety is indirectly related to IBS symptom severity [ 9 ].
While population-based studies suggest that IBS has a bidirectional interaction with both depressive and anxiety-related complaints, it remains unclear how exactly the psychological complaints, at the individual level, are related to somatic symptoms on a daily basis. Are increased psychological complaints (such as depression, tension, and nervousness) on one day preceded by IBS complaints on the previous day, or is it the other way around? A previous study showed that week-to-week stress and IBS symptoms were strongly cross-correlated in the same week, but were not temporally related across several weeks [ 10 ]. However, a day-by-day measure is needed to identify more fine-grained and direct relations. Furthermore, the focus of the study was on the mean values from a large patient sample, therefore potentially differing relationships in individual patients may not have been reflected in the aggregated data analysis.
Another interesting topic in patients suffering from IBS is the mutual relationship between coping strategies and IBS symptoms. A recent study reported that levels of coping resources were associated with gastrointestinal and extraintestinal symptom severity [ 11 ]. Also, catastrophizing and a lower self-perceived ability to reduce symptoms appeared to have a negative effect on health outcome in gastrointestinal disorders [ 12 ]. Interestingly, IBS patients have been reported to use passive coping strategies more frequently (such as escape-avoidance strategies instead of intended problem solving) compared to healthy controls [ 13 ]. Here too, the question arises to what extent coping strategies are related to IBS complaints and whether or not they are able to influence IBS complaints.
Overall, IBS symptoms and psychological distress are bi-directionally related, and coping strategies purportedly play an important role in the up- or down-regulation of IBS symptoms. However, individual mechanisms are not yet understood, and previous studies lack the longitudinal data on a day-by-day basis. Longitudinal data is necessary in order to obtain information about direct interactions, to better understand how temporal interactions between IBS symptoms and psychological complaints are related. As aggregated data can eliminate individual effects within the heterogeneous IBS patient sample, a single case study can provide important insights into specific mechanism to generate hypotheses for personalized clinical studies [ 14 ]. Conversely, inferences from singe case studies do not automatically apply to the patient population. However, results from single case studies can be used to generate hypotheses that can be examined in a sample of patients with similar characteristics.
This case study has, for the first time, applied a longitudinal time series design to a patient with IBS. Study objectives of this single-case analysis were: (1) to explore temporal relationships and interactions between the somatic and psychological complaints of the patient and (2) to investigate the impact of personal coping strategies on somatic symptoms.
Case presentation
Study design.
The study used a longitudinal, observational, single-case design. The study was approved by the medical ethics committee of the University Hospital Heidelberg. The patient was recruited in the frame of a pilot intervention study, conducted between July, 2014 and June, 2015 [ 15 ]. During her waiting period—and before the beginning of the therapy group—the patient answered questions daily regarding somatic and psychological complaints as well as coping strategies with the use of an online diary.
The diary data of the patient was collected following presentation in our outpatient specialty clinic for functional gastrointestinal disorders [ 16 ], and before group therapy. The data thereby showed the classic course of IBS without specific group intervention. The patient filled out the diaries from 10/2014 to 01/2015; over twelve weeks a total of 72 diary days were collected.
Measurements in the online diary
At the beginning of the study the patient received individual training in how to use the online diary; she was instructed to fill out the diary on a daily basis (between 4 pm and 12 am) via internet access. Validated questionnaires for IBS, as well as for psychological complaints and coping strategies, were used and adapted for the daily diary design. The most discriminating items of the questionnaires were derived in order to shorten the completion time of the diary (approximately 5–10 min). All items were rated by a visual analogue scale (VAS) with bipolar labels. The marked points were then converted by the computer program to a numeric scale ranging from 1 to 101. In addition, it was possible to enter a short free text in the diary.
For the measurement of somatic symptoms, we used the items “How severe is your abdominal (tummy) pain?” and “Please indicate how much your irritable bowel syndrome is affecting or interfering with your life today?”. Higher scores on these items reflected higher pain or higher somatic impairment. Psychological variables and coping strategies measured in the online diary are shown in Table 1 .
In January 2014, a German student (female in her mid-twenties), was referred to the outpatient specialty clinic of the University Hospital of Heidelberg for functional gastrointestinal disorders. She reported frequent soft bowel movements (5–6 times per day), as well as flatulence and abdominal pain. According to ROM-III [ 22 ] and the clinical assessment, an IBS (subtype IBS-diarrhea, IBS-D) was diagnosed. In addition, the patient was suffering from comorbid gluten, lactose, and sorbitol intolerance. No mental illness was present. Despite professional nutritional advice that included a gluten-, lactose- and sorbitol-reduced diet, gastrointestinal complaints persisted. In the course of the three-month follow-up appointments that included multimodal treatment [ 16 ] (04/2014, 07/2014, 11/2014), the patient correlated intestinal complaints and stress. She reported, for example, that the intestinal symptoms increased at the beginning of the semester and in the examination period. In the course of the diary study the patient did not describe any long-lasting stressor (such as an examination phase), but rather shorter week- or day-specific stressful events (such as Christmas holidays or looking for a part-time job) associated with an onset of IBS-symptoms on the same day. As an additional stressor, she described shame and the fear of a recurrence of the IBS complaints (particularly of soft bowel movements and flatulence), especially in social settings and situations where she could not easily reach a toilet. Relaxation techniques (yoga and gut-directed hypnosis using a CD) slightly improved her symptoms and the associated fear. Regarding the short stressful events, she described a good improvement of symptoms when using a strategy of calming down, with no further subsequent exacerbation. After the online diary study presented here, the patient received a group intervention [ 15 ] from which she has benefited.
In conclusion, according to IBS symptoms, symptom specific fears and avoidance behavior, the presented case of a young female patient resembled a typical IBS patient; however, a marked feature of the patient was her high motivation for psychosomatic treatment as well as her willingness to try new strategies regarding the management of her symptoms.
Statistical analysis
Initially, the following analyses were conducted for each time series: graphic examinations; calculations of descriptive statistics (range, median, mean, standard deviation), autocorrelation functions (ACF), and tests for stationarity with the Augmented Dickey–Fuller (ADF) procedure. Autocorrelation is the bivariate correlation of a time series with a lagged copy of itself. Therefore, instantaneous (lag = 0) autocorrelation is always equals one, significant autocorrelations on other lags imply predictability of the future time series values from the past values. Stability or instability as well as memory characteristics of time series can be inferred from their autocorrelation functions: non-zero autocorrelations at only a few lags are typical for stable short-memory processes, whereas significant autocorrelations on many lags indicate long memory or instability. Stationarity means that the statistical characteristics of a process under study do not change over time (e.g., exhibit no trends or distinct fluctuations of mean or variance). The Augmented Dickey-Fuller algorithms tests the null hypothesis “time series is stationary”.
In addition, cross-correlation functions (CCF), instantaneous correlations, and simultaneous regressions with psychological measures—both as dependent and somatic variables as predictors—were estimated. Cross-correlation measures similarity of two different time series as a function of the displacement of one relative to the other. Generally, instantaneous (lag = 0) correlations or simultaneous (lag = 0) regressions do not imply causation. For lagged correlations and regressions, however, it is different, since they explore the ability to predict the future values of a time series from prior values of another times series. The idea behind this is as follows: Since time does not run backwards, the cause cannot come after its effect. Therefore, events in the past can cause events to happen today, but future events cannot influence the present. The concept of Granger causality incorporates this idea: if lagged values of a time series X improve prediction of future values of a series Y, the former series Granger-causes the latter. For example, if lagged values of a somatic times series improve prediction of future values of a psychological one, the former series Granger-causes the latter. The vector autoregressive (VAR) methodology investigated the temporal dynamics between two or more time series by separating the time-lagged from the simultaneous relations. Therefore, temporal interdependencies between time series were analyzed using this approach. The VAR technique thereby allowed inferences about the temporal order of the effects by employing the temporal causality concept introduced by Granger. Furthermore, the VAR approach can handle time series that mutually influence each other and thus reveal feedback effects. In VAR modelling, interpretation of the regression coefficients is problematic because the lagged values of the dependent variables are used as predictors (i.e. dependent and independent variables are both endogenous, that is, determined and interrelated inside the organism or system), consequently, external influences can enter the autoregressive system exclusively through the residual term, which is also called “exogenous shock”. The behaviour of a VAR system can be modelled using impulse response analyses (IRA) and forecast error variance decompositions (FEVD). Impulse response functions (IRF) examine interdependencies within a VAR system by tracing the effect of an exogenous shock in one of the series on other variables. The FEVD estimates the amount of variance in each variable that can be explained by the other variables of the system during a specific period (h). For instance, in case of daily measurements, FEVD = 0.24 (h = 10) means that 24% of the forecast error variance in a dependent variable can be explained by exogenous shocks (random changes) of the predictors for a time horizon of 10 days.
The analyses were conducted using the R software. (Please consult Stadnitski & Wild (2019) and Stadnitski (2014, 2020) for descriptions, detailed explanations, and implementation of all analyses with the R software [ 23 , 24 , 25 ]).
Figure 1 visualizes the patient’s development of somatic symptoms, abdominal pain (AP), and daily impairment (DI) over 72 successive days together with their autocorrelation and cross-correlation function. In both series there appeared strong discomfort with values distinctly higher than 20 on 7 days. Almost 90% of the measurements varied between 1 and 20 on the 100-point scale. The average (Mean AP = 11.10, DI = 14.35) and variability (Standard Deviation: AP = 15.90, DI = 18.55) were higher for DI than AP (see also Table 2 ). Both time series exhibited no trends. Figure 2 shows the time series of additional psychological variables and coping strategies.
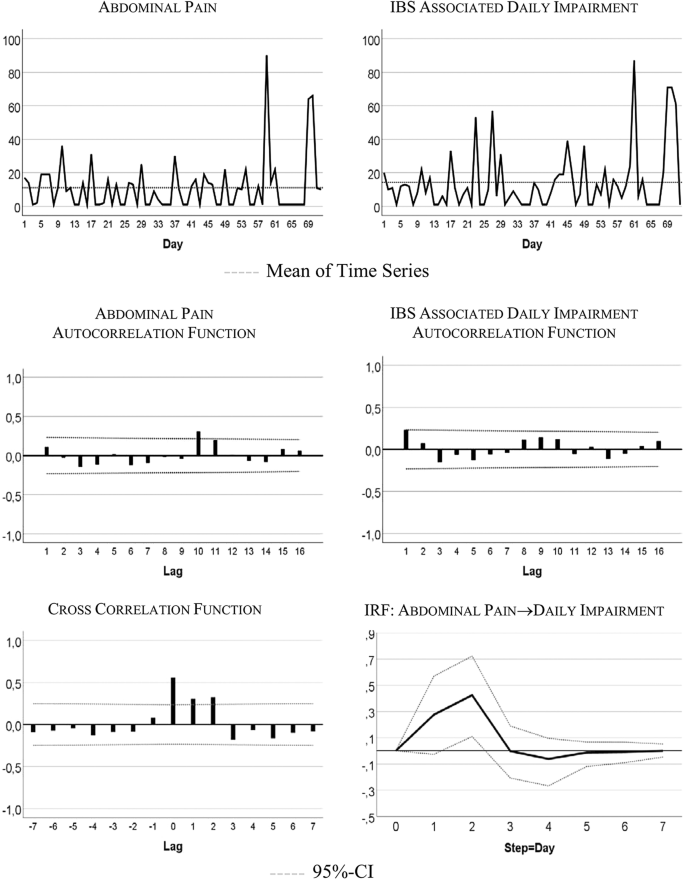
Somatic time series: abdominal pain (AP) and IBS-associated daily impairment (DI)
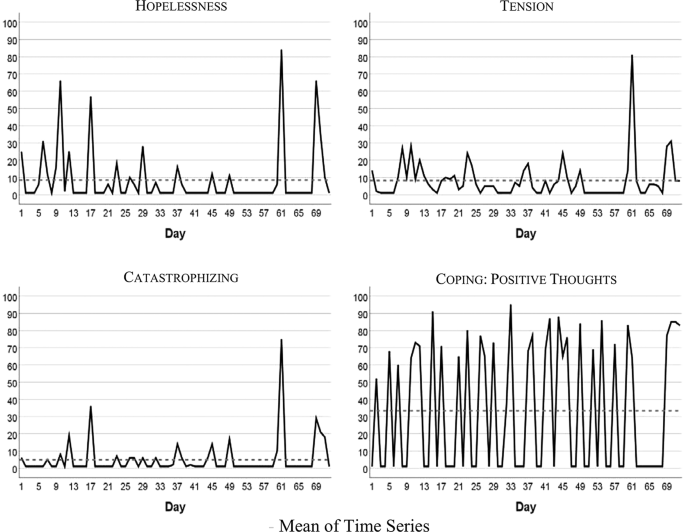
Time series of hopelessness, tension, catastrophizing, coping
The time series quantitatively reflect the free text descriptions of the patient. The highest scores in AP and DI were recorded between days 57 and 68 of the study period. In the free text passages of the diary the patient noted that she experienced the Christmas holidays (days 52–67) as a period of high stress and increased IBS pain. In addition, on days 59–61 she described the occurrence of menstrual cramps together with IBS-associated pain and impairment.
Table 2 summarizes characteristics of somatic and psychological and coping time series. In the majority of cases all of the series except “Coping with positive thoughts” (CPT) ranged between 1 and 20 on the 100-point scale, with high values observed about 10% of the time. CPT values alternated between very low and high with values equal on 1 out of 40 days, and values higher than 50 on 31 days. All series were stationary, i.e., exhibited no trends. Three series (tension, catastrophizing, and hopelessness) demonstrated no autocorrelations.
Table 3 shows instantaneous correlations between the somatic and psychological (including coping) time series. In most cases, strong and positive correlations were observed. Interestingly, the relationship between psychological and coping variables with DI was stronger than with AP. The amount of predicted variance (R 2 ) from linear regressions with psychological and coping measures as dependent variables and somatic variables as predictors varied between 12 and 94%. The non-significant correlation between depressiveness and abdominal pain could be due to the very limited range of the variable depressiveness over the course of the 72 days.
Table 4 summarizes the significant results of the VAR analyses for interdependencies between abdominal pain and psychological distress or coping strategies; only statistically significant findings from calculations for all possible combinations of variables are provided. Identified lagged or temporal relations showed mostly the same direction, indicating that previous values in the somatic variable (AP) were predictive of values in the psychological variables or coping strategies. The variance decomposition estimates show that somatic symptoms in the psychological (and coping) time series explain 12% to 41% of variability.
Figure 3 visualizes responses of psychological states and coping strategies to increases in AP; it shows that psychological and coping aspects reacted with higher symptoms to an increase in AP. For instance, increasing AP caused a strong delayed increase in catastrophizing: + 0.60 standard deviations, i.e., about 7 points on the 100-point scale.
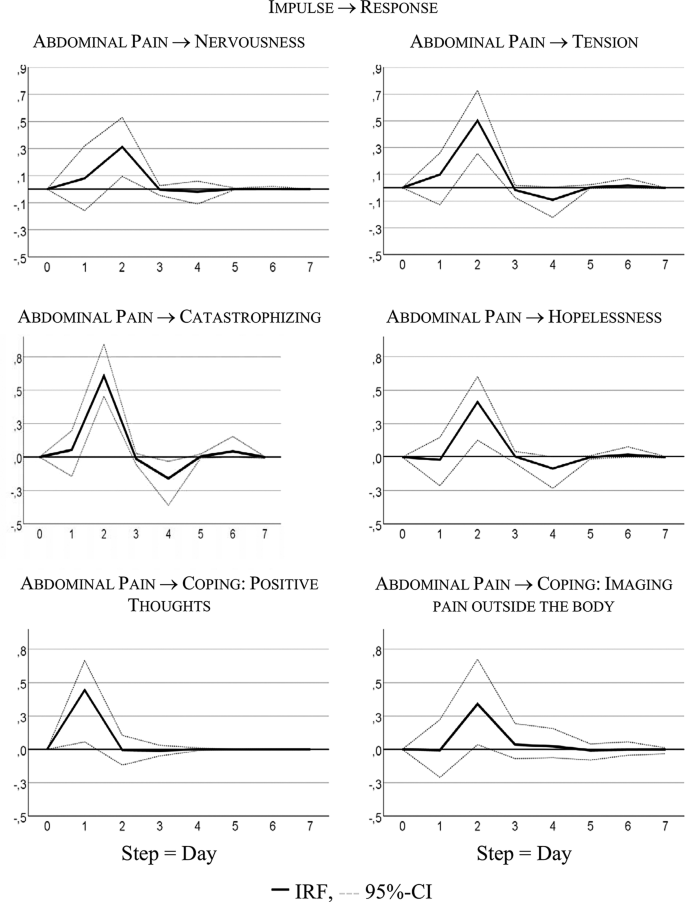
Time lagged psychological variables
Table 4 shows that the bivariate system, including AP and CPT, is characterized by a bidirectional or feedback predictive causality. AP Granger-caused CPT with 24% of explained variance, CPT Granger-caused AP with 6% of explained variance. Both series also correlated instantaneously: r = 0.43, R² = 18%.
Figure 4 visualizes the feedback relationship. An increase in AP caused more CPT next day. Intensified CPT resulted in less pain on the subsequent day: i.e., a decrease of 0.25 standard deviations, 4-point on the 100-point scale.
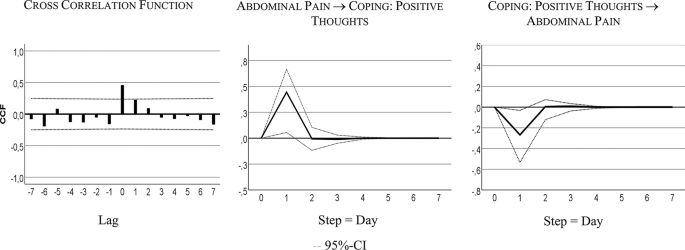
Cross-correlation and time lagged relationships: abdominal pain (AP) and coping with positive thoughts (CPT)
Discussion and conclusion
This is the first study to investigate the temporal relationships between somatic and psychological variables on a daily basis. We analyzed a female patient with IBS in her mid-twenties with symptoms of diarrhea, flatulence, and abdominal pain. She reported stress-related IBS symptoms as well as symptom related fears. In most variables, strong same-day correlations between somatic (especially daily impairment) and psychological (including coping) time series were observed. The day-lagged relationships indicated that higher values in abdominal pain on one day were predictive of higher values in psychological complaints (nervousness and tension) or of negative coping strategies (catastrophizing, hopelessness) on the following day. The use of positive thinking as a positive coping strategy was helpful in reducing the pain on the following days.
All variables remained stationary—that is, time series exhibited no trends over the measured time period (72 days). In the study period, the patient did not receive additional psychotherapeutic treatment, nor did she report long-lasting stressors. Therefore, we did not expect her symptoms to change over a longer period of time. The stability of IBS symptoms is supported by literature that usually describes IBS as a chronic disease. The diagnostic criteria for IBS also imply some symptom stability, because the symptoms must occur for a period of at least 3 months (with an onset at least 6 months prior the diagnosis) [ 22 ]. In addition, for IBS, population-based studies report a remission rate of about 55% only over a period of more than 10 years [ 26 ]. In addition to the general stationary trend of the variables, individual outliers with more severe symptoms were visible (e.g. the Christmas Holidays on days 52–67).
The patient stated that stressful or stress-free episodes would influence her symptoms; this was also reflected in the same-day analysis. In the free text of the diary the patient also described that in specific stressful situations she was ashamed of her symptoms and related consequences. The high same-day correlations between the somatic (AP, DI) and psychological time series (nervousness, tension, depressiveness, catastrophizing, hopelessness) reflect this interdependency—which the patient is aware of—between IBS symptoms and psychological state. Interestingly, this correlation was even higher for DI, meaning that functionality is especially important. The interaction between somatic and psychological distress is also described in previous studies. Midenfjord et al. (2019), for instance, showed in a cross-sectional study that IBS patients with psychological distress demonstrated more severe somatic symptoms and a lower quality of life [ 27 ]. Varni et al. (2017) found in a sample of pediatric patients with functional gastrointestinal disorders that somatic symptoms were differentially related to decreased health-related quality of life [ 28 ]. Another study reported a correlation between pain intensity and intensity of psychopathological symptoms (such as low spirits or anxiety) in IBS patients [ 29 ] while Dong et al. (2020) showed that IBS symptom severity predicted health-related quality of life influenced by stressful life events [ 30 ]. Interestingly, there is evidence that this association between current abdominal symptoms and psychological distress is not limited to functional gastrointestinal diseases but can also be seen in inflammatory bowel diseases [ 31 ]. The underlying physiological mechanism for the interaction between somatic and psychological distress could be explained by the concept of the (microbiome-) gut-brain axis. The (microbiome-)gut-brain axis refers to the complex network of connections between the microbiota, the enteric nervous system, and the central nervous system. [ 3 , 4 , 32 , 33 ]. Previous research has shown that the link between gastrointestinal symptoms and psychological distress could be based on a complex and bidirectional interaction between biological, psychological, and social factors [ 5 ]. For example, visceral hypersensitivity and an enhanced perceptual response to gastrointestinal sensations can trigger gastrointestinal specific anxiety [ 5 , 32 ]. On the other hand, psychosocial distress can lead, for instance, to an activation of the enteric and autonomic nervous system, which may trigger a change in smooth muscle activity or glandular secretion thus leading to IBS-symptoms. [ 32 ].
In addition to the daily correlation, it is also useful to look at day-to-day relationships in order to make time-delayed effects more visible and to answer the question whether or not psychological complaints precede IBS complaints, or vice versa. In literature, both perspectives are described for mental illnesses and IBS [ 6 , 7 , 8 ]. However, for this particular patient we found a strong time-delayed relationship between IBS symptoms, the following psychological complaints (nervousness, tension), and negative coping strategies (catastrophizing, hopelessness). This shows that having abdominal pain on one day was associated with more psychological stress the next day, not vice versa. This is in line with another study showing the temporal relationship that abdominal symptoms lead to increased stress and negative affect, while increased daily life stressors even lowered the IBS-symptoms [ 34 ]. This is interesting, as in literature frequently the opposite temporal direction or a feedback-loop is assumed [ 35 ]. Patel et al. (2016), for instance, investigated the relationship between sleep, mood and somatic symptoms in a sample of IBS patients and healthy controls over the course of 7 days [ 36 ]. In IBS patients, sleep disturbances were predictive for abdominal pain on the following day. Additional analyses showed that the sleep effects on abdominal pain in IBS patients could be mediated by depression and anxiety [ 36 ].
The question arises why our data show that the patient first develops gastrointestinal complaints and only afterwards psychological complaints. The patient herself had the impression that increased stress would lead to an increase in symptoms. For instance, during the short stressful event of applying for a new job the patient reported an onset of IBS complaints. She also reported that in this case the immediate application of a coping strategy (such as calming down) had helped her to reduce the symptoms. However, this sequence occurred over the course of only several hours—and would thus be reflected in the high same-day correlations of the time series (and not in the day-lagged correlations). On the other hand, shorter time intervals had been tested in Chan's study with an outcome similar to ours [ 34 ]. It is also possible that shorter daily stressors could also lead to a distraction from the IBS-symptoms, while longer stressors (like Christmas Holidays in the case of our study) may lead to an increase in symptoms.
Another interesting approach to feelings and symptoms of IBS is the concept of alexithymia. This concept states, among others, that feelings in IBS-patients may be misinterpreted as negative bodily sensations [ 37 ]. For our patient, this could mean that in stressful situations (such as job search or exam phases) she may initially perceive her feelings only physically and interpret them as a preliminary stage of a new outbreak of her IBS. The hyper-focus on the symptoms could initially intensify them. Shortly afterwards, the patient may get negative feelings from the IBS symptoms themselves.
The time-lagged correlation between IBS complaints and the following psychological complaints and negative coping strategies could be related to the patient’s social anxiety and the pressure to perform. In the free text of the diary the patient described that with the occurrence of abdominal complaints she would fear that soft bowel movements would follow, and that she would not be able to reach a toilet in a timely manner; she also felt ashamed when she had to leave certain events because of her IBS symptoms. Physiologically, this relationship between IBS complaints and following psychological distress could again be explained by the (microbiome-)gut-brain axis [ 5 , 32 ]. The occurrence of abdominal complaints (maybe as an expression of visceral hypersensitivity) can trigger gastrointestinal specific anxiety and the autonomic nervous systems as well as the hypothalamic pituitary axis are sending stress signals to the gut, resulting, among others, in a higher bowel motility and secretion leading to diarrhea and pain [ 32 ].
Interestingly, abdominal pain was not associated with a depressive feeling in general, but with negative processing (such as hopelessness and catastrophizing) as well as tense or anxious arousal (nervousness, tension). These negative feelings and coping strategies had no effect on the patient’s increased abdominal pain the next day; in contrast, the use of positive coping strategies was helpful.
The patient reported using positive coping strategies to reduce her symptoms; this was also seen in the data analysis. The intensified use of a specific coping strategy on one day (thinking of things the patient enjoyed doing) was followed by a decrease in pain on the subsequent day. Conversely, an increase in pain was followed by an increased use of this coping strategy. This corresponds to the clinical impression and the self-report of the patient: She considered relaxation techniques and new coping strategies such as distraction as beneficial for her condition. This result is supported by literature that considers psychotherapeutic treatment, including positive coping strategies, as a possible treatment of IBS [ 38 ].
In summary, the results of the time series analysis partly reflect the self-report of the patient as well as the clinical impression of the outpatient caretaker. However, our results expand upon these insights by showing temporal relationships between IBS symptoms and psychological variables over consecutive days—with psychological changes following changes in abdominal pain and related impairment. In addition, a mutual day-lagged relationship between IBS symptoms and coping could be detected.
This study has several implications: Overall, it shows that at the very least this patient is aware of her individual process of personal change, her fears, and her coping strategies––all of which to a large extent, could be confirmed by the time series analysis––an analysis that also provided additional information. This supports the hypothesis that individual characterizations are promising in terms of providing a better understanding of specific mechanisms, as well as an understanding of how temporal interactions between IBS symptoms and psychological symptoms are related. In clinical practice, practitioners should consider individual explanatory models of aggravating factors and coping strategies and stay open to psychosomatic as well as somatopsychic mechanisms. Previous psychological treatment recommendations for IBS patients concluded that a change in illness-specific cognitions as well as gastrointestinal anxiety as key mechanisms may have an effect on the outcomes of IBS symptom severity and quality of life [ 39 ]. In this case study, only positive thinking had a time-lagged effect on a decrease in abdominal pain, while catastrophizing and hopelessness were a result of having abdominal pain previously. Although it is not possible to generalize the results of an individual case, this supports the fact that treatments which more directly target abdominal symptoms (e.g., hypnotherapy) may have promising effects on IBS symptoms as well as associated psychological complaints. Therefore, a disorder-oriented integrative group intervention for IBS with gut-directed hypnotherapy seems promising [ 15 ].
From a methodological point of view, we have to point out that the here applied concept of Granger-causality does not equal causality. Causality according to Hill [ 40 ] can be assessed by using the following 9 criteria: strength, consistency, specificity, temporality, biological gradient, plausibility, coherence, experiment, analogy. The definition of Granger-causality, however, implies only that previous values of a time series X (e.g. somatic symptoms) improve prediction of future values of another series Y (e.g. nervousness of the patient). It does not imply the causality of X for Y.
Our study has several limitations. Firstly, we examined only one patient suffering from IBS; the generalizability of the results is therefore limited. We cannot simply transfer the results to other IBS patients but must carefully investigate further patient samples in regard to temporal relationships and interactions between somatic and psychological variables. Secondly, we were able to detect day-to-day changes only; shorter periods of time could not be captured. Nevertheless, previous studies mainly focused on longer time periods which is why this approach is still more advantageous in terms of capturing the direct relationships. Nevertheless, we were able to show a clear picture of a single IBS-patient. This is helpful as IBS is a complex illness with, in all likelihood, heterogeneous genesis and factors. A comprehensive case study could help identify subclasses of IBS to arrive at a better treatment and avoid dilution effects.
In conclusion we found in the presented case that somatic symptoms temporally precede psychological complaints. In addition, for this patient, the use of positive thoughts as a coping strategy was helpful in reducing pain. Further analyses should be conducted to verify if these relationships can be found in other patients who suffer from IBS symptoms.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Irritable bowel syndrome
Abdominal pain
IBS-associated daily impairment
Nervousness
Depressiveness
Pain-associated discomfort
Catastrophizing
Hopelessness
Coping with positive thoughts
Coping with imagining pain outside the body
Schmulson MJ, Drossman DA. What is new in Rome IV. J Neurogastroenterol Motil. 2017;23(2):151–63.
Article Google Scholar
Sperber AD, Dumitrascu D, Fukudo S, Gerson C, Ghoshal UC, Gwee KA, Hungin APS, Kang J-Y, Minhu C, Schmulson M. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review. Gut. 2017;66:1075-82.
Drossman DA, Hasler WL. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257–61.
De Palma G, Collins SM, Bercik P, Verdu EF. The microbiota-gut-brain axis in gastrointestinal disorders: stressed bugs, stressed brain or both? J Physiol. 2014;592(Pt 14):2989–97.
Van Oudenhove L, Levy RL, Crowell MD, Drossman DA, Halpert AD, Keefer L, Lackner JM, Murphy TB, Naliboff BD. Biopsychosocial aspects of functional gastrointestinal disorders: how central and environmental processes contribute to the development and expression of functional gastrointestinal disorders. Gastroenterology. 2016;150(6):1355–67.
Jones MP, Tack J, Van Oudenhove L, Walker MM, Holtmann G, Koloski NA, Talley NJ. Mood and anxiety disorders precede development of functional gastrointestinal disorders in patients but not in the population. Clin Gastroenterol Hepatol. 2017; 15(7):1014–1020 e1014.
Ford AC, Forman D, Bailey AG, Axon AT, Moayyedi P. Irritable bowel syndrome: a 10-yr natural history of symptoms and factors that influence consultation behavior. Am J Gastroenterol. 2008;103(5):1229–39.
Koloski NA, Jones M, Talley NJ. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment Pharmacol Ther. 2016;44(6):592–600.
Article CAS Google Scholar
van Tilburg MA, Palsson OS, Whitehead WE. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. J Psychosom Res. 2013;74(6):486–92.
Blanchard EB, Lackner JM, Jaccard J, Rowell D, Carosella AM, Powell C, Sanders K, Krasner S, Kuhn E. The role of stress in symptom exacerbation among IBS patients. J Psychosom Res. 2008;64(2):119–28.
Wilpart K, Tornblom H, Svedlund J, Tack JF, Simren M, Van Oudenhove L. Coping skills are associated with gastrointestinal symptom severity and somatization in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2017;15(10):1565–71.
Drossman DA, Leserman J, Li Z, Keefe F, Hu YJ, Toomey TC. Effects of coping on health outcome among women with gastrointestinal disorders. Psychosom Med. 2000;62(3):309–17.
Jones MP, Wessinger S, Crowell MD. Coping strategies and interpersonal support in patients with irritable bowel syndrome and inflammatory bowel disease. Clin Gastroenterol Hepatol. 2006;4(4):474–81.
Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D, Group C. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014;67(1):46–51.
Berens S, Stroe-Kunold E, Kraus F, Tesarz J, Gauss A, Niesler B, Herzog W, Schaefert R. Pilot-RCT of an integrative group therapy for patients with refractory irritable bowel syndrome (ISRCTN02977330). J Psychosom Res. 2018;105:72–9.
Berens S, Kraus F, Gauss A, Tesarz J, Herzog W, Niesler B, Stroe-Kunold E, Schaefert R. A specialty clinic for functional gastrointestinal disorders in tertiary care: concept and patient population. Clin Gastroenterol Hepatol. 2017;15(7):1127–9.
Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11(2):395–402.
Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66.
Robinson ME, Riley JL, Myers CD, Sadler IJ, Kvaal SA, Geisser ME, Keefe FJ. The Coping Strategies Questionnaire: a large sample, item level factor analysis. Clin J Pain. 1997;13(1):43–9.
Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–91.
Stadnitski T. Multivariate time series analyses for psychological research: VAR, SVAR, VEC, SVEC models and cointegration as useful tools for understanding psychological processes. Hamburg: Dr. Kovač; 2014.
Stadnitski T, Wild B. How to deal with temporal relationships between biopsychosocial variables: a practical guide to time series analysis. Psychosom Med. 2019;81(3):289–304.
Stadnitski T. Time series analyses with psychometric data. PLoS ONE. 2020;15(4):e0231785.
Olafsdottir LB, Gudjonsson H, Jonsdottir HH, Bjornsson E, Thjodleifsson B. Natural history of functional gastrointestinal disorders: comparison of two longitudinal population-based studies. Dig Liver Dis. 2012;44(3):211–7.
Midenfjord I, Polster A, Sjovall H, Tornblom H, Simren M. Anxiety and depression in irritable bowel syndrome: Exploring the interaction with other symptoms and pathophysiology using multivariate analyses. Neurogastroenterol Motil. 2019;31(8):e13619.
Varni JW, Shulman RJ, Self MM, Nurko S, Saps M, Saeed SA, Patel AS, Dark CV, Bendo CB, Pohl JF, et al. Gastrointestinal symptoms predictors of health-related quality of life in pediatric patients with functional gastrointestinal disorders. Qual Life Res. 2017;26(4):1015–25.
Gorczyca R, Filip R, Walczak E. Psychological aspects of pain. Ann Agric Environ Med. 2013; Spec no. 1:23–27.
Dong Y, Baumeister D, Berens S, Eich W, Tesarz J. Stressful Life Events moderate the relationship between changes in symptom severity and health-related quality of life in patients with irritable bowel syndrome. J Clin Gastroenterol. 2020;54(5):445–51.
Berens S, Schaefert R, Baumeister D, Gauss A, Eich W, Tesarz J. Does symptom activity explain psychological differences in patients with irritable bowel syndrome and inflammatory bowel disease? Results from a multi-center cross-sectional study. J Psychosom Res. 2019;126:109836.
Tait C, Sayuk GS. The Brain-Gut-Microbiotal Axis: a framework for understanding functional GI illness and their therapeutic interventions. Eur J Intern Med. 2021;84:1–9.
Kennedy PJ, Cryan JF, Dinan TG, Clarke G. Irritable bowel syndrome: a microbiome-gut-brain axis disorder? World J Gastroenterol. 2014;20(39):14105–25.
Chan Y, So SH, Mak ADP, Siah KTH, Chan W, Wu JCY. The temporal relationship of daily life stress, emotions, and bowel symptoms in irritable bowel syndrome-Diarrhea subtype: a smartphone-based experience sampling study. Neurogastroenterol Motil. 2019;31(3):e13514.
Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features, and Rome IV. Gastroenterology. 2016; 150(6):1262–1279. e1262.
Patel A, Hasak S, Cassell B, Ciorba MA, Vivio EE, Kumar M, Gyawali CP, Sayuk GS. Effects of disturbed sleep on gastrointestinal and somatic pain symptoms in irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44(3):246–58.
Kano M, Endo Y, Fukudo S. Association between alexithymia and functional gastrointestinal disorders. Front Psychol. 2018;9:599.
Torkzadeh F, Danesh M, Mirbagher L, Daghaghzadeh H, Emami MH. Relations between coping skills, symptom severity, psychological symptoms, and quality of life in patients with irritable bowel syndrome. Int J Prev Med. 2019;10:72.
Windgassen S, Moss-Morris R, Chilcot J, Sibelli A, Goldsmith K, Chalder T. The journey between brain and gut: a systematic review of psychological mechanisms of treatment effect in irritable bowel syndrome. Br J Health Psychol. 2017;22(4):701–36.
Hill AB. The environment and disease: association or causation? Proc R Soc Med. 1965;58(5):295–300.
CAS PubMed PubMed Central Google Scholar
Download references
Acknowledgements
The authors thank the participating patient and the contributing research assistants.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Department of General Internal Medicine and Psychosomatics, University of Heidelberg, Im Neuenheimer Feld 410, 69120, Heidelberg, Germany
Felicitas Engel, Esther Stroe-Kunold, Sabrina Berens, Rainer Schaefert & Beate Wild
Department of Quantitative Methods in Psychology, University of Ulm, Albert-Einstein-Allee 47, 89081, Ulm, Germany
Tatjana Stadnitski
Department of Psychosomatic Medicine, Division of Internal Medicine, University Hospital Basel, Hebelstrasse 2, 4031, Basel, Switzerland
Rainer Schaefert
You can also search for this author in PubMed Google Scholar
Contributions
BW, FE, ES and RS conceived and designed the study. FE, SB, ES and RS collected the data. TS statistically analyzed and all authors interpreted the data. FE, BW and TS drafted the manuscript. All authors critically revised the manuscript and provided important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Beate Wild .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the medical ethics committee of the University Hospital Heidelberg.
Consent for publication
The patient gave written informed consent for analysis and publication of the data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Engel, F., Stadnitski, T., Stroe-Kunold, E. et al. Pain and psyche in a patient with irritable bowel syndrome: chicken or egg? A time series case report. BMC Gastroenterol 21 , 309 (2021). https://doi.org/10.1186/s12876-021-01879-2
Download citation
Received : 06 October 2020
Accepted : 08 July 2021
Published : 03 August 2021
DOI : https://doi.org/10.1186/s12876-021-01879-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Functional gastrointestinal disorders
- Time series analysis
- Single case study
BMC Gastroenterology
ISSN: 1471-230X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Remember Me


- Nutrition counsellor
- Food Allergy
- gastroenterology
- Heptologist In Delhi
- Liver transplant
Case Study On IBS
- Case Study On Irritable Bowel Syndrome (IBS)
What does Irritable bowel syndrome (IBS) mean?
Irritable bowel syndrome (IBS), also known as mucus colitis, nervous colon, and spastic colitis. IBS is a common functional disorder of the gastrointestinal tract. It is characterized by current episodes of abdominal pain, bloating, gas, and discomfort along with changes in the consistency of stool. This condition is heterogeneous, exhibiting variability in the symptoms reported within and between males and females.
What are the symptoms of IBS?
I ndividuals suffering from IBS will experience symptoms like belly discomfort, pain, diarrhea, constipation. However, these symptoms tend to change over some time. It can either be cured by treatment or may get severe over time, depending on the individual’s condition. Some common irritable bowel syndrome symptoms are listed below-
- Abdominal pains and cramps usually in the lower abdomen after taking meals
- Bloating of abdomen
- Increased gas
- Passing whitish mucus through the stool
- Constipation
- Harder or looser stool than usual
- Sudden urge to go to the washroom
- Food intolerance
- Weight loss and loss of appetite
Irritable bowel syndrome symptoms in females
Most of the symptoms of IBS in females are similar to males. Sometimes the symptoms tend to worsen during the time of menstruation. Women often experience worsening diarrhea just before menstrual periods. Bloating is a common symptom of IBS. Females with IBS are more likely to experience more bloating during their menstrual cycle than those women without IBS. However, menopausal women experience fewer symptoms than those women who are menstruating. Some females reported that their symptoms increased during pregnancy.
Irritable bowel syndrome symptoms in males
Researchers suggest due to hormonal differences, the male gut is less sensitive to signs of IBS than females. Males do experience problems with sexual intimacy just like females. They face difficulty in fulfilling their work and most likely suffer from depression. However, many think males simply avoid symptoms of IBS.
Irritable bowel syndrome symptoms in infants
If anyone or both the parents are suffering from this disorder, children are at higher risk. Both boys and girls are equally affected. They face symptoms like, belly pain that can persist for more than 3 months, mucus seen in the stool, loss of appetite, bloating, and gas.
Are you looking for a gastroenterologist? No worries we got you covered! Book an appointment with Dr. Nivedita Pandey, one of the best gastro doctors in Delhi. Can simply go for a gastroenterologist live chat session with her. She is there to solve all your tummy problems with compassionate care.
Irritable bowel syndrome (IBS) causes
Researchers are not aware of the exact cause of IBS. There are several factors like alteration in the gastrointestinal tract, food intolerance, hypersensitivity to pain. These factors are believed to be the causes of IBS. Let’s discuss some common causes of IBS-
- Brain-gut dysfunction- When there is a miscommunication between the nerves of the brain and gut, there are chances to develop IBS.
- Dysmotility- When individuals suffer from the abnormal movement of food in the gastrointestinal tract.
- Bacterial infection in the gastrointestinal tract.
- Overgrowth of small intestinal bacteria- An increase in number or change in the type of bacteria can cause IBS.
- Genetic influences- Researchers say that genes can make some people develop irritable bowel syndrome.
Mental disorders- Depression, stress, anxiety can be causes of IBS.
Irritable bowel syndrome symptoms treatment
When it comes to nonsurgical treatment, changing lifestyle and diet is the primary treatment for IBS. Some of the lifestyle changes are-
- Exercise regularly
- Avoid drinking alcohol and smoking
- Sleep properly
- Get involved in stress management and relaxation techniques
- Practice mindful training
- Avoid taking caffeine
- Walk regularly and practice yoga
- Go for psychotherapy and cognitive behavioral therapy
- Drink enough water and fluids
- Avoid taking foods that trigger your symptoms, look for foods with low-fat content, intake cooked vegetables other than cabbage, cauliflower, and broccoli which might cause bloating of the abdomen.
- For those who are lactose intolerant try to avoid dairy products that can trigger your symptoms.
- Enjoy eating chicken and fish
In case lifestyle and dietary changes do not provide relief to your symptoms, the individual should immediately seek urgent medical attention by consulting an online doctor chat or simply get in touch with the best gastroenterologist in Jammu. Most cases of IBP can be treated by nonsurgical measures. But if the symptoms get more severe, the patient might have to undergo surgery.
Irritable bowel syndrome risk factors
IBS can affect both females and males of all ages. However, it is more likely to affect individuals during their teens to adulthood. Researchers have studied that genes play a vital role in the development of IBS. Records show that more females are affected than males. The reason can be, males do not reach out for help to a specialist, and females experience hormonal changes during their menstrual cycle.
On the other hand, irritable bowel syndrome health risks can be mental illness, stress, depression, and traumatic events in their lives like sexual abuse. These conditions during irritable bowel syndrome can be cured by providing stress management and behavioral therapy to the patients to decrease the symptoms.
Only a small number of people have severe cases of irritable bowel syndrome. Severe symptoms can be treated with medication and therapies. Most patients can control their symptoms by changing their lifestyle and diet. These individuals come under the category of mild cases of irritable bowel syndrome. On the other hand, some individuals might have extremely serious symptoms like bloody diarrhea, shortness of breath, palpitation, swelling of the tummy. These individuals are considered the worst cases of irritable bowel syndrome. Later in their lives, they might be diagnosed with colon cancer.
Irritable bowel syndrome case study
A 43-year-old woman with a history of recurrent abdominal pain for 25 years, loose stool, fecal urgency. In the last 1-2 years, her symptoms have worsened and she experienced severe abdomen pain, fecal urgency, and inconsistency along with 6 to 8 times loose bowel movements per day. She is not exposed to alcohol. Her symptoms started deteriorating in recent years with the increase in stress in her personal and professional life. Due to her improper bowel movements, she had to quit her job which requires a lot of traveling and her body is not permitting to do that. There is no family history of irritable bowel syndrome or colon cancer. Physical examinations and laboratory test reports showed no signs of weight loss, no blood in stool, CPC and laboratory negative for celiac serologies, colonoscopy with biopsy was negative, and fecal protection was negative. Previous treatment of this patient included a low-FODMAP diet with mild improvement in symptoms. The patient wants to resolve physical urgency and inconsistency and at the same time hopes for a solution to her other symptoms.
Irritable bowel syndrome case definition
This particular case of a 43-year-old woman suffers from symptoms like abdominal pain, fecal urgency, inconsistency, and loose bowel movements. From the patient’s history, one of the renowned gastroenterologists in Delhi was able to conclude that it is a functional gastrointestinal disorder, called irritable bowel syndrome.
Irritable bowel syndrome case report
Diagnosis- The 43-year-old woman is suffering from irritable bowel syndrome. It is a digestive system disorder and is concerned with abnormal bowel movements, and abdomen pain.
Signs and symptoms- The signs and symptoms shown by this patient are recurrent abdominal pain, fecal inconsistency, loose stools for 6-8 times a day, fecal urgency and her symptoms have worsened in the last few years, with an increase in stress in her professional and personal life.
Treatment- Firstly, based on the patient’s history, the best gastroenterologist in Delhi and her team suggested going for therapeutic sessions like CBT (Cognitive-behavioral therapy). The next important thing they paid attention to is diet. The patient was asked to continue taking a low-FODMAP diet, but at the same time consulting a dietician is recommended, to make sure she is getting her daily nutrition requirements.
When it comes to pharmacological management, such patients with severe symptoms should consider taking therapies of rifaximin or eluxadoline. Lastly, the doctor made sure the patient is aware that her symptoms might be minimized with a better lifestyle and medication, but it’s not realistic to completely resolve the symptoms.
Follow up- A follow-up was recommended by the doctor. Approximately 5 to 6 weeks later, the patient visited the clinic again. Dr. Nivedita and her team ran some tests and diagnosed her. With the right treatment and therapies, her symptoms got minimized. Abdominal pain, fecal urgency, inconsistency have improved, also her anxiety and stress got better. The Patient was sent back home in a better state and her family was thankful to the doctor and her team.
To solve your gastroenterology problems, get in touch with Dr. Nivedita and fix your appointment online. You can find her among the top 10 gastroenterologists in Delhi. She is considered one of the best doctors in Patna for the stomach, the best liver specialist in Delhi NCR, and the best liver expert doctor in Jaipur. Also, her ability to treat patients online by gastroenterologist live chat is remarkable. So take this opportunity and get yourself and your loved ones treated.
Consult the best Hepatologist in India, Dr. Nivedita Pandey through online dr chat if any abnormality occurs. She is also well known for her nutritional counseling services online services of hepatologist or teleconsultation services. Fill the form below to book an appointment with us now. She is also famous for her care from afar service and as a food pipe specialist . You can also find her as the best liver specialist doctor in Patna , Bihar or hepatologist in Patna or the best doctor for hepatitis b in Patna or at the gastro and liver clinic Patna Bihar, Gooddeed Clinic and also as a gastroenterologist in Faridabad , the best gastro doctor in Delhi, NCR , a gastroenterologist In Uttarakhand , a liver specialist in Jhansi or Best female Gynecologist in Jhansi, best gastroenterologist in Jammu or best physician in Jammu city, take advantage of the online gastroenterology consultation to gastroenterologist live chat and receive the best treatment that your body deserves!
Is IBS considered a serious health condition?
The severity of irritable bowel syndrome varies from person to person. In some individuals, IBS leads to symptoms that are manageable and can be cured by changing their lifestyle. But for others, the symptoms might get severe and interfere with their quality of life. However, with proper treatment, the symptoms can be minimized.
Is IBS a common disorder?
IBS is the most common functional disorder of the gastrointestinal tract. It affects both men and women starting from the age of 2 to 60.
Privacy Preference Center
Privacy preferences.
An IBS Case Study | 10 Years of IBS Ended + Reduced Anxiety
At Goodpath, our mission is to improve quality of life.
This is the real story of Anthony. He found Goodpath through his employer for support with his IBS.
Who Is Anthony
Anthony is a 44-year old man who had more than just a bad belly. He was once an active cyclist and liked to be outside. However, his digestive symptoms had been troubling him over the past 10 years, affecting his day-to-day quality of life.
Anthony had tried to resolve his symptoms before:
He visited multiple doctors and had blood tests done, but results always came up normal
He also tried to treat it himself with medicines and changes in his diet but those did not work for him either
He also had moderate anxiety which was exacerbating his IBS symptoms.
Anthony's Personalized Treatment Included Treating Anxiety
Following the short assessment, Goodpath created a completely personalized IBS treatment program for him. Goodpath has over 500 possible treatments available across multiple modalities of care. And each treatment is validated for clinically proven positive outcomes for a condition or aspects of a condition.
In Anthony’s case, the Goodpath process took the unique details of his condition, like his IBS severity and the presence of anxiety, and matched those details to specific treatment options that were right for him.
This was all supported by 1:1 video calls with his Goodpath health coach, who made modifications to his program as his health improved.
Measurable Results
After 3 months of treatment with Goodpath, Anthony feels much better with results that can be measured in addition to felt.
Previously, Anthony had an IBS Severity Score of 180, which was moderate severity. After Goodpath treatment, this dropped to well within normal ranges and is considered in remission.
Anthony had a moderate anxiety disorder, as measured on the GAD-2 scale. After Goodpath, his anxiety is also much lower and is well-controlled.
Anthony’s IBS symptoms are now so much better that he can start biking again.
He has completed his IBS program but keeps doing the mindfulness exercises for his stress and has new discipline on a diet that avoids trigger foods.
He valued the Goodpath treatment so much that he asked to keep staying with Goodpath, saying “Can we add focusing on my back pain now?”
Case study of PPIs causing irritable bowel syndrome (IBS)

- Demographics
- Introduction
- Diagnostics
Gastric acid is a major component that delineates the delicate balance between successful digestion and malabsorption, playing a critical role in conditions such as irritable bowel syndrome and reflux disease. In addition, our gut lumen is primarily an acidic environment due to the presence of stomach acid, and it should be treated as such. Any interference, such as drug administration (including over-the-counter medications), hormonal imbalance, or environmental input, disrupts the timely and adequate production of hydrochloric acid, leading to malabsorption and gradual alteration of intestinal physiology. The most common symptoms triggered by chronic PPI use are small intestinal bacterial overgrowth, flatulence, altered stool habits, and gas, which are often associated with heartburn.
Han, Yiping W. “Fusobacterium nucleatum: a commensal-turned pathogen.” Current opinion in microbiology 23 (2015): 141-147.
Carter, Chris J., et al. “The Porphyromonas gingivalis/host interactome shows enrichment in GWASdb genes related to alzheimer’s disease, diabetes and cardiovascular diseases.” Frontiers in aging neuroscience 9 (2017): 408.
Scher, Jose U., et al. “Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis.” elife 2 (2013): e01202.
Malinowski, Bartosz, et al. “The role of Tannerella forsythia and Porphyromonas gingivalis in pathogenesis of esophageal cancer.” Infectious agents and cancer 14.1 (2019): 3.
Regrettably, the number of patients remaining on PPI treatment for more than 24 weeks is steadily increasing, primarily due to the rapid and efficient symptomatic relief it provides for conditions like heartburn and reflux disease. Often, physicians themselves recommend that the patient continues the treatment, although there are cases where patients persist with the treatment despite their physicians advising them otherwise. Moreover, most patients continue the treatment even after being diagnosed with B12 deficiency. Oral bacteria such as Fusobacterium , Porphyromonas , Tannerella , and others capitalize on the more hospitable gastric environment and may infiltrate the gut and circulation, predisposing individuals to various other disorders, including cardiovascular, metabolic, autoimmune diseases, and even cancer.
George was a typical case of unnecessary chronic PPI use. His symptoms started very mild. He was prescribed omeprazole for just a 2-day incident of gastric reflux. The relief was immediate and with the consent of his doctor, George was still on PPI’s 6 years later!!
His lifestyle pattern set the stage for his stomach symptoms. Many coffees, very late dinners, no salads, and symptoms that kept changing and worsening. Episodic, diarrhea, unexplained fatigue… Several years later, he was still on the stomach treatment but his life was a mess. He had already consulted several specialties and performed tests like gastroscopy and colonoscopy without significant findings, except non-specific gastritis and redness throughout his colon.

Aware of the harmful effects PPIs, such as omeprazole, have on the GI system and the hormonal changes that occur following their chronic administration (e.g., gastrinemia), I asked George to undergo several stool and blood tests. I wanted to rule out some of the most severe side effects of chronic acid suppression, like hypochlorhydria, exocrine pancreatic insufficiency, and ADMA (an early indicator of hypertension). Additionally, I aimed to assess the extent of microflora distortion and the degree of SIBO to plan appropriate treatment, considering the symptoms of IBS, such as abdominal pain and digestive issues.
The quality and the quantity of indisgested particles that reach the colon are the determining factors of fermentation rate (and gas production)
Chronic lowering of acid production makes the stomach less capable of digestion. And while acid-induced pain is limited, dyspepsia is heightened.
The trapped air within the colon along with the loss of defecation timing leads to the constant feeling of colonic content and bowel movement
Besides B12 deficiency, which is the commonest culprit of chronic acid suppression, many more vitamins and nutrients are depletes through indirect consequences of hypochlorhydria
In cases like this, certain tests, including the hydrogen breath test, consistently return positive results. The small intestinal microbiome may comprise only a small portion of the total bacterial load of the GI system, but it can take advantage of the persistent low gastric acid (hypochlorhydria) and expand manyfold, leading to acid reflux and other symptoms. Several more results should be evaluated collectively before proposing a treatment plan to address the small intestinal bacterial overgrowth and related symptoms.
Low diversity index
Fragments and residues of indigested food particles produce mixed movements of the gut giving rise to alternating defecation pattern

Elevated ADMA
Dysregulated nitric oxide metabolism leads to fluctuation in blood pressure. Elevated ADMA is detected in chronic PPI users
Bacterial overgrowth of the small intestine interferes with proper absorption of nutrients and produces gas
Probiotic sterility
Probiotic sterility leads to abnormal fermentation of starch, sugars, and fiber. Bloating and gas are the main symptoms
In George’s case (and all similar cases) the treatment plan should cover the entire gastrointestinal system. Gastric inflammation reduction, small intestinal overgrowth reduction, and colonic microbiome restoration. Although it is a very difficult and possibly time-consuming process, there is no other way to complete healing. Many factors also play a major role: Patient’s age, gallbladder removal, diet, and of course lifestyle habits. The rule is “the earlier the intervention, the better the results”.

Our third appointment was done by phone because he was out of the city. He told me that although he had seen a significant improvement in his stool pattern -one or two times per day, nearly formed- he had also noticed an increase in his allergic symptoms. I explained to him that this was normal and something desirable. As the histamine-producing bacteria die off they release histamine in large quantities. I also explained that this exacerbation of his allergies would be greatly reduced when he completed both antimicrobial treatments. He had managed to eat mostly before 9:00 pm and to take his breakfast after 10 am. Although this was a great accomplishment I urged him to take his dinner even earlier than that…
Long-term PPI use causes a multitude of changes in both the secretory machinery of the digestive tract and the gut microbiome. The secretion of hormones like gastrin, acetylcholine, and histamine is compromised and the continuous enrichment of the small intestine with oral and environmental bacteria inevitably leads to small intestinal bacterial overgrowth. This is why IBS is much more prevalent in past or current users of this kind of medication . PPis, like omeprazole, are not designed to be taken for more than 8 consecutive weeks.
- Long-term PPI use, such as omeprazole, disrupts gastric acid production and intestinal physiology, leading to IBS symptoms like small intestinal bacterial overgrowth, flatulence, and altered stool habits
- Chronic acid suppression from PPIs can result in hypochlorhydria, vitamin deficiencies, and hormone dysfunction, ultimately causing IBS symptoms like bloating and gastric discomfort
- Tests confirm small intestinal bacterial overgrowth, low diversity index, elevated ADMA, and probiotic sterility, which are associated with PPI-induced IBS
- Treating PPI-related IBS symptoms requires a comprehensive approach that targets gastric inflammation, small intestinal overgrowth, and restoration of the colonic microbiome, with early intervention yielding better results
- IBS is more prevalent in past or current users of PPIs like omeprazole, which are not intended for use beyond 8 consecutive weeks, due to the medication's effects on secretory machinery and gut microbiome

- Theodoros Prevedoros
- [email protected]
Privacy Overview
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Post-infection irritable bowel syndrome following Coronavirus disease-19: A systematic review and meta-analysis
Affiliations.
- 1 Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, 226 014, India.
- 2 Institute of Gastrosciences and Liver Transplantation, Apollo Multispeciality Hospitals, Kolkata, 700 054, India.
- 3 Department of Microbiology, All India Institute of Medical Science, Kalyani, 741 245, India.
- 4 Department of Gastroenterology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, 226 014, India. [email protected].
- 5 Institute of Gastrosciences and Liver Transplantation, Apollo Multispeciality Hospitals, Kolkata, 700 054, India. [email protected].
- PMID: 38261245
- DOI: 10.1007/s12664-023-01486-x
BACKGROUND AND OBJECTIVES: Persistent gastrointestinal (GI) symptoms and functional gastrointestinal disorders (FGIDs) are increasingly being recognized after Coronavirus disease-19 (COVID-19). Though quite a few studies addressed irritable bowel syndrome (IBS) following COVID-19, the disorders' prevalence varies greatly. We evaluated, (i) overall frequency of post-COVID-19 IBS, (ii) relative risk of development of IBS among COVID-19 patients compared to healthy controls using systematic review and meta-analysis techniques.
Methods: Literature search was performed for studies on GI symptoms and FGIDs after COVID-19 using electronic databases (Medline, Scopus, Cochrane Central Register of Controlled Trials, Google Scholar and Web of Science) till April 28, 2023. We included studies reporting IBS after COVID-19 with any duration of follow-up and any number of subjects. Studies on pediatric population and those not providing relevant information were excluded. Relative risk of development of IBS using Rome criteria among COVID-19 patients compared to healthy controls was calculated. Analysis was done using MedCalc (Applied Math, Mariakerke, Belgium, version 7.2) and Comprehensive Meta-Analysis version 3.3.070 (Biostat Inc. Englewood, NJ 07631, USA).
Results: Of the available studies, 13 (four case-control) reporting on IBS after COVID-19 met inclusion criteria. Among 3950 COVID-19 patients and 991 controls, 7.2% of COVID-19 patients and 4.9% of healthy controls developed IBS. Of the four case-control studies reporting post-COVID-19 IBS, patients with COVID-19 were 2.65 (95% confidence interval [CI] 0.538 to 13.039) times more likely to have post-COVID-19 IBS as compared to healthy controls.
Conclusions: Patients with COVID-19 are more likely to develop post-COVID-19 IBS than healthy controls. The heterogeneity of studies, different criteria used by various studies to diagnose post-COVID-19 IBS and some studies not meeting the six-month follow-up duration of the Rome criteria for diagnosing IBS are limitations of this systematic review.
Keywords: COVID-19; Functional bowel disorders; Functional dyspepsia; Irritable bowel syndrome; Post-infection IBS.
© 2024. Indian Society of Gastroenterology.
PubMed Disclaimer
Similar articles
- Post-infection functional gastrointestinal disorders following coronavirus disease-19: a prospective follow-up cohort study. Zhang D, Chen C, Xie Y, Zeng F, Chen S, Chen R, Zhang X, Huang S, Li D, Bai F. Zhang D, et al. BMC Infect Dis. 2023 Jun 21;23(1):422. doi: 10.1186/s12879-023-08401-x. BMC Infect Dis. 2023. PMID: 37344782 Free PMC article.
- Meta-analysis: Post-COVID-19 functional dyspepsia and irritable bowel syndrome. Marasco G, Maida M, Cremon C, Barbaro MR, Stanghellini V, Barbara G. Marasco G, et al. Aliment Pharmacol Ther. 2023 Jul;58(1):6-15. doi: 10.1111/apt.17513. Epub 2023 Apr 10. Aliment Pharmacol Ther. 2023. PMID: 37038318 Review.
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P. Crider K, et al. Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217. Cochrane Database Syst Rev. 2022. PMID: 36321557 Free PMC article.
- Post-infection functional gastrointestinal disorders following coronavirus disease-19: A case-control study. Ghoshal UC, Ghoshal U, Rahman MM, Mathur A, Rai S, Akhter M, Mostafa T, Islam MS, Haque SA, Pandey A, Kibria MG, Ahmed F. Ghoshal UC, et al. J Gastroenterol Hepatol. 2022 Mar;37(3):489-498. doi: 10.1111/jgh.15717. Epub 2021 Nov 4. J Gastroenterol Hepatol. 2022. PMID: 34672022 Free PMC article.
- Tegaserod for the treatment of irritable bowel syndrome. Evans BW, Clark WK, Moore DJ, Whorwell PJ. Evans BW, et al. Cochrane Database Syst Rev. 2004;(1):CD003960. doi: 10.1002/14651858.CD003960.pub2. Cochrane Database Syst Rev. 2004. Update in: Cochrane Database Syst Rev. 2007 Oct 17;(4):CD003960. doi: 10.1002/14651858.CD003960.pub3. PMID: 14974049 Updated. Review.
- Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–3. - DOI - PubMed
- Ghoshal UC, Ghoshal U, Mathur A, et al. The spectrum of gastrointestinal symptoms in patients with Coronavirus disease-19: Predictors, relationship with disease severity, and outcome. Clin Transl Gastroenterol. 2020;11:e00259. - DOI - PubMed - PMC
- Merola E, Armelao F, de Pretis G. Prevalence of gastrointestinal symptoms in coronavirus disease 2019: a meta-analysis. Acta Gastro-Enterol Belg. 2020;83:603–15.
- Barbara G, Grover M, Bercik P, et al. Rome Foundation Working Team Report on Post-Infection Irritable Bowel Syndrome. Gastroenterology. 2019;156:46–58.e7.
- Klem F, Wadhwa A, Prokop LJ, et al. Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: A systematic review and meta-analysis. Gastroenterology. 2017;152:1042–54.e1.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources, miscellaneous.
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Case study : Irritable Bowel Syndrome (IBS), Male, 41 years old
Case study 3 : Irritable Bowel Syndrome (IBS), Male, 41 years old
Fair health state, IBS in history 15 years, followed by a low back injury at age of 15, injury of cervical spine later in life. Not taking any medication, in the past was taking anti-inflammatory and immodium. Diet is not great, drinking cider, wine, eating spicy foods. History of IBS: started off discomfort in the lower abdomen in response to stress further developed to an agonising pain and instant desire to go to toilet. Very disturbing for life. Observation: Periodically stressed, sleep well. Abdomen is distended. Palpation: lower abdomen and sacral area are tender to palpation.
- 1st treatment – Assessment, shows that the Active region is cervical. Treated with Flex Array – significant relaxation + 6 points
- 2nd treatment – pain in the lower back focused on Lumbar zone
- 3rd & 4th treatments – treatment of the lower abdomen and Flex array on the Lumbar-Sacral zone;
- 4th & 5th treatments – exacerbation of pain in the lower abdomen, focused on the Sigmoid projection,;
Treatment outcome – mid course – pain is a lot less and even poor diet would not stimulate it.
- 6th and 7th treatments – focus on the Lumbar back region with Flex array and working on the upper abdomen (complaint zone);
- 8th treatment –Assessment – Active zone shifted to mid Thoracic, focused on it.
- 9th and 10th treatments – spinal roots L4, L5 with Flex array focused on the dermatomes.
- 11th and 12th treatments – assessment + 6 points, readings shifted again to Low back. Treated with the Flex array.
Treatment result: Pain is completely absent, even when stressed or poor diet.
Recommended to purchase a home use device to maintain the result and get further improvement.
A resent progress was checked three years from his first treatment.
During the first year he used his personal device occasionally, mostly as a preventative treatment. Now the patient reported that there were no symptoms of pain or discomfort, even in stressful situations.
Stomach aches and diarrhoea: How can we tell if it’s food poisoning, IBS or inflammatory bowel disease?
Advertisement.
How do you tell if that stomach ache and diarrhoea are from last night's dodgy dinner, irritable bowel syndrome (IBS) or an inflammatory bowel disease (IBD) such as Crohn's disease or ulcerative colitis?
(Photo: iStock/Sitthiphong)
This audio is generated by an AI tool.

Khoo Bee Khim
With our love for food and penchant for food hunting (sometimes on dubious grounds), ingesting the odd tummy-upsetting pathogen is almost par for the course – along with a bout or two of abdominal discomfort, diarrhoea or changes in bowel habits.
But what if that stomach pain means more than just a case of food poisoning because, as it turns out, there are many other bowel conditions that can also elicit similar reactions?
For example, irritable bowel syndrome or IBS is always characterised by abdominal pain after eating, though it may also be accompanied with diarrhoea, constipation or a change in stool consistency, said Dr Eric Wee, a senior consultant gastroenterologist with Nobel Gastroenterology Centre at Mount Elizabeth Novena Hospital.
Another gastrointestinal issue, inflammatory bowel disease or IBD, may also share similar symptoms.

“Many patients consult gastroenterologists thinking they might have an IBD or IBS, and are eventually diagnosed to have the other condition, or some other illness such as a gastroenteritis (infection) instead,” said Dr Wee .
“Much of the confusion stems from the fact that both conditions may present with abdominal pain, diarrhoea or a change in the bowel habit. The more serious condition is IBD and fortunately, it occurs infrequently.”
HOW DO WE TELL IF IT’S JUST FOOD POISONING OR SOMETHING ELSE?
It can be difficult to tell because d iarrhoea, stomach pain and bloating are signs of many digestive diseases, including IBS, IBD, c eliac disease, gluten intolerance and lactose intolerance , according to Dr Wee , who said the most common cause is usually food poisoning or gastroenteritis.
IBS refers to a functional condition where the digestive system is over-sensitive to different triggers that cause it to move too fast or too slowly, resulting in diarrhoea or constipation, and often in association with abdominal pain, said Dr Melvin Look, the d irector of PanAsia Surgery in Mount Elizabeth Hospital, Mount Elizabeth Novena Hospital and Parkway East Hospital.
The reasons for the excessive muscle contractions are often not completely understood, according to Singhealth , although they can include “diet intolerance, stress, depression, abnormality in intestinal bacteria content or abnormal intestinal tract movement”.

There is ground to suspect IBS if your abdominal pain or discomfort persists for at least three days per month in the last three months – and is accompanied by at least two of the following:
- Pain improves after passing motion
- Changes in the frequency of passing motion
- Changes in stool form
IBD is another tough one to know for sure. “T here are no unique symptoms for IBD”, said Dr Wee . “However, patients often have mucous and blood in their stools. Their symptoms tend to have a longer and more chronic history as compared to gastroenteritis, which hits an individual relatively hard and fast. In severe cases of IBD, there may be fatigue, anaemia, fever and weight loss.”
SO, IS THAT IBS OR IBD?
One way to know what you have is through medical tests such as scans, stool tests, colonoscopies and biopsies. For IBS, “biopsies of the bowel generally do not show any abnormality”, said Dr Sulaiman Bin Yusof, a colorectal and general surgeon with Colorectal Clinic Associates. In contrast, IBD biopsies often show up distinct abnormalities, he said.
IBD is an autoimmune disease caused by the inflammation of the digestive tract, explained Dr Wee . “Immune cells from the body inadvertently cause damage to the digestive tract.” Depending on which part of the gastrointestinal tract is affected, IBD is categorised as Crohn’s disease or ulcerative colitis.

In Crohn’s disease, the mouth, oesophagus, stomach, small bowel, colon and anus can be affected. The damaged areas may appear in patches that are next to areas of healthy tissue, according to the US Centers for Disease Control and Prevention .
“Crohn’s disease may affect one location in the digestive tract or multiple places simultaneously,” said Dr Wee . “In severe cases, the inflammation may extend through the bowel wall and into other organs or the skin.”
Meanwhile, u lcerative colitis mainly affects the large intestine or colon, said Dr Sulaiman. “In some cases, u lcerative colitis can also affect the last part of the small intestine before it joins the colon. Typically, u lcerative colitis affects the left side of the colon and rectum. Its hallmark feature is continuous areas of shallow ulceration of the colon.”
Both of these conditions may also manifest with joint pain in the knee or elbow, added Dr Wee .
Why aren’t celiac disease, gluten intolerance and lactose intolerance considered IBDs?
They are primarily due to the gastrointestinal tract's inability to process and digest certain foods such gluten or lactose, said Dr Melvin Look, the director of PanAsia Surgery in Mount Elizabeth Hospital, Mount Elizabeth Novena Hospital and Parkway East Hospital. " They do not cause chronic inflammation of the bowels and are not considered to be IBDs," he said.
HOW COMMON ARE IBS AND IBD IN SINGAPORE?
Nearly one in 10 Singaporeans suffers from IBS, according to HealthXchange . When it comes to IBD, the number is lower. "Currently, it is estimated that there are 1,500 individuals who may be suffering from IBD in Singapore, of which 200 are children," said Dr Sulaiman.
While low, IBD cases appear to be on the rise. “ Singapore General Hospital saw close to 600 patients diagnosed with the disease in the year 2017, a two-fold increase from a decade ago in 2007,” said Dr Sulaiman, citing press reports. “National University Hospital saw a striking eight-fold increase in IBD patients, from below 50 in 2013 to close to 400 cases in 2018. The rise in numbers can be attributed to better awareness and better diagnostic capabilities in recent years.”
Of the two IBD conditions, “ulcerative colitis is more common than Crohn’s disease and fortunately, ulcerative colitis is easier to treat”, said Dr Wee . “Crohn’s disease has more complications and is more resistant to treatment.”

WHAT ARE THE POSSIBLE REPERCUSSIONS OF IBS AND IBD?
When it comes to IBD, one word: Cancer – or more specifically, colorectal cancer. In Crohn’s disease that only affects the small intestine, it may also cause cancer in that part of your gastrointestinal system, said Dr Sulaiman.
Added Dr Look: “ Patients with u lcerative colitis , for example, have four to 10 times the risk of developing colorectal cancer".
“The c onstant inflammation results in a high cell turnover, which predisposes to mutations resulting in cancer,” explained Dr Wee . “ Other factors include increased oxidative stress from the inflammation that leads to changes in the genes driving mutation.” Even the changes the gut microbiota undergo, owing to the medicines used to treat the autoimmune disease, may increase cancer risk, he said.
Unlike IBD, IBS does not cause inflammation, a key factor in colorectal cancer risk.
ARE DIARRHOEA AND FREQUENT BOWEL MOVEMENTS THE SAME?
The two are not interchangeable. "Diarrhoea" refers to the texture and consistency of the stools, which are often "watery", "lack form" and are "mushy or purely liquid", explained Dr Eric Wee, a senior consultant gastroenterologist with Nobel Gastroenterology Centre at Mount Elizabeth Novena Hospital.
"Frequent bowel movements" refers to an excessive number of bowel movements a day, said Dr Wee. There isn't a “normal” number of daily bowel movements as it varies from person to person. But it generally refers to defecating more often than you usually do. "Frequent bowel movements need not always mean passing soft, watery stools. It can also include normal or even hard stools," said Dr Wee.
WHAT ARE THE TREATMENTS AVAILABLE?
There may be a myriad of IBS treatments out there but research that backs their effectiveness remains to be seen. Here are some, according to studies :
- Peppermint oil: It supposedly calms the intestine by relaxing its muscles. Research suggests taking 500mg to 800mg per day in capsules.
- Probiotics: Introducing beneficial gut bacteria may help. However, experts have yet to determine the bacteria type and dose.
- Anti-cramping medications: They relieve pain by relaxing the muscles of the intestine but may create side effects such as dry mouth, dizziness and blurred vision.
- Cognitive behavioural therapy: It is thought that stress may contribute to IBS and there is some evidence that such therapy may help.

When it comes to IBD such as Crohn’s disease and u lcerative colitis, patients are usually treated with medicines that control the immune system, said Dr Wee, citing tablets and monthly injections. “There are many modern treatment options available and they include classes of drugs such as steroids, aminosalicylates, immunomodulators, biologic therapies, small molecule drugs and JAK inhibitors ."
Medicines aside, manipulating your diet may also help IBD, said Dr Wee, citing d ata from clinical trials. That means avoiding triggering foods such as processed food, preservatives, artificial sweeteners and emulsifiers as well as minimising gluten, dairy and alcohol.
“Complete avoidance is not mandatory but one needs to exercise restraint. Limiting the intake of red meat is believed to be important, too,” said Dr Wee. Unfortunately, changing your diet alone is often not adequate. “Almost all individuals with IBD will require medical treatment concurrently.”
Surgery to remove the affected gastrointestinal parts is only used when medical therapy fails, said Dr Sulaiman. For instance, s urgery may be used to manage the complications from Crohn’s disease to preserve as much of the bowel as possible.
Related Topics
Recommended, recent searches, trending topics, this browser is no longer supported.
We know it's a hassle to switch browsers but we want your experience with CNA to be fast, secure and the best it can possibly be.
To continue, upgrade to a supported browser or, for the finest experience, download the mobile app.
Upgraded but still having issues? Contact us
- Search the site GO Please fill out this field.
- Newsletters
Health Benefits of Mint
:max_bytes(150000):strip_icc():format(webp)/image-70f484bba39c42cbb162c0961ac3f1ed.png)
- Side Effects
Mint is the collective name for a number of plants that belong to the mint or Lamiaceae plant family.
Mint, including peppermint, is commonly used as an ingredient in drinks, desserts, and other recipes and can also be taken as a dietary supplement.
Studies show that supplementing with mint may benefit health in several ways, including improving certain digestive conditions and soothing nausea.
Design by Health / Getty Images
May Benefit Digestive Conditions
Mint has certain properties that make it an effective natural treatment for digestive conditions such as irritable bowel syndrome (IBS) and indigestion, a medical term for discomfort in the upper abdomen.
Mint, like peppermint, is packed with therapeutic compounds, such as L-menthol, a monoterpenoid compound with muscle-relaxing properties. L-menthol blocks calcium channels that initiate contractions in smooth muscles, preventing the spasming that causes symptoms like abdominal pain and diarrhea in people with IBS.
Mint also contains anti-inflammatory and antioxidant compounds, which may benefit people with IBS by decreasing inflammation and cellular damage.
One review of 12 studies involving 835 people with IBS found that peppermint oil supplementation over a period of two to 12 weeks significantly improved symptoms like abdominal pain, bloating , and gas compared to placebo treatments.
One review of 96 studies found that, when used with other ingredients like caraway oil, peppermint oil supplements were effective for reducing certain symptoms of indigestion, including abdominal pain and abdominal pressure. Research on the effectiveness of peppermint supplements for treating indigestion is limited, and there's currently no evidence that mint-only treatments are effective for treating this condition.
May Improve Cognitive Performance
Some research suggests that peppermint oil supplements may improve cognitive performance .
Mint contains compounds that may boost cognitive function by interacting with certain neurotransmitters, like γ-aminobutyric acid (GABA), and inhibiting acetylcholinesterase (AChE). This enzyme breaks down a neurotransmitter called acetylcholine, which plays important roles in attention and memory.
One study involving 24 people found that treatment with a single dose of 100 microliters (µl) of peppermint oil improved cognitive test performance and reduced mental fatigue associated with extended cognitive task performance compared to a placebo treatment.
Could Soothe Nausea
Mint has a soothing aroma and smelling it may help reduce nausea symptoms. For example, studies show that mint aromatherapy may be helpful for reducing nausea and vomiting in people undergoing treatment for cancer .
Taking mint supplements may also be effective against certain types of nausea and vomiting. One study of 84 people with breast cancer who were undergoing chemotherapy found that treatment with 40 drops of peppermint essential oil in water every eight hours significantly reduced nausea, vomiting, and low appetite at 24 and 48 hours after treatment compared to a placebo.
However, most studies investigating mint's effects on nausea and vomiting have focused on mint aromatherapy, not oral mint supplements.
Might Boost Athletic Performance
Though research is limited, some evidence suggests that mint supplements may be helpful for those looking for a natural way to improve stamina and power during exercise. Mint has antispasmodic properties and may help relax smooth muscles in the lungs and improve tissue oxygenation, which can support exercise performance.
One small study of 12 men found that treatment with 500 milliliters (ml) of mineral water containing 0.05 ml of peppermint essential oil for ten days significantly improved exercise performance, lung function, heart rate, and power during a treadmill exercise test compared to before the treatment.
Another study of 30 healthy men found that a single oral dose of 50 µl of peppermint essential oil significantly improved exercise performance and lung function parameters compared to a placebo treatment. While these results are promising, more studies are needed to understand how oral mint supplements may benefit exercise performance.
How To Use Mint Supplements
Mint supplements are available in several forms, including capsules and liquids. Because dosing and use instructions vary, following the directions on the supplement label is important.
It's best to talk to your healthcare provider before using a mint supplement. This is especially important if you have a health condition like a digestive disorder.
Although mint supplements may be helpful for people with certain medical conditions, they're not appropriate or safe for everyone.
Dosing recommendations for mint supplements vary depending on the type and what it's being used to treat.
For example, some research suggests that peppermint oil in doses of 50-100 µl may be effective for improving athletic performance and cognitive performance, respectively.
One study found that treatment with 182 milligrams (mg) of peppermint oil daily for eight weeks was effective for improving IBS symptoms.
Always speak with a healthcare provider for specific dosing advice.
Is Mint Safe?
Mint supplements are generally considered safe but aren't appropriate for everyone.
Because little is known about the safety of oral mint supplements during pregnancy and breastfeeding, it's best to avoid oral mint supplements during these stages of life.
Peppermint oil has been shown to be safe when taken in appropriate amounts. However, people with certain medical conditions, such as gallstones, hiatal hernia, or gastroesophageal reflux disease (GERD), should consult a healthcare provider before taking peppermint supplements.
Potential Drug Interactions
Mint supplements may interact with or increase the bioavailability of some commonly prescribed medications, such as:
- Blood pressure medications: Though human research is limited, peppermint oil may increase the bioavailability of certain blood pressure medications, like felodipine, increasing their effects in the body.
- Cytochrome P450 substrates: Some evidence suggests that peppermint oil may interact with drugs that are metabolized by cytochrome P450 enzymes, including the blood thinner Warfarin and the blood pressure medication metoprolol.
- Chemotherapy drugs: Peppermint oil may interfere with certain chemotherapy agents, like docetaxel and cisplatin.
If you're taking one or more medications, it's important to consult your doctor before adding any new supplement into your routine, including mint products.
What To Look For
When shopping for a mint supplement, there are a few things to remember.
It’s important to choose high-quality products from trusted supplement brands. When possible, purchase mint supplements from companies certified by organizations like UL, USP, and NSF International, which set strict standards for supplement quality and safety.
Check with your healthcare provider before taking a mint supplement. Mint supplements aren't safe or appropriate for everyone and may interact with common medications
Can You Take Too Much Mint?
Though mint supplements are generally considered safe, extremely high doses can be toxic. For example, high doses of peppermint oil can cause kidney and liver injury and even lead to acute kidney failure. There have been cases of near-fatal peppermint oil overdoses.
Again: always consult a healthcare provider if you have any questions about supplement dosing.
Side Effects of Mint
Though mint supplements aren't associated with serious side effects when taken in appropriate doses, they may cause a few side effects.
Possible side effects related to taking mint supplements include:
- Abdominal pain
- Dermatitis (skin inflammation)
If you experience any side effects after taking a mint supplement, stop taking the supplement and contact your healthcare provider if the symptom doesn't resolve.
Best Ways To Use Fresh Mint
If you're interested in reaping the benefits of mint but don't want to take supplements, consider incorporating fresh mint into your diet.
Mint, like peppermint, has a refreshing taste and is high in protective plant compounds, like polyphenols, which have antioxidant and anti-inflammatory effects in the body.
Here are a few ways to use fresh mint:
- Chop up fresh mint and add it to green salads
- Make a flavorful side dish using fresh mint, watermelon , and feta
- Add fresh mint to water and cocktails
- Use chopped mint in homemade pestos and dressings
- Incorporate fresh mint into pasta dishes
- Use fresh, chopped mint as a garnish for meat, chicken , and fish dishes
Fresh and dried mint can also be used in desserts, like ice cream and baked goods. It pairs especially well with chocolate and can be used to make delicious chocolate-based recipes like cakes and cookies.
A Quick Review
Mint is a common ingredient in sweet and savory dishes and cocktails. When used as a dietary supplement, mint, including peppermint, may benefit health in several ways.
Studies show that mint supplements may improve symptoms of certain digestive conditions, like IBS, and may support exercise performance and cognitive function.
While mint supplements are generally considered safe, they're not the right choice for everyone and can lead to dangerous side effects when taken in high doses.
Alammar N, Wang L, Saberi B, et al. The impact of peppermint oil on the irritable bowel syndrome: a meta-analysis of the pooled clinical data . BMC Complement Altern Med . 2019;19:21. doi:10.1186/s12906-018-2409-0
Chumpitazi BP, Kearns G, Shulman RJ. Review article: The physiologic effects and safety of Peppermint Oil and its efficacy in irritable bowel syndrome and other functional disorders . Aliment Pharmacol Ther . 2018;47(6):738-752. doi:10.1111/apt.14519
Kennedy D, Okello E, Chazot P, et al. Volatile terpenes and brain function: investigation of the cognitive and mood effects of mentha × piperita l. Essential oil with in vitro properties relevant to central nervous system function . Nutrients . 2018;10(8):1029. doi:10.3390/nu10081029
Efe Ertürk N, Taşcı S. The effects of peppermint oil on nausea, vomiting and retching in cancer patients undergoing chemotherapy: an open label quasi-randomized controlled pilot study . Complement Ther Med . 2021;56:102587. doi:10.1016/j.ctim.2020.102587
Jafarimanesh H, Akbari M, Hoseinian R, Zarei M, Harorani M. The effect of peppermint (Mentha piperita) extract on the severity of nausea, vomiting and anorexia in patients with breast cancer undergoing chemotherapy: a randomized controlled trial . Integr Cancer Ther . 2020;19:1534735420967084. doi:10.1177/1534735420967084
Meamarbashi A, Rajabi A. The effects of peppermint on exercise performance . J Int Soc Sports Nutr . 2013;10:15. doi:10.1186/1550-2783-10-15
Meamarbashi A. Instant effects of peppermint essential oil on the physiological parameters and exercise performance . Avicenna J Phytomed . 2014;4(1):72-78.
Weerts ZZRM, Essers BAB, Jonkers DMAE, et al. A trial‐based economic evaluation of peppermint oil for the treatment of irritable bowel syndrome . United European Gastroenterol J . 2021;9(9):997-1006. doi:10.1002/ueg2.12134
National Institutes of Health: National Center for Complementary and Integrative Health. Peppermint oil .
Memorial Sloane Kettering. Peppermint Oil .
Nath SS, Pandey C, Roy D. A near fatal case of high dose peppermint oil ingestion- Lessons learnt . Indian J Anaesth . 2012;56(6):582-584. doi:10.4103/0019-5049.104585
Tafrihi M, Imran M, Tufail T, et al. The wonderful activities of the genus mentha: not only antioxidant properties . Molecules . 2021;26(4):1118. doi:10.3390/molecules26041118
Related Articles
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Studies & Experts
Struggling with Lower Back Pain? This One Simple Habit Can Help, According to a New Study
Slip on your walking shoes and let’s go!
:max_bytes(150000):strip_icc():format(webp)/carrie-myers-0434bbef1a7f4cb7a9572c41ca3d7bd3.jpg)
How Was This Study Conducted?
What did this study find, how does this apply to real life.
If you’ve ever had low back pain, you know how limiting it can be. And you’re not alone. According to 2019 statistics from the Centers for Disease Control and Prevention, 39% of U.S. adults experience back pain, and prevalence increases with age—from 28.4% in those ages 18 to 29, up to 45.6% in those ages 65 and up . Women are more likely to experience back pain than men—40.6% versus 37.2% respectively.
And back pain is expensive. According to a 2023 review in BMJ Open , direct medical and indirect costs of low back pain are at least $50 billion per year and upward of $100 billion in medical costs, lost wages and lost productivity .
But a new study published on June 19, 2024, in The Lancet suggests that back pain recurrence could be prevented—or at least delayed—by the simple act of walking . Let’s take a closer look.
Participants were chosen based on criteria related to back pain and current exercise status. They had to be at least 18 years old and to have recovered from an episode of nonspecific back pain within the previous six months. Nonspecific means that there was not a specific diagnosis for the back pain.
Researchers further defined an episode of nonspecific back pain as one that lasted at least 24 hours with a pain intensity of at least a 2 on a 0 to 10 pain scale. The pain had to be located within the area between the 12th rib and the crease of the buttocks to qualify as low back pain. It also had to have interfered with daily activities, including work.
To be included in the study, participants could not have been exercising regularly prior to the study, since researchers were looking at how exercise influenced the frequency of back pain episodes. They also could not have a condition that prevented them from being able to participate in a walking program.
After dismissing those who did not qualify, there ended up being 701 participants, who were randomly assigned to one of two groups—the intervention group or the control group. The average age of the participants was 54 and the majority of them (81%) were female. Participants were followed for a minimum of 12 months and up to 36 months, depending on when they entered the study.
Baseline data was gathered from both groups, including the number of previous back pain episodes, time since the last episode, levels of physical activity, time spent sitting (sedentary behavior), mental health status (depression, anxiety), stress levels and sleep quality.
Sociodemographic information was also collected, including sex, age, BMI, education level, income level, current work status, smoking status and occupational tasks—like if they had to lift heavy loads or were placed into awkward positions during manual labor.
The control group received no education or training from the research team. They could, however, seek out treatment and prevention strategies on their own during the study period—and many did, in the form of physical therapy, massage and chiropractic care.
The intervention group received education on back pain, as well as individualized training with one of 24 physical therapists. Each participant received a walking program designed specifically for them based on their baseline fitness level, abilities and limitations. The physical therapists were also trained in health coaching methods to help increase adherence to the program and to more effectively coach participants in behavior change. There were six available sessions participants could attend. While these sessions were initially intended to be in-person, the COVID pandemic occurred after the study had begun, so they had to switch to telehealth sessions.
The education component of the program included information about back pain, what current research suggests about pain, and coaching to help reduce the fear of movement. This was important, as many who experience back pain fear that exercise will exacerbate the pain and limitations of it.
Each participant in the intervention group also received a pedometer and walking diary. For seven days during the minimal 12-month study period, they wore an accelerometer, which is similar to a pedometer, but registers all movement, not just walking.
All participants—both the intervention group and the control group—were required to complete monthly questionnaires to establish whether they had experienced another episode of back pain.
According to the 12-week walking diaries, the intervention group progressively worked up to averaging four walking sessions per week for a total of 130 minutes. This is close to the recommended 150 minutes of moderate activity per week recommended in the 2018 Physical Activity Guidelines for Americans .
The primary outcome researchers were looking at was the number of days between a participant entering the study and their next occurrence of activity-limiting back pain. They wanted to know if the education, training and intentional walking for exercise increased the number of days between back pain episodes.
In the intervention group, the average number of days to recurrence of activity-limiting back pain was 208, and in the control group 112 days.
The researchers concluded that compared to the no-treatment control group, the group that received an individualized, progressive walking program, education and health coaching substantially reduced the recurrence of low back pain. The intervention group also experienced reductions in back pain-related disability (i.e., missing work, not able to perform normal daily activities) for up to 12 months. Researchers also stated that taking all things into consideration, including lost work time and wages, and medical expenses due to back pain, the intervention was likely cost-effective.
This study shows how walking alone may benefit back pain. Participants were not taught any strength-training exercises or stretches for back pain. They simply learned how to make walking a habit.
What we know about behavior change is that it takes consistent practice to form new habits . This study drives this home since participants were followed for at least a year (remember, some were followed for as long as three years if they entered the study early on).
While you may have heard that it takes just 21 days to form a new habit, research, like a 2023 study in PNAS, suggests that it depends on the complexity of the habit you’re trying to form . In that study, the habit of hand-washing took several weeks to establish, whereas forming a new exercise habit can take several months—and that’s if you’re committed and consistent with practicing the new habit.
The reason it takes time for habit formation is because it involves the brain cells and nerve pathways. Your habits are essentially well-worn, frequently used nerve pathways in the brain. That’s why they’re habits—they’re the pathways your brain can automatically go to. So when trying to create new habits, you’re fighting your brain for what it already knows and is familiar with. So creating new pathways—and ultimately habits—requires consistent practice of the new behavior so that brain cells will wire together to form new pathways. It’s pretty cool and is called neuroplasticity (this is where I geek out!).
If, for example, you’re trying to create a new exercise habit, the first step is to start where you’re at. Too many times we try to start at the end goal and quickly get burnt out. If you’re not currently exercising, then start with fewer sessions per week and fewer minutes per session—even if it sounds like a really small amount of time. Then gradually increase your time and frequency over several weeks. This can help your body adjust to the increase in movement and reduce muscle soreness and the risk of injury.
Simple habits, like hand-washing, can be stacked with habits you already have. You probably formed this habit as a child when you were reminded to wash your hands after using the toilet. Boom—new habit formed!
But more complex habits can also be stacked. Going back to the exercise example, what if you stacked going for a walk with eating lunch? So after eating lunch, you’ll go for a 10-minute walk. Eating lunch is your trigger to go for a walk. Or, stack brushing your teeth in the morning with doing a set of pushups, squats and planks. In this case, brushing your teeth is the trigger for doing some exercises—not necessarily at the same time, although I’ve been known to do squats, leg lifts, heel raises and pushups off the kitchen counter while doing dishes. It’s the same idea.
The Bottom Line
This study showed that regularly walking for exercise helped to increase the number of days between low back pain episodes. It also highlights the importance of consistently practicing the behaviors you want to become habits. Start slowly and gradually increase the number of days and amount of time to form new habits. Be patient and show yourself some compassion. It can take months to form more complex habits like exercise, so keep practicing consistently and before long it will be a regular part of your lifestyle.
Centers for Disease Control and Prevention. Back, lower limb, and upper limb pain among U.S. adults, 2019 .
Fatoye F, Gebrye T, Mbada C, Useh U. Clinical and economic burden of low back pain in low- and middle-income countries: a systematic review. BMJ Open . 2024. doi: 10.1136/bmjopen-2022-06411 9
Pocovi N, Lin C, French S, et al. Effectiveness and cost-effectiveness of an individualised, progressive walking and education intervention for the prevention of low back pain recurrence in Australia (WalkBack): a randomised controlled trial . The Lancet . 2024. doi.org/10.1016/S0140-6736(24)00755-4
U.S. Department of Health and Human Services. Physical activity guidelines for America, 2nd edition .
Buyalskaya A, Ho H, Milkman K, Camerer C. What can machine learning teach us about habit formation? Evidence from exercise and hygiene . PNAS . 2023. https://doi.org/10.1073/pnas.2216115120
Related Articles
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Gastroenterol

Pain and psyche in a patient with irritable bowel syndrome: chicken or egg? A time series case report
Felicitas engel.
1 Department of General Internal Medicine and Psychosomatics, University of Heidelberg, Im Neuenheimer Feld 410, 69120 Heidelberg, Germany
Tatjana Stadnitski
2 Department of Quantitative Methods in Psychology, University of Ulm, Albert-Einstein-Allee 47, 89081 Ulm, Germany
Esther Stroe-Kunold
Sabrina berens, rainer schaefert.
3 Department of Psychosomatic Medicine, Division of Internal Medicine, University Hospital Basel, Hebelstrasse 2, 4031 Basel, Switzerland
Associated Data
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Irritable bowel syndrome (IBS) appears to have a bidirectional interaction with both depressive and anxiety-related complaints. However, it remains unclear how exactly the psychological complaints, at the individual level, are related to somatic symptoms on a daily basis. This single case study investigates how somatic and psychological variables are temporally related in a patient with irritable bowel syndrome.
Case report
The patient was a woman in her mid-twenties with an IBS diagnosis. She reported frequent soft bowel movements (5–6 times per day), as well as flatulence and abdominal pain. She resembled a typical IBS patient; however, a marked feature of the patient was her high motivation for psychosomatic treatment as well as her willingness to try new strategies regarding the management of her symptoms. As an innovative approach this single case study used a longitudinal, observational, time series design. The patient answered questions regarding somatic and psychological variables daily over a period of twelve weeks with an online diary. The diary data was analysed using an autoregressive (VAR) modeling approach. Time series analyses showed that in most variables, strong same-day correlations between somatic (abdominal pain, daily impairment) and psychological time series (including coping strategies) were present. The day-lagged relationships indicated that higher values in abdominal pain on one day were predictive of higher values in the psychological variables on the following day (e.g. nervousness, tension, catastrophizing, hopelessness). The use of positive thinking as a coping strategy was helpful in reducing the pain on the following days.
In the presented case we found a high correlation between variables, with somatic symptoms temporally preceding psychological variables. In addition, for this patient, the use of positive thoughts as a coping strategy was helpful in reducing pain.
Irritable bowel syndrome (IBS) is characterized by recurrent abdominal pain that is associated with a change in frequency or form (appearance) of stool and can be related to defecation [ 1 ]. Currently, the symptom pattern is not sufficiently explained by peripheral organ pathology. IBS affects about 8% of the European population [ 2 ] and is most recently understood as a disorder of (microbiota-) gut-brain interaction [ 3 , 4 ] with a multifactorial origin that includes biological, psychological, and social factors [ 5 ]. Many patients who suffer from IBS also suffer from comorbid depressive or anxiety-related disorders [ 5 ]. Mood and anxiety disorders can precede or follow an IBS diagnosis due to the high discomfort caused by IBS [ 6 – 8 ]. By looking at specific psychological variables it was found that catastrophizing is directly associated with IBS symptom severity, while anxiety is indirectly related to IBS symptom severity [ 9 ].
While population-based studies suggest that IBS has a bidirectional interaction with both depressive and anxiety-related complaints, it remains unclear how exactly the psychological complaints, at the individual level, are related to somatic symptoms on a daily basis. Are increased psychological complaints (such as depression, tension, and nervousness) on one day preceded by IBS complaints on the previous day, or is it the other way around? A previous study showed that week-to-week stress and IBS symptoms were strongly cross-correlated in the same week, but were not temporally related across several weeks [ 10 ]. However, a day-by-day measure is needed to identify more fine-grained and direct relations. Furthermore, the focus of the study was on the mean values from a large patient sample, therefore potentially differing relationships in individual patients may not have been reflected in the aggregated data analysis.
Another interesting topic in patients suffering from IBS is the mutual relationship between coping strategies and IBS symptoms. A recent study reported that levels of coping resources were associated with gastrointestinal and extraintestinal symptom severity [ 11 ]. Also, catastrophizing and a lower self-perceived ability to reduce symptoms appeared to have a negative effect on health outcome in gastrointestinal disorders [ 12 ]. Interestingly, IBS patients have been reported to use passive coping strategies more frequently (such as escape-avoidance strategies instead of intended problem solving) compared to healthy controls [ 13 ]. Here too, the question arises to what extent coping strategies are related to IBS complaints and whether or not they are able to influence IBS complaints.
Overall, IBS symptoms and psychological distress are bi-directionally related, and coping strategies purportedly play an important role in the up- or down-regulation of IBS symptoms. However, individual mechanisms are not yet understood, and previous studies lack the longitudinal data on a day-by-day basis. Longitudinal data is necessary in order to obtain information about direct interactions, to better understand how temporal interactions between IBS symptoms and psychological complaints are related. As aggregated data can eliminate individual effects within the heterogeneous IBS patient sample, a single case study can provide important insights into specific mechanism to generate hypotheses for personalized clinical studies [ 14 ]. Conversely, inferences from singe case studies do not automatically apply to the patient population. However, results from single case studies can be used to generate hypotheses that can be examined in a sample of patients with similar characteristics.
This case study has, for the first time, applied a longitudinal time series design to a patient with IBS. Study objectives of this single-case analysis were: (1) to explore temporal relationships and interactions between the somatic and psychological complaints of the patient and (2) to investigate the impact of personal coping strategies on somatic symptoms.
Case presentation
Study design.
The study used a longitudinal, observational, single-case design. The study was approved by the medical ethics committee of the University Hospital Heidelberg. The patient was recruited in the frame of a pilot intervention study, conducted between July, 2014 and June, 2015 [ 15 ]. During her waiting period—and before the beginning of the therapy group—the patient answered questions daily regarding somatic and psychological complaints as well as coping strategies with the use of an online diary.
The diary data of the patient was collected following presentation in our outpatient specialty clinic for functional gastrointestinal disorders [ 16 ], and before group therapy. The data thereby showed the classic course of IBS without specific group intervention. The patient filled out the diaries from 10/2014 to 01/2015; over twelve weeks a total of 72 diary days were collected.
Measurements in the online diary
At the beginning of the study the patient received individual training in how to use the online diary; she was instructed to fill out the diary on a daily basis (between 4 pm and 12 am) via internet access. Validated questionnaires for IBS, as well as for psychological complaints and coping strategies, were used and adapted for the daily diary design. The most discriminating items of the questionnaires were derived in order to shorten the completion time of the diary (approximately 5–10 min). All items were rated by a visual analogue scale (VAS) with bipolar labels. The marked points were then converted by the computer program to a numeric scale ranging from 1 to 101. In addition, it was possible to enter a short free text in the diary.
For the measurement of somatic symptoms, we used the items “How severe is your abdominal (tummy) pain?” and “Please indicate how much your irritable bowel syndrome is affecting or interfering with your life today?”. Higher scores on these items reflected higher pain or higher somatic impairment. Psychological variables and coping strategies measured in the online diary are shown in Table Table1 1 .
List of Online-Diary Items included in the time series analysis
| Items implemented in the online diary | |
|---|---|
| Abdominal pain (AP) | “How severe is your abdominal (tummy) pain” → Adapted from the irritable bowel severity scoring system (IBS-SSS) [ ] |
| IBS associated daily impairment (DI) | “Please indicate how much your irritable bowel syndrome is affecting or interfering with your life today” → Adapted from the irritable bowel severity scoring system (IBS-SSS) [ ] |
| Nervousness (N) | “Today, how much were you distressed by nervousness or shakiness inside?” → Adapted from the brief symptom inventory (BSI) [ ] |
| Tension (T) | “Today, how much were you distressed by feeling tense or keyed up” → Adapted from the brief symptom inventory (BSI) [ ] |
| Depressiveness (D) | “Today, how often have you been bothered by feeling down, depressed, or hopeless?” → Adapted from the Patient-Health-Questionnaire (PHQ) [ ] |
| Pain associated discomfort (PD) | “Today, how much have you been bothered by stomach pain” → Adapted from the Patient-Health-Questionnaire (PHQ) [ ] |
| Catastrophizing (C) | “Today, when experiencing IBS-pain you had the feeling that you couldn’t go on” → Adapted from the coping strategies questionnaire (CSQ) [ ] |
| Hopelessness (H) | “When you had IBS-pain today, you thought: “It’s terrible and I feel it’s never going to get any better” → Adapted from the coping strategies questionnaire (CSQ) [ ] |
| Coping: positive thoughts (CPT) | “Today, when experiencing IBS-pain I thought of things I enjoy doing” → Adapted from the coping strategies questionnaire (CSQ) [ ] |
| Coping: Imagining pain outside the body (CIP) | “When experiencing IBS-pain, today I imagined that the pain is outside of my body” → Adapted from the coping strategies questionnaire (CSQ) [ ] |
All the variables are quantified on a 1 to 101 numeric scale. For AP, DI, N, T, D, PD, C, and H a higher score reflects higher somatic or psychological burden. For CPT and CIP, a higher score reflects an increased use of coping strategies
In January 2014, a German student (female in her mid-twenties), was referred to the outpatient specialty clinic of the University Hospital of Heidelberg for functional gastrointestinal disorders. She reported frequent soft bowel movements (5–6 times per day), as well as flatulence and abdominal pain. According to ROM-III [ 22 ] and the clinical assessment, an IBS (subtype IBS-diarrhea, IBS-D) was diagnosed. In addition, the patient was suffering from comorbid gluten, lactose, and sorbitol intolerance. No mental illness was present. Despite professional nutritional advice that included a gluten-, lactose- and sorbitol-reduced diet, gastrointestinal complaints persisted. In the course of the three-month follow-up appointments that included multimodal treatment [ 16 ] (04/2014, 07/2014, 11/2014), the patient correlated intestinal complaints and stress. She reported, for example, that the intestinal symptoms increased at the beginning of the semester and in the examination period. In the course of the diary study the patient did not describe any long-lasting stressor (such as an examination phase), but rather shorter week- or day-specific stressful events (such as Christmas holidays or looking for a part-time job) associated with an onset of IBS-symptoms on the same day. As an additional stressor, she described shame and the fear of a recurrence of the IBS complaints (particularly of soft bowel movements and flatulence), especially in social settings and situations where she could not easily reach a toilet. Relaxation techniques (yoga and gut-directed hypnosis using a CD) slightly improved her symptoms and the associated fear. Regarding the short stressful events, she described a good improvement of symptoms when using a strategy of calming down, with no further subsequent exacerbation. After the online diary study presented here, the patient received a group intervention [ 15 ] from which she has benefited.
In conclusion, according to IBS symptoms, symptom specific fears and avoidance behavior, the presented case of a young female patient resembled a typical IBS patient; however, a marked feature of the patient was her high motivation for psychosomatic treatment as well as her willingness to try new strategies regarding the management of her symptoms.
Statistical analysis
Initially, the following analyses were conducted for each time series: graphic examinations; calculations of descriptive statistics (range, median, mean, standard deviation), autocorrelation functions (ACF), and tests for stationarity with the Augmented Dickey–Fuller (ADF) procedure. Autocorrelation is the bivariate correlation of a time series with a lagged copy of itself. Therefore, instantaneous (lag = 0) autocorrelation is always equals one, significant autocorrelations on other lags imply predictability of the future time series values from the past values. Stability or instability as well as memory characteristics of time series can be inferred from their autocorrelation functions: non-zero autocorrelations at only a few lags are typical for stable short-memory processes, whereas significant autocorrelations on many lags indicate long memory or instability. Stationarity means that the statistical characteristics of a process under study do not change over time (e.g., exhibit no trends or distinct fluctuations of mean or variance). The Augmented Dickey-Fuller algorithms tests the null hypothesis “time series is stationary”.
In addition, cross-correlation functions (CCF), instantaneous correlations, and simultaneous regressions with psychological measures—both as dependent and somatic variables as predictors—were estimated. Cross-correlation measures similarity of two different time series as a function of the displacement of one relative to the other. Generally, instantaneous (lag = 0) correlations or simultaneous (lag = 0) regressions do not imply causation. For lagged correlations and regressions, however, it is different, since they explore the ability to predict the future values of a time series from prior values of another times series. The idea behind this is as follows: Since time does not run backwards, the cause cannot come after its effect. Therefore, events in the past can cause events to happen today, but future events cannot influence the present. The concept of Granger causality incorporates this idea: if lagged values of a time series X improve prediction of future values of a series Y, the former series Granger-causes the latter. For example, if lagged values of a somatic times series improve prediction of future values of a psychological one, the former series Granger-causes the latter. The vector autoregressive (VAR) methodology investigated the temporal dynamics between two or more time series by separating the time-lagged from the simultaneous relations. Therefore, temporal interdependencies between time series were analyzed using this approach. The VAR technique thereby allowed inferences about the temporal order of the effects by employing the temporal causality concept introduced by Granger. Furthermore, the VAR approach can handle time series that mutually influence each other and thus reveal feedback effects. In VAR modelling, interpretation of the regression coefficients is problematic because the lagged values of the dependent variables are used as predictors (i.e. dependent and independent variables are both endogenous, that is, determined and interrelated inside the organism or system), consequently, external influences can enter the autoregressive system exclusively through the residual term, which is also called “exogenous shock”. The behaviour of a VAR system can be modelled using impulse response analyses (IRA) and forecast error variance decompositions (FEVD). Impulse response functions (IRF) examine interdependencies within a VAR system by tracing the effect of an exogenous shock in one of the series on other variables. The FEVD estimates the amount of variance in each variable that can be explained by the other variables of the system during a specific period (h). For instance, in case of daily measurements, FEVD = 0.24 (h = 10) means that 24% of the forecast error variance in a dependent variable can be explained by exogenous shocks (random changes) of the predictors for a time horizon of 10 days.
The analyses were conducted using the R software. (Please consult Stadnitski & Wild (2019) and Stadnitski (2014, 2020) for descriptions, detailed explanations, and implementation of all analyses with the R software [ 23 – 25 ]).
Figure 1 visualizes the patient’s development of somatic symptoms, abdominal pain (AP), and daily impairment (DI) over 72 successive days together with their autocorrelation and cross-correlation function. In both series there appeared strong discomfort with values distinctly higher than 20 on 7 days. Almost 90% of the measurements varied between 1 and 20 on the 100-point scale. The average (Mean AP = 11.10, DI = 14.35) and variability (Standard Deviation: AP = 15.90, DI = 18.55) were higher for DI than AP (see also Table Table2). 2 ). Both time series exhibited no trends. Figure 2 shows the time series of additional psychological variables and coping strategies.

Somatic time series: abdominal pain (AP) and IBS-associated daily impairment (DI)
Characteristics of somatic and psychological (including coping) time series used in the diary study
| Min | Max | Med | M | S | Lag AC | P ADF | |
|---|---|---|---|---|---|---|---|
| Abdominal Pain (AP) | 1 | 90 | 6.5 | 11.10 | 15.90 | 10 | .03 |
| IBS Associated Daily Impairment (DI) | 1 | 87 | 8.5 | 14.35 | 18.55 | 1 | .01 |
| Nervousness (N) | 1 | 86 | 10.5 | 14.40 | 14.75 | 1 | .02 |
| Tension (T) | 1 | 81 | 5.0 | 8.24 | 11.59 | – | .01 |
| Depressiveness (D) | 1 | 30 | 2.0 | 4.06 | 4.42 | 1 | .03 |
| Pain-associated discomfort (PD) | 1 | 91 | 6.0 | 11.99 | 17.51 | 10 | .02 |
| Catastrophizing (C) | 1 | 75 | 1.0 | 5.13 | 10.76 | – | .01 |
| Hopelessness (H) | 1 | 84 | 1.0 | 8.46 | 16.71 | – | .03 |
| Coping: Positive thoughts (CPT) | 1 | 95 | 1.0 | 33.32 | 37.25 | 7 | .04 |
| Coping: Imagining pain outside the body (CIP) | 1 | 74 | 1.0 | 3.96 | 12.27 | 9 | .01 |
Med, Median; M, Mean; S, Standard Deviation; Lag AC, lag number with significant autocorrelation; P ADF, p value of the Augmented Dickey–Fuller test with the alternative hypothesis “time series is stationary”. All the variables are quantified on a 1–101 numeric scale. For AP, DI, N, T, D, PD, C, and H a higher score reflects higher somatic or psychological burden. For CPT and CIP, a higher score reflects an increased use of coping strategies

Time series of hopelessness, tension, catastrophizing, coping
The time series quantitatively reflect the free text descriptions of the patient. The highest scores in AP and DI were recorded between days 57 and 68 of the study period. In the free text passages of the diary the patient noted that she experienced the Christmas holidays (days 52–67) as a period of high stress and increased IBS pain. In addition, on days 59–61 she described the occurrence of menstrual cramps together with IBS-associated pain and impairment.
Table Table2 2 summarizes characteristics of somatic and psychological and coping time series. In the majority of cases all of the series except “Coping with positive thoughts” (CPT) ranged between 1 and 20 on the 100-point scale, with high values observed about 10% of the time. CPT values alternated between very low and high with values equal on 1 out of 40 days, and values higher than 50 on 31 days. All series were stationary, i.e., exhibited no trends. Three series (tension, catastrophizing, and hopelessness) demonstrated no autocorrelations.
Table Table3 3 shows instantaneous correlations between the somatic and psychological (including coping) time series. In most cases, strong and positive correlations were observed. Interestingly, the relationship between psychological and coping variables with DI was stronger than with AP. The amount of predicted variance (R 2 ) from linear regressions with psychological and coping measures as dependent variables and somatic variables as predictors varied between 12 and 94%. The non-significant correlation between depressiveness and abdominal pain could be due to the very limited range of the variable depressiveness over the course of the 72 days.
Significant instantaneous correlations of somatization with psychological and coping variables
| Abdominal Pain | Daily Impairment | R | |
|---|---|---|---|
| Nervousness (N) | .24 | .63 | .41 |
| Tension (T) | .32 | .66 | .44 |
| Depressiveness (D) | - | .47 | .25 |
| Pain-associated discomfort (PD) | .97 | .61 | .94 |
| Catastrophizing (C) | .42 | .77 | .59 |
| Hopelessness (H) | .53 | .70 | .52 |
| Coping: Positive thoughts (CPT) | .43 | .55 | .34 |
| Coping: Imagining pain outside the body (CIP) | - | .33 | .12 |
R 2 , portion of predicted variance in psychological variables, from the regressions PV t = β 1 AP t + β 2 DI t + e t where PV, psychological/coping variable
Table Table4 4 summarizes the significant results of the VAR analyses for interdependencies between abdominal pain and psychological distress or coping strategies; only statistically significant findings from calculations for all possible combinations of variables are provided. Identified lagged or temporal relations showed mostly the same direction, indicating that previous values in the somatic variable (AP) were predictive of values in the psychological variables or coping strategies. The variance decomposition estimates show that somatic symptoms in the psychological (and coping) time series explain 12% to 41% of variability.
Significant temporal dependencies between psychological variables and abdominal pain
| Psychological /coping variable | Type of dependency | VAR order | Granger- Causality Test | % FEVD h = 10 | Instantaneous correlation | |
|---|---|---|---|---|---|---|
| F | p | |||||
| Nervousness (N) | SS → N | 2 | 3.39 | .04 | .17 | .24 |
| Tension (T) | SS → T | 2 | 9.49 | < .01 | .31 | .32 |
| Catastrophizing (C) | SS → C | 2 | 16.3 | < .01 | .41 | .42 |
| Hopelessness (H) | SS → H | 2 | 6.04 | < .01 | .35 | .53 |
| Coping: Positive Thoughts (CPT) | SS → CPT | 1 | 8.09 | < .01 | .24 | .43 |
| CPT → SS | 1 | 4.34 | .04 | .06 | ||
| Coping: Imagining pain outside the body (CIP) | SS → CIP | 2 | 3.74 | .03 | .12 | .07 |
SS, somatic symptoms, measured by the item “How severe is your abdominal (tummy) pain”
A significant Granger Test implies that the first variable has impact on the second variable. The test statistic is F(df 1 ,df 2 ), where df 1 is a number of tested restrictions (k) and df 2 = 2 T − 4 k − 2 for bivariate VAR models, T is length of time series, k is order of VAR model. Forecast Error Variance (FEV) Decomposition estimates the amount of variance in a dependent variable, explained by a corresponding cause variable during a period h; h = 10 means 10 days
Figure 3 visualizes responses of psychological states and coping strategies to increases in AP; it shows that psychological and coping aspects reacted with higher symptoms to an increase in AP. For instance, increasing AP caused a strong delayed increase in catastrophizing: + 0.60 standard deviations, i.e., about 7 points on the 100-point scale.

Time lagged psychological variables
Table Table4 4 shows that the bivariate system, including AP and CPT, is characterized by a bidirectional or feedback predictive causality. AP Granger-caused CPT with 24% of explained variance, CPT Granger-caused AP with 6% of explained variance. Both series also correlated instantaneously: r = 0.43, R² = 18%.
Figure 4 visualizes the feedback relationship. An increase in AP caused more CPT next day. Intensified CPT resulted in less pain on the subsequent day: i.e., a decrease of 0.25 standard deviations, 4-point on the 100-point scale.

Cross-correlation and time lagged relationships: abdominal pain (AP) and coping with positive thoughts (CPT)
Discussion and conclusion
This is the first study to investigate the temporal relationships between somatic and psychological variables on a daily basis. We analyzed a female patient with IBS in her mid-twenties with symptoms of diarrhea, flatulence, and abdominal pain. She reported stress-related IBS symptoms as well as symptom related fears. In most variables, strong same-day correlations between somatic (especially daily impairment) and psychological (including coping) time series were observed. The day-lagged relationships indicated that higher values in abdominal pain on one day were predictive of higher values in psychological complaints (nervousness and tension) or of negative coping strategies (catastrophizing, hopelessness) on the following day. The use of positive thinking as a positive coping strategy was helpful in reducing the pain on the following days.
All variables remained stationary—that is, time series exhibited no trends over the measured time period (72 days). In the study period, the patient did not receive additional psychotherapeutic treatment, nor did she report long-lasting stressors. Therefore, we did not expect her symptoms to change over a longer period of time. The stability of IBS symptoms is supported by literature that usually describes IBS as a chronic disease. The diagnostic criteria for IBS also imply some symptom stability, because the symptoms must occur for a period of at least 3 months (with an onset at least 6 months prior the diagnosis) [ 22 ]. In addition, for IBS, population-based studies report a remission rate of about 55% only over a period of more than 10 years [ 26 ]. In addition to the general stationary trend of the variables, individual outliers with more severe symptoms were visible (e.g. the Christmas Holidays on days 52–67).
The patient stated that stressful or stress-free episodes would influence her symptoms; this was also reflected in the same-day analysis. In the free text of the diary the patient also described that in specific stressful situations she was ashamed of her symptoms and related consequences. The high same-day correlations between the somatic (AP, DI) and psychological time series (nervousness, tension, depressiveness, catastrophizing, hopelessness) reflect this interdependency—which the patient is aware of—between IBS symptoms and psychological state. Interestingly, this correlation was even higher for DI, meaning that functionality is especially important. The interaction between somatic and psychological distress is also described in previous studies. Midenfjord et al. (2019), for instance, showed in a cross-sectional study that IBS patients with psychological distress demonstrated more severe somatic symptoms and a lower quality of life [ 27 ]. Varni et al. (2017) found in a sample of pediatric patients with functional gastrointestinal disorders that somatic symptoms were differentially related to decreased health-related quality of life [ 28 ]. Another study reported a correlation between pain intensity and intensity of psychopathological symptoms (such as low spirits or anxiety) in IBS patients [ 29 ] while Dong et al. (2020) showed that IBS symptom severity predicted health-related quality of life influenced by stressful life events [ 30 ]. Interestingly, there is evidence that this association between current abdominal symptoms and psychological distress is not limited to functional gastrointestinal diseases but can also be seen in inflammatory bowel diseases [ 31 ]. The underlying physiological mechanism for the interaction between somatic and psychological distress could be explained by the concept of the (microbiome-) gut-brain axis. The (microbiome-)gut-brain axis refers to the complex network of connections between the microbiota, the enteric nervous system, and the central nervous system. [ 3 , 4 , 32 , 33 ]. Previous research has shown that the link between gastrointestinal symptoms and psychological distress could be based on a complex and bidirectional interaction between biological, psychological, and social factors [ 5 ]. For example, visceral hypersensitivity and an enhanced perceptual response to gastrointestinal sensations can trigger gastrointestinal specific anxiety [ 5 , 32 ]. On the other hand, psychosocial distress can lead, for instance, to an activation of the enteric and autonomic nervous system, which may trigger a change in smooth muscle activity or glandular secretion thus leading to IBS-symptoms. [ 32 ].
In addition to the daily correlation, it is also useful to look at day-to-day relationships in order to make time-delayed effects more visible and to answer the question whether or not psychological complaints precede IBS complaints, or vice versa. In literature, both perspectives are described for mental illnesses and IBS [ 6 – 8 ]. However, for this particular patient we found a strong time-delayed relationship between IBS symptoms, the following psychological complaints (nervousness, tension), and negative coping strategies (catastrophizing, hopelessness). This shows that having abdominal pain on one day was associated with more psychological stress the next day, not vice versa. This is in line with another study showing the temporal relationship that abdominal symptoms lead to increased stress and negative affect, while increased daily life stressors even lowered the IBS-symptoms [ 34 ]. This is interesting, as in literature frequently the opposite temporal direction or a feedback-loop is assumed [ 35 ]. Patel et al. (2016), for instance, investigated the relationship between sleep, mood and somatic symptoms in a sample of IBS patients and healthy controls over the course of 7 days [ 36 ]. In IBS patients, sleep disturbances were predictive for abdominal pain on the following day. Additional analyses showed that the sleep effects on abdominal pain in IBS patients could be mediated by depression and anxiety [ 36 ].
The question arises why our data show that the patient first develops gastrointestinal complaints and only afterwards psychological complaints. The patient herself had the impression that increased stress would lead to an increase in symptoms. For instance, during the short stressful event of applying for a new job the patient reported an onset of IBS complaints. She also reported that in this case the immediate application of a coping strategy (such as calming down) had helped her to reduce the symptoms. However, this sequence occurred over the course of only several hours—and would thus be reflected in the high same-day correlations of the time series (and not in the day-lagged correlations). On the other hand, shorter time intervals had been tested in Chan's study with an outcome similar to ours [ 34 ]. It is also possible that shorter daily stressors could also lead to a distraction from the IBS-symptoms, while longer stressors (like Christmas Holidays in the case of our study) may lead to an increase in symptoms.
Another interesting approach to feelings and symptoms of IBS is the concept of alexithymia. This concept states, among others, that feelings in IBS-patients may be misinterpreted as negative bodily sensations [ 37 ]. For our patient, this could mean that in stressful situations (such as job search or exam phases) she may initially perceive her feelings only physically and interpret them as a preliminary stage of a new outbreak of her IBS. The hyper-focus on the symptoms could initially intensify them. Shortly afterwards, the patient may get negative feelings from the IBS symptoms themselves.
The time-lagged correlation between IBS complaints and the following psychological complaints and negative coping strategies could be related to the patient’s social anxiety and the pressure to perform. In the free text of the diary the patient described that with the occurrence of abdominal complaints she would fear that soft bowel movements would follow, and that she would not be able to reach a toilet in a timely manner; she also felt ashamed when she had to leave certain events because of her IBS symptoms. Physiologically, this relationship between IBS complaints and following psychological distress could again be explained by the (microbiome-)gut-brain axis [ 5 , 32 ]. The occurrence of abdominal complaints (maybe as an expression of visceral hypersensitivity) can trigger gastrointestinal specific anxiety and the autonomic nervous systems as well as the hypothalamic pituitary axis are sending stress signals to the gut, resulting, among others, in a higher bowel motility and secretion leading to diarrhea and pain [ 32 ].
Interestingly, abdominal pain was not associated with a depressive feeling in general, but with negative processing (such as hopelessness and catastrophizing) as well as tense or anxious arousal (nervousness, tension). These negative feelings and coping strategies had no effect on the patient’s increased abdominal pain the next day; in contrast, the use of positive coping strategies was helpful.
The patient reported using positive coping strategies to reduce her symptoms; this was also seen in the data analysis. The intensified use of a specific coping strategy on one day (thinking of things the patient enjoyed doing) was followed by a decrease in pain on the subsequent day. Conversely, an increase in pain was followed by an increased use of this coping strategy. This corresponds to the clinical impression and the self-report of the patient: She considered relaxation techniques and new coping strategies such as distraction as beneficial for her condition. This result is supported by literature that considers psychotherapeutic treatment, including positive coping strategies, as a possible treatment of IBS [ 38 ].
In summary, the results of the time series analysis partly reflect the self-report of the patient as well as the clinical impression of the outpatient caretaker. However, our results expand upon these insights by showing temporal relationships between IBS symptoms and psychological variables over consecutive days—with psychological changes following changes in abdominal pain and related impairment. In addition, a mutual day-lagged relationship between IBS symptoms and coping could be detected.
This study has several implications: Overall, it shows that at the very least this patient is aware of her individual process of personal change, her fears, and her coping strategies––all of which to a large extent, could be confirmed by the time series analysis––an analysis that also provided additional information. This supports the hypothesis that individual characterizations are promising in terms of providing a better understanding of specific mechanisms, as well as an understanding of how temporal interactions between IBS symptoms and psychological symptoms are related. In clinical practice, practitioners should consider individual explanatory models of aggravating factors and coping strategies and stay open to psychosomatic as well as somatopsychic mechanisms. Previous psychological treatment recommendations for IBS patients concluded that a change in illness-specific cognitions as well as gastrointestinal anxiety as key mechanisms may have an effect on the outcomes of IBS symptom severity and quality of life [ 39 ]. In this case study, only positive thinking had a time-lagged effect on a decrease in abdominal pain, while catastrophizing and hopelessness were a result of having abdominal pain previously. Although it is not possible to generalize the results of an individual case, this supports the fact that treatments which more directly target abdominal symptoms (e.g., hypnotherapy) may have promising effects on IBS symptoms as well as associated psychological complaints. Therefore, a disorder-oriented integrative group intervention for IBS with gut-directed hypnotherapy seems promising [ 15 ].
From a methodological point of view, we have to point out that the here applied concept of Granger-causality does not equal causality. Causality according to Hill [ 40 ] can be assessed by using the following 9 criteria: strength, consistency, specificity, temporality, biological gradient, plausibility, coherence, experiment, analogy. The definition of Granger-causality, however, implies only that previous values of a time series X (e.g. somatic symptoms) improve prediction of future values of another series Y (e.g. nervousness of the patient). It does not imply the causality of X for Y.
Our study has several limitations. Firstly, we examined only one patient suffering from IBS; the generalizability of the results is therefore limited. We cannot simply transfer the results to other IBS patients but must carefully investigate further patient samples in regard to temporal relationships and interactions between somatic and psychological variables. Secondly, we were able to detect day-to-day changes only; shorter periods of time could not be captured. Nevertheless, previous studies mainly focused on longer time periods which is why this approach is still more advantageous in terms of capturing the direct relationships. Nevertheless, we were able to show a clear picture of a single IBS-patient. This is helpful as IBS is a complex illness with, in all likelihood, heterogeneous genesis and factors. A comprehensive case study could help identify subclasses of IBS to arrive at a better treatment and avoid dilution effects.
In conclusion we found in the presented case that somatic symptoms temporally precede psychological complaints. In addition, for this patient, the use of positive thoughts as a coping strategy was helpful in reducing pain. Further analyses should be conducted to verify if these relationships can be found in other patients who suffer from IBS symptoms.
Acknowledgements
The authors thank the participating patient and the contributing research assistants.
Abbreviations
| IBS | Irritable bowel syndrome |
| AP | Abdominal pain |
| DI | IBS-associated daily impairment |
| N | Nervousness |
| T | Tension |
| D | Depressiveness |
| PD | Pain-associated discomfort |
| C | Catastrophizing |
| H | Hopelessness |
| CPT | Coping with positive thoughts |
| CIP | Coping with imagining pain outside the body |
Authors' contributions
BW, FE, ES and RS conceived and designed the study. FE, SB, ES and RS collected the data. TS statistically analyzed and all authors interpreted the data. FE, BW and TS drafted the manuscript. All authors critically revised the manuscript and provided important intellectual content. All authors read and approved the final manuscript.
Open Access funding enabled and organized by Projekt DEAL.
Availability of data and materials
Declarations.
The study was approved by the medical ethics committee of the University Hospital Heidelberg.
The patient gave written informed consent for analysis and publication of the data.
The authors declare that they have no competing interests.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

COMMENTS
Introduction. Irritable bowel syndrome (IBS) is the most prevalent gastrointestinal (GI) diagnosis with a world-wide prevalence of 14% 1.It is a functional GI disorder characterized by bloating, diarrhea, constipation, abdominal pain, and presents with a high prevalence of psychological comorbidity of depression and anxiety. 2 The pathophysiology of IBS is marked by complex interactions ...
Case Presentation SN is a 32-year-old white woman who presents with symptoms of recurrent abdominal pain and loose stools. ... The hallmark symptoms of irritable bowel syndrome (IBS) are abdominal pain or discomfort associated with at least two of the following characteristics: (1) pain or discomfort associated with a change in the form of the ...
The IBS in America survey showed that three-quarters of per - sons with IBS symptoms tried an average of 3.6 nonprescrip-tion products before seeking medical care. 8,9 Abdominal pain was the most common reason people sought medical care. CASE STUDY 1 SC is a 25-year-old woman with symptoms of constipation that
A case-control study investigated the predictive accuracy of a 10-biomarker algorithm for differentiating IBS from non-IBS; sensitivity and specificity were 50% and 88%, respectively . Low sensitivity would render these tests inadequate for routine use.
Irritable bowel syndrome (IBS) is a highly prevalent disorder that reduces patients' quality of life and imposes a significant economic burden to the healthcare system. The prevalence of IBS in the United States is estimated to be 9 -22%, 1 - 3 and the yearly incidence is approximately 1.5%. 4 IBS is one of the most common medical disorders ...
Irritable Bowel Syndrome (IBS) is a functional disorder marked by some gastrointestinal symptoms frequently associated with extradigestive symptoms with unknown organic causes. In this study the ...
Case Study: Irritable Bowel Syndrome Working Group A Journey Through Time Ninth Annual Patient-Reported Outcome Consortium Workshop April 25 - 26, 2018 • Silver Spring, MD. Disclaimer ... BM = bowel movement; IBS-C = irritable bowel syndrome with constipation; IBS-D = irritable bowel syndrome with diarrhea; IBS -M = mixed irritable bowel ...
Irritable bowel syndrome (IBS) appears to have a bidirectional interaction with both depressive and anxiety-related complaints. However, it remains unclear how exactly the psychological complaints, at the individual level, are related to somatic symptoms on a daily basis. This single case study investigates how somatic and psychological variables are temporally related in a patient with ...
Case Study Series Gastroenterology & Hepatology October 2023 ... Results from the BURDEN IBS-C study published in 2018 echoed that health care providers shared their Table 3. Multifactorial Pathophysiology of IBS-C9-14 ... IBS-C, irritable bowel syndrome with constipation. Table 2. Diagnostic Criteria for IBS-C1-4
Licensed User Case Access. Toggle Navigation. ≡; HOME
Irritable bowel syndrome case study A 43-year-old woman with a history of recurrent abdominal pain for 25 years, loose stool, fecal urgency. In the last 1-2 years, her symptoms have worsened and she experienced severe abdomen pain, fecal urgency, and inconsistency along with 6 to 8 times loose bowel movements per day.
serologic testing because IBS-D can mimic this disorder. 9 CASE STUDY (CONTINUED) A detailed history ruled out warning signs for other organic dis-eases. Further information to quantify the duration and frequency of symptoms, the proportion of days with symptomatic stools, TABLE 2 Alarm signs/symptoms that warrant further investigation3,8
The irritable bowel syndrome ... Sharp, D. Risk of ovarian cancer in women with symptoms in primary care: population based case-control study. BMJ 2009;339:b2998-b2998. Crossref. PubMed. ISI.
We identified 45 studies, comprising 21,421 individuals with enteritis, followed for 3 months to 10 years for development of IBS. The pooled prevalence of IBS at 12 months after infectious enteritis was 10.1% (95% confidence interval [CI], 7.2−14.1) and at more than 12 months after infectious enteritis was 14.5% (95% CI, 7.7−25.5).
Irritable bowel syndrome (IBS) is a functional disorder characterized by frequent abdominal pain, ... This case-control study was approved by the Ethics Committee of the National Nutrition and Food Technology Research Institute (NNFTRI), with the ethics number of NNFTRI206. Study participants included ninety patients with IBS, and 355 healthy ...
In Anthony's case, the Goodpath process took the unique details of his condition, like his IBS severity and the presence of anxiety, and matched those details to specific treatment options that were right for him. This was all supported by 1:1 video calls with his Goodpath health coach, who made modifications to his program as his health ...
A burden on both patients and the healthcare system, irritable bowel syndrome (IBS) is a prevalent condition that can result in high medical costs, frequent visits to the doctor, missed work, and anxiety and depression in the patient. ... An Evidence-based Approach to Therapy in IBS-D: A Case Study Compendium Gastroenterol Hepatol (N Y). 2010 ...
irritable bowel syndrome (IBS). The disruption occurring in the GBA determines the changes in intestinal motility and secretion, causes visceral hypersensitivity and leads to cellular alterations of the entero-endocrine and immune systems. Microbiota may interplay with multiple of these different pathophysiological IBS targets.5 Case study
Case study about the link between long-term proton pump inhibitor (PPI) use, such as omeprazole, and irritable bowel syndrome (IBS). This is George's story. ... playing a critical role in conditions such as irritable bowel syndrome and reflux disease. In addition, our gut lumen is primarily an acidic environment due to the presence of stomach ...
Patient Case A 36-year-old woman presents with persistent abdominal pain and constipation (Table 1). Upon inquiry, she states ... Management of IBS-C: A Case Study Anthony J. Lembo, MD Cleveland Clinic Vice Chair of Research, Digestive Disease Institute Cleveland, Ohio recommendation of a friend. She reports that the low-
Among 3950 COVID-19 patients and 991 controls, 7.2% of COVID-19 patients and 4.9% of healthy controls developed IBS. Of the four case-control studies reporting post-COVID-19 IBS, patients with COVID-19 were 2.65 (95% confidence interval [CI] 0.538 to 13.039) times more likely to have post-COVID-19 IBS as compared to healthy controls. ...
Case study 3 : Irritable Bowel Syndrome (IBS), Male, 41 years old. Fair health state, IBS in history 15 years, followed by a low back injury at age of 15, injury of cervical spine later in life. Not taking any medication, in the past was taking anti-inflammatory and immodium. Diet is not great, drinking cider, wine, eating spicy foods.
IBS: case study. main symptoms of IBS. Click the card to flip 👆. -abdomial pain/cramps that may be relieved after a BM. -bloating. -diarrhea/constipation sometimes both, just one. -hypersecretion of colonic mucous. -dyspeptic symptoms (faltulence, nausea, anorexia) -anxiety/depression.
"Many patients consult gastroenterologists thinking they might have an IBD or IBS, and are eventually diagnosed to have the other condition, or some other illness such as a gastroenteritis (infection) instead," said Dr Wee. "Much of the confusion stems from the fact that both conditions may present with abdominal pain, diarrhoea or a change in the bowel habit.
One review of 12 studies involving 835 people with IBS found that peppermint oil supplementation over a period of two to 12 weeks significantly improved symptoms like abdominal pain, bloating, and ...
Overview of IBS. In 2016, the fourth iteration of the Rome Diagnostic Criteria for Irritable Bowel Syndrome (IBS; Rome IV criteria) was released (Table 2). 1 Developed by expert consensus, the Rome IV criteria incorporated key changes designed to improve their clinical utility and to reflect an increased understanding of IBS pathophysiology.In the Rome IV criteria, IBS is defined as a disorder ...
A new study suggests that regularly walking for exercise may increase the time between low back pain episodes and decrease disability time. ... Or, stack brushing your teeth in the morning with doing a set of push-ups, squats and plank. In this case, brushing your teeth is the trigger for doing some exercises—not necessarily at the same time ...
This case study has, for the first time, applied a longitudinal time series design to a patient with IBS. Study objectives of this single-case analysis were: (1) to explore temporal relationships and interactions between the somatic and psychological complaints of the patient and (2) to investigate the impact of personal coping strategies on ...