An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
ten Cate O, Custers EJFM, Durning SJ, editors. Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students [Internet]. Cham (CH): Springer; 2018. doi: 10.1007/978-3-319-64828-6_1


Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students [Internet].
Chapter 1 introduction.
Olle ten Cate .
Affiliations
Published online: November 7, 2017.
This chapter introduces the concept of clinical reasoning. It attempts to define what clinical reasoning is and what its features are. Solving clinical problems involves the ability to reason about causality of pathological processes, requiring knowledge of anatomy and the working and pathology of organ systems, and it requires the ability to compare patient problems as patterns with instances of illness scripts of patients the clinician has seen in the past and stored in memory.
The purpose of the book, supporting the teaching of clinical reasoning before students enter the clinical arena, faces the paradoxical problem of the lack of clinical experience that is so essential for building proficiency in clinical reasoning. So where to start if students are to be best prepared for first clinical encounters?
The method of case-based clinical reasoning is summarized and explained in its potential to provide early rudimentary illness scripts through elaboration and systematic discussion of the courses of action between the initial presentation of the patient and the final steps of clinical management. Meanwhile, the method requires student to apply knowledge of anatomy, physiology, and pathology.
The CBCR method has been applied successfully in several medical schools over a period of decades, and support for its validity is provided.
This chapter provides a general background and summarizes the CBCR method.
Clinical reasoning is a professional skill that experts agree is difficult and takes time to acquire, and, once you have the skill, it is difficult to explain what you actually do when you apply it—clinical reasoning then sometimes even feels as an easy process. The input, a clinical problem or a presenting patient, and the outcome, a diagnosis and/or a plan for action, are pretty clear, but what happens in the doctor’s mind in the meantime is quite obscure. It can be a very short process, happening in seconds, but it can also take days or months. It can require deliberate, painstaking thinking, consultation of written sources, and colleague opinions, or it may just seem to happen effortless. And “reasoning” is such a nicely sounding word that doctors would agree captures what they do, but is it always reasoning? Reasoning sounds like building a chain of thoughts, with causes and consequences, while doctors sometimes jump at a conclusion, sometimes before they even realize they are clinically reasoning. Is that medical magic? No, it’s not. Laypeople do the same. Any adult witnessing a motorcycle accident and seeing a victim on the street showing a lower limb in a strange angle will instantly “reason” the diagnosis is a fracture. Other medical conditions are less obvious and require deep thinking or investigations or literature study. Whatever presentation, doctors need to have the requisite skills to tackle the medical problems of patients that are entrusted to their care. No matter how obscure clinical reasoning is, students need to acquire that ability. So how does a student begin to learn clinical reasoning? How must teachers organize the training of students?
Case-based clinical reasoning (CBCR) education is a design of training of preclinical medical students, in small groups, in the art of coping with clinical problems as they are encountered in practice. As will be apparent from the description later in this chapter, CBCR is not identical to problem-based learning (Barrows and Tamblyn 1980 ), although some features (small groups, no traditional teacher role) show resemblance. While PBL is intended as a method to arrive at personal educational objectives and subsequently acquire new knowledge (Schmidt 1983 ), CBCR has a focus on training in the application of systematically acquired prior knowledge, but now in a clinical manner. It aims at building illness scripts—mental representations of diseases—while at the same time supports the acquisition of a diagnostic thinking habit. CBCR is not an algorithm or a heuristic to be used in clinical practice to efficiently solve a new medical problem. CBCR is no more and no less than educational method to acquire clinical reasoning skill. That is what this book is about.
The elaboration of the method (Part II and III of the book) is preceded in Part I by chapters on the general background of clinical reasoning and its teaching.
- What Is Clinical Reasoning?
Clinical reasoning is usually defined in a very general sense as “The thinking and decision -making processes associated with clinical practice” (Higgs and Jones 2000 ) or simply “diagnostic problem solving” (Elstein 1995 ).
For the purpose of this book, we define clinical reasoning as the mental process that happens when a doctor encounters a patient and is expected to draw a conclusion about (a) the nature and possible causes of complaints or abnormal conditions of the patient, (b) a likely diagnosis, and (c) patient management actions to be taken. Clinical reasoning is targeted at making decisions on gathering diagnostic information and recommending or initiating treatment. The mental reasoning process is interrupted to collect information and resumed when this information has arrived.
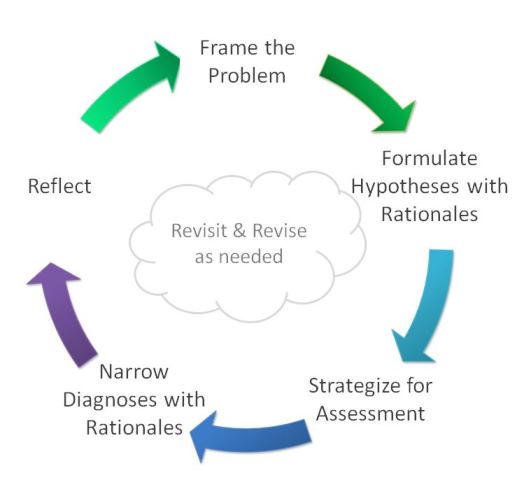
It is well established that clinicians have a range of mental approaches to apply. Somewhat simplified, they are categorized in two thinking systems, sometimes subsumed under the name dual-process theory (Eva 2005 ; Kassirer 2010 ; Croskerry 2009 ; Pelaccia et al. 2011 ). Based in the work of Croskerry ( 2009 ) and the Institute of Medicine (Balogh et al. 2015 ), Fig. 1.1 shows a model of how clinical reasoning and the use of System 1 and 2 thinking can be conceptualized graphically.
A model of clinical reasoning (Adapted from Croskerry 2009)
The first thinking approach is rapid and requires little mental effort. This mode has been called System 1 thinking or pattern recognition , sometimes referred to as non-analytical thinking. Pattern recognition happens in various domains of expertise. Based on studies in chess, it is estimated that grand master players have over 50,000 patterns available in their memory, from games played and games studied (Kahneman and Klein 2009 ). These mental patterns allow for the rapid comparison of a pattern in a current game with patterns stored in memory and for a quick decision which move to make next. This huge mental library of patterns may be compared with the mental repository of illness scripts that an experienced clinician has and that allows for the rapid recognition of a pattern of signs and symptoms in a patient with patients encountered in the past (Feltovich and Barrows 1984 ; Custers et al. 1998 ). See Box 1.1 .
Box 1.1 Illness Script
An illness script is a general representation in the physician’s mind of an illness. An illness script includes details on typical causal or associated preceding features (“enabling conditions”); the actual pathology (“fault”); the resulting signs, symptoms, and expected diagnostic findings (“consequences”); and, added to the original illness script definition (Feltovich and Barrows 1984 ), the most likely course and prognosis with suitable management options (“management”). An illness script may be stored as one comprehensive unit in the long-term memory of the physician. It can be triggered to be retrieved during new clinical encounters, to facilitate comparison and contrast, in order to generate a diagnostic hypothesis.
A mental matching process can lead to an instant recognition and generation of a hypothesis, if sufficient features of the current patient resemble features of a stored illness script.
Next to this rapid mental process, clinicians use System 2 thinking: the analytical thinking mode of presumed causes-and-effects reasoning that is slow and takes effort and is used when a System 1 process does not lead to an acceptable proposition to act. Analytic, often pathophysiological, thinking is typically the approach that textbooks of medicine use to explain signs and symptoms related to pathophysiological conditions in the human body. Both approaches are needed in clinical health care, to arrive at decisions and actions and to retrospectively justify actions taken. The two thinking modes can be viewed on a cognitive continuum between instant recognition and a reasoning process that may take a long time (Kassirer et al. 2010 ; Custers 2013 ). In routine medical practice, the rapid System 1 thinking prevails. This thinking often leads to correct decisions but is not infallible. However, the admonition to slow down the thinking when System 1 thinking fails and move to System 2 thinking may not lead to more accurate decisions (Norman et al. 2014 ). In fact, emerging fMRI studies seem to indicate that in complex cases, inexperienced learners search for rule-based reasoning solutions (System 2), while experienced clinicians keep searching for cases from memory (System 1) (Hruska et al. 2015 ).
- How to Teach Clinical Reasoning to Junior Students?
It is not exactly clear how medical students acquire clinical reasoning skills (Boshuizen and Schmidt 2000 ), but they eventually do, whether they had a targeted training in their curriculum or not. Williams et al. found a large difference in reasoning skill between years of clinical experience and across different schools (Williams et al. 2011 ). Even if reasoning skill would develop naturally across the years of medical training, it does not mean that educational programs cannot improve.
One way to approach the training of students in clinical reasoning is to focus on things that can go wrong in the practice of clinical reasoning and on threats to effective thinking in clinical care. Box 1.2 shows the most prevalent errors and cognitive biases in clinical reasoning (Graber et al. 2005 ; Kassirer et al. 2010 ). See also Chap. 3 .
Box 1.2 Summary of Prevalent Causes of Errors and Cognitive Biases
Errors (graber et al. 2005 ; kassirer et al. 2010 ).
Lack or faulty knowledge
Omission of, or faulty, data gathering and processing
Faulty estimation of disease prevalence
Faulty test result interpretation
Lack of diagnostic verification
Biases (Balogh et al. 2015 )
Anchoring bias and premature closure (stop search after early explanation)
Affective bias (emotion-based deviance from rational judgment)
Availability bias (dominant recall of recent or common cases)
Context bias (contextual factors that mislead)
In general, diagnostic errors are considered to occur too often in practice (McGlynn et al. 2015 ; Balogh et al. 2015 ), and it is important that student preparation for clinical encounters be improved (Lee et al. 2010 ). In a qualitative study, Audétat et al. observed five prototypical clinical reasoning difficulties among residents: generating hypotheses to guide data gathering, premature closure, prioritizing problems, painting an overall picture of the clinical situation, and elaborating a management plan (Audétat et al. 2013 ), not unlike the prevalent errors in clinical practice as summarized in Box 1.2 . Errors in clinical reasoning pertain to both System 1 and System 2 thinking and cognitive biases causing errors are not easily amenable to teaching strategies. An inadequate knowledge base appears the most consistent reason for error (Norman et al. 2017 ). A number of authors have recommended tailored teaching strategies for clinical reasoning (Rencic 2011 ; Guerrasio and Aagaard 2014 ; Posel et al. 2014 ). Most approaches pertain to education in the clinical workplace. Box 1.3 gives a condensed overview.
Let students
- Maximize learning by remembering many patient encounters.
- Recall similar cases as they increase experience.
- Build a framework for differential diagnosis using anatomy, pathology, and organ systems combined with semantic qualifiers: age, gender, ethnicity, and main complaint.
- Differentiate between likely and less likely but important diagnoses.
- Contrast diagnoses by listing necessary history questions and physical exam maneuvers in a tabular format and indicating what supports or does not support the respective diagnoses.
- Utilize epidemiology, evidence, and Bayesian reasoning.
- Practice deliberately; request and reflect on feedback; and practice mentally.
- Generate self-explanations during clinical problem solving.
- Talk in buzz groups at morning reports with oral and written patient data.
- Listen to clinical teachers reasoning out loud.
- Summarize clinical cases often using semantic qualifiers and create problem representations.
One dominant approach that clinical educators use when teaching students to solve medical problems is ask them to analyze pathophysiologically, in other words to use System 2 thinking. While this seems the only option with students who do not possess a mental library of illness scripts to facilitate System 1 thinking, those teachers teach something they usually do not do themselves when solving clinical problems This teaching resembles the “do as I say, not as I do” approach, in part because they simply cannot express “how they do” when they engaged in clinical reasoning.
In a recent review of approaches to the teaching of clinical reasoning, Schmidt and Mamede identified two groups of approaches: a predominant serial-cue approach (teachers provide bits of patient information to students and ask them to reason step by step) and a rare whole-task (or whole-case) approach in which all information is presented at once. They conclude that there is little evidence for the serial-cue approach, favored by most teachers and recommend a switch to whole-case approaches (Schmidt and Mamede 2015 ). While cognitive theory does support whole-task instructional techniques (Vandewaetere et al. 2014 ), the description of a whole-case in clinical education is not well elaborated. Evidently a whole-case cannot include a diagnosis and must at least be partly serial. But even if all the information that clinicians in practice face is provided to students all at once, the clinical reasoning process that follows has a serial nature, even if it happens quickly. Schmidt and Mamede’s proposal to first develop causal explanations, second to encapsulate pathophysiological knowledge, and third to develop illness scripts (Schmidt and Mamede 2015 ) runs the risk of separating biomedical knowledge acquisition from clinical training and regressing to a Flexnerian curriculum. Flexner advocated a strong biomedical background before students start dealing with patients (Flexner 1910 ). This separation is currently not considered the most useful approach to clinical reasoning education (Woods 2007 ; Chamberland et al. 2013 ).
Training students in the skill of clinical reasoning is evidently a difficult task, and Schuwirth rightly once posed the question “Can clinical reasoning be taught or can it only be learned?” (Schuwirth 2002 ). Since the work of Elstein and colleagues, we know that clinical reasoning is not a skill that is trainable independent of a large knowledge base (Elstein et al. 1978 ). There simply is not an effective and teachable algorithm of clinical problem solving that can be trained and learned, if there is no medical knowledge base. The actual reasoning techniques used in clinical problem solving can be explained rather briefly and may not be very different from those of a car mechanic. Listen to the patient (or the car owner), examine the patient (or the car), draw conclusions, and identify what it takes to solve the problem. There is not much more to it. In difficult cases, medical decision-making can require knowledge of Bayesian probability calculations, understanding of sensitivity and specificity of tests (Kassirer et al. 2010 ), but clinicians seldom use these advanced techniques explicitly at the bedside.
These recommendations are of no avail if students do not have background knowledge, both about anatomical structures and pathophysiological processes and about patterns of signs and symptoms related to illness scripts. When training medical students to think like doctors, we face the problem that we cannot just look how clinicians think and just ask students to mimic that technique. That is for two reasons: one is that clinicians often cannot express well how they think, and the second is simply that the huge knowledge base required to think like an experienced clinician is simply not present in students.
As System 1 pattern recognition is so overwhelmingly dominant in the clinician’s thinking (Norman et al. 2007 ), the lack of a knowledge base prohibits junior students to think like a doctor. It is clear that students cannot “recognize” a pattern if they do not have a similar pattern in their knowledge base. It is unavoidable that much effort and extensive experience are needed before a reasonable repository of illness scripts is built that can serve as the internal mirror of patterns seen in clinical practice. Ericsson’s work suggests that it may take up to 10,000 hours of deliberate practice to acquire expertise in any domain, although there is some debate about this volume (Ericsson et al. 1993 ; Macnamara et al. 2014 ). Clearly, students must see and experience many, many cases and construct and remember illness scripts. What a curriculum can try to offer is just that, i.e., many clinical encounters, in clinical settings or in a simulated environment. Clinical context is likely to enhance clinical knowledge, specifically if students feel a sense of responsibility or commitment (Koens et al. 2005 ; Koens 2005 ). This sense of commitment in practice relates to the patient, but it can also be a commitment to teach peers.
System 2 analytic reasoning is clearly a skill that can be trained early in a curriculum (Ploger 1988 ). Causal reasoning, usually starting with pathology (a viral infection of the liver) and a subsequent effect (preventing the draining of red blood cell waste products) and ending with resulting symptoms (yellow stains in the blood, visible in the sclerae of the eyes and in the skin, known as jaundice or icterus), can be understood and remembered, and the reasoning can include deeper biochemical or microbiological explanations (How does it operate the chemical degradation of hemoglobin? Which viruses cause hepatitis? How was the patient infected?). This basically is a systems-based reasoning process. The clinician however must reason in the opposite direction, a skill that is not simply the reverse of this chain of thought, as there may be very different causes of the same signs and symptoms (a normal liver, but an obstruction in the bile duct, or a normal liver and bile duct, but a profuse destruction of red blood cells after an immune reaction). So analytic reasoning is trainable, and generating hypotheses of what may have caused the symptoms requires a knowledge base of possible physiopathology mechanisms. That can be acquired step by step, and many answers to analytic problems can be found in the literature. But clearly, System 2 reasoning too requires prior knowledge. So both a basic science knowledge base and a mental illness script repository must be available.
The case-based clinical reasoning training method acknowledges this difficulty and therefore focuses on two simultaneous approaches (1) building illness scripts from early on in the curriculum, beginning with simple cases and gradually building more complex scripts to remember, and (2) conveying a systematic, analytic reasoning habit starting with patient presentation vignettes and ending with a conclusion about the diagnosis, the disease mechanism, and the patient management actions to be taken.
Summary of the CBCR Method
When applying these principles to preclinical classroom teaching, a case-based approach is considered superior to other methods (Kim et al. 2006 ; Postma and White 2015 ). Case-based clinical reasoning was designed at the Academic Medical Center of University of Amsterdam in 1992, when a new undergraduate medical curriculum was introduced (ten Cate and Schadé 1993 ; ten Cate 1994 , 1995 ). This integrated medical curriculum with multidisciplinary block modules of 6–8 weeks had existed since 10 years, but was found to lack a proper preparation of students to think like a doctor before entering clinical clerkships. Notably, while all block modules stressed the knowledge acquisition structured in a systematic way, usually based on organ systems and resulting in a systems knowledge base, a longitudinal thread of small group teaching was created to focus on patient-oriented thinking, with application of acquired knowledge (ten Cate and Schadé 1993 ). This CBCR training was implemented in curriculum years 2, 3, and 4, at both medical schools of the University of Amsterdam and the Free University of Amsterdam, which had been collaborating on curriculum development since the late 1980s. After an explanation of the method in national publications (ten Cate 1994 , 1995 ), medical schools at Leiden and Rotterdam universities adopted variants of it. In 1997 CBCR was introduced at the medical school of Utrecht University with minor modifications and continued with only little adaptations throughout major undergraduate medical curriculum changes in 1999, 2006, and 2015 until the current day (2017).
CBCR can be summarized as the practicing of clinical reasoning in small groups. A CBCR course consists of a series of group sessions over a prolonged time span. This may be a semester, a year, or usually, a number of years. Students regularly meet in a fixed group of 10–12, usually every 3–4 weeks, but this may be more frequent. The course is independent of concurrent courses or blocks. The rationale for this is that CBCR stresses the application of previously acquired knowledge and should not be programmed as an “illustration” of clinical or basic science theory. More importantly, when the case starts, students must not be cued in specific directions or diagnoses, which would be the case if a session were integrated in, say, a cardiovascular block. A patient with shortness of breath would then trigger too easily toward a cardiac problem.
CBCR cases, always titled with age, sex, and main complaint or symptom, consist of an introductory case vignette reflecting the way a patient presents at the clinician’s office. Alternatively, two cases with similar presentations but different diagnoses may be worked through in one session, usually later in the curriculum when the thinking process can be speeded up. The context of the case may be at a general practitioner’s office, at an emergency department, at an outpatient clinic, or at admission to a hospital ward. The case vignette continues with questions and assignments (e.g., What would be first hypotheses based on the information so far? What diagnostic tests should be ordered? Draw a table mapping signs and symptoms against likelihood of hypotheses ), at fixed moments interrupted with the provision of new findings about the patient from investigations (more extensive history, additional physical examination, or new results of diagnostic tests), distributed or read out loud by a facilitator during the session at the appropriate moment. A full case includes the complete course of a problem from the initial presentation to follow-up after treatment, but cases often concentrate on key stages of this course. Case descriptions should refer to relevant pathophysiological backgrounds and basic sciences (such as anatomy, biochemistry, cell biology, physiology) during the case.
The sessions are led by three (sometimes two) students of the group. They are called peer teachers and take turns in this role over the whole course. Every student must act as a peer teacher at multiple sessions across the year. Peer teachers have more information in advance about the patient and disclose this information at the appropriate time during the session, in accordance with instructions they receive in advance. In addition, a clinician is present. Given the elaborated format and case description, this teacher only acts as a consultant, when guidance is requested or helpful, and indeed is called “consultant” throughout all CBCR education.
Study materials include a general study guide with explanations of the rules, courses of action, assessment procedures, etc. (see Chap. 10 ): a “student version ” of the written CBCR case material per session, a “peer teacher version” of the CBCR case per session with extra information and hints to guide the group, and a full “consultant version” of the CBCR case per session. Short handouts are also available for all students, covering new clinical information when needed in the course of the diagnostic process. Optionally, homemade handouts can be prepared by peer teachers. The full consultant version of the CBCR case includes all answers to all questions in detail, sufficient to enable guidance by a clinician who is not familiar with the case or discipline, all suggestions and hints for peer teachers, and all patient information that should be disclosed during the session. Examples are shown in Appendices of this book.
Students are assessed at the end of the course on their knowledge of all illnesses and to a small extent on their active participation as a student and a peer teacher (see Chap. 7 ).
- Essential Features of CBCR Education
While a summary is given above, and a detailed procedural description is given in Part II, it may be helpful to provide some principles to help understand some of the rationale behind the CBCR method.
Switching Between System-Oriented Thinking and Patient-Oriented Thinking
It is our belief that preclinical students must learn to acquire both system-oriented knowledge and patient-oriented knowledge and that they need to practice switching between both modes of thinking (Eva et al. 2007 ). In that sense, our approach not only differs from traditional curricula with no training in clinical reasoning but also from curricula in which all education is derived from clinical presentations (Mandin et al. 1995 , 1997 ).
By scheduling CBCR sessions spread over the year, with each session requiring the clinical application of system knowledge of previous system courses, this practice of switching is stimulated. It is important to prepare and schedule CBCR cases carefully to enable this knowledge application. It is inevitable, because of differential diagnostic thinking, that cases draw upon knowledge from different courses and sometimes knowledge that may not have been taught. In that case, additional information may be provided during the case discussion. Peer teachers often have an assignment to summarize relevant system information between case questions in a brief presentation (maximum 10 min), to enable further progression.
Managing Cognitive Load and the Development of Illness Scripts
Illness scripts are mental representations of disease entities combining three elements in a script (Custers et al. 1998 ; Charlin et al. 2007 ): (1) factors causing or preceding a disease, (2) the actual pathology, and (3) the effect of the pathology showing as signs, symptoms, and expected diagnostic findings. While some authors, including us, add (4) course and management as the fourth element (de Vries et al. 2006 ), originally the first three, “enabling conditions,” “fault,” and “consequences,” were proposed to constitute the illness script (Feltovich and Barrows 1984 ). Illness scripts are stored as units in the long-term memory that are simultaneously activated and subsequently instantiated (i.e., recalled instantly) when a pattern recognition process occurs based on a patient seen by a doctor. This process is usually not deliberately executed, but occurs spontaneously. Illness scripts have a temporal nature like a film script, because of their cause and effect features, which enables clinicians to quickly take a next step, suggested by the script, in managing the patient. “Course and management” can therefore naturally be considered part of the script.
A shared explanation why illness scripts “work” in clinical reasoning is that the human working memory is very limited and does not allow to process much more than seven units or chunks of information at a time (Miller 1956 ) and likely less than that. Clinicians cannot process all separate signs and symptoms, history, and physical examination information simultaneously—that would overload their working memory capacity, but try to use one label to combine many bits of information in one unit (e.g., the illness script “diabetes type II” combines its enabling factors, pathology, signs and symptoms, disease course, and standard treatment in one chunk). If necessary, those units can be unpacked in elements (Figs. 1.1 and 1.2 ).
One information chunk in the working memory may be decomposed in smaller chunks in the long-term memory (Young et al. 2014)
To create illness scripts stored in the long-term memory, students must learn to see illnesses as a unit of information. In case-based clinical reasoning education, students face complete patient scripts, i.e., with enabling conditions (often derived from history taking) to consequences (as presenting signs and symptoms). Although illness scripts have an implicit chronology, from a clinical reasoning perspective, there is an adapted chronology of (a) consequences → (b) enabling conditions → (c) fault and diagnosis → (d) course and management, as the physician starts out observing the signs and symptoms, then takes a history, performs a physical examination, and orders tests if necessary before arriving at a conclusion about the “fault.” To enable building illness script units in the long-term memory, students must start out with simple, prototype cases that can be easily remembered. CBCR aims to develop in second year medical students stable but still somewhat limited illness scripts. This still limited repository should be sufficient to quickly recognize the causes, symptoms, and management of a limited series of common illnesses, and handle prototypical patient problems in practice if they would encounter these, resonating with Bordage’s prototype approach (Bordage and Zacks 1984 ; Bordage 2007 ). See Chap. 3 . The assessment of student knowledge at the end of a CBCR course focuses on the exact cases discussed, including, of course, the differential diagnostic considerations that are activated with the illness script, all to reinforce the same carefully chosen illness scripts. The aim is to provide a foundation that enables the addition in later years of variations to the prototypical cases learned, to enrich further illness script formation and from there add new illness scripts. We believe that working with whole, but not too complex, cases in an early phase in the medical curriculum serves to help students in an early phase in the medical curriculum to learn to recognize common patterns.
Educational Philosophies: Active Reasoning by Oral Communication and Peer Teaching
A CBCR education in the format elaborated in this book reflects the philosophy that learning clinical reasoning is enhanced by reasoning aloud. The small group arrangement, limited to no more than about 12 students, guarantees that every student actively contributes to the discussion. Even when listening, this group size precludes from hiding as would be a risk in a lecture setting.
Students act as peer teachers for their fellow students. Peer teaching is an accepted educational method with a theoretical foundation (ten Cate and Durning 2007 ; Topping 1996 ). It is well known that taking the role of teacher for peers stimulates knowledge acquisition in a different and often more productive way than studying for an exam (Bargh and Schul 1980 ). Social and cognitive congruence concepts explain why students benefit from communicating with peers or near-peers and should understand each other better than when students communicate with expert teachers (Lockspeiser et al. 2008 ). The peer teaching format used in CBCR is an excellent way to achieve active participation of all students during small group education. An additional benefit of using peer teachers is that they are instrumental in the provision of just-in-time information about the clinical case for their peers in the CBCR group, e.g., as a result of a diagnostic test that was proposed to be ordered.
Case-based clinical reasoning has most of the features that are recommended by Kassirer et al.: “First, clinical data are presented, analyzed and discussed in the same chronological sequence in which they were obtained in the course of the encounter between the physician and the patient. Second, instead of providing all available data completely synthesized in one cohesive story, as is in the practice of the traditional case presentation, data are provided and considered on a little at a time. Third, any cases presented should consist of real, unabridged patient material. Simulated cases or modified actual cases should be avoided because they may fail to reflect the true inconsistencies, false leads, inappropriate cues, and fuzzy data inherent in actual patient material. Finally, the careful selection of examples of problem solving ensures that a reasonable set of cognitive concepts will be covered” (Kassirer et al. 2010 ). While we agree with the third condition for advanced students, i.e., in clerkship years, for pre-clerkship medical students, a prototypical illness script is considered more appropriate and effective (Bordage 2007 ). The CBCR method also matches well with most recommendations on clinical reasoning education (see Box 1.3 ).
Chapter 4 of this book describes six prerequisites for clinical reasoning by medical students in the clinical context: having clinical vocabulary, experience with problem representation, an illness script mental repository, a contrastive learning approach, hypothesis-driven inquiry skill, and a habit of diagnostic verification. The CBCR approach helps to prepare students with most of these prerequisites.
Indications for the Effectiveness of the CBCR Method
The CBCR method finds its roots in part in problem-based learning (PBL) and other small group active learning approaches. Since the 1970s, various small group approaches have been recommended for medical education, notably PBL (Barrows and Tamblyn 1980 ) and team-based learning (TBL) (Michaelsen et al. 2008 ). In particular PBL has gained huge interest in the 1980s onward, due to the developmental work done by its founder Howard Barrows from McMaster University in Canada and from Maastricht University in the Netherlands, which institution derived its entire identity to a large part from problem-based learning. Despite significant research efforts to establish the superiority of PBL curricula, the general outcomes have been somewhat less than expected (Dolmans and Gijbels 2013 ). However, many studies on a more detailed level have shown that components of PBL are effective. In a recent overviews of PBL studies, Dolmans and Wilkerson conclude that “a clearly formulated problem, an especially socially congruent tutor, a cognitive congruent tutor with expertise, and a focused group discussion have a strong influence on students’ learning and achievement” (Dolmans and Wilkerson 2011 ). These are components that are included in the CBCR method.
While there has not been a controlled study to establish the effect of a CBCR course per se, compared to an alternative approach to clinical reasoning training, there is some indirect support for its validity, apart from the favorable reception of the teaching model among clinicians and students over the course of 20 years and different schools. A recent publication by Krupat and colleagues showed that a “case-based collaborative learning” format, including small group work on patient cases with sequential provision of patient information, led to higher scores of a physiology exam and high appreciation among students, compared with education using a problem-based learning format (Krupat et al. 2016 ). A more indirect indication of its effectiveness is shown in a comparative study among three schools in the Netherlands two decades ago (Schmidt et al. 1996 ). One of the schools, the University of Amsterdam medical school, had used the CBCR training among second and third year students at that time (ten Cate 1994 ). While the study does not specifically report on the effects of clinical reasoning education, Schmidt et al. show how students of the second and third year in this curriculum outperform students in both other curricula in diagnostic competence.
CBCR as an Approach to Ignite Curriculum Modernization
Since 2005, the method of CBCR has been used as leverage for undergraduate medical curriculum reform in Moldova, Georgia, Ukraine, and Azerbaijan (ten Cate et al. 2014 ). It has proven to be useful in medical education contexts with heavily lecture-based curricula—likely because the method can be applied within an existing curriculum, causing little disruption, while also being exemplary for recommended modern medical education (Harden et al. 1984 ). It stimulates integration, and the method is highly student-centered and problem-based. While observing CBCR in practice, a school can consider how these features can also be applied more generally in preclinical courses. This volume provides a detailed description that allows a school to pilot CBCR for this purpose.
- Audétat, M.-C., et al. (2013). Clinical reasoning difficulties: A taxonomy for clinical teachers. Medical Teacher, 35 (3), e984–e989. Available at: http://www .ncbi.nlm.nih .gov/pubmed/23228082 . [ PubMed : 23228082 ]
- Balogh, E. P., Miller, B. T., & Ball, J. R. (2015). Improving diagnosis in healthcare . Washington, DC: The Institute of Medicine and the National Academies Press. Available at: http://www .nap.edu/catalog /21794/improving-diagnosis-in-health-care . [ PubMed : 26803862 ]
- Balslev, T., et al. (2015). Combining bimodal presentation schemes and buzz groups improves clinical reasoning and learning at morning report. Medical Teacher, 37 (8), 759–766. Available at: http: //informahealthcare .com/doi/abs/10.3109/0142159X .2014.986445 . [ PubMed : 25496711 ]
- Bargh, J. A., & Schul, Y. (1980). On the cognitive benefits of teaching. Journal of Educational Psychology, 72 (5), 593–604. [ CrossRef ]
- Barrows, H. S., & Tamblyn, R. M. (1980). Problem-based learning. An approach to medical education . New York: Springer.
- Bordage, G. (2007). Prototypes and semantic qualifiers: From past to present. Medical Education, 41 (12), 1117–1121. [ PubMed : 18045363 ] [ CrossRef ]
- Bordage, G., & Zacks, R. (1984). The structure of medical knowledge in the memories of medical students and general practitioners: Categories and prototypes. Medical Education, 18 (11), 406–416. [ PubMed : 6503748 ] [ CrossRef ]
- Boshuizen, H., & Schmidt, H. (2000). The development of clinical reasoning expertise. In J. Higg & M. Jones (Eds.), Clinical reasoning in the health professions (pp. 15–22). Butterworth Heinemann: Oxford.
- Bowen, J. L. (2006). Educational strategies to promote clinical diagnostic reasoning. The New England Journal of Medicine, 355 (21), 2217–2225. [ PubMed : 17124019 ] [ CrossRef ]
- Chamberland, M., et al. (2013). Students’ self-explanations while solving unfamiliar cases: The role of biomedical knowledge. Medical Education, 47 (11), 1109–1116. [ PubMed : 24117557 ] [ CrossRef ]
- Chamberland, M., et al. (2015). Self-explanation in learning clinical reasoning: The added value of examples and prompts. Medical Education, 49 , 193–202. [ PubMed : 25626750 ] [ CrossRef ]
- Charlin, B., et al. (2007). Scripts and clinical reasoning. Medical Education, 41 (12), 1178–1184. [ PubMed : 18045370 ] [ CrossRef ]
- Croskerry, P. (2009). A universal model of diagnostic reasoning. Academic Medicine: Journal of the Association of American Medical Colleges, 84 (8), 1022–1028. [ PubMed : 19638766 ] [ CrossRef ]
- Custers, E. J. F. M. (2013). Medical education and cognitive continuum theory: An alternative perspective on medical problem solving and clinical reasoning. Academic Medicine, 88 (8), 1074–1080. [ PubMed : 23807108 ] [ CrossRef ]
- Custers, E. J. F. M., Boshuizen, H. P. A., & Schmidt, H. G. (1998). The role of illness scripts in the development of medical diagnostic expertise: Results from an interview study. Cognition and Instruction, 14 (4), 367–398. [ CrossRef ]
- de Vries, A., Custers, E., & ten Cate, O. (2006). Teaching clinical reasoning and the development of illness scripts: Possibilities in medical education. [Dutch]. Dutch Journal of Medical Education, 25 (1), 2–2.
- Dolmans, D., & Gijbels, D. (2013). Research on problem-based learning: Future challenges. Medical Education, 47 (2), 214–218. Available at: http://www .ncbi.nlm.nih .gov/pubmed/23323661 . Accessed 26 May 2013. [ PubMed : 23323661 ]
- Dolmans, D. H. J. M., & Wilkerson, L. (2011). Reflection on studies on the learning process in problem-based learning. Advances in Health Sciences Education: Theory and Practice, 16 (4), 437–441. Available at: http://www .pubmedcentral .nih.gov/articlerender .fcgi?artid=3166125&tool =pmcentrez&rendertype=abstract . Accessed 11 Mar 2012. [ PMC free article : PMC3166125 ] [ PubMed : 21861136 ]
- Elstein, A. (1995). Clinical reasoning in medicine. In J. Higgs & M. Jones (Eds.), Clinical reasoning in the health professions (pp. 49–59). Oxford: Butterworth Heinemann.
- Elstein, A. S., Shulman, L. S., & Sprafka, S. A. (1978). Medical problem solving. In An analysis of clinical reasoning . Cambridge, MA: Harvard University Press.
- Ericsson, K. A., et al. (1993). The role of deliberate practice in the acquisition of expert performance. Psychological Review, 100 (3), 363–406. [ CrossRef ]
- Eva, K. W. (2005). What every teacher needs to know about clinical reasoning. Medical Education, 39 (1), 98–106. [ PubMed : 15612906 ] [ CrossRef ]
- Eva, K. W., et al. (2007). Teaching from the clinical reasoning literature: Combined reasoning strategies help novice diagnosticians overcome misleading information. Medical Education, 41 (12), 1152–1158. [ PubMed : 18045367 ] [ CrossRef ]
- Feltovich, P., & Barrows, H. (1984). Issues of generality in medical problem solving. In H. G. Schmidt & M. L. de Voider (Eds.), Tutorials in problem-based learning (pp. 128–170). Assen: Van Gorcum.
- Flexner, A., 1910. Medical Education in the United States and Canada. A report to the Carnegie Foundation for the Advancement of Teaching . Repr. ForgottenBooks. Boston: D.B. Updike, the Merrymount Press.
- Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165 (13), 1493–1499. [ PubMed : 16009864 ] [ CrossRef ]
- Guerrasio, J., & Aagaard, E. M. (2014). Methods and outcomes for the remediation of clinical reasoning. Journal of General Internal Medicine , 1607–1614. [ PMC free article : PMC4242871 ] [ PubMed : 25092006 ]
- Harden, R. M., Sowden, S., & Dunn, W. (1984). Educational strategies in curriculum development: The SPICES model. Medical Education, 18 , 284–297. [ PubMed : 6738402 ] [ CrossRef ]
- Higgs, J., & Jones, M. (2000). In J. Higgs & M. Jones (Eds.), Clinical reasoning in the health professions (2nd ed.). Woburn: Butterworth-Heinemann.
- Hruska, P., et al. (2015). Hemispheric activation differences in novice and expert clinicians during clinical decision making. Advances in Health Sciences Education, 21 , 1–13. [ PubMed : 26530736 ]
- Kahneman, D., & Klein, G. (2009). Conditions for intuitive expertise: A failure to disagree. The American Psychologist, 64 (6), 515–526. [ PubMed : 19739881 ] [ CrossRef ]
- Kassirer, J. P. (2010). Teaching clinical reasoning: Case-based and coached. Academic Medicine, 85 (7), 1118–1124. [ PubMed : 20603909 ] [ CrossRef ]
- Kassirer, J., Wong, J., & Kopelman, R. (2010). Learning clinical reasoning (2nd ed.). Baltimore: Lippincott Williams & Wilkins.
- Kim, S., et al. (2006). A conceptual framework for developing teaching cases: A review and synthesis of the literature across disciplines. Medical Education, 40 (9), 867–876. [ PubMed : 16925637 ] [ CrossRef ]
- Koens, F. (2005). Vertical integration in medical education. Doctoral dissertation, Utrecht University, Utrecht.
- Koens, F., et al. (2005). Analysing the concept of context in medical education. Medical Education, 39 (12), 1243–1249. [ PubMed : 16313584 ] [ CrossRef ]
- Krupat, E., et al. (2016). Assessing the effectiveness of case-based collaborative learning via randomized controlled trial. Academic Medicine, 91(5), 723–729. [ PubMed : 26606719 ]
- Lee, A., et al. (2010). Using illness scripts to teach clinical reasoning skills to medical students. Family Medicine, 42 (4), 255–261. [ PubMed : 20373168 ]
- Lockspeiser, T. M., et al. (2008). Understanding the experience of being taught by peers: The value of social and cognitive congruence. Advances in Health Sciences Education: Theory and Practice, 13 (3), 361–372. [ PubMed : 17124627 ] [ CrossRef ]
- Macnamara, B. N., Hambrick, D. Z., & Oswald, F. L. (2014). Deliberate practice and performance in music, games, sports, education, and professions: A meta-analysis. Psychological Science, 24 (8), 1608–1618. [ PubMed : 24986855 ] [ CrossRef ]
- Mandin, H., et al. (1995). Developing a “clinical presentation” curriculum at the University of Calgary. Academic Medicine, 70 (3), 186–193. [ PubMed : 7873005 ] [ CrossRef ]
- Mandin, H., et al. (1997). Helping students learn to think like experts when solving clinical problems. Academic Medicine, 72 (3), 173–179. [ PubMed : 9075420 ] [ CrossRef ]
- McGlynn, E. A., McDonald, K. M., & Cassel, C. K. (2015). Measurement is essential for improving diagnosis and reducing diagnostic error. JAMA, 314 , 1. [ PubMed : 26571126 ] [ CrossRef ]
- Michaelsen, L., et al. (2008). Team-based learning for health professions education . Sterling: Stylus Publishing, LLC.
- Miller, G. A. (1956). The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychological Review, 63 , 81–97. [ PubMed : 13310704 ] [ CrossRef ]
- Norman, G., Young, M., & Brooks, L. (2007). Non-analytical models of clinical reasoning: The role of experience. Medical Education, 41 (12), 1140–1145. [ PubMed : 18004990 ]
- Norman, G., et al. (2014). The etiology of diagnostic errors: A controlled trial of system 1 versus system 2 reasoning. Academic Medicine: Journal of the Association of American Medical Colleges, 89 (2), 277–284. [ PubMed : 24362377 ] [ CrossRef ]
- Norman, G. R., et al. (2017). The causes of errors in clinical reasoning: Cognitive biases, knowledge deficits, and dual process thinking. Academic Medicine, 92 (1), 23–30. [ PubMed : 27782919 ] [ CrossRef ]
- Pelaccia, T., et al. (2011). An analysis of clinical reasoning through a recent and comprehensive approach: The dual-process theory. Medical Education Online, 16 , 1–9. [ PMC free article : PMC3060310 ] [ PubMed : 21430797 ] [ CrossRef ]
- Ploger, D. (1988). Reasoning and the structure of knowledge in biochemistry. Instructional Science, 17 (1988), 57–76. [ CrossRef ]
- Posel, N., Mcgee, J. B., & Fleiszer, D. M. (2014). Twelve tips to support the development of clinical reasoning skills using virtual patient cases. Medical Teacher , 0 (0), 1–6.
- Postma, T. C., & White, J. G. (2015). Developing clinical reasoning in the classroom – Analysis of the 4C/ID-model. European Journal of Dental Education, 19 (2), 74–80. [ PubMed : 24810116 ] [ CrossRef ]
- Rencic, J. (2011). Twelve tips for teaching expertise in clinical reasoning. Medical Teacher, 33 (11), 887–892. Available at: http://www .ncbi.nlm.nih .gov/pubmed/21711217 . Accessed 1 Mar 2012. [ PubMed : 21711217 ]
- Schmidt, H. (1983). Problem-based learning: Rationale and description. Medical Education, 17 (1), 11–16. [ PubMed : 6823214 ] [ CrossRef ]
- Schmidt, H. G., & Mamede, S. (2015). How to improve the teaching of clinical reasoning: A narrative review and a proposal. Medical Education, 49 (10), 961–973. [ PubMed : 26383068 ] [ CrossRef ]
- Schmidt, H., et al. (1996). The development of diagnostic competence: Comparison of a problem-based, and integrated and a conventional medical curriculum. Academic Medicine, 71 (6), 658–664. [ PubMed : 9125924 ] [ CrossRef ]
- Schuwirth, L. (2002). Can clinical reasoning be taught or can it only be learned? Medical Education, 36 (8), 695–696. [ PubMed : 12191050 ] [ CrossRef ]
- ten Cate, T. J. (1994). Training case-based clinical reasoning in small groups [Dutch]. Nederlands Tijdschrift voor Geneeskunde, 138 , 1238–1243. [ PubMed : 8015623 ]
- ten Cate, T. J. (1995). Teaching small groups [Dutch]. In J. Metz, A. Scherpbier, & C. Van der Vleuten (Eds.), Medical education in practice (pp. 45–57). Assen: Van Gorcum.
- ten Cate, T. J., & Schadé, E. (1993). Workshops clinical decision-making. One year experience with small group case-based clinical reasoning education. In J. Metz, A. Scherpbier, & E. Houtkoop (Eds.), Gezond Onderwijs 2 – proceedings of the second national conference on medical education [Dutch] (pp. 215–222). Nijmegen: Universitair Publikatiebureau KUN.
- ten Cate, O., & Durning, S. (2007). Dimensions and psychology of peer teaching in medical education. Medical Teacher, 29 (6), 546–552. [ PubMed : 17978967 ] [ CrossRef ]
- ten Cate, O., Van Loon, M., & Simonia, G. (Eds.). (2014). Modernizing medical education through case-based clinical reasoning (1st ed.). Utrecht: University Medical Center Utrecht. with translations in Georgian, Ukrainian, Azeri and Spanish.
- Topping, K. J. (1996). The effectiveness of peer tutoring in further and higher education: A typology and review of the literature. Higher Education, 32 , 321–345. [ CrossRef ]
- Vandewaetere, M., et al. (2014). 4C/ID in medical education: How to design an educational program based on whole-task learning: AMEE guide no. 93. Medical Teacher, 93 , 1–17. [ PubMed : 25053377 ]
- Williams, R. G., et al. (2011). Tracking development of clinical reasoning ability across five medical schools using a progress test. Academic Medicine: Journal of the Association of American Medical Colleges, 86 (9), 1148–1154. [ PubMed : 21785314 ] [ CrossRef ]
- Woods, N. N. (2007). Science is fundamental: The role of biomedical knowledge in clinical reasoning. Medical Education, 41 (12), 1173–1177. [ PubMed : 18045369 ] [ CrossRef ]
- Young, J. Q., et al. (2014). Cognitive load theory: Implications for medical education: AMEE guide no. 86. Medical Teacher, 36 (5), 371–384. [ PubMed : 24593808 ] [ CrossRef ]
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
- Cite this Page ten Cate O. Introduction. 2017 Nov 7. In: ten Cate O, Custers EJFM, Durning SJ, editors. Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students [Internet]. Cham (CH): Springer; 2018. Chapter 1. doi: 10.1007/978-3-319-64828-6_1
- PDF version of this page (506K)
- PDF version of this title (3.4M)
In this Page
- Summary of the CBCR Method
- Indications for the Effectiveness of the CBCR Method
- CBCR as an Approach to Ignite Curriculum Modernization
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students [ 2018] Review Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students ten Cate O, Custers EJFM, Durning SJ. 2018
- Teaching clinical reasoning to medical students: A brief report of case-based clinical reasoning approach. [J Educ Health Promot. 2024] Teaching clinical reasoning to medical students: A brief report of case-based clinical reasoning approach. Alavi-Moghaddam M, Zeinaddini-Meymand A, Ahmadi S, Shirani A. J Educ Health Promot. 2024; 13:42. Epub 2024 Feb 26.
- Student and educator experiences of maternal-child simulation-based learning: a systematic review of qualitative evidence protocol. [JBI Database System Rev Implem...] Student and educator experiences of maternal-child simulation-based learning: a systematic review of qualitative evidence protocol. MacKinnon K, Marcellus L, Rivers J, Gordon C, Ryan M, Butcher D. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):14-26.
- Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. [Acad Med. 2000] Scripts and medical diagnostic knowledge: theory and applications for clinical reasoning instruction and research. Charlin B, Tardif J, Boshuizen HP. Acad Med. 2000 Feb; 75(2):182-90.
- Review Understanding Clinical Reasoning from Multiple Perspectives: A Conceptual and Theoretical Overview. [Principles and Practice of Cas...] Review Understanding Clinical Reasoning from Multiple Perspectives: A Conceptual and Theoretical Overview. ten Cate O, Durning SJ. Principles and Practice of Case-based Clinical Reasoning Education: A Method for Preclinical Students. 2018
Recent Activity
- Introduction - Principles and Practice of Case-based Clinical Reasoning Educatio... Introduction - Principles and Practice of Case-based Clinical Reasoning Education
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Clinical problem...
Clinical problem solving and diagnostic decision making: selective review of the cognitive literature
- Related content
- Peer review
This article has a correction. Please see:
- Clinical problem solving and diagnostic decision making: selective review of the cognitive literature - November 02, 2006
- Arthur S Elstein , professor ( aelstein{at}uic.edu ) ,
- Alan Schwarz , assistant professor of clinical decision making.
- Department of Medical Education, University of Illinois College of Medicine, Chicago, IL 60612-7309, USA
- Correspondence to: A S Elstein
This is the fourth in a series of five articles
This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential approaches: problem solving 1 , 2 , 3 and decision making. 4 , 5 , 6 , 7 , 8 Problem solving research was initially aimed at describing reasoning by expert physicians, to improve instruction of medical students and house officers. Psychological decision research has been influenced from the start by statistical models of reasoning under uncertainty, and has concentrated on identifying departures from these standards.
Summary points
Problem solving and decision making are two paradigms for psychological research on clinical reasoning, each with its own assumptions and methods
The choice of strategy for diagnostic problem solving depends on the perceived difficulty of the case and on knowledge of content as well as strategy
Final conclusions should depend both on prior belief and strength of the evidence
Conclusions reached by Bayes's theorem and clinical intuition may conflict
Because of cognitive limitations, systematic biases and errors result from employing simpler rather than more complex cognitive strategies
Evidence based medicine applies decision theory to clinical diagnosis
Problem solving
Diagnosis as selecting a hypothesis.
The earliest psychological formulation viewed diagnostic reasoning as a process of testing hypotheses. Solutions to difficult diagnostic problems were found by generating a limited number of hypotheses early in the diagnostic process and using them to guide subsequent collection of data. 1 Each hypothesis can be used to predict what additional findings ought to be present if it were true, and the diagnostic process is a guided search for these findings. Experienced physicians form hypotheses and their diagnostic plan rapidly, and the quality of their hypotheses is higher than that of novices. Novices struggle to develop a plan and some have difficulty moving beyond collection of data to considering possibilities.
It is possible to collect data thoroughly but nevertheless to ignore, to misunderstand, or to misinterpret some findings, but also possible for a clinician to be too economical in collecting data and yet to interpret accurately what is available. Accuracy and thoroughness are analytically separable.
Pattern recognition or categorisation
Expertise in problem solving varies greatly between individual clinicians and is highly dependent on the clinician's mastery of the particular domain. 9 This finding challenges the hypothetico-deductive model of clinical reasoning, since both successful and unsuccessful diagnosticians use hypothesis testing. It appears that diagnostic accuracy does not depend as much on strategy as on mastery of content. Further, the clinical reasoning of experts in familiar situations frequently does not involve explicit testing of hypotheses. 3 10 , 11 , 12 Their speed, efficiency, and accuracy suggest that they may not even use the same reasoning processes as novices. 11 It is likely that experienced physicians use a hypothetico-deductive strategy only with difficult cases and that clinical reasoning is more a matter of pattern recognition or direct automatic retrieval. What are the patterns? What is retrieved? These questions signal a shift from the study of judgment to the study of the organisation and retrieval of memories.
Problem solving strategies
Hypothesis testing
Pattern recognition (categorisation)
By specific instances
By general prototypes
Viewing the process of diagnosis assigning a case to a category brings some other issues into clearer view. How is a new case categorised? Two competing answers to this question have been put forward and research evidence supports both. Category assignment can be based on matching the case to a specific instance (“instance based” or “exemplar based” recognition) or to a more abstract prototype. In the former, a new case is categorised by its resemblance to memories of instances previously seen. 3 11 This model is supported by the fact that clinical diagnosis is strongly affected by context—for example, the location of a skin rash on the body—even when the context ought to be irrelevant. 12
The prototype model holds that clinical experience facilitates the construction of mental models, abstractions, or prototypes. 2 13 Several characteristics of experts support this view—for instance, they can better identify the additional findings needed to complete a clinical picture and relate the findings to an overall concept of the case. These features suggest that better diagnosticians have constructed more diversified and abstract sets of semantic relations, a network of links between clinical features and diagnostic categories. 14
The controversy about the methods used in diagnostic reasoning can be resolved by recognising that clinicians approach problems flexibly; the method they select depends upon the perceived characteristics of the problem. Easy cases can be solved by pattern recognition: difficult cases need systematic generation and testing of hypotheses. Whether a diagnostic problem is easy or difficult is a function of the knowledge and experience of the clinician.
The strategies reviewed are neither proof against error nor always consistent with statistical rules of inference. Errors that can occur in difficult cases in internal medicine include failure to generate the correct hypothesis; misperception or misreading the evidence, especially visual cues; and misinterpretations of the evidence. 15 16 Many diagnostic problems are so complex that the correct solution is not contained in the initial set of hypotheses. Restructuring and reformulating should occur as data are obtained and the clinical picture evolves. However, a clinician may quickly become psychologically committed to a particular hypothesis, making it more difficult to restructure the problem.
Decision making
Diagnosis as opinion revision.
From the point of view of decision theory, reaching a diagnosis means updating opinion with imperfect information (the clinical evidence). 8 17 The standard rule for this task is Bayes's theorem. The pretest probability is either the known prevalence of the disease or the clinician's subjective impression of the probability of disease before new information is acquired. The post-test probability, the probability of disease given new information, is a function of two variables, pretest probability and the strength of the evidence, measured by a “likelihood ratio.”
Bayes's theorem tells us how we should reason, but it does not claim to describe how opinions are revised. In our experience, clinicians trained in methods of evidence based medicine are more likely than untrained clinicians to use a Bayesian approach to interpreting findings. 18 Nevertheless, probably only a minority of clinicians use it in daily practice and informal methods of opinion revision still predominate. Bayes's theorem directs attention to two major classes of errors in clinical reasoning: in the assessment of either pretest probability or the strength of the evidence. The psychological study of diagnostic reasoning from this viewpoint has focused on errors in both components, and on the simplifying rules or heuristics that replace more complex procedures. Consequently, this approach has become widely known as “heuristics and biases.” 4 19
Errors in estimation of probability
Availability —People are apt to overestimate the frequency of vivid or easily recalled events and to underestimate the frequency of events that are either very ordinary or difficult to recall. Diseases or injuries that receive considerable media attention are often thought of as occurring more commonly than they actually do. This psychological principle is exemplified clinically in the overemphasis of rare conditions, because unusual cases are more memorable than routine problems.
Representativeness —Representativeness refers to estimating the probability of disease by judging how similar a case is to a diagnostic category or prototype. It can lead to overestimation of probability either by causing confusion of post-test probability with test sensitivity or by leading to neglect of base rates and implicitly considering all hypotheses equally likely. This is an error, because if a case resembles disease A and disease B equally, and A is much more common than B, then the case is more likely to be an instance of A. Representativeness is associated with the “conjunction fallacy”—incorrectly concluding that the probability of a joint event (such as the combination of findings to form a typical clinical picture) is greater than the probability of any one of these events alone.
Heuristics and biases
Availability
Representativeness
Probability transformations
Effect of description detail
Conservatism
Anchoring and adjustment
Order effects
Decision theory assumes that in psychological processing of probabilities, they are not transformed from the ordinary probability scale. Prospect theory was formulated as a descriptive account of choices involving gambling on two outcomes, 20 and cumulative prospect theory extends the theory to cases with multiple outcomes. 21 Both prospect theory and cumulative prospect theory propose that, in decision making, small probabilities are overweighted and large probabilities underweighted, contrary to the assumption of standard decision theory. This “compression” of the probability scale explains why the difference between 99% and 100% is psychologically much greater than the difference between, say, 60% and 61%. 22
Support theory
Support theory proposes that the subjective probability of an event is inappropriately influenced by how detailed the description is. More explicit descriptions yield higher probability estimates than compact, condensed descriptions, even when the two refer to exactly the same events. Clinically, support theory predicts that a longer, more detailed case description will be assigned a higher subjective probability of the index disease than a brief abstract of the same case, even if they contain the same information about that disease. Thus, subjective assessments of events, while often necessary in clinical practice, can be affected by factors unrelated to true prevalence. 23
Errors in revision of probability
In clinical case discussions, data are presented sequentially, and diagnostic probabilities are not revised as much as is implied by Bayes's theorem 8 ; this phenomenon is called conservatism. One explanation is that diagnostic opinions are revised up or down from an initial anchor, which is either given in the problem or subjectively formed. Final opinions are sensitive to the starting point (the “anchor”), and the shift (“adjustment”) from it is typically insufficient. 4 Both biases will lead to collecting more information than is necessary to reach a desired level of diagnostic certainty.
It is difficult for everyday judgment to keep separate accounts of the probability of a disease and the benefits that accrue from detecting it. Probability revision errors that are systematically linked to the perceived cost of mistakes show the difficulties experienced in separating assessments of probability from values, as required by standard decision theory. There is a tendency to overestimate the probability of more serious but treatable diseases, because a clinician would hate to miss one. 24
Bayes's theorem implies that clinicians given identical information should reach the same diagnostic opinion, regardless of the order in which information is presented. However, final opinions are also affected by the order of presentation of information. Information presented later in a case is given more weight than information presented earlier. 25
Other errors identified in data interpretation include simplifying a diagnostic problem by interpreting findings as consistent with a single hypothesis, forgetting facts inconsistent with a favoured hypothesis, overemphasising positive findings, and discounting negative findings. From a Bayesian standpoint, these are all errors in assessing the diagnostic value of clinical evidence—that is, errors in implicit likelihood ratios.
Educational implications
Two recent innovations in medical education, problem based learning and evidence based medicine, are consistent with the educational implications of this research. Problem based learning can be understood as an effort to introduce the formulation and testing of clinical hypotheses into the preclinical curriculum. 26 The theory of cognition and instruction underlying this reform is that since experienced physicians use this strategy with difficult problems, and since practically any clinical situation selected for instructional purposes will be difficult for students, it makes sense to provide opportunities for students to practise problem solving with cases graded in difficulty. The finding of case specificity showed the limits of teaching a general problem solving strategy. Expertise in problem solving can be separated from content analytically, but not in practice. This realisation shifted the emphasis towards helping students acquire a functional organisation of content with clinically usable schemas. This goal became the new rationale for problem based learning. 27
Evidence based medicine is the most recent, and by most standards the most successful, effort to date to apply statistical decision theory in clinical medicine. 18 It teaches Bayes's theorem, and residents and medical students quickly learn how to interpret diagnostic studies and how to use a computer based nomogram to compute post-test probabilities and to understand the output. 28
We have selectively reviewed 30 years of psychological research on clinical diagnostic reasoning. The problem solving approach has focused on diagnosis as hypothesis testing, pattern matching, or categorisation. The errors in reasoning identified from this perspective include failure to generate the correct hypothesis; misperceiving or misreading the evidence, especially visual cues; and misinterpreting the evidence. The decision making approach views diagnosis as opinion revision with imperfect information. Heuristics and biases in estimation and revision of probability have been the subject of intense scrutiny within this research tradition. Both research paradigms understand judgment errors as a natural consequence of limitations in our cognitive capacities and of the human tendency to adopt short cuts in reasoning.
Both approaches have focused more on the mistakes made by both experts and novices than on what they get right, possibly leading to overestimation of the frequency of the mistakes catalogued in this article. The reason for this focus seems clear enough: from the standpoint of basic research, errors tell us a great deal about fundamental cognitive processes, just as optical illusions teach us about the functioning of the visual system. From the educational standpoint, clinical instruction and training should focus more on what needs improvement than on what learners do correctly; to improve performance requires identifying errors. But, in conclusion, we emphasise, firstly, that the prevalence of these errors has not been established; secondly, we believe that expert clinical reasoning is very likely to be right in the majority of cases; and, thirdly, despite the expansion of statistically grounded decision supports, expert judgment will still be needed to apply general principles to specific cases.
Series editor J A Knottnerus
Preparation of this review was supported in part by grant RO1 LM5630 from the National Library of Medicine.
Competing interests None declared.
“The Evidence Base of Clinical Diagnosis,” edited by J A Knottnerus, can be purchased through the BMJ Bookshop ( http://www.bmjbookshop.com/ )
- Elstein AS ,
- Shulman LS ,
- Bordage G ,
- Schmidt HG ,
- Norman GR ,
- Boshuizen HPA
- Kahneman D ,
- Sox HC Jr . ,
- Higgins MC ,
- Mellers BA ,
- Schwartz A ,
- Chapman GB ,
- Sonnenberg F
- Glasziou P ,
- Pliskin J ,
- Brooks LR ,
- Coblentz CL ,
- Lemieux M ,
- Kassirer JP ,
- Kopelman RI
- Sackett DL ,
- Haynes RB ,
- Guyatt GH ,
- Richardson WS ,
- Rosenberg W ,
- Tversky A ,
- Fischhoff B ,
- Bostrom A ,
- Quadrell M J
- Redelmeier DA ,
- Koehler DJ ,
- Liberman V ,
- Wallsten TS
- Bergus GR ,

- About this site
- Curricular Affairs Contact
- FID Philosophy
- Faculty Mentoring
- Educational Program Objectives
- ARiM Initiatives
- Faculty Support
- Active Learning Theory
- Curriculum Development
- Developmental Learning Theory
- Peer Review of Teaching
- Resources & Strategies
- Flipped Learning
- Teaching Guides
- Educational Strategies
- Large Group Sessions
- Team Learning
- Constructive Feedback
- Ed Tech & Training
- Med Ed Distinction Track
- Affiliate Clinical Faculty
- Faculty Instructional Development Series
- Microskills 1-Min Preceptor
- BDA for Teaching
- Med Ed Resources
- RIME Framework
- WBA in Clerkship
- About Instructional Tech
- Software Worth Using
- Apps for Learning
- Apps for Teaching
- Apps for Research
- Copyright Resources
- Application Online
- Program Goals
- Program Competence Areas
- Program Timeline
- Program Activities
- Projects & Presentations
- Participants
- SOS Series Calendar
- Presentation Tools
- Communication Tools
- Data Collection & Analysis
- Document Preparation
- Project Management Tools
You are here
Structured approach to medical problem-solving.
To achieve the goals for the Clinical Reasoning Course, students learn a structured approach to medical problem solving that emphasizes the process skills, and combines self-regulation with collaborative/facilitated learning components. The idea is to promote deliberative self-regulation as well as the consultation of colleagues' ideas and perspectives while using a sy stematic approach to problem-solving .
The key to teaching problem-solving is effective problem-construction based on real-world situations that evince a range of cognitive dimensions and provide a framework or structure for solving them (Jonassen, 2000 ; also 2010 ).
The UA COM approach incorporates this stance in its structured approach to medical problem-solving, a hybrid of scientific method and Polya's ( 1954 ) model for problem-solving . ( Learn more about Polya's approach )
This 5-step medical problem-solving structure we use in the Clinical Reasoning Course (Figure below) is also inspired by the concept of evidence-based decision making, and is aligned with learning theory that underlies the developmental curriculum at the UA College of Medicine .
Problem-solving Step by Step
Each "step" focuses on the process of generating a desired outcome. For example, when students formulate hypotheses and articulate their reasoning for each, they are generating a list of provisional diagnoses.
We emphasize process by naming the step for how students will engage in producing that outcome, and not by the outcome itself.
By the time students work through a case they will have engaged in the kind of thinking and critical reflection highlighted by each step.
Why a structured approach?
The purpose of using a structured approach to medical problem-solving is to scaffold students' internalization of a systematic approach to clinical reasoning.
As students progress toward clinical years, they will need less scaffolding and greater challenges. The Clinical Reasoning Course is a longitudinal learning experience that expects to apply and extend what they are learning throughout the curriculum. The course is designed to increase challenges in content as well as the type of critical thinking and reflective reasoning.
Online Tools
Students use an online tool that visualizes this structure, allowing them to share what they think, and learn how peers develop their thinking in each case.
Related Resources
5-Step Guide Polya-How to Solve it Cognitive Error Dr. Putnam on the 5-steps
From problem solving to problem definition: scrutinizing the complex nature of clinical practice
Affiliations.
- 1 Centre for Education Research & Innovation, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada. [email protected].
- 2 Centre for Education Research & Innovation, Schulich School of Medicine and Dentistry, Western University, London, Ontario, Canada.
- 3 Centre for Health Education Scholarship, Faculty of Medicine, University of British Columbia, Vancouver, Canada.
- PMID: 27921218
- PMCID: PMC5285274
- DOI: 10.1007/s40037-016-0314-0
In medical education, we have tended to present problems as being singular, stable, and solvable. Problem solving has, therefore, drawn much of medical education researchers' attention. This focus has been important but it is limited in terms of preparing clinicians to deal with the complexity of the 21st century healthcare system in which they will provide team-based care for patients with complex medical illness. In this paper, we use the Soft Systems Engineering principles to introduce the idea that in complex, team-based situations, problems usually involve divergent views and evolve with multiple solution iterations. As such we need to shift the conversation from (1) problem solving to problem definition, and (2) from a problem definition derived exclusively at the level of the individual to a definition derived at the level of the situation in which the problem is manifested. Embracing such a focus on problem definition will enable us to advocate for novel educational practices that will equip trainees to effectively manage the problems they will encounter in complex, team-based healthcare.
Keywords: Interactions; Perspectives; Systems Engineering.
Grants and funding
- 123239-1/Canadian Institutes of Health Research/Canada
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Cases : Clinical Problem-Solving Cases
Harriet S.MeyerMD, Contributing EditorJonathan D.EldredgeMLS, PhD, Journal Review EditorRobertHoganMD, adviser for new media
Not Available
Developing practical clinical problem-solving skills is an important professional endeavor for health care providers. Patient management problems and clinical problem-solving cases have been incorporated into certifying examinations and continuing education programs. Such simulations, in print or electronic form, allow users to select diagnostic or treatment options for hypothetical patients with immediate feedback on management decisions. The course of such simulated patient cases depends on user choices. Patient simulations have been popular and effective but difficult to develop.
Cases : Clinical Problem-Solving Cases . JAMA. 2000;283(13):1755–1756. doi:10.1001/jama.283.13.1755-JBK0405-4-1
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is Problem-Solving Therapy?
Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.
:max_bytes(150000):strip_icc():format(webp)/ArlinCuncic_1000-21af8749d2144aa0b0491c29319591c4.jpg)
Daniel B. Block, MD, is an award-winning, board-certified psychiatrist who operates a private practice in Pennsylvania.
:max_bytes(150000):strip_icc():format(webp)/block-8924ca72ff94426d940e8f7e639e3942.jpg)
Verywell / Madelyn Goodnight
Problem-Solving Therapy Techniques
How effective is problem-solving therapy, things to consider, how to get started.
Problem-solving therapy is a brief intervention that provides people with the tools they need to identify and solve problems that arise from big and small life stressors. It aims to improve your overall quality of life and reduce the negative impact of psychological and physical illness.
Problem-solving therapy can be used to treat depression , among other conditions. It can be administered by a doctor or mental health professional and may be combined with other treatment approaches.
At a Glance
Problem-solving therapy is a short-term treatment used to help people who are experiencing depression, stress, PTSD, self-harm, suicidal ideation, and other mental health problems develop the tools they need to deal with challenges. This approach teaches people to identify problems, generate solutions, and implement those solutions. Let's take a closer look at how problem-solving therapy can help people be more resilient and adaptive in the face of stress.
Problem-solving therapy is based on a model that takes into account the importance of real-life problem-solving. In other words, the key to managing the impact of stressful life events is to know how to address issues as they arise. Problem-solving therapy is very practical in its approach and is only concerned with the present, rather than delving into your past.
This form of therapy can take place one-on-one or in a group format and may be offered in person or online via telehealth . Sessions can be anywhere from 30 minutes to two hours long.
Key Components
There are two major components that make up the problem-solving therapy framework:
- Applying a positive problem-solving orientation to your life
- Using problem-solving skills
A positive problem-solving orientation means viewing things in an optimistic light, embracing self-efficacy , and accepting the idea that problems are a normal part of life. Problem-solving skills are behaviors that you can rely on to help you navigate conflict, even during times of stress. This includes skills like:
- Knowing how to identify a problem
- Defining the problem in a helpful way
- Trying to understand the problem more deeply
- Setting goals related to the problem
- Generating alternative, creative solutions to the problem
- Choosing the best course of action
- Implementing the choice you have made
- Evaluating the outcome to determine next steps
Problem-solving therapy is all about training you to become adaptive in your life so that you will start to see problems as challenges to be solved instead of insurmountable obstacles. It also means that you will recognize the action that is required to engage in effective problem-solving techniques.
Planful Problem-Solving
One problem-solving technique, called planful problem-solving, involves following a series of steps to fix issues in a healthy, constructive way:
- Problem definition and formulation : This step involves identifying the real-life problem that needs to be solved and formulating it in a way that allows you to generate potential solutions.
- Generation of alternative solutions : This stage involves coming up with various potential solutions to the problem at hand. The goal in this step is to brainstorm options to creatively address the life stressor in ways that you may not have previously considered.
- Decision-making strategies : This stage involves discussing different strategies for making decisions as well as identifying obstacles that may get in the way of solving the problem at hand.
- Solution implementation and verification : This stage involves implementing a chosen solution and then verifying whether it was effective in addressing the problem.
Other Techniques
Other techniques your therapist may go over include:
- Problem-solving multitasking , which helps you learn to think clearly and solve problems effectively even during times of stress
- Stop, slow down, think, and act (SSTA) , which is meant to encourage you to become more emotionally mindful when faced with conflict
- Healthy thinking and imagery , which teaches you how to embrace more positive self-talk while problem-solving
What Problem-Solving Therapy Can Help With
Problem-solving therapy addresses life stress issues and focuses on helping you find solutions to concrete issues. This approach can be applied to problems associated with various psychological and physiological symptoms.
Mental Health Issues
Problem-solving therapy may help address mental health issues, like:
- Chronic stress due to accumulating minor issues
- Complications associated with traumatic brain injury (TBI)
- Emotional distress
- Post-traumatic stress disorder (PTSD)
- Problems associated with a chronic disease like cancer, heart disease, or diabetes
- Self-harm and feelings of hopelessness
- Substance use
- Suicidal ideation

Specific Life Challenges
This form of therapy is also helpful for dealing with specific life problems, such as:
- Death of a loved one
- Dissatisfaction at work
- Everyday life stressors
- Family problems
- Financial difficulties
- Relationship conflicts
Your doctor or mental healthcare professional will be able to advise whether problem-solving therapy could be helpful for your particular issue. In general, if you are struggling with specific, concrete problems that you are having trouble finding solutions for, problem-solving therapy could be helpful for you.
Benefits of Problem-Solving Therapy
The skills learned in problem-solving therapy can be helpful for managing all areas of your life. These can include:
- Being able to identify which stressors trigger your negative emotions (e.g., sadness, anger)
- Confidence that you can handle problems that you face
- Having a systematic approach on how to deal with life's problems
- Having a toolbox of strategies to solve the issues you face
- Increased confidence to find creative solutions
- Knowing how to identify which barriers will impede your progress
- Knowing how to manage emotions when they arise
- Reduced avoidance and increased action-taking
- The ability to accept life problems that can't be solved
- The ability to make effective decisions
- The development of patience (realizing that not all problems have a "quick fix")
Problem-solving therapy can help people feel more empowered to deal with the problems they face in their lives. Rather than feeling overwhelmed when stressors begin to take a toll, this therapy introduces new coping skills that can boost self-efficacy and resilience .
Other Types of Therapy
Other similar types of therapy include cognitive-behavioral therapy (CBT) and solution-focused brief therapy (SFBT) . While these therapies work to change thinking and behaviors, they work a bit differently. Both CBT and SFBT are less structured than problem-solving therapy and may focus on broader issues. CBT focuses on identifying and changing maladaptive thoughts, and SFBT works to help people look for solutions and build self-efficacy based on strengths.
This form of therapy was initially developed to help people combat stress through effective problem-solving, and it was later adapted to address clinical depression specifically. Today, much of the research on problem-solving therapy deals with its effectiveness in treating depression.
Problem-solving therapy has been shown to help depression in:
- Older adults
- People coping with serious illnesses like cancer
Problem-solving therapy also appears to be effective as a brief treatment for depression, offering benefits in as little as six to eight sessions with a therapist or another healthcare professional. This may make it a good option for someone unable to commit to a lengthier treatment for depression.
Problem-solving therapy is not a good fit for everyone. It may not be effective at addressing issues that don't have clear solutions, like seeking meaning or purpose in life. Problem-solving therapy is also intended to treat specific problems, not general habits or thought patterns .
In general, it's also important to remember that problem-solving therapy is not a primary treatment for mental disorders. If you are living with the symptoms of a serious mental illness such as bipolar disorder or schizophrenia , you may need additional treatment with evidence-based approaches for your particular concern.
Problem-solving therapy is best aimed at someone who has a mental or physical issue that is being treated separately, but who also has life issues that go along with that problem that has yet to be addressed.
For example, it could help if you can't clean your house or pay your bills because of your depression, or if a cancer diagnosis is interfering with your quality of life.
Your doctor may be able to recommend therapists in your area who utilize this approach, or they may offer it themselves as part of their practice. You can also search for a problem-solving therapist with help from the American Psychological Association’s (APA) Society of Clinical Psychology .
If receiving problem-solving therapy from a doctor or mental healthcare professional is not an option for you, you could also consider implementing it as a self-help strategy using a workbook designed to help you learn problem-solving skills on your own.
During your first session, your therapist may spend some time explaining their process and approach. They may ask you to identify the problem you’re currently facing, and they’ll likely discuss your goals for therapy .
Keep In Mind
Problem-solving therapy may be a short-term intervention that's focused on solving a specific issue in your life. If you need further help with something more pervasive, it can also become a longer-term treatment option.
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
Shang P, Cao X, You S, Feng X, Li N, Jia Y. Problem-solving therapy for major depressive disorders in older adults: an updated systematic review and meta-analysis of randomized controlled trials . Aging Clin Exp Res . 2021;33(6):1465-1475. doi:10.1007/s40520-020-01672-3
Cuijpers P, Wit L de, Kleiboer A, Karyotaki E, Ebert DD. Problem-solving therapy for adult depression: An updated meta-analysis . Eur Psychiatry . 2018;48(1):27-37. doi:10.1016/j.eurpsy.2017.11.006
Nezu AM, Nezu CM, D'Zurilla TJ. Problem-Solving Therapy: A Treatment Manual . New York; 2013. doi:10.1891/9780826109415.0001
Owens D, Wright-Hughes A, Graham L, et al. Problem-solving therapy rather than treatment as usual for adults after self-harm: a pragmatic, feasibility, randomised controlled trial (the MIDSHIPS trial) . Pilot Feasibility Stud . 2020;6:119. doi:10.1186/s40814-020-00668-0
Sorsdahl K, Stein DJ, Corrigall J, et al. The efficacy of a blended motivational interviewing and problem solving therapy intervention to reduce substance use among patients presenting for emergency services in South Africa: A randomized controlled trial . Subst Abuse Treat Prev Policy . 2015;10(1):46. doi:doi.org/10.1186/s13011-015-0042-1
Margolis SA, Osborne P, Gonzalez JS. Problem solving . In: Gellman MD, ed. Encyclopedia of Behavioral Medicine . Springer International Publishing; 2020:1745-1747. doi:10.1007/978-3-030-39903-0_208
Kirkham JG, Choi N, Seitz DP. Meta-analysis of problem solving therapy for the treatment of major depressive disorder in older adults . Int J Geriatr Psychiatry . 2016;31(5):526-535. doi:10.1002/gps.4358
Garand L, Rinaldo DE, Alberth MM, et al. Effects of problem solving therapy on mental health outcomes in family caregivers of persons with a new diagnosis of mild cognitive impairment or early dementia: A randomized controlled trial . Am J Geriatr Psychiatry . 2014;22(8):771-781. doi:10.1016/j.jagp.2013.07.007
Noyes K, Zapf AL, Depner RM, et al. Problem-solving skills training in adult cancer survivors: Bright IDEAS-AC pilot study . Cancer Treat Res Commun . 2022;31:100552. doi:10.1016/j.ctarc.2022.100552
Albert SM, King J, Anderson S, et al. Depression agency-based collaborative: effect of problem-solving therapy on risk of common mental disorders in older adults with home care needs . The American Journal of Geriatric Psychiatry . 2019;27(6):619-624. doi:10.1016/j.jagp.2019.01.002
By Arlin Cuncic, MA Arlin Cuncic, MA, is the author of The Anxiety Workbook and founder of the website About Social Anxiety. She has a Master's degree in clinical psychology.
- Architecture and Design
- Asian and Pacific Studies
- Business and Economics
- Classical and Ancient Near Eastern Studies
- Computer Sciences
- Cultural Studies
- Engineering
- General Interest
- Geosciences
- Industrial Chemistry
- Islamic and Middle Eastern Studies
- Jewish Studies
- Library and Information Science, Book Studies
- Life Sciences
- Linguistics and Semiotics
- Literary Studies
- Materials Sciences
- Mathematics
- Social Sciences
- Sports and Recreation
- Theology and Religion
- Publish your article
- The role of authors
- Promoting your article
- Abstracting & indexing
- Publishing Ethics
- Why publish with De Gruyter
- How to publish with De Gruyter
- Our book series
- Our subject areas
- Your digital product at De Gruyter
- Contribute to our reference works
- Product information
- Tools & resources
- Product Information
- Promotional Materials
- Orders and Inquiries
- FAQ for Library Suppliers and Book Sellers
- Repository Policy
- Free access policy
- Open Access agreements
- Database portals
- For Authors
- Customer service
- People + Culture
- Journal Management
- How to join us
- Working at De Gruyter
- Mission & Vision
- De Gruyter Foundation
- De Gruyter Ebound
- Our Responsibility
- Partner publishers

Your purchase has been completed. Your documents are now available to view.
Medical Problem Solving
An analysis of clinical reasoning.
- Arthur S. Elstein , Lee S. Shulman and Sarah A. Sprafka
- In collaboration with: Linda Allal , Michael Gordon , Jason Hilliard , Norman Kagan , Michael J. Loupe and Ronald D. Jordan
- X / Twitter
Please login or register with De Gruyter to order this product.
- Language: English
- Publisher: Harvard University Press
- Copyright year: 1978
- Edition: Reprint 2014
- Audience: Professional and scholarly;
- Front matter: 16
- Main content: 330
- Other: 15 illustrations and tables
- Keywords: Medical logic. ; Medicine -- Decision making. ; Diagnosis. ; Problem Solving.
- Published: October 1, 2013
- ISBN: 9780674189089
- Published: February 5, 1978
- ISBN: 9780674189072
- Industry News
- Access and Reimbursement
- Law & Malpractice
- Coding & Documentation
- Practice Management
- Patient Engagement & Communications
- Billing & Collections
- Staffing & Salary
Eight-Step Problem Solving Process for Medical Practices
Whether you are hoping to solve a problem at your practice or simply trying to improve a process, the easy-to-follow OODA Loop method can help.
Practice managers know that there are four key objectives at the core of process improvement:
• To remove waste and inefficiencies • To increase productivity and asset availability • To improve response time and agility • To sustain safe and reliable operations
The question is, how do we do all this? I would suggest a proven technique known as the OODA Loop.
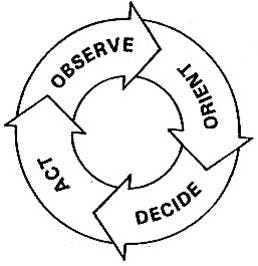
Top Challenges survey results
See what challenges practices are facing this year.

Practice Administration Stability and Key Determinants of Success
Sachin Gupta, CEO of IKS Health, discusses how independent practices can remain administratively stable during the pandemic and after, as well as provides the key determinants of success for new and growing practices.

The key to reducing administrative burden for clinical trials
Sponsors can play an especially critical role in alleviating the three key challenges facing clinical trial site administrators today.

When Physicians are Owners AND Employees
The professional model of medicine is trying to reach a sweet spot, allowing physicians to remain independent but maximize the power of a larger organization.

Two things every standout healthcare manager does
The managerial role, which historically emphasized operational knowledge and experience is now demanding the familiarity of clinical operations as well.
Duties to Give to Your Medical Practice Administrator
Are your physicians and staff members juggling too many responsibilities? Your practice administrator may be able to help.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


Become a Member
Problem Solving
Problem Solving in the Medical Practice Using the Five Whys
Ron Harman King, MS | Neil Baum, MD
December 8, 2018

There is no doctor or medical practice that hasn’t experienced a problem or a crisis in either the care of patients or the business aspect of the practice. Unfortunately, most doctors have few or no skills in crisis management or nonclinical problem solving. This task often is left to the office manager or the practice’s medical director. This article discusses the use of the root cause analysis and how it can be applied to nearly every medical practice. The “five whys” concept is a way to try to find the causes of potentially complex problems. When done properly, this strategy will help you to get to the root cause of many issues so that it can be addressed, rather than just focusing on symptoms of that problem.
When done properly, the “five whys” strategy has been shown not only to be effective, but also to be easy to use on a wide range of issues throughout many medical practices. It also can be combined and used with a variety of other techniques used to identify and solve workplace problems.
The five whys technique, which began in Japan at the Toyota Motor Company, is based on a scientific approach to problem solving. It has been applied through just about every type of industry around the world and could easily be used in the healthcare profession as well.
In the five whys process, you ask “why?” at least five times to get to the root cause of a problem. The process starts out with a problem that is affecting the practice, and then keeps asking why things happened until the root cause of the issue has been identified.
One of the best ways to get a good understanding of the five whys is to look at examples of how it has been explained with an example from the automotive industry. The following example is commonly used—how to discover the root cause of a car that will not start. The initial problem is “The car will not start.” From there, the five whys are asked:
Why won’t the car start? Answer: The battery is dead.
Why is the battery dead? Answer: The alternator is not working properly.
Why isn’t the alternator working? Answer: The serpentine belt has broken.
Why did the serpentine belt break? Answer: It was not replaced when worn.
Why wasn’t it replaced? Answer: The owner did not follow the recommended service schedule.
The last why is considered the root cause of the problem. If the owner of the vehicle had followed the recommended service schedule, this issue would not have happened. Not only that, but following the recommended service schedule will help to prevent a wide range of other problems including a decrease in radiator, brake, and oil fluids.
Applying the Five Whys Process to the Healthcare Practice
The problem to be solved is the practice is running behind schedule:
Why is the practice already one hour behind schedule in seeing patients by mid-morning when the doctor is supposed to start seeing patients at 9:00 AM? Answer: Patients are arriving 30 to 60 minutes late for their appointments.
Why are patients showing up late for their appointments? Answer: The doctor is usually 30 to 60 minutes late, and patients don’t want to wait to be seen so they arrive and check in 30 to 60 minutes after their designated appointment times.
Why is the doctor 30 to 60 minutes late by mid-morning? Answer: The doctor arrives for his office clinic 30 minutes late because patients usually are not taken to the exam rooms until 9:30. Instead the doctor goes to the computer to check e-mails.
Why are patients put in the rooms 30 minutes after their appointment times? Answer: The staff doesn’t arrive until 8:30 and is not ready to place patients in the rooms until 9:30.
Why is the lab data previously ordered not placed in the chart or recorded on the electronic medical record causing delays making decisions regarding patient care? Answer: The results have been sent to the office via fax but not recorded in the patient’s cart.
Solution: Start the day at 8:00 A.M. and start putting patients in the room at 8:45. Inform the doctor that he or she should arrive in the office by at least 8:45, allowing a few minutes to look at the computer, and that patients are to be seen starting promptly at 9:00.
Finding the Root Cause
The primary goal of the five whys is to take a problem and find the root cause so a solution can be identified and put in place. When done properly, a practice can find the root cause of most problems so that they can take actions to prevent it from happening in the future.
One of the best things about the five whys is that it is inexpensive to implement. A medical practice or a hospital can begin using it without added expense. The only cost is the time required to go through the process.
Why Look for the Root Cause
Most medical practices solve problems by identifying a problem and then using a quick fix for prompt resolution. In the long run, it is much better to identify the root cause of the issue and fix it—that will prevent the problem from occurring again. Seeking a root cause solution rather than just addressing the symptoms allows the practice to reduce recurrence (by dealing with the root cause, the symptoms are less likely to happen again in the future); prevent problems before they occur; gather information that identifies other issues that are impacting the practice; and place an emphasis on quality and safety over speed by avoiding a quick fix that temporarily solves the problem.
Every practice is unique, and all workplaces have their own set of problems that need to be dealt with. Implementing the use of the five whys can help medical practices to better understand their issues, and give them a clear roadmap on how those issues can be addressed permanently.
Getting Started with the Five Whys
The five whys system can be customized based on the specific needs of a given practice. Most practices or hospitals that are implementing this type of strategy will use some general rules or guidelines that can help keep the strategy focused on finding the root cause of the problem. Here are a few rules of performing the five whys:
Form the questions from the patient’s point of view. For example, when the practice runs behind schedule, patients are not happy that they are being seen 60 or even 90 minutes after their designated appointment. Another example would be that patients complain that they don’t receive results of lab tests or imaging studies until two or three weeks after the test or the procedure.
Keep asking or drilling until the root cause is discovered (even if more than five whys are required). This strategy is looking to find the root cause of the problem, not to place blame on any person(s) in the practice.
Base all statements on facts, not assumptions or hearsay.
Make sure to clearly distinguish the causes of problems from the symptoms of the problem (example: Doctor doesn’t start on time is a problem; Patients are upset is a symptom).
Involve physicians, nurses, administration, and ancillary personal as needed.
Focus on long-term success rather than short-term or quick-fix solutions.
Write down the problem at the top of a white board or flip chart and make sure that everyone understands the problem.
Try to make your answers concise and precise.
Be patient and don’t jump to conclusions.
Focus on the process, not on finding someone to blame.
Perform a root cause analysis as soon as possible after the error or variance occurs; otherwise, important details may be missed.
Explain that the purpose of the root cause analysis process is to focus on fixing or correcting the error and the systems involved. Make a point of stressing that the purpose of the analysis is not to assign blame but to solve problems.
Ask the question “Why?” until the root cause is determined. It is important to understand that in healthcare there may be more than one root cause for an event or a problem. The difficult part of identifying the root cause often requires persistence.
Finally, after the root cause is identified, conclude with the solution that will prevent the error from occurring again
It is this last step—identifying corrective action(s)—that will prevent recurrence of the problem that initially started the analysis. It is necessary to check that each corrective action, if it were to be implemented, is likely to reduce or prevent the specific problem from occurring.
The purpose of identifying solutions to a problem is to prevent recurrence. If there are alternative solutions that are equally effective, then the simplest or lowest-cost approach is preferred.
It is important that the group that identifies the solutions that will be implemented agrees on those solutions. Obtaining a consensus of the group that all are in agreement before solutions are implemented is important. You want to make every effort not to introduce or create a new problem that is worse than the original issue that you were attempting to solve.
The primary aims of root cause analysis are:
To identify the factors that caused the problem that may even result in harmful outcomes;
To determine what behaviors, actions, inactions, or conditions need to be changed;
To prevent recurrence of similar and perhaps harmful outcomes; and
To identify solutions that will promote the achievement of better outcomes and improved patient satisfaction.
To be effective, root cause analysis must be performed systematically using the five whys to drill down to the seminal event that initiates or produces the problem. The best result occurs when the root cause is identified and then backed up by documented evidence. For this systematic process to succeed, a team effort is typically required.
Bottom Line: Root cause analysis can help transform a reactive culture or one that moves from one crisis to the next into a forward-looking culture or a practice that solves problems before they occur or escalate into a full-blown crisis. More importantly, a practice that uses the five whys/root cause analysis reduces the frequency of problems occurring over time.
Strategic Perspective
Action Orientation
This article is available to Subscribers of JMPM .
Log in to view., career & learning, leadership library, membership & community, for over 45 years..
The American Association for Physician Leadership has helped physicians develop their leadership skills through education, career development, thought leadership and community building.
The American Association for Physician Leadership (AAPL) changed its name from the American College of Physician Executives (ACPE) in 2014. We may have changed our name, but we are the same organization that has been serving physician leaders since 1975.
CONNECT WITH US
Looking to engage your staff.
AAPL providers leadership development programs designed to retain valuable team members and improve patient outcomes.
American Association for Physician Leadership®
formerly known as the American College of Physician Executives (ACPE)
Privacy Policy | Advertising Kit | Press Room
An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Book/Report
Medical Problem Solving: An Analysis of Clinical Reasoning.
Elstein AS, ed. Cambridge, MA: Harvard University Press; 1978. ISBN: 9780674561250.
Clinical reasoning lies at the heart of formulating diagnoses and selecting treatments. The results of these medical decisions determine a substantial portion of the dollars spent on health care. Considering the fundamental importance of clinical reasoning, the topic has received surprisingly little systematic study. Even with the widespread interest in medical error and patient safety in recent years, diagnostic errors and other errors in clinical reasoning have received little attention. This classic collection of empiric studies on clinical reasoning in action thus remains highly relevant more than 25 years after its original publication. One finding of particular relevance for those interested in patient safety and quality improvement is that competence may be problem specific; thus, there is no generic approach to clinical problem solving that, when followed, ensures excellent, or even competent, performance in a variety of domains within a field. The authors also provide an excellent overview of theoretic models relevant to the study of clinical reasoning.
Medical Harm: Historical, Conceptual, and Ethical Dimensions of Iatrogenic Illness. March 27, 2005
Human Error. March 27, 2005
Merry and McCall Smith's Errors, Medicine, and the Law. 2nd ed. March 6, 2005
Judgment under Uncertainty: Heuristics and Biases. March 6, 2005
Working Knowledge: How Organizations Manage What They Know. September 14, 2005
First, Do Less Harm: Confronting the Inconvenient Problems of Patient Safety. June 6, 2012
Accountability: Patient Safety and Policy Reform. March 6, 2005
Error and Uncertainty in Diagnostic Radiology. March 20, 2019
Improving Quality and Safety in Healthcare. April 16, 2024
Speaking Up Constructively: Managerial Practices that Elicit Solutions from Front-Line Employees. March 9, 2011
Work Design Drivers of Organizational Learning about Operational Failures: A Laboratory Experiment on Medication Administration. January 9, 2013
A Randomized Field Study of a Leadership WalkRounds-Based Intervention. September 5, 2012
2014 Annual Benchmarking Report: Malpractice Risks in the Diagnostic Process. January 14, 2015
2011 Annual Benchmarking Report: Malpractice Risks in Emergency Medicine. September 26, 2012
Sources of Power: How People Make Decisions. March 6, 2005
Out of the Crisis. March 27, 2005
Unity of Mistakes: A Phenomenological Interpretation of Medical Work. March 6, 2005
The Cognitive Autopsy: A Root Cause Analysis of Medical Decision Making. January 27, 2021
Closing Death’s Door: Legal Innovations to End the Epidemic of Healthcare Harm. July 7, 2021
Oxford Professional Practice: Handbook of Patient Safety. July 27, 2022
Are Workarounds Ethical? Managing Moral Problems in Health Care Systems. February 3, 2016
Listening for What Matters: Avoiding Contextual Errors in Health Care. March 9, 2016
Organizing for Reliability: A Guide for Research and Practice. January 30, 2019
Practical Patient Safety. October 14, 2009
Talking with Patients and Families about Medical Error: A Guide for Education and Practice. February 16, 2011
Improving Patient Safety Through Teamwork and Team Training. January 29, 2014
Patient Safety Ethics: How Vigilance, Mindfulness, Compliance, and Humility can Make Healthcare Safer. July 24, 2019
Quality and Safety in Anesthesia and Perioperative Care. July 17, 2019
Still Not Safe: Patient Safety and the Middle-Managing of American Medicine. December 18, 2019
After Harm: Medical Error and the Ethics of Forgiveness. September 14, 2005
The Challenger Launch Decision: Risky Technology, Culture, and Deviance at NASA. March 27, 2005
The Limits of Safety: Organizations, Accidents and Nuclear Weapons. March 6, 2005
Demanding Medical Excellence. Doctors and Accountability in the Information Age. March 6, 2005
Forgive and Remember: Managing Medical Failure. 2nd ed. March 6, 2005
Failure in Safety-Critical Systems: A Handbook of Accident and Incident Reporting. March 6, 2005
Engaging Patients as Safety Partners: a Guide for Reducing Errors and Improving Satisfaction. June 18, 2008
Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2nd ed. February 13, 2017
Patient Safety: Achieving a New Standard for Care. March 6, 2005
Misadventures in Health Care: Inside Stories. August 24, 2005
Principles of Risk Management and Patient Safety. March 9, 2011
Patient Safety Handbook, Second Edition. August 17, 2013
When We Do Harm: A Doctor Confronts Medical Error. April 22, 2020
A Crisis in Health Care: A Call to Action on Physician Burnout. January 30, 2019
Learning in Action: A Guide to Putting the Learning Organization to Work. March 27, 2005
Maternal and Infant Health Inequality: New Evidence from Linked Administrative Data. February 22, 2023
The Power to Predict: Leveraging Medical Malpractice Data to Reduce Patient Harm and Financial Loss. June 24, 2020
Addressing the Opioid Crisis in the United States. November 2, 2016
IHI Skilled Nursing Facility Trigger Tool for Measuring Adverse Events. January 27, 2016
Malpractice Risks in Communication Failures: 2015 Annual Benchmarking Report. February 10, 2016
Respectful Management of Serious Clinical Adverse Events. Second Edition. October 27, 2010
How-to Guide: Multidisciplinary Rounds. March 10, 2010
Annual Benchmarking Report: Malpractice Risks in Surgery. June 9, 2010
Thinking Outside the Pillbox: A System-wide Approach to Improving Patient Medication Adherence for Chronic Disease. September 9, 2009
Achieving an Exceptional Patient and Family Experience of Inpatient Hospital Care. March 23, 2011
How-to Guides: Improving Transitions from the Hospital to Reduce Avoidable Rehospitalizations. August 8, 2012
How-to Guide: Prevent Obstetrical Adverse Events. October 24, 2012
Optimizing a Business Case for Safe Health Care: An Integrated Approach to Safety and Finance. July 12, 2017
A Framework for Safe, Reliable, and Effective Care. February 15, 2017
Closing the Loop: A Guide to Safer Ambulatory Referrals in the EHR Era. December 13, 2017
Addressing the Opioid Epidemic: Is There a Role for Physician Education? August 23, 2017
IHI Framework for Improving Joy in Work. August 9, 2017
Patient Safety in the Home: Assessment of Issues, Challenges, and Opportunities. September 6, 2017
Safer Together Survey: Advancing Patient and Workforce Safety January 18, 2023
IHI Global Trigger Tool for Measuring Adverse Events. 2nd Edition. May 9, 2009
Leadership Guide to Patient Safety: Resources and Tools for Establishing and Maintaining Patient Safety. September 28, 2005
Seven Leadership Leverage Points for Organization-Level Improvement in Health Care. Second edition. June 1, 2005
Organizational Learning from Experience in High-Hazard Industries: Problem Investigations as Off-line Reflective Practice. March 6, 2005
The Public's Views on Medical Error in Massachusetts. December 17, 2014
Safety Quality and Informatics Leadership Program. January 7, 2015
When safety event reporting is seen as punitive: "I've been PSN-ed!" September 9, 2020
Organizational readiness to change as a leverage point for improving safety: a national nursing home survey. September 8, 2021
Adverse events present on arrival to the emergency department: the ED as a dual safety net. March 11, 2020
The Emperor’s New Clothes: Or Whatever Happened To “Human Error”? January 1, 2001
Resident Projects for Improvement. June 19, 2013
Normal Accidents: Living with High-Risk Technologies. March 6, 2005
Patient Safety: Research into Practice. September 13, 2006
Medication errors reported in a pediatric intensive care unit for oncologic patients. September 14, 2011
The Patient Safety Leadership WalkRounds Guide. November 19, 2008
Hospitalists as emerging leaders in patient safety: targeting a few to affect many. August 31, 2005
Drug, Healthcare and Patient Safety. November 7, 2012
Mistaking error. March 27, 2005
Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. August 2, 2017
Organisational Failure: An Exploratory Study in the Steel Industry and Medical Domain. March 6, 2005
Implementing Patient Safety: Addressing Culture, Conditions and Values to Help People Work Safely. October 23, 2019
SHOT Annual Report. July 19, 2023
Patient Safety Culture: Theory, Methods and Application. January 21, 2015
Patient Safety: Perspectives on Evidence, Information and Knowledge Transfer. June 4, 2014
The Role of Hospitalists in Patient Safety. December 2, 2009
Pediatric Patient Safety in the Emergency Department. April 28, 2010
The Value of Close Calls in Improving Patient Safety. February 2, 2011
Error Reduction in Health Care: A Systems Approach to Improving Patient Safety, Second edition. June 1, 2011
Impact of Medical Errors and Malpractice on Health Economics, Quality, and Patient Safety. April 26, 2017
Surgical Patient Safety: A Case-Based Approach. October 18, 2017
Getting Results: Reliably Communicating and Acting on Critical Test Results. July 12, 2006
Improving Healthcare Team Communication: Building on Lessons from Aviation and Aerospace. June 25, 2008
Clinical Risk Management. Enhancing Patient Safety. 2nd ed. March 27, 2005
Human Error in Medicine. March 27, 2005
Saving Mothers' Lives: Reviewing Maternal Deaths to Make Motherhood Safer—2003–2005. January 2, 2008
The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. May 19, 2021
Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. January 30, 2003
All in Her Head. The Truth and Lies Early Medicine Taught Us About Women's Bodies and Why It Matters Today. March 20, 2024
The good, the bad, and the ugly: operative staff perspectives of surgeon coping with intraoperative errors. June 14, 2023
Annual Perspective
Formalizing the hidden curriculum of performance enhancing errors. March 22, 2023
Impact of medical education on patient safety: finding the signal through the noise. February 8, 2023
Improved Diagnostic Accuracy Through Probability-Based Diagnosis. September 28, 2022
Medical malpractice lawsuits involving trainees in obstetrics and gynecology in the USA. September 21, 2022
Does a suggested diagnosis in a general practitioners' referral question impact diagnostic reasoning: an experimental study. April 27, 2022
NCICLE Pathways to Excellence: Expectations for an Optimal Clinical Learning Environment to Achieve Safe and High-Quality Patient Care, 2021. November 24, 2021
Developing critical thinking skills for delivering optimal care July 28, 2021
Resident-faculty overnight discrepancy rates as a function of number of consecutive nights during a week of night float. January 13, 2021
ACGME Summary Report: The Pursuing Excellence Pathway Leaders Patient Safety Collaborative. November 18, 2020
Misdiagnosis, mistreatment, and harm - when medical care ignores social forces. April 8, 2020
Assessing clinical reasoning: targeting the higher levels of the pyramid. September 18, 2019
Professionalism lapses and adverse childhood experiences: reflections from the island of last resort. August 14, 2019
Association of residency work hour reform with long term quality and costs of care of US physicians: observational study. July 24, 2019
Effects on resident work hours, sleep duration and work experience in a Randomized Order Safety Trial Evaluating Resident-physician Schedules (ROSTERS). June 26, 2019
Pediatric faculty knowledge and comfort discussing diagnostic errors: a pilot survey to understand barriers to an educational program. June 12, 2019
Health Professions Education. June 12, 2019
Associations between in-hospital mortality, health care utilization, and inpatient costs with the 2011 resident duty hour revision. May 15, 2019
Perception of the usability and implementation of a metacognitive mnemonic to check cognitive errors in clinical setting. April 10, 2019
Patient safety outcomes under flexible and standard resident duty-hour rules. March 13, 2019
Sleep and alertness in a duty-hour flexibility trial in internal medicine. March 13, 2019
"Does your knee make more of a click or a clack?"; teaching "Car Talk" to new docs. March 13, 2019
Teaching about diagnostic errors through virtual patient cases: a pilot exploration. February 27, 2019
Adjusting to duty hour reforms: residents' perception of the safety climate in interdisciplinary night-float rotations. February 20, 2019
Data omission by physician trainees on ICU rounds. February 6, 2019
Utilizing a Systems and Design Thinking Approach for Improving Well-Being Within Health Professional Education and Health Care. January 16, 2019

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
- CPSolvers Academy
- Morning Report
- Diagnostic frameworks
- Illness scripts
- Residency Match
- Spaced Learning
Download PDF Here
From Collective Conflict to Collaborative Problem Solving: Unraveling the Knots of Perception to Solve Functional Problems
This session uncovers the nuanced distinction between conflicts, (which often arise from subjective perspectives and perception misalignments such as patient-provider conflicts, nurse-doctor conflicts, etc., that obscure the underlying, objective challenges that teams face) and functional problems within any multidisciplinary effort. Join two experts explore how to transform conflict into a catalyst for uncovering and addressing the core issues at hand by understanding the nature of conflict and employing practical frameworks.
Learning Objectives:
- Understand the nature of conflict and functional problems, gain insight into the psychological underpinnings of conflicts and how they differ from objective, functional problems and identify the heart of collective challenges, moving beyond subjective disagreements.
- Leverage conflict for collaborative problem-solving, learn to apply principles and tools to harness conflict constructively and discover how to use conflicts as a focus area to address and solve underlying functional problems, leading to enhanced team cohesion, satisfaction and productivity.
- Learn how to shift focus from individual disagreements to collaborative problem-solving, fostering a culture of engagement and shared success.
Brian R. Spisak, PhD , independent consultant; research associate, National Preparedness Leadership Initiative, Harvard University; ACHE Faculty
Rick van Pelt, MD chief clinical transformation officer, leader of the Clinical Practice Transformation Department, University of Alabama at Birmingham Medicine
Cancellation:
To cancel your webinar registration, please notify the Customer Service Center, at [email protected] , at least two business days before the start of the webinar for a refund or credit. After that time, a refund or credit is forfeited.
Continuing Education Credit
Ache qualifying education credit.
This webinar is eligible for 1 ACHE Qualifying Education credit. ACHE Qualifying Education credits will be automatically updated in your My ACHE account upon completion of the recording.

Interprofessional Continuing Education Credit
In support of improving patient care, the American College of Healthcare Executives is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), the American Nurses Credentialing Center (ANCC), and the American Academy of PAs (AAPA) to provide continuing education for the healthcare team.
This activity was planned by and for the healthcare team, and learners will receive a maximum of 1 Interprofessional Continuing Education (IPCE) credit for learning and change. For further information about Joint Accreditation credits and certificates, please click here .
Physician Continuing Medical Education
The American College of Healthcare Executives (ACHE) designates this live activity for a maximum of 1 AMA PRA Category 1 Credits ™ . Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Continuing Nursing Education
The American College of Healthcare Executives designates this live activity for a maximum of 1 contact hours of continuing nursing education.
Continuing Pharmacy Education
The American College of Healthcare Executives designates this knowledge-based activity for a maximum 1 contact hours of continuing pharmacy education credit.
Continuing Social Work Education
The American College of Healthcare Executives designates this knowledge-based activity for a maximum 1 contact hours of continuing social work education credit.
Continuing Education for Dietitians
The American College of Healthcare Executives designates this knowledge-based activity for a maximum 1 contact hours of continuing education credit for Registered Dietitians and Dietetic Technicians, Registered. RDs and DTRs should enter activities offered by jointly accredited providers as type 102 on Professional Development Portfolio (PDP) activity logs. CPEUs awarded must be commensurate with participation in the activity.
Physician Associate/Physician Assistant Continuing Education
The American College of Healthcare Executives has been authorized by the American Academy of PAs (AAPA) to award AAPA Category 1 CME credit for activities planned in accordance with AAPA CME Criteria. This activity is designated for a maximum of 1 AAPA Category 1 CME credits. PAs should only claim credit commensurate with the extent of their participation.
What is decision making?

Decisions, decisions. When was the last time you struggled with a choice? Maybe it was this morning, when you decided to hit the snooze button—again. Perhaps it was at a restaurant, with a miles-long menu and the server standing over you. Or maybe it was when you left your closet in a shambles after trying on seven different outfits before a big presentation. Often, making a decision—even a seemingly simple one—can be difficult. And people will go to great lengths—and pay serious sums of money—to avoid having to make a choice. The expensive tasting menu at the restaurant, for example. Or limiting your closet choices to black turtlenecks, à la Steve Jobs.
Get to know and directly engage with senior McKinsey experts on decision making
Aaron De Smet is a senior partner in McKinsey’s New Jersey office, Eileen Kelly Rinaudo is McKinsey’s global director of advancing women executives and is based in the New York office, Frithjof Lund is a senior partner in the Oslo office, and Leigh Weiss is a senior adviser in the Boston office.
If you’ve ever wrestled with a decision at work, you’re definitely not alone. According to McKinsey research, executives spend a significant portion of their time— nearly 40 percent , on average—making decisions. Worse, they believe most of that time is poorly used. People struggle with decisions so much so that we actually get exhausted from having to decide too much, a phenomenon called decision fatigue.
But decision fatigue isn’t the only cost of ineffective decision making. According to a McKinsey survey of more than 1,200 global business leaders, inefficient decision making costs a typical Fortune 500 company 530,000 days of managers’ time each year, equivalent to about $250 million in annual wages. That’s a lot of turtlenecks.
How can business leaders ease the burden of decision making and put this time and money to better use? Read on to learn the ins and outs of smart decision making—and how to put it to work.
Learn more about our People & Organizational Performance Practice .
How can organizations untangle ineffective decision-making processes?
McKinsey research has shown that agile is the ultimate solution for many organizations looking to streamline their decision making . Agile organizations are more likely to put decision making in the right hands, are faster at reacting to (or anticipating) shifts in the business environment, and often attract top talent who prefer working at companies with greater empowerment and fewer layers of management.
For organizations looking to become more agile, it’s possible to quickly boost decision-making efficiency by categorizing the type of decision to be made and adjusting the approach accordingly. In the next section, we review three types of decision making and how to optimize the process for each.
What are three keys to faster, better decisions?
Business leaders today have access to more sophisticated data than ever before. But it hasn’t necessarily made decision making any easier. For one thing, organizational dynamics—such as unclear roles, overreliance on consensus, and death by committee—can get in the way of straightforward decision making. And more data often means more decisions to be taken, which can become too much for one person, team, or department. This can make it more difficult for leaders to cleanly delegate, which in turn can lead to a decline in productivity.
Leaders are growing increasingly frustrated with broken decision-making processes, slow deliberations, and uneven decision-making outcomes. Fewer than half of the 1,200 respondents of a McKinsey survey report that decisions are timely, and 61 percent say that at least half the time they spend making decisions is ineffective.
What’s the solution? According to McKinsey research, effective solutions center around categorizing decision types and organizing different processes to support each type. Further, each decision category should be assigned its own practice—stimulating debate, for example, or empowering employees—to yield improvements in effectiveness.
Here are the three decision categories that matter most to senior leaders, and the standout practice that makes the biggest difference for each type of decision.
- Big-bet decisions are infrequent but high risk, such as acquisitions. These decisions carry the potential to shape the future of the company, and as a result are generally made by top leaders and the board. Spurring productive debate by assigning someone to argue the case for and against a potential decision can improve big-bet decision making.
- Cross-cutting decisions, such as pricing, can be frequent and high risk. These are usually made by business unit heads, in cross-functional forums as part of a collaborative process. These types of decisions can be improved by doubling down on process refinement. The ideal process should be one that helps clarify objectives, measures, and targets.
- Delegated decisions are frequent but low risk and are handled by an individual or working team with some input from others. Delegated decision making can be improved by ensuring that the responsibility for the decision is firmly in the hands of those closest to the work. This approach also enhances engagement and accountability.
In addition, business leaders can take the following four actions to help sustain rapid decision making :
- Focus on the game-changing decisions, ones that will help an organization create value and serve its purpose.
- Convene only necessary meetings, and eliminate lengthy reports. Turn unnecessary meetings into emails, and watch productivity bloom. For necessary meetings, provide short, well-prepared prereads to aid in decision making.
- Clarify the roles of decision makers and other voices. Who has a vote, and who has a voice?
- Push decision-making authority to the front line—and tolerate mistakes.

Introducing McKinsey Explainers : Direct answers to complex questions
How can business leaders effectively delegate decision making.
Business is more complex and dynamic than ever, meaning business leaders are faced with needing to make more decisions in less time. Decision making takes up an inordinate amount of management’s time—up to 70 percent for some executives—which leads to inefficiencies and opportunity costs.
As discussed above, organizations should treat different types of decisions differently . Decisions should be classified according to their frequency, risk, and importance. Delegated decisions are the most mysterious for many organizations: they are the most frequent, and yet the least understood. Only about a quarter of survey respondents report that their organizations make high-quality and speedy delegated decisions. And yet delegated decisions, because they happen so often, can have a big impact on organizational culture.
The key to better delegated decisions is to empower employees by giving them the authority and confidence to act. That means not simply telling employees which decisions they can or can’t make; it means giving employees the tools they need to make high-quality decisions and the right level of guidance as they do so.
Here’s how to support delegation and employee empowerment:
- Ensure that your organization has a well-defined, universally understood strategy. When the strategic intent of an organization is clear, empowerment is much easier because it allows teams to pull in the same direction.
- Clearly define roles and responsibilities. At the foundation of all empowerment efforts is a clear understanding of who is responsible for what, including who has input and who doesn’t.
- Invest in capability building (and coaching) up front. To help managers spend meaningful coaching time, organizations should also invest in managers’ leadership skills.
- Build an empowerment-oriented culture. Leaders should role model mindsets that promote empowerment, and managers should build the coaching skills they want to see. Managers and employees, in particular, will need to get comfortable with failure as a necessary step to success.
- Decide when to get involved. Managers should spend effort up front to decide what is worth their focused attention. They should know when it’s appropriate to provide close guidance and when not to.
How can you guard against bias in decision making?
Cognitive bias is real. We all fall prey, no matter how we try to guard ourselves against it. And cognitive and organizational bias undermines good decision making, whether you’re choosing what to have for lunch or whether to put in a bid to acquire another company.
Here are some of the most common cognitive biases and strategies for how to avoid them:
- Confirmation bias. Often, when we already believe something, our minds seek out information to support that belief—whether or not it is actually true. Confirmation bias involves overweighting evidence that supports our belief, underweighting evidence against our belief, or even failing to search impartially for evidence in the first place. Confirmation bias is one of the most common traps organizational decision makers fall into. One famous—and painful—example of confirmation bias is when Blockbuster passed up the opportunity to buy a fledgling Netflix for $50 million in 2000. (Actually, that’s putting it politely. Netflix executives remember being “laughed out” of Blockbuster’s offices.) Fresh off the dot-com bubble burst of 2000, Blockbuster executives likely concluded that Netflix had approached them out of desperation—not that Netflix actually had a baby unicorn on its hands.
- Herd mentality. First observed by Charles Mackay in his 1841 study of crowd psychology, herd mentality happens when information that’s available to the group is determined to be more useful than privately held knowledge. Individuals buy into this bias because there’s safety in the herd. But ignoring competing viewpoints might ultimately be costly. To counter this, try a teardown exercise , wherein two teams use scenarios, advanced analytics, and role-playing to identify how a herd might react to a decision, and to ensure they can refute public perceptions.
- Sunk-cost fallacy. Executives frequently hold onto underperforming business units or projects because of emotional or legacy attachment . Equally, business leaders hate shutting projects down . This, researchers say, is due to the ingrained belief that if everyone works hard enough, anything can be turned into gold. McKinsey research indicates two techniques for understanding when to hold on and when to let go. First, change the burden of proof from why an asset should be cut to why it should be retained. Next, categorize business investments according to whether they should be grown, maintained, or disposed of—and follow clearly differentiated investment rules for each group.
- Ignoring unpleasant information. Researchers call this the “ostrich effect”—when people figuratively bury their heads in the sand , ignoring information that will make their lives more difficult. One study, for example, found that investors were more likely to check the value of their portfolios when the markets overall were rising, and less likely to do so when the markets were flat or falling. One way to help get around this is to engage in a readout process, where individuals or teams summarize discussions as they happen. This increases the likelihood that everyone leaves a meeting with the same understanding of what was said.
- Halo effect. Important personal and professional choices are frequently affected by people’s tendency to make specific judgments based on general impressions . Humans are tempted to use simple mental frames to understand complicated ideas, which means we frequently draw conclusions faster than we should. The halo effect is particularly common in hiring decisions. To avoid this bias, structured interviews can help mitigate the essentializing tendency. When candidates are measured against indicators, intuition is less likely to play a role.
For more common biases and how to beat them, check out McKinsey’s Bias Busters Collection .
Learn more about Strategy & Corporate Finance consulting at McKinsey—and check out job opportunities related to decision making if you’re interested in working at McKinsey.
Articles referenced include:
- “ Bias busters: When the crowd isn’t necessarily wise ,” McKinsey Quarterly , May 23, 2022, Eileen Kelly Rinaudo , Tim Koller , and Derek Schatz
- “ Boards and decision making ,” April 8, 2021, Aaron De Smet , Frithjof Lund , Suzanne Nimocks, and Leigh Weiss
- “ To unlock better decision making, plan better meetings ,” November 9, 2020, Aaron De Smet , Simon London, and Leigh Weiss
- “ Reimagine decision making to improve speed and quality ,” September 14, 2020, Julie Hughes , J. R. Maxwell , and Leigh Weiss
- “ For smarter decisions, empower your employees ,” September 9, 2020, Aaron De Smet , Caitlin Hewes, and Leigh Weiss
- “ Bias busters: Lifting your head from the sand ,” McKinsey Quarterly , August 18, 2020, Eileen Kelly Rinaudo
- “ Decision making in uncertain times ,” March 24, 2020, Andrea Alexander, Aaron De Smet , and Leigh Weiss
- “ Bias busters: Avoiding snap judgments ,” McKinsey Quarterly , November 6, 2019, Tim Koller , Dan Lovallo, and Phil Rosenzweig
- “ Three keys to faster, better decisions ,” McKinsey Quarterly , May 1, 2019, Aaron De Smet , Gregor Jost , and Leigh Weiss
- “ Decision making in the age of urgency ,” April 30, 2019, Iskandar Aminov, Aaron De Smet , Gregor Jost , and David Mendelsohn
- “ Bias busters: Pruning projects proactively ,” McKinsey Quarterly , February 6, 2019, Tim Koller , Dan Lovallo, and Zane Williams
- “ Decision making in your organization: Cutting through the clutter ,” McKinsey Quarterly , January 16, 2018, Aaron De Smet , Simon London, and Leigh Weiss
- “ Untangling your organization’s decision making ,” McKinsey Quarterly , June 21, 2017, Aaron De Smet , Gerald Lackey, and Leigh Weiss
- “ Are you ready to decide? ,” McKinsey Quarterly , April 1, 2015, Philip Meissner, Olivier Sibony, and Torsten Wulf.

Want to know more about decision making?
Related articles.
What is productivity?

What is the future of work?

What is leadership?

Federal Acquisition Regulation
Full far download in various formats, browse far part/subpart and download in various formats.
- Data Initiatives
- Regulations
- Smart Matrix
- Regulations Search
- Acquisition Regulation Comparator (ARC)
- Large Agencies
- Small Agencies
- CAOC History
- CAOC Charter
- Civilian Agency Acquisition Council (CAAC)
- Federal Acquisition Regulatory Council
- Interagency Suspension and Debarment Committee (ISDC)

ACQUISITION.GOV
An official website of the General Services Administration

Game Central
Histology MCQ PDF Book | Medical Histology MCQ Questions and Answers PDF
Quiz questions chapter 1-29 & practice tests with answers key (histology textbook notes, mcqs & study guide), publisher description.
The Histology Multiple Choice Questions (MCQ Quiz) with Answers PDF (Histology MCQ PDF Download): Quiz Questions Chapter 1-29 & Practice Tests with Answers Key (Medical Histology Textbook MCQs, Notes & Study Guide) includes revision guide for problem solving with hundreds of solved MCQs. Histology MCQ with Answers PDF book covers basic concepts, analytical and practical assessment tests. "Histology MCQ" PDF book helps to practice test questions from exam prep notes. The Histology MCQs with Answers PDF eBook includes revision guide with verbal, quantitative, and analytical past papers, solved MCQs. Histology Multiple Choice Questions and Answers (MCQs) PDF : Free download chapter 1, a book covers solved quiz questions and answers on chapters: Blood, bones, cartilages, cell, cerebrum, cerebellum and spinal cord, circulatory system, connective tissues, connective tissues proper, digestive system, ear, endocrine system, epithelium, eye, eye: ciliary body, eye: fibrous coat, eye: iris, eye: lens and conjunctiva, eye: lens, accessory structure of eye, eye: retina, eye: vascular coat, female reproductive system, glands, immune system and lymphoid organs, integumentary system, male reproductive system, muscular tissue, nervous tissue, respiratory system, urinary system tests for college and university revision guide. Histology Quiz Questions and Answers PDF download, free eBook’s sample covers beginner's solved questions, textbook's study notes to practice tests. The book Histology MCQs Chapter 1-29 PDF includes high school question papers to review practice tests for exams. Histology Multiple Choice Questions (MCQ) with Answers PDF digital edition eBook, a study guide with textbook chapters' tests for NEET/Jobs/Entry Level competitive exam. Histology Practice Tests Chapter 1-29 PDF covers problem solving exam tests from life sciences textbook and practical eBook chapter-wise as: Chapter 1: Blood MCQ Chapter 2: Bones MCQ Chapter 3: Cartilages MCQ Chapter 4: Cell MCQ Chapter 5: Cerebrum, Cerebellum and Spinal Cord MCQ Chapter 6: Circulatory System MCQ Chapter 7: Connective Tissues MCQ Chapter 8: Connective Tissues Proper MCQ Chapter 9: Digestive System MCQ Chapter 10: Ear MCQ Chapter 11: Endocrine System MCQ Chapter 12: Epithelium MCQ Chapter 13: Eye MCQ Chapter 14: Eye: Ciliary Body MCQ Chapter 15: Eye: Fibrous Coat MCQ Chapter 16: Eye: Iris MCQ Chapter 17: Eye: Lens and Conjunctiva MCQ Chapter 18: Eye: Lens, Accessory Structure of Eye MCQ Chapter 19: Eye: Retina MCQ Chapter 20: Eye: Vascular Coat MCQ Chapter 21: Female Reproductive System MCQ Chapter 22: Glands MCQ Chapter 23: Immune System and Lymphoid Organs MCQ Chapter 24: Integumentary System MCQ Chapter 25: Male Reproductive System MCQ Chapter 26: Muscular Tissue MCQ Chapter 27: Nervous Tissue MCQ Chapter 28: Respiratory System MCQ Chapter 29: Urinary System MCQ Practice "Blood MCQ" PDF, book's chapter 1 test to solve MCQ questions: Erythrocytes, leukocytes, plasma, and platelets. Practice "Bones MCQ" PDF, book's chapter 2 test to solve MCQ questions: Bone formation, bone matrix, bone tissues, joints, and structure of bone tissues. Practice "Cartilages MCQ" PDF, book's chapter 3 test to solve MCQ questions: Classification of cartilage. Practice "Cell MCQ" PDF, book's chapter 4 test to solve MCQ questions: Cell death, cell division, cell junctions, cell membrane, cell organelles: Golgi apparatus, cell renewal, cytoplasm, cytoplasmic inclusions: pigments, cytoplasmic inclusions: stored food materials, cytoplasmic organelles: endoplasmic reticulum, cytoplasmic organelles: mitochondria, cytoplasmic organelles: ribosomes, cytoskeleton, nucleus, shape, and size of human cells. Practice "Cerebrum, Cerebellum and Spinal Cord MCQ" PDF, book's chapter 5 test to solve MCQ questions: Cerebellum, cerebrum, and spinal cord. Practice "Circulatory System MCQ" PDF, book's chapter 6 test to solve MCQ questions: Blood vascular system. Practice "Connective Tissues MCQ" PDF, book's chapter 7 test to solve MCQ questions: Adipose tissues, connective tissue cells, dense connective tissues, extracellular matrix of connective tissues, loose connective tissues, and reticular connective tissue. Practice "Connective Tissues Proper MCQ" PDF, book's chapter 8 test to solve MCQ questions: Adipose tissues, dense connective tissues, loose connective tissues, and reticular connective tissue. Practice "Digestive system MCQ" PDF, book's chapter 9 test to solve MCQ questions: Colon and appendix, digestive system: esophagus, gallbladder, large intestine, liver, oral cavity, pancreas and exocrine pancreas, rectum and anal canal, salivary glands and saliva, small intestine, and stomach. Practice "Ear MCQ" PDF, book's chapter 10 test to solve MCQ questions: External ear, inner ear, and middle ear. Practice "Endocrine System MCQ" PDF, book's chapter 11 test to solve MCQ questions: Adrenal glands, hormone and hormone receptors, hypophysis, hypophysis: adenohypophysis, hypophysis: neurohypophysis, parathyroid glands, pineal gland, and thyroid glands. Practice "Epithelium MCQ" PDF, book's chapter 12 test to solve MCQ questions: Body tissues, epithelium, and classification covering epithelia. Practice "Eye MCQ" PDF, book's chapter 13 test to solve MCQ questions: Choroid, ciliary muscles and ciliary layer, conjunctiva, eyelids, lacrimal glands, cornea, elements of neural retina, fibrous coat, iris, iris stroma and layers of iris, layers of retina and pigment epithelium, lens capsule, sub-capsular epithelium, lens substance, and sclera. Practice "Eye: Ciliary Body MCQ" PDF, book's chapter 14 test to solve MCQ questions: Ciliary muscles and ciliary layer. Practice "Eye: Fibrous Coat MCQ" PDF, book's chapter 15 test to solve MCQ questions: Cornea, and sclera. Practice "Eye: IRIS MCQ" PDF, book's chapter 16 test to solve MCQ questions: Iris, iris stroma and layers of iris. Practice "Eye: Lens and Conjunctiva MCQ" PDF, book's chapter 17 test to solve MCQ questions: Lens capsule, sub-capsular epithelium, and lens substance. Practice "Eye: Lens, Accessory Structure of Eye MCQ" PDF, book's chapter 18 test to solve MCQ questions: Conjunctiva, eyelids, and lacrimal glands. Practice "Eye: Retina MCQ" PDF, book's chapter 19 test to solve MCQ questions: Elements of neural retina, layers of retina, and pigment epithelium. Practice "Eye: Vascular Coat MCQ" PDF, book's chapter 20 test to solve MCQ questions: Choroid. Practice "Female Reproductive System MCQ" PDF, book's chapter 21 test to solve MCQ questions: Corpus luteum, external genitalia, ovaries: ovarian follicles, uterine tube, and uterus. Practice "Glands MCQ" PDF, book's chapter 22 test to solve MCQ questions: Classification of glands, classification on basis of morphology, classification on basis of secretory products, classification on mode of secretion, and histological structure of exocrine glands. Practice "Immune System and Lymphoid Organs MCQ" PDF, book's chapter 23 test to solve MCQ questions: Immune system, and lymphoid tissues. Practice "Integumentary System MCQ" PDF, book's chapter 24 test to solve MCQ questions: Dermis, glands of skin, hair, nails, and skin. Practice "Male Reproductive System MCQ" PDF, book's chapter 25 test to solve MCQ questions: accessory glands of male reproductive system, corpus luteum, external genitalia, male genital duct, ovaries: Ovarian follicles, testes, testes: seminiferous epithelium, testes: seminiferous epithelium, spermatozoa, testes: seminiferous tubules, uterine tube, and uterus. Practice "Muscular Tissue MCQ" PDF, book's chapter 26 test to solve MCQ questions: Cardiac muscles, skeletal muscles, and smooth muscles. Practice "Nervous Tissue MCQ" PDF, book's chapter 27 test to solve MCQ questions: Ganglia and neuroglia, grey-matter and white-matter, meninges and dura-mater, nerve fibers, nerve termination, neurons and types, and synapses. Practice "Respiratory System MCQ" PDF, book's chapter 28 test to solve MCQ questions: Nasopharynx and larynx, respiratory bronchioles, respiratory epithelium, nasal cavity, trachea, and lungs. Practice "Urinary System MCQ" PDF, book's chapter 29 test to solve MCQ questions: Kidney, urethra, ureter, and urinary bladder.
More Books by Arshad Iqbal
Other books in this series.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Washington warns of danger from China in remembering the 1989 Tiananmen crackdown
People gather at the base of the Victims of Communism Memorial during a candlelight vigil to mark the 35th anniversary of the Tiananmen Square, Tuesday, June 3, 2024, in Washington. (AP Photo/Didi Tang)
Rep. Nancy Pelosi, D-Calif., the speaker emerita, joins member of the House Select Committee on the Chinese Communist Party and other lawmakers at an event to commemorate the 35th anniversary of the bloody 1989 crackdown on pro-democracy protests in Tiananmen Square in Beijing, at the Capitol in Washington, Tuesday, June 4, 2024. (AP Photo/J. Scott Applewhite)
Rep. Nancy Pelosi, D-Calif., the speaker emerita, joins members of the House Select Committee on the Chinese Communist Party and other lawmakers at an event to commemorate the 35th anniversary of the bloody 1989 crackdown on pro-democracy protests in Tiananmen Square in Beijing, at the Capitol in Washington, Tuesday, June 4, 2024. (AP Photo/J. Scott Applewhite)
- Copy Link copied
WASHINGTON (AP) — Members of the U.S. Congress on Tuesday said the ruling Chinese Communist Party that sent in tanks against peaceful student protesters 35 years ago in the heart of Beijing is as ruthless and suppressive today as it was in 1989, a stark warning as they commemorated the anniversary of China’s bloody crackdown in Tiananmen Square .
Rep. Raja Krishnamoorthi, the ranking Democratic member of the House Select Committee on the Chinese Communist Party, warned that Chinese leader Xi Jinping would resort to violence, as his predecessors did, to achieve his goals.
“We have to remember that when Chairman Xi Jinping says he will crack down hard on subversion and separatist activities ... he’s telling the world that the (party) will send those tanks again against anyone that stands up for freedom,” the Illinois congressman said, with the iconic image of a lone man facing down a line of tanks nearby.
The Tuesday commemorations, which included former student leaders of the Tiananmen movement and younger activists from mainland China and Hong Kong, come as Washington has shifted its China policy from engagement to competition meant to curb China’s growing influences, which the U.S. sees as potentially upsetting the world order. The two countries also are clashing over Beijing’s militarization of the South China Sea and its increasing military threats against the self-governed island of Taiwan.
“This is now the source of legitimacy for the U.S. rivalry with China,” said Guo Baosheng, a political commentator, remembering the Tiananmen movement and victims of the military crackdown that killed hundreds — if not thousands — of people in 1989.
The commemorations in Washington, which also included a candlelight vigil at the foot of a replica of the Goddess of Democracy — a statue erected in Tiananmen Square during the 1989 movement — are part of the worldwide remembrance of the historic event. It is strictly a taboo in China, however, with no commemoration allowed there or in Hong Kong after Beijing imposed a national security law in 2020.
The Chinese embassy in Washington said in a statement that Beijing “has already drawn a clear conclusion on the political disturbance in the late 1980s.”
“The great achievements we made in the past 75 years since the establishment of the People’s Republic of China speak volumes about the right development path we have chosen with the endorsement by our people,” the embassy said.
“We have found a path toward better human rights that reflects the trend of the times and fits our national realities,” read the statement.
The embassy said China opposes the U.S. politicization of human rights issues, use of double standards and interference in China’s internal affairs in the name of human rights.
Rep. Nancy Pelosi, a former House speaker and a longtime supporter of China’s pro-democracy cause, said Tuesday that Beijing has failed to progress democratically.
“What has happened in China under the circumstances in the past 35 years has not been positive in terms of global democracy, in terms of human rights, in terms of promoting democratic freedoms,” Pelosi said.
She urged Americans to stand up against human rights abuses. If Americans don’t, “we lose all moral authority to speak out about human rights in any country in the world,” she said.
Zhou Fengsuo, a former student leader, said the Tiananmen crackdown is once again resonating today, for those who are seeing the danger of the Communist Party.
“Be it the Western society, the general public or China’s younger people, they have shown unprecedented interest,” Zhou said. “Especially after the pandemic, many people have realized all is nothing without freedom.”
Wang Dan, another former student leader, said the bloody Tiananmen crackdown should serve as a wake-up call for those who are still harboring any illusion about the Chinese communist party. “The world needs to be ready for this, that this regime habitually resorts to violence to solve problems,” Wang said.
The U.S. State Department said it remembered the victims of the Tiananmen crackdown and honored those whose voices are now silenced throughout China, including in Xinjiang, Tibet and Hong Kong.
“As Beijing attempts to suppress the memory of June 4, the United States stands in solidarity with those who continue the struggle for human rights and individual freedom,” the agency said in a statement. “The courage and sacrifice of the people who stood up in Tiananmen Square thirty-five years ago will not be forgotten.”

IMAGES
VIDEO
COMMENTS
Problem solving has, therefore, drawn much of medical education researchers' attention. This focus has been important but it is limited in terms of preparing clinicians to deal with the complexity of the 21st century healthcare system in which they will provide team-based care for patients with complex medical illness. ... As such we need to ...
Vasculopathy - CNS. Visceral Air. Visual Field Defects. Weakness Thought Train. Weight loss. Wide complex tachycardia. Frameworks alphabetically Cardiac Neuro Lung GI Renal Infectious Liver Rheum Blood Electrolytes Endocrine Miscellaneous Icons made by Kara Lau All Frameworks Abdominal DistensionAbdominal Pain OverviewAbdominal Pain - Image ...
The Clinical Problem Solvers Democratizing clinical reasoning education Podcast Morning Report RLR CPSolvers Frameworks - Scripts Get Involved!
This chapter introduces the concept of clinical reasoning. It attempts to define what clinical reasoning is and what its features are. Solving clinical problems involves the ability to reason about causality of pathological processes, requiring knowledge of anatomy and the working and pathology of organ systems, and it requires the ability to compare patient problems as patterns with instances ...
M.K. Finta and OthersN Engl J Med 2024;390:456-462. A 43-year-old woman presented with a 1-week history of dysuria and lower abdominal pressure but no fevers, hematuria, or flank pain. She had had ...
Some aspects of medical problem solving have received little attention. For example, research on medical problem solving typically employs cases that can best be called "medical whodunnits,"—clear-cut cases in which a single diagnosis can account for all the findings. In such cases, problem solving is equivalent to arriving at the diagnosis.
This is the fourth in a series of five articles This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential ...
The purpose of using a structured approach to medical problem-solving is to scaffold students' internalization of a systematic approach to clinical reasoning. As students progress toward clinical years, they will need less scaffolding and greater challenges. The Clinical Reasoning Course is a longitudinal learning experience that expects to ...
Problem solving has, therefore, drawn much of medical education researchers' attention. This focus has been important but it is limited in terms of preparing clinicians to deal with the complexity of the 21st century healthcare system in which they will provide team-based care for patients with complex medical illness.
Patient management problems and clinical problem-solving cases have been incorporated into certifying examinations and continuing education programs. Such simulations, in print or electronic form, allow users to select diagnostic or treatment options for hypothetical patients with immediate feedback on management decisions.
A physician with a master's degree in biomedical informatics, Chin has started two health tech companies that employ artificial intelligence to solve problems. "I think as a physician, you always feel like things can be better," he said. "When you are in med school, you learn a lot of medical knowledge.
The clinical problem solving/diagnostic reasoning session is designed to provide a window into the master clinician's thought process and reasoning strategies. The session serves as a valuable tool to learn and teach the process of hypothesis generation (eliciting the right question), problem representation (problem list), prioritized ...
Problem-solving therapy is a short-term treatment used to help people who are experiencing depression, stress, PTSD, self-harm, suicidal ideation, and other mental health problems develop the tools they need to deal with challenges. This approach teaches people to identify problems, generate solutions, and implement those solutions.
problem solving: the process of recognizing a problem, defining it, identifying alternative plans to resolve the problem, selecting a plan, organizing steps of the plan, implementing the plan, and evaluating the outcome; a performance component of occupational therapy.
Instructions to selected subjects in investigation of early hypothesis generation. Medical Problem Solving by Arthur S. Elstein, Lee S. Shulman, Sarah A. Sprafka was published on October 1, 2013 by Harvard University Press.
The OODA Loop can be subdivided further into an eight-step problem solving process. Observe. Step 1: Clarify the Problem. This is a critical step. You need to recognize the correct problem and be sure it is completely understood by all. It helps to state the problem by developing a "problem statement" in terms of what, where, when, and the ...
Most medical practices solve problems by identifying a problem and then using a quick fix for prompt resolution. In the long run, it is much better to identify the root cause of the issue and fix it—that will prevent the problem from occurring again. ... Focus on long-term success rather than short-term or quick-fix solutions. Write down the ...
Medical Problem Solving: An Analysis of Clinical Reasoning. Elstein AS, ed. Cambridge, MA: Harvard University Press; 1978. ISBN: 9780674561250. Elstein AS, ed. Cambridge, MA: Harvard University Press; 1978. ISBN: 9780674561250. View more articles from the same authors. Clinical reasoning lies at the heart of formulating diagnoses and selecting ...
Download PDF Here. Search for... Navigation Menu
Leverage conflict for collaborative problem-solving, learn to apply principles and tools to harness conflict constructively and discover how to use conflicts as a focus area to address and solve underlying functional problems, leading to enhanced team cohesion, satisfaction and productivity.
But decision fatigue isn't the only cost of ineffective decision making. According to a McKinsey survey of more than 1,200 global business leaders, inefficient decision making costs a typical Fortune 500 company 530,000 days of managers' time each year, equivalent to about $250 million in annual wages. That's a lot of turtlenecks.
FAC Number Effective Date HTML DITA PDF Word EPub Apple Books Kindle; 2024-05: 05/22/2024
Solve your math problems using our free math solver with step-by-step solutions. Our math solver supports basic math, pre-algebra, algebra, trigonometry, calculus and more. ... For any term t except 0, t^{0}=1. 89 . For any term t, t\times 1=t and 1t=t. Examples. Quadratic equation { x } ^ { 2 } - 4 x - 5 = 0.
The Histology Multiple Choice Questions (MCQ Quiz) with Answers PDF (Histology MCQ PDF Download): Quiz Questions Chapter 1-29 & Practice Tests with Answers Key (Medical Histology Textbook MCQs, Notes & Study Guide) includes revision guide for problem solving with hundreds of solved MCQs.Histology MCQ with Answers PDF book covers basic concepts, analytical and practical assessment tests.
EPTV NA ESCOLA 2024 | Tema deste ano é: "Inteligência artificial, aliada ou inimiga do nosso futuro?". #eptv #eptvsuldeminas #eptv1 #eptvnaescola
The Tuesday commemorations, which included former student leaders of the Tiananmen movement and younger activists from mainland China and Hong Kong, come as Washington has shifted its China policy from engagement to competition meant to curb China's growing influences, which the U.S. sees as potentially upsetting the world order. The two countries also are clashing over Beijing's ...