Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Center for Bloodless Medicine and Surgery
Case study: urology, severe prostatic hypertrophy with urinary tract obstruction and acute kidney injury.
A 62-year old male presented with a mild fever and acute renal failure with an elevated creatinine of 14.5, and a BUN of 143. Urology and Nephrology were consulted and a renal ultrasound showed bilateral hydronephrosis. A foley catheter was placed to relieve the obstruction and the laboratory tests indicated that his renal function had normalized: creatinine 1.9, and BUN 6. He was sent home with a hemoglobin level of 10.0 g/dL, with a plan to treat his anemia and bring him back for a simple prostatectomy to treat his benign prostatic hypertrophy (BPH).
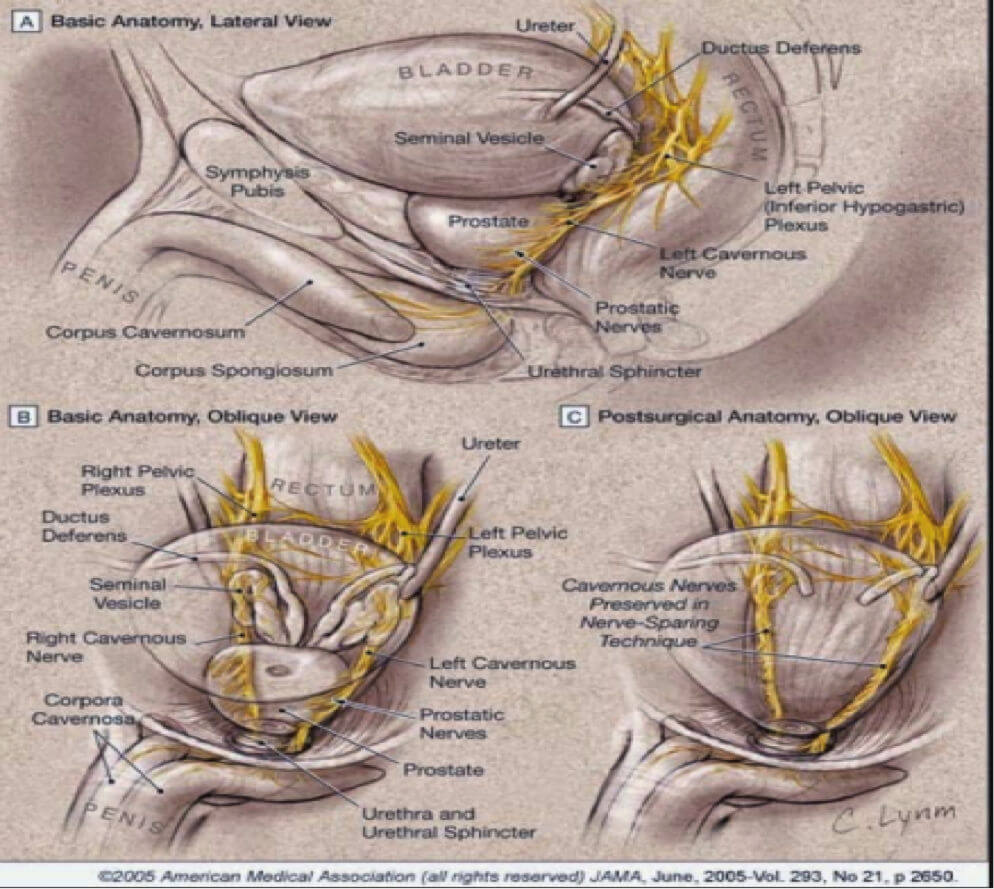
Discussion between the Bloodless Medicine team and the Urologist (Dr. Misop Han) resulted in the somewhat counterintuitive determination that the typical blood loss from a simple prostatectomy is greater than the blood loss with a radical prostatectomy. Therefore, the target hemoglobin level prior to his surgery was 13 g/dL. Since his laboratory tests revealed iron deficiency, he was started on an oral regimen of iron sulfate 325 mg, three times per day. We recommended that he take it with orange juice to enhance gastrointestinal absorption, and we also recommended Miralax prophylactically to prevent constipation from the iron. The patient was also counseled by our Nurse Coordinator (Liz Dackiw) on foods that were rich in iron.
Two months later he was admitted to the hospital to undergo a Robot-assisted laparoscopic simple prostatectomy by Dr. Han. The preoperative hemoglobin level was 12.9, his estimated blood loss during the procedure was 500 mLs, and his hemoglobin upon discharge on postoperative day 3 was 9.3 g/dL. His creatinine upon discharge was 0.9 indicating that his kidney function had returned to normal. His foley catheter was removed a week later on a follow up visit.

Patient Case 1: A 65-Year-Old Man With Prostate Cancer
Specialist Brian Helfand, MD, PhD, reviews the case of a 65-year-old man with prostate cancer and shares insight on strategies to monitor for recurrence.
EP: 1 . Patient Case 1: A 65-Year-Old Man With Prostate Cancer
Ep: 2 . overview of available imaging for patients with prostate cancer, ep: 3 . optimizing selection of imaging modalities for patients with prostate cancer, ep: 4 . prostate cancer: imaging considerations for patients receiving adt, ep: 5 . patient case 2: a 77-year-old man with prostate cancer, ep: 6 . prostate cancer: recommendations after negative imaging results, ep: 7 . future directions in imaging for patients with prostate cancer.
Transcript:
Brian Helfand, MD, PhD: Hello, I’m Brian Helfand. I’m a urologist at NorthShore University HealthSystem in Chicago, Illinois. Today I’m going to talk about 2 cases. The first presentation is a gentleman who’s 65 years old who was previously diagnosed with clinically localized favorable intermediate-risk prostate cancer. He previously underwent radical prostatectomy and pelvic lymph node dissection. Although lymph nodes at the time of surgery were negative, he had positive surgical margins. Subsequently, he received external beam radiation therapy and was started on leuprolide with instructions to follow up and recheck his PSA [prostate-specific antigen] levels every 6 months.
We subsequently followed this patient, and while he was on hormone deprivation therapy, his PSA remained undetectable through 18 months. However, the PSA level increased to 0.8 ng/mL at his 24-month follow-up. His PSA levels were checked 3 months later and were determined to be 1.2 ng/mL, which is a significant increase. The patient then underwent a fluciclovine F-18 PET [positron emission tomography] imaging for suspicion of reoccurrence, and the results demonstrated 2 positive pelvic lymph nodes.
In discussion of this patient who underwent a definitive curative therapy and subsequently had a relatively quick PSA recurrence within the first 24 months, what are we starting to think when we see these type of patients? The truth is that this is a very common scenario. Whether it’s the first 18 months, 24 months, or even 5 years of following patients, you will see a significant number of biochemical recurrences. When you look at the actual numbers, within 15 to 20 years, you see that 40% to 50% of patients—depending on their initial pathology—may experience recurrence. When you think about this, this is something we have to be able to identify because localizing where that recurrence is imperative to subsequent therapy and certainly a personalized treatment plan.
When we look at the grand scope of things, this has been a problem for a long time. When we’ve used the technologies that we’ve had available, meaning a CT scan, a bone scan, or more recently an MRI, we haven’t had the sensitivity or specificity to diagnose these patients or [pinpoint] where their recurrences are localized to. That’s why we’ve had a very high rate of recurrence after we treated these patients with salvage therapies. And the ability to localize where the recurrence is coming from is imperative.
Transcript edited for clarity.
TRANSFORM trial to evaluate screening methods in prostate cancer
Investigators will begin setting up the TRANSFORM trial in spring 2024, with study recruitment set to begin later in the year

Dr. Murphy on increasing diversity in cancer clinical trials
In this podcast episode, Adam B. Murphy, MD, MBA, MSCI, discusses the need to increase diversity in clinical trials, specifically focusing on studies in prostate cancer.
Study progresses of NK cell therapy in mCRPC
All patients have been successfully dosed in the first cohort of patients, and the Safety Review Committee has granted approval for progression of the study to the second dose level of INKmune.
Dr. Schwen on focal therapies for prostate cancer
Zeyad Schwen, MD, a urologic oncologist at Cleveland Clinic, discusses how patient factors and cancer characteristics are key to deciding between focal therapies and whole gland treatment for prostate cancer.
Enzalutamide granted approval in EU for nmHSPC
The approval is supported by data from the phase 3 EMBARK trial, which demonstrated that enzalutamide with or without leuprolide prolonged metastasis-free survival compared with leuprolide alone in patients with high-risk biochemically recurrent nmHSPC.
Trial of ONCT-534 in mCRPC progresses to higher dose level
"We look forward to announcing initial efficacy and safety data from the study, which we expect will be at the end of this quarter," says Salim Yazji, MD.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

VICTORIA J. SHARP, MD, DANIEL K. LEE, MD, AND ERIC J. ASKELAND, MD
A more recent article on office-based urinalysis is available.
Am Fam Physician. 2014;90(8):542-547
Author disclosure: No relevant financial affiliations.
Urinalysis is useful in diagnosing systemic and genitourinary conditions. In patients with suspected microscopic hematuria, urine dipstick testing may suggest the presence of blood, but results should be confirmed with a microscopic examination. In the absence of obvious causes, the evaluation of microscopic hematuria should include renal function testing, urinary tract imaging, and cystoscopy. In a patient with a ureteral stent, urinalysis alone cannot establish the diagnosis of urinary tract infection. Plain radiography of the kidneys, ureters, and bladder can identify a stent and is preferred over computed tomography. Asymptomatic bacteriuria is the isolation of bacteria in an appropriately collected urine specimen obtained from a person without symptoms of a urinary tract infection. Treatment of asymptomatic bacteriuria is not recommended in nonpregnant adults, including those with prolonged urinary catheter use.
Urinalysis with microscopy has proven to be an invaluable tool for the clinician. Urine dipstick testing and microscopy are useful for the diagnosis of several genitourinary and systemic conditions. 1 , 2 In 2005, a comprehensive review of urinalysis was published in this journal. 3 This article presents a series of case scenarios that illustrate how primary care physicians can utilize the urinalysis in common clinical situations.
Microscopic Hematuria: Case 1
Microscopic hematuria is common and has a broad differential diagnosis, ranging from completely benign causes to potentially invasive malignancy. Causes of hematuria can be classified as glomerular, renal, or urologic 3 – 5 ( Table 1 6 ) . The prevalence of asymptomatic microscopic hematuria varies among populations from 0.18% to 16.1%. 4 The American Urological Association (AUA) defines asymptomatic microscopic hematuria as three or more red blood cells per high-power field in a properly collected specimen in the absence of obvious causes such as infection, menstruation, vigorous exercise, medical renal disease, viral illness, trauma, or a recent urologic procedure. 5 Microscopic confirmation of a positive dipstick test for microscopic hematuria is required. 5 , 7
DIAGNOSTIC APPROACH
Case 1: microscopic hematuria.
A 58-year-old truck driver with a 30-year history of smoking one pack of cigarettes per day presents for a physical examination. He reports increased frequency of urination and nocturia, but does not have gross hematuria. Physical examination reveals an enlarged prostate. Results of his urinalysis with microscopy are shown in Table 2 .
Based on this patient's history, symptoms, and urinalysis findings, which one of the following is the most appropriate next step?
A. Repeat urinalysis in six months.
B. Obtain blood urea nitrogen and creatinine levels, perform computed tomographic urography, and refer for cystoscopy.
C. Treat with an antibiotic and repeat the urinalysis with microscopy.
D. Inform him that his enlarged prostate is causing microscopic hematuria, and that he can follow up as needed.
E. Perform urine cytology to evaluate for bladder cancer.
The correct answer is B .
For the patient in case 1 , because of his age, clinical history, and lack of other clear causes, the most appropriate course of action is to obtain blood urea nitrogen and creatinine levels, perform computed tomographic urography, and refer the patient for cystoscopy. 5 An algorithm for diagnosis, evaluation, and follow-up of patients with asymptomatic microscopic hematuria is presented in Figure 1 . 5 The AUA does not recommend repeating urinalysis with microscopy before the workup, especially in patients who smoke, because tobacco use is a risk factor for urothelial cancer ( Table 3 ) . 5
A previous article in American Family Physician reviewed the American College of Radiology's Appropriateness Criteria for radiologic evaluation of microscopic hematuria. 8 Computed tomographic urography is the preferred imaging modality for the evaluation of patients with asymptomatic microscopic hematuria. 5 , 8 It has three phases that can detect various causes of hematuria. The non–contrast-enhanced phase is optimal for detecting stones in the urinary tract; the nephrographic phase is useful for detecting renal masses, such as renal cell carcinoma; and the delayed phase outlines the collecting system of the urinary tract and can help detect urothelial malignancies of the upper urinary tract. 9 Although the delayed phase can detect some bladder masses, it should not replace cystoscopy in the evaluation for bladder malignancy. 9 After a negative microscopic hematuria workup, the patient should continue to be followed with yearly urinalysis until at least two consecutive normal results are obtained. 5
In patients with microscopic hematuria, repeating urinalysis in six months or treating empirically with antibiotics could delay treatment of potentially curable diseases. It is unwise to assume that benign prostatic hyperplasia is the explanation for hematuria, particularly because patients with this condition typically have risk factors for malignancy. Although urine cytology is typically part of the urologic workup, it should be performed at the time of cystoscopy; the AUA does not recommend urine cytology as the initial test. 5
Dysuria and Flank Pain After Lithotripsy: Case 2
After ureteroscopy with lithotripsy, a ureteral stent is often placed to maintain adequate urinary drainage. 10 The stent has one coil that lies in the bladder and another that lies in the renal pelvis. Patients with ureteral stents may experience urinary frequency, urgency, dysuria, flank pain, and hematuria. 10 They may have dull flank pain that becomes sharp with voiding. This phenomenon occurs because the ureteral stent bypasses the normal nonrefluxing uretero-vesical junction, resulting in transmission of pressure to the renal pelvis with voiding. Approximately 80% of patients with a ureteral stent experience stent-related pain that affects their daily activities. 11
POTENTIALLY MISLEADING URINALYSIS
Case 2: dysuria and flank pain after lithotripsy.
A 33-year-old woman with a history of nephrolithiasis presents with a four-week history of urinary frequency, urgency, urge incontinence, and dysuria. She recently had ureteroscopy with lithotripsy of a 9-mm obstructing left ureteral stone; she does not know if a ureteral stent was placed. She has constant dull left flank pain that becomes sharp with voiding. Results of her urinalysis with microscopy are shown in Table 4 .
A. Treat with three days of ciprofloxacin (Cipro), and tailor further antibiotic therapy according to culture results.
B. Treat with 14 days of ciprofloxacin, and tailor further antibiotic therapy according to culture results.
C. Obtain a urine culture and perform plain radiography of the kidneys, ureters, and bladder.
D. Perform a 24-hour urine collection for a metabolic stone workup.
E. Perform computed tomography.
The correct answer is C .
The presence of a ureteral stent causes mucosal irritation and inflammation; thus, findings of leukocyte esterase with white and red blood cells are not diagnostic for urinary tract infection, and a urine culture is required. In this setting, plain radiography of the kidneys, ureters, and bladder would be useful to determine the presence of a stent. If a primary care physician identifies a neglected ureteral stent, prompt urologic referral is indicated for removal. Retained ureteral stents may become encrusted, and resultant stone formation may lead to obstruction. 10
Flank discomfort and recent history of urinary tract manipulation suggest that this is not an uncomplicated urinary tract infection; therefore, a three-day course of antibiotics is inadequate. Although flank pain and urinalysis suggest possible pyelonephritis, this patient should not be treated for simple pyelonephritis in the absence of radiography to identify a stent. A metabolic stone workup may be useful for prevention of future kidney stones, but it is not indicated in the acute setting. Finally, although computed tomography would detect a ureteral stent, it is not preferred over radiography because it exposes the patient to unnecessary radiation. Typically, microscopic hematuria requires follow-up to ensure that there is not an underlying treatable etiology. In this case , the patient's recent ureteroscopy with lithotripsy is likely the etiology.
Urinalysis in a Patient Performing Clean Intermittent Catheterization: Case 3
Case 3: urinalysis in a patient performing clean intermittent catheterization.
A 49-year-old man who has a history of neurogenic bladder due to a spinal cord injury and who performs clean intermittent catheterization visits your clinic for evaluation. He reports that he often has strong-smelling urine, but has no dysuria, urge incontinence, fever, or suprapubic pain. Results of his urinalysis with microscopy are shown in Table 5 .
A. Inform the patient that he has a urinary tract infection, obtain a urine culture, and treat with antibiotics.
B. Refer him to a urologist for evaluation of a complicated urinary tract infection.
C. Perform computed tomography of the abdomen and pelvis to evaluate for kidney or bladder stones.
D. Inform him that no treatment is needed.
E. Obtain a serum creatinine level to evaluate for chronic kidney disease.
The correct answer is D .
Although the urinalysis results are consistent with a urinary tract infection, the clinical history suggests asymptomatic bacteriuria. Asymptomatic bacteriuria is the isolation of bacteria in an appropriately collected urine specimen obtained from a person without symptoms of a urinary tract infection. 12 The presence of bacteria in the urine after prolonged catheterization has been well described; one study of 605 consecutive weekly urine specimens from 20 chronically catheterized patients found that 98% contained high concentrations of bacteria, and 77% were polymicrobial. 13
Similar results have been reported in patients who perform clean intermittent catheterization; another study of 1,413 urine cultures obtained from 407 patients undergoing clean intermittent catheterization found that 50.6% contained bacteria. 14 Guidelines from the Infectious Diseases Society of America recommend against treatment of asymptomatic bacteriuria in nonpregnant patients with spinal cord injury who are undergoing clean intermittent catheterization or in those using a chronic indwelling catheter. 12
In the absence of symptoms of a urinary tract infection or nephrolithiasis, there is no need to culture the urine, treat with antibiotics, refer to a urologist, or perform imaging of the abdomen and pelvis. There is no reason to suspect acute kidney injury in this setting; thus, measurement of the serum creatinine level is also unnecessary.
Data Sources : Literature searches were performed in PubMed using the terms urinalysis review, urinalysis interpretation, microscopic hematuria, CT urogram, urinary crystals, indwelling ureteral stent, asymptomatic bacteriuria, and bacteriuria with catheterization. Guidelines from the American Urological Association were also reviewed. Search dates: October 2012 and June 2013.
Wu X. Urinalysis: a review of methods and procedures. Crit Care Nurs Clin North Am. 2010;22(1):121-128.
Hardy PE. Urinalysis interpretation. Neonatal Netw. 2010;29(1):45-49.
Simerville JA, Maxted WC, Pahira JJ. Urinalysis: a comprehensive review [published correction appears in Am Fam Physician . 2006;74(7):1096]. Am Fam Physician. 2005;71(6):1153-1162.
Cohen RA, Brown RS. Clinical practice. Microscopic hematuria. N Engl J Med. 2003;348(23):2330-2338.
American Urological Association. Diagnosis, evaluation and follow-up of asymptomatic microhematuria (AMH) in adults. http://www.auanet.org/education/asymptomatic-microhematuria.cfm . Accessed June 6, 2014.
Ahmed Z, Lee J. Asymptomatic urinary abnormalities. Hematuria and proteinuria. Med Clin North Am. 1997;81(3):641-652.
Rao PK, Jones JS. How to evaluate ‘dipstick hematuria’: what to do before you refer. Cleve Clin J Med. 2008;75(3):227-233.
Choyke PL. Radiologic evaluation of hematuria: guidelines from the American College of Radiology's Appropriateness Criteria. Am Fam Physician. 2008;78(3):347-352.
Sadow CA, Wheeler SC, Kim J, Ohno-Machado L, Silverman SG. Positive predictive value of CT urography in the evaluation of upper tract urothelial cancer. AJR Am J Roentgenol. 2010;195(5):W337-W343.
Haleblian G, Kijvikai K, de la Rosette J, Preminger G. Ureteral stenting and urinary stone management: a systematic review. J Urol. 2008;179(2):424-430.
Joshi HB, Stainthorpe A, MacDonagh RP, Keeley FX, Timoney AG, Barry MJ. Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol. 2003;169(3):1065-1069.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults [published correction appears in Clin Infect Dis . 2005;40(10):1556]. Clin Infect Dis. 2005;40(5):643-654.
Warren JW, Tenney JH, Hoopes JM, Muncie HL, Anthony WC. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982;146(6):719-723.
Bakke A, Digranes A. Bacteriuria in patients treated with clean intermittent catheterization. Scand J Infect Dis. 1991;23(5):577-582.
Continue Reading
More in AFP
More in pubmed.
Copyright © 2014 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

Ethical Dimensions of Urology: Four Case Studies
- First Online: 01 January 2012
Cite this chapter

- Marc S. Cohen MD 3 &
- Ray E. Moseley PhD 4
2011 Accesses
In recent years, the progression of medical science has led to what used to be extremely rare ethical problems on the cutting edge of urological management of male infertility to become a more routine part of urological practice. These ethical problems, even though they have become more common in urological practice, still cause significant issues for the physician. In this chapter we discuss four cases that illustrate the ethical problems associated with identification and framing of the ethical problem, analysis of the problem, and the resolution of the problem. The basic purpose of these case discussions is that it is much easier to avoid and/or satisfactorily resolve an ethical problem when it is recognized early before a crisis mode arises or before poor ethical decisions are made and have to be unraveled after the fact. These cases represent four possible scenarios but are by no means exhaustive of the possible ethical issues that may arise from the current urological practice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Neal MS, Nagel K, Duckworth J, Bissessar H, Fischer MA, Portwine C, Tozer R, Barr RD. Effectiveness of sperm banking in adolescents and young adults with cancer: a regional experience. Cancer. 2007;110:1125–30.
Article PubMed Google Scholar
Miller VA, Drotar D, Kodish E. Children’s competence for assent and consent: a review of empirical findings. Ethics Behav. 2004;14:255–96.
Covey Stephen R. The seven habits of highly effective people: powerful lessons in personal change. New York: Simon and Schuster Inc; 1990. p. 237.
Google Scholar
Goldstein MM. Health information technology and the idea of informed consent. J Law Med Ethics. 2010;38:27–36.
Howard G. Who asks for vasectomy reversal and why? Br Med J (Clin Res Ed). 1982;285:490–3.
Article CAS Google Scholar
Lachance D. In re Grady: the mentally retarded individual’s right to choose sterilization. Am J Law Med. 1981;6:559–91.
PubMed CAS Google Scholar
Zuba-Ruggieri R. Making links, making connections: internet resources for self-advocates and people with developmental disabilities. Intellect Dev Disabil. 2007;45:209–16.
Article Google Scholar
Download references
Author information
Authors and affiliations.
Department of Urology, Shands at the University of Florida, 1600 SW Archer Boulevard, 100247 HSC, Gainesville, FL, 32610, USA
Marc S. Cohen MD
Department of Community Health and Family Medicine, University of Florida Health Science Center, 100237, Gainesville, FL, 100234, USA
Ray E. Moseley PhD
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Marc S. Cohen MD .
Editor information
Editors and affiliations.
University of Florida, Director, Robotic Surgery, Winter Haven Hospital &, 200 Avenue F. N.E., Winter Haven, 33881, Florida, USA
Sijo J. Parekattil
Center for Reproductive Medicine, Department of Urology, Cleveland Clinic, Euclid Avenue 9500, Cleveland, 44195, Ohio, USA
Ashok Agarwal
Rights and permissions
Reprints and permissions
Copyright information
© 2012 Springer Science+Business Media, LLC
About this chapter
Cohen, M.S., Moseley, R.E. (2012). Ethical Dimensions of Urology: Four Case Studies. In: Parekattil, S., Agarwal, A. (eds) Male Infertility. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-3335-4_16
Download citation
DOI : https://doi.org/10.1007/978-1-4614-3335-4_16
Published : 02 May 2012
Publisher Name : Springer, New York, NY
Print ISBN : 978-1-4614-3334-7
Online ISBN : 978-1-4614-3335-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
ED. Obstructing stones with fever and leukocytosis. emergency- be worried. Study with Quizlet and memorize flashcards containing terms like lower urinary tract symptoms (LUTS) Mr. Jones states that he has been extremely bothered over the last few months with the need to urinate every 30-60 minutes.
-keep the foley bag below the level of the bladder at all times. Keep latched to leg with stat lock, and empty bag when it becomes 2/3 full-hand hygiene before touching the catheter.Catheter care with soap and water twice daily-drink 2-3 liters of water daily-teach about signs/symptoms of CAUTI (cloudy urine, foul smelling, generalized abdominal pain, hematuria, malaise and fever)
Challenging cases in urology: A case of hydronephrosis, sepsis, and pain. A 61-year-old female complains of acute-onset right-sided flank and abdominal pain. She describes associated nausea, but denied urinary symptoms, hematuria, fever, or chills. Sara Valente, MD, is a fourth-year urology resident at the University of Connecticut School of ...
The patient-described in this article is a typical case. D-J tubes are widely used in urology. Long-term retention in the body can form a large number of stones with the D-J tube as the core. ... Mikhail A, et al. Prospective randomized study of various techniques of percutaneous nephrolithotomy. Urology 2001; 58:345-50. 10.1016/S0090-4295(01 ...
A 62-year old male presented with a mild fever and acute renal failure with an elevated creatinine of 14.5, and a BUN of 143. Urology and Nephrology were consulted and a renal ultrasound showed bilateral hydronephrosis. A foley catheter was placed to relieve the obstruction and the laboratory tests indicated that his renal function had ...
URINALYSIS CASE STUDIES You will answer the questions for each of these short case studies in your Lab Assignment. Do some research and use Table 1 (p) in the UNF Lab Manual or in the PowerPoint to help diagnose the patients. CASE STUDY. History:
Case Study 1. Patient J.O., currently 42 years of age, consulted our practice seeking additional information about and optimal care of her rare kidney stone disorder. ... In the modern era of advanced minimally invasive urology, chronic kidney disease is still common in cystinuria, and end stage kidney disease requiring dialysis or ...
Chapter 50 Renal and Urologic Problems Answer Keys for Questions - Rationales for Bridge to NCLEX Examination Questions. Correct answer: b Rationale: When teaching a patient to prevent a recurrence of a urinary tract infection, the nurse should explain the importance of emptying the bladder before and after sexual intercourse.
2. Urinary System Case Study Handout Instructions: Below is a case study presentation of a patient with a urinary condition. Read the case study and answer the questions. Some questions ask for information not included within this lesson. Use your text, a medical dictionary, or any other reference material you choose to answer these questions.
• Due to low fluid intake, urine stasis, persistent UTIs, primary metabolic disturbances (e.g in diabetes) • Leads to increased concentration of solutes predisposes to calculi formation • Can make 'gravel like' or staghorn calculi - a large calculus shaped to the contours of the pelvicalyceal system • Can cause intense pain aka renal colic = may radiate from the back to the flank of ...
The first presentation is a gentleman who's 65 years old who was previously diagnosed with clinically localized favorable intermediate-risk prostate cancer. He previously underwent radical prostatectomy and pelvic lymph node dissection. Although lymph nodes at the time of surgery were negative, he had positive surgical margins.
Nursing questions and answers. Case Study, Chapter 37, Urinary Elimination 1. You are a urologic nurse whose patient has voiced concern over his kidneys losing their function within the past few weeks. He has maintained a log of the past week, recording his urination and fluid intake. He has a history of diabetes mellitus and hypertension ...
The prevalence of asymptomatic microscopic hematuria varies among populations from 0.18% to 16.1%. 4 The American Urological ... For the patient in case 1, ... another study of 1,413 urine ...
Giant hydronephrosis secondary to ureteropelvic junction obstruction, a rare occurrence, case report. Seid Mohammed Hassen, Feysel Hassen Issack, Ferid Ousman Mummed, Ibsa Kedir Hassen. Article 101803. View PDF.
Urology Case Reports is one of a series of specialist open access titles launched by the journal Urology.It is dedicated to publishing case reports in all areas of adult and pediatric urology.Accepted case reports must be authentic, understandable, educational, and clinically interesting to an international audience of practicing urologists, trainees, and researchers.
Ethical dilemmas in urology. Cryopreservation. Legal concerns. In recent years, the progression of medical science has led to what used to be extremely rare ethical problems on the cutting edge of urological management of male infertility to become a more routine part of urological practice. These ethical problems, even though they have become ...
1. Introduction. In urology, lower urinary tract symptoms (LUTS) are common complaints associated with ageing. ... Because the first option for least urgency in the third question was excluded by some participants as a possible answer (see Section 3.1.3), ... In our study, this was also the case with the IPSS. With the visual alternatives, VPSS ...
Study with Quizlet and memorize flashcards containing terms like To respond to the following questions refer to the case study preceding this assignment. William Thomas is a 66 y/o man who received a renal transplant in 12/2009. He presents to Urology Associates, Inc. clinic with _____ (complaint). He received the renal transplant because he had irreversible loss of the function of both kidneys.
Answer: a. To drain urine from the bladder when the patient …. Use CASE 1 -Urology Consultation: Acute Urinary Retention to answer--What is the purpose of a urinary catheter? O a. To drain urine from the bladder when the patient is unable to void normally or to obtain a urine specimen for diagnostic evaluation O b.
2. Urinary System Case Study Handout Instructions: Below is a case study presentation of a patient with a urinary condition. Read the case study and answer the questions. Some questions ask for information not included within this lesson. Use your text, a medical dictionary, or any other reference material you choose to answer these questions.
Operations Management questions and answers; Case Study 34.1 Managing change in the urology department of a hospital in England The Department of Urology in an NHS hospital in England is struggling to respond to external pressures for change. The manager responsible for the department has approached you for advice about how to manage the situation.
Case Study: Cystitis. approx 30 min. Ms. Vance, age 28 years, has noticed urgency, frequency, and dysuria recently, as well as an unusual odor to the urine. Urinalysis indicated a heavy concentration of Escherichia coli in the urine, some pus, and WBCs. Ms. T was prescribed antibiotics, which she took for the first few days.
A. is supplied by the same nerves from the spinal cord that supply the skin of the abdomen. B. lines the walls of the abdominal cavity and is stimulated when the solid abdominal organs contract. C. is less likely to become inflamed or infected because it lines the abdominal organs themselves. D. is supplied by nerves of the autonomic nervous ...