Take Action Against Addiction
Drug abuse affects all of us, and we must act to prevent more unnecessary deaths.

iStockPhoto
It's time to take action against addiction.
In recent weeks, a spate of media attention has once again alerted Americans to our epidemic of narcotic drug abuse – and its destructive and fatal consequences. My recent piece in this publication spoke to the political promise for a response in this country because an epidemic is indifferent to whether a person is Republican, Democrat or independent. We are all besieged by this problem; an epidemic makes no distinctions between white, black, Hispanic or Asian, rich or poor, urban or rural, or young or old.
For the doers among us, we need to decide and act on what can be done to contain this epidemic. Unnecessary deaths can be averted, and we can do far better to protect against the personal, community and economic devastation that addiction wreaks on a society. At the risk of missing a few things, I offer below 10 actions individuals, families and communities (including our policymakers and insurers) can do. These are not meant to be taken in rank order; rather, the more taken, the greater our chances of success.
1. Reduce overdose deaths by providing easy access to naloxone. Naloxone, now available as a nasal spray, immediately blocks the deadly respiratory suppression caused by heroin, methadone and narcotic pain pills (like OxyContin, Percodan and Vicodin), and it should be made easily available to first responders, families and those dependent on narcotics and their friends. In 2014, overdose deaths from prescription pain pills reached nearly 19,000, a more than threefold increase from 2001. Over 47,000 people total overdosed that same year.
2. Identify and crack down on prescribers who are providing large quantities of narcotics in so-called pill mills. Use state prescription databases to identify these prescirbers, and distinguish them from doctors legitimately practicing with populations of pain and cancer patients.
3. Employ TV, radio and social media to educate families about drug-abuse prevention. This has been repeatedly shown to reduce the non-medical use of narcotic pain pills.
4. Establish and implement medical guidelines for the treatment of chronic pain. This can be done through quality improvement techniques and performance improvement strategies.
5. Make problem drug and alcohol use screening a standard of care. Screening for this abuse should be a universal practice, used with adult patients seen in primary care settings to identify and intervene early before addiction sets in and overtakes an individual. Screening, brief intervention and referral for treatment, or SBIRT , is a proven intervention that is generally covered by insurers, including Medicaid and Medicare. This intervention has also been adapted for teenage detection and intervention of drug and alcohol problems.
6. Increase the availability, affordability and access to drug treatment programs. An estimated 80 to 90 percent of individuals who could benefit from treatment are not getting it. Celebrities who can pay vast sums for private treatment programs should not be the only ones able to enter them. The Affordable Care Act requires as an essential service element coverage and parity for mental health and substance use disorders, meaning that insurance benefits for addiction must be equivalent to any other covered general medical condition. The opportunity for proper reimbursement for substance disorder treatment has never been better.
7. Educate doctors, patients and families about what good addiction treatment must include. Medical providers, not just addiction specialists, need to appreciate the underlying neuroscience of addiction and fashion their treatment accordingly. Patients and families need to be far more informed consumers in order to advocate for effective treatments.
8. Expose treatment centers not providing comprehensive treatment for substance abuse as falling below standards of quality of care . 12-Step recovery programs (like Alcoholics Anonymous and Narcotics Anonymous) are important as a part of a comprehensive treatment program, but have low rates of effectiveness alone. Treatment options must include motivational enhancement, cognitive-behavioral treatments, relapse prevention, family education and support, wellness efforts and medication to help prevent relapse and maintain sobriety.
9. Promote and pay for the use of medication-assisted treatment. This means that recovery efforts can include medication . The use of medication should not be exhorted as a violation of sobriety. A number of medications now exist for drug and alcohol addiction (tobacco too) that improve rates of abstinence – or reduce use, called harm reduction. These include buprenorphine (Suboxone), methadone, naltrexone (including the 28-day injectable Vivitrol) and naloxone. Let's give people in recovery as good a chance as possible not be drawn into puritanical and outdated notions of recovery.
10. Keep hope alive. People with substance use disorders can recover. That takes good treatment, hard work, ongoing support and keeping hope alive. People with addictions do get on the path to recovery – but it is hard to predict when that will happen. For some it is early, even after one or two rehabilitation programs. For others it may take five, 10 or 20 rehab programs, and the pain and suffering of too many relapses. Persons affected, their families and clinical providers need to sustain hope that recovery can happen during what can be a protracted and very dark time. The darkest moments, the most deadly, are when hope evaporates, which is when exile from family, friends and communities and suicide are more likely.
We surely have an epidemic of drug use and abuse. This country, and others, have successfully faced and overcome many an epidemic. The sooner we act, the more comprehensively we act, the more lives and families will be spared.
Tags: drugs , drug abuse , alcohol , addiction

More Opinion


U.S. Government Accountability Office
The Crisis of Drug Misuse and Federal Efforts to Address It
Earlier this week, many media outlets ran stories highlighting the growing crisis of drug misuse in the United States. Citing Centers for Disease Control and Prevention (CDC) data, the New York Times said that more than 100,000 Americans died from drug overdoses during a yearlong period ending in April 2021.
Drug misuse—the use of illicit drugs and the misuse of prescription drugs, such as opioids—has been a persistent and long-standing public health issue in the United States. National rates of drug misuse have increased over the last two decades, and are a serious risk to public health, our society, and the economy.
GAO has issued numerous reports highlighting steps the federal government can take to improve its response to this crisis. In 2019, before the pandemic, we raised this issue as a critical one needing attention and in 2020, we decided to add drug misuse to our High Risk List —a list of areas that need immediate attention. And since then we have been looking at how the pandemic has impacted these issues.
Today’s WatchBlog post looks at our work on the drug misuse crisis, and federal efforts to address it.

The federal strategy
In recent years, the federal government has spent billions of dollars and has enlisted more than a dozen agencies to help address drug misuse and its effects.
The National Drug Control Strategy is the federal effort to reduce substance use disorders through a coordinated national drug control policy. The Office of National Drug Control Policy (ONDCP) is responsible for overseeing and coordinating this effort.
Our work has identified deficiencies in the most recent iterations of the Strategy, which could serve as an action plan for addressing this high-risk area. In December 2019 , we recommended that ONDCP develop and implement key planning elements, like resource investments and roles and responsibilities, to help it structure its ongoing efforts and to better position the agency to meet statutory requirements for future iterations of the Strategy.
In November 2020 , we recommended that agencies clarify how their programs help to achieve specific goals of the Strategy.
The availability of treatment and recovery programs
As drug misuse has increased, so has demand for treatment and care. But in December 2020 , we reported that treatment availability has not kept pace with need. The Substance Abuse and Mental Health Services Administration (SAMHSA) told us that while drug misuse is widespread, nearly one-third of U.S. counties (31%) did not have facilities offering any level of substance use disorder treatment.
Some key barriers in addressing demand for treatment include workforce shortages, insurance reimbursement and payment models, federal and state requirements, and the stigma of drug abuse.
SAMHSA administers grant programs aimed at expanding access to treatment for substance misuse. But we found that the data SAMHSA relies on to understand the impact of its awards and efforts was unreliable because it included both individuals who received treatments funded by its grant programs and those who didn’t. We recommended that it improve the quality of data it uses.
After treatment, there are some federal programs for those recovering from drug misuse. For example, the Department of Labor (Labor) provides grants to states to address the employment and training needs of those affected by and recovering from substance use disorders.
In May 2020 , we recommended that Labor share information, such as lessons learned, from states participating in the program with all states, tribal governments, and outlying areas. Labor agreed with our recommendation.
Monitoring the impact of federal efforts
Our past work has identified gaps in the availability and reliability of data for measuring the federal government’s progress with addressing drug misuse.
For example, ONDCP and other federal, state, and local government officials have identified challenges with the timeliness, accuracy, and accessibility of data on overdose cases (both fatal and non-fatal) from law enforcement and public health sources. In March 2018 , we recommended that ONDCP lead a review on ways to improve overdose data.
ONDCP is also responsible for evaluating the effectiveness of national drug control policy efforts across the government. But, in March 2020 , we reported that ONDCP had not fully developed performance evaluation plans to measure progress against each of the Strategy’s long-range goals, as required by law.
Without effective long-term plans that clearly articulate goals and objectives as well as specific measures to track performance, federal agencies cannot fully assess whether taxpayer dollars are invested in ways that will achieve desired outcomes, such as reducing access to illicit drugs and expanding treatment for substance use disorders.
COVID-19’s effects on drug misuse and new federal assistance
It’s not yet known just how much the pandemic has impacted mental health and substance use. But, in September 2020, SAMHSA reported opioid overdose deaths have increased in some areas of the country by as much as 25% to 50% during the pandemic compared to the previous year.
In March 2021 , we reported on the effects that the COVID-19 pandemic was having on demand for behavioral health services, including mental health and substance use disorders. The added stressors caused by the pandemic—such as feelings of isolation and financial stress—have contributed to increases in emergency room visits for overdoses and suicide attempts and requests for other behavioral health services. Our podcast with GAO health care expert John Dicken discusses this report.
Under the CARES Act and other subsequent pandemic relief acts, SAMHSA was appropriated around $8 billion for behavioral health services, which include substance abuse prevention and treatment services and community mental health services, among other activities. For example, specific funds are available for the Certified Community Behavioral Health Clinic Expansion Grant program while other funds can be spent to address emergency substance abuse or mental health needs in local communities.
Our work monitoring the federal response to the drug misuse crisis is ongoing, but to learn more about our findings and recommendations so far, visit our High Risk page on this issue.
- Comments on GAO’s WatchBlog? Contact [email protected] .
GAO Contacts

Related Posts

For World Health Day (April 7), We Look At U.S. Efforts to Promote Global Wellness

American Credit Card Debt Hits a New Record—What’s Changed Post-Pandemic?

In the Next Pandemic Antiviral Drugs Could Be Key, But Are They Ready?
Related products, drug misuse: sustained national efforts are necessary for prevention, response, and recovery, product number, drug misuse: agencies have not fully identified how grants that can support drug prevention education programs contribute to national goals, drug misuse: most states have good samaritan laws and research indicates they may have positive effects, drug control: the office of national drug control policy should develop key planning elements to meet statutory requirements, substance use disorder: reliable data needed for substance abuse prevention and treatment block grant program, workforce innovation and opportunity act: additional dol actions needed to help states and employers address substance use disorder, illicit opioids: while greater attention given to combating synthetic opioids, agencies need to better assess their efforts, behavioral health: patient access, provider claims payment, and the effects of the covid-19 pandemic.

GAO's mission is to provide Congress with fact-based, nonpartisan information that can help improve federal government performance and ensure accountability for the benefit of the American people. GAO launched its WatchBlog in January, 2014, as part of its continuing effort to reach its audiences—Congress and the American people—where they are currently looking for information.
The blog format allows GAO to provide a little more context about its work than it can offer on its other social media platforms. Posts will tie GAO work to current events and the news; show how GAO’s work is affecting agencies or legislation; highlight reports, testimonies, and issue areas where GAO does work; and provide information about GAO itself, among other things.
Please send any feedback on GAO's WatchBlog to [email protected] .
What led to the opioid crisis—and how to fix it
February 9, 2022 – Without urgent intervention, 1.2 million people in the U.S. and Canada will die from opioid overdoses by the end of the decade, in addition to the more than 600,000 who have died since 1999, according to a February 2 report from the Stanford-Lancet Commission on the North American Opioid Crisis. In this Big 3 Q&A, Howard Koh , professor of the practice of public health leadership and a member of the Commission, discusses factors contributing to the crisis and recommendations on how to curb it.
Q: What was the impetus behind this new report on the opioid crisis, and why was it important for this commission to issue the report at this time?
A: The current opioid crisis ranks as one of the most devastating public health catastrophes of our time. It started in the mid-1990s when the powerful agent OxyContin, promoted by Purdue Pharma and approved by the Food and Drug Administration (FDA), triggered the first wave of deaths linked to use of legal prescription opioids. Then came a second wave of deaths from a heroin market that expanded to attract already addicted people. More recently, a third wave of deaths has arisen from illegal synthetic opioids like fentanyl. In addition to the crushing public health burden of preventable deaths, millions more are affected by related problems involving homelessness, joblessness, truancy, and family disruption, for example.
The pandemic has both masked and amplified this crisis. Rising death trends are linked to drivers such as the anxiety and isolation of COVID-19 as well as continued lack of access to quality care and prevention. The crisis seems unchecked. It demands an urgent, unified, and comprehensive response.
Q: What were the main drivers of the opioid crisis, and what are the report’s main takeaways on how to minimize the damage?
A: One major conclusion is that the crisis represents a multi-system failure of regulation. OxyContin approval is one example—Purdue Pharma was later shown to have presented a fraudulent description of the drug as less addictive than other opioids. The profit motive of the pharmaceutical industry remains ever present.
And that’s just the tip of the iceberg. Post-approval, it’s usually left up to industry—not regulators—to educate and advise prescribers on how to evaluate and mitigate risk. Donations from opioid manufacturers to politicians continue to influence policy decisions. In addition, a revolving door of officials leaving government regulatory agencies such as the Drug Enforcement Agency regularly join the pharmaceutical industry with little to no “cooling off” periods. The report details these and other glaring examples.
The report recommends ways to curb pharmaceutical industry influence while also upholding quality care that balances benefits and risks for people with chronic pain. We must continue progress in promoting opioid stewardship—safer prescribing initiatives led by physicians.
Care, treatment, and prevention are all absolutely critical. Currently, addiction care, for example, is not only often separate from mainstream medicine but also unequal. It is also often clouded by stigma, uneven quality, and inaccessibility. Addiction remains a constant long-term threat to human health and won’t respond to only short-term fixes or short-term funding. We have to fully integrate addiction care into mainstream health care, provide enduring and sustained funding, and assure that both public and private insurance cover the full range of addiction services. Parity laws require that most private health plans cover substance use disorder services and not limit them more stringently than services associated with other medical conditions. But such laws are not always followed and that must change.
Addiction training should be an essential part of all health professional education. The public health community can also work with the criminal justice system to move more affected people away from incarceration and towards treatment.
And prevention, starting with kids, is absolutely key. We have to support stronger and more resilient children and families to address threats from opioids, tobacco, alcohol, and other substances that rob so many people of well-being.
Q: When you look at the current state of this crisis, does anything give you hope?
We can see progress in some vital areas. For example, more health professionals are using the term “substance use disorder” instead of “substance abuse” to recognize the condition as a medical and health issue and not a moral failing. And instead of references to people being “clean” or “dirty,” people are increasingly using the medical terms “recovery” and “relapse.” It’s gratifying to see this change in the language of addiction.
The Affordable Care Act has also helped in major ways, starting by requiring that private insurance plans cover substance use disorder services as part of essential health benefits. It also has facilitated expansion of Medicaid, the single largest payer of opioid use disorder services. The report notes that states that have expanded Medicaid eligibility have shown evidence of decreased overdose deaths and increased receipt of treatment.
It is inspiring to celebrate the estimated 25 million people who are in recovery. People in recovery are heroes for me. So many have been able to rebuild relationships with people they care for, contribute again to society, and regain a sense of purpose and meaning in their lives. It may seem to be a hopeless situation but it’s not. In the midst of this terrible crisis, that’s what gives me the greatest hope for the future.
– Karen Feldscher
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How to Overcome Drug Addiction
Treatment options.
- Steps to Take
Intervention
Frequently asked questions.
Drug addiction, or substance use disorder (SUD), is when someone continues using a drug despite harmful consequences to their daily functioning, relationships, or health. Using drugs can change brain structure and functioning, particularly in areas involved in reward, stress, and self-control. These changes make it harder for people to stop using even when they really want to.
Drug addiction is dangerous because it becomes all-consuming and disrupts the normal functioning of your brain and body. When a person is addicted, they prioritize using the drug or drugs over their wellbeing. This can have severe consequences, including increased tolerance to the substance, withdrawal effects (different for each drug), and social problems.
Verywell / Ellen Lindner
Recovering from SUD is possible, but it takes time, patience, and empathy. A person may need to try quitting more than once before maintaining any length of sobriety.
This article discusses how drug addiction is treated and offers suggestions for overcoming drug addiction.
How Common Is Addiction?
Over 20 million people aged 12 or older had a substance use disorder in 2018.
Substance use disorders are treatable. The severity of addiction and drug or drugs being used will play a role in which treatment plan is likely to work the best. Treatment that addresses the specific situation and any co-occurring medical, psychiatric, and social problems is optimal for leading to long-term recovery and preventing relapse.
Detoxification
Drug and alcohol detoxification programs prepare a person for treatment in a safe, controlled environment where withdrawal symptoms (and any physical or mental health complications) can be managed. Detox may occur in a hospital setting or as a first step to the inpatient or outpatient rehabilitation process.
Going through detox is a crucial step in recovery, and it's these first few weeks that are arguably most critical because they are when the risk of relapse is highest.
Detox Is Not Stand-Alone Treatment
Detoxification is not equivalent to treatment and should not be solely relied upon for recovery.
Counseling gets at the core of why someone began using alcohol or drugs, and what they can do to make lasting changes. This may include cognitive behavioral therapy (CBT), in which the patient learns to recognize problematic thinking, behaviors, and patterns and establish healthier ways of coping. CBT can help someone develop stronger self-control and more effective coping strategies.
Counseling may also involve family members to develop a deeper understanding of substance use disorder and improve overall family functioning.
Cognitive behavioral therapy has been shown effective in helping people overcome addiction. In one study, 60% of people with cocaine use dependence who underwent CBT along with prescription medication provided cocaine-free toxicology screens a year after their treatment.
Medication can be an effective part of a larger treatment plan for people who have nicotine use disorder, alcohol use disorder, or opioid use disorder. They can be used to help control drug cravings, relieve symptoms of withdrawal, and to help prevent relapses.
Current medications include:
- Nicotine use disorder : A nicotine replacement product (available as patches, gum, lozenges, or nasal spray) or an oral medication, such Wellbutrin (bupropion) and Zyban (varenicline)
- Alcohol use disorder : Campral (acamprosate), Antabuse (disulfiram), and ReVia and Vivitrol (naltrexone).
- Opioid use disorder : Dolophine and Methados (methadone), buprenorphine, ReVia and Vivitrol (naltrexone), and Lucemyra (lofexidine).
Lofexidine was the first medication approved by the Food and Drug Administration (FDA) to treat opioid withdrawals. Compared to a placebo (a pill with no therapeutic value), it significantly reduces symptoms of withdrawal and may cause less of a drop in blood pressure than similar agents.
Support Groups
Support groups or self-help groups can be part of in-patient programs or available for free use in the community. Well-known support groups include narcotics anonymous (NA), alcoholics anonymous (AA), and SMART Recovery (Self-Management and Recovery Training).
Roughly half of all adults being treated for substance use disorders in the United States participated in self-help groups in 2017.
Online Support Group Options
Since the COVID-19 pandemic, these groups that were often out of reach to many are now available online around the clock through video meetings. Such groups are not considered part of a formal treatment plan, but they are considered as useful in conjunction with professional treatment.
Other Options
Due to the complex nature of any substance use disorder, other options for treatment should also include evaluation and treatment for co-occurring mental health issues such as depression and anxiety (known as dual diagnosis).
Follow-up care or continuing care is also recommended, which includes ongoing community- or family-based recovery support systems.
Substance Use Helpline
If you or a loved one are struggling with substance use or addiction, contact the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 800-662-4357 for information on support and treatment facilities in your area.
For more mental health resources, see our National Helpline Database .
Steps for Overcoming Drug Addiction
Bear in mind that stopping taking drugs is only one part of recovery from addiction. Strategies that help people stay in treatment and follow their recovery plan are essential. Along with medical and mental health treatments, the following are steps you can take to help overcome substance use disorder.
Commit to Change
Committing to change includes stages of precontemplation and contemplation where a person considers changing, cutting down, moderating, or quitting the addictive behavior. Afterward, committing to change can look like working with a professional in identifying specific goals, coming up with a specific plan to create change, following through with that plan, and revising goals as necessary.
Surround Yourself With Support
Enlisting positive support can help hold you accountable to goals. SAMHSA explains that family and friends who are supportive of recovery can help someone change because they can reinforce new behaviors and provide positive incentives to continue with treatment.
Eliminate Triggers
Triggers can be any person, place, or thing that sparks the craving for using. Common triggers include places you've done drugs, friends you've used with, and anything else that brings up memories of your drug use.
You may not be able to eliminate every trigger, but in the early stages of recovery it's best to avoid triggers to help prevent cravings and relapse .
Find Healthier Ways to Cope With Stress
Stress is a known risk factor or trigger for drug use. Managing stress in healthy ways means finding new ways of coping that don’t involve drug use.
Tips to Cope With Stress
Coping with stress includes:
- Putting more focus on taking care of yourself (eating a balanced diet, getting adequate sleep, and exercising)
- Concentrating on one challenge at a time to avoid becoming overwhelmed
- Stepping away from triggering scenarios
- Learning to recognize and communicate emotions
Learn More: Strategies for Stress Relief
Cope With Withdrawal
Coping with withdrawal may require hospitalization or inpatient care to ensure adequate supervision and medical intervention as necessary. This isn’t always the case, though, because different drugs have different withdrawal symptoms. The severity of use also plays a role, so knowing what to expect—and when to seek emergency help—is important.
For example, a person withdrawing from alcohol can experience tremors (involuntary rhythmic shaking), dehydration, and increased heart rate and blood pressure. On the more extreme end, they can experience seizures (sudden involuntary electrical disturbance in the brain), hallucinations (seeing, hearing, smelling, or tasting things that do not actually exist outside the mind), and delirium (confusion and reduced awareness of one's environment).
Withdrawing from drugs should be done under the guidance of a medical professional to ensure safety.
Deal With Cravings
Learning to deal with cravings is a skill that takes practice. While there are several approaches to resisting cravings, the SMART recovery programs suggest the DEADS method:
- D elay use because urges disappear over time.
- E scape triggering situations.
- A ccept that these feelings are normal and will pass.
- D ispute your irrational “need” for the drug.
- S ubstitute or find new ways of coping instead of using.
Avoid Relapse
The relapse rate for substance use disorders is similar to other illnesses and estimated to be between 40%–60%. The most effective way to avoid relapse and to cope with relapse is to stick with treatment for an adequate amount of time (no less than 90 days). Longer treatment is associated with more positive outcomes. Still, relapse can happen and should be addressed by revising the treatment plan as needed with medical and mental health professionals.
An intervention is an organized effort to intervene in a person's addiction by discussing how their drinking, drug use, or addiction-related behavior has affected everyone around them.
How Does an Intervention Work?
An intervention includes trained professionals like a drug and alcohol counselor, therapist, and/or interventionist who can help guide a family through the preparation and execution. It occurs in a controlled setting (not in the person’s home or family home). Intervention works by confronting the specific issues and encouraging the person to seek treatment.
Who Should Be Included at an Intervention?
Depending on the situation, interventions can include the following people:
- The person with the substance use disorder
- Friends and family
- A therapist
- A professional interventionist
The Association of Intervention Specialists (AIS) , Family First Interventions , and the Network of Independent Interventionists are three organizations of professional interventionists.
You may also want to consider if anyone in the list of friends and family should not be included. Examples are if a person is dealing with their own addiction and may not be able to maintain sobriety, is overly self-motivated or self-involved, or has a strained relationship with the person the intervention is for.
What Should Be Said During an Intervention?
While a person is free to say anything they want during an intervention, it’s best to be prepared with a plan to keep things positive and on track. Blaming, accusing, causing guilt, threatening, or arguing isn’t helpful.
Whatever is said during an intervention should be done so with the intention of helping the person accept help.
Bear in mind that setting boundaries such as “I can no longer give you money if you continue to use drugs,” is not the same as threatening a person with punishment.
Overcoming drug addiction is a process that requires time, patience, and empathy. A person will want to consider actions they can take such as committing to change, seeking support, and eliminating triggers. Depending on the addiction, medications may also be available to help.
Loved ones who are concerned about a person’s drug or alcohol use may consider an intervention . Interventions are meant to encourage treatment. Ongoing support and follow-up care are important in the recovery process to prevent relapse.
A Word From Verywell
No one grows up dreaming of becoming addicted to a substance. If someone you love is experiencing a substance use disorder, please bear in mind that they have a chronic illness and need support and help. Learning about addiction and how not to enable a person is one way you can help them. Having the ongoing support of loved ones and access to professionals can make all the difference.
Helping someone overcome drug addiction requires educating yourself on the drug and on substance use disorder, not enabling the person's use, avoiding having unrealistic expectations of their immediate recovery and change, practicing patience and empathy, and encouraging the person to seek and stick with professional treatment.
Common signs of drug addiction include:
- Drug-seeking behaviors
- Drug cravings
- Using drugs despite the negative consequences
- Being unable to cut back or stop using
Overcoming drug addiction is a complex process that can occur at different paces for different people. There are 30-, 60-, and 90-day treatment programs, but even afterwards a person can benefit from follow-up care or continued care in the form of support groups or personalized therapy. These can get at the root of what was causing the person to start using.
American Psychological Association. What is addiction? .
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health .
Manning V, Garfield JBB, Staiger PK, et al. Effect of cognitive bias modification on early relapse among adults undergoing inpatient alcohol withdrawal treatment: a randomized clinical trial . JAMA Psychiatry . 2020 ;78(2):133-140. doi:10.1001/jamapsychiatry.2020.3446
National Institute on Drug Abuse. Principles of drug addiction treatment: A research-based guide; Cognitive behavioral therapy .
McHugh RK, Hearon BA, Otto MW. Cognitive-behavioral therapy for substance use disorders . Psychiatr Clin North Am . 2010;33(3):511-525. doi:10.1016%2Fj.psc.2010.04.012
National Institute on Drug Abuse. Principles of effective treatment.
Fishman M, Tirado C, Alam D, Gullo K, Clinch T, Gorodetzky CW. Safety and efficacy of lofexidine for medically managed opioid withdrawal: a randomized controlled clinical trial . Journal of Addiction Medicine . 2019;13(3):169-176. doi:10.1097/ADM.0000000000000474
Center for Behavioral Health Statistics and Quality. Results from the 2017 National Survey on Drug Use and Health: detailed tables . Rockville, MD: Substance Abuse and Mental Health Services Administration (SAMHSA).
Wen H, Druss BG, Saloner B. Self-help groups and medication use in opioid addiction treatment: A national analysis . Health Aff (Millwood) . May;39(5):740-746. doi:10.1377/hlthaff.2019.01021
National Institute on Drug Abuse. Treatment approaches for addiction .
Lassiter PS, Culbreth JR. Theory and Practice of Addiction Counseling . SAGE Publications; 2017.
SAMHSA. Enhancing motivation for change in substance use disorder treatment .
Mental Health America. How can I stop using drugs? .
NIDA and Scholastic. Stress and drug abuse .
Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings . 4, Withdrawal Management. Geneva:World Health Organization; 2009.
SMART Recovery. 5 ways to deal with urges and cravings .
National Institute on Drug Abuse. Treatment and recovery .
National Institute on Drug Abuse. How long does drug addiction treatment usually last? .
Association of Intervention Specialists. Intervention-A starting point for change .
Cornerstone of Recovery. Things not to do during an intervention for a drug addict or an alcoholic.
By Michelle Pugle Pulge is a freelance health writer focused on mental health content. She is certified in mental health first aid.
A monthly newsletter from the National Institutes of Health, part of the U.S. Department of Health and Human Services
Search form
Print this issue
Dealing with Drug Problems
Preventing and Treating Drug Abuse

Drug abuse can be a painful experience—for the person who has the problem, and for family and friends who may feel helpless in the face of the disease. But there are things you can do if you know or suspect that someone close to you has a drug problem.
Certain drugs can change the structure and inner workings of the brain. With repeated use, they affect a person’s self-control and interfere with the ability to resist the urge to take the drug. Not being able to stop taking a drug even though you know it’s harmful is the hallmark of addiction.
A drug doesn’t have to be illegal to cause this effect. People can become addicted to alcohol, nicotine, or even prescription drugs when they use them in ways other than prescribed or use someone else’s prescription.
People are particularly vulnerable to using drugs when going through major life transitions. For adults, this might mean during a divorce or after losing a job. For children and teens, this can mean changing schools or other major upheavals in their lives.
But kids may experiment with drug use for many different reasons. “It could be a greater availability of drugs in a school with older students, or it could be that social activities are changing, or that they are trying to deal with stress,” says Dr. Bethany Deeds, an NIH expert on drug abuse prevention. Parents may need to pay more attention to their children during these periods.
The teenage years are a critical time to prevent drug use. Trying drugs as a teenager increases your chance of developing substance use disorders. The earlier the age of first use, the higher the risk of later addiction. But addiction also happens to adults. Adults are at increased risk of addiction when they encounter prescription pain-relieving drugs after a surgery or because of a chronic pain problem. People with a history of addiction should be particularly careful with opioid pain relievers and make sure to tell their doctors about past drug use.
There are many signs that may indicate a loved one is having a problem with drugs. They might lose interest in things that they used to enjoy or start to isolate themselves. Teens’ grades may drop. They may start skipping classes.
“They may violate curfew or appear irritable, sedated, or disheveled,” says child psychiatrist Dr. Geetha Subramaniam, an NIH expert on substance use. Parents may also come across drug paraphernalia, such as water pipes or needles, or notice a strange smell.
“Once drug use progresses, it becomes less of a social thing and more of a compulsive thing—which means the person spends a lot of time using drugs,” Subramaniam says.
If a loved one is using drugs, encourage them to talk to their primary care doctor. It can be easier to have this conversation with a doctor than a family member. Not all drug treatment requires long stays in residential treatment centers. For someone in the early stages of a substance use problem, a conversation with a doctor or another professional may be enough to get them the help they need. Doctors can help the person think about their drug use, understand the risk for addiction, and come up with a plan for change.
Substance use disorder can often be treated on an outpatient basis. But that doesn’t mean it’s easy to treat. Substance use disorder is a complicated disease. Drugs can cause changes in the brain that make it extremely difficult to quit without medical help.
For certain substances, it can be dangerous to stop the drug without medical intervention. Some people may need to be in a hospital for a short time for detoxification, when the drug leaves their body. This can help keep them as safe and comfortable as possible. Patients should talk with their doctors about medications that treat addiction to alcohol or opioids, such as heroin and prescription pain relievers.
Recovering from a substance use disorder requires retraining the brain. A person who’s been addicted to drugs will have to relearn all sorts of things, from what to do when they’re bored to who to hang out with. NIH has developed a customizable wallet card to help people identify and learn to avoid their triggers, the things that make them feel like using drugs. You can order the card for free at drugpubs.drugabuse.gov/publications/drugs-brain-wallet-card .
“You have to learn ways to deal with triggers, learn about negative peers, learn about relapse, [and] learn coping skills,” Subramaniam says.
NIH-funded scientists are studying ways to stop addiction long before it starts—in childhood. Dr. Daniel Shaw at the University of Pittsburgh is looking at whether teaching healthy caregiving strategies to parents can help promote self-regulation skills in children and prevent substance abuse later on.
Starting when children are two years old, Shaw’s study enrolls families at risk of substance use problems in a program called the Family Check-Up. It’s one of several parenting programs that have been studied by NIH-funded researchers.
During the program, a parenting consultant visits the home to observe the parents’ relationship with their child. Parents complete several questionnaires about their own and their family’s well-being. This includes any behavior problems they are experiencing with their child. Parents learn which of their children’s problem behaviors might lead to more serious issues, such as substance abuse, down the road. The consultant also talks with the parents about possible ways to change how they interact with their child. Many parents then meet with the consultants for follow-up sessions about how to improve their parenting skills.
Children whose parents are in the program have fewer behavioral problems and do better when they get to school. Shaw and his colleagues are now following these children through their teenage years to see how the program affects their chances of developing a substance abuse problem. You can find video clips explaining different ways parents can respond to their teens on the NIH Family Checkup website at www.drugabuse.gov/family-checkup .
Even if their teen has already started using drugs, parents can still step in. They can keep closer tabs on who their children’s friends are and what they’re doing. Parents can also help by finding new activities that will introduce their children to new friends and fill up the after-school hours—prime time for getting into trouble. “They don’t like it at first,” Shaw says. But finding other teens with similar interests can help teens form new habits and put them on a healthier path.
A substance use problem is a chronic disease that requires lifestyle adjustments and long-term treatment, like diabetes or high blood pressure. Even relapse can be a normal part of the process—not a sign of failure, but a sign that the treatment needs to be adjusted. With good care, people who have substance use disorders can live healthy, productive lives.
Related Stories

How Many Is Too Many?

Drug Allergies

Opioid Facts for Parents

How Much Alcohol Is Too Much?
NIH Office of Communications and Public Liaison Building 31, Room 5B52 Bethesda, MD 20892-2094 [email protected] Tel: 301-451-8224
Editor: Harrison Wein, Ph.D. Managing Editor: Tianna Hicklin, Ph.D. Illustrator: Alan Defibaugh
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov .
For wellness toolkits, visit www.nih.gov/wellnesstoolkits .
Drugs, Brains, and Behavior: The Science of Addiction Treatment and Recovery
Can addiction be treated successfully.
Yes, addiction is a treatable disorder. Research on the science of addiction and the treatment of substance use disorders has led to the development of research-based methods that help people to stop using drugs and resume productive lives, also known as being in recovery.
Can addiction be cured?
Like treatment for other chronic diseases such as heart disease or asthma, addiction treatment is not a cure, but a way of managing the condition. Treatment enables people to counteract addiction's disruptive effects on their brain and behavior and regain control of their lives.
Does relapse to drug use mean treatment has failed?
No. The chronic nature of addiction means that for some people relapse, or a return to drug use after an attempt to stop, can be part of the process, but newer treatments are designed to help with relapse prevention. Relapse rates for drug use are similar to rates for other chronic medical illnesses. If people stop following their medical treatment plan, they are likely to relapse.
Treatment of chronic diseases involves changing deeply rooted behaviors, and relapse doesn’t mean treatment has failed. When a person recovering from an addiction relapses, it indicates that the person needs to speak with their doctor to resume treatment, modify it, or try another treatment. 52
While relapse is a normal part of recovery, for some drugs, it can be very dangerous—even deadly. If a person uses as much of the drug as they did before quitting, they can easily overdose because their bodies are no longer adapted to their previous level of drug exposure. An overdose happens when the person uses enough of a drug to produce uncomfortable feelings, life-threatening symptoms, or death.
What are the principles of effective treatment?
Research shows that when treating addictions to opioids (prescription pain relievers or drugs like heroin or fentanyl), medication should be the first line of treatment, usually combined with some form of behavioral therapy or counseling. Medications are also available to help treat addiction to alcohol and nicotine.
Additionally, medications are used to help people detoxify from drugs, although detoxification is not the same as treatment and is not sufficient to help a person recover. Detoxification alone without subsequent treatment generally leads to resumption of drug use.
For people with addictions to drugs like stimulants or cannabis, no medications are currently available to assist in treatment, so treatment consists of behavioral therapies. Treatment should be tailored to address each patient's drug use patterns and drug-related medical, mental, and social problems.
What medications and devices help treat drug addiction?
Different types of medications may be useful at different stages of treatment to help a patient stop abusing drugs, stay in treatment, and avoid relapse.
- Treating withdrawal. When patients first stop using drugs, they can experience various physical and emotional symptoms, including restlessness or sleeplessness, as well as depression, anxiety, and other mental health conditions. Certain treatment medications and devices reduce these symptoms, which makes it easier to stop the drug use.
- Staying in treatment. Some treatment medications and mobile applications are used to help the brain adapt gradually to the absence of the drug. These treatments act slowly to help prevent drug cravings and have a calming effect on body systems. They can help patients focus on counseling and other psychotherapies related to their drug treatment.
- Preventing relapse. Science has taught us that stress cues linked to the drug use (such as people, places, things, and moods), and contact with drugs are the most common triggers for relapse. Scientists have been developing therapies to interfere with these triggers to help patients stay in recovery.
Common medications used to treat drug addiction and withdrawal
- Buprenorphine
- Extended-release naltrexone
- Nicotine replacement therapies (available as a patch, inhaler, or gum)
- Varenicline
- Acamprosate
How do behavioral therapies treat drug addiction?
Behavioral therapies help people in drug addiction treatment modify their attitudes and behaviors related to drug use. As a result, patients are able to handle stressful situations and various triggers that might cause another relapse. Behavioral therapies can also enhance the effectiveness of medications and help people remain in treatment longer.
- Cognitive-behavioral therapy seeks to help patients recognize, avoid, and cope with the situations in which they're most likely to use drugs.
- Contingency management uses positive reinforcement such as providing rewards or privileges for remaining drugfree, for attending and participating in counseling sessions, or for taking treatment medications as prescribed.
- Motivational enhancement therapy uses strategies to make the most of people's readiness to change their behavior and enter treatment.
- Family therapy helps people (especially young people) with drug use problems, as well as their families, address influences on drug use patterns and improve overall family functioning.
- Twelve-step facilitation (TSF) is an individual therapy typically delivered in 12 weekly session to prepare people to become engaged in 12-step mutual support programs. 12-step programs, like Alcoholic Anonymous, are not medical treatments, but provide social and complementary support to those treatments. TSF follows the 12-step themes of acceptance, surrender, and active involvement in recovery.
How do the best treatment programs help patients recover from addiction?

Stopping drug use is just one part of a long and complex recovery process. When people enter treatment, addiction has often caused serious consequences in their lives, possibly disrupting their health and how they function in their family lives, at work, and in the community.
Because addiction can affect so many aspects of a person's life, treatment should address the needs of the whole person to be successful. Counselors may select from a menu of services that meet the specific medical, mental, social, occupational, family, and legal needs of their patients to help in their recovery.
For more information on drug treatment , see Principles of Drug Addiction Treatment: A Research-Based Guide , and Principles of Adolescent Substance Use Disorder Treatment: A Research-Based Guide .
How do we tackle the opioid crisis?
Subscribe to the economic studies bulletin, christen linke young and christen linke young deputy assistant to the president for health and veterans affairs - domestic policy council for health and veterans, former fellow - usc-brookings schaeffer initiative for health policy @clinkeyoung abigail durak abigail durak former center coordinator - center for health policy, brookings.
October 18, 2019
Opioids are a class of drugs that affect the brain, including by relieving pain, and they are extremely addictive. Policymakers can combat the opioid epidemic by:
- limiting inappropriate use of prescription opioids;
- reducing the flow of illicit opioids (like heroin);
- helping people seek treatment for opioid misuse; and
- deploying harm reduction tools that blunt the risks of death, illness, or injury.
These strategies are reflected in ongoing work at the federal, state, and local levels.
A Closer Look
Opioids include prescription drugs like oxycodone as well as illicit drugs like heroin. These drugs are extremely addictive. While opioids have existed for hundreds of years, health care providers generally limited their use because of concerns about addiction. However, beginning in the 1990s, a constellation of factors led to increased use of prescription opioids, including growing attention to pain management as an important clinical goal and the manufacture and marketing of a new generation of prescription opioids. The rise in prescriptions was also associated with increased availability of illegal opioids like heroin.
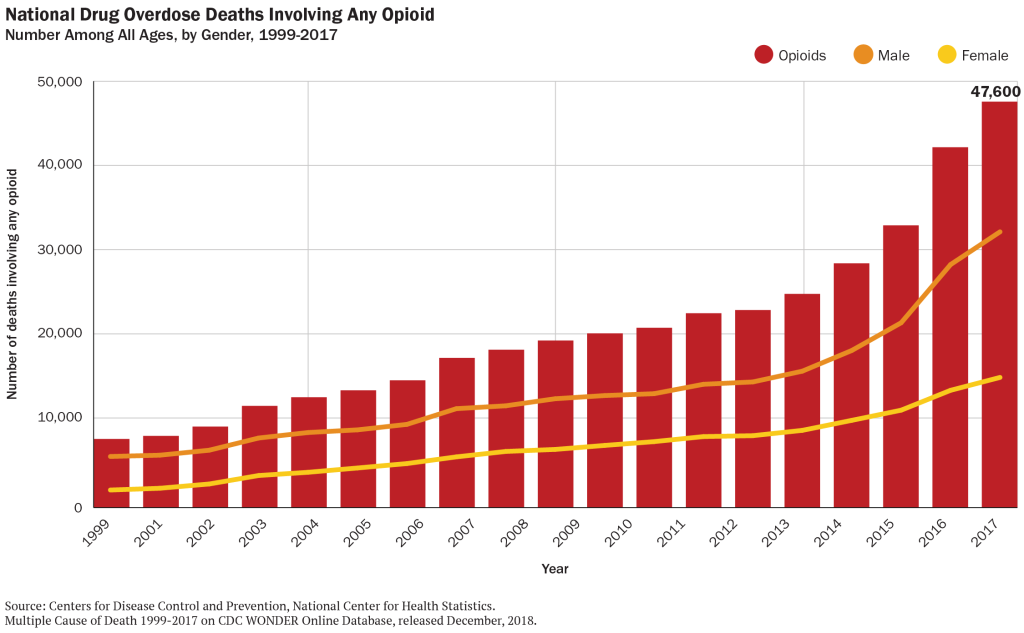
We have seen a dramatic rise in illness and death associated with improper use of opioids. According to federal data:
- 12 million people reported misuse of opioids in 2016.
- Estimates suggest that 2.1 million people struggled with opioid use disorder in 2017.
- Doctors wrote 59 opioid prescriptions per 100 residents in 2017, down from a peak of about 81 per 100 residents in 2010.
- There were 140,000 visits to an emergency room because of an opioid overdose in 2015.
- About 48,000 people died from an opioid overdose in 2017, or about 130 people per day.
For context, the number of deaths from opioid overdose in 2017 is comparable to the number of deaths from HIV-related causes at the height of that epidemic in the 1990s, and is nearly 8 times larger than the number of HIV deaths today.
What can policymakers do to combat the opioid epidemic?
Addressing a public health crisis of this magnitude is a complex undertaking. Policymakers can work to prevent people from becoming addicted to opioids and to help people who are already misusing opioids to treat their addiction and minimize the risk of death or other harm. In general, there are four kinds of strategies:
Limiting prescription opioids
For the last 15 years, physicians have been prescribing opioids at high rates. In a handful of states, there is more than one opioid prescription per person each year. Some overprescribing is the result of “pill mills”—unethical providers who write prescriptions with indifference to clinical need. Other times, patients may be visiting multiple prescribers to seek prescription opioids. And in still other cases, providers may be using prescription opioids to combat pain when other treatments, smaller quantities, or less potent drugs may suffice.
The overuse of prescription opioids fuels the epidemic in two ways. First, it introduces patients (even when taking these drugs as prescribed) to an addictive substance, which creates the risk of subsequently developing opioid use disorder. Second, it creates a flow of opioids that can be diverted from their intended purpose.
Therefore, policymakers can take actions that reduce opportunities for misuse of prescription opioids. These include:
- Prescription Drug Monitoring Programs (PDMPs). 49 states and the District of Columbia have established a PDMP, a statewide database that shows every opioid prescription. Health care providers can check (or be required to check) this database before writing a prescription, allowing them to see if the patient has received opioids from other doctors.
- Prescriber limits. In 2016 the federal government released guidelines for prescribing opioids for chronic pain outside of active cancer treatment, palliative care, and end-of-life care. Consistent with these guidelines, many states have made it unlawful for providers in many circumstances to write opioid prescriptions that exceed a particular strength or that span longer than a few days or weeks.
- Law enforcement. Cracking down on “pill mills” and other unethical and illegal overprescribing behavior by health care providers can have a major impact on the volume of prescription opioids.
- Stakeholder education. Provider education can emphasize the appropriate and limited role of opioids. Similarly, insurance companies can be encouraged to cover non-drug pain therapies and to monitor their own data for early warning signs of opioid misuse or prescriber misconduct.
All of these strategies must balance opioids’ valuable benefits in pain control against the risk of misuse. Policymakers should always be cognizant of the possibility that they could enact too many or the wrong kinds of restrictions and leave patients unnecessarily struggling with unmanaged pain.
Reducing the flow of illicit opioids
Many opioid deaths are associated with illicit opioids like heroin and illegally produced fentanyl. (Fentanyl, in particular, is an extremely potent and deadly opioid, and its use is on the rise .) Although there are no simple solutions, many communities have invested in funding for law enforcement efforts that target large scale opioid distribution.
Collaborative efforts that work across borders and jurisdictions are necessary to share up-to-date information. The federal government has helped facilitate intelligence sharing across agencies, which can help federal, state, and local law enforcement identify and respond to emerging trends. Federal law enforcement agencies have also brought cases against major drug trafficking organizations using this shared information.
In addition, communication among law enforcement, public health professionals, and first responders about distribution patterns can help target public health efforts.
Promoting treatment
A variety of treatment options exist to help people already suffering from opioid use disorder. Experts believe that the most effective treatment for many people will be “medication assisted treatment,” or MAT. MAT involves taking one or more drugs that are intended prevent opioid misuse. These drugs can reduce cravings for opioid misuse or prevent opioids from causing a “high.” (Some of the drugs involved in MAT are themselves opioids.) MAT also involves structured counseling and other support.
Only 17.5 % of people who could benefit from specialized treatment for prescription opioid use disorder received it in 2016. Obstacles to treatment include lack of insurance coverage for treatment, difficulty finding a provider, and patients’ unwillingness to begin treatment. Strategies to promote treatment include:
- Medicaid expansion. In states that have expanded Medicaid under the Affordable Care Act , any low-income individual can enroll in Medicaid, where they will have coverage for a wide variety of opioid treatment options. Many studies have linked Medicaid expansion to improved take-up of MAT therapies. Therefore, in states that have not yet expanded, Medicaid expansion can help many people access treatment.
- Payments for opioid treatment. Policymakers can also provide funding for opioid treatment for people who are uninsured or underinsured. This can include supporting treatment directly (like paying for MAT therapies) or subsidizing services like housing support that can make treatment more successful.
- Expanding treatment capacity. Communities can invest in training providers to treat opioid use disorder or supporting the development of new treatment facilities or modalities . Policymakers may also wish to consider updates to policies about how physicians can become certified to prescribe MAT.
- Peer support. There are many successful models of peer support interventions where people in treatment help encourage others with opioid use disorder initiate treatment and offer support throughout recovery. Peer supports can bridge the gap between the clinical treatment setting and everyday life.
- Treatment and the criminal justice system. The federal government has also recently released new guidance to states on MAT in the criminal justice system, suggesting that criminal justice agencies may choose to provide MAT in-house, or partner with community-based providers to deliver treatment to voluntary participants in custody. Establishing relationships with community-based providers can help ensure continuity of care once individuals have been released from incarceration.
The federal government has provided significant grants to states, and states and local communities are also investing their own resources in these kinds of treatment strategies. Policymakers may also recognize that injury and death associated with opioid use has been concentrated in communities experiencing lower rates of economic growth , which can help target treatment investments.
Reducing harm
Finally, policymakers can also focus on “harm reduction” – that is, mitigating the risk that opioid use disorder will cause illness, injury, or death. This includes:
- Naloxone. One of the most important tools is broad availability of naloxone, a drug that can immediately reverse the effects of an opioid overdose. Making naloxone widely available to first responders (including police officers) and to individuals can dramatically reduce the risk of death from overdose.
- Prisons and jails. Individuals recently released from prison are 40 times more likely than others to die of opioid overdose. Making naloxone available to individuals about to be released from incarceration can be a particularly impactful harm reduction strategy.
- Needle exchange. Opioid misuse often involves intravenous drug use, which can lead to transmission of infections like HIV and Hepatitis C. Making clean needles available can reduce the risk of these diseases, and can connect drug users with vital health care services . Needle exchange programs can also link individuals with opioid use disorder to treatment services when they are ready to seek treatment.
Carol Graham
October 15, 2019
October 25, 2018
Dayna Bowen Matthew
January 23, 2018
Economic Studies
Loren Adler, Matthew Fiedler, Richard G. Frank
May 16, 2024
Loren Adler, Matthew Fiedler
May 8, 2024
Keith Humphreys, Christina Andrews, Richard G. Frank
May 6, 2024

With the new President's Commission on Combating Drug Addiction and the Opioid Crisis, we've updated this article which first appeared in August 2016 written by Marty Harding, Director of Training and Consultation, Hazelden Betty Ford Foundation
These are difficult times for many communities. Budgets are being cut; resources are dwindling. Law enforcement personnel, county officials, social services agencies, and healthcare providers are struggling to do more with less. At the same time, the opioid epidemic is devastating families and communities throughout America.
(Editor's Note) With 91 Americans dying each day from opioid overdoses, the Centers for Disease Control and Prevention have characterized it as an epidemic.
For the past year, I’ve had the opportunity to work in six states to mobilize communities to address this epidemic: Massachusetts, Minnesota, Wisconsin, Kentucky, Florida, and Arkansas. In each state, people from every community sector have shared devastating stories of how they have been affected by opioid use. People who work in emergency rooms of their local hospitals are seeing a flood of overdose patients (from young teens to older adults), and first responders tell of the role they are now playing in saving lives by administering Narcan.
Law enforcement officers talk about their struggle to crack down on dealers and distribution networks. Employers are worried about lost productivity in the workplace due to opioid use. Faith leaders are overwhelmed by the number of deaths in their congregations. Community leaders are concerned about public safety. Educators ask if they’re doing enough to prevent opioid use among adolescents and how to intervene. And probably the most heartbreaking of all the stories are those told by parents who have lost a child to an opioid overdose.
As a local government administrator, you’ve seen and heard it all. Opioid use affects all of the departments you administer: public safety, facility management, transportation, fire and emergency services, and community and economic development. People turn to you for guidance about public policy.
Fortunately, communities are finding solutions to these concerns and working together across sectors to prevent opioid use, intervene, and provide resources for those who are affected by opioid use. This is a critical time for cities and counties to mobilize and provide their communities with vital information and tools to combat heroin and prescription painkiller abuse with the goal of minimizing its social and economic impact.
There is hope! Communities can successfully mobilize and take action.
On August 31, 2016, ICMA conducted a webinar on solutions that cities and counties are implementing to respond to the opioid epidemic. Lee Feldman, 2016-2017 ICMA president, and city manager, Fort Lauderdale, Florida, joined me for this webinar, and we explored these ideas that counties and cities have explored:
- Creating community coalitions to work together across sectors. Managers have joined or started community coalitions that focus directly on the opioid crisis. They have recruited members from such diverse sectors of the community as employers, youth workers, faith community leaders, school administrators, teachers and counselors, public health and human services personnel, treatment professionals, law enforcement and county court services personnel, local pharmacists, and doctors, as well as other committed individuals, including people from the recovering community. These coalitions have joined forces and disseminated relevant information, conducted visioning sessions, developed and implemented action plans, and conducted educational sessions and informational campaigns throughout their communities.
- Developing ordinances and places for safe drug disposal. Generally, these safe disposal sites are located in city halls under the supervision of law enforcement. Although drug take-back days are effective in increasing public awareness of the problem of unwanted prescriptions, a consistent, 24-7 lockbox for safe drug disposal dramatically increases the pounds of unwanted prescriptions that are collected, keeping them out of the hands of children and out of our water and landfills.
- Establishing drug diversion task forces. Dedicated to sharing information and investigations to combat prescription fraud and illegal trafficking of prescription painkillers.
- Providing training for first responders in the use of naloxone (Narcan) for reducing opioid overdoses. This strategy has been successfully implemented in many communities throughout the country, saving countless lives. New intranasal Narcan makes administration easier for both law enforcement and emergency personnel. Stigma about using Narcan still abounds, however, and city/county administrators must be armed with a strong rationale for counteracting negativity toward this approach.
- Using drug courts to fight opioid addiction and trafficking. This approach reduces recidivism, encourages compliance with treatment, and supports families of drug court participants. It also reduces some of the burdens on jails by creating an effective diversion program.
- Creating referral programs through law enforcement agencies. Some communities are trying innovative programs that allow people to voluntarily obtain help by going to the local sheriff’s office and requesting assistance. The community, county, or individual donors often cover the cost of treatment in these instances.
- Disseminating information about state laws that encourage intervention. Good Samaritan laws protect citizens when they intervene to save a life due to an opioid overdose. Drug overdose amnesty laws allow people to call 911 when a friend or family member is overdosing without fear of being arrested themselves for opioid use or possession.
- Building awareness about their state’s prescription drug monitoring program (PDMP). These efforts are critical to cutting down on “doctor shopping” and preventing opioid overdoses, but they are underused for a variety of reasons. Cities and counties are involving local doctors and pharmacies to build awareness of PDMPs and remove barriers to implementing them fully.
- Hosting community mobilization events to put tools into the hands of every community sector. Community mobilization events, using Hazelden’s “Toolkit for Community Action,” have reached more than a 1,000 people in the past six months. We’ll share what we’ve learned from these events, and let you know how you can plan and launch an event in your community.
Mobilizing your community doesn’t happen overnight, and it requires hard work. But the return on your investment of time, money, and effort is worth it. Imagine…. If hospital admissions for overdose death decrease. If law enforcement costs are reduced. If employers in your community see a rise in productivity. If violence, theft, and other crimes in your community decrease. If schools are a safer place for your children. If one life is saved. It’s worth it.
Related Resources:
- Podcast: Episode 5--The Opioid Epidemic
- Article: How One City Went "All-In" to Fight the Opioid Epidemic
- Article: Leading the Fight Against the Opioid Crisis
- Article: The Opioid Mission of Broome County, New York
- Blog Post: Virginia Launches New Tool to Combat Heroin, Prescription Opioid Abuse
New, Reduced Membership Dues
A new, reduced dues rate is available for CAOs/ACAOs, along with additional discounts for those in smaller communities, has been implemented. Learn more and be sure to join or renew today!
Appointments at Mayo Clinic
- Tween and teen health
Teen drug abuse: Help your teen avoid drugs
Teen drug abuse can have a major impact on your child's life. Find out how to help your teen make healthy choices and avoid using drugs.
The teen brain is in the process of maturing. In general, it's more focused on rewards and taking risks than the adult brain. At the same time, teenagers push parents for greater freedom as teens begin to explore their personality.
That can be a challenging tightrope for parents.
Teens who experiment with drugs and other substances put their health and safety at risk. The teen brain is particularly vulnerable to being rewired by substances that overload the reward circuits in the brain.
Help prevent teen drug abuse by talking to your teen about the consequences of using drugs and the importance of making healthy choices.
Why teens use or misuse drugs
Many factors can feed into teen drug use and misuse. Your teen's personality, your family's interactions and your teen's comfort with peers are some factors linked to teen drug use.
Common risk factors for teen drug abuse include:
- A family history of substance abuse.
- A mental or behavioral health condition, such as depression, anxiety or attention-deficit/hyperactivity disorder (ADHD).
- Impulsive or risk-taking behavior.
- A history of traumatic events, such as seeing or being in a car accident or experiencing abuse.
- Low self-esteem or feelings of social rejection.
Teens may be more likely to try substances for the first time when hanging out in a social setting.
Alcohol and nicotine or tobacco may be some of the first, easier-to-get substances for teens. Because alcohol and nicotine or tobacco are legal for adults, these can seem safer to try even though they aren't safe for teens.
Teens generally want to fit in with peers. So if their friends use substances, your teen might feel like they need to as well. Teens also may also use substances to feel more confident with peers.
If those friends are older, teens can find themselves in situations that are riskier than they're used to. For example, they may not have adults present or younger teens may be relying on peers for transportation.
And if they are lonely or dealing with stress, teens may use substances to distract from these feelings.
Also, teens may try substances because they are curious. They may try a substance as a way to rebel or challenge family rules.
Some teens may feel like nothing bad could happen to them, and may not be able to understand the consequences of their actions.
Consequences of teen drug abuse
Negative consequences of teen drug abuse might include:
- Drug dependence. Some teens who misuse drugs are at increased risk of substance use disorder.
- Poor judgment. Teenage drug use is associated with poor judgment in social and personal interactions.
- Sexual activity. Drug use is associated with high-risk sexual activity, unsafe sex and unplanned pregnancy.
- Mental health disorders. Drug use can complicate or increase the risk of mental health disorders, such as depression and anxiety.
- Impaired driving. Driving under the influence of any drug affects driving skills. It puts the driver, passengers and others on the road at risk.
- Changes in school performance. Substance use can result in worse grades, attendance or experience in school.
Health effects of drugs
Substances that teens may use include those that are legal for adults, such as alcohol or tobacco. They may also use medicines prescribed to other people, such as opioids.
Or teens may order substances online that promise to help in sports competition, or promote weight loss.
In some cases products common in homes and that have certain chemicals are inhaled for intoxication. And teens may also use illicit drugs such as cocaine or methamphetamine.
Drug use can result in drug addiction, serious impairment, illness and death. Health risks of commonly used drugs include the following:
- Cocaine. Risk of heart attack, stroke and seizures.
- Ecstasy. Risk of liver failure and heart failure.
- Inhalants. Risk of damage to the heart, lungs, liver and kidneys from long-term use.
- Marijuana. Risk of impairment in memory, learning, problem-solving and concentration; risk of psychosis, such as schizophrenia, hallucination or paranoia, later in life associated with early and frequent use. For teens who use marijuana and have a psychiatric disorder, there is a risk of depression and a higher risk of suicide.
- Methamphetamine. Risk of psychotic behaviors from long-term use or high doses.
- Opioids. Risk of respiratory distress or death from overdose.
- Electronic cigarettes (vaping). Higher risk of smoking or marijuana use. Exposure to harmful substances similar to cigarette smoking; risk of nicotine dependence. Vaping may allow particles deep into the lungs, or flavorings may include damaging chemicals or heavy metals.
Talking about teen drug use
You'll likely have many talks with your teen about drug and alcohol use. If you are starting a conversation about substance use, choose a place where you and your teen are both comfortable. And choose a time when you're unlikely to be interrupted. That means you both will need to set aside phones.
It's also important to know when not to have a conversation.
When parents are angry or when teens are frustrated, it's best to delay the talk. If you aren't prepared to answer questions, parents might let teens know that you'll talk about the topic at a later time.
And if a teen is intoxicated, wait until the teen is sober.
To talk to your teen about drugs:
- Ask your teen's views. Avoid lectures. Instead, listen to your teen's opinions and questions about drugs. Parents can assure teens that they can be honest and have a discussion without getting in trouble.
- Discuss reasons not to use drugs. Avoid scare tactics. Emphasize how drug use can affect the things that are important to your teen. Some examples might be sports performance, driving, health or appearance.
- Consider media messages. Social media, television programs, movies and songs can make drug use seem normal or glamorous. Talk about what your teen sees and hears.
- Discuss ways to resist peer pressure. Brainstorm with your teen about how to turn down offers of drugs.
- Be ready to discuss your own drug use. Think about how you'll respond if your teen asks about your own drug use, including alcohol. If you chose not to use drugs, explain why. If you did use drugs, share what the experience taught you.
Other preventive strategies
Consider other strategies to prevent teen drug abuse:
- Know your teen's activities. Pay attention to your teen's whereabouts. Find out what adult-supervised activities your teen is interested in and encourage your teen to get involved.
- Establish rules and consequences. Explain your family rules, such as leaving a party where drug use occurs and not riding in a car with a driver who's been using drugs. Work with your teen to figure out a plan to get home safely if the person who drove is using substances. If your teen breaks the rules, consistently enforce consequences.
- Know your teen's friends. If your teen's friends use drugs, your teen might feel pressure to experiment, too.
- Keep track of prescription drugs. Take an inventory of all prescription and over-the-counter medications in your home.
- Provide support. Offer praise and encouragement when your teen succeeds. A strong bond between you and your teen might help prevent your teen from using drugs.
- Set a good example. If you drink, do so in moderation. Use prescription drugs as directed. Don't use illicit drugs.
Recognizing the warning signs of teen drug abuse
Be aware of possible red flags, such as:
- Sudden or extreme change in friends, eating habits, sleeping patterns, physical appearance, requests for money, coordination or school performance.
- Irresponsible behavior, poor judgment and general lack of interest.
- Breaking rules or withdrawing from the family.
- The presence of medicine containers, despite a lack of illness, or drug paraphernalia in your teen's room.
Seeking help for teen drug abuse
If you suspect or know that your teen is experimenting with or misusing drugs:
- Plan your action. Finding out your teen is using drugs or suspecting it can bring up strong emotions. Before talking to your teen, make sure you and anyone who shares caregiving responsibility for the teen is ready. It can help to have a goal for the conversation. It can also help to figure out how you'll respond to the different ways your teen might react.
- Talk to your teen. You can never step in too early. Casual drug use can turn into too much use or addiction. This can lead to accidents, legal trouble and health problems.
- Encourage honesty. Speak calmly and express that you are coming from a place of concern. Share specific details to back up your suspicion. Verify any claims your child makes.
- Focus on the behavior, not the person. Emphasize that drug use is dangerous but that doesn't mean your teen is a bad person.
- Check in regularly. Spend more time with your teen. Know your teen's whereabouts and ask questions about the outing when your teen returns home.
- Get professional help. If you think your teen is involved in drug use, contact a health care provider or counselor for help.
It's never too soon to start talking to your teen about drug abuse. The conversations you have today can help your teen make healthy choices in the future.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Children’s health information and parenting tips to your inbox.
Sign-up to get Mayo Clinic’s trusted health content sent to your email. Receive a bonus guide on ways to manage your child’s health just for subscribing. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Our e-newsletter will keep you up-to-date on the latest health information.
Something went wrong with your subscription.
Please try again in a couple of minutes
- Dulcan MK, ed. Substance use disorders and addictions. In: Dulcan's Textbook of Child and Adolescent Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2021. https://psychiatryonline.org. Accessed Jan. 24, 2023.
- 6 parenting practices: Help reduce the chances your child will develop a drug or alcohol problem. Partnership to End Addiction. https://drugfree.org/addiction-education/. Accessed Jan. 24, 2023.
- Why do teens drink and use substances and is it normal? Partnership to End Addiction. https://drugfree.org/article/why-do-teens-drink-and-use-substances/. Accessed Jan. 24, 2023.
- Teens: Alcohol and other drugs. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/aacap/families_and_youth/facts_for_families/fff-guide/Teens-Alcohol-And-Other-Drugs-003.aspx. Accessed Dec. 27, 2018.
- Drugged driving. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/drugged-driving. Accessed Jan. 24, 2023.
- Marijuana talk kit. Partnership for Drug-Free Kids. https://drugfree.org/drugs/marijuana-what-you-need-to-know/. Accessed Jan. 24, 2023.
- Drug guide for parents: Learn the facts to keep your teen safe. Partnership for Drug-Free Kids. https://www.drugfree.org/resources/. Accessed Dec. 12, 2018.
- Vaping: What you need to know and how to talk with your kids about vaping. Partnership to End Addiction. https://drugfree.org/addiction-education/. Accessed Jan. 24, 2023.
- How to listen. Partnership for Drug-Free Kids. https://www.drugfree.org/resources/. Accessed Dec. 12, 2018.
- Drug abuse prevention starts with parents. American Academy of Pediatrics. https://publications.aap.org/patiented/article/doi/10.1542/peo_document352/81984/Drug-Abuse-Prevention-Starts-With-Parents. Accessed Jan. 24, 2023.
- How to talk to your kids about drugs if you did drugs. Partnership for Drug-Free Kids. https://www.drugfree.org/resources/. Accessed Dec. 12, 2018.
- My child tried drugs, what should I do? Partnership to End Addiction. https://drugfree.org/article/my-child-tried-drugs-what-should-i-do/. Accessed Jan. 24, 2023.
- Gage SH, et al. Association between cannabis and psychosis: Epidemiologic evidence. Biological Psychiatry. 2016;79:549.
- Quick facts on the risks of e-cigarettes for kids, teens and young adults. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/Quick-Facts-on-the-Risks-of-E-cigarettes-for-Kids-Teens-and-Young-Adults.html. Accessed Jan. 30, 2023.
- Distracted Driving
- Piercings: How to prevent complications
- Talking to your teen about sex
- Teen suicide
- Teens and social media use
- Mayo Clinic Minute: Weight loss surgery for kids
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Teen drug abuse Help your teen avoid drugs
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Australian Government Department of Health and Aged Care
How to reduce or quit drugs
Many different services are available to help you or someone you know quit drugs.
Why quit drugs?
It’s never too late to quit using drugs.
Reducing or quitting drugs can improve your life in many ways. It can:
- improve your physical and mental wellbeing
- reduce your risk of permanent damage to vital organs and death
- improve your relationships with friends and family
- help you reconnect with your emotions
- increase your energy
- help you sleep better
- improve your appearance
- save you money.
Recovered addicts say that they’ve never felt better after quitting drugs, although this can take time. Knowing why you want to quit drugs can help you to stay motivated during the withdrawal process.
What quitting drugs feels like
When you reduce or quit using drugs your body goes through a detoxification process (detox) or withdrawal.
Symptoms vary between people, and between drugs, and range from mild to serious. They can last from a few days to a few weeks — it's different for every person — but they are temporary. Cravings for the drug will sometimes be weak and at other times very strong. Learning how to manage them is important for staying drug-free.
Find out what withdrawal symptoms are for specific drugs .
Preparing to quit drugs
Reducing or quitting drugs can be hard – you may have become dependent or addicted. It’s a good idea to be prepared for what’s involved.
Admit you have a problem
The first step in quitting drugs is to admit that you have a problem. If you’re not sure, ask yourself the following questions:
- Are you taking drugs first thing in the morning or to get through the day?
- Do friends or family worry or complain about your drug use?
- Do you lie about how much you’re using?
- Have you sold possessions or stolen to pay for your drug habit?
- Have you participated in dangerous or risky activities, such as driving under the influence, having unprotected sex, or using dirty needles?
- Do you feel that you’ve lost control of your drug taking?
- Are you having problems with relationships?
If you answered yes to any of these questions it might be time to accept that you have a problem and ask for help.
See your specialist alcohol and other drugs service or local doctor
It’s important to talk to your specialist alcohol and other drugs (AOD) service or doctor about reducing or quitting drugs. They can help you get appropriate help and support.
It takes courage for someone to admit they may have a problem with drugs or alcohol. Recognising you might have an issue and asking for help is an important first step to making a change.
For free and confidential advice about alcohol and other drug treatment services, you can call the Alcohol and Other Drug hotline on 1800 250 015. It will automatically direct you to the Alcohol and Drug Information Service in your state and territory. These local alcohol and other drug telephone services offer support, information, counselling and referral to services. You can also visit a specialist alcohol and other drugs service or doctor directly.
If you’ve become addicted or dependent on drugs, it might be dangerous to quit on your own . Your AOD specialist or doctor can refer you to treatment such as detox, medication and counselling to help you manage withdrawal symptoms .
Remember, conversations with these services are private and confidential.
Know your triggers
Keeping track of your drug use can help you identify habits, emotions, and social situations that trigger the desire to take drugs.
It can be hard to completely avoid all those situations, but steps you can take include:
- avoiding places where you know drugs and alcohol will be available
- surrounding yourself with friends who don't use drugs
- knowing how to resist temptation
- learning how to cope with stress and relax without drugs
- distracting yourself with activities like exercise or listening to music.
Make a plan
Making a plan and writing it down can help you commit to quitting.
Setting goals for your recovery helps you stay motivated and can make the process less stressful. It’s important to set realistic goals – both short and long-term. Be specific and make them measurable.
Some examples of realistic, short-term goals are:
- I will see my doctor this week.
- I’m going to walk for half an hour 3 times this week.
- I want to be drug free for 2 weeks straight.
Long-term goals might include:
- being drug-free for a year
- having friends that are healthy and sober and provide support
- rebuilding family relationships by having regular get-togethers.
Reward yourself for success – with an enjoyable, drug-free activity such as going to a movie, or planning a holiday – and take it easy on yourself if you mess up.
It’s OK to fail, just don’t give up trying.
Ways to reduce or quit drugs
There is no treatment that works for everyone. Just as drugs affect each person differently, treatment needs to be individual. It’s important to find a program that works for you.
Treatment options range from counselling through to hospital care – it depends on which drugs are involved and how serious your dependence or addiction is. They include:
- going cold turkey – you stop taking drugs suddenly, with no outside help or support
- counselling and lifestyle changes – individual or group therapy can help you learn to cope without drugs. This can be successful if your drug use has been mild. Peer support groups are often run by recovered addicts – their personal experience can be helpful to others
- detoxification (detox) – you stop taking drugs and have medical treatment (known as pharmacotherapy) while your body clears the drug from your system
- rehabilitation (rehab) – this is a longer term treatment where you stay in a hospital or clinic, or at home . It also involves psychological treatment to help you deal with issues that may have contributed to your drug use
If you have mental health issues your treatment will need to address that at the same time for your overall treatment to be effective.
Support services
Quitting drugs on your own is difficult – it’s much easier with support. Tell your friends and family that you’re quitting so they can help you.
There are many support services available to help you. You can:
- call the National Alcohol and Other Drugs Hotline
- visit Counselling Online and email or chat to a counsellor
- find help and support services on the Alcohol and Drug Foundation website
- join a support group, such as Narcotics Anonymous or Alcoholics Anonymous
- find a support service in our list of contacts .
Remember, your AOD specialist or doctor can also direct you to support services that are appropriate for your needs.
What if I relapse?
If you have a relapse and start using again, remember that recovery doesn’t happen overnight. Take the opportunity to remind yourself why you are quitting, forgive yourself and refocus on your plan.
Talk to your doctor. They can work out how to best resume treatment, or they may suggest a different type of treatment.
When you’re back on track, learn from what happened:
- What triggered the relapse?
- What went wrong?
- What could you have done differently?
Discover more about managing a relapse on the Alcohol and Drug Foundation website.
A relapse can be deadly!
If you’ve developed a tolerance for a particular drug over time and then quit taking it, your tolerance levels drop. If you have a relapse and use as much of the drug as you did before quitting, you can easily overdose.
If you, or someone you know, is in danger of overdosing, phone 000 immediately and ask for an ambulance.
Helping someone quit drugs
Watching someone you care about use drugs is stressful. Their behaviour can be erratic and talking to them about their problem is challenging.
Here are some tips on how you can help:
- Learn about the effects of drugs – this will help you understand why quitting can be hard.
- Show that you care without judging – being calm and respectful may encourage them to be open and honest with you.
- Be positive and encouraging rather than negative and nagging – remember relapses may happen, but they don’t mean the person can’t try again, and succeed.
- Offer practical support – sometimes just being there is enough, but you can offer to go with them to parties or join them for a walk or run.
Find more tips on helping someone quit drugs on the Alcohol and Drug Foundation site.
Is addiction hereditary?
Research shows that genetics does play a part in whether someone is likely to become an addict, but it’s not the only factor. Other factors include a person’s:
- environment – for example, growing up amongst addiction where drugs are more available
- temperament – for example, being more sensitive to stress or more impulsive.
Scientists continue to learn about the role of genes in drug addiction so they can develop new ways of preventing and treating it.
Is there anything wrong with this page?
Help us improve health.gov.au
If you would like a response please use the enquiries form instead.
Science, evidence-based facts, key to help end scourge of drug abuse: UN chief

Facebook Twitter Print Email
The world’s drug problem remains an urgent challenge that threatens to exacerbate COVID-19 pandemic impacts and hinder a healthy and inclusive recovery, warned the UN Secretary General ahead of The International Day Against Drug Abuse and Illicit Trafficking.
In a statement published on Friday, Antonio Guterres underscored that trusting science is the “hero and lesson of the pandemic”, and the same action based on evidence is crucial for the responses to drugs.
Worsening problem
The World Drug Report published this week by the UN Office on Drugs and Crime ( UNODC ) showed that drug related deaths have nearly doubled over the past decade. Moreover, 10% of HIV cases in 2019, were due to people injecting themselves with harmful substances.
The UN chief warned that although international cooperation has helped limit the proliferation of new psychoactive drugs, the problem is shifting to poorer regions where control systems are weaker.
Meanwhile, dark web drug sales continue to rise, and non-medical use of pharmaceuticals, including opioids, is expanding.
“ Drug trafficking and organized crime fuel and perpetuate cycles of violence and conflict. Armed groups and terrorists’ profit from the illicit drug trade, and the economic fallout of the COVID-19 pandemic has left millions of people even more vulnerable to drug crime and illicit crop cultivation”, Mr. Guterres underscored.
Invest in prevention
The Secretary General pointed out that investing in balanced prevention as well as control of drug use and drug use disorders produces solid returns such as lives saved, healthier populations, improved workforce participation and productivity, and reduced criminal justice costs.
“ Many of the risk factors associated with crime and violent behaviour are also drivers of drug use, and targeted efforts focusing on these overlapping dynamics - including childhood maltreatment and lack of social support - can help to strengthen prevention”, he said.
More partnerships and data
Public-private partnerships - with tech companies, postal and courier services, and shipping companies - represent an essential frontline response in the new fight against drug traffickers, who “are increasingly exploiting the legal cargo trade and postal services to move their illicit product”, added Mr. Guterres, underscoring that better data is also useful to identify trends and enable real-time monitoring of the trafficking routes.
The Secretary General urged Member States to listen to the science and take action, building on agreed international frameworks and drawing on UN support for health and justice initiatives.
He also reminded that greater cooperation and support are needed to help low-income countries take advantage of cutting edge anti-drug enforcement techniques.
‘Share facts on drugs and save lives’
The head of UNODC, Ms. Ghada Waly, echoed the UN chief’s call for leveraging trustworthy, scientific information and the power of community in influencing health choices and addressing the world drug problem.
“Drugs are destroying health and stealing futures, with drug use alone killing almost half a million people in 2019. Awareness of the risks and access to evidence-based treatment and care can help prevent such tragedies”, she said.
In a statement, Ms. Waly explained the theme of this year’s International Day: Share facts on drugs. Save lives . “It highlights the need for evidence-based approaches to equip the public, as well as health and service providers, and decision makers with the tools to inform choices and effective services”, she emphasized.
The campaign highlights key statistics and data drawn from UNODC’s yearly World Drug Report. Thus, providing facts and practical solutions to the current world drug problem, to attain a vision of health for all, based on science.
Ms. Waly urged governments to expand evidence-based prevention and treatment programmes, as well as monitoring and early warning mechanisms to help lower-income countries detect and counter new substances and use trends.
About the day
Through resolution 42/112 of 7 December 1987, the General Assembly decided to observe 26 June as the International Day against Drug Abuse and Illicit Trafficking as an expression of its determination to strengthen action and cooperation to achieve the goal of an international society free of drug abuse.
Supported each year by individuals, communities, and various organizations all over the world, this global observance aims to raise awareness of the major problem that illicit drugs represent to society.
- International Days
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Managing Substance Use Disorders
- Health Equity
- Data Resources
- Additional HHS Resources
- Overdose Prevention Resources
- Management and Treatment of Pain
- Clinical Practice Guideline at a Glance
- Clinical Care and Treatment
- Health Care Provider Toolkits
- Electronic CDS Tools for Opioids
- Strategies and Partnerships
- Resources for Public Health Professionals
- Journal Articles
- MMWR Articles
- Guides and Meeting Reports
- Related Publications
- Overdose Data to Action
- Drug-Free Communities (DFC)
Treatment of Substance Use Disorders
- Millions of Americans have a substance use disorder (SUD), and it remains an important health issue in our country.
- In 2022, more than one in six Americans aged 12 or older reported experiencing a SUD.
- With effective treatment, recovery is possible for everyone. There is strength in getting help.

What is an SUD?
A substance use disorder (SUD) is a treatable, chronic disease characterized by a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues using the substance despite significant substance-related problems. 1 In 2022, more than one in six Americans aged 12 or older reported experiencing a SUD. 2
SUDs can lead to significant problems in all aspects of a person's life. Patterns of symptoms resulting from substance use (drugs or alcohol) can help a doctor diagnose a person with a SUD or SUDs and connect them to appropriate treatment.
For certain drug types, some symptoms are less prominent, and in some cases, not all symptoms apply. For example, withdrawal symptoms are not specified for inhalant use.
SUDs can range in severity from mild to severe and can affect people of any race, gender, income level, or social class. A SUD can be applied to the following types of drugs: 1
- Hallucinogens
- Opioids (Prescription and Illegal)
- Sedatives, hypnotics, or anxiolytics
- Stimulants and Psychostimulants
- Tobacco (nicotine)
- Other (unknown) substance
Treatment and recovery options
Addiction is a disease, not a character flaw. People experiencing SUDs have trouble controlling their drug use even though they know drugs are harmful.
Overcoming an SUD is not as simple as resisting the temptation to take drugs. Recovery may involve medication to help with cravings and withdrawal as well as different forms of therapy. It may even require checking into a rehabilitation facility.
Addiction is a treatable disease
Like many other chronic conditions, treatment is available for substance use disorders. While no single treatment method is right for everyone, recovery is possible, and help is available for patients with SUDs.
Evidence-based guidelines can assist doctors with choosing the right treatment options. These guidelines help evaluate a patient's clinical needs and situation to match them with the right level of care, in the most appropriate available setting. For more information on evidence-based guidelines visit Addiction Medicine Primer .
Recovery options
There are safe and effective ways to recover from SUDs. Finding the right treatment option can be the key to a successful recovery journey.
Outpatient counseling
Helps people understand addiction, their triggers, and their reasons for using drugs. This form of treatment can be done at a doctor’s office or via telehealth appointment.
Inpatient rehabilitation
A full-time facility provides a supportive environment to help people recover without distractions or temptations.
Behavioral health care
Trained providers who help with mental health concerns.
Medications for opioid use disorder (MOUD)
Specific conditions like opioid use disorder may require medication as the first course of treatment. MOUD can help with cravings and withdrawal symptoms. 3 MOUD is effective in helping people reduce illegal opioid use, stay in treatment longer, and reduce the risk of opioid-involved overdose. 4
MOUD medications approved by the Food and Drug Administration (FDA):
- Buprenorphine
Research has demonstrated that MOUD is effective in helping people recover from their OUD. 5 6 7 It is important to find what works best each individual.
Resource
Reducing stigma is important, addiction can happen to anyone.
SUD is a treatable, chronic disease that can affect people of any race, gender, income level, or social class. No one driving factor leads to SUD. Some people may use drugs to help cope with stress and trauma or to help with mental health issues. Some may develop a SUD after taking opioids that are prescribed to them by doctors. In any case, using drugs over time may cause changes in a person's brain, leading to intense cravings and continued use. 8
Some may view acknowledging and receiving treatment for an SUD as a sign of personal failure and weakness. The associated shame felt by patients and families can make it difficult to seek treatment. Finding a doctor who is comfortable discussing SUDs can help ensure long-term recovery.
Find treatment services
Use these resources to find services that fit your needs:
Mental Health and Addiction Insurance Help (HHS)
Health Center Locator (HRSA)
Behavioral Health Treatment Services (SAMHSA)
Opioid Treatment Program Directory by State (SAMHSA)
Buprenorphine Providers Locator (SAMHSA)
Learn more about recovery
SAMHSA Behavioral Health Treatment Services Locator

Rx Awareness: Real Stories

Recovery is Possible: Know the Options
What You Need to Know About Treatment and Recovery

Opioid Therapy and Different Types of Pain

Addiction Medicine Toolkit
Medication-Assisted Treatment (MAT) | SAMHSA
Decisions in Recovery: Treatment for Opioid Use Disorder
Stigma Reduction
Addiction Treatment Locator, Assessment, and Standards (ATLAS) Platform

Linking People with Opioid Use Disorder to Medication Treatment
Working Together With Your Doctor to Manage Your Pain
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA, American Psychiatric Association, 2013.
- Substance Abuse and Mental Health Services Administration. (2023). Key substance use and mental health indicators in the United States: Results from the 2022 National Survey on Drug Use and Health (HHS Publication No. PEP23-07-01-006, NSDUH Series H-58). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2022-nsduh-annual-national-report
- SAMHSA. 2022, March 22. Medications, Counseling, and Related Conditions. Retrieved from https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions
- TIP 63: Medications for Opioid Use Disorder - Full Document | SAMHSA
- Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2014;(6): CD002207. https://doi.org/10.1002/14651858.CD002207.pub4 PMID:24500948
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev 2009;(3): CD002209. https://doi.org/10.1002/14651858.CD002209.pub2 PMID:19588333
- Fullerton CA, Kim M, Thomas CP, et al. Medication-assisted treatment with methadone: assessing the evidence. Psychiatr Serv 2014;65: 146–57. https://doi.org/10.1176/appi.ps.201300235 PMID:24248468
- https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction
Overdose Prevention
Overdose prevention is a CDC priority that impacts families and communities. Drug overdose is a leading cause of preventable death in the U.S.
For Everyone
Health care providers, public health.
How Schools Can Work to Prevent Substance Abuse

School Health and Wellness //
January 29, 2023
Increasing levels of drug use is a problem among American youth. Today’s teenagers are likely to encounter and exploit a wide variety of dangerous substances, including prescription medications, marijuana, alcohol, opioids, methamphetamine, mushrooms, ecstasy, and other commonly used street drugs.
Drug use among preadolescents and adolescents is a high-profile public health concern. As a physical, social, and psychological “home away from home” for most children, schools have become a primary resource for substance abuse education, early identification, and prevention.
Additionally, substance use affects learning ability. Students under the influence of mind-altering chemicals are not ready to learn and risk long-term impairment of cognitive ability and memory. Using illicit substances is also linked to loss of motivation and self-discipline, absenteeism, and increased risk of antisocial and even violent behavior.
Poor school performance, underachievement, and truancy can all be manifestations of substance use.
The degree of illicit substance abuse among students has led to a societal search for ways to address this problem.
Here’s what your school can do to be a part of the solution.
Establish a Drug Prevention Program
Schools provide a good arena for drug prevention programs because prevention must focus on children before their beliefs and expectations about substance abuse are established. Schools also offer the most systematic way to reach young people, and they can promote a broad spectrum of drug-related educational policies.
Educators must share relevant and impactful information about drug use without enticing students to try drugs. Numerous practical, interactive, and developmentally appropriate curricula support these initiatives. Successful focus includes:
- enhancing students’ problem-solving skills;
- evaluating media influence;
- improving their self-esteem;
- reducing their stress and anxiety; and
- increasing their engagement in meaningful activities.
Prevention programs must be designed to do more than just provide facts about drugs and the impact drugs have on mental and physical health . Teaching students healthy coping skills plays a pivotal role in preventing future experimentation with dangerous substances.
Emphasis on emotional regulation is critical. Children must know how to:
- recognize their own negative feelings;
- identify and name what they are feeling;
- express and manage those feelings; and
- learn practical communication skills, including addressing conflict and asking for what they need.
They also need to explore what healthy peer relationships look like and learn refusal skills—learning to say “no.”
Educators can help students build “exit plans.” For example, some students may not be interested in alcohol or other drugs but will feel they need to participate just to fit in. Work with them to consider options and feel empowered when faced with peer pressure.

Tune in to live webinars every week during the school year to get specific, research-backed insight you can immediately apply at your school.
REGISTER NOW
Leverage Relationships
Students spend most of their day in school, and school personnel are influential role models. Students who believe their teachers care about them are less likely to engage in risky behaviors, including drug and alcohol use.
Relationships with teachers and school counselors are among the most important and formative ones for many students. Those who have developed close ties to trusted adults are more likely to recognize the many ways substance abuse can negatively impact their future. Ensure all students are connected with teachers they trust and respect—teachers who know them well enough to identify warning signs.
Establish firm boundaries that allow teachers to share relatable stories about smart decisions regarding alcohol and other drugs. These stories could illustrate the consequences of engaging in risky behavior or stories about experiences with difficult decisions prioritizing personal well-being over friendships.
Create an Early Intervention/Wellness Team
Every staff member should know the warning signs of substance use and the protocols for intervention. But there are faculty members that students gravitate toward—teachers students feel comfortable with. By identifying those individuals, you can create a “Wellness Team,” perhaps championed by a trusted school counselor. The adults on the team need not be credentialed counselors, but can be trained in strategies that add a layer of prevention and intervention for students who talk to them.
This team should be nondisciplinary. Instead, it should include adults who generate safe spaces for students to report concerns about their peers and worries about themselves.
The best strategies for substance abuse prevention and intervention are those that work for a school’s community and culture . Schools must enlist the help of parents and encourage similar discussions at home. When students hear the prevention message at school and home, they are much less likely to try drugs or alcohol. In addition, communities that can establish a positive peer prevention program will see even better results.
*Content courtesy of D&G Wellness Consulting.
Share this article: | |
24/7/365 Digital Access to Live Mental Health Professionals
Wellness in Independent Secondary Education (WISE) Program
Mental health crises have reached a high point in the news and in schools around the world. The impact on students who often don’t get the care they need is unimaginable. ISM’s Wellness in Independent Secondary Education (WISE) is the only program that provides resources for both students and school leaders to receive support from mental health professionals when they need it most. Students have 24/7 access to health experts through our custom phone app—enabling them to speak to a provider when their need is greatest.

Upcoming Events

1/29/2024 — 1/31/2024
Strategic Financial Planning: A Comprehensive Approach
Status: Open
More Events
NA and Other Peer Support Groups for Drug Addiction
Opioid addiction, overcoming drug addiction, choosing an alcohol rehab treatment program, staying social when you quit drinking.
- Vaping: The Health Risks and How to Quit
Women and Alcohol
- Binge Drinking: Effects, Causes, and Help
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Healthy Eating
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Childhood Issues
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Aging Issues
- Alzheimer’s Disease & Dementia
- Senior Housing
- End of Life
- Meet Our Team
The effects of drug abuse and addiction on family and friends
Understanding your loved one’s substance abuse, recognizing drug abuse in a loved one, how to talk to someone about their drug abuse, supporting a loved one’s addiction recovery, setting healthy boundaries, taking care of yourself, helping someone with a drug addiction.
Does someone you love have a drug problem? Whether it’s illegal substances or prescription medication, you can’t force anyone to stop abusing drugs. But there are ways to support their recovery.

Witnessing someone you care about battle a substance use disorder can be extremely distressing and take a heavy toll on your own mental and emotional well-being. Whether the drug abuser is a close friend, spouse, parent, child, or other family member, it’s easy for their addiction to take over your life. It can pile stress upon stress, test your patience, strain your bank balance, and leave you racked by feelings of guilt, shame, anger, fear, frustration, and sadness.
You may worry about where your loved one is at any given time, their risk of overdosing, or the damage they’re doing to their health, future, and home life. You may be in debt from paying their living expenses, the cost of legal troubles resulting from their drug abuse, or from failed attempts at rehab and recovery. You may also be worn down by covering for your loved one at home or work, having to shoulder the responsibilities they neglect, or being unable to devote more time to other family, friends, and interests in your life.
As despairing as you may feel, you’re not alone in your struggle. A Pew Research Center survey in 2017 found that nearly half of Americans have a family member or close friend who’s been addicted to drugs. Across the Western world, the abuse of prescription pain relievers and tranquillizers has skyrocketed in recent years, creating a public health crisis. (Along with marijuana, they’re now among the most frequently abused drugs.)
Whether the problem is with recreational drugs or prescription medications, drug abuse and addiction can affect people from all walks of life, wrecking families, tearing relationships apart, and destroying lives. But there is help available. While you can’t force someone to tackle their addiction, your love, support, and patience can play a vital part in their recovery. With these guidelines, you can learn to support your loved one’s efforts, set the necessary boundaries to preserve your own health and welfare, and find some stability for both yourself and your loved one.
People start using drugs for a lot of different reasons. Many turn to substances to cope with the emotional pain of a mental health problem, such as depression, anxiety, or PTSD. Known as self-medicating , some people may be aware they have a mental health issue but are unable to find healthier ways of coping, while others remain undiagnosed and use drugs to manage specific symptoms.
Other people turn to drugs to change how they feel, to fit in, or to alleviate boredom or dissatisfaction with their lives. Then there are those whose substance abuse develops from a doctor’s well-intentioned efforts to treat a medical condition. Of all the people prescribed opioids to relieve pain, for example, estimates suggest that more than a quarter will end up misusing the drug.
[Read: Opioid Addiction]
Whatever your loved one’s reason for starting, though, not everyone who uses drugs develops a problem. While the exact causes of addiction aren’t clear, genetics likely plays a role, along with environmental factors. While one person is able to use substances without detrimental effects, another finds even casual use quickly escalates into compulsion and addiction—a very dark hole from which they can feel powerless to emerge.
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
It’s not always easy to recognize if a loved one is abusing drugs. In teens, for example, drug abuse can often resemble normal adolescent moodiness. Furthermore, there’s no specific amount or frequency of use that indicates someone’s drug use has become a cause for concern. Whether your loved one is using every day or every month, it’s the adverse impact their drug abuse has on their life that indicates a problem.
[Read: Drug Abuse and Addiction]
Signs your loved one may have a substance use disorder include:
Experiencing problems at work, school, or home . They appear high more often, for example, and take more days away from work or school to compensate. Their work performance or school grades suffer, they neglect their responsibilities at home, and encounter more and more relationship difficulties. They may even lose their job, drop out of school, or separate from a long-term partner.
New health issues , such as changes in sleep schedule, often appearing fatigued or run-down, pronounced weight loss or weight gain, glassy or bloodshot eyes, and forgetfulness or other cognition problems. Depending on the type of drug they’re abusing, they may also exhibit frequent sniffing, nosebleeds, or shaking.
Changes in their mood and behavior . Your loved one may be more secretive and lie about what they’re doing, where they’re going, or how much they’re using. They may be quick to anger or lash out, especially if you try to talk to them about their drug use. Heavy drug users often lose interest in old hobbies, lack energy, and become more moody, withdrawn, and sad. They may even neglect their appearance and personal hygiene, and suffer withdrawal symptoms if deprived of their drug of choice.
Recurring financial problems . Your loved one may run up credit card debt to support their drug use, seek loans, or ask to borrow money without any solid reason. They may even steal money or valuables to sell for drugs.
Drug paraphernalia to look out for
You may also be able to spot a loved one’s substance abuse through the new or increased presence of drug paraphernalia.
- Paper wraps, small pieces of cling film, and tiny plastic bags are used to store drugs.
- Rolling papers, pipes, bongs, or pierced plastic bottles or cans are often used to smoke drugs.
- Burnt foil, spoons, and syringes may indicate heroin use.
- Those abusing prescription medications may be renewing their prescriptions more frequently or have bottles of medication prescribed for someone else.
Starting a conversation with someone about their drug addiction is never easy, but it’s important you come from a place of compassion and understanding. Remember, no one sets out to become an addict. Drug abuse is often a misguided attempt to cope with painful issues or mental health problems. Stress tends to fuel addictive behavior, so criticizing, demeaning, or shaming them will only push your loved one away and may even encourage them to seek further comfort in substance abuse.
Discovering someone you love has a drug problem can generate feelings of shock, fear, and anger, especially if it’s your child or teen who’s using. These strong emotions can make communicating with a drug user even more challenging. So, it’s important to choose a time when you’re both calm, sober, and free of distractions to talk. Offer your help and support without being judgmental.
Don’t delay . You don’t have to wait for your loved one to hit rock bottom—to get arrested, lose their job, suffer a medical emergency, or publicly humiliate themselves—to speak out. The earlier an addiction is treated, the better.
Express your concerns honestly . Emphasize that you care for the person and are worried about their well-being. Offer specific examples of your loved one’s drug-related behavior that have made you concerned—and be honest about your own feelings.
Listen . Even when you don’t agree with the person, take the time to listen to what they have to say, without trying to argue or contradict them. The more your loved one feels heard, the more they’ll see you as supportive, someone they can confide in.
Offer them information about how they can address their drug problem—whether that’s calling a helpline, talking to a doctor or counselor, entering a treatment program , or going to a group meeting such as SMART Recovery, or a 12-step program like Narcotics Anonymous (NA) .
[Read: Overcoming Drug Addiction]
Be prepared for denial. Your loved one may become defensive or angry and refuse to discuss their drug use. Many people feel a sense of shame when confronted by their behavior and will try to deny they have a problem. Don’t argue with them, just revisit the issue another time.
Avoid trying to lecture, threaten, bribe, or punish the person. Getting angry or making emotional appeals will likely only add to the user’s feelings of guilt and reinforce their compulsion to use.
Don’t expect a single conversation to fix the problem. This will likely be the first of many conversations you’ll need to have regarding your loved one’s drug use. There’s no quick fix to overcoming addiction. It may take several conversations for them to even acknowledge they have a problem, the first step on the road to recovery.
Staging an intervention
Staging an intervention tends to be a last-ditch effort to make someone realize they need treatment. However, many addicts can react angrily when confronted by a group or feel their loved ones are ganging up on them.
If you decide to stage a family meeting or intervention, it’s important everyone involved comes from the same place of compassion and understanding. This is not an excuse for people to vent their grievances about the addict’s behavior or make them feel bullied or ashamed. The problem is the disease of addiction, not the person in its grip.
There’s no one-size-fits-all solution to overcoming an addiction to drugs, and it’s rarely a process that’s quick or straightforward. While you can support your loved one and encourage treatment , you can’t force them to change or control their decision-making. Letting your loved one assume responsibility for their behavior and choices is an important step on their road to sobriety.
Adjust your expectations . Everyone is different. Recovery for one person may mean total abstinence from drugs. For another, it could mean cutting back or staying mostly drug-free. Being too rigid in your expectations can lead to disappointment and a sense of failure, even if your loved one finds stability in their life again.
Encourage your loved one to seek help . While some people are able to quit drugs on their own, the more help and support a person has, the better their chances of success. Offer to sit with your loved one while they call a helpline or accompany them to a doctor’s appointment, counseling session, or peer support group meeting .
Ensure they address any co-occurring issues . The problems that triggered your loved one’s drug use in the first place will still be there once they get sober. If they turned to drugs to self-medicate a mental health problem such as anxiety or depression, they’ll need to find healthier ways of coping with these issues without resorting to substance abuse. To achieve long-term recovery, it’s vital they tackle both their addiction and their mental health issue at the same time.
[Read: Dual Diagnosis: Substance Abuse and Mental Health]
Help plan for triggers and cravings . Your loved one will need to find ways to cope with drug cravings and triggers . You can help distract them with other activities or encourage them to learn how to ride out the urge, but ultimately, they have to be responsible for their own sobriety.
Encourage them to explore new interests . Quitting drugs can leave your loved one with a lot of extra time to fill. To help them avoid slipping back into old habits, encourage them to develop new interests—ones that don’t involve drugs but do add meaning to their life. Think volunteering , taking up a new sport or hobby, enrolling in a class, or spending time in nature hiking or camping, for example—anything that doesn’t generate a trigger to use.
Accept the likelihood of relapse . Despite your efforts and your loved one’s best intentions, the truth is that recovery often involves relapse. If that happens, encourage the person to recommit to getting clean and support them as they try again. Try to stay patient. Each relapse is an opportunity for your loved one to learn from their mistakes and find a new way forward.
Treatment options
Treatment can take place at home, as a hospital outpatient, or in a residential facility or sober living community. While it can vary according to the type of drug your loved one is addicted to, their age, and any other issues they’re facing, most treatment plans include some of the following elements:
- Detox to purge the body of drugs, manage withdrawal symptoms, and achieve stability.
- Treatment for any co-occurring mental health problems.
- Counseling , whether it’s individual, group, or family therapy —or a combination of all three—to tackle the root cause of the drug use and learn better ways of coping.
- Medication to help with withdrawal or treat any co-occurring disorders.
- Ongoing peer support meetings, such as a 12-step program, to keep the recovery on track and maintain sobriety.
[Read: Choosing Drug Rehab and Addiction Treatment]
When someone you love has a problem with drugs, it’s easy to fall into the trap of shielding them from the consequences of their addiction. Referred to as “enabling”, you may cover up for the person, take over their responsibilities, put their feelings before your own or other family members’, rearrange your life to accommodate their addiction, or provide financial assistance when they’re unable to pay bills or get into legal trouble because of their drug use.
While it may seem that you’re being supportive, enabling your loved one will only help maintain their addiction—and damage your own health and well-being along the way. Of course, it can be extremely hard to say “no” to someone you love, especially if it’s your child, but protecting the person from the consequences of their drug abuse often means you’re removing the motivation for them to seek help and change.
To better help someone with a drug addiction, it’s often necessary to hold them accountable for their actions by establishing limits or boundaries for what is and isn’t acceptable behavior. Without boundaries, your loved one never has to face the consequences of their actions—and you’ll eventually feel burned out from all the attempts to cover up, excuse, or compensate for their behavior.
Establishing boundaries for a loved one abusing drugs could include:
- Not allowing drug use, drug paraphernalia, or other drug users in the home.
- Not covering up for them if they miss work or school, not lying to get them out of trouble, or not taking over any responsibilities they’ve neglected.
- Requiring they pay their share of rent and other bills on time.
- Refusing to give them money to pay off debts or cover legal expenses if they’re arrested.
- Insisting that they always treat you with respect, even when high.
How to set boundaries—and stick to them
- Talk to your loved one about boundaries at a time when you’re both calm and not under the influence of drugs. Clearly outline what behavior you will and will not tolerate and what the consequences will be if they break your rules.
- Follow through . It’s almost inevitable that someone with an addiction will test any limits you set, so be prepared to follow through. If you don’t enforce the consequences you’ve outlined, your loved one will know the boundaries are worthless and their destructive behavior will continue.
- Remind yourself why you’re doing this . No one wants to see someone they care about suffer, but a meaningful, respectful relationship cannot exist without boundaries. Having to face the negative consequences of their behavior could be the impetus your loved one needs to get clean.
Establishing financial boundaries
In addition to the heavy emotional costs, money problems can also mount for families of drug abusers. Heavy drug use can be expensive, as can the cost of rehab and resolving legal problems stemming from your loved one’s drug dependency. It’s not uncommon for spouses to lose their homes bankrolling their loved one’s addiction, parents to empty their retirement accounts bailing their child out of debt, or for other family members to max out their credit cards paying for costly rehab programs.
That doesn’t make cutting off your loved one any easier. When setting financial boundaries, it’s important to consider how far you’re willing go. For example, are you willing to see your loved one spend time in jail instead of covering their legal fees? Are you willing to see them evicted or living on the street instead of paying their living expenses?
While setting boundaries won’t cure your loved one of their drug addiction or guarantee they seek help, neither will spending money. If your loved one chooses not to address their addiction, it won’t matter how much money you spend trying to change that. Ultimately, all you can control is how well you look after your own health and welfare.
Your loved one’s recovery from drug addiction can be a long process and the negative impact on your own health, outlook, and well-being can multiply over time. It’s important you maintain a balance in your life to avoid burnout from all the stress and frustration that comes from helping someone get clean.
Find support . Expressing what you’re going through can be very cathartic, so look for support from trusted friends and family, or a peer support group for family members of drug addicts. Talking to others who are facing similar challenges can help you find comfort, reassurance, and new ways of coping.
Manage stress . The stress of witnessing someone you love battle addiction can take a heavy toll. You can reduce your stress levels by eating right, exercising regularly , sleeping well, and practicing a relaxation technique such as yoga, deep breathing, or meditation. Since stress levels can escalate when quitting drugs, you can even encourage your loved one to do the same.
[Listen: Eye of the Storm Meditation]
Practice acceptance . At some point, you’ve probably asked yourself “Why me?” or even blamed yourself for your loved one’s struggle with addiction. But dwelling on circumstances outside your control will only sap your energy and damage your mood. Instead of searching for someone to blame or asking questions with no easy answers, learning to accept the things you can’t change can help you focus on the things that you do have control over.
Maintain other interests and relationships . It’s easy for your loved one’s battle with addiction to become all-consuming. But you’ll find it easier to cope with a difficult situation when other areas of your life are rewarding. Set aside time in your day to pursue activities and relationships that bring you joy—and try to keep up with work, hobbies, and social plans.
Support for sufferers of substance use disorders
Call the SAMHSA helpline at 1-800-662-4357.
Find NHS drug addictions support services or call the Frank helpline at 0800 776600.
Download the PDF Finding Quality Addiction Care from the Canadian Centre on Substance Use and Addiction.
Find support or call the Alcohol and Drug Foundation helpline at 1800 250 015.
Support for families and loved ones
For parents in the U.S.: Get One-on-One Help to Address Your Child’s Substance Use or call the Partnership for Drug-Free Kids helpline at 1-855-378-4373.
Nar-Anon , a 12-Step Program for Family & Friends of Addicts, with worldwide chapters and online support groups.
SMART Recovery offers online and in-person support worldwide for family and friends.
Group and 12-step programs for your loved one (most have worldwide chapters)
SMART Recovery
Narcotics Anonymous
Cocaine Anonymous
Crystal Meth Anonymous
Marijuana Anonymous
More Information
- Intervention: Help a loved one overcome addiction - Tips on holding a successful intervention. (Mayo Clinic)
- Coping When a Parent Has an Alcohol or Drug Problem - Help for teenagers and adolescents. (TeensHealth)
- Step by Step Guides to Finding Treatment for Drug Use Disorders (PDF) - Guides for adults, teens, or those helping someone addicted to drugs. (National Institute on Drug Abuse)
- Effective Treatments for Opioid Addiction - Medications used in the treatment of opioid addiction. (National Institute on Drug Abuse)
- What is Substance Abuse Treatment? A Booklet for Families - Learn about treatment options and what you can do. (SAMHSA)
- How can prescription drug addiction be treated? - Treatment options for prescription drug addiction including addiction to opioid painkillers. (National Institute on Drug Abuse)
- Overcoming Addiction: Find an effective path toward recovery - Special health report from Harvard Medical School. (Harvard Health Publishing)
- Substance-Related and Addictive Disorders. (2013). In Diagnostic and Statistical Manual of Mental Disorders . American Psychiatric Association. Link
- O’Brien, C. P. (2011). Evidence-Based Treatments of Addiction. FOCUS, 9 (1), 107–117. Link
- Gramlich, J. (2017, October 26). Nearly half of Americans have a family member or close friend who’s been addicted to drugs. Pew Research Center . Link
- 2019 National Survey of Drug Use and Health (NSDUH) Releases | CBHSQ Data . (2020, September). Substance Abuse and Mental Health Services Administration (SAMHSA). Link
- Magill, M., & Ray, L. A. (2009). Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs, 70 (4), 516–527. Link
- Vowles, K. E., McEntee, M. L., Julnes, P. S., Frohe, T., Ney, J. P., & van der Goes, D. N. (2015). Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. PAIN, 156 (4), 569–576. Link
More in Addiction
The different options and what they offer

Tips for treatment and recovery

A guide to help you cope with cravings and deal with relapse

A guide to alcohol addiction treatment services

Cutting down on alcohol doesn’t have to mean losing your social life

The health risks in young people and how to quit

The hidden risks of drinking

Binge Drinking
Help if you have trouble stopping drinking once you start

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
The Drug Crisis: Problems and Solutions for Local Policymakers

While most Americans have focused on the Covid-19 pandemic, the nation’s other great epidemic has continued to burn. Drug overdoses now claim the lives of over 100,000 Americans every year, a rate that appears likely to continue or grow for the foreseeable future. While the crisis once was concentrated predominantly in rural, white communities, the introduction of novel synthetic opioids, particularly fentanyl, into the illicit drug supply has spread overdoses across urbanizations.
Today, small-town and big-city leaders alike desperately need tools to fight back against the drug crisis. It can often seem as though drug policy is outside the ambit of local leaders, who lack the capacity to go after international traffickers or spend trillions of dollars on care. But local government, as the closest entity to the front lines of the crisis, plays a vital role in addressing it.
This paper, therefore, explores options for local policymakers to respond to the drug crisis. In particular, it considers six frequently discussed local-scale policies:
- Naloxone access and distribution
- Investing in treatment capacity
- Drug court programs
- Wastewater tracking
- Supervised consumption sites
- Drug market interventions
For each policy, this paper examines the evidence, offers estimates of costs, and provides caution where necessary. The overall goal is to give local policymakers a better understanding of what tools they have to more effectively tackle the other health crisis in their communities.
DOWNLOAD PDF
From Urban to Rural: The Spread of the Drug Crisis
Between 2000 and 2021, the annual drug overdose (OD) death rate in the U.S. quadrupled, to roughly 107,000 deaths by the end of last year.[ 1 ] Drug overdose deaths now routinely exceed those from homicide, suicide, car crashes, and many medical causes.[ 2 ] By best estimates, the drug OD death rate is now six times higher than its highest point in the 20th century[ 3 ] and well above any point since the initiation of the modern drug-control regime.[ 4 ]
Public perception of this crisis lagged behind its growth. About 20 years ago, drug OD deaths were rising disproportionately among white, middle-aged Americans in predominantly rural or small metropolitan areas, particularly in Appalachia and the upper Midwest, areas particularly affected by the decline in manufacturing employment. As depicted in books like J. D. Vance’s Hillbilly Elegy or Beth Macy’s Dopesick , the white, rural drug crisis is often thought to combine longstanding socioeconomic disenfranchisement with the acute effects of predatory pharmaceutical firms, which flooded communities with highly potent prescription opioids and created iatrogenic (physician-caused) addiction.
While this picture remains accurate in some regards, it is also incomplete. Figure 1 breaks out OD death rates by level of urbanization for three years: 2000, 2010, and 2020.[ 5 ] The percentages over the 2010 and 2020 bars represent the percent increase in the OD death rate compared to the same urbanization in the prior decade.
Drug Overdose Death Rates in 2000, 2010, and 2020, by County Urbanization

As of the year 2000—near the beginning of the crisis—OD deaths were more common in more urban counties, that is, those that contained large or medium-sized cities or large cities’ suburbs (“large fringe metro”),[ 6 ] and less common in small cities, towns, and rural (“NonCore [Nonmetro]”) counties. Over the next 10 years, OD death rates rose across urbanizations, but they rose more—as captured by the percent change—in less urban areas. The total effect was that by 2010, OD death rates were higher in more rural areas than they were in more urban ones, particularly in the most rural counties—creating the impression of the crisis as a predominantly rural problem.
But between 2010 and 2020, the pattern again reversed. Although all urbanization types saw a large increase in OD death rates, the increases this time were largest for cities. Although the drug crisis continued to worsen in rural areas, the increases in OD deaths in cities were so extreme that cities overtook rural areas and again had the highest death rates.[ 7 ]
Figure 2 shows OD death rates by year, urbanization, and type of drug involved. This chart shows in clearer detail the phenomenon captured in Figure 1. In particular, it shows how precipitously from 2000–10 OD deaths rose in small-town and rural America, driven primarily by prescription opioids (included in “other opioids” in the CDC’s system). Then, between 2010 and 2020, illegally manufactured fentanyl (IMF) and other novel synthetic opioids arrived on the scene, eclipsing death rates from other types of drugs. This is particularly true in large and medium cities, where illegal opioids (formerly heroin, now also IMF) are a far larger problem than methamphetamine, which is a bigger issue relative to IMF for more rural Americans.[ 8 ]
Drug Overdose Death Rates 1999–2020, by Type and Urbanization

These data illustrate what drug policy scholar Daniel Ciccarone has called the “triple wave” epidemic.[ 9 ] A first iatrogenic wave was caused by the widespread distribution, diversion, and consumption of prescription opioids, particularly Purdue Pharmaceutica’s OxyContin.[ 10 ] Policymakers responded to this wave through pressure on pharmaceutical firms and tighter controls on prescription opioids. Those now-dependent individuals responded by switching from prescription opioids to heroin, igniting the second “wave” driven by heroin deaths.[ 11 ]
The third wave was ushered in by drug suppliers introducing synthetic opioids into the drug supply. This shift was the product of a variety of factors: the acquisition of relevant chemistry knowledge by Mexican drug trafficking organizations, China’s production of fentanyl, and then, later, grey-market precursor chemicals.[ 12 ] Synthetic opioids are, from a producer’s perspective, a vastly superior product: easier and much cheaper to produce and transport, as well as more potent and therefore more compact.
Whereas the second wave stemmed from people with an opioid-use disorder joining an (existing) illegal market, the third wave was instigated by the producers. As one RAND analysis notes, “dealers are not transparent when it comes to the distribution of synthetic opioids, using them to adulterate heroin or pressing them into tablets made to look like prescription medications.”[ 13 ] Unlike the iatrogenic wave, there is no reason to believe that fentanyl has drawn in many more users. Rather, the wave of deaths comes from increasing the death rate of a preexisting stock of users.[ 14 ] In fact, users are often alarmed by the introduction of far more potent fentanyl into their supply of illegal opioids (that had previously been mostly heroin).[ 15 ]
Many other drugs are now adulterated with IMF. Such multidrug combinations are increasingly common and particularly dangerous. Drug deaths regularly involve multiple substances, with the simultaneous presence of opioids and cocaine, methamphetamine, benzodiazepines, or alcohol leading to death.[ 16 ] Figure 3 shows drug OD death rates, distinguishing between deaths that did and did not involve synthetic opioids.
Drug Overdose Death Rates 1999–2020, by Urbanization and Synthetic Involvement
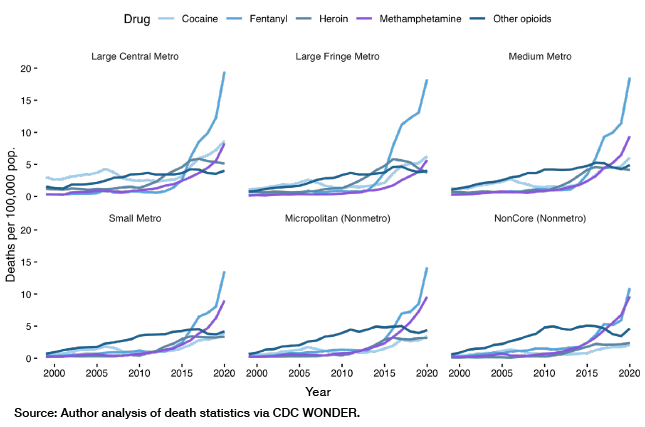
This figure recapitulates Figure 2, insofar as IMF is a bigger share of the problem in large and medium-sized cities than it is in small cities and rural areas. Absent IMF-involved deaths, for example, the OD death rate in more urban areas would be below its 2016 peak; in less urban areas, it would be at or above it. But Figure 3 underscores that IMF in isolation is not the problem. Rather, it is IMF leaching into the urban drug supply more generally, which can cause people with histories of (comparatively) less harmful use to experience deadly overdoses.[ 17 ]
How Local Leaders Can Respond
Drug policy interfaces uncomfortably with America’s federalized system. Drug selling, consumption, addiction, and death play out at the local level, but supply is driven by forces at the national and international scale—high-level, wholesale distribution organizations that span state borders, the international drug market and border enforcement, and the socioeconomic factors that marginally affect the tendency to produce and consume drugs, among others. It may be easy for local policymakers to feel like the drug crisis is simply too big a problem for them to cope with, and that only national or international action can stem the tide.
While drug policy must be conducted at all levels of government, there is a significant role for local leaders to play in combatting the crisis. In this section, I discuss policy approaches uniquely suited for the local level.
Naloxone Access/Distribution
Naloxone is an FDA-approved medication that can rapidly reverse the effects of opioid overdose by binding to opioid receptors without causing the respiratory depression and other harmful effects of opioids that lead to overdose.[ 18 ] Because of these potent properties, naloxone is a powerful lifesaving tool. Many jurisdictions already equip first responders with naloxone, while some have experimented with wider distribution, including to people at risk of OD or to the general public.
But does such distribution have a significant impact on overdose death rates? In allocating scarce dollars, is naloxone a good use of money? And to whom should naloxone be distributed?
One view is that widespread naloxone availability will uniformly reduce overdose deaths by increasing the probability that the drug will be available at the time of overdose. Some argue, however, that this effect could be counterbalanced by “moral hazard”—by reducing the risk associated with each individual use, greater naloxone access may lead to more use, cancelling out beneficial effects or actually leading to more overdose deaths. It is also the case that having a naloxone supply is not necessarily enough: just because naloxone is available does not mean that people will use it.
One way to understand the effect of naloxone availability on OD deaths is to look at research on “naloxone access laws” (NALs). Such laws make naloxone more available, for example, by allowing the purchase of naloxone with or without prescription, or preventing prescribers or bystanders from being held liable for administering naloxone to someone other than the person to whom it was prescribed or in the process of a criminal act (i.e., consuming drugs).[ 19 ] What is the impact? A comprehensive review of studies on NALs finds that the passage of NALs is generally associated with either no effect on or a decrease in opioid overdose mortality.[ 20 ]
Not all NALs are the same, however, and different laws may have different effects. Of the studies covered by the aforementioned review, one found that NALs immunizing prescribers from liability reduced OD deaths by 23%, while other NALs had no impact.[ 21 ] Another found that removing criminal liability for possession of naloxone was associated with a 16% reduction in overdose mortality.[ 22 ] And a third found that the only NAL with an impact contained provisions that allowed pharmacists to dispense naloxone directly, reducing OD deaths by 34%.[ 23 ] Lastly, one paper found no effects of NALs except for laws permitting civilians to administer naloxone, which was associated with a significant increase in OD deaths.[ 24 ] Why so much ambiguity? One possible answer is that naloxone-access laws tend to go into effect at the same time, often across many locales, which means there is little variation to exploit for purposes of identifying their effect. There may be effects that we can’t easily measure.
What should policymakers take away from this (confusing) evidence? One safe conclusion is that there is little evidence that NALs, with the possible exception of lay administration laws, lead to an increase in OD deaths, and at least some evidence that they reduce them. Another reasonable inference is based on the insight that NALs expand access to people other than first responders. If there is some evidence that giving naloxone to the man on the street can reduce OD deaths, it stands to reason that trained responders equipped with naloxone are very likely to reduce deaths.
Another way to think about naloxone is in terms of costs and benefits. Naloxone is relatively cheap—usually somewhere around $20 to $50 per dose for the generic form and up to $150 per dose for name-brand Narcan.[ 25 ] That cost is almost always worth it, insofar as naloxone is rarely going to be used in a situation where the harm it prevents is worth less—for example, in terms of quality-adjusted life-years—than the cost of using it. There may be individuals on the margins for whom naloxone use is harmful, but it’s likely that in most individual instances, it is beneficial.
Local policymakers, then, should certainly support giving their first responders—EMTs, firefighters, and police officers—naloxone. In addition, distributing naloxone to the average person on the street, and even the average person who uses drugs, is as at least unlikely to do net harm, and quite possibly, it may have a net benefit. Policymakers worried about the risk of “moral hazard” should think about how to minimize downside without losing the upside of naloxone distribution. Distribution could be tied to offers of treatment, for example, and repeated emergency department visits as a sign that someone may need more intensive attention. Fitting naloxone into the matrix of other drug treatment and control methods, in other words, may help to mitigate any risks associated with it while preserving its benefits.
Invest in Treatment Capacity
Drug treatment is a dramatically underutilized resource. The federal Substance Abuse and Mental Health Services Administration (SAMHSA), a division of the Department of Health and Human Services, estimated that as of 2020, some 40.3 million Americans needed treatment for a substance-use disorder (SUD), including about 18.4 million suffering from an illicit drug–use disorder, and 4.2 million suffering from a substance-use disorder related to an illicit drug other than marijuana. By comparison, only about 4 million Americans actually received treatment, roughly two-thirds of whom were in treatment for a drug-use disorder (many in addition to an alcohol-use disorder).[ 26 ]
One explanation for this “treatment gap”—sometimes the only explanation offered—is inadequate funding of treatment. But some of the gap also reflects disinterest on the part of users. Some disagree with the premise that they need treatment—SAMHSA’s definition of a SUD is quite broad, and denial is a hallmark of addiction. Yet even among people who said they needed treatment, only one in five actually made an effort to get it.[ 27 ] In other words, even among those who believe they would benefit from drug treatment, many are not actually getting into treatment.
Of course, there are many barriers to getting someone into treatment: health insurance, stigma, lack of childcare, etc. And not all drug treatment is created equal—some approaches are far more efficacious than others (a full review is beyond the scope of this paper, but the issue is treated briefly below). That acknowledged, it is worthwhile for municipal policymakers to ask holistically whether they have adequate capacity to meet the demand for drug treatment, and whether they are successfully connecting those who want help with the help that they need.
Local government has a role to play in treatment access. As of 2020, local, county, and community governments operated about 4% of treatment facilities—a small share but double that administered by state, federal, or tribal governments.[ 28 ] And government at all levels funds drug treatment that is provided by non- and for-profit providers.[ 29 ] In addition, local government often oversees drug treatment in jails, a place where some people get access to treatment while others lose it, thereby increasing their risk of an overdose. Government can also play a role in advertising for drug treatment and connecting people with substance-use disorders to treatment through the social services system, criminal justice system, and street outreach.
Treatment for substance-abuse disorders is not bulletproof. The National Institute of Drug Abuse estimates a 40 to 60% relapse rate, which NIDA attributes to a failure to understand treatment as an ongoing, rather than one-time, intervention.[ 30 ] On the other hand, much treatment depends on therapeutic approaches, from cognitive behavioral therapy to contingency management. In the case of opioid-use disorders, however, several medications—buprenorphine, methadone, and naltrexone—exist to effectively substitute for harmful opioids, mitigating cravings without leading to respiratory depression and death. Such “medication assisted treatment” has been shown to substantially reduce overdose mortality.[ 31 ] Although local government cannot necessarily set regulations about the use of “medication assisted treatment,” it can in many cases encourage or even mandate its use in treatment facilities or jails it oversees, funds, or operates.
Cost estimates for treatment will necessarily vary based on the kind of treatment. NIDA estimates, for example, that methadone maintenance costs roughly $4,700 per year per patient; somewhat older estimates (vintage 2001–02) peg the cost of outpatient treatment at between $1,500 and $8,200 per patient per year, though these may have changed.[ 32 ] Those costs can be balanced against their benefits: analysis usually indicates that the social benefits yielded by drug treatment are worth the cost, with one commonly cited estimate being seven dollars saved to one dollar spent.[ 33 ] This comes from reduced health harms as well as reduced social harms, as expanding substance abuse treatment also reduces crime in the surrounding area, for example.[ 34 ] But they can also be balanced against alternatives: as mentioned below, the cost of methadone maintenance therapy is similar to the cost of supervised consumption.
Limited as it is, treatment is often the only way to mitigate the long-run risks and harms of disordered drug use. Filling the “treatment gap” is not innovative, but it is lifesaving, and local leaders should ask if they have done so before trying other, more daring, approaches.
Drug Courts
Many people with substance-abuse disorders interact with the criminal justice system, either because they are apprehended for drug possession/distribution, because of behavior driven by their SUD (for instance, theft or public disorder), or simply incidentally, that is, they both offend and have a SUD. In many jurisdictions today, some of these people are diverted from the regular criminal justice process of trial, conviction, and incarceration to specialized courts meant to target the “root cause” of their behavior, namely their drug abuse. Such courts usually offer enrollees (“clients”) an opportunity to have their sentences reduced or waived altogether, assuming they complete a course of drug treatment actively overseen by the court, including through regular check-ins and the dispensing of rewards and punishments. The model depends, in essence, on a carrot-and-stick approach: if a client gets clean, he stays out of jail; if he fails, he gets locked up.[ 35 ]
The first drug court opened in 1989 in Miami-Dade, Florida, in response to the crack cocaine epidemic.[ 36 ] As of 2014, there were over 3,000 drug courts nationwide, serving an estimated 127,000 participants. That number of drug courts represents a 24% increase over 2009, meaning almost certainly that even more exist today. As of 2014, drug courts cost an average of $6,008 per participant, though the range of reported costs extended from $1,200 to $17,000, and much data was missing.[ 37 ]
Drug courts appear to have a significant effect on clients’ tendency to reoffend—a proxy for both their drug use and the harmful effects of their drug use on their communities. Multiple meta-analyses find that drug courts reduce enrollees’ recidivism rates by between 9 and 24%, albeit with substantial heterogeneity in the effectiveness of different kinds of drug courts.[ 38 ] These effects persist for at least three years after leaving the program, with one study finding effects up to 14 years later.[ 39 ] A 23-site study confirmed that drug court involvement not only reduced criminal behavior but also actual criminal drug use.[ 40 ] These findings suggest drug courts are a winning option for local executives who want to reduce crime while being compassionate.
Depending on the laws within their jurisdiction, local administrators have the power to establish drug court programs. This is in part because many judges are locally elected, and successful drug court programs require a committed judge to spearhead the effort. But it is also because a successful drug court program requires coordinating many resources—access to treatment, housing, jail capacity, etc.—across multiple local government agencies. Such coordination requires local administrative competency to get it done, and so local executives should see doing it as partially their responsibility.
Wastewater Tracking
In spite of the scale of the drug overdose crisis, the U.S. continues to struggle with tracking drug overdose and use in real time. The elimination of previous surveillance systems, namely the Drug Abuse Warning Network (DAWN) and Arrestee Drug Abuse Monitoring (ADAM) programs, have effectively blinded policymakers at a time when up-to-date information is essential.[ 41 ] The CDC does, as of recently, report provisional and partial estimates of monthly OD deaths on a one-month lag. Local coroners can track deaths, and local emergency departments can track nonfatal overdoses, but a death or overdose is the outcome we want to avoid. Policymakers at all levels of government need tools for tracking drug use in real time, so as to enable a proactive response before drugs kill.
One solution is to track the level of drug metabolites—the excreted byproduct of metabolizing a given substance—in municipal wastewater. Wastewater testing has been shown to be an effective indicator for nearly two decades, and it has been used to compare drug consumption rates in major European cities.[ 42 ] Australia has conducted a nationwide drug wastewater surveillance program since 2016, and as of 2021 was monitoring the consumption of 12 substances across 58 waste-treatment sites covering 57% of the population.[ 43 ] It is in many ways preferable to surveys, as it can be tracked day-to-day and avoids social desirability bias—people can lie, but pee can’t.
The information derived from wastewater surveillance can be used for a variety of purposes. It can, according to one review of the approach, “monitor temporal and spatial trends in drug use at different scales, provide updated estimates of drug use, and identify changing habits and the use of new substances.”[ 44 ] Because it can tell authorities what drugs are being used, and where, in real time, it allows the targeting of relevant resources—law enforcement, social services, treatment, etc.—both to the areas where they are most needed and with the tools they most need (naloxone, e.g., is more useful in the case of a surging opioid OD than a methamphetamine OD). The great boon of wastewater surveillance is that it allows real-time response to trends, precisely what is missing from many locales’ toolboxes.
Wastewater surveillance is particularly attractive because it is universally identified as cost-effective method of gathering information compared to more conventional approaches.[ 45 ] The European Monitoring Center for Drugs and Drugs Addiction estimates the cost of analysis as between €100 and €200 (roughly $105 to $210) per sample, where a sample represents many, many people—the number of people contributing to a waste treatment site could be tens of thousands or more.[ 46 ] Comparisons from other wastewater-based epidemiology approaches are instructive: wastewater monitoring of alcohol, nicotine, and caffeine consumption reduced costs from roughly $127 per person (the cost of a conventional questionnaire) to $0.58 per person, a 200-fold reduction.[ 47 ] A World Bank analysis pegs the cost of wastewater surveillance for Covid to between $0.20 and $3 per person per year.[ 48 ]
The U.S. has lagged far behind in this area, but some cities are now using wastewater testing to track the Covid-19 pandemic, working with the CDC under the auspices of the National Wastewater Surveillance System.[ 49 ] Wastewater testing allows cities like Boston and Minneapolis to project a rise in Covid cases before they impact hospitals;[ 50 ] wastewater testing for drugs can produce similar ahead-of-the-curve information. In fact, the infrastructure already in place for Covid-19 testing should lower the start-up cost of adding wastewater testing to the fight against opioids.
Supervised Consumption Sites
A number of major cities across the U.S.—including New York, Seattle, and Philadelphia—have opened or attempted to open “supervised consumption sites” (SCSs) within their jurisdictions.[ 51 ] Such venues, sometimes also called “safe consumption sites” or “overdose prevention centers,” offer a place for people to use drugs under supervision—usually by medical professionals—who can administer oxygen, naloxone, or other lifesaving support as necessary. Although officially sanctioned SCSs are new to the U.S., they have a long history in other countries, with over 120 sites operating in Australia, Canada, and across Europe. Unsanctioned SCSs have operated in the U.S. since at least 2014.[ 52 ]
Proponents of SCSs argue that they reduce drug-related harms for existing users, both because they make it easier for people using drugs to access overdose-reversing medication and because they can connect those same people to sterile use equipment (needles, pipes, etc.) and treatment. Critics, meanwhile, argue that they normalize drug use, may only delay overdose deaths (since most SCS clients continue to also use outside of SCSs) without necessarily leading to cessation of drug use, all while contributing to crime, disorder, and drug consumption in the broader community. They also note that SCSs supervise only a small share of use sessions—about 5% of use sessions in Vancouver in the early 2000s, for example.[ 53 ] That small share of use sessions is likely concentrated among the most risk-avoidant (and therefore least overdose-prone) users, mitigating the claimed benefits.
The total evidence, in either direction, is best characterized as both lacking and somewhat mixed. Research focuses disproportionately on just two SCSs (one in Vancouver and one in Sydney), which may not be representative. One RAND Corporation review of the literature notes that most of the studies on SCSs—especially those which underpin estimates of their cost-effectiveness—“ merely report associations that do not permit causal inference.” They offer, for example, evidence that safe drug use—sanitary practices, for example—is positively correlated with frequency of visits to Vancouver’s SCSs. This association could mean that SCS attendance drives safer use, but it could also mean that those who are prone to safer use anyway are also more likely to go to SCSs.[ 54 ] Such problems limit what we can conclude about SCSs’ effects in general.
Several studies do offer quasi-experimental measures of the effects of SCSs. Two studies based on the SCS established in Sydney, Australia, find that it reduced opioid-related calls for ambulance service relative to the rest of New South Wales but not a reduction in actual overdose deaths.[ 55 ] Another, based on Vancouver, identified a reduction in overdose mortality in the half kilometer around the SCS relative to the rest of the city.[ 56 ] The causal literature also finds no adverse effects on crime and few adverse effects except possibly on public disorder.[ 57 ]
There are issues, however, about which the literature does not speak. It is particularly hard to isolate the general effect of SCSs on the intensity and extent of drug use. Use at SCSs may delay, rather than accelerate, transition to treatment, increasing the cumulative lifetime risk of overdose death outside of the facility.[ 58 ] And tacit social sanction of drug use, even in the name of harm reduction, may shift potential users’ willingness to start using at the margin. There has also not been much attention in the literature to a SCS’s possible effects on neighbors, including effects on their sense of safety or property values.
These concerns are speculative, of course. But negative social effects from SCSs have been documented. A 2020 review by the government of Alberta found that the seven SCSs the province had opened since 2018 were associated with an increase in drug OD deaths, drug-involved aggressive behavior, crime, and debris in their immediate vicinity. The committee responsible for the review noted that, “Except for Edmonton, stakeholder feedback predominantly suggested that the SCSs have had a negative social and economic impact on the community. In Edmonton, however, there were reports that stakeholders felt intimidated and were prevented from expressing their true sentiments and opinions about these sites out of fear of retribution from site supporters.”[ 59 ]
SCSs are also probably illegal under the “Crack House Statute” of the federal Anti-Drug Abuse Act (ADAA) of 1986, which makes it unlawful to “knowingly open, lease, rent, use, or maintain any place, whether permanently or temporarily, for the purpose of manufacturing, distributing, or using any controlled substance.”[ 60 ] Advocates argue that that prohibition does not apply when a “third-party visitor” acts with criminal intent, and that the original intent of the ADAA did not include the regulation of “public health facilities.”[ 61 ] But federal courts sided against Philadelphia’s SCS, which made that argument in its legal dispute with the Department of Justice.[ 62 ] The Biden administration has signaled that it may not interfere with more recent city experiments with SCSs, although such a stance is likely to change from administration to administration.[ 63 ]
Should these issues scare policymakers off from setting up SCSs? Bracketing the question of legality, not necessarily. The scale and urgency of the drug crisis may mean that radical policy solutions are the appropriate way forward. At the same time, there is much we do not know about the true impact of SCSs—they may have positive impacts, no impact, or negative impacts. And they may or may not be the best use of scarce dollars.
As ever, it is worth weighing costs against benefits. Most cost-benefit analyses focus on Vancouver’s InSite SCS, which cost between $2 and $3 million (Canadian) per year in 2007 dollars, including about $1.5 million for the supervised injection component of its services (i.e., not counting counseling, primary health care, or other services).[ 64 ] That amounts to an annual operating cost of between $2 and $3.1 million (U.S.) in today’s dollars, including about $1.5 million in the cost of providing supervised consumption services.65[ 65 ] Is this cost worth it? It depends on how one thinks about it. As the RAND report notes, “supervising all injections for someone who uses twice a day could cost approximately Can$5500–7300 per year. That might be in the same range as the cost of providing methadone for a year to a patient in the United States.” Whether a SCS or treatment is a better use of the marginal dollar is a matter of municipal priority.
If a municipality does opt to set up a SCS, it should first and foremost prioritize rigorous evaluation of its impact. That should include both quantitative metrics—overdose-related deaths and ER admissions, drug-associated and not-associated crime, even measures of disposed needles—and qualitative ones, including regular surveys of all relevant stakeholders, including neighbors. If individual people cannot be pseudo-randomly assigned to access the SCS, then policy evaluators should at least predesignate “treatment” and “control” areas of the city that are substantively similar on observable qualities and measure how the introduction of the SCS affects the aforementioned metrics.
In other words, policymakers should understand any foray into SCS not so much as a guarantee of success as an experiment. Experimentation may be warranted, but it should be regarded with the sober caution that experimental policymaking demands.
Drug Market Interventions
Much of drug control policy works either by reducing demand—discouraging people from initiating drug use or helping them desist—or by reducing the harms of drug use. Supply-side approaches are the province of law enforcement: the interdiction of drugs and the cash it generates, and the arrest and incarceration of those who benefit, from street-level dealers up to kingpins.
A longstanding question in drug policy is how, or if, these policies can be effective. On the one hand, it is likely that policing can reduce the criminal behavior incidental to and often overlapping with drug use or sales. But it’s less clear how effective law enforcement is at controlling supply. Arresting low-level dealers or sweeping up even tons of drugs is just a drop in the bucket of the massive international drug market. The rise of synthetic drugs likely exacerbates this problem because the dramatic cost-savings they have brought makes it harder for supply reduction to drive up the price and thus reduce use.[ 66 ] This is a particular challenge for local administrators, who lack the reach or capacity to bring down international drug smuggling rings, a task usually reserved to the DEA. Local cops can often feel like arresting drug dealers and users is little more than an exercise in catch-and-release.[ 67 ]
In recent years, however, there has been promising evidence in favor of another supply-side approach, the “Drug Market Intervention” or “Initiative” (DMI). The approach applies policing methods of “focused deterrence” or “pulling levers,” which entail targeting the small number of offenders who drive the majority of crime in a given area.[ 68 ] DMIs target areas with high concentrations of active drug sales, the “drug markets” that crop up in many American cities and are a significant contributor to OD deaths, at least as measured by spatial concentration.[ 69 ] During a DMI, a police department will identify drug dealers in a target area, build cases against them, then execute a “call in,” in which offenders are rounded up and notified that they can either get out of the drug game—with the support of the city’s arrayed social services—or go to prison.[ 70 ] Doing so creates a clear and powerful disincentive for offenders to continue to deal, a deterrent far more certain than the often random arrests under the conventional approach.
The earliest DMI was set up in High Point, North Carolina, in 2004. It initially targeted a large drug market in the city’s West End neighborhood, then expanded to three other drug markets. During implementation, “overt drug activity … was almost entirely eliminated,” with no displacement of drug activity to other areas. Violent crime also fell, driven by the areas where the drug markets were.[ 71 ]
Since then, a number of other jurisdictions have created their own DMIs, with varying levels of success. Successful implementations have been identified in Rockford, Illinois, and Nashville, Tennessee.[ 72 ] But a DMI in Peoria, Illinois, did not have a significant impact.[ 73 ] And in a seven-site study of implementation, just four had any actual call-in meetings, and only one successfully reduced crime overall.[ 74 ]
This last finding, the authors note, reflects the challenges of following the original High Point model successfully: “The DMI program was challenging for sites to implement and resulted in significant reductions in crime in the site with the implementation fidelity that was highest and most similar to the original site.”[ 75 ] Indeed, implementing a DMI is more complicated than doing standard drug busts. They entail coordination across government, including the police department, state/district/county attorneys, social services providers, mayors or other executive’s offices, and, ideally, civil society actors like nonprofits and churches. They can also be costly: a study of DMIs implemented in two cities suggested they cost police departments on the order of $100,000 to $150,000 per intervention.[ 76 ]
That said, the cost and risk of failure should be balanced against current approaches to local-level interdiction, which are often of limited efficacy. Particularly given the scale of the crisis, any jurisdiction willing to consider radical harm-reduction interventions (e.g., SCSs) should also be willing to consider a DMI.
Thanks in large part to miraculous medical innovation, Covid-19 is now far less a threat to life today than it was two years ago. But as one epidemic recedes, another continues. Unlike Covid, there is no sign of the drug crisis abating: it is likely that, at current rates, drugs will eventually kill more people cumulatively than Covid did in its first three years. There does not appear to be any vaccine or any virus-destroying medication coming.
But while the current scale of death is unprecedented, there are steps that government, particularly local government, can take to stem the tide. Naloxone distribution, treatment capacity, and drug courts are all effective tools for reducing death and minimizing the harms of drug use. Wastewater surveillance, long an underappreciated tool in the U.S., is primed for expansion thanks to its use during the pandemic. More experimental approaches like SCSs or DMIs are also worth investigating, assuming local leaders do so with an eye to their harms, benefits, and cost.
The drug crisis is not the rural problem it was 10 years ago. It is now, more so than ever, everyone’s battle. Local leaders are on the front lines of this conflict—it is incumbent on them, therefore, to act.
About the Author
Charles Fain Lehman is a fellow at the Manhattan Institute for Policy Research, working primarily on the Policing and Public Safety Initiative, and a contributing editor of City Journal . He has addressed public safety policy before the House of Representatives, at universities including Cornell and Carnegie Mellon, and in the Wall Street Journal , Dallas Morning News , New York Post , National Review , and elsewhere. He was previously a staff writer with the Washington Free Beacon , where he covered domestic policy from a data-driven perspective. Lehman graduated from Yale in 2016 with a BA in history.
Acknowledgments
The Manhattan Institute thanks the Klinsky Leadership Series for its support in the publication of this paper.
Please see Endnotes in PDF
Are you interested in supporting the Manhattan Institute’s public-interest research and journalism? As a 501(c)(3) nonprofit, donations in support of MI and its scholars’ work are fully tax-deductible as provided by law (EIN #13-2912529).
Further Reading
- Terms of Use
- Privacy Policy
Copyright © 2024 Manhattan Institute for Policy Research, Inc. All rights reserved.
- Public Safety
- Publications
- Research Integrity
- Press & Media
EIN #13-2912529
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Pharmacol
Drug Shortage: Causes, Impact, and Mitigation Strategies
Sundus shukar.
1 Department of Pharmacy Administration and Clinical Pharmacy, School of Pharmacy, Xi’an Jiaotong University, Xi’an, China
2 Center for Drug Safety and Policy Research, Xian Jiaotong University, Xi’an, China
3 Shaanxi Centre for Health Reform and Development Research, Xi’an, China
4 Research Institute for Drug Safety and Monitoring, Institute of Pharmaceutical Science and Technology, China’s Western Technological Innovation Harbor, Xi’an, China
Fatima Zahoor
5 Department of Pharmacy, Quaid-i-Azam University, Islamabad, Pakistan
6 Yusra Institute of Pharmaceutical Sciences, Islamabad, Pakistan
Khezar Hayat
7 Institute of Pharmaceutical Sciences, University of Veterinary and Animal Sciences, Lahore, Pakistan

Ali Hassan Gillani
Sumaira omer, zaheer-ud-din babar.
8 Department of Pharmacy, School of Applied Sciences, University of Huddersfield, Huddersfield, United Kingdom
Caijun Yang
Róbert György Vida , University of Pécs, Hungary
Drug shortage is a global issue affecting low, middle, and high-income countries. Many countries have developed various strategies to overcome the problem, while the problem is accelerating, affecting the whole world. All types of drugs, such as essential life-saving drugs, oncology medicines, antimicrobial drugs, analgesics, opioids, cardiovascular drugs, radiopharmaceutical, and parenteral products, are liable to the shortage. Among all pharmaceutical dosage forms, sterile injectable products have a higher risk of shortage than other forms. The causes of shortage are multifactorial, including supply issues, demand issues, and regulatory issues. Supply issues consist of manufacturing problems, unavailability of raw materials, logistic problems, and business problems. In contrast, demand issues include just-in-time inventory, higher demand for a product, seasonal demand, and unpredictable demand. For regulatory issues, one important factor is the lack of a unified definition of drug shortage. Drug shortage affects all stakeholders from economic, clinical, and humanistic aspects. WHO established global mitigation strategies from four levels to overcome drug shortages globally. It includes a workaround to tackle the current shortage, operational improvements to reduce the shortage risk and achieve early warning, changes in governmental policies, and education and training of all health professionals about managing shortages.
Introduction
Medicines are vital elements to health-care, and access to medicines is a fundamental human right ( Hogerzeil, 2006 ). The World Health Organization (WHO) defines essential medicines that “satisfy the population’s priority health care needs” ( De Weerdt et al., 2015 ). However, the prevailing drug shortage problems bring significant challenges to the health care system.
The shortage of drugs remained a problem in history up to the present date. The first time of drug scarcity in the record could be traced back to the insulin shortage in the early 1920s. Since then, the drug shortage is more common worldwide ( Yang et al., 2016 ; Walker et al., 2017 ; Unguru et al., 2019 ; Zwaida et al., 2019 ). In 2012, Gray and Manasse found that 21 countries were affected by drug shortages ( Russell et al., 2017 ), and the recent data of the University of Utah Drug Information Services reported 129 medicine shortages in the United States in 2020, as shown in Figure 1 ( American Society of Health System Pharmacists, 2020 , june 30).

Number of drugs in shortage per year reported by University of Utah Drug Information Services (UUDIS) ( American Society of Health System Pharmacists, 2020 , June 30).
Drug shortage has prevailed throughout the globe affecting high, middle, and low-income countries. In high-income countries, the drug shortage has been in excessive focus compared to other regions. The causes include manufacturing problems, business decisions, raw material unavailability, and regulatory issues ( Ventola, 2011 ). Many agencies, associations, and governments have developed different policies, programs, research studies, and guidelines to address this event ( Ferrario et al., 2017 ; Bochenek et al., 2018 ). However, drug shortage still causes severe health and economic crises ( Dill and Ahn, 2014 ; Dave et al., 2018 ). Unlike high-income countries, low-middle income countries (LMICs) have several new causes for drug shortage, including licensing of manufacturers/products, shortage of raw material for a local manufacturer, drug smuggling, and lodging tax government policies ( Khan, 2019 ). Research studies in these countries found a need for government strategies to build research information platforms ( Yang et al., 2016 ) to mitigate this issue ( Walker et al., 2017 ; Atif et al., 2019 ). Low-income countries have few research studies and lack policies to deal with this event. A few studies reported a stock-out of essential medicines in Malawi, Egypt, and Uganda ( Alsirafy and Farag, 2016 ; Khuluza and Heide, 2017 ). Literature also reported shortages of TB drugs, Ketamine, and drugs against HIV in African countries ( Seunanden and Day, 2013 ; Gray, 2014 ; Addo et al., 2018 ; Wall and Bangalee, 2019 ).
Drug shortages have diverse impacts on different stakeholders, especially patients. Patients are facing issues such as increased patient monitoring, suboptimal treatment through the use of alternative drugs, delayed care, being transferred to other institutions, increased length of hospitalization, readmission due to adverse events/treatment failure/relapse, associated care cancellations (surgery: bone marrow transplantation), or even death ( Mclaughlin et al., 2013 ; Rider et al., 2013 ; Souliotis et al., 2014 ; Blaine et al., 2016 ; Yang et al., 2016 ; Alruthia et al., 2017 ). Irrespective of the nature of the cause, the effects of the drug shortage are so endless that most of the professionals in health institutions are affected and well aware of its long-lasting drastic impact, reported by the survey performed by the European Association of Hospital Pharmacists (EAHP) among 27 countries ( Dill and Ahn, 2014 ; Tan et al., 2016 ; Haider et al., 2019 ; Phuong et al., 2019 ).
Different countries have developed various strategies to address the drug shortage. These strategies vary depending upon the financial condition, the health system strength, and research studies, such as increased reporting systems, changes in policies, drug shortage platforms, and accelerated drug approval ( Thoma et al., 2014 ; Yang et al., 2016 ). Some authorities evaluate drug shortages and deliver guidelines directly to health stakeholders ( Ferrario et al., 2017 ; Bochenek et al., 2018 ), while some hospitals purchase extra inventory as a buffer stock to prevent shortages ( Fox et al., 2014 ). Some regulatory authorities establish platforms for tracking and reporting shortages ( Quilty, 2014 ), and some countries are trying to strengthen their food and drug institutions ( Alruthia et al., 2018 ; ASHP and Healthcare, September 30, 2020 ). As reported by the FDA from 117 (2012) to 23 (2016), the decrease in drug shortage showed that the US’s approaches have worked to some degree. However, the issue is still playing with the healthcare system and patients, as seen with 98 (2020) drug shortages ( ASHP and Healthcare, 30/09/2020 ; Food, 2018 ; Fox and McLaughlin, 2018 ; Phuong et al., 2019 ). Data from low and middle-income countries is not enough to compare them with high-income countries. Similarly, the US has more data in comparison ( Schwartzberg et al., 2017 ).
The drug shortage problem has severe aggressive impacts on the health care system and public health. This review aims to evaluate the current drug shortage situation in high, middle, and low-income countries and summarize its causes, impacts, and mitigation strategies that the world can implement to overcome.
Definition of Drug Shortage
Lack of standardized definition.
There is a lack of a standardized definition of drug shortage globally. The definition varies from one regulatory authority to another. Some authorities define the drug shortage from the supply side, and some define it from the demand side. Some authorities define it according to their level in the drug supply chain (whether it’s low supply or increased demand), and some define it concerning the timeframe or duration, for example, inability to dispense to a patient in a specific time ( Videau et al., 2019a ). A study in the EU reported 26 unique definitions 2), and WHO found 56 definitions worldwide. Three possible reasons could contribute to the above event. First, different authorities representing various stakeholders define drug shortages according to different criteria. Second, there is a lack of high-quality scientific research on drug shortage to provide a widely accepted definition ( Kaakeh et al., 2011 ; Klobuchar, 2011 ; Bochenek et al., 2018 ). Third, a lack of transparent quantitative data also impedes a global definition of shortage ( Bogaert et al., 2015 ; Meloni et al., 2017 ). The standard global definition is needed because different definitions used by different countries, which define medicine shortages at different scales, make it impossible to estimate and analyze medicine shortages at the international level ( Bochenek et al., 2018 ).
Fortunately, the WHO and the EU are working on this problem. In 2016, WHO convened an informal consultation of experts to develop technical definitions of shortages and stock-outs of medicines and vaccines. In the meeting, they analyzed those 56 definitions used for drug shortages. Terms were mapped to different supply chain areas, from manufacturing to dispensing to patients, and then the mapped terms were grouped according to whether they were related to supply or demand. Finally, two draft definitions, one from the supply-side and the other from the demand-side, were developed by consensus and some additional notes for future refinement of the drugs shortage definition ( Organization, 2017 ). On the supply-side, a shortage occurs “when the supply of medicines, health products, and vaccines identified as essential by the health system is considered to be insufficient to meet public health and patient needs.” While on the demand-side, a shortage occurs “when demand exceeds supply at any point in the supply chain and may ultimately create a stock-out at the point of appropriate service delivery to the patient if the cause of the shortage cannot be resolved promptly relative to the clinical needs of the patient.” Usually, shortages on the demand-side may not be found shortages on the supply-side, while the supply-side shortage would ultimately cause a shortage on the demand-side. And in 2019, the EMA and HMA joint task force released the first harmonized “shortage” definition for all the EU countries, stated as “a shortage of a medicinal product for human and veterinary use occurs when supply does not meet demand at a national level” ( Musazzi et al., 2020 ). Comparatively, the EU’s definition of shortage makes the international comparison feasible. While the two definitions proposed by WHO gives the stakeholders a standard from the demand or supply-side to define and manage their shortages.
Widely Used Definitions
There are several definitions widely used by researchers, including definitions given by the University of Utah Drug Information Service (UUDIS), the American Society of Health-System Pharmacists (ASHP) ( Fox et al., 2014 ; Phuong et al., 2019 ), the United States Food and Drug ( Administration US FDA, 2020 ), the Health Canada ( Dill and Ahn, 2014 ), the International Society of Pharmaceutical Engineering (ISPE), the European Federation of Pharmaceutical Industries and Associations (EFPIA) ( Fox and Tyler, 2013 ) and the International Pharmaceutical Federation (FIP).
University of Utah Drug Information Services (UUDIS) and American Society of Hospital Pharmacists (ASHP) define drug shortage as “a supply issue that affects how the pharmacy prepares or dispenses a drug product or influences patient care when prescribers must use an alternate agent” ( Fox et al., 2014 ; Phuong et al., 2019 ). The United States FDA has given three definitions. The first one defines the medicine shortage from the supply side as “a period of time when the demand or projected demand for drug exceeds the supply of drug” ( Phuong et al., 2019 ), and the second one defines it from the demand side as “a shortage will occur when demands exceeds supply at any point in the supply chain may ultimately create a “stock-out” at the point of appropriate service delivery to the patient if the cause of shortage cannot be resolved in a timely manner relative to the clinical needs of the patients” ( Acosta et al., 2019 ). The third one defines drug shortage as “a situation in which the total supply of all clinically interchangeable versions of an FDA regulated drug product is inadequate to meet the projected demand at the user level” ( Schwartzberg et al., 2017 ). Health Canada describes a drug shortage as “when a manufacturer/importer anticipates that they cannot supply a drug to meet projected demand” ( Dill and Ahn, 2014 ). ISPE defines drug shortage as “a situation in which total supply of an approved medicine is inadequate to meet the current projected demand at the user level.” EFPIA defines medication shortage as “a crisis situation caused by any ability of any Market Authorization Holder (MAH) to supply a medicine with a specific API to market over an extended period of time resulting in the unavailability of this medication for patients” ( Fox et al., 2014 ). The International Pharmaceutical Federation (FIP) has defined medicines shortages as “A drug supply issue requiring a change. It impacts patient care and requires the use of alternative agents” (FIP), September 14, 2020).
Moreover, the low and middle-income countries have the absence of an official definition. Middle-income countries like Iran ( Setayesh and Mackey, 2016 ), Iraq ( Acosta et al., 2019 ), Jardon ( Zu’bi and Abdallah, 2016 ), Egypt ( Abdelrahman et al., 2016 ), China ( Acosta et al., 2019 ) used definitions of United States FDA, ASHP, and FIP in their research studies. Similarly, low-income countries like Pakistan and Kenya do not have their official definition ( Fatima and Khaliq, 2017 ; Atif et al., 2019 ). These definitions are widely used but vary from each other based on some parameters, give different reporting criteria, and do not provide the exact estimation of drug shortage ( Bochenek et al., 2018 ). It is evident from the different number of products reported as shortages by the FDA and ASHP simultaneously, due to different reporting systems’ characteristics and different definitions ( Alsheikh et al., 2016 ).
Drugs Reported in Shortage
Nearly all types of drugs have been reported in shortage, including antibiotics (A07AA/D01AA/G01AA/J02AA/S01AA), antiretroviral drugs (J05AR), anti-protozoal (P01), antineoplastic agents (L01), cardiovascular medicines (C), analgesics (N02), etc. Different countries or areas encounter different drugs in shortage depending upon health conditions ( Mazer-Amirshahi et al., 2014 ; Rinaldi et al., 2017 ). However, essential medicines ( Hedman, 2016 ) and emergency medicines ( Dill and Ahn, 2014 ; Mazer-Amirshahi et al., 2014 ; Alsirafy and Farag, 2016 ; Fox and McLaughlin, 2018 ; Benge and Burka, 2019 ) are more liable to shortage than other medicines. In high economic countries, research studies found different classes of drugs in short supply. Still, too few studies in low-middle income and low-income countries are found to depict the complete picture; only some research studies focus on the affordability/availability and shortage of some essential medicines ( Phuong et al., 2019 ). Almost all classes of medicines were in short supply in high-income countries. Antimicrobial agents are the most affected class by drug shortage ( Mazer-Amirshahi et al., 2017 ), along with oncology drugs (both chemotherapeutic (D06B/D06C/D06BX) and non-chemotherapeutic drugs) ( Woodcock and Wosinska, 2013 ; Costelloe et al., 2015 ). Benzathine Penicillin G (J01CE08) shortage occurred in the United States (2014), and the reason reported by ASHP was a delay in manufacturing ( Organization, 2016 ). A study in Iran found 73 cancer drugs in shortage, covering most areas ( Setayesh and Mackey, 2016 ). Many oncology drugs were reported in shortage in the US, for example, Mechlorethamine, Leucovorin (L01BA), Daunorubicin (L01DB02), PEGylated liposomal Doxorubicin (L01DB01), etc. ( Phuong et al., 2019 ). In Canada, the Sandoz crisis (2011) started with slow production, ultimately to the plant’s shut to meet United States FDA standards. It led to the shortage of morphine (N02AA01) used for patients at the end stage of their lives, and Ondansetron is used to relieve nausea during chemotherapy ( Videau et al., 2019a ). Cardiovascular drugs like Labetalol (C07A G01) and Metoprolol (C07AB02), Methyldopa (C02AB), and pindolol (C07AA03) are found in the United States FDA drug shortage list ( Administration UF, 2020 ). Adrenaline has repeatedly been reported in short supply by Therapeutic Goods Administration Australia (2014, 2020) caused by commercial changes and unexpectedly increased demand-effected critical patients ( Organization, 2016 ). Shortages of analgesics were also reported, such as Salsalate 500 mg (N02BA06) drug in the United States ( Dave et al., 2018 ). Currently, the United States FDA shortage drug list still includes Ketoprefen (M01AE03) ( Administration USF.A.D, 2020 ). A study done in Canada in 2017 on the impacts of Clobazam (N05BA09) (benzodiazepine) shortages on patients with epilepsy found that patients complained about out-of-pocket cost ( Phuong et al., 2019 ). The most affected drugs in the United States in 2016 were antibiotics, followed by electrolytes, chemotherapy medicines, cardiovascular drugs, and CNS agents. But in 2020, analgesics, sedatives, paralytics were short due to their increased demand in COVID-19. Moreover, cardiovascular and CNS agents in injectables were also short ( Pharmacists, 2020 ). On the other hand, a study of EU in 2014 found that CNS drugs were most short, followed by anti-infective drugs, cardiovascular drugs, antineoplastic/immunomodulatory agents, and GIT drugs ( Pauwels et al., 2014 ), but the EAHP survey in 2019 found that antimicrobial agents were on the top with oncology medicines second, followed by anaesthetic agents The shortage of oncology medicines increased in comparison to the data from 2018 EAHP survey ( Miljković et al., 2020a ).
In middle-income and low-income countries, literature found shortages of essential medicines. Stock-out of antiretroviral drugs (ART) occurred many times in African countries ( Meloni et al., 2017 ). Besides, Deslanoside (C01AA07), Digoxin (C01AA05), Enalapril (C09AA02), Adrenaline, Noradrenaline, Isosorbide dinitrate (C01DA08), and Nifedipine (C08CA05) were reported in shortage in China ( Yang et al., 2016 ). The shortage of antimalarial drugs was seen in many low and middle-income countries. Acute shortage of antimalarial drugs (Artemether (P01BE02)/Lumefantrine (P01BF01) was found in Kenya, Sub-Saharan Africa, and Uganda due to the delayed procurement process which led to an increased mortality rate ( Malik et al., 2013 ). Shortage of Chloroquine and Sulphadoxine/Pyrimethamine (Fansidar) was also found in the public and private sector of Pakistan, creating a gap in effective malaria control ( Malik et al., 2013 ). Shortage of Chloroquine (P01BA01) and Hydroxychloroquine (P01BA02) was found during the COVID-19 pandemic in many countries due to increased demand ( Mazer-Amirshahi et al., 2020 ). In the surge of the COVID-19 pandemic, a shortage of Sertraline (N06AB06) and Midazolam (N05CD08) occurred due to the increased demand for antidepressant drugs (N06A/N06CA) to manage stress ( Administration USF.A.D, 2020 ). In low-income countries, literature cited medicines used for TB, Malaria, and HIV due to the increased incidence of these diseases and the unavailability of essential drugs rather than drug shortages or stock-out. Table 1 shows the medicines affected by shortages in different countries ( Elbagir et al., 1995 ; Kangwana et al., 2009 ; Tren et al., 2009 ; Ballinger, 2010 ; Ventola, 2011 ; Griffith et al., 2012 ; Liang and Mackey, 2012 ; Malik et al., 2013 ; Quilty, 2014 ; Ricci et al., 2016 ; Donohue and Angus, 2017 ; Gross et al., 2017 ; Hsueh et al., 2017 ; Meloni et al., 2017 ; Tan et al., 2017 ; Vail et al., 2017 ; Banerjee et al., 2018 ; Dave et al., 2018 ; Gundlapalli et al., 2018 ; Holcombe et al., 2018 ; Said et al., 2018 ; Benge and Burka, 2019 ; Visage et al., 2019 ; Yellapu et al., 2019 ; Benhabib et al., 2020 ; Choo and Rajkumar, 2020 ; Clark et al., 2020 ; Honda et al., 2020 ; Siow et al., 2020 ; Sun et al., 2020 ; Mclaughlin et al., 2017 ; Dave et al., 2018 ).
Medicines involved in shortage.
Causes of Drug Shortage
There are various reasons for drug shortages, depending upon the type of drug ( Mazer-Amirshahi et al., 2014 ). Overall, drug shortage causes can be classified as supply issues, demand issues, or regulatory issues, as shown in Figure 2 . The causes of drug shortages are multifactorial. For example, manufacturing problems, financial pressures, shortage of raw materials, and just in time inventory are found as essential causes of medicine shortages in developed countries of the EU, United States, Saudi Arabia, and developing countries like Pakistan, Fiji ( Malik et al., 2013 ; Hedman, 2016 ; Zu’bi and Abdallah, 2016 ; Schwartzberg et al., 2017 ; Walker et al., 2017 ; Jenzer et al., 2019 ).

Causes of drug shortages.
According to the UUDIS, the quality delays and capacity issues were most dominant in the United States, in 2012 followed by quality manufacturing issues and discontinuation ( Figure 3 ) ( Dill and Ahn, 2014 ), whereas a more significant percentage of reasons was unknown, in 2020, followed by business issues and supply/demand issues ( Figure 4 ) ( Pharmacists, 2020 ). In addition, the 2019 EAHP survey found that the global shortage of APIs, manufacturing problems, and supply chain issues dominated most ( Miljković et al., 2020a ).

Reasons of drugs in shortages in 2012 reported by University of Utah Drug Information Services (UUDIS) ( Dill and Ahn, 2014 ).

Reasons of drugs in shortages in 2020 reported by University of Utah Drug Information Services (UUDIS) ( Pharmacists, 2020 ).

Mitigation strategies.
Supply Issues
Supply issues mean manufacturers are unwilling or unable to produce enough medicines to satisfy the demand. It can be classified into manufacturing problems, unavailability of raw materials, business reasons (economic reasons like low-profit margin, low market size, cost raise of raw materials, capacity constraints), and logistic problems (supply chain issues) ( Dill and Ahn, 2014 ; Bogaert et al., 2015 ; Organization, 2015 ; Alsheikh et al., 2016 ; Fox and Tyler, 2017 ; Walker et al., 2017 ; Alruthia et al., 2018 ; Fox and McLaughlin, 2018 ; Pharmacists, 2018 ; Videau et al., 2019b ; Phuong et al., 2019 ). In high-income countries, these causes have been controlled to some extent, but in the low and middle-income countries, financial burden affects manufacturing quality and capability, medicines availability, affordability, and drug supply chain quantification ( Malik et al., 2013 ; Walker et al., 2017 ).
Manufacturing Issues
The manufacturing issues include quality problems and competing priorities. The EMA is associated mainly with medicine shortages due to manufacturing issues ( Hedman, 2016 ; Schwartzberg et al., 2017 ). Studies done in Finland, Saudi Arabia, Canada, and the EU mentioned manufacturing issues, the most promising ones ( Alsheikh et al., 2016 ; Heiskanen et al., 2017 ; Unit, 2017 ; Videau et al., 2019b ). Middle-income countries like Brazil and Venezuela cited shortages of injectable products with disregarded quality due to decreased incidence of some diseases and the availability of other valued alternatives ( Acosta et al., 2019 ). Whereas low-income countries like Pakistan reported manufacturing issues due to lack of regulatory policies and financial pressure ( Malik et al., 2013 ; Fatima and Khaliq, 2017 ).
- 1) Quality problems
The quality problems are the most frequent reason for the drug shortage found during daily quality checks and inspections after manufacturing, even after being released to customers. The quality problems usually lead to voluntary recall when found after medicine dispatching in the market. Such issues occur due to microbial contamination (bacteria/fungi), endotoxin, tablet disintegration, particulate matter (glass, metal, fiber, foreign matter) in vials, precipitate formation, or unexpected reaction between products and containers. Good Manufacturing Practice (GMP) violation can also be classified as a quality issue, as those violations may cause quality defects, and ultimately shortages ( Dill and Ahn, 2014 ). In the United States, 67% of drug shortages were due to quality issues in 2012, and the trend was found the same in 2013 ( Gray and Manasse, 2012 ; Mazer-Amirshahi et al., 2014 ; Alsheikh et al., 2016 ). The United States FDA warned six renowned sterile product manufacturers for violating the current Good Manufacturing Practices in 2014 ( Mazer-Amirshahi et al., 2014 ).
- 2) Competing priorities
When a manufacturer can produce several products, these products compete for raw materials, manufacturing lines, and markets. Therefore, manufacturers have a lower motivation to invest or produce medicines with low profitability, such as generics and injectable products, which require a stricter quality environment for manufacturing compared with those medicines with higher profitability, as found for generic products in the United States ( Dave et al., 2018 ) and injectable products in Brazil ( Acosta et al., 2019 ).
Unavailability of Raw Material
Drug shortages may occur when there is a problem in the supply of raw materials. It could be a shortage of active pharmaceutical ingredients (API), excipients, or packaging materials ( Dill and Ahn, 2014 ). India and China are the important active pharmaceutical ingredient suppliers for almost all economic levels. Unavailability of raw materials could be due to political turmoil, armed conflicts, animal disease, trade disputes, environmental conditions, degradation during transport, or low plant yield as a source of material from the source country ( Ventola, 2011 ; Coustasse et al., 2020 ). In 1998, there were shortages of many drugs due to Hurricane George in Puerto Rico ( Gu et al., 2011 ; Rinaldi et al., 2017 ).
In the COVID-19 pandemic, shortages of active pharmaceutical ingredients (APIs), excipients, and drugs occurred worldwide. As a result, the countries (India, China, United States) the producers of APIs stopped supplying some APIs to other countries that led to the global shortage of many drugs. Moreover, many other challenges, including shortage of packing material, disrupted transport, delayed shipping, delayed customer clearance, restricted import-export of APIs and drugs throughout the world ( Ayati et al., 2020 ; Badreldin and Atallah, 2021 ). Moreover, in the COVID-19 pandemic, shortages of API were also found in the United States ( Coustasse et al., 2020 ). When a sole supplier provides the API and excipients of any product, any problem with the supplier may lead to a medicine shortage ( Ventola, 2011 ). Therefore, a product with at least three suppliers for materials is usually considered desirable ( Hedman, 2016 ). The unavailability of raw materials was an important reason for drug shortages in Saudi Arabia ( Alsheikh et al., 2016 ), Canada ( Videau et al., 2019b ), and Pakistan ( Atif et al., 2019 ).
Business Issues
Business issues are economic factors, including little profit margin, small market size, consolidation, absence of maintenance, and low procurement ability ( Dill and Ahn, 2014 ; Dranitsaris et al., 2017 ).
In high-income countries, drug shortages frequently occurred due to business issues. The low market price is the leading cause of generics shortages. Some manufacturers found it difficult to cope with a branded counterpart and upgrade their infrastructures to comply with GMP requirements. Such manufacturers maintained the expensive high-quality standard for their low-profit generic products and left the market, leading to the plant's closure, i.e., the shortage of generic injectable products in the United States ( Dill and Ahn, 2014 ). Even complying with GMP requirements is also costly for some generics manufacturers ( Alsheikh et al., 2016 ; Dave et al., 2018 ). The absence of industrial plants and other facilities maintenance leads to inefficiency, less production capability, and ultimately drug shortages. Sometimes, different companies combine their manufacturing plants for common drugs to minimize costs and gain significant benefits. Consolidation of manufacturers results in a reduction in the number of manufacturers ( Schweitzer, 2013 ). For a supply chain with only a few manufacturers, flexibility may become an important issue, and the risk of drug shortage will increase ( Dill and Ahn, 2014 ; Emmett, 2019 ). Drugs with small market size, e.g., orphan drugs, are vulnerable to the shortage as manufacturers rarely prefer manufacturing such drugs ( Mazer-Amirshahi et al., 2014 ). For example, GlaxoSmithKline pulled the Lymerix vaccine off the market as the demand decreased ( Gu et al., 2011 ). Studies in low and middle-income countries reported procurement processes as causes of shortages, e.g., Kenya, Fiji, Pakistan, and Sub-Saharan ( Malik et al., 2013 ; Walker et al., 2017 ). The drug procurement process needs a specific period, but poor coordination among the departments delayed the procedures, resulting in a shortage. In this situation, local drug purchasing at increased prices puts a financial burden. Still, a further delay of the procurement process beyond the bid validity period leads to increased costs for bidders at quoted rates, worsening the situation ( Herath et al., 2011 ). For example, the delayed procurement process was involved in the antimalarial drug stock-out in Kenya ( Malik et al., 2013 ).
Logistic Issues
Logistic issues, including transportation issues and drug supply chain management incompetency, are the causes of drug shortages. The transportation problem is usually due to horrible weather, bad traffic, and natural disasters ( Dill and Ahn, 2014 ; Mazer-Amirshahi et al., 2014 ). In addition, the United States FDA reported logistical issues as an important reason for the recovery of disruption ( Administration UF, 2020 ).
Demand Issues
Demand issues include just-in-time inventory and increased marketing (average growth demand, outbreaks ( Alsheikh et al., 2016 ), epidemic, and seasonal demand). It may be predictable or unpredictable. A well-established system can predict the shortage caused by just-in-time inventory, average demand growth, and seasonal demand; however, outbreaks, epidemics, and disasters are unpredictable ( Dill and Ahn, 2014 ; Fox and Tyler, 2017 ; Walker et al., 2017 ; Phuong et al., 2019 ). Moreover, in low and middle-income countries, irrational use of medicines, lack of patients’ education, and prescription adherence lead to medication wastage, compromised outcomes, and increased demand ( Walker et al., 2017) . Other causes include prescribing practices and unethical medicines promotion by pharmaceutical companies ( Malik et al., 2013 ).
Just-In-Time Inventory
Just-in-time (JIT) inventory system is a management stratagem that aligns fixed raw materials/drugs from suppliers directly with the currently scheduled requirement. In the circumstances of a low financial budget, stakeholders purchase a fixed quantity of stock for a fixed duration that fulfills only the current needs of the pharmacy/institution without any backup plan. It is a widespread strategy to run the system with minimum cost but with a greater risk of drug shortage because of no buffer stock reported in high-income countries ( Ventola, 2011 ; Alruthia et al., 2017 ; Emmett, 2019 ).
Increased Marketing
Increased marketing of a new product or an older one may be predictable or unpredictable. Predictable marketing increases the focus of professionals and the public towards a product. Unethical/uncontrolled marketing strategies are used chiefly in low-income countries where drug-related policies are rare ( Abdelrahman et al., 2016 ). A study performed in Pakistan found that pharmaceutical companies’ unethical marketing of Artemether/Lumefantrine resulted in stock-out of Sulphadoxine/Pyrimethamine (Fansidar) and Chloroquine ( Malik et al., 2013 ). Increased marketing of particular medicines for rare diseases with more incredible physicians’ benefits leads to a significant supply and demand gap ( Hedman, 2016 ).
An unpredictable increase in demand may occur due to an outbreak, natural disaster, fire, or other accident. In such a situation, drug shortage may occur because the lead time of manufacturing is longer for medicines, and sparing lines for manufacturing specific medicines is complex ( Dill and Ahn, 2014 ). For example, saline bags were in shortage in Hurricane Maria in Puerto Rico ( Emmett, 2019 ), and Tamiflu for pediatric use was in short supply in pandemic H1N1 in 2009 ( Gu et al., 2011 ). Such disasters, in return, could cease manufacturing ( Dill and Ahn, 2014 ).
The demands of some medicines depend upon seasons. For example, the demands of cough syrup, pediatric antipyretic syrup, antihistamines, and anti-asthmatic drugs increase in winter. Seasonal demand is often predictable, but it is still a risk factor for drug shortage. For example, Oseltamivir shortage occurred when seasonal influenza attacks ( Mazer-Amirshahi et al., 2014 ).
Tendering System
Tendering system caused drug shortages in the United States and EU. Awarding a drug tender to a single supplier would put it at high risk of shortage. Moreover, the low pricing of medicines through tendering compelled some manufacturers to leave the market, leading to the loss of competition and rising prices. The group procurement also caused drug shortages as it changed the purchasing pattern ( Dranitsaris et al., 2017 ).
Regulatory Causes
Drug regulatory authorities are accountable for effective drug regulation to safeguard drug quality, safety, efficacy, and appropriateness/accuracy of drug information accessible to the public. Still, their compromised roles lead to many problems, including drug shortage. Some of the regulatory issues found in low and middle-income countries are the inflexibility in regulatory processes, lack of policies, and unavailability of communication among stakeholders. These events also included the lack of implementation of essential drug lists that led to the disruption of supply chain management in multiple ways ( Malik et al., 2013 ). A study in Jordan found regulatory issues as one of the four causes of drug shortage ( Gu et al., 2011 ; Bogaert et al., 2015 ; Zu’bi and Abdallah, 2016 ). Many studies also mentioned unknown causes of drug shortage due to the unavailability of regulations from the government ( Bogaert et al., 2015 ).
The safety and efficacy standards implemented by United States FDA compelled the entry of new manufacturers into the market, marketed drugs, and some old drugs to review their qualifications, which will take a long time, ultimately leading to the shortage of many drugs ( Mazer-Amirshahi et al., 2014 ). Introduction of new guidelines, changes in drug use guidelines or therapy management guidelines from the government, such as new indications for a drug, changes in therapeutic character, can change supply and demand, resulting in a shortage. For example, changes in CDC guidelines in classifying children to the age range of 6–59 months resulted in a shortage of pediatric flu vaccines in 2006 provided by the solo manufacturer ( Ventola, 2011 ). United States and EU have introduced many advanced initiatives to optimize the drug supply chain. One of them is the Falsified Medicines Directive (FMD) by the EU to keep counterfeit and quality compromised medicines away from the drug supply chain. Though this policy effectively keeps fake medication away, the implementation process caused medicine shortages because the system needed time to improve the quality up to the mark ( Bouvy and Rotaru, 2021 ). The EU (European Union) implemented new GMP (Good Manufacturing Procedure) regulations in 2013 to control and ensure better quality. However, these new guidelines, especially the one related to purchasing and processing raw materials, may delay the production procedure and cause medicines shortages to a certain extent ( Academy, 2013 ).
Al Ruthia et al., in 2018 found that poor drug supply chain management was the main reason for drug shortage in large hospitals of Saudi Arabia (34). The absence of a uniform definition is one of the main issues from the regulatory side. It created gaps to judge the severity of the problem and diminished the mitigation strategies ( Kaakeh et al., 2011 ; Klobuchar, 2011 ).
Impact of Drug Shortage
The drug shortage affects all stakeholders, especially patients/consumers, in economic, clinical, or humanistic aspects ( Dill and Ahn, 2014 ; Phuong et al., 2019 ). In developed countries, due to policies, guidelines, associations, and platforms, the problem has been managed to some extent, so the level of impact is not so high but still alarming. It will remain until the management of this issue globally; for example, studies cited the out-of-pocket cost in the United States, Canada, Europe, Australia, and South Africa. On the other hand, most institutions in LMICs have their strategies, but the government introduces no policies to tackle the vast impacts ( Hayes et al., 2014 ; Pauwels et al., 2014 ; Perumal-Pillay and Suleman, 2017 ; Lukmanji et al., 2018 ; Phuong et al., 2019 ).
Economic Impacts
Drug shortages usually result in an extra cost or budget for different stakeholders, especially patients, at all economic levels. In high-income countries, the stakeholders are aware of drug shortages, and the suppliers have to manage unavailability of raw materials through additional operations. The retailers have to purchase a many short-supplied drugs with increased prices or purchase expensive alternative brands, start compounding or logistic modifications. The hospitals have to put extra costs to manage the shortage, such as purchasing costly brands, excess inventories, and awareness programs to deliver staff knowledge. Studies estimated $200 million in purchasing expensive alternatives (“Drug Shortage Cost United States Care Providers” 2011) accompanied by additional labor costs of $359 million (Kacik 2019) in United States hospitals due to drug shortage annually ( Fox and Tyler, 2013 ; Dill and Ahn, 2014 ; Fox et al., 2014 ; Mazer-Amirshahi et al., 2014 ; Costelloe et al., 2015 ; Hughes et al., 2015 ; Food and Administration, 2019 ; Phuong et al., 2019 ). On the other side, medicine price increases after a drug shortage, especially for lower-priced generics, medicines with a solo manufacturer, unapproved medicines, and orphan drugs ( Fox and Tyler, 2017 ; Dave et al., 2018 ). An increase in medicine price is also an illegal practice in the grey market that stocks up a large share of medicine in advance and provides them at a higher price to customers in short supply. For example, Cytarabine was in shortage for $12, but it was sold on the grey market with an increased price of $900 ( Gu et al., 2011 ). The out-of-the-pocket cost of patients increased as they have to purchase costly brands, expensive alternatives, costly compounded medicines, pay more for a prolonged duration of therapy, extended hospital stay, and compromised treatment, as cited in studies done in Canada, the United States, Europe, and Australia ( Phuong et al., 2019 ). In a study done on 1,650 oncology pharmacists in the United States in 2011, it was found that 93 participants agreed that the drug shortage resulted in altered treatment or delay in chemotherapy administration, whereas 85% of participants agreed that the shortage led to increasing cost of the regimen ( Dill and Ahn, 2014 ). Drug shortages also lead to online purchasing from illegitimate vendors that are difficult to differentiate for the consumers. In addition, such purchasing increased the financial burden for patients as they are available at increased prices than in pharmacies ( Jackson et al., 2012 ; Fittler et al., 2018 ; Koenraadt and van De Ven, 2018 ).
Very few studies have been done in low and middle-income countries, only reporting increased out-of-pocket expenses as the economic impact of drug shortages ( Fatima and Khaliq, 2017 ; Walker et al., 2017 ; Acosta et al., 2019 ). Management of medicines shortages depends strongly on the health care system with a well-managed drug supply chain and adopted health care model. The high-income countries have adopted the Beveridge Model (Spain, New Zealand, Cuba, Hong Kong), Bismarck Model (Germany France, Belgium, Netherlands, Latin America), and National Health Insurance Model (Canada, South Korea, Taiwan), where patients are relieved from the out-of-pocket costs. However, in the middle and low-income countries, the Out-of-Pocket Model (remote areas of China, India, Africa, and South America) is working, burdening the patients ( Kos, 2019 ).
Importation of medicines in the case of national shortage leads to severe economic impacts burdening the government. In the EU, the import/export criteria are not harmonized, and different countries have different policies to allow the import and export of medicines in shortage. The lack of harmony and the parallel import from EU or extra-EU countries may threaten the medicines’ availability in a country with a ripple effect. The uncontrolled movement of drugs could be worsened by this ripple effect, causing severe economic impacts ( Musazzi et al., 2020 ; Vida et al., 2016 ).
Clinical Impacts
Clinical outcomes of drug shortage have been reported in the majority of studies in developed countries. It included alterations in treatment, inferior treatment, prescription inaccuracies, dispensing errors, administration errors, delayed or denied treatment, prolonged hospitalization, adverse drug interactions, and even death reported by studies done in the United States, Saudi Arabia, Europe, Australia, Canada, United Kingdom ( Becker et al., 2013 ; Mclaughlin et al., 2013 ; Dill and Ahn, 2014 ; Fox et al., 2014 ; Alsheikh et al., 2016 ; Mclaughlin et al., 2017 ; Rinaldi et al., 2017 ; Schwartzberg et al., 2017 ; Walker et al., 2017 ; Dave et al., 2018 ; Phuong et al., 2019 ). A survey conducted in North Carolina, South Carolina, Georgia, and Florida reported that drug shortage caused a significant percentage of medication errors in patients leading to compromised health outcomes and increased patient burden creating an unsafe situation for both staff and patients (97). Alfuzosin replaced Tamsulosin which was in short supply, but Alfuzosin increases QT interval ( Hsia et al., 2015 ; Shaban et al., 2018 ). The shortage of antimicrobial drugs is critical as their shortages leading to delayed treatment, chronic infection, and other deadly outcomes ( Fox et al., 2014 ). In addition, some drugs in the grey market become substandard with time as stored in non-optimal conditions and lead to compromised health outcomes ( Fox et al., 2014 ; Zwaida et al., 2019 ).
The available online medicines may have quality problems. Many research studies found that online purchasing occurs in high-income countries like Malta, the United Kingdom, Netherlands, with an increased risk of counterfeit medicines and increased drug prices than local purchasing ( Jackson et al., 2012 ; Fittler et al., 2018 ; Koenraadt and van De Ven, 2018 ).
Drug shortages lead to inappropriate alternatives in prescription, compromised health, prolonged hospital stay, readmission, morbidity, and mortality in developing countries (Uganda, Fiji, Zambia, Nigeria, Egypt) ( Malik et al., 2013 ; Walker et al., 2017 ). Scientific studies have proven that the interrupted treatment due to the drug shortage for antiretroviral therapy (ART) led to substandard outcomes, accumulations of drug resistance mutations, and treatment failure ( Meloni et al., 2017 ). For some critical medicines, their shortage will result in the cancellation of surgery. For example, the shortage of protamine sulfate will lead to the cancellation of heart surgery. Surgery cancellation may worsen the disease, prolong hospital stay, and expose hospital-acquired infections ( Burki, 2017 ; Khan, 2019 ). More seriously, the shortage of some medicines may lead to higher mortality. Due to chemotherapeutic drug shortage, the mortality rate was high, but essential drugs, including antibiotics, Phytonadione, electrolyte solutions, analgesics, and opioids, were also involved ( Mazer-Amirshahi et al., 2014 ). Drug shortage also increased online purchasing of counterfeit products in middle-income countries ( Yin et al., 2016 ; Huang and Xu, 2017 ).
Humanistic Impacts
The consequences of treatment or disease on patient quality of life (QOL) are humanistic outcomes, e.g., patient satisfaction with treatment outcomes and hospital services.
Drug shortages resulted in varied humanistic impacts on patients, and health-care professionals noticed many types of research in developed countries ( Dill and Ahn, 2014 ) and developing countries. Studies in the United Kingdom, Canada, and the United States found that shortages usually give rise to patient complaints, frustration, anger, dissatisfaction, decreased adherence, and psychological effects. Patients also complain of traveling anxiety about other medicines, and face delayed surgery ( Schwartzberg et al., 2017 ; Dave et al., 2018 ; Phuong et al., 2019 ). The drug shortage situation makes physicians dissatisfied, stressed, exasperated, lost patients’ trust, even threatening them ( Hedman, 2016 ; Rinaldi et al., 2017 ; Walker et al., 2017 ). Physicians have to choose patients for receiving limited available drugs or are forced to select alternative therapy ( Russell et al., 2017 ). The situation becomes more critical for cancer patients ( Dill and Ahn, 2014 ; Hedlund et al., 2018 ).
A few studies in LIMCs reported that professionals face increased frustration, threat, violence, negative workplace situation. They have to put extra effort and time into managing the shortages. The patients lost trust in the hospitals and concern about alternates effects ( Walker et al., 2017 ; Phuong et al., 2019 ).
Mitigation Strategies
Drug shortages were studied well in the United States (South and North America), European Union, Oceania countries (Fiji, Australia). In contrast, few related studies were found in Asia (Saudi Arabia, Pakistan, China, Iran, Iraq, Jordan, and Israel) and Africa (Kenya, South Africa, Egypt, and Uganda). In the United States and European countries, extensive work has been done to implement policies for drug shortages mitigation, but there is an extensive research gap in the rest of the world and policies ( Acosta et al., 2019 ).
Different strategies are proposed in most of the high-income and some middle-income countries to cope with drug shortages. International and national organizations, including the World Health Organization (WHO), the International Pharmaceutical Federation (FIP), American Society of Health-System Pharmacist (ASHP), and the European Association of Hospital Pharmacists (EAHP), are involved a lot in taking initiatives, providing information and guidelines to mitigate the drug shortage situation as shown in Figure 3 ( Fda, 2013 ). Simultaneously, many approaches were proposed by the United States, European countries, Canada, Australia, China, etc., However, this problem is still on the ground and has been ignored in most low and middle-income countries, so there is a need for ever-growing, universal, and updated versions of the strategies to put the issue on the knee internationally.
In hospitals, the health care team uses following strategies managing drug shortages: 1) informing prescribers and recommending them alternative agents, 2) contacting other suppliers for the short medicine, 3) investigating supply restoration and planning, 4) substituting the prescribed medication and 5) updating the formulary. However, in the community pharmacies, community pharmacists and working staff use to manage the drug shortages by adopting strategies: 1) management of current shortages, 2) contacting the authorized supplier, 3) contacting other pharmacies, and 4) suggesting an alternative treatment to the patient ( Tan et al., 2016 ; Panic et al., 2020 ).
Management of Current Drug Shortage
- 1) Restrictions on the use of current stock. When there is limited stock of some medicine in a medical institution and no supply for an unknown period, the institution should limit the stock to specific patients. Some modelling methods or mechanisms can be used to give priority to patients, like the A4R framework. Such modelling methods prioritize patients with restorative therapy, pediatrics patients, cancer patients with no alternative available, patients in clinical trials, and patients on treatment regimens with authentic survival benefits ( Valgus et al., 2013 ). The strategy is crucial for the drugs with rarely marketed generics, anticancer drugs, and emergency drugs reported by health professionals of different Fiji institutions. It will also give time to staff to search for other alternatives ( Walker et al., 2017 ).
- 2) Use of products with minor defects. Products with minor defects like particulate matter, the viable substance, can be used after proper handling in case of shortage. The United States FDA has adopted the strategy, and they allowed the use of medicines with improper packaging, labelling defects, glass particles in an injectable (filter before use), and non-registered drugs after risk evaluation or proper handling to overcome the shortage ( Mazer-Amirshahi et al., 2014 ).
- 3) Increase of expiry date. When shortage occurs, drugs with near expiry dates can be used by extending the printed expiry date. For example, the United States FDA has used this strategy and extended the expiry date of coral snake antivenin, which was discontinued by the manufacturer ( Mazer-Amirshahi et al., 2014 ).
- 4) Redistribution of available stock. In the drug shortage situation, the manufacturer is responsible for the redistribution of currently available supply in a consistent manner among different areas or different institutions. Good communication and transparency among stakeholders with an adequate reporting system are required to achieve an efficient and equitable redistribution of the available quantity of shortage drugs ( Fox et al., 2014 ; Schwartzberg et al., 2017 ).
- 5) Development of the medical expert platform. A medical expert’s platform at the institution level will help handle the shortage of drugs proactively. The experts’ team should comprise pharmacists, physicians, and nurses. The platform should provide information about future shortages, manage current shortages, tackle and review alternative treatment, stock alternatives, and guidelines for restriction on medicine use through enhanced communication within the institution and other institutions ( Dill and Ahn, 2014 ; Rhodes et al., 2016 ). The United States has established a platform that conducts institutional level analyses and forecasts drug shortages ( Valgus et al., 2013 ; Modisakeng et al., 2020 ). Moreover, compounding low-risk medicines in severe shortage can be used when there is no other option, but high-risk medications could lead to severe adverse effects ( Lyon, 2012 ; Badreldin and Atallah, 2021 ). Similarly, a study found that off-label medicines for cancer patients could only use when there is no other option to treat them ( Valgus et al., 2013 ; Frattarelli et al., 2014 ).
- 6) Wastage management. In treating chronic conditions, especially oncology and pediatric patients, the dose is small (e.g., 12 mg/250 mg containing vial), so the leftover drug goes to waste due to short shelf life. To utilize the leftover drug in vials, United States hospitals’ oncology departments schedule their chemotherapy by clustering the patients on a specific date. This strategy is also adopted in the anaesthesia department through a double syringe technique ( Khan, 2019 ; Rowe et al., 2020 ). The benefits of this strategy are multidimensional, including overcoming the shortage, preventing drug wastage, and educating the caregivers about the shortage and its management ( Mazer-Amirshahi et al., 2014 ; Rowe et al., 2020 ).
Improvement in Operations
- 1) Increase communication among stakeholders. Communication among regulatory authorities and stakeholders at the national and international level is critical in administering drug shortages ( Costelloe et al., 2015 ; Schwartzberg et al., 2017 ; Walker et al., 2017 ). Good communications make proactive actions possible, which can manage the issue with minimum loss. It should be accompanied by harmonization and transparency among all stakeholders ( Fox and Tyler, 2003 ; Hedman, 2016 ; Nixon, 2021 ). Health Canada started Regulations Amending the Food and Drug Regulations, a reporting system for drug shortages, in 2015 that helped prevent and manage drug shortages by enhancing communication in the Canadian market ( Pauwels et al., 2015 ).
- 2) Drug shortage reporting and tracking system. A reporting and tracking system can report all related aspects of a drug shortage, including its period, drugs involved, frequency, duration, causes, impacts, managing strategies, and predict future shortages. Such a system should be present at every institution ( Giammona et al., 2020 ) as done by the Drug Shortage Program (DSP) developed by the FDA in 1990 ( Dill and Ahn, 2014 ; Said et al., 2018 ) and Texas Medical Board ( Mazer-Amirshahi et al., 2014 ). The databases and public websites are found in many middle and high-income countries of the European Union, the United States, and Western Asian countries. Still, they have no information about the impact of shortages and need improvements ( Acosta et al., 2019 ).
- 3) Increase in manufacturers for generics. Some medicines have a higher risk of shortage, such as injectables and generics. High costs caused by strict GMP protocols for injectable medicines and low prices for generics lead to a few manufacturers and a vulnerable supply chain. The incentive pricing mechanism is needed to spur more manufactures to produce these medicines ( Alspach, 2012 ; Panzitta et al., 2017 ).
- 4) Improved quality system. The quality of a drug is vital for its optimum efficacy, and it can compromise during its manufacturing, storage, transportation, and until the time of administration. The drug shortages rising through recalls due to compromised quality can be prevented through quality assurance and quality control departments ( Mazer-Amirshahi et al., 2014 ; Said et al., 2018 ). The regulatory authorities should implement strict protocols for manufacturers to comply with quality and reward manufacturers with a sound quality system to encourage more manufacturers to value the quality system ( Alspach, 2012 ; Panzitta et al., 2017 ).
- 5) Multiple suppliers. Manufacturers should contact more than one supplier for a single raw material ( Dill and Ahn, 2014 ). In evaluating new suppliers, the regulatory authorities also should pay special attention to those medicines currently with only one supplier ( Fox et al., 2014 ). And sometimes, speeding up the reviewing process is needed when there is a higher risk of shortage.
Changes in Governmental Policy
- 1) Changes in governmental policies and programs. The governments of many countries have introduced various organizations to manage drug shortages by adopting policies and programs. United States FDA established Drug Shortage Program (DSP) to deal with the shortage issue specifically. Some researchers also suggest an upgrading of DSP by focusing on all types of drugs. The developing countries should follow the foot's steps of developed countries in conducting researches, establishing platforms, policies, and guidelines for medicines and their shortages ( Babar, 2021 ). There is a need for a more robust, well-organized, and optimized management system under governmental organizations, as adopted by developed countries, to update, monitor, and control the whole drug supply chain. It should focus on national pedigree laws that will automatically restrict pharmaceutical product distribution to licensed distributors, as seen in the EU through catalogue development ( Gu et al., 2011 ) and price gouging ( Gu et al., 2011 ; Zu’bi and Abdallah, 2016 ; Nematollahi et al., 2018 ; Jia and Zhao, 2019 ), along with penalties for those who will violate the policies ( Gu et al., 2011 ; Dill and Ahn, 2014 ; Schwartzberg et al., 2017 ). For this purpose, governmental policies should involve more trained professionals and other medical experts for better procurement, stock evaluation, logistics, and mitigation plans for drug shortages ( Bazargani et al., 2014 ; Hedman, 2016 ), as found in France ( Dranitsaris et al., 2017 ). In low and middle-income countries, governmental policies and programs are absent. Adopting a robust system will portray a better, viable, and fair picture of the whole chain to manage drug distribution and drug shortage ( Alazmi and AlRashidi, 2019 ).
The pandemic warned the medicines supply chain globally. For example, the United States started to resume home production and stop trading with other countries. This de-globalization strategy decreases the risk of medicines shortages due to disruption of the supply chain outside of the country ( Vida et al., 2016 ; Coustasse et al., 2020 ; Roehr, 2020 ); however, it also increases the risk of medicine shortages in countries without pharmaceutical manufacturing.
- 2) Advance notification system. Many countries have adopted an advance notification system like France (2004), Belgium (2006), Spain (2010), Switzerland (2015), and Canada (2017) ( Fda, 2013 ; Dill and Ahn, 2014 ; Iyengar et al., 2016 ; Alazmi and Alrashidi, 2019 ), where it is enforced for the manufacturers to give notice to regulatory authorities in case of any disruption ( Schwartzberg et al., 2017 ; Walker et al., 2017 ). Still, there is no regulation or penalty for those who do not provide early notification to the health authorities ( Gu et al., 2011 ; Mazer-Amirshahi et al., 2014 ). United States FDA prevented 170 shortages in 2013 due to the advance notification system ( Dill and Ahn, 2014 ; Fox et al., 2014 ). A study conducted in Europe and Israel stated that the respective authority usually gets notification two months before shortage ( Miljković et al., 2020b ). There is no strict regulation and policy for advanced notification by manufacturers in developing countries like Pakistan, but multinational companies rarely notify severe shortages ( Atif et al., 2019 ).
- 3) National and international guidelines. International organizations worked in collaboration and presented guidelines for drug shortage mitigation ( Fox and McLaughlin, 2018 ). WHO gave global mitigation guidelines that included: increased training and global communication among stakeholders, patient-focused care, rising production rates, engagement of Non-Governmental Organizations (NGOs) to provide buffer stock, availability of worldwide reporting systems, an advance notification from manufacturers, reasonable quality control, and feasible medicine pricing ( Alsheikh et al., 2016 ; Miljković et al., 2020c ). These guidelines, along with other approaches proposed by the FDA, ASHP, and EMA, act as a foundation for other countries for making national guidelines ( Alazmi and AlRashidi, 2019 ). Many countries also develop guidelines at the national level. Israel Ministry of Health (MOH) put guidelines in which the manufacturers have to send an early notification to MOH about any shortage. It has shared protocols to manage the shortage involving all stakeholders. Each country should develop and upgrade national guidelines covering all necessary aspects of drug shortages ( Schwartzberg et al., 2017 ).
- 4) Uniform definition. Drug shortage is a global event. And it needs a uniform scale to apply it at the international level, cover all stakeholders, and overcome humanistic, economic, and clinical impacts. The uniform definition willbetter picturethis issue’s severity by measuring with standard scales and a better strategy to handle it ( Alsheikh et al., 2016 ; Schwartzberg et al., 2017 ; Bochenek et al., 2018 ).
- 5) Pricing. The regulatory authorities should design a viable pricing policy by considering all stakeholders. There should be fair criteria for the manufacturers of low-priced generics to gain appropriate profits. For expensive products like oncology drugs, the price must be placed in an acceptable range of customers ( Mazer-Amirshahi et al., 2014 ; Hedman, 2016 ; Morgan and Persaud, 2018 ). A viable pricing policy helps developing countries, keeps stock up to their level, and controls the false scarcity (to increase prices) ( Emmett, 2019 ).
- 6) Expedited drug review. Each country’s regulatory authority reviews the medical products to check whether they comply with the standard and launch new products in time. The lengthy process with a high fee will automatically delay the production and cause a drug shortage. Therefore, one of the critical steps to prevent shortages by the United States FDA in 2012 and 2013 was expediting drug reviews to restore production and introduce new products. Some researchers also suggest that United States FDA can accelerate the review process of abbreviated new generic drug applications and exclude user fees for selected drugs or manufacturer evaluation to boost new market entries ( Fox and Tyler, 2017 ).
Education and Training
Education and training of all staff involved in the drug supply chain are crucial to tackling the shortage. In addition, using alternatives properly (dose, administration, and side effects), optimizing inventory management, and scheduling stocked-out medicines are critical to mitigating the situation. Many organizations from the developed countries are providing such kinds of information on their websites, such as the Drug Shortage Program (DSP), American Society of Health-System Pharmacists (ASHP), Texas Medical Board, and European Association of Hospital Pharmacists (EAHP) ( Dill and Ahn, 2014 ; Mazer-Amirshahi et al., 2014 ).
With the help of health professionals, especially pharmacists, developing countries’ regulatory authorities can play their role in educating other professionals and giving awareness to the public ( Caulder et al., 2015 ). There is a need for special training and knowledge in treating pediatric patients, especially neonates ( Ziesenitz et al., 2019 ). Ongoing information and communication provided by clinical pharmacists on drug shortage duration resulted in a promising decrease in medication errors in the Pediatric Intensive Care Unit (ICU) ( Hughes et al., 2015 ).
Public education and awareness through advertisements, campaigns, notices about drug shortages are also essential to correct their perceptions, rebuild their behavior (increase adherence), and trust in the healthcare system for positive outcomes ( Ziesenitz et al., 2019 ). Patients should be aware of the availability of drugs in nearby clinics rather than general hospitals as increased patient flow to public hospitals causes drug shortages ( Alsheikh et al., 2016 ; Alazmi et al., 2017 ; Walker et al., 2017 ). Patients want to know about their surgeries and drug choices ( Hsia et al., 2015 ), so the decision-making process should include their preferences when the drug is unavailable ( Orlovich et al., 2020 ).
Discussion and Conclusion
Drugs shortage is a multifactorial issue and affects globally. It has gained plenty of attention in most high-income countries with the development of many associations, governmental agencies, platforms, and policies ( Acosta et al., 2019 ). On the other hand, only a few research studies are found in some middle-income countries, and there is a scarcity of studies in low-income countries ( Schwartzberg et al., 2017 ). The drug shortage situation also varied among different countries. In high-income countries, almost all classes of medicines are affected and found short in different periods. This could be due to the increased research studies that highlighted the issue. The high-income countries have developed comprehensive strategies to manage this shortage issue to some extent, which are the example for the rest of the world. The two draft definitions by the WHO ( Organization, 2017 ) and the adaptation of uniform definition in the EU ( Musazzi et al., 2020 ) are the milestones in managing drug shortages.
However, in low and middle-income countries, the issue is rising. In low-income countries, the availability and affordability of essential medicines are still the priority issues. To tackle the drug shortages, evidence from all countries, especially low-income countries, is needed to compare and develop global mitigation strategies.
International regulatory authorities need to cooperate in developing a global mitigation plan with a uniform definition. The global mitigation plan must include strategies for low and middle-income countries. Moreover, at the national level, low and middle-income countries should take steps to develop a proactive system for advance notification, reporting, and tracking of drug shortage information. Effective policies should be implemented to: develop a robust supply chain, motivate manufacturers for valued quality systems, and manufacture those medicines with a higher risk of shortage. Special attention is needed on the clinical side by training health professionals and educating the public to minimize health loss. In conclusion, it is essential to involve all the stakeholders at the national and international levels to cope with this global threat at all economic levels.
Author Contributions
Conceptualization: SS Online database searching: SS, FZ, KH, AS, AHG, SO, and SH Critical revision of the manuscript: Z-U-DB, FZ, YF, and CY Approval of the final version of the manuscript: all. Supervision of the whole study: CY.
This work was funded by the Department of Science and Technology of Shaanxi Province (2020SF-279) and “the Fundamental Research Funds for the Central Universities.”
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
- Abdelrahman A. A., Saad A. A., Sabry N. A., Farid S. F. (2016). Perceptions of Egyptian Physicians about Drug Shortage during Political Disturbances: Survey in Greater Cairo . Bull. Fac. Pharm. Cairo Univ. 54 , 191–196. 10.1016/j.bfopcu.2016.05.004 [ CrossRef ] [ Google Scholar ]
- Academy E.. (2013). ECA Academy, Handling of APIs and Excipients - New Guidelines in Chapter 5 of EU GMP Guide . Availableat: https://www.gmp-compliance.org/gmp-news/handling-of-apis-and-excipients-new-guidelines-in-chapter-5-of-eu-gmp-guide
- Acosta A., Vanegas E. P., Rovira J., Godman B., Bochenek T. (2019). Medicine Shortages: Gaps between Countries and Global Perspectives . Front. Pharmacol. 10 , 763. 10.3389/fphar.2019.00763 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Addo S. A., Abdulai M., Yawson A., Baddoo A. N., Zhao J., Workneh N., et al. (2018). Availability of HIV Services along the Continuum of HIV Testing, Care and Treatment in Ghana . BMC Health Serv. Res. 18 , 739. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Administration, U.F. (2020). USA F&D Administration . Availableat: https://www.fda.gov/ .
- Administration, U.S.F.a.D. (2020). Current and Resolved Drug Shortages and Discontinuations Reported to FDA . [ Google Scholar ]
- Alazmi A., Alhamdan H., Abualezz R., Bahadig F., Abonofal N., Osman M. (2017). Patients’ Knowledge and Attitude toward the Disposal of Medications . J. pharmaceutics 2017 , 8516741. 10.1155/2017/8516741 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alazmi A., Alrashidi F. (2019). Medication Exchange and Sharing Network Program (MESNP) Initiative to Cope with Drug Shortages in the Kingdom of Saudi Arabia (KSA) . Rmhp Vol. 12 , 115–121. 10.2147/rmhp.s198375 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alruthia Y. S., Alkofide H., Alajmi R. h., Balkhi B., Alghamdi A., Alnasser A., et al. (2017). Drug Shortages in Large Hospitals in Riyadh: a Cross-Sectional Study . Ann. Saudi Med. 37 , 375–385. 10.5144/0256-4947.2017.375 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alruthia Y. S., Alwhaibi M., Alotaibi M. F., Asiri S. A., Alghamdi B. M., Almuaythir G. S., et al. (2018). Drug Shortages in Saudi Arabia: Root Causes and Recommendations . Saudi Pharm. J. 26 , 947–951. 10.1016/j.jsps.2018.05.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alsheikh M., Seoane-Vazquez E., Rittenhouse B., Fox E. R., Fanikos J. (2016). A Comparison of Drug Shortages in the Hospital Setting in the United States and Saudi Arabia: an Exploratory Analysis . Hosp. Pharm. 51 , 370–375. 10.1310/hpj5105-370 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alsirafy S. A., Farag D. E. (2016). A Shortage of Oral Morphine in Egypt . Bull. World Health Organ. 94 , 3. 10.2471/blt.15.156240 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alspach J. G. (2012). Is the Drug Shortage Affecting Patient Care in Your Critical Care Unit? . Crit. Care Nurse 32 , 8–13. 10.4037/ccn2012810 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- American Society of Health System Pharmacists (2020). ASHP . Available at: https://www.ashp.org/Drug-Shortages/Shortage-Resources/Drug-Shortages-Statistics Accessed.june 30.2020
- Ashp and Healthcare (2020). ASHP Drug Shortages Statistics . [ Google Scholar ]
- Atif M., Malik I., Mushtaq I., Asghar S. (2019). Medicines Shortages in Pakistan: a Qualitative Study to Explore Current Situation, Reasons and Possible Solutions to Overcome the Barriers . BMJ open 9 , e027028. 10.1136/bmjopen-2018-027028 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ayati N., Saiyarsarai P., Nikfar S. (2020). Short and Long Term Impacts of COVID-19 on the Pharmaceutical Sector . DARU J. Pharm. Sci. 28 , 799–805. 10.1007/s40199-020-00358-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Babar Z.-U.-D. (2021). Ten Recommendations to Improve Pharmacy Practice in Low and Middle-Income Countries (LMICs) . J. Pharm. Pol. Pract. 14 , 1–5. 10.1186/s40545-020-00288-2 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Badreldin H. A., Atallah B. (2021). Global Drug Shortages Due to COVID-19: Impact on Patient Care and Mitigation Strategies . Res. Soc. Administrative Pharm. 17 , 1946–1949. 10.1016/j.sapharm.2020.05.017 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ballinger J. R. (2010). 99Mo Shortage in Nuclear Medicine: Crisis or challenge? . J. Labelled Compounds Radiopharm. Official J. Int. Isotope Soc. 53 , 167–168. [ Google Scholar ]
- Banerjee R., Thurm C. W., Fox E. R., Hersh A. L. (2018). Antibiotic Shortages in Pediatrics . Pediatrics 142 . 10.1542/peds.2018-0858 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bazargani Y. T., Ewen M., De Boer A., Leufkens H. G., Mantel-Teeuwisse A. K. (2014). Essential Medicines Are More Available Than Other Medicines Around the globe . PloS one 9 . 10.1371/journal.pone.0087576 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Becker D. J., Talwar S., Levy B. P., Thorn M., Roitman J., Blum R. H., et al. (2013). Impact of Oncology Drug Shortages on Patient Therapy: Unplanned Treatment Changes . Jop 9 , e122–e128. 10.1200/jop.2012.000799 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Benge C. D., Burka A. T. (2019). Heparin Drug Shortage Conservation Strategies . Fed. Pract. 36 , 449–454. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Benhabib A., Ioughlissen S., Ratignier-Carbonneil C., Maison P. (2020). The French Reporting System for Drug Shortages: Description and Trends from 2012 to 2018: an Observational Retrospective Study . BMJ open 10 , e034033. 10.1136/bmjopen-2019-034033 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blaine K. P., Press C., Lau K., Sliwa J., Rao V. K., Hill C. (2016). Comparative Effectiveness of Epsilon-Aminocaproic Acid and Tranexamic Acid on Postoperative Bleeding Following Cardiac Surgery during a National Medication Shortage . J. Clin. Anesth. 35 , 516–523. 10.1016/j.jclinane.2016.08.037 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bochenek T., Abilova V., Alkan A., Asanin B., De Miguel Beriain I., Besovic Z., et al. (2018). Systemic Measures and Legislative and Organizational Frameworks Aimed at Preventing or Mitigating Drug Shortages in 28 European and Western Asian Countries . Front. Pharmacol. 8 , 942. 10.3389/fphar.2017.00942 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bogaert P., Bochenek T., Prokop A., Pilc A. (2015). A Qualitative Approach to a Better Understanding of the Problems Underlying Drug Shortages, as Viewed from Belgian, French and the European Union’s Perspectives . PloS one 10 . 10.1371/journal.pone.0125691 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bouvy F., Rotaru M. (2021). Medicine Shortages: From Assumption to Evidence to Action-A Proposal for Using the FMD Data Repositories for Shortages Monitoring . Front. Med. 8 . 10.3389/fmed.2021.579822 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Burki T. K. (2017). Ongoing Drugs Shortage in Venezuela and Effects on Cancer Care . Lancet Oncol. 18 , 578. 10.1016/s1470-2045(17)30258-9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Caulder C. R., Mehta B., Bookstaver P. B., Sims L. D., Stevenson B., Pharmacists S. C. S. O. H.-S. (2015). Impact of Drug Shortages on Health System Pharmacies in the Southeastern United States . Hosp. Pharm. 50 , 279–286. 10.1310/hpj5004-279 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Choo E. K., Rajkumar S. V. (2020). “ "Medication Shortages during the COVID-19 Crisis: what We Must Do ,” in Mayo Clinic Proceedings (Elsevier; ), 1112–1115. 10.1016/j.mayocp.2020.04.001 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clark S. L., Levasseur-Franklin K., Pajoumand M., Barra M., Armahizer M., Patel D. V., et al. (2020). Collaborative Management Strategies for Drug Shortages in Neurocritical Care . Neurocrit. Care , 1–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Costelloe E. M., Guinane M., Nugent F., Halley O., Parsons C. (20151971). An Audit of Drug Shortages in a Community Pharmacy Practice . Ir J. Med. Sci. 184 , 435–440. 10.1007/s11845-014-1139-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coustasse A., Kimble C., Maxik K. (2020). Rethinking Supply Chain Management Strategies for Ventilator Related Medications during COVID-19 Pandemic in the United States . Int. J. Healthc. Management 13 , 352–354. 10.1080/20479700.2020.1801162 [ CrossRef ] [ Google Scholar ]
- Dave C. V., Pawar A., Fox E. R., Brill G., Kesselheim A. S. (2018). Predictors of Drug Shortages and Association with Generic Drug Prices: a Retrospective Cohort Study . Value in health 21 , 1286–1290. 10.1016/j.jval.2018.04.1826 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- De Weerdt E., Simoens S., Casteels M., Huys I. (2015). Toward a European Definition for a Drug Shortage: a Qualitative Study . Front. Pharmacol. 6 , 253. 10.3389/fphar.2015.00253 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dill S., Ahn J. (2014). Drug Shortages in Developed Countries-Reasons, Therapeutic Consequences, and Handling . Eur. J. Clin. Pharmacol. 70 , 1405–1412. 10.1007/s00228-014-1747-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Donohue J. M., Angus D. C. (2017). National Shortages of Generic Sterile Injectable Drugs . Jama 317 , 1415–1417. 10.1001/jama.2017.2826 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dranitsaris G., Jacobs I., Kirchhoff C., Popovian R., Shane L. G. (2017). Drug Tendering: Drug Supply and Shortage Implications for the Uptake of Biosimilars . Ceor Vol. 9 , 573–584. 10.2147/ceor.s140063 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elbagir M. N., Eltom M. A., Rosling H., Berne C. (1995). Glycaemic Control of Insulin-dependent Diabetes Mellitus in Sudan: Influence of Insulin Shortage . Diabetes Res. Clin. Pract. 30 , 43–52. 10.1016/0168-8227(95)01145-5 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Emmett D. (2019). Supply Chains in Healthcare Organizations: Lessons Learned from Recent Shortages . Hosp. Top. 97 , 133–138. 10.1080/00185868.2019.1644264 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fatima S. A., Khaliq A. (2017). A Survey Regarding Drug Shortage in Tertiary Care Hospitals of Karachi, Pakistan . Jppcm 3 , 262–266. 10.5530/jppcm.2017.4.69 [ CrossRef ] [ Google Scholar ]
- Fda U. (2013). Strategic Plan for Preventing and Mitigating Drug Shortages . Tech. rep., US Food Drug Adm. . [ Google Scholar ]
- Ferrario A., Arāja D., Bochenek T., Čatić T., Dankó D., Dimitrova M., et al. (2017). The Implementation of Managed Entry Agreements in Central and Eastern Europe: Findings and Implications . Pharmacoeconomics 35 , 1271–1285. 10.1007/s40273-017-0559-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fittler A., Vida R. G., Rádics V., Botz L. (2018). A challenge for Healthcare but Just Another Opportunity for Illegitimate Online Sellers: Dubious Market of Shortage Oncology Drugs . PloS one 13 , e0203185. 10.1371/journal.pone.0203185 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Food U. (2018). Drug Administration. Current and Resolved Drug Shortages and Discontinuations Reported to FDA . [ Google Scholar ]
- Food U., Administration D. (2019). Drug Shortages: Root Causes and Potential Solutions. A Report By the Drug Shortages Task Force . Available at: https://www.fda.gov/media/131130/download .
- Fox E. R., Tyler L. S. (2013). Call to Action: Finding Solutions for the Drug Shortage Crisis in the United States . Clin. Pharmacol. Ther. 93 , 145–147. 10.1038/clpt.2012.225 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fox E. R., Mclaughlin M. M. (2018). ASHP Guidelines on Managing Drug Product Shortages . Am. J. health-system Pharm. 75 , 1742–1750. 10.2146/ajhp180441 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fox E. R., Sweet B. V., Jensen V. (2014). “ Drug Shortages: a Complex Health Care Crisis ,” in Mayo Clinic Proceedings (Elsevier; ), 89 , 361–373. 10.1016/j.mayocp.2013.11.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fox E. R., Tyler L. S. (2003). Managing Drug Shortages: Seven Years' Experience at One Health System . Am. J. Health-System Pharm. 60 , 245–253. 10.1093/ajhp/60.3.245 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fox E. R., Tyler L. S. (2017). Potential Association between Drug Shortages and High-Cost Medications . Pharmacotherapy 37 , 36–42. 10.1002/phar.1861 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frattarelli D. A., Galinkin J. L., Green T. P., Johnson T. D., Neville K. A., Paul I. M., et al. (2014). Off-label Use of Drugs in Children . Pediatrics 133 ( 3 ), 563–567. 10.1542/peds.2013-4060 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Giammona R., Di Martino E., Vinci D. L., Provenzani A., Polidori P. (2020). 5PSQ-096 Hazard Vulnerability Analysis to Evaluate the Risk of Drug Shortages According to Therapeutic Class . Br. Med. J. Publishing Group 27 . 10.1136/ejhpharm-2020-eahpconf.413 [ CrossRef ] [ Google Scholar ]
- Gray A. (2014). Medicines Shortages-Unpicking the Evidence from a Year in South Africa . Amj 7 , 208–212. 10.4066/amj.2014.1932 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gray A., Manasse H. R., Jr (2012). Shortages of Medicines: a Complex Global challenge . SciELO Public Health 90 , 158–158A. 10.2471/BLT.11.101303 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Griffith M. M., Gross A. E., Sutton S. H., Bolon M. K., Esterly J. S., Patel J. A., et al. (2012). The Impact of Anti-infective Drug Shortages on Hospitals in the United States: Trends and Causes . Clin. Infect. Dis. 54 , 684–691. 10.1093/cid/cir954 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gross A. E., Johannes R. S., Gupta V., Tabak Y. P., Srinivasan A., Bleasdale S. C. (2017). The Effect of a Piperacillin/tazobactam Shortage on Antimicrobial Prescribing and Clostridium difficile Risk in 88 US Medical Centers . Clin. Infect. Dis. 65 , 613–618. 10.1093/cid/cix379 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gu A., Wertheimer A. I., Brown B., Shaya F. T. (2011). Drug Shortages in the US–Causes, Impact, and Strategies . Inov Pharm. 2 , 6. [ Google Scholar ]
- Gundlapalli A. V., Beekmann S. E., Graham D. R., Polgreen P. M., Network E. I. (2018). “ "Antimicrobial Agent Shortages: the New Norm for Infectious Diseases Physicians ,” in Open Forum Infectious Diseases , 5 , ofy068. 10.1093/ofid/ofy068 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haider A., Qian Y., Lu Z., Naqvi S., Zhuang A., Reddy A., et al. (2019). Implications of the Parenteral Opioid Shortage for Prescription Patterns and Pain Control Among Hospitalized Patients with Cancer Referred to Palliative Care . JAMA Oncol. 5 , 841–846. 10.1001/jamaoncol.2019.0062 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hayes M. S., Ward M. A., Slabaugh S. L., Xu Y. (2014). Lessons from the Leucovorin Shortages between 2009 and 2012 in a Medicare Advantage Population: where Do We Go from Here? . Am. Health Drug benefits 7 , 264. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hedlund N. G., Isgor Z., Zwanziger J., Rondelli D., Crawford S. Y., Hynes D. M., et al. (2018). Drug Shortage Impacts Patient Receipt of Induction Treatment . Health Serv. Res. 53 , 5078–5105. 10.1111/1475-6773.13028 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hedman L. (2016). Global Approaches to Addressing Shortages of Essential Medicines in Health Systems . WHO Drug Inf. 30 , 180. [ Google Scholar ]
- Heiskanen K., Ahonen R., Kanerva R., Karttunen P., Timonen J. (2017). The Reasons behind Medicine Shortages from the Perspective of Pharmaceutical Companies and Pharmaceutical Wholesalers in Finland . PloS one 12 , e0179479. 10.1371/journal.pone.0179479 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Herath H., Ranaweera K., Rodrigo E. (2011). Procurement Monitoring and Coordination through Information Technology to Overcome Drug Shortage in the Health Sector . Sri Lanka J. Bio-Medical Inform. 1 . 10.4038/sljbmi.v1i0.3554 [ CrossRef ] [ Google Scholar ]
- Hogerzeil H. (2006). Essential Medicines and Human Rights: what Can They Learn from Each Other? . Bull. World Health Organ. 84 , 371–375. 10.2471/blt.06.031153 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Holcombe B., Mattox T. W., Plogsted S. (2018). Drug Shortages: Effect on Parenteral Nutrition Therapy . Nutr. Clin. Pract. 33 , 53–61. 10.1002/ncp.10052 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Honda H., Murakami S., Tokuda Y., Tagashira Y., Takamatsu A. (2020). Critical National Shortage of Cefazolin in Japan: Management Strategies . Clin. Infect. Dis. 71 ( 7 ), 1783–1789. 10.1093/cid/ciaa216 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hsia I. K.-H., Dexter F., Logvinov I., Tankosic N., Ramakrishna H., Brull S. J. (2015). Survey of the National Drug Shortage Effect on Anesthesia and Patient Safety . Anesth. Analgesia 121 , 502–506. 10.1213/ane.0000000000000798 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hsueh K., Reyes M., Krekel T., Casabar E., Ritchie D. J., Jafarzadeh S. R., et al. (2017). Effective Antibiotic Conservation by Emergency Antimicrobial Stewardship during a Drug Shortage . Infect. Control. Hosp. Epidemiol. 38 , 356–35910. 10.1017/ice.2016.289. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang B., Xu M. (2017). Commentary: Combating Sale of Counterfeit and Falsified Medicines Online: a Losing Battle . Front. Pharmacol. 8 , 909. 10.3389/fphar.2017.00909 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hughes K. M., Goswami E. S., Morris J. L. (2015). Impact of a Drug Shortage on Medication Errors and Clinical Outcomes in the Pediatric Intensive Care Unit . J. Pediatr. Pharmacol. Ther. 20 , 453–461. 10.5863/1551-6776-20.6.453 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Iyengar S., Hedman L., Forte G., Hill S. (2016). Medicine Shortages: a Commentary on Causes and Mitigation Strategies . BMC Med. 14 , 124. 10.1186/s12916-016-0674-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jackson G., Patel S., Khan S. (2012). Assessing the Problem of Counterfeit Medications in the United Kingdom . Int. J. Clin. Pract. 66 , 241–250. 10.1111/j.1742-1241.2011.02826.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jenzer H., Sadeghi L., Maag P., Scheidegger-Balmer F., Uhlmann K., Groesser S. (2019). “ The European Medicines Shortages Research Network and its mission to Strategically Debug Disrupted Pharmaceutical Supply Chains ,” in Pharmaceutical Supply Chains-Medicines Shortages (Springer; ), 1–22. 10.1007/978-3-030-15398-4_1 [ CrossRef ] [ Google Scholar ]
- Jia J., Zhao H. (2019). Reflection on "Mitigating the U.S. Drug Shortages through Pareto‐Improving Contracts" . Prod. Oper. Manag. 28 , 2716–2718. 10.1111/poms.13079 [ CrossRef ] [ Google Scholar ]
- Kaakeh R., Sweet B. V., Reilly C., Bush C., Deloach S., Higgins B., et al. (2011). Impact of Drug Shortages on U.S. Health Systems . Am. J. Health-System Pharm. 68 , 1811–1819. 10.2146/ajhp110210 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kangwana B. B., Memusi D. N., Snow R. W., Njogu J., Goodman C. A., Wasunna B., et al. (2009). Malaria Drug Shortages in Kenya: a Major Failure to Provide Access to Effective Treatment . Am. J. Trop. Med. Hyg. 80 , 737–738. 10.4269/ajtmh.2009.80.737 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Khan F. A. (2019). Anesthetic Drugs Shortage in Lower and Middle Income Countries: a Safety and Quality Issue . Anaesth. Pain Intensive Care , 337–339. [ Google Scholar ]
- Khuluza F., Heide L. (2017). Availability and Affordability of Antimalarial and Antibiotic Medicines in Malawi . PloS one 12 , e0175399. 10.1371/journal.pone.0175399 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Klobuchar S. (2011). Shortages of Cancer Drugs in the USA . Lancet Oncol. 12 , 70150–70154. [ PubMed ] [ Google Scholar ]
- Koenraadt R., Van De Ven K. (2018). The Internet and Lifestyle Drugs: an Analysis of Demographic Characteristics, Methods, and Motives of Online Purchasers of Illicit Lifestyle Drugs in the Netherlands . Drugs Educ. Prev. Pol. 25 , 345–355. 10.1080/09687637.2017.1369936 [ CrossRef ] [ Google Scholar ]
- Kos M. (2019). “ Introduction to Healthcare Systems ,” in The Pharmacist Guide to Implementing Pharmaceutical Care (Springer; ), 437–441. 10.1007/978-3-319-92576-9_34 [ CrossRef ] [ Google Scholar ]
- Liang B. A., Mackey T. K. (2012). Vaccine Shortages and Suspect Online Pharmacy Sellers . Vaccine 30 , 105–108. 10.1016/j.vaccine.2011.11.016 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lukmanji S., Sauro K. M., Josephson C. B., Altura K. C., Wiebe S., Jetté N. (2018). A Longitudinal Cohort Study on the Impact of the Clobazam Shortage on Patients with Epilepsy . Epilepsia 59 , 468–478. 10.1111/epi.13974 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lyon J. (2012). Drug Shortage Compounding: the Only Safe Medication Source in a Time of Crisis . Int. J. Pharm. compounding 16 , 456–460. [ PubMed ] [ Google Scholar ]
- Malik M., Hassali M. a. A., Shafie A. A., Hussain A. (2013). Why Hospital Pharmacists Have Failed to Manage Antimalarial Drugs Stock-Outs in Pakistan? A Qualitative Insight . Malar. Res. Treat. 2013 , 342843. 10.1155/2013/342843 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mazer-Amirshahi M., Fox E. R., Farmer B. M., Stolbach A. I. (2020). ACMT Position Statement: Medication Shortages during Coronavirus Disease Pandemic . J. Med. Toxicol. 1 . [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mazer-Amirshahi M., Goyal M., Umar S. A., Fox E. R., Zocchi M., Hawley K. L., et al. (2017). U.S. Drug Shortages for Medications Used in Adult Critical Care (2001-2016) . J. Crit. Care 41 , 283–288. 10.1016/j.jcrc.2017.06.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mazer-Amirshahi M., Pourmand A., Singer S., Pines J. M., Van Den Anker J. (2014). Critical Drug Shortages: Implications for Emergency Medicine . Acad. Emerg. Med. 21 , 704–711. 10.1111/acem.12389 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mclaughlin M., Kotis D., Thomson K., Harrison M., Fennessy G., Postelnick M., et al. (2013). Effects on Patient Care Caused by Drug Shortages: a Survey . Jmcp 19 , 783–788. 10.18553/jmcp.2013.19.9.783 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mclaughlin M. M., Sutton S. H., Jensen A. O., Esterly J. S. (2017). Use of High-Dose Oral Valacyclovir during an Intravenous Acyclovir Shortage: a Retrospective Analysis of Tolerability and Drug Shortage Management . Infect. Dis. Ther. 6 , 259–264. 10.1007/s40121-017-0157-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Meloni S. T., Chaplin B., Idoko J., Agbaji O., Akanmu S., Imade G., et al. (2017). Drug Resistance Patterns Following Pharmacy Stock Shortage in Nigerian Antiretroviral Treatment Program . AIDS Res. Ther. 14 , 58. 10.1186/s12981-017-0184-5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miljković N., Batista A., Polidori P., Kohl S., Horák P. (2020a). Results of EAHP’s 2019 Medicines Shortages Survey . Eur. J. Hosp. Pharm. 27 , 202–208. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miljković N., Godman B., Kovačević M., Polidori P., Tzimis L., Hoppe-Tichy T., et al. (2020b). Prospective Risk Assessment of Medicine Shortages in Europe and Israel: Findings and Implications . Front. Pharmacol. 11 , 357. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miljković N., Godman B., Van Overbeeke E., Kovačević M., Tsiakitzis K., Apatsidou A., et al. (2020c). Risks in Antibiotic Substitution Following Medicine Shortage: a Health-Care Failure Mode and Effect Analysis of Six European Hospitals . Front. Med. 7 , 157. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Modisakeng C., Matlala M., Godman B., Meyer J. C. (2020). Medicine Shortages and Challenges with the Procurement Process Among Public Sector Hospitals in South Africa; Findings and Implications . BMC Health Serv. Res. 20 , 1–10. 10.1186/s12913-020-05080-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morgan S. G., Persaud N. (2018). New Generic Pricing Scheme Maintains High Prices and Risks of Shortages . Cmaj 190 , E410–E411. 10.1503/cmaj.180197 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Musazzi U. M., Di Giorgio D., Minghetti P. (2020). New Regulatory Strategies to Manage Medicines Shortages in Europe . Int. J. pharmaceutics 579 , 119171. 10.1016/j.ijpharm.2020.119171 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nematollahi M., Hosseini-Motlagh S.-M., Ignatius J., Goh M., Saghafi Nia M. (2018). Coordinating a Socially Responsible Pharmaceutical Supply Chain under Periodic Review Replenishment Policies . J. Clean. Prod. 172 , 2876–2891. 10.1016/j.jclepro.2017.11.126 [ CrossRef ] [ Google Scholar ]
- Nixon H. C. (2021). Drug Shortages in Obstetrics . Curr. Anesthesiology Rep. , 1–9. [ Google Scholar ]
- Organization W. H. (2015). Addressing the Global Shortages of Medicines, and the Safety and Accessibility of Children’s Medication–Eb138/41 . Geneva: WHO. [ Google Scholar ]
- Organization W. H. (2016). Medicines Shortages: Global Approaches to Addressing Shortages of Essential Medicines in Health Systems . WHO Drug Inf. 30 , 180–185. [ Google Scholar ]
- Organization W. H. (2017). Technical Definitions of Shortages and Stockouts of Medicines and Vaccines . Geneva: World Health Organization. [ Google Scholar ]
- Orlovich D. S., Mincer S. L., Domino K. B. (2020). Analgesic Medication Shortages . Anesth. Analgesia 130 , 265–270. 10.1213/ane.0000000000004514 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Panic G., Yao X., Gregory P., Austin Z. (2020). How Do Community Pharmacies in Ontario Manage Drug Shortage Problems? Results of an Exploratory Qualitative Study . Can. Pharm. J. 153 , 371–377. 10.1177/1715163520958023 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Panzitta M., Ponti M., Bruno G., Cois G., D’Arpino A., Minghetti P., et al. (2017). The Strategic Relevance of Manufacturing Technology: An Overall Quality Concept to Promote Innovation Preventing Drug Shortage . Int. J. pharmaceutics 516 , 144–157. 10.1016/j.ijpharm.2016.11.018 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pauwels K., Huys I., Casteels M., Simoens S. (2014). Drug Shortages in European Countries: a Trade-Off between Market Attractiveness and Cost Containment? . BMC Health Serv. Res. 14 , 438. 10.1186/1472-6963-14-438 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pauwels K., Simoens S., Casteels M., Huys I. (2015). Insights into European Drug Shortages: a Survey of Hospital Pharmacists . PloS one 10 , e0119322. 10.1371/journal.pone.0119322 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Perumal-Pillay V. A., Suleman F. (2017). Parents’ and Guardians’ Perceptions on Availability and Pricing of Medicines and Healthcare for Children in eThekwini, South Africa–a Qualitative Study . BMC Health Serv. Res. 17 , 1–11. 10.1186/s12913-017-2385-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pharmacists A. S. O. H.-S. (2018). Drug Shortages Roundtable: Minimizing the Impact on Patient Care . Am. J. Health-System Pharm. 75 , 816–820. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pharmacists A. S. O. H. (2020). ASHP . Available: https://www.ashp.org/Drug-Shortages/Shortage-Resources/Drug-Shortages-Statistics?loginreturnUrl=SSOCheckOnly .
- Phuong J. M., Penm J., Chaar B., Oldfield L. D., Moles R. (2019). The Impacts of Medication Shortages on Patient Outcomes: a Scoping Review . PloS one 14 , e0215837. 10.1371/journal.pone.0215837 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Quilty S. (2014). Medicine Shortages in Australia--the Reality . amj 7 , 240–242. 10.4066/amj.2014.1933 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rhodes N. J., Gilbert E. M., Skoglund E., Esterly J. S., Postelnick M. J., Mclaughlin M. M. (2016). Prediction of Inventory Sustainability during a Drug Shortage . Am. J. Health-System Pharm. 73 , 1094–1098. 10.2146/ajhp150532 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ricci J. A., Koolen P. G., Shah J., Tobias A. M., Lee B. T., Lin S. J. (2016). Comparing the Outcomes of Different Agents to Treat Vasospasm at Microsurgical Anastomosis during the Papaverine Shortage . Plast. Reconstr. Surg. 138 , 401e–408e. 10.1097/prs.0000000000002430 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rider A. E., Templet D. J., Daley M. J., Shuman C., Smith L. V. (2013). Clinical Dilemmas and a Review of Strategies to Manage Drug Shortages . J. Pharm. Pract. 26 , 183–191. 10.1177/0897190013482332 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rinaldi F., De Denus S., Nguyen A., Nattel S., Bussières J.-F. (2017). Drug Shortages: Patients and Health Care Providers Are All Drawing the Short Straw . Can. J. Cardiol. 33 , 283–286. 10.1016/j.cjca.2016.08.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roehr B. (2020). Bringing Drug Production home: How the US Is Rebuilding the Drug Supply Chain after Covid-19 . bmj 370 , m3393. 10.1136/bmj.m3393 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rowe W. B., Morgan B., Whitehurst R., Bush P. A. (2020). Increasing Medication Access by Promoting Appropriate Use of Multi-Dose Vials . Plast. Surg. Nurs. 40 , 177–182. 10.1097/psn.0000000000000323 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Russell H. V., Bernhardt M. B., Berg S. (2017). Using Decision Modeling to Guide Drug Allocation during a Shortage . Pediatr. Blood Cancer 64 , e26331. 10.1002/pbc.26331 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Said A., Goebel R., Ganso M., Zagermann-Muncke P., Schulz M. (2018). Drug Shortages May Compromise Patient Safety: Results of a Survey of the Reference Pharmacies of the Drug Commission of German Pharmacists . Health Policy 122 , 1302–1309. 10.1016/j.healthpol.2018.09.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schwartzberg E., Ainbinder D., Vishkauzan A., Gamzu R. (2017). Drug Shortages in Israel: Regulatory Perspectives, Challenges and Solutions . Isr. J. Health Pol. Res. 6 , 1–8. 10.1186/s13584-017-0140-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schweitzer S. O. (2013). How the US Food and Drug Administration Can Solve the Prescription Drug Shortage Problem . Am. J. Public Health 103 , e10–e14. 10.2105/ajph.2013.301239 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Setayesh S., Mackey T. K. (2016). Addressing the Impact of Economic Sanctions on Iranian Drug Shortages in the Joint Comprehensive Plan of Action: Promoting Access to Medicines and Health Diplomacy . Globalization and health 12 , 31. 10.1186/s12992-016-0168-6 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seunanden T., Day C. (2013). The Extent and Impact of TB Drug Stock-Outs . South Afr. Health Rev. 2013 , 173–189. [ Google Scholar ]
- Shaban H., Maurer C., Willborn R. J. (2018). Impact of Drug Shortages on Patient Safety and Pharmacy Operation Costs . Fed. Pract. 35 , 24–31. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Siow W. T., Tang S. H., Agrawal R. V., Tan A. Y., See K. C. (2020). Essential ICU Drug Shortages for COVID-19: what Can Frontline Clinicians Do? . Crit. Care 24 , 1–3. 10.1186/s13054-020-02971-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Souliotis K., Papageorgiou M., Politi A., Ioakeimidis D., Sidiropoulos P. (2014). Barriers to Accessing Biologic Treatment for Rheumatoid Arthritis in Greece: the Unseen Impact of the Fiscal Crisis-The Health Outcomes Patient Environment (HOPE) Study . Rheumatol. Int. 34 , 25–33. 10.1007/s00296-013-2866-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sun L., Tamboli M., Wang R. R., Kandarian B. S., Wong A., Lochbaum G. M., et al. (2020). How Anesthesiologists Adapted to a Nationwide Spinal Bupivacaine Drug Shortage . J. Clin. Anesth. 61 , 109668. 10.1016/j.jclinane.2019.109668 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tan V. S., Nash D. M., Mcarthur E., Jain A. K., Garg A. X., Juurlink D. N., et al. (2017). Impact of Injectable Furosemide Hospital Shortage on Congestive Heart Failure Outcomes: a Time Series Analysis . Can. J. Cardiol. 33 , 1498–1504. 10.1016/j.cjca.2017.09.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tan Y. X., Moles R. J., Chaar B. B. (2016). Medicine Shortages in Australia: Causes, Impact and Management Strategies in the Community Setting . Int. J. Clin. Pharm. 38 , 1133–1141. 10.1007/s11096-016-0342-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thoma B. N., Li J., Mcdaniel C. M., Wordell C. J., Cavarocchi N., Pizzi L. T. (2014). Clinical and Economic Impact of Substituting Dexmedetomidine for Propofol Due to a US Drug Shortage: Examination of Coronary Artery Bypass Graft Patients at an Urban Medical centre . Pharmacoeconomics 32 , 149–157. 10.1007/s40273-013-0116-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tren R., Hess K., Bate R. (2009). Drug Procurement, the Global Fund and Misguided Competition Policies . Malar. J. 8 , 305. 10.1186/1475-2875-8-305 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Unguru Y., Bernhardt M. B., Berg S. L., Johnson L.-M., Pyke-Grimm K., Woodman C., et al. (2019). Chemotherapy and Supportive Care Agents as Essential Medicines for Children with Cancer . JAMA Pediatr. 173 , 477–484. 10.1001/jamapediatrics.2019.0070 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Unit E. I. (2017). Cancer Medicines Shortages in Europe: Policy Recommendations to Prevent and Manage Shortages . London: The Economist). [ Google Scholar ]
- Vail E., Gershengorn H. B., Hua M., Walkey A. J., Rubenfeld G., Wunsch H. (2017). Association between US Norepinephrine Shortage and Mortality Among Patients with Septic Shock . Jama 317 , 1433–1442. 10.1001/jama.2017.2841 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Valgus J., Singer E. A., Berry S. R., Rathmell W. K. (2013). Ethical Challenges: Managing Oncology Drug Shortages . Jop 9 , e21–e23. 10.1200/jop.2012.000779 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ventola C. L. (2011). The Drug Shortage Crisis in the United States: Causes, Impact, and Management Strategies . Pharm. Ther. 36 , 740. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vida R. G., Nyaka B., Hornyák J. K., Botz L. (2016). A Gyógyszerhiányok Intézmé Nyi Kö Ltsé Gekre Kifejtett Hatá Sainak É Rté Kelé Se . J. Hungarian Interdiscip. Med. (INFORMATIKA ES MENEDZSMENT AZ EGÉ SZSÉ GU GYBEN) 15 , 42–46. [ Google Scholar ]
- Videau M., Chemali L., Stucki C., Saavedra-Mitjans M., Largana S., Guerin A., et al. (2019a). Drug Shortages in Canada and Selected European Countries: a Cross-Sectional, Institution-Level Comparison . Can. J. Hosp. Pharm. 72 , 7. 10.4212/cjhp.v72i1.2863 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Videau M., Lebel D., Bussières J.-F. (2019b). “ Drug Shortages in Canada: Data for 2016–2017 and Perspectives on the Problem ,” in Annales Pharmaceutiques Francaises (Elsevier; ), 77 , 205–211. 10.1016/j.pharma.2018.11.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Visage R., Kaiser N., Williams M., Kim A. (2019). Oral Methods of Urinary Alkalinization for High-Dose Methotrexate Administration: Alternatives to Intravenous Sodium Bicarbonate during a Critical Drug Shortage . J. Pediatr. Hematology/Oncology 41 , 371–375. 10.1097/mph.0000000000001348 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Walker J., Chaar B. B., Vera N., Pillai A. S., Lim J. S., Bero L., et al. (2017). Medicine Shortages in Fiji: A Qualitative Exploration of Stakeholders’ Views . PloS one 12 , e0178429. 10.1371/journal.pone.0178429 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wall S., Bangalee V. (2019). The Ketamine Crisis: Does South Africa Have a Plan B? . S Afr. Med. J. 109 , 911–913. 10.7196/samj.2019.v109i12.14188 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Woodcock J., Wosinska M. (2013). Economic and Technological Drivers of Generic Sterile Injectable Drug Shortages . Clin. Pharmacol. Ther. 93 , 170–176. [ PubMed ] [ Google Scholar ]
- Yang C., Wu L., Cai W., Zhu W., Shen Q., Li Z., et al. (2016). Current Situation, Determinants, and Solutions to Drug Shortages in Shaanxi Province, China: a Qualitative Study . PloS one 11 , e0165183. 10.1371/journal.pone.0165183 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yellapu V., Malik Q. Z., Perez Figueroa I., Singh A., Longo S. V., Nanda S. (2019). Global burden of Rheumatic Heart Disease and the Shortage of Penicillin . Circulation 140 , A15479. [ Google Scholar ]
- Yin M., Li Q., Qiao Z. (2016). " A Study on Consumer Acceptance of Online Pharmacies in China ", in: Proceedings of the 18th Annual International Conference on Electronic Commerce: e-Commerce in Smart connected World), 1–8. 10.1145/2971603.2971616 [ CrossRef ] [ Google Scholar ]
- Ziesenitz V. C., Fox E., Zocchi M., Samiee-Zafarghandy S., van den Anker J. N., Mazer-Amirshahi M. (2019). Prescription Drug Shortages: Impact on Neonatal Intensive Care . Neonatology 115 , 108–115. 10.1159/000493119 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zu’bi M., Abdallah A. (2016). A Quantitative Analysis of the Causes of Drug Shortages in Jordan: a Supply Chain Perspective . Int. Business Res. 9 . [ Google Scholar ]
- Zwaida T. A., Beauregard Y., Elarroudi K. (2019). Comprehensive Literature Review about Drug Shortages in the canadian Hospital's Pharmacy Supply Chain . International Conference on Engineering, Science, and Industrial Applications. IEEE, 1–5. [ Google Scholar ]
- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes
You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
The Worsening Prescription Drug Shortage and How to Cope With It

Many or all of the products featured here are from our partners who compensate us. This influences which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
Drug shortages are an ongoing fact of life, and many Americans have known the inconvenience of having to wait to fill a prescription. But shortages have mounted in recent years, alarming observers and generating headlines.
The number of prescription drugs in shortage climbed to a 10-year high of 323 in the first quarter of 2024 — but it’s not just about the numbers. Patients and their health care providers are also being hit with much more consequential shortages, some with potentially life-altering results.
Hospital crash carts, used to provide emergency treatment to patients with critical conditions like cardiac arrest, have run short of premeasured packages of drugs like epinephrine, forcing clinicians to spend extra time measuring a dose from a vial, and increasing the odds of a medication error.
Some cancer patients, if their first-choice chemotherapy is unavailable, have had to take another drug that has much worse side effects.
Shortages can affect everyone connected with health care in any setting. “Drug shortages impact patients, families, caregivers, pharmacists, hospitals, nursing homes, hospices, and other individuals and entities across the health care system,” according to an April 2024 white paper from the U.S. Department of Health and Human Services.
To make matters worse, over the past 12 months, there have been shortages of medicines for which there is no alternative, says Erin Fox, senior pharmacy director at University of Utah Health. Fox gives one example: oxytocin, a drug that’s ordered by obstetricians to induce labor or, after delivery, to help stop maternal bleeding.
Which drugs are in short supply?
Hundreds of prescription medications are difficult or impossible to obtain as of April 2024. Among them are quinapril, which is primarily used to treat hypertension; injectable acyclovir, an antiviral; and propofol, for general anesthesia.
You can check the availability of a prescription drug by searching the U.S. Food and Drug Administration's FDA Drug Shortages database or the American Society of Health-System Pharmacists' ASHP Drug Shortages List . Click on any drug name to learn more about that specific shortage.
The effects of shortages on patients and their providers can be profound. Scott Matsuda, a member of the Patient and Family Advisory Council at the nonprofit Patient Access Network (PAN) Foundation, has worked with cancer patients “who, all of a sudden, find their chemotherapy drugs aren’t available.” Sometimes, patients report that symptoms of their cancers return soon after they stop taking their first-choice chemo, he adds.
No health care setting has been spared, not even hospital operating rooms. Dr. Jesse Ehrenfeld, an anesthesiologist and the president of the American Medical Association, at times has had to use second-choice drugs to induce anesthesia. These medications may have additional side effects, such as lasting longer than necessary, he said.
“Complex workarounds also have the potential to introduce errors,” says Ehrenfeld. “And I’ve had colleagues who had to delay or cancel care due to a shortage.”
Why are so many drugs in short supply?
What causes shortages? About 12% of them are due to manufacturing problems, as when a tornado hit a Pfizer plant in North Carolina, according to drugmakers’ reports compiled by the ASHP. Another 14% of shortages happen when demand suddenly outruns supply; for example, that occurs when demand for the antiviral Tamiflu spikes during a severe flu season. And 12% are due to a business decision, like when a drug manufacturer decides they can reap greater profits by making a different drug.
But the biggest category of reasons that manufacturers give for a shortage, at 60%, is “unknown/would not provide.” Ehrenfeld says, “That’s called flying blind. In most cases, we really don’t have an attributable cause, which makes it hard to pinpoint sustainable solutions.”
What’s being done to solve this multifaceted problem?
Drug shortages are a tough problem because they have such diverse causes. Stakeholders have been seeking solutions for decades, but shortages have continued throughout health care.
ASHP has recommended that, for starters, Congress give the FDA the power to levy “meaningful penalties” on drugmakers that fail to report manufacturing and supply chain problems. Failure to report is rampant in the industry.
“We think FDA requiring greater transparency in manufacturing and distribution could help us understand the causes and mitigate the challenges,” says Ehrenfeld.
The pharmacist group also recommends that to improve the profitability of generics, the FDA waive some fees on manufacturers who promptly bring these lower-priced drugs to market.
Some observers are hopeful that momentum is gathering for impactful action. “I’ve been working on drug shortages since 2001, and we now have the most interest in Congress and elsewhere that I’ve ever seen,” says Fox, who has testified about the problem at Senate committee hearings.
How can you work around a shortage of your drug?
The bottom line for health care consumers is that systemic problems with prescription drug supplies will likely persist. If you’re faced with a shortage of a drug you need, these steps will improve your chances of getting hold of it more quickly.
Refill prescriptions as early as your insurer will let you. Ordering prescriptions ahead can give you more options for obtaining a refill before you run out.
Contact your prescriber. Let them know that your prescription isn’t available at your pharmacy or will be delayed. Solicit their suggestions for other ways to get the drug, a generic or brand-name equivalent, or an alternative medication that would work for you.
Ask your insurer to cover the brand-name version if the generic drug is unavailable. If your insurer resists paying for the more expensive brand-name drug, ask your prescriber to go to bat for you.
Develop a long-term working relationship with your pharmacist.
If the pharmacist knows you’re a regular customer, they may be more likely to hustle to find a supplier that has your medication.
Try other pharmacies. Drugs in shortage are often distributed unevenly among pharmacies. Call around and see if another retailer in your area has a supply. If your insurer has a mail-order prescription option, consider trying it.
(Photo by Sean Rayford/Getty Images )
On a similar note...

on Capitalize's website

We Need to Stop Trying to Raise “Drug-Free” Kids
The important shift away from abstinence to addiction resistance..
Posted May 13, 2024 | Reviewed by Michelle Quirk
- What Is Addiction?
- Find a therapist to overcome addiction
- Kids and teens lack basic knowledge about what alcohol and drugs actually do in their brains and bodies.
- School-based alcohol and drug education programs are incomplete, and there is an important role for parents.
- Addiction resistance is a more realistic goal than abstinence.

“Beer then liquor, never sicker… Liquor then beer, never fear .” This was a common refrain when I was a Gen X teenager. Besides “Don’t drink and drive,” this was the extent of how I was taught to drink responsibly. Like most kids, most of my knowledge about alcohol and drugs didn’t come from my parents or my school’s alcohol and drug education programs.
Now I am a clinical psychologist, professor of psychology, and mother to three young kids who have a genetic vulnerability to addiction . I’ve spent the past 20 years studying addiction and providing evidence-based addiction treatment. I’ve helped thousands of people better understand the risk and protective factors that influence why one person develops addiction when another doesn’t. I’ve heard countless “If only I had...” stories from parents, students, and people in addiction recovery.
Problems With School Alcohol/Drug Prevention Programs
Each semester that I taught college courses on addiction, I was dismayed by students' lack of basic knowledge about what psychoactive substances actually do in their brains and bodies. They shared their personal experiences with “alcohol/drug education” programs they encountered in their school settings, and these accounts typically share a common refrain—these “prevention” initiatives become jokes, trigger rebellious substance use, or have little to no impact on their substance use decisions.
At worst, prevention programs create shame for people struggling with their substance use and actually impede help-seeking by shutting down communication with adults. Abstinence-only and anti-drug programs cause people to internalize stigmatizing messages like “Users Are Losers,” “Just Say No” (like it’s just that simple and easy for everyone), and “Good Kids Don’t Get High.” Yet they also recognize the disparity between the way that alcohol is discussed compared to other drugs, and that inconsistency leads to confusion.
To receive federal funding, schools must check a box on the annual paperwork stating they deliver alcohol/drug education programming to their students. But there is no metric for what that education includes. So, many schools are able to check that box (and retain their funding) with “Red Ribbon Week” activities like “On Wednesday, wear neon to show you’re too bright for drugs!”
When we talk about addiction prevention, we typically focus on school-based curricula. But that misses two key elements that are critical for helping kids develop the resilience and protective factors they need to combat addiction and other mental health struggles—school policies and parent training. At home, many parents assume their kids are either too young to talk about alcohol and drugs or that the school will provide the essential knowledge their kids need to be “drug-free.”
My parenting tactics are different, and definitely the minority (for now). My 9-year-old knows how to recognize the signs of alcohol intoxication and knows that drugs like methamphetamine can alter one’s perception of reality. I am purposely raising my kids to know that it’s not the substance (alcohol or drugs) that is the problem, but that other factors make some people more vulnerable to substance use becoming dysfunctional. My kids will all know at a young age that since genetic predisposition accounts for 50 percent of the chance of developing addiction, they are 10 times more likely to develop addiction than their friends without a family history of addiction.
Building Addiction Resistance
Why does my 9-year-old know more about the risk factors for addiction than most college students? Because I’m not trying to raise “drug-free” kids . As a clinical psychologist specializing in evidence-based addiction treatment, I’m trying to raise addiction-resistant kids. I fully accept the likelihood that they will use alcohol or other drugs at some point. Instead of trying to scare them out of that choice or build shame and stigma around the addiction history in our family, I am choosing to provide them with the essential knowledge and skills they need to make informed decisions about substance use. Building their addiction resistance gives them the best chance to navigate the hellscape of adolescence with healthy coping skills instead of turning to alcohol and drugs to self-medicate, tolerate distressing thoughts or feelings, or foster a sense of belonging with their peers.
My approach definitely isn’t popular (yet), but I am developing the Raising Resilient and Addiction-Resistant Kids program to provide a viable alternative to abstinence-only messaging. Many parents have trouble stepping outside of the narrative that trained them to think that providing honest education about alcohol and drugs somehow condones their use and leads to a higher risk of addiction, but many others are ready for a different approach.

In a feel-good-all-the-time society like the United States, how can we expect kids and teens to make informed choices about alcohol and drugs if we don’t provide them with the foundational knowledge and skills they need to do so? How can we tell them to “Just Say No" when that message is overly simplistic and fuels stigma against substance users that perpetuates innumerable social injustices in the pursuit of “drug-free communities”?
The “Users Are Losers” message shuts down communication lines between students and educators, and children and parents. We’ve made so much progress destigmatizing mental health struggles like depression , anxiety , autism , and posttraumatic stress disorder, yet we continue to perpetuate the Us vs. Them mentality when it comes to substance use and addiction. Where does that leave kids whose risk factors for addiction outweigh their protective factors?
If we truly want to reduce addiction… If we truly want to reduce drug overdose deaths… If we truly want to “save our kids” from drugs, then we need to stop trying to raise “drug-free” kids and focus on raising addiction-resistant kids instead.
Copyright 2024 Kelly E. Green and Grind Wellness, LLC

Kelly E. Green, Ph.D. , is a psychologist specializing in evidence-based addiction treatment, the author of Relationships in Recovery , and an Associate Professor of Psychology at St. Edward’s University in Austin, Texas.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
United States Drug Enforcement Administration
- Get Updates
- Submit A Tip
DEA Releases 2024 National Drug Threat Assessment
WASHINGTON – Today, DEA Administrator Anne Milgram announced the release of the 2024 National Drug Threat Assessment (NDTA), DEA’s comprehensive strategic assessment of illicit drug threats and trafficking trends endangering the United States.
For more than a decade, DEA’s NDTA has been a trusted resource for law enforcement agencies, policy makers, and prevention and treatment specialists and has been integral in informing policies and laws. It also serves as a critical tool to inform and educate the public.
DEA’s top priority is reducing the supply of deadly drugs in our country and defeating the two cartels responsible for the vast majority of drug trafficking in the United States. The drug poisoning crisis remains a public safety, public health, and national security issue, which requires a new approach.
“The shift from plant-based drugs, like heroin and cocaine, to synthetic, chemical-based drugs, like fentanyl and methamphetamine, has resulted in the most dangerous and deadly drug crisis the United States has ever faced,” said DEA Administrator Anne Milgram. “At the heart of the synthetic drug crisis are the Sinaloa and Jalisco cartels and their associates, who DEA is tracking world-wide. The suppliers, manufacturers, distributors, and money launderers all play a role in the web of deliberate and calculated treachery orchestrated by these cartels. DEA will continue to use all available resources to target these networks and save American lives.”
Drug-related deaths claimed 107,941 American lives in 2022, according to the Centers for Disease Control and Prevention (CDC). Fentanyl and other synthetic opioids are responsible for approximately 70% of lives lost, while methamphetamine and other synthetic stimulants are responsible for approximately 30% of deaths.
Fentanyl is the nation’s greatest and most urgent drug threat. Two milligrams (mg) of fentanyl is considered a potentially fatal dose. Pills tested in DEA laboratories average 2.4 mg of fentanyl, but have ranged from 0.2 mg to as high as 9 mg. The advent of fentanyl mixtures to include other synthetic opioids, such as nitazenes, or the veterinary sedative xylazine have increased the harms associated with fentanyl. Seizures of fentanyl, in both powder and pill form, are at record levels. Over the past two years seizures of fentanyl powder nearly doubled. DEA seized 13,176 kilograms (29,048 pounds) in 2023. Meanwhile, the more than 79 million fentanyl pills seized by DEA in 2023 is almost triple what was seized in 2021. Last year, 30% of the fentanyl powder seized by DEA contained xylazine. That is up from 25% in 2022.
Social media platforms and encrypted apps extend the cartels’ reach into every community in the United States and across nearly 50 countries worldwide. Drug traffickers and their associates use technology to advertise and sell their products, collect payment, recruit and train couriers, and deliver drugs to customers without having to meet face-to-face. This new age of digital drug dealing has pushed the peddling of drugs off the streets of America and into our pockets and purses.
The cartels have built mutually profitable partnerships with China-based precursor chemical companies to obtain the necessary ingredients to manufacturer synthetic drugs. They also work in partnership with Chinese money laundering organizations to launder drug proceeds and are increasingly using cryptocurrency.
Nearly all the methamphetamines sold in the United States today is manufactured in Mexico, and it is purer and more potent than in years past. The shift to Mexican-manufactured methamphetamine is evidenced by the dramatic decline in domestic clandestine lab seizures. In 2023, DEA’s El Paso Intelligence Center (EPIC) documented 60 domestic methamphetamine clandestine lab seizures, which is a stark comparison to 2004 when 23,700 clandestine methamphetamine labs were seized in the United States.
DEA’s NDTA gathers information from many data sources, such as drug investigations and seizures, drug purity, laboratory analysis, and information on transnational and domestic criminal groups.
It is available DEA.gov to view or download.
- Open access
- Published: 11 May 2024
How do we understand the value of drug checking as a component of harm reduction services? A qualitative exploration of client and provider perspectives
- Lissa Moran 1 ,
- Jeff Ondocsin 1 , 2 ,
- Simon Outram 1 ,
- Daniel Ciccarone 2 ,
- Daniel Werb 3 , 4 ,
- Nicole Holm 2 &
- Emily A. Arnold 1
Harm Reduction Journal volume 21 , Article number: 92 ( 2024 ) Cite this article
234 Accesses
Metrics details
Mortality related to opioid overdose in the U.S. has risen sharply in the past decade. In California, opioid overdose death rates more than tripled from 2018 to 2021, and deaths from synthetic opioids such as fentanyl increased more than seven times in those three years alone. Heightened attention to this crisis has attracted funding and programming opportunities for prevention and harm reduction interventions. Drug checking services offer people who use drugs the opportunity to test the chemical content of their own supply, but are not widely used in North America. We report on qualitative data from providers and clients of harm reduction and drug checking services, to explore how these services are used, experienced, and considered.
We conducted in-depth semi-structured key informant interviews across two samples of drug checking stakeholders: “clients” (individuals who use drugs and receive harm reduction services) and “providers” (subject matter experts and those providing clinical and harm reduction services to people who use drugs). Provider interviews were conducted via Zoom from June-November, 2022. Client interviews were conducted in person in San Francisco over a one-week period in November 2022. Data were analyzed following the tenets of thematic analysis.
We found that the value of drug checking includes but extends well beyond overdose prevention. Participants discussed ways that drug checking can fill a regulatory vacuum, serve as a tool of informal market regulation at the community level, and empower public health surveillance systems and clinical response. We present our findings within three key themes: (1) the role of drug checking in overdose prevention; (2) benefits to the overall agency, health, and wellbeing of people who use drugs; and (3) impacts of drug checking services at the community and systems levels.
This study contributes to growing evidence of the effectiveness of drug checking services in mitigating risks associated with substance use, including overdose, through enabling people who use and sell drugs to test their own supply. It further contributes to discussions around the utility of drug checking and harm reduction, in order to inform legislation and funding allocation.
The opioid crisis in the U.S. consists of multiple overlapping and inter-related waves of surging opioid exposure, dependency, overdose, and death rates. Each wave has emerged from different eras of an evolving drug market and multiple intersecting contextual factors such as trends in pharmaceutical manufacturing and prescription, socioeconomic inequities, and positive supply shocks of both licit and illicit opioids [ 1 , 2 , 3 ]. Though its history can be traced back to the 1980s and 1990s, the past decade has redefined the crisis [ 4 ].
By the time the U.S. Department of Health and Human Services (HHS) declared the opioid crisis a public health emergency in 2017 [ 5 ], a wave of unprecedented magnitude had been on the rise for nearly 4 years, marked by the rapid proliferation of fentanyl and synthetic analogues into the drug market [ 4 , 6 ]. Even as mortality from heroin and prescription opioids leveled off or decreased, opioid overdose and death rates rose precipitously [ 6 ]. From 2018 to 2021, the rates of opioid overdose deaths in the U.S. nearly doubled, and by 2021, roughly 9 out of every 10 opioid overdoses in the country (88%) were fentanyl-related [ 7 ].
In California, home to the highest number of opioid-related deaths in the U.S. [ 8 ], the opioid overdose death rate curve from 2011 to 2021 tells a harrowing story. The third wave was later to arrive in California than the national average, but its onset was rapid and dramatic. Opioid overdose death rates more than tripled from 2018 to 2021, and synthetic opioid (e.g., fentanyl) deaths increased 7.2 times, responsible for 37% of opioid overdose deaths in 2018, and 86% just three years later [ 9 ].
In response, the California Department of Public Health has committed to the expansion and promotion of policies, programs, and services to combat the overdose epidemic, with a special focus on harm reduction and drug checking strategies [ 10 ].
Drug checking services
Drug checking services (DCS) have garnered particular interest as an expansion of harm reduction strategies, as they offer the opportunity for people who use drugs to test the chemical content of their own supply [ 11 , 12 ]. In doing so, people who use drugs may be afforded the possibility of changing their use behavior to remove or reduce the likelihood of harm [ 13 , 14 ]. Multiple DCS have been operating in Europe for years—particularly in venues known for high rates of recreational drug use like music festivals [ 14 , 15 ]—but are less common in North America. In the U.S. and Canada, DCS have emerged primarily in response to the needs of marginalized people who use opioids, and operate predominantly within the context of frontline services [ 16 , 17 , 18 ].
Though not mainstream or broadly implemented, studies from North America indicate that DCS are generally acceptable among people who use drugs [ 19 , 20 ], and report that both service users and providers have expressed desire for better access to DCS, legal protections for those providing and using drug checking, and advanced technologies that provide information on drug concentrations—not just drugs present—at the point of care [ 21 , 22 , 23 , 24 ]. Several studies explore the potential impact of drug checking when used at various points along the supply chain [ 25 , 26 ], with findings that suggest feasibility, acceptability, and uptake of DCS among drug sellers [ 27 ], noting particular importance to drug sellers who are embedded in their community and hold long-term trusted relationships with customers [ 28 , 29 ].
Arguably the most common and well-known drug checking modality in North America are fentanyl testing strips (FTS), or lateral flow assays, which were originally designed for the clinical use of detecting fentanyl in urine samples, but have been publicly available for several years for modified use with drug samples [ 30 , 31 , 32 , 33 ]. FTS have been a powerful tool to combat accidental fentanyl exposure: they are small, portable, relatively accessible, and detect fentanyl in minute concentrations that could still be enough to trigger an overdose in an opiate-naïve individual [ 31 , 34 ]. They have been found to be particularly useful for outreach and street use [ 13 , 25 , 35 ]. That said, FTS are not useful in the same way for those who intend to use fentanyl, where the overdose risk is not in the presence of fentanyl, but in the concentration and presence of additional adulterants like sedatives [ 36 ].
Drug checking technology has advanced, and continues to advance, such that a greater amount can be known about the chemical components of a drug sample in a shorter period of time, in a broader array of environments [ 37 ]. Multiple drug checking modalities can inform people who use drugs about the presence of unexpected adulterants, such as benzodiazepines and xylazine, among others. Technologies that offer the greatest specificity and sensitivity include Gas Chromatography Mass Spectrometry and High-Performance Liquid Chromatography, which can detect the presence and concentrations of a wide array of chemicals present in even small amounts in a sample, but must be used in a laboratory setting by a trained technician [ 37 ]. More flexible technologies have emerged, like Fourier-Transform Infrared Spectroscopy (FTIR) [ 38 ], which is semi-portable, and returns information on the main chemical components of a drug sample (above 5% concentration) in a matter of minutes [ 31 ]. Paper spray mass spectrometry is more expensive than FTIR but is just as fast, and provides quantitative results [ 39 ]. Today, multi-technology-based drug checking services are available in some areas as standalone programs, or as added components to existing harm reduction centers [ 30 , 40 ].
These innovations continue to advance amidst complex and evolving social, legal, political, and funding conditions [ 11 , 21 , 41 , 42 ]. Legally, drug checking can be complicated as a public service, requiring the handling and, often, exchange of illicit drug material, of which possession and distribution is often criminalized [ 21 ]. Harm reduction initiatives more broadly—DCS, syringe access services, naloxone distribution, HIV/HCV testing, wound care, supervised consumption sites, and medications for opioid use disorder (MOUD), among others—can at times be unpopular socially and politically, as stigma associated with addiction and drug use combined with concerns about the goals and practices of harm reduction can generate powerful community pushback [ 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Legislators and policymakers at local, state, and federal levels who rely on constituent support may therefore shy away from supporting various harm reduction strategies, despite endorsement from public health officials and robust evidence showing that harm reduction improves the health, survival, and recovery potential for people who use drugs, without compromising community safety [ 48 , 49 ]. At the same time, California was one of several states to bring lawsuits against opioid manufacturers, distributors, and pharmacy chains, alleging that they played an active and/or negligent role in the genesis and exacerbation of the opioid crisis [ 50 ]. Of the $43.3 billion in settlement funds that have been awarded thus far, California may receive nearly $4 billion [ 51 ]. These funds are specifically earmarked for activities that are to include “prevention, intervention, harm reduction, treatment and recovery services.” [ 52 ].
As the opioid crisis reaches an unprecedented magnitude and strategies to address it are at once both a priority and a topic of controversy, we aimed to explore the value of drug checking services and their role within harm reduction more broadly. In this study, we report on qualitative data from providers and clients of harm reduction and drug checking services, to explore how these services are used, experienced, and considered. We aim to contribute to an existing qualitative evidence base exploring the value and utility of drug checking services, particularly as data are leveraged to inform political narratives, legislation, and funding allocation.
For this study, we conducted in-depth semi-structured key informant interviews across two samples: a “provider” sample and a “client” sample. The “provider” sample consisted of individuals providing clinical and harm reduction services to people who use drugs, as well as drug checking subject matter experts such as researchers and program heads. The “client” sample consisted of individuals who use drugs and were receiving harm reduction services at an agency where multiple forms of drug checking were included in the services provided.
From June to November 2022, two authors (DC & LM) conducted in-depth semi-structured key informant interviews with 11 providers—8 working in the U.S., 2 working in Canada, and one working in both countries. Included in the sample were 2 clinical providers, 4 researchers, and 5 harm reduction service providers [Table 1 ].
We employed purposive sampling of known providers first, then snowball sampling, contacting additional potential participants at informants’ recommendation. All potential participants were contacted via email and invited to participate. If the participant agreed, an appointment was made for the interview to take place over Zoom. Interviews lasted between approximately 45 and 60 min, and solicited provider perspectives on the state of the drug market in their area, the perceived needs of and challenges faced by their local client population, and their attitudes and experiences with drug checking methods and programs and integrating such programs into existing services. Verbal consent was collected at the outset of the interviews, which were then recorded. Audio from the recordings was isolated and transcribed using a secure third-party professional transcription service. All transcripts were deidentified and researchers created unique anonymous ID numbers for each participant. Participating providers were offered an honorarium of $100 in the form of a gift card. The study protocol was reviewed by the University of California San Francisco Institutional Review Board (IRB #22-36262).
Client participant ( n = 13) recruitment and data collection took place over a one-week period in November 2022 [Table 2 ].
We employed a non-random convenience sample, recruiting from four harm reduction programs in San Francisco, where clients were approached either by interviewers (NH & JO) or program staff who had been instructed on eligibility requirements. Eligible participants were at least 18 years of age, and currently using fentanyl, heroin, or methamphetamine. Clients were excluded from eligibility if they were intoxicated or otherwise unable to provide informed consent. Given that current drug use was an eligibility requirement, we assessed “intoxicated” as an inability to respond to simple questions, providing responses that are incoherent or unintelligible, or if the participant indicates that they are too high to continue. Potential participants who were eligible and interested were then formally verbally consented and interviewed on-site. Client interviews explored participants’ history of drug use and experiences with harm reduction services, as well as their awareness of, attitudes about, and experiences with various drug checking modalities. Interviews lasted approximately 30–60 min and were recorded, then submitted to the same external third-party transcription service being used for provider interviews. Participants were provided a $25 cash incentive as a token of appreciation for their time and expertise, and were provided unique ID numbers to anonymize their data. This study protocol, distinct from the protocol covering provider interviews, was reviewed and approved as well by the UCSF IRB (#22-36640).
Client interview transcripts were uploaded to Dedoose, a qualitative analytic program [ 53 ]. Four analysts (EA, LM, SO, and JO), two of whom were involved in data collection (LM & JO), read transcribed interviews from both client and provider data sets and drafted summaries which were then systematically reviewed as a team. Following the tenets of thematic analysis and adopting the framework developed by Miles and Huberman (1994) [ 54 ], the team collaboratively identified cross-cutting themes from interview summaries, covering areas of concordance, discordance, and particular importance, as well as exemplar and negative cases. Once major themes and sub-themes were identified and articulated, authors drafted analytic memos which consolidated and explored in detail each major theme.
Following publication of an article focused on findings from the provider data set [ 55 ], further analysis of the client data set included the development of a formal coding scheme (SO), based on a priori codes extracted from the interview guide, as well as codes reflecting themes and sub-themes identified in the summarizing process and further refined via ongoing weekly analytic meetings. Coding was led by the primary qualitative analyst [SO] with secondary coding by client interviewer and author [JO]. The application of codes was discussed regularly among all team members, focusing on discrepancies between primary and secondary coders, insights developed, and the potential emergent themes. Discrepancies occurred approximately 10% of the time, and these were resolved through group consensus in accordance with established qualitative research methods [ 56 ].
Through key informant interviews, we captured diverse perspectives on how existing and emerging drug checking services are being used, and their potential for future impact within the harm reduction suite of services.
We present our findings within three key themes: (1) the role of drug checking in overdose prevention; (2) benefits to the overall agency, health, and wellbeing of people who use drugs; and (3) impacts of drug checking services at the community and systems levels.
The role of drug checking in overdose prevention
Service providers and clients expressed varying opinions on the extent to which information from drug checking services would prevent overdose and, indeed, whether overdose prevention is the appropriate metric by which drug checking’s impact should be measured. Clients reported diverse experiences and perspectives on how they use (or don’t use) drug checking, and expectations for their own future use.
Fentanyl test strips
Almost all client participants reported having had some experience with fentanyl testing strips (FTS), either using them personally or seeing others use them. Attitudes about FTS varied. Some expressed concern that they are difficult to use correctly or that they have heard they may be unreliable (prone to false positives or negatives):
We were using them constantly when they were telling us that all the drugs had fentanyl in them. But then we found out that if you don’t put enough water on speed, that it can come up positive because of some chemical. [Client, 40, female].
Others reported relying on them heavily and using them often:
I’ve just got to have that insurance that there’s no fentanyl in [my drugs]. … I have a drawer. Like that? That’s all full of test strips. Usually every time I come to a needle exchange, if they have them, I grab as many as I can and just put them in the drawer. [Client, 43, male].
Spectrometry
Although many had not heard of spectrometry, spectroscopy, or anything beyond FTS, once it was described what a range of drug checking services could look like, clients were interested and excited about the possibilities. Some expressed interest in using mobile or site-based spectroscopy, but were concerned about their safety, one expressing worry about “ judgment from the community ” or bystanders taking videos and calling the police, another wondering if they would be an “ easy target ” for law enforcement harassment. Those who reported having used FTIR as part of their harm reduction visits, however, had positive things to say:
Interviewer: And how do you feel about that testing service at the van? Participant: I think it’s remarkably great. Interviewer: yeah? Participant: Yeah. They answered my questions, exactly what I wanted to know. [Client, 66, male]
Some participants described high percentages of testing experiences coming back with a positive or unexpected result, like a client who said that he’d used the FTIR mobile service four times with meth from four different suppliers, and “ only one came back pure .”
Using drug checking results
What participants reported doing with the results of checking their drugs varied as well. Some participants spoke about specific situations where drug checking prompted them to avoid buying contaminated drugs.
Actually I just used [drug checking] yesterday. Luckily, I didn’t buy the heroin I was going to, because it tested for fentanyl . [Client, 32, male]
Other community members expressed disinterest in checking drugs, often citing a lack of realistic options for using test results in a way that made sense for them. One participant stated directly that they didn’t want to test because they didn’t want to have to not use drugs if they got a result they didn’t like:
What if it comes up with fentanyl in it? Then I bought it but I can’t do it? They’re not going to take it back, the people I bought it from. I mean even if I get them to write me a receipt, you know? [Client, 49, male]
Another client said that she was interested in drug checking generally, but wouldn’t bother if she only had a little bit and was relying on it to keep her from getting sick:
If I was trying to [check my drugs], I would do it when I had enough to do that, you know. Because if I was dope sick and I only had two hits of fentanyl, I probably would not [test]. [Client, 24, female]
Data from service provider interviews echoed these dynamics. We heard from provider participants that, broadly, drug checking services prevent overdose directly some of the time, but not all the time, by way of individual behavior change on a case-by-case basis. One provider—a clinician with a lengthy career in addiction medicine and harm reduction—echoed doubts about how common it would be for a patient to make use choices based on drug checking results, broadening the focus to personal harm reduction behavior change rather than abstinence behavior alone:
And then the question is, what do you do about it? I’ve had a patient who is, like, yeah, I tested it. It was positive for fentanyl. I go, well, what did you do? Well, we just used anyway because it’s all we had. And we had, like, the Narcan out, and I – I just felt really sleepy afterwards. … So I guess that’s the other question – if you do drug testing and it isn’t what you expect, like, you can’t take it back to the dealer and say, hey, this isn’t – I want a refund; right? So what do you do with that information? And if, you know, if you’re in withdrawal and you really need to use that drug, like, what kind of safeguards are you going to take if you decide, yeah, I’m going to go ahead and use this; right? [Clinician, U.S.]
Other service providers similarly drew a distinction between drug checking sparking behavior change that prevents overdose versus behavior change that reduces the risk of death from overdose, situating drug checking services as a set of tools that dovetail with existing personal harm reduction strategies.
The reality is, you know, people still are using their drugs. Now, a large proportion of people who use our service say that they’ll do something differently after, you know, accessing our service, so they maybe will do a test dose first, or start, like, start with a smaller dose, or use with a friend, or use at an SCS [supervised consumption site]. [Direct service provider, Canada].
Overdose prevention versus overdose rates
Interestingly, many service providers when asked for their perspective on the role of drug checking services in overdose prevention expressed concern about a gulf between the overdose prevention they observe at the service level versus what they see represented in population-level data.
Will drug checking save a life? Absolutely. Yes, for sure. Will it, at a population level, drop overdose rates? I don’t know the answer to that. [Researcher, U.S.]
Participants offered multiple explanations for this. One described challenges inherent in proving prevention, while another explained how population overdose rates can obscure the impact of drug checking programs when they operate within a rapidly-changing drug supply:
It will be very hard to prove within these prevention paradoxes. I think prevention is one of those things that is so important, but within our scientific frameworks … preventable events are so rare and on the grand scheme of things, they’re really hard to prove. … But will [DCS] save lives? Yeah. [Clinician, U.S.] The numbers aren’t showing [an overall decrease in overdose], right, because at the same time, even though we’re offering this service, the supply is just getting worse and worse, so overdose rates are rising. [Direct service provider, Canada].
Not every participant who commented on this gulf found it to be wide or troubling, but instead remarked on it as a neutral distance between two related but distinct constructs, one of which is a measure of what outcomes drug checking information could yield, and the other of which is a fundamental right to that information.
It’s really a great question if we’re going to see things pan out in the numbers. I certainly hope so and I certainly think so, but I think that we just have the right to know what we’re putting into our bodies, regardless of what outcome measures are. We deserve to know what’s in our drugs . [Direct service provider, U.S.]
Similarly, a direct service provider offered a structural perspective on overdose prevention, decoupling the value of drug checking services from overdose outcomes, prioritizing instead the intrinsic value of equipping people with critical information about what they are putting in their body and the importance of empowering people to make decisions with as much information as possible.
I don’t really know if [drug checking] is going to decrease the rate of overdose. In my mind, the problems that contribute to overdose are prohibition, law enforcement harassment, and everything that surrounds that that creates a shitty drug supply and then prevents people from investigating it. But what [drug checking] does do, again, is this piece around like, people should know that they can find out there’s more in their drug. … I think that it just enables people to make better educated decisions around their substance use and to understand their bodies better . [Direct service provider, U.S.]
Benefits to the overall agency, health, and wellbeing of people who use drugs
Drug checking services offer users the tools to independently identify risks in the drug supply and make decisions about what to do with that information in the short and long term. Many of the service providers interviewed for this study, when asked how drug checking would impact overdose rates, gave some version of a reframed response, repositioning the focus from the drug use decisions themselves to the importance of information in fortifying the overall agency, health, and wellbeing of people who use drugs.
The provider quoted in the above section went on to reflect on the intrinsic value of giving people information, arguing that it contributes to essential experiences of bodily autonomy and health equity:
What’s really important to me as well is just sort of building this momentum around people feeling entitled to bodily autonomy and seeing that [drug checking] is a part of [that], and having folks know that, yeah, they fucking deserve to have this information. They are entitled to know what is in their stuff. And so, that’s not the only piece to health equity and justice around substances and substance use, but I think that it’s a significant piece. [Direct service provider, U.S.]
Knowledge of what is in their drugs can also confirm users’ internal experience. One provider, who had piloted an early drug checking intervention in a major metropolitan area in the U.S., believed that drug checking for people who use drugs offers confirmation of the embodied experience of their substance use, which in this provider’s experience was often regarded with skepticism by health workers:
I think that people are able to connect experiences that they’re feeling in their body with real information. And I think that actually validates the really organic knowledge and experiential knowledge of drug users as the true experts about drugs. You know, when we were doing our project in [city] and fentanyl was not everywhere [yet]—almost 100% of the time, if someone brought us a sample and said, “I think this has fentanyl in it,” it was true. … It validates experience where people’s experiential knowledge is not really validated by an educational system. It’s always this kind of thing where public health people are telling drug users what’s true. And drug checking sort of validates that drug users actually know what’s true, and we’re just using science to confirm it.” [Direct service provider, U.S.]
Client interviews echoed this theme. Several clients recounted experiences that illustrated how navigating the drug market is becoming increasingly difficult, and that drug checking provides an important tool that they can pair with their own instincts and expertise as they try to keep themselves safe.
I can look at it and I can be like, “Wait a minute, we might want to test that.” Because speed and fentanyl are different. They actually look different than the other one, so when I start seeing traces of fentanyl being in the speed, I go, “We need to check that before we do any of it.” And, hey, sometimes I’m wrong. [Client, 43, male] The [meth] that was in the medicine bottle [tested positive for fentanyl], yeah. But I kind of knew it was going to because I packed a bowl right before and if it’s dirty … yeah, the color starts changing wrong right away. [Client, 43, male] I like that [drug checking] gives us some certainty of what’s in the drug … like with the heroin, there was stuff in that that just did not feel good. I’d love to know what they were cutting that stuff with. We used to joke it was shoe polish because it was so dark and dirty, but it’s really important what you put in your body . [Client, 48, female]
Our client data further provide evidence that people who use drugs are making health-related decisions for themselves and care about their own health and wellbeing. Woven throughout community member interviews were examples of health-seeking decision-making in users’ everyday lives, demonstrating agency in considering health behaviors and expressing both implicitly and explicitly a desire to care for themselves. Examples of these pro-health micro-decisions include choosing not to smoke out of foil (it’s “ not healthy to smoke out of ” and “ it’s going to give us Alzheimer’s or something ”) or reducing smoking marijuana due to a “ sensitive ” respiratory system. One informant laid out explicitly their hopes for their future, shaped too by an acute awareness of the risks of the current drug market:
I don’t want to be a statistic out here. I want to go back to regular life and experience all the rest of the highs that there still are out there before I die. I want to jump out of an airplane, or take a balloon ride, or ride more rollercoasters. … I don’t want to limit myself to one freaking high. … it’s not worth it anymore at all. … You’d never OD on meth before. Meth and weed were two things you just didn’t overdose on. If you did too much, you passed out and you slept it off and that was it. Now, no matter what drugs you’re doing, every time you use, it’s a 50–50 chance that you could die. [Client, 49, female]
These excerpts from client interviews highlight the demand among potential DCS users for strategies that contribute to their agency, health, and wellbeing, even within the context of continued drug use in the short- or long-term.
Impacts of drug checking services at community and systems levels
In addition to use at the individual level, participants talked extensively about the ways that they experience and imagine DCS having an impact at community and systems levels. They described the ways that drug checking could facilitate upstream regulation of the drug market, how the information and transparency made possible by checking drugs can fill a policy and regulatory vacuum, and how drug checking can empower public health surveillance systems and clinical response.
Community level regulation of the drug market
Multiple informants, both service providers and clients, reflected on the use—or potential use—of drug checking as a grassroots tool to regulate the drug market.
Participants talked about using, or thinking one could use, DCS as a vetting tool for sellers or suppliers.
And if people could get their shit tested, almost every time if not every time, not only would it help them to be safer by them regulating themselves and knowing what’s in their stuff … But I feel like if they knew exactly what was in it, they could go tell their guys that they got it from, “Look, man, I’m not buying that shit anymore if it’s like that. If that shit -- if this or that’s in it or whatever. Or if you don’t, whatever, I’m not buying it from you. I’m buying it from someone else.” And that might even make them be… It’ll hold them more accountable. [Client, 32, male]
This use was so important to one participant that they expressed interest in their samples being sent for more extensive in-lab spectrometry testing that could give them greater detail about the compounds and amounts in their sample:
Hey, [a full spectrometry report] may take a week, but at least in that week, I find out if I should go back to that person or not. [Client, 43, male]
Client participants frequently referred to DCS as a tool to “keep [suppliers] honest”; that is, as informal regulatory pressure on currently unregulated illegal drug markets. Some reported that they spread the word if drugs from a supplier come up contaminated or low-grade. One participant, who uses fentanyl, reported using FTS to ensure that what they are about to buy is, indeed, fentanyl:
I keep them [FTS] around. … Then I say, “Can I test it?” and I test it in front of them. And like some of it’s turned up negative. And so I totally outed them out on the block with it. It pisses them off – it kind of keeps them honest. … When you got a bunch of test strips, I can go down the line and keep, yeah, at least trying to keep them honest, you know. I got a pile of those things right now. That’s actually what I use them for. [Client, 40, male]
Of particular value, according to our participants, was the idea that spectrometry would provide formal documentation of drugs’ contents. Analytical evidence that something was either dangerously contaminated or not what the seller claimed it to be can shift the balance of power in the transactional dynamic, placing upstream pressure on suppliers to better monitor what they are contributing to the market.
If you could get results that are on paper or on a text or on a whatever, then you could bring it to them that, “Look, dude. I’m not fucking around. You need to make this shit right or I’m not buying it anymore.” That would be a game-changer . [Client, 32, male]
From the service provider standpoint, one participant, a drug checking technician and program manager with a longstanding history in their city’s drug scene, identified similar opportunities for DCS to impact the drug market, were it made easily accessible to those at multiple points in the drug supply chain in addition to consumers.
It’s not just people who are consuming the drugs that can use the service. It’s also people who are selling them. And so, oftentimes people who are not essentially the first or second hands that are creating the substance and then moving it down the chain towards the end consumer, they don’t know what is in their product. For folks who are selling drugs, if they’re able to come and get an ingredient list, they can then kind of know what to say to folks who are buying. [Direct service provider, U.S.]
This was not discussed as just a hypothetical. One informant who sells drugs validated this use as feasible and valuable:
I want to make sure what I’m buying is what it is. … I do sell it myself, so [spectrometry]’s a good service because that’s what I want to know is the chemical balance as to how much it is and how much it isn’t and whether it’s good every time. [Client, 66, male]
Filling a policy and regulatory vacuum
In the absence of a government or regulatory body that will monitor and report on the verified contents of illicit drugs, our data suggest that drug checking services, and spectrometry in particular, may be filling a policy and regulatory vacuum.
Clients likened the idea of having access to a list of drugs present in a sample to knowing ingredients of something that they would eat.
I mean we know what’s in our food, right? The packaging is all labeled and the ingredients are listed. It’s just too important, especially with drugs. Especially because we don’t know who’s making them. We don’t know exactly where they’re coming from. And every single one is different. Every week is different. Even if you buy it from the same person all the time, they’re always having something different. Maybe you’ll have the same thing twice or three times but that’s it. [Client, 48, female]
Providers, meanwhile, explicitly framed the value of drug checking within the context of an unmet regulatory need. One service provider qualified many of their statements about drug checking services with “until prohibition goes away,” situating DCS as being necessary only in a regulatory vacuum. Another spoke more directly to the relationship between drug checking and regulation:
And with drugs, because of prohibition, we just have this unknown, unregulated supply, and people are – what they’re putting in their bodies and what they’re purchasing is obscured, right? And so, drug checking is like a series of sort of imperfect tools to help consumers of drugs regain a little bit of control in the form of information around what it is that they are using. …. And there’s a very good argument that, if we had some kind of safe, regulated supply, we wouldn’t need drug checking at all, which is true . [Direct service provider, U.S.]
Empowering public health surveillance systems and clinical response
Data from our interviews suggest that drug checking technologies and programming may also contribute meaningfully at a structural level, to public health surveillance systems and clinical response. Aggregated sample results provide real-time data about what drug compositions are trending across regions, and what the clinical implications may be for providers treating clients who use drugs [ 57 ]. One drug checking program team posted results to their website in the hopes of informing local clinicians and public health policy makers about what was circulating in the drug supply. This program manager talked about making results available “at the societal level”:
And then at the kind of societal level what we do … [is] every other week we take all of the results from the samples that we’ve checked, and we combine them, and then we put out a report and update our website about, like, what’s circulating in the drug supply. So we talk about, you know, trends in the drug supply over that period, and new drugs that have been introduced, and what those drugs could mean, that type of thing. So service doesn’t only benefit individuals, but it also benefits the larger community by being able to say, okay, this is what we’re seeing. If you can’t access the service, you still at least know, you know, what is circulating. [Direct service provider, Canada]
Community members expressed an awareness of this function. One participant cited drug checking’s role in a larger tracking network as one of the things they value most about the service:
I liked a lot about [drug checking]. One, that it was available in the first place. Two, that it was not just doing its own thing. It was part of a larger network that was keeping track of what drugs were popping up on the streets and what their makeup was. I really like that that’s happening. [Client, 30, male]
At the point-of-service level, provider informants discussed significant benefits that drug checking could provide to clinicians and other medical professionals who work closely with people who use drugs. This informant posited specifically that having more detailed knowledge about what was circulating in the drug supply could help clinicians better formulate strategies for managing opioid use disorder and transitioning patients onto MOUD:
Understanding what’s actually in the supply… allows clinicians to tailor the care that they are providing to people who use drugs. So, you know, if they know that the average amount of fentanyl in a fentanyl sample is this and they want to transition someone off the unregulated drug supply onto, like, a pharmaceutical alternative, well, what pharmaceutical alternative is actually suitable based on what they’ve been using? [Direct service provider, Canada]
This is especially critical given the significant difficulties that have been recently reported when transitioning people using fentanyl to appropriate longitudinal services [ 58 ]. A provider we interviewed who runs a mail-based drug checking service in the U.S. reported that developing a more thorough knowledge of the drug supply outside of the current surveillance panoply may provide important clinical toxicology assistance to help physicians connect health outcomes to specific substances or components of the drug supply, and more quickly provide tailored treatment:
There’s one other really big one for me, which is that it allows us to link specific physiological harms with specific chemicals. So, we’re not just talking about dope anymore. We’re talking about this component of dope causing this specific reaction. What we have been able to do is, we’ll get calls from our central hospital on campus, and they’ll say, “We have this patient with an idiosyncratic presentation. Boom, boom, boom, boom, boom, boom. Here it is. We think it might be… You know, they’ve been injecting this, this, and this. We have some of their samples. Can we get them tested?” Or if they don’t have the samples, they’re like, “This is what the symptoms are. This is where they’re from. What are you seeing about the drug supply in their area?” And I can be like, “Well, yeah, there’s been a spike in levamisole in that area or xylazine,” you know, whatever it is. And then they can get to treatment quicker because the physicians have a more specific knowledge about the ideology of the harm that they’re observing in clinic. [Researcher, U.S.]
Negative cases
While the vast majority of participant responses reflected positive experiences with or attitudes about DCS, some participants additionally expressed ambivalence or concern. Many of these perspectives are embedded within the themes reported above, but deserve reiteration: service users expressed concerns about the accuracy of drug checking technologies, their privacy and safety relative to community stigma and law enforcement, and anxiety about having to make hard choices about drug use in the face of an unexpected result. Service providers expressed concern about the “then what” of drug checking, citing constrained choices and limits to what could be realistically expected in terms of behavior change without other supports in place. Some further lamented the challenges of translating the benefits of what they were seeing in practice to what is visible to a broader audience.
Not included in the above findings, but important to note, are two additional concerns that arose in interviews. First, service users and providers cautioned that the street drug supply changes so quickly that new compounds may be showing up on the street before they are identified in spectrometry libraries, potentially limiting their ability to accurately identify contaminants. Finally, one provider, a clinician with a longstanding career in addiction medicine and harm reduction, closed their interview with a somber caution against decontextualizing drug checking from a broader commitment to multi-method harm reduction, health equity, and social justice.
[I worry that] we’re just throwing yet another technology at a much bigger problem. My fear is that people will say, oh, now we have drug checking, so now we can stop trying to dismantle, you know, structures of racism and oppression in society, right? We can stop looking for homes for people because we have this technology that’s going to prevent people from dying. … It doesn’t work that way. [Clinician, U.S.]
While the magnitude of the opioid crisis is often communicated in terms of overdose and death rates, the harms associated with opioid use—intentional or unintentional—in an unregulated drug market extend far beyond those data points alone, and so too must the strategies leveed to combat them. Our findings demonstrate that drug checking services offer diverse benefits at the individual, community, public health, and health systems levels.
Overdose prevention and beyond
If the question is, do and will these technologies contribute to overdose prevention , our findings suggest that the answer is yes, with some important caveats. The first being that, according to our participants, they do not prevent overdose all the time. Our findings reflect that individuals make complex and highly contextualized decisions regarding their use behavior each time they use drugs. Information about the chemical composition of a drug sample sometimes leads to decisions to abstain, but more often leads to decisions to engage in other types of harm reduction behaviors—like using with a friend rather than alone, making sure to have naloxone on hand, using at a supervised consumption site, alerting others to a bad batch, using a tester first, or avoiding a certain supplier in the future. Sometimes it leads to no observable behavior change at all.
Further, DCS have not been scaled up to meet the needs of everyone at risk for overdose; until it is, it is premature to discuss population-level prevention. This study does not purport DCS to be in and of themselves sufficient to prevent overdose, but they are clearly part of a continuum of services that can prevent overdose mortality.
Many participants took care to note as well that the needs of people who use drugs are not solely to avoid overdose; people navigating drug use are whole people, and the stigmatization and criminalization of drug use regulates their access to a multitude of essential needs and liberties, like health care, housing, employment, agency, and a host of social and legal protections. Access to information that contributes to agency and autonomy, and enables more informed decision-making, is an essential service regardless of other outcomes.
Of course, among harm reductionists and researchers acquainted with the diverse and dynamic ways that harm reduction functions within communities, this is not news. Our findings reflect and reinforce much of the existing evidence from studies aiming to understand the role of drug checking within the larger constellation of harm reduction and, indeed, the role of harm reduction itself.
One recent qualitative study in particular reported themes with striking similarities to the prevailing themes from our interviews. Wallace et al. [ 59 ] explored the potential impacts of community drug checking on prospective service users, finding drug checking to “increase quality control in an unregulated market,” “improve the health and wellbeing of people who use substances,” and “mediate policies around substance use.”
Our findings further add to existing evidence that links drug checking with consumer empowerment within an opaque drug market [ 25 , 26 , 29 ] and underlines the reciprocal relationship between individual agency and the adoption of harm reduction strategies [ 46 , 60 , 61 ].
Of note is the shifting context in which many existing drug checking studies, including ours, are situated. In some areas, fentanyl appears most often as an unwanted adulterant in another drug—be it a non-opioid or a less potent opioid like heroin—and DCS are used primarily for fentanyl avoidance [ 13 , 19 ]. Increasingly, however, pockets of consumers are preferring fentanyl, as seen in our San Francisco client sample and within populations reflected in recent drug checking studies. Our data echo the broader finding that drug checking technologies are likely to be used differently by fentanyl-seeking opioid users versus fentanyl-avoiding opioid users, and differently still among those using stimulants, psychedelics, or other non-opioid drugs [ 22 , 62 ].
On the subject of behavior change—whether and how drug checking can be understood to prompt changes in drug use behavior—our findings align with existing evidence showing that drug checking is at times followed by contaminated drug disposal, and at times followed by the employment of personal harm reduction techniques such as spreading information within the community [ 30 , 63 ], and reduction in polysubstance use or dosage [ 13 , 14 , 15 , 64 ]. Lacking as we do a robust methodological-empirical foundation to assess this type of causality, whether and to what extent drug checking in various contexts leads to less use or more safe use among different populations cannot be stated concretely [ 16 , 65 , 66 ]. Whether individuals change their use behavior based on drug checking results is highly informed by such matters as how limited their access to drugs is, realistic options for modified use, and their perceived relative risks of knowingly ingesting a potentially dangerous compound or compounds versus not.
The tension at the center of harm reduction policy
The role of harm reduction services within communities have long reflected a central tension: in contrast with abstinence and criminalization models, harm reduction is often socially and politically criticized as enabling drug use and making neighborhoods less safe [ 67 , 68 , 69 ], while research consistently finds harm reduction to yield positive outcomes for both service users and surrounding communities [ 70 , 71 ]. In addition to improving the health and wellbeing of people using drugs, evidence suggests that those accessing harm reduction services are more likely to ultimately seek treatment and pursue recovery [ 49 , 70 , 72 , 73 ]. Concerns about public safety, too, while in many cases expressed in good faith, have been shown to be largely misplaced: multiple studies show harm reduction programs to have no significant impact on nearby violent or property-related crime, with some findings suggesting improved indicators of public order and safety [ 48 , 49 , 74 , 75 ]. Harm reduction strategies have additionally been found to be cost-effective in the short term and cost-saving to public monies in the medium- and long-term [ 76 ]. Nonetheless, public perception of harm reduction has historically been interwoven with deeply entrenched cultural stigmas related to race and ethnicity, socioeconomics, and an imprecise moralism that positions access to health and protection as a privilege that should be earned or denied based on behavior [ 67 , 69 , 71 ].
This tension plays out most concretely in the public policy space. Even as the opioid crisis dominates public health discourse and funding is earmarked for research and programming to combat it [ 77 ], harm reduction programs on the ground are under siege. At the federal level, the House Appropriations bill for the Fiscal Year 2024 HHS budget dramatically cuts funding to HIV/AIDS programs—a budget umbrella under which many harm reduction, substance use support and treatment programs are funded [ 78 , 79 ]. In California, a $15.2 million state grant supporting syringe access services has dried up amidst an overdose crisis at its peak, with no plans for replacement [ 80 ]. In 2022, a landmark bill (SB58) that would have authorized overdose prevention programs with supervised consumption in Los Angeles, Oakland, and San Francisco was vetoed by the Governor, despite broad support and robust evidence behind it [ 81 ]. Funds for such safe consumption sites have further been excluded from receiving opioid settlement funds in San Francisco [ 82 ], and in September of 2023, a bill was put forth by the San Francisco Mayor’s office to require drug screening and mandatory treatment for anyone receiving public services [ 83 ]. This, despite the expressly articulated commitment to and acknowledged necessity of harm reduction services—services explicitly aimed at helping people who use drugs to be more safe rather than abstaining from use—highlighted in policy language across multiple levels of government and legislature [ 10 , 84 , 85 , 86 , 87 ].
It is worth noting that one of the harm reduction sites where several of this study’s client participants were receiving services was defunded shortly after we completed data collection, and since then, overdose death rates in the city have climbed [ 88 ] and public order in that area has reportedly deteriorated [ 89 ].
The framing of effectiveness is crucial in this policy environment
In light of these tensions, we offer the findings of this study as a contribution to an evidence base that may play an increasingly central role in California’s—and the nation’s—opioid crisis response. The allowable expenditures for opioid settlement funds list “evidence-informed programs to reduce the harms associated with intravenous drug use” as a focus area [ 51 ] and California’s Overdose Prevention Initiative describes its approach as being “data-driven.” [ 10 ] The proposed HHS FY2024 budget, in addition to cutting much of the funding that covers harm reduction programming, proposes the rejection of “controversial programs” while maintaining funding for “an effective opioid response.” [ 78 ] As California faces a $68 billion budget deficit [ 90 ] and supplementary federal and settlement funds are to be apportioned based on strategy effectiveness and the body of scientific evidence, the role of research comes into sharper focus. It is the strength or weakness of the evidence base—of the complexity of the research inquiry and integrity of the data—that may ultimately frame which initiatives are eligible for support.
When asked about the place and promise of drug checking within the broader constellation of harm reduction services, it was drug users’ humanity and right to health, more so than the public health implications, that grounded many of our participants’ responses. Their responses implicated, too, the underlying operating principle that, ultimately, people make choices that make sense for them. Whether by the hand of addiction or desire, constrained options or access, or every individual’s complex hierarchy of relative dangers and needs, people’s choices are reflections of their full humanity. Approaches to stemming the tide of this crisis cannot be effective unless they are built on respect for the individuals living it, and focused on understanding their needs.
We encourage continued research and reporting on drug checking services and emerging technologies, with an emphasis on exploring effectiveness within a broad scope, reflective of the impacts of these services on whole lives and systems.
Limitations
Many of the community members we interviewed had not heard of spectrometry or spectroscopy, and the interview represented the first time they were introduced to the technology as a concept and the first time they considered whether and how they could see themselves using it in their own lives. This limits the range of our findings among the client sample, given that much of our qualitative data speaks to hypothetical future use rather than past or current use of emerging technologies. The absence of data on client use should not be interpreted to mean that participants chose not to use DCS.
Additionally, the sampling frame for clients was limited to one setting, while providers were sampled from across North America, and the small sample size for both groups may have limited saturation. Finally, providers did not reflect all North American regions where drug checking has been implemented, nor all DCS models, limiting the generalizability of findings.
Our manuscript contributes to growing evidence of the effectiveness of drug checking services in mitigating a range of risks associated with substance use, including overdose, and offer diverse benefits at the individual, community, public health, and health systems levels. For that reason, policymakers should consider allocating resources towards its implementation and scale-up in settings impacted by overdose mortality.
Data availability
Due to ethical restrictions, the data generated and analyzed during the current study are not available to those outside the study team. Data and materials are of a sensitive nature, and participants did not consent to transcripts of their interviews being publicly available. Portions of interviews about which editors have questions or concerns may be provided upon request after any details that may risk the confidentiality of the participants beyond de-identification have been removed. Researchers who meet the criteria for access to confidential data may send requests for the interview transcripts to the Human Research Protection Program (HRPP)/IRB at the University of California, San Francisco at 415-476-1814 or [email protected].
Abbreviations
Fourier–Transform Infrared Spectroscopy
Fentanyl testing strips
US Department of Health and Human Services
Medications for opioid use disorder
Volkow ND, Blanco C. The changing Opioid Crisis: development, challenges and opportunities. Mol Psychiatry. 2021;26(1):218–33.
Article PubMed Google Scholar
Ciccarone D. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int J Drug Policy. 2017;46:107–11.
Article PubMed PubMed Central Google Scholar
Dasgupta N, Beletsky L, Ciccarone D. Opioid Crisis: no Easy fix to its Social and Economic determinants. Am J Public Health. 2018;108(2):182–6.
Ciccarone D. The rise of Illicit fentanyls, stimulants and the Fourth Wave of the Opioid Overdose Crisis. Curr Opin Psychiatry. 2021;34(4):344–50.
U.S. Department of Health and Human Services (HHS). List of Public Health Emergency Declarations [Internet]. Administration for Strategic Preparedness & Response. [cited 2023 Oct 11]. https://aspr.hhs.gov:443/legal/PHE/Pages/default.aspx .
Center for Disease Control and Prevention (CDC). Understanding the Opioid Overdose Epidemic [Internet]. 2023. https://www.cdc.gov/opioids/basics/epidemic.html .
Center for Disease Control and Prevention (CDC). Data brief - Overdose deaths in the United States [Internet]. https://www.cdc.gov/nchs/data/databriefs/db457-tables.pdf#4 .
Center for Disease Control and Prevention, National Center for Health Statistics. Drug Overdose Mortality by State [Internet]. 2022. https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_mortality/drug_poisoning.htm .
California Department of Public Health (CDPH) - Substance and Addiction Prevention Branch (SAPB). CDPH Center for Health Statistics and Informatics Vital Statistics - Multiple Cause of Death and California Comprehensive Death Files [Internet]. California Overdose Surveillance Dashboard. [cited 2023 Nov 6]. https://skylab.cdph.ca.gov/ODdash/?tab=CA .
California Department of Public Health (CDPH). Substance and Addiction Prevention Branch. California’s Approach to the Overdose Epidemic [Internet]. [cited 2023 Oct 11]. https://www.cdph.ca.gov/Programs/CCDPHP/sapb/Pages/CA-Approach.aspx .
Barratt MJ, Measham F. What is drug checking. Anyway? Drugs Habits Soc Policy. 2022;23(3):176–87.
Article Google Scholar
Brunt T. Drug checking as a harm reduction tool for recreational drug users: opportunities and challenges. Background paper commissioned by the EMCDDA for Health and social responses to drug problems: a European guide [Internet]. 2017 Oct 30 [cited 2023 Oct 11]; https://apo.org.au/node/219011 .
Peiper NC, Clarke SD, Vincent LB, Ciccarone D, Kral AH, Zibbell JE. Fentanyl test strips as an opioid overdose prevention strategy: findings from a syringe services program in the Southeastern United States. Int J Drug Policy. 2019;63:122–8.
Measham F, Turnbull G. Intentions, actions and outcomes: a follow up survey on harm reduction practices after using an English festival drug checking service. Int J Drug Policy. 2021;95:103270.
Measham F, Simmons H. Who uses drug checking services? Assessing uptake and outcomes at English festivals in 2018. Drugs Habits Soc Policy. 2022;23(3):188–99.
Maghsoudi N, Tanguay J, Scarfone K, Rammohan I, Ziegler C, Werb D, et al. Drug checking services for people who use drugs: a systematic review. Addict Abingdon Engl. 2022;117(3):532–44.
Maghsoudi N, McDonald K, Stefan C, Beriault DR, Mason K, Barnaby L, et al. Evaluating networked drug checking services in Toronto, Ontario: study protocol and rationale. Harm Reduct J. 2020;17(1):9.
Article CAS PubMed PubMed Central Google Scholar
Johns Hopkins Bloomberg School of Public Health and Bloomberg American Health Initiative. Fentanyl Overdose Reduction Checking Analysis Study (FORECAST). Baltimore, MD; 2018.
Krieger MS, Yedinak JL, Buxton JA, Lysyshyn M, Bernstein E, Rich JD, et al. High willingness to use rapid fentanyl test strips among young adults who use drugs. Harm Reduct J. 2018;15(1):7.
Rammohan I, Bouck Z, Fusigboye S, Bowles J, McDonald K, Maghsoudi N, et al. Drug checking use and interest among people who inject drugs in Toronto, Canada. Int J Drug Policy. 2022;107:103781.
Davis CS, Lieberman AJ, O’Kelley-Bangsberg M. Legality of drug checking equipment in the United States: a systematic legal analysis. Drug Alcohol Depend. 2022;234:109425.
Swartz JA, Lieberman M, Jimenez AD, Mackesy-Amiti ME, Whitehead HD, Hayes KL, et al. Current attitudes toward drug checking services and a comparison of expected with actual drugs present in street drug samples collected from opioid users. Harm Reduct J. 2023;20(1):87.
Reagan-Udall Foundation for the FDA. Fentanyl Drug Checking and Screening: Roundtable on Clinical Perspectives [Internet]. 2021. https://reaganudall.org/sites/default/files/2022-06/FTS_Clinician%20Roundtable_Final_Complete%206.30.pdf .
Reagan-Udall Foundation for the FDA. Fentanyl Drug Checking and Screening: Roundtable on Community Perspectives [Internet]. 2021. https://reaganudall.org/sites/default/files/2022-06/FTS_Community%20Roundtable_Final_Complete%206.30.pdf .
Weicker NP, Owczarzak J, Urquhart G, Park JN, Rouhani S, Ling R, et al. Agency in the fentanyl era: exploring the utility of fentanyl test strips in an opaque drug market. Int J Drug Policy. 2020;84:102900.
Bardwell G, Boyd J, Arredondo J, McNeil R, Kerr T. Trusting the source: the potential role of drug dealers in reducing drug-related harms via drug checking. Drug Alcohol Depend. 2019;198:1–6.
Long V, Arredondo J, Ti L, Grant C, DeBeck K, Milloy MJ, et al. Factors associated with drug checking service utilization among people who use drugs in a Canadian setting. Harm Reduct J. 2020;17(1):100.
Carroll JJ, Rich JD, Green TC. The protective effect of trusted dealers against opioid overdose in the U.S. Int J Drug Policy. 2020;78:102695.
Betsos A, Valleriani J, Boyd J, Bardwell G, Kerr T, McNeil R. I couldn’t live with killing one of my friends or anybody: a rapid ethnographic study of drug sellers’ use of drug checking. Int J Drug Policy. 2021;87:102845.
Wallace B, Hills R, Rothwell J, Kumar D, Garber I, van Roode T, et al. Implementing an integrated multi-technology platform for drug checking: Social, scientific, and technological considerations. Drug Test Anal. 2021;13(4):734–46.
Article CAS PubMed Google Scholar
McCrae K, Tobias S, Grant C, Lysyshyn M, Laing R, Wood E, et al. Assessing the limit of detection of Fourier-transform infrared spectroscopy and immunoassay strips for fentanyl in a real-world setting. Drug Alcohol Rev. 2020;39(1):98–102.
Center for Disease Control and Prevention (CDC). Fentanyl Test Strips: A Harm Reduction Strategy [Internet]. 2023 [cited 2023 Oct 11]. https://www.cdc.gov/stopoverdose/fentanyl/fentanyl-test-strips.html .
Miller A. More states allow fentanyl test strips as a tool to prevent overdoses [Internet]. CNN. 2022 [cited 2023 Oct 12]. https://www.cnn.com/2022/05/04/health/fentanyl-test-strips-khn/index.html .
Green TC, Park JN, Gilbert M, McKenzie M, Struth E, Lucas R, et al. An assessment of the limits of detection, sensitivity and specificity of three devices for public health-based drug checking of fentanyl in street-acquired samples. Int J Drug Policy. 2020;77:102661.
Park JN, Frankel S, Morris M, Dieni O, Fahey-Morrison L, Luta M, et al. Evaluation of fentanyl test strip distribution in two Mid-atlantic syringe services programs. Int J Drug Policy. 2021;94:103196.
Laing MK, Ti L, Marmel A, Tobias S, Shapiro AM, Laing R, et al. An outbreak of novel psychoactive substance benzodiazepines in the unregulated drug supply: preliminary results from a community drug checking program using point-of-care and confirmatory methods. Int J Drug Policy. 2021;93:103169.
Harper L, Powell J, Pijl EM. An overview of forensic drug testing methods and their suitability for harm reduction point-of-care services. Harm Reduct J. 2017;14(1):52.
Tupper KW, McCrae K, Garber I, Lysyshyn M, Wood E. Initial results of a drug checking pilot program to detect fentanyl adulteration in a Canadian setting. Drug Alcohol Depend. 2018;190:242–5.
Borden SA, Saatchi A, Vandergrift GW, Palaty J, Lysyshyn M, Gill CG. A new quantitative drug checking technology for harm reduction: pilot study in Vancouver, Canada using paper spray mass spectrometry. Drug Alcohol Rev. 2022;41(2):410–8.
Gozdzialski L, Wallace B, Hore D. Point-of-care community drug checking technologies: an insider look at the scientific principles and practical considerations. Harm Reduct J. 2023;20:39.
Barry CL. Fentanyl and the evolving opioid epidemic: what strategies should Policy makers consider? Psychiatr Serv Wash DC. 2018;69(1):100–3.
Tsai AC, Kiang MV, Barnett ML, Beletsky L, Keyes KM, McGinty EE, et al. Stigma as a fundamental hindrance to the United States opioid overdose crisis response. PLOS Med. 2019;16(11):e1002969.
Khan GK, Harvey L, Johnson S, Long P, Kimmel S, Pierre C, et al. Integration of a community-based harm reduction program into a safety net hospital: a qualitative study. Harm Reduct J. 2022;19:35.
Kulesza M, Teachman BA, Werntz AJ, Gasser ML, Lindgren KP. Correlates of public support toward federal funding for harm reduction strategies. Subst Abuse Treat Prev Policy. 2015;10:25.
Socia KM, Stone R, Palacios WR, Cluverius J. Focus on prevention: the public is more supportive of overdose prevention sites than they are of safe injection facilities. Criminol Public Policy. 2021;20(4):729–54.
Vearrier L. The value of harm reduction for injection drug use: a clinical and public health ethics analysis. Dis–Mon DM. 2019;65(5):119–41.
Csák R, Shirley-Beavan S, McHenry AE, Daniels C, Burke-Shyne N. Harm reduction must be recognised an essential public health intervention during crises. Harm Reduct J. 2021;18:128.
Levengood TW, Yoon GH, Davoust MJ, Ogden SN, Marshall BDL, Cahill SR, et al. Supervised Injection facilities as Harm reduction: a systematic review. Am J Prev Med. 2021;61(5):738–49.
Kennedy MC, Karamouzian M, Kerr T. Public Health and Public Order Outcomes Associated with supervised drug Consumption facilities: a systematic review. Curr HIV/AIDS Rep. 2017;14(5):161–83.
Plaintiff’s Executive Committee. National Opioids Settlement [Internet]. [cited 2023 Oct 11]. https://nationalopioidsettlement.com/ .
California Department of Heathcare Services (DHCS). California’s Opioid Settlements [Internet]. https://www.dhcs.ca.gov/provgovpart/Pages/California-Opioid-Settlements.aspx .
California Department of Heathcare Services (DHCS). Janssen & Distributors Settlement Funds Allowable Expenditures [Internet]. https://www.dhcs.ca.gov/Documents/CSD/CA-OSF-Allowable-Expenses.pdf .
SocioCultural R, Consultants LLC. Dedoose 9.0.17, web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA; 2021.
Miles M, Huberman A. Qualitative data analysis: an expanded sourcebook. 2nd ed. Sage; 1994.
Ondocsin J, Ciccarone D, Moran L, Outram S, Werb D, Thomas L, et al. Insights from drug checking programs: Practicing Bootstrap Public Health whilst Tailoring to local drug user needs. Int J Environ Res Public Health. 2023;20(11):5999.
Saldaña J. The coding manual for qualitative researchers. London: Sage; 2009.
Google Scholar
Ciccarone D, Ondocsin J, Mars S. Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin’. Int J Drug Policy. 2017;46:146–55.
Duber HC, Barata IA, Cioè-Peña E, Liang SY, Ketcham E, Macias-Konstantopoulos W, et al. Identification, management, and transition of care for patients with opioid Use Disorder in the Emergency Department. Ann Emerg Med. 2018;72(4):420–31.
Wallace B, van Roode T, Pagan F, Hore D, Pauly B. The potential impacts of community drug checking within the overdose crisis: qualitative study exploring the perspective of prospective service users. BMC Public Health. 2021;21(1):1156.
Boucher LM, Marshall Z, Martin A, Larose-Hébert K, Flynn JV, Lalonde C, et al. Expanding conceptualizations of harm reduction: results from a qualitative community-based participatory research study with people who inject drugs. Harm Reduct J. 2017;14(1):18.
Gowan T, Whetstone S, Andic T. Addiction, agency, and the politics of self-control: doing harm reduction in a heroin users’ group. Soc Sci Med 1982. 2012;74(8):1251–60.
Beaulieu T, Wood E, Tobias S, Lysyshyn M, Patel P, Matthews J, et al. Is expected substance type associated with timing of drug checking service utilization? A cross-sectional study. Harm Reduct J. 2021;18(1):66.
Ivers JH, Killeen N, Keenan E. Drug use, harm-reduction practices and attitudes toward the utilisation of drug safety testing services in an Irish cohort of festival-goers. Ir J Med Sci 1971 -. 2022;191(4):1701–10.
Mars SG, Ondocsin J, Ciccarone D. Toots, tastes and tester shots: user accounts of drug sampling methods for gauging heroin potency. Harm Reduct J. 2018;15(1):26.
Tilhou AS, Zaborek J, Baltes A, Salisbury-Afshar E, Malicki J, Brown R. Differences in drug use behaviors that impact overdose risk among individuals who do and do not use fentanyl test strips for drug checking. Harm Reduct J. 2023;20(1):41.
Aarhus Universitet. Literature Review of Drug Checking in Nightlife – Methods, Services, and Effects [Internet], Aarhus. Denmark: Center for Rusmiddelforskning, Psykologisk Institut; 2019. https://www.sst.dk/-/media/Udgivelser/2019/Engelsk-version-Litteraturgennemgang-om-stoftest-i-nattelivet.ashx .
Des Jarlais DC. Harm reduction in the USA: the research perspective and an archive to David Purchase. Harm Reduct J. 2017;14(1):51.
Jackson LA, Dechman M, Mathias H, Gahagan J, Morrison K. Safety and danger: perceptions of the implementation of harm reduction programs in two communities in Nova Scotia, Canada. Health Soc Care Community. 2022;30(1):360–71.
Keane H. Critiques of harm reduction, morality and the promise of human rights. Int J Drug Policy. 2003;14(3):227–32.
Armbrecht E, Guzauskas G, Hansen R, Pandey R, Fazioli K, Chapman R. Supervised injection facilities and other supervised consumption sites: effectiveness and value; final evidence report [Internet]. Institute for Clinical and Economic Review; 2021 Jan. https://icer.org/wp-content/uploads/2020/10/ICER_SIF_Final-Evidence-Report_010821.pdf .
Klein A. Harm reduction works: evidence and inclusion in Drug Policy and Advocacy. Health Care Anal HCA J Health Philos Policy. 2020;28(4):404–14.
DeBeck K, Kerr T, Bird L, Zhang R, Marsh D, Tyndall M, et al. Injection drug use cessation and use of North America’s first medically supervised safer injecting facility. Drug Alcohol Depend. 2011;113(2–3):172–6.
Hagan H, McGough JP, Thiede H, Hopkins S, Duchin J, Alexander ER. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J Subst Abuse Treat. 2000;19(3):247–52.
Fixler AL, Jacobs LA, Jones DB, Arnold A, Underwood EE. There Goes the Neighborhood? The Public Safety Enhancing Effects of a Mobile Harm Reduction Intervention [Internet]. medRxiv; 2023 [cited 2023 Nov 1]. p. 2023.05.30.23290739. https://www.medrxiv.org/content/ https://doi.org/10.1101/2023.05.30.23290739v1 .
Chalfin A, Del Pozo B, Mitre-Becerril D. Overdose Prevention Centers, Crime, and disorder in New York City. JAMA Netw Open. 2023;6(11):e2342228.
Wilson DP, Donald B, Shattock AJ, Wilson D, Fraser-Hurt N. The cost-effectiveness of harm reduction. Int J Drug Policy. 2015;26:S5–11.
Weiss M, Zoorob M. Political frames of public health crises: discussing the opioid epidemic in the US Congress. Soc Sci Med. 2021;281:114087.
Committee Releases FY, Labor. Health and Human Services, Education, and Related Agencies Appropriations Bill [Internet]. House Committee on Appropriations - Republicans. 2023 [cited 2023 Oct 11]. https://appropriations.house.gov/news/press-releases/committee-releases-fy24-labor-health-and-human-services-education-and-related .
San Francisco AIDS, Foundation. Devastating cuts proposed to Federal HIV budget [Internet]. San Francisco AIDS Foundation. 2023 [cited 2023 Oct 11]. https://www.sfaf.org/collections/breaking-news/devastating-cuts-proposed-to-federal-hiv-budget/ .
Emily Alpert Reyes. Amid an overdose crisis, a California grant that helped syringe programs is drying up. Los Angeles Times [Internet]. 2023 Feb 19 [cited 2023 Oct 11]; https://www.latimes.com/california/story/2023-02-19/overdose-california-grant-syringe-programs .
Healthright 360. Outrage at Governor Newsom’s decision to veto SB 57, landmark overdose prevention bill | News | HealthRIGHT 360 [Internet]. [cited 2023 Oct 11]. https://www.healthright360.org/news/outrage-governor-newsom%E2%80%99s-decision-veto-sb-57-landmark-overdose-prevention-bill# .
Sjostedt D. SF Can’t Use Opioid Settlement on Drug Sites, Attorney Says. The San Francisco Standard [Internet]. 2023 Jan 21 [cited 2023 Oct 11]; https://sfstandard.com/2023/01/20/san-francisco-cant-use-opioid-settlement-funds-for-drug-sites-attorney-says/ .
City and County of San Francisco - News. Mayor London Breed Announces New Initiative to Require Screening and Treatment for Substance Use Disorder in Order to Receive County-Funded Cash Assistance | San Francisco [Internet]. [cited 2023 Oct 11]. https://sf.gov/news/mayor-london-breed-announces-new-initiative-require-screening-and-treatment-substance-use .
Executive Office of the President, Office of National Drug Control Policy. The Biden-Harris Administration’s Statement of Drug Policy Priorities for Year One [Internet]. Washington, DC; https://www.whitehouse.gov/wp-content/uploads/2021/03/BidenHarris-Statement-of-Drug-Policy-Priorities-April-1.pdf .
U.S. Department of Health and Human Services (HHS). Harm Reduction [Internet]. Overdose Prevention Strategy. 2021 [cited 2023 Oct 11]. https://www.hhs.gov/overdose-prevention/harm-reduction .
California Department of Public Health (CDPH). Substance and Addiction Prevention Branch. OPI Landing Page [Internet]. Overdose Prevention Initiative (OPI). [cited 2023 Oct 11]. https://www.cdph.ca.gov/Programs/CCDPHP/sapb/Pages/OPI-landing.aspx .
Center for Disease Control and Prevention (CDC). Opioid Rapid Response Program (ORRP) | Opioids | CDC [Internet]. 2022 [cited 2023 Oct 11]. https://www.cdc.gov/opioids/opioid-rapid-response-program.html .
Thadani T, Jung Y. After Mayor Breed’s Tenderloin Center closed, S.F. overdose deaths jumped. Here’s what the data shows. San Francisco Chronicle [Internet]. [cited 2023 Dec 20]; https://www.sfchronicle.com/sf/article/sf-mayor-breed-overdose-tenderloin-center-fentanyl-17846320.php .
Quintana S. Closure of SF’s Controversial Tenderloin Linkage Center Creates New Issue for the City [Internet]. NBC Bay Area. 2022. https://www.nbcbayarea.com/news/local/san-francisco/tenderloin-linkage-center-closure/3101390/ .
Petek G. The 2024-25 Budget: California’s Fiscal Outlook [Internet]. Legislative Analyst’s Office; 2023 Dec. https://lao.ca.gov/reports/2023/4819/2024-25-Fiscal-Outlook-120723.pdf .
Download references
Acknowledgements
This study would not have been possible without the client participants who so generously shared insights about their lives and how they access harm reduction services, and our provider key informants and their work on behalf of people who use drugs. The authors would also like to thank the staff of the Northern California HIV/AIDS Policy Research Center who supported the project during its inception, data collection, and writing.
This research was funded by the California HIV/AIDS Research Program (CHRP) to the Northern California HIV/AIDS Policy Research Center (PI Arnold), H21PC3238. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Author information
Authors and affiliations.
Center for AIDS Prevention Studies, Department of Medicine, University of California, San Francisco, CA, 94143, USA
Lissa Moran, Jeff Ondocsin, Simon Outram & Emily A. Arnold
Family & Community Medicine, Department of Medicine, University of California, San Francisco, CA, 94143, USA
Jeff Ondocsin, Daniel Ciccarone & Nicole Holm
Centre on Drug Policy Evaluation, St. Michael’s Hospital, Toronto, ON, M5B 1W8, Canada
Daniel Werb
Division of Infectious Diseases & Global Public Health, UC San Diego School of Medicine, University of California, San Diego, CA, 92093, USA
You can also search for this author in PubMed Google Scholar
Contributions
E.A.A. and D.C. conceptualized and designed the study; J.O., L.M., D.C., and N.H. were responsible for data collection, each conducting in-depth key informant interviews. L.M., J.O., S.O., and E.A.A. analyzed the data. L.M. led the writing of the original manuscript draft with significant contributions from J.O., S.O., and E.A.A. L.M., J.O., D.C., S.O., D.W., N.H., and E.A.A. were directly involved in iterative review and revision. E.A.A. provided supervision, project administration, and funding acquisition. All authors have read and agreed to the submitted version of the manuscript.
Corresponding author
Correspondence to Lissa Moran .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted in accordance with the Declaration of Helsinki and informed consent was obtained from all subjects involved in the study. The study protocol and consent procedures were reviewed and approved by the UCSF IRB (#22-36640) on 12 September 2022.
Consent for publication
Not applicable.
Competing interests
D.W. is a founder of DoseCheck, a commercial entity that is developing a mobile drug checking technology. D.C. reports the following relevant financial relationships during the past 12 months: (1) he is a scientific advisor to Celero Systems; and (2) he has been retained as an expert witness in ongoing prescription opioid litigation by Motley Rice, LLP. The remaining authors have no relevant financial or non-financial interests to disclose. The remaining authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Moran, L., Ondocsin, J., Outram, S. et al. How do we understand the value of drug checking as a component of harm reduction services? A qualitative exploration of client and provider perspectives. Harm Reduct J 21 , 92 (2024). https://doi.org/10.1186/s12954-024-01014-w
Download citation
Received : 23 January 2024
Accepted : 02 May 2024
Published : 11 May 2024
DOI : https://doi.org/10.1186/s12954-024-01014-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug checking
- Harm reduction
- Substance use
- Qualitative
- North america
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]
Opinion: The real reason why Oregon recriminalizing drugs is a cautionary tale

- Show more sharing options
- Copy Link URL Copied!
In a move widely hailed as a failure for the drug decriminalization movement, Oregon restored criminal penalties for low-level drug possession in April. Headlines chalked up this policy reversal to mounting overdoses , evoking a crisis in the state.
In reality, Oregon’s overdose rate remains in the middle of the pack nationally, with more than half of U.S. states having a greater number of deaths per capita. But increasing homelessness and visible drug use have spurred panic over drugs, which overruled statistics and scientific recommendations — and offers a cautionary tale about the fight for sensible drug laws.

Opinion: ‘Just say no’ can kill kids. Teach them how to stay safe in the fentanyl era
Drug use has become deadlier for teens, and Southern California is an overdose hot spot.
Feb. 3, 2024
In 2020, a majority of Oregon voters approved decriminalization via Measure 110 — a landmark ballot measure that made simple possession of a small quantity of drugs for personal use subject to citation instead of jail. It diverted tax revenue from cannabis, which the state legalized for recreational use in 2014; in its first round of grants alone, the measure infused $300 million into the state’s threadbare drug treatment system and funded harm reduction services.
These were solid steps, backed by decades of science about addiction and consistent with United Nations recommendations in support of drug decriminalization. Other nations, including Portugal , Spain and Uruguay , have seen success with similar shifts away from arrest and toward healthcare-based approaches.
However, the same year Measure 110 passed, fentanyl use rose sharply on the West Coast. Despite nearly a decade of advance notice from the fentanyl crisis in the East, the region failed to prepare. As in other Western states, overdose rates in Oregon soared — from among the lowest in the country to nearly reaching the national average in 2022. Although data suggest that rates of drug use in Oregon have remained fairly stable in recent years, fentanyl makes for a much deadlier drug supply. At the same time, homelessness in Oregon has risen rapidly . As more people live outside, more drug use that used to occur behind closed doors now happens in plain sight.
The combination of these factors fed the perception that Oregon’s drug crisis was uniquely severe. Even though research shows that drug decriminalization did not increase the death rate and broadly supports leaving it in place to reduce the harms and wasteful spending of incarceration, Measure 110 became a scapegoat for Oregon’s social problems. Democrats, including Portland’s typically progressive district attorney , reversed their support and in effect repealed it.

World & Nation
Oregon’s first-in-the-nation drug decriminalization law faces growing resistance
Since the law’s approval, the state has seen a surge in public drug use fueled by fentanyl and an increase in synthetic opioid overdose deaths.
Nov. 21, 2023
Criminal penalties do little to affect rates of drug use . Typically they just increase the degree to which people with addiction bounce between the street and jail, a cycle of imprisonment and release known to drive overdose deaths. Occasional anecdotes of people finding their way into recovery through contact with the criminal justice system are outliers. If police massively scale up arrests of people who use drugs, increased overdose deaths will be the predictable result .
Countries such as Portugal and Norway have followed a well-defined, alternative path to reduce drug-related deaths and public drug use. The steps include: Scale up opportunities for compassionate contact with the system, such as with free walk-in clinics for vulnerable people who use drugs. Make it easier and cheaper to access buprenorphine and methadone, medications that treat opioid addiction, than street fentanyl. Give people safe, controlled spaces to keep their drug use out of the public sphere while connecting with healthcare and shelter. Defend their human dignity and help them build positive relationships with health professionals and social workers. Drug decriminalization is worthwhile, but it does not replace these larger solutions.
Public drug use and streets full of tents are distressing for many Oregonians. They also provide images that are easily exploited by mainstream media and politicians to stoke public fears. But recriminalizing drugs is unlikely to decrease homelessness or eliminate public drug use.

California seized enough fentanyl last year to kill everyone in the world ‘nearly twice over’
Seizures of fentanyl smuggled into California have dramatically surged over the last few years, according to officials.
Feb. 27, 2024
Although blaming drugs for homelessness is a common mistake, the scientific consensus shows that increased housing costs are the single most important cause. And Oregon simply does not have sufficient shelter beds or public housing options for those affected by extremely sharp increases in those costs. The state also struggles to hospitalize people in need of treatment for severe mental illness, both because there aren’t beds available and because its laws inhibit holding people involuntarily in many cases , including serious episodes of psychosis.
Oregon’s public safety system is struggling. Calling 911 frequently means being put on hold for several minutes. There are often no ambulances to dispatch. It took police 21 minutes on average to respond to a high-priority crime as of last year, five minutes longer than the year before.
These real public safety issues demand urgency. They also have nothing to do with the fact that drug users were not being arrested for possession. Under Measure 110, theft, public indecency, assault — and selling drugs — remained illegal. Focusing on punishing people who use drugs will further stretch the police force while not solving the larger problems.
Measure 110 took steps in the right direction by investing in social services. However, a single round of funding cannot undo decades of inadequate spending on addiction treatment and prevention. Robust mental health, substance treatment and public housing systems take years to build.
With the nation’s housing and overdose crises worse than ever, what’s happening in Oregon is not unique. Similar tensions between scientific approaches to addiction and concerns about homelessness and public drug use are playing out in San Francisco, Philadelphia, Boston and other cities. Our task is to resist the temptation to cave to panic and instead commit to evidence-backed solutions.
Morgan Godvin (@MorganGodvin) is a lifelong Oregonian, writer and drug policy researcher who served on the Measure 110 Oversight and Accountability Council and the Multnomah County Local Public Safety Coordinating Council. Joseph Friedman (@JosephRFriedman) is a researcher at UCLA who has published widely on the U.S. overdose crisis.
More to Read

Opinion: This tough-on-crime proposal won’t solve California retail theft, but it would crowd our prisons
May 7, 2024

Editorial: Reclassifying marijuana is not decriminalization, but is a welcome step in that direction
May 1, 2024

State senators respond to fentanyl and retail theft crises with new legislation
Feb. 26, 2024
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.
More From the Los Angeles Times
Opinion: Alice Munro’s stories gave voice to women’s unspoken, almost unspeakable, inner lives
May 16, 2024

Calmes: The Supreme Court’s conservatives onstage, unplugged, unrepentant

Opinion: A job can’t always lift someone out of homelessness. What more is needed?

Opinion: I’m an American doctor stuck in Gaza. As Israel moves into Rafah, where will physicians and our patients go?
May 15, 2024
Uber has a new way to solve the concert traffic problem

Uber is taking a shuttle product it developed for commuters in India and Egypt and converting it for an American audience.
The ride-hail and delivery giant announced Wednesday at its annual Go-Get event in New York City that it will launch a shuttle service in certain U.S. cities this summer. The service will eventually cater to events like concerts and sports games, as well as airport pickups and drop-offs.
Uber Shuttle in the U.S. will repurpose the technology and business model that Uber has built to help commuters in emerging markets where there’s a public transportation gap. Rather than tapping regular gig workers to drive the shuttles, Uber will work with existing local fleet providers who employ commercially licensed drivers to drive vans and buses that range from 14 to 55 seats.
“If you look at what we do in India and Egypt, we go, ‘Where do we want to lay out our own routes based on a predicted demand we see across the city,’” Anthony Le Roux, general manager of Uber Shuttle, told TechCrunch. “We build a network and work with fleet operators in those markets to deploy buses along those routes, and we build and manage the whole system.”
In the U.S., Le Roux said such shuttle services don’t make as much sense because there’s public transit infrastructure and Americans are attached to driving their own vehicles. What does make sense, though, is tapping the instances where people are less likely to take their own vehicles. Like if they want to have a few drinks at the ball game or need a cheap way to get to the airport.
The biggest challenge will be to find out exactly where to pick people up and at what times, said Le Roux. That’s where Uber’s massive stores of aggregate data will come in to give developers a better idea of how people are actually moving from airports, stadiums and amphitheaters, he said.
How Uber Shuttle will work

Uber will launch event shuttles this summer as part of a partnership with entertainment company Live Nation. As part of that partnership, Uber Shuttle will be available at some Live Nation amphitheaters for concertgoers in Pittsburgh, Charlotte and Chicago. Uber said it will also partner with Miami’s Hard Rock Stadium, home of the Miami Dolphins, Formula One, Crypto.com Miami Grand Prix and other events to provide shuttle services.
Airport shuttles will come later, said an Uber spokesperson, without specifying when exactly.
Uber Shuttle will let riders reserve a seat for themselves or up to five people in a shuttle that goes to and from an airport, a concert or a game for “a fraction of the price” of an UberX, a spokesperson from the company told TechCrunch. Uber promises shuttle prices won’t be impacted by surge pricing, the dynamic pricing structure that causes ride-hail fares to skyrocket when demand is high.
Riders will be able to book their seats anywhere from seven days to five minutes before their shuttle’s scheduled departure. They’ll get a notification about 25 minutes before their departure time to alert them to the designated pickup location. When their shuttle arrives, riders will present a QR code ticket to the driver so they can board, and the rest of the trip goes much like a normal Uber ride, with the ability to tip and rate the driver in the app after the ride.
During the Go-Get event, Uber also announced a number of other ride-hail and delivery products, like the ability to reserve shared rides and have products delivered from bulk-buy store Costco. The company said Go-Get’s theme this year was on “togetherness,” but from where we’re sitting, it looks like the theme is really on cost savings. All of the products offered Wednesday, including a $4.99 per month, $48 per year, Uber One membership for students, seem geared toward giving users cheaper options for travel and delivery.
This article has been updated to include more information on other products announced at Uber Go-Get 2024.
More TechCrunch
Get the industry’s biggest tech news, techcrunch daily news.
Every weekday and Sunday, you can get the best of TechCrunch’s coverage.
Startups Weekly
Startups are the core of TechCrunch, so get our best coverage delivered weekly.
TechCrunch Fintech
The latest Fintech news and analysis, delivered every Sunday.
TechCrunch Mobility
TechCrunch Mobility is your destination for transportation news and insight.
A US Trustee wants troubled fintech Synapse to be liquidated via Chapter 7 bankruptcy, cites ‘gross mismanagement’
The prospects for troubled banking-as-a-service startup Synapse have gone from bad to worse this week after a United States Trustee filed an emergency motion on Wednesday. The trustee is asking…

Seraphim’s latest space accelerator welcomes nine companies
U.K.-based Seraphim Space is spinning up its 13th accelerator program, with nine participating companies working on a range of tech from propulsion to in-space manufacturing and space situational awareness. The…

OpenAI inks deal to train AI on Reddit data
OpenAI has reached a deal with Reddit to use the social news site’s data for training AI models. In a blog post on OpenAI’s press relations site, the company said…

X pushes more users to Communities
X users will now be able to discover posts from new Communities that are trending directly from an Explore tab within the section.

Mark Zuckerberg’s makeover: Midlife crisis or carefully crafted rebrand?
For Mark Zuckerberg’s 40th birthday, his wife got him a photoshoot. Zuckerberg gives the camera a sly smile as he sits amid a carefully crafted re-creation of his childhood bedroom.…

Strava taps AI to weed out leaderboard cheats, unveils ‘family’ plan, dark mode and more
Strava announced a slew of features, including AI to weed out leaderboard cheats, a new ‘family’ subscription plan, dark mode and more.

Astronauts fall over. Robotic limbs can help them back up.
We all fall down sometimes. Astronauts are no exception. You need to be in peak physical condition for space travel, but bulky space suits and lower gravity levels can be…

Microsoft’s custom Cobalt chips will come to Azure next week
Microsoft will launch its custom Cobalt 100 chips to customers as a public preview at its Build conference next week, TechCrunch has learned. In an analyst briefing ahead of Build,…
Tesla keeps cutting jobs and the feds probe Waymo
What a wild week for transportation news! It was a smorgasbord of news that seemed to touch every sector and theme in transportation.

Sony Music warns tech companies over ‘unauthorized’ use of its content to train AI
Sony Music Group has sent letters to more than 700 tech companies and music streaming services to warn them not to use its music to train AI without explicit permission.…

GrubMarket buys Butter to give its food distribution tech an AI boost
Winston Chi, Butter’s founder and CEO, told TechCrunch that “most parties, including our investors and us, are making money” from the exit.

Bolt founder Ryan Breslow wants to settle an investor lawsuit by returning $37 million worth of shares
The investor lawsuit is related to Bolt securing a $30 million personal loan to Ryan Breslow, which was later defaulted on.

With the end of Workplace, it’s fair to wonder if Meta was ever serious about the enterprise
Meta, the parent company of Facebook, launched an enterprise version of the prominent social network in 2015. It always seemed like a stretch for a company built on a consumer…

Meta Threads is testing pinned columns on the web, similar to the old TweetDeck
X, formerly Twitter, turned TweetDeck into X Pro and pushed it behind a paywall. But there is a new column-based social media tool in town, and it’s from Instagram Threads.…

Google expands hands-free and eyes-free interfaces on Android
As part of 2024’s Accessibility Awareness Day, Google is showing off some updates to Android that should be useful to folks with mobility or vision impairments. Project Gameface allows gamers…

Hacker claims theft of India’s Samco account data
A hacker listed the data allegedly breached from Samco on a known cybercrime forum.

Ireland privacy watchdog confirms Dell data breach investigation
A top European privacy watchdog is investigating following the recent breaches of Dell customers’ personal information, TechCrunch has learned. Ireland’s Data Protection Commission (DPC) deputy commissioner Graham Doyle confirmed to…

Ampere teams up with Qualcomm to launch an Arm-based AI server
Ampere and Qualcomm aren’t the most obvious of partners. Both, after all, offer Arm-based chips for running data center servers (though Qualcomm’s largest market remains mobile). But as the two…

Google I/O was an AI evolution, not a revolution
At Google’s I/O developer conference, the company made its case to developers — and to some extent, consumers — why its bets on AI are ahead of rivals. At the…

Meet the Magnificent Six: A tour of the stages at Disrupt 2024
TechCrunch Disrupt has always been the ultimate convergence point for all things startup and tech. In the bustling world of innovation, it serves as the “big top” tent, where entrepreneurs,…

Khosla Ventures, Pear VC triple down on Honey Homes, a smart way to hire a handyman
There’s apparently a lot of demand for an on-demand handyperson. Khosla Ventures and Pear VC have just tripled down on their investment in Honey Homes, which offers up a dedicated…

TikTok tests 60-minute video uploads as it continues to take on YouTube
TikTok is testing the ability for users to upload 60-minute videos, the company confirmed to TechCrunch on Thursday. The feature is available to a limited group of users in select…

Flock Safety’s solar-powered cameras could make surveillance more widespread
Flock Safety is a multibillion-dollar startup that’s got eyes everywhere. As of Wednesday, with the company’s new Solar Condor cameras, those eyes are solar-powered and use wireless 5G networks to…

Agora raises $34M Series B to keep building the Carta for real estate
Since he was very young, Bar Mor knew that he would inevitably do something with real estate. His family was involved in all types of real estate projects, from ground-up…

Poshmark’s ‘Promoted Closet’ tool lets sellers boost all their listings at once
Poshmark, the social commerce site that lets people buy and sell new and used items to each other, launched a paid marketing tool on Thursday, giving sellers the ability to…

Google adds Gemini to its Education suite
Google is launching a Gemini add-on for educational institutes through Google Workspace.

YC-backed Recall.ai gets $10M Series A to help companies use virtual meeting data
More money for the generative AI boom: Y Combinator-backed developer infrastructure startup Recall.ai announced Thursday it has raised a $10 million Series A funding round, bringing its total raised to over…

CoLab’s collaborative tools for engineers line up $21M in new funding
Engineers Adam Keating and Jeremy Andrews were tired of using spreadsheets and screenshots to collab with teammates — so they launched a startup, CoLab, to build a better way. The…

Reddit reintroduces its awards system
Reddit announced on Wednesday that it is reintroducing its awards system after shutting down the program last year. The company said that most of the mechanisms related to awards will…

Sigma is building a suite of collaborative data analytics tools
Sigma Computing, a startup building a range of data analytics and business intelligence tools, has raised $200 million in a fresh VC round.

'Gilbert Goons' must pay for their crimes. But that won't fully solve the problem
Opinion: stopping the 'gilbert goons' for good requires a deeper understanding of the problem and a much wider response. here's how to get started..

Everyone wants justice for the “ Gilbert Goons .”
We want to see those who violently attacked teens pay for their crimes — and rightly so.
Multiple communities were terrorized. A young man is dead .
But it’s also widely believed that once we get arrests and convictions , the problem goes away.
Which misunderstands the problem.
How the Gilbert Goons attacked
Understand how these attacks took shape:
Some have been random, but others started in school and carried over to social media, where threats, plans and discussion of past attacks proliferated in multiple group chats.
Some attacks occurred at or were catalyzed by parties with ample alcohol — word of which also was spread on social media.
Others occurred in very public locations, including an In-N-Out Burger that not only faces one of the busiest corners in Gilbert, but where calls for service had increased exponentially in a short amount of time.
Yet police failed to put the pieces together on these brazen assaults — as did school resource officers and high school administrators who were notified about some of the bullying but did little to step in.
Several aggressors faced child trauma
And what of the aggressors?
They may have hailed from wealthy neighborhoods.
Yet, based on interviews with those familiar with these families, many also grew up with little discipline and few positive influences.
Police reports detail drug and alcohol use among several Gilbert Goons. One parent is now facing drug possession charges.
Court records also reveal that parents of some accused teens had previously been convicted of dealing drugs, stealing cars, illegally possessing weapons and propositioning an undercover police officer for oral sex.
A protective order was issued against one parent amid allegations of domestic violence.
Why did so many look the other way?
Ample research suggests that adverse childhood experiences like these can increase the risk of teens turning to violence, particularly the more adverse events they experience.
But the opposite also is true: Strong relationships with positive role models — including parents, other adults and teens who refuse to tolerate deviant behavior — can lower the risk of kids with adverse experiences turning to violence.
Which brings us to the most troubling thing about the Gilbert Goons:
Lots of folks knew about their behavior. Yet few stepped in to stop it.
It’s not fully clear why.
But it suggests that beneath Gilbert’s low crime rates and family-friendly image, holes have formed not only in the institutions that are supposed to protect young people, but in the fabric of the community itself.
For hundreds of teens, this is normal
Consider that dozens of other teens never threw a punch but filmed the violence or hung out in the background as these brutal attacks occurred.
Hundreds more attended the alcohol-filled parties that helped catalyze some attacks — many of which occurred with, at best, willful ignorance from hosting parents.
At least some of these teens must think it’s normal to watch kids get drunk or high and beat the tar out of others on the weekends.
And that’s also a giant red flag, considering that research also suggests teens who witness bullying are more likely to struggle in school, feel depressed or use alcohol and drugs.
A recent Arizona Republic investigation found that bullying and emotional distress have largely driven the proliferation of school gun threats .
We cannot allow this behavior to fester.
Promising steps, but only partial solutions
Gilbert and Chandler are working on new laws that should give police more leeway to break up unruly parties .
They also may ban teens from owning or purchasing brass knuckles , which some Goons used in fights.
These are important steps. But they also are just partial solutions.
Fully addressing the Gilbert Goons problem requires a communitywide press — from police and schools to parents and, yes, even residents without teens — to stop these troubling behaviors.
It’s promising to see orange ribbons — the favorite color of murder victim Preston Lord — and “Be an Upstander” signs persistently dot the community.
What's missing from our response
What’s missing is a sustained effort to educate parents and others about bullying, problematic social media behavior or underage alcohol and drug abuse.
Bullying plays likely role in 'Goons': How to respond
That’s where district and charter schools — which have been oddly quiet in all of this — need to step in.
To help educate, but also to play a critical role in prevention.
The problem is that most school mental-health counselors have hundreds of students under their watch . They are often triaging crises, leaving little time to counsel troubled students or connect them with mentors.
Schools need the resources to hire more counselors.
They also can leverage school resource officers to help identify at-risk teens, before they engage in destructive behavior.
School resource officers, in turn, must work a lot closer with area police to address issues that occur off campus, despite the wonky jurisdictional boundaries that often put a school in a different city from where its district is based.
And police must redouble their efforts to restore broken community trust — starting with more fully explaining why they failed to connect the dots between these assaults.
Are we ready to put in this effort?
This isn’t going to be easy.
Changing ingrained mindsets and behaviors won’t happen overnight.
But that’s what it takes, if we want to ensure that no group like the Gilbert Goons ever gains a foothold in this community again.
Are we ready for that?
Reach Allhands at [email protected] . On X, formerly Twitter: @joannaallhands .
If you love this content (or love to hate it – hey, I won't judge), why not subscribe to get more ?

IMAGES
VIDEO
COMMENTS
3. Employ TV, radio and social media to educate families about drug-abuse prevention. This has been repeatedly shown to reduce the non-medical use of narcotic pain pills. 4. Establish and ...
8 keys to end the nation's drug-overdose epidemic. America's drug-overdose epidemic is getting worse. Nearly 90,000 U.S. overdose deaths took place between September 2019 and September 2020, a tally that represents the highest figure since the late 1990s, based on provisional data from the Centers for Disease Control and Prevention (CDC).
Remember, drugs change the brain—and this can lead to addiction and other serious problems. So, preventing early use of drugs or alcohol may go a long way in reducing these risks. Risk of drug use increases greatly during times of transition. For an adult, a divorce or loss of a job may increase the risk of drug use.
Director. [email protected]. (202) 512-8777. Director. [email protected]. (202) 512-7114. [email protected]. Earlier this week, many media outlets ran stories highlighting the growing crisis of drug misuse in the United States. Citing Centers for Disease Control and Prevention (CDC) data, the New York Times said that more than 100,000 Americans died ...
February 9, 2022 - Without urgent intervention, 1.2 million people in the U.S. and Canada will die from opioid overdoses by the end of the decade, in addition to the more than 600,000 who have died since 1999, according to a February 2 report from the Stanford-Lancet Commission on the North American Opioid Crisis. In this Big 3 Q&A, Howard Koh, professor of the practice of public health ...
Drug addiction is a serious and complex problem that affects millions of people. If you or someone you love is struggling with substance abuse, you may wonder how to overcome drug addiction and regain control of your life. This article explains the causes and signs of drug addiction, the different types of treatment options available, and how to plan an intervention for a loved one who needs help.
For someone in the early stages of a substance use problem, a conversation with a doctor or another professional may be enough to get them the help they need. Doctors can help the person think about their drug use, understand the risk for addiction, and come up with a plan for change. Substance use disorder can often be treated on an outpatient ...
The first step to overcoming drug abuse and addiction. Developing an addiction to drugs isn't a character flaw or a sign of weakness, and it takes more than willpower to overcome the problem. Abusing illegal or certain prescription drugs can create changes in the brain, causing powerful cravings and a compulsion to use that makes sobriety ...
Treatment enables people to counteract addiction's disruptive effects on their brain and behavior and regain control of their lives. These images showing the density of dopamine transporters in the brain illustrate the brain's remarkable ability to recover, at least in part, after a long abstinence from drugs—in this case, methamphetamine. 51.
The Vitals. Opioids are a class of drugs that affect the brain, including by relieving pain, and they are extremely addictive. Policymakers can combat the opioid epidemic by: limiting ...
Diagnosis. Diagnosing drug addiction (substance use disorder) requires a thorough evaluation and often includes an assessment by a psychiatrist, a psychologist, or a licensed alcohol and drug counselor. Blood, urine or other lab tests are used to assess drug use, but they're not a diagnostic test for addiction.
Providing effective prevention, treatment and care services for drug use disorders as part of an integrated and well-coordinated treatment system is therefore an investment in the health of people with drug use disorders. It is also an investment in the healthy and safe development of families, communities and countries. According to the 11th ...
Using drug courts to fight opioid addiction and trafficking. This approach reduces recidivism, encourages compliance with treatment, and supports families of drug court participants. It also reduces some of the burdens on jails by creating an effective diversion program. Creating referral programs through law enforcement agencies.
Risk of impairment in memory, learning, problem-solving and concentration; risk of psychosis, such as schizophrenia, hallucination or paranoia, later in life associated with early and frequent use. ... Discuss ways to resist peer pressure. ... Help reduce the chances your child will develop a drug or alcohol problem. Partnership to End ...
Reducing or quitting drugs can improve your life in many ways. It can: improve your physical and mental wellbeing. reduce your risk of permanent damage to vital organs and death. improve your relationships with friends and family. help you reconnect with your emotions.
Worsening problem. The World Drug Report published this week by the UN Office on Drugs and Crime ( UNODC) showed that drug related deaths have nearly doubled over the past decade. Moreover, 10% of HIV cases in 2019, were due to people injecting themselves with harmful substances. The UN chief warned that although international cooperation has ...
SUDs can lead to significant problems in all aspects of a person's life. Patterns of symptoms resulting from substance use (drugs or alcohol) can help a doctor diagnose a person with a SUD or SUDs and connect them to appropriate treatment. For certain drug types, some symptoms are less prominent, and in some cases, not all symptoms apply.
enhancing students' problem-solving skills; evaluating media influence; improving their self-esteem; reducing their stress and anxiety; and; increasing their engagement in meaningful activities. Prevention programs must be designed to do more than just provide facts about drugs and the impact drugs have on mental and physical health. Teaching ...
Your loved one may become defensive or angry and refuse to discuss their drug use. Many people feel a sense of shame when confronted by their behavior and will try to deny they have a problem. Don't argue with them, just revisit the issue another time. Avoid trying to lecture, threaten, bribe, or punish the person.
Educated and empowered parents and guardians are the first line of defense in preventing illicit drug use by students. ED partnered with DEA to release a new version of the popular publication, Growing Up Drug-Free: A Parent's Guide to Substance Use Prevention.The Guide includes an overview of substance use among children, youth, and young adults, and includes suggestions for how to talk to ...
Between 2000 and 2021, the annual drug overdose (OD) death rate in the U.S. quadrupled, to roughly 107,000 deaths by the end of last year.[] Drug overdose deaths now routinely exceed those from homicide, suicide, car crashes, and many medical causes.[] By best estimates, the drug OD death rate is now six times higher than its highest point in the 20th century[] and well above any point since ...
Abstract. Drug shortage is a global issue affecting low, middle, and high-income countries. Many countries have developed various strategies to overcome the problem, while the problem is accelerating, affecting the whole world. All types of drugs, such as essential life-saving drugs, oncology medicines, antimicrobial drugs, analgesics, opioids ...
Just find the right pill and your problem is solved. The creation and use of pharmaceuticals to treat problems such as weight, fatigue, anxiety and sleep problems has a checkered history. In the ...
The number of prescription drugs in shortage climbed to a 10-year high of 323 in the first quarter of 2024 - including some crucial hard-to-substitute drugs.
Problems With School Alcohol/Drug Prevention Programs. Each semester that I taught college courses on addiction, I was dismayed by students' lack of basic knowledge about what psychoactive ...
WASHINGTON - Today, DEA Administrator Anne Milgram announced the release of the 2024 National Drug Threat Assessment (NDTA), DEA's comprehensive strategic assessment of illicit drug threats and trafficking trends endangering the United States. For more than a decade, DEA's NDTA has been a trusted resource for law enforcement agencies, policy makers, and prevention and treatment ...
Participants discussed ways that drug checking can fill a regulatory vacuum, serve as a tool of informal market regulation at the community level, and empower public health surveillance systems and clinical response. ... Background paper commissioned by the EMCDDA for Health and social responses to drug problems: a European guide [Internet ...
Rising homelessness and visible crime in Portland fed panic over a drug decriminalization measure passed in 2020. But rolling that back won't solve the state's problems.
Uber has a new way to solve the concert traffic problem. Rebecca Bellan. 10:08 AM PDT • May 15, 2024 ... Like if they want to have a few drinks at the ball game or need a cheap way to get to the ...
But that won't fully solve the problem Opinion: Stopping the 'Gilbert Goons' for good requires a deeper understanding of the problem and a much wider response. Here's how to get started.