An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.2(1); Jan-Mar 2013

Systematic Reviews and Meta-analysis: Understanding the Best Evidence in Primary Healthcare
S. gopalakrishnan.
Department of Community Medicine, SRM Medical College, Hospital and Research Centre, Kattankulathur, Tamil Nadu, India
P. Ganeshkumar
Healthcare decisions for individual patients and for public health policies should be informed by the best available research evidence. The practice of evidence-based medicine is the integration of individual clinical expertise with the best available external clinical evidence from systematic research and patient's values and expectations. Primary care physicians need evidence for both clinical practice and for public health decision making. The evidence comes from good reviews which is a state-of-the-art synthesis of current evidence on a given research question. Given the explosion of medical literature, and the fact that time is always scarce, review articles play a vital role in decision making in evidence-based medical practice. Given that most clinicians and public health professionals do not have the time to track down all the original articles, critically read them, and obtain the evidence they need for their questions, systematic reviews and clinical practice guidelines may be their best source of evidence. Systematic reviews aim to identify, evaluate, and summarize the findings of all relevant individual studies over a health-related issue, thereby making the available evidence more accessible to decision makers. The objective of this article is to introduce the primary care physicians about the concept of systematic reviews and meta-analysis, outlining why they are important, describing their methods and terminologies used, and thereby helping them with the skills to recognize and understand a reliable review which will be helpful for their day-to-day clinical practice and research activities.
Introduction
Evidence-based healthcare is the integration of best research evidence with clinical expertise and patient values. Green denotes, “Using evidence from reliable research, to inform healthcare decisions, has the potential to ensure best practice and reduce variations in healthcare delivery.” However, incorporating research into practice is time consuming, and so we need methods of facilitating easy access to evidence for busy clinicians.[ 1 ] Ganeshkumar et al . mentioned that nearly half of the private practitioners in India were consulting more than 4 h per day in a locality,[ 2 ] which explains the difficulty of them in spending time in searching evidence during consultation. Ideally, clinical decision making ought to be based on the latest evidence available. However, to keep abreast with the continuously increasing number of publications in health research, a primary healthcare professional would need to read an insurmountable number of articles every day, covered in more than 13 million references and over 4800 biomedical and health journals in Medline alone. With the view to address this challenge, the systematic review method was developed. Systematic reviews aim to inform and facilitate this process through research synthesis of multiple studies, enabling increased and efficient access to evidence.[ 1 , 3 , 4 ]
Systematic reviews and meta-analyses have become increasingly important in healthcare settings. Clinicians read them to keep up-to-date with their field and they are often used as a starting point for developing clinical practice guidelines. Granting agencies may require a systematic review to ensure there is justification for further research and some healthcare journals are moving in this direction.[ 5 ]
This article is intended to provide an easy guide to understand the concept of systematic reviews and meta-analysis, which has been prepared with the aim of capacity building for general practitioners and other primary healthcare professionals in research methodology and day-to-day clinical practice.
The purpose of this article is to introduce readers to:
- The two approaches of evaluating all the available evidence on an issue i.e., systematic reviews and meta-analysis,
- Discuss the steps in doing a systematic review,
- Introduce the terms used in systematic reviews and meta-analysis,
- Interpret results of a meta-analysis, and
- The advantages and disadvantages of systematic review and meta-analysis.
Application
What is the effect of antiviral treatment in dengue fever? Most often a primary care physician needs to know convincing answers to questions like this in a primary care setting.
To find out the solutions or answers to a clinical question like this, one has to refer textbooks, ask a colleague, or search electronic database for reports of clinical trials. Doctors need reliable information on such problems and on the effectiveness of large number of therapeutic interventions, but the information sources are too many, i.e., nearly 20,000 journals publishing 2 million articles per year with unclear or confusing results. Because no study, regardless of its type, should be interpreted in isolation, a systematic review is generally the best form of evidence.[ 6 ] So, the preferred method is a good summary of research reports, i.e., systematic reviews and meta-analysis, which will give evidence-based answers to clinical situations.
There are two fundamental categories of research: Primary research and secondary research. Primary research is collecting data directly from patients or population, while secondary research is the analysis of data already collected through primary research. A review is an article that summarizes a number of primary studies and may draw conclusions on the topic of interest which can be traditional (unsystematic) or systematic.
Terminologies
Systematic review.
A systematic review is a summary of the medical literature that uses explicit and reproducible methods to systematically search, critically appraise, and synthesize on a specific issue. It synthesizes the results of multiple primary studies related to each other by using strategies that reduce biases and random errors.[ 7 ] To this end, systematic reviews may or may not include a statistical synthesis called meta-analysis, depending on whether the studies are similar enough so that combining their results is meaningful.[ 8 ] Systematic reviews are often called overviews.
The evidence-based practitioner, David Sackett, defines the following terminologies.[ 3 ]
- Review: The general term for all attempts to synthesize the results and conclusions of two or more publications on a given topic.
- Overview: When a review strives to comprehensively identify and track down all the literature on a given topic (also called “systematic literature review”).
- Meta-analysis: A specific statistical strategy for assembling the results of several studies into a single estimate.
Systematic reviews adhere to a strict scientific design based on explicit, pre-specified, and reproducible methods. Because of this, when carried out well, they provide reliable estimates about the effects of interventions so that conclusions are defensible. Systematic reviews can also demonstrate where knowledge is lacking. This can then be used to guide future research. Systematic reviews are usually carried out in the areas of clinical tests (diagnostic, screening, and prognostic), public health interventions, adverse (harm) effects, economic (cost) evaluations, and how and why interventions work.[ 9 ]
Cochrane reviews
Cochrane reviews are systematic reviews undertaken by members of the Cochrane Collaboration which is an international not-for-profit organization that aims to help people to make well-informed decisions about healthcare by preparing, maintaining, and promoting the accessibility of systematic reviews of the effects of healthcare interventions.
Cochrane Primary Health Care Field is a systematic review of primary healthcare research on prevention, treatment, rehabilitation, and diagnostic test accuracy. The overall aim and mission of the Primary Health Care Field is to promote the quality, quantity, dissemination, accessibility, applicability, and impact of Cochrane systematic reviews relevant to people who work in primary care and to ensure proper representation in the interests of primary care clinicians and consumers in Cochrane reviews and review groups, and in other entities. This field would serve to coordinate and promote the mission of the Cochrane Collaboration within the primary healthcare disciplines, as well as ensuring that primary care perspectives are adequately represented within the Collaboration.[ 10 ]
Meta-analysis
A meta-analysis is the combination of data from several independent primary studies that address the same question to produce a single estimate like the effect of treatment or risk factor. It is the statistical analysis of a large collection of analysis and results from individual studies for the purpose of integrating the findings.[ 11 ] The term meta-analysis has been used to denote the full range of quantitative methods for research reviews.[ 12 ] Meta-analyses are studies of studies.[ 13 ] Meta-analysis provides a logical framework to a research review where similar measures from comparable studies are listed systematically and the available effect measures are combined wherever possible.[ 14 ]
The fundamental rationale of meta-analysis is that it reduces the quantity of data by summarizing data from multiple resources and helps to plan research as well as to frame guidelines. It also helps to make efficient use of existing data, ensuring generalizability, helping to check consistency of relationships, explaining data inconsistency, and quantifies the data. It helps to improve the precision in estimating the risk by using explicit methods.
Therefore, “systematic review” will refer to the entire process of collecting, reviewing, and presenting all available evidence, while the term “meta-analysis” will refer to the statistical technique involved in extracting and combining data to produce a summary result.[ 15 ]
Steps in doing systematic reviews/meta-analysis
Following are the six fundamental essential steps while doing systematic review and meta-analysis.[ 16 ]
Define the question
This is the most important part of systematic reviews/meta-analysis. The research question for the systematic reviews may be related to a major public health problem or a controversial clinical situation which requires acceptable intervention as a possible solution to the present healthcare need of the community. This step is most important since the remaining steps will be based on this.
Reviewing the literature
This can be done by going through scientific resources such as electronic database, controlled clinical trials registers, other biomedical databases, non-English literatures, “gray literatures” (thesis, internal reports, non–peer-reviewed journals, pharmaceutical industry files), references listed in primary sources, raw data from published trials and other unpublished sources known to experts in the field. Among the available electronic scientific database, the popular ones are PUBMED, MEDLINE, and EMBASE.
Sift the studies to select relevant ones
To select the relevant studies from the searches, we need to sift through the studies thus identified. The first sift is pre-screening, i.e., to decide which studies to retrieve in full, and the second sift is selection which is to look again at these studies and decide which are to be included in the review. The next step is selecting the eligible studies based on similar study designs, year of publication, language, choice among multiple articles, sample size or follow-up issues, similarity of exposure, and or treatment and completeness of information.
It is necessary to ensure that the sifting includes all relevant studies like the unpublished studies (desk drawer problem), studies which came with negative conclusions or were published in non-English journals, and studies with small sample size.
Assess the quality of studies
The steps undertaken in evaluating the study quality are early definition of study quality and criteria, setting up a good scoring system, developing a standard form for assessment, calculating quality for each study, and finally using this for sensitivity analysis.
For example, the quality of a randomized controlled trial can be assessed by finding out the answers to the following questions:
- Was the assignment to the treatment groups really random?
- Was the treatment allocation concealed?
- Were the groups similar at baseline in terms of prognostic factors?
- Were the eligibility criteria specified?
- Were the assessors, the care provider, and the patient blinded?
- Were the point estimates and measure of variability presented for the primary outcome measure?
- Did the analyses include intention-to-treat analysis?
Calculate the outcome measures of each study and combine them
We need a standard measure of outcome which can be applied to each study on the basis of its effect size. Based on their type of outcome, following are the measures of outcome: Studies with binary outcomes (cured/not cured) have odds ratio, risk ratio; studies with continuous outcomes (blood pressure) have means, difference in means, standardized difference in means (effect sizes); and survival or time-to-event data have hazard ratios.
Combining studies
Homogeneity of different studies can be estimated at a glance from a forest plot (explained below). For example, if the lower confidence interval of every trial is below the upper of all the others, i.e., the lines all overlap to some extent, then the trials are homogeneous. If some lines do not overlap at all, these trials may be said to be heterogeneous.
The definitive test for assessing the heterogeneity of studies is a variant of Chi-square test (Mantel–Haenszel test). The final step is calculating the common estimate and its confidence interval with the original data or with the summary statistics from all the studies. The best estimate of treatment effect can be derived from the weighted summary statistics of all studies which will be based on weighting to sample size, standard errors, and other summary statistics. Log scale is used to combine the data to estimate the weighting.
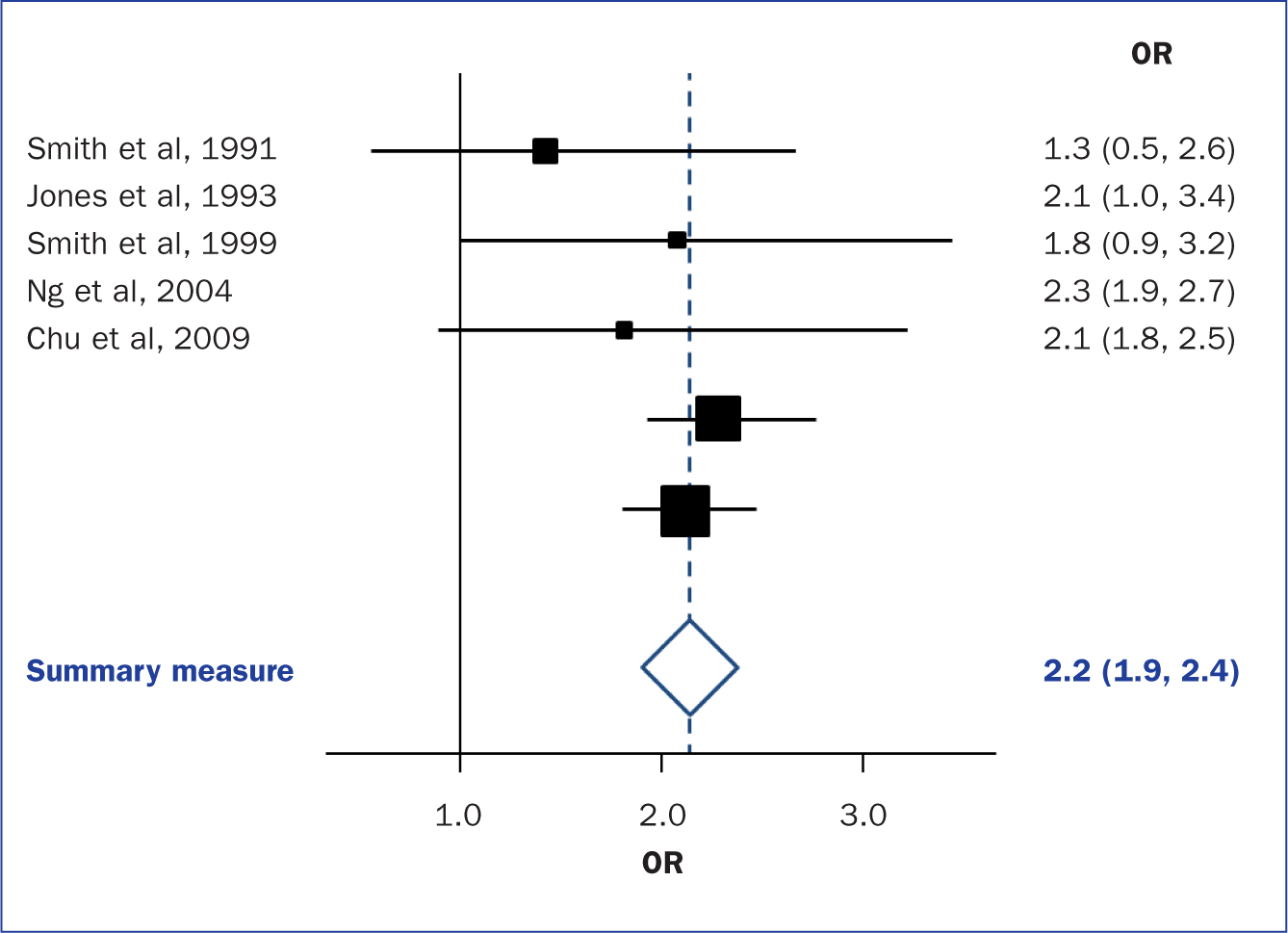
Interpret results: Graph
The results of a meta-analysis are usually presented as a graph called forest plot because the typical forest plots appear as forest of lines. It provides a simple visual presentation of individual studies that went into the meta-analysis at a glance. It shows the variation between the studies and an estimate of the overall result of all the studies together.
Forest plot
Meta-analysis graphs can principally be divided into six columns [ Figure 1 ]. Individual study results are displayed in rows. The first column (“study”) lists the individual study IDs included in the meta-analysis; usually the first author and year are displayed. The second column relates to the intervention groups and the third column to the control groups. The fourth column visually displays the study results. The line in the middle is called “the line of no effect.” The weight (in %) in the fifth column indicates the weighting or influence of the study on the overall results of the meta-analysis of all included studies. The higher the percentage weight, the bigger the box, the more influence the study has on the overall results. The sixth column gives the numerical results for each study (e.g., odds ratio or relative risk and 95% confidence interval), which are identical to the graphical display in the fourth column. The diamond in the last row of the graph illustrates the overall result of the meta-analysis.[ 4 ]

Interpretation of meta-analysis[ 4 ]
Thus, the horizontal lines represent individual studies. Length of line is the confidence interval (usually 95%), squares on the line represent effect size (risk ratio) for the study, with area of the square being the study size (proportional to weight given) and position as point estimate (relative risk) of the study.[ 7 ]
For example, the forest plot of the effectiveness of dexamethasone compared with placebo in preventing the recurrence of acute severe migraine headache in adults is shown in Figure 2 .[ 17 ]

Forest plot of the effectiveness of dexamethasone compared with placebo in preventing the recurrence of acute severe migraine headache in adults[ 17 ]
The overall effect is shown as diamond where the position toward the center represents pooled point estimate, the width represents estimated 95% confidence interval for all studies, and the black plain line vertically in the middle of plot is the “line of no effect” (e.g., relative risk = 1).
Therefore, when examining the results of a systematic reviews/meta-analysis, the following questions should be kept in mind:
- Heterogeneity among studies may make any pooled estimate meaningless.
- The quality of a meta-analysis cannot be any better than the quality of the studies it is summarizing.
- An incomplete search of the literature can bias the findings of a meta-analysis.
- Make sure that the meta-analysis quantifies the size of the effect in units that you can understand.
Subgroup analysis and sensitivity analysis
Subgroup analysis looks at the results of different subgroups of trials, e.g., by considering trials on adults and children separately. This should be planned at the protocol stage itself which is based on good scientific reasoning and is to be kept to a minimum.
Sensitivity analysis is used to determine how results of a systematic review/meta-analysis change by fiddling with data, for example, what is the implication if the exclusion criteria or excluded unpublished studies or weightings are assigned differently. Thus, after the analysis, if changing makes little or no difference to the overall results, the reviewer's conclusions are robust. If the key findings disappear, then the conclusions need to be expressed more cautiously.
Advantages of Systematic Reviews
Systematic reviews have specific advantages because of using explicit methods which limit bias, draw reliable and accurate conclusions, easily deliver required information to healthcare providers, researchers, and policymakers, help to reduce the time delay in the research discoveries to implementation, improve the generalizability and consistency of results, generation of new hypotheses about subgroups of the study population, and overall they increase precision of the results.[ 18 ]
Limitations in Systematic Reviews/Meta-analysis
As with all research, the value of a systematic review depends on what was done, what was found, and the clarity of reporting. As with other publications, the reporting quality of systematic reviews varies, limiting readers’ ability to assess the strengths and weaknesses of those reviews.[ 5 ]
Even though systematic review and meta-analysis are considered the best evidence for getting a definitive answer to a research question, there are certain inherent flaws associated with it, such as the location and selection of studies, heterogeneity, loss of information on important outcomes, inappropriate subgroup analyses, conflict with new experimental data, and duplication of publication.
Publication Bias
Publication bias results in it being easier to find studies with a “positive” result.[ 19 ] This occurs particularly due to inappropriate sifting of the studies where there is always a tendency towards the studies with positive (significant) outcomes. This effect occurs more commonly in systematic reviews/meta-analysis which need to be eliminated.
The quality of reporting of systematic reviews is still not optimal. In a recent review of 300 systematic reviews, few authors reported assessing possible publication bias even though there is overwhelming evidence both for its existence and its impact on the results of systematic reviews. Even when the possibility of publication bias is assessed, there is no guarantee that systematic reviewers have assessed or interpreted it appropriately.[ 20 ]
To overcome certain limitations mentioned above, the Cochrane reviews are currently reported in a format where at the end of every review, findings are summarized in the author's point of view and also give an overall picture of the outcome by means of plain language summary. This is found to be much helpful to understand the existing evidence about the topic more easily by the reader.
A systematic review is an overview of primary studies which contains an explicit statement of objectives, materials, and methods, and has been conducted according to explicit and reproducible methodology. A meta-analysis is a mathematical synthesis of the results of two or more primary studies that addressed the same hypothesis in the same way. Although meta-analysis can increase the precision of a result, it is important to ensure that the methods used for the reviews were valid and reliable.
High-quality systematic reviews and meta-analyses take great care to find all relevant studies, critically assess each study, synthesize the findings from individual studies in an unbiased manner, and present balanced important summary of findings with due consideration of any flaws in the evidence. Systematic review and meta-analysis is a way of summarizing research evidence, which is generally the best form of evidence, and hence positioned at the top of the hierarchy of evidence.
Systematic reviews can be very useful decision-making tools for primary care/family physicians. They objectively summarize large amounts of information, identifying gaps in medical research, and identifying beneficial or harmful interventions which will be useful for clinicians, researchers, and even for public and policymakers.
Source of Support: Nil
Conflict of Interest: None declared.
The Systematic Literature Review: Advantages and Applications in Nonprofit Scholarship
- Research Papers
- Published: 28 September 2021
- Volume 33 , pages 1256–1262, ( 2022 )
Cite this article

- Beth Gazley ORCID: orcid.org/0000-0002-7352-4476 1
1676 Accesses
7 Citations
5 Altmetric
Explore all metrics
Voluntary and nonprofit sector studies are relatively young and still seeking common intellectual ground. One vehicle for accomplishing this task is the systematic literature review (SLR). SLRs approach knowledge generation through a rules-driven comprehensive process for finding and analyzing prior knowledge. SLRs support the voluntary sector’s current emphasis on data transparency in publication. They also support the growth of voluntary sector empiricism by offering a greater claim to reliability and generalizability of findings. Finally, they support goals of inclusiveness and knowledge unification that are important to the voluntary sector academy, its funders, and its constituents. This explanatory article draws on examples from the nonprofit and voluntary sector to describe the rationale and methods of the SLR.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Literature reviews as independent studies: guidelines for academic practice

Reflections on the Methodological Approach of Systematic Reviews

On being ‘systematic’ in literature reviews
Data availabilty.
There is no data, therefore the data-sharing statement is not applicable.
For more on publication bias, see https://methods.cochrane.org/bias/reporting-biases .
Grey literature is industry and government publications outside of academic and commercial publishing channels. They are commonly considered a legitimate element of SLRs. For more, see www.greylit.org .
Alegre, I., & Moleskis, M. (2019). Beyond Financial Motivations in Crowdfunding: A Systematic Literature Review of Donations and Rewards. VOLUNTAS: International Journal of Voluntary and Nonprofit Organizations , pp 1–12.
Bach-Mortensen, A. M., & Montgomery, P. (2018). What are the barriers and facilitators for third sector organisations (non-profits) to evaluate their services? A systematic review. Systematic Reviews, 7 (1), 13.
Article Google Scholar
Bearman, M., Smith, C., Carbone, A., Slade, S., Baik, C., Hughes-Warrington, M., & Neumann, D. L. (2012). Systematic review methodology in higher education. Higher Education Research & Development, 31 , 625–640.
Beugelsdijk, S., van Witteloostuijn, A., & Meyer, K. E. (2020). A new approach to data access and research transparency (DART). Journal of International Business Studies, 51 , 887–905.
Brass, J. N., Longhofer, W., Robinson, R. S., & Schnable, A. (2018). NGOs and international development: A review of thirty-five years of scholarship. World Development, 112 , 136–149.
Brudney, J. L., & Durden, T. K. (1993). Twenty years of the Journal of Voluntary Action Research/Nonprofit and Voluntary Sector Quarterly: An assessment of past trends and future directions. Nonprofit and Voluntary Sector Quarterly, 22 (3), 207–218.
Cooper, H. M. (1988). Organizing knowledge syntheses: A taxonomy of literature reviews. Knowledge in Society, 1 , 104–126.
Google Scholar
Cooper, H. M., Hedges, L.V., & Valentine, J.C. (Eds.). (2009). The handbook of research synthesis and meta-analysis . Russell Sage Foundation.
Corry, O. (2010). Defining and theorizing the third sector. In R. Taylor (Ed.), Third sector research (pp. 11–20). Springer.
Chapter Google Scholar
Coule, T. M., Dodge, J., & Eikenberry, A. M. (2020). Toward a typology of critical nonprofit studies: A literature review. Nonprofit and Voluntary Sector Quarterly . https://doi.org/10.1177/0899764020919807
Denyer, D., & Tranfield, D. (2009). Producing a systematic review. In D. A. Buchanan & A. Bryman (Eds.), The SAGE handbook of organizational research methods (pp. 671–689). Sage.
DiMaggio, P. J. (1995). Comments on" What theory is not". Administrative Science Quarterly, 40 (3), 391–397.
do Adro, F. J. N., & Leitão, J. C. C. (2020). Leadership and organizational innovation in the third sector: A systematic literature review. International Journal of Innovation Studies, 4 (2), 51–67.
Englert, B., & Helmig, B. (2018). Volunteer performance in the light of organizational success: A systematic literature review. Voluntas: International Journal of Voluntary and Nonprofit Organizations , 29 (1), 1–28.
Gazley, B., & Guo, C. (2020). What do we know about nonprofit collaboration? A systematic review of the literature. Nonprofit Management and Leadership, 31 (2), 211–232.
Genet, N., Boerma, W. G., Kringos, D. S., Bouman, A., Francke, A. L., Fagerström, C., Melchiorre, M. G., Greco, C., & Devillé, W. (2011). Home care in Europe: A systematic literature review. BMC Health Services Research, 11 (1), 207.
Hallett, C., Klug, G., Lauber, C., & Priebe, S. (2012). Volunteering in the care of people with severe mental illness: A systematic review. BMC Psychiatry, 12 (1), 226.
Hardwick, R., Anderson, R., & Cooper, C. (2015). How do third sector organisations use research and other knowledge? A Systematic Scoping Review. Implementation Science, 10 (1), 84.
Helmig, B., Ingerfurth, S., & Pinz, A. (2014). Success and failure of nonprofit organizations: Theoretical foundations, empirical evidence, and future research. Voluntas: International Journal of Voluntary and Nonprofit Organizations , 25 (6), 1509–1538.
Hofstede, G. H. (2001). Culture's consequences: Comparing values, behaviors, institutions and organizations across nations . Geert Hofstede (Ed.). Sage.
Hyde, M. K., Dunn, J., Scuffham, P. A., & Chambers, S. K. (2014). A systematic review of episodic volunteering in public health and other contexts. BMC Public Health, 14 (1), 992.
Igalla, M., Edelenbos, J., & van Meerkerk, I. (2019). Citizens in action, what do they accomplish? A systematic literature review of citizen initiatives, their main characteristics, outcomes, and factors. Voluntas: International Journal of Voluntary and Nonprofit Organizations , 30 (5), 1176–1194.
Knutsen, W. L. & Brock, K. L. (2014). Introductory essay: From a closed system to an open system: A parallel critical review of the intellectual trajectories of publicness and nonprofitness. Voluntas: International Journal of Voluntary and Nonprofit Organizations , 25 (5), 1113–1131.
Kuhn, T. S. (1970). The structure of scientific revolutions, 2nd Ed . University of Chicago press.
Laurett, R., & Ferreira, J. J. (2018). Strategy in nonprofit organisations: A systematic literature review and agenda for future research. Voluntas: International Journal of Voluntary and Nonprofit Organizations , 29 (5), 881–897.
Lehner, O. M., & Kansikas, J. (2013). Pre-paradigmatic status of social entrepreneurship research: A systematic literature review. Journal of Social Entrepreneurship, 4 (2), 198–219.
Maier, F., Meyer, M., & Steinbereithner, M. (2016). Nonprofit organizations becoming business-like: A systematic review. Nonprofit and Voluntary Sector Quarterly, 45 (1), 64–86.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med, 6 (7), e1000097.
Ortega-Rodríguez, C., Licerán-Gutiérrez, A., & Moreno-Albarracín, A. L. (2020). Transparency as a Key Element in Accountability in Non-Profit Organizations: A Systematic Literature Review. Sustainability, 12 (14), 5834.
Ouimet, M., Jette, D., Fonda, M., Jacob, S., & Bédard, P. O. (2017). Use of systematic literature reviews in Canadian government departments: Where do we need to go? Canadian Public Administration, 60 (3), 397–416.
Rainey, S., Wakunuma, K., & Stahl, B. (2017). Civil society organisations in research: a literature-based typology. VOLUNTAS: International Journal of Voluntary and Nonprofit Organizations , 28 (5), 1988–2010.
Ringquist, E. (2013). Meta-analysis for public management and policy . John Wiley & Sons.
Salido-Andres, N., Rey-Garcia, M., Alvarez-Gonzalez, L. I., & Vazquez-Casielles, R. (2020). Mapping the field of donation-based crowdfunding for charitable causes: systematic review and conceptual framework. Voluntas: International Journal of Voluntary and Nonprofit Organizations , pp 1–15.
Santos, M. R., Laureano, R. M., & Moro, S. (2020). Unveiling research trends for organizational reputation in the nonprofit sector. VOLUNTAS: International Journal of Voluntary and Nonprofit Organizations , 31 (1), 56–70.
Snyder, H. (2019). Literature review as a research methodology: An overview and guidelines. Journal of Business Research, 104 , 333–339.
Sutton, R. I., & Staw, B. M. (1995). What theory is not. Administrative Science Quarterly , pp 371–384.
Tian, Y., & Konrath, S. (2019). The effects of similarity on charitable giving in donor–donor dyads: A systematic literature review. Voluntas: International Journal of Voluntary and Nonprofit Organizations , pp. 1–24.
Tranfield, D., Denyer, D., & Smart, P. (2003). Towards a methodology for developing evidence-informed management knowledge by means of systematic review. British Journal of Management, 14 (3), 207–222.
van Teunenbroek, C., Bekkers, R., & Beersma, B. (2020). Look to others before you leap: A systematic literature review of social information effects on donation amounts. Nonprofit and Voluntary Sector Quarterly, 49 (1), 53–73.
Yasin, K. I., Adams, A. G., & King, D. P. (2020). How does religion affect giving to outgroups and secular organizations? A systematic literature review. Religions, 11 (8), 405.
Download references
No funding was received for conducting this submitted work.
Author information
Authors and affiliations.
O’Neill School of Public & Environmental Affairs, Indiana University-Bloomington, 1315 East Tenth Street, SPEA 353, Bloomington, IN, 47405, USA
Beth Gazley
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Beth Gazley .
Ethics declarations
Conflict of interest.
There are no potential conflicts of interest and no financial interests to declare.
Human or Animal Participants
There is no research involving human subjects or animals.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Gazley, B. The Systematic Literature Review: Advantages and Applications in Nonprofit Scholarship. Voluntas 33 , 1256–1262 (2022). https://doi.org/10.1007/s11266-021-00410-1
Download citation
Accepted : 28 August 2021
Published : 28 September 2021
Issue Date : December 2022
DOI : https://doi.org/10.1007/s11266-021-00410-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic literature review
- Social equity
- Find a journal
- Publish with us
- Track your research
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Bashir Y, Conlon KC. Step by step guide to do a systematic review and meta-analysis for medical professionals. Ir J Med Sci. 2018; 187:(2)447-452 https://doi.org/10.1007/s11845-017-1663-3
Bettany-Saltikov J. How to do a systematic literature review in nursing: a step-by-step guide.Maidenhead: Open University Press; 2012
Bowers D, House A, Owens D. Getting started in health research.Oxford: Wiley-Blackwell; 2011
Hierarchies of evidence. 2016. http://cjblunt.com/hierarchies-evidence (accessed 23 July 2019)
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2008; 3:(2)37-41 https://doi.org/10.1191/1478088706qp063oa
Developing a framework for critiquing health research. 2005. https://tinyurl.com/y3nulqms (accessed 22 July 2019)
Cognetti G, Grossi L, Lucon A, Solimini R. Information retrieval for the Cochrane systematic reviews: the case of breast cancer surgery. Ann Ist Super Sanita. 2015; 51:(1)34-39 https://doi.org/10.4415/ANN_15_01_07
Dixon-Woods M, Cavers D, Agarwal S Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006; 6:(1) https://doi.org/10.1186/1471-2288-6-35
Guyatt GH, Sackett DL, Sinclair JC Users' guides to the medical literature IX. A method for grading health care recommendations. JAMA. 1995; 274:(22)1800-1804 https://doi.org/10.1001/jama.1995.03530220066035
Hanley T, Cutts LA. What is a systematic review? Counselling Psychology Review. 2013; 28:(4)3-6
Cochrane handbook for systematic reviews of interventions. Version 5.1.0. 2011. https://handbook-5-1.cochrane.org (accessed 23 July 2019)
Jahan N, Naveed S, Zeshan M, Tahir MA. How to conduct a systematic review: a narrative literature review. Cureus. 2016; 8:(11) https://doi.org/10.7759/cureus.864
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1997; 33:(1)159-174
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res. 2014; 14:(1) https://doi.org/10.1186/s12913-014-0579-0
Moher D, Liberati A, Tetzlaff J, Altman DG Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6:(7) https://doi.org/10.1371/journal.pmed.1000097
Mueller J, Jay C, Harper S, Davies A, Vega J, Todd C. Web use for symptom appraisal of physical health conditions: a systematic review. J Med Internet Res. 2017; 19:(6) https://doi.org/10.2196/jmir.6755
Murad MH, Asi N, Alsawas M, Alahdab F. New evidence pyramid. Evid Based Med. 2016; 21:(4)125-127 https://doi.org/10.1136/ebmed-2016-110401
National Institute for Health and Care Excellence. Methods for the development of NICE public health guidance. 2012. http://nice.org.uk/process/pmg4 (accessed 22 July 2019)
Sambunjak D, Franic M. Steps in the undertaking of a systematic review in orthopaedic surgery. Int Orthop. 2012; 36:(3)477-484 https://doi.org/10.1007/s00264-011-1460-y
Siddaway AP, Wood AM, Hedges LV. How to do a systematic review: a best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annu Rev Psychol. 2019; 70:747-770 https://doi.org/0.1146/annurev-psych-010418-102803
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008; 8:(1) https://doi.org/10.1186/1471-2288-8-45
Wallace J, Nwosu B, Clarke M. Barriers to the uptake of evidence from systematic reviews and meta-analyses: a systematic review of decision makers' perceptions. BMJ Open. 2012; 2:(5) https://doi.org/10.1136/bmjopen-2012-001220
Carrying out systematic literature reviews: an introduction
Alan Davies
Lecturer in Health Data Science, School of Health Sciences, University of Manchester, Manchester
View articles · Email Alan
Systematic reviews provide a synthesis of evidence for a specific topic of interest, summarising the results of multiple studies to aid in clinical decisions and resource allocation. They remain among the best forms of evidence, and reduce the bias inherent in other methods. A solid understanding of the systematic review process can be of benefit to nurses that carry out such reviews, and for those who make decisions based on them. An overview of the main steps involved in carrying out a systematic review is presented, including some of the common tools and frameworks utilised in this area. This should provide a good starting point for those that are considering embarking on such work, and to aid readers of such reviews in their understanding of the main review components, in order to appraise the quality of a review that may be used to inform subsequent clinical decision making.
Since their inception in the late 1970s, systematic reviews have gained influence in the health professions ( Hanley and Cutts, 2013 ). Systematic reviews and meta-analyses are considered to be the most credible and authoritative sources of evidence available ( Cognetti et al, 2015 ) and are regarded as the pinnacle of evidence in the various ‘hierarchies of evidence’. Reviews published in the Cochrane Library ( https://www.cochranelibrary.com) are widely considered to be the ‘gold’ standard. Since Guyatt et al (1995) presented a users' guide to medical literature for the Evidence-Based Medicine Working Group, various hierarchies of evidence have been proposed. Figure 1 illustrates an example.
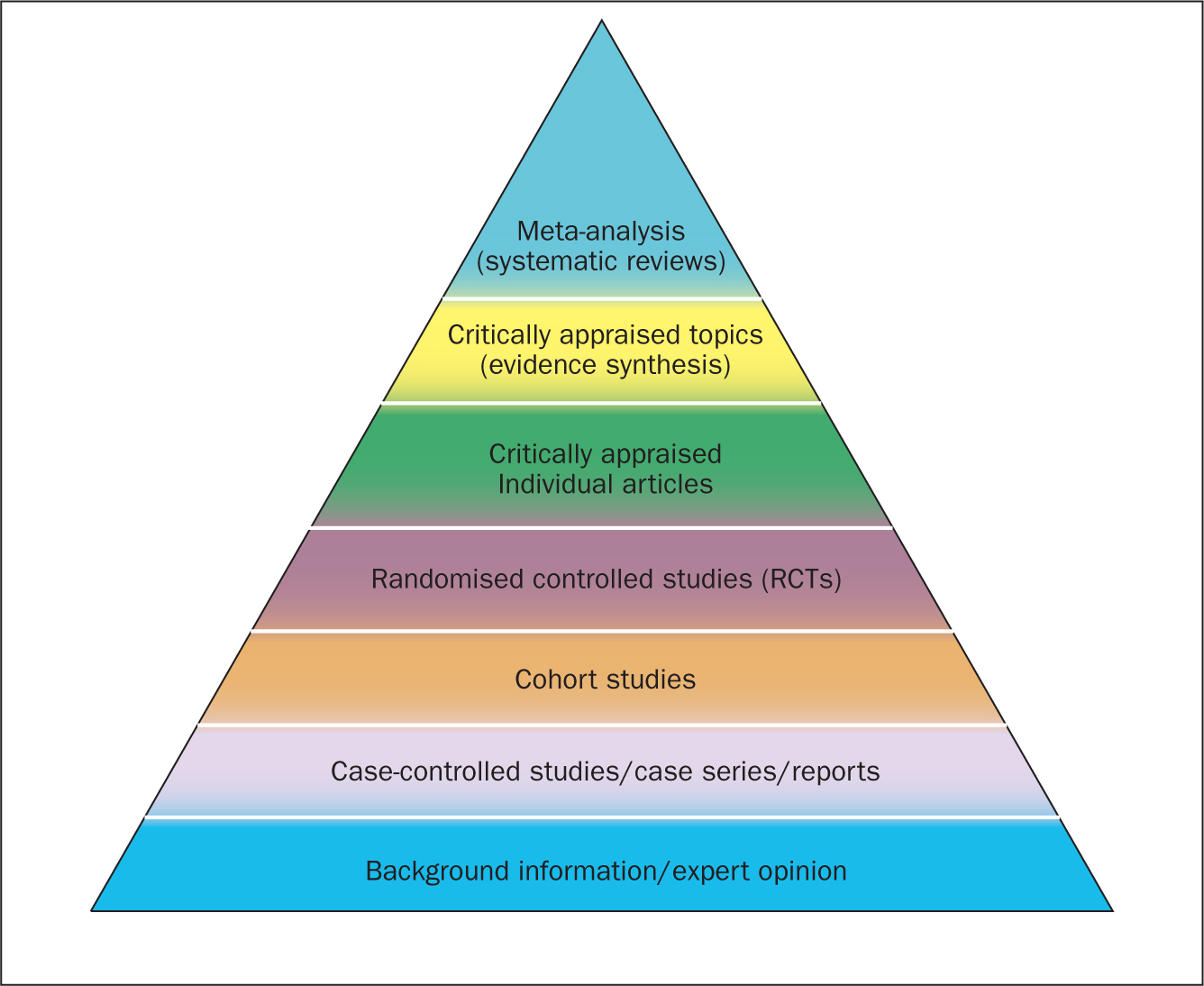
Systematic reviews can be qualitative or quantitative. One of the criticisms levelled at hierarchies such as these is that qualitative research is often positioned towards or even is at the bottom of the pyramid, thus implying that it is of little evidential value. This may be because of traditional issues concerning the quality of some qualitative work, although it is now widely recognised that both quantitative and qualitative research methodologies have a valuable part to play in answering research questions, which is reflected by the National Institute for Health and Care Excellence (NICE) information concerning methods for developing public health guidance. The NICE (2012) guidance highlights how both qualitative and quantitative study designs can be used to answer different research questions. In a revised version of the hierarchy-of-evidence pyramid, the systematic review is considered as the lens through which the evidence is viewed, rather than being at the top of the pyramid ( Murad et al, 2016 ).
Both quantitative and qualitative research methodologies are sometimes combined in a single review. According to the Cochrane review handbook ( Higgins and Green, 2011 ), regardless of type, reviews should contain certain features, including:
- Clearly stated objectives
- Predefined eligibility criteria for inclusion or exclusion of studies in the review
- A reproducible and clearly stated methodology
- Validity assessment of included studies (eg quality, risk, bias etc).
The main stages of carrying out a systematic review are summarised in Box 1 .
Formulating the research question
Before undertaking a systemic review, a research question should first be formulated ( Bashir and Conlon, 2018 ). There are a number of tools/frameworks ( Table 1 ) to support this process, including the PICO/PICOS, PEO and SPIDER criteria ( Bowers et al, 2011 ). These frameworks are designed to help break down the question into relevant subcomponents and map them to concepts, in order to derive a formalised search criterion ( Methley et al, 2014 ). This stage is essential for finding literature relevant to the question ( Jahan et al, 2016 ).
It is advisable to first check that the review you plan to carry out has not already been undertaken. You can optionally register your review with an international register of prospective reviews called PROSPERO, although this is not essential for publication. This is done to help you and others to locate work and see what reviews have already been carried out in the same area. It also prevents needless duplication and instead encourages building on existing work ( Bashir and Conlon, 2018 ).
A study ( Methley et al, 2014 ) that compared PICO, PICOS and SPIDER in relation to sensitivity and specificity recommended that the PICO tool be used for a comprehensive search and the PICOS tool when time/resources are limited.
The use of the SPIDER tool was not recommended due to the risk of missing relevant papers. It was, however, found to increase specificity.
These tools/frameworks can help those carrying out reviews to structure research questions and define key concepts in order to efficiently identify relevant literature and summarise the main objective of the review ( Jahan et al, 2016 ). A possible research question could be: Is paracetamol of benefit to people who have just had an operation? The following examples highlight how using a framework may help to refine the question:
- What form of paracetamol? (eg, oral/intravenous/suppository)
- Is the dosage important?
- What is the patient population? (eg, children, adults, Europeans)
- What type of operation? (eg, tonsillectomy, appendectomy)
- What does benefit mean? (eg, reduce post-operative pyrexia, analgesia).
An example of a more refined research question could be: Is oral paracetamol effective in reducing pain following cardiac surgery for adult patients? A number of concepts for each element will need to be specified. There will also be a number of synonyms for these concepts ( Table 2 ).
Table 2 shows an example of concepts used to define a search strategy using the PICO statement. It is easy to see even with this dummy example that there are many concepts that require mapping and much thought required to capture ‘good’ search criteria. Consideration should be given to the various terms to describe the heart, such as cardiac, cardiothoracic, myocardial, myocardium, etc, and the different names used for drugs, such as the equivalent name used for paracetamol in other countries and regions, as well as the various brand names. Defining good search criteria is an important skill that requires a lot of practice. A high-quality review gives details of the search criteria that enables the reader to understand how the authors came up with the criteria. A specific, well-defined search criterion also aids in the reproducibility of a review.
Search criteria
Before the search for papers and other documents can begin it is important to explicitly define the eligibility criteria to determine whether a source is relevant to the review ( Hanley and Cutts, 2013 ). There are a number of database sources that are searched for medical/health literature including those shown in Table 3 .
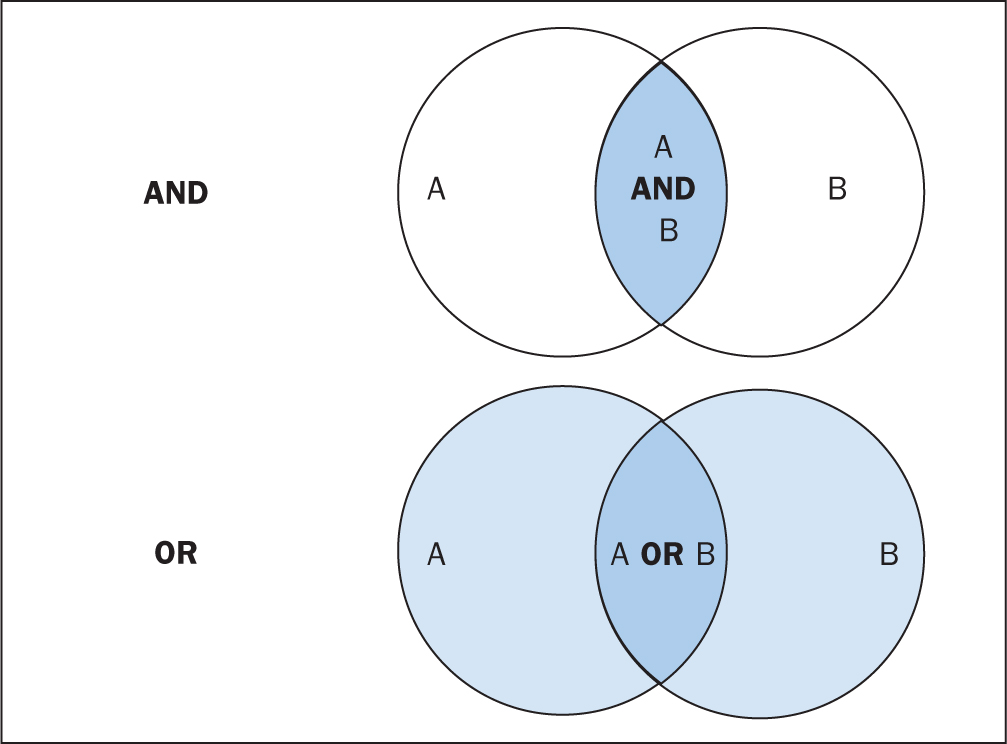
The various databases can be searched using common Boolean operators to combine or exclude search terms (ie AND, OR, NOT) ( Figure 2 ).
Although most literature databases use similar operators, it is necessary to view the individual database guides, because there are key differences between some of them. Table 4 details some of the common operators and wildcards used in the databases for searching. When developing a search criteria, it is a good idea to check concepts against synonyms, as well as abbreviations, acronyms and plural and singular variations ( Cognetti et al, 2015 ). Reading some key papers in the area and paying attention to the key words they use and other terms used in the abstract, and looking through the reference lists/bibliographies of papers, can also help to ensure that you incorporate relevant terms. Medical Subject Headings (MeSH) that are used by the National Library of Medicine (NLM) ( https://www.nlm.nih.gov/mesh/meshhome.html) to provide hierarchical biomedical index terms for NLM databases (Medline and PubMed) should also be explored and included in relevant search strategies.
Searching the ‘grey literature’ is also an important factor in reducing publication bias. It is often the case that only studies with positive results and statistical significance are published. This creates a certain bias inherent in the published literature. This bias can, to some degree, be mitigated by the inclusion of results from the so-called grey literature, including unpublished work, abstracts, conference proceedings and PhD theses ( Higgins and Green, 2011 ; Bettany-Saltikov, 2012 ; Cognetti et al, 2015 ). Biases in a systematic review can lead to overestimating or underestimating the results ( Jahan et al, 2016 ).
An example search strategy from a published review looking at web use for the appraisal of physical health conditions can be seen in Box 2 . High-quality reviews usually detail which databases were searched and the number of items retrieved from each.
A balance between high recall and high precision is often required in order to produce the best results. An oversensitive search, or one prone to including too much noise, can mean missing important studies or producing too many search results ( Cognetti et al, 2015 ). Following a search, the exported citations can be added to citation management software (such as Mendeley or Endnote) and duplicates removed.
Title and abstract screening
Initial screening begins with the title and abstracts of articles being read and included or excluded from the review based on their relevance. This is usually carried out by at least two researchers to reduce bias ( Bashir and Conlon, 2018 ). After screening any discrepancies in agreement should be resolved by discussion, or by an additional researcher casting the deciding vote ( Bashir and Conlon, 2018 ). Statistics for inter-rater reliability exist and can be reported, such as percentage of agreement or Cohen's kappa ( Box 3 ) for two reviewers and Fleiss' kappa for more than two reviewers. Agreement can depend on the background and knowledge of the researchers and the clarity of the inclusion and exclusion criteria. This highlights the importance of providing clear, well-defined criteria for inclusion that are easy for other researchers to follow.
Full-text review
Following title and abstract screening, the remaining articles/sources are screened in the same way, but this time the full texts are read in their entirety and included or excluded based on their relevance. Reasons for exclusion are usually recorded and reported. Extraction of the specific details of the studies can begin once the final set of papers is determined.
Data extraction
At this stage, the full-text papers are read and compared against the inclusion criteria of the review. Data extraction sheets are forms that are created to extract specific data about a study (12 Jahan et al, 2016 ) and ensure that data are extracted in a uniform and structured manner. Extraction sheets can differ between quantitative and qualitative reviews. For quantitative reviews they normally include details of the study's population, design, sample size, intervention, comparisons and outcomes ( Bettany-Saltikov, 2012 ; Mueller et al, 2017 ).
Quality appraisal
The quality of the studies used in the review should also be appraised. Caldwell et al (2005) discussed the need for a health research evaluation framework that could be used to evaluate both qualitative and quantitative work. The framework produced uses features common to both research methodologies, as well as those that differ ( Caldwell et al, 2005 ; Dixon-Woods et al, 2006 ). Figure 3 details the research critique framework. Other quality appraisal methods do exist, such as those presented in Box 4 . Quality appraisal can also be used to weight the evidence from studies. For example, more emphasis can be placed on the results of large randomised controlled trials (RCT) than one with a small sample size. The quality of a review can also be used as a factor for exclusion and can be specified in inclusion/exclusion criteria. Quality appraisal is an important step that needs to be undertaken before conclusions about the body of evidence can be made ( Sambunjak and Franic, 2012 ). It is also important to note that there is a difference between the quality of the research carried out in the studies and the quality of how those studies were reported ( Sambunjak and Franic, 2012 ).
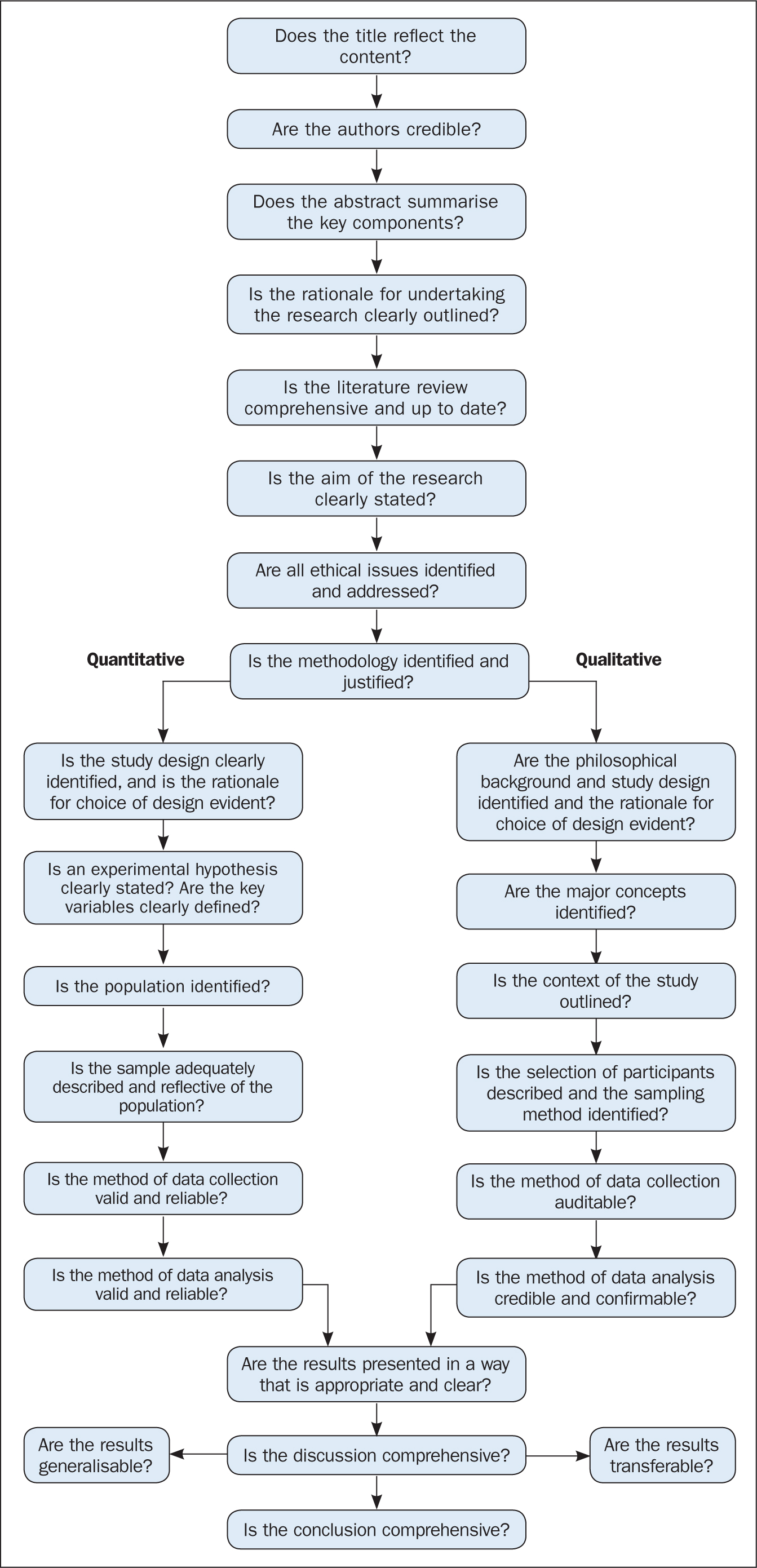
The quality appraisal is different for qualitative and quantitative studies. With quantitative studies this usually focuses on their internal and external validity, such as how well the study has been designed and analysed, and the generalisability of its findings. Qualitative work, on the other hand, is often evaluated in terms of trustworthiness and authenticity, as well as how transferable the findings may be ( Bettany-Saltikov, 2012 ; Bashir and Conlon, 2018 ; Siddaway et al, 2019 ).
Reporting a review (the PRISMA statement)
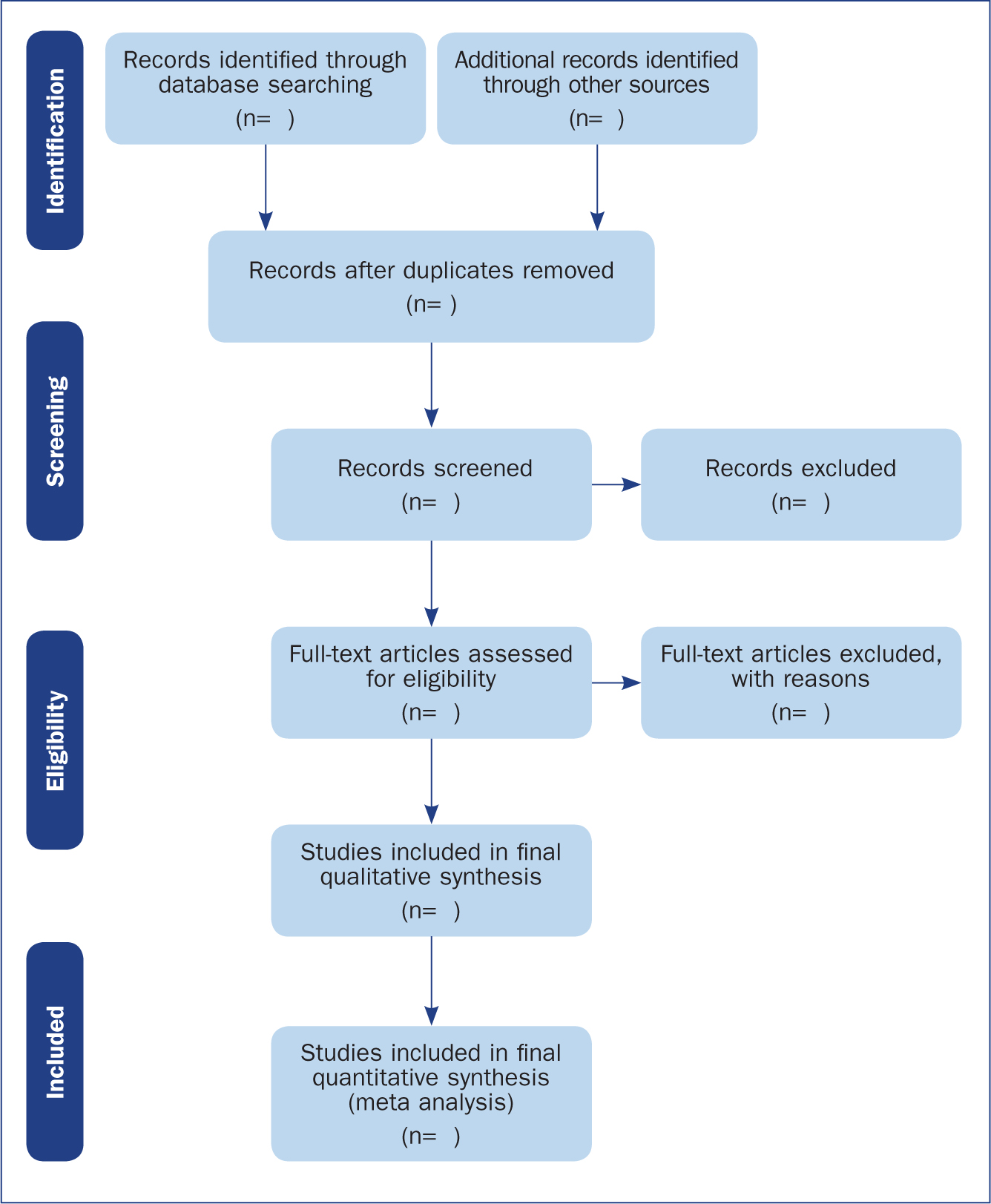
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) provides a reporting structure for systematic reviews/meta-analysis, and consists of a checklist and diagram ( Figure 4 ). The stages of identifying potential papers/sources, screening by title and abstract, determining eligibility and final inclusion are detailed with the number of articles included/excluded at each stage. PRISMA diagrams are often included in systematic reviews to detail the number of papers included at each of the four main stages (identification, screening, eligibility and inclusion) of the review.
Data synthesis
The combined results of the screened studies can be analysed qualitatively by grouping them together under themes and subthemes, often referred to as meta-synthesis or meta-ethnography ( Siddaway et al, 2019 ). Sometimes this is not done and a summary of the literature found is presented instead. When the findings are synthesised, they are usually grouped into themes that were derived by noting commonality among the studies included. Inductive (bottom-up) thematic analysis is frequently used for such purposes and works by identifying themes (essentially repeating patterns) in the data, and can include a set of higher-level and related subthemes (Braun and Clarke, 2012). Thomas and Harden (2008) provide examples of the use of thematic synthesis in systematic reviews, and there is an excellent introduction to thematic analysis by Braun and Clarke (2012).
The results of the review should contain details on the search strategy used (including search terms), the databases searched (and the number of items retrieved), summaries of the studies included and an overall synthesis of the results ( Bettany-Saltikov, 2012 ). Finally, conclusions should be made about the results and the limitations of the studies included ( Jahan et al, 2016 ). Another method for synthesising data in a systematic review is a meta-analysis.
Limitations of systematic reviews
Apart from the many advantages and benefits to carrying out systematic reviews highlighted throughout this article, there remain a number of disadvantages. These include the fact that not all stages of the review process are followed rigorously or even at all in some cases. This can lead to poor quality reviews that are difficult or impossible to replicate. There also exist some barriers to the use of evidence produced by reviews, including ( Wallace et al, 2012 ):
- Lack of awareness and familiarity with reviews
- Lack of access
- Lack of direct usefulness/applicability.
Meta-analysis
When the methods used and the analysis are similar or the same, such as in some RCTs, the results can be synthesised using a statistical approach called meta-analysis and presented using summary visualisations such as forest plots (or blobbograms) ( Figure 5 ). This can be done only if the results can be combined in a meaningful way.
Meta-analysis can be carried out using common statistical and data science software, such as the cross-platform ‘R’ ( https://www.r-project.org), or by using standalone software, such as Review Manager (RevMan) produced by the Cochrane community ( https://tinyurl.com/revman-5), which is currently developing a cross-platform version RevMan Web.
Carrying out a systematic review is a time-consuming process, that on average takes between 6 and 18 months and requires skill from those involved. Ideally, several reviewers will work on a review to reduce bias. Experts such as librarians should be consulted and included where possible in review teams to leverage their expertise.
Systematic reviews should present the state of the art (most recent/up-to-date developments) concerning a specific topic and aim to be systematic and reproducible. Reproducibility is aided by transparent reporting of the various stages of a review using reporting frameworks such as PRISMA for standardisation. A high-quality review should present a summary of a specific topic to a high standard upon which other professionals can base subsequent care decisions that increase the quality of evidence-based clinical practice.
- Systematic reviews remain one of the most trusted sources of high-quality information from which to make clinical decisions
- Understanding the components of a review will help practitioners to better assess their quality
- Many formal frameworks exist to help structure and report reviews, the use of which is recommended for reproducibility
- Experts such as librarians can be included in the review team to help with the review process and improve its quality
CPD reflective questions
- Where should high-quality qualitative research sit regarding the hierarchies of evidence?
- What background and expertise should those conducting a systematic review have, and who should ideally be included in the team?
- Consider to what extent inter-rater agreement is important in the screening process

Strengths and Weaknesses of Systematic Reviews

Automate every stage of your literature review to produce evidence-based research faster and more accurately.
Systematic reviews are considered credible sources since they are comprehensive, reproducible, and precise in stating the outcomes. The type of review system used and the approach taken depend on the goals and objectives of the research. To choose the best-suited review system, researchers must be aware of the strengths and weaknesses of each one.
Let us now look at the strengths and limitations of systematic reviews.
Strengths Of Systematic Reviews
Systematic reviews have become increasingly popular owing to their transparency, accuracy, replicability, and reduced risk of bias. Some of the main benefits of systematic reviews are;
Specificity
Researchers can answer specific research questions of high importance. For example, the efficacy of a particular drug in the treatment of an illness.
Explicit Methodology
A systematic review requires rigorous planning. Each stage of the review is predefined to the last detail. The research question is formulated using the PICO (population, intervention, comparison, and outcome) approach. A strict eligibility criteria is then established for inclusion and exclusion criteria for selecting the primary studies for the review. Every stage of the systematic review methodology is pre-specified to the last detail and made publicly available, even before starting the review process. This makes all the stages in the methodology transparent and reproducible.
Reliable And Accurate Results
The results of a systematic review are either analyzed qualitatively and presented as a textual narrative or quantitatively using statistical methods such as meta-analyses and numeric effect estimates. The quality of evidence or the confidence in effect estimates is calculated using the standardized GRADE approach.
Comprehensive And Exhaustive
A systematic review involves a thorough search of all the available data on a certain topic. It is exhaustive and considers every bit of evidence in synthesizing the outcome. Primary sources for the review are collected from databases and multiple sources, such as blogs from pharmaceutical companies, unpublished research directly from researchers, government reports, and conference proceedings. These are referred to as grey literature. The search criteria and keywords used in sourcing are specific and predefined.
Reproducible
Learn more about distillersr.
(Article continues below)
Weaknesses Of Systematic Reviews
Although systematic reviews are robust tools in scientific research they are not immune to errors. They can be misleading, or even harmful if the data is inappropriately handled or if they are biased. Some of the limitations of systematic reviews include:
Mass Production
Due to the popularity systematic reviews have gained, they tend to be used more than required. The growth rate of systematic reviews has outpaced the growth rate of studies overall. This results in redundancy. For example, a survey published in the BMJ[1], included 73 randomly selected meta-analyses published in 2010 found that for two-thirds of these studies, there was at least one, and sometimes as many as 13, additional meta-analyses published on the same topic by early 2013.
Risk of Bias
Although systematic reviews have many advantages, they are also more susceptible to certain types of biases. A bias is a systematic or methodological error that causes misrepresentation of the study outcomes. As bias can appear at any stage, authors should be aware of the specific risks at each stage of the review process. Most of the known errors in systematic reviews arise in the selection and publication stages. The eligibility criterion in a systematic review helps to avoid selection bias. Poor study design and execution can also result in a biased outcome. It’s important to learn about the types of bias in systematic reviews .
Expressing Strong Opinions by Stealth
Selective outcome reporting is a major threat to a systematic review. The author or reviewer may decide to only report a selection of the statistically significant outcomes that suit his interest. The possibility of unfair or misleading interpretation of evidence outcomes in a systematic review can have serious implications.
Like any review system, systematic reviews have their advantages and disadvantages. Understanding them is essential to making a choice of which review system to use.
Overlapping meta-analyses on the same topic: survey of published studies. BMJ 2013; 347:f4501
3 Reasons to Connect
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 May 2024
Efficacy and safety of vitamin C supplementation in the treatment of community-acquired pneumonia: a systematic review and meta-analysis with trial sequential analysis
- Yogesh Sharma 1 , 2 ,
- Subodha Sumanadasa 3 ,
- Rashmi Shahi 4 ,
- Richard Woodman 5 ,
- Arduino A. Mangoni 6 ,
- Shailesh Bihari 7 &
- Campbell Thompson 8
Scientific Reports volume 14 , Article number: 11846 ( 2024 ) Cite this article
Metrics details
- Respiratory tract diseases
Community-acquired pneumonia (CAP) poses a significant global health challenge, prompting exploration of innovative treatments. This systematic review and meta-analysis aimed to evaluate the efficacy and safety of vitamin C supplementation in adults undergoing treatment for CAP. A comprehensive search of the MEDLINE, Embase, CINAHL, the Cochrane Central Register of Controlled Trials, and Clinical Trials.gov databases from inception to 17 November 2023 identified six randomized-controlled-trials (RCTs) meeting inclusion criteria. The primary outcome analysis revealed a non-significant trend towards reduced overall mortality in the vitamin C group compared to controls (RR 0.51; 95% CI 0.24 to 1.09; p = 0.052; I 2 = 0 ; p = 0.65). Sensitivity analysis, excluding corona-virus-disease 2019 (COVID-19) studies and considering the route of vitamin C administration, confirmed this trend. Secondary outcomes, including hospital length-of-stay (LOS), intensive-care-unit (ICU) LOS, and mechanical ventilation, exhibited mixed results. Notably, heterogeneity and publication bias were observed in hospital LOS analysis, necessitating cautious interpretation. Adverse effects were minimal, with isolated incidents of nausea, vomiting, hypotension, and tachycardia reported. This meta-analysis suggests potential benefits of vitamin C supplementation in CAP treatment. However, inconclusive findings and methodological limitations warrants cautious interpretation, emphasising the urgency for high-quality trials to elucidate the true impact of vitamin C supplementation in CAP management.
Similar content being viewed by others
Adjunctive intravenous then oral vitamin C for moderate and severe community-acquired pneumonia in hospitalized adults: feasibility of randomized controlled trial
Oral versus intravenous antibiotic treatment of moderate-to-severe community-acquired pneumonia: a propensity score matched study
Azithromycin combination therapy for community-acquired pneumonia: propensity score analysis
Introduction.
Community acquired pneumonia (CAP) is defined as an acute infection of the pulmonary parenchyma acquired outside hospital and is a leading cause of morbidity and mortality worldwide. Globally, CAP is the second most common cause of hospitalisation and is the most common infectious cause of death 1 . According to the World Health Organisation (WHO) 2 , lower respiratory tract infections remain the primary infective cause of death globally accounting for 6.1% of deaths.
Inpatient mortality from CAP ranges between 4.2 and 5.5% while mortality at 6 months can be as high as 23% 3 . Recent evidence 4 suggest that despite advancements in clinical care, mortality rates from pneumonia have not any shown any substantial change over time. An excess inflammatory response seems to be partly responsible for treatment failure in some patients with CAP and has been associated with poor clinical response to antibiotics 5 . Therefore, there is a need to explore adjunctive therapies that have immunomodulatory and barrier-enhancing functions augmenting treatment of CAP.
Vitamin C is a water-soluble vitamin with powerful antioxidant properties that can scavenge free radicals 6 . This vitamin has immune mediating properties as it has been found to support neutrophil migration to the site of infection and is responsible for production of hormones such as noradrenaline and vasopressin 6 . These properties have led to an investigation of its potential role as an additional therapeutic agent in the treatment of pneumonia.
Clinical studies of vitamin C supplementation in pneumonia have yielded varied results. While some studies 7 , 8 have suggested that vitamin C supplementation may reduce severity of pneumonia 7 , the impact on mortality remains unclear with one study 9 suggesting a significant reduction in mortality while the other 10 showing no difference in mortality but a trend towards reduction of hospital length of stay (LOS). In addition, the safety of vitamin C in CAP remains unclear. Therefore, we conducted a systematic review to assess the efficacy and safety of parenteral and or oral vitamin C alone or in combination with other therapies in adults being treated for CAP.
Materials and methods
This systematic review and meta-analysis adheres to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA) 2020 standards. The research protocol was registered with the International Prospective Registry of Systematic Reviews (PROSPERO) number CRD42023483860.
Search strategy
We searched the following electronic databases: MEDLINE, Embase, CINAHL, the Cochrane Central Register of Controlled Trials, and Clinical Trials.gov from inception to 17 November 2023 with the help of a medical librarian. The search strategy for this systematic review is provided in Supplementary File 2 . We used a combination of keywords and medical subject headings (MeSH) as follows: adults, community acquired pneumonia, bronchopneumonia, lower respiratory tract infections, hospitalisation, inpatients, critical care, vitamin C, ascorbic acid, ascorbate, mortality, randomised controlled trials (RCTs), placebo, intravenous administration and oral vitamin C. No language restrictions were applied.
Eligibility criteria
Design and population.
We included parallel-arm RCTs of adults aged ≥ 18 years with CAP. Pneumonia was defined as symptoms of fever, dyspnoea, cough, and sputum production along with imaging evidence of a pulmonary infiltrate requiring hospitalisation and possibly intensive care unit (ICU) admission. We included publications in which authors did not clearly define pneumonia but instead used terms such as 'pneumonia' or ‘consolidation on imaging studies' to identify their target population.
Intervention
Clinical trials with at least one arm involving the administration of parenteral and or oral vitamin C alone or in combination with other micronutrients and therapies were included.
Comparator arm
We included studies which had at least one control arm which included patients who were not prescribed parenteral and or oral vitamin C. The control arm may have received placebo or any other active treatment.
Types of outcome measures
Data extraction.
Two reviewers (YS and SS) screened identified citations at the title and abstract screening level using predefined eligibility criteria electronically by use of reference manager. Potentially eligible citations were then reviewed at the level of full-text screening by the paired reviewers. The screening was completely independent and in duplicate and any disagreements were resolved by involvement of a third reviewer (RS). We included studies based upon the eligibility criteria and reporting at least one primary or secondary outcome of interest.
Study quality assessment
The quality of studies was independently assessed by two reviewers (YS and RS) who evaluated the risk of bias using the modified version of the RoB tool (Rob 2.0) 11 and the modified Jadad scale 12 . Risk of bias were classified as low risk, high risk or unclear risk after assessment of the following key domains: generation of random sequence, use of allocation concealment method, blinding of participants, data collectors, and outcome assessors, and incomplete or missing outcome data and other biases. In addition, the quality of studies was independently assessed by the two reviewers by using the modified Jadad scale. Studies with a modified Jadad scale score of 1–3 are considered low-quality studies and those with a score of 4- 7 were considered as high quality studies 12 .
Outcome measures
Primary outcomes.
The primary outcome was overall mortality from date of admission including in-hospital deaths. Different studies have used in-hospital mortality or 30-day mortality. We included mortality data closest to the time points of interest.
Secondary outcomes
The secondary outcomes included length of hospital stay (LOS), intensive care unit (ICU) LOS, 30-day readmission risk, use of vasopressor support, use of non-invasive and invasive ventilation, time to clinical stabilisation (defined previously 13 as patients achieving all the following criteria: (1) temperature ≤ 37.8 °C; (2) heart rate ≤ 100 beats/minute; (3) respiratory rate ≤ 24 breaths/minute; (4) systolic blood pressure ≥ 90 mmHg; and (5) arterial oxygen saturation ≥ 90% or partial pressure of oxygen ≥ 60 mmHg on room air), and adverse events relating to the use of vitamin C.
Effect measures
Binary outcomes were reported as relative risks (RR), while continuous outcomes as standardised mean differences (SMD) with their corresponding 95% confidence intervals (CI).
Statistical analyses
For data processing we converted medians and interquartile ranges (IQR) to means and standard deviations (SD) as suggested by the Cochrane Collaboration Group 14 . The interventions were compared by use of the random effects modelling and Forest plots were generated. The statistical heterogeneity among studies was assessed by use of the chi-squared test and the I 2 statistics. If significant heterogeneity was detected, then a leave-one-out sensitivity analysis 15 was performed in STATA to evaluate the influence of individual studies on the pooled estimate. Publication bias was assessed by visual inspection of the funnel plots and use of the Egger’s test for small-study effects 16 . In case of fewer than 10 studies, Egger’s test reliability is compromised. In such instances, a fail-safe calculation following the Rosenthal approach 17 estimated additional studies needed to assess and mitigate potential publication bias. All statistical analyses were performed by use of Stata software version 18.0 and all estimates were reported with a 95% CI.
Sensitivity analyses
We performed sensitivity analysis after excluding: (1) studies which included only COVID-19 positive patients (as diagnosed by a positive viral reverse transcription polymerase chain reaction (RT-PCR) test results), and (2) studies which used only oral preparations of vitamin C, to determine the differential impact of vitamin C on mortality among CAP patients according to their COVID status and route of vitamin C administration, respectively. In addition, if significant heterogeneity was observed in the included studies, then further exploration was done by use of a leave-one-out sensitivity analysis using STATA.
Trial sequential analysis (TSA)
We conducted a TSA for overall mortality to control for both type-1 and type-2 errors and to further validate the findings of our meta-analysis 18 . The chosen parameters for this analysis were alpha = 5% and beta = 20%. The DerSimonian–Laird random effects model was employed, with between-trial heterogeneity adjusted by the diversity-estimate ( D 2 ) 19 . We used the control group mortality of 15.2%, as determined by this meta-analysis, and the effect size (relative risk reduction (RRR)) of 40% as observed in a previous meta-analysis 20 . Sensitivity analyses were also performed for RRRs of 30% and 20%, respectively.
Additionally, a sensitivity analysis using the Biggerstaff-Tweedie random effects model 21 was conducted, attributing more weight to larger trials than smaller trials. The TSA data analysis was carried out using TSA software (0.9.5.10 Beta, The Copenhagen Trial Unit, Denmark).
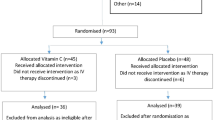
Study identification and selection
Our initial search identified 276 studies from Scopus, Cochrane CENTRAL, ClinicalTrials.gov, MEDLINE and CINHAL (Fig. 1 ) and 2 studies were identified by manual citation searching. Finally, six eligible studies enrolling a total of 366 patients were included in the meta-analysis 7 , 10 , 22 , 23 , 24 , 25 . It is noteworthy that two additional studies 26 , 27 discovered through manual searches of references were excluded from our review. For detailed information, please refer to Supplementary File 3 .
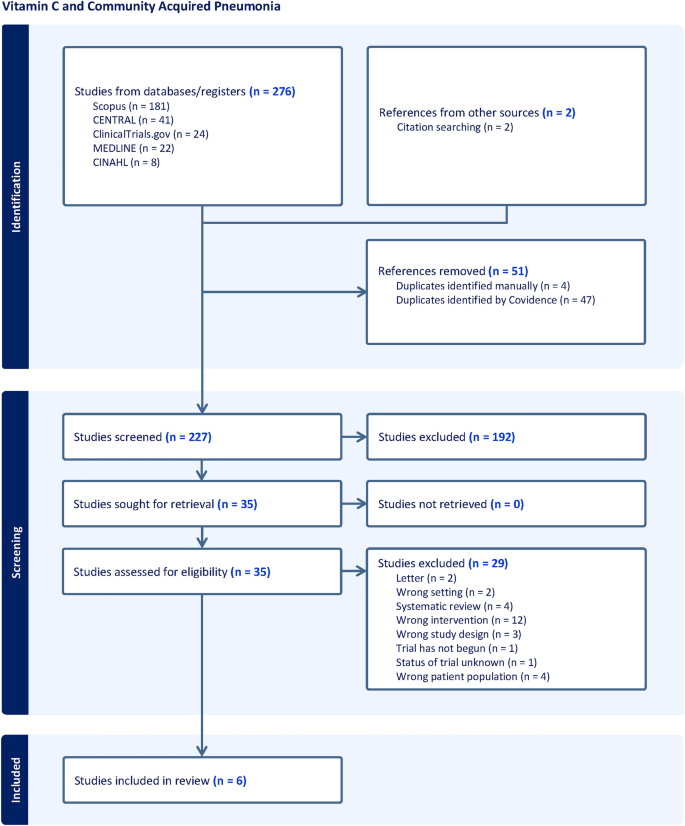
PRISMA flow diagram showing four phases of the study.
Study characteristics
The characteristics of six studies are shown in Table 1 . Two studies included only COVID-19 patients 23 , 25 while two studies used only oral preparations of vitamin C 7 , 24 . Four studies 7 , 10 , 22 , 24 compared vitamin C with a matching placebo and one study 22 included CAP patients who were admitted in the ICU. Five studies 22 , 23 , 24 , 25 were published in 2021 or later.
Assessment of the quality of the included studies based on the Cochrane Collaboration’s Tool is shown in Fig. 2 and the scores of the modified Jadad scale are presented in Table 1 . Apart from two studies 10 , 22 , all studies were graded low quality according to the assessment tools.
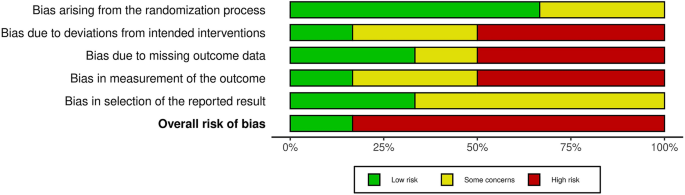
Risk of bias assessment.
Primary outcome
Overall mortality.
Five of the six studies 7 , 10 , 22 , 23 , 25 were included in the analysis for overall mortality, consisting of 314 patients, which included 150 patients in the vitamin C supplemented group and 164 patients in the control group. The overall mortality was lower in the vitamin C supplemented group when compared to the control group, however, this difference was not statistically significant (RR 0.51; 95% CI 0.24 to 1.09; p = 0.052; I 2 = 0 ; p = 0.65) (Fig. 3 ). The Funnel plot (Fig. 4 ) and the regression-based Egger’s test for small-study effects, did not reveal apparent publication bias (p = 0.206). To assess the robustness of the findings and potential publication bias, we conducted a Fail-Safe calculation using the Rosenthal approach. This analysis suggested that an additional 5 studies with a similar effect size (RR = 0.51) would be needed to confirm the absence of publication bias.
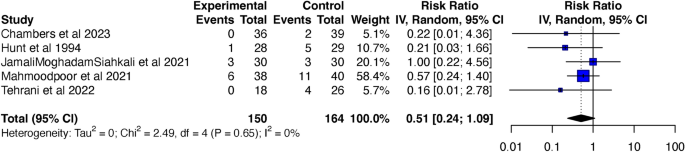
Forest plot showing comparison of overall mortality between vitamin C supplemented group and control group. CI confidence interval.
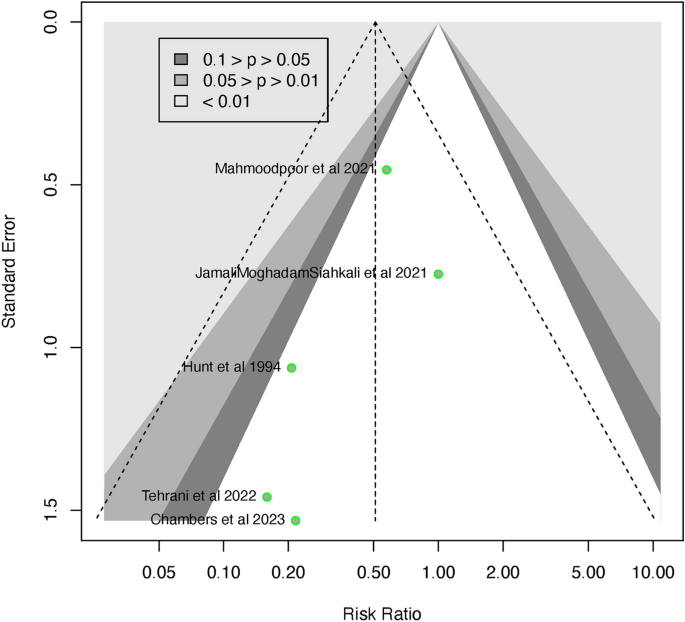
Funnel plot for overall mortality.
Trial sequential analysis
The TSA graphs are presented in Supplementary Figs. S1 , S2 and S3 . Although a relatively large sample size of 908 would be required for a treatment effect of 40%, there was a trend towards significant mortality reduction in the vitamin C supplemented group when compared to control group (RR 0.57; 95% CI 0.28 to 1.17, p = 0.127, I 2 = 0, p = 0.655). Sensitivity analysis using the Biggerstaff-Tweedie random effects model confirmed these findings (RR 0.57; 95% CI 0.44 to 0.74, p = 0.157, I 2 = 0, p = 0.655). Similar trends were also observed for treatment effects of 30% and 20%, although much larger sample sizes, 1699 and 4012, respectively, would be needed to demonstrate a mortality reduction with vitamin C supplementation of patients being treated for pneumonia (Supplementary Figs. S2 and S3 ).
Subgroup analysis
Exclusion of covid19 studies.
After exclusion of COVID-19 studies 23 , 25 , the overall mortality remained lower in patients who were in the vitamin C supplemented group compared to the control group, but the difference remained statistically non-significant (RR 0.46; 95% CI 0.13 to 1.62; p = 0.131 I 2 = 0; p = 0.593) (Supplementary Fig. S4 ). The funnel plot (Supplementary Fig. S5 ) and the Egger’s test did not reveal any apparent publication bias (p = 0.339). The fail-safe calculation using the Rosenthal approach suggested that additional 3 studies, each with a similar effect size (RR = 0.46) would be needed to confirm absence of publication bias.
Route of vitamin C administration
After exclusion of a study which used oral vitamin C 7 , the mortality remained lower among patients in the vitamin C supplemented group compared to those in the control group but was not statistically significant (RR 0.57; 95% CI 0.24 to 1.36; p = 0.122; I 2 = 0, p = 0.64) Supplementary Fig. S6 ). The funnel plot (Supplementary Fig. S7 ) and the Egger’s test did not reveal any publication bias (p = 0.421). The fail-safe calculation using the Rosenthal approach suggested that 1 additional study with a similar effect size (RR = 0.57) would be needed to confirm absence of publication bias.
Hospital LOS
Only three of the six studies 10 , 23 , 25 involving 179 patients determined the efficacy of vitamin C supplementation on hospital LOS. Patients who were in the vitamin C supplemented group had a shorter hospital LOS but this difference was not statistically significant and there was marked heterogeneity between studies (SMD – 0.23; 95% CI – 1.68 to 1.21; p = 0.558; I 2 = 81.1%, p = 0.005) (Supplementary Fig. S8 ). The funnel plot (Supplementary Fig. S9 ) did show some evidence of publication bias, however, the Egger’s test was not significant (p = 0.810).
Exploration of heterogeneity by use of the leave-one-out sensitivity analysis identified one outlier 23 , an open-label randomized controlled trial (RCT). Upon exclusion of this study from the meta-analysis, a statistically significant reduction in hospital LOS was observed in patients receiving vitamin C supplementation compared to the control group, accompanied by a decrease in heterogeneity (SMD – 0.59; 95% CI – 0.96 to – 0.22; p = 0.001 I 2 = 0, p = 0.36) (Supplementary Fig. S10 ). The funnel plot (Supplementary Fig. S11 ) revealed evidence of publication bias and the Egger’s test remained non-significant. To assess the robustness of findings regarding publication bias, a fail-safe calculation using the Rosenthal approach was performed. This calculation suggested that an additional 5 studies, each with a similar effect size (SMD = – 0.23), would be needed to confirm the absence of publication bias.
Analysis of ICU LOS included data from only two of the six studies (Jamali Moghadam Siahkali et al. 23 ; Mahmoodpoor et al. 22 ), comprising a total of 140 patients. The comparison between patients in the vitamin C supplemented group and the control group did not reveal a statistically significant difference in ICU LOS, and the studies exhibited heterogeneity (standardized mean difference [SMD] – 0.13; 95% Confidence Interval [CI] – 3.77 to 3.52; p = 0.737; I 2 = 64.2%, p = 0.09) (see Supplementary Fig. S12 ).
Given the limited number of studies, we refrained from exploring the sources of heterogeneity. Although the funnel plot (Supplementary Fig. S13 ) may not provide statistically informative insights due to the small sample size, it did not exhibit any apparent asymmetry.
Mechanical ventilation
Two studies 22 , 23 involving 140 CAP patients determined the risk of intubation. There was no significant difference in intubation rates in the vitamin C supplemented group when compared to the control group (RR 0.77; 95% CI 0.00 to 122.06, p = 0.634, I 2 = 2%, p = 0.312) (Supplementary Fig. S14 ). The funnel plot (Supplementary Fig. S15 ) did not show any publication bias and the Egger’s test could not be performed due to insufficient number of studies. The fail-safe calculation using the Rosenthal approach suggested that no additional study with a similar effect size (RR = 0.77) would be needed to confirm absence of publication bias.
Vasopressor use
Vasopressor use was reported by only one study 22 which found that the duration of vasopressor use was significantly reduced among patients being treated for CAP who were in the vitamin C supplemented group when compared to placebo (2.28 ± 1.24 days vs. 3.39 ± 1.23 days, p = 0.003). There was no significant difference in the dose of vasopressor used between the two groups (6.8 ± 3.18 mcg/min vs. 8.26 ± 3.58 mcg/min, p = 0.14) in vitamin C and control groups, respectively.
Readmission risk
Only one study 10 reported risk of 30-day readmissions which was not significantly different among treated CAP patients who received vitamin C compared to the control group (3% vs. 11% respectively, p = 0.22).

Time to clinical stabilisation
Time to clinical stability was reported by only one study 10 which found a trend towards early stability among patients with CAP with the administration of vitamin C compared to the control group (median 22 h (IQR 40, 90) vs. 49 h (IQR 18, 137), p = 0.083).
Adverse effects of vitamin C
Only two studies 10 , 22 reported data on adverse effects of supplementation of vitamin C. Chambers et al. 10 reported 2 adverse events which could be possibly related to vitamin C administration including nausea and vomiting, while Mahmoodpoor et al. 22 reported 3 episodes of hypotension and tachycardia during IV administration of vitamin C which were self-limited and resolved after reduction in dose of vitamin C. No study attributed AKI to administration of vitamin C. One study 10 also reported minor adverse effects associated with the use of placebo, including nausea, vomiting and distaste for the medication.
This systematic review and meta-analyses evaluated the efficacy and safety of vitamin C in the treatment of patients with CAP. By including recent RCTs with a substantial number of CAP patients, our primary outcome analysis indicated a noteworthy trend towards a reduction in overall mortality in the vitamin C treatment group when compared to the control group. However, this observed reduction in mortality did not reach statistical significance, warranting careful interpretation of the findings. The TSA confirmed the trend towards reduced mortality in the vitamin C supplemented group but suggested that a sample size of 908 would be required to achieve statistical significance for a 40% reduction in relative risk.
After excluding studies 23 , 25 which included only COVID-19 patients and an older study incorporating oral vitamin C supplementation, the non-significant reduction in mortality persisted between the two groups. The absence of statistical significance in our primary outcome may be attributed to the limited number of studies included in the meta-analysis. This highlights the critical need for future well-designed and adequately powered trials to offer more robust evidence regarding the role of vitamin C in CAP treatment. It is notable that a previous meta-analysis 28 did not identify any studies investigating the mortality benefits of vitamin C in CAP.
Our systematic review contradicts a recent harmonised study 27 combining data from two RCTs 26 , 29 on vitamin C use in COVID-19 patients. This study suggests futility with vitamin C supplementation, but acknowledges limitations, including study design variations, post-randomisation care discrepancies, and lack of COVID-19 vaccination data. These limitations stress the need for cautious interpretation and highlight the importance of additional research to understand the relationship between vitamin C supplementation and outcomes in COVID-19 patients.
Our findings, although non-significant, align with a recent systematic review 30 which included 24 RCTs and suggested that intravenous vitamin C might improve short-term mortality (RR 0.82; 95% CI 0.65 to 1.02; p = 0.07) and overall mortality (RR 0.86; 95% CI 0.74 to 1.01; p = 0.06) in septic patients; their review was not just limited to those with CAP. Despite these promising trends, it is essential to consider the limitations of the studies included in the above meta-analysis, such as high heterogeneity and publication bias. Thus, current evidence on the mortality benefits of vitamin C supplementation during treatment for severe infections, including CAP, remains inconclusive.
Our meta-analysis indicates a potential trend towards a reduction in hospital LOS in the vitamin C supplemented group compared to the control group. However, the studies included in our review exhibited significant heterogeneity. Following sensitivity analysis and the exclusion of an outlier study, our review revealed a statistically significant decrease in hospital LOS in the vitamin C supplemented group compared to the control group. It is crucial to approach this finding with caution due to the inclusion of a limited number of studies with smaller sample sizes in this review, raising the potential for inflated effect sizes as has been highlighted by Zhang et al. 31 .
In contrast, our analysis of ICU length of stay did not reveal a statistically significant difference between the vitamin C and control groups. While this non-significant finding could be influenced by the limited number of studies available for analysis and the observed heterogeneity in study designs, it remains possible that the beneficial effects of vitamin C supplementation are more visible in those less critically unwell. These results are, however, similar to a recent systematic review in septic patients which found that vitamin C did not reduce ICU LOS when compared to the control group (RR – 0.05; 95% CI – 0.19 to 0.09; p = 0.50).
This study suggests that the duration of vasopressor use was significantly shorter among critically ill CAP patients who received vitamin C. However, only one study was available for review, preventing a meta-analysis. Nonetheless, a prior meta-analysis by Muhammad et al. 32 , that included twelve studies on septic patients also reported a statistically significant reduction in vasopressor support time for those treated with vitamin C compared to placebo (SMD = – 1.03; 95% CI – 1.62 to – 0.44; p = 0.001; I 2 = 88.96%). The substantial heterogeneity observed in the studies included in this meta-analysis limits the certainty of the evidence. Therefore, further research is needed to explore the role of vitamin C in reducing vasopressor support among septic patients.
A critical consideration in our analysis is the overall poor quality of the included studies, with the exception of two studies 10 , 22 . The methodological limitations and potential biases in the majority of studies underscore the need for rigorously conducted trials to enhance the reliability of our findings.
Recent research 26 , 32 has primarily focused on the efficacy of vitamin C in critically ill septic patients, who are inherently at a heightened risk for adverse clinical outcomes. There has also been an ongoing debate about the choice of vitamin C preparation used in these studies, with concerns raised that using ascorbic acid instead of sodium ascorbate may exacerbate metabolic acidosis and lead to poorer outcomes 33 . Furthermore, the abrupt discontinuation of vitamin C supplementation could potentially cause a further decline in plasma vitamin C levels, resulting in a rebound increase in oxidant stress 34 . This has contributed to lingering clinical equipoise regarding the benefits of vitamin C in patients with sepsis.
Urgent future research is needed to elucidate the differential effects of vitamin C supplementation in pneumonia and sepsis, considering factors such as dosage, route of administration (intravenous vs. oral), and type of preparation used (sodium ascorbate vs. ascorbic acid). Additionally, exploring a slow tapering regimen instead of abrupt discontinuation could help maintain stable serum vitamin C levels. In addition, more studies are needed to ascertain benefits of vitamin C among non-critically ill patients to determine whether it can prevent further clinical deterioration.
Moreover, future studies should incorporate the vaccination status of participants to better understand the impact of vitamin C on patient outcomes. Considering the potentially protective role of pneumococcal vaccination in patients with CAP 35 , this could be a crucial variable to consider in future research.
Conclusions
In conclusion, our study offers insights into potential benefits of vitamin C supplementation in CAP treatment. While an apparent reduction in overall mortality and hospital LOS was observed, the lack of statistical significance and poor study quality, necessitates cautious interpretation. Our findings emphasise the need for rigorous trials to clarify vitamin C’s true impact on CAP outcomes.
Data availability
Data used for this study are available from the corresponding author on request.
Ferreira-Coimbra, J., Sarda, C. & Rello, J. Burden of community-acquired pneumonia and unmet clinical needs. Adv. Ther. 37 , 1302–1318. https://doi.org/10.1007/s12325-020-01248-7 (2020).
Article PubMed PubMed Central Google Scholar
World Health Organization (WHO). The top 10 causes of death 2019. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (2020).
Ramirez, J. A. et al. Adults hospitalized with pneumonia in the United States: Incidence, epidemiology, and mortality. Clin. Infect. Dis. 65 , 1806–1812. https://doi.org/10.1093/cid/cix647 (2017).
Article PubMed Google Scholar
Pletz, M. W. et al. Unmet needs in pneumonia research: A comprehensive approach by the CAPNETZ study group. Respir. Res. 23 , 239. https://doi.org/10.1186/s12931-022-02117-3 (2022).
Sibila, O., Rodrigo-Troyano, A. & Torres, A. Nonantibiotic adjunctive therapies for community-acquired pneumonia (corticosteroids and beyond): Where are we with them?. Semin. Respir. Crit. Care Med. 37 , 913–922. https://doi.org/10.1055/s-0036-1593538 (2016).
Carr, A. C. & Maggini, S. Vitamin C and immune function. Nutrients https://doi.org/10.3390/nu9111211 (2017).
Hunt, C., Chakravorty, N. K., Annan, G., Habibzadeh, N. & Schorah, C. J. The clinical effects of vitamin C supplementation in elderly hospitalised patients with acute respiratory infections. Int. J. Vitam. Nutr. Res. Int. Z. Vitam. Ernahrungsforschung. J. Int. Vitaminol. Nutr. 64 , 212–219 (1994).
CAS Google Scholar
Khan, I. et al. Efficacy of vitamin C in reducing duration of severe pneumonia in children. J. Rawalpindi Med. Coll. 18 , 55–57 (2014).
Google Scholar
Kim, W. Y. et al. Combined vitamin C, hydrocortisone, and thiamine therapy for patients with severe pneumonia who were admitted to the intensive care unit: Propensity score-based analysis of a before-after cohort study. J. Crit. Care 47 , 211–218. https://doi.org/10.1016/j.jcrc.2018.07.004 (2018).
Article CAS PubMed Google Scholar
Chambers, S. T. et al. Adjunctive intravenous then oral vitamin C for moderate and severe community-acquired pneumonia in hospitalized adults: Feasibility of randomized controlled trial. Sci. Rep. 13 , 11879. https://doi.org/10.1038/s41598-023-37934-z (2023).
Article ADS CAS PubMed PubMed Central Google Scholar
Robertson, C. et al. Practicalities of using a modified version of the Cochrane Collaboration risk of bias tool for randomised and non-randomised study designs applied in a health technology assessment setting. Res. Synth. Methods 5 , 200–211. https://doi.org/10.1002/jrsm.1102 (2014).
Mohsina, S. et al. Assessment of the quality of randomized controlled trials in surgery using Jadad score: Where do we stand?. J. Postgrad. Med. 68 , 207–212. https://doi.org/10.4103/jpgm.JPGM_104_21 (2022).
Article CAS PubMed PubMed Central Google Scholar
Halm, E. A. et al. Time to clinical stability in patients hospitalized with community-acquired pneumonia: Implications for practice guidelines. JAMA 279 , 1452–1457. https://doi.org/10.1001/jama.279.18.1452 (1998).
Clarke, M. The cochrane collaboration and the cochrane library. Otolaryngol. Head Neck Surg. 137 , S52-54. https://doi.org/10.1016/j.otohns.2007.05.050 (2007).
Cordero, C. P. & Dans, A. L. Key concepts in clinical epidemiology: Detecting and dealing with heterogeneity in meta-analyses. J. Clin. Epidemiol. 130 , 149–151. https://doi.org/10.1016/j.jclinepi.2020.09.045 (2021).
Lin, L., Shi, L., Chu, H. & Murad, M. H. The magnitude of small-study effects in the cochrane database of systematic reviews: An empirical study of nearly 30 000 meta-analyses. BMJ Evid. Based Med. 25 , 27–32. https://doi.org/10.1136/bmjebm-2019-111191 (2020).
Fragkos, K. C., Tsagris, M. & Frangos, C. C. Publication bias in meta-analysis: Confidence intervals for rosenthal’s fail-safe number. Int. Sch. Res. Not. 2014 , 825383. https://doi.org/10.1155/2014/825383 (2014).
Article Google Scholar
Imberger, G., Thorlund, K., Gluud, C. & Wetterslev, J. False-positive findings in Cochrane meta-analyses with and without application of trial sequential analysis: An empirical review. BMJ Open 6 , e011890. https://doi.org/10.1136/bmjopen-2016-011890 (2016).
Lew, C. C. H., Lee, Z. Y. & Gluud, C. Trial sequential analysis in critical care medicine: The way forward. Crit. Care Med. 50 , e809–e810. https://doi.org/10.1097/ccm.0000000000005634 (2022).
Lee, Z. Y. et al. Intravenous vitamin C monotherapy in critically ill patients: A systematic review and meta-analysis of randomized controlled trials with trial sequential analysis. Ann. Intensive Care 13 , 14. https://doi.org/10.1186/s13613-023-01116-x (2023).
Thorlund, K. E. J., Wetterslev, J., Brok, J., Imberger, G. & Gluud, C. User Manual for Trial Sequential Analysis (TSA) 2nd edn. (Copenhagen Trial Unit, 2017).
Mahmoodpoor, A. et al. Effect of vitamin C on mortality of critically ill patients with severe pneumonia in intensive care unit: A preliminary study. BMC Infect. Dis. 21 , 616. https://doi.org/10.1186/s12879-021-06288-0 (2021).
JamaliMoghadamSiahkali, S. et al. Safety and effectiveness of high-dose vitamin C in patients with COVID-19: A randomized open-label clinical trial. Eur. J. Med. Res. 26 , 20. https://doi.org/10.1186/s40001-021-00490-1 (2021).
Nikzad, M., Banafshe, H. R., Momen-Heravi, M., Haddad Kashani, H. & Shiehmorteza, M. The effect of vitamin C on procalcitonin biomarker in community-acquired pneumonia. Clin. Mol. Allergy https://doi.org/10.1186/s12948-021-00140-1 (2021).
Tehrani, S. et al. An investigation into the effects of intravenous vitamin C on pulmonary CT findings and clinical outcomes of patients with COVID 19 pneumonia a randomized clinical trial. Urol. J. 19 , 460–465. https://doi.org/10.22037/uj.v18i.6863 (2022).
Lamontagne, F. et al. Intravenous vitamin C in adults with sepsis in the intensive care unit. N. Engl. J. Med. 386 , 2387–2398. https://doi.org/10.1056/NEJMoa2200644 (2022).
Adhikari, N. K. J. et al. Intravenous vitamin C for patients hospitalized with COVID-19: Two harmonized randomized clinical trials. JAMA 330 , 1745–1759. https://doi.org/10.1001/jama.2023.21407 (2023).
Padhani, Z. A. et al. Vitamin C supplementation for prevention and treatment of pneumonia. Cochrane database Syst. Rev. 11 , CD013134. https://doi.org/10.1002/14651858.CD013134.pub3 (2021).
Angus, D. C. et al. The REMAP-CAP (randomized embedded multifactorial adaptive platform for community-acquired pneumonia) study. Rationale and design. Ann. Am. Thorac. Soc. 17 , 879–891. https://doi.org/10.1513/AnnalsATS.202003-192SD (2020).
Wen, C. et al. IV vitamin C in sepsis: A latest systematic review and meta-analysis. Int. J. Clin. Pract. 2023 , 6733465. https://doi.org/10.1155/2023/6733465 (2023).
Zhang, Z., Xu, X. & Ni, H. Small studies may overestimate the effect sizes in critical care meta-analyses: A meta-epidemiological study. Crit. Care 17 , R2. https://doi.org/10.1186/cc11919 (2013).
Muhammad, M. et al. The role and efficacy of vitamin C in sepsis: A systematic review and meta-analysis. Adv. Respir. Med. 90 , 281–299. https://doi.org/10.3390/arm90040038 (2022).
Plummer, M. P., Lankadeva, Y. R. & Bellomo, R. Apples and oranges-all “Vitamin C” may not be created equal. Crit. Care Med. 51 , e281–e282. https://doi.org/10.1097/ccm.0000000000006042 (2023).
Hemilä, H. & Chalker, E. Abrupt termination of vitamin C from ICU patients may increase mortality: Secondary analysis of the LOVIT trial. Eur. J. Clin. Nutr. 77 , 490–494. https://doi.org/10.1038/s41430-022-01254-8 (2023).
Del Rosal, T. et al. Outcome of severe bacterial pneumonia in the era of pneumococcal vaccination. Front. Pediatr. 8 , 576519. https://doi.org/10.3389/fped.2020.576519 (2020).
Download references
Acknowledgements
The authors thank Ms. Catherine Brady, Flinders University Library Services for help in database searches for this review.
Author information
Authors and affiliations.
College of Medicine and Public Health, Flinders University, Adelaide, SA, 5042, Australia
Yogesh Sharma
Division of Medicine, Cardiac & Critical Care, Flinders Medical Centre, Adelaide, SA, 5042, Australia
Flinders Medical Centre, Adelaide, SA, 5042, Australia
Subodha Sumanadasa
Rashmi Shahi
Department of Biostatistics, College of Medicine and Public Health, Flinders University, Adelaide, SA, 5042, Australia
Richard Woodman
Discipline of Clinical Pharmacology, College of Medicine and Public Health, Flinders University, Adelaide, SA, 5042, Australia
Arduino A. Mangoni
Shailesh Bihari
Discipline of Medicine, The University of Adelaide, Adelaide, SA, 5005, Australia
Campbell Thompson
You can also search for this author in PubMed Google Scholar
Contributions
Study Design, Y.S. and C.T.; Methodology, Y.S and R.W.; Data Analysis, Y.S., A.M., R.W., S.B. and C.T.; Data curation, Y.S., S.S. and R.S.; writing—original draft preparation, Y.S.; writing—review and editing, Y.S., A.M. and C.T.
Corresponding author
Correspondence to Yogesh Sharma .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information 1., supplementary information 2., supplementary information 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Sharma, Y., Sumanadasa, S., Shahi, R. et al. Efficacy and safety of vitamin C supplementation in the treatment of community-acquired pneumonia: a systematic review and meta-analysis with trial sequential analysis. Sci Rep 14 , 11846 (2024). https://doi.org/10.1038/s41598-024-62571-5
Download citation
Received : 23 January 2024
Accepted : 19 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1038/s41598-024-62571-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Microbiology newsletter — what matters in microbiology research, free to your inbox weekly.
- Systematic Review
- Open access
- Published: 23 May 2024
Prevalence of human papillomavirus in head and neck cancer patients in India: a systematic review and meta-analysis
- Prakasini Satapathy 1 , 2 ,
- Mahalaqua Nazli Khatib 3 ,
- Shilpa Gaidhane 4 ,
- Quazi Syed Zahiruddin 5 ,
- Hashem Abu Serhan 6 ,
- Rakesh Kumar Sharma 7 , 8 ,
- Divya Sharma 9 ,
- Mithhil Arora 10 ,
- Sarvesh Rustagi 11 ,
- AlKaabi NA ORCID: orcid.org/0000-0002-7680-1141 12 , 13 ,
- Ahmed Alsayyah 14 ,
- Marwan Al-Hajeili 15 ,
- Maha F. Al-Subaie ORCID: orcid.org/0000-0001-5486-8057 16 , 17 ,
- Mubarak Alfaresi ORCID: orcid.org/0000-0003-2523-835X 18 , 19 ,
- Mohammed Alissa ORCID: orcid.org/0000-0002-4045-0810 20 &
- Ali A. Rabaan ORCID: orcid.org/0000-0002-6774-9847 17 , 21 , 22
BMC Infectious Diseases volume 24 , Article number: 516 ( 2024 ) Cite this article
Metrics details
Human papillomavirus (HPV) is increasingly recognized as a significant risk factor in the development of head and neck cancers (HNCs), with varying prevalence and impact. This study aims to systematically review and analyze the prevalence of HPV in HNCs in India, providing insights into regional variations.
A comprehensive literature search was carried out using PubMed, Embase, and Web of Science up to November 10, 2023. Inclusion criteria focused on original research reporting HPV-positive cases among HNC patients in India. We used Nested-Knowledge software, for screening, and data extraction. The modified Newcastle-Ottawa Scale was used for quality assessment of included studies. We pooled the prevalence of HPV among HNC patients and performed a random-effects model meta-analysis using R software (version 4.3).
The search yielded 33 studies, encompassing 4654 HNC patients. The pooled prevalence of HPV infection was found to be 33% (95% CI: 25.8–42.6), with notable heterogeneity (I² = 95%). Analysis of subgroups according to geographical location indicated varying prevalence rates. Specifically, the prevalence was 47% (95% CI: 32.2–62.4) in the eastern regions and 19.8% (95% CI: 10.8–33.4) in the western regions. No evidence of publication bias was detected.
The observed considerable regional disparities on the prevalence of HPV in HNC patients in India emphasizes the need for integrated HPV vaccination and screening programs in public health strategies. The findings underline the necessity for further research to explore regional variations and treatment responses in HPV-associated HNCs, considering the impact of factors such as tobacco use and the potential benefits of HPV vaccination.
Peer Review reports
Introduction
Head and neck cancers (HNC), also known as head and neck squamous cell carcinomas (HNSCC), consist of various malignancies impacting the mucosal surfaces of the upper aerodigestive tract, in areas like the nasopharynx, oral cavity, larynx, oropharynx, hypopharynx, and paranasal sinuses [ 1 ]. Annually, HNSCC is responsible for over 650,000 new cancer cases and causes more than 350,000 deaths worldwide [ 2 , 3 , 4 ]. Traditional primary risk factors for these cancers have been alcohol and tobacco use. However, in recent years, the human papillomavirus (HPV) has been recognized as a significant emerging risk factor, particularly for oropharyngeal squamous cell carcinoma (OPSCC). This has led to the identification of a distinct subtype of HPV-related tumors, which differ from those not associated with HPV. The prevalence of HNSCC tends to vary based on the specific anatomical location and the geographic area [ 5 ].
The carcinogenic nature of HPV was definitively established in 1983 when Durst et al. successfully cloned HPV type 16 from cervical carcinoma tissue [ 6 ]. It is now widely acknowledged that high-risk HPV types are accountable for almost all cases of cervical cancer. While most HPV infections are asymptomatic and tend to resolve spontaneously, persistent HPV infection in the basal cells of the cervix can lead to the development of cervical cancer [ 6 , 7 ].
Numerous research articles indicate that epithelial cells from the oral cavity and tonsils can undergo immortalization through the influence of the full-length HPV-16 or its E6/E7 oncogenes [ 8 , 9 , 10 , 11 , 12 ]. Furthermore, studies using transgenic mice have shown that the E6/E7 genes of HPV 16 significantly heighten the risk of developing oral and oropharyngeal cancers [ 13 ]. It was found that the E7 gene, in particular, is more effective in triggering these cancers, yet there is a noticeable synergistic effect between E6 and E7 in the genesis of HNSCC [ 14 ].
In 2020, India accounted for 7% of the total cancer cases worldwide and a significant 24% of the global incidence of HPV-related cancers [ 15 ]. Additionally, it was reported that 80% of cervical cancer cases in India were attributed to HPV subtypes 16 and 18 [ 16 , 17 ]. As part of its cancer control strategy, India has started implementing opportunistic screening programs for common cancers, including those of the cervix and oral cavity, in its healthcare facilities [ 18 ]. A notable increase in HNC occurrences was observed in the population-based cancer registries (PBCRs) for cities such as Aurangabad, Delhi, Chennai, and Bhopal among men, and in Nagpur among women, in India [ 19 ]. The age-adjusted incidence rate of HNC stood at approximately 25.9 (95% CI 25.7–26.1) and 8.0 (95% CI 7.9–8.1) per 100,000 people for men and women, respectively [ 20 ]. HNC represented around 26% of all cancer diagnoses in men and 8% in women. The likelihood of being diagnosed with HNC was 1 in 33 for men and 1 in 107 for women [ 20 ].
Despite the growing body of literature on HPV’s role in HNC, there remains a lack of consensus on its prevalence and impact. This variability is partly due to differences in study designs, population demographics, and detection methods used across various research studies. A systematic review and meta-analysis of the existing studies can provide a more comprehensive understanding of HPV’s prevalence in HNC, offering insights into regional variations.
This systematic review was conducted in accordance with PRISMA guidelines [ 21 ] (Table S1 ) and has been registered in PROSPERO.
Literature search
An electronic literature search was conducted in various databases, including PubMed, Embase, and Web of Science from inception up to November 10, 2023. Keywords and MeSH terms related to HPV and HNC were used to devise the search strategy. No restrictions have been placed on the type of article, year of publication, or language in the search. Table S2 shows the detailed search strategy.
Inclusion criteria
Original research that reports the number of HPV-positive cases among HNC patients is included in this study. We are considering only studies conducted in India. Excluded from this study are case reports, case series, or studies lacking quantitative data. The same exclusion criteria apply to animal studies, commentaries, in vitro studies, and reviews. Studies from any location within India, whether conducted in a hospital or community setting, are eligible. There are no restrictions on the type of test used to detect HPV. A detailed inclusion criterion is specified in Table S3 .
Screening and study selection
Two independent reviewers performed the screening of the articles. Nested-Knowledge software was employed for this process. The screening involved a primary review of titles and abstracts, followed by a full-text reading to assess the eligibility of studies for inclusion. An independent third reviewer was consulted to resolve any discrepancies.
Data extraction and quality assessment
Data extraction was performed using the Tag function of the Nested-Knowledge software. Three reviewers carried out the data extraction process. A fourth reviewer cross-checked and validated the extracted data. The data extracted covered the author’s name, year of publication, state/location of the study, study design, age and percentage of males in the sample, total number of HNC patients in the study, number of HPV-positive samples, and the type of test employed for detecting HPV. Quality assessment was done using a modified Newcastle-Ottawa Scale (NOS) version [ 22 , 23 ].
Statistical analysis
A pooled prevalence of HPV is determined by performing a meta-analysis. A random-effects model is employed to conduct the meta-analysis. The variability in study outcomes was measured using the I 2 statistic, which quantifies heterogeneity on a scale from 0 to 100%, where higher values indicate greater heterogeneity [ 24 ]. The heterogeneity was further assessed using the 95% prediction interval. We calculated the tau-squared value using maximum likelihood estimation to gain additional insights into heterogeneity [ 25 , 26 , 27 , 28 ]. Subgroup analysis was conducted based on the location of the study. We used a funnel plot and the Egger test to detect any potential publication bias. A p-value below 0.05 was typically regarded as statistically significant. All statistical analyses were performed using R software, version 4.3 [ 23 , 29 , 30 ].
In the literature search, 4,972 articles were identified from multiple databases. Among these, 521 were duplicates. After removing duplicates, 4,451 articles were subjected to screening, of which 3,981 were excluded. The remaining 470 articles were screened by full text for eligibility, resulting in the exclusion of 440, leaving 30 for inclusion. Additionally, 3 studies were added from a citation search. Finally, 33 studies were included in the review. Figure 1 depicts the PRISMA flow chart of the selection and screening process.
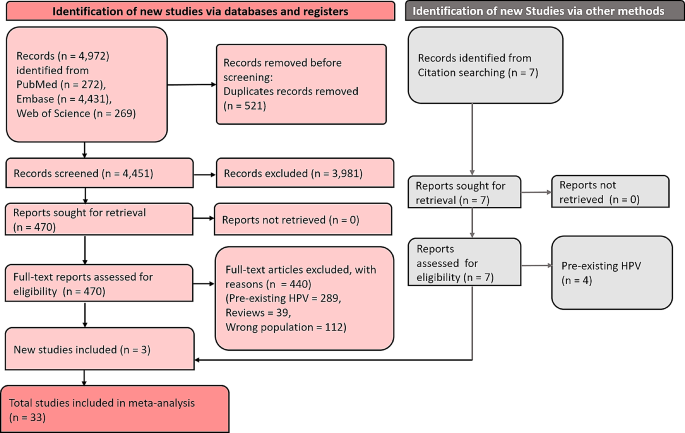
PRISMA flow diagram showing the screening and selection process
Characteristics of included studies
The studies included in this review examining the prevalence of HPV in HNC cases in India are characterized by a diverse methodology and geographical spread. Table 1 summarises the characteristics of included studies. These investigations employ various study designs, including prospective, retrospective, case-control, cohort, and cross-sectional studies, providing a thorough exploration of the subject. The studies are conducted across multiple states and regions of India, representing a broad geographic distribution, and include participants across different age groups, offering insights into age-related variations in HPV prevalence. The proportion of male participants in these studies varies, suggesting potential gender differences in HPV prevalence. The primary diagnostic methods used in these studies are Polymerase Chain Reaction (PCR), genotyping, PCR and P16 Immunohistochemistry (IHC), and Chromogenic In Situ Hybridization (ISH), noted for their high sensitivity. The size of the study populations ranges from small cohorts to large groups, affecting the statistical power of the findings. Rates of HPV positivity exhibit considerable variability, underlining the complexity of understanding HPV prevalence in HNC in this context. These studies span a wide time frame, allowing for the analysis of temporal trends in HPV prevalence. New Delhi contributed 4 studies to the research on HPV prevalence in HNC [ 31 , 32 , 33 ], while Uttar Pradesh was represented by 5 studies [ 34 , 35 , 36 , 37 , 38 ]. Maharashtra was the focus of 4 studies [ 39 , 40 , 41 , 42 ]. Multiple studies were conducted in South India [ 43 , 44 ], Haryana [ 45 , 46 , 47 ], and Tamil Nadu [ 48 , 49 ]. Single studies were conducted in several other locations: Andhra Pradesh [ 50 ], Kerala [ 51 ], Kolkata [ 52 ], Mumbai [ 53 , 54 ], Karnataka [ 55 , 56 ], Chandigarh [ 57 , 58 ], and Assam [ 59 , 60 ]. Additionally, one study was a multi-regional study encompassing several states [ 42 ]. The included studies were overall of moderate to high quality in modified NOS (Table S4 ).
Meta-analysis
From 33 studies encompassing a total of 4654 patients with HNC, the pooled prevalence of HPV infection was determined to be 33% (95% CI: 25–42%). Notably, substantial heterogeneity was observed among these studies (I² = 96%). A prediction interval ranging from 6.2 to 79% was also observed. Figure 2 illustrates the forest plot depicting the pooled prevalence.
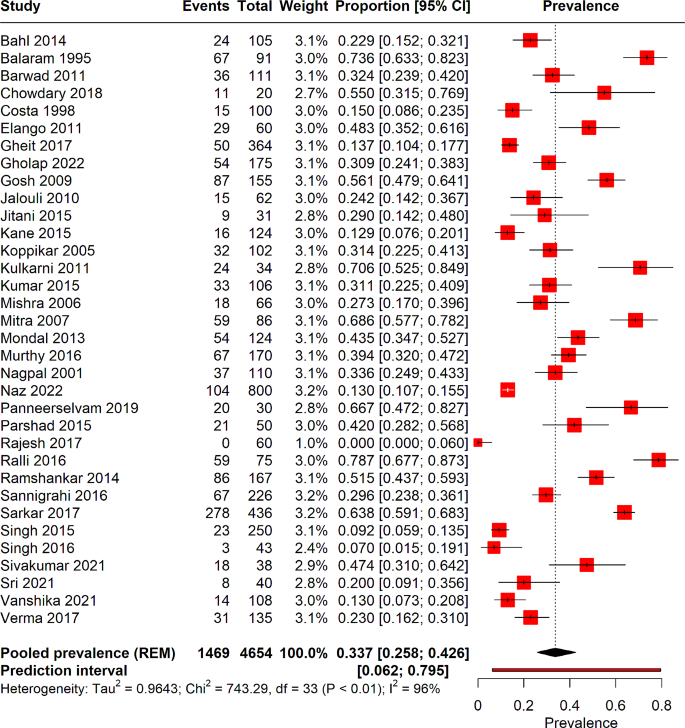
Forest plot depicting the overall HPV pooled prevalence in head and neck cancer patients
Subgroup analysis
Subgroup analysis was performed on the basis of the location of the study (Fig. 3 ). The North region is represented by 14 studies encompassing a total of 2236 patients, revealing a pooled HPV prevalence of 27% (95% CI: 17.4–40.4%), and a high degree of heterogeneity (I² = 95%). The South region, with 7 studies and 335 patients, has a pooled prevalence of 46.3% (95% CI: 15.6–80%), also accompanied by significant heterogeneity (I² = 87%). In the West Middle region, 5 studies totalling 865 patients show a pooled prevalence of 19.8% (95% CI: 10.8–33.4%) with substantial heterogeneity (I² = 88%). A single study spans multiple locations—Madhya Pradesh, Gujarat, Rajasthan, Uttar Pradesh, West Bengal, and Assam—encompassing 170 patients and reporting a higher pooled prevalence of 39% (95% CI: 32–47%). Lastly, the East region, represented by 7 studies with 1048 patients, presents a pooled prevalence of 47% (95% CI: 32.2–62.4%) with high heterogeneity (I² = 92%).
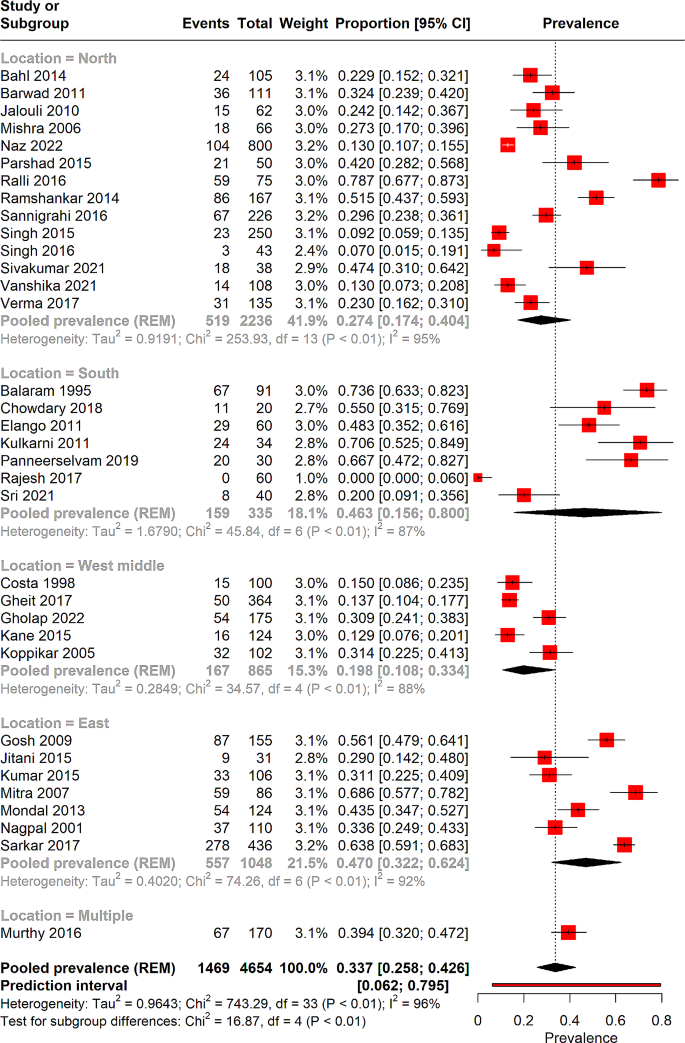
Forest plot illustrating the results of sub-group analysis-based location
Meta-regression and sensitivity analysis
Meta-regression was performed to determine the effect of sample size on the pooled prevalence of HPV in HNC cases, as depicted in Fig. 4 . However, the meta-regression analysis indicated that sample size was not significantly associated with the pooled prevalence results ( p = 0.20). Additionally, a leave-one-out sensitivity analysis was conducted to identify individual studies that might affect the overall prevalence rate. This analysis revealed that the exclusion of no single study resulted in any significant changes to the overall pooled prevalence, as illustrated in Fig. 5 .
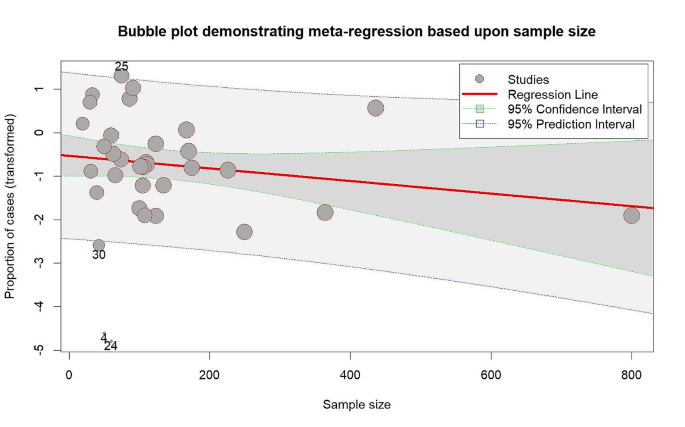
Bubble plot depicting the results of meta-regression based on sample size
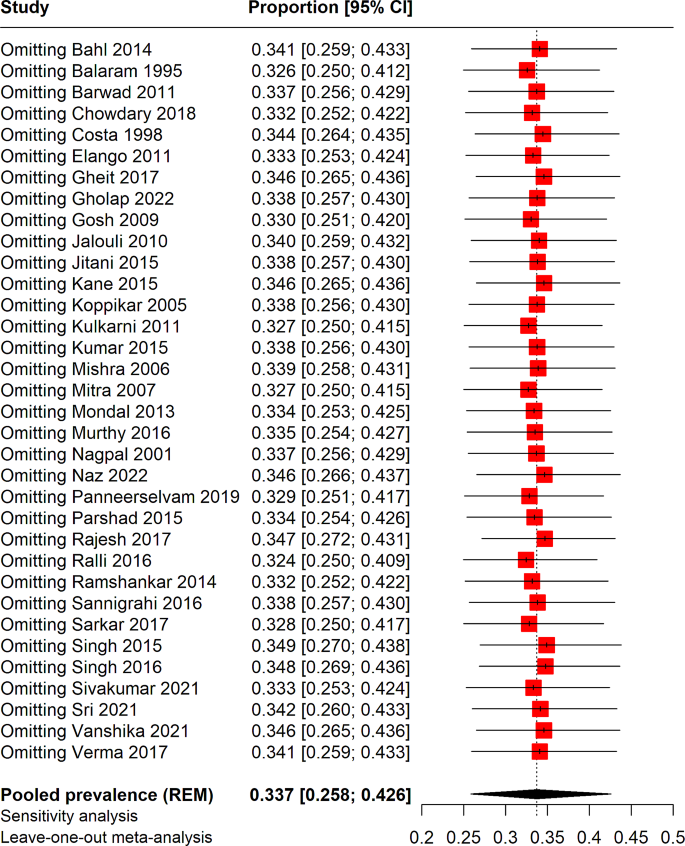
Sensitivity analysis of pooled prevalence
Publication bias
Publication bias was assessed using funnel plot asymmetry and Egger’s test, as shown in Figure S1 . The results of our analysis did not provide evidence of publication bias (Egger’s test, p = 0.71).
In the best of our knowledge, this is the first meta-analysis to determine the prevalence of HPV among HNC patients in India. In our analysis, we found an overall prevalence of 33% for HPV among HNC patients. South India and the eastern part of India have shown slightly greater prevalence compared to the north and west parts of India. Meta-regression, sensitivity analysis couldn’t resolve the s0000ource of heterogeneity.
Previous systematic reviews have established evidence that infection with HPV is a distinct risk factor for developing HNCs [ 61 , 62 ]. The risk associated with tonsil carcinoma is notably high and aligns with what one would anticipate from an infectious cause. Our findings indicate that HPV’s involvement in tonsil cancer is similar to the role of Epstein-Barr virus in nasopharyngeal cancer, suggesting that this is yet another instance of a virus-induced cancer in the pharyngeal lymphoid tissue [ 62 ].
The risk associated with the progression or death, along with the likelihood of developing a secondary primary HNOSCC, increases by 1% and 1.5% respectively for each additional year of smoking. This remains true even when accounting for the HPV tumor status and other important factors. Importantly, the risk of death doubles for patients who continue smoking during radiation therapy. The detection of HPV in HNCs is highly significant for prognosis and can influence the modification of treatment plans based on the HPV status [ 63 ]. Thus, the accurate identification of HPV as a contributing factor in HNCs is of paramount importance. Typically, a biopsy or cytological analysis from the primary tumor site or enlarged lymph nodes is crucial for an initial diagnosis. PCR or RT-PCR (Reverse Transcriptase-PCR) are commonly employed methods for detecting HPV in tumor tissues, particularly for identifying E6/E7 in fresh frozen samples. However, these methods are associated with high setup costs and longer turnaround times [ 64 ].
The presence of HPV in HNCs significantly alters the disease’s prognosis and therapeutic approach. HPV-positive HNCs typically present with a better response to standard treatment modalities like radiotherapy and chemotherapy, leading to an overall better prognosis compared to HPV-negative cases [ 65 ]. This is primarily attributed to the distinct biological behavior of HPV-positive tumors, which tend to be more sensitive to radiation and cytotoxic agents. Studies has indicated that individuals diagnosed with HPV-positive oropharyngeal cancer have higher survival rates and lower risks of recurrence [ 66 ].
Given these differences, there is an emerging consensus on tailoring treatment strategies based on HPV status. For instance, the concept of treatment de-escalation for HPV-positive HNCs is gaining traction. This approach involves reducing the intensity of standard treatments to minimize long-term side effects without compromising the efficacy of cancer control [ 67 ]. Clinical trials are currently exploring various de-escalation strategies, including reduced-dose radiotherapy, omission of chemotherapy, and the use of minimally invasive surgeries [ 68 , 69 ]. However, it’s important to approach de-escalation cautiously, ensuring that patient selection is based on robust biomarkers and clinical criteria to avoid under-treatment.
The accurate determination of HPV status in HNCs is pivotal for both prognostic assessment and guiding treatment decisions. Polymerase Chain Reaction (PCR) and Reverse Transcriptase-PCR (RT-PCR) are the gold standards for detecting HPV, particularly E6/E7 mRNA, in tumor tissues [ 70 , 71 , 72 ]. These methods are highly sensitive and specific but are often hindered by high costs and longer turnaround times, posing challenges in resource-limited settings. Emerging diagnostic techniques, such as liquid biopsies and next-generation sequencing (NGS), are promising alternatives. Liquid biopsies, which detect circulating tumor DNA (ctDNA) in blood samples, offer a less invasive method for HPV detection and monitoring [ 73 , 74 , 75 ]. NGS, on the other hand, allows for the comprehensive analysis of HPV integration sites and co-mutations, providing a more detailed tumor profile [ 76 ]. These technologies not only improve the accessibility of HPV testing but also enhance our understanding of the tumor biology, which is crucial for personalized medicine.
The significant role of HPV in HNCs necessitates public health interventions, particularly in countries like India where the burden of these cancers is high. HPV vaccination, which has been successful in reducing the incidence of cervical cancer, presents a viable strategy to curb HPV-related HNCs. The expansion of HPV vaccination programs to include both girls and boys could significantly reduce the future burden of these cancers [ 77 , 78 ]. It is crucial to integrate HPV vaccination into national immunization programs and to raise public awareness about its benefits. Furthermore, the compounded risk of tobacco use in HPV-positive HNC patients highlights the urgent need for effective tobacco cessation programs. Tobacco, being a well-established risk factor for HNCs, exacerbates the risk even in the context of HPV-positive cancers. Public health campaigns targeting tobacco cessation are not only essential for preventing HNCs but also for improving outcomes in patients with existing HPV-related cancers [ 79 , 80 , 81 ].
Our study acknowledges certain limitations that should be considered. Firstly, our analysis was restricted to articles published in the English language, potentially omitting relevant research published in other languages. Additionally, the geographic coverage of our data is not comprehensive; studies from all regions of India were not available, which may affect the generalizability of our findings. While subgroup analysis was conducted, it was not sufficient to completely address the sources of heterogeneity observed in the results. We were unable to perform subgroup analysis based on site-specific cancer prevalence due to the unavailability of reported data. Future studies should include detailed data on site-specific HNC and HPV to facilitate more comprehensive analyses. This heterogeneity could stem from various factors such as differences in study design, populations, or methodologies, which our subgroup analysis could not fully disentangle. The overall sample size of the included studies was relatively small. This limitation could impact the statistical power of our findings and might lead to less precise estimates. Given these constraints, we recommend that future research should include a broader range of languages and geographic areas, especially underrepresented regions of India. More extensive studies with larger sample sizes would also be beneficial to provide more robust and generalizable results, and to further explore the sources of heterogeneity observed in this study. The absence of publication bias in our findings further strengthens the reliability of these insights.
This comprehensive study underscores the significant role of HPV in the epidemiology of HNCs in India. Through a detailed systematic review and meta-analysis, we determined that the pooled prevalence of HPV among HNC patients in India is 33%, revealing a substantial impact of this virus on such cancers. Notably, the study highlighted regional variations, with the highest prevalence in eastern India (47%) and lowest in the western regions ( ∼ 20%). This variability suggests the influence of regional factors in the prevalence and impact of HPV in HNCs. Overall, our study provides valuable data for healthcare professionals and policymakers, emphasizing the need for targeted interventions and policies to address the HPV-related burden in HNC patients in India, while also considering the regional disparities in prevalence and risk factors.
Data availability
All the data used in this review has been provided in the manuscript and supplementary files.
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR. Head and neck squamous cell carcinoma. Nat Reviews Disease Primers. 2020;6(1):92.
Article PubMed Google Scholar
Leemans CR, Snijders PJ, Brakenhoff RH. The molecular landscape of head and neck cancer. Nat Rev Cancer. 2018;18(5):269–82.
Article CAS PubMed Google Scholar
Hashim D, Genden E, Posner M, Hashibe M, Boffetta P. Head and neck cancer prevention: from primary prevention to impact of clinicians on reducing burden. Ann Oncol. 2019;30(5):744–56.
Article CAS PubMed PubMed Central Google Scholar
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2018;68(6):394–424.
Article Google Scholar
Sabatini ME, Chiocca S. Human papillomavirus as a driver of head and neck cancers. Br J Cancer. 2020;122(3):306–14.
Dürst M, Gissmann L, Ikenberg H, Zur Hausen H. A papillomavirus DNA from a cervical carcinoma and its prevalence in cancer biopsy samples from different geographic regions. Proc Natl Acad Sci. 1983;80(12):3812–5.
Article PubMed PubMed Central Google Scholar
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–9.
Lace MJ, Anson JR, Klussmann JP, Wang DH, Smith EM, Haugen TH, et al. Human papillomavirus type 16 (HPV-16) genomes integrated in head and neck cancers and in HPV-16-immortalized human keratinocyte clones express chimeric virus-cell mRNAs similar to those found in cervical cancers. J Virol. 2011;85(4):1645–54.
Sexton CJ, Proby CM, Banks La, Stables JN, Powell K, Navsaria H, et al. Characterization of factors involved in human papillomavirus type 16-mediated immortalization of oral keratinocytes. J Gen Virol. 1993;74(4):755–61.
Smeets SJ, van der Plas M, Schaaij-Visser TB, van Veen EA, van Meerloo J, Braakhuis BJ, et al. Immortalization of oral keratinocytes by functional inactivation of the p53 and pRb pathways. Int J Cancer. 2011;128(7):1596–605.
Park N-H, Min B-M, Li S-l, Huang MZ, Doniger J. Immortalization of normal human oral keratinocytes with type 16 human papillomavirus. Carcinogenesis. 1991;12(9):1627–31.
Chen R, Aalto Y, Teesalu T, Dürst M, Knuutila S, Aaltonen L-M, et al. Establishment and characterisation of human papillomavirus type 16 DNA immortalised human tonsillar epithelial cell lines. Eur J Cancer. 2003;39(5):698–707.
Strati K, Pitot HC, Lambert PF. Identification of biomarkers that distinguish human papillomavirus (HPV)-positive versus HPV-negative head and neck cancers in a mouse model. Proc Natl Acad Sci. 2006;103(38):14152–7.
Jabbar S, Strati K, Shin MK, Pitot HC, Lambert PF. Human papillomavirus type 16 E6 and E7 oncoproteins act synergistically to cause head and neck cancer in mice. Virology. 2010;407(1):60–7.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71(3):209–49.
Basu P, Roychowdhury S, Bafna UD, Chaudhury S, Kothari S, Sekhon R, et al. Human papillomavirus genotype distribution in cervical cancer in India: results from a multi-center study. Asian Pac J Cancer Prev. 2009;10(1):27–34.
PubMed Google Scholar
Senapati R, Nayak B, Kar SK, Dwibedi B. HPV genotypes distribution in Indian women with and without cervical carcinoma: implication for HPV vaccination program in Odisha, Eastern India. BMC Infect Dis. 2017;17:1–10.
Lohiya A, Daniel RA, Smith RD, Nagar M, Shankar A, Lahariya C. Cancer prevention and control in India can get a boost through primary health care-based approach: a review. J Family Med Prim Care. 2022;11(8):4286.
ICMR National Centre for Disease Informatics and Research: National Cancer Registry Programme Report Bengaluru, India. 2020 [ https://ncdirindia.org/All_Reports/PBCR_Annexures/Default.aspx .
Bagal S, Budukh A, Thakur JS, Dora T, Qayyumi B, Khanna D et al. Head and neck cancer burden in India: an analysis from published data of 37 population-based cancer registries. Ecancermedicalscience. 2023;17.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906.
Bushi G, Shabil M, Padhi BK, Ahmed M, Pandey P, Satapathy P, et al. Prevalence of acute kidney injury among dengue cases: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2023;118(1):1–11.
Bushi G, Padhi BK, Shabil M, Satapathy P, Rustagi S, Pradhan KB, et al. Cardiovascular Disease outcomes Associated with Obstructive Sleep Apnea in diabetics: a systematic review and Meta-analysis. Diseases. 2023;11(3):103.
Gandhi AP, Satapathy P, Rustagi S, Hermis AH, Sah R, Padhi BK. Comments on shigellosis in Southeast Asia: a systematic review and meta-analysis. Travel Med Infect Dis. 2023:102593-.
Langan D, Higgins JP, Jackson D, Bowden J, Veroniki AA, Kontopantelis E, et al. A comparison of heterogeneity variance estimators in simulated random-effects meta‐analyses. Res Synthesis Methods. 2019;10(1):83–98.
Gandhi AP, Shamim MA, Padhi BK. Steps in undertaking meta-analysis and addressing heterogeneity in meta-analysis. Evid. 2023;1(1):44–59.
Google Scholar
Shabil M, Bushi G, Beig MA, Rais MA, Ahmed M, Padhi BK. Cardiovascular manifestation in tuberculosis cases: a systematic review and Meta-analysis. Curr Probl Cardiol. 2023;48(7):101666.
Bushi G, Shabil M, Padhi BK, Ahmed M, Pandey P, Satapathy P, et al. Prevalence of acute kidney injury among dengue cases: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2024;118(1):1–11.
Alrahbeni T, Mahal A, Alkhouri A, Alotaibi HF, Rajagopal V, Behera A et al. Surgical interventions for intractable migraine: a systematic review and meta-analysis. International Journal of Surgery.10.1097.
Swarup SS, Padhi BK, Satapathy P, Shabil M, Bushi G, Gandhi AP et al. Cardiovascular consequences of financial stress: a systematic review and meta-analysis. Curr Probl Cardiol. 2023:102153.
Bahl A, Kumar P, Dar L, Mohanti BK, Sharma A, Thakar A, et al. Prevalence and trends of human papillomavirus in oropharyngeal cancer in a predominantly north Indian population. Head Neck. 2014;36(4):505–10.
Mishra A, Bharti AC, Varghese P, Saluja D, Das BC. Differential expression and activation of NF-κB family proteins during oral carcinogenesis: role of high risk human papillomavirus infection. Int J Cancer. 2006;119(12):2840–50.
Naz F, Verma H, Tanveer N, Sudheer AK, Kakkar A, Tanwar P. Demographic Profile of p16 immunopositive and HPV DNA PCR positive oral squamous cell carcinoma in a large cohort of Indian patients. Asian Pac J Cancer Prevention: APJCP. 2022;23(2):529.
Article CAS Google Scholar
Jalouli J, Ibrahim SO, Mehrotra R, Jalouli MM, Sapkota D, Larsson P-A, et al. Prevalence of viral (HPV, EBV, HSV) infections in oral submucous fibrosis and oral cancer from India. Acta Otolaryngol. 2010;130(11):1306–11.
Singh V, Husain N, Akhtar N, Kumar V, Tewari S, Mishra S, et al. Do human papilloma viruses play any role in oral squamous cell carcinoma in North indians? Asian Pac J Cancer Prev. 2015;16(16):7077–84.
Singh AK, Kushwaha JK, Anand A, Sonkar AA, Husain N, Srivastava K, et al. Human papilloma virus in oral cavity cancer and relation to change in quality of life following treatment—A pilot study from Northern India. Indian J Surg Oncol. 2016;7:386–91.
Vanshika S, Preeti A, Sumaira Q, Vijay K, Shikha T, Shivanjali R, et al. Incidence OF HPV and EBV in oral cancer and their clinico-pathological correlation–a pilot study of 108 cases. J Oral Biology Craniofac Res. 2021;11(2):180–4.
Verma G, Vishnoi K, Tyagi A, Jadli M, Singh T, Goel A, et al. Characterization of key transcription factors as molecular signatures of HPV-positive and HPV‐negative oral cancers. Cancer Med. 2017;6(3):591–604.
Gheit T, Anantharaman D, Holzinger D, Alemany L, Tous S, Lucas E, et al. Role of mucosal high-risk human papillomavirus types in head and neck cancers in central India. Int J Cancer. 2017;141(1):143–51.
Gholap D, Mhatre S, Chaturvedi P, Nair S, Gheit T, Tommasino M et al. Prevalence of human papillomavirus types in head and neck cancer sub-sites in the Indian population. Ecancermedicalscience. 2022;16.
Kane S, Patil V, Noronha V, Joshi A, Dhumal S, D’Cruz A, et al. Predictivity of human papillomavirus positivity in advanced oral cancer. Indian J câncer. 2015;52(3):403–5.
Murthy V, Swain M, Teni T, Pawar S, Kalkar P, Patil A, et al. Human papillomavirus/p16 positive head and neck cancer in India: prevalence, clinical impact, and influence of tobacco use. Indian J Cancer. 2016;53(3):387–93.
Elango KJ, Suresh A, Subhadradevi L, Ravindran HK, Iyer SK, Iyer S, et al. Role of human papilloma virus in oral tongue squamous cell carcinoma. Asian Pac J Cancer Prev. 2011;12(4):889–96.
Panneerselvam K, Rameshkumar A, Rajkumar K, Ramadoss R. Detection of human papillomavirus 16 and 18 in patients with oral squamous cell carcinoma and potentially malignant oral disorders in South Indian population: a pilot study. J Cancer Res Ther. 2019;15(3):571–5.
Parshad S, Nandi S, Marwah N, Mehta P, Tripathi M, Gogna S, et al. Human papillomavirus 16 and 18 in squamous cell carcinoma of oral cavity and sexual practices: a pilot study at a Tertiary Care Hospital of North India. Natl J Maxillofacial Surg. 2015;6(2):185.
Ralli M, Singh S, Yadav S, Sharma N, Verma R, Sen R. Assessment and clinicopathological correlation of p16 expression in head and neck squamous cell carcinoma. J Cancer Res Ther. 2016;12(1):232–7.
Sivakumar N, Narwal A, Kamboj M, Devi A, Kumar S, Bhardwaj R. Molecular and immunohistochemical cognizance of HPV16 in oral leukoplakia, oral squamous cell carcinoma and oropharyngeal squamous cell carcinoma. Head Neck Pathol. 2021;15:882–92.
Ramshankar V, Soundara VT, Shyamsundar V, Ramani P, Krishnamurthy A. Risk stratification of early stage oral tongue cancers based on HPV status and p16 immunoexpression. Asian Pac J Cancer Prev. 2014;15(19):8351–9.
Sri S, Ramani P, Premkumar P, Ramshankar V, Ramasubramanian A, Krishnan RP. Prevalence of human papillomavirus (HPV) 16 and 18 in oral malignant and potentially malignant disorders: a polymerase chain reaction analysis–A comparative study. Annals Maxillofacial Surg. 2021;11(1):6.
Chowdary SD, Sekhar PC, Kattapagari KK, Deepthi CM, Neelima D, Reddy BVR. A study to assess expression of human papillomavirus types 16 and 18 in oral squamous cell carcinoma using polymerase chain reaction. J Oral Maxillofacial Pathology: JOMFP. 2018;22(3):347.
Balaram P, Nalinakumari KR, Abraham E, Balan A, Hareendran NK, Bernard HU, et al. Human papillomaviruses in 91 oral cancers from Indian betel quid chewers–high prevalence and multiplicity of infections. Int J Cancer. 1995;61(4):450–4.
Jitani AK, Raphael V, Mishra J, Shunyu NB, Khonglah Y, Medhi J. Analysis of human papilloma virus 16/18 DNA and its correlation with p16 expression in oral cavity squamous cell carcinoma in North-Eastern India: a chromogenic in-situ hybridization based study. J Clin Diagn Research: JCDR. 2015;9(8):EC04.
CAS Google Scholar
D’Costa J, Saranath D, Dedhia P, Sanghvi V, Mehta AR. Detection of HPV-16 genome in human oral cancers and potentially malignant lesions from India. Oral Oncol. 1998;34(5):413–20.
Koppikar P, deVilliers EM, Mulherkar R. Identification of human papillomaviruses in tumors of the oral cavity in an Indian community. Int J Cancer. 2005;113(6):946–50.
Kulkarni SS, Kulkarni SS, Vastrad PP, Kulkarni BB, Markande AR, Kadakol G, et al. Prevalence and distribution of high risk human papillomavirus (HPV) types 16 and 18 in Carcinoma of cervix, saliva of patients with oral squamous cell carcinoma and in the general population in Karnataka, India. Asian Pac J Cancer Prev. 2011;12(3):645–8.
Rajesh D, Mohiyuddin SA, Kutty AM, Balakrishna S. Prevalence of human papillomavirus in oral squamous cell carcinoma: a rural teaching hospital-based cross-sectional study. Indian J Cancer. 2017;54(3):498–501.
Barwad A, Sood S, Gupta N, Rajwanshi A, Panda N, Srinivasan R. Human papilloma virus associated head and neck cancer: a PCR based study. Diagn Cytopathol. 2012;40(10):893–7.
Sannigrahi M, Singh V, Sharma R, Panda N, Radotra B, Khullar M. Detection of active human papilloma virus-16 in head and neck cancers of Asian north Indian patients. Oral Dis. 2016;22(1):62–8.
Kumar R, Rai AK, Das D, Das R, Kumar RS, Sarma A, et al. Alcohol and tobacco increases risk of high risk HPV infection in head and neck cancer patients: study from North-East Region of India. PLoS ONE. 2015;10(10):e0140700.
Mondal R, Ghosh SK, Choudhury JH, Seram A, Sinha K, Hussain M, et al. Mitochondrial DNA copy number and risk of oral cancer: a report from Northeast India. PLoS ONE. 2013;8(3):e57771.
Pinkiewicz M, Dorobisz K, Zatoński T. Human Papillomavirus-Associated Head and Neck Cancers. Where are we now? A systematic review. Cancer Manage Res. 2022:3313–24.
Hobbs C, Sterne J, Bailey M, Heyderman R, Birchall M, Thomas S. Human papillomavirus and head and neck cancer: a systematic review and meta-analysis. Clin Otolaryngol. 2006;31(4):259–66.
Gillison ML, Zhang Q, Jordan R, Xiao W, Westra WH, Trotti A, et al. Tobacco smoking and increased risk of death and progression for patients with p16-positive and p16-negative oropharyngeal cancer. J Clin Oncol. 2012;30(17):2102.
Würdemann N, Wagner S, Sharma SJ, Prigge E-S, Reuschenbach M, Gattenlöhner S, et al. Prognostic impact of AJCC/UICC 8th edition new staging rules in oropharyngeal squamous cell carcinoma. Front Oncol. 2017;7:129.
Saba NF, Pamulapati S, Patel B, Mody M, Strojan P, Takes R, et al. Novel immunotherapeutic approaches to treating HPV-Related Head and Neck Cancer. Cancers. 2023;15(7):1959.
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24–35.
Economopoulou P, Kotsantis I, Psyrri A. De-escalating strategies in HPV-associated head and neck squamous cell carcinoma. Viruses. 2021;13(9):1787.
Mirghani H, Blanchard P. Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Translational Radiation Oncol. 2018;8:4–11.
Mensour EA, Alam S, Mawani S, Bahig H, Lang P, Nichols A, et al. What is the future of treatment de-escalation for HPV-positive oropharyngeal cancer? A review of ongoing clinical trials. Front Oncol. 2022;12:1067321.
Sun Y, Wang Z, Qiu S, Wang R. Therapeutic strategies of different HPV status in head and neck squamous cell carcinoma. Int J Biol Sci. 2021;17(4):1104.
Eggersmann TK, Baumeister P, Kumbrink J, Mayr D, Schmoeckel E, Thaler CJ, et al. Oropharyngeal HPV detection techniques in HPV-associated head and neck cancer patients. Anticancer Res. 2020;40(4):2117–23.
Shabil M, Murti K, Kumar VU, Kumar R, Kumar N, Dhingra S, et al. Older PLHIV are at Higher Cardiovascular Risk with Poor Quality of Life. Curr HIV Res. 2023;21(6):354–60.
Rostami A, Bratman SV, Han K. Liquid Biopsy goes viral: next-generation sequencing to enhance HPV detection. Clin Cancer Res. 2021;27(19):5158–60.
Faden DL. Liquid biopsy for the diagnosis of HPV-associated head and neck cancer. Cancer Cytopathol. 2022;130(1):12–5.
Goel S, Shabil M, Kaur J, Chauhan A, Rinkoo AV. Safety, efficacy and health impact of electronic nicotine delivery systems (ENDS): an umbrella review protocol. BMJ open. 2024;14(1):e080274.
Zhou L, Qiu Q, Zhou Q, Li J, Yu M, Li K, et al. Long-read sequencing unveils high-resolution HPV integration and its oncogenic progression in cervical cancer. Nat Commun. 2022;13(1):2563.
Qendri V, Bogaards JA, Berkhof J. Who will benefit from expanding HPV vaccination programs to boys? JNCI cancer spectrum. 2018;2(4):pky076.
Pearson AL, Kvizhinadze G, Wilson N, Smith M, Canfell K, Blakely T. Is expanding HPV vaccination programs to include school-aged boys likely to be value-for-money: a cost-utility analysis in a country with an existing school-girl program. BMC Infect Dis. 2014;14(1):1–15.
Hoover DS, Spears CA, Vidrine DJ, Walker JL, Shih Y-CT, Wetter DW. Smoking cessation treatment needs of low SES cervical cancer survivors. Am J Health Behav. 2019;43(3):606–20.
Patterson JG, Borger TN, Burris JL, Conaway M, Klesges R, Ashcraft A, et al. A cluster randomized controlled trial for a multi-level, clinic-based smoking cessation program with women in Appalachian communities: study protocol for the Break Free program. Addict Sci Clin Pract. 2022;17(1):1–15.
Shabil M, Kumar VU, Dhingra S, Ravichandiran V, Parihar VK, Kumar N, et al. Current scenario and strategies to Tackle Cardiovascular Disease Risk in HIV Geriatrics. Curr Pharmacol Rep. 2023;9(6):523–39.
Mitra S, Banerjee S, Misra C, Singh RK, Roy A, Sengupta A, et al. Interplay between human papilloma virus infection and p53 gene alterations in head and neck squamous cell carcinoma of an Indian patient population. J Clin Pathol. 2007;60(9):1040–7.
Nagpal JK, Patnaik S, Das BR. Prevalence of high-risk human papilloma virus types and its association with P53 codon 72 polymorphism in tobacco addicted oral squamous cell carcinoma (OSCC) patients of Eastern India. Int J Cancer. 2002;97(5):649–53.
Sarkar S, Alam N, Chakraborty J, Biswas J, Mandal SS, Roychoudhury S, et al. Human papilloma virus (HPV) infection leads to the development of head and neck lesions but offers better prognosis in malignant Indian patients. Med Microbiol Immunol. 2017;206:267–76.
Download references
Acknowledgements
The authors acknowledge the Nested-Knowledge, MN, USA for providing the access to the software.
This research received no external funding.
Author information
Authors and affiliations.
Center for Global Health Research, Saveetha Institute of Medical and Technical Sciences, Saveetha Medical College and Hospital, Saveetha University, Chennai, India
Prakasini Satapathy
Medical Laboratories Techniques Department, AL-Mustaqbal University, Hillah, Babil, 51001, Iraq
Division of Evidence Synthesis, Global Consortium of Public Health and Research, Datta Meghe Institute of Higher Education, Wardha, India
Mahalaqua Nazli Khatib
One Health Centre (COHERD), Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education, Wardha, India
Shilpa Gaidhane
Global South Asia Infant Feeding Research Network (SAIFRN), Division of Evidence Synthesis, Global Consortium of Public Health and Research, Datta Meghe Institute of Higher Education, Wardha, India
Quazi Syed Zahiruddin
Department of Ophthalmology, Hamad Medical Corporation, Doha, Qatar
Hashem Abu Serhan
Graphic Era (Deemed to be University), Clement Town, Dehradun, India
Rakesh Kumar Sharma
Graphic Era Hill University, Clement Town, Dehradun, India
Centre of Research Impact and Outcome, Chitkara University, Rajpura, 140417, Punjab, India
Divya Sharma
Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, 174103, India
Mithhil Arora
School of Applied and Life Sciences, Uttaranchal University, Dehradun, Uttarakhand, India
Sarvesh Rustagi
College of Medicine and Health Science, Khalifa University, 127788, Abu Dhabi, United Arab Emirates
Sheikh Khalifa Medical City, Abu Dhabi Health Services Company (SEHA), 51900, Abu Dhabi, United Arab Emirates
Department of Pathology, College of Medicine, Imam Abdulrahman Bin Faisal University, 31441, Dammam, Saudi Arabia
Ahmed Alsayyah
Department of Medicine, College of Medicine, King Abdulaziz University, 23624, Jeddah, Saudi Arabia
Marwan Al-Hajeili
Research Center, Dr. Sulaiman Alhabib Medical Group, 13328, Riyadh, Saudi Arabia
Maha F. Al-Subaie
College of Medicine, Alfaisal University, 11533, Riyadh, Saudi Arabia
Maha F. Al-Subaie & Ali A. Rabaan
Department of Microbiology, National Reference laboratory, Cleveland clinic Abu Dhabi, 92323, Abu Dhabi, United Arab Emirates
Mubarak Alfaresi
Department of Pathology, College of Medicine, Mohammed Bin Rashid University of Medicine and Health Sciences, 505055, Dubai, United Arab Emirates
Department of Medical Laboratory, College of Applied Medical Sciences, Prince Sattam bin Abdulaziz University, 11942, Al-Kharj, Saudi Arabia
Mohammed Alissa
Molecular Diagnostic Laboratory, Johns Hopkins Aramco Healthcare, 31311, Dhahran, Saudi Arabia
Ali A. Rabaan
Department of Public Health and Nutrition, The University of Haripur, 22610, Haripur, Pakistan
You can also search for this author in PubMed Google Scholar
Contributions
Substantial contribution to the conception or design of the work: PS, HAS, RKS. Acquisition of data: MNK, SG, QSZ, MA. Analysis and interpretation of data for the work: SR, AAR, MFS. Drafting the work: HAA, ASA, PS, MNK, DS, MA. Revising it critically for important intellectual content: AA, HAS, HAR, QSZ, AN, MA. Resources: Q.S.Z, P.S, M.N.K, B.K.P, J.K.G, D.N, MA. Final approval of the version to be published: All authors (PS, MNK, SG, QSZ, HAS, RKS, DS, MA, SR, AN, AA, MA, MFA, MA, MA, AR). Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: All authors (PS, MNK, SG, QSZ, HAS, RKS, DS, MA, SR, AN, AA, MA, MFA, MA, MA, AR).
Corresponding authors
Correspondence to Prakasini Satapathy or Hashem Abu Serhan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Conflict of interest
Authors declare no conflicts of interests.
Ethical approval
Not applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Satapathy, P., Khatib, M.N., Gaidhane, S. et al. Prevalence of human papillomavirus in head and neck cancer patients in India: a systematic review and meta-analysis. BMC Infect Dis 24 , 516 (2024). https://doi.org/10.1186/s12879-024-09357-2
Download citation
Received : 30 January 2024
Accepted : 26 April 2024
Published : 23 May 2024
DOI : https://doi.org/10.1186/s12879-024-09357-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Head and neck cancers
- Vaccination
- Public health interventions
- Epidemiology
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
- Open access
- Published: 17 May 2024
Ferroptosis is a protective factor for the prognosis of cancer patients: a systematic review and meta-analysis
- Shen Li 1 na1 ,
- Kai Tao 2 na1 ,
- Hong Yun 1 na1 ,
- Jiaqing Yang 1 , 2 ,
- Yuanling Meng 3 ,
- Fan Zhang 4 &
- Xuelei Ma 1
BMC Cancer volume 24 , Article number: 604 ( 2024 ) Cite this article
211 Accesses
1 Altmetric
Metrics details
Cancer is a leading global cause of death. Conventional cancer treatments like surgery, radiation, and chemotherapy have associated side effects. Ferroptosis, a nonapoptotic and iron-dependent cell death, has been identified and differs from other cell death types. Research has shown that ferroptosis can promote and inhibit tumor growth, which may have prognostic value. Given the unclear role of ferroptosis in cancer biology, this meta-analysis aims to investigate its impact on cancer prognosis.
This systematic review and meta-analysis conducted searches on PubMed, Embase, and the Cochrane Library databases. Eight retrospective studies were included to compare the impact of ferroptosis inhibition and promotion on cancer patient prognosis. The primary endpoints were overall survival (OS) and progression-free survival (PFS). Studies lacking clear descriptions of hazard ratios (HR) and 95% confidence intervals for OS and PFS were excluded. Random-effects meta-analysis and meta-regression were performed on the included study data to assess prognosis differences between the experimental and control groups. Meta-analysis results included HR and 95% confidence intervals.
This study has been registered with PROSPERO, CRD 42023463720 on September 27, 2023.
A total of 2,446 articles were screened, resulting in the inclusion of 5 articles with 938 eligible subjects. Eight studies were included in the meta-analysis after bias exclusion. The meta-analysis, after bias exclusion, demonstrated that promoting ferroptosis could increase cancer patients’ overall survival (HR 0.31, 95% CI 0.21–0.44) and progression-free survival (HR 0.26, 95% CI 0.16–0.44) compared to ferroptosis inhibition. The results showed moderate heterogeneity, suggesting that biological activities promoting cancer cell ferroptosis are beneficial for cancer patient’s prognosis.
Conclusions
This systematic review and meta-analysis demonstrated that the promotion of ferroptosis yields substantial benefits for cancer prognosis. These findings underscore the untapped potential of ferroptosis as an innovative anti-tumor therapeutic strategy, capable of addressing challenges related to drug resistance, limited therapeutic efficacy, and unfavorable prognosis in cancer treatment.
Registration
CRD42023463720.
Peer Review reports
Cancer has progressively become the world’s leading cause of mortality, imposing substantial disease burdens. According to GLOBOCAN 2020, the global cancer burden will reach 28.4 million cases in 2040 [ 1 ]. And approximately one in every five men and one in every six women will develop cancer, with one in eight men and one in ten women succumbing to cancer before reaching 75 years of age [ 2 ]. It is estimated that over half of all cancer-related deaths (57.3%) and nearly half of all new cancer cases (48.4%) are concentrated in Asia [ 2 ]. Presently, common treatments for cancer encompass surgery, radiation, and chemotherapy [ 3 , 4 ]. However, these approaches may harm normal cells and result in significant side effects, including hepatotoxicity, ototoxicity, cardiotoxicity, nausea, vomiting, and more [ 5 , 6 ]. Despite advancements in therapy, cancer remains the second leading global cause of death, following ischemic heart disease, and is projected to become the leading cause by 2060 [ 7 ].
In 2012, a nonapoptotic, iron-dependent form of cell death initiated by the oncogenic Ras-selective lethal small molecule erastin was termed “ferroptosis” [ 8 ]. Ferroptosis exhibits distinct morphological characteristics compared to other regulated cell death forms. Notably, ferroptosis lacks the hallmark signs of apoptosis, such as chromatin condensation and apoptotic bodies, instead manifesting as shrunken mitochondria, reduced mitochondrial cristae, and an accumulation of lipid peroxides [ 8 , 9 , 10 ]. Its underlying mechanism also differs from other regulated cell death processes. Ferroptosis is inhibited by the system xc-—GSH—GPX4 pathway and is induced by the accumulation of phospholipid hydroperoxides, rather than the involvement of cell death executioner proteins such as caspases and mixed lineage kinase domain-like protein, among others [ 9 , 11 ].
An increasing body of research has explored the role of ferroptosis in tumors, suggesting its dual role in tumor promotion and inhibition. Various experimental agents, including erastin, RSL3, and drugs such as sorafenib, sulfasalazine, statins, and artemisinin, along with ionizing radiation and cytokines like IFN-γ and TGF-β1, can induce ferroptosis and inhibit tumors [ 12 ]. However, emerging evidence hints at ferroptosis potentially promoting tumor growth by triggering inflammation-associated immunosuppression within the tumor microenvironment [ 12 , 13 ]. Numerous studies have also indicated the prognostic value of ferroptosis [ 14 , 15 , 16 , 17 , 18 ].
Given the unclear role of ferroptosis in cancer biology, we conducted this meta-analysis to investigate its impact on cancer prognosis.
Search strategy and selection criteria
This systematic review and meta-analysis were conducted following PRISMA guidelines. PubMed, EMBASE, and the Cochrane Library were systematically searched from their inception until February 27, 2024, with no language restrictions. The search strategy included the following terms: (ferroptosis or oxytosis) AND (Neoplasm or Tumor or Tumors or Neoplasia or Cancer or Cancers or Malignant Neoplasm or Malignancy or Malignant Neoplasms or Neoplasms, Malignant or Benign Neoplasms or Neoplasm, Benign or Malignancies or Neoplasm, Malignant or Benign Neoplasm or Neoplasms, Benign or Neoplasias) AND (prognosis or Prognoses or Prognostic Factors or Prognostic Factor or Factor, Prognostic or Factors, Prognostic) as free text.
The objective of this study is to investigate and elucidate the impact of ferroptosis on cancer patients’ prognosis. We will compare the differences in prognosis between cancer patients with genes that promote ferroptosis and those with genes that inhibit it. The primary endpoints of the study include HRs and 95% confidence intervals for OS and PFS. It is important to note that the upregulation and downregulation of ferroptosis-related genes are not used as criteria for grouping; rather, the experimental and control groups are divided based on the ultimate impact of genes on ferroptosis. This meta-analysis was limited to studies conducted in humans. Participant data from cohort studies were extracted and analyzed. The collected information included the first author, study period, country of study, study size, ferroptosis-related gene, the effect of genes on ferroptosis, type of cancer, HR, and 95% confidence intervals for OS and PFS.
Both exclusion and inclusion criteria were pre-specified. Studies demonstrating a relationship between prognosis and ferroptosis in cancer patients were selected. Inclusion criteria were as follows: (1) Articles were limited to those involving human samples only. (2) All cancer patients had been diagnosed by pathological evidence. (3) Expression of ferroptosis-related genes had been assessed through immunohistochemistry from tumor specimens, conducted according to standard protocols. (4) All patients had been subject to follow-up, and results had been reported. Exclusion criteria encompassed: (1) Duplicate articles. (2) Article types other than original research, such as reviews, meta-analyses, letters, or editorial comments. (3) Studies involving cellular or animal-based research. (4) Patients with multiple primary cancers. The literature search, study selection, and data extraction were independently performed by Shen Li and Kai Tao, with any discrepancies reviewed and resolved by another author, Xuelei Ma, through consensus.
Data analysis
We employed Stata 14 software to calculate statistics. The specific analysis method is as follows: (1) We collected and analyzed the HR for OS and PFS reported in the included studies. The results were visualized using forest plots to illustrate the differences in prognosis between cancer patients whose genes promote ferroptosis and those whose genes inhibit it, thereby demonstrating the impact of ferroptosis on the prognosis of cancer patients. (2) Heterogeneity test was conducted by I 2 statistic to assess the heterogeneity of the results. Low heterogeneity was defined as an I 2 value less than or equal to 25%, moderate heterogeneity as between 25 and 75%, and high heterogeneity as exceeding 75%. (3) To evaluate potential publication bias, we employed funnel plots and conducted Egger tests. A p -value greater than 0.05 in Egger test indicates no significant bias. (4) Sensitivity analysis was conducted to examine any studies with significant influence on the overall results. (5) Meta-regression was conducted to assess the potential influence of covariates on the outcome [ 19 , 20 ]. We subjected the included covariates to regression testing, including country of study, ferroptosis-related gene, the effect of genes on ferroptosis, and type of cancer, to explore possible sources of heterogeneity and reduce potential bias. This study has been registered with PROSPERO, CRD 42023463720.
Bias analysis and quality assessment
Three researchers (LS, YJQ and TK) independently conducted a bias risk assessment following the Cochrane Bias Assessment Handbook. Considering that all included studies were retrospective articles, this study employed the Cochrane bias risk tool, which comprises five domains, to evaluate the risk of bias in each included study: (1) selection bias, (2) measurement bias, (3) data integrity bias, (4) outcome selection bias, and (5) other biases. Each researcher independently assessed the risk as low, high, or unclear for each domain. In cases of any uncertainty, Dr. Xuelei Ma made the final judgment. Based on the risk of bias, the quality of evidence was categorized as very low, low, moderate, or high. The quality assessment of this study adheres to the GRADE system.
We identified a total of 2,446 articles through literature searches, with 6 articles from the Cochrane Library and 2,440 from other databases, including PubMed and Embase. We excluded 962 duplicate articles. Among the remaining literature, we excluded 1,477 articles after abstract screening as they did not align with our research objectives. Subsequently, we conducted full-text reviews and eligibility assessments on the remaining 7 articles. Ultimately, we included 5 articles in our analysis. The review process was conducted independently by LS, TK and MYL, with a third reviewer, Xuelei Ma, reassessing articles with uncertain eligibility. The process is illustrated in Fig. 1 .
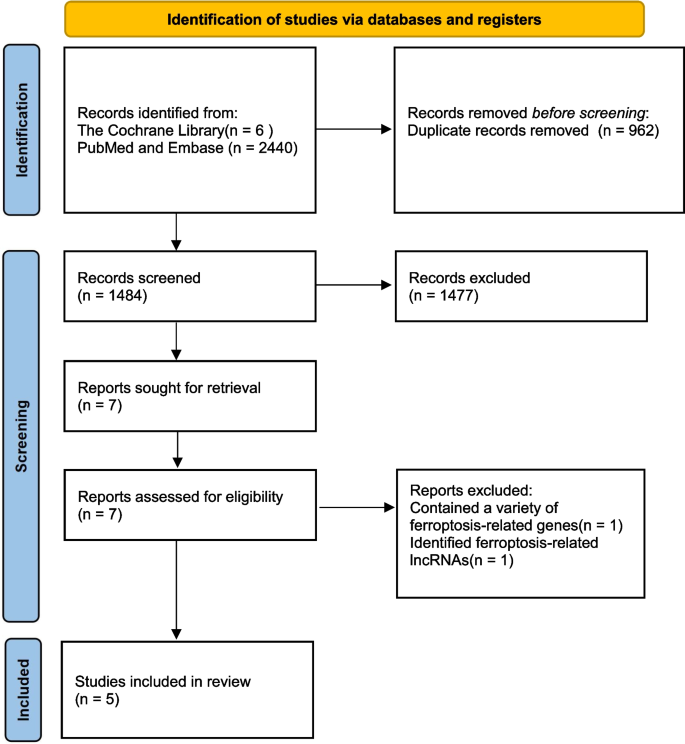
Study selection
Among the five clinical articles, all studies were conducted in Asia, with 2 studies in China (40%) and 3 in Japan (60%). The research covered various cancer types, including gastric cancer and esophageal cancer of the digestive system, epithelial ovarian cancer of the female reproductive system, and osteosarcoma originating from undifferentiated bone fibrous tissue. In terms of age reporting, the median age of patients with epithelial ovarian cancer was 52 years, while osteosarcoma patients had an average age of 30.2 years, which is consistent with the characteristics of these two diseases. Three out of the five articles included two studies each, resulting in a total of 8 studies. Glutathione peroxidase 4 (GPX4) was the most studied gene (4/8, 50%) related to regulating ferroptosis. Like most other genes, GPX4 plays a role in inhibiting ferroptosis by suppressing lipid peroxidation. In contrast, heme oxygenase 1 (HMOX1), through catalyzing the degradation of heme into divalent iron ions, biliverdin, and CO, can promote ferroptosis by increasing the labile iron pool (LIP) (1/8, 12.5%). It’s worth noting that, as shown in Table 1 , only 3 studies (3/8, 37.5%) reported cut-off values, while the rest did not report them. We will discuss the importance of this missing data in the Discussion section.
Main outcome
A total of 8 studies reported HRs and 95% confidence intervals for OS. The forest plot indicates that the ferroptosis-promoting group had better OS compared to the ferroptosis-inhibiting group (HR 0.43, 95% CI 0.22–0.83). Data analysis reports substantial heterogeneity (I 2 = 87.8%, 95% CI 45.6%-94.7%) (Fig. 2 ). After conducting sensitivity analysis, we found that the study by Song et al. might introduce significant bias. After excluding this study and reanalyzing the data, the results showed that the ferroptosis-promoting group had better OS compared to the ferroptosis-inhibiting group (HR 0.31, 95% CI 0.21–0.44), with decreased heterogeneity (I 2 = 58.1%, 95% CI 0%-82.7%), indicating moderate heterogeneity (Fig. 3 ).
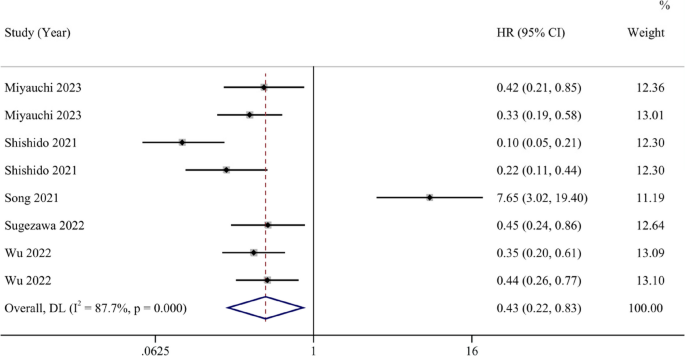
Forest plot of the pooled overall survival between the ferroptosis-promoting group and the ferroptosis-inhibiting group
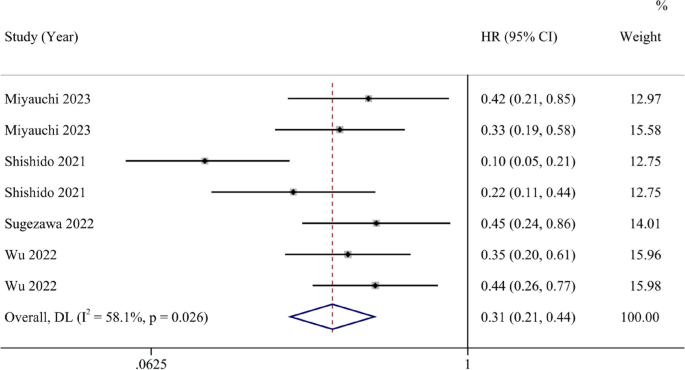
Forest plot of the pooled overall survival between the ferroptosis-promoting group and the ferroptosis-inhibiting group after excluding one study with a large bias
Six studies reported HRs and 95% CIs for PFS. The analysis results suggest that the ferroptosis-promoting group had better PFS compared to the ferroptosis-inhibiting group (HR 0.47, 95% CI 0.17–1.30), although it was not statistically significant. Data analysis reports high heterogeneity (I 2 = 93.2%, 95% CI 43.5%-97.5%) (Fig. 4 ). After conducting sensitivity analysis, similar to the OS results, we found that the study by Song et al. might introduce significant bias. After excluding this study, the results showed that the ferroptosis-promoting group had significantly better PFS prognosis compared to the ferroptosis-inhibiting group (HR 0.26, 95% CI 0.16–0.44), with moderate heterogeneity (I 2 = 69.7%, 95% CI 0%-89.6%), and the results were statistically significant (Fig. 5 ).
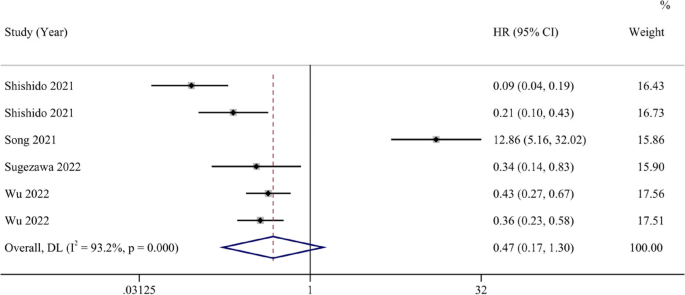
Forest plot of the pooled progression-free survival between the ferroptosis-promoting group and the ferroptosis-inhibiting group
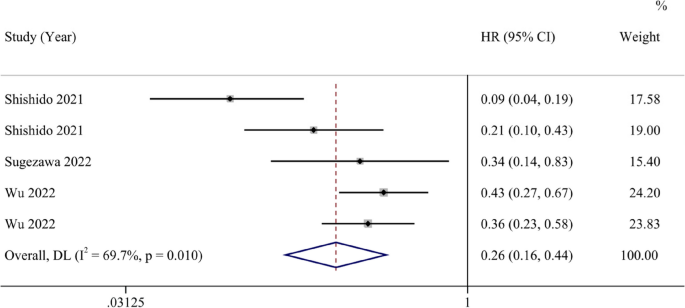
Forest plot of the pooled progression-free survival between the ferroptosis-promoting group and the ferroptosis-inhibiting group after excluding one study with a large bias
Separate meta-regression analyses for OS and PFS results revealed that covariates such as country of study, ferroptosis-related gene, the effect of genes on ferroptosis, and type of cancer had no influence on the results.
Risk of bias in studies
All included studies underwent a risk of bias assessment following the guidelines recommended by the Cochrane Handbook, which includes five bias domains. We classified 2 studies as having low bias risk (2/8, 25%), indicating low bias risk across all domains. Five studies exhibited some lower risk (5/8, 62.5%), suggesting mild uncertainty in at least one domain but no definite high risk. One study had a high risk (1/8, 12.5%), indicating high bias risk in more than one domain. No studies presented a higher risk overall. The reasons for non-low bias risk were predominantly due to incomplete outcome data (9/14, 64%). In multiple lower risk studies, the reason for uncertain bias in other domains was the lack of reported cut-off values. We believe that different cut-off values can introduce a certain degree of bias into study results, which may affect the interpretation of the results of the study Moreover, we excluded a study of Song, which have introduced a large bias because its results were not reported clearly and correctly with low credibility. We conducted a thorough review of their experimental procedures and relevant sensitivity analysis, concluding that it could affect the overall bias risk of the study. After excluding the study by Song et al., the Egger tests for OS and PFS had p -values of 0.20 and 0.205, respectively, indicating no significant publication bias.
To the best of our knowledge, this systematic review represents the pioneering effort to explore the correlation between ferroptosis and cancer prognosis. Through a comprehensive meta-analysis, we aimed to determine whether ferroptosis influences cancer prognosis and its potential applicability as a therapeutic target. The hallmarks of tumorigenesis encompass the evasion of regulatory cell death, unbridled proliferation, and cellular immortality [ 26 , 27 ]. The resistance exhibited by cancer cells poses a formidable challenge in cancer treatment, as conventional chemotherapy agents often fall short in inducing effective cell death [ 28 ]. Ferroptosis emerges as a promising strategy to overcome this resistance [ 27 ]. Nevertheless, ferroptosis assumes a dual role in the context of anti-tumor immunity. CD8 + T cells, for instance, can secrete Interferon-γ to promote ferroptosis in cancer cells, while ferroptotic cancer cells can reciprocally enhance the maturation of dendritic cells and macrophage efficiency [ 13 ]. However, it’s worth noting that some T helper cell subsets and CD8 + T cells can themselves undergo ferroptosis, thereby tempering the overall impact of ferroptosis on anti-tumor immunity [ 13 ].
In our study, we have uncovered that the promotion of ferroptosis in cancer cells serves as a protective factor for cancer patient prognosis. In our analysis of OS, involving eight studies, the results indicate that patients in the group where ferroptosis is promoted exhibit improved overall survival rates compared to the group where it is inhibited (HR 0.43, 95% CI 0.22–0.83). Following a sensitivity analysis, we observed certain biases in the study conducted by Song et al. Upon a thorough review of the research, we discovered that this study found ZFP36 can express in both tumor and para-carcinoma tissues, and the expression of ZFP36 was higher in para-carcinoma tissues Elevated ZFP36 expression inhibits ferroptosis, consequently leading to fewer instances of ferroptosis in the tumor-adjacent tissue, resulting in better patient prognoses. However, in the other studies included, ferroptosis-regulating genes were all found to be overexpressed or suppressed in tumor tissue instead of tumor-adjacent tissue. Meanwhile, the low accuracy of results from the study of Song et al. can introduce bias to our study. So we exclude this particular article to assure the quality of our results. Upon its exclusion, patients in the group where ferroptosis is promoted demonstrated better overall survival rates (HR 0.31, 95% CI 0.21–0.44), with reduced study heterogeneity and a higher p -value in the Egger test. For this intriguing study, we look forward to future research that directly investigates the role of ZFP36 in tumor tissue and whether it presents contrasting effects on patient prognosis. In our study on PFS, after sensitivity analysis, forest plots indicated that patients in the group where ferroptosis is promoted exhibit improved overall survival rates compared to the group where it is inhibited (HR 0.26, 95% CI 0.16–0.44). The heterogeneity could have raised from the absence of the cut-off values, different countries, the differences of ferroptosis-related genes, the type of cancers and the effect of genes on ferroptosis. After conducting meta-regression, we did not identify covariates including country, ferroptosis-related genes, type of cancer and the effect of genes influencing the results. Considering that 5 of the 8 studies we included did not report the cut-off value, we could not include this in meta-regression, which can lead to potential heterogeneity.
As the pioneering meta-analysis investigating the impact of ferroptosis on cancer patient prognosis, we are pleased to find that it serves as a protective factor for cancer patient prognoses. Ferroptosis, as a novel biological behavior distinct from apoptosis, holds promise as a potential approach in cancer treatment. Currently, we have identified numerous key genes in the ferroptosis pathways, and if ferroptosis proves to be an effective cancer treatment modality, targeting these genes would hold significant clinical relevance. These potential targets included down-regulation of GPX4, ZFP36, SLC7A11, FSP1 expression and up-regulation of HMOX1 expression. Moving forward, there is a promising potential to translate these interventions targeting specific factors into practical applications in clinical therapy. This holds great promise as an exciting new avenue in the realm of cancer bio-therapy.
Despite our rigorous article selection, feature extraction, and analysis, this study has certain limitations. Firstly, we require more clinical research, whether retrospective or randomized controlled studies, to substantiate the favorable impact of promoting ferroptosis in cancer cells on the prognosis of cancer patients, including both OS and PFS, both of which are pivotal for patients’ quality of life. Secondly, the cut-off value is a critical parameter; regrettably, many of the articles we included did not report this metric, making it challenging to assess the extent of bias in prognosis results due to cut-off value variations. We also hope that future related meta-analyses will delve further into the influence of cut-off values.
This meta-analysis, by comparing the promotion and inhibition of ferroptosis in cancer patients, reveals that fostering ferroptosis in cancer cells is a protective factor for cancer patient prognosis. Ferroptosis-related genes hold the potential to become novel biomarkers for targeted therapy, and promoting ferroptosis in cancer cells could represent a new and effective approach to cancer treatment.
Availability of data and materials
To ensure transparency and reproducibility of the study, all data generated or analyzed during this study are included in this published article and its supplementary information files. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request. Please note that data sharing is intended for academic research purposes only and not for other purposes.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Article PubMed Google Scholar
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Wang Y, Jiang H, Fu L, Guan L, Yang J, Ren J, et al. Prognostic value and immunological role of PD-L1 gene in pan-cancer. BMC Cancer. 2024;24(1):20.
Article PubMed PubMed Central Google Scholar
Zaimy MA, Saffarzadeh N, Mohammadi A, Pourghadamyari H, Izadi P, Sarli A, et al. New methods in the diagnosis of cancer and gene therapy of cancer based on nanoparticles. Cancer Gene Ther. 2017;24(6):233–43.
Article CAS PubMed Google Scholar
Oun R, Moussa YE, Wheate NJ. The side effects of platinum-based chemotherapy drugs: a review for chemists. Dalton Trans. 2018;47(19):6645–53.
Wang K, Tepper JE. Radiation therapy-associated toxicity: etiology, management, and prevention. CA Cancer J Clin. 2021;71(5):437–54.
Mattiuzzi C, Lippi G. Current cancer epidemiology. Journal of epidemiology and global health. 2019;9(4):217–22.
Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–72.
Article CAS PubMed PubMed Central Google Scholar
Jiang X, Stockwell BR, Conrad M. Ferroptosis: mechanisms, biology and role in disease. Nat Rev Mol Cell Biol. 2021;22(4):266–82.
Stockwell BR, Friedmann Angeli JP, Bayir H, Bush AI, Conrad M, Dixon SJ, et al. Ferroptosis: a regulated cell death nexus linking metabolism, redox biology, and disease. Cell. 2017;171(2):273–85.
Galluzzi L, Vitale I, Aaronson SA, Abrams JM, Adam D, Agostinis P, et al. Molecular mechanisms of cell death: recommendations of the nomenclature committee on cell death 2018. Cell Death Differ. 2018;25(3):486–541.
Chen X, Kang R, Kroemer G, Tang D. Broadening horizons: the role of ferroptosis in cancer. Nat Rev Clin Oncol. 2021;18(5):280–96.
Lei G, Zhuang L, Gan B. Targeting ferroptosis as a vulnerability in cancer. Nat Rev Cancer. 2022;22(7):381–96.
Chen H, He Y, Pan T, Zeng R, Li Y, Chen S, et al. Ferroptosis-related gene signature: a new method for personalized risk assessment in patients with diffuse large B-cell lymphoma. Pharmgenomics Pers Med. 2021;14:609–19.
PubMed PubMed Central Google Scholar
Hsieh PL, Chao SC, Chu PM, Yu CC. Regulation of ferroptosis by non-coding RNAs in head and neck cancers. Int J Mol Sci. 2022;23(6):3142.
Liu Y, Duan C, Dai R, Zeng Y. Ferroptosis-mediated crosstalk in the tumor microenvironment implicated in cancer progression and therapy. Front Cell Dev Biol. 2021;9:739392.
Yu S, Jia J, Zheng J, Zhou Y, Jia D, Wang J. Recent progress of ferroptosis in lung diseases. Front Cell Dev Biol. 2021;9:789517.
Zeng H, You C, Zhao L, Wang J, Ye X, Yang T, et al. Ferroptosis-associated classifier and indicator for prognostic prediction in cutaneous melanoma. J Oncology. 2021;2021:3658196.
Article Google Scholar
Wang Y, Fu L, Lu T, Zhang G, Zhang J, Zhao Y, et al. Clinicopathological and prognostic significance of long non-coding RNA MIAT in human cancers: a review and meta-analysis. Front Genet. 2021;12:729768.
Wang Y, Jiang X, Zhang D, Zhao Y, Han X, Zhu L, et al. LncRNA DUXAP8 as a prognostic biomarker for various cancers: a meta-analysis and bioinformatics analysis. Front Genet. 2022;13:907774.
Shishido Y, Amisaki M, Matsumi Y, Yakura H, Nakayama Y, Miyauchi W, et al. Antitumor effect of 5-aminolevulinic acid through ferroptosis in esophageal squamous cell carcinoma. Ann Surg Oncol. 2021;28(7):3996–4006.
Song P, Xie Z, Chen C, Chen L, Wang X, Wang F, et al. Identification of a novel iron zinc finger protein 36 (ZFP36) for predicting the overall survival of osteosarcoma based on the Gene Expression Omnibus (GEO) database. Annals of translational medicine. 2021;9(20):1552.
Sugezawa K, Morimoto M, Yamamoto M, Matsumi Y, Nakayama Y, Hara K, et al. GPX4 regulates tumor cell proliferation via suppressing ferroptosis and exhibits prognostic significance in gastric cancer. Anticancer Res. 2022;42(12):5719–29.
Wu X, Shen S, Qin J, Fei W, Fan F, Gu J, et al. High co-expression of SLC7A11 and GPX4 as a predictor of platinum resistance and poor prognosis in patients with epithelial ovarian cancer. BJOG. 2022;129 Suppl 2(Suppl 2):40–9.
Miyauchi W, Shishido Y, Matsumi Y, Matsunaga T, Makinoya M, Shimizu S, et al. Simultaneous regulation of ferroptosis suppressor protein 1 and glutathione peroxidase 4 as a new therapeutic strategy of ferroptosis for esophageal squamous cell carcinoma. Esophagus. 2023;20(3):492–501.
Wang Y, Lin K, Xu T, Wang L, Fu L, Zhang G, et al. Development and validation of prognostic model based on the analysis of autophagy-related genes in colon cancer. Aging. 2021;13(14):19028–47.
Zhao L, Zhou X, Xie F, Zhang L, Yan H, Huang J, et al. Ferroptosis in cancer and cancer immunotherapy. Cancer communications (London, England). 2022;42(2):88–116.
Xu T, Ding W, Ji X, Ao X, Liu Y, Yu W, et al. Molecular mechanisms of ferroptosis and its role in cancer therapy. J Cell Mol Med. 2019;23(8):4900–12.
Download references
Acknowledgements
Not applicable.
No funding.
Author information
Shen Li, Kai Tao and Hong Yun contributed equally to this work.
Authors and Affiliations
Department of Biotherapy, West China Hospital and State Key Laboratory of Biotherapy, Sichuan University, Chengdu, Sichuan, China
Shen Li, Hong Yun, Jiaqing Yang & Xuelei Ma
West China School of Medicine, West China Hospital, Sichuan University, Chengdu, Sichuan, China
Kai Tao & Jiaqing Yang
West China School of Stomatology, Sichuan University, Chengdu, Sichuan, China
Yuanling Meng
Health Management Center, General Practice Medical Center, West China Hospital, Sichuan University, Chengdu, Sichuan, China
You can also search for this author in PubMed Google Scholar
Contributions
Study Concept and design: MXL, LS, ZF; Search Strategy: TK, LS, YH; Selection Criteria: TK, LS, YJQ, YH; Quality Assessment: LS, YJQ, MXL and TK; Drafting of the Manuscript: LS, TK, YH. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Fan Zhang or Xuelei Ma .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, S., Tao, K., Yun, H. et al. Ferroptosis is a protective factor for the prognosis of cancer patients: a systematic review and meta-analysis. BMC Cancer 24 , 604 (2024). https://doi.org/10.1186/s12885-024-12369-5
Download citation
Received : 07 November 2023
Accepted : 10 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12885-024-12369-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ferroptosis
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 14 May 2024
Effectiveness of vestibular rehabilitation on postural balance in Parkinson’s disease: a systematic review and meta-analysis of randomized controlled trials
- Carla Marineli Saraiva do Amaral ORCID: orcid.org/0000-0002-0145-0770 1 ,
- Samuel Brito de Almeida ORCID: orcid.org/0000-0001-6174-1839 1 ,
- Renata Parente de Almeida ORCID: orcid.org/0000-0002-8116-8483 2 ,
- Simony Lira do Nascimento ORCID: orcid.org/0000-0001-6248-5590 3 ,
- Rodrigo Mariano Ribeiro ORCID: orcid.org/0000-0002-3040-4909 1 &
- Pedro Braga-Neto ORCID: orcid.org/0000-0001-9186-9243 1
BMC Neurology volume 24 , Article number: 161 ( 2024 ) Cite this article
374 Accesses
10 Altmetric
Metrics details
Introduction
Postural balance impairment can affect the quality of life of patients with Parkinson’s disease. Previous studies have described connections of the vestibular system with postural functions, suggesting a potential participation of the basal ganglia in receiving vestibular stimuli. This systematic review aims to summarize the evidence on the effectiveness of vestibular rehabilitation on postural balance in patients with Parkinson’s disease.
A systematic review was conducted using the electronic databases: PubMed, Embase, Scopus and PEDro. The study selection was independently conducted by two reviewers, and disagreements were evaluated by a third reviewer. The included studies had no restrictions on publication dates or languages and the last update occurred in July 2023.
From the 485 studies found in the searches, only 3 studies were deemed eligible for the systematic review involving a total of 130 participants. The Berg Balance Scale was described as the tool for evaluation of postural balance in all studies. The meta-analysis showed statistically significant results in favor of vestibular rehabilitation (MD = 5.35; 95% CI = 2.39, 8.31; P < 0.001), regardless of the stage of Parkinson’s disease. Although the effect size was suggested as a useful functional gain, the analysis was done with caution, as it only included 3 randomized controlled trials. The risk of bias using the RoB-2 was considered as being of “some concern” in all studies. Furthermore, the quality of the evidence based on the Grading of Recommendations Assessment Development and Evaluation system, produced by pooling the included studies was considered very low.
Compared to other interventions, vestibular rehabilitation has potential to assist the postural balance of patients with Parkinson’s disease. However, the very low quality of the evidence demonstrates uncertainty about the impact of this clinical practice. More robust studies are needed to confirm the benefits of this therapy in patients with Parkinson’s disease. This study was prospectively registered in PROSPERO: CRD42020210185.
Peer Review reports
Patients with Parkinson’s disease (PD) usually present postural imbalance [ 1 , 2 ]. The involvement of vestibular afferents in the basal ganglia and in the integration of vestibular, visual and proprioceptive information is well described in previous studies in patients wirh PD [ 3 , 4 , 5 ]. Alterations in the vestibular nuclei, in the lateral vestibulospinal system and in the vestibulo-ocular reflex gain may also occur [ 6 , 7 ]. Furthermore, degeneration of cholinergic neurons, the pedunculopontine nucleus complex and its thalamic efferent terminals may contribute to postural imbalance [ 8 , 9 ].
Studies have shown distinct peripheral and central alterations in the vestibular function of patients with PD. Vestibulo-ocular reflex impairment has been evidenced in previous studies. Findings of unilateral peripheral vestibular hypofunction were described in the caloric test in patients with PD with lateral trunk flexion [ 10 ]. Furthermore, a reduction in gains in the anterior and posterior semicircular canals in the Video Head Impulse Test (V-HIT) [ 11 ] was also significant when compared to the control group. Unilateral and bilateral absent responses were found in cervical and ocular vestibular evoked myogenic potentials, with latencies and amplitudes being significantly lower compared to the control group [ 11 ].
Changes in vestibular function in PD can trigger postural imbalance and high rates of disability and falls [ 12 ]. Thus, rehabilitation programs have been extensively studied to overcome these issues [ 13 ]. Vestibular rehabilitation is a treatment option for several cases of dizziness, instabilities and postural imbalance [ 14 ]. We questioned whether vestibular rehabilitation would be a therapy for body balance in patients with PD. Our hypothesis was that vestibular rehabilitation would be effective as a therapy for postural balance in PD, when compared to other interventions.
This type of therapy was introduced in the 1940s [ 15 ] and encompasses neuroplasticity mechanisms to reduce symptoms, repair and adapt functions [ 16 ]. Vestibular rehabilitation exercises stimulate visual stabilization, reduce sensitivity during head movements and increase vestibulo-visual interaction. The stimulation of the vestibulo-ocular reflex promotes changes in neuronal responses to head movements, enables better head alignment and contributes to the function of postural balance. Furthermore, vestibulospinal reflex exercises provide improved static and dynamic stability and functional balance in daily life situations [ 16 ].
Vestibular rehabilitation therapy needs to be planned according to the signs and symptoms of each patient, regardless of the peripheral or central findings of the vestibular evaluation [ 17 ]. However, there is little evidence about its application in patients with PD. Establishing the effectiveness of vestibular rehabilitation on postural imbalance in PD is important for a better prognosis. This systematic review aims to summarize the evidence on the effectiveness of vestibular rehabilitation on postural balance in PD patients in comparison with other interventions.
Review protocol and registration
This study is a systematic review aimed evaluating the effectiveness of vestibular rehabilitation on postural balance in patients with PD. This review protocol was registered in International Prospective Register of Systematic Reviews (PROSPERO) (CRD42020210185). This study was conducted according to Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines [ 18 ].
Eligibility criteria
The eligibility criteria were based on the following PICOS – Population (Parkinson’s disease patients), Intervention (vestibular rehabilitation), Comparison (other interventions), Outcome (postural balance) and Study type (randomized controlled trials) [ 18 ]. We included studies in which participants were diagnosed with PD according to the Movement Disorder Society Clinical Diagnostic Criteria [ 19 ]. Studies including patients with benign paroxysmal positional vertigo, dementia, or other neurological disorders (e.g., stroke, essential tremor, ataxias, or amyotrophic lateral sclerosis) were excluded. Vestibular rehabilitation was defined as a therapy to improve postural balance and was included in the intervention group, with exercises that moved the eyes, head, body and provoked sensory conflict between the vestibular, visual and somatosensory systems. The exercises included neuroplasticity mechanisms such as adaptation, habituation, and/or substitution. The use of several protocols was considered, with or without virtual or augmented reality and exergaming support. Vestibular rehabilitation associated with physical activities, strength training (weight training, functional training), aerobic training, Tai Chi, yoga, pilates, dance, aquatic exercises, multimodal and multicomponent exercises were not included.
We included any comparator groups such as no intervention, placebo, medication, balance training program, and health education guidelines. To be included, studies should present data on postural balance (scores) at the beginning and the end of vestibular rehabilitation program in the intervention and control groups. The selected studies should present at least one of the following tools for measuring balance outcomes: the Romberg test, Berg Balance Scale (BBS), Tinetti’s balance and mobility scale, static and dynamic posturography, Functional Range Test (FR), Mini Balance Evaluation Systems Test (Mini-BESTest), Time Up and Go Test (TUG), Dynamic Gait Index (DGI), vectonystagmography, subjective visual vertical, dynamic visual acuity, 2-Minute Walk Test (2MWT) and Activities-specific Balance Confidence (ABC) scale. The additional outcomes, risks of falls arising from the postural balance score at the beginning and end of vestibular rehabilitation and comparison of differences between the intervention and control groups were also extracted. The narrative synthesis of eligible studies was performed according to the characteristics of the vestibular rehabilitation intervention, sample size and outcome measure.
Search strategy
The PubMed, Embase, Scopus and Physiotherapy Evidence Database (PEDro) electronic databases were searched. The search used the terms MeSH. The combinations of the search terms and Boolean operators were performed by an independent librarian. The following search terms were used: Parkinson, Parkinson disease, Parkinson’s disease, Parkinson’s patient, rehabilitation vestibular, central compensation, central clearing, adaptation, habituation, replacement, vestibular, vestibular function test, functional readaptation, readaptation, equilibrium, postural balance, body equilibrium, body sway, musculoskeletal equilibrium, postural equilibrium, Instability, and postural instability. The last update occurred in July 2023 and the randomized controlled trials included had no restrictions on publication dates or languages. The full search strategy is shown in Supplementary Material 1 .
Study selection
The first stage of study selection by titles and abstracts was independently performed by two expert reviewers in vestibular rehabilitation (CMSA, RPA) and disagreements were arbitrated by a third reviewer (PBN). The selection considered the eligibility criteria and duplicate studies were excluded. The full texts of the eligible studies and those in doubt were fully read with the same procedure as the first stage of data selection.
Data extraction
Data regarding year of publication, authors, title, study design, participant characteristics, the vestibular rehabilitation intervention characteristics, types of control, control group activities, outcome values from study baseline to study endpoint and conclusion were extracted from each study by two independent reviewers (CMSA, RPA). Any disagreement between the two reviewers was resolved through discussion or arbitration by a third reviewer (PBN). E-mails and virtual messages were sent to some authors of studies to ask for information that was not included in the original studies.
Risk of bias assessment
The Revised Cochrane risk-of-bias tool for randomized trials (RoB-2) [ 20 ] was used to assess the methodological quality of the selected trials. This analysis tool has five domains: domain 1 - risk of bias arising from the randomization process; domain 2 - risk of bias due to deviations from the intended interventions, effect of assignment to intervention or effect of adhering to intervention; domain 3 - risk of bias due to missing outcome data; domain 4 - risk of bias in measurement of the outcome and domain 5 - risk of bias in selection of the reported result. Thus, 3–7 signaling questions were asked in each domain. The response options were: yes, probably yes, probably no, no and no information. The judgment on the risk of bias for each domain was proposed by an algorithm based on signaling questions. Each domain was classified as “low risk of bias”, “high risk of bias” or “some concern”. After analysis of each domain, an overall assessment of each study was performed following the same classification criteria. The study was evaluated to have a “low risk of bias” when all domains were considered. The classification of “some concern” was determined when at least one domain was partially met or was not clearly described in the manuscript. The study was defined as “high risk of bias” if at least one domain was not met, or when it had “some concerns” in various domains. The evaluation was performed by two independent reviewers (CMSA, RPA) and disagreements were analyzed by a third reviewer (SLN).
Quality of evidence
The quality of evidence was determined by the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system. The quality of evidence reflects the extent to which we are confident that an estimate of the effect is correct for each patient-important outcome [ 21 ]. The data evaluated encompassed five main domains: risk of bias evaluation, heterogeneity, indirectness of evidence, the imprecision of findings and potential publication bias. The evidence was classified as: “high quality” (we are very confident that the true effect lies close to that of the estimate of the effect); “moderate” (the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different); “low” (confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect); and “very low quality” (very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect). “High quality” was assigned for each included randomized controlled trial, and the evidence was then downgraded according to the analysis of each domain.
Statistical analysis
The mean and standard deviation (SD) at baseline and follow-up were extracted for each study group. The mean difference between the scores of intervention and control groups was computed, as well as its 95% confidence intervals (CI). The random effects model was used to estimate the mean differences between the scores of intervention and control groups. Statistical heterogeneity of evaluations among studies was evaluated by Cochran’s Q test and the I 2 inconsistency test; it was considered that values > 50% indicated high heterogeneity and p-values lower than 0.05 were considered significant. If 10 or more studies were included in the analysis of each outcome, a sub analysis was conducted considering the intervention number of sessions and length, disease stage degree according to Hoehn and Yahr classification, the patients’ medication status, and a publication bias analysis was also performed [ 22 ]. All analyses were performed using the Review Manager version 5.4 program.
Of the 485 studies obtained from the aforementioned searches, 137 were duplicates. Of the remaining 348, 320 were excluded by title and abstract and 28 were screened by reading the full text. Then, 20 were excluded according to the eligibility criteria, and 5 were analyzed by a third reviewer for discrepancies, all of which were excluded, with 3 studies remaining for the systematic review. The data were summarized and the reasons for exclusions are described in the PRISMA flowchart (Fig. 1 and Supplementary Material 2 ).
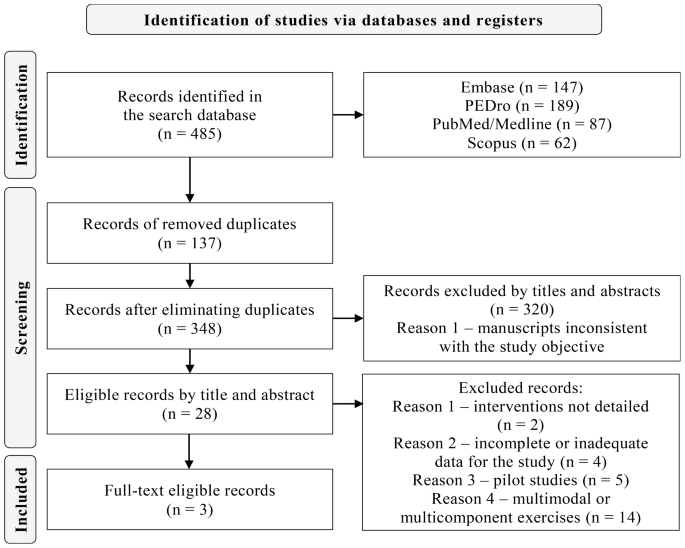
PRISMA Flowchart of the systematic review execution
Characteristics of the included studies and interventions
Of three included trials, one was conducted in Iran by Hadian et al. (2018) [ 23 ]. The other two studies took place in Italy; one by Smania et al. (2010) [ 24 ] and the other by Pazzaglia et al. (2019) [ 25 ].
The staging grade of PD was only described in two studies [ 23 , 24 ], showing great variety in Hoehn and Yahr from 1 to 4. The mean duration of PD in the intervention group ranged from 3.3 to 10.3 years and from 3.7 to 8.6 years in the control group. Subjects were on PD medication in all studies [ 23 , 24 , 25 ] and the evaluations and interventions occurred in the “on” clinical status. Exercises in the vestibular rehabilitation intervention groups were varied, including visual exercises with eye and head movements and static and dynamic balance exercises, with eyes open and closed on stable and unstable surfaces, with and without virtual reality support [ 23 , 24 , 25 ]. The frequency of the interventions was three times a week and the duration ranged from three [ 23 , 24 , 25 ] to eight [ 23 ] weeks. The time of each session was 40 min [ 25 ], 50 min [ 24 ] and 55 to 60 min [ 23 ]. The characteristics of the included studies and interventions are described in Table 1 .
Effect of interventions
Association between bbs and vestibular rehabilitation in pd.
The BBS was described in all of the selected studies [ 23 , 24 , 25 ]. The pre- and post-BBS scores of the intervention group were 47.83 and 55.0 [ 23 ], 44.5 and 49.8 [ 24 ] and 45.6 and 49.2 [ 25 ], Respectively. The pre- and post-BBS scores in the control group were 45.9 and 46.0 [ 23 ], 41.8 and 41.0 [ 24 ] and 47.3 and 48.1 [ 25 ], respectively. A meta-analysis with three studies that used the BBS tool was performed comparing vestibular therapy to other interventions as comparator groups. The results are presented as a forest plot [ 23 , 24 , 25 ] (Fig. 2 ). The analysis showed a difference in favor of vestibular rehabilitation (MD = 5.35; 95% CI = 2.39, 8.31; P < 0.001, number of studies = 3, number of participants = 130). The heterogeneity found was not significant ( P = 0.070) according to Cochrane’s Q test and equivalent to 62% according to the I 2 test. Care must be taken in the interpretation of the chi-squared test, since it has low power in a meta-analysis when studies have small sample size. This level of heterogeneity is considered high [ 22 ], indicating that the effects of different interventions may differ between studies. Therefore, caution is suggested when generalizing these results.
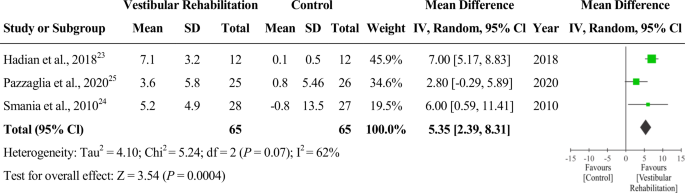
Forest plot comparing BBS between vestibular rehabilitation intervention group and control group
Other outcomes not included in the meta-analysis
The effects of other outcomes could not be analyzed because the instruments were described in only one study. However, all results in the intervention group were significant when compared before and after vestibular rehabilitation: FR [ 23 ] (MD = 7; 95% CI = 5.61, 8.38; P < 0.001), 2MWT [ 23 ] (MD = 23.75; 95% CI = 13.11, 34.38; P = 0.004), total DHI [ 23 ] (MD = -11.33; 95% CI = -15.25, -7.41; P < 0.001), ABC [ 24 ] (MD = 6.9; 95% CI = 4.5, 9.3; P < 0.001), CFP [ 24 ] (MD = 3.5; 95% CI = 1.9, 5.2; P < 0.001), DGI [ 25 ] (MD = 1.6; 95% CI = 0.6, 2.5; P = 0.003) and number of falls [ 24 ] (MD = -2.9; 95% CI = -5.3, -0.6; P < 0.001). Only the ABC scale showed statistically significant outcomes when comparing pre- and post-intervention in the control group: ABC [ 24 ] (MD = -1.3; 95% CI = -2.6, -0.0; P = 0.03).
Risk of bias
Fig. 3 describes the summary of the risk of bias analysis according to the RoB2 [ 20 ]. Overall, the risk of bias was considered as being of “some concern” in all studies [ 23 , 24 , 25 ]. A risk of bias with “some concern” occurred in domain 2 due to the lack of information on whether a proper analysis was performed to estimate the attribution effect for the intervention [ 23 , 24 , 25 ]. In addition, there was no description of whether the loss of participants impacted the analysis of the results in one of the studies [ 24 ]. It was not reported whether the analysis of outcomes in domain 5 was performed according to prespecified registries [ 23 , 25 ]
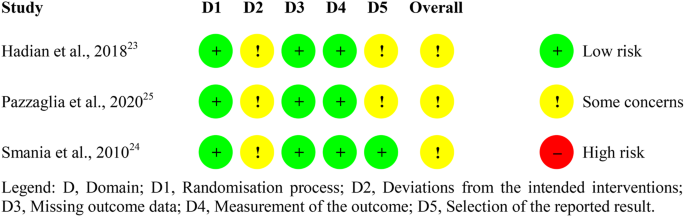
Summary of risk of bias by domain and study
The evaluation involved GRADE [ 21 ] aspects related to BBS outcomes. The quality of evidence produced by union of the included studies was considered very low (Table 2 ).
To the best of our knowledge, this is the first systematic review with meta-analysis that investigated the effectiveness of vestibular rehabilitation on postural balance in PD patients. Our meta-analysis compared vestibular rehabilitation with other exercise interventions, regardless of disease staging. Postural balance of patients with PD showed statistically significant improvements with vestibular rehabilitation [ 23 , 24 , 25 ].
Previous evidence in the literature also shows that patients with PD can improve postural balance with vestibular rehabilitation. The vestibular rehabilitation intervention in one of the studies was applied for 8 weeks in PD patients and compared to a control group [ 26 ]. The authors found a significant improvement in the BBS scores and in other instruments for assessing postural balance. Another study found improvement in balance in PD patients with Hoehn & Yahr scores of 3 and 4 after vestibular rehabilitation [ 27 ]. The therapy was performed in 9 sessions of 30 min each. The results sustained statistically significant improvements in all assessments and were maintained one year after the intervention. A rehabilitation program for PD patients was proposed in another study [ 28 ] for 4 weeks, in a total of 28 sessions. The results in the intervention group showed improvements in balance, gait, physical performance and trunk rotations, when compared to the control group. Other research has demonstrated beneficial results of vestibular rehabilitation in PD. One study with 24 PD patients had 12 take part in the experimental group with exercises from the Cawthorne & Cooksey protocol, which involves eye, head and body movements. Rehabilitation was carried out in 60-minute sessions, three times a week, for 12 weeks. The control group (12 patients) received the usual treatment during the research period. The BBS was used to assess postural balance. The experimental group had significantly higher scores in all BBS tests when compared to the control group, with statistically significant results [ 29 ]. Furthermore, a network meta-analysis investigated the efficacy of exergames and virtual reality in the rehabilitation of postural balance and gait in PD patients. We included 23 randomized controlled trials, of which 21 articles presented postural balance outcomes. Exergame and virtual reality were favorable strategies for vestibular rehabilitation. The proposed therapy improved postural balance in PD compared to treatment as usual and other active control interventions [ 30 ].
To explain our clinical findings, we first raised the hypothesis that the eye movements used in vestibular rehabilitation [ 23 , 24 , 25 ] favored the therapy results. The correlation of the extrinsic musculature of the eyes with the vestibular nuclear complex may have contributed to better postural balance function [ 31 ]. Exercises with eye movements may have improved the latency and accuracy of saccades, fixation and gain of pursuit movements. It is believed that changes in eye movements correlate with disturbances in the subcortical connections of the brainstem [ 32 , 33 ]. The substantia nigra pars reticulata modulates saccade and pursuit movements [ 34 ]. One study evaluated pre- and post intervention oculomotor tests with 24 vestibular rehabilitation sessions in PD patients [ 35 ]. The authors observed better performance in the oculomotor function of fixation, saccadic, and pursuit movements, as well as in postural balance in a small cohort. These findings corroborate another previous study [ 36 ] in which correlations between oculomotor changes, postural balance and gait were suggested in PD patients. Another aspect to be considered for the purposes of our meta-analysis is the correlation of the basal ganglia with postural adjustment control [ 3 , 4 , 5 ]. Postural stability, static and dynamic balance exercises were proposed during the vestibular rehabilitation sessions [ 23 , 24 , 25 ], which may have contributed to the postural adjustment performance.
Vestibular rehabilitation is a therapy indicated for cases of postural imbalance, regardless of the degree of PD staging. It is known that postural instability manifests itself with greater intensity from stage 3 of the Hoehn and Yahr scale, which can trigger recurrent episodes of postural imbalance [ 37 ]. In addition, the PD phenotype of Postural Instability and Gait Difficulty (PIGD) presents postural instability and imbalance earlier than the Dominant Tremor phenotype [ 38 ]. Thus, subtypes of PIGD will probably need an earlier and more complex intervention. Some vestibular rehabilitation therapy protocols are used in clinical practice and research. The Cawthorne and Cooksey protocol [ 39 , 40 ] which involves eye, head and body movements, was created to treat older adults who have vestibular disorders. Herdman’s protocol [ 41 ] encompasses an exercise program to increase vestibular adaptation, stabilization of static and dynamic posture and gaze and are indicated for unilateral and bilateral hypofunction. The Davis & O’Leary protocol [ 42 ] encompasses vertical and horizontal vestibulo-ocular reflex exercises and is indicated for patients with unilateral and bilateral hypofunction who present sensitivity to movement, ataxia and imbalance. Other possibilities, such as association of protocols, can be used in the therapeutic process for a broader approach to exercises. In addition, personalized vestibular rehabilitation exercises with the support of virtual reality [ 43 ] are also strategies used in therapy. There is currently a scarcity in the literature on the most suitable protocols depending on the stage of PD, the phenotype, and the structures affected at the peripheral or central level. The strategies and resources used in vestibular rehabilitation will depend on the signs and symptoms presented by PD patients. The exercises should be performed with the help of a professional for systematic guidance and with execution levels according to the difficulties of each patient [ 44 ].
The BBS measured in our meta-analysis, is a 14-item test scale which assesses performance completing balance tasks in different situations [ 45 ]. Each task is scored from (0–4), for a maximum of 56 points, which represents excellent balance and a score of 0 indicates severe equilibrium damage. The psychometric properties of the BBS show satisfactory internal consistency, intra- and interrater viability and construct validity [ 46 ]. According to the Movement Disorder Society [ 47 , 48 ], the BBS is considered a valid, reliable and recommended scale to be applied to PD patients. Therefore, vestibular rehabilitation therapy can use the BBS as a viable evaluation instrument. For scales such as the BBS, it is essential to identify the Minimum Important Change (MIC) [ 49 ], which is the smallest change that an instrument can detect on the improvement or worsening of results. The European Physiotherapy Guideline for Parkinson’s disease [ 49 ] suggests using Minimal Detectable Alteration (MDC), which corresponds to the actual improvement of the effect, when MIC is not available. In a previous study [ 50 ], the MDC of 5/56 points (95% CI) was calculated for BBS in 35 patients with PD and Hoehn and Yahr from 1 to 4. The difference of 5 points of MDC, could be considered as a useful functional gain, since it is associated with the perception of improvement of the patient, which corroborates the results of our meta-analysis (DM = 5.35; 95% CI = 2.39, 8.31). In any case, our results should be interpreted with caution, as they only included three randomized clinical trials and the risk of bias was considered as being of “some concern” in all studies. Thus, a larger evidence base is needed to validate this clinical significance. In addition, according to the GRADE criteria, our systematic review provided evidence of very low quality for the use of vestibular rehabilitation in postural balance in patients with PD. Thus, the actual effects may have been distorted from the estimated effects. The classification of the GRADE instrument was considered “serious” in relation to “risk of bias”, “inconsistency” and “imprecision”. The three studies that comprise the meta-analysis of the BBS outcome presented a risk of bias classified as “some concern” bias. In relation inconsistency, it was shown that the effect and magnitude of the intervention varied between primary studies. Detection was carried out based on both the overlapping confidence intervals of the studies included in the meta-analysis and the high heterogeneity. In the criteria of imprecision, the number of patients included in the analysis was low ( n = 130), so optimal information size was not achieved [ 21 , 51 ]. The high heterogeneity of our review (I² = 62%) also requires care in generalizing the results in the PD population. Possible reasons or explanations could be considered, some of them regarding clinical features and another about methodological differences between the included studies. The patients who composed the samples of the included studies differed in terms of disease staging (Hoehn and Yahr stage), as well as time since diagnosis (Table 1 ). The interventions applied also showed differences in their composition. The protocols included virtual reality [ 25 ], balance exercises to improve feed forward and feedback postural reaction [ 24 ] and adaptation exercises (vestibulo-ocular reflex) [ 23 ], constituting a factor which may have influenced the differences in BBS responses.
Another important aspect to be considered in our systematic review and meta-analysis was the risk of bias. Blinding of participants and outcome assessors was reported in only one of the studies [ 24 ]. The lack of description of blinding in the other two studies [ 23 , 25 ] may have interfered with the analyzed results. In addition, it was not described whether there was an intention-to-treat analysis to maintain group randomization [ 23 , 25 ].
Strengths and limitations
A strength of this study is that the study selection and data extraction process were conducted by two independent reviewers. Another point to be highlighted is that no co-intervention with vestibular rehabilitation was considered in any of the included studies [ 23 , 24 , 25 ]. Thus, the therapy effectiveness could be analyzed without any confounding factors. However, some limitations can be mentioned. The studies samples [ 23 , 24 , 25 ] were small, which may have impacted the generalizability of the results. Second, the heterogeneity of the studies [ 23 , 24 , 25 ] was substantial, and it was not possible to explore it with sensitivity analyses due to the low number of included studies. Finally, the intervention programs [ 23 , 24 , 25 ] were not uniform and the meta-analysis was performed regardless of the Hoehn and Yahr stage.
Implications
The evidence from this study has important clinical implications. Identifying patients with postural imbalance in PD is essential for therapeutic referral. There is a need to guide health professionals about vestibular rehabilitation as a possibility for treating postural imbalance in PD. Regarding the implications of the research, further clinical trials are needed to prove the efficacy of vestibular rehabilitation in patients with PD. It is essential that studies designate which exercises are most appropriate for postural imbalance, at each stage of PD and for each phenotype. Specific strategies and protocols, personalized vestibular rehabilitation, and the use of technological resources, such as virtual reality, also need to be validated in this population. The effect size of vestibular rehabilitation on the postural balance of patients with PD in the short and long term becomes essential to evaluate the clinical outcome. Public policy reformulations may be necessary in some countries in order for PD patients to have access to this therapy.
The present study demonstrated that vestibular rehabilitation has the potential to assist the postural balance of PD patients compared to other interventions. However, the very low quality of the evidence shows uncertainty about the impact of this clinical practice on the studied population. Vestibular rehabilitation interventions in PD should be applied with caution by health professionals until larger, well-conducted studies can confirm their benefits and determine their true effect size.
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Abbreviations
2-Minute Walk Test
Activities-specific Balance Confidence
Berg Balance Scale
Confidence Intervals
Dynamic Gait Index
Functional Range Test
Grading of Recommendations Assessment, Development and Evaluation
Minimal Detectable Alteration
Minimum Important Change
Mini Balance Evaluation Systems Test
Parkinson’s Disease
Physiotherapy Evidence Database
Population, Intervention, Comparasion, Outcome, Study type
Reporting Items for Systematic Reviews and Meta-Analyses
International Prospective Register of Systematic Reviews
Revised Cochrane risk-of-bias tool for randomized trials
Standard Deviation
Time Up and Go Test
Jankovic J. Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79(4):368–76. https://doi.org/10.1136/jnnp.2007.131045 .
Article CAS PubMed Google Scholar
Campos-Sousa IS, Campos-Sousa RN, Ataíde L, Soares MMB, Almeida KJ. Executive dysfunction and motor symptoms in Parkinson’s disease. Arq Neuropsiquiatr. 2010;68(2):246–51. https://doi.org/10.1590/S0004-282X2010000200018 .
Article PubMed Google Scholar
Bronstein AM, Hood JD, Gresty MA, Panagi C. Visual control of balance in cerebellar and parkinsonian syndromes. Brain. 1990;113(3):767–79. https://doi.org/10.1093/brain/113.3.767 .
Chong RKY, Horak FB, Woollacott MH. Parkinson’s disease impairs the ability to change set quickly. J Neurol Sci. 2000;175(1):57–70. https://doi.org/10.1016/S0022-510X(00)0027 .
Horak FB, Dimitrova D, Nutt JG. Direction-specific postural instability in subjects with Parkinson’s disease. Exp Neurol. 2005;193(2):504–21. https://doi.org/10.1016/j.expneurol.2004.12 .
Lv W, Guan Q, Hu X, Chen J, Jiang H, Zhang L, et al. Vestibulo-ocular reflex abnormality in Parkinson’s disease detected by video head impulse test. Neurosci Lett. 2017;657:211–4. https://doi.org/10.1016/j.neulet.2017.08.021 .
Smith PF. Vestibular functions and Parkinson’s disease. Front Neurol. 2018;9:1085. https://doi.org/10.3389/fneur.2018.01085 .
Article PubMed PubMed Central Google Scholar
Frenklach A, Louie S, Koop MM, Bronte-Stewart HM. Excessive postural sway and the risk of falls at different stages of Parkinson’s disease. Mov Disord. 2009;24(3):377–85. https://doi.org/10.1002/mds.22358 .
Müller MLTM, Bohnen NI. Cholinergic dysfunction in Parkinson’s disease. Curr Neurol Neurosci Rep. 2013;13(9):377. https://doi.org/10.1007/s11910-013-0377-9 .
Article CAS PubMed PubMed Central Google Scholar
Vitale C, Marcelli V, Furia T, Santangelo G, Cozzolino A, Longo K, et al. Vestibular impairment and adaptive postural imbalance in parkinsonian patients with lateral trunk flexion. Mov Disord. 2011;26(8):1458–63. https://doi.org/10.1002/mds.23657 .
Berkiten G, Tutar B, Atar S, Kumral TL, Saltürk Z, Akan O, et al. Assessment of the clinical use of vestibular evoked myogenic potentials and the video head impulse test in the diagnosis of early-stage Parkinson’s disease. Ann Otol Rhinol Laryngol. 2023;132(1):41–9. https://doi.org/10.1177/00034894211067838 .
Zampogna A, Mileti I, Martelli F, Paoloni M, Del Prete Z, Palermo E, et al. Early balance impairment in Parkinson’s Disease: evidence from Robot-assisted axial rotations. Clin Neurophysiol. 2021;132(10):2422–30. https://doi.org/10.1016/j.clinph.2021.06.023 .
Abbruzzese G, Marchese R, Avanzino L, Pelosin E. Rehabilitation for Parkinson’s disease: current outlook and future challenges. Park Relat Disord. 2016;22(Suppl 1):S60–4. https://doi.org/10.1016/j.parkreldis.2015.09.005 .
Article Google Scholar
Herdman SJ. Vestibular rehabilitation. Curr Opin Neurol. 2013;26(1):96–101. 10. 1097/WCO.0b013e32835c5ec4.
Cawthorne T. Vestibular injuries. Proc R Soc Med. 1946;39(5):270–3. https://doi.org/10.1177/003591574603900522 .
Balaban CD, Hoffer ME, Gottshall KR. Top-down approach to vestibular compensation: translational lessons from vestibular rehabilitation. Brain Res. 2012;1482:101–11. https://doi.org/10.1016/j.brainres.2012.08.040 .
Han BI. Simplified vestibular rehabilitation therapy. Singapore: Springer; 2021.
Book Google Scholar
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. https://doi.org/10.1016/j.ijsu.2021.105906 .
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591–601. 10. 1002/mds.26424.
Cochrane. RoB 2: a revised Cochrane risk-of-bias tool for randomized trials. London: Cochrane; c2023. https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials Accessed 16 Mar 2023.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94. https://doi.org/10.1016/j.jclinepi.2010.04.026 .
Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342(7804):964–7. https://doi.org/10.1136/bmj.d549 .
Hadian M, Raji P, Abasi A, Hoseinabadi R, Baghestani A. Evaluation of the effect of vestibular exercises on dizziness and postural control in Parkinson patients. J Mod Rehabil. 2018;12(1):13–20. https://doi.org/10.32598/jmr.12.1.13 .
Smania N, Corato E, Tinazzi M, Stanzani C, Fiaschi A, Girardi P, et al. Effect of balance training on postural instability in patients with idiopathic parkinsong’s disease. Neurorehabil Neural Repair. 2010;24(9):826–34. https://doi.org/10.1177/1545968310376057 .
Pazzaglia C, Imbimbo I, Tranchita E, Minganti C, Ricciardi D, Lo Monaco R, et al. Comparison of virtual reality rehabilitation and conventional rehabilitation in Parkinson’s disease: a randomised controlled trial. Physiotherapy. 2020;106:36–42. 10.1016/j. physio.2019.12.007.
Acarer A, Karapolat H, Celebisoy N, Ozgen G, Colakoglu Z. Is customized vestibular rehabilitation effective in patients with Parkinson’s? NeuroRehabilitation. 2015;37(2):255–62. https://doi.org/10.3233/NRE-151258 .
Zeigelboim BS, Klagenberg KF, Teive HAG, Munhoz RP, Martins-Bassetto J. Vestibular rehabilitation: clinical benefits to patients with Parkinson’s disease. Arq Neuropsiquiatr. 2009;67(2–A):219–23. https://doi.org/10.1590/S0004-282X2009000200009 .
Stożek J, Rudzińska M, Pustułka-Piwnik U, Szczudlik A. The effect of the rehabilitation program on balance, gait, physical performance and trunk rotation in Parkinson’s disease. Aging Clin Exp Res. 2016;28(6):1169–77. https://doi.org/10.1007/s40520-015-0506-1 .
Seyedahmadi M, Taherzadeh J, Akbari H. The effect of 12 weeks of cawthorne-cooksey exercises on balance and quality of life in patients with Parkinson’s Disease. Med J Islam Repub Iran. 2023;37:125. https://doi.org/10.47176/mjiri.37.125 .
Chuang CS, Chen YW, Zeng BY, Hung CM, Tu YK, Tai YC, et al. Effects of modern technology (exergame and virtual reality) assisted rehabilitation vs conventional rehabilitation in patients with Parkinson’s disease: a network meta-analysis of randomised controlled trials. Physiotherapy. 2022;117:35–42. https://doi.org/10.1016/j.physio.2022 .
Gdowski GT, McCrea RA. Integration of vestibular and head movement signals in the vestibular nuclei during whole-body rotation. J Neurophysiol. 1999;82(1):436–49. https://doi.org/10.1152/jn.1999.82.1.436 .
Zhang JY, Zhang B, Ren QG, Zhong Q, Li Y, Liu GT, et al. Eye movement especially vertical oculomotor impairment as an aid to assess Parkinson’s disease. Neurol Sci. 2021;42(6):2337–45. https://doi.org/10.1007/s10072-020-04796-6 .
Frei K. Abnormalities of smooth pursuit in Parkinson’s disease: a systematic review. Clin Park Relat Disord. 2021;4:100085. https://doi.org/10.1016/j.prdoa.2020.100085 .
Basso MA, Pokorny JJ, Liu P. Activity of substantia Nigra pars reticulata neurons during smooth pursuit eye movements in monkeys. Eur J Neurosci. 2005;22(2):448–64. https://doi.org/10.1111/j.1460-9568.2005.04215.x .
Abasi A, Hoseinabadi R, Raji P, Friedman JH, Hadian MR. Evaluating oculomotor tests before and after vestibular rehabilitation in patients with Parkinson’s disease: a pilot pre-post study. Parkinsons Dis. 2022;2022:6913691. https://doi.org/10.1155/2022/6913691 .
Zhang Y, Yan A, Liu B, Wan Y, Zhao Y, Liu Y, et al. Oculomotor performances are associated with motor and non-motor symptoms in Parkinson’s disease. Front Neurol. 2018;9:960. https://doi.org/10.3389/fneur.2018.00960 .
Hely MA, Morris JG, Rail D, Reid WG, O’Sullivan DJ, Williamson PM, et al. The Sydney multicentre study of Parkinson’s disease: a report on the first 3 years. J Neurol Neurosurg Psychiatry. 1989;52(3):324–8. https://doi.org/10.1136/jnnp.52.3.324 .
Kulisevsky J, Luquin MR, Arbelo JM, Burguera JA, Carrillo F, Castro A, et al. Enfermedad De Parkinson avanzada. Características clínicas y tratamiento (parte I). Neurologia. 2013;28(8):503–21. https://doi.org/10.1016/j.nrl.2013.05.001 .
Cawthorne T. The physiological basis for head exercises. J Chart Soc Physio Ther. 1944;30:106–7.
Google Scholar
Cooksey FS. Rehabilitation in vestibular injuries. Proc R Soc Med. 1946;39(5):273–8. https://doi.org/10.1177/003591574603900523 .
Turano KA, Dagnelie G, Herdman SJ. Visual stabilization of posture in persons with central visual field loss. Invest Ophthalmol Vis Sci. 1996;37(8):1483–91.
CAS PubMed Google Scholar
Hoffman DL, O’Leary DP, Munjack DJ. Autorotation test abnormalities of the horizontal and vertical vestibulo-ocular reflexes in panic disorder. Otolaryngol Head Neck Surg. 1994;110(3):259–69. https://doi.org/10.1177/019459989411000302 .
Carvalho HAS, Sousa LCS, Conceição LP, Santos NV, Novanta GGR. Realidade virtual como proposta de intervenção nas patologias vestibulares: revisão integrativa. Braz J Hea Rev. 2023;6(5):24549–61. https://doi.org/10.34119/bjhrv6n5-501 .
Lacour M, Bernard-Demanze L. Interaction between vestibular compensation mechanisms and vestibular rehabilitation therapy: 10 recommendations for optimal functional recovery. Front Neurol. 2015;5:285. https://doi.org/10.3389/fneur.2014.00285 .
Kornetti DL, Fritz SL, Chiu YP, Light KE, Velozo CA. Rating scale analysis of the Berg Balance Scale. Arch Phys Med Rehabil. 2004;85(7):1128–35. https://doi.org/10.1016/j.apmr.2003 . 11.019.
Taghizadeh G, Martinez-Martin P, Fereshtehnejad SM, Habibi SA, Nikbakht N, Alizadeh NH, et al. Psychometric properties of the Berg Balance Scale in idiopathic Parkinson’ disease in the drug off-phase. Neurol Sci. 2018;39(12):2175–81. https://doi.org/10.1007/s10072-018-3570-4 .
Bloem BR, Marinus J, Almeida Q, Dibble L, Nieuwboer A, Post B, et al. Measurement instruments to assess posture, gait, and balance in Parkinson’s disease: critique and recommendations. Mov Disord. 2016;31(9):1342–55. https://doi.org/10.1002/mds.26572 .
Opara J, Małecki A, Małecka E, Socha T. Motor assessment in Parkinson’s disease. Ann Agric Environ Med. 2017;24(3):411–5. https://doi.org/10.5604/12321966.1232774 .
Keus S, Munneke M, Graziano M, Paltamaa J, Pelosin E, Domingos J, et al. European physiotherapy guideline for Parkinson’s disease. Netherlands: KNGF/ParkinsonNet; 2014.
Steffen T, Seney M. Test-retest reliability and minimal detectable change on balance and ambulation tests, the 36-item short-form health survey, and the unified Parkinson disease rating scale in people with parkinsonism. Phys Ther. 2008;88(6):733–46. https://doi.org/10.2522/ptj.20070214 .
Bonner A, Alexander PE, Brignardello PR, Furukawa TA, Siemieniuk RA, Zhang Y, et al. Applying GRADE to a network meta-analysis of antidepressants led to more conservative conclusions. J Clin Epidemiol. 2018;102:87–98. https://doi.org/10.1016/j.jclinepi.2018.05.009 .
Download references
Acknowledgements
The author Pedro Braga-Neto received funding from the Brazilian National Council for Scientific and Technological Development (CNPq) as research grant funding (Research Productivity scholarship).
No specific funding was received for this work.
Author information
Authors and affiliations.
Division of Neurology, Department of Clinical Medicine, Faculty of Medicine, Federal University of Ceará, Rodolfo Teófilo – Fortaleza – Ceará, R.Prof. Costa Mendes Street – 4th floor, Fortaleza, 1608, Brazil
Carla Marineli Saraiva do Amaral, Samuel Brito de Almeida, Rodrigo Mariano Ribeiro & Pedro Braga-Neto
Department of Health Sciences, Faculty of Phonoaudiology, University of Fortaleza, Fortaleza, Brazil
Renata Parente de Almeida
Department of Physical Therapy, Faculty of Medicine, Federal University of Ceará, Fortaleza, Brazil
Simony Lira do Nascimento
You can also search for this author in PubMed Google Scholar
Contributions
C.M.S.A., S.B.A. and P.B.N. contributed to the concept, idea and research project. C.M.S.A., R.P.A., S.L.N. and P.B.N. participated in the editorial team. C.M.S.A. and R.P.A. collected data. All authors participated in the data analysis, read and approved the final version of the manuscript. The project was managed by C.M.S.A. and P.B.N.
Corresponding author
Correspondence to Pedro Braga-Neto .
Ethics declarations
Ethics approval and consent to participate.
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines. The authors confirm that the approval of an institutional review board was not required for this work. The authors confirm that patient consent was not required for this work.
Consent for publication
We grant publication of the article to BMC journal. We confirm that we understand BMC Neurology is an open access journal that levies an article processing charge per articles accepted for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
do Amaral, C.M.S., de Almeida, S.B., de Almeida, R.P. et al. Effectiveness of vestibular rehabilitation on postural balance in Parkinson’s disease: a systematic review and meta-analysis of randomized controlled trials. BMC Neurol 24 , 161 (2024). https://doi.org/10.1186/s12883-024-03649-5
Download citation
Received : 04 September 2023
Accepted : 22 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12883-024-03649-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Parkinson’s disease
- Balance dysfunction
- Vestibular disease
- Rehabilitation
- Movement disorder
BMC Neurology
ISSN: 1471-2377
- General enquiries: [email protected]

COMMENTS
Systematic reviews have specific advantages because of using explicit methods which limit bias, draw reliable and accurate conclusions, easily deliver required information to healthcare providers, researchers, and policymakers, help to reduce the time delay in the research discoveries to implementation, improve the generalizability and ...
Systematic reviews can help us know what we know about a topic, and what is not yet known, often to a greater extent than the findings of a single study. 4 The process is comprehensive enough to establish consistency and generalizability of research findings across settings and populations. 3 A meta-analysis is a type of systematic review that ...
The continuous growth of research, coupled with the demand to systematically summarize the available evidence to inform decisions from consumers and stakeholders, led to the formal development of systematic reviews (SRs) in the late 20th century 1-3. Systematic reviews search, appraise and collate all relevant empirical evidence in order to ...
A Cochrane Review is a systematic review of research in health care and health policy that is published in the Cochrane Database of Systematic Reviews. ... Many Cochrane Reviews measure benefits and harms by collecting data from more than one trial, and combining them to generate an average result. This aims to provide a more precise estimate ...
A systematic review identifies and synthesizes all relevant studies that fit prespecified criteria to answer a research question (Lasserson et al. 2019; IOM 2011).What sets a systematic review apart from a narrative review is that it follows consistent, rigorous, and transparent methods established in a protocol in order to minimize bias and errors.
Systematic reviews are usually peer-reviewed at different stages in the process. Furthermore, they are often registered with systematic review research networks, for instance, the Cochrane Collaboration in the medicine field or the Campbell Collaboration for reviews in education, crime and justice and social welfare.
A systematic review is a type of review that uses repeatable methods to find, select, and synthesize all available evidence. It answers a clearly formulated research question and explicitly states the methods used to arrive at the answer. Example: Systematic review. In 2008, Dr. Robert Boyle and his colleagues published a systematic review in ...
In recent years, there has been an explosion in the number of systematic reviews conducted and published (Chalmers & Fox 2016, Fontelo & Liu 2018, Page et al 2015) - although a systematic review may be an inappropriate or unnecessary research methodology for answering many research questions.Systematic reviews can be inadvisable for a variety of reasons.
A systematic review is a form of analysis that medical researchers carry out to synthesize all the available evidence on a particular question, such as how effective a drug is. A meta-analysis is ...
Although systematic literature reviews have many permutations and decision points, experts generally agree on their overall structure. SLRs begin by (1) establishing the research question and determining the parameters for a literature search, then (2) conduct the search using keyword searches and screening to produce the "content" to be analyzed, then (3) analyse and synthesize the ...
Abstract. Systematic reviews provide a synthesis of evidence for a specific topic of interest, summarising the results of multiple studies to aid in clinical decisions and resource allocation. They remain among the best forms of evidence, and reduce the bias inherent in other methods. A solid understanding of the systematic review process can ...
A systematic review aims to bring evidence together to answer a pre-defined research question. This involves the identification of all primary research relevant to the defined review question, the critical appraisal of this research, and the synthesis of the findings.13 Systematic reviews may combine data from different.
Systematic reviews are usually peer-reviewed at different stages in the process. Furthermore, they are often registered with systematic review research networks, for instance, the Cochrane Collaboration in the medicine field or the Campbell Collaboration for reviews in education, crime and justice and social welfare. The objective of registering
A systematic review can be explained as a research method and process for identifying and critically appraising relevant research, as well as for collecting and analyzing data from said research (Liberati et al., 2009). The aim of a systematic review is to identify all empirical evidence that fits the pre-specified inclusion criteria to answer ...
Systematic reviews are at the top level of the evidence pyramid. Systematic reviews are considered credible sources since they are comprehensive, reproducible, and precise in stating the outcomes. The type of review system used and the approach taken depend on the goals and objectives of the research. To choose the best-suited review system ...
Strategic Sense. Undertaking qualitative systematic reviews also provides a range of useful strategic benefits. Proposals seek to make arguments of the benefits of the research, but also establish a credibility narrative for the researcher—that "I know my stuff," the lay of the research land.
Our systematic review contradicts a recent harmonised study 27 combining data from two RCTs 26,29 on vitamin C use in COVID-19 patients. This study suggests futility with vitamin C supplementation ...
This variability is partly due to differences in study designs, population demographics, and detection methods used across various research studies. A systematic review and meta-analysis of the existing studies can provide a more comprehensive understanding of HPV's prevalence in HNC, offering insights into regional variations.
Systematic review methods: JHL, SY, and TDP are experts in systematic review methods. Information retrieval: SY is an expert in information retrieval. Statistical analysis: TDP is an expert in meta-analysis. DECLARATIONS OF INTEREST. MAB, TMO, and JRS have been involved in the conduct and reporting of primary research on the topic.
This systematic review and meta-analysis followed the principles of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 statement (PRISMA 2020). ... Further research is needed to study the effect of muscle mass in distinct anatomical regions on knee osteoarthritis. 3.4. The association between low muscle mass and knee ...
In recent years, there has been a surge in research examining the correlation between training load and injury risk among professional football players. One prominent model proposed for this purpose is the acute-to-chronic workload ratio (ACWR). This review aimed to compile studies focusing on professional footballers that explored the association between the ACWR and injury risk, offering ...
Research has shown that ferroptosis can promote and inhibit tumor growth, which may have prognostic value. Given the unclear role of ferroptosis in cancer biology, this meta-analysis aims to investigate its impact on cancer prognosis. This systematic review and meta-analysis conducted searches on PubMed, Embase, and the Cochrane Library databases.
Introduction Postural balance impairment can affect the quality of life of patients with Parkinson's disease. Previous studies have described connections of the vestibular system with postural functions, suggesting a potential participation of the basal ganglia in receiving vestibular stimuli. This systematic review aims to summarize the evidence on the effectiveness of vestibular ...
Skyrise greenery, including green roofs and vertical gardens, has emerged as an indispensable tool for sustainable urban planning with multiple ecological and economic benefits. A bibliometric analysis was used to provide a systematic review of the functions associated with skyrise greenery in urban landscapes. Key research tools, including the "Bibliometrix" R package and "CiteSpace ...