- Open access
- Published: 29 October 2019

A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components
- Zheng Liu ORCID: orcid.org/0000-0002-8904-6034 1 na1 ,
- Han-Meng Xu 1 na1 ,
- Li-Ming Wen 2 ,
- Yuan-Zhou Peng 1 ,
- Li-Zi Lin 1 ,
- Shuang Zhou 1 ,
- Wen-Hao Li 1 &
- Hai-Jun Wang 1
International Journal of Behavioral Nutrition and Physical Activity volume 16 , Article number: 95 ( 2019 ) Cite this article
20k Accesses
81 Citations
23 Altmetric
Metrics details
Childhood obesity is a serious public health concern . School-based interventions hold great promise to combat the rising trend of childhood obesity. This systematic review aimed to assess the overall effects of school-based obesity prevention interventions, and to investigate characteristics of intervention components that are potentially effective for preventing childhood obesity.
We systematically searched MEDLINE, CENTRAL and Embase databases to identify randomized- or cluster randomized- controlled trials of school-based obesity interventions published between 1990 and 2019. We conducted meta-analyses and subgroup analyses to determine the overall effects of obesity prevention programs and effect differences by various characteristics of intervention components on body mass index (BMI) or BMI Z-score of children.
This systematic review included a total of 50 trials (reported by 56 publications). Significant differences were found between groups on BMI (− 0.14 kg/m 2 (95% confidence interval: − 0.21, − 0.06)) and BMI Z-score (− 0.05 (− 0.10, − 0.01)) for single-component interventions; significant differences were also found between groups on BMI (− 0.32 (− 0.54, − 0.09) kg/m 2 ) and BMI Z-score (− 0.07 (− 0.14, − 0.001)) for multi-component interventions. Subgroup analyses consistently demonstrated that effects of single-component (physical activity) interventions including curricular sessions (− 0.30 (− 0.51, − 0.10) kg/m 2 in BMI) were stronger than those without curricular sessions (− 0.04 (− 0.17, 0.09) kg/m 2 in BMI); effects of single-component (physical activity) interventions were also strengthened if physical activity sessions emphasized participants’ enjoyment (− 0.19 (− 0.33, − 0.05) kg/m 2 in BMI for those emphasizing participants’ enjoyment; − 0.004 (− 0.10, 0.09) kg/m 2 in BMI for those not emphasizing participants’ enjoyment). The current body of evidence did not find specific characteristics of intervention components that were consistently associated with improved efficacy for multi-component interventions ( P > 0.05).
Conclusions
School-based interventions are generally effective in reducing excessive weight gain of children. Our findings contribute to increased understandings of potentially effective intervention characteristics for single-component (physical activity) interventions. The impact of combined components on effectiveness of multi-component interventions should be the topic of further research. More high-quality studies are also needed to confirm findings of this review.
Introduction
Childhood overweight and obesity are global public health issues. The prevalence has increased from 16.9 to 23.8% in boys and from 16.2 to 22.6% in girls from 1980 to 2013 in developed countries, while in developing countries, the prevalence has also increased from 8.1 to 12.9% in boys and 8.4 to 13.4% in girls [ 1 ]. Childhood obesity is associated with a variety of adverse consequences [ 2 , 3 ], which often persist into adulthood [ 4 ]. Therefore, prevention of childhood obesity has become one of the important public health priorities.
The main cause of childhood overweight and obesity is an energy imbalance between calories consumed and calories expended. Children spend half of their waking hours and consume at least one-third of their daily calories at school, and thus schools are being recognized as ideal vehicles for delivering obesity interventions to most children [ 5 ].
Based on the Environmental Research framework for weight Gain prevention as well as an energy balance approach [ 6 ], the goal of obesity prevention might be achieved by improvement of energy balance-related behaviors (physical activity (PA)), dietary improvement (DI)), which can be influenced by environmental influence (school policy (SP)) directly or indirectly. The direct influence reflects the “automatic, unconscious” influence of the SP on behavior. The indirect mechanism reflects the mediating role of knowledge, cognitions related to behavior (health education (HE)) in the influence of the environment on behavior. As such, a range of intervention components (PA, DI, SP, HE) have been widely used in childhood obesity prevention interventions.
Notably, a great deal of variability existed in the frequency, duration and content of intervention components [ 5 , 7 , 8 ]. For instance, some school-based interventions focused on increasing students’ daily physical activity [ 9 , 10 ], while others only increased the frequency of physical activity by 2–3 times/week [ 11 , 12 ]. Topics of health education interventions also varied. Some focused primarily on nutrition education with few physical activity or sedentary behaviors education [ 13 , 14 ], some mainly on physical activity or sedentary behaviors education with few nutrition education [ 15 , 16 ], while others covered both physical activity and nutrition education [ 9 , 17 ]. The variety of characteristics of intervention components raises the question of what is specifically associated with intervention efficacy.
Previous reviews attempted to address question of this kind and revealed some general findings. That is, interventions covering multiple components and involving families tended to be effective [ 5 , 6 ]. Three issues remained yet. First, some reviews only summarized intervention components that were commonly used in previous trials [ 5 , 18 ], but they did not compare various components used in effective or non-effective trials. In other words, the identified components could be used in both effective and non-effective trials, so that the exact components uniquely related to intervention effectiveness were still unknown. Second, a previous review, focusing on the specific role of behavior change techniques, summarized “effectiveness ratio” which was determined by the ratio of intervention components used in effective trials relative to those used in both effective and non-effective trials [ 19 ]. However, the trials included in the review were weighted equally by this approach regardless of the sample size and standard error of the outcomes. Third, another review compared sub-group differences in effect sizes between trials with and without the intervention characteristics by using meta-analytic technique [ 20 ]. However, to our knowledge, this approach has not been used in specifying the effective intervention components in school-based obesity prevention interventions.
To fill the research gaps in this field, we conducted a systematic review and meta-analysis of the best available evidence from randomized controlled trials (RCT). This review aimed to firstly summarize the overall effect size of school-based obesity prevention interventions, and secondly to explore characteristics of intervention components that were associated with the improved intervention efficacy.
Literature search
We systematically searched three databases including MEDLINE, CENTRAL and Embase to identify RCTs of school-based obesity interventions. We included publications between January 1990 and July 2019. Our searching strategy primarily contained terms in relation to participants, interventions, body weight and study design. The full search strategy was attached in the online supporting document. The reference lists of all retrieved full text reviews were further searched for additional relevant publications. The date for our final search was July 8th, 2019.
Inclusion criteria for this review were: (1) individual- or cluster-RCT, (2) interventions implemented among students of elementary or secondary schools (aged 5~18 years), (3) studies assessing students’ body mass index (BMI) or BMI Z-score, (4) anthropometric data being collected by physical examination, (5) interventions lasting for at least 3 months, (6) intervention groups aiming for promoting healthy weight or prevention of overweight or obesity rather than treatment of overweight or obesity, (7) comparison groups being active controls, usual practice controls (maintaining “normal” school activities) or wait-list controls, (8) the English version of full-text publications available (for pragmatic reasons), as well as (9) studies providing data for meta-analyses (means, standard deviations (SDs) or 95% confidence intervals (CIs)).
Exclusion criteria included (1) studies only using questionnaires to collect the adiposity outcomes, and (2) studies specifically designed for the treatment of obesity-related diseases (e.g., type 2 diabetes or hypertension).
Screening and data extraction
First, two reviewers (HMX; YZP) independently screened the titles and abstracts of publications obtained by the searches. Second, full texts were further identified for their eligibility. Reference lists of reviews were additionally checked for their eligibility. Discrepancies between the two reviewers (HMX; YZP) were discussed by themselves or with a third reviewer (ZL) and resolved with consensus.
The first reviewer (ZL) developed a detailed coding scheme, and the extraction items included authors, year of publication, study design, sample size, age of participants, percentages of female participants, components and characteristics of interventions, outcome measures and assessment of risk of bias. The components and characteristics of interventions were extracted from both the main papers and the intervention protocols [ 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 ]. Authors were further contacted for details that were not reported in the publications (in three cases). A second reviewer (HMX) independently extracted data from all the included studies, and 20% of the extracted data were double checked by the first reviewer (ZL). Disagreements in relation to data extraction were resolved by a brief discussion (kappa statistics: 0.62; in five cases).
Assessment of risk of bias
Risk of bias of individual studies was assessed following the Cochrane guidance [ 31 ]. The assessment contains the following domains including (1) random sequence generation ( whether or not the study used a randomized sequence of assignments ), (2) concealment of the allocation sequence ( whether or not the allocation sequences were protected by adequate concealment ), (3) blinding of participants and personnel ( whether or not participants or healthcare providers were aware of intervention assignments ), (4) blinding of outcome assessment ( whether or not people who determined outcome measurements were aware of intervention assignments ), (5) incomplete outcome data ( the possibility of bias due to missing outcome data ), (6) selective outcome reporting ( whether or not the results reported were consistent with the original variables in the protocol ) and (7) other bias ( the possibility of bias not reported in the previous domains ). The leading author (ZL) was responsible for training the other author (HMX) to ensure a consistent understanding of the evaluation criteria of risk of bias between the two authors (ZL; HMX). Each domain was rated as having a high, low or unclear risk of bias. We also paid particular attention to the use of statistical methods specific to cluster-randomized trials (whether or not considering the cluster effect), and rated them in the domain of other bias.
Data synthesis
We calculated differences in means of BMI and BMI Z-score between intervention and control groups that were reported change from baseline or follow-up BMI indices controlled for baseline measures. If the trials reported data at both immediately post-intervention and subsequent follow-ups, only the data at immediately post-intervention was included in the meta-analyses (as most of the included studies did not report the sustained effect of interventions).
As we expected considerable heterogeneity across studies, the random-effects model was used to pool the weighted results by inverse variance methods. We used the I 2 statistic to provide a measure of heterogeneity. Results with P < 0.05 are reported as significant. The level of heterogeneity across studies were rated as low (I 2 = 25%), moderate (I 2 = 50%) or high (I 2 = 75%). We used Stata/SE 15.0 (StataCorp) for all analyses.
Subgroup analyses
To identify the characteristics of interventions potentially contributing to the improved effects, we first categorized interventions into those having the specified intervention components (i.e., SP, HE, PA and DI) and those without these. Then, we classified interventions into those using single or multiple components, as their effect sizes were detected as significantly different in previous reviews [ 6 , 32 ]. Further, we used subgroup analyses to examine differences in effect sizes by inclusion of SP related to obesity prevention (for multi-component interventions; yes vs. no), whether or not topics in HE covering both energy input and expenditure (for both single- and multi-component interventions; yes vs. no), duration and frequency of PA (for both single- and multi-component interventions; ≥3 times/week and ≥ 10 min/time vs. < 3 times/week or < 10 min/time), whether or not including curricular PA (for both single- and multi-component interventions; yes vs. no), whether or not focusing on students’ enjoyment of PA (for both single- and multi-component interventions; yes vs. no), and whether or not including the DI component (for multi-component interventions; yes vs. no).
Sensitivity analyses
We conducted sensitivity analyses for the following considerations:
1. If heterogeneity in the meta-analyses was moderate or high, we additionally obtained the pooled results by excluding individual studies for which the 95% CI of the intervention effect does not overlap with others.
2. We compared the pooled results obtained by all studies with those excluding individual studies at high risk of bias.
3. We grouped all comparisons according to characteristics of the study population ( sex : exclusively boys, exclusively girls; weight status at baseline : not overweight or obesity, overweight or obese; country : middle-income countries, high-income countries). If a minimum of 2 studies (data available) was included in each group, we would further conduct sub-group analyses to investigate whether intervention effectiveness differed within sub-groups.
Assessment of publication bias
We assessed the possibility of publication bias by drawing funnel plots. We recognized that asymmetry of funnel plots can be due to publication bias or a genuine relationship between effect size and trial size. There were a minimum of 10 studies required for the meaningful interpretation of funnel plots. We also conducted Egger’s regression test to more definitely ascertain whether publication bias was present.
Literature screening
We identified 12,614 relevant records, and 2866 were excluded due to duplicates. The titles or abstracts of 9748 records were then screened and 456 full-text articles were further checked for their eligibility. Finally, 50 trials (involving 63,734 children) reported by 56 articles [ 9 , 12 , 13 , 14 , 15 , 16 , 17 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 ] that met the eligibility criteria were included in this review. The flowchart of screening process is presented in Fig. 1 . The list of excluded studies is shown in Additional file 1 : Table S8.
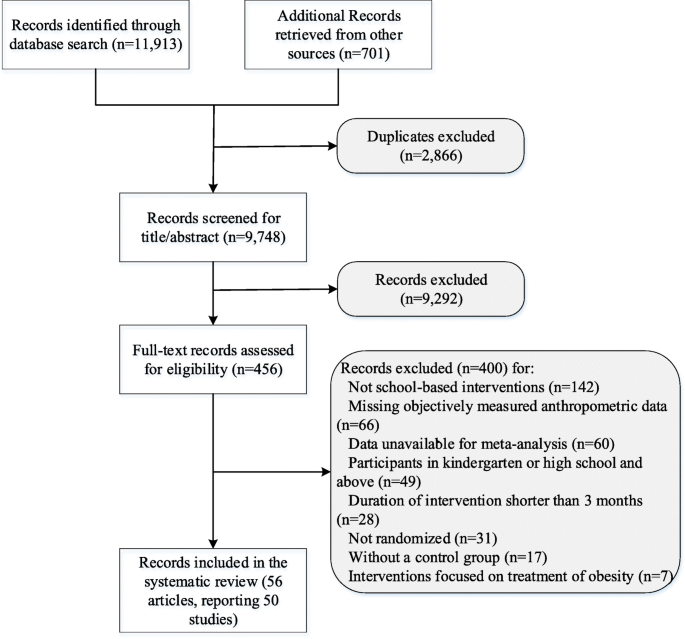
Study flow of the review
Characteristics of included trials
Characteristics of the included trials are demonstrated in Table 1 and Additional file 1 : Tables S1-S3. Most of them ( n = 47, 94%) were cluster RCTs using the school or class as the unit of randomization. All studies had one arm as the intervention group with exception of three studies [ 35 , 57 , 64 ]. All studies used usual practice controls except one using an active control, in order to mitigate the potential of the Hawthorne effect [ 13 ]. A large proportion of the studies were implemented in high-income countries ( n = 40, 80%). Most of them ( n = 43, 86.0%) were implemented exclusively in elementary schools (mean age: 8.1 years). The follow-up period of trials ranged from 3 months to 6 years, and more than half ( n = 32, 64%) of them maintained shorter than 12 months.
Thirty-five (70%) interventions were multi-component while others adopted single component. HE ( n = 7) or PA ( n = 7) was mostly used among single-component interventions. The combinations of components mostly used in multi-component interventions were PA + HE+/−SP ( n = 10; “+/−”: with or without), and PA + HE+DI+/−SP ( n = 8), followed by HE+DI+/−SP ( n = 7), HE+SP ( n = 5), PA + DI+/−SP ( n = 3), and PA + SP ( n = 2).
Assessment of risk of bias was summarized in Fig. 2 . Most of the trials ( n = 47, 98%) were assessed as having a low risk of bias in allocation concealment. And most of the trials ( n = 49, 98%) were judged as having a high risk of bias in blinding of participants and (or) personnel because it was usually not possible for interventions of this nature. Approximately half of the studies were assessed as having an unclear risk of bias due to insufficient descriptions in terms of random sequence generation ( n = 30, 60%), blinding of outcome assessment ( n = 25, 50.0%), incomplete outcome data ( n = 27, 54%) or the possibility of selective reporting ( n = 32, 64%).
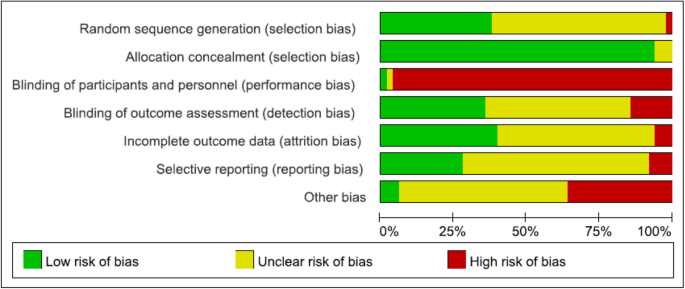
Risk of bias graph
Overall effect size
Overall effect size was summarized in Figs. 3 and 4 . The quantitative synthesis of the single-component interventions showed a significant, but small reduction of 0.14 (95% CI: 0.06, 0.21) kg/m 2 in BMI, and a small reduction of BMI Z-score (0.05, 95% CI: 0.01, 0.10) compared with the control group. For the multi-component interventions, the pooled results showed a significant, but mild reduction of 0.32 (0.09, 0.54) kg/m 2 in BMI, and 0.07 (0.001, 0.14) in BMI Z-score compared with the control group. Although the pooled effect sizes in BMI indices of multi-component interventions were slightly larger than that of single-component interventions, the differences were not statistically significant ( P = 0.41 for BMI, P = 0.71 for BMI Z-score).
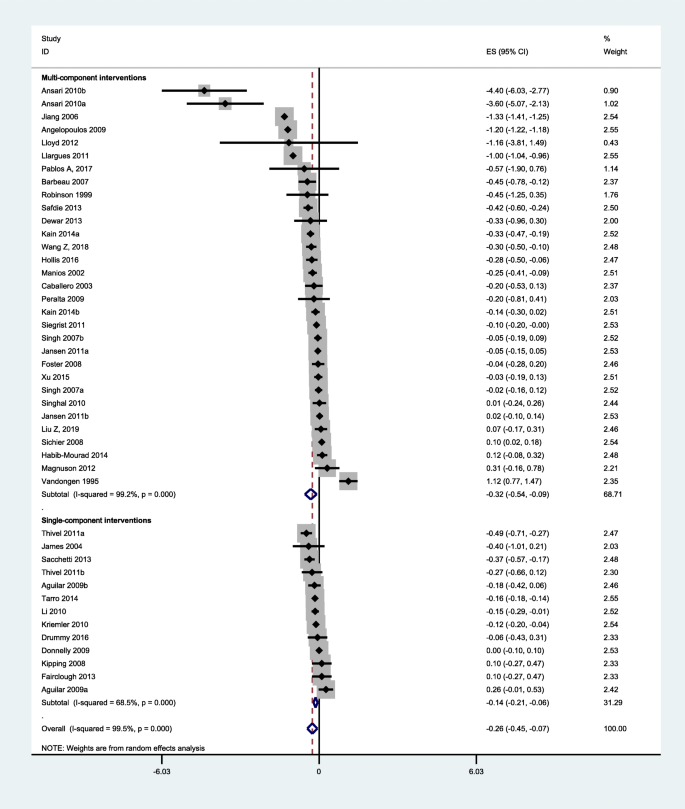
Pooled intervention effect (BMI)
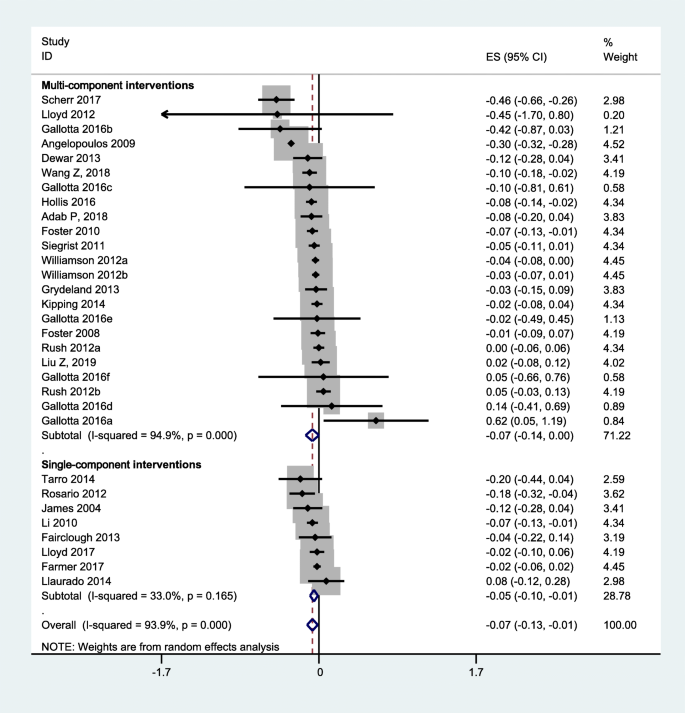
Pooled intervention effect (BMI Z-score)
Findings of overall effect size were robust to the exclusion of heterogeneous studies or studies of high risk of bias (Additional file 1 : Figures S1-S3). Results were also not significantly different across sex, weight status and country of the study population (Additional file 1 : Table S4).
Subgroup analyses showed that means of BMI differed significantly by whether or not studies including curricular PA sessions or emphasizing enjoyment in PA among single-component interventions (Table 2 ). The pooled BMI from single-component interventions including curricular PA ( n = 3) was − 0.30 (95% CI: − 0.51, − 0.10) kg/m 2 , while the effect size from single-component interventions not including curricular PA ( n = 4) was − 0.04 (95% CI: − 0.17, 0.09) kg/m 2 . The pooled BMI from interventions focusing on enjoyment of participants during PA ( n = 5) was − 0.19 (95% CI: − 0.33, − 0.05) kg/m 2 , while the effect size for interventions not emphasizing enjoyment of participants ( n = 2) was − 0.004 (95% CI: − 0.10, 0.09) kg/m 2 . The effect sizes did not differ significantly on other intervention characteristics among single-component interventions ( P > 0.05). Findings of subgroup analyses for single-component interventions were consistent with results from sensitivity analyses (Additional file 1 : Table S6).
Concerning multi-component interventions, subgroup analyses demonstrated that the mean BMI or BMI Z-score differed significantly by interventions emphasizing enjoyment in PA (Table 3 ); however, this difference was disappeared when excluding one heterogeneous study (Additional file 1 : Table S5). No significant differences in effect sizes ( P > 0.05) were detected between multi-component interventions with and without other intervention characteristics, which was consistent with results from sensitivity analyses (Additional file 1 : Table S5, S7).
As shown in Fig. 5 , the funnel plot of the observed effect showed a slightly asymmetric scatter consistent with publication bias, but P value for Egger’s regression test was larger than 0.05.
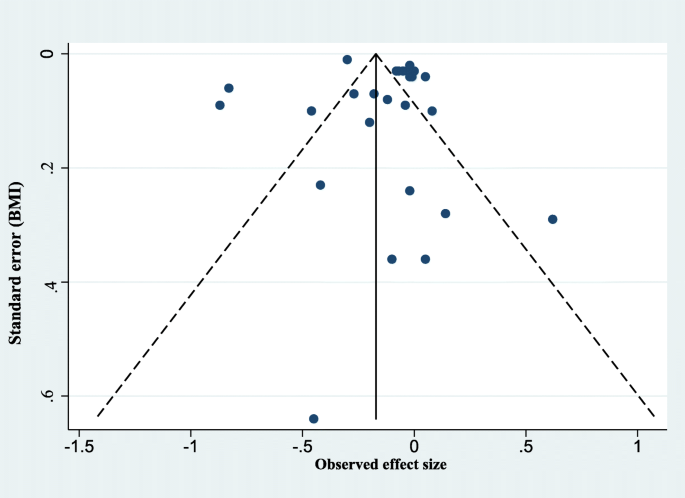
Assessment of publication bias: funnel plot
This review is one of the first to use meta-analyses and subgroup analyses to systematically review a number of more recent studies, and analyze the potentially effective characteristics of school-based interventions for preventing obesity.
Interpretation of the study findings
This review found that emphasizing enjoyment in PA sessions was critical for single-component (PA) interventions. This finding was echoed by previous reviews suggesting that lack of motivation and pleasure of physical activity was a barrier to physical activity for children [ 82 , 83 ]. Including curricular PA sessions was also found to be associated with improved efficacy of single-component (PA) interventions. This is, at least partly, explained by the fact that curricular PA sessions were usually led by physical education teachers, and thus intensity of exercise was superior to those including only extracurricular activities, after-school sessions or short activity breaks. Further, the curricular PA sessions were usually structured and compulsory for all children in a class and thus adherence could be relatively guaranteed. Significant associations between intervention components and efficacy were not consistently found in multi-component interventions. It is likely that multi-component interventions demonstrated to be effective were influenced by a combination of intervention components. The impact of combining components on intervention effectiveness should be the topic of further research.
For the current body of evidence, we did not find significant associations between dietary improvement components with improved intervention efficacy. This finding was consistent with another recent systematic review of school-based childhood obesity interventions [ 84 ]. The non-significant finding in relation to diet might be interpreted by poor adherence to diet intervention or the complex interplay of intervention components. We acknowledge that interaction analyses of intervention components (“intervention × component”) within individual studies would have provided a powerful method of understanding the complex interplay of intervention components. However, of the studies screened for this review, none reported such “intervention × component” analyses. Therefore, future obesity prevention interventions should address the specific interplay of intervention components, providing the possibility for further systematic reviews.
Findings of the study should also be interpreted in the context. The reporting of intervention characteristics (dose, frequency, and content) varied so much between trials that we were obliged to dichotomise it simply as “including the specific characteristics of component: yes/no” for the purpose of analysis, being nevertheless aware that resolution of the measure might be compromised in the process.
Comparison with other studies
Some previous reviews of obesity interventions have attempted to address the question of “what” (characteristics or components of interventions) really works for the targeted population [ 5 , 17 , 18 ], but only general findings were revealed. Further, research gaps remained in relation to the weakness of methods that were used (i.e., no comparisons between effective and non-effective trials; equal weighting of the included trials). The present review not only provided an update on a recent review [ 5 ] by including several new studies, but also identified the characteristics of effective interventions through meta-analyses and subgroup analyses. Thus, this review provides important and helpful evidence of the potentially effective intervention components with different characteristics.
Limitations and strengths of the study
Our results should be weighted cautiously considering the following limitations. First, the studies included in this review were restricted to English full-text publications found in three electronic databases. Second, the considerable level of heterogeneity was detected across studies in this review, which is relatively common among complex obesity interventions. Heterogeneity might be originated from the fidelity of the intervention and the population targeted among other factors. We have conducted sensitivity analyses to address this concern. Third, precisely evaluating the contents of some interventions is difficult and problematic due to inconsistent reporting. Future trials should be required to report interventions in accordance with TIDieR (template for intervention description and replication) [ 85 ] or other tools. Fourth, solely using BMI indices as outcome measures in this review is relatively narrow and insensitive, especially when studying PA interventions, as PA interventions might have an impact on BMI by affecting intermediate outcomes (increasing PA). We are planning to consider using behavioral outcomes in a future systematic review. Fifth, we only included RCTs in this review, which cannot address complex interplay of behaviors and real-world settings. However, RCTs are the best available approach to answer “can it work?”, as non-randomized trials might result in incomparable baseline data between the two groups, and uncontrolled trials can hardly eliminate the risk of self-selection bias. Sixth, due to the limited number of included studies as well as the limited sub-group data available for meta-analyses, we cannot investigate whether our findings of potentially effective intervention components were influenced by sex, weight status or socio-economic status of the study population. This is thus should be a potential focus for future trials, which provides a basis for the coming meta-analyses.
Despite these limitations, our study, based on a systematical review of the best available evidence from RCTs, took a first step towards distinguishing characteristics of effective school-based obesity prevention interventions. The findings of this review enable a better understanding of the effectiveness of complex school-based obesity prevention interventions. Specifically, the findings of this review suggest that school-based interventions could have significant effects on reducing students’ BMI. The effects of single-component (PA) interventions can be improved when emphasizing students’ enjoyment in physical activity, or including curricular PA sessions.
Overall, school-based interventions are effective in reducing excessive weight gain of children. Findings of this review increase our understandings of potentially effective characteristics of interventions. Future high-quality studies should focus more on the interplay of intervention components, which could deepen our understandings of the complexity of obesity prevention interventions delivered in school settings.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Body mass index
Confidence interval
Dietary improvement
Health education
Physical activity
Randomized controlled trial
Standard deviation
School policy
Template for intervention description and replication
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384:766–81.
Article PubMed PubMed Central Google Scholar
Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360:473–82.
Article PubMed Google Scholar
Braet C, Mervielde I, Vandereycken W. Psychological aspects of childhood obesity: a controlled study in a clinical and nonclinical sample. J Pediatr Psychol. 1997;22:59–71.
Article CAS PubMed Google Scholar
Twig G, Yaniv G, Levine H, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med. 2016;374:2430–40.
Bleich SN, Vercammen KA, Zatz LY, et al. Interventions to prevent global childhood overweight and obesity: a systematic review. Lancet Diabetes Endocrinol. 2018;6:332–46.
Kremers SP, de Bruijn GJ, Visscher TL, et al. Environmental influences on energy balance-related behaviors: a dual-process view. Int J Behav Nutr Phys Act. 2006;3:9.
Feng L, Wei DM, Lin ST, et al. Systematic review and meta-analysis of school-based obesity interventions in mainland China. PLoS One. 2017;12:e0184704.
Article CAS PubMed PubMed Central Google Scholar
Waters E, de Silva-Sanigorski A, Burford BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:CD001871.
Lloyd J, Creanor S, Logan S, et al. Effectiveness of the healthy lifestyles Programme (HeLP) to prevent obesity in UK primary-school children: a cluster randomised controlled trial. Lancet Child Adolesc Health. 2018;2:35–45.
Meyer U, Schindler C, Zahner L, et al. Long-term effect of a school-based physical activity program (KISS) on fitness and adiposity in children: a cluster-randomized controlled trial. PLoS One. 2014;9:e87929.
Marcus C, Nyberg G, Nordenfelt A, et al. A 4-year, cluster-randomized, controlled childhood obesity prevention study: STOPP. Int J Obes. 2009;33:408.
Article CAS Google Scholar
Aguilar FS, Martínez-Vizcaíno V, López MS, et al. Impact of an after-school physical activity program on obesity in children. J Pediatr. 2010;157:36–42.
Article Google Scholar
Sichieri R, Trotte AP, de Souza RA, et al. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public Health Nutr. 2009;12:197–202.
Scherr RE, Linnell JD, Dharmar M, et al. A multicomponent, school-based intervention, the shaping healthy choices program, improves nutrition-related outcomes. J Nutr Educ Behav. 2017;49:368–79.
Singh AS, Paw MJ, Brug J, et al. Short-term effects of school-based weight gain prevention among adolescents. Arch Pediatr Adolesc Med. 2007;161:565–71.
Robinson TN. Reducing children's television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–7.
Xu F, Ware RS, Leslie E, et al. Effectiveness of a randomized controlled lifestyle intervention to prevent obesity among Chinese primary school students: CLICK-obesity study. PLoS One. 2015;10:e0141421.
Katz DL, O’Connell M, Njike VY, et al. Strategies for the prevention and control of obesity in the school setting: systematic review and meta-analysis. Int J Obes. 2008;32:1780.
Martin J, Chater A, Lorencatto F. Effective behaviour change techniques in the prevention and management of childhood obesity. Int J Obes. 2013;37:1287.
Schippers M, Adam PC, Smolenski DJ, et al. A meta-analysis of overall effects of weight loss interventions delivered via mobile phones and effect size differences according to delivery mode, personal contact, and intervention intensity and duration. Obes Rev. 2017;18:450–9.
Kremers SP, Visscher TL, Brug J, et al. Netherlands research programme weight gain prevention (NHF-NRG): rationale, objectives and strategies. Eur J Clin Nutr. 2005;59:498.
Zahner L, Puder JJ, Roth R, et al. A school-based physical activity program to improve health and fitness in children aged 6–13 years (" kinder-Sportstudie KISS"): study design of a randomized controlled trial [ISRCTN15360785]. BMC Public Health. 2006;6:147.
DuBose KD, Mayo MS, Gibson CA, et al. Physical activity across the curriculum (PAAC): rationale and design. Contemp Clin Trials. 2008;29:83–93.
Williamson DA, Champagne CM, Harsha D, et al. Louisiana (LA) health: design and methods for a childhood obesity prevention program in rural schools. Contemp Clin Trials. 2008;29:783–95.
Giralt M, Albaladejo R, Tarro L, et al. A primary-school-based study to reduce prevalence of childhood obesity in Catalunya (Spain)-EDAL-Educació en alimentació: study protocol for a randomised controlled trial. Trials. 2011;12:54.
Lawlor DA, Jago R, Noble SM, et al. The active for life year 5 (AFLY5) school based cluster randomised controlled trial: study protocol for a randomized controlled trial. Trials. 2011;12:181.
Xu F, Ware RS, Tse LA, et al. A school-based comprehensive lifestyle intervention among chinese kids against obesity (CLICK-obesity): rationale, design and methodology of a randomized controlled trial in Nanjing city, China. BMC Public Health. 2012;12:316.
Sutherland R, Campbell E, Lubans DR, et al. A cluster randomised trial of a school-based intervention to prevent decline in adolescent physical activity levels: study protocol for the ‘physical activity 4 Everyone’trial. BMC Public Health. 2013;13:57.
Scherr RE, Linnell JD, Smith MH, et al. The shaping healthy choices program: design and implementation methodologies for a multicomponent, school-based nutrition education intervention. J Nutr Educ Behav. 2014;46:e13–21.
Lloyd J, Wyatt K. The healthy lifestyles Programme (HeLP)—an overview of and recommendations arising from the conceptualisation and development of an innovative approach to promoting healthy lifestyles for children and their families. Int J Environ Res Public Health. 2015;12:1003–19.
Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity. 2013;21:2422–8.
Farmer VL, Williams SM, Mann JI, et al. The effect of increasing risk and challenge in the school playground on physical activity and weight in children: a cluster randomised controlled trial (PLAY). Int J Obes. 2017;41:793.
Hollis JL, Sutherland R, Campbell L, et al. Effects of a ‘school-based’physical activity intervention on adiposity in adolescents from economically disadvantaged communities: secondary outcomes of the ‘physical activity 4 Everyone’RCT. Int J Obes. 2016;40:1486.
Gallotta MC, Iazzoni S, Emerenziani GP, et al. Effects of combined physical education and nutritional programs on schoolchildren’s healthy habits. PeerJ. 2016;4:e1880.
Drummy C, Murtagh EM, McKee DP, et al. The effect of a classroom activity break on physical activity levels and adiposity in primary school children. J Paediatr Child Health. 2016;52:745–9.
Creanor S, Lloyd J, Hillsdon M, et al. Detailed statistical analysis plan for a cluster randomised controlled trial of the healthy lifestyles Programme (HeLP), a novel school-based intervention to prevent obesity in school children. Trials. 2016;17:599.
Kain J, Concha F, Moreno L, et al. School-based obesity prevention intervention in Chilean children: effective in controlling, but not reducing obesity. J Obes. 2014;2014:618293.
Tarro L, Llauradó E, Albaladejo R, et al. A primary-school-based study to reduce the prevalence of childhood obesity–the EdAl (Educació en Alimentació) study: a randomized controlled trial. Trials. 2014;15:58.
Safdie M, Jennings-Aburto N, Lévesque L, et al. Impact of a school-based intervention program on obesity risk factors in Mexican children. Salud Publica Mex. 2013;55:374–87.
PubMed Google Scholar
Habib-Mourad C, Ghandour LA, Moore HJ, et al. Promoting healthy eating and physical activity among school children: findings from Health-E-PALS, the first pilot intervention from Lebanon. BMC Public Health. 2014;14:940.
Dewar DL, Morgan PJ, Plotnikoff RC, et al. The nutrition and enjoyable activity for teen girls study: a cluster randomized controlled trial. Am J Prev Med. 2013;45:313–7.
Jansen W, Borsboom G, Meima A, et al. Effectiveness of a primary school-based intervention to reduce overweight. Int J Pediatr Obes. 2011;6:e70–7.
Siegrist M, Hanssen H, Lammel C, et al. Effects of the school-based intervention programme JuvenTUM 3 on physical fitness, physical activity, and the prevalence of overweight. Eur J Prev Cardiolog. 2012;19:S2.
Google Scholar
Thivel D, Isacco L, Lazaar N, et al. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur J Pediatr. 2011;170:1435–43.
Group HS, Foster GD, Linder B, et al. A school-based intervention for diabetes risk reduction. N Engl J Med. 2010;363:1769.
Angelopoulos PD, Milionis HJ, Grammatikaki E, et al. Changes in BMI and blood pressure after a school based intervention: the CHILDREN study. Eur J Pub Health. 2009;19:319–25.
Vizcaíno VM, Aguilar FS, Gutiérrez RF, et al. Assessment of an after-school physical activity program to prevent obesity among 9-to 10-year-old children: a cluster randomized trial. Int J Obes. 2008;32:12.
Donnelly JE, Greene JL, Gibson CA, et al. Physical activity across the curriculum (PAAC): a randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med. 2009;49:336–41.
Barbeau P, Johnson MH, Howe CA, et al. Ten months of exercise improves general and visceral adiposity, bone, and fitness in black girls. Obesity. 2007;15:2077–85.
Caballero B, Clay T, Davis SM, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–8.
Foster GD, Sherman S, Borradaile KE, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121:e794–802.
Jiang J, Xia X, Greiner T, et al. The effects of a 3-year obesity intervention in schoolchildren in Beijing. Child Care Health Dev. 2007;33:641–6.
Li YP, Hu XQ, Schouten EG, et al. Report on childhood obesity in China (8): effects and sustainability of physical activity intervention on body composition of Chinese youth. Biomed Environ Sci. 2010;23:180–7.
Singhal N, Misra A, Shah P, et al. Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. Eur J Clin Nutr. 2010;64:364.
Peralta LR, Jones RA, Okely AD. Promoting healthy lifestyles among adolescent boys: the fitness improvement and lifestyle awareness program RCT. Prev Med. 2009;48:537–42.
Vandongen R, Jenner DA, Thompson C, et al. A controlled evaluation of a fitness and nutrition intervention program on cardiovascular health in 10-year-old to 12-year-old children. Prev Med. 1995;24:9–22.
El Ansari W, El Ashker S, Moseley L. Associations between physical activity and health parameters in adolescent pupils in Egypt. Int J Environ Res Public Health. 2010;7:1649–69.
Manios Y, Moschandreas J, Hatzis C, et al. Health and nutrition education in primary schools of Crete: changes in chronic disease risk factors following a 6-year intervention programme. Br J Nutr. 2002;88:315–24.
Kafatos A, Manios Y, Moschandreas J. Health and nutrition education in primary schools of Crete: follow-up changes in body mass index and overweight status. Eur J Clin Nutr. 2005;59:1090.
Kipping RR, Payne C, Lawlor DA. Randomised controlled trial adapting US school obesity prevention to England. Arch Dis Child. 2008;93:469–73.
James J, Thomas P, Cavan D, et al. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ. 2004;328:1237.
James J, Thomas P, Kerr D. Preventing childhood obesity: two year follow-up results from the Christchurch obesity prevention programme in schools (CHOPPS). BMJ. 2007;335:762.
Williamson DA, Champagne CM, Harsha DW, et al. Effect of an environmental school-based obesity prevention program on changes in body fat and body weight: a randomized trial. Obesity. 2012;20:1653–61.
Lloyd JJ, Wyatt KM, Creanor S. Behavioural and weight status outcomes from an exploratory trial of the healthy lifestyles Programme (HeLP): a novel school-based obesity prevention programme. BMJ Open. 2012;2:e000390.
Llargues E, Franco R, Recasens A, et al. Assessment of a school-based intervention in eating habits and physical activity in school children: the AVall study. J Epidemiol Community Health. 2011;65:896.
Llargués E, Recasens A, Franco R, et al. Medium-term evaluation of an educational intervention on dietary and physical exercise habits in schoolchildren: the Avall 2 study. Endocrinol Nutr. 2012;59:288–95.
Magnusson KT, Hrafnkelsson H, Sigurgeirsson I, et al. Limited effects of a 2-year school-based physical activity intervention on body composition and cardiorespiratory fitness in 7-year-old children. Health Educ Res. 2012;27:484.
Fairclough SJ, Hackett AF, Davies IG, et al. Promoting healthy weight in primary school children through physical activity and nutrition education: a pragmatic evaluation of the CHANGE! Randomised intervention study. BMC Public Health. 2013;13:626.
Rosário R, Oliveira B, Araújo A, et al. The impact of an intervention taught by trained teachers on childhood overweight. Int J Environ Res Public Health. 2012;9:1355–67.
Rush E, Reed P, Mclennan S, et al. A school-based obesity control programme: project energize. Two-year outcomes. Br J Nutr. 2012;107:581.
Grydeland M, Bjelland M, Anderssen SA, et al. Effects of a 20-month cluster randomised controlled school-based intervention trial on BMI of school-aged boys and girls: the HEIA study. Br J Sports Med. 2014;48:768–73.
Grydeland M, Bergh IH, Bjelland M, et al. Intervention effects on physical activity: the HEIA study - a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:17.
Sacchetti R, Ceciliani A, Garulli A, et al. Effects of a 2-year school-based intervention of enhanced physical education in the primary school. J Sch Health. 2013;83:639–46.
Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785.
Llauradó E, Tarro L, Moriña D, et al. EdAl-2 (Educacio en Alimentacio) programme: reproducibility of a cluster randomised, interventional, primary-school-based study to induce healthier lifestyle activities in children. BMJ Open. 2014;4:e005496.
Kipping RR, Howe LD, Jago R, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: active for life year 5 (AFLY5) school based cluster randomised controlled trial. BMJ. 2014;348:g3256.
Adab P, Pallan MJ, Lancashire ER, et al. Effectiveness of a childhood obesity prevention programme delivered through schools, targeting 6 and 7 year olds: cluster randomised controlled trial (WAVES study). BMJ. 2018;360:k211.
Pablos A, Nebot V, Vañó-Vicent V, et al. Effectiveness of a school-based program focusing on diet and health habits taught through physical exercise. Appl Physiol Nutr Metab. 2018;43:331–7.
Wang Z, Xu F, Ye Q, et al. Childhood obesity prevention through a community-based cluster randomized controlled physical activity intervention among schools in China: the health legacy project of the 2 nd world summer youth olympic games (YOG-obesity study). Int J Obes. 2018;42:625–33.
Liu Z, Li Q, Maddison R, et al. A school-based comprehensive intervention for childhood obesity in China: a cluster randomized controlled trial. Child Obes. 2019;15(2):105–15.
Kebbe M, Damanhoury S, Browne N, et al. Barriers to and enablers of healthy lifestyle behaviours in adolescents with obesity: a scoping review and stakeholder consultation. Obes Rev. 2017;18:1439–53.
Zabinski MF, Saelens BE, Stein RI, et al. Overweight children's barriers to and support for physical activity. Obes Res. 2003;11:238–46.
Brown T, Moore TH, Hooper L, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2019;Cd001871.
Hoffmann TC, Glaszlou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687.
Download references
Acknowledgments
We thank all the members in our research team.
This work was supported by National Key R&D Program of China (2016YFC1300204), National Natural Science Fund (81703240; 81903343) and Postdoctoral Research Foundation of China (2019 M650391).
Author information
Zheng Liu and Han-Meng Xu contributed equally to this work.
Authors and Affiliations
Department of Maternal and Child Health, School of Public Health, Peking University, Beijing, China
Zheng Liu, Han-Meng Xu, Yuan-Zhou Peng, Li-Zi Lin, Shuang Zhou, Wen-Hao Li & Hai-Jun Wang
School of Public Health, Sydney Medical School, University of Sydney, Sydney, Australia
Li-Ming Wen
You can also search for this author in PubMed Google Scholar
Contributions
ZL and HMX contributed equally and are considered co-first authors. Study design: HJW and ZL; Study selection: ZL, HMX, YZP and LZL; Data extraction: HMX, ZL; Quality assessment: HMX, ZL; Data analysis: ZL, HMX, LMW, YZP, LZL, SZ, WHL, HJW; Drafting of the manuscript: ZL, HMX, LMW, YZP, LZL, SZ, WHL, HJW; Critical revision of the manuscript for important intellectual content: HJW, LMW. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Hai-Jun Wang .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:.
Table S1. Description of the included trials. Table S2. Description of the characteristics of the PA component for the included studies. Table S3. Description of the characteristics of the DI component for the included studies. Table S4. Differences of overall effect size by sex, weight status and country of the study population. Table S5. Subgroup analyses by characteristics of multi-component interventions (excluding heterogeneous studies). Table S6. Subgroup analyses by characteristics of single-component interventions (excluding trials assessed as high risk of bias). Table S7. Subgroup analyses by characteristics of multi-component interventions (excluding trials assessed as high risk of bias). Table S8. The list of excluded studies. Figure S1. Pooled intervention effect after excluding heterogeneous studies (BMI). Figure S2. Pooled intervention effect after excluding studies at high risk of bias (BMI). Figure S3. Pooled intervention effect after excluding studies at high risk of bias (BMI Z-score).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Liu, Z., Xu, HM., Wen, LM. et al. A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int J Behav Nutr Phys Act 16 , 95 (2019). https://doi.org/10.1186/s12966-019-0848-8
Download citation
Received : 22 January 2019
Accepted : 16 September 2019
Published : 29 October 2019
DOI : https://doi.org/10.1186/s12966-019-0848-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
- Meta-analysis
International Journal of Behavioral Nutrition and Physical Activity
ISSN: 1479-5868
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 13 August 2022
Overview of systematic reviews of health interventions that aim to prevent and treat overweight and obesity among children
- Edgar Denova-Gutiérrez 1 ,
- Lucía Méndez-Sánchez 2 ,
- Berenice Araiza-Nava 2 ,
- Alejandra González-Rocha 1 ,
- Teresa Shamah 3 ,
- Anabelle Bonvechio 1 ,
- Simón Barquera 1 &
- Juan Rivera 1
Systematic Reviews volume 11 , Article number: 168 ( 2022 ) Cite this article
3237 Accesses
2 Citations
17 Altmetric
Metrics details
Childhood overweight and obesity is a global public health issue. Although there is evidence of a reduced prevalence in some countries, there is still much controversy about the efficacy of health interventions that aim to prevent and treat obesity in this specific population. The objective of the present study is to develop an overview of systematic reviews (OSRs) that assesses the effects of school-based, family, and multi-component health interventions for the prevention and treatment of obesity, change in physical activity, dietary, and/or hydration behaviors, and change in metabolic risk factors in school-aged children.
This protocol was developed using the methodology proposed by Cochrane. It outlines a comprehensive search in 12 electronic databases to identify systematic reviews of health interventions, including studies that evaluate and how to prevent and/or treat overweight and/or obesity in children aged 6 to 12 years. The risk of bias of the included Systematic Reviews will be assessed with the ROBIS tool.
Since the OSRs methodology’s purpose is only to harmonize evidence from open access publications, ethical consent is not necessary for the present protocol. In terms of diffusion, a paper will be submitted for publication in a scientific journal to describe the main results obtained through the OSRs.
Trial registration
The present overview of the systematic review protocol has been registered in PROSPERO (ID number 218296).
Peer Review reports
Childhood obesity is a global public health problem. Since 1975, epidemiological statistics indicate that this problem has nearly tripled worldwide [ 1 ]. In 2016, over 340 million children and adolescents (5–19 years) were overweight or obese, and this disease has risen dramatically from 4 to 18% in the last three decades [ 1 ]. The rate of increase childhood obesity in many countries is alarmingly greater than the rate in adults, even though the prevalence of obesity in this population is projected to be lower than the adult prevalence [ 2 ]. These trends are expected to continue if no radical actions to tackle the epidemic are implemented.
Obesity in childhood can pose an imminent threat to children’s health as it has been associated with multiple metabolic conditions (i.e., hyperlipidemia, hypertension, and abnormal glucose tolerance, as well as other illnesses) [ 3 , 4 ]. In addition, psychological issues (i.e. attention deficit, impaired educational attainment, and hyperactivity disorder) and social stigmatization can affect children who live with obesity, impacting their physical and mental health [ 5 ]. It can also have substantial long-term health consequences into adulthood. Hence, the risk of having obesity as an adult is double for children with obesity compared to those who do not have this condition. Furthermore, they have a greater risk of experiencing more severe health outcomes, such as hypertension, type 2 diabetes, and cardiovascular diseases, among others [ 6 , 7 ].
Schools are conducive settings for the promotion of healthy behavior; thus, there great interest in school-based interventions for the prevention of childhood obesity, and the proof is the high volume of related evidence produced in the last years. Bahia et al. 2019 [ 8 ] recognized this high volume of research in the field as an obstacle for decision-makers, so they conducted an overview of systematic reviews (OSR) to try and clarify the available evidence through a meta-analysis of health interventions in children and adolescents. They found six systematic reviews (SRs) of interventions aimed at prevention, 17 for treatment, and one with mixed interventions (prevention and treatment); only four of these were considered to be of high quality. The outcomes assessed were weight, body mass index Z -score (BMI Z -score), fat content, fat distribution, anthropometric measures, dietary behavior, sedentary behavior, physical activity behavior, and cardiovascular risk factors. Prevention interventions did not show any significant effect on BMI Z -score when compared with control, but nutritional education, TV screen time, and physical activity did produce modest short-term weight reduction. Treatment interventions such as diet, physical activity promotion, supervised exercise, lifestyle, or multi-component interventions (including different interventions such as diet, physical activity, education, the use of digital technologies for public health “m-health”, in different settings such as school, family or the community), and school-based education in ten SRs were associated with a reduction in the main outcomes. Mixed interventions for treatment showed improvements in BMI Z -score, but these were not consistent across the reviews. These OSRs describe great heterogeneity and low quality of primary studies reported by the SRs authors, stating the need to combine different approaches across settings to effectively control the obesity epidemic. Amini et al. 2015 [ 9 ] also tried to summarize the existing SRs evidence on the effect of school-based interventions to control childhood obesity. They concluded that multi-component interventions appear to be superior to single ones in terms of adiposity reduction, but differences must be considered by sex, psychological, physiological, and cultural aspects. Also, these OSRs report that sustainability and evaluation of adverse or unwanted effects are essential in the study of effectiveness. Bussiek et al. 2018 [ 10 ] also developed an OSRs protocol to summarize the existing evidence in child and adolescent prevention interventions, with changes in behaviors and the BMI Z -score as the main outcomes. One of the issues surrounding OSRs is that the methodology for its development is currently vague, even though there have been efforts to clarify it [ 11 , 12 , 13 , 14 , 15 ]. Ells et al. presented an OSRs for children and adolescents, part of their findings is the vast majority presented lifestyle interventions (141/163 trials), showing us the opportunity to look deeper into those kinds of interventions [ 16 ]. Also, recently a position paper based on an umbrella review, about the interventions and prevention of pediatric obesity and overweight, suggest prevention from the school interventions and regulated screen time for children (6–12 years) but it is necessary deep information about the interventions and focus on this age group [ 17 , 18 ].
OSRs would allow us to provide a general view of a public health problem that is widely studied by the scientific community and facilitate the decision-making process, also guiding future research. Conducting an OSRs with a focus on a specific group of age gives the opportunity to deepen the interventions of prevention and treatment. Therefore, considering the advances that have been made in researching this topic, it is necessary to develop an OSR that identifies effective public health strategies to prevent and manage childhood obesity. It must also communicate the impact of unique and multi-component lifestyle interventions that consider socio-cultural and economic context, as well as the quality of the existing evidence. This could provide a comprehensive and non-fragmented view of the problem that enables researchers and policymakers to generate new, feasible approaches to address obesity in this population.
Thus, the present protocol for an Overview of Systematic Reviews provides a methodology to summarize systematic reviews that assess the effects of school-based, family, and multi-component health interventions to prevent and treat overweight and obesity among school-aged children.
This Overview of Systematic Reviews follows the methodology proposed by The Cochrane Collaboration [ 14 ]. Additionally, registration is in PROSPERO (ID number 218296). Two reviewers will be involved in pilot testing for the search strategy (DG-E, MS-L), independent screening by duplicate (MS-L, AN-B), selection, overlapping, and extraction process, also by duplicate (GR-A, AN-B).
Inclusion criteria for systematic reviews
SRs of interventions will be included. Studies evaluating health interventions to prevent and/or treat overweight and/or obesity in children aged 6 to 12 years will be considered. These interventions may be based in school, family, and primary care settings (including mixed settings). SRs that included controlled trials, non-randomized trials (aiming to detect health interventions in this age group), or interventions that evaluate public health policies applied in this population will be analyzed, and those clinical trials will be presented separately. To be considered, SRs must report at least one of the following outcomes: (a) a change in weight, (b) a change in BMI Z-score, (c) a change in body composition and anthropometric measures (i.e., body fat percent, waist circumference), (d) change in metabolic risk factors (i.e., blood pressure, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, and/or glucose), (e) change in physical activity, dietary and/or hydration behaviors, (f) psycho-social changes. For a study to be considered an SR it has to have: (1) perform a comprehensive literature search in at least three electronic databases; (2) utilize paired independent reviewers in multiple stages; (3) undergoes a critical assessment; and (4) complete a risk of bias assessment. Studies that do not comply with these characteristics will not be considered an SR. In addition, studies that do not include a stratified analysis of children from 6 to 12 years of age, that carry out pharmacological or surgical interventions will be excluded from this overview.
Search methods to identify reviews
Previously validated search strategies, which are shown in Table 1 , will be used to perform the search for SRs in electronic databases, also, different terms will be used as adapted per database for example; (obesity) AND (overweight) AND (prevention) AND (treatment) AND (child) for PubMed. The electronic search will be conducted in the following databases; PubMed, Embase, The Cochrane Library, LILACs, CINAHL, PsycINFO, PROSPERO, OT Seeker, TripDatabase, DARE, Epistemonikos, and Health Interventions. Additionally, a manual search will be conducted for scanning references lists of the preview overviews, similar overviews and the included SRs. The search will be performed with no language restriction up until December 2021. The descriptors included will be obesity, overweight, treatment, and prevention. The results of these searches will be assessed by title and abstract by two independent reviewers [MS-L, AN-B], and all the relevant citations will be retrieved for full-text review. The same two independent reviewers will assess the full-text articles for potential inclusion. In the event of disagreement, a third author will decide whether or not to include the article (DG-E).
Data collection and analysis
Selection of reviews.
All relevant Cochrane and non-Cochrane SRs that match the previously mentioned criteria will be selected. The SRs selected for inclusion will be assessed to identify duplicate studies using a reference matrix (overlapping process) and the corrected area will be calculated following the proposed methods by Pieper et al. 2014 [ 15 ]. This method ensures that no outcome data is double-counted and that all outcome data from relevant SRs are included. The selection of the studies will be realized by an excel spreadsheet designed by the researchers that collaborate on this overview. As noted previously, a pilot testing was conducted and consensus meetings for disagreements.
Retrieved protocols will be checked for publication status and in specific cases, authors will be contacted to confirm the progress or publication status. When the scope of the included SRs is wider than ours, subsets of information regarding our target population (school-age children from 6–12 years old) or outcomes will be retrieved.
Data extraction and management
Data extraction will be performed independently by the two reviewers in a predefined platform, retrieving the following information: Author, year, the language of publication, date last assessed as up-to-date, objective, number of included studies, author’s information of the included primary studies, country of publication, the studied population, types of studies included, SR search strategies, names of databases searched in each SRs; date ranges of databases searched in each SRs; date of last search update in each SRs, participant characteristics such as age, sex, ethnicity, stage of the disease, co-morbidities; definition of disorder; type of intervention (s), time of application, frequency, intensity and dose, the follow-up time, setting, target population of the intervention (s), primary and secondary outcome (s), adverse events, the risk of bias of the included primary studies, quantitative outcomes data, the certainty of the evidence, limitations, conflicts of interest, and funding source.
Data analysis will be stratified by the objective of the health intervention, being either prevention and/or treatment. Subgroup analysis will be performed by the type of outcome measure and type of setting where the health intervention(s) is done. As the main goal is to present and describe the body of evidence currently available, all outcome data will be presented as extracted from the SRs, and no re-analysis will be performed.
Narrative summaries will be presented by the objective of the intervention (treatment or prevention) per SR, also, as summary tables of the findings of each SR. The health interventions will be categorized by their effectiveness or clinical importance as far as possible; with a summary table of findings as a preliminary synthesis of the included studies and identifying: (1) how the intervention works, (2) why, and (3) for who. To assess and report the certainty of the evidence found, the GRADE [ 19 ] assessments presented in the included systematic review will be extracted and reported. If the information is not available, it will be reported as not available data.
Assessment of methodological quality of included reviews
The assessment of the methodological quality of the included reviews will be performed independently by two reviewers using the ROBIS tool [ 20 ] and a summary developed with the same visualization tool. The three phases contemplated in the ROBIS tool will be assessed for each included SR using pre-formatted extraction forms, which will be presented in tables consensus meetings will be conducted between the researchers for discordant appraisals. Also, data on the risk of bias of each primary study contained in the included SRs will be extracted and presented as a summary by domain. Considering the possibility of having different instruments used in the primary studies, the results will be presented and summarized in a narrative and tabular form, classifying them by the type of instrument used for their assessment and the potential impact on the quality of the SR.
Recording the data
In order to extract the information, an outline was developed. The framework incorporates 11 categories to evaluate the full review articles included (Table 2 ). In order to guarantee that the outline is applied reliably by the two reviewers, it will be pilot tested by two members of the team on a subsample of the included studies. Following the data extraction outline, the same two researchers independently will record the data from each involved review study. Finally, if necessary, differences in extracted information will be discussed between the two reviewers until an agreement or by the mediation of a third reviewer of the team.
Since the OSRs methodology’s purpose is only to harmonize the evidence, ethical consent is not necessary for the present protocol. In terms of diffusion, a paper will be submitted for publication in a scientific journal to describe the main results obtained through the OSRs. The products of the OSRs will offer a widespread overview of effective interventions to prevent or treat overweight or obesity in children and emphasize areas where data is debatable or absent. This study will have some strengths; first, the exhausted search will be conducted in several databases and citation searching. Second, an assessment of the quality of the review with a validated tool will be conducted. There might be limitations; for example, the study will be specific for interventions in scholarly children between 6 and 12 years, those studies that include a population from 0 to 18 years old will be missing. It will also provide health professionals and policymakers with crucial evidence for designing, financing, and delivering evidence-based interventions.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
Overview of systematic reviews
Systematic reviews
Body mass index Z -score
World Health Organization. Obesity and overweight - fact sheet [internet]: World Health Organization; 2020. Accessed Sep 2020: http://www.who.int/mediacentre/factsheets/fs311/en/
Afshin A, Forouzanfar MH, Reitsma MB, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Article Google Scholar
Dietz W. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–25.
Article CAS Google Scholar
Pulgarón ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther. 2013;35:A18–32.
Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5:4–85.
Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876–85.
Engeland A, Bjørge T, Tverdal A, Søgaard AJ. Obesity in adolescence and adulthood and the risk of adult mortality. Epidemiology. 2004;15:79–85.
Bahia L, Schaan CW, Sparrenberger K, De Azevedo AG, Barufaldi LA, Coutinho W, et al. Overview of meta-analysis on prevention and treatment of childhood obesity. J Pediatr. 2019;95(4):385–400.
Amini M, Djazayery A, Majdzadeh R, Taghdisi M-H, Jazayeri S. Effect of school-based interventions to control childhood obesity: a review of reviews. Int J Prev Med. 2015;6:68.
Bussiek PV, De Poli C, Bevan G. A scoping review protocol to map the evidence on interventions to prevent overweight and obesity in children. BMJ Open. 2018;8(2):e019311. https://doi.org/10.1136/bmjopen-2017-019311 .
Article PubMed PubMed Central Google Scholar
Hunt H, Pollock A, Campbell P, et al. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(39).
McKenzie JE, Brennan SE. Overviews of systematic reviews: great promise, greater challenge. Syst Rev. 2017;6(1):6–9.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29.
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of reviews | Cochrane Training [Internet]. [cited 2020 Jul 15]. Available from: https://training.cochrane.org/handbook/current/chapter-v
Pieper D, Antoine SL, Mathes T, Neugebauer EAM, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Ells LJ, Rees K, Brown T, Mead E, Al-Khudairy L, Azevedo L, et al. Interventions for treating children and adolescents with overweight and obesity: an overview of Cochrane reviews. Int J Obes. 2018;42(11):1823–33.
Hoelscher DM, Brann LS, O'Brien S, Handu D, Rozga M. Prevention of pediatric overweight and obesity: position of the academy of nutrition and dietetics based on an umbrella review of systematic reviews. J Acad Nutr Diet. 2022;122(2):410–423.e6.
Kirk S, Ogata B, Wichert E, Handu D, Rozga M. Treatment of pediatric overweight and obesity: position of the academy of nutrition and dietetics based on an umbrella review of systematic reviews. J Acad Nutr Diet. 2022;18:S2212-2672(22)00039-9.
Google Scholar
Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013: The GRADE Working Group; 2013. Available from guidelinedevelopment.org/handbook
Whiting P, Savović J, Higgins JP, Caldwell DM, Reeves BC, Shea B, et al. ROBIS group. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Download references
This work was supported by [Fundación Gonzalo Río Arronte], grant number [S680] and the [Consejo Nacional de Ciencia y Tecnología], grant number [FOSISS-CONACYT 290382].
Author information
Authors and affiliations.
Nutrition and Health Research Center, National Institute of Public Health, Cuernavaca, Mexico
Edgar Denova-Gutiérrez, Alejandra González-Rocha, Anabelle Bonvechio, Simón Barquera & Juan Rivera
Clinical Epidemiology Research Unit, Hospital Infantil de Mexico Federico Gomez, Faculty of Medicine of National Autonomous University of Mexico (Universidad Nacional Autónoma de México), Mexico City, Mexico
Lucía Méndez-Sánchez & Berenice Araiza-Nava
Center for Research in Evaluation and Surveys, National Institute of Public Health, Cuernavaca, Mexico
Teresa Shamah
You can also search for this author in PubMed Google Scholar
Contributions
JR, SB, and ED-G, developed the research question; ED-G, LM-S, and BA-N, formulated the idea of the overview of systematic reviews and develop the methods section. ED-G and LM-S wrote the first version of the manuscript. TS, AB, SB, AG-R, and JR participated considerably in the designing and editing of the manuscript; ED-G, LM-S, BA-N, TS, AB, AG-R, SB, and JR, read and approved the final version of the protocol.
Corresponding authors
Correspondence to Lucía Méndez-Sánchez or Juan Rivera .
Ethics declarations
Ethics approval and consent to participate.
No individuals were included in the present protocol of overview of systematic reviews.
Consent for publication
The present protocol does not contain any individual person’s data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Denova-Gutiérrez, E., Méndez-Sánchez, L., Araiza-Nava, B. et al. Overview of systematic reviews of health interventions that aim to prevent and treat overweight and obesity among children. Syst Rev 11 , 168 (2022). https://doi.org/10.1186/s13643-022-02047-7
Download citation
Received : 16 November 2020
Accepted : 03 August 2022
Published : 13 August 2022
DOI : https://doi.org/10.1186/s13643-022-02047-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Systematic review
- Health interventions
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Effectiveness of...
Effectiveness of weight management interventions for adults delivered in primary care: systematic review and meta-analysis of randomised controlled trials
- Related content
- Peer review
- Claire D Madigan , senior research associate 1 ,
- Henrietta E Graham , doctoral candidate 1 ,
- Elizabeth Sturgiss , NHMRC investigator 2 ,
- Victoria E Kettle , research associate 1 ,
- Kajal Gokal , senior research associate 1 ,
- Greg Biddle , research associate 1 ,
- Gemma M J Taylor , reader 3 ,
- Amanda J Daley , professor of behavioural medicine 1
- 1 Centre for Lifestyle Medicine and Behaviour (CLiMB), The School of Sport, Exercise and Health Sciences, Loughborough University, Loughborough LE11 3TU, UK
- 2 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
- 3 Department of Psychology, Addiction and Mental Health Group, University of Bath, Bath, UK
- Correspondence to: C D Madigan c.madigan{at}lboro.ac.uk (or @claire_wm and @lboroclimb on Twitter)
- Accepted 26 April 2022
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care.
Design Systematic review and meta-analysis of randomised controlled trials.
Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary care compared with no treatment, attention control, or minimal intervention and weight change at ≥12 months follow-up.
Data sources Trials from a previous systematic review were extracted and the search completed using the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021.
Data extraction and synthesis Two reviewers independently identified eligible studies, extracted data, and assessed risk of bias using the Cochrane risk of bias tool. Meta-analyses were conducted with random effects models, and a pooled mean difference for both weight (kg) and waist circumference (cm) were calculated.
Main outcome measures Primary outcome was weight change from baseline to 12 months. Secondary outcome was weight change from baseline to ≥24 months. Change in waist circumference was assessed at 12 months.
Results 34 trials were included: 14 were additional, from a previous review. 27 trials (n=8000) were included in the primary outcome of weight change at 12 month follow-up. The mean difference between the intervention and comparator groups at 12 months was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, P<0.001), favouring the intervention group. At ≥24 months (13 trials, n=5011) the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, P<0.001) favouring the intervention. The mean difference in waist circumference (18 trials, n=5288) was −2.5 cm (−3.2 to −1.8 cm, I 2 =69%, P<0.001) in favour of the intervention at 12 months.
Conclusions Behavioural weight management interventions for adults with obesity delivered in primary care are effective for weight loss and could be offered to members of the public.
Systematic review registration PROSPERO CRD42021275529.
Introduction
Obesity is associated with an increased risk of diseases such as cancer, type 2 diabetes, and heart disease, leading to early mortality. 1 2 3 More recently, obesity is a risk factor for worse outcomes with covid-19. 4 5 Because of this increased risk, health agencies and governments worldwide are focused on finding effective ways to help people lose weight. 6
Primary care is an ideal setting for delivering weight management services, and international guidelines recommend that doctors should opportunistically screen and encourage patients to lose weight. 7 8 On average, most people consult a primary care doctor four times yearly, providing opportunities for weight management interventions. 9 10 A systematic review of randomised controlled trials by LeBlanc et al identified behavioural interventions that could potentially be delivered in primary care, or involved referral of patients by primary care professionals, were effective for weight loss at 12-18 months follow-up (−2.4 kg, 95% confidence interval −2.9 to−1.9 kg). 11 However, this review included trials with interventions that the review authors considered directly transferrable to primary care, but not all interventions involved primary care practitioners. The review included interventions that were entirely delivered by university research employees, meaning implementation of these interventions might differ if offered in primary care, as has been the case in other implementation research of weight management interventions, where effects were smaller. 12 As many similar trials have been published after this review, an updated review would be useful to guide health policy.
We examined the effectiveness of weight loss interventions delivered in primary care on measures of body composition (weight and waist circumference). We also identified characteristics of effective weight management programmes for policy makers to consider.
This systematic review was registered on PROSPERO and is reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. 13 14
Eligibility criteria
We considered studies to be eligible for inclusion if they were randomised controlled trials, comprised adult participants (≥18 years), and evaluated behavioural weight management interventions delivered in primary care that focused on weight loss. A primary care setting was broadly defined as the first point of contact with the healthcare system, providing accessible, continued, comprehensive, and coordinated care, focused on long term health. 15 Delivery in primary care was defined as the majority of the intervention being delivered by medical and non-medical clinicians within the primary care setting. Table 1 lists the inclusion and exclusion criteria.
Study inclusion and exclusion criteria
- View inline
We extracted studies from the systematic review by LeBlanc et al that met our inclusion criteria. 11 We also searched the exclusions in this review because the researchers excluded interventions specifically for diabetes management, low quality trials, and only included studies from an Organisation for Economic Co-operation and Development country, limiting the scope of the findings.
We searched for studies in the Cochrane Central Register of Controlled Trials, Medline, PubMed, and PsychINFO from 1 January 2018 to 19 August 2021 (see supplementary file 1). Reference lists of previous reviews 16 17 18 19 20 21 and included trials were hand searched.
Data extraction
Results were uploaded to Covidence, 22 a software platform used for screening, and duplicates removed. Two independent reviewers screened study titles, abstracts, and full texts. Disagreements were discussed and resolved by a third reviewer. All decisions were recorded in Covidence, and reviewers were blinded to each other’s decisions. Covidence calculates proportionate agreement as a measure of inter-rater reliability, and data are reported separately by title or abstract screening and full text screening. One reviewer extracted data on study characteristics (see supplementary table 1) and two authors independently extracted data on weight outcomes. We contacted the authors of four included trials (from the updated search) for further information. 23 24 25 26
Outcomes, summary measures, and synthesis of results
The primary outcome was weight change from baseline to 12 months. Secondary outcomes were weight change from baseline to ≥24 months and from baseline to last follow-up (to include as many trials as possible), and waist circumference from baseline to 12 months. Supplementary file 2 details the prespecified subgroup analysis that we were unable to complete. The prespecified subgroup analyses that could be completed were type of healthcare professional who delivered the intervention, country, intensity of the intervention, and risk of bias rating.
Healthcare professional delivering intervention —From the data we were able to compare subgroups by type of healthcare professional: nurses, 24 26 27 28 general practitioners, 23 29 30 31 and non-medical practitioners (eg, health coaches). 32 33 34 35 36 37 38 39 Some of the interventions delivered by non-medical practitioners were supported, but not predominantly delivered, by GPs. Other interventions were delivered by a combination of several different practitioners—for example, it was not possible to determine whether a nurse or dietitian delivered the intervention. In the subgroup analysis of practitioner delivery, we refer to this group as “other.”
Country —We explored the effectiveness of interventions by country. Only countries with three or more trials were included in subgroup analyses (United Kingdom, United States, and Spain).
Intensity of interventions —As the median number of contacts was 12, we categorised intervention groups according to whether ≤11 or ≥12 contacts were required.
Risk of bias rating —Studies were classified as being at low, unclear, and high risk of bias. Risk of bias was explored as a potential influence on the results.
Meta-analyses
Meta-analyses were conducted using Review Manager 5.4. 40 As we expected the treatment effects to differ because of the diversity of intervention components and comparator conditions, we used random effects models. A pooled mean difference was calculated for each analysis, and variance in heterogeneity between studies was compared using the I 2 and τ 2 statistics. We generated funnel plots to evaluate small study effects. If more than two intervention groups existed, we divided the number of participants in the comparator group by the number of intervention groups and analysed each individually. Nine trials were cluster randomised controlled trials. The trials had adjusted their results for clustering, or adjustment had been made in the previous systematic review by LeBlanc et al. 11 One trial did not report change in weight by group. 26 We calculated the mean weight change and standard deviation using a standard formula, which imputes a correlation for the baseline and follow-up weights. 41 42 In a non-prespecified analysis, we conducted univariate and multivariable metaregression (in Stata) using a random effects model to examine the association between number of sessions and type of interventionalist on study effect estimates.
Risk of bias
Two authors independently assessed the risk of bias using the Cochrane risk of bias tool v2. 43 For incomplete outcome data we defined a high risk of bias as ≥20% attrition. Disagreements were resolved by discussion or consultation with a third author.
Patient and public involvement
The study idea was discussed with patients and members of the public. They were not, however, included in discussions about the design or conduct of the study.
The search identified 11 609 unique study titles or abstracts after duplicates were removed ( fig 1 ). After screening, 97 full text articles were assessed for eligibility. The proportionate agreement ranged from 0.94 to 1.0 for screening of titles or abstracts and was 0.84 for full text screening. Fourteen new trials met the inclusion criteria. Twenty one studies from the review by LeBlanc et al met our eligibility criteria and one study from another systematic review was considered eligible and included. 44 Some studies had follow-up studies (ie, two publications) that were found in both the second and the first search; hence the total number of trials was 34 and not 36. Of the 34 trials, 27 (n=8000 participants) were included in the primary outcome meta-analysis of weight change from baseline to 12 months, 13 (n=5011) in the secondary outcome from baseline to ≥24 months, and 30 (n=8938) in the secondary outcome for weight change from baseline to last follow-up. Baseline weight was accounted for in 18 of these trials, but in 14 24 26 29 30 31 32 44 45 46 47 48 49 50 51 it was unclear or the trials did not consider baseline weight. Eighteen trials (n=5288) were included in the analysis of change in waist circumference at 12 months.

Studies included in systematic review of effectiveness of behavioural weight management interventions in primary care. *Studies were merged in Covidence if they were from same trial
- Download figure
- Open in new tab
- Download powerpoint
Study characteristics
Included trials (see supplementary table 1) were individual randomised controlled trials (n=25) 24 25 26 27 28 29 32 33 34 35 38 39 41 44 45 46 47 50 51 52 53 54 55 56 59 or cluster randomised controlled trials (n=9). 23 30 31 36 37 48 49 57 58 Most were conducted in the US (n=14), 29 30 31 32 33 34 35 36 37 45 48 51 54 55 UK (n=7), 27 28 38 41 47 57 58 and Spain (n=4). 25 44 46 49 The median number of participants was 276 (range 50-864).
Four trials included only women (average 65.9% of women). 31 48 51 59 The mean BMI at baseline was 35.2 (SD 4.2) and mean age was 48 (SD 9.7) years. The interventions lasted between one session (with participants subsequently following the programme unassisted for three months) and several sessions over three years (median 12 months). The follow-up period ranged from 12 months to three years (median 12 months). Most trials excluded participants who had lost weight in the past six months and were taking drugs that affected weight.
Meta-analysis
Overall, 27 trials were included in the primary meta-analysis of weight change from baseline to 12 months. Three trials could not be included in the primary analysis as data on weight were only available at two and three years and not 12 months follow-up, but we included these trials in the secondary analyses of last follow-up and ≥24 months follow-up. 26 44 50 Four trials could not be included in the meta-analysis as they did not present data in a way that could be synthesised (ie, measures of dispersion). 25 52 53 58 The mean difference was −2.3 kg (95% confidence interval −3.0 to −1.6 kg, I 2 =88%, τ 2 =3.38; P<0.001) in favour of the intervention group ( fig 2 ). We found no evidence of publication bias (see supplementary fig 1). Absolute weight change was −3.7 (SD 6.1) kg in the intervention group and −1.4 (SD 5.5) kg in the comparator group.

Mean difference in weight at 12 months by weight management programme in primary care (intervention) or no treatment, different content, or minimal intervention (control). SD=standard deviation
Supplementary file 2 provides a summary of the main subgroup analyses.
Weight change
The mean difference in weight change at the last follow-up was −1.9 kg (95% confidence interval −2.5 to −1.3 kg, I 2 =81%, τ 2 =2.15; P<0.001). Absolute weight change was −3.2 (SD 6.4) kg in the intervention group and −1.2 (SD 6.0) kg in the comparator group (see supplementary figs 2 and 3).
At the 24 month follow-up the mean difference in weight change was −1.8 kg (−2.8 to −0.8 kg, I 2 =88%, τ 2 =3.13; P<0.001) (see supplementary fig 4). As the weight change data did not differ between the last follow-up and ≥24 months, we used the weight data from the last follow-up in subgroup analyses.
In subgroup analyses of type of interventionalist, differences were significant (P=0.005) between non-medical practitioners, GPs, nurses, and other people who delivered interventions (see supplementary fig 2).
Participants who had ≥12 contacts during interventions lost significantly more weight than those with fewer contacts (see supplementary fig 6). The association remained after adjustment for type of interventionalist.
Waist circumference
The mean difference in waist circumference was −2.5 cm (95% confidence interval −3.2 to −1.8 cm, I 2 =69%, τ 2 =1.73; P<0.001) in favour of the intervention at 12 months ( fig 3 ). Absolute changes were −3.7 cm (SD 7.8 cm) in the intervention group and −1.3 cm (SD 7.3) in the comparator group.

Mean difference in waist circumference at 12 months. SD=standard deviation
Risk of bias was considered to be low in nine trials, 24 33 34 35 39 41 47 55 56 unclear in 12 trials, 25 27 28 29 32 45 46 50 51 52 54 59 and high in 13 trials 23 26 30 31 36 37 38 44 48 49 53 57 58 ( fig 4 ). No significant (P=0.65) differences were found in subgroup analyses according to level of risk of bias from baseline to 12 months (see supplementary fig 7).

Risk of bias in included studies
Worldwide, governments are trying to find the most effective services to help people lose weight to improve the health of populations. We found weight management interventions delivered by primary care practitioners result in effective weight loss and reduction in waist circumference and these interventions should be considered part of the services offered to help people manage their weight. A greater number of contacts between patients and healthcare professionals led to more weight loss, and interventions should be designed to include at least 12 contacts (face-to-face or by telephone, or both). Evidence suggests that interventions delivered by non-medical practitioners were as effective as those delivered by GPs (both showed statistically significant weight loss). It is also possible that more contacts were made with non-medical interventionalists, which might partially explain this result, although the metaregression analysis suggested the effect remained after adjustment for type of interventionalist. Because most comparator groups had fewer contacts than intervention groups, it is not known whether the effects of the interventions are related to contact with interventionalists or to the content of the intervention itself.
Although we did not determine the costs of the programme, it is likely that interventions delivered by non-medical practitioners would be cheaper than GP and nurse led programmes. 41 Most of the interventions delivered by non-medical practitioners involved endorsement and supervision from GPs (ie, a recommendation or checking in to see how patients were progressing), and these should be considered when implementing these types of weight management interventions in primary care settings. Our findings suggest that a combination of practitioners would be most effective because GPs might not have the time for 12 consultations to support weight management.
Although the 2.3 kg greater weight loss in the intervention group may seem modest, just 2-5% in weight loss is associated with improvements in systolic blood pressure and glucose and triglyceride levels. 60 The confidence intervals suggest a potential range of weight loss and that these interventions might not provide as much benefit to those with a higher BMI. Patients might not find an average weight loss of 3.7 kg attractive, as many would prefer to lose more weight; explaining to patients the benefits of small weight losses to health would be important.
Strengths and limitations of this review
Our conclusions are based on a large sample of about 8000 participants, and 12 of these trials were published since 2018. It was occasionally difficult to distinguish who delivered the interventions and how they were implemented. We therefore made some assumptions at the screening stage about whether the interventionalists were primary care practitioners or if most of the interventions were delivered in primary care. These discussions were resolved by consensus. All included trials measured weight, and we excluded those that used self-reported data. Dropout rates are important in weight management interventions as those who do less well are less likely to be followed-up. We found that participants in trials with an attrition rate of 20% or more lost less weight and we are confident that those with high attrition rates have not inflated the results. Trials were mainly conducted in socially economic developed countries, so our findings might not be applicable to all countries. The meta-analyses showed statistically significant heterogeneity, and our prespecified subgroups analysis explained some, but not all, of the variance.
Comparison with other studies
The mean difference of −2.3 kg in favour of the intervention group at 12 months is similar to the findings in the review by LeBlanc et al, who reported a reduction of −2.4 kg in participants who received a weight management intervention in a range of settings, including primary care, universities, and the community. 11 61 This is important because the review by LeBlanc et al included interventions that were not exclusively conducted in primary care or by primary care practitioners. Trials conducted in university or hospital settings are not typically representative of primary care populations and are often more intensive than trials conducted in primary care as a result of less constraints on time. Thus, our review provides encouraging findings for the implementation of weight management interventions delivered in primary care. The findings are of a similar magnitude to those found in a trial by Ahern et al that tested primary care referral to a commercial programme, with a difference of −2.7 kg (95% confidence interval −3.9 to −1.5 kg) reported at 12 month follow-up. 62 The trial by Ahern et al also found a difference in waist circumference of −4.1 cm (95% confidence interval −5.5 to −2.3 cm) in favour of the intervention group at 12 months. Our finding was smaller at −2.5 cm (95% confidence interval −3.2 to −1.8 cm). Some evidence suggests clinical benefits from a reduction of 3 cm in waist circumference, particularly in decreased glucose levels, and the intervention groups showed a 3.7 cm absolute change in waist circumference. 63
Policy implications and conclusions
Weight management interventions delivered in primary care are effective and should be part of services offered to members of the public to help them manage weight. As about 39% of the world’s population is living with obesity, helping people to manage their weight is an enormous task. 64 Primary care offers good reach into the community as the first point of contact in the healthcare system and the remit to provide whole person care across the life course. 65 When developing weight management interventions, it is important to reflect on resource availability within primary care settings to ensure patients’ needs can be met within existing healthcare systems. 66
We did not examine the equity of interventions, but primary care interventions may offer an additional service and potentially help those who would not attend a programme delivered outside of primary care. Interventions should consist of 12 or more contacts, and these findings are based on a mixture of telephone and face-to-face sessions. Previous evidence suggests that GPs find it difficult to raise the issue of weight with patients and are pessimistic about the success of weight loss interventions. 67 Therefore, interventions should be implemented with appropriate training for primary care practitioners so that they feel confident about helping patients to manage their weight. 68
Unanswered questions and future research
A range of effective interventions are available in primary care settings to help people manage their weight, but we found substantial heterogeneity. It was beyond the scope of this systematic review to examine the specific components of the interventions that may be associated with greater weight loss, but this could be investigated by future research. We do not know whether these interventions are universally suitable and will decrease or increase health inequalities. As the data are most likely collected in trials, an individual patient meta-analysis is now needed to explore characteristics or factors that might explain the variance. Most of the interventions excluded people prescribed drugs that affect weight gain, such as antipsychotics, glucocorticoids, and some antidepressants. This population might benefit from help with managing their weight owing to the side effects of these drug classes on weight gain, although we do not know whether the weight management interventions we investigated would be effective in this population. 69
What is already known on this topic
Referral by primary care to behavioural weight management programmes is effective, but the effectiveness of weight management interventions delivered by primary care is not known
Systematic reviews have provided evidence for weight management interventions, but the latest review of primary care delivered interventions was published in 2014
Factors such as intensity and delivery mechanisms have not been investigated and could influence the effectiveness of weight management interventions delivered by primary care
What this study adds
Weight management interventions delivered by primary care are effective and can help patients to better manage their weight
At least 12 contacts (telephone or face to face) are needed to deliver weight management programmes in primary care
Some evidence suggests that weight loss after weight management interventions delivered by non-medical practitioners in primary care (often endorsed and supervised by doctors) is similar to that delivered by clinician led programmes
Ethics statements
Ethical approval.
Not required.
Data availability statement
Additional data are available in the supplementary files.
Contributors: CDM and AJD conceived the study, with support from ES. CDM conducted the search with support from HEG. CDM, AJD, ES, HEG, KG, GB, and VEK completed the screening and full text identification. CDM and VEK completed the risk of bias assessment. CDM extracted data for the primary outcome and study characteristics. HEJ, GB, and KG extracted primary outcome data. CDM completed the analysis in RevMan, and GMJT completed the metaregression analysis in Stata. CDM drafted the paper with AJD. All authors provided comments on the paper. CDM acts as guarantor. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: AJD is supported by a National Institute for Health and Care Research (NIHR) research professorship award. This research was supported by the NIHR Leicester Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. ES’s salary is supported by an investigator grant (National Health and Medical Research Council, Australia). GT is supported by a Cancer Research UK fellowship. The funders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/disclosure-of-interest/ and declare: This research was supported by the National Institute for Health and Care Research Leicester Biomedical Research Centre; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
The lead author (CDM) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported, and that no important aspects of the study have been omitted.
Dissemination to participants and related patient and public communities: We plan to disseminate these research findings to a wider community through press releases, featuring on the Centre for Lifestyle Medicine and Behaviour website ( www.lboro.ac.uk/research/climb/ ) via our policy networks, through social media platforms, and presentation at conferences.
Provenance and peer review: Not commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/ .
- Renehan AG ,
- Heller RF ,
- Bansback N ,
- Birmingham CL ,
- Abdullah A ,
- Peeters A ,
- de Courten M ,
- Stoelwinder J
- Aghili SMM ,
- Ebrahimpur M ,
- Arjmand B ,
- KETLAK Study Group
- ↵ Department of Health and Social Care. New specialised support to help those living with obesity to lose weight UK2021. www.gov.uk/government/news/new-specialised-support-to-help-those-living-with-obesity-to-lose-weight [accessed 08/02/2021].
- U.S. Preventive Services Task Force
- ↵ National Institute for Health and Care Excellence. Maintaining a Healthy Weight and Preventing Excess Weight Gain in Children and Adults. Cost Effectiveness Considerations from a Population Modelling Viewpoint. 2014, NICE. www.nice.org.uk/guidance/ng7/evidence/evidence-review-2-qualitative-evidence-review-of-the-most-acceptable-ways-to-communicate-information-about-individually-modifiable-behaviours-to-help-maintain-a-healthy-weight-or-prevent-excess-weigh-8733713.
- ↵ The Health Foundation. Use of primary care during the COVID-19 pandemic. 17/09/2020: The Health Foundation, 2020.
- ↵ Australian Bureau of Statistics. Patient Experiences in Australia: Summary of Findings, 2017-18. 2019 ed. Canberra, Australia, 2018. www.abs.gov.au/AUSSTATS/[email protected]/Lookup/4839.0Main+Features12017-18?OpenDocument.
- LeBlanc ES ,
- Patnode CD ,
- Webber EM ,
- Redmond N ,
- Rushkin M ,
- O’Connor EA
- Damschroder LJ ,
- Liberati A ,
- Tetzlaff J ,
- Altman DG ,
- PRISMA Group
- McKenzie JE ,
- Bossuyt PM ,
- ↵ WHO. Main terminology: World Health Organization; 2004. www.euro.who.int/en/health-topics/Health-systems/primary-health-care/main-terminology [accessed 09.12.21].
- Aceves-Martins M ,
- Robertson C ,
- REBALANCE team
- Glasziou P ,
- Isenring E ,
- Chisholm A ,
- Wakayama LN ,
- Kettle VE ,
- Madigan CD ,
- ↵ Covidence [program]. Melbourne, 2021.
- Welzel FD ,
- Carrington MJ ,
- Fernández-Ruiz VE ,
- Ramos-Morcillo AJ ,
- Solé-Agustí M ,
- Paniagua-Urbano JA ,
- Armero-Barranco D
- Bräutigam-Ewe M ,
- Hildingh C ,
- Yardley L ,
- Christian JG ,
- Bessesen DH ,
- Christian KK ,
- Goldstein MG ,
- Martin PD ,
- Dutton GR ,
- Horswell RL ,
- Brantley PJ
- Wadden TA ,
- Rogers MA ,
- Berkowitz RI ,
- Kumanyika SK ,
- Morales KH ,
- Allison KC ,
- Rozenblum R ,
- De La Cruz BA ,
- Katzmarzyk PT ,
- Martin CK ,
- Newton RL Jr . ,
- Nanchahal K ,
- Holdsworth E ,
- ↵ RevMan [program]. 5.4 version: Copenhagen, 2014.
- Sterne JAC ,
- Savović J ,
- Gomez-Huelgas R ,
- Jansen-Chaparro S ,
- Baca-Osorio AJ ,
- Mancera-Romero J ,
- Tinahones FJ ,
- Bernal-López MR
- Delahanty LM ,
- Tárraga Marcos ML ,
- Panisello Royo JM ,
- Carbayo Herencia JA ,
- Beeken RJ ,
- Leurent B ,
- Vickerstaff V ,
- Hagobian T ,
- Brannen A ,
- Rodriguez-Cristobal JJ ,
- Alonso-Villaverde C ,
- Panisello JM ,
- Conroy MB ,
- Spadaro KC ,
- Takasawa N ,
- Mashiyama Y ,
- Pritchard DA ,
- Hyndman J ,
- Jarjoura D ,
- Smucker W ,
- Baughman K ,
- Bennett GG ,
- Steinberg D ,
- Zaghloul H ,
- Chagoury O ,
- Leslie WS ,
- Barnes AC ,
- Summerbell CD ,
- Greenwood DC ,
- Huseinovic E ,
- Leu Agelii M ,
- Hellebö Johansson E ,
- Winkvist A ,
- Look AHEAD Research Group
- LeBlanc EL ,
- Wheeler GM ,
- Aveyard P ,
- de Koning L ,
- Chiuve SE ,
- Willett WC ,
- ↵ World Health Organization. Obesity and Overweight, 2021, www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Starfield B ,
- Sturgiss E ,
- Dewhurst A ,
- Devereux-Fitzgerald A ,
- Haesler E ,
- van Weel C ,
- Gulliford MC
- Fassbender JE ,
- Sarwer DB ,
- Brekke HK ,
- Search Menu
- Sign in through your institution
- Advance articles
- Themed Collections
- Editor's Choice
- Ilona Kickbusch Award
- Supplements
- Author Guidelines
- Submission Online
- Open Access Option
- Self-Archiving Policy
- About Health Promotion International
- Editorial Board
- Advertising and Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Lay summary, introduction, conclusions, supplementary material, acknowledgements, protocol and registration, conflict of interest.
- < Previous
Systematic review of the effectiveness of health promotion interventions targeting obesity prevention in school-based staff
- Article contents
- Figures & tables
- Supplementary Data
Amy Hill, Laura Alston, Cindy Needham, Anna Peeters, Anthony D LaMontagne, Melanie Nichols, Systematic review of the effectiveness of health promotion interventions targeting obesity prevention in school-based staff, Health Promotion International , Volume 37, Issue 3, June 2022, daac061, https://doi.org/10.1093/heapro/daac061
- Permissions Icon Permissions
School-based employee interventions can benefit the health of staff and have the potential to influence the health of school students through role-modelling. However, interventions within schools typically focus on students, with very few studies addressing obesity and related health behaviours among school staff. A systematic review of the peer-reviewed literature published between January 2000 and May 2020 was undertaken to synthesize the evidence on the impact that school-based obesity prevention programmes have on the staff they employ. Search terms were derived from four major topics: (i) school; (ii) staff; (iii) health promotion and (iv) obesity. Terms were adapted for six databases and three independent researchers screened results. Studies were included if they reported on the outcomes of body weight, dietary behaviours and/or physical activity. Of 3483 papers identified in the search, 13 studies met the inclusion criteria. All 13 studies included an intervention that focussed on improving nutrition, physical activity or both. All included studies demonstrated a positive outcome for either dietary intake, weight or body mass index or physical activity outcomes, however not all results were statistically significant. The included studies showed promising, although limited, impacts on employee health outcomes. This review demonstrated a lack of global focus and investment in interventions targeting school staff, particularly in contrast to the large amount of research on school-based health promotion initiatives focussed on students. There is a need for further research to understand effective interventions to promote health and prevent obesity in this large, diverse and influential workforce.
School-based health promotion interventions that focus on employees can benefit the health of staff and have the potential to also influence the health of school students through role-modelling. Most published intervention studies within schools have typically focussed on students, however, with very few studies addressing obesity and related health behaviours among school staff. This systematic review summarizes the evidence on the impact of school-based obesity prevention programmes on the outcomes of physical activity, weight or dietary practices of school staff. The search identified 13 relevant studies published since 2000. The findings of this review show that school staff focussed health promotion interventions can positively impact obesity-related outcomes. The small number of available studies, however, demonstrates a lack of research focus and investment in interventions targeting school staff and teachers’ health. The majority of included studies used relatively weak study designs and included small numbers of schools and staff members. This is particularly contrasting to the large body of research on school-based health promotion initiatives focussed on students. There is a need for further research to understand effective interventions to promote health and prevent obesity in this large, diverse and influential workforce.
The Global Burden of Disease Study estimated that obesity affected 2 billion people globally in 2015, imposing an economic burden of US $2.0 trillion in health care costs, mortality and permanent disability, slowed economic growth and lost productivity ( Tremmel et al. , 2017 ; Swinburn et al. , 2019 ). If current trends continue, it is estimated that more than half of the world’s population will meet the classifications of overweight and obesity by 2030, posing further significant risks to human health ( Kelly et al. , 2008 ). High quality evidence is needed to understand ways to address adult overweight and obesity that can deliver sustained population level benefits.
Workplaces are an important setting for health promotion, given that many adults spend a large proportion of their week in employment settings, and that poor health may lead to detrimental impacts not only for employees themselves, but also for productivity and organizational success ( Chalupka, 2011 ). Workplace health promotion interventions have been shown to be effective in relation to obesity prevention in various employment sectors, including health care settings, office-based workplaces and university settings ( Anderson et al. , 2009 ; Verweij et al. , 2011 ; Power et al. , 2014 ; Weerasekara et al. , 2016 ; Tam and Yeung, 2018 ; Proper and van Oostrom, 2019 ). A recent review of reviews on the effectiveness of workplace health promotion interventions that synthesized evidence from 23 reviews, found strong evidence for favourable impacts on weight-related outcomes and prevention of mental health disorders ( Proper and van Oostrom, 2019 ).
Despite published evidence on the effectiveness of health promotion interventions in various workplaces, little is known about their effectiveness when targeting school staff and the unique school workplace environment that is characterized by high job demands, busy workload and inflexibility of staff time ( Katz et al. , 2005 ).
Health promotion interventions focussed on the education sector have become of increasing interest for governments and policy makers given not only the potential for school employees’ own health benefits, but also the potential for school employees to be positive role-models of healthful behaviour for the children they teach and interact with ( Hartline-Grafton et al. , 2009 ; Snelling et al. , 2013 ; Herbert et al. , 2017 ). The World Health Organization’s Health Promoting Schools Framework further highlights the opportunities available through schools towards taking a whole of setting approach to obesity prevention ( World Health Organisation, 2017 ). A recent review of the framework demonstrated its effectiveness with regard to some weight-related and behavioural (diet and physical activity) contributors to obesity in children ( Langford et al. , 2014 ). However, the majority of studies only targeted school students, with little published evidence available on the effectiveness of obesity-related health promotion interventions for school staff ( Katz et al. , 2005 ).
The Australian school-based workforce comprises a diverse group of adults with a broad range of ages and ethnicities across all localities nationally ( Department of Education, 2014 ). The school-based workforce includes the categories of teaching staff (approximately 70% of the Australian school-based workforce), and non-teaching staff comprising specialist support staff, administrative and clerical staff (including teacher aides and assistants), building operations, general maintenance and other staff. In 2019, there were over 288 000 full-time equivalent (FTE) teaching staff and 132 000 FTE non-teaching staff employed in Australian schools, with over 3.9 million enrolled students ( Australian Bureau of Statistics, 2019 ).
A recent Australian study explored potential opportunities for schools to support healthy eating and physical activity amongst staff ( Huse et al. , 2020 ) and found that key barriers to school staff eating healthily and being physically active included lack of time and support for these behaviours and lack of necessary physical infrastructure in the workplace ( Huse et al. , 2020 ). Recommendations from this study included adopting a whole of school health promotion policy to support teachers to pursue healthier lifestyles and reduce workplace stress ( Huse et al. , 2020 ).
Given the potential that school-based interventions have for improving health, evidence synthesis with a specific focus on staff members health and wellbeing is needed in order to inform future interventions, health promotion programmes and research. We therefore sought to:
Synthesize the literature from quantitative studies reporting on the effectiveness of obesity prevention interventions for school staff; and
Identify the common characteristics of successful interventions.
Eligibility criteria
Studies were included if (i) they were published in English between 2000 and 2020; (ii) intervention participants were school staff (primary or secondary schools or equivalent), including teaching, administrative and leadership staff; (iii) the study included a health promotion intervention; (iv) the study design included a control group or before and after measures [i.e. randomized controlled trials (RCTs), quasi-experimental and non-randomized designs] and (v) outcome measures included at least one of; a measure of weight [including body mass index (BMI)], dietary behaviours and/or physical activity. Literature reviews, conference abstracts and editorials were excluded. The decision to include studies from the year 2000 onwards was made following initial trials of the search strategy where it was found that the majority of school-based health promotion literature was published after this date.
Search strategy
The search strategy was developed following a preliminary review of workplace and school-based health promotion interventions. The search was initially conducted on 25 March 2019 and updated on the 14 May 2020 to capture any new publications since initial search. The following databases were included in the search: Medline, CINAHL, EMBASE, Health and Society database (Informit), ERIC and Google Scholar; the search strategy was adjusted for each database and limited to original research published in peer-reviewed journals, published in the English language. The search strategy terms used and journal-specific syntax can be found in Supplementary Table 1 . Search terms included combinations, truncations and synonyms of the following: (i) ‘School OR Staff*’ OR teacher* OR employee* OR worker* OR workplace, (ii) Intervention* OR program* OR ‘health promotion’ OR prevent* OR strategy* OR initiative*, (iii) Diet* OR nutrition* OR eating OR consumption OR weight OR overweight OR obesity* OR ‘physical* activity’ OR ‘sedentary behaviour’ OR exercise. Additional articles were identified via a manual search of reference lists.
Study selection
Search results were extracted from databases into Endnote X9 (Clarivate Analytics, USA). Results were then loaded into systematic review software Covidence (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia), and three reviewers independently screened titles and abstracts using a pre-determined eligibility assessment form. Full texts of all articles included after title and abstract screening were also each reviewed by two reviewers. Any discrepancies through the review process were adjudicated by a senior researcher and resolved by consensus discussion.
Data extraction
Data extraction was completed by the lead researcher; with data from a 10% subsample ( n = 3) of papers extracted by a second reviewer which were checked for agreement which was achieved. Key study characteristics were identified and extracted into a pre-determined data extraction form to enable identification of prominent and recurrent themes. The following data were extracted: author, year of publication; type of school (i.e. primary/elementary, secondary); country; study design; participants (i.e. teachers, administration staff); intervention strategies; intervention timeframe; outcome measures; results; conclusions. The detailed data extraction results can be found in Supplementary Table 2 .
Data synthesis and analysis
The key characteristics of the included studies were summarized from the information collected in the data extraction form. The primary outcomes of interest were statistically significant changes in diet, physical activity or unhealthy weight measures among school staff as a result of the school-based intervention. Where possible, for all study arms, the mean or median of primary outcome measures was recorded at baseline, post-intervention and any additional follow-up(s). Measures of error were standard error or SD and associated p values for change between or within groups at follow-up(s), and over time were recorded if available. The diverse characteristics of included studies precluded a meta-analysis, with variation in study design, outcome measures and intervention strategies.
Quality assessment
Following data extraction, assessment of methodological quality of included studies was undertaken using the Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group ( National Heart Lung and Blood Institute, 2020 ). Each study was assigned an overall quality rating; good, fair or poor, based on an evaluation of risk of bias through key concepts raised in the 12 questions of the quality assessment tool.
The searches retrieved 4300 relevant abstracts in total and after the removal of duplicates ( n = 817), 3483 studies were screened by title and abstract as summarized in the PRISMA diagram ( Figure 1 ). The full texts of 46 studies were reviewed and 13 papers were identified that met all inclusion criteria ( Shi-Chang et al. , 2004 ; Cheung et al. , 2008 ; Chen et al. , 2010 ; Farag et al. , 2010 ; Siegel et al. , 2010 ; Berger-Jenkins et al. , 2014 ; Lemon et al. , 2014 ; Merrill and Sloan, 2014 ; Wang et al. , 2015 ; Frerichs et al. , 2016 ; Wang et al. , 2016 ; LeCheminant et al. , 2017 ; Kupolati et al. , 2019 ). Reasons for exclusion at the full text stage included no data reported on changes in staff behaviours, not an intervention study design and not a peer-reviewed publication (e.g. conference abstracts). One relevant abstract was identified via reference searching; however the full manuscript was not available in English and was therefore excluded.

PRISMA flow diagram of included studies.
The key characteristics of included studies are summarized in Table 1 , and the detail of all extracted data is provided in Supplementary Table 2 . Figure 2 provides a graphical summary of the results with a harvest plot of the intervention effect of studies reporting key obesity-related outcomes (anthropometric indices, dietary behaviour, nutrition knowledge, physical activity behaviour and physical activity knowledge). Six studies focussed specifically on increasing nutrition knowledge or behaviours, two on physical activity alone and five described interventions that addressed both physical activity and nutrition. Study designs included cluster-randomized control trials (four studies), quasi-experimental (four studies), and pre- and post-evaluations without a control group (five studies). Six studies included small sample sizes of participants (<50) ( Cheung et al. , 2008 ; Farag et al. , 2010 ; Berger-Jenkins et al. , 2014 ; Frerichs et al. , 2016 ; Wang et al. , 2016 ; Kupolati et al. , 2019 ).
Summary of included studies
Significant change.
![systematic review of obesity prevention interventions Harvest plot of the intervention effect of included studies reporting key obesity-related outcomes. Height depicts quality assessment [tall (third line) = good, medium (second line) = fair, low (first line) = poor]. Shading of bar = intervention focus (dark grey = physical activity and nutrition, light grey = nutrition, pattern = physical activity). Alphabet characters represent the studies. Studies: a (Berger-Jenkins et al., 2014), b (Chen et al., 2010), c (Cheung et al., 2008), d (Farag et al., 2010), e (Frerichs et al., 2016), f (Kupolati et al., 2019), g (LeCheminant et al., 2017), h (Lemon et al., 2014), i (Merrill and Sloan, 2014), j (Shi-Chang et al., 2004), k (Siegel et al., 2010), l (Wang et al., 2016), m (Wang et al., 2015).](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/heapro/37/3/10.1093_heapro_daac061/2/m_daac061_fig2.jpeg?Expires=1719021572&Signature=kDIzYVt6Jkx0Iq~PMiT8lJwd1JpA1g8DrufTcVYDbANS8bXjwuGF2WnUdbjq0mEoVlUDFl7yrEu5MK0I7Gjckuc1k3lqRYSxswNVW0BlwwWJTOpfI~ux7Aft~QTHeiyKfSA59gO3gHGkUvHyJ9-YP-Mevamo-W4VFb919oca22KQuzVw30FwoELlCsgEvrELVSoLCuV~SEabNOOlVy4-7aXV1YkGU7qyYKgXvxZUB~cvMiWuoVuLMr9iK1vNU5DwZm0yVAbMuojXJIGAKJYSKaQpg417Y6YYtZCGh5nom67aFmjIgfiP3jkm7mXEcee8iVrIoh3ogTzM9lzdf2MRww__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Harvest plot of the intervention effect of included studies reporting key obesity-related outcomes. Height depicts quality assessment [tall (third line) = good, medium (second line) = fair, low (first line) = poor]. Shading of bar = intervention focus (dark grey = physical activity and nutrition, light grey = nutrition, pattern = physical activity). Alphabet characters represent the studies. Studies: a ( Berger-Jenkins et al. , 2014 ), b ( Chen et al. , 2010 ), c ( Cheung et al. , 2008 ), d ( Farag et al. , 2010 ), e ( Frerichs et al. , 2016 ), f ( Kupolati et al. , 2019 ), g ( LeCheminant et al. , 2017 ), h ( Lemon et al. , 2014 ), i ( Merrill and Sloan, 2014 ), j ( Shi-Chang et al. , 2004 ), k ( Siegel et al. , 2010 ), l ( Wang et al. , 2016 ), m ( Wang et al. , 2015 ).
Studies identified were predominantly in the USA (seven studies) and China (four studies), and there was one study each in South Africa and Taiwan. Four studies were implemented in schools located in rural areas ( Farag et al. , 2010 ; Wang et al. , 2015 ; Frerichs et al. , 2016 ; Wang et al. , 2016 ).
Twelve of the 13 studies demonstrated positive impacts on either nutrition knowledge ( Shi-Chang et al. , 2004 ; Chen et al. , 2010 ; Berger-Jenkins et al. , 2014 ; Wang et al. , 2015 ; Kupolati et al. , 2019 ), dietary behaviours ( Chen et al. , 2010 ; Berger-Jenkins et al. , 2014 ; Frerichs et al. , 2016 ; LeCheminant et al. , 2017 ), BMI ( Siegel et al. , 2010 ; Lemon et al. , 2014 ; Merrill and Sloan, 2014 ) or physical activity behaviours ( Cheung et al. , 2008 ; Farag et al. , 2010 ; Berger-Jenkins et al. , 2014 ). One study showed no impact of the intervention on staff knowledge or behaviours ( Wang et al. , 2016 ).
Nutrition interventions
Six studies ( Shi-Chang et al. , 2004 ; Chen et al. , 2010 ; Wang et al. , 2015 ; Frerichs et al. , 2016 ; Wang et al. , 2016 ; Kupolati et al. , 2019 ) focussed on improving the nutrition knowledge and behaviours of school staff. Chen et al. ( Chen et al. , 2010 ) attempted to assess the impact of a government-initiated Health Promoting School (HPS) programme in Taiwan on staff nutrition knowledge and dietary behaviours. The quasi-experimental study included three study arms: HPS aimed at dietary intervention ( n = 1), HPS not aimed at dietary intervention ( n = 2) and non-health-promoting school ( n = 2). Although no significant difference in BMI was found between the three study arms post-intervention, staff at HPS with a dietary intervention had significantly higher nutrition knowledge scores ( p ≤ 0.001) than HPS not aimed at dietary intervention and non-health-promoting schools. Staff at HPS with a dietary intervention also reported better nutrient intake behaviours post-intervention such as eating breakfast, consuming five serves of vegetables and fruits and reading food labels ( Chen et al. , 2010 ). However, without baseline measurements, and given the relatively small sample of schools involved, it is difficult to preclude pre-existing differences in behaviours.
Frerichs et al. ( Frerichs et al. , 2016 ) studied the impact of environmental changes resulting from a school building renovation in the USA, guided by the evidence-based Healthy Eating Design Guidelines for School Architecture, on school staff members’ eating behaviours. The intervention included environmental changes such as the addition of a teaching kitchen, school garden, removal of vending machines and signage promoting healthy eating. The intervention was associated with a significant reduction in the proportion of school staff reporting consuming a high-fat diet [from 73.7 to 57.1% ( p = 0.05)], and several staff health and wellness activities were initiated. Key weaknesses of this study included the small sample size and high attrition rate with greater than 50% lost to follow-up.
A pilot study, by Shi-Chang et al. ( Shi-Chang et al. , 2004 ), also implemented a multi-level intervention (The China/WHO project), targeting all levels of the school from individual knowledge, to policy and infrastructure. The pre- to post-intervention design included approximately 700 employees in 12 schools (6 intervention and 6 control) and demonstrated an increase in nutrition knowledge from baseline to study end in the intervention schools. An improvement in nutrition behaviours of staff in intervention schools was also reported, with those staff self-reporting they were more likely to pay attention to the nutritional content of their lunch after the programme was implemented [an increase from 24 to 38% ( p ≤ 0.01)]. While the proportion of staff reporting the same dropped in control schools. However, the measures of nutrition knowledge and behaviour used in the study were not robust, overall compromising the reliability of evidence of actual behaviour change or health outcomes. In addition, it was unclear if the staff surveyed at baseline and follow-up were in fact the same staff, further compromising the reliability of the evaluation of nutrition-related knowledge and behaviour change.
One small study by Wang et al. ( Wang et al. , 2016 ) ( n = 40 teachers surveyed) implemented a randomized intervention trial of a holistic school-based programme to improve nutrition knowledge, attitudes and behaviours in China. The study found no significant difference between intervention and control schools in staff members’ nutrition knowledge, attitudes and behaviours post-intervention ( Wang et al. , 2016 ). A similar study, also conducted in China in 2015 ( n = 60) aimed to improve nutrition knowledge and eating behaviours of students, parents and school staff by randomly assigning schools to either (i) a holistic intervention using the HPS framework, (ii) a partial intervention with a modified Health Education curriculum or (iii) a non-intervention control. School staff members’ nutrition knowledge increased over the course of the study for all three schools, with the largest improvements in nutrition knowledge among school staff in the partial intervention school ( Wang et al. , 2015 ). Eating behaviour scores for staff also improved for all schools, with the greatest improvement seen in the school assigned to the HPS intervention. These studies were limited by their small sample size and short intervention duration (6 and 3 months, respectively).
Kupolati et al. ( Kupolati et al. , 2019 ) used a quasi-experimental design to evaluate the implementation of a contextual nutrition education programme (comprising a teachers’ manual, picture book, learners’ workbooks and posters) in primary schools in Gauteng Province, South Africa. Pre- and post-testing were used in the small sample (12 teachers in the intervention school, 11 teachers in the comparison school) and showed significant improvement in intervention teachers’ nutrition knowledge post-implementation compared with controls. Improvements were also seen in dietary practices and nutrition attitudes; however these were not significant when compared with controls.
Physical activity interventions
Two studies ( Cheung et al. , 2008 ; Farag et al. , 2010 ) evaluated interventions targeting improvements in physical activity behaviours and knowledge. Cheung et al. ( Cheung et al. , 2008 ) reported on a 6-week physical activity intervention in Hong Kong that aimed to increase the physical activity levels of school staff during school hours ( n = 38 in the intervention group and 14 in the control). The intervention included text message reminders, education in the form of flyers and posters, as well as providing participants with pedometers ( Cheung et al. , 2008 ). Following the intervention, the intervention group had a greater increase in steps at work compared with the control group ( p < 0.001) ( Cheung et al. , 2008 ). The study design did not allow for differentiation between the effectiveness of each element of the intervention, but a post-intervention survey found that pedometers were most commonly cited as motivating teachers in the intervention group to undertake more steps in their work day ( Cheung et al. , 2008 ).
Farag et al. ( Farag et al. , 2010 ) describe an intervention to promote physical activity among US school staff that included changing school environments to include physical activity equipment and promotion posters, and provision of pedometers and a physical activity handbook to individual staff members. No significant changes were seen pre- and post-intervention in self-reported physical activity levels [expressed in Metabolic Equivalent Task (MET) minutes per week, from 2337 [95% confidence interval (CI): 1521–3152] MET-minutes/week, to 2566 (95% CI: 1822–3309) MET-minutes/week] ( Farag et al. , 2010 ).
Interventions targeting both nutrition and physical activity
Five studies included both nutrition and physical activity outcomes ( Siegel et al. , 2010 ; Berger-Jenkins et al. , 2014 ; Lemon et al. , 2014 ; Merrill and Sloan, 2014 ; LeCheminant et al. , 2017 ). Berger-Jenkins et al. ( Berger-Jenkins et al. , 2014 ) describe a 2-year school-based intervention study named ‘Choosing Healthy and Active Lifestyles for Kids’ (CHALK) in the USA, which included a school-wide social marketing campaign. The intervention outcomes included changes in nutrition and physical activity knowledge, attitudes and behaviours of students and staff over time, with a control group added in year two of the study ( Berger-Jenkins et al. , 2014 ). The intervention group showed significant improvements in staff nutrition knowledge ( p ≤ 0.0001) and nutrition behaviour ( p ≤ 0.0001) post-intervention. Self-reported physical activity also increased over time, however not to the point of statistical significance ( p = 0.06). Post-intervention no significant differences were detected between the intervention and control group of school staff for nutrition and physical activity knowledge, attitude and behaviour in year 2 of the study. The evaluation had low response rates and high levels of attrition; of the 370 intervention group staff surveyed at baseline, only 99 completed follow-up surveys after 2 years, while among the control group the final survey included only 17 staff.
LeCheminant et al. ( LeCheminant et al. , 2017 ) reported on a worksite wellness programme that included 1873 US school employees (75% female). The comprehensive outcome assessment included physical activity behaviours, fruit and vegetable consumption, restful sleep, smoking, alcohol consumption, self-rated health, mental health-related outcomes (stress, depression, life-satisfaction and loneliness) and job-related outcomes (job performance, absenteeism, job-related satisfaction). At the end of 2 years, participants reported a significant increase in physical activity with a 4.8% increase in days participating in exercise each week and a 12.8% increase in minutes participating in exercise each week compared with baseline. Dietary behaviour also improved with a 6.7% increase in fruit consumption (serves per day) and 4.1% increase in vegetable consumption (serves per day) ( LeCheminant et al. , 2017 ). The study design did not include a control group and researchers did not measure how much (if at all) the employees engaged with the wellness programme over time, making it difficult to attribute the reported behaviour changes to the programme activities.
Two RCTs evaluated the impact of multi-component interventions in the USA. The study by Lemon et al. evaluated the impact of interventions targeting individual knowledge, attitudes skills, along with organizational culture and nutrition and physical activity policies among 782 school employees, across 12 public schools ( Lemon et al. , 2014 ). At the end of the 2-year follow-up, there was a drop-out of 26.5% participants in the intervention group and 20.3% from the control group. The intervention group lost significantly more weight on average, relative to the control group (−1.37 kg, p = 0.04, equal to a reduction of 0.48 units in BMI). There were also improvements in nutrition knowledge and skills among staff who participated in the intervention. Another RCT, by Siegel et al. recruited 413 school staff from eight intervention and eight control schools ( Siegel et al. , 2010 ). Employees in the intervention schools reduced their BMI by an average of 0.04 kg/m 2 , compared with the control group who increased their BMI by an average of 0.37 kg/m 2 , although overall sample sizes were small ( Siegel et al. , 2010 ).
Merrill et al. undertook a large evaluation of the effectiveness of a worksite wellness programme in reducing health risk involving 2411 school staff in the USA ( Merrill and Sloan, 2014 ). The intervention comprised nutrition education and physical activity initiatives in the workplace including biometric screening, culture change and behaviour change campaigns. Post-intervention, 46.0% of all participants in this pre- and post-test study design reduced their BMI, along with reductions in blood pressure, blood cholesterol and blood glucose ( Merrill and Sloan, 2014 ).
Overall, the studies included were assessed to be of moderate to high risk of bias. No quality threshold was applied, and therefore the results of all 13 included studies is reported here. Most studies had small samples sizes and did not include a control group to assess the effectiveness of the interventions (see Supplementary Table 3 ). Five of the included studies did not clearly describe their inclusion criteria and four studies did not clearly describe the interventions. Out of the total 13 studies, four did not describe an intervention that would have been equally distributed across the study population (e.g. some parts of the intervention may not have reached all school staff, with teachers being more likely to be exposed).
The findings of this review demonstrate a lack of research focus and investment in interventions targeting school staff and teachers’ health over the past two decades internationally. Despite widespread acknowledgement of the importance of school staff as an important population for health promotion, there have only been 13 studies published since 2000, and the majority used relatively weak study designs and included small numbers of schools and staff members. In this review, we found that school staff focussed health promotion interventions positively impacted dietary intake, weight or BMI or physical activity outcomes for staff.
The lack of studies in this review is especially striking when compared with school-based obesity prevention interventions for children, of which there have been at least 50 high quality randomized—or cluster randomized—controlled trials published over the same period, largely in the USA, UK and Europe ( Liu et al. , 2019 ). A recent systematic review and meta-analysis of the effect of school-based obesity prevention interventions on BMI or BMI- z score of children and found significant reductions in intervention schools compared with controls for both single- and multi-component interventions ( Liu et al. , 2019 ). Such school-based studies have the potential to also impact the staff they employ, however the direct impacts remain unknown because interventions and evaluations rarely focus on school staff.
Despite good evidence internationally for workplace health promotion, we found that in the school setting high quality studies evaluating the impacts on staff are lacking. The staff focussed interventions identified in this review showed promise, especially those that aimed to improve both physical activity and diet, however sample sizes were small and research designs lacked robustness, severely limiting the generalizability of results. Almost half of the included papers had an evaluation sample comprising fewer than 50 participants, and despite comprehensive intervention strategies, were under-powered to identify intervention effects. Also, the main positive findings were of knowledge gain, which we know is a very early step in the complex pathway to behaviour change.
Several of the studies that used multi-level interventions showed promise ( Shi-Chang et al. , 2004 ; Chen et al. , 2010 ; Farag et al. , 2010 ; Lemon et al. , 2014 ; Merrill and Sloan, 2014 ; Wang et al. , 2015 ; LeCheminant et al. , 2017 ). Addressing multiple drivers of obesity and ill-health through more comprehensive approaches recognizes the complex nature of behaviour change and preventing obesity; however, far more research would be required to identify and prioritize the most effective strategies and approaches to achieve healthier behaviours and weight status among school staff.
Schools have been identified as a priority target for addressing childhood overweight and obesity ( Dehghan et al. , 2005 ). An important consideration for research focussed on school staff health and behaviour, is that staff are also in a position to facilitate improvements in children’s health behaviours, and subsequently overweight and obesity rates. A recent study showed that teachers who are focussed on improvements in their own health tend to create classrooms in which obesity prevention efforts are better supported ( Esquivel et al. , 2016 ). For example, a teacher who is actively increasing their physical activity level, along with experiencing positive health effects of the change, will be more likely to encourage physical activity among their students ( Esquivel et al. , 2016 ). Joint interventions, with components tailored towards improving both staff and students’ health have the potential to prevent obesity across the lifespan, in both children and adults, and should be priority areas for future research.
It is recognized that the working conditions of the school-based workforce can be stressful, characterized by high job stress-related workers compensation claims, high burnout reflecting high workload requirements and poor work/life balance ( Lever et al. , 2017 ; Arvidsson et al. , 2019 ). As outlined in the WHO Healthy Workplaces Model, interventions targeting the school-based workforce should address both the working conditions that affect health behaviours and offering health behaviour change to optimize impacts ( World Health Organisation, 2007 ). This is an important consideration for future research.
Strengths and weaknesses
This is the first systematic review of the literature to synthesize the evidence on interventions targeting the health of school staff internationally. A strength of this study is that we used broad search terms in five databases, across literature from the years 2000 to 2020. Despite this, there was only a small number of highly diverse, and largely poor quality, studies that met the inclusion criteria, and this precluded a meta-analysis. As with all systematic reviews, the evidence synthesis here could be limited by publication bias, where studies with neutral or negative results may not be published thus skewing results.
This review demonstrates extensive gaps in the evidence base for interventions that seek to improve the health of teachers and school staff, globally. Studies are needed across all contexts and especially in rural or disadvantaged communities. Although the interventions here showed promise in improving diet and physical activity in school staff and associated health risk factors, the health of this large and influential population group needs further focus and research investment.
Supplementary material is available at Health Promotion International online.
Supplementary Table 1: Search strategy terms.
Supplementary Table 2: Detailed data extraction.
Supplementary Table 3: Quality assessment of included studies.
This work was supported by Teachers Health Foundation.
We also acknowledge the contribution of the Deakin University librarian.
This systematic review was conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement guidelines ( Moher et al. , 2009 ) and followed the pre-specified methods documented in the review protocol as submitted to the International Prospective Register of Systematic Reviews (PROSPERO ID: CRD42019127773) on 14 March 2019.
There are no conflicts of interest to declare.
Anderson , L. M. , Quinn , T. A. , Glanz , K. , Ramirez , G. , Kahwati , L. C. , Johnson , D. B. et al. . ( 2009 ) The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. American Journal of Preventive Medicine , 37 , 340 – 357 .
Google Scholar
Arvidsson , I. , Leo , U. , Larsson , A. , Håkansson , C. , Persson , R. and Björk , J. ( 2019 ) Burnout among school teachers: quantitative and qualitative results from a follow-up study in southern Sweden. BMC Public Health , 19 , 655 .
Australian Bureau of Statistics. ( 2019 ) 4221.0—Schools, Australia, 2019 . https://www.abs.gov.au/statistics/people/education/schools/latest-release (last accessed 13 August 2020 ).
Berger-Jenkins , E. , Rausch , J. , Okah , E. , Tsao , D. , Nieto , A. , Lyda , E. et al. . ( 2014 ) Evaluation of a coordinated school-based obesity prevention program in a Hispanic community: choosing healthy and active lifestyles for kids/healthy schools healthy families. American Journal of Health Education , 45 , 261 – 270 .
Chalupka , S. ( 2011 ) Workplace obesity prevention. AAOHN Journal , 59 , 236 .
Chen , Y.-H. , Yeh , C.-Y. , Lai , Y.-M. , Shyu , M.-L. , Huang , K.-C. and Chiou , H.-Y. ( 2010 ) Significant effects of implementation of health-promoting schools on schoolteachers’ nutrition knowledge and dietary intake in Taiwan. Public Health Nutrition , 13 , 579 – 588 .
Cheung , P. P. Y. , Chow , B. C. and Parfitt , G. ( 2008 ) Using environmental stimuli in physical activity intervention for school teachers: a pilot study. International Electronic Journal of Health Education , 11 , 47 – 56 .
Dehghan , M. , Akhtar-Danesh , N. and Merchant , A. T. ( 2005 ) Childhood obesity, prevalence and prevention. Nutrition Journal , 4 , 24 .
Department of Education. ( 2014 ) National Teaching Workforce Dataset—Data Analysis Report . Commonwealth of Australia , Canberra, ACT .
Google Preview
Esquivel , M. K. , Nigg , C. R. , Fialkowski , M. K. , Braun , K. L. , Li , F. and Novotny , R. ( 2016 ) Influence of teachers’ personal health behaviors on operationalizing obesity prevention policy in head start preschools: a project of the Children’s Healthy Living Program (CHL). Journal of Nutrition Education and Behavior , 48 , 318 – 325.e311 .
Farag , N. H. , Moore , W. E. , Thompson , D. M. , Kobza , C. E. , Abbott , K. and Eichner , J. E. ( 2010 ) Evaluation of a community-based participatory physical activity promotion project: effect on cardiovascular disease risk profiles of school employees. BMC Public Health , 10 , 313 .
Frerichs , L. , Brittin , J. , Intolubbe-Chmil , L. , Trowbridge , M. , Sorensen , D. and Huang , T. T. K. ( 2016 ) The role of school design in shaping healthy eating-related attitudes, practices, and behaviors among school staff. Journal of School Health , 86 , 11 – 22 .
Hartline-Grafton , H. L. , Rose , D. , Johnson , C. C. , Rice , J. C. and Webber , L. S. ( 2009 ) Are school employees role models of healthful eating? Dietary intake results from the ACTION Worksite Wellness Trial. Journal of the American Dietetic Association , 109 , 1548 – 1556 .
Herbert , P. C. , Lohrmann , D. K. and Hall , C. ( 2017 ) Targeting obesity through health promotion programs for school staff. Strategies , 30 , 28 – 34 .
Huse , O. , Palermo , C. , Evans , M. and Peeters , A. ( 2020 ) Factors influencing healthy eating and physical activity amongst school staff. Health Promotion International , 35 , 123 – 131 .
Katz , D. L. , O’Connell , M. , Yeh , M. C. , Nawaz , H. , Njike , V. , Anderson , L. M. et al. . ( 2005 ) Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: a report on recommendations of the Task Force on Community Preventive Services. Morbidity and Mortality Weekly Report , 54 , 1 – 12 .
Kelly , T. , Yang , W. , Chen , C. S. , Reynolds , K. and He , J. ( 2008 ) Global burden of obesity in 2005 and projections to 2030. International Journal of Obesity , 32 , 1431 – 1437 .
Kupolati , M. D. , MacIntyre , U. E. , Gericke , G. J. and Becker , P. ( 2019 ) A contextual nutrition education program improves nutrition knowledge and attitudes of South African teachers and learners. Frontiers in Public Health , 7 , 258 .
Langford , R. , Bonell , C. P. , Jones , H. E. , Pouliou , T. , Murphy , S. M. , Waters , E. et al. . ( 2014 ) The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database of Systematic Reviews . doi: 10.1002/14651858.CD008958.pub2
LeCheminant , J. , Merrill , R. M. and Masterson , T. D. ( 2017 ) Changes in behaviors and outcomes among school-based employees in a wellness program. Health Promotion Practice , 18 , 895 – 901 .
Lemon , S. C. , Wang , M. L. , Wedick , N. M. , Estabrook , B. , Druker , S. , Schneider , K. L. et al. . ( 2014 ) Weight gain prevention in the school worksite setting: results of a multi-level cluster randomized trial. Preventive Medicine , 60 , 41 – 47 .
Lever , N. , Mathis , E. and Mayworm , A. ( 2017 ) School mental health is not just for students: why teacher and school staff wellness matters. Report on Emotional & Behavioral Disorders in Youth , 17 , 6 – 12 .
Liu , Z. , Xu , H.-M. , Wen , L.-M. , Peng , Y.-Z. , Lin , L.-Z. , Zhou , S. et al. . ( 2019 ) A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. International Journal of Behavioral Nutrition and Physical Activity , 16 , 95 .
Merrill , R. M. and Sloan , A. ( 2014 ) Effectiveness of a health promotion program among employees in a western United States school district. Journal of Occupational and Environmental Medicine , 56 , 639 – 644 .
Moher , D. , Liberati , A. , Tetzlaff , J. and Altman , D. G. ( 2009 ) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology , 62 , 1006 – 1012 .
National Heart Lung and Blood Institute. ( 2020 ) Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group . https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (last accessed August 2020 ).
Power , B. T. , Kiezebrink , K. , Allan , J. L. and Campbell , M. K. ( 2014 ) Effects of workplace-based dietary and/or physical activity interventions for weight management targeting healthcare professionals: a systematic review of randomised controlled trials. BMC Obesity , 1 , 23 .
Proper , K. I. and van Oostrom , S. H. ( 2019 ) The effectiveness of workplace health promotion interventions on physical and mental health outcomes—a systematic review of reviews. Scandinavian Journal of Work, Environment & Health , 45 , 546 – 559 .
Shi-Chang , X. , Xin-Wei , Z. , Shui-Yang , X. , Shu-Ming , T. , Sen-Hai , Y. , Aldinger , C. et al. . ( 2004 ) Creating health-promoting schools in China with a focus on nutrition. Health Promotion International , 19 , 409 – 418 .
Siegel , J. M. , Prelip , M. L. , Erausquin , J. T. and Kim , S. A. ( 2010 ) A worksite obesity intervention: results from a group-randomized trial. American Journal of Public Health , 100 , 327 – 333 .
Snelling , A. M. , Ernst , J. and Belson , S. I. ( 2013 ) Teachers as role models in solving childhood obesity. Journal of Pediatric Biochemistry , 3 , 55 – 60 .
Swinburn , B. A. , Kraak , V. I. , Allender , S. , Atkins , V. J. , Baker , P. I. and Bogard , J. R. ( 2019 ) The global syndemic of obesity, undernutrition, and climate change: the lancet commission report. Lancet , 393 , 791 – 846 .
Tam , G. and Yeung , M. P. S. ( 2018 ) A systematic review of the long-term effectiveness of work-based lifestyle interventions to tackle overweight and obesity. Preventive Medicine , 107 , 54 – 60 .
Tremmel , M. , Gerdtham , U. G. , Nilsson , P. M. and Saha , S. ( 2017 ) Economic burden of obesity: a systematic literature review. International Journal of Environmental Research and Public Health , 14 , 435 . doi: 10.3390/ijerph14040435
Verweij , L. M. , Coffeng , J. , van Mechelen , W. and Proper , K. I. ( 2011 ) Meta-analyses of workplace physical activity and dietary behaviour interventions on weight outcomes. Obesity Reviews , 12 , 406 – 429 .
Wang , D. , Stewart , D. , and Chang , C. ( 2016 ) A holistic school-based nutrition program fails to improve teachers’ nutrition-related knowledge, attitudes and behaviour in rural China. Health Education , 116 , 467 – 475 .
Wang , D. , Stewart , D. , Yuan , Y. and Chang , C. ( 2015 ) Do health-promoting schools improve nutrition in China? Health Promotion International , 30 , 359 – 368 .
Weerasekara , Y. K. , Roberts , S. B. , Kahn , M. A. , LaVertu , A. E. , Hoffman , B. and Das , S. K. ( 2016 ) Effectiveness of workplace weight management interventions: a systematic review. Current Obesity Reports , 5 , 298 – 306 .
World Health Organisation. ( 2007 ) Workers’ health: global plan of action . https://www.who.int/occupational_health/WHO_health_assembly_en_web.pdf?ua=1 (last accessed 20 October 2020 ).
World Health Organisation. ( 2017 ) Health Promoting Schools: an effective approach to early action on noncommunicable disease risk factors . https://apps.who.int/iris/bitstream/handle/10665/255625/WHO-NMH-PND-17.3-eng.pdf (last accessed 20 October 2020 ).
Supplementary data
Email alerts, citing articles via.
- Recommend to Your Librarian
- Journals Career Network
Affiliations
- Online ISSN 1460-2245
- Print ISSN 0957-4824
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Open access
- Published: 17 May 2024
Qualitative multi-stakeholder evaluation of the adoption, implementation and sustainment of the school-based dietary intervention “Jump-in”
- Froukje E. Takens 1 , 2 , 3 ,
- Indira Indyk 3 ,
- Mai J. M. Chinapaw 1 , 2 ,
- Joanne K. Ujčič-Voortman 3 ,
- Femke van Nassau 1 , 2 &
- Vincent Busch 3
BMC Public Health volume 24 , Article number: 1337 ( 2024 ) Cite this article
173 Accesses
Metrics details
Comprehensive school-based programs applying the WHO Health Promoting School Model have the potential to initiate and sustain behavior change and impact health. However, since they often include intervention efforts on a school’s policies, physical environment, curriculum, health care and involving parents and communities, they significantly ‘intrude’ on a complex system that is aimed primarily at education, not health promotion. More insights into and concrete strategies are therefore needed regarding their adoption, implementation, and sustainment processes to address the challenge to sustainable implementation of HPS initiatives in a primarily educational setting. This study consequently evaluates adoption, implementation and sustainment processes of Amsterdam’s Jump-in healthy nutrition HPS intervention from a multi-stakeholder perspective.
We conducted semi-structured interviews and focus groups with all involved stakeholders ( n = 131), i.e., Jump-in health promotion professionals ( n = 5), school principals ( n = 7), at-school Jump-in coordinators ( n = 7), teachers ( n = 20), parents ( n = 50, 9 groups) and children ( n = 42, 7 groups) from 10 primary schools that enrolled in Jump-in in the school year 2016–2017. Included schools had a higher prevalence of overweight and/or obesity than the Dutch average and they were all located in Amsterdam’s low-SEP neighborhoods. Data were analyzed using a directed content analysis, in which the Determinants of Innovation Model was used for obtaining theory-based predetermined codes, supplemented with new codes emerging from the data.
During intervention adoption, all stakeholders emphasized the importance of parental support, and accompanying workshops and promotional materials. Additionally, parents and teachers indicated that a shared responsibility for children’s health and nuanced framing of health messages were important. During implementation, all stakeholders needed clear guidelines and support structures. Teachers and children highlighted the importance of peer influence, social norms, and uniform application of guidelines. School staff also found further tailoring of the intervention and dealing with financial constraints important. For long-term intervention sustainment, incorporating the intervention policies into the school statutes was crucial according to health promotion professionals.
Conclusions
This qualitative evaluation provides valuable insights into factors influencing the adoption, implementation, and sustainment processes of dietary interventions, such as the importance of transparent and consistent intervention guidelines, clear communication regarding the rationale behind intervention guidelines, and, stakeholders’ involvement in decision-making.
Peer Review reports
Globally, almost one in every five children and adolescents aged 5–19 years has overweight or obesity [ 1 ]. This prevalence is specifically on the rise among people with a lower socio-economic position (SEP) [ 1 , 2 , 3 ]. Childhood obesity often persists into adulthood [ 4 ] and has various short- and long-term detrimental effects on children’s health [ 1 , 5 ]. Many childhood obesity prevention efforts aim to stimulate healthy dietary and physical activity (PA) habits through supportive environments, health promotion policies and other intervention initiatives [ 6 , 7 ]. Schools have become a popular setting for health promotion interventions as schools enable reaching many children from different SEP and cultural backgrounds, in an environment with a strong social, and potentially supportive network of teachers and peers. Every school day children spend a considerable proportion of their time at school and consume their lunch, mid-morning snacks, occasionally treats, and several drinks. Consequently, school-based interventions hold much potential to improve child health behaviors, especially regarding healthy dietary and PA habits [ 8 , 9 , 10 , 11 ].
However, to date, the effects of different types of school-based health promotion interventions have been mixed [ 9 , 10 , 11 , 12 , 13 , 14 ] and realizing effective changes among children with a lower socio-economic position seems especially challenging [ 15 ]. Moreover, research also shows that even with initial success, sustaining children’s behavioral change over time often remains challenging [ 16 ]. Often, facilitators and barriers to interventions’ adoption, implementation and sustainment processes are presented as stand-alone factors. However, in the complex reality, these factors may interact. Therefore, it should be considered to change or tackle these factors in order to more successfully adopt, implement and/or sustain school-based interventions [ 17 ]. As such, more insights are needed from all different types of actors involved in the implementation process in order to facilitate the improvement of these processes in the context of their real-world, dynamic practices and to have a more sustainable impact on daily public health practice [ 18 , 19 ].
An example of a Health Promoting School intervention [ 10 ] that has been successfully embedded in practice is the Jump-in intervention [ 20 , 21 , 22 ]. Jump-in primarily focusses on stimulating healthy dietary and PA habits among primary school children in Amsterdam, the Netherlands [ 20 , 23 ]. This intervention was first designed and implemented in 2002 and was primarily implemented at schools located in the low-SEP regions of Amsterdam, where prevalence rates of childhood overweight and obesity are often relatively high [ 20 ]. The current study aims to evaluate the adoption, implementation and sustainment processes of the dietary component of the Jump-in Health Promoting School intervention, in order to identify factors to optimize these processes within this intervention and similar Health Promoting School interventions.
Intervention description
Part of the larger obesity prevention program, the Amsterdam Healthy Weight Approach (AHWA [ 20 ]), Jump-in was originally designed and shown to be effective in stimulating PA [ 21 , 22 , 24 ]. Following this original positive evaluation, Jump-in was expanded to also include a healthy dietary component and to be further shaped after the Health-Promoting School model (HPS) [ 23 , 25 , 26 ]. Alongside HPS components such as “structurally involving parents” Jump-in comprises three main behavioral change intervention components: stimulating healthy dietary habits, stimulating PA and stimulating active recess play. The City of Amsterdam primarily implements Jump-in in the low-SEP areas of Amsterdam, where overweight/obesity rates are higher than the Dutch national averages. The Jump-in dietary intervention component consists of a set of healthy school nutrition policies, see Table 1 . More details on Jump-in [ 21 , 22 , 27 ] and the AHWA [ 20 , 28 ] have been published elsewhere.
Study design
This study used a combination of interviews and focus groups to distill lessons learned from the intervention’s design, adoption, implementation, and sustainment (or embedding). This study is part of a larger mixed methods evaluation study of the Jump-in program [ 27 ].
Interviews and focus group discussions
Semi-structured (group) interviews and focus group discussions were conducted approximately 12 or 24 months after the start of the intervention’s implementation. Their focus was to gain insight into participants’ overall experience with the intervention and the contextual factors that (potentially) hampered or facilitated its adoption, implementation and sustainment processes. By involving such a broad range of relevant actors, we aimed to obtain different perspectives on the adoption, implementation and sustainment processes of the intervention. All interviews and focus group discussions were conducted in person within the confines of participants’ school, by two researchers in different combinations (FT and V.B., V.D., V.T. or S.J.). The interview and focus group guides were based on the implementation model of Fleuren et al.: Determinants of Innovation Model [ 30 ] with additions from previous interviews conducted by De Meij et al. [ 22 ] and Van Nassau et al. [ 31 ]. Per school, individual interviews were held with the school principal, Jump-in coordinator, two teachers, and the involved HPP. In some cases, interviews with different respondents were combined into one interview upon participants' request. We collected their views on contextual factors (e.g., socio-political, organizational, user and innovation context, and innovation strategies) across adoption, implementation, and sustainment phases. An example question was: “What factors are hindering the implementation of the Jump-in nutrition policy at this school?".
In addition, for each school, one focus group discussion was held with approximately six to eight parents of 4-to-12-year-old children and another with the same number of 8-to-12-year-old children. We decided for sessions of 6–8 individuals to both provide a variety of perspectives and allow everyone a chance to speak and share their views. However, in some cases, we were unable to reach the minimum of six participants, and we conducted a group interview instead. Discussions with parents mainly focused on the alignment of the intervention with existing school culture (socio-political context), clarity of intervention guidelines (innovation context), and their perception of the workshops and promotional materials (innovation strategies). We gathered opinions on contextual factors (e.g., socio-political, innovation and innovation strategies) across intervention phases using statements, sticky notes and plenary discussions. An example statement was:”I agree with the school restricting regulations with regards to healthy eating and drinking in the classroom, And why (not)?”. When transitioning from a focus group to group interviews, the topics remained similar, the guide was simplified, and statements and sticky notes were not used. The discussions with children mainly focused on their opinions on the intervention (innovation context) and its impact on their (school) lives (socio-political context), and their opinions on workshops and promotional materials (innovation strategies). For children, we used more creative methods such as drawings and sticky notes, along with plenary discussions. An example exercise was: "Draw your life after the Jump-in nutrition policy" after which the drawings were discussed. Detailed information on the interview guide, codebook and researcher characteristics are described in the Consolidated criteria for reporting qualitative studies questionnaire (COREQ) [ 32 ] in additional file 1 and the study protocol [ 27 ]. The topic list for the interviews and/or focus groups (in Dutch) are available on request.
Recruitment & data collection
Schools’ enrollment in the Jump-in intervention occurred during the school year 2016–2017. Schools were eligible to participate in the evaluation study based on identical criteria to those for participation in the Jump-in intervention: schools where obesity rates exceed national averages and that are not participating in other health promotion interventions. At the time of this study, Jump-in was already (being) implemented at more than 100 other primary schools in Amsterdam. From all 10 participating schools, we recruited a convenience sample of teachers, parents and children. The schools’ usual communication channels (e.g., website, newsletters) were used to recruit children and parents, and further adjusted in consultation with the Jump-in coordinator to promote participation. Furthermore, we aimed for a diverse sample of participants, including teachers (across gender and teaching grade), parents (across gender and their child’s age), and children (across gender and age). On a few occasions, we exceeded the required subscription (i.e. two teachers, eight parents and children), enabling us to select a sample with more diversity in terms of gender, grade levels and children’s age, If the number of subscriptions allowed it, we also attempted to prevent the participation of both parent and child from the same family. The interviews and focus groups took place between November 2017 and July 2019.
Data analysis
The interviews and focus group discussions were recorded, transcribed verbatim and analyzed in MaxQDA 2018. The latter was done independently by two researchers. We used Directed Content Analysis [ 33 ], a methodology that enabled us to build upon existing research and theories as well as distill novel codes derived from our findings. Prior to data collection, we developed a backbone coding scheme using Fleuren’s Determinants of Innovation Model [ 30 ], yet allowing for a significant degree of open coding. Per phase, this model describes determinants and processes at the level of the sociopolitical context, organization, user, and intervention/innovation, i.e., adoption, implementation, and sustainment. The comprehensive coding of all data according to this model, identifying barriers and facilitators within each phase, generated an extensive results section characterized by substantial overlap due to the abundance of data. Subsequently our approach involved thematically summarizing and analyzing the data to distill overarching themes.
In total, 13 focus groups and 39 (group) interviews were conducted, involving a total of 131 participants. Six focus groups and three group interviews were conducted with parents (Mean 74 min) and seven focus groups were held with children (M 40 min). These sessions lasted between 26 and 89 min. Additionally, individual interviews were held with seven school principals (M 44 min), seven Jump-in coordinators (M 43 min), 20 school teachers (M 28 min) and five HPPs. These interviews ranged in duration from 15 and 93 min (M 74 min). Background characteristics are shown in Table 2 . Specific recurring key themes are discussed below, structured according to their relevance to the adoption, implementation and sustainment phases of the intervention. Some themes were relevant for multiple phases of the intervention. However, to avoid repetition, the themes are discussed in the phase they are most relevant to.
Adoption phase
Support and shared responsibility.
The intervention dietary components were generally well-accepted and easily implemented. At times, especially the treats policy led to some resistance, because parents or teachers believed that healthy products were less festive than unhealthy treats.
Generally, parents and school staff felt a sense of shared responsibility towards children’s health. Both actors felt that schools should play a supporting role, while respecting parents’ autonomy. If they felt this was the case, parents felt more inclined to be positively engaged.
Apart from their personal beliefs, teachers’ acceptance and support for the intervention was also influenced by how they were included by the school board in the decision-making process to participate. Active participation in the decision-making process was said to increase their ownership, motivation, and encourage better implementation overall. Involving teachers and parents in deciding which intervention elements would (not) fit the school, gave them the opportunity to anticipate and respond to issues more effectively. However, some school principals and teachers expressed other viewpoints, including that a larger school size, time constraints and clear communication regarding the reasons behind policy/intervention choices decreased this willingness or desire to be part of the decision-making process.
Framing of the intervention
From the initial communication onward, the intervention goals, materials, and all communications explicitly aimed to convey a focus on a healthy and balanced lifestyle. However, some parents and teachers mainly perceived it as an obesity-focused program, which led to fears of it being stigma-inducing. This was mentioned as a barrier for parental support and consequently for successful implementation, because many parents and teachers considered it important to teach children that enjoying an occasional unhealthy treat is acceptable as long as it is integrated into an overall healthy diet.
“I believe you should teach children the nuance, [...] now it is ‘chocolate bad’. No, chocolate is not always bad. That is what I want to teach children […] sometimes you may cheat” - Teacher
Workshops, activities and materials
To facilitate a more effective implementation of the nutritional policy, the intervention provided several educational workshops, and promotional and educational materials to children and parents throughout the adoption phase. The intervention´s activities and materials, especially the interactive parent theatre, were generally well-received and facilitated active engagement and support among all actors.
Teachers also valued the interactive format and educational quality of the workshops. They felt the workshops were educational and created support, which facilitated adoption and implementation processes. The same was said about the promotional materials. Children found them fun and engaging, while parents believed they contributed to creating a positive social norm towards healthy dietary habits.
However, some promotional materials were viewed as redundant and recurring criticism was expressed regarding most of the materials being cheap plastics and hence environmentally unfriendly. For example, the intervention’s “birthday treat guidelines” often led to children treating their classmates to small toys instead of food. Parents and teachers felt it would be good if such guidelines were to represent a more holistic view that integrates both health and environmental sustainability. Another point for improvement was the further tailoring of materials to children’s cognitive abilities to fit a broader age range of children.
In addition, parents and teachers pointed out that workshops were generally attended by those parents that were already aware of the importance of stimulating a healthy lifestyle among their children. Therefore, they indicated that involvement of a more diverse range of families should be a priority, e.g., via digital mobile school applications.
Implementation phase
Peer influence and social norms.
Children, parents and teachers noted that peer influence in class (mostly positively) impacted intervention adherence. This became apparent during, for instance, the use of promotional materials that visually expressed a social norm. “So-called” water trackers, which showed the percentage of children adhering to the water drinking policy, and were consequently perceived to stimulate water consumption. Especially among younger children, teachers said it stimulated them to adhere to the healthy nutrition policies. Some parents noticed how their child(ren) only wanted to bring water to school, because otherwise they would ’ruin the water tracker for the rest of the class’ . However, in some cases, these norm setting techniques were said to be counterproductive in older children.
“I notice there is a lot of social control. The children check it themselves or they come to me ‘huh I brought this [non-compliant food]’. I’m actually surprised how strict they are.” Teacher
Teacher beliefs and practices
Teachers indicated their main priority was having a good relationship with parents and providing children with the best education possible, not being a health promoter enforcing nutritional guidelines. Forcing them to ‘be police officers’ endangers that relationship, which teachers found unacceptable. Some teachers therefore occasionally allowed children to bring foods they were not supposed to, because they felt unable to combine to roles of a good educator and health promotor. Also, some teachers felt that the intervention content was not congruent with their personal view on health. For instance, some believed a child’s birthday should be a celebration, and did not feel it was right to deny them an unhealthy treat. This sometimes led to intervention dilution.
“I feel like not all colleagues support it [the intervention] to the same extent. Especially for lunch, people say ‘but I’m not gonna check that, this is not my responsibility’.” Teacher
Perceived fairness
According to several interviewed teachers and children, acceptance of and commitment to the intervention depended on the transparent, consistent enforcement of the guidelines. When “the rules” applied to everyone, including their teachers, children accepted them and agreed with them. If not, they perceived this as “really unfair”, which made them resistant to accept the guidelines.
“ The teachers tell us to bring healthy birthday treats, but then they receive chocolates as treats. They just tell us ‘if you want sweet treats you should become a teacher yourself’; it is really unfair when we can’t have any sweets and they can ” - Child
Healthy eating on a budget
All interviewed actors except for children indicated that some parents had mixed feelings about the intervention due to budget constraints. Sometimes the healthy policies created difficult situations for teachers. They did not feel comfortable obliging children to bring fruits, vegetables, and whole-wheat products, which are perceived as expensive, knowing that many families have to deal with financial difficulties.
“ Parents feel ashamed for their poverty and we as teachers don’t want to create uncomfortable situations by obliging these parents to bring expensive fruits to school .” – Teacher
Conversely, the water-only policy was often popular, as was the provision of materials such as lunchboxes, water bottles and fruit holders. Not only did it save money, but some parents mentioned children could no longer derive social status from brand materials.
Tailoring the intervention
Schools (i.e., school principals, Jump-in coordinators and teachers) considered it essential to be able to tailor the intervention to schools’ needs and culture. Some appreciated how they could implement the policies in several phases over longer periods of time, while others wanted to implement everything at once. However, some HPPs, school principals, Jump-in coordinators and teachers stated the importance of finding a balance between ensuring the nutrition policies fit the wishes of parents, children and teachers, and providing clarity to maintain fidelity. Some parents expressed a preference for guidelines that allowed for more variety, creativity and cultural adaptations. However, allowing for such adaptations was said to make it increasingly hard for teachers to monitor adherence to the guidelines. Schools therefore often allowed for a relatively limited number of options for foods that could be brought school, because they valued clarity over variety and diversity. This was experienced as a difficult balance at times, because parents and children sometimes expressed finding the policies overly restrictive and boring. Several parents stated that recurring discussions on whether certain consumptions were healthy enough to meet the guidelines could have been prevented with more transparency on why the nutrition policies were designed that way.
“ Brown bread is very limiting for a school with so many different nationalities. (…) I want my kids to eat soup, wholegrain rice dishes and tortilla wraps because there is so much more than bread.” - Parent

Additional support for implementation and sustainment
Despite generally being satisfied with the intervention, some teachers stated that the received implementation support could be improved.
Teachers experienced a shortage of time due to “additional projects” surrounding health promotion. It would benefit them to have better work protocols with clear work instructions and support regarding e.g., how to deal with parents that disagree with the healthy school policies, how to best deal with related conflicts or resistance, how to monitor adherence to the new policies and how to best deal with children bringing consumptions that violate the nutrition policies. Furthermore, teachers indicated that children value and are very aware of whether their teachers ‘practice what they preach’, so several teachers stated they welcomed practical support on how to set the right example as a role model.
School principals indicated needing better support in keeping their teaching staff and parents engaged. This meant providing sufficient opportunities for teachers to discuss concerns, give and receive inter-collegial support and to keep reminding them of the school policies. However, with teachers’ busy schedules in mind, and the fact that teachers are first and foremost educators and not professional health promoters , school principals indicated they also needed help via, e.g., work protocols or practical guidelines on how to best support their teaching staff in combining their roles as educators and health promoters.
Parents often said fresh fruits and vegetables are more expensive than unhealthy alternatives and that birthday treats and celebrations are often associated with unhealthy foods. Support on how to mix ‘healthy’ and ‘festive’ was said to be needed. Only few parents were aware of the already existing intervention tool ‘birthday treat book’. In addition, parents indicated they would be better supported with an easily accessible, central place to express concerns and ask questions.
Lastly, several HPPs indicated they struggled with their two-fold agenda, i.e., getting schools enthusiastic about adopting the new healthy nutrition policies, while also empowering them to feel ownership and take responsibility for those changes. They were often the driving force behind important changes. However, this role as change leaders simultaneously caused schools not to consider these changes as ‘theirs’, but rather as ‘Jump-in rules’. Trying to balance taking on this supportive role with simultaneously encouraging a school to take charge and feel ownership was experienced as particularly challenging by the HPPs. The importance of schools feeling ownership was emphasized by the process of structurally embedding the intervention in a school. This is done by integrating all nutrition policies into the school’s curriculum and statutes, which is intended to ensure long-term sustainment of the nutrition policies. Enforcement of these policies often watered down when a school came under new management. Therefore, HPPs stressed that developments regarding intervention sustainment are still needed.
Sustainment of the intervention
Although data collection took place before the sustainment phase and hence insights regarding sustainment were limited, we deemed these insights important to include. The intervention aims to facilitate sustainment by integrating its content (i.e., the nutrition policies) into the school statutes. HPPs indicated that this worked well most of the times, but sometimes did not prove sustainable in the long term. It was recurrently indicated that innovations were needed to create better intervention sustainment. Some interviewees stated that intervention acceptance, ownership and habit formation were important conditions for a sustainable implementation. Additionally, the HPPs said they needed more tools to adapt the intervention in real life together with the main actors without compromising the intervention’s effective elements.
This study presents a qualitative evaluation of the adoption, implementation and sustainment processes of the Jump-in dietary intervention. We collected perspectives from children, parents, teachers, school principals, at-school Jump-in coordinators and municipal HPPs in a total of 13 focus groups and 39 (group) interviews, including a total of 131 participants. Overall, the intervention was well-accepted and received with enthusiasm among all stakeholders, yet various opportunities for improvement came to light.
Regarding the adoption phase, participants felt it was important for the HPPs and school principals to be transparent about the intervention’s goals and processes. It also stood out that parents, children, and teachers wanted to have a voice in the decision-making processes regarding intervention content and implementation. Although each school’s Jump-in team included several stakeholders (generally a HPP, school principal, a local Jump-in coordinator and several teachers), parents and teachers indicated they wanted to be better included in the decision-making process. This corresponds with previous recommendations to design and implement health promotion interventions together with all end-users for more appropriate, better fitting and more effective interventions [ 34 ].
The main lessons regarding the implementation phase were that having clear, transparent nutrition rules that apply to all children as well as their teachers (i.e., role modelling) and having a clear way to unanimously communicate and enforce those rules, were considered essential for their sustained support. Allowing children to bring a limited selection of “healthy” food options to school was experienced as overly restrictive and boring, especially in a multicultural city such as Amsterdam. However, having to discuss these rules with children and parents, teachers felt the pressure to act as “the health police”, which, in their view, endangered their relationship with parents as well as the intervention’s sustainability. The role of health promotor sometimes conflicted with their role as educator. Other studies have also reported difficulties when merging the roles of health promotor and educator in school health promotion [ 35 ], stating the need to align health promotion efforts with educational goals [ 36 ] and the need for innovations and support structures for sustainable success in comprehensive HPS efforts in real-world contexts [ 37 ]. It therefore seems vital to make health promotion a core business for schools, align efforts with national policies, use local data to show their need and effectiveness, and provide high-quality, pragmatic and accessible staff training [ 38 ].
For the sustainment phase , integration into the school statutes was often noted as being crucial to the sustainable implementation of the Jump-in intervention. Efforts to stimulate sustainable implementation start at intervention design and adoption, e.g., providing support that fits involved participants/actors within the structures, workings, and culture of their school’s system.
Interacting barriers and facilitators
Many of the factors (either barriers or facilitators) that we found in our study did not act as stand-alone, individual influences, but rather as parts of specific, sometimes elaborate, interactions impacting the program’s adoption, implementation or sustainment. For example, some parents wished for an expansion of the healthy policies by including a selection of foods and drinks that were considered more culturally inclusive, which simultaneously complicated the teacher’s role that included checking whether all children adhered to the school policies. Also, teachers emphasized the importance of educating children about nuances, such as instances where exceptions to the guidelines are permissible. However, children perceived differences in how teachers enforced the nutrition guidelines as unfair. Qualitative evaluations of health promotion interventions often present lists of barriers and facilitators [ 18 , 30 , 39 ], yet rarely note their complex interactions, which sometimes leads to oversimplified recommendations. Instead, Darlington and colleagues describe five types of interactions: hindering, moderating, counterbalancing, enabling and neutral [ 35 ]. Such distinctions may help report and understand how factors are positioned within more complex mechanisms of change. With our thematic analyses, we aimed to understand the influence of certain barriers and facilitators, in a broader context. Such considerations and views could benefit the development of context- and phase-specific strategies to help implement interventions in a real-world setting [ 18 ].
Tailoring while maintaining fidelity and effectiveness
A recurring theme in our study was the challenge to implement the intervention as intended (i.e., maintaining intervention fidelity) while simultaneously allowing for, and even stimulating, local adaptation, ownership, and shared responsibility. Allowing for local adaptations makes an intervention more (culturally) appropriate, stimulating feelings of ownership and intrinsic motivation among actors, which may also benefit effectiveness and long-term sustainment. For HPPs this was challenging, confirming HPS intervention studies [ 9 , 40 , 41 ]. Jump-in’s HPPs aimed to adapt the intervention to the local context together with relevant stakeholders while building on evidence-based behavioral change techniques [ 42 , 43 ] and their peer-to-peer learning network. In addition, there is a need for tools that HPPs can use to distinguish crucial versus adaptable intervention components, so that the intervention’s effectiveness is secured, e.g., Intervention Mapping Adapt [ 44 , 45 ]. Taking the lead in the implementation processes, however, also hampered the process of ensuring schools feel the sense of ownership and responsibility required to create long-term embedment of the desired system changes [ 17 , 41 ]. We recommend more research on practical tools for HPPs that enable school actors to feel ownership while simultaneously facilitating smooth implementation processes.
Schools as complex systems
Several hampering factors might be better understood when viewed in the context of a systems approach. For instance, challenges encountered by some teachers in playing the role of “police officers”. Each school represents a unique context, and it is therefore also important to address contextual differences between schools. For example, some teaching teams perceived it as a barrier when they were not involved in the decision-making process, whereas teachers at other schools preferred a small group to handle this, as long as they were kept updated. Additionally, variations were observed in the extent to which parents accepted information from health professionals as accurate. It is therefore crucial to consider the context within schools. Accomplishing sustained changes in schools – as in most complex adaptive systems – often requires coordinated, complementary actions on different socioecological levels [ 17 , 25 , 26 , 28 ]. Viewing schools as such in public health promotion efforts can advance the evolution of the symbiosis between health and education [ 9 , 17 , 46 ]. Looking at the implementation processes via the systems view of the Action Scales Model (ASM) [ 47 ] shows how aiming to change certain system structures without also dealing with root system goals is unlikely to lead to durable, effective changes. This model states that a system is shaped by a combination of concrete, visible elements (i.e., actions and structures, the tip of the iceberg) and the underlying beliefs and goals that shape them. Schools, for example, revolve around the belief that providing a child with the best possible education is vital to its success in life. Given that belief, and consequent goals, structures, and actions (or: events) naturally emerge to achieve those goals. Therefore, changing certain system structures (e.g., implementing certain healthy nutrition policies in schools) is more likely to succeed when aligned with the underlying system beliefs and goals (e.g., education). Requiring teachers to place their role of health promotor above that of educator in a system that revolves around providing education is unlikely to be successful and sustainable. However, results indicate this is what happens when teachers are expected to argue with parents over healthy nutrition guidelines, thereby endangering their parent-teacher relationship. Creating more lasting impact is likelier to succeed with a simultaneous integration of intervention change objectives focused on targeting underlying systems goals and relevant actors’ beliefs. It would help, for instance, to get school boards to prioritize children’s health alongside their educational achievements. This way, taking such a systems perspective, can provide new insights into potential new leverage points to intervene on and help to create more durable, impactful health promotion initiatives. Therefore, future research could benefit from integrating such approaches during the initial phases of HPS evaluations.
Strengths and limitations
A strength of the current study is its large size. With 39 individual and group interviews and 13 focus groups with a total of 131 participants, it provides a broad range of perspectives from all main actors involved in the intervention’s adoption, implementation, and sustainment processes in a real-world setting. Shaping the data collection and analysis with a clear theoretical framework also added to the study’s strength. In addition, the qualitative evaluation was generally carried out one to two years after intervention adoption, which provided sufficient time to experience recurring, structural barriers and lessons learned. Yet, this timeframe was most of the times not sufficient to capture sustainment.
The study also had certain limitations. Firstly, as is generally the case in research, parents that were willing to participate were potentially more likely to have relatively extreme opinions on the intervention leading to an overrepresentation of their strong views, a phenomenon known as self-selection bias [ 48 ]. In addition, despite efforts to mainly select parents from a low SEP, informal data on occupation suggest parents from high SEP backgrounds also participated in the focus groups discussions. However, due to the sampling size this influence is likely minimal and still allowed for obtaining a representative view on the perspectives from both low and high socioeconomic position (SEP) groups.
This qualitative evaluation provides novel insights and lessons about the adoption, implementation, and sustainment processes of the Jump-in dietary intervention. Including all stakeholders in the decision-making and implementation processes appeared to be key to the intervention’s early adoption and acceptance. Transparency and uniformity of intervention guidelines appeared important for parental and child support. Parents requested better communication about the reasons behind guidelines. Furthermore, identified key challenges included understanding how barriers and facilitators operate and interact within more intricate mechanisms of change, maintaining a balance between intervention fidelity and tailoring the intervention to the local context, and successfully implementing and structurally embedding a health promotion initiative within a larger system (i.e. a school) that prioritizes promoting good education over health as its primary goal [ 49 , 50 , 51 ].
Availability of data and materials
Data can be obtained from the corresponding authors upon reasonable request.
Abbreviations
Health promotion professional
Health promoting school
Amsterdam healthy weight approach
Physical activity
Socio-economic position
Determinants of innovation model
World Health Organization. Fact sheet: obesity and overweight. World Health Organization; 2021. www.who.int/news-room/fact-sheets/detail/obesity-and-overweight .
Bouthoorn SH, Wijtzes AI, Jaddoe VWV, et al. Development of socioeconomic inequalities in obesity among Dutch pre-school and school-aged children. Obesity. 2014;22:2230–7.
Article PubMed Google Scholar
van Dommelen P, Schonbeck Y, HiraSing RA, et al. Call for early prevention: prevalence rates of overweight among Turkish and Moroccan children in The Netherlands. Eur J Public Health. 2015;25(5):828–33.
Singh AS, Mulder C, Twisk JWR, et al. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes Rev. 2008;9:474–88.
Article CAS PubMed Google Scholar
Sahoo K, Sahoo B, Choudhury AK, et al. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4(2):187–92.
Article PubMed PubMed Central Google Scholar
World Health Organization. Population-based approaches to childhood obesity prevention; ISBN 978 92 4 150478 2; 2012.
Seidell JC, Halberstadt J. National and local strategies in the netherlands for obesity prevention and management in children and adolescents. Obes Facts. 2020;13(4):418–29.
Khambalia AZ, Dickinson S, Hardy LL, et al. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obesity Rev. 2012;13:214–33.
Article CAS Google Scholar
Langford R, Bonell C, Jones H, et al. Obesity prevention and the Health promoting Schools framework: essential components and barriers to success. Int J Behav Nutr Phys Act, 2015 12:1. 2015;12:1–17.
Langford R, Bonell CP, Jones HE, et al. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst Rev. 2014;2014(4):CD008958. https://doi.org/10.1002/14651858.CD008958.pub2 .
Wang D, Stewart D. The implementation and effectiveness of school-based nutrition promotion programmes using a health-promoting schools approach: a systematic review. Public Health Nutr. 2013;16:1082–100.
Day RE, Sahota P, Christian MS. Effective implementation of primary school-based healthy lifestyle programmes: A qualitative study of views of school staff. BMC Public Health. 2019;19:1–16.
Article Google Scholar
Liu Z, Xu HM, Wen LM, et al. A systematic review and meta-analysis of the overall effects of school-based obesity prevention interventions and effect differences by intervention components. Int J Behav Nutr Phys Act. 2019;16(1):95.
Williams AJ, Henley WE, Williams CA, et al. Systematic review and meta-analysis of the association between childhood overweight and obesity and primary school diet and physical activity policies. Int J Behav Nutr Phys Act. 2013;10:101.
van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: Systematic review of controlled trials. BMJ. 2007;335:703.
Shoesmith A, Hall A, Wolfenden L, et al. Barriers and facilitators influencing the sustainment of health behaviour interventions in schools and childcare services: a systematic review. Implement Sci. 2021;16(1):62.
Rosas SR. Systems thinking and complexity: considerations for health promoting schools. Health Promot Int. 2017;32(2):301–11.
PubMed Google Scholar
Cassar S, Salmon J, Timperio A, et al. Adoption, implementation and sustainability of school-based physical activity and sedentary behaviour interventions in real-world settings: a systematic review. Int J Behav Nutr Phys Act. 2019;16(1):120.
Durlak JA, DuPre EP. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Comm Psychol. 2008;41:327–50.
UNICEF, City of Amsterdam, EAT. The Amsterdam Healthy Weight Approach: Investing in healthy urban childhoods: A case study on healthy diets for children. Amsterdam: 2020. www.unicef.org/media/89401/file/Amsterdam-Healthy-Weight-Approach-Investing-healthy-urban-childhoods.pdf .
de Meij JS, Chinapaw MJ, van Stralen MM, et al. Effectiveness of JUMP-in, a Dutch primary school-based community intervention aimed at the promotion of physical activity. Br J Sports Med. 2011;45(13):1052–7.
de Meij JSB, van der Wal MF, van Mechelen W, et al. A mixed methods process evaluation of the implementation of JUMP-in, a multilevel school-based intervention aimed at physical activity promotion. Health Prom Pract. 2013;14:777–90.
Busch V, Van Opdorp PAJ, Broek J, et al. Bright spots, physical activity investments that work: JUMP-in: promoting physical activity and healthy nutrition at primary schools in Amsterdam. Br J Sports Med. 2018;52:1299–301.
De Meij JS, Chinapaw MJ, Kremers SP, et al. Promoting physical activity in children: The stepwise development of the primary school-based JUMP-in intervention applying the RE-AIM evaluation framework. Br J Sports Med. 2010;44(12):879–87.
Rasberry CN, Slade S, Lohrmann DK, et al. Lessons learned from the whole child and coordinated school health approaches. J Sch Health. 2015;85(11):759–65.
Rooney LE, Videto DM, Birch DA. Using the whole school, whole community, whole child model: implications for practice. J Sch Health. 2015;85(11):817–23.
Takens FE, Busch V, Ujcic-Voortman JK, et al. The unique extended selection cohorts design for the evaluation of the school-based jump-in intervention on dietary habits: a study protocol. Int J Environ Res Public Health. 2020;17(4):1145.
Sawyer A, den Hertog K, Verhoeff AP, et al. Developing the logic framework underpinning a whole-systems approach to childhood overweight and obesity prevention: Amsterdam Healthy Weight Approach. Obesity Sci Pract. 2021;7(5):591–605.
Battjes-Fries MC, Haveman-Nies A, Renes R-J, et al. Effect of the Dutch school-based education programme ‘Taste Lessons’ on behavioural determinants of taste acceptance and healthy eating: a quasi-experimental study. Public Health Nutr. 2015;18:2231–41.
Fleuren M, Wiefferink K, Paulussen T. Determinants of innovation within health care organizations: literature review and Delphi study. Int J Qual Health Care. 2004;16:107–23.
van Nassau F, Singh AS, Broekhuizen D, et al. Barriers and facilitators to the nationwide dissemination of the Dutch school-based obesity prevention programme DOiT. Eur J Public Health. 2016;26:611–6.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88.
Leask CF, Sandlund M, Skelton DA, et al. Framework, principles and recommendations for utilising participatory methodologies in the co-creation and evaluation of public health interventions. Res Involv Engagem. 2019;5:2.
Darlington EJ, Violon N, Jourdan D. Implementation of health promotion programmes in schools: an approach to understand the influence of contextual factors on the process? BMC Public Health. 2018;18(1):163.
Butler H, Bowes G, Drew S, Glover S, Godfrey C, Patton G, Trafford L, Bond L. Harnessing complexity: taking advantage of context and relationships in dissemination of school-based interventions. Health Promot Pract. 2010M;11(2):259–67. https://doi.org/10.1177/1524839907313723 .
Ekornes S. Teacher perspectives on their role and the challenges of inter-professional collaboration in mental health promotion. Sch Mental Health. 2015;7:193–211.
Sadjadi M, Blanchard L, Brulle R, et al. Barriers and facilitators to the implementation of Health-Promoting School programmes targeting bullying and violence: a systematic review. Health Educ Res. 2022;36(5):581–99.
Flottorp SA, Oxman AD, Krause J, et al. A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci. 2013;8:35.
Bopp M, Saunders RP, Lattimore D. The tug-of-war: fidelity versus adaptation throughout the health promotion program life cycle. J Prim Prev. 2013;34(3):193–207.
Koelen M, Vaandrager L, Colómer C. Health promotion research: dilemmas and challenges. J Epidemiol Community Health. 2001;55:257–62.
Article CAS PubMed PubMed Central Google Scholar
Kok G, Schaalma H, Ruiter RA, et al. Intervention mapping: protocol for applying health psychology theory to prevention programmes. J Health Psychol. 2004;9(1):85–98.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
Fernandez ME, Ruiter RAC, Markham CM, et al. Intervention mapping: theory- and evidence-based health promotion program planning: perspective and examples. Front Public Health. 2019;7:209.
Highfield L, Hartman MA, Mullen PD, et al. Intervention mapping to adapt evidence-based interventions for use in practice: increasing mammography among African American women. Biomed Res Int. 2015;2015:160103.
PubMed PubMed Central Google Scholar
Angawi K, Gaissi A. Systematic review of setting-based interventions for preventing childhood obesity. Biomed Res Int. 2021;2021:4477534.
Nobles JD, Radley D, Mytton OT. The Action Scales Model: A conceptual tool to identify key points for action within complex adaptive systems. Perspectives in Public Health. 2022;142(6):328–37. https://doi.org/10.1177/17579139211006747 .
Collier D, Mahoney J. Insights and pitfalls: Selection bias in qualitative research. World politics. 1996;49(1):56–91.
Government efficiency, transparency and accountability, GOV UK. What Works Network. The What Works Network: Five Years On. 2018. https://assets.publishing.service.gov.uk/media/5a82425b40f0b62305b93557/6.4154_What_works_report_Final.pdf .
Callahan KM, Stuart EA. Bringing evidence to bear on public health in the United States. Public Health Rep. 2018;133(1_suppl):20S-3S.
Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Annu Rev Public Health. 2018;39:55–76.
Download references
Acknowledgements
We thank all primary schools, parents and children that participated in this study. Furthermore, we thank Jobien Groen, Esmée Oude Geerdink and Malou Friedhoff for their help setting up the data collection. We also thank Simone Janssen, Valerie Tijhuis and Virginie Domsdorf for their contributions to conducting the (focus group) interviews.
This study was financially supported by Sarphati Amsterdam and the Amsterdam Healthy Weight Approach. This research received no external grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Public and Occupational Health, Amsterdam UMC, Vrije Universiteit Amsterdam, De Boelelaan 1117, Amsterdam, The Netherlands
Froukje E. Takens, Mai J. M. Chinapaw & Femke van Nassau
Amsterdam Public Health Research Institute, Health Behaviour and Chronic Diseases, Amsterdam, The Netherlands
Department Gezond Leven, Public Health Service of Amsterdam, Team Sarphati Amsterdam, Nieuwe Achtergracht 100, 1018 WT, Amsterdam, The Netherlands
Froukje E. Takens, Indira Indyk, Joanne K. Ujčič-Voortman & Vincent Busch
You can also search for this author in PubMed Google Scholar
Contributions
M.C., V.B., F.v.N. and F.T. contributed to the conception and design. F.T. conducted the data collection. I.I., V.B. and F.T. analyzed the data. I.I., V.B. and F.T. wrote the manuscript draft. M.C., J.U., F.v.N. reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Froukje E. Takens or Indira Indyk .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Medical Ethical committee of the VU University Medical Centre as part of a larger evaluation study (protocol number 2016.415, amendment number A2017.421). Written informed consent was provided by all participants. For children, informed consent was obtained from one parent or caregiver. All participants, apart from the health promotion professionals, received a small incentive for participation; a 10-euro gift voucher for adults and a small toy for children. Verbal consent for audio recording the interviews was provided at the start of interviews.
Consent for publication
For this study we only made use of data that we obtained. Other databases were not used for this study. Therefore, no further specific permissions were required to use the data to publish our study’s results.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Takens, F.E., Indyk, I., Chinapaw, M.J.M. et al. Qualitative multi-stakeholder evaluation of the adoption, implementation and sustainment of the school-based dietary intervention “Jump-in”. BMC Public Health 24 , 1337 (2024). https://doi.org/10.1186/s12889-024-18814-1
Download citation
Received : 12 October 2023
Accepted : 09 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12889-024-18814-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- School-based
- Nutrition policy
- Dietary behavior
- Implementation evaluation
- Qualitative
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Preventing Childhood Obesity
- Health Care Strategies
- About Obesity
- What Can Be Done
- About Healthy Weight and Growth
- Body Mass Index (BMI)
- About Nutrition
- About Physical Activity
Evidence-Based Guidelines for Child Obesity
What to know.
Many professional associations offer evidence-based guidelines for comprehensive care for children with obesity. The guidelines include obesity screening and referral to effective obesity interventions. These guidelines inform pediatricians and other pediatric health care providers about the standard of care for screening, evaluating, and treating obesity and related chronic diseases.

American Academy of Pediatrics
In 2023, the American Academy of Pediatrics (AAP) released the Clinical Practice Guideline (CPG) for the Evaluation and Treatment of Children and Adolescents With Obesity .
The AAP CPG recommends that pediatric health care providers (PHCPs) screen all children 2–18 years for overweight, obesity, and severe obesity at least annually. To do so, they should:
- Measure height and weight.
- Calculate body mass index (BMI).
- Assess BMI percentile using age- and sex-specific CDC growth charts.
The AAP CPG also provides guidelines on how to treat and manage obesity. This includes guidelines for offering or referring patients to intensive health behavior and lifestyle treatment.
Weight stigma
Us preventive services taskforce (uspstf).
In 2017, the USPSTF recommended that clinicians:
- Screen for obesity in children and adolescents 6 years and older, and
- Offer or refer them to comprehensive, intensive behavioral interventions to promote improvements in weight status.
This recommendation was Grade B. This means there was moderate certainty that the net benefit was moderate. USPSTF found no direct evidence of harm in screening for obesity. This recommendation was based on a thorough evidence review of behavioral interventions for obesity targeting lifestyle change.
Other organizations
American Psychological Association In 2018, the association released the Clinical Practice Guideline for Multicomponent Behavioral Treatment of Obesity and Overweight in Children and Adolescents . This CPG strongly supported the use of family-based multicomponent behavioral interventions with at least 26 contact hours for children and adolescents 2-18 with overweight and obesity.
Pediatric Endocrine Society In 2017, the society convened a task force of experts who released a clinical practice guideline titled Pediatric Obesity- Assessment, Treatment, and Prevention . It includes BMI screening, evaluating children with overweight or obesity for obesity-related comorbidities, and referring to intensive family-centered lifestyle programs.
CDC-Recognized Family Healthy Weight Programs Evidence-based programs ready to implement in clinical, community, and public health settings.
CDC's Child and Teen BMI Calculator Tool to calculate BMI, BMI percentile, and the corresponding BMI category for children and teens aged 2–19 years, as well as plot the BMI on a growth chart.
CDC's Growth Chart Training Interactive, self-guided modules to train health care providers and others on how to use and interpret growth charts, including CDC's 2022 Extended BMI-for-Age growth charts.
Clinical Growth Charts CDC's 2000 and 2022 growth charts available online or in downloadable format.
CDC's obesity prevention efforts focus on policy and environmental strategies to make healthy eating and active living accessible for everyone.
For Everyone
Health care providers, public health.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 May 2024
Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial
- Donna H. Ryan 1 ,
- Ildiko Lingvay ORCID: orcid.org/0000-0001-7006-7401 2 ,
- John Deanfield 3 ,
- Steven E. Kahn 4 ,
- Eric Barros ORCID: orcid.org/0000-0001-6613-4181 5 ,
- Bartolome Burguera 6 ,
- Helen M. Colhoun ORCID: orcid.org/0000-0002-8345-3288 7 ,
- Cintia Cercato ORCID: orcid.org/0000-0002-6181-4951 8 ,
- Dror Dicker 9 ,
- Deborah B. Horn 10 ,
- G. Kees Hovingh 5 ,
- Ole Kleist Jeppesen 5 ,
- Alexander Kokkinos 11 ,
- A. Michael Lincoff ORCID: orcid.org/0000-0001-8175-2121 12 ,
- Sebastian M. Meyhöfer 13 ,
- Tugce Kalayci Oral 5 ,
- Jorge Plutzky ORCID: orcid.org/0000-0002-7194-9876 14 ,
- André P. van Beek ORCID: orcid.org/0000-0002-0335-8177 15 ,
- John P. H. Wilding ORCID: orcid.org/0000-0003-2839-8404 16 &
- Robert F. Kushner 17
Nature Medicine ( 2024 ) Cite this article
37k Accesses
1 Citations
2404 Altmetric
Metrics details
- Health care
- Medical research
In the SELECT cardiovascular outcomes trial, semaglutide showed a 20% reduction in major adverse cardiovascular events in 17,604 adults with preexisting cardiovascular disease, overweight or obesity, without diabetes. Here in this prespecified analysis, we examined effects of semaglutide on weight and anthropometric outcomes, safety and tolerability by baseline body mass index (BMI). In patients treated with semaglutide, weight loss continued over 65 weeks and was sustained for up to 4 years. At 208 weeks, semaglutide was associated with mean reduction in weight (−10.2%), waist circumference (−7.7 cm) and waist-to-height ratio (−6.9%) versus placebo (−1.5%, −1.3 cm and −1.0%, respectively; P < 0.0001 for all comparisons versus placebo). Clinically meaningful weight loss occurred in both sexes and all races, body sizes and regions. Semaglutide was associated with fewer serious adverse events. For each BMI category (<30, 30 to <35, 35 to <40 and ≥40 kg m − 2 ) there were lower rates (events per 100 years of observation) of serious adverse events with semaglutide (43.23, 43.54, 51.07 and 47.06 for semaglutide and 50.48, 49.66, 52.73 and 60.85 for placebo). Semaglutide was associated with increased rates of trial product discontinuation. Discontinuations increased as BMI class decreased. In SELECT, at 208 weeks, semaglutide produced clinically significant weight loss and improvements in anthropometric measurements versus placebo. Weight loss was sustained over 4 years. ClinicalTrials.gov identifier: NCT03574597 .
Similar content being viewed by others

Effects of a personalized nutrition program on cardiometabolic health: a randomized controlled trial

Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial

What is the pipeline for future medications for obesity?
The worldwide obesity prevalence, defined by body mass index (BMI) ≥30 kg m − 2 , has nearly tripled since 1975 (ref. 1 ). BMI is a good surveillance measure for population changes over time, given its strong correlation with body fat amount on a population level, but it may not accurately indicate the amount or location of body fat at the individual level 2 . In fact, the World Health Organization defines clinical obesity as ‘abnormal or excessive fat accumulation that may impair health’ 1 . Excess abnormal body fat, especially visceral adiposity and ectopic fat, is a driver of cardiovascular (CV) disease (CVD) 3 , 4 , 5 , and contributes to the global chronic disease burden of diabetes, chronic kidney disease, cancer and other chronic conditions 6 , 7 .
Remediating the adverse health effects of excess abnormal body fat through weight loss is a priority in addressing the global chronic disease burden. Improvements in CV risk factors, glycemia and quality-of-life measures including personal well-being and physical functioning generally begin with modest weight loss of 5%, whereas greater weight loss is associated with more improvement in these measures 8 , 9 , 10 . Producing and sustaining durable and clinically significant weight loss with lifestyle intervention alone has been challenging 11 . However, weight-management medications that modify appetite can make attaining and sustaining clinically meaningful weight loss of ≥10% more likely 12 . Recently, weight-management medications, particularly those comprising glucagon-like peptide-1 receptor agonists, that help people achieve greater and more sustainable weight loss have been developed 13 . Once-weekly subcutaneous semaglutide 2.4 mg, a glucagon-like peptide-1 receptor agonist, is approved for chronic weight management 14 , 15 , 16 and at doses of up to 2.0 mg is approved for type 2 diabetes treatment 17 , 18 , 19 . In patients with type 2 diabetes and high CV risk, semaglutide at doses of 0.5 mg and 1.0 mg has been shown to significantly lower the risk of CV events 20 . The SELECT trial (Semaglutide Effects on Heart Disease and Stroke in Patients with Overweight or Obesity) studied patients with established CVD and overweight or obesity but without diabetes. In SELECT, semaglutide was associated with a 20% reduction in major adverse CV events (hazard ratio 0.80, 95% confidence interval (CI) 0.72 to 0.90; P < 0.001) 21 . Data derived from the SELECT trial offer the opportunity to evaluate the weight loss efficacy, in a geographically and racially diverse population, of semaglutide compared with placebo over 208 weeks when both are given in addition to standard-of-care recommendations for secondary CVD prevention (but without a focus on targeting weight loss). Furthermore, the data allow examination of changes in anthropometric measures such as BMI, waist circumference (WC) and waist-to-height ratio (WHtR) as surrogates for body fat amount and location 22 , 23 . The diverse population can also be evaluated for changes in sex- and race-specific ‘cutoff points’ for BMI and WC, which have been identified as anthropometric measures that predict cardiometabolic risk 8 , 22 , 23 .
This prespecified analysis of the SELECT trial investigated weight loss and changes in anthropometric indices in patients with established CVD and overweight or obesity without diabetes, who met inclusion and exclusion criteria, within a range of baseline categories for glycemia, renal function and body anthropometric measures.
Study population
The SELECT study enrolled 17,604 patients (72.3% male) from 41 countries between October 2018 and March 2021, with a mean (s.d.) age of 61.6 (8.9) years and BMI of 33.3 (5.0) kg m − 2 (ref. 21 ). The baseline characteristics of the population have been reported 24 . Supplementary Table 1 outlines SELECT patients according to baseline BMI categories. Of note, in the lower BMI categories (<30 kg m − 2 (overweight) and 30 to <35 kg m − 2 (class I obesity)), the proportion of Asian individuals was higher (14.5% and 7.4%, respectively) compared with the proportion of Asian individuals in the higher BMI categories (BMI 35 to <40 kg m − 2 (class II obesity; 3.8%) and ≥40 kg m − 2 (class III obesity; 2.2%), respectively). As the BMI categories increased, the proportion of women was higher: in the class III BMI category, 45.5% were female, compared with 20.8%, 25.7% and 33.0% in the overweight, class I and class II categories, respectively. Lower BMI categories were associated with a higher proportion of patients with normoglycemia and glycated hemoglobin <5.7%. Although the proportions of patients with high cholesterol and history of smoking were similar across BMI categories, the proportion of patients with high-sensitivity C-reactive protein ≥2.0 mg dl −1 increased as the BMI category increased. A high-sensitivity C-reactive protein >2.0 mg dl −1 was present in 36.4% of patients in the overweight BMI category, with a progressive increase to 43.3%, 57.3% and 72.0% for patients in the class I, II and III obesity categories, respectively.
Weight and anthropometric outcomes
Percentage weight loss.
The average percentage weight-loss trajectories with semaglutide and placebo over 4 years of observation are shown in Fig. 1a (ref. 21 ). For those in the semaglutide group, the weight-loss trajectory continued to week 65 and then was sustained for the study period through week 208 (−10.2% for the semaglutide group, −1.5% for the placebo group; treatment difference −8.7%; 95% CI −9.42 to −7.88; P < 0.0001). To estimate the treatment effect while on medication, we performed a first on-treatment analysis (observation period until the first time being off treatment for >35 days). At week 208, mean weight loss in the semaglutide group analyzed as first on-treatment was −11.7% compared with −1.5% for the placebo group (Fig. 1b ; treatment difference −10.2%; 95% CI −11.0 to −9.42; P < 0.0001).
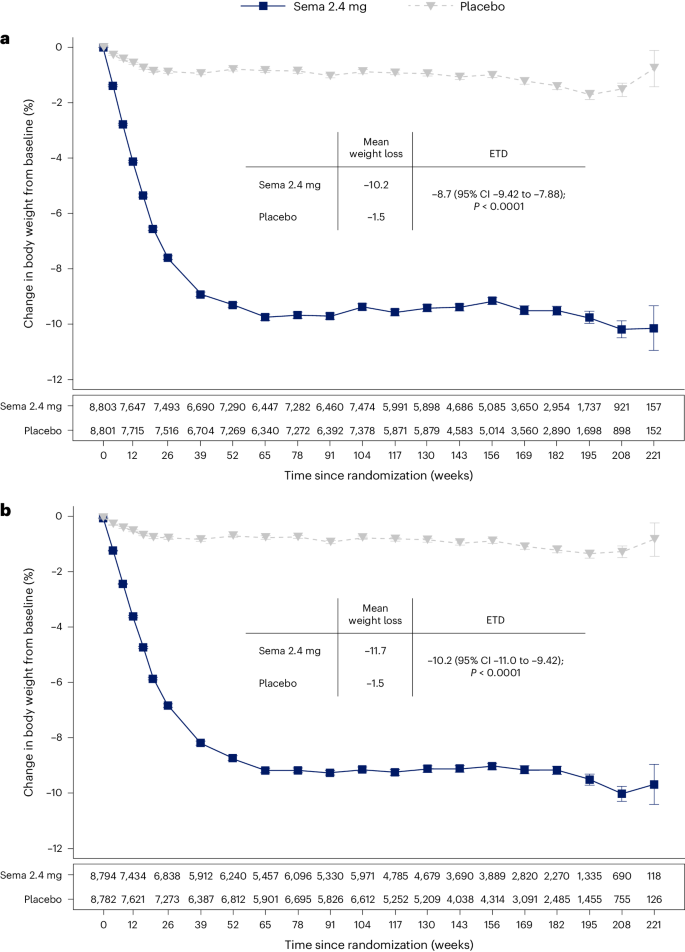
a , b , Observed data from the in-trial period ( a ) and first on-treatment ( b ). The symbols are the observed means, and error bars are ±s.e.m. Numbers shown below each panel represent the number of patients contributing to the means. Analysis of covariance with treatment and baseline values was used to estimate the treatment difference. Exact P values are 1.323762 × 10 −94 and 9.80035 × 10 −100 for a and b , respectively. P values are two-sided and are not adjusted for multiplicity. ETD, estimated treatment difference; sema, semaglutide.
Categorical weight loss and individual body weight change
Among in-trial (intention-to-treat principle) patients at week 104, weight loss of ≥5%, ≥10%, ≥15%, ≥20% and ≥25% was achieved by 67.8%, 44.2%, 22.9%, 11.0% and 4.9%, respectively, of those treated with semaglutide compared with 21.3%, 6.9%, 1.7%, 0.6% and 0.1% of those receiving placebo (Fig. 2a ). Individual weight changes at 104 weeks for the in-trial populations for semaglutide and placebo are depicted in Fig. 2b and Fig. 2c , respectively. These waterfall plots show the variation in weight-loss response that occurs with semaglutide and placebo and show that weight loss is more prominent with semaglutide than placebo.
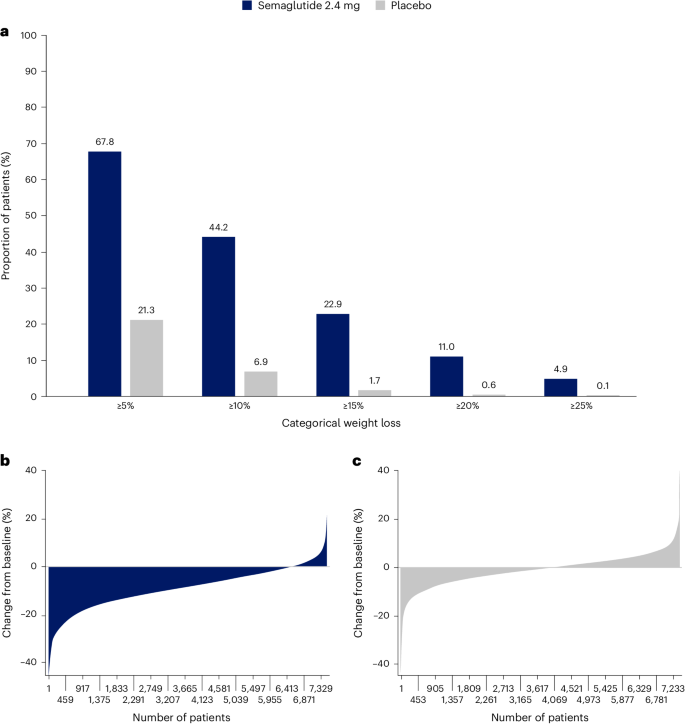
a , Categorical weight loss from baseline at week 104 for semaglutide and placebo. Data from the in-trial period. Bars depict the proportion (%) of patients receiving semaglutide or placebo who achieved ≥5%, ≥10%, ≥15%, ≥20% and ≥25% weight loss. b , c , Percentage change in body weight for individual patients from baseline to week 104 for semaglutide ( b ) and placebo ( c ). Each patient’s percentage change in body weight is plotted as a single bar.
Change in WC
WC change from baseline to 104 weeks has been reported previously in the primary outcome paper 21 . The trajectory of WC change mirrored that of the change in body weight. At week 208, average reduction in WC was −7.7 cm with semaglutide versus −1.3 cm with placebo, with a treatment difference of −6.4 cm (95% CI −7.18 to −5.61; P < 0.0001) 21 .
WC cutoff points
We analyzed achievement of sex- and race-specific cutoff points for WC by BMI <35 kg m − 2 or ≥35 kg m − 2 , because for BMI >35 kg m − 2 , WC is more difficult technically and, thus, less accurate as a risk predictor 4 , 25 , 26 . Within the SELECT population with BMI <35 kg m − 2 at baseline, 15.0% and 14.3% of the semaglutide and placebo groups, respectively, were below the sex- and race-specific WC cutoff points. At week 104, 41.2% fell below the sex- and race-specific cutoff points for the semaglutide group, compared with only 18.0% for the placebo group (Fig. 3 ).
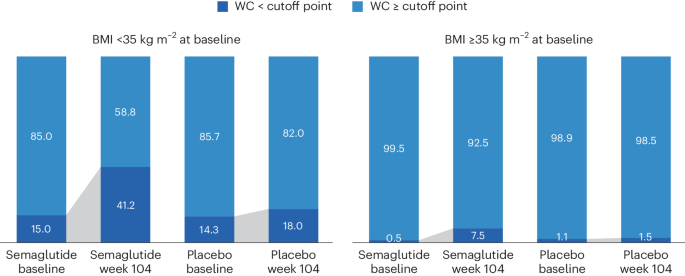
WC cutoff points; Asian women <80 cm, non-Asian women <88 cm, Asian men <88 cm, non-Asian men <102 cm.
Waist-to-height ratio
At baseline, mean WHtR was 0.66 for the study population. The lowest tertile of the SELECT population at baseline had a mean WHtR <0.62, which is higher than the cutoff point of 0.5 used to indicate increased cardiometabolic risk 27 , suggesting that the trial population had high WCs. At week 208, in the group randomized to semaglutide, there was a relative reduction of 6.9% in WHtR compared with 1.0% in placebo (treatment difference −5.87% points; 95% CI −6.56 to −5.17; P < 0.0001).
BMI category change
At week 104, 52.4% of patients treated with semaglutide achieved improvement in BMI category compared with 15.7% of those receiving placebo. Proportions of patients in the BMI categories at baseline and week 104 are shown in Fig. 4 , which depicts in-trial patients receiving semaglutide and placebo. The BMI category change reflects the superior weight loss with semaglutide, which resulted in fewer patients being in the higher BMI categories after 104 weeks. In the semaglutide group, 12.0% of patients achieved a BMI <25 kg m − 2 , which is considered the healthy BMI category, compared with 1.2% for placebo; per study inclusion criteria, no patients were in this category at baseline. The proportion of patients with obesity (BMI ≥30 kg m − 2 ) fell from 71.0% to 43.3% in the semaglutide group versus 71.9% to 67.9% in the placebo group.
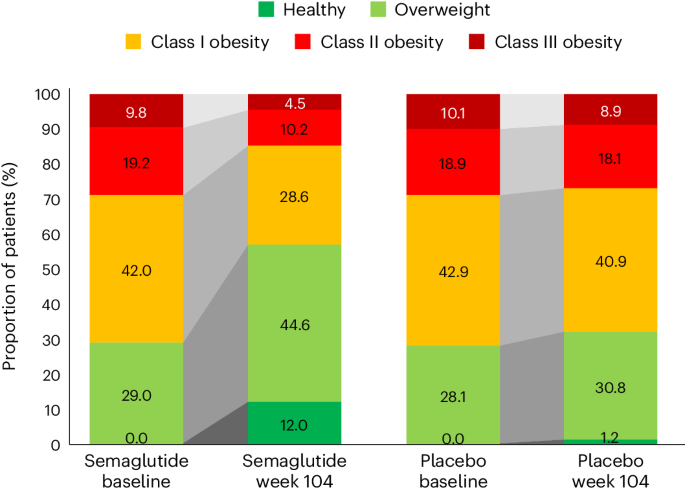
In the semaglutide group, 12.0% of patients achieved normal weight status at week 104 (from 0% at baseline), compared with 1.2% (from 0% at baseline) for placebo. BMI classes: healthy (BMI <25 kg m − 2 ), overweight (25 to <30 kg m − 2 ), class I obesity (30 to <35 kg m − 2 ), class II obesity (35 to <40 kg m − 2 ) and class III obesity (BMI ≥40 kg m − 2 ).
Weight and anthropometric outcomes by subgroups
The forest plot illustrated in Fig. 5 displays mean body weight percentage change from baseline to week 104 for semaglutide relative to placebo in prespecified subgroups. Similar relationships are depicted for WC changes in prespecified subgroups shown in Extended Data Fig. 1 . The effect of semaglutide (versus placebo) on mean percentage body weight loss as well as reduction in WC was found to be heterogeneous across several population subgroups. Women had a greater difference in mean weight loss with semaglutide versus placebo (−11.1% (95% CI −11.56 to −10.66) versus −7.5% in men (95% CI −7.78 to −7.23); P < 0.0001). There was a linear relationship between age category and degree of mean weight loss, with younger age being associated with progressively greater mean weight loss, but the actual mean difference by age group is small. Similarly, BMI category had small, although statistically significant, associations. Those with WHtR less than the median experienced slightly lower mean body weight change than those above the median, with estimated treatment differences −8.04% (95% CI −8.37 to −7.70) and −8.99% (95% CI −9.33 to −8.65), respectively ( P < 0.0001). Patients from Asia and of Asian race experienced slightly lower mean weight loss (estimated treatment difference with semaglutide for Asian race −7.27% (95% CI −8.09 to −6.46; P = 0.0147) and for Asia −7.30 (95% CI −7.97 to −6.62; P = 0.0016)). There was no difference in weight loss with semaglutide associated with ethnicity (estimated treatment difference for Hispanic −8.53% (95% CI −9.28 to −7.76) or non-Hispanic −8.52% (95% CI −8.77 to 8.26); P = 0.9769), glycemic status (estimated treatment difference for prediabetes −8.53% (95% CI −8.83 to −8.24) or normoglycemia −8.48% (95% CI −8.88 to −8.07; P = 0.8188) or renal function (estimated treatment difference for estimated glomerular filtration rate (eGFR) <60 or ≥60 ml min −1 1.73 m − 2 being −8.50% (95% CI −9.23 to −7.76) and −8.52% (95% CI −8.77 to −8.26), respectively ( P = 0.9519)).
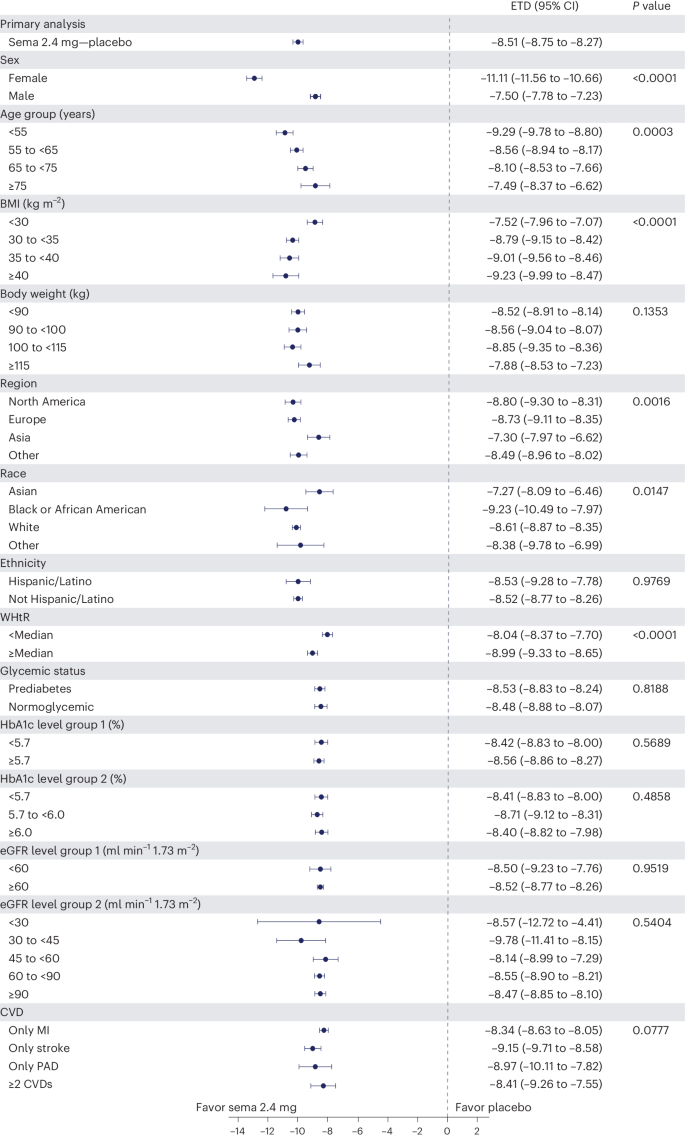
Data from the in-trial period. N = 17,604. P values represent test of no interaction effect. P values are two-sided and are not adjusted for multiplicity. The dots show estimated treatment differences, and the error bars show 95% CIs. Details of the statistical models are available in Methods . ETD, estimated treatment difference; HbA1c, glycated hemoglobin; MI, myocardial infarction; PAD, peripheral artery disease; sema, semaglutide.
Safety and tolerability according to baseline BMI category
We reported in the primary outcome of the SELECT trial that adverse events (AEs) leading to permanent discontinuation of the trial product occurred in 1,461 patients (16.6%) in the semaglutide group and 718 patients (8.2%) in the placebo group ( P < 0.001) 21 . For this analysis, we evaluated the cumulative incidence of AEs leading to trial product discontinuation by treatment assignment and by BMI category (Fig. 6 ). For this analysis, with death modeled as a competing risk, we tracked the proportion of in-trial patients for whom drug was withdrawn or interrupted for the first time (Fig. 6 , left) or cumulative discontinuations (Fig. 6 , right). Both panels of Fig. 6 depict a graded increase in the proportion discontinuing semaglutide, but not placebo. For lower BMI classes, discontinuation rates are higher in the semaglutide group but not the placebo group.
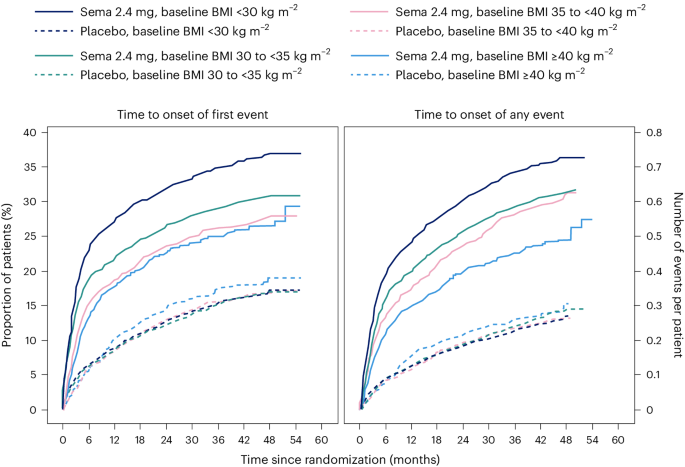
Data are in-trial from the full analysis set. sema, semaglutide.
We reported in the primary SELECT analysis that serious adverse events (SAEs) were reported by 2,941 patients (33.4%) in the semaglutide arm and by 3,204 patients (36.4%) in the placebo arm ( P < 0.001) 21 . For this study, we analyzed SAE rates by person-years of treatment exposure for BMI classes (<30 kg m − 2 , 30 to <35 kg m − 2 , 35 to <40 kg m − 2 , and ≥40 kg m − 2 ) and provide these data in Supplementary Table 2 . We also provide an analysis of the most common categories of SAEs. Semaglutide was associated with lower SAEs, primarily driven by CV event and infections. Within each obesity class (<30 kg m − 2 , 30 to <35 kg m − 2 , 35 to <40 kg m − 2 , and ≥40 kg m − 2 ), there were fewer SAEs in the group receiving semaglutide compared with placebo. Rates (events per 100 years of observation) of SAEs were 43.23, 43.54, 51.07 and 47.06 for semaglutide and 50.48, 49.66, 52.73 and 60.85 for placebo, with no evidence of heterogeneity. There was no detectable difference in hepatobiliary or gastrointestinal SAEs comparing semaglutide with placebo in any of the four BMI classes we evaluated.
The analyses of weight effects of the SELECT study presented here reveal that patients assigned to once-weekly subcutaneous semaglutide 2.4 mg lost significantly more weight than those receiving placebo. The weight-loss trajectory with semaglutide occurred over 65 weeks and was sustained up to 4 years. Likewise, there were similar improvements in the semaglutide group for anthropometrics (WC and WHtR). The weight loss was associated with a greater proportion of patients receiving semaglutide achieving improvement in BMI category, healthy BMI (<25 kg m − 2 ) and falling below the WC cutoff point above which increased cardiometabolic risk for the sex and race is greater 22 , 23 . Furthermore, both sexes, all races, all body sizes and those from all geographic regions were able to achieve clinically meaningful weight loss. There was no evidence of increased SAEs based on BMI categories, although lower BMI category was associated with increased rates of trial product discontinuation, probably reflecting exposure to a higher level of drug in lower BMI categories. These data, representing the longest clinical trial of the effects of semaglutide versus placebo on weight, establish the safety and durability of semaglutide effects on weight loss and maintenance in a geographically and racially diverse population of adult men and women with overweight and obesity but not diabetes. The implications of weight loss of this degree in such a diverse population suggests that it may be possible to impact the public health burden of the multiple morbidities associated with obesity. Although our trial focused on CV events, many chronic diseases would benefit from effective weight management 28 .
There were variations in the weight-loss response. Individual changes in body weight with semaglutide and placebo were striking; still, 67.8% achieved 5% or more weight loss and 44.2% achieved 10% weight loss with semaglutide at 2 years, compared with 21.3% and 6.9%, respectively, for those receiving placebo. Our first on-treatment analysis demonstrated that those on-drug lost more weight than those in-trial, confirming the effect of drug exposure. With semaglutide, lower BMI was associated with less percentage weight loss, and women lost more weight on average than men (−11.1% versus −7.5% treatment difference from placebo); however, in all cases, clinically meaningful mean weight loss was achieved. Although Asian patients lost less weight on average than patients of other races (−7.3% more than placebo), Asian patients were more likely to be in the lowest BMI category (<30 kg m − 2 ), which is known to be associated with less weight loss, as discussed below. Clinically meaningful weight loss was evident in the semaglutide group within a broad range of baseline categories for glycemia and body anthropometrics. Interestingly, at 2 years, a significant proportion of the semaglutide-treated group fell below the sex- and race-specific WC cutoff points, especially in those with BMI <35 kg m − 2 , and a notable proportion (12.0%) fell below the BMI cutoff point of 25 kg m − 2 , which is deemed a healthy BMI in those without unintentional weight loss. As more robust weight loss is possible with newer medications, achieving and maintaining these cutoff point targets may become important benchmarks for tracking responses.
The overall safety profile did not reveal any new signals from prior studies, and there were no BMI category-related associations with AE reporting. The analysis did reveal that tolerability may differ among specific BMI classes, since more discontinuations occurred with semaglutide among lower BMI classes. Potential contributors may include a possibility of higher drug exposure in lower BMI classes, although other explanations, including differences in motivation and cultural mores regarding body size, cannot be excluded.
Is the weight loss in SELECT less than expected based on prior studies with the drug? In STEP 1, a large phase 3 study of once-weekly subcutaneous semaglutide 2.4 mg in individuals without diabetes but with BMI >30 kg m − 2 or 27 kg m − 2 with at least one obesity-related comorbidity, the mean weight loss was −14.9% at week 68, compared with −2.4% with placebo 14 . Several reasons may explain the observation that the mean treatment difference was −12.5% in STEP 1 and −8.7% in SELECT. First, SELECT was designed as a CV outcomes trial and not a weight-loss trial, and weight loss was only a supportive secondary endpoint in the trial design. Patients in STEP 1 were desirous of weight loss as a reason for study participation and received structured lifestyle intervention (which included a −500 kcal per day diet with 150 min per week of physical activity). In the SELECT trial, patients did not enroll for the specific purpose of weight loss and received standard of care covering management of CV risk factors, including medical treatment and healthy lifestyle counseling, but without a specific focus on weight loss. Second, the respective study populations were quite different, with STEP 1 including a younger, healthier population with more women (73.1% of the semaglutide arm in STEP 1 versus 27.7% in SELECT) and higher mean BMI (37.8 kg m − 2 versus 33.3 kg m − 2 , respectively) 14 , 21 . Third, major differences existed between the respective trial protocols. Patients in the semaglutide treatment arm of STEP 1 were more likely to be exposed to the medication at the full dose of 2.4 mg than those in SELECT. In SELECT, investigators were allowed to slow, decrease or pause treatment. By 104 weeks, approximately 77% of SELECT patients on dose were receiving the target semaglutide 2.4 mg weekly dose, which is lower than the corresponding proportion of patients in STEP 1 (89.6% were receiving the target dose at week 68) 14 , 21 . Indeed, in our first on-treatment analysis at week 208, weight loss was greater (−11.7% for semaglutide) compared with the in-trial analysis (−10.2% for semaglutide). Taken together, all these issues make less weight loss an expected finding in SELECT, compared with STEP 1.
The SELECT study has some limitations. First, SELECT was not a primary prevention trial, and the data should not be extrapolated to all individuals with overweight and obesity to prevent major adverse CV events. Although the data set is rich in numbers and diversity, it does not have the numbers of individuals in racial subgroups that may have revealed potential differential effects. SELECT also did not include individuals who have excess abnormal body fat but a BMI <27 kg m − 2 . Not all individuals with increased CV risk have BMI ≥27 kg m − 2 . Thus, the study did not include Asian patients who qualify for treatment with obesity medications at lower BMI and WC cutoff points according to guidelines in their countries 29 . We observed that Asian patients were less likely to be in the higher BMI categories of SELECT and that the population of those with BMI <30 kg m − 2 had a higher percentage of Asian race. Asian individuals would probably benefit from weight loss and medication approaches undertaken at lower BMI levels in the secondary prevention of CVD. Future studies should evaluate CV risk reduction in Asian individuals with high CV risk and BMI <27 kg m − 2 . Another limitation is the lack of information on body composition, beyond the anthropometric measures we used. It would be meaningful to have quantitation of fat mass, lean mass and muscle mass, especially given the wide range of body size in the SELECT population.
An interesting observation from this SELECT weight loss data is that when BMI is ≤30 kg m − 2 , weight loss on a percentage basis is less than that observed across higher classes of BMI severity. Furthermore, as BMI exceeds 30 kg m − 2 , weight loss amounts are more similar for class I, II and III obesity. This was also observed in Look AHEAD, a lifestyle intervention study for weight loss 30 . The proportion (percentage) of weight loss seems to be less, on average, in the BMI <30 kg m − 2 category relative to higher BMI categories, despite their receiving of the same treatment and even potentially higher exposure to the drug for weight loss 30 . Weight loss cannot continue indefinitely. There is a plateau of weight that occurs after weight loss with all treatments for weight management. This plateau has been termed the ‘set point’ or ‘settling point’, a body weight that is in harmony with the genetic and environmental determinants of body weight and adiposity 31 . Perhaps persons with BMI <30 kg m − 2 are closer to their settling point and have less weight to lose to reach it. Furthermore, the cardiometabolic benefits of weight loss are driven by reduction in the abnormal ectopic and visceral depots of fat, not by reduction of subcutaneous fat stores in the hips and thighs. The phenotype of cardiometabolic disease but lower BMI (<30 kg m − 2 ) may be one where reduction of excess abnormal and dysfunctional body fat does not require as much body mass reduction to achieve health improvement. We suspect this may be the case and suggest further studies to explore this aspect of weight-loss physiology.
In conclusion, this analysis of the SELECT study supports the broad use of once-weekly subcutaneous semaglutide 2.4 mg as an aid to CV event reduction in individuals with overweight or obesity without diabetes but with preexisting CVD. Semaglutide 2.4 mg safely and effectively produced clinically significant weight loss in all subgroups based on age, sex, race, glycemia, renal function and anthropometric categories. Furthermore, the weight loss was sustained over 4 years during the trial.
Trial design and participants
The current work complies with all relevant ethical regulations and reports a prespecified analysis of the randomized, double-blind, placebo-controlled SELECT trial ( NCT03574597 ), details of which have been reported in papers describing study design and rationale 32 , baseline characteristics 24 and the primary outcome 21 . SELECT evaluated once-weekly subcutaneous semaglutide 2.4 mg versus placebo to reduce the risk of major adverse cardiac events (a composite endpoint comprising CV death, nonfatal myocardial infarction or nonfatal stroke) in individuals with established CVD and overweight or obesity, without diabetes. The protocol for SELECT was approved by national and institutional regulatory and ethical authorities in each participating country. All patients provided written informed consent before beginning any trial-specific activity. Eligible patients were aged ≥45 years, with a BMI of ≥27 kg m − 2 and established CVD defined as at least one of the following: prior myocardial infarction, prior ischemic or hemorrhagic stroke, or symptomatic peripheral artery disease. Additional inclusion and exclusion criteria can be found elsewhere 32 .
Human participants research
The trial protocol was designed by the trial sponsor, Novo Nordisk, and the academic Steering Committee. A global expert panel of physician leaders in participating countries advised on regional operational issues. National and institutional regulatory and ethical authorities approved the protocol, and all patients provided written informed consent.
Study intervention and patient management
Patients were randomly assigned in a double-blind manner and 1:1 ratio to receive once-weekly subcutaneous semaglutide 2.4 mg or placebo. The starting dose was 0.24 mg once weekly, with dose increases every 4 weeks (to doses of 0.5, 1.0, 1.7 and 2.4 mg per week) until the target dose of 2.4 mg was reached after 16 weeks. Patients who were unable to tolerate dose escalation due to AEs could be managed by extension of dose-escalation intervals, treatment pauses or maintenance at doses below the 2.4 mg per week target dose. Investigators were allowed to reduce the dose of study product if tolerability issues arose. Investigators were provided with guidelines for, and encouraged to follow, evidence-based recommendations for medical treatment and lifestyle counseling to optimize management of underlying CVD as part of the standard of care. The lifestyle counseling was not targeted at weight loss. Additional intervention descriptions are available 32 .
Sex, race, body weight, height and WC measurements
Sex and race were self-reported. Body weight was measured without shoes and only wearing light clothing; it was measured on a digital scale and recorded in kilograms or pounds (one decimal with a precision of 0.1 kg or lb), with preference for using the same scale throughout the trial. The scale was calibrated yearly as a minimum unless the manufacturer certified that calibration of the weight scales was valid for the lifetime of the scale. Height was measured without shoes in centimeters or inches (one decimal with a precision of 0.1 cm or inches). At screening, BMI was calculated by the electronic case report form. WC was defined as the abdominal circumference located midway between the lower rib margin and the iliac crest. Measures were obtained in a standing position with a nonstretchable measuring tape and to the nearest centimeter or inch. The patient was asked to breathe normally. The tape touched the skin but did not compress soft tissue, and twists in the tape were avoided.
The following endpoints relevant to this paper were assessed at randomization (week 0) to years 2, 3 and 4: change in body weight (%); proportion achieving weight loss ≥5%, ≥10%, ≥15% and ≥20%; change in WC (cm); and percentage change in WHtR (cm cm −1 ). Improvement in BMI category (defined as being in a lower BMI class) was assessed at week 104 compared with baseline according to BMI classes: healthy (BMI <25 kg m − 2 ), overweight (25 to <30 kg m − 2 ), class I obesity (30 to <35 kg m − 2 ), class II obesity (35 to <40 kg m − 2 ) and class III obesity (≥40 kg m − 2 ). The proportions of individuals with BMI <35 or ≥35 kg m − 2 who achieved sex- and race-specific cutoff points for WC (indicating increased metabolic risk) were evaluated at week 104. The WC cutoff points were as follows: Asian women <80 cm, non-Asian women <88 cm, Asian men <88 cm and non-Asian men <102 cm.
Overall, 97.1% of the semaglutide group and 96.8% of the placebo group completed the trial. During the study, 30.6% of those assigned to semaglutide did not complete drug treatment, compared with 27.0% for placebo.
Statistical analysis
The statistical analyses for the in-trial period were based on the intention-to-treat principle and included all randomized patients irrespective of adherence to semaglutide or placebo or changes to background medications. Continuous endpoints were analyzed using an analysis of covariance model with treatment as a fixed factor and baseline value of the endpoint as a covariate. Missing data at the landmark visit, for example, week 104, were imputed using a multiple imputation model and done separately for each treatment arm and included baseline value as a covariate and fit to patients having an observed data point (irrespective of adherence to randomized treatment) at week 104. The fit model is used to impute values for all patients with missing data at week 104 to create 500 complete data sets. Rubin’s rules were used to combine the results. Estimated means are provided with s.e.m., and estimated treatment differences are provided with 95% CI. Binary endpoints were analyzed using logistic regression with treatment and baseline value as a covariate, where missing data were imputed by first using multiple imputation as described above and then categorizing the imputed data according to the endpoint, for example, body weight percentage change at week 104 of <0%. Subgroup analyses for continuous and binary endpoints also included the subgroup and interaction between treatment and subgroup as fixed factors. Because some patients in both arms continued to be followed but were off treatment, we also analyzed weight loss by first on-treatment group (observation period until first time being off treatment for >35 days) to assess a more realistic picture of weight loss in those adhering to treatment. CIs were not adjusted for multiplicity and should therefore not be used to infer definitive treatment effects. All statistical analyses were performed with SAS software, version 9.4 TS1M5 (SAS Institute).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data will be shared with bona fide researchers who submit a research proposal approved by the independent review board. Individual patient data will be shared in data sets in a deidentified and anonymized format. Information about data access request proposals can be found at https://www.novonordisk-trials.com/ .
Obesity and overweight. World Health Organization https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (2021).
Cornier, M. A. et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation 124 , 1996–2019 (2011).
Article PubMed Google Scholar
Afshin, A. et al. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377 , 13–27 (2017).
Jensen, M. D. et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 63 , 2985–3023 (2014).
Poirier, P. et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss: an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation 113 , 898–918 (2006).
Dai, H. et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the Global Burden of Disease Study. PLoS Med. 17 , e1003198 (2020).
Article PubMed PubMed Central Google Scholar
Ndumele, C. E. et al. Cardiovascular–kidney–metabolic health: a presidential advisory from the American Heart Association. Circulation 148 , 1606–1635 (2023).
Garvey, W. T. et al. American Association of Clinical Endocrinologists and American College of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr. Pr. 22 , 1–203 (2016).
Article Google Scholar
Ryan, D. H. & Yockey, S. R. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. Curr. Obes. Rep. 6 , 187–194 (2017).
Wing, R. R. et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 34 , 1481–1486 (2011).
Article CAS PubMed PubMed Central Google Scholar
Wadden, T. A., Tronieri, J. S. & Butryn, M. L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 75 , 235–251 (2020).
Tchang, B. G. et al. Pharmacologic treatment of overweight and obesity in adults. in (eds. Feingold, K. R. et al.) Endotext https://www.ncbi.nlm.nih.gov/books/NBK279038/ (MDText.com, 2000).
Müller, T. D., Blüher, M., Tschöp, M. H. & DiMarchi, R. D. Anti-obesity drug discovery: advances and challenges. Nat. Rev. Drug Discov. 21 , 201–223 (2022).
Wilding, J. P. H. et al. Once-weekly semaglutide in adults with overweight or obesity. N. Engl. J. Med. 384 , 989–1002 (2021).
Article CAS PubMed Google Scholar
Wegovy (semaglutide) summary of product characteristics. European Medicines Agency https://www.ema.europa.eu/en/documents/product-information/wegovy-epar-product-information_en.pdf (2023).
WEGOVY (semaglutide) prescribing information. Food and Drug Administration https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215256s007lbl.pdf (2023).
Sorli, C. et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): a double-blind, randomised, placebo-controlled, parallel-group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol. 5 , 251–260 (2017).
Ozempic (semaglutide) summary of product characteristics. European Medicines Agency https://www.ema.europa.eu/en/documents/product-information/ozempic-epar-product-information_en.pdf (2023).
OZEMPIC (semaglutide) prescribing information. Food and Drug Administration https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209637lbl.pdf (2017).
Marso, S. P. et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 375 , 1834–1844 (2016).
Lincoff, A. M. et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N. Engl. J. Med. 389 , 2221–2232 (2023).
Ross, R. et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 16 , 177–189 (2020).
Snijder, M. B., van Dam, R. M., Visser, M. & Seidell, J. C. What aspects of body fat are particularly hazardous and how do we measure them? Int. J. Epidemiol. 35 , 83–92 (2006).
Lingvay, I. et al. Semaglutide for cardiovascular event reduction in people with overweight or obesity: SELECT study baseline characteristics. Obesity 31 , 111–122 (2023).
Basset, J. The Asia-Pacific perspective: redefining obesity and its treatment. International Diabetes Institute, World Health Organization Regional Office for the Western Pacific, International Association for the Study of Obesity & International Obesity Task Force https://www.vepachedu.org/TSJ/BMI-Guidelines.pdf (2000).
Hu, F. in Obesity Epidemiology (ed. Hu, F.) 53–83 (Oxford University Press, 2008).
Browning, L. M., Hsieh, S. D. & Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr. Res. Rev. 23 , 247–269 (2010).
Sattar, N. et al. Treating chronic diseases without tackling excess adiposity promotes multimorbidity. Lancet Diabetes Endocrinol. 11 , 58–62 (2023).
Obesity classification. World Obesity https://www.worldobesity.org/about/about-obesity/obesity-classification (2022).
Unick, J. L. et al. Effectiveness of lifestyle interventions for individuals with severe obesity and type 2 diabetes: results from the Look AHEAD trial. Diabetes Care 34 , 2152–2157 (2011).
Speakman, J. R. et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis. Model. Mech. 4 , 733–745 (2011).
Ryan, D. H. et al. Semaglutide effects on cardiovascular outcomes in people with overweight or obesity (SELECT) rationale and design. Am. Heart J. 229 , 61–69 (2020).
Download references
Acknowledgements
Editorial support was provided by Richard Ogilvy-Stewart of Apollo, OPEN Health Communications, and funded by Novo Nordisk A/S, in accordance with Good Publication Practice guidelines ( www.ismpp.org/gpp-2022 ).
Author information
Authors and affiliations.
Pennington Biomedical Research Center, Baton Rouge, LA, USA
Donna H. Ryan
Department of Internal Medicine/Endocrinology and Peter O’ Donnell Jr. School of Public Health, University of Texas Southwestern Medical Center, Dallas, TX, USA
Ildiko Lingvay
Institute of Cardiovascular Science, University College London, London, UK
John Deanfield
VA Puget Sound Health Care System and University of Washington, Seattle, WA, USA
Steven E. Kahn
Novo Nordisk A/S, Søborg, Denmark
Eric Barros, G. Kees Hovingh, Ole Kleist Jeppesen & Tugce Kalayci Oral
Endocrinology and Metabolism Institute, Cleveland Clinic, Cleveland, OH, USA
Bartolome Burguera
Institute of Genetics and Cancer, University of Edinburgh, Edinburgh, UK
Helen M. Colhoun
Obesity Unit, Department of Endocrinology, Hospital das Clínicas, University of São Paulo, São Paulo, Brazil
Cintia Cercato
Internal Medicine Department D, Hasharon Hospital-Rabin Medical Center, Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
Dror Dicker
Center for Obesity Medicine and Metabolic Performance, Department of Surgery, University of Texas McGovern Medical School, Houston, TX, USA
Deborah B. Horn
First Department of Propaedeutic Internal Medicine, School of Medicine, National and Kapodistrian University of Athens, Athens, Greece
Alexander Kokkinos
Department of Cardiovascular Medicine, Cleveland Clinic, and Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH, USA
A. Michael Lincoff
Institute of Endocrinology & Diabetes, University of Lübeck, Lübeck, Germany
Sebastian M. Meyhöfer
Cardiovascular Division, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA, USA
Jorge Plutzky
University of Groningen, University Medical Center Groningen, Department of Endocrinology, Groningen, the Netherlands
André P. van Beek
Department of Cardiovascular and Metabolic Medicine, University of Liverpool, Liverpool, UK
John P. H. Wilding
Northwestern University Feinberg School of Medicine, Chicago, IL, USA
Robert F. Kushner
You can also search for this author in PubMed Google Scholar
Contributions
D.H.R., I.L. and S.E.K. contributed to the study design. D.B.H., I.L., D.D., A.K., S.M.M., A.P.v.B., C.C. and J.P.H.W. were study investigators. D.B.H., I.L., D.D., A.K., S.M.M., A.P.v.B., C.C. and J.P.H.W. enrolled patients. D.H.R. was responsible for data analysis and manuscript preparation. All authors contributed to data interpretation, review, revisions and final approval of the manuscript.
Corresponding author
Correspondence to Donna H. Ryan .
Ethics declarations
Competing interests.
D.H.R. declares having received consulting honoraria from Altimmune, Amgen, Biohaven, Boehringer Ingelheim, Calibrate, Carmot Therapeutics, CinRx, Eli Lilly, Epitomee, Gila Therapeutics, IFA Celtics, Novo Nordisk, Pfizer, Rhythm, Scientific Intake, Wondr Health and Zealand Pharma; she declares she received stock options from Calibrate, Epitomee, Scientific Intake and Xeno Bioscience. I.L. declares having received research funding (paid to institution) from Novo Nordisk, Sanofi, Mylan and Boehringer Ingelheim. I.L. received advisory/consulting fees and/or other support from Altimmune, AstraZeneca, Bayer, Biomea, Boehringer Ingelheim, Carmot Therapeutics, Cytoki Pharma, Eli Lilly, Intercept, Janssen/Johnson & Johnson, Mannkind, Mediflix, Merck, Metsera, Novo Nordisk, Pharmaventures, Pfizer, Regeneron, Sanofi, Shionogi, Structure Therapeutics, Target RWE, Terns Pharmaceuticals, The Comm Group, Valeritas, WebMD and Zealand Pharma. J.D. declares having received consulting honoraria from Amgen, Boehringer Ingelheim, Merck, Pfizer, Aegerion, Novartis, Sanofi, Takeda, Novo Nordisk and Bayer, and research grants from British Heart Foundation, MRC (UK), NIHR, PHE, MSD, Pfizer, Aegerion, Colgate and Roche. S.E.K. declares having received consulting honoraria from ANI Pharmaceuticals, Boehringer Ingelheim, Eli Lilly, Merck, Novo Nordisk and Oramed, and stock options from AltPep. B.B. declares having received honoraria related to participation on this trial and has no financial conflicts related to this publication. H.M.C. declares being a stockholder and serving on an advisory panel for Bayer; receiving research grants from Chief Scientist Office, Diabetes UK, European Commission, IQVIA, Juvenile Diabetes Research Foundation and Medical Research Council; serving on an advisory board and speaker’s bureau for Novo Nordisk; and holding stock in Roche Pharmaceuticals. C.C. declares having received consulting honoraria from Novo Nordisk, Eli Lilly, Merck, Brace Pharma and Eurofarma. D.D. declares having received consulting honoraria from Novo Nordisk, Eli Lilly, Boehringer Ingelheim and AstraZeneca, and received research grants through his affiliation from Novo Nordisk, Eli Lilly, Boehringer Ingelheim and Rhythm. D.B.H. declares having received research grants through her academic affiliation from Novo Nordisk and Eli Lilly, and advisory/consulting honoraria from Novo Nordisk, Eli Lilly and Gelesis. A.K. declares having received research grants through his affiliation from Novo Nordisk and Pharmaserve Lilly, and consulting honoraria from Pharmaserve Lilly, Sanofi-Aventis, Novo Nordisk, MSD, AstraZeneca, ELPEN Pharma, Boehringer Ingelheim, Galenica Pharma, Epsilon Health and WinMedica. A.M.L. declares having received honoraria from Novo Nordisk, Eli Lilly, Akebia Therapeutics, Ardelyx, Becton Dickinson, Endologix, FibroGen, GSK, Medtronic, Neovasc, Provention Bio, ReCor, BrainStorm Cell Therapeutics, Alnylam and Intarcia for consulting activities, and research funding to his institution from AbbVie, Esperion, AstraZeneca, CSL Behring, Novartis and Eli Lilly. S.M.M. declares having received consulting honoraria from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Daichii-Sankyo, esanum, Gilead, Ipsen, Eli Lilly, Novartis, Novo Nordisk, Sandoz and Sanofi; he declares he received research grants from AstraZeneca, Eli Lilly and Novo Nordisk. J.P. declares having received consulting honoraria from Altimmune, Amgen, Esperion, Merck, MJH Life Sciences, Novartis and Novo Nordisk; he has received a grant, paid to his institution, from Boehringer Ingelheim and holds the position of Director, Preventive Cardiology, at Brigham and Women’s Hospital. A.P.v.B. is contracted via the University of Groningen (no personal payment) to undertake consultancy for Novo Nordisk, Eli Lilly and Boehringer Ingelheim. J.P.H.W. is contracted via the University of Liverpool (no personal payment) to undertake consultancy for Altimmune, AstraZeneca, Boehringer Ingelheim, Cytoki, Eli Lilly, Napp, Novo Nordisk, Menarini, Pfizer, Rhythm Pharmaceuticals, Sanofi, Saniona, Tern Pharmaceuticals, Shionogi and Ysopia. J.P.H.W. also declares personal honoraria/lecture fees from AstraZeneca, Boehringer Ingelheim, Medscape, Napp, Menarini, Novo Nordisk and Rhythm. R.F.K. declares having received consulting honoraria from Novo Nordisk, Weight Watchers, Eli Lilly, Boehringer Ingelheim, Pfizer, Structure and Altimmune. E.B., G.K.H., O.K.J. and T.K.O. are employees of Novo Nordisk A/S.
Peer review
Peer review information.
Nature Medicine thanks Christiana Kartsonaki, Peter Rossing, Naveed Sattar and Vikas Sridhar for their contribution to the peer review of this work. Primary Handling Editor: Sonia Muliyil, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended data fig. 1 effect of semaglutide treatment or placebo on waist circumference from baseline to week 104 by subgroups..
Data from the in-trial period. N = 17,604. P values represent test of no interaction effect. P values are two-sided and not adjusted for multiplicity. The dots show estimated treatment differences and the error bars show 95% confidence intervals. Details of the statistical models are available in Methods . BMI, body mass index; CI, confidence interval; CV, cardiovascular; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate; ETD, estimated treatment difference; HbA1c, glycated hemoglobin; MI, myocardial infarction; PAD, peripheral artery disease; sema, semaglutide.
Supplementary information
Reporting summary, supplementary tables 1 and 2.
Supplementary Table 1. Baseline characteristics by BMI class. Data are represented as number and percentage of patients. Renal function categories were based on the eGFR as per Chronic Kidney Disease Epidemiology Collaboration. Albuminuria categories were based on UACR. Smoking was defined as smoking at least one cigarette or equivalent daily. The category ‘Other’ for CV inclusion criteria includes patients where it is unknown if the patient fulfilled only one or several criteria and patients who were randomized in error and did not fulfill any criteria. Supplementary Table 2. SAEs according to baseline BMI category. P value: two-sided P value from Fisher’s exact test for test of no difference.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ryan, D.H., Lingvay, I., Deanfield, J. et al. Long-term weight loss effects of semaglutide in obesity without diabetes in the SELECT trial. Nat Med (2024). https://doi.org/10.1038/s41591-024-02996-7
Download citation
Received : 01 March 2024
Accepted : 12 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1038/s41591-024-02996-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Text Messages With Financial Incentives for Men With Obesity : A Randomized Clinical Trial
- 1 NMAHP Research Unit, Pathfoot Building, Stirling University, United Kingdom
- 2 Faculty of Kinesiology, University of New Brunswick, Canada
- 3 Health Services Research Unit, University of Aberdeen, United Kingdom
- 4 Centre for Healthcare Randomised Trials, University of Aberdeen, United Kingdom
- 5 Health Economics Research Unit, University of Aberdeen, United Kingdom
- 6 School of Social and Political Sciences, University of Glasgow, United Kingdom
- 7 Institute for Social Marketing and Health, University of Stirling, United Kingdom
- 8 Centre for Public Health, Queen’s University Belfast, United Kingdom
- 9 Queen’s University Belfast, United Kingdom
- 10 Centre for Academic Primary Care, University of Bristol, United Kingdom
- Editorial Lifestyle Interventions for Obesity in the Era of GLP-1 Receptor Agonists Jamy D. Ard, MD; Kristina H. Lewis, MD; Justin B. Moore, PhD JAMA
- Original Investigation An Adaptive Behavioral Intervention for Weight Loss Management Bonnie Spring, PhD; Angela F. Pfammatter, PhD; Laura Scanlan, BA; Elyse Daly, BA; Jean Reading, PhD; Sam Battalio, MS; H. Gene McFadden, BA; Don Hedeker, PhD; Juned Siddique, PhD; Inbal Nahum-Shani, PhD JAMA
Question Do text messages with or without financial incentives promote weight loss in men with obesity?
Findings In this randomized trial that included 585 men with obesity, text messaging with behavioral messages combined with a financial incentive resulted in a 5% weight loss at 12 months, compared with weight loss of 3% for text messaging alone, and 1% for the control group. The difference in weight loss was statistically significant for the comparison between text messaging with financial incentives and the control group but not between the text messaging alone and the control group.
Meaning In men with obesity, a 12-month intervention consisting of text messaging with financial incentives resulted in modest but statistically significant weight loss compared with control.
Importance Effective weight loss interventions are needed for men with obesity.
Objective To determine whether an intervention that combined text messaging with financial incentives attained significant weight loss at the 12-month follow-up compared with the control group and whether an intervention of text messaging alone attained significant weight loss at the 12-month follow-up compared with the control group.
Design, Setting, and Participants An assessor-blinded randomized clinical trial conducted in Belfast, Bristol, and Glasgow areas in the UK. A total of 585 men with body mass index (BMI) of 30 or more were enrolled between July 2021 and May 2022. Final follow-up occurred June 2023.
Interventions Participants were randomly assigned to 12 months of behavioral focused text messages combined with financial incentives (n = 196), 12 months of behavioral focused text messages alone (n= 194), or a waiting list (control group; n= 195). The financial incentive consisted of a monetary reward that was lost if weight loss targets were not met. All participants received weight management information and a pedometer at baseline.
Main Outcomes and Measures The 2 primary comparisons were the 12-month comparison of within-participant weight change between the text messaging with financial incentive group and the control group and the comparison between the text messaging alone group and the control group (minimum clinically important difference, 3%). The P value defined for statistical significance was P < .025 for each comparison.
Results Of the 585 men (mean [SD] age, 50.7 [13.3] years; mean weight, 118.5 [19.9] kg; mean BMI, 37.7 [5.7]; 525 [90%] White), 227 (39%) lived in postal code areas with lower socioeconomic status, and 426 (73%) completed the 12-month follow-up. At the 12-month follow-up, compared with the control group, the mean percent weight change was significantly greater in the text messaging with financial incentive group (mean difference, −3.2%; 97.5% CI, −4.6% to −1.9%; P < .001) but was not significantly greater in the text messaging alone group (mean difference, −1.4%; 97.5% CI, −2.9% to 0.0, P = .05). The mean (SD) weight changes were −5.7 (7.4) kg for the text messaging with financial incentives group, −3.0 (7.5) kg for the text messaging alone group, and −1.5 (6.6) kg for the control group. The 12-month mean (SD) percentage weight changes from baseline were −4.8% (6.1%) for the text messaging with financial incentives group, −2.7% (6.3%) for text messaging alone group, and −1.3% (5.5%) for the control group. Of 366 adverse events reported, the most common were infections (83 [23%]). Of the 23 serious adverse events (6.3%), 12 (52%) occurred in the text messaging with financial incentives group, 5 (22%) in the texts messaging alone group, and 6 (26%) in the control group. None were considered related to participating in a trial group.
Conclusion and Relevance Among men with obesity, an intervention with text messaging with financial incentive significantly improved weight loss compared with a control group, whereas text messaging alone was not significantly better than the control condition. These findings support text messaging combined with financial incentives to attain weight loss in men with obesity.
Trial Registration isrctn.org Identifier: ISRCTN91974895
- Editorial Lifestyle Interventions for Obesity in the Era of GLP-1 Receptor Agonists JAMA
Read More About
Hoddinott P , O’Dolan C , Macaulay L, et al. Text Messages With Financial Incentives for Men With Obesity : A Randomized Clinical Trial . JAMA. Published online May 14, 2024. doi:10.1001/jama.2024.7064
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
A systematic review of economic evidence for community-based obesity prevention interventions in children
Affiliations.
- 1 Deakin Health Economics, Institute for Health Transformation, School of Health and Social Development, Deakin University, Geelong, Victoria, Australia.
- 2 Global Centre for Preventive Health and Nutrition (GLOBE), Institute for Health Transformation, School of Health and Social Development, Deakin University, Geelong, Victoria, Australia.
- PMID: 37308321
- PMCID: PMC10909472
- DOI: 10.1111/obr.13592
Multicomponent community-based obesity prevention interventions that engage multiple sectors have shown promise in preventing obesity in childhood; however, economic evaluations of such interventions are limited. This systematic review explores the methods used and summarizes current evidence of costs and cost-effectiveness of complex obesity prevention interventions. A systematic search was conducted using 12 academic databases and grey literature from 2006 to April 2022. Studies were included if they reported methods of costing and/or economic evaluation of multicomponent, multisectoral, and community-wide obesity prevention interventions. Results were reported narratively based on the Consolidated Health Economic Evaluation Reporting Standards. Seventeen studies were included, reporting costing or economic evaluation of 13 different interventions. Five interventions reported full economic evaluations, five interventions reported economic evaluation protocols, two interventions reported cost analysis, and one intervention reported a costing protocol. Five studies conducted cost-utility analysis, three of which were cost-effective. One study reported a cost-saving return-on-investment ratio. The economic evidence for complex obesity prevention interventions is limited and therefore inconclusive. Challenges include accurate tracking of costs for interventions with multiple actors, and the limited incorporation of broader benefits into economic evaluation. Further methodological development is needed to find appropriate pragmatic methods to evaluate complex obesity prevention interventions.
Keywords: community; cost; obesity; prevention.
© 2023 The Authors. Obesity Reviews published by John Wiley & Sons Ltd on behalf of World Obesity Federation.
Publication types
- Systematic Review
- Research Support, Non-U.S. Gov't
- Cost-Benefit Analysis
- Cost-Effectiveness Analysis
- Pediatric Obesity* / prevention & control
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10745722

Nutrition Interventions for Pediatric Obesity Prevention: An Umbrella Review of Systematic Reviews
Associated data.
Nutrition interventions to prevent pediatric obesity can help to establish healthy habits to improve current and future health. The objective of this umbrella review of systematic reviews (SRs) is to examine the impact of obesity prevention interventions with a nutrition component on body mass index measures, overweight/obesity prevalence, and cost-effectiveness in participants 2–17 years old. Grading of Recommendations Assessment, Development and Evaluation (GRADE) methods were used, and this umbrella review was registered on PROSPERO (CRD42023443033). Included SRs were required to search ≥2 databases and to assess the risk of bias (RoB) of primary studies, and they were published 2017–June 2023. Database searches identified 4776 articles, and 31 SRs were included. In all age groups combined, interventions with both nutrition and physical activity were effective and cost-effective in all settings combined, and in the community setting specifically. In children ≤5 years old, interventions in the home and family, community, and healthcare settings demonstrated some efficacy, whereas in children 6–12 years old, school interventions were most effective. Evidence with individuals 13–17 years was limited. The certainty of evidence was generally low due to RoB in included studies, inconsistency, and imprecision. Pediatric obesity prevention interventions with nutrition should be tailored to the developmental stage to ensure appropriateness and efficacy.
1. Introduction
Pediatric obesity can impact physical and psychological health and can lead to several adverse health conditions, including type 2 diabetes mellitus (T2DM), cardiovascular problems, and gastroesophageal reflux [ 1 ]. Accordingly, a Healthy People 2030 goal is to reduce the proportion of children and adolescents with obesity from its current rate of 19.7% [ 2 ]. The United States Preventive Task Force recommends that children and adolescents be screened for obesity and referred for or offered comprehensive behavioral interventions, which may include parent involvement and instruction on nutrition and physical activity [ 3 ]. The nutrition component of interventions is ideally led or designed by dietitians, who may provide nutrition counseling in child-based settings, develop and deliver theory-based nutrition education programs, and implement environmental and policy changes to improve access to healthy foods [ 4 ].
Interventions to prevent pediatric obesity can help to establish healthy habits to improve current and future health. Childhood and adolescence are stages of dynamic growth in which developmental skills, interests, and emotional maturity vary between peers and within individuals over time. Whereas younger children rely more on caregivers to learn how to eat and prepare food, older children become increasingly autonomous in choosing foods [ 5 ]. Thus, for interventions to be effective, they must accommodate diverse contexts and changing needs, including level of involvement in home life, in school, and with peers.
A recent overview of systematic reviews (SRs), also called an umbrella review, found that interventions for pediatric obesity prevention for children 6–12 years old improved BMI measures [ 6 ]. Another overview of reviews from 2019 found no overall effect of prevention interventions on BMI measures in pediatric participants but did not discuss results by type of intervention or age [ 7 ]. These umbrella reviews included 3–5 SRs each, though a recent scoping review identified many current SRs addressing a wide range of nutrition interventions to prevent pediatric obesity [ 8 ]. A 2020 overview of reviews identified 13 SRs that generally demonstrated little to no effect of prevention interventions on BMI measures in adolescents [ 9 ]. In 2021, the Academy of Nutrition and Dietetics conducted an umbrella review on pediatric obesity prevention interventions with nutrition to inform a Position Paper for nutrition practitioners, funders, and policymakers working to prevent pediatric obesity [ 4 ]. However, the umbrella review was never published. To provide those working in the nutrition field with detailed evidence to assess and to inform practice, the current manuscript provides a comprehensive account of updated evidence on nutrition interventions to prevent pediatric obesity.
Given the importance of facilitating healthy behaviors in children and adolescents and the uncertainty about which types of interventions are effective at which developmental stages, a comprehensive umbrella review is needed to inform practitioners, program funders, and policymakers working in the nutrition field about effective methods to prevent obesity throughout childhood and adolescence. The objective of this umbrella review is to examine the research question: In presumably healthy children and adolescents in the general population, what is the impact of pediatric obesity prevention interventions with nutrition on BMI measures, overweight and obesity incidence, and cost-effectiveness?
This umbrella review of SRs was designed using a social-ecological model [ 10 ], used methods described by the Cochrane Collaboration [ 11 ] and the Academy of Nutrition and Dietetics [ 12 ], and was reported according to the PRIOR checklist for overviews of SRs [ 13 ]. This umbrella review was registered on PROSPERO (CRD42023443033) [ 14 ].
2.1. Eligibility Criteria
Eligibility criteria are described in Table 1 . Included SRs addressed all aspects of the Population-Intervention-Comparison-Outcome (PICO) question: In presumably healthy children and adolescents (2–17 years) what is the impact of pediatric obesity prevention interventions that include nutrition, compared to no intervention, on BMI measures, prevalence of overweight and obesity and cost-effectiveness? SRs were excluded if they targeted individuals with diagnosed diseases, including those with overweight or obesity. SRs were eligible if they searched at ≥2 databases, assessed the risk of bias (RoB) of included primary studies, and were published after January 2017 to ensure the inclusion of recent primary research. SRs conducting meta-analysis or grading the certainty of evidence (CoE) for outcomes of interest were prioritized. When SRs using gold-standard methods were not available, SRs without these methods were included [ 8 ].
Eligibility Criteria for Umbrella Review of Systematic Reviews Examining the Effect of Nutrition Interventions to Prevent Pediatric Obesity.
ADD—attention deficit disorder; ADHD—attention deficit hyperactivity disorder; BMI—body mass index; CKD—chronic kidney disease; ESRD—end stage renal disease; IBD—irritable bowel disease; IBS—irritable bowel syndrome; SRs—systematic reviews.
2.2. Information Sources
Authors utilized search terms from a supporting scoping review [ 8 ], which was designed by an information specialist for Medline (Ebsco, Ipswich, MA, USA), CINAHL (Ebsco), Cochrane Database of Systematic Reviews (Ebsco), and Food Science Source (Ebsco) databases. This search was updated by M.R. The full search plan can be found in Supplementary Tables S1–S5 .
2.3. Study Selection
A sample of titles and abstracts were independently screened by M.R. and D.H. using Rayyan screening software ( https://rayyan.ai/cite ), and >80% agreement was achieved [ 15 ]. Therefore, the remaining titles and abstracts were screened by M.R., consulting with D.H. as needed. SRs included from the title and abstract screening were reviewed independently and in full by M.R. and D.H. Any disagreements between reviewers were resolved by consensus.
2.4. Data Collection
Data were extracted from the SRs by M.R. and cross-checked by D.H. Data were extracted onto a study-characteristics table and included: bibliographic information; participant ages; number and study designs of articles included in the SR; description of the intervention of interest and comparison groups; setting (e.g., school, healthcare); reported outcomes of interest; if the SR conducted meta-analysis or graded CoE, and the tool used to assess the RoB in primary studies. Interventions were required to have a nutrition component. However, results from interventions that additionally included physical activity were prioritized when interpreting findings, as multi-component interventions may be more effective [ 16 ]. For each study, quantitative and narrative results were extracted for each outcome of interest in each age group and setting of interest. In addition, primary studies included for each SR were compared to primary studies included in other SRs examining interventions in the same settings and age groups.
2.5. Quality Assessment
Included SRs were required to assess the RoB of included primary studies ( Table 1 ). Additionally, each included SR was assessed for quality using the AMSTAR2 tool [ 17 ]. SR quality was determined independently by two reviewers and discrepancies were resolved through consensus.
2.6. Synthesis of Results and Certainty Assessment
The inclusion process for this study was documented in a PRISMA flowchart [ 18 ]. Characteristics and results from each included SR were described in tables. If SRs included interventions from all settings or age groups, results were categorized as “all settings” or “all age groups combined” only unless sub-group analysis was provided for specific settings or age groups. SRs examining interventions in a specific setting (e.g., school) or age group (e.g., 6–12 years) were included in results for those categories only. The highest-quality SRs as determined by AMSTAR2 ratings and SRs that were the most comprehensive were used to inform conclusions. However, we were not able to conduct novel meta-analysis of included primary studies, as included SRs did not report sufficient data.
If SRs reported CoE using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) method, this grade was used to report CoE in this umbrella review. If the SRs used a different method or did not assess CoE, evidence was graded using the GRADE method [ 19 ], which was documented in summary of findings tables. CoE was graded as high, moderate, low, or very low [ 19 ]. Heterogeneity and sensitivity analyses conducted in the included SRs were used to inform conclusions.
There were 4776 unique articles identified by the database searches, and authors reviewed the full text of 445 articles. A list of articles excluded during full-text review, including reasons for exclusion is available in Supplementary Table S6 . Thirty-one SRs were included in this umbrella review [ 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 ]. SRs examined nutrition interventions for pediatric obesity prevention in all settings combined [ 20 , 22 , 30 , 33 , 34 , 43 , 44 , 47 ] or in the home and family [ 20 , 22 , 35 ], healthcare [ 22 , 37 , 49 , 50 ], school [ 20 , 22 , 23 , 25 , 27 , 28 , 29 , 36 , 38 , 40 , 41 , 42 , 46 ], or community settings [ 21 , 22 ], or examined the efficacy of food assistance programs [ 24 , 26 , 27 , 31 , 32 , 39 ] or electronic interventions [ 45 , 48 ]. The study selection process is described in Figure 1 . Study characteristics are described in Table 2 , and SR quality, as measured by the AMSTAR2 tool, can be found in Supplementary Table S7 . Some SRs reported findings for more than one age group or settings category ( Table 2 ).

PRISMA flow chart demonstrating the study inclusion process for the umbrella review of systematic reviews on nutrition interventions to prevent pediatric obesity.
Study characteristics of included systematic reviews examining the impact of nutrition interventions for pediatric obesity prevention.
BMI—body mass index; NRCT—nonrandomized controlled trial; RCT—randomized controlled trial; RoB—risk of bias.
3.1. All Settings
Eight included SRs examined the impact of nutrition interventions for pediatric obesity prevention in all settings, including in all ages combined [ 20 , 34 , 43 , 47 ], or in those ≤5 years [ 22 ], 6–12 years [ 20 , 22 , 44 ], or 13–17 years [ 22 , 30 , 33 ]. The eight SRs analyzed data from a total of 142 primary studies, and 33 of these studies were represented in more than one SR.
3.1.1. Age Groups Combined
Four SRs examined the effect of nutrition interventions for pediatric obesity prevention in combined age groups [ 20 , 34 , 43 , 47 ]. Results are described in Table 3 and CoE is described in Table 4 . Salam et al., published in 2020, found that nutrition and physical activity interventions reduced BMI z-score [mean difference (MD) (95 % confidence interval (CI)):−0.12 (−0.18, −0.06)] and BMI [−0.41 kg/m 2 (−0.06, −0.21)], and CoE was low due to high heterogeneity in results [ 43 ]. Long et al. 2021 agreed with these results but found smaller effect sizes [ 34 ]. In Abdel Rahman et al. 2018, there was no effect of the interventions to reduce sugar-sweetened beverage intake on BMI z-scores in three primary studies [ 20 ]. Specchia et al. 2018 reported that multi-component, multi-level, or multi-setting interventions reduced overweight and obesity prevalence [ 47 ]. In the supplementary materials , Salam et al. also reported effects on obesity prevalence, but there were errors in the analysis. Salam et al. 2020 [ 43 ] was the only SR to examine the cost-effectiveness of nutrition interventions to prevent obesity, and five out of six of the included primary studies demonstrated cost-effectiveness or cost savings. Salam et al. 2020 [ 43 ] and Specchia et al. 2018 [ 47 ] had a low quality score and the remaining SRs had critically low quality scores ( Table S7 ).
Quantitative results of included systematic reviews examining the impact of pediatric obesity prevention interventions with nutrition.
BMI—body mass index; CoE—certainty of evidence; CI—confidence interval; HALY—health-adjusted life years; ICER—incremental cost-effectiveness ratio; IQR—interquartile range; MD—mean difference; N—number; NR—not reported; SMD—standardized mean difference; SR—systematic review. a As determined by systematic review authors.
Summary of findings table describing systematic reviews examining the effects of nutrition interventions for pediatric obesity prevention in all settings in individuals 2–17 years old.
BMI—body mass index; CI—confidence interval; MD—mean difference; NR—not reported; RCT—randomized controlled trial. Explanations: a High heterogeneity. b Risk of bias in included studies. c Small sample size or wide confidence interval. d No effect size described.
3.1.2. Specific Age Groups
In SRs examining children ≤5 years, Brown et al. found moderate CoE that interventions including both diet and physical activity reduced BMI z-score [−0.07 (−0.14, −0.01)] and BMI [−0.11 kg/m 2 (−0.21, 0.00)] compared to control groups [ 22 ]. Two SRs targeted children 6–12 years old [ 22 , 44 ]. Interventions with both diet and physical activity reduced BMI z-score [−0.05 (−0.10, −0.01)], but not BMI [−0.05 kg/m 2 (−0.11, 0.01)] in 6–12-year-old children, and CoE was low ( Table 3 ) [ 22 ]. Seral-Cortes et al. found that health programs targeting obesity prevention with nutrition and physical activity did not affect BMI z-score or BMI [ 44 ]. Brown had a high quality score and Seral-Cortes had a critically low quality score ( Supplementary Table S7 ).
Three SRs examined the effect of nutrition interventions in all settings for adolescents 13–17 years old [ 22 , 30 , 33 ]. Brown et al. and Hayba et al. were high quality SRs and Kornet van der Aa was of moderate quality. Hayba et al. and Kornet van der Aa targeted adolescents from under-represented groups. Nutrition and physical activity interventions did not affect BMI z-score or BMI, and CoE was low [ 22 , 30 ]. Overweight and obesity prevalence decreased in the intervention group compared to the control group in one study [ 33 ] and CoE was very low ( Table 3 and Table 4 ).
Based on the current evidence, nutrition and physical activity interventions to prevent pediatric obesity may reduce BMI z-score and may be cost-effective for participants <18 years old. Interventions in all settings were most effective for individuals ≤12 years old. Obesity prevention programs that were multi-component, multi-level and/or within multiple settings may reduce overweight/obesity prevalence.
3.2. Home and Family Setting
Three SRs examined the impact of interventions of interest in the home and family setting [ 20 , 22 , 35 ] in all ages combined [ 35 ] and for children ≤5 years old [ 22 ], 6–12 years old [ 20 , 22 ], and 13–18 years old [ 22 ]. In the three SRs, 12 primary studies were represented, and there was no overlap in primary studies between SRs.
3.2.1. Age Groups Combined
Morgan et al. 2020 reported no pooled effect of interventions with children as active participants and caregivers involved in at least one aspect of the intervention compared to interventions in which a caregiver was not involved on BMI [standardized mean difference (95%CI): 0.05 (−0.04, 0.15) I 2 = 0%] or overweight/obesity prevalence [relative risk (95% CI): 1.02 (0.89, 1.17)] ( Table 3 ) [ 35 ]. CoE was low ( Supplementary Table S8 ).
3.2.2. Specific Age Groups
Brown et al. reported that interventions in the home and family setting improved BMI [MD (95% CI): −0.33 kg/m 2 (−0.55, −0.10)] but not BMI z-score [−0.13 (−0.35, 0.09)] in children ≤5 years old [ 22 ]. In 6–12-year-old children, there was no effect on BMI z-score compared to the control group in one RCT [0.03 (−0.04, 0.10)] [ 22 ], and CoE was low. Brown et al. found no effect of nutrition and physical activity intervention in the home setting on BMI z-score in 13–18 years olds [0.06 (−0.13, 0.26)] [ 22 ], and CoE was very low ( Table 3 and Table S8 ).
Based on the current evidence, nutrition and physical activity interventions in the home setting or with a caregiver may be most effective for improving BMI measures in children ≤5 years old but may have little or no effect in individuals 6–18 years old compared to no intervention.
3.3. Healthcare Setting
Four SRs examined pediatric obesity prevention interventions with nutrition in healthcare settings [ 22 , 37 , 49 , 50 ], and included SRs with all age groups combined [ 49 ] and for children ≤5 years old [ 22 , 37 , 50 ]. The four SRs included 12 total primary studies, and there was no overlap in primary studies between SRs.
3.3.1. Age Groups Combined
In an SR by Tissot et al. reported in 2021, primary care-led interventions in individuals 10–19 years old reduced BMI percentile or z-scores in four studies, there was no effect in four studies, and findings were unclear in the remaining study. No meta-analysis was conducted and CoE was very low due to RoB, inconsistency in findings between studies, and small sample sizes ( Supplementary Table S9 ) [ 49 ].
3.3.2. Specific Age Groups
Three SRs identified interventions provided for children ≤5 years old. BMI z-score improved in the intervention groups compared to control groups in 2–4-year-old Latino children [MD (95%CI): −0.24 (−0.46, −0.02)] [ 22 ]. BMI z-score improved in children when nurses trained childcare staff in obesity prevention compared to controls −0.14 (−0.26 to −0.02) [ 50 ]. In the final SR, there was no significant difference in children’s prevalence of overweight according to group assignment in children ≤5 years old [ 37 ].
Based on the current evidence, nutrition and physical activity interventions delivered in the healthcare setting may reduce BMI z-scores in children ≤5 years old, but the effect on overweight or obesity prevalence and effect in older children and adolescents is uncertain.
3.4. School Setting
Thirteen SRs examined the impact of obesity prevention interventions with nutrition in the school setting in all age groups combined [ 20 , 23 , 27 , 28 , 29 , 38 , 40 ], children ≤5 years old [ 22 ], children 6–12 years old [ 22 , 25 , 36 , 41 , 42 , 46 ] and adolescents 13–18 years old [ 22 ]. No studies reported the cost-effectiveness of these interventions. There were 139 unique primary studies analyzed in the 13 SRs combined, and 36 primary studies were represented in more than one SR.
3.4.1. Age Groups Combined
Of the seven SRs that examined the impact of nutrition interventions in age groups combined [ 20 , 23 , 27 , 28 , 29 , 38 , 40 ], Nury et al. 2021 [ 38 ] had a high quality score, Gonclaves et al. 2021 and Durão et al. 2023 had a moderate quality score [ 28 , 29 ], and the remaining SRs had a critically low quality score ( Table S7 ). Nury et al. 2021 demonstrated little to no effect of school nutrition interventions on BMI z-score [MD (95% CI): −0.09 (−0.18, 0.00)], BMI [0.03 kg/m 2 (−0.10, 0.16)], or overweight and obesity prevalence [OR (95% CI): 1.19 (0.95, 1.49)] ( Table 3 ). CoE was low due to RoB in included studies and imprecision [ 38 ]. Results were similar in SRs examining interventions influencing school food environment [ 29 , 52 ] and reducing sugar-sweetened beverage intake in schools [ 20 ]. However, three SRs with a critically low quality score found improvements in outcomes from school interventions ( Table 3 ) [ 23 , 27 , 40 ].
3.4.2. Specific Age Groups
Brown et al. described no difference in BMI z-score [MD (95%CI): −0.04 (−0.09, 0.01)] or BMI [−0.05 kg/m 2 (−0.14, 0.05)] for children ≤5 years old participating in nutrition and physical activity interventions in the childcare/preschool setting compared to control groups [ 22 ]. Additionally, Brown et al. demonstrated no effect on BMI z-score [MD (95%CI): 0.00 (−0.06, 0.06)] or BMI [−0.02 kg/m 2 (−0.10, 0.05)(I 2 = 58%)] in 13–18-year-olds ( Table 3 ), but heterogeneity of results was very high ( Supplementary Table S10 ).
Six SRs examined nutrition interventions for obesity prevention in children 6–12 years old [ 22 , 25 , 36 , 41 , 42 , 46 ]. Brown et al. 2019 and Smit et al. 2023 had a high quality score [ 22 , 46 ], and the remaining SRs had a critically low quality score ( Table S7 ). Smit et al. was more recent, but Brown et al. was more comprehensive and there were only two primary studies that overlapped between these SRs. Brown et al., published in 2019, demonstrated that interventions with both diet and physical activity reduced BMI z-score [−0.04 (−0.08, −0.01)], but there was no difference in BMI [−0.04 kg/m 2 (−0.10, 0.02)] [ 22 ]. Smit et al. found no effect of primary school-based obesity prevention interventions on BMI z-score [MD (95% CI): −0.08 (−0.20, 0.05)], BMI [0.06 (−0.38, 0.50)], or overweight prevalence (studies not pooled) in children 6–12 years old. Smit rated all outcomes as having very low CoE ( Table 3 ) [ 46 ].
Nally et al. 2021 demonstrated an improvement in BMI z-scores and BMI, respectively, in children 5–12 years old [ 36 ]. Rochira et al., published in 2020,examined school garden interventions in children 6–13 years old and found an improvement in BMI percentile, but no impact on BMI z-score or BMI [ 42 ]. Cerrato-Carretero et al. 2021 and Qi et al. 2021 also found a null impact on BMI z-scores [ 41 ] and BMI [ 25 , 41 ].
Based on the current evidence, in all age groups combined, nutrition and physical activity interventions in the school setting may not reduce BMI z-score, BMI, or overweight or obesity prevalence. Interventions in school settings likely reduce BMI z-score in children 6–12 years old.
3.5. Community Setting
Two SRs examined the impact of obesity prevention interventions with nutrition in the community setting in all children combined [ 21 ], and in children ≤5 years old [ 22 ], 6–12 years old [ 21 , 22 ], and 13–17 years old [ 22 ]. One SR reported on the cost-effectiveness of community interventions in Australia [ 21 ]. Twenty-three primary studies were identified in these SRs, and there was no overlap between SRs.
3.5.1. All Age Groups
In the SR by Ananthapavan et al. published in 2018, community interventions decreased BMI z-score [MD (95% CI): −0.07 (−0.13, −0.01)] in Australia [ 21 ], and CoE was low ( Table 4 ). Using results from included studies, authors analyzed cost-effectiveness and found that the mean incremental cost-effectiveness ratio (ICER) was AUD 8155 (AUD 237 to AUD 81,021) per health-adjusted life year, and there was a 95% probability of interventions being cost-effective at the defined threshold [ 21 ]. Evidence certainty was low ( Supplementary Table S11 ).
3.5.2. Specific Age Groups
Brown et al. found that diet and physical activity interventions had no effect on BMI z-score in children ≤5 years old, but reduced BMI by −0.59 kg/m 2 (−0.94, −0.24) [ 22 ] ( Table 3 ).
Two SRs reported on intervention efficacy in children around 6–12 years old [ 21 , 22 ]. Brown et al. found no effect of community interventions, including nutrition and physical activity, on BMI z-score [−0.04 (−0.39, 0.31); I 2 = 94%] or BMI kg/m 2 [−0.08 (−0.29, 0.13); I 2 = 25%] [ 22 ]. Ananthapavan et al. found an improvement in BMI z-score, but their total sample size was unclear. Ananthapavan et al. 2018 found no effect on BMI z-score in adolescents 12–18 years old [MD (95% CI): −0.02 (−0.07, 0.03)] [ 21 ]. Brown had a high quality score and Ananthapavan had a critically low quality score. CoE ranged from low to very low ( Table 3 and Table S11 ).
Based on the current evidence, pediatric obesity prevention interventions with nutrition in the community setting may improve BMI z-score and be cost-effective in all age groups combined. Nutrition and physical activity interventions in the community setting may decrease BMI in children ≤5 years old, but interventions were ineffective, or evidence was lacking for older children and adolescents.
3.6. Federal Food Assistance Programs
Six SRs examined the impact of federal food assistance programs on obesity prevention. Programs assessed included the Supplemental Nutrition Program for Women, Infants and Children (WIC) [ 24 ], universal school meals [ 26 , 27 ], the Supplemental Nutrition Assistance Program (SNAP) [ 31 ], the Child and Adult Care Food Program (CACFP) [ 32 ], and food assistance programs in general [ 39 ]. Twenty-two primary studies were represented in total and only one study was cited in more than one SR. CoE is described in Supplementary Table S12 .
3.6.1. All Age Groups
Hudak et al., published in 2019, investigated the impact of SNAP in participants 2–18 years old. Of the studies that addressed selection bias, results were heterogeneous, including lower risk of overweight or obesity in participants who were boys or younger girls but increased risk for girls 5–18 years old or who were long-term participants. Results were not pooled in the meta-analysis [ 31 ].
Kenney et al. 2023 identified one study with 4050 participants ages 2–18 years old that reported that CACFP participation was not associated with the prevalence of overweight and obesity [ 32 ].
Both Cohen et al. (2021) and Dabravolskaj et al. (2020) examined the impact of universal school meals. Cohen et al. demonstrated mixed findings for the effect on BMI z-score, and no effect on BMI or obesity prevalence [ 26 ]. Dabravolskaj et al. agreed with these findings [ 27 ].
3.6.2. Specific Age Groups
Caulfield et al. 2022 examined the impact of the revised 2009 WIC food package for children ≤5 years old and identified three studies with >16 million participants [ 24 ]. The authors concluded that the revised food package reduced overweight and obesity prevalence and rated CoE as low.
Olstad et al., published in 2017, evaluated primary studies targeting government policies for disadvantaged populations. Primary studies investigating the SNAP program were excluded, and just one primary quasi-experimental study was identified that reported that the USDA Fresh Fruit and Vegetable Program decreased BMI z-score and BMI in elementary school students after four years [ 39 ].
Based on the current evidence, few SRs assessed the impact of federal food assistance programs on the prevention of pediatric obesity. The 2009 revised WIC package reduced obesity prevalence in young children, and a USDA program providing fresh fruits and vegetables outside of the school reduced BMI z-score and BMI in elementary-aged children. The impact of the SNAP program was mixed, depending on the sub-population examined. The CACFP program and universal school meals did not impact BMI outcomes or obesity prevalence.
3.7. Electronic Interventions
Two SRs examined the effects of electronic interventions with nutrition to prevent pediatric obesity [ 45 , 48 ]. There were eight primary studies represented in the SRs with no overlap in primary studies between SRs. Suleiman-Martos et al. 2021 identified five RCTs, three of which demonstrated an improvement of gamification on BMI z-scores and two of which found no effect. Results from two of these trials were pooled, and there was no effect on BMI z-scores [MD (95% CI): −0.05 (−0.21, 0.11)] [ 48 ]. Silva et al. 2022 found no effect of computer-based nutrition interventions compared to controls on BMI in 10–19-year-olds in three trials [−0.02 kg/m 2 (−0.18, 0.14)] ( Table 3 , Supplementary Table S13 ) [ 45 ]. There may be no effect of electronic nutrition interventions on BMI or BMI z-score in children and adolescents.
4. Discussion
This umbrella review analyzed 31 recent SRs examining the impact of pediatric obesity prevention interventions with a nutrition component. In SRs with pediatric individuals aged 2–17 years combined, interventions with both nutrition and physical activity were effective and cost-effective in all settings combined, and in the community setting specifically. In children ≤5 years old, interventions in the home and family, community, and healthcare settings all demonstrated some efficacy, as did the 2009 revised WIC package. In children 6–12 years old, interventions in schools were most effective and a federal food assistance program providing fresh fruits and vegetables also may be effective. Limited evidence in individuals 13–17 years old did not demonstrate efficacy for nutrition interventions aiming to prevent obesity ( Figure 2 ). CoE was generally low due to RoB in included studies, inconsistency in results between studies, and imprecision in findings.

Impact of obesity pediatric prevention interventions with nutrition according to age and intervention setting. Nutrition and physical activity interventions in all settings and age groups combined are effective in improving BMI measures and overweight and obesity prevalence, as were interventions in all age groups combined in the community setting. Interventions in the home and family setting and in healthcare settings were beneficial for children ≤5 years old, school interventions were most effective for children 6–12 years old, and there is evidence of benefits from food assistance programs in children ≤12 years old. Beyond the impacts of interventions seen in all age groups combined, little is known about effective interventions for adolescents 13–17 years old.
A 2019 umbrella review of pediatric obesity prevention interventions demonstrated that mixed interventions were most effective in improving cardiovascular profile, but had little impact on BMI, though efficacy was not examined according to intervention type or participant age [ 7 ]. In another recent umbrella review, Denova-Gutierrez [ 6 ] identified five SRs targeting pediatric obesity prevention in children 6–12 years old and described that multi-component interventions, including nutrition, physical activity, and behavior change were most effective in preventing pediatric overweight and obesity [ 6 ]. However, the authors also described a gap in methodological quality in primary studies, which prevents the establishment of robust recommendations. This umbrella review supports and expands upon these findings by demonstrating the efficacy of obesity prevention interventions with at least a nutrition component in specific age groups and settings, thus providing a potential path for effective obesity prevention interventions throughout childhood and adolescence.
The impacts of pediatric obesity interventions identified in this umbrella review were heterogeneous, which can be explained by the wide variety of interventions delivered and of methods used to implement interventions. Future SRs and umbrella reviews may focus on the efficacy of specific implementation strategies for nutrition interventions to provide robust guidance on the best methods for delivering interventions to children and adolescents in the general population.
Among the target audiences for this umbrella review are nutrition program funders and policymakers, as these individuals are responsible for facilitating effective interventions to prevent pediatric obesity by using available resources most efficiently. However, there was very little evidence available about the cost-effectiveness of pediatric obesity prevention programs with nutrition to support policy decisions. After the search was performed for this umbrella review, Sultana et al. published a SR in 2023, examining the economic evidence for community-based interventions for pediatric obesity prevention [ 53 ]. Authors identified five studies conducting cost-utility analysis, three of which found interventions to be cost-effective. An additional primary study reported a cost-saving return-on-investment ratio [ 53 ]. These results were consistent with those found by Ananthapavan et al. in 2019, who reported that community interventions may be cost-effective [ 21 ]. Disease prevention may be difficult to prioritize in the context of what seem like more pressing health needs. More research investigating the cost-efficacy of pediatric obesity prevention programs is crucial for demonstrating that facilitating healthy lifestyle behaviors can prevent not only the suffering associated with obesity-related diseases but also the financial costs of treating these diseases.
This umbrella review utilized a social-ecological model to examine the contexts in which interventions were most effective. However, a space that is not typically represented in the social-ecological framework is that of digital and electronic media, which extend throughout home, school, and community settings and are an integral part of food assistance programs. There were very few SRs examining the efficacy of electronic interventions, and neither of those included in this study found that electronic interventions were efficacious in preventing obesity. More research is needed to leverage the time children and adolescents are spending with electronic devices to contribute to healthy lifestyle behaviors.
4.1. Strengths and Limitations
Results from this umbrella review provide a comprehensive picture of the impact of pediatric obesity prevention programs with a nutrition component and demonstrate the need for a multi-faceted approach to establishing healthy habits that are dynamic according to needs and preferences throughout childhood and adolescence. This umbrella review utilized rigorous methods, including a systematic search, a screening process, and rigorous evidence synthesis. The wide breadth of research examined allows for the comparison of quantitative evidence from the highest-quality SRs available and can guide policymakers to support evidence-based programs. Finally, although it was not possible to perform novel meta-analyses due to the lack of information reported in many SRs, this umbrella review graded a CoE for each age group in each setting, which provides a common metric by which to compare evidence availability and efficacy.
A limitation of this umbrella review was the gap in the underlying research, particularly on effective interventions for teenagers in the general population, which was also demonstrated in an overview of SRs by Flodgren et al. published 2020 [ 9 ], and in research on electronic and food assistance interventions. Another limitation was the limited outcomes examined in this umbrella review. Although focusing on BMI measures and overweight and obesity prevalence allowed for the inclusion of a broad evidence base and comparisons between SRs, the goal of obesity prevention programs is not to change a number on a scale or chart, but rather to improve the health and well-being of children and adolescents now and in their futures. Thus, future studies and SRs should aim to assess outcomes that are more client-centered such as the development of T2DM, quality of life, or academic achievements.
4.2. Implications for Practice
Nutrition practitioners are a key target audience of this umbrella review. This review highlights that efforts to prevent pediatric obesity may be successful when delivered in the context of multi-component interventions that include nutrition. Although interventions ideally include interdisciplinary practitioners, nutrition practitioners can and should encourage the meeting of national physical activity recommendations [ 54 ] in addition to providing nutrition interventions. Practitioners should be aware that the efficacy of certain interventions varies greatly according to participant age. Thus, a life-course approach to obesity prevention should be implemented to consistently deliver the most effective interventions and the most optimal developmental stage to ensure long-term benefits into adulthood. Nutrition practitioners, funders, and policymakers should advocate for increased access to effective prevention services for children across developmental stages and settings [ 4 ].
5. Conclusions
Multi-component pediatric obesity prevention interventions with a nutrition component may improve BMI outcomes and overweight and obesity prevalence and may be cost-effective. Interventions in different settings may have varying efficacy for different age groups, and obesity prevention approaches should be tailored to developmental stages to ensure appropriateness and efficacy. Although interventions in the home, healthcare, and community settings have proven efficacious for young children and school interventions have proven efficacious for elementary-aged children, it is unclear which type of interventions may be effective for teens. Program funders and policymakers can facilitate investment in a life-course approach to disease prevention by advocating for the implementation of interventions tailored to developmental stages and research investigating effective methods in adolescents.
Acknowledgments
The authors would like to acknowledge the content experts who contributed to the original umbrella review and the Position Paper that it supported, including Deanna M. Hoelscher; Lynn S. Brann; and Sara O’Brien.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15245097/s1 .
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization, M.R. and D.H.; Methodology, M.R.; Analysis, M.R.; Data Curation, M.R. and D.H.; Writing—Original Draft Preparation, M.R.; Writing—Review and Editing, M.R. and D.H.; Visualization, M.R. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar
information for practice
news, new scholarship & more from around the world
- gary.holden@nyu.edu
- @ Info4Practice
School bullying prevention and intervention strategies in the United Arab Emirates: a scoping review
Introduction
Schools in the United Arab Emirates (UAE) witnessed an increase of 7% in bullying prevalence since 2005. This review aimed to map antibullying interventions in the UAE.
A systematic search was performed in five electronic databases (EMBASE, PubMed, PsycINFO, Scopus and Eric) using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Review. Studies addressing antibullying interventions and grey literature in the UAE from 2010 to 2021 were included. Interventions were mapped using distribution across key sectors, public health practice levels, and organisation types.
Of the 2122 identified papers, only 2 were included. Both articles were published in 2019 and used qualitative methods. From the search of governmental and non-governmental websites, 22 multilevel interventions were included and presented on the three levels of public health practice across the different sectors and target stakeholders. Eight interventions were at the federal level, and six were by private stakeholders. The government funded 59% of all interventions. Four interventions addressed cyberbullying, and three used multisectoral collaboration.
Conclusions
Although the UAE is building capacity for bullying prevention, we found limited knowledge of antibullying prevention efforts. Further studies are needed to assess current interventions, strategies and policies.
Read the full article ›

IMAGES
VIDEO
COMMENTS
This updated synthesis of obesity prevention interventions for children aged 6-18 years, found a small beneficial impact on child BMI for school-based obesity prevention interventions. A more comprehensive assessment of interventions is required to identify mechanisms of effective interventions to inform future obesity prevention public health policy, which may be particularly salient in for ...
Inclusion and Exclusion Criteria. We carried out an electronic and systematic search in the literature review on setting-based interventions related to childhood obesity both in developed and developing countries across the world. To answer the study question, the eligibility of a study was contingent for inclusion if it was a randomized ...
Obesity, once established, is difficult to treat, and therefore effective preventive interventions are essential. SBU has updated the report "Treating and Preventing Obesity" (2002) to include works published from 2001 through 2004 that address the prevention of obesity in children / adolescents and adults. The questions investigated include:
We conducted an updated literature review of multilevel interventions for obesity prevention and reduction. We identified six protocols and six articles on completed studies that were published between January 2016 and September 2018. Of the completed studies, four found significant intervention effects on body mass index and/or waist ...
Background: Childhood obesity is a serious public health concern. School-based interventions hold great promise to combat the rising trend of childhood obesity. This systematic review aimed to assess the overall effects of school-based obesity prevention interventions, and to investigate characteristics of intervention components that are potentially effective for preventing childhood obesity.
Childhood obesity is a serious public health concern. School-based interventions hold great promise to combat the rising trend of childhood obesity. This systematic review aimed to assess the overall effects of school-based obesity prevention interventions, and to investigate characteristics of intervention components that are potentially effective for preventing childhood obesity.
Childhood overweight and obesity is a global public health issue. Although there is evidence of a reduced prevalence in some countries, there is still much controversy about the efficacy of health interventions that aim to prevent and treat obesity in this specific population. The objective of the present study is to develop an overview of systematic reviews (OSRs) that assesses the effects of ...
This article reports a systematic review of interventions aimed to reducing or preventing obesity under-fives. The search was performed with six different databases: Web of Science, PsycINFO, Cochrane, PubMed, Medline, and CINAHL. ... A number of obesity prevention interventions in this review (n = 5) focused on new mothers or mothers and their ...
Aim: Effective evidence-based interventions have an important role in obesity prevention. Our aim was to present a qualitative synthesis of setting-based health promotion interventions on obesity, from Nordic countries and the Netherlands.
Objective To examine the effectiveness of behavioural weight management interventions for adults with obesity delivered in primary care. Design Systematic review and meta-analysis of randomised controlled trials. Eligibility criteria for selection of studies Randomised controlled trials of behavioural weight management interventions for adults with a body mass index ≥25 delivered in primary ...
This is the first systematic review of obesity interventions in early childcare and education settings to focus primarily on external validity using the RE-AIM framework. This review is an important step in the progress of translational research for obesity prevention interventions for preschool-aged children.
This paper aims to systematically review the evidence for spillover effects of childhood obesity prevention interventions on individuals and communities not specifically targeted by the intervention but who may be connected to recipients through physical or social proximity. 6, 7 Findings from this systematic review will be useful to decision ...
In this review, we comprehensively retrieved and screened 4,541 studies on obesity intervention published between 2018 and 2022 in the Web of Science Core Collection, and objectively presented research frontiers using bibliometric analysis. The research frontiers of intervention are mainly focused on dietary, exercise, pharmacological ...
Aim . Effective evidence-based interventions have an important role in obesity prevention. Our aim was to present a qualitative synthesis of setting-based health promotion interventions on obesity, from Nordic countries and the Netherlands. Methods . A systematic review of the literature was completed for studies in the community, schools, and worksite, with BMI as an outcome.
A recent systematic review and meta-analysis of the effect of school-based obesity prevention interventions on BMI or BMI-z score of children and found significant reductions in intervention schools compared with controls for both single- and multi-component interventions (Liu et al., 2019). Such school-based studies have the potential to also ...
This systematic review explores the methods used and summarizes current evidence of costs and cost-effectiveness of complex obesity prevention interventions. A systematic search was conducted using 12 academic databases and grey literature from 2006 to April 2022. Studies were included if they reported methods of costing and/or economic ...
The aim of this review was to systematically assess the effectiveness of obesity prevention and control interventions in US immigrant populations across the life course, from preschool-age to adults. A systematic review of relevant studies was undertaken and eligible articles included. The initial search identified 684 potentially relevant ...
Intervention, Surgery, Transplantation; Quality and Outcomes ... advances in implementation science that hold promise to bridge the know-do gap in obesity prevention and treatment are discussed. ... The expert peer review of AHA-commissioned documents (eg, scientific statements, clinical practice guidelines, systematic reviews) is conducted by ...
Along with clinic-based interventions, researchers have attempted to manage obesity by virtue of family, community, school, and after school programs. Based on Cochrane review of obesity prevention programs in children, most of the well-designed interventions had positive results especially in 6-12-year-old children. Clearly targeted ...
Intervention description. Part of the larger obesity prevention program, the Amsterdam Healthy Weight Approach (AHWA []), Jump-in was originally designed and shown to be effective in stimulating PA [21, 22, 24].Following this original positive evaluation, Jump-in was expanded to also include a healthy dietary component and to be further shaped after the Health-Promoting School model (HPS) [23 ...
Overall, SMIs were deemed to have a small impact, but the absence of harmful effects and potential cumulative benefits indicated a favourable balance of effects, despite low certainty, and recommendations' certainty and applicability were made. Self-management interventions (SMIs) may improve disease management in adults living with obesity. We formulated evidence-based recommendations for ...
Other organizations. American Psychological Association In 2018, the association released the Clinical Practice Guideline for Multicomponent Behavioral Treatment of Obesity and Overweight in Children and Adolescents.This CPG strongly supported the use of family-based multicomponent behavioral interventions with at least 26 contact hours for children and adolescents 2-18 with overweight and ...
The worldwide obesity prevalence, defined by body mass index (BMI) ≥30 kg m − 2, has nearly tripled since 1975 (ref. 1). BMI is a good surveillance measure for population changes over time ...
A systematic review that included 12 randomized clinical trials reported that text messaging-based weight loss interventions were associated with a mean weight change of −2.3 kg (95% CI, −3.2 to −1.4 kg) compared with control. 7 However, in this systematic review, only 3 clinical trials reported weight loss at 12 months (mean ...
This systematic review explores the methods used and summarizes current evidence of costs and cost-effectiveness of complex obesity prevention interventions. A systematic search was conducted using 12 academic databases and grey literature from 2006 to April 2022. Studies were included if they reported methods of costing and/or economic ...
Success factors of growth-stage digital health companies: protocol for a systematic literature review Estelle Pfitzer1,2, Laura Bitomsky 1, Marcia Nißen1, Christoph Kausch 2, Tobias Kowatsch*1,3,4 Affiliations: 1 Centre for Digital Health Interventions, School of Medicine, University of St. Gallen, St. Gallen, Switzerland 2 MTIP AG, Basel, Switzerland
Nutrition interventions to prevent pediatric obesity can help to establish healthy habits to improve current and future health. The objective of this umbrella review of systematic reviews (SRs) is to examine the impact of obesity prevention interventions with a nutrition component on body mass index measures, overweight/obesity prevalence, and cost-effectiveness in participants 2-17 years old.
A systematic search was performed in five electronic databases (EMBASE, PubMed, PsycINFO, Scopus and Eric) using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Review. Studies addressing antibullying interventions and grey literature in the UAE from 2010 to 2021 were included.