
How Research England supports research excellence
The Research Excellence Framework (REF) was the first exercise to assess the impact of research outside of academia. Impact was defined as ‘an effect on, change or benefit to the economy, society, culture, public policy or services, health, the environment or quality of life, beyond academia’.
Impact case studies
As part of the 2014 Research Excellence Framework exercise, UK higher education institutions (HEIs) submitted 6,975 impact case studies demonstrating the impact of their research on wider society.
These case studies provide a unique and invaluable source of information on the impact of UK research. UK higher education (HE) research has wide and varied benefits on the economy, society, culture, policy, health, the environment and quality of life — both within the UK and overseas.
Universities engage with a range of public, private and charitable organisations and local communities. Analysis found that these wider impacts and benefits often stem from multidisciplinary work.
Latest report: Patterns in research outputs
Publication patterns in research underpinning impact in REF2014 describes patterns in research outputs submitted by UK higher education institutions to the 2014 Research Excellence Framework and to previous Research Assessment Exercises (RAEs).
The REF impact case study database
The impact case study database is a searchable tool that will make the impact case studies widely available and will enable analysis and automated text mining.
The licence arrangements relating to the use of this database can be accessed on the National Archive .
An initial analysis of the REF impact case studies is captured in the report, The nature, scale and beneficiaries of research impact .
The REF impact case studies were analysed by Digital Science, a division of Macmillan Science and Education, working in conjunction with its sister company Nature Publishing Group and the policy institute at King’s College London. This analysis was co-funded by the UK Funding Bodies, Research Councils UK and Wellcome Trust.
Maps of impact case studies
The maps of impact case studies indicate the local and global spread of research impact for UK higher education institutions (HEIs) by impact type and research area.
They are based on the names of locations referenced in REF2014 impact case studies and categorised in the REF impact case study database.
Last updated: 31 March 2022
This is the website for UKRI: our seven research councils, Research England and Innovate UK. Let us know if you have feedback or would like to help improve our online products and services .

Impact Case Studies
This section provides you with resources, tools and examples to support you to write your impact case studies

What are Impact Case Studies?
Impact case studies are evidence based stories about the difference your research has made to the world. They explain why the research was necessary, the journey your research has taken, and the difference (impact) your research has made i.e. they cover the what, where, when, who and how.
Impact case studies are useful ways of conveying, in engaging and compelling stories, complex areas of research. They can be used to tell your story on websites, as part of your CV, grant applications, impact awards as well as submission to assessment frameworks such as the Research Excellence Framework (REF).
Research Excellence Framework

The Research Excellence Framework (REF) is the process of assessing the quality and impact of research within UK Higher Education Institutions.
This process enables UK funding bodies to benchmark and allocate funding to higher education institutions as well as provide accountability for their investments.
The first assessment process took place in 2014 and our most recent submission was in 2021 with results due in March 2022. For more information about REF 2021 please visit: https://www.ref.ac.uk
REF Impact Case Studies
As a part of the REF assessment process, higher education institutions are asked to prepare and write impact case studies for peer review. These impact case studies outline the changes and benefits that research has had on society, economy, public policy and practice, environment and quality of life. They are presented within a template, are up to 5 pages in length and undergo peer review by a panel of experts.
A full database of impact case studies from the previous exercise conducted in 2014 are available from Research England.
REF Impact Definitions
For REF 2021 “Impact is defined as an effect on, change or benefit to the economy, society, culture, public policy or services, health, the environment or quality of life, beyond academia”. ( Research England, REF 2021 )
Impact needs to show both:
- Significance = the degree to which impact has enabled, enriched, influenced, informed or changed the performance, policies, practices, products, services, understanding, awareness or well-being of the beneficiaries.
- Reach = the extent and/or diversity of the beneficiaries of the impact, as relevant to the nature of the impact.
REF eligibility criteria
Your case study was eligible for submission to the Research Excellence Framework in 2021 if…
- Your research was carried out between 1st January 2000 and 31 December 2020 at the University of Bath
- Your impact occurred between 1 August 2013 and 31st July 2020 (this was extended to 31st December 2021 due to COVID-19)
The following are some top-tips to writing your Impact Case Study
- Know your audience – it is important to be able to tell your story so that it is accessible and engaging to your intended audience
- Articulate your impact and how it was achieved – start by setting out the context (why was this research important, what problem was it addressing), the difference you made (what did it change, who did it affect, influence, inform?) and how this was achieved. Think why, what, who, when, where and how.
- Be specific as possible – give tangible and relatable examples, name countries, policies, organisations etc
- Evidence your impact – provide evidence to support your claims and include quotes and extracts in your Impact Case Study so that it is accessible to the audience
- Look at Examples – the REF 2014 Impact Case Study database provide a range of examples.
For more top tips Read our blog , visit our FAQ page for answers to your impact case study and REF related questions, or use our checklist to ensure your impact case study meets the key requirements.
Our writing retreats and writing sprints can help you to draft your Impact Case Study, check the training and development pages for up and coming workshops.
Below provides some examples of our research and the impact that they have achieved.

Addressing driver behaviour
Helping to create Ashwoods Lightfoot® and enable fleet managers to reduce the fuel costs and CO2 footprint from 2,500 vehicles

Creating fast, accurate tests for disease
Attaching electrochemical tags to DNA could allow GPs to diagnose and treat patients in just one visit.

Bio-banding – the search for tomorrow’s champions
The role of biobanding in improving the identification of future atheletes
For more examples of Research Excellence Framework (REF) impact case studies, visit the impact database for those submitted in the 2014 assessment exercise.
Recording your impact story
The University of Bath use PURE as their system for managing information about your research publications, projects, activities and impacts.
Explore UCD
- (opens in a new window) University Strategy
- University Governance
- President's Office
- Equality, Diversity & Inclusion
- Campus Development
- Study at UCD
- Current Students
- Campus Accommodation
- International Student Experience
- Access & Lifelong Learning
- Careers Network
- Sports Clubs
- (opens in a new window) Student Societies
Research & Innovation
- Innovation at NovaUCD
- Graduate Studies
- Support for Researchers
- (opens in a new window) Find a UCD Researcher
- UCD College of Arts and Humanities
- UCD College of Business
- UCD College of Engineering and Architecture
- UCD College of Health and Agricultural Sciences
- UCD College of Science
- UCD College of Social Sciences and Law
- All Colleges and Schools
- News & Opinion
- Work at UCD
- UCD in the Community
- Global Partnerships
- (opens in a new window) UCD Foundation
- University Relations
Key Services
- Staff Directory
- Sport & Fitness
- IT Services
- (opens in a new window) Commuting
- (opens in a new window) UCD Map
- (opens in a new window)
Writing an impact case study
We believe case studies are one of the best ways to share and celebrate the impact of your research. Evidence alone can’t capture the richness of your impact story: it requires a narrative. A story to describe how your research made a difference in the world.
These stories are often text-based, but you might also consider multimedia case studies, like those we produce of the finalists of our annual Impact Competition ' page"> Impact Competition .
On this page you will find various tools and guides to help you write the best case study possible.
Impact case study template
Our case study template [docx] is designed to make writing a case study as painless as possible. As the word count is limited, we encourage you to write concisely, avoiding technical jargon. This template doubles as the application form for our Impact Competition ' page"> Impact Competition , so if you’re thinking about writing a case study, why not enter?
What makes an excellent case study?
This image shows what we at UCD believe goes into a good case study. These are also the three criteria that the judging panel use to assess case studies in UCD’s Impact Competition.

Case study examples
One of the best ways to learn how to write a case study is to read others:
- UCD Case Studies ' page"> UCD Case Studies – a sample of case studies from researchers at UCD, using the template above.
- UK REF Case Studies ' page" tabindex="0"> (opens in a new window) UK REF Case Studies – this database from the 2021 Research Excellence Framework contains more than 6,000 impact case studies. You can use the search function or filter by Unit of Assessment to find case studies in areas similar to your own. You can also view studies a similar database of case studies from the (opens in a new window) 2014 REF .
- Australian Research Council Case Studies ' page" tabindex="0"> (opens in a new window) Australian Research Council Case Studies – another searchable database of case studies from a national research assessment exercise.
- (opens in a new window) University of Limerick Case Studies – you can sort this selection of case studies by QS Ranking Subject Areas and by the relevant Sustainable Development Goals.
Tips for writing your own case study
The tips in this infographic will help you tell a compelling story that celebrates the societal impact of your work. Click here to download the guide as a PDF booklet .
Case study tips

Reflections on Research Impact video series
Episode 7 of NUI Galway’s (opens in a new window) nine-part video series offers further guidance on how to write an impact case study:
UCD Research and Innovation
Stephen Kemp
funding + impact
REF2021: 4* impact case studies
We all know there’s more to impact than REF impact case studies. However, they represent a lot of hard work and the new REF2021 database of 6,781 impact case studies is so big and wide-ranging that it’s a major resource for anyone interested in research impact. A look at these impact case studies can help academics and research managers understand what impact may look like in a particular area, plan and articulate impact, scope relevant stakeholders and engagement strategies, and consider what evidence and indicators might be relevant when describing different kinds of impact.
The database can be searched and filtered in a number of ways but (beyond sitting with a spreadsheet of REF results) there is no easy way to pick out the highest scoring examples. That’s why many REF and impact managers in universities across the UK will be making lists of 4* impact case studies from REF2021. Here’s mine – click on the UoA of interest below and you’ll uncover links to the (publicly available) 4* impact case studies in that area. These are case studies that are unambiguously identifiable as scoring 4* – there are many other 4* examples but they are buried in submissions.
Of course, it is highly reductionist to focus on these 246 publicly available, identifiable 4* case studies – they represent less than 4% of the whole REF2021 impact case study database – but I know (from my own work with academics and research managers) that this list is a useful entry point to exploring the database more widely.
It’s worth noting that not every UoA had unambiguously identifiable 4* case studies. In case the UoA you are interested in doesn’t appear below, watch this space because I’ll be putting together an accompanying list of the top 5 impact submissions in every UoA .
I hope this all makes sense and helps you find some useful impact case study examples, whatever your area. Any issues, just leave a comment or get in touch !
Published by Stephen Kemp
View all posts by Stephen Kemp

The RAE2020 Impact Case Studies database contains 342 documents that describe the wider impact of research that took place in UGC-funded universities. These case studies have been enhanced using various data-mining techniques to provide additional metadata relating to impact topics, impact sectors, research categories, geographic locations and funder acknowledgements. These data have also been used to produce a series of reports including 11 thematic commentaries and an analytical overview drawing the information together.
The full list of case studies is provided below. Use the filters to refine the list according to specific metadata fields, or search for case studies that contain certain text or keywords. Refer to the FAQs page to find out more about search and filtering.
Loading Case Studies
- Publications
- Results & submissions
- Expert panels
- Equality & diversity
- About the REF
Research Excellence Framework
The Research Excellence Framework (REF) is the new system for assessing the quality of research in UK higher education institutions.
The results of the 2014 REF were published on 18 December 2014.
REF 2014 - key links
- 2014 REF Results and submissions
- Evaluation of the 2014 REF
- REF Manager's report (March 2015)
- Panel overview reports (Jan 2015)
- EDAP's report on equality and diversity (Jan 2015)
- Key facts leaflet about the REF
REF impact case studies
- A searchable online database and an initial analysis of REF impact case studies are available.
Contact REF | Copyright ©2014 REF | Disclaimer
We use some essential cookies to make this website work. We’d like to set some additional cookies to understand how you use the website and to improve it. We also use cookies set by other sites to help us deliver content from their services. You can read more about our cookies before you choose.
- Accept additional cookies
- Reject additional cookies
This is a new website – your feedback will help us to improve it.
What are they?
Impact case studies help share best practice and learnings from across the NHS.
Health librarians and knowledge specialists, working closely with staff and organisations within the NHS and wider health sector, bring tangible benefits, including:
- savings in time
- better operational efficiency
Case Studies
Case studies can be used to effectively capture and summarise the outcome of interviews.
The information can be used for advocacy, marketing and promotion of knowledge and library services (KLS).
Examples of our impact
Impact Case Studies database - a collection of good impact case studies submitted by KLSs.
Vignettes showcase impact case studies. Combining visual imagery and text, they highlight the importance of your service and its impact on your organisation and/or the wider NHS.
Contact the Knowledge for Healthcare team on [email protected] for any of the vignettes in an accessible format.
Create your own vignette using the Impact Case Study Vignette Template .
Page last reviewed: 15 June 2021
- How to search
- Terms of Use
- REF2014 Home
The Higher Education Funding Council for England (HEFCE), on behalf of a steering group representing the UK Funding Bodies, Research Councils and the Wellcome Trust, commissioned Digital Science, working in conjunction with the Policy Institute and Digital Humanities at King’s College London, as well as Nature Publishing Group, to analyse the impact case studies submitted to the 2014 Research Excellence Framework (REF). The case studies outline changes and benefits to the UK economy, society, culture, public policy and services, health, the environment and quality of life and impacts in these sectors beyond the UK.
Digital Science created and developed this website and its underpinning database. Digital Science, a Holtzbrinck company, develops software, delivers consulting and works with entrepreneurs to make research more efficient ( http://www.digital-science.com/ ).
The Policy Institute at King’s produced a synthetic analytical report, building on extensive work carried out by the Institute and drawing on the data indexed here ( http://www.kcl.ac.uk/sspp/policy-institute/index.aspx ).
Nature Publishing Group published a separate report on the REF and impact analysis ( http://www.nature.com/nature/supplements/collections/npgpublications/impact ).
REF impact case studies were written by HEIs, following a four-page template provided for REF submissions. The template was structured across a title and five sections (summary, research, references, impact and evidence). For further information on REF criteria, please see: http://www.ref.ac.uk/pubs/2011-02/
This website presents a normalized version of the case studies, preserving original text with modifications to a common format to support accessibility. PDF originals can also be downloaded. The development of the website was informed by interviews with representative individuals and bodies for user groups including academics, HEI managers, funding bodies, Government departments, commercial research users and UK and overseas policy analysts. Their requirements and expectations formed part of the design and the subsequent testing for functionality.
Case studies have been tagged with information about fields of research, impact types and location of activity to enable indexing and faster searching. Flexible keyword-bsed search is also available, supported by a high level of search functionality.
Research publication references in case studies have been individually identified where possible, to improve access to supporting information. Not all authors provided DOIs and additional identification has been carried out by Thomson Reuters to enable links to the Web of Science TM
- Thomson Reuters is the world’s leading source of intelligent information for businesses and professionals. It combines industry expertise with innovative technology to deliver critical information to leading decision makers in the financial and risk, legal, tax and accounting, intellectual property and science and media markets, powered by the world's most trusted news organization. ( http://thomsonreuters.com/about-us/ )
- Whether looking at data, books, journals, proceedings or patents, Web of Science provides a single destination to access the most reliable, integrated, multidisciplinary research. Quality, curated content delivered alongside information on emerging trends, subject specific content and analysis tools make it easy for students, faculty, researchers, analysts, and program managers to pinpoint the most relevant research to inform their work. ( http://thomsonreuters.com/thomson-reuters-web-of-science/ )
Case studies can be selected and downloaded for further study.
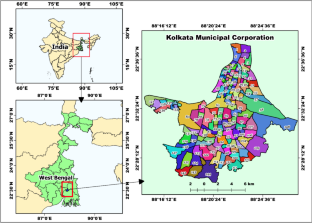
Changing urban land types and its locational impact on groundwater resources: a case study on Megacity Kolkata
- Published: 06 June 2024
Cite this article

- Suddhasil Bose ORCID: orcid.org/0000-0003-4836-7779 1 ,
- Asis Mazumdar 1 &
- Snehamanju Basu 2
Groundwater exploitation poses significant challenges in urban areas, as the depletion of groundwater levels (GWL) and degradation of groundwater quality (GWQ) are pervasive issues worldwide. This article aims to examine the locational influence of significant urban land types on groundwater resources, with Kolkata selected as the study area due to its pronounced GWL depletion and deteriorated GWQ. By utilizing remote sensing technology, this study individually identifies different urban land categories, such as built-up areas, green spaces, and surface water bodies, at intervals of a decade. The combined impact of these urban land types is then analysed and clustered into three distinct segments. To assess the spatial variation of GWQ, data on groundwater resources from the study area are collected, and the water quality index (WQI) is generated. Additionally, spatial autocorrelation (SA) analysis is employed to comprehend the spatial distribution of groundwater resources. Correlation coefficients are calculated to establish the relationship between different urban land types and groundwater resources. Subsequently, geographically weighted regression (GWR) is implemented to observe and identify local variations in GWL and GWQ concerning built-up areas, green spaces, and surface water bodies. The results obtained from this modelling approach demonstrate that the expansion of built-up areas positively contributes to groundwater degradation, while the presence of greater green spaces and surface water bodies in urban areas helps mitigate groundwater deterioration. The accuracy of the findings is evaluated, yielding satisfactory results with a quasi R 2 value exceeding 0.80 for groundwater resources in both years separately and by mapping local R 2 values. This study successfully identifies the impact of different urban land types on groundwater resources at a local level, thereby revealing spatial variations among the variables. The findings offer valuable insights for fostering better sustainable development at the local scale within cities.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Data availability
Availability of data can be available upon request.
Abed, A. O., & Mohsin, M. K. (2022). Using the NDVI and NDBI indicators to study the urban expansion of the city of mahaweel for the period from 2003 to 2020 using geographic information systems. Journal of Optoelectronics Laser, 41 (6), 924–932. https://doi.org/10.5772/intechopen.97350
Article Google Scholar
Almadrones-Reyes, K. J., & Dagamac, N. H. A. (2022). Land-use/land cover change and land surface temperature in Metropolitan Manila, Philippines using landsat imagery. GeoJournal . https://doi.org/10.1007/s10708-022-10701-9
Al-Sefry, S. A., & Şen, Z. (2006). Groundwater rise problem and risk evaluation in major cities of arid lands—Jedddah Case in Kingdom of Saudi Arabia. Water Resources Management, 20 (1), 91–108. https://doi.org/10.1007/s11269-006-4636-2
An, X., Jin, W., Long, X., Chen, S., Qi, S., & Zhang, M. (2022). Spatial and temporal evolution of carbon stocks in Dongting Lake wetlands based on remote sensing data. Geocarto International, 8 , 1–20. https://doi.org/10.1080/10106049.2022.2093412
Aragaw, T. T., & Gnanachandrasamy, G. (2021). Evaluation of groundwater quality for drinking and irrigation purposes using GIS-based water quality index in urban area of Abaya-Chemo sub-basin of Great Rift Valley, Ethiopia. Applied Water Science, 11 (9), 1–20. https://doi.org/10.1007/s13201-021-01482-6
Article CAS Google Scholar
Ball, R. O., & Church, R. L. (1980). Water quality indexing and scoring. Journal of the Environmental Engineering Division, 106 (4), 757–771. https://doi.org/10.1061/JEEGAV.0001067
Boateng, T. K., Opoku, F., Acquaah, S. O., & Akoto, O. (2016). Groundwater quality assessment using statistical approach and water quality index in Ejisu-Juaben Municipality, Ghana. Environmental Earth Sciences, 75 (6), 1–14. https://doi.org/10.1007/s12665-015-5105-0
Bose, S, Mazumdar, A., & Basu, S. (2020). Review on present situation of groundwater scenario on Kolkata Municipal Area. In IOP conference series: Earth and environmental science (Vol. 505, p. 12022). https://doi.org/10.1088/1755-1315/505/1/012022
Bose, S., Mazumdar, A., & Basu, S. (2023). Evolution of groundwater quality assessment on urban area—A bibliometric analysis. Groundwater for Sustainable Development, 20 , 100894. https://doi.org/10.1016/j.gsd.2022.100894
Bose, S., Mazumdar, A., & Halder, S. (2024). Groundwater sustainability in the face of urban expansion: A case study on Kolkata’s ongoing challenge. Groundwater for Sustainable Development, 25 , 101162. https://doi.org/10.1016/j.gsd.2024.101162
Brown, R. M., McClelland, N. I., Deininger, R. A., & Tozer, R. G. (1970). A water quality index-do we dare. Water and Sewage Works, 117 , 10.
Google Scholar
Brunsdon, C., Fotheringham, S., & Charlton, M. (1998). Geographically weighted regression. Journal of the Royal Statistical Society: Series D (The Statistician), 47 (3), 431–443.
Brunsdont, C., Fotheringham, S., & Charlton, M. (1998). Geographically weighted regression—Modelling spatial non-stationarity. Journal of the Royal Statistical Society: Series D Statistics, 47 (3), 431–443. https://doi.org/10.1111/1467-9884.00145
Dinius, S. H. (1987). Design of an index of water quality. Journal of the American Water Resources Association, 23 (5), 833–843. https://doi.org/10.1111/j.1752-1688.1987.tb02959.x
Dutta, K., Basu, D., & Agrawal, S. (2021). Synergetic interaction between spatial land cover dynamics and expanding urban heat islands. Environmental Monitoring and Assessment, 193 (4), 184. https://doi.org/10.1007/s10661-021-08969-4
Elmahdy, S., Mohamed, M., & Ali, T. (2020). Land use/land cover changes impact on groundwater level and quality in the northern part of the United Arab Emirates. Remote Sensing, 12 (11), 1715. https://doi.org/10.3390/RS12111715
Fatemi, M., & Narangifard, M. (2019). Monitoring LULC changes and its impact on the LST and NDVI in District 1 of Shiraz City. Arabian Journal of Geosciences, 12 (4), 1–12. https://doi.org/10.1007/s12517-019-4259-6
Gascon, M., Cirach, M., Martinez, D., Dadvand, P., Valentin, A., Plasència, A., & Nieuwenhuijsen, M. J. (2016). Normalized difference vegetation index (NDVI) as a marker of surrounding greenness in epidemiological studies: The case of Barcelona city. Urban Forestry & Urban Greening, 19 , 88–94. https://doi.org/10.1016/j.ufug.2016.07.001
Gesels, J., Dollé, F., Leclercq, J., Jurado, A., & Brouyère, S. (2021). Groundwater quality changes in peri-urban areas of the Walloon region of Belgium. Journal of Contaminant Hydrology, 240 , 103780. https://doi.org/10.1016/j.jconhyd.2021.103780
Getis, A. (2007). Reflections on spatial autocorrelation. Regional Science and Urban Economics, 37 (4), 491–496. https://doi.org/10.1016/j.regsciurbeco.2007.04.005
Ghosh, S., Kumar, D., & Kumari, R. (2022). Assessing spatiotemporal dynamics of land surface temperature and satellite-derived indices for new town development and suburbanization planning. Urban Governance . https://doi.org/10.1016/j.ugj.2022.05.001
He, S., & Wu, J. (2019). Relationships of groundwater quality and associated health risks with land use/land cover patterns: A case study in a loess area, Northwest China. Human and Ecological Risk Assessment: an International Journal, 25 (1–2), 354–373. https://doi.org/10.1080/10807039.2019.1570463
Horton, R. K. (1965). An index number system for rating water quality. Journal of Water Pollution Control Federation, 37 (3), 300–306.
Hussain, S., Mubeen, M., Ahmad, A., Majeed, H., Qaisrani, S. A., Hammad, H. M., & Nasim, W. (2022). Assessment of land use/land cover changes and its effect on land surface temperature using remote sensing techniques in Southern Punjab, Pakistan. Environmental Science and Pollution Research . https://doi.org/10.1007/s11356-022-21650-8
John, B., Das, S., & Das, R. (2022). Natural groundwater level fluctuations of Kolkata City based on seasonal field data and population growth using geo-spatial application and characterised statistical techniques. Environment, Development and Sustainability . https://doi.org/10.1007/s10668-022-02313-7
Khan, A., Atta-Ur-rahman, S., & Ali, M. (2019). Impact of built environment on groundwater depletion in Peshawar, Pakistan. Journal of Himalayan Earth Sciences, 52 (1), 86–105.
Khan, M. R., Koneshloo, M., Knappett, P. S. K., Ahmed, K. M., Bostick, B. C., Mailloux, B. J., et al. (2016). Megacity pumping and preferential flow threaten groundwater quality. Nature Communications, 7 (1), 12833. https://doi.org/10.1038/ncomms12833
Krishna Kumar, S., Logeshkumaran, A., Magesh, N. S., Godson, P. S., & Chandrasekar, N. (2015). Hydro-geochemistry and application of water quality index (WQI) for groundwater quality assessment, Anna Nagar, part of Chennai City, Tamil Nadu, India. Applied Water Science, 5 (4), 335–343. https://doi.org/10.1007/s13201-014-0196-4
Krogulec, E., Małecki, J. J., Porowska, D., & Wojdalska, A. (2020). Assessment of causes and effects of groundwater level change in an urban area (Warsaw, Poland). Water, 12 (11), 3107. https://doi.org/10.3390/w12113107
Li, W., Zhang, W., Li, Z., Wang, Y., Chen, H., Gao, H., et al. (2022). A new method for surface water extraction using multi-temporal Landsat 8 images based on maximum entropy model. European Journal of Remote Sensing, 55 (1), 303–312. https://doi.org/10.1080/22797254.2022.2062054
Liaqat, M. U., Mohamed, M. M., Chowdhury, R., Elmahdy, S. I., Khan, Q., & Ansari, R. (2021). Impact of land use/land cover changes on groundwater resources in Al Ain region of the United Arab Emirates using remote sensing and GIS techniques. Groundwater for Sustainable Development, 14 , 100587. https://doi.org/10.1016/j.gsd.2021.100587
Lopez-Gunn, E., Llamas, M. R., Garrido, A., & Sanz, D. (2011). Groundwater management. In Treatise on water science (Vol. 1, pp. 97–127). Elsevier. https://doi.org/10.1016/B978-0-444-53199-5.00010-5
Lv, G., Zheng, S., & Hu, W. (2022). Exploring the relationship between the built environment and block vitality based on multi-source big data: An analysis in Shenzhen, China. Geomatics, Natural Hazards and Risk, 13 (1), 1593–1613. https://doi.org/10.1080/19475705.2022.2091484
Mansour, K., Aziz, M. A., Hashim, S., & Effat, H. (2022). Impact of anthropogenic activities on urban heat islands in major cities of El-Minya Governorate, Egypt. The Egyptian Journal of Remote Sensing and Space Science . https://doi.org/10.1016/j.ejrs.2022.03.014
Mishra, B., Sandifer, J., & Gyawali, B. R. (2019). Urban heat island in kathmandu, nepal: Evaluating relationship between ndvi and lst from 2000 to 2018. International Journal of Environment, 8 (1), 17–29. https://doi.org/10.3126/ije.v8i1.22546
Montgomery, D. C., Peck, E. A., & Vining, G. G. (2021). Introduction to linear regression analysis . John Wiley & Sons.
Mukherjee, F. (2022). Environmental impacts of urban Sprawl in Surat, Gujarat: An examination using Landsat data. Journal of the Indian Society of Remote Sensing . https://doi.org/10.1007/s12524-022-01509-8
Mulyadi, A., Dede, M., & Widiawaty, M. A. (2020). Spatial interaction of groundwater and surface topographic using geographically weighted regression in built-up area. In IOP conference series: Earth and environmental science (Vol. 477, p. 012023). IOP Publishing. https://doi.org/10.1088/1755-1315/477/1/012023
Okotto, L., Okotto-Okotto, J., Price, H., Pedley, S., & Wright, J. (2015). Socio-economic aspects of domestic groundwater consumption, vending and use in Kisumu, Kenya. Applied Geography, 58 , 189–197. https://doi.org/10.1016/j.apgeog.2015.02.009
Patra, S., Sahoo, S., Mishra, P., & Mahapatra, S. C. (2018). Impacts of urbanization on land use /cover changes and its probable implications on local climate and groundwater level. Journal of Urban Management, 7 (2), 70–84. https://doi.org/10.1016/j.jum.2018.04.006
Pius, A., Jerome, C., & Sharma, N. (2011). Evaluation of groundwater quality in and around Peenya industrial area of Bangalore, South India using GIS techniques. Environmental Monitoring and Assessment, 184 (7), 4067–4077. https://doi.org/10.1007/S10661-011-2244-Y
Prasad, S., & Singh, R. B. (2022). Urban Heat Island (UHI) assessment using the satellite data: A case study of Varanasi City, India. In Smart cities for sustainable development (pp. 287–299). Springer. https://doi.org/10.1007/978-981-16-7410-5_17
Ray, B., & Shaw, R. (2016). Water stress in the megacity of Kolkata, India, and its implications for urban resilience. In Urban disasters and resilience in Asia (pp. 317–336). Elsevier. https://doi.org/10.1016/B978-0-12-802169-9.00020-3
Siddik, M. S., Tulip, S. S., Rahman, A., Islam, M. N., Haghighi, A. T., & Mustafa, S. M. T. (2022). The impact of land use and land cover change on groundwater recharge in northwestern Bangladesh. Journal of Environmental Management, 315 , 115130. https://doi.org/10.1016/j.jenvman.2022.115130
Sinaga, K. P., & Yang, M. S. (2020). Unsupervised K-means clustering algorithm. IEEE Access, 8 , 80716–80727. https://doi.org/10.1109/ACCESS.2020.2988796
Tavares, A. O., Pato, R. L., & Magalhães, M. C. (2012). Spatial and temporal land use change and occupation over the last half century in a peri-urban area. Applied Geography, 34 (2), 432–444. https://doi.org/10.1016/j.apgeog.2012.01.009
Vaddiraju, S. C., & Reshma, T. (2022). Urbanization implications on hydro-meteorological parameters of Saroor Nagar Watershed of Telangana. Environmental Challenges . https://doi.org/10.1016/j.envc.2022.100562
Vázquez-Suñé, E., Sánchez-Vila, X., & Carrera, J. (2005). Introductory review of specific factors influencing urban groundwater, an emerging branch of hydrogeology, with reference to Barcelona, Spain. Hydrogeology Journal, 13 (3), 522–533. https://doi.org/10.1007/s10040-004-0360-2
Verma, P., Singh, P., & Srivastava, S. K. (2020). Impact of land use change dynamics on sustainability of groundwater resources using earth observation data. Environment, Development and Sustainability, 22 (6), 5185–5198. https://doi.org/10.1007/s10668-019-00420-6
Wakode, H. B., Baier, K., Jha, R., & Azzam, R. (2018). Impact of urbanization on groundwater recharge and urban water balance for the city of Hyderabad, India. International Soil and Water Conservation Research, 6 (1), 51–62. https://doi.org/10.1016/j.iswcr.2017.10.003
Xiao, S., Fügener, T., Wende, W., Yan, W., Chen, H., Syrbe, R., & Xue, B. (2022). The dynamics of vegetation and implications for ecosystem services in the context of urbanisation: An example from Huangyan-Taizhou, China. Ecological Engineering, 179 , 106614. https://doi.org/10.1016/j.ecoleng.2022.106614
Yadav, V., & Bhagat, R. B. (2015). Spatial dynamics of population in Kolkata urban agglomeration. In Urban development challenges, risks and resilience in Asian mega cities (pp. 157–173). Springer. https://doi.org/10.1007/978-4-431-55043-3_9
Yang, W., Deng, M., Tang, J., & Luo, L. (2022). Geographically weighted regression with the integration of machine learning for spatial prediction. Journal of Geographical Systems . https://doi.org/10.1007/s10109-022-00387-5
Yang, X., & Chen, L. (2017). Evaluation of automated urban surface water extraction from Sentinel-2A imagery using different water indices. Journal of Applied Remote Sensing, 11 (2), 026016. https://doi.org/10.1117/1.jrs.11.026016
Zhu, K., Bayer, P., Grathwohl, P., & Blum, P. (2015). Groundwater temperature evolution in the subsurface urban heat island of Cologne, Germany. Hydrological Processes, 29 (6), 965–978. https://doi.org/10.1002/hyp.10209
Download references
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
School of Water Resources Engineering, Jadavpur University, Kolkata, West Bengal, 700032, India
Suddhasil Bose & Asis Mazumdar
Department of Geography, Lady Brabourne College, Kolkata, West Bengal, 700017, India
Snehamanju Basu
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Suddhasil Bose .
Ethics declarations
Conflict of interest.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Bose, S., Mazumdar, A. & Basu, S. Changing urban land types and its locational impact on groundwater resources: a case study on Megacity Kolkata. Environ Dev Sustain (2024). https://doi.org/10.1007/s10668-024-05095-2
Download citation
Received : 17 July 2022
Accepted : 27 May 2024
Published : 06 June 2024
DOI : https://doi.org/10.1007/s10668-024-05095-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Urban lands
- Groundwater resources
- Locational impact
- Water quality index
- Spatial autocorrelation
- Geographical weightage regression
- Find a journal
- Publish with us
- Track your research

Center for Regional Food Systems
Small Potatoes, Big Impact: Michigan Farm to School Potato Processing Partnership Case Study
June 4, 2024 - Mariel Borgman <[email protected]> and Garrett Ziegler <[email protected]>
Potatoes are a highly accepted vegetable among students and have a high-volume potential. This resource examines the results of potato processing trials at a Michigan school district. Dan Gorman, farm to school innovator and food service director for Montague Area Public Schools, wanted to explore the possibility of processing Michigan produce in-house along with a more nutritious implementation as roasted potatoes, in place of french fries.

As recipients of a sub-award from the Michigan Department of Education’s Specialty Crop Block Grant Program, through the Michigan Department of Agriculture and Rural Development, MSU Extension supported the development of this potato processing program at Montague Area Public Schools. This aligns with the award’s goal to fund farm to school supply chain development in support of the 10 Cents a Meal program.
This resource can be used to explore the possibility of in-school processing for Michigan grown produce, as well as the supply chain challenges that may arise between farmers and institutions.
DOWNLOAD FILE
Tags: agriculture , beginning farmer , center for regional food systems , community , community food systems , farm management , farm marketing , field crops , food hubs , food processing , michigan farm to institution , msu extension , organic agriculture , product center , vegetables

Mariel Borgman [email protected]

Garrett Ziegler [email protected]
new - method size: 1 - Random key: 0, method: personalized - key: 0
You Might Also Be Interested In
Accessibility questions:.
For questions about accessibility and/or if you need additional accommodations for a specific document, please send an email to ANR Communications & Marketing at [email protected] .
- agriculture,
- beginning farmer,
- center for regional food systems,
- community food systems,
- farm management,
- farm marketing,
- field crops,
- food processing,
- michigan farm to institution,
- msu extension,
- organic agriculture,
- product center,
Food System Infrastructure, Planning and Policy
- Michigan Food Hub Learning and Innovation Network
- Michigan Food System Workforce Assessment
- Michigan Local Food Council Network
- National Food Hub Survey
- Racial Equity in the Food System Workgroup
Michigan Good Food
- Michigan Good Food Charter
- Michigan Good Food Charter Shared Measurement Project
- Michigan Good Food Fund Technical Assistance Providers
Farm to Institution/School
- 10 Cents a Meal
- Michigan Farm to ECE
- Michigan Farm to ECE Network
- Michigan Farm to Institution Network
- Michigan Farm to School

- Case Studies
- Sharestates
Sharestates’ smooth transition to AWS infrastructure delivers improved user experience and optimizes operations
This real estate lending and investing marketplace modernized its database, enhanced security and accelerated system responsiveness..

Modernize legacy infrastructure to optimize performance and security, improve scalability and adopt new technologies.
Professional & Managed Services
Our customer
Sharestates , an online real estate lending and investing marketplace based in Great Neck, NY, offers investors access to institutional-quality real estate investments through its online marketplace. Since its 2014 founding, the company has funded more than $3 billion in projects nationwide. Sharestates' achievements are rooted in its experienced leadership team, prudent underwriting practices and focus on building strong relationships with borrowers and brokers.
Sharestates' platform allows accredited investors to participate in commercial mortgage investments with as little as $5,000 and receive monthly interest payments. Registered borrowers submit detailed information about the properties including text files, photos and video which are reviewed as part of the investor’s due diligence process. The system connects the two parties, and borrowers can log into a portal to track loan requests, monitor loans and manage payments. The entire process is data intensive, and the platform must be highly responsive, able to access this data quickly as investors review many properties.
“I highly recommend to anyone that’s going to make this move to use Rackspace Technology because it makes things a lot easier. They’ve done it, they know what to do and they will walk you through it.”

The obstacles they faced
To align with future growth goals and enhance infrastructure, Sharestates strategically decided to migrate to Amazon Web Services (AWS). This move aimed to improve customer experience with faster response time, optimize operations with faster access to internal and external systems, improve scalability and provide the company access to the latest cloud technologies and best practices.
“We had a very good experience with Rackspace Technology,” said Radni Davoodi, CTO and Co-founder of Sharestates. “So when we found out that they were willing to not only help us migrate and map everything out for us, but also stay to monitor and support us, it was a no-brainer.”
"Over the past few years, we knew that AI was coming down the pike,” said Davoodi. “We knew we wanted to go mobile, we knew how important remote working would become based on the experience with the pandemic. We concluded that we needed to be fully operational in the cloud."

"Our goal has always been to connect investors and borrowers in a streamlined process. This move is going to allow us to take our platform to a mobile environment, keep up with our competitors' technology and stay at the forefront of the commercial real estate lending industry."
How we helped
Sharestates chose AWS for its cost-effectiveness, industry adoption and redundancy capabilities. Rackspace Technology connected Sharestates with an AWS representative early on, enabling the company to secure AWS funding and cost savings.
Rackspace recommended a single-phase migration, allowing the transition to be completed over a weekend without downtime. Using the Landing Zone Accelerator on AWS (LZA), the Rackspace team deployed a secure and compliant landing zone in less than two weeks, providing a solid foundation for Sharestates' AWS environment.
The migration team utilized various tools and services, including AWS Application Migration Service and proprietary scripts to efficiently migrate Sharestates' 3TB of data across 11 servers, ensuring a smooth and secure transition.
During the migration process, Rackspace identified and addressed potential vulnerabilities by implementing proper security groups, network access controls and monitoring to safeguard sensitive data. It also upgraded outdated and unsupported database versions, refactoring database schemas and queries to resolve compatibility issues.
Using infrastructure-as-code, Rackspace efficiently deployed a consistent infrastructure within the landing zone set up by the LZA. The team leveraged managed database services to provide automated backups, patching and monitoring, delivering a reliable and scalable environment for Sharestates' databases.
One significant upgrade was the migration of the Maria DB instance on Amazon Elastic Compute Cloud (EC2) to Amazon Relational Database Service (RDS), which optimized Sharestates' database performance, resulting in faster speeds and improved performance for extensive reports and large data pulls. Rackspace performed the migration by writing custom scripts to transfer the data.
"Once we did the migration, we felt this was the right 'next step' because we wanted to just build a foundation the right way," said Davoodi. "With the Rackspace team recommending it and our internal tech teams agreeing that it's the right time to do it, we then decided to move it, upgrade it, optimize it."
The move has simplified the deployment of new services and infrastructure for Sharestates, as many third-party providers build systems and APIs specifically for AWS, enabling faster integration and the development of new features.
"After the optimization, we realized that things were going a lot faster, and many of the reporting problems that we were experiencing from time to time were resolved," Davoodi said. "It improved not only our internal experiences but also the external experiences for our users."
Sharestates now relies on Modern Operations to provide post-migration support for its internal team. “It is helping our internal team to know that there’s somebody there to rely on in case we can’t figure it out,” said Davoodi. “That allows us to keep pushing and then know that we can always come back for guidance if necessary.”
These enhancements positioned Sharestates favorably within the financial technology community, particularly in terms of integrating third-party tools and developing new features that could provide a competitive edge.
"Our goal has always been to connect investors and borrowers in a streamlined process,” Davoodi said. “Looking ahead, this move is going to allow us to take our platform to a mobile environment, keep up with our competitors' technology and stay at the forefront of the commercial real estate lending industry."

Sharestates completed its migration to Amazon Web Services (AWS) over a weekend with zero downtime.

What we achieved together
The migration to AWS has modernized Sharestates' infrastructure, enhancing security and efficiency through a three-pronged approach: AWS provides a secure foundation, Rackspace Technology offers additional monitoring and Sharestates maintains its own internal system.
The transition was a significant milestone for Sharestates, and the Rackspace team played a crucial role in helping to ensure a smooth process. The comprehensive documentation provided by the Rackspace team served as a valuable resource for Davoodi to communicate the changes and gain necessary approvals.
"The Rackspace team mapped everything so brilliantly, that anybody could follow it very easily and see where everything is set up," said Davoodi. "It was almost like a roadmap, or a cheat sheet. It made my life easier to be the person signing off on things."
“Since the migration, Sharestates has been actively working to leverage the benefits of AWS,” Davoodi said. “We have seen several improvements:
- Faster user interface experience by investors
- Improved internal reporting experience by staff
- Faster processing speed by borrowers
- Improved performance of web application modules by all users
- Improved banking transfer processing speed
We have really tried to maximize everything that AWS offers,” he added. “Our new tech team has really pushed almost all the integrations that are available to us through AWS."
The database upgrade and cloud infrastructure deployment will continue to provide value for Sharestates as the company adapts to future business needs.
“We are looking into doing certain things for the application that we weren’t expecting to be able to accomplish,” said Davoodi. “We can do this in a much more efficient and cost-effective way because we have an optimized database and AWS infrastructure. Those two things are allowing us to give a great user experience to our clients. We hope that we can continue to develop and improve and keep building things with the help of Rackspace Technology, AWS and our tech team to cater to our industry.”
About Rackspace Technology
Rackspace Technology is a hybrid, multicloud solutions expert. We combine our expertise with the world’s leading technologies — across AI, applications, data and security — to deliver end-to-end solutions. We have a proven record of advising customers based on their business challenges, designing solutions that scale, building and managing those solutions, and optimizing returns into the future.
As a global hybrid, multicloud technology services pioneer, we deliver innovative capabilities to help customers build new revenue streams, increase efficiency and create incredible experiences. Named a best place to work, year after year according to Fortune, Forbes and Glassdoor, we attract and develop world-class talent to deliver the best expertise to our customers. Everything we do is wrapped in Fanatical Experience® — our obsession with customer success that drives us to help each customer work faster, smarter and stay ahead of what’s next.
Let’s Talk Strategy
Tell us a little about your challenges and we’ll contact you.
Please complete this form to have a specialist contact you.
By submitting this form, I acknowledge that someone from Rackspace Technology will contact me via email or phone to discuss my request.
You may withdraw your consent to receive additional information from Rackspace Technology at any time. Information collected in this form is subject to the Rackspace Technology Privacy Notice .
Rackspace Technology Support
To create a ticket or chat with a specialist regarding your account, log into your account.
- Legacy Datapipe One (Service Now)
- Rackspace Sovereign Services UK
Support Phone
1-800-961-4454
International Support
+1-512-361-4935
Help Documentation
- Support Documentation
- API Documentation
System status
- Email & Apps system status
- Rackspace system status
Rackspace Technology Careers
Rackspace Technology accelerates the value of the cloud during every phase of a customer’s digital transformation. Join us on our mission.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 June 2024
Psychiatric adverse events following COVID-19 vaccination: a population-based cohort study in Seoul, South Korea
- Hong Jin Kim ORCID: orcid.org/0000-0002-8162-9585 1 ,
- Min-Ho Kim ORCID: orcid.org/0000-0003-4909-2308 2 ,
- Myeong Geun Choi 3 &
- Eun Mi Chun ORCID: orcid.org/0000-0001-9616-2722 3
Molecular Psychiatry ( 2024 ) Cite this article
277 Accesses
37 Altmetric
Metrics details
- Bipolar disorder
- Schizophrenia
Evidence has suggested an increased risk of psychiatric manifestations following viral infections including coronavirus disease-2019 (COVID-19). However, psychiatric adverse events (AEs) after COVID-19 vaccination, which were documented in case reports and case series, remain unclear. This study is aimed to investigate the psychiatric AEs after COVID-19 vaccination from a large population-based cohort in Seoul, South Korea. We recruited 50% of the Seoul-resident population randomly selected from the Korean National Health Insurance Service (KNHIS) claims database on 1, January, 2021. The included participants ( n = 2,027,353) from the Korean National Health Insurance Service claims database were divided into two groups according to COVID-19 vaccination. The cumulative incidences per 10,000 of psychiatric AEs were assessed on one week, two weeks, one month, and three months after COVID-19 vaccination. Hazard ratios (HRs) and 95% Confidence interval (CIs) of psychiatric AEs were measured for the vaccinated population. The cumulative incidence of depression, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders at three months following COVID-19 vaccination were higher in the vaccination group than no vaccination group. However, schizophrenia and bipolar disorders showed lower cumulative incidence in the vaccination group than in the non-vaccinated group. Depression (HR [95% CI] = 1.683 [1.520–1.863]), anxiety, dissociative, stress-related, and somatoform disorders (HR [95% CI] = 1.439 [1.322–1.568]), and sleep disorders (HR [95% CI] = 1.934 [1.738–2.152]) showed increased risks after COVID-19 vaccination, whereas the risks of schizophrenia (HR [95% CI] = 0.231 [0.164–0.326]) and bipolar disorder (HR [95% CI] = 0.672 [0.470–0.962]). COVID-19 vaccination increased the risks of depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders while reducing the risk of schizophrenia and bipolar disorder. Therefore, special cautions are necessary for administering additional COVID-19 vaccinations to populations vulnerable to psychiatric AEs.
Similar content being viewed by others
Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population

Association of preexisting psychiatric disorders with post-COVID-19 prevalence: a cross-sectional study
COVID-19 and severe mental illness in Israel: testing, infection, hospitalization, mortality and vaccination rates in a countrywide study
Introduction.
In the unprecedented era of coronavirus disease-2019 (COVID-19), the global outbreak of COVID-19 has had an unpredictable and heterogeneous impact on the healthcare system worldwide [ 1 , 2 ]. Especially in mental illness, COVID-19 showed an increased risk of mental health problems together with lockdown, social distancing, and uncertain causes [ 3 , 4 ]. There have been growing concerns that the COVID-19 pandemic has increasingly had a detrimental effect on long-term mental health at an early stage in the development of vaccines [ 5 , 6 ].
The rapid development of COVID-19 vaccines, ranging from mRNA-based vaccines (BNT162b2, mRNA-1273) to viral vector vaccines (cDNA-based vaccines; AZD1222, JNJ-78436735), has contributed to overcoming the COVID-19 pandemic in the view of severity and mortality [ 1 , 7 ]. However, it has also given rise to new issues such as post-COVID-19 sequelae and vaccine-related adverse events (AEs) [ 2 , 5 , 6 , 7 , 8 , 9 , 10 ]. With their issues, mental health is still an unsolved concern in the post-COVID-19 era [ 4 , 6 ]. Many studies have focused on the correlation between mental health and COVID-19 breakthrough [ 11 ]. However, mental illness as a result of the COVID-19 vaccine itself, specifically post-vaccination psychiatric AEs was not well-studied, with scant evidence in the literature, which was documented primarily in the form of case reports and case series [ 12 , 13 , 14 , 15 ].
In this study, we investigated the psychiatric AEs including schizophrenia, depression, bipolar disorder, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders after COVID-19 vaccination from a population-based cohort using the Korean National Health Insurance Service (KNHIS) claims database in Seoul, South Korea.
Materials and methods
The concept and protocol of this study were approved by the Institutional Review Board (IRB) of our institute, which waived the requirement for informed consent because data analyses were performed retrospectively using anonymized data derived from the South Korean NHIS database.
Data source
We used the KNHIS claims database to recruit a randomly selected 50% of the population residing in Seoul on 1 January 2021 with their diagnostic records up to 31 December 2021. The process of selecting a random 50% of the population in Seoul was carried out by the KNHIS system. After authorization by KNHIS, the data collection was performed in November 2022. The psychiatric AEs included schizophrenia, mood disorders (depression, and bipolar disorder), anxiety, dissociative, stress-related, and somatoform disorders (anxiety disorders, obsessive-compulsive disorder, reacting to severe stress, and adjustment disorders, conversion disorders, somatoform disorders, and other neurotic disorders), sleep disorders, eating disorders, and sexual disorders using the International Classification of Diseases (ICD) Tenth Revision codes after the index date. This population-based cohort study was also conducted by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [ 16 ].
Study population
A total of 4,348,412 individuals living in Seoul, South Korea, constituting 50% of the population, were included and investigated as of January 1, 2021. Individuals under 20 years (n = 144,525) were excluded, leaving 4,203,887 individuals for analysis. We initially divided into two groups based on COVID-19 vaccination and defined as vaccinated group as individuals who received two doses of the COVID-19 vaccine. For the 3,839,014 vaccinated population, we excluded 1,684,625 individuals who did not receive a second dose by 1, October 2021. For 364,873 unvaccinated population, we excluded 13,890 individuals who died on 1, October 2021. The diagnostic records for the year preceding the index date were traced to investigate the causal relationship between vaccine administration and AEs. The occurrence of the target psychiatric disorders was defined as receiving a primary diagnosis of the disease from the day following the index date. Individuals who had received a primary or secondary diagnosis of any target disease for a year prior to index date were excluded from the study. We finally included the participants defined by two groups in this study: the vaccinated group (n = 1,718,999) and the non-vaccinated group (n = 308,354) (Fig. 1 ).
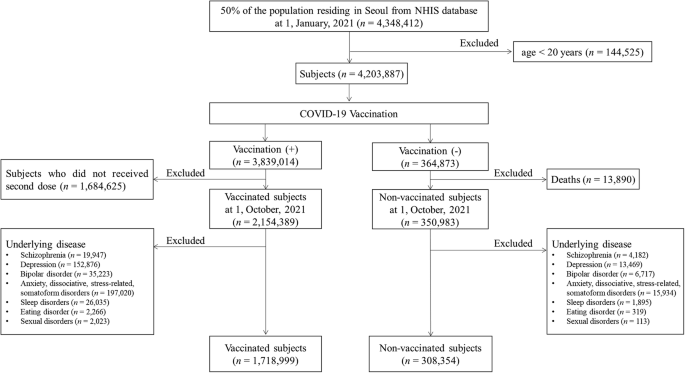
Flowchart of this study.
Outcome measurements
The primary outcome measure was the cumulative incidence of psychiatric AEs per 10,000 population at one week, two weeks, one month, and three months between two groups. The secondary outcome measures were risks of psychiatric target AEs for COVID-19 vaccination using the odd ratios (ORs) and hazard ratios (HRs). Furthermore, subgroup analyses were also conducted based on gender, age, the number of COVID-19 vaccine doses, the vaccine type (mRNA vaccine, cDNA vaccine, and heterologous vaccination), health insurance level, presence of diabetes mellitus (DM), hypertension (HTN), hyperlipidemia, and chronic obstructive pulmonary disease (COPD). Age, gender, insurance level, Charlson’s comorbidity index (CCI), presence of DM, HTN, hyperlipidemia, and COPD, and prior COVID-19 infection history were extracted using their ICD-19 codes, which were suggested by Sundararajan et al. [ 17 ]. The presence of comorbid diseases (i.e., DM, HTN, hyperlipidemia, and COPD), categories of CCI, and the prior COVID-19 infection history were determined based on receiving a primary or secondary diagnosis at least twice within one year before the index date. The National Health Insurance (NHI) premium was used as a proxy for income, as it is proportional to monthly income, encompassing both earnings and capital gains. The income quantiles of the enrolled participants were subdivided into three groups (low-, middle- and high-income groups in medical aid enrollees and the 0–33, 34–66, and 67–100 centiles of NHI enrollees). Detailed information for ICD-10 codes used for analysis is presented in Supplementary Table 1 .
Statistical analysis
Statistical analysis was performed using the SAS Enterprise Guide (version 8.3., SAS Institute, Cary, NC, USA). A normal distribution was confirmed with the Kolmogorov–Smirnov test. Baseline patient characteristics and comorbidities were reported as means ± standard deviation for continuous variables and ratio for categorical variables. Student’s t test was performed for continuous variables and the chi-square test for categorical variables. The cumulative incidence was calculated per 10,000 populations. To identify the association between COVID-19 vaccination and psychiatric AEs, a multiple logistic regression model was used for ORs, corresponding to 95% CIs. Cox proportional hazards regression was used to estimate the HRs and 95% CIs. Two-sided p values of 0.05 or less were considered to indicate statistical significance.
The participants’ characteristics
In total, 2,027,353 subjects were included in this study. Among them, 308,354 (15.21%) had not received the COVID-19 vaccine (i.e., non-vaccinated subjects, no vaccination group in this study), whereas 1,718,999 (84.79%) were vaccinated against COVID-19 (i.e., vaccinated subjects, the vaccinated group in this study). The baseline characteristics of the vaccinated and non-vaccinated groups are presented in Table 1 .
The cumulative incidences per 10,000 of psychiatric AEs following the COVID-19 vaccination
The cumulative incidence of the psychiatric AEs at three months was 0.51 (95% CI, 0.40–0.62) vs 1.98 (95% CI, 1.48–2.47) for schizophrenia, 18.30 (95% CI, 17.66-18.93) vs 14.24 (95% CI, 12.91–15.57) for depression, 0.79 (95% CI, 0.66–0.92) vs 1.39 (95% CI, 0.98–1.81) for bipolar disorder, 28.41 (95% CI, 27.62–29.21) vs 20.27 (95% CI, 18.68–21.86) for anxiety, dissociative, stress-related, and somatoform disorders, 0.30 (95% CI, 0.22–0.38) vs 0.32 (95% CI, 0.12–0.53) for eating disorder, 28.85 (95% CI, 28.05–29.96) vs 12.19 (95% CI, 10.96–13.43) for sleep disorders, 0.27 (95% CI, 0.19–0.34) vs 0.03 (95% CI, 0.00–0.10) for sexual disorders between the vaccinated group and non-vaccinated group. Therefore, the cumulative incidences of schizophrenia ( p < 0.001) and bipolar disorder ( p = 0.002) were significantly lower in the vaccinated group than in the non-vaccinated group. Meanwhile, depression ( p < 0.001), anxiety, dissociative, stress-related, and somatoform disorders ( p < 0.001), sleep disorders ( p < 0.001), and sexual disorders ( p = 0.007) showed significantly higher cumulative incidence in the vaccinated group than in the non-vaccinated group. There was no statistical difference in the cumulative incidence of eating disorders at three months between the two groups ( p = 0.724). Detailed information of cumulative incidence was presented in Table 2 .
The cumulative incidences per 10,000 of psychiatric AEs according to vaccine types
Our data was also stratified by vaccine type including vaccination using mRNA-based vaccine only (only mRNA vaccine), vaccination using cDNA-based vaccine only (only cDNA vaccine), and heterologous vaccination, which were compared by non-vaccinated group. For decreased incidences of schizophrenia and bipolar disorder following COVID-19 vaccination, schizophrenia showed the lowest cumulative incidence at three months in the case of heterologous vaccination (0.42; 95% CI, 0.05–0.79) compared to other vaccine types with statistical significances ( p < 0.001). The lowest cumulative incidence of bipolar disorder at three months was observed in the case of vaccination using only cDNA vaccine (0.39; 95% CI, 0.23-0.55) with a statistical difference ( p < 0.001). For increased incidences of depression, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders following COVID-19 vaccination, the highest cumulative incidence of depression at three months was significantly observed in heterologous vaccination (23.31; 95% CI, 20.56–26.05) compared to other vaccine types ( p < 0.001). However, the cumulative incidence of depression at three months was lower in the case of vaccination using only cDNA vaccine (12.26; 95% CI, 11.37–13.15) than in the non-vaccinated group (14.24; 95% CI, 12.91–15.57) with statistical differences ( p = 0.014). The incidence of anxiety, dissociative, stress-related, and somatoform disorders was significantly observed to be highest in the case of heterologous vaccination (31.75; 95% CI, 28.55–34.95), followed by only mRNA vaccination (29.13; 95% CI, 28.08–30.18) and only cDNA vaccination (26.53; 95% CI, 25.22–27.83) ( p < 0.001). The incidence of sleep disorders at three months was significantly observed to be high level in both cases of only cDNA vaccination (34.78; 95% CI, 33.28–36.28), and heterologous vaccination (32.09; 95% CI, 28.87–35.31), followed by only mRNA vaccination (24.98; 95% CI, 24.00–25.96) ( p < 0.001). The cumulative incidences of sexual disorders showed no statistical differences up to one month ( p > 0.05). At three months, the sexual disorder showed differences in cumulative incidence according to vaccine types ( p = 0.04). There was no statistical difference in the cumulative incidence of eating disorders at three months ( p = 0.785) according to vaccine types. The cumulative incidences of psychiatric AEs according to vaccine type are presented in Fig. 2 and Supplementary Table 2 .
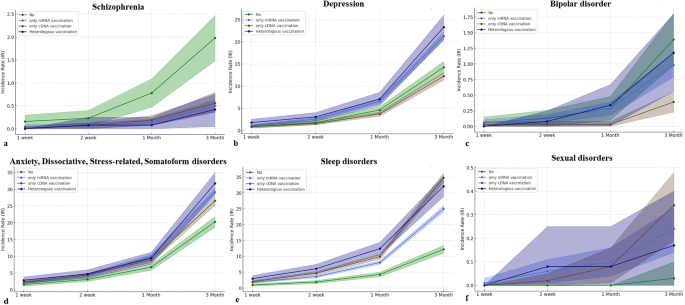
a Schizophrenia. b Depression. c Bipolar disorder. d Anxiety, dissociative, stress-related, and somatoform disorders. e Sleep disorder. f Sexual disorders.
The risks of psychiatric AEs following the COVID-19 vaccination
In the Cox proportional hazard model in this study, the HR for COVID-19 vaccination was 0.231 (95% CI, 0.164–0.326) for schizophrenia, 1.683 (95% CI, 1.520–1.863) for depression, 0.672 (95% CI, 0.470–0.962) for bipolar disorder, 1.439 (95% CI, 1.322–1.568) for anxiety, dissociative, stress-related, and somatoform disorders, 0.796 (95% CI, 0.395–1.604) for eating disorders, 1.934 (95% CI, 1.738–2.152) for sleep disorders, and 6.556 (95% CI, 0.890–48.296) for sexual disorders. Therefore, COVID-19 vaccination significantly decreased the risks of occurrence for schizophrenia and bipolar disorder, while significantly increasing the risks for depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders. There was no effect of COVID-19 vaccination on the occurrence of eating disorders and sexual disorders (Fig. 3a ).
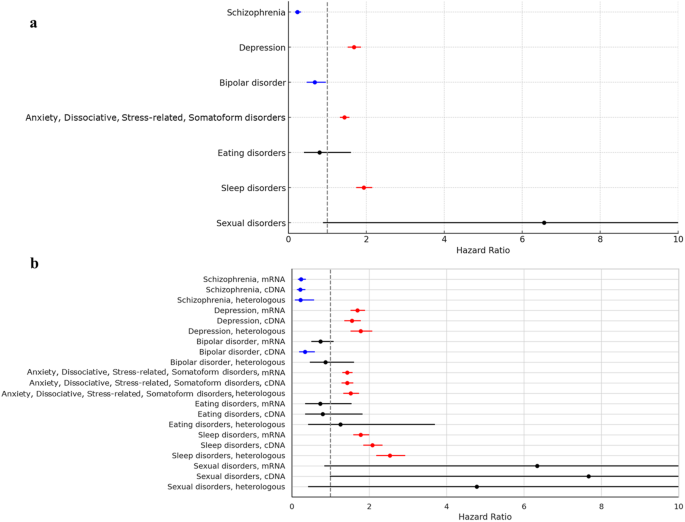
a The risks of psychiatric adverse events (AEs) according to COVID-19 vaccination. b The risks of psychiatric adverse events according to the COVID-19 vaccine types.
In the multivariate logistic model in this study, the ORs of target psychiatric AEs, except for bipolar disorder at one week, two weeks, and one month showed statistical significance, indicating similar patterns for HRs in the Cox proportional hazard model. For bipolar disorder, the OR showed 1.166 (95% CI, 0.240–5.670; p = 0.849) at one week, 0.946 (95% CI, 0.304–2.949; p = 0.924) at two weeks, 0.982 (95% CI, 0.463–2.079; p = 0.962) at one month, and 0.674 (95% CI, 0.471–0.964; p = 0.031). The detailed information for ORs of target psychiatric AEs was described in Supplementary Table 3 .
The risks of psychiatric AEs according to the COVID-19 vaccine type
We further assessed the risks of target psychiatric AEs according to the COVID-19 vaccine. For schizophrenia and bipolar disorder which were observed to have lower occurrences following COVID-19 vaccination, the HRs of schizophrenia were 0.239 (95% CI, 0.163–0.352) in only mRNA vaccination, 0.218 (95% CI, 0.138–0.343) in only cDNA vaccination, and 0.227 (95% CI, 0.091–0.566) in heterologous vaccination with statistical significances. On the other hand, the HR of bipolar disorder was statistically significant only in the case of only cDNA vaccination (0.339; 95% CI, 0.196–0.587). For depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders which were observed to have higher occurrences following COVID-19 vaccination, the HRs of depression (1.777; 95% CI, 1.527–2.067), anxiety, dissociative, stress-related, and somatoform disorders (1.521; 95% CI, 1.338–1.729), and sleep disorders (2.080; 95% CI, 1.855–2.332) showed the highest levels in the case of heterologous vaccination with statistical significances, respectively. There were no statistical differences in risks of eating disorders and sexual disorders according to vaccine types (Fig. 3b ).
The ORs of target psychiatric AEs, except for bipolar disorder at one week, two weeks, and one month also showed statistical significance, indicating similar patterns for HRs in the Cox proportional hazard model. For bipolar disorder, the OR for only cDNA vaccination showed 1.581 (95% CI, 0.172–14.496; p = 0.685) at one week, 0.459 (95% CI, 0.073–2.893; p = 0.407) at two weeks, 0.191 (95% CI, 0.039–0.939; p = 0.042) at one month, and 0.340 (95% CI, 0.197–0.589; p < 0.001). The detailed information for ORs of target psychiatric AEs according to vaccine types was described in Supplementary Table 3 .
Subgroup analysis for psychiatric AEs based on gender, age, insurance level, and CCI
As age increases, the risks of schizophrenia (HR, 1.027; 95% CI, 1.016–1.039) and sleep disorders (HR, 1.014; 95% CI, 1.012–1.016) significantly increase and the risks of depression (HR, 0.969; 95% CI, 0.966–0.971), bipolar disorder (HR, 0.982; 95% CI, 0.971–0.993), anxiety, dissociative, stress-related, somatoform disorders (HR, 0.988; 95% CI, 0.986–0.990) significantly decrease. Considering the HR values, age does not seem to largely affect the risk of psychiatric AEs. For the insurance level, the HR of schizophrenia at the high insurance level was 0.593 ( p = 0.007) with statistical differences compared to the low insurance level. The HRs of depression at the high insurance level and middle insurance level were respectively 0.904 ( p = 0.014) and 0.824 ( p < 0.001) with statistical differences. There were no statistical differences in other psychiatric disorders for the insurance levels. For CCI, a higher score of CCI more than 2 significantly increased the risks of depression (HR, 1.393; 95% CI, 1.217–1.596), anxiety, dissociative, stress-related, somatoform disorders (HR, 1.440; 95% CI, 1.306–1.587), and sleep disorders (HR, 1.315; 95% CI, 1.198–1.444) than zero score of CCI. Based on these results, women are mostly susceptible to psychiatric AEs (except for sexual disorders) compared to men. Detailed information for Cox proportional hazard model for psychiatric AEs was presented in Supplementary Table 4 .
The post-sequelae of COVID-19 and vaccine-related AEs have globally been concerns for mental illness, ranging from mild signs of mental symptoms to psychiatric disorders [ 18 ]. During the prolonged COVID-19 pandemic, there has been an emerging trend in complications of COVID-19 infection and vaccination, intensifying the psychosocial burdens [ 5 , 18 , 19 ]. Despite the considerable clinical benefits of the COVID-19 vaccination, it paradoxically made managing psychiatric disorders more challenging due to the contradictory outcomes associated with COVID-19 vaccination [ 11 , 13 , 14 , 15 , 18 , 19 , 20 , 21 ]. Here, we conducted a population-based retrospective cohort study for psychiatric AEs after COVID-19 vaccination in Seoul, South Korea. From our cohort between 1,718,999 vaccinated subjects and 308,354 non-vaccinated subjects, we found that the vaccinated subjects showed a significantly higher incidence of depression, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders and a significantly lower incidence of schizophrenia and bipolar disorder than the non-vaccinated subjects. Furthermore, COVID-19 vaccination increased risks of depression, anxiety, dissociative, stress-related, and somatoform disorders and sleep disorders but reduced risks of schizophrenia and bipolar disorder.
Some evidence between COVID-19 and mental illness has gradually grown since the most common symptoms of the long-COVID-19 pandemic were depression/anxiety, psychotic disorder, and cognitive impairment (called brain fog) experienced by 22% of patients within 6 months after COVID-19 infections [ 4 , 14 ]. However, there have been contradictory reports between mental illness and COVID-19 vaccinations. Chaudhuri et al. reported that vaccination significantly alleviated psychological distress measured by the General Health Questionnaire in the UK Household Longitudinal cohort study [ 18 ]. Meanwhile, Balasubramanian et al. reviewed the reports of psychiatric AEs to COVID-19 vaccines, which illustrated 14 cases of psychiatric reactions including psychosis, depression, and anxiety, dissociative, stress-related, and somatoform disorders [ 15 ]. To our knowledge, there are scarce studies on the association between vaccines and psychiatric AEs. Therefore, our population-based cohort study provides robust evidence for the psychiatric AEs after COVID-19 vaccinations. Furthermore, our study provided risks of psychiatric AEs according to vaccine type, revealing that the psychiatric disorders (depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders) with increased risks due to COVID-19 vaccination showed the highest risk in the case of heterogeneous vaccination. Meanwhile, occurrences of schizophrenia consistently decreased risks according to vaccine type but bipolar disorder showed significantly decreased risks from only cDNA vaccination.
Two representative mood disorders, depression, and bipolar disorders, showed contrasting trends for COVID-19 vaccination. The serotonin theory is that depression is caused by an alternation of the hypothalamic-pituitary-adrenal (HPA) axis, particularly serotonin (5-hydroxytryptamine or 5-HT) [ 22 , 23 , 24 ]. Along with this theory, the selective serotonin reuptake inhibitor is currently the main drug to treat depression [ 22 ]. Serotonin, known as a neurotransmitter, is important to immune systems as the regulator of immune responses and inflammatory processes by central and peripheral mechanisms [ 22 , 24 ]. For reports of COVID-19 vaccines, the association between adrenal crisis and COVID-19 vaccination has been suggested with the possible risk of heterologous vaccination [ 25 , 26 ] Therefore, COVID-19 may alternate the HPA axis, which can potentially increase the risk of depression from our study. In our study, HR for bipolar disorder was found to be 0.672 (95% CI, 0.470–0.962) in association with COVID-19 vaccination. However, this result was primarily caused by only cDNA vaccination with a notable lower HR of 0.339 (95% CI, 0.196–0.587). Interestingly, other types of COVID-19 vaccinations did not demonstrate a significant impact on the occurrences of bipolar disorder. These distinctive findings suggested that the differential effects along with vaccine types may be underestimated in mental illness, particularly bipolar disorder [ 12 , 27 ].
The immune response mediated by COVID-19 vaccination manifests in a variety of ways across different sites in our body [ 28 ]. Trougakos et al. described that the AEs following COVID-19 vaccination may related to the proinflammatory action of the lipid nanoparticles or the delivered mRNA and proinflammatory effects of the produced antigens-spike protein and/or its peptides fragments [ 29 ]. The COVID-19 vaccination activated proinflammatory cytokines such as interleukin (IL)-1, IL-6, and tumor necrosis factor-α mediated by CD4 + T cells [ 28 ]. Many immune-related factors have been suggested for the expression of psychosis [ 13 ]. The hyperinflammatory status can increase dopamine with N-inhibition of methyl-d-aspartate receptor (NMDAR), which leads to psychosis [ 30 ]. Furthermore, an autoimmune response caused by the spike protein and encoded viral protein in the vaccine can be a potential factor in the manifestation of schizophrenia [ 31 , 32 ]. Of many vaccination methods, Lee et al. described that the heterologous vaccination enhanced B cells and CD4 + T cell responses [ 33 ]. Proinflammatory effects can be exacerbated by preexisting inflammatory conditions after administration of mRNA lipid nanoparticles [ 29 ]. This heightened immune response may influence the occurrence of schizophrenia, as presented in our study. However, the profound pathophysiological mechanisms should be performed in future translational research [ 27 ].
Anxiety and stress-related disorders are the main concerns for COVID-19 infection and vaccination, which were widely studied from fear to vaccine hesitancy [ 34 ]. Conversion disorders, characterized by paralysis, sensory disturbances, and seizures are associated with alternation of brain function networks [ 35 ]. Our study showed increased risks of anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders, which were heightened by heterologous vaccination. Most patients who were infected with COVID-19 experienced chronic fatigue with mild cognitive impairment (i.e., brain fog) [ 21 , 35 , 36 ]. Abel et al. described that COVID-19 infection increased the risks of fatigue and sleep disorders from the UK primary care data [ 21 ]. The mechanism is thought to be caused by a decrease in cerebral blood flow, and it is similar to neuropsychiatric disorders affected by inflammatory processes and immune responses [ 37 ]. Since COVID-19 vaccination is also associated with immune responses, both clinicians and vaccinated subjects should be cautious of these manifestations, especially anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders that can also be affected by COVID-19 vaccination in our study. Therefore, the COVID-19 vaccination increases the manifestation of neurosis-related disorders but decreases that of psychosis-related disorders.
With the increasing evidence of extrapulmonary manifestations including neurological and psychiatric symptoms, COVID-19 infection as well as vaccination may affect the central and peripheral nervous system with profound cellular and molecular mechanisms [ 6 , 38 , 39 ]. The spike protein, especially brain-infiltrating SARS-CoV-2 spike protein has been suggested as an important target for the development of neurological and psychiatric disorders. Several mechanisms involved in spike protein have been proposed at the mice level such as TLR2-mediated depression, TLR4-mediated cognitive dysfunction, and anxiety mediated by non-cell autonomous hippocampal neuronal cell deaths by inducing IL-1β from glial cells [ 40 ]. Importantly, a recent study suggested that mRNA vaccines have slippery sequences inducing +1 ribosomal frameshifting products after vaccinations as a consequence of N 1 -methylpseudouridine-induced ribosome stalling [ 41 ]. Although the pathogenesis remains unclear, our study suggests that neuroinflammation caused by spike proteins may contribute to occurrences of some psychiatric AEs such as depression and anxiety, dissociative, stress-related, and somatoform disorders. Therefore, future translational research may provide the pathophysiological differences between psychosis and neurosis from the COVID-19 vaccination.
To supplement our hypothesis regarding the mechanism of action after COVID-19 vaccination, we tried further study using the gene sets enrichment analysis (Supplementary Table 5 ). We found that schizophrenia-related genes share the enrichment pathway for bile acid metabolism. Bile acids prevent the binding of spike protein with angiotensin-converting enzyme II (ACE2) and modulate the expression of ACE2, suggesting the protective role [ 42 ]. Our study also showed that COVID-19 vaccination reduced risks of schizophrenia. For depression, as an increased risk after COVID-19 vaccination, the results were shown for the deep interaction of spike protein-related factors such as NLRP3 inflammasome [ 40 ]. This supports that the presence of the spike protein plays a crucial role in the manifestation of diseases after COVID-19 vaccination. Regarding the neurosis, the Rap1 signaling was observed as an enrichment pathway in the genes of neuroticisms. It regulates MAPK pathways that are important for SARS-CoV-2 virus replication [ 43 , 44 ]. However, these findings will have to be validated by future experimental studies.
This study has several limitations. First, we collected the claims data based on ICD-19 codes, which led to potential errors regarding mismatching or misclassification could have occurred. Second, previous studies have suggested the impact of poverty rates on mental disorders but there are differences in the baseline characteristics between the two groups in this study [ 45 , 46 ]. Although propensity score matching could be a statistical option to overcome this limitation, the real-world data is scarce on the psychiatric AEs following the COVID-19 vaccination so future studies through the process of propensity score matching should be addressed for COVID-19 vaccine-related psychiatric AEs. Meanwhile, both schizophrenia and bipolar disorders often manifest at a young age (under 20 years old) [ 47 ]. However, our study protocol didn’t include the adolescent population group because our study protocol has been approved by our IRB to analyze adults more than 20 years old. Furthermore, the COVID-19 vaccination for adolescents in South Korea has been authorized since October 2021, which made it impossible to collect COVID-19 vaccine-related AEs of the population under 20 years old in our study protocol. Thus, future studies for adolescents considering the manifestation of psychiatric disorders will be needed on COVID-19 vaccine-related AEs. Third, we measured psychiatric AEs up to three months following COVID-19 vaccination. This study did not contain the long-term follow-up COVID-19 vaccine-associated AEs. Last, despite being a population-based study targeting the population in Seoul, South Korea, it cannot be generalized to the entire population, globally since psychiatric disorders could be related to ethnic and genetic backgrounds. Therefore, a global-scale real-world study for adverse events of COVID-19 vaccination will be important in the future.
In conclusion, this population-based cohort study revealed that COVID-19 vaccination differentially affects occurrences of psychiatric disorders. It increased the risks of depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders while reducing the incidence and risk of schizophrenia and bipolar disorder. Our findings suggested that the relationship between COVID-19 vaccination and mental illness may be underestimated along with the complexity of its impact on mental health. Thus, close observation and special caution are necessary for administering additional COVID-19 vaccinations to populations vulnerable to psychiatric AEs.
Data availability
The datasets analyzed during the current study are available through an application to the National Health Insurance Service, South Korea. This protects the confidentiality of the data and ensures that Information Governance is robust.
Lundberg-Morris L, Leach S, Xu Y, Martikainen J, Santosa A, Gisslén M, et al. Covid-19 vaccine effectiveness against post-covid-19 condition among 589 722 individuals in Sweden: population based cohort study. Bmj. 2023;383:e076990.
Article PubMed PubMed Central Google Scholar
Lee DS, Kim JW, Lee KL, Jung YJ, Kang HW. Adverse events following COVID-19 vaccination in South Korea between February 28 and August 21, 2021: a nationwide observational study. Int J Infect Dis. 2022;118:173–82.
Article CAS PubMed PubMed Central Google Scholar
Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–24.
Jefsen OH, Kolbaek P, Gil Y, Speed M, Dinesen PT, Sonderskov KM, et al. COVID-19 vaccine willingness amongst patients with mental illness compared with the general population. Acta Neuropsychiatr. 2021;33:273–6.
Article PubMed Google Scholar
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–15.
Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26:1017–32.
Article CAS PubMed Google Scholar
Barouch DH. Covid-19 vaccines - immunity, variants, boosters. N Engl J Med. 2022;387:1011–20.
Wang W, Wang CY, Wang SI, Wei JC. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: a retrospective cohort study from the TriNetX US collaborative networks. EClinicalMedicine. 2022;53:101619.
Patone M, Handunnetthi L, Saatci D, Pan J, Katikireddi SV, Razvi S, et al. Neurological complications after first dose of COVID-19 vaccines and SARS-CoV-2 infection. Nat Med. 2021;27:2144–53.
Buchan SA, Seo CY, Johnson C, Alley S, Kwong JC, Nasreen S, et al. Epidemiology of Myocarditis and Pericarditis Following mRNA vaccination by vaccine product, schedule, and interdose interval among adolescents and adults in Ontario, Canada. JAMA Netw Open. 2022;5:e2218505.
Sun HL, Zhao YJ, Sha S, Li XH, Si TL, Liu YF, et al. Depression and anxiety among caregivers of psychiatric patients during the late stage of the COVID-19 pandemic: a perspective from network analysis. J Affect Disord. 2024;344:33–40.
Kita A, Fuyuno Y, Matsuura H, Yamaguchi Y, Okuhira K, Kimoto S. Psychiatric adverse reaction to COVID-19 vaccine booster presenting as first-episode acute mania with psychotic features: A case report. Psychiatry Res Case Rep. 2023;2:100143.
Google Scholar
Grover S, Rani S, Kohat K, Kathiravan S, Patel G, Sahoo S, et al. First episode psychosis following r eceipt of first dose of COVID-19 vaccine: a case report. Schizophr Res. 2022;241:70–1.
Harrison PJ, Taquet M. Neuropsychiatric disorders following SARS-CoV-2 infection. Brain. 2023;146:2241–7.
Balasubramanian I, Faheem A, Padhy SK, Menon V. Psychiatric adverse reactions to COVID-19 vaccines: a rapid review of published case reports. Asian J Psychiatr. 2022;71:103129.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bmj. 2007;335:806–8.
Article Google Scholar
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57:1288–94.
Chaudhuri K, Howley P. The impact of COVID-19 vaccination for mental well-being. Eur Econ Rev. 2022;150:104293.
Penninx B, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. 2022;28:2027–37.
Nishimi K, Neylan TC, Bertenthal D, Seal KH, O’Donovan A. Association of psychiatric disorders with incidence of SARS-CoV-2 breakthrough infection among vaccinated adults. JAMA Netw Open. 2022;5:e227287.
Abel KM, Carr MJ, Ashcroft DM, Chalder T, Chew-Graham CA, Hope H, et al. Association of SARS-CoV-2 Infection With Psychological distress, psychotropic prescribing, fatigue, and sleep problems among UK primary care patients. JAMA Netw Open. 2021;4:e2134803.
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, et al. Major depressive disorder. Nat Rev Dis Primers. 2016;2:16065.
Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Primers. 2018;4:18008.
Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry. 2023;28:3243–56.
Maguire D, McLaren DS, Rasool I, Shah PM, Lynch J, Murray RD. ChAdOx1 SARS-CoV-2 vaccination: a putative precipitant of adrenal crises. Clin Endocrinol. 2023;99:470–3.
Article CAS Google Scholar
Markovic N, Faizan A, Boradia C, Nambi S. Adrenal crisis secondary to COVID-19 vaccination in a patient with hypopituitarism. AACE Clin Case Rep. 2022;8:171–3.
Cozzolino A, Hasenmajer V, Newell-Price J, Isidori AM. COVID-19 pandemic and adrenals: deep insights and implications in patients with glucocorticoid disorders. Endocrine. 2023;82:1–14.
Li C, Lee A, Grigoryan L, Arunachalam PS, Scott MKD, Trisal M, et al. Mechanisms of innate and adaptive immunity to the Pfizer-BioNTech BNT162b2 vaccine. Nat Immunol. 2022;23:543–55.
Trougakos IP, Terpos E, Alexopoulos H, Politou M, Paraskevis D, Scorilas A, et al. Adverse effects of COVID-19 mRNA vaccines: the spike hypothesis. Trends Mol Med. 2022;28:542–54.
Tang SW, Helmeste D, Leonard B. Inflammatory neuropsychiatric disorders and COVID-19 neuroinflammation. Acta Neuropsychiatrica. 2021;33:165–77.
Yonker LM, Swank Z, Bartsch YC, Burns MD, Kane A, Boribong BP, et al. Circulating spike protein detected in Post-COVID-19 mRNA vaccine myocarditis. Circulation. 2023;147:867–76.
Yesilkaya UH, Sen M, Tasdemir BG. A novel adverse effect of the BNT162b2 mRNA vaccine: first episode of acute mania with psychotic features. Brain Behav Immun Health. 2021;18:100363.
Lee HK, Go J, Sung H, Kim SW, Walter M, Knabl L, et al. Heterologous ChAdOx1-BNT162b2 vaccination in Korean cohort induces robust immune and antibody responses that includes Omicron. iScience. 2022;25:104473.
McNeil A, Purdon C. Anxiety disorders, COVID-19 fear, and vaccine hesitancy. J Anxiety Disord. 2022;90:102598.
Espay AJ, Aybek S, Carson A, Edwards MJ, Goldstein LH, Hallett M, et al. Current concepts in diagnosis and treatment of functional neurological disorders. JAMA Neurol. 2018;75:1132–41.
Morin CM, Drake CL, Harvey AG, Krystal AD, Manber R, Riemann D, et al. Insomnia disorder. Nat Rev Dis Primers. 2015;1:15026.
Theoharides TC, Stewart JM, Hatziagelaki E, Kolaitis G. Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front Neurosci. 2015;9:225.
Khayat-Khoei M, Bhattacharyya S, Katz J, Harrison D, Tauhid S, Bruso P, et al. COVID-19 mRNA vaccination leading to CNS inflammation: a case series. J Neurol. 2022;269:1093–106.
Theoharides TC. Could SARS-CoV-2 spike protein be responsible for long-COVID syndrome? Mol Neurobiol. 2022;59:1850–61.
Fontes-Dantas FL, Fernandes GG, Gutman EG, De Lima EV, Antonio LS, Hammerle MB, et al. SARS-CoV-2 Spike protein induces TLR4-mediated long-term cognitive dysfunction recapitulating post-COVID-19 syndrome in mice. Cell Rep. 2023;42:112189.
Mulroney TE, Pöyry T, Yam-Puc JC, Rust M, Harvey RF, Kalmar L, et al. N 1 -methylpseudouridylation of mRNA causes +1 ribosomal frameshifting. Nature. 2024;625:189–94.
Fiorucci S, Urbani G, Biagioli M, Sepe V, Distrutti E, Zampella A. Bile acids and bile acid activated receptors in the treatment of Covid-19. Biochem Pharmacol. 2023;115983. https://doi.org/10.1016/j.bcp.2023.115983 .
Zhang YL, Wang RC, Cheng K, Ring BZ, Su L. Roles of Rap1 signaling in tumor cell migration and invasion. Cancer Biol Med. 2017;14:90–9.
Hadzega D, Babisova K, Hyblova M, Janostiakova N, Sabaka P, Janega P, et al. Analysis of transcriptomics data from COVID-19 patients: a pilot research. Folia Microbiol. 2024;69:155–64.
Das-Munshi J, Chang CK, Bakolis I, Broadbent M, Dregan A, Hotopf M, et al. All-cause and cause-specific mortality in people with mental disorders and intellectual disabilities, before and during the COVID-19 pandemic: cohort study. Lancet Reg Health Eur. 2021;11:100228.
Bennett JE, Pearson-Stuttard J, Kontis V, Capewell S, Wolfe I, Ezzati M. Contributions of diseases and injuries to widening life expectancy inequalities in England from 2001 to 2016: a population-based analysis of vital registration data. Lancet Public Health. 2018;3:e586–97.
Ortiz-Orendain J, Gardea-Resendez M, Castiello-de Obeso S, Golebiowski R, Coombes B, Gruhlke PM, et al. Antecedents to first episode psychosis and mania: comparing the initial prodromes of schizophrenia and bipolar disorder in a retrospective population cohort. J Affect Disord. 2023;340:25–32.
Download references
Author information
Authors and affiliations.
Department of Orthopedic Surgery, Inje University Sanggye Paik Hospital, College of Medicine, Inje University, Seoul, Republic of Korea
Hong Jin Kim
Informatization Department, Ewha Womans University Seoul Hospital, Seoul, Republic of Korea
Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, School of Medicine, Ewha Womans University, Seoul, Republic of Korea
Myeong Geun Choi & Eun Mi Chun
You can also search for this author in PubMed Google Scholar
Contributions
EMC conceptualized the study. HJK, M-HK, and EMC designed the study. HJK, M-HK, and EMC analyzed and interpreted the data. M-HK acquired the data. HJK and EMC drafted the manuscript. HJK, M-HK, MGC, and EMC critically reviewed the work. MGC verified the data in the study. All authors had full access to all the data and had final responsibility for the decision to submit for publication.
Corresponding author
Correspondence to Eun Mi Chun .
Ethics declarations
Competing interests.
The authors declare no competing interests.
The study protocol was approved by the Institutional Review Board of our institute (IRB No.: EUMC 2022-07-003), which waived the requirement for informed consent because data analyses were performed retrospectively using anonymized data derived from the South Korean NHIS database.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary tables, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Kim, H.J., Kim, MH., Choi, M.G. et al. Psychiatric adverse events following COVID-19 vaccination: a population-based cohort study in Seoul, South Korea. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02627-0
Download citation
Received : 09 January 2024
Revised : 22 May 2024
Accepted : 24 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1038/s41380-024-02627-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Impact case study database
The coffee historian: achieving impact through industry collaboration, education and public engagement.
- Historical Studies
1. Summary of the impact
2. underpinning research, 3. references to the research, 4. details of the impact, 5. sources to corroborate the impact, additional contextual information, grant funding.
- Switzerland
- United States
- grid.434257.3
- Economic and Social Research Council
- 0000-0002-1514-8484
- Open access
- Published: 01 June 2024
The impact of hyperkalemia on ICU admission and mortality: a retrospective study of Chinese emergency department data
- Jian Sun 1 na1 ,
- Qingyuan Liu 2 na1 ,
- Samuel Seery 3 , 4 na1 ,
- Lu Sun 1 na1 ,
- Yuan Yuan 1 ,
- Wenwen Wang 1 ,
- Yan Wang 1 ,
- Ziwei Cui 1 ,
- Yueguo Wang 1 ,
- Yulan Wang 1 ,
- Jiashan Zhu 1 ,
- Mengping Zhang 3 ,
- Yinglei Lai 3 &
- Kui Jin 1
BMC Emergency Medicine volume 24 , Article number: 95 ( 2024 ) Cite this article
116 Accesses
Metrics details
This study assesses the influence of hyperkalemia on both disease severity and the risk of mortality among patients admitted to the emergency room.
This retrospective observational study utilized data from the Chinese Emergency Triage Assessment and Treatment database (CETAT, version 2.0), which was designed to evaluate and optimize management strategies for emergency room (ER) patients. Patients were systematically categorized based on serum potassium levels. Relationships between serum potassium levels, risk of mortality, and the severity of illness were then analyzed using multifactorial logistic regression and through Receiver Operating Characteristic (ROC) analysis. The effectiveness of various treatments at lowering potassium levels was also investigated.
12,799 emergency patients were enrolled, of whom 20.1% ( n = 2,577) were hypokalemic and 2.98% ( n = 381) were hyperkalemic. Among hyperkalemic patients, the leading reasons for visiting the ER were altered consciousness 23.88% ( n = 91), cardiovascular symptoms 22.31% ( n = 85), and gastrointestinal symptoms 20.47% ( n = 78). Comparative analysis with patients exhibiting normal potassium levels revealed hyperkalemia as an independent factor associated with mortality in the ER. Mortality risk appears to positively correlate with increasing potassium levels, reaching peaks when blood potassium levels ranged between 6.5 and 7.0. Hyperkalemia emerged as a strong predictor of death in the ER, with an Area Under the Curve (AUC) of 0.89. The most frequently prescribed treatment for hyperkalemia patients was diuretics (57.32%, n = 188), followed by intravenous sodium bicarbonate (50.91%, n = 167), IV calcium (37.2%, n = 122), insulin combined with high glucose (27.74%, n = 91), and Continuous Renal Replacement Therapy (CRRT) for 19.82% ( n = 65). Among these, CRRT appeared to be the most efficacious at reducing potassium levels. Diuretics appeared relatively ineffective, while high-glucose insulin, sodium bicarbonate, and calcium preparations having no significant effect on the rate of potassium decline.
Hyperkalemia is common in emergency situations, especially among patients with altered consciousness. There is a strong positive correlation between the severity of hyperkalemia and mortality risk. CRRT appears to be the most effective potassium reducting strategy, while the use of diuretics should be approached with caution.
Peer Review reports
Hyperkalemia is a frequently encountered electrolyte imbalance in clinical settings [ 1 ], Which is traditionally defined as a serum potassium level > 5.5 mmol/l [ 2 ]. This condition can give rise to various complications, notably cardiac arrhythmias, wherein elevated potassium disrupt the heart’s electrical impulses, potentially causing in life-threatening arrhythmias like ventricular tachycardia or fibrillation. Patients with hyperkalemia may also manifest symptoms such as muscle weakness, fatigue, and, in severe cases, paralysis. Hence, early diagnosis of hyperkalemia is of critical importance for patients visiting emergency rooms (ERs). However, the incidence of hyperkalemia in ERs varies across studies suggesting an approximate range of 1.7–2.6% [ 3 ]. Patients particularly susceptible to hyperkalemia are those with chronic kidney disease, diabetes, cardiovascular disease, and those on medications such as angiotensin-converting enzyme inhibitors and/or aldosterone antagonists [ 2 ]. Given the prevalence of hyperkalaemia among these at-risk populations, a comprehensive examination of the reasons for ER visits, patient management, and the effect of this becomes imperative.
Failure to promptly address elevated potassium levels can lead to severe consequences, such as cardiac arrest and arrhythmias, significantly increasing the risk of patient mortality [ 4 , 5 ]. Research highlights a correlation between serum potassium levels in hyperkalemic patients and the occurrence of cardiovascular complications, as well as a 28-day mortality risk among hospitalized patients [ 6 ]. Immediate interventions are imperative in cases of severe hyperkalemia (serum potassium > 6.0-6.5mmol/L), as this condition poses a potential life-threatening risk [ 7 ]. The judicious selection and timely administration of effective treatments to reduce potassium levels are critical to managing emergency cases in involving hyperkalemia. However, current treatment modalities for hyperkalemia exhibit significant variability. In a study by Singer et al. [ 8 ] calcium emerged as the most common choice for emergency hyperkalemia patients in Suffolk County, Massachusetts. By contrast, Peacock et al. [ 9 ] found in the ER insulin/glucose therapy was the most commonly employed, either alone or in combination with other treatments, constituting 64% of cases. This finding aligns with a study by Wu et al. [ 10 ] conducted in China. However, despite these insights, the most effective intervention for hyperkalemia treatment in ERs remains unclear.
In order to comprehensively explore hyperkalaemia epidemiology and to understand the influence of this condition in relation to outcomes, this study relies on the robust and extensive data available within the Chinese Emergency Triage, Assessment, and Treatment (CETAT) database. The dataset spans from January 2020 to July 2021 and involves a diverse range of cases treated in emergency resuscitation rooms, details of the data set are published elsewhere [ 11 ]. Leveraging this rich source of information, the study aims to equip emergency physicians with nuanced insights into the varying severity levels of hyperkalemia and the associated risks of mortality across a spectrum of serum potassium concentrations. The methodological approach hinges on this data to offer a foundation for timely and informed decision-making, ultimately contributing to the optimization of treatment strategies for patients with hyperkalemia.
Participants
The data utilized in this study was abstracted from the multicenter emergency triage database of the Chinese Emergency Specialty Medical Association (CETAT), version 2.0. This database integrates information from patients admitted to the emergency rooms of eight tertiary teaching hospitals nationwide (Peking Union Medical College Hospital, The First Affiliated Hospital of University of Science and Technology of China, The Cardio-Cerebrovascular Hospital affiliated with the University of Science and Technology of China, Suqian People’s Hospital, Wuhan University People’s Hospital, Huai’an Second People’s Hospital, Hefei No. 2 People’s Hospital, and Subei People’s Hospital), amounting to over 80,000 records. The University of Science and Technology of China’s (USTC) School of Mathematics supervise CETAT data quality. All data undergo privacy protection processes, with personal identifiers systematically removed. Data were abstracted from January 2020 to July 2021, focusing on patients admitted to the resuscitation room at the First Affiliated Hospital of USTC and The Cardio-Cerebrovascular Hospital affiliated with the University of Science and Technology of China (Data are available upon request from the corresponding author).
This research strictly adhered to medical ethical standards and has obtained approval from the Ethics Committee of the First Affiliated Hospital of USTC (USTC reference no.22KY079). Given the retrospective nature of this study and the absence of any clinical intervention, the hospital ethics committee waived the requirement for patient-informed consent forms.
Eligibility criteria
Age ≥ 18 years old;
The patient, upon admission, must have available laboratory test results for blood potassium, and complete necessary data.
Incomplete data or lost to follow-up.
Patients with hyperkalemia who did not undergo a recheck their blood potassium levels within 24 h;
Individuals who requested restrictive treatment and did not adhere to the prescribed medical treatments by the doctor.
Definition and outcomes
Patients were classified based on their initial biochemical serum potassium ion concentrations upon admission for emergency care measured using ion-selective electrode method. Hyperkalemia is defined according to the international standards [ 12 ], as a serum potassium concentration exceeding 5.5 mmol/L (1 mmol/L = 1 meq/L). Patients with hyperkalaemia were further classified as either: stage I (Mild hyperkalemia,5.5< [K + ] ≤ 6mmol/L), stage II (Moderate hyperkalemia, 6< [K + ] ≤ 6.5mmol/L), stage III (Severe hyperkalemia,6.5< [K + ] ≤ 7mmol/L) or stage IV (Extreme hyperkalemia, [K + ] > 7mmol/L).
Patients were allocated to one of nine categories based on their primary complaints at the time of presentation. These included cardiovascular symptoms, consciousness disorders, gastrointestinal symptoms, respiratory symptoms, urinary system symptoms, endocrine symptoms, trauma, cardiopulmonary arrest, among others. Categorization relied on the predominant complaints observed during patient presentations and was determined by three emergency doctors who were not blinded to the research plan. In cases where a patient had two or more complaints, classification was based on the primary reason for presentation.
The potassium reduction rate (∆k/k1) was defined as the difference (∆k) between the initial blood potassium level (k1) at hospital admission and the lowest blood potassium level (k2) reviewed within 24 h as a percentage of the initial blood potassium level (k1) upon entry. If ∆k/k1 ≥ 25%, it indicates a faster potassium reduction rate, and vice versa.
Data Collection
After obtaining hospital ethical board approval (USTC reference No.22KY079.), we obtained data from the CETAT database, which includes all patients who were admitted to the ER at the first affiliated hospital of USTC from 2020 to 2021. Information containing demographic data, diagnoses, chief complaint at presentation, laboratory results, and various test elements such as reports, triage summaries as well as physiology information, which includes BP, respiration rate, temperature, heart rate, oxygen et al. were collected. Once diagnosed as hyperkalemia the following treatments.
Patients diagnosed with hyperkalemia had their subsequent management measures within 24 h after enrollment collected by four clinical physicians, primarily including the following interventions: administration of calcium gluconate or calcium chloride to stabilize cardiac membranes, insulin and glucose to facilitate potassium entry into cells, sodium bicarbonate for cases of metabolic acidosis, beta-2 agonists to stimulate potassium uptake, and diuretics to enhance potassium excretion.
The primary outcome is mortality in the emergency room following admission. The secondary outcome is progression of patient’s condition to critically ill status, define as the necessity for intensive care unit (ICU) admission, categorized as the high-risk (HR) group. The third study endpoint investigates whether the potassium reduction rate for the mentioned five potassium-lowering measures exceeds 25%.
Statistical analysis
Statistical analysis was performed by personnel not informed of the research plan and independently by two statistical experts who cross-checked the related results. For continuous variables, Wilcoxon’s rank-sum test compares differences between groups. The Chi-squared test or Fisher’s exact test were used to compare inter-group differences for categorical variables. Odds ratios (OR) were used compares in-hospital mortality rates between the hyperkalemia and the normal potassium level groups. The influence of different serum potassium levels in hyperkalemia on patients’ severity and mortality risk is assessed using binary logistic regression with other factors as independent variables. A p-value of < 0.05 was taken as the threshold for statistical significance.
Baseline characteristics and exposures
A total of 12,799 patients were included, among whom 2.98% ( n = 381) presented with hyperkalemia. Notably, data related to potassium-lowering treatments were unavailable for 53 of these patients, eight of whom succumbed upon admission to the ER without a secondary potassium check. Consequently, the final study group comprises hyperkalaemia 320 patients with hyperkalaemia (see Fig. 1 (a) for further details). In 381 patients with hyperkalemia, stage IV hyperkalemia was observed in 0.44% ( n = 56), stage III hyperkalemia in 0.46% ( n = 59), stage II hyperkalemia in 0.66% ( n = 79), and stage I hyperkalemia in 1.46% ( n = 187). The three most common complaints among hyperkalemia patients at presentation were altered consciousness at 23.88% ( n = 91), cardiovascular symptoms at 22.31% ( n = 85), and gastrointestinal symptoms at 20.47% ( n = 78), see Fig. 1 (b) for further details.

Participant selection process( a ), and Percentage Of Patients With Hyperkalemia In The Emergency Room With Related Symtoms ( b )
Patients with hyperkalemia generally present with more severe conditions compared to those without hyperkalemia. In general, individuals with hyperkalemia exhibited lower body temperatures, blood pressures, blood oxygen levels, hemoglobin concentrations, platelet counts, albumin levels and so forth. Conversely, they displayed higher SOFA and NEWs scores, as well as increased age, heart rate, white blood cell count, percentage of neutrophils, creatinine, phosphorus, and anion gap analysis (see Table 1 for details). Multifactorial logistic regression analysis indicated that age, body temperature, sodium ion concentration, hematocrit (red blood cell ratio), hemoglobin concentration, creatinine, PT (prothrombin time), and carbon dioxide binding capacity are independent factors associated with hyperkalemia. See Table 2 for further details.
Severity and mortality of hyperkalemia patients
Of the 381 patients with hyperkalemia, 40.4% ( n = 154) ones were categorized as critically ill (i.e., high risk) and 7.1% ( n = 27) experienced in-hospital mortality. Following adjustment for patient confounding factors using the NEWS Score, an elevated potassium concentration was significantly associated with an increased odds ratio of death in the emergency room. Interestingly, patients with severe hyperkalemia (6.5mmol/L < [K + ] ≤ 7mmol/L) exhibited the highest risk of death in the emergency room (OR = 6.253, 95%CI: 1.982–17.285, p < 0.001) when compared to patients with highly severe stage IV hyperkalemia ([K + ] > 7mmol/L) (OR = 5.868, 95%CI: 2.271–15.164, p < 0.001). A similar trend is evident when assessing the requirement for high risk intensive care. The severity of hyperkalemia demonstrated a positively association with the severity of illness, with serum [K + ] > 7mmol/L exhibiting the highest odds ratio for ICU admission (OR = 7.567, 95%CI: 4.104-13.949, p = 0.001). See Fig. 2 for further details.
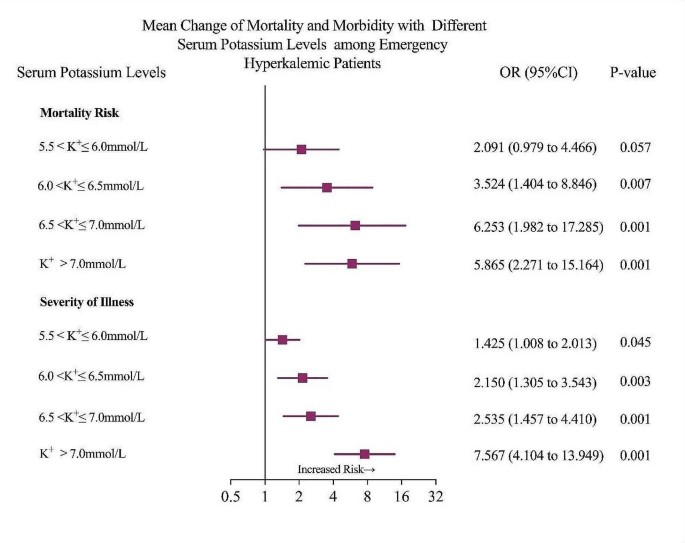
Mortality and morbidity of different serum potassium levels among emergency hyperkalemic patients
Our findings reveal that potassium concentration serves as a predictor for both mortality and illness severity among emergency room patients. The Area Under the Curve (AUC) of the ROC curve for forecasting the risk of mortality due to hyperkalemia in the emergency room is 0.890, while the AUC of the ROC curve for predicting the severity of the patient’s condition is 0.712. Both values suggest a relatively high predictive value (Fig. 3 a and b).

ROC analyses of ( a ) ICU admission and ( b ) in-room fatality risk
Efficacy of Potassium lowering interventions
In this study, we collected data from 328 emergency-admitted hyperkalemia patients who underwent various measures to reduce their potassium levels. Diuretic usage was the most common clinical measure to decrease potassium levels (57.32%, n = 188), followed by bicarbonate (50.91%, n = 167), calcium agents (37.2%, n = 122), insulin with glucose (27.74%, n = 91), and continuous renal replacement therapy (19.82%, n = 65). The relationship of combination therapy between potassium-lowering drugs is detailed in Fig. 4 . After adjusting with the NEWS score (Table 3 ), renal replacement therapy therapy emerged as the most effective method for rapidly reducing potassium levels (OR = 1.90, 95%CI: 1.05–3.45, p = 0.035). Interestingly, the use of high glucose with insulin, bicarbonate, and calcium agents did not significantly impact the speed of potassium reduction. Notably, potassium levels were reduced more slowly with diuretics than without diuretics in this study. (OR = 0.33, 95%CI: 0.20–0.55, p = 0.001).

Venn diagram of therapeutic combinations with potassium-lowering drugs
This study provides a thorough epidemiological analysis of hyperkalemia among patients in emergency rooms and several noteworthy findings emerged. Firstly, elevated potassium is not uncommon, with an incidence rate of 2.98%. In addition, elevated potassium levels significantly increase the risk of mortality, and is a strong indicator of disease severity and death in emergency rooms (AUC 0.89 for mortality and 0.71 for ICU admission). Notably, patients diagnosed with Stage III hyperkalemia (Severe hyperkalemia,6.5< [K + ] ≤ 7mmol/L) in the emergency exhibited the highest risk of mortality more than six-fold compared to patients with normal K + , surpassing even Stage IV hyperkalemia. This finding suggests the possibility of delayed recognition among individuals with moderately elevated potassium concentrations. CRRT emerged as the most effective intervention for high potassium levels. However, despite their frequent use, diuretics appear less effective at reducing blood potassium compared to the other four methods studied here. This study contributes to a deeper understanding of the associated risk of hyperkalemia in clinical settings and offer evidence to support decisions regarding potassium-lowing interventions.
The reported incidence of hyperkalemia varies across different studies. Humphrey et al. reported a global prevalence of hyperkalemia at 6.3% [ 13 ]. A study of U.S emergency departments reported an incidence rate of 3.6% [ 14 , 15 , 16 , 17 ], whereas Canadian emergency department reported a rate of 2.6% [ 18 ]. In a multicenter study conducted by Xu et al., the incidence rate in Chinese emergency departments was reported to be 3.52% [ 19 ]. The rate in this study was higher than that of the Canadian study but slightly lower than that of the United States at 2.98%, suggesting our findings are within a normal range. Additionally, the observed variation in incidence could be attributed to diverse populations included in the different studies. For instance, in the Xu et al. study participants were predominantly hypertensive, with dyslipidemia and having other trauma [ 17 ]. While those in the Canadian study were mainly patients with coronary artery disease and heart failure [ 18 ]. Past studies in China have primarily enrolled patients with heart failure, diabetes, hypertension, and chronic kidney disease. This study primarily included individuals presenting with complaints of disturbances in consciousness and with cardiovascular symptoms. Prior investigations have indicated the presence of cardiovascular symptoms and disordered consciousness can increase the likelihood of developing hyperkalemia by approximately 40% [ 20 ]. Taken together, these findings provide only partial insight into regional variations in the incidence of hyperkalemia. However, this study highlights the importance of promptly assessing serum potassium levels for emergency department patients presenting with disturbances of consciousness and symptoms of cardiovascular disease.
This study revealed that patients at Stage III (6.5 < [K + ] ≤ 7mmol/L) had the highest risk of death in the emergency room, although the probability of being admitted to an intensive care unit was lower compared to those with Stage IV hyperkalemia ([K + ] > 7mmol/L). These findings strongly suggest a need for increase our attention on individuals with extremely high potassium levels, but also that patients with potassium levels within the range of 6.5-7.0 may not receive adequate attention. This is particularly common in the ER, where medical resources are relatively limited. Our team’s earlier work demonstrated that ERs in developing countries, such as China, often encounter an excess of patients who do not actually require emergency services. This situation influences ‘patient encounter time’ and therefore individuals with moderately elevated potassium may not be monitored as they should. Given that hyperkalemia can lead to serious arrhythmias and life-threatening risks [ 21 , 22 ], our study aligns with a retrospective study in 2017 which found a 5-fold increase in the probability of death compared to patients with ‘normal’ potassium levels (3.5-5.0mmol/L) [ 17 ]. This provides further context which must be considered in further detail, and it may be necessary to reconsider the categorization ‘moderate’ and conduct further research into the implications for triaging.
Another notable finding in our study that merits special attention is the frequent use of diuretics to lower potassium levels ( n = 188, 57.32%). However, the speed of potassium reduction with diuretics was slower than in those who did not receive this intervention. These findings are consistent with several other studies [ 15 , 23 ], indicating that although diuretics can effectively enhance the excretion of potassium, their role in the treatment of acute hyperkalemia remains unclear, and should only be considered as an adjunctive treatment. Several factors may contribute to these findings, particularly among ER patients. Firstly, patients with hyperkalemia included in this study often presented with renal insufficiency, limiting the effectiveness of diuretics and also because fluid status is often inadequate in emergency admission patients. The inappropriate use of diuretics may further worsen fluid status, slowing down the reduction of serum potassium. Lastly, high doses of diuretics may cause renal damage [ 24 ], reducing the efficiency of renal reabsorption of both water and sodium, thereby limiting the excretion of potassium. This has significant implications, suggesting that clinicians need to carefully assess the patient’s condition and renal function during the treatment of hyperkalemia. In case of severe hyperkalemia requiring prompt reduction of serum potassium, diuretics may not be the optimal choice. In our study, up to 20% of patients received renal replacement therapy treatment which emerged as the most efficient method for reducing potassium. Numerous studies have shown that compared to other potassium-lowering measures, renal replacement therapy remains the most effective approach to reduce serum potassium [ 15 , 25 ]. Nevertheless, a nationwide study in China revealed that only 61.46% of emergency departments had access to renal replacement therapy [ 26 ]. Suggesting potential limitations in its use due to inadequate manpower, equipment, and relatively high costs.
The observed higher mortality in the group of patients with potassium levels between 6.5 and 7.0 may be partially explained by delayed admission to the intensive care unit and a lower rate of receiving Continuous Renal Replacement Therapy. This raises important questions regarding socio-economic factors, from both the patients’ and practitioners’ perspectives. For instance, several studies have highlighted income and economic stability, education level and social support networks as key factors in health-seeking behaviours [ 27 , 28 ], as are cultural and social norms. This in turn implicates access disparities, health care insurance and geographical healthcare imbalances as reported by Jin et al., the allocation of resources for emergency medical services in China exhibits geographical disparities, with pronounced inequalities between secondary and tertiary hospitals, a disparity that is notably accentuated in rural regions [ 29 ]. There are also other issues, from a practitioners’ perspective, such as the perceived frailty of patients and perhaps the clinicians’ reliance on chronological age and the sensitivity to what might be perceived as ‘alarm symptoms.’ Along with the socio-economic disparities which likely influence health-seeking behaviours these issues require further research to understand delayed admissions and the factors which influence clinical judgments in relation to the decision to administer CRRT. This might include electrolyte imbalance, hemodynamic stability, underlying conditions, and perceived urgency as well as responses to other therapies. This requires further primary qualitative research to explore decision making processes in situ.
Limitations
This study had several limitations which should be addressed before reaching conclusions. Firstly, this was an observational study which pioneers the use of a large database of emergency admission patients for such research in China; however, the sample size of hyperkalemia patients was relatively small. Additionally, the inability to collect extensive data, including comorbidities, renal function, and long-term mortality among others, limited our ability to analyze the etiologies of elevated serum potassium. Also, the data used in this study was from only two regional medical centers of large tertiary hospitals, and the results may not be fully representative of practices across diverse healthcare settings. For instance, emergency renal replacement therapy may not be available in some suburban hospitals. Thirdly, when evaluating the effect of different therapies, despite adjusting for possible biases, our data did not support the analysis of the effects of each individual therapy as well as those therapies that were not available in our study such as intestinal potassium exchange resins. Therefore, caution is necessary when applying this subset of results in clinical practices. Finally, considering the diverse pathophysiological mechanisms underlying hyperkalemia, including factors such as renal failure, drug interactions, and imbalances between intracellular and extracellular potassium, further research is recommended within these specific subgroups and perhaps through a 360-degree analysis of the pathways that balance the kidney and the heart physiologies.
Hyperkalaemia is not uncommon in emergency room patients and is associated with increased mortality and the need for ICU admission. Diuretics should be used with caution and CRRT remained the most effective treatment. However, there are disparities with some high-risk patients not receiving CRRT interventions. Factors which influence health-seeking behaviours are not well-understood in this field nor are the factors which influence clinical judgments in ERs, these are two areas which require further investigation to improve outcomes.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Abbreviations
Chinese Emergency Triage Assessment and Treatment database
Emergency Room
Receiver Operating Characteristic
Area Under the Curve, IV: Intravenoustherapy
University of Science and Technology of China
Intensive Care Unit
Systolic Blood Pressure
Diastolic Blood Pressure
White Blood Cell Count NEUT%:Neutrophil Percentage
Platelet Count
Alanine Aminotransferas
Aspartate Aminotransferase
Total Bilirubin
Carbon Dioxide Combining Power
Prothrombin Time
Sequential Organ Failure Assessment
National Early Warning Score IQR: Interquartile Range
Continuous Renal Replacement Therapy
Confidence Interva
Durfey N, Lehnhof B, Bergeson A, Durfey S, Leytin V, McAteer K, et al. Severe hyperkalemia: can the Electrocardiogram Risk Stratify for short-term adverse. Events? WestJEM. 2017;18:963–71.
Article PubMed Google Scholar
Sarnowski A, Gama RM, Dawson A, Mason H, Banerjee D. Hyperkalemia in chronic kidney disease: links, risks and management. Int J Nephrol Renovasc Dis. 2022;15:215–28.
Article CAS PubMed PubMed Central Google Scholar
Einhorn LM, Zhan M, Hsu VD, Walker LD, Moen MF, Seliger SL, et al. The frequency of Hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169:1156.
Article PubMed PubMed Central Google Scholar
Chen Y, Chang AR, Demarco MA, Inker LA, Grams ME. Serum Potassium, Mortality, and Kidney Outcomes in the Atherosclerosis Risk in Communities Study. Mayo Clinic Proceedings. 2016;91:1403–12.
Hayes J, Kalantar-Zadeh K, Lu JL, Turban S, Anderson JE, Kovesdy CP. Association of Hypo- and hyperkalemia with Disease Progression and Mortality in males with chronic kidney disease: the role of race. Nephron Clin Pract. 2012;120:8–16.
Google Scholar
Bouadma L, Mankikian S, Darmon M, Argaud L, Vinclair C, Siami S, et al. Influence of dyskalemia at admission and early dyskalemia correction on survival and cardiac events of critically ill patients. Crit Care. 2019;23:415.
Kovesdy CP. Updates in hyperkalemia: outcomes and therapeutic strategies. Rev Endocr Metab Disord. 2017;18:41–7.
Singer AJ, Thode HC, Peacock WF. Rapid correction of hyperkalemia is associated with reduced mortality in ED patients. Am J Emerg Med. 2020;38:2361–4.
Peacock WF, Rafique Z, Clark CL, Singer AJ, Turner S, Miller J, et al. Real World Evidence for Treatment of Hyperkalemia in the Emergency Department (REVEAL–ED): a Multicenter, prospective, observational study. J Emerg Med. 2018;55:741–50.
Wu Y, Fu Yangyang T, Hanqi L. Treatment and factors associated with prognosis of hyperkalemia in the emergency department. Chin Crit Care Med. 2023;35:5.
Jin Kui W, Kaipeng L, Qingyuan W, Yueguo W, Yulan C, Huan, et al. The influence of calling emergency medical services (EMS) on severity of disease among patients admitted to emergency room: a propensity-matched study. Chin J Emerg Med. 2021;30:9.
Formiga F, Chivite D, Corbella X, Conde-Martel A, Arévalo-Lorido JC, Trullàs JC, et al. Influence of potassium levels on one-year outcomes in elderly patients with acute heart failure. Eur J Intern Med. 2019;60:24–30.
Article CAS PubMed Google Scholar
Humphrey T, Davids MR, Chothia M-Y, Pecoits-Filho R, Pollock C, James G. How common is hyperkalaemia? A systematic review and meta-analysis of the prevalence and incidence of hyperkalaemia reported in observational studies. Clin Kidney J. 2022;15:727–37.
Betts KA, Woolley JM, Mu F, McDonald E, Tang W, Wu EQ. The prevalence of hyperkalemia in the United States. Curr Med Res Opin. 2018;34:971–8.
Rafique Z, Peacock F, Armstead T, Bischof JJ, Hudson J, Weir MR, et al. Hyperkalemia management in the emergency department: an expert panel consensus. J Am Coll Emerg Physicians Open. 2021;2:e12572.
Aggarwal S, Topaloglu H, Kumar S, Trends. Emergency room visits due to Hyperkalemia in the United States. Value Health. 2015;18:A386.
Article Google Scholar
Singer AJ, Thode HC, Peacock WF. A retrospective study of emergency department potassium disturbances: severity, treatment, and outcomes. Clin Exp Emerg Med. 2017;4:73–9.
Fleet JL, Shariff SZ, Gandhi S, Weir MA, Jain AK, Garg AX. Validity of the International classification of diseases 10th revision code for hyperkalaemia in elderly patients at presentation to an emergency department and at hospital admission. BMJ Open. 2012;2:e002011.
Bian Jiaming H, Haijian Y, Xuezhong Z, Li Z, Houyu. Descriptive epidemiological study of hyperkalemia among patients in the emergency department. Chin J Emerg Med. 2021;30:312–7.
Rosano GMC, Tamargo J, Kjeldsen KP, Lainscak M, Agewall S, Anker SD, et al. Expert consensus document on the management of hyperkalaemia in patients with cardiovascular disease treated with renin angiotensin aldosterone system inhibitors: coordinated by the Working Group on Cardiovascular Pharmacotherapy of the European Society of Cardiology. Eur Heart J - Cardiovasc Pharmacotherapy. 2018;4:180–8.
Kovesdy CP. Management of Hyperkalemia: an update for the internist. Am J Med. 2015;128:1281–7.
Ahee P. The management of hyperkalaemia in the emergency department. J Accid Emerg Med. 2000;17:188–91.
Lindner G, Burdmann EA, Clase CM, Hemmelgarn BR, Herzog CA, Małyszko J, et al. Acute hyperkalemia in the emergency department: a summary from a kidney disease: improving global outcomes conference. Eur J Emerg Med. 2020;27:329–37.
Banerjee D, Rosano G, Herzog CA. Management of heart failure patient with CKD. Clin J Am Soc Nephrol. 2021;16:1131–9.
Montford JR, Linas S. How dangerous is Hyperkalemia? J Am Soc Nephrol. 2017;28:3155–65.
Cui Qinghong S, Feng L, Shuyuan X, Jun Z, Huadong Y, Xuezhong. A survey of regional citrate anticoagulation for emergency continuous renal replacement therapy. Chin Crit Care Med. 2020;32:6.
Ye L, Zhang X. The association mechanism between social network types and health-related behaviours among the elderly in rural Hubei Province, China. Int J Health Plann Manag. 2021;36:826–46.
Zeng Y, Xu W, Chen L, Chen F, Fang Y. The influencing factors of Health-Seeking Preference and Community Health Service utilization among patients in Primary Care Reform in Xiamen, China. Patient Prefer Adherence. 2020;14:653–62.
Jin K, Zhang H, Seery S, Fu Y, Yu S, Zhang L et al. Comparing public and private emergency departments in China: early evidence from a national healthcare quality survey. Int J Health Plann Manage. 2020;35.
Download references
Acknowledgements
We gratefully acknowledge the support and contribution of participating institutions’ clinical and research staff.
Applicable Funding Source University of Science and Technology of China (USTC) [Yinglei].
National Natural Science Foundation of China (National Science Foundation of China) − 12126604 [Mengping] R&D project of Pazhou Lab (Huangpu) under Grant2023K0609 [Mengping] Anhui Major Science and Technology Project under grant number 2020b07050001 [Kui].
Author information
Jian Sun, Qingyuan Liu, Samuel Seery and Lu Sun contributed equally to this work.
Authors and Affiliations
Department of Emergency Medicine, Division of Life Sciences and Medicine, The First Affiliated Hospital of USTC, University of Science and Technology of China, Hefei, Anhui, 230001, China
Jian Sun, Lu Sun, Yuan Yuan, Wenwen Wang, Yan Wang, Ziwei Cui, Yueguo Wang, Yulan Wang, Jiashan Zhu & Kui Jin
School of Mathematics and Physics, Anhui Jianzhu University, Hefei, Anhui, 230009, China
Qingyuan Liu
School of Mathematical Sciences, University of Science and Technology of China, 96 Jinzhai Road, Hefei, Anhui, 230026, China
Samuel Seery, Mengping Zhang & Yinglei Lai
Faculty of Health and Medicine, Division of Health Research, Lancaster University, Lancaster, LA1 4YW, UK
Samuel Seery
You can also search for this author in PubMed Google Scholar
Contributions
KJ, YL, and MZ equally contributed to the conception and design of the research; JS, QL SS, YY WW, LS, YW , ZC, YW, YW, and JZ contributed to the acquisition, analysis, and interpretation of the data; JS, SS, QL, KJ and YL drafted the manuscript; and KJ, SS, MZ and YL critically revised the manuscript, All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Mengping Zhang , Yinglei Lai or Kui Jin .
Ethics declarations
Ethics approval and consent to participate.
This research received approval from the Ethics Committee of the First Affiliated Hospital of USTC, Hefei, China, under the approval number 2022-KY079. It was conducted in strict adherence to the ethical guidelines established by the 1964 Declaration of Helsinki and its subsequent amendments, ensuring compliance with international ethical standards. Given the retrospective nature of this study and the absence of any clinical intervention, the Medical Research Ethics Committee of the First Affiliated Hospital of USTC (Anhui Provincial Hospital) waived the requirement for patient-informed consent forms.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sun, J., Liu, Q., Seery, S. et al. The impact of hyperkalemia on ICU admission and mortality: a retrospective study of Chinese emergency department data. BMC Emerg Med 24 , 95 (2024). https://doi.org/10.1186/s12873-024-01011-z
Download citation
Received : 12 January 2024
Accepted : 22 May 2024
Published : 01 June 2024
DOI : https://doi.org/10.1186/s12873-024-01011-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hyperkalemia
- Emergency room
- Mortality risk
- Disease severity
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]

COMMENTS
The impact case study database allows you to browse and search for impact case studies submitted to the REF 2021. Use the search and filters below to find the impact case studies you are looking for. Impact case study database FAQs. Download all impact case studies (spreadsheet)
The database allows detailed searching and filtering of the impact case studies submitted as part of REF 2021. Detailed guidance on using the database and further information about the data it contains are available on our website. The database will continue to be enhanced in the period ahead, including to incorporate additional metadata fields ...
The REF impact case study database. The impact case study database is a searchable tool that will make the impact case studies widely available and will enable analysis and automated text mining. The licence arrangements relating to the use of this database can be accessed on the National Archive.
Text Searching. The Case Study database is linked to a powerful indexed text search engine, which allows you to search for relevant case studies using a sophisticated search query syntax (see Lucene search help for more details). The basic principle on which the search engine operates is to return a set of results ranked according to how closely they meet your search criteria.
The REF Impact case studies database includes 6,637 documents (at 18 November 2015) submitted by UK Higher Education Institutions (HEIs) to the 2014 Research Excellence Framework (REF2014). The documents have been processed by Digital Science, normalised to a common format to improve searchability and tagged against select fields. ...
A full database of impact case studies from the previous exercise conducted in 2014 are available from Research England. REF Impact Definitions. For REF 2021 "Impact is defined as an effect on, change or benefit to the economy, society, culture, public policy or services, health, the environment or quality of life, beyond academia". ...
Impact Case Studies. AHRQ's evidence-based tools and resources are used by organizations nationwide to improve the quality, safety, effectiveness, and efficiency of health care. The Agency's Impact Case Studies highlight these successes, describing the use and impact of AHRQ-funded tools by State and Federal policy makers, health systems ...
UCD Case Studies - a sample of case studies from researchers at UCD, using the template above. (opens in a new window) UK REF Case Studies - this database from the 2021 Research Excellence Framework contains more than 6,000 impact case studies. You can use the search function or filter by Unit of Assessment to find case studies in areas ...
Of course, it is highly reductionist to focus on these 246 publicly available, identifiable 4* case studies - they represent less than 4% of the whole REF2021 impact case study database - but I know (from my own work with academics and research managers) that this list is a useful entry point to exploring the database more widely. It's ...
The RAE2020 Impact Case Studies database contains 342 documents that describe the wider impact of research that took place in UGC-funded universities. These case studies have been enhanced using various data-mining techniques to provide additional metadata relating to impact topics, impact sectors, research categories, geographic locations and ...
REF impact case studies. A searchable online database and an initial analysis of REF impact case studies are available. Contact REF ...
Case Studies. Case studies can be used to effectively capture and summarise the outcome of interviews. The information can be used for advocacy, marketing and promotion of knowledge and library services (KLS). Examples of our impact. Impact Case Studies database - a collection of good impact case studies submitted by KLSs. Vignettes showcase ...
Case studies have been tagged with information about fields of research, impact types and location of activity to enable indexing and faster searching. Flexible keyword-bsed search is also available, supported by a high level of search functionality. Research publication references in case studies have been individually identified where ...
This study successfully identifies the impact of different urban land types on groundwater resources at a local level, thereby revealing spatial variations among the variables. ... Mazumdar, A. & Basu, S. Changing urban land types and its locational impact on groundwater resources: a case study on Megacity Kolkata. Environ Dev Sustain (2024 ...
Washington, D.C. - Five student teams advanced to the finals this week in the 2024 CSBS Community Bank Case Study Competition, emerging from a second round of eleven teams. This is the tenth year of the competition, which is open to undergraduate students in all fields of study as an opportunity to gain valuable first-hand knowledge of the banking industry.
Potatoes are a highly accepted vegetable among students and have a high-volume potential. This resource examines the results of potato processing trials at a Michigan school district.
With the case study of Helsinki, characterized by a high share of green areas, the paper first examines how construction year and urban density affect the amount and structure of vegetation on residential properties. Second, it estimates the carbon sequestration and summer temperatures in the present-day climate.
Sharestates, an online real estate lending and investing marketplace based in Great Neck, NY, offers investors access to institutional-quality real estate investments through its online marketplace. Since its 2014 founding, the company has funded more than $3 billion in projects nationwide. Sharestates' achievements are rooted in its ...
Soil erodibility (K) is an essential factor for erosion prediction, conservation planning and assessment of sediment-related environmental problems. K estimation methods have been developed in many soil erosion and water quality models, which are developed for soil data-rich areas and pose a challenge for areas with limited data. Unlike others, using the erosion productivity impact calculator ...
However, psychiatric adverse events (AEs) after COVID-19 vaccination, which were documented in case reports and case series, remain unclear. This study is aimed to investigate the psychiatric AEs ...
Impact case study database. The impact case study database allows you to browse and search for impact case studies submitted to the REF 2021. Use the search and filters below to find the impact case studies you are looking for. Impact case study database FAQs. Download all impact case studies (spreadsheet)
64 contextualised case study of the direct and indirect impacts of COVID-19 on women and 65 children, with some assessment of their uneven distribution across socio-economic, age and 66 gender groups. We used different types of primary and secondary data from multiple sources 67 to produce a holistic descriptive analysis.
This study assesses the influence of hyperkalemia on both disease severity and the risk of mortality among patients admitted to the emergency room. This retrospective observational study utilized data from the Chinese Emergency Triage Assessment and Treatment database (CETAT, version 2.0), which was designed to evaluate and optimize management strategies for emergency room (ER) patients.