An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Oral Maxillofac Pathol
- v.24(2); May-Aug 2020

Non-Hodgkins lymphoma – A case report and review of literature
Sasidhar singaraju.
Department of Oral Pathology and Microbiology, Rishiraj College of Dental Sciences and Research Centre, Bhopal, Madhya Pradesh, India
Shubham Patel
Ashish sharma, medhini singaraju.
Lymphomas are solid tumors of the immune system and include 14% of all head and neck malignancies. Non-Hodgkin lymphomas (NHLs) are a heterogeneous group of lymphoproliferative disorders originating in B-, T-, or natural killer T-cells. They have a wide range of histological appearances and clinical features at presentation, which can make diagnosis difficult. A 58-year-old male patient presented with a 1-month history of swelling in the upper right back tooth region, which developed after extraction. On intraoral examination, there was small nodular lesion proliferation from the extracted socket. Biopsy specimen on histological examination revealed sheets of small round cells with hyperchromatic nucleus resembling lymphoblast. Immunohistochemistry (IHC) confirms the NHL of T-cell origin. This article is an attempt to correlate the clinical presentation and histological importance of small round cell tumors of the jaw and to discuss the differential diagnosis of small round cell tumors. Typically, a multimodal approach is employed, and the principal ancillary technique that have been found to be useful in classification is IHC.
INTRODUCTION
Lymphomas are a heterogeneous group of malignancies arising from lymphocytes. Over recent years, improved clinical, pathological and molecular data have helped guide an evolution in the classification of lymphomas that is reflected in the 2016 revision of the World Health Organization (WHO) classification. This recognizes >40 mature B-cell neoplasms and >25 mature T-cell and natural killer (NK)-cell neoplasms.[ 1 ] Non-Hodgkin lymphoma (NHL) includes all lymphomas, except Hodgkin's lymphoma (HL). During the past three decades, there have been consistent reports of an increase in the incidence of NHL worldwide. The incidence rates are about 1.5 times higher in men than in women. The average age at diagnosis is about the sixth decade of life, although certain subtypes of NHL, such as Burkitt lymphoma and lymphoblastic lymphoma, have been diagnosed at a younger age.[ 2 ]
Lymphomas present themselves as enlarged nontender lymph nodes but may involve extranodal regions, commonly involving the gastrointestinal tract and head and neck. Extranodal involvement is much less common in HL than in NHL.[ 3 ]
Recent advances in molecular genetics have significantly deepened our understanding of the biology of these diseases. The introduction of gene expression profiling, especially has led to the discovery of novel oncogenic pathways involved in the process of malignant transformation. Equally important, these analyses have identified novel molecular lymphoma subtypes that are histologically indistinguishable.[ 4 ] There is a significant distinction in the clinical course of germinal center B-cell-like, diffuse large B-cell lymphoma (DLBCL), and activated B-cell-like DLBCL, as they have a huge variation in the survival rates after standard treatment.
CASE REPORT
A 58-year-old male patient reported to the college with a chief complaint of swelling and pain in gums in the right upper back tooth region for the past 1 month. Lesion initially started as a small swelling and gradually increased to the present size. Medical history was positive for epistaxis a month back and blood on coughing for 1 month. The patient also gave a history of extraction 2 months in that region after he noticed a loosening of his teeth, which was uneventful. Family history was noncontributory. Extraoral examination revealed mild swelling in the middle-third of the face on the right side [ Figure 1 ].

Extraoral photograph showing mild extraoral swelling on the right side of the face
Intraorally, single large, noduloproliferative growth was seen on the right maxillary ridge, extending from the right second premolar region to maxillary tuberosity area and also up to mid-palate region not crossing the midline [ Figure 2 ]. It was tender on palpation. There was presence of soft-tissue mass protruding from the extraction socket behind 14. The overlying mucosa was reddish pink. The swelling was sessile with ill-defined borders, reddish pink in color and was firm in consistency. Regional lymph nodes were not palpable.

Intraoral swelling seen on the right maxillary ridge
Based on the history and clinical findings, a provisional diagnosis of nasopharyngeal carcinoma of maxillary antrum with a differential diagnosis carcinoma of maxillary antrum was made.
A series of radiological and routine hematological investigations were performed. Radiological investigation included orthopantomography and paranasal sinus view. The orthopantomograph revealed loss of maxillary antral bone with ragged borders on the right side. The bone loss is evident up till the floor of the right orbit. There was presence of soft-tissue shadow over the alveolar ridge with complete destruction of the alveolar bone on the right side. Coronoid and condylar processes were normal [ Figure 3a ]. Para nasal sinuses view showed destruction of the superior, lateral, and facial wall of the right maxillary antrum, expansion of the malar bone on the right side laterally with involvement of middle and inferior nasal conchae medially. Furthermore, there was destruction of the right infraorbital margin with the haziness of both antra [ Figure 3b ]. Routine hemogram analysis, urine analysis, and X-ray chest were normal. The patient was negative for HIV and hepatitis B virus.

(a) Orthopantomograph, (b) PNS view
Incisional biopsy under local anesthesia was done. Microscopic pictures revealed squamous mucosa with underlying connective tissue composed of diffuse, uniform monotonous proliferation of small, round cells with large darkly staining nucleus, and little eosinophilic cytoplasm resembling lymphocytes in loose fibrocellular stroma and comedo necrosis suggestive of lymphoproliferative disease [ Figure 4 ].

(a-c) Photomicrographs showing squamous mucosa with underlying connective tissue composed of lymphocytes in loose fibrocellular stroma (H&E stain), (a) ×4, (b) ×10, (c) ×10
Immunohistochemistry (IHC) was performed [ Figure 5 ]. Markers used were CD45 and CD20 which revealed CD45 positivity in tumor cell indicating the tumor cell is hematopoietic in origin and was CD20 negative indicating that it is not B-lymphocytic in origin.

(a and b) CD45, (immunohistochemistry stain, ×4, ×40) (c and d) CD20 (immunohistochemistry stain, ×4, ×40)
Based on the above findings, a diagnosis of NHL of T-cell origin was made.
Surgical excision of the lesion was done under general anesthesia, and postoperative radiotherapy and chemotherapy were planned. A follow-up of 2 years revealed no local relapse.
Malignant small round cell tumors is a term used for tumors composed of malignant round cells that are slightly larger or double the size of red blood cells in air-dried smears. This group of neoplasms is characterized by small, round, relatively undifferentiated cells. They generally include Ewing's sarcoma, peripheral neuroectodermal tumor, rhabdomyosarcoma, synovial sarcoma, NHL, retinoblastoma, neuroblastoma, hepatoblastoma, and nephroblastoma. Other differential diagnoses of small round cell tumors include small cell osteogenic sarcoma, undifferentiated hepatoblastoma, granulocytic sarcoma, and intraabdominal desmoplastic small round.[ 5 ] Accurate diagnosis of these cancers is essential because the treatment options, responses to therapy, and prognoses vary widely depending on the diagnosis, and therefore, investigations are needed.
Lymphoma is a general term for a complex group of malignancies of the lymphoreticular system. These malignancies initially arise within the lymphatic tissues and may progress to an extranodular mass (NHL) or to a nontender mass or masses in a lymph node region (HL) that later may spread to other lymph node groups and involve the bone marrow. Lymphoma in the oral soft tissues usually presents as an extranodal, soft to firm asymptomatic lesion, although the mass may also be painful.[ 6 ]
The WHO modification of the Revised European–American Lymphoma Classification recognizes three major categories of lymphoid malignancies, which are B-cell lymphoma, T-cell/NK cell lymphoma, and Hodgkin's lymphoma. NHL is one of the possible cancers in the head-and-neck region, and among extranodal NHLs, this is the second most common site after the gastrointestinal tract. In the head and neck, Waldeyer's ring is the most common site of origin and may be accompanied by cervical node involvement. Nose, paranasal sinus, orbits, and salivary glands are other possible organs affected in decreasing order of frequency, with rare spread to the regional lymph nodes.[ 3 ] NHL has long been recognized as a heterogeneous group of disorders based on clinical presentation, morphological appearance, and response to therapy. In recent years, the use of immunological and molecular biological techniques has led to important advances in our knowledge of lymphocyte differentiation and has provided the basis for a better understanding of the cellular origin and pathogenesis of NHL.[ 6 ] Various types of NHL represents neoplastic cells arrested at various stages in the normal differentiation scheme or the gain of a proliferative or anti-apoptotic abnormality, whose precise phenotype depends on the developmental stage, at which the lymphocyte is affected.
T-cell NHLs are uncommon malignancies that represent approximately 12% of all lymphomas.[ 7 ] There are no characteristic clinical features of lymphomas of the oral region, and they depend on the site of the swelling, the lymph node involvement, and/or the presence of metastasis. The most common beginning symptoms are local mass, pain or discomfort, dysphagia or sensation of a foreign body in the throat, in the case of tonsillar NHL.[ 3 ] T-cell NHL commonly presents with extranodal disease and often contains varying amounts of necrosis/apoptosis on biopsy specimens, making differentiation between a reactive process and lymphoma challenging. Immunophenotypic, cytogenetic, and molecular analyses have enhanced diagnostic capabilities and improved classification and prognostication for T-cell NHL. There are 28 different established and provisional mature T-cell/NK cell entities in the 2016 WHO classification of lymphoid neoplasms, broadly subdivided into two groups: peripheral T-cell lymphoma and cutaneous T-cell lymphoma.[ 8 ]
IHC is an integral part of the diagnostic chematopathology. IHC with various antibodies identifies the specific lineage and developmental stage of the lymphoma. Panel of markers is decided based on morphologic differential diagnosis (no single marker is specific), which includes leukocyte common antigen (LCA), B-cell markers (CD20 and CD79a), T-cell markers (CD3 and CD5), and other markers such as CD23, bcl-2, CD10, cyclinD1, CD15, CD30, ALK-1, and CD138 (based on cytoarchitectural pattern).[ 9 ]
Basic immunohistochemistry panel for non-Hodgkin lymphoma
- Expression of CD45 (LCA) rules out an epithelial tumor and suggests the tumor is of hematopoietic origin.
NHL is further subclassified based on the stage of maturation (immature vs. mature) and the cell of origin (B-cell, T-cell, or NK cell).
- CD20 is the most widely used pan-B-cell marker
- CD3 is the most commonly used pan-T-cell antigen
- CD4 is for helper T-cells, CD8 for suppressor cells, and CD57 for NK cells.
In our case, apart from epistaxis and blood after coughing, the patient did not show any other specific signs. Extraoral examination revealed mild facial asymmetry. Primary lymphomas are more common in females. However, in our case, it was an old-aged male. The occurrence of NHL is common in developed countries than developing nations. Among the developing nations, few of the Middle Eastern nations show moderate-to-high intensity. In a study, it was uncovered that the average age-adjusted rate of incidence and percentage of annual change in adjusted rates of age for NHL by sex in five cities of India showed a statistically significant increase in number over a period of two decades.[ 10 ]
The management of NHL affecting head and neck relies on the Ann Arbor staging. An indolent assortment might be treated with radiation therapy alone, whereas a disseminated variety requires a combination of radiotherapy and chemotherapy. Isolated lesions are managed by surgical enucleation. However surgery is combined with radiotherapy and chemotherapy for better results. The prognosis of the disease depends on the stage of the disease, which has reported 5-year survival rate for 50% of cases in the maxilla and mandible.[ 10 ]
Small round cell tumors are difficult to distinguish by light microscopy, and currently, no single test is available, which can precisely distinguish these tumors. Hence to confirm the diagnosis, pathologists should go for several other techniques like IHC. IHC for individual protein markers is used to establish the diagnosis in many instances, and its accuracy rate is also quite satisfactory. Thus, IHC can be helpful in narrowing the differential diagnosis of small round cell tumors, so as the treatment outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
- Sign In to save searches and organize your favorite content.
- Not registered? Sign up
Recently viewed (0)
- Save Search
- Subscriptions
- Join E-mail List
Patient Case Studies and Panel Discussion: Lymphoma
- Get Citation Alerts
- Download PDF to Print
A heterogeneous group of diseases, lymphomas encompass a range of diagnoses that call for varied treatment approaches. Although some lymphomas require minimal intervention for cure or remission, others can be very difficult to treat and are associated with poor outcomes. At the NCCN 2019 Annual Congress: Hematologic Malignancies, a panel of experts used 3 case studies to develop an evidence-based approach for the treatment of patients with lymphomas. Moderated by Ranjana H. Advani, MD, the session focused on peripheral T-cell lymphoma, primary mediastinal large B-cell lymphoma, follicular lymphoma, and diffuse large B-cell lymphoma.
Lymphomas are a heterogeneous group of diseases with a range of diagnoses that require varied treatment approaches. Although some lymphomas require minimal intervention for cure or remission, others can be difficult to treat and are associated with poor patient outcomes. At the NCCN 2019 Annual Congress: Hematologic Malignancies, a panel of experts identified clinical challenges in managing patients with lymphoma. Moderated by Ranjana H. Advani, MD, Saul A. Rosenberg Professor of Lymphoma, Stanford Cancer Institute, the session focused on 3 case studies, which were used to develop an evidence-based approach for treatment of these patients. Panelists included Jeremy S. Abramson, MD, MMSc, Massachusetts General Hospital Cancer Center; Mrinal Dutia, MD, The Permanente Medical Group; Richard I. Fisher, MD, Fox Chase Cancer Center; and Andrew D. Zelenetz, MD, PhD, Memorial Sloan Kettering Cancer Center.
- Patient Case Study 1: Peripheral T-Cell Lymphoma
In the first case study, a 44-year-old woman presented with a dry, nonproductive cough that she had been experiencing for 2 to 3 months, intermittent bouts of severe shortness of breath, decreased appetite, and a 20-pound weight loss. Chest radiograph revealed mild bilateral pleural effusion and bilateral pulmonary nodules, with the largest nodule measuring 5 cm in the right upper lobe. The patient was admitted for further evaluation, and additional testing was performed (see Figure 1 for results). Bone marrow evaluation revealed no morphologic abnormalities, but complex cytogenetics and the same T-cell clone was found as in the lung biopsy. Therefore, a diagnosis was made of stage IVB peripheral T-cell lymphoma (PTCL) with T-follicular helper (TFH) phenotype most consistent with angioimmunoblastic T-cell lymphoma (AITL).

Patient case study 1: results of further testing.
Abbreviations: NGS, next-generation sequencing; RUL, right upper lobe; SUV, standard uptake value; VATS, video-assisted thoracic surgery.
Citation: Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw 17, 11.5; 10.6004/jnccn.2019.5028
Dr. Advani explained that this “complicated terminology” comes from recent updates to the WHO classification for PTCL. 1 , 2 Furthermore, she explained that in recent years, advances in molecular biology have helped elucidate the underlying genetic complexity of PTCL and identify mutations and signaling pathways involved in lymphomagenesis. Importantly, many of the same genetic changes observed in AITL are also seen in PTCL not otherwise specified (NOS) that manifest a TFH phenotype. For this designation, the neoplastic cells should express at least 2 or 3 TFH-related antigens, including PD-1, CD10, BCL6, CXCL13, ICOS, SAP, and CCR5.
One potential treatment regimen to use in this patient population is CHOP (cyclophosphamide/doxorubicin/vincristine/prednisone), which is associated with complete response (CR) rates of 50% to 60% in non–anaplastic large cell lymphoma (ALCL) and a 5-year overall survival rate of 40% to 60%. According to Dr. Advani, patients with low International Prognostic Index (IPI) scores perform significantly better; however, relapse is associated with poor patient outcomes. “The ongoing challenge is to achieve higher CR rates and to translate those remissions into long-term survival,” said Dr. Advani.
Another treatment option is the CHOEP regimen, which adds etoposide to CHOP. Retrospective studies suggest that outcomes may be better than historical data with CHOP. 3 – 5 In a prospective trial, the Nordic group evaluated the role of autologous stem cell transplantation after patients achieved a CR/partial response with CHOEP. 6 At a median follow-up of 5 years, the 5-year progression-free survival (PFS) and overall survival (OS) rates for AITL were 49% and 52%, respectively, and 38% and 47% for PTCL-NOS, respectively.
Finally, the phase III ECHELON-2 study was the first prospective trial in PTCL to show an OS benefit over CHOP. 7 Frontline therapy for CD30-positive PTCL comparing brentuximab vedotin + cyclophosphamide/doxorubicin/prednisone (BV-CHP) versus CHOP led to a significant improvement in PFS and OS for patients, with a comparable safety profile. The FDA subsequently approved brentuximab vedotin in combination with CHP for adults with previously untreated systematic ALCL or other CD30-expressing PTCL, including AITL and PTCL-NOS. “Based on these data, currently BV-CHP should be the standard regimen for untreated ALCL and other histologies that are CD30-postive,” said Dr. Advani.
In the current case study, the patient received treatment with CHOEP and growth factor support. However, after 2 cycles, PET/CT scan showed no change in lung lesions with a worsening of right-sided pleural effusion (Deauville score 5). Thoracentesis of the pleural effusion was negative for infection but positive for abnormal T-cell population, with morphologic and immunophenotypic findings consistent with the initial diagnosis of PTCL with TFH phenotype most consistent with AITL. The patient was then started on single-agent brentuximab vedotin every 3 weeks. After 4 cycles, PET/CT scan revealed marked improvement in all lesions (Deauville score 4) and was continued on brentuximab vedotin for an additional 4 doses. PET/CT after 8 cycles revealed the resolution of lung nodules and adenopathy in the right axilla with increased metabolic activity (Deauville score 4).
Currently, 4 agents are FDA-approved for use in relapsed/refractory PTCL: pralatrexate, romidepsin, belinostat, and brentuximab vedotin. Aside from brentuximab vedotin use in ALCL, however, overall response rates are low. Brentuximab vedotin has been evaluated in relapsed/refractory AITL, showing an ORR of 54%. 8 Responses did not correlate with level of CD30 expression.
Although no randomized studies have analyzed the role of consolidative hematopoietic stem cell transplantation, data from the prospective COMPLETE study suggested improved outcomes in patients with PTCL AITL and PTCL-NOS. 9 On the other hand, said Dr. Advani, data from the LYSA study do not support the use of autologous stem cell transplant for upfront consolidation in patients with PTCL-NOS, AITL, or ALK-ALCL who have achieved a complete or partial response after induction. 10
“If patients are young and have achieved remission or even a partial response, most of us tend to transplant because outcomes with relapsed disease are very poor,” Dr. Advani concluded. “None of the approved drugs are home runs. The best chance you get is your first chance.”
- Patient Case Study 2: Primary Mediastinal Large B-Cell Lymphoma
In the second case study, a 21-year-old woman presented with severe cough and weight loss. Physical examination showed dilated veins on the anterior chest wall and no palpable peripheral lymphadenopathy. Chest radiograph revealed right-sided pleural effusion and a large mediastinal mass measuring 10.8 cm. Additional testing was performed. PET/CT scan showed a bulky anterior mediastinal mass with SUV max of 24.1 and subcarinal and right hilar adenopathy. However, no evidence of disease was observed below the diaphragm. Bone marrow biopsy was negative. Mediastinoscopy with a biopsy of the mass showed diffuse lymphoid proliferation of intermediate-size atypical cells positive for CD20, CD79A, PAX5, CD30 (dim), MUM1, BCL2, and BCL6, and negative for CD10, BCL1, and EBER. Florescence in situ hybridization was negative for MYC , BCL2 , and BCL6 rearrangements. The final diagnosis of primary mediastinal large B-cell lymphoma (PMBL) was made.
According to Dr. Advani, current treatment choices for PMBL are CHOP + rituximab (R-CHOP) with radiotherapy versus more intensive regimens, such as dose-adjusted etoposide/prednisone/vincristine/cyclophosphamide/doxorubicin + rituximab (DA-EPOCH-R), without radiotherapy. In one study of DA-EPOCH-R with median follow-up of 8.4 years, PFS and OS were both 90%. 11 Another retrospective multicenter analysis that stratified patients by frontline regimen of either DA-EPOCH-R or R-CHOP showed a higher complete response with DA-EPOCH-R (84% vs 70%; P =.046), but the patients in this arm were also more likely to experience treatment-related toxicities. 12 At 2 years, 89% of patients in the R-CHOP arm and 91% of those in DA-EPOCH-R arm were still alive. Despite these similar outcomes, the consensus among panelists was that DA-EPOCH-R was the preferred option.
The patient in the current case report was started on DA-EPOCH-R, with an initial favorable response: interim imaging showed a reduction in size of the anterior mediastinal mass (5 x 6.3 x 9.6 cm) and resolution of left upper pulmonary nodules. The patient continued on DA-EPOCH-R for 4 additional cycles. PET/CT scans 4 weeks posttreatment revealed a metabolically inactive, irregularly shaped anterior mediastinal mass (5.5 x 4 x 5.2 cm) and a focal area of low metabolic activity within the mass (SUV max 3.5; Deauville score 4). She was asymptomatic, and the decision was made to follow with observation. After 2 months, PET/CT scans showed a stable mediastinal mass with increased metabolic activity (SUV max 6). Biopsy of the mediastinal mass was performed and immunohistochemistry results were consistent with relapsed PMBL; immunohistochemistry showed 30% of large cells were CD20- and CD30-positive.
“With PMBL, most of the cures are from initial therapy,” said Dr. Advani. “Salvage rates in recurrent/refractory disease are quite poor.” Overall response rates in PMBL are 25% versus 48% for diffuse large B-cell lymphoma (DLBCL), and 2-year overall survival is only 15% versus 24%, respectively. 13
Although CD19 CAR T-cell therapy has been approved, said Dr. Advani, there are very limited data on its use in relapsed/refractory PMBL. According to Jeremy S. Abramson, MD, MMSc, Associate Professor of Medicine, Harvard Medical School, and Director of the Lymphoma Center, Massachusetts General Hospital Cancer Center, the limited available data are indeed encouraging in relapsed/refractory PMBL, and are “looking similar” to those for third-line treatment in DLBCL. Currently 3 randomized clinical trials are evaluating CAR T-cells versus autologous stem cell transplant (the current standard of care) as second-line therapy for relapsed/refractory DLBCL, PMBL, and high-grade B-cell lymphomas, and these trials may ultimately change the standard of care in these patients.
Another treatment option for use in patients with relapsed/refractory PMBL is immune checkpoint inhibitors. Pembrolizumab has shown response rates of 40% to 50% and is now approved by the FDA for use in the third-line and beyond. 14 Furthermore, combination brentuximab vedotin + nivolumab showed even more robust activity, with an overall response rate of 73%. 15
The patient in this case study received 5 cycles of pembrolizumab, and PET/CT scans showed a complete metabolic response.
- Patient Case Study 3: From Follicular Lymphoma to DLBCL
In the last case study, a 48-year-old man presented with enlarged lymph nodes in his left neck and right groin measuring up to 2 cm. He was asymptomatic and had no evidence of B symptoms. Laboratory test results were all normal. Excisional biopsy of the left cervical node showed follicular lymphoma (grade 1–2). PET/CT scan revealed left cervical, axillary, and right external iliac and inguinal adenopathy, with the largest node measuring 1.0 x 2.0 cm (SUV max 5.5). There was no splenomegaly or effusions. Bone marrow biopsy showed normal trilineage hematopoiesis. The diagnosis of stage IIIA follicular lymphoma (grade 1–2) was made, with a Follicular Lymphoma International Prognostic Index (FLIPI) score of 1. Panelists agreed that the best approach for this patient was watchful waiting. Therapy was deferred, and the patient was followed with observation.
Two years later, the patient presented with enlarging lymph nodes in his left neck. He was anxious and had mild fatigue. Results of laboratory tests were normal. PET/CT scan showed increased adenopathy above and below the diaphragm, with the largest node (right external iliac node) measuring 3.4 x 2.8 cm (SUV max 8.4). A biopsy of the right external iliac node was performed, with results showing follicular lymphoma (grade 1–2).
Panelists agreed that observation was an acceptable approach for an asymptomatic patients diagnosed with follicular lymphoma with low-volume disease. However, the patient opted for 4 doses of weekly rituximab. Repeat PET/CT (3 months posttreatment with rituximab) showed that most lymph nodes had resolved. Three years later, the patients presented with a new severe pain in the low back radiating down his right leg. MRI of the L-spine showed a T1 hypointense infiltrative mass replacing the L3 vertebral body. A core biopsy of right psoas mass showed that his follicular lymphoma had transformed to DLBCL, germinal center B-cell–like subtype, with double expressors of MYC >40% and BCL2 >50% and MYC translocation–negative, and expression of Ki67 was 90%. IPI score was 4.
Andrew D. Zelenetz, MD, PhD, Professor of Medicine, Memorial Sloan Kettering Cancer Center, explained the unique biology of the “double-expressor” phenotype in DLBCL. “This is the one circumstance where DA-EPOCH-R may have a distinct benefit,” he said. “However, in the absence of MYC translocation, it is not clear that overexpression of MYC, which is biologically driven without the translocation, shows a benefit from this intensive regimen.”
The patient received 6 cycles of DA-EPOCH-R with 4 doses of intrathecal methotrexate. Results of interim and end-of-therapy PET scans showed a metabolic complete response (Deauville score 2).
Double-hit and double-expressor lymphomas tend to have inferior outcomes with R-CHOP therapy, Dr. Advani stated. Several retrospective studies and one prospective trial suggest improved outcomes with intensive chemotherapy for double-hit lymphomas. 16 – 18 “Patients with a very high IPI, advanced-stage disease, or extranodal involvement are the ones that I consider good candidates for DA-EPOCH-R,” she said, and also noted that double-expressor DLBCLs have a higher risk of central nervous system (CNS) relapse independent of CNS-IPI.
The patient in the current case study had a CNS-IPI of 3 and an 11% cumulative incidence of CNS relapse at 2 years. Data support some form of CNS prophylaxis, 19 Dr. Advani concluded, but the jury is still out regarding optimal treatment for double-expressor non-Hodgkin’s lymphoma.
Swerdlow SH , Campo E , Pileri SA , et al. . The 2016 revision of the World Health Organization classification of lymphoid neoplasms . Blood 2016 ; 127 : 2375 – 2390 .
- Search Google Scholar
- Export Citation
Hildyard C , Shiekh S , Browning J , Collins GP . Toward a biology-driven treatment strategy for peripheral T-cell lymphoma . Clin Med Insights Blood Disord 2017 ; 10 :1179545X17705863.
Cederleuf H , Bjerregard Pedersen M , Jerkeman M . The addition of etoposide to CHOP is associated with improved outcome in ALK+ adult anaplastic large cell lymphoma: a Nordic Lymphoma Group study . Br J Haematol 2017 ; 178 : 739 – 746 .
Schmitz N , Trümper L , Ziepert M , et al. . Treatment and prognosis of mature T-cell and NK-cell lymphoma: an analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin Lymphoma Study Group . Blood 2010 ; 116 : 3418 – 3425 .
Janikova A , Chloupkova R , Campr V , et al. . First-line therapy for T cell lymphomas: a retrospective population-based analysis of 906 T cell lymphoma patients . Ann Hematol 2019 ; 98 : 1961 – 1972 .
d’Amore F , Relander T , Lauritzsen GF , et al. . Up-front autologous stem-cell transplantation in peripheral T-cell lymphoma: NLG-T-01 . J Clin Oncol 2012 ; 30 : 3093 – 3099 .
Horwitz S , O’Connor OA , Pro B , et al. . Brentuximab vedotin with chemotherapy for CD30-positive peripheral T-cell lymphoma (ECHELON-2): a global, double-blind, randomised, phase 3 trial . Lancet 2019 ; 393 : 229 – 240 .
Horwitz SM , Advani RH , Bartlett NL , et al. . Objective responses in relapsed T-cell lymphomas with single-agent brentuximab vedotin . Blood 2014 ; 123 : 3095 – 3100 .
Park SI , Horwitz SM , Foss FM , et al. . The role of autologous stem cell transplantation in patients with nodal peripheral T-cell lymphomas in first complete remission: Report from COMPLETE, a prospective, multicenter cohort study . Cancer 2019 ; 125 : 1507 – 1517 .
Fossard G , Broussais F , Coelho I , et al. . Role of up-front autologous stem-cell transplantation in peripheral T-cell lymphoma for patients in response after induction: an analysis of patients from LYSA centers . Ann Oncol 2018 ; 29 : 715 – 723 .
Melani C , Advani R , Roschewski M , et al. . End-of-treatment and serial PET imaging in primary mediastinal B-cell lymphoma following dose-adjusted EPOCH-R: a paradigm shift in clinical decision making . Haematologica 2018 ; 103 : 1337 – 1344 .
Shah NN , Szabo , Huntington SF , et al. . R-CHOP versus dose-adjusted R-EPOCH in frontline management of primary mediastinal B-cell lymphoma: a multi-centre analysis . Br J Haematol 2018 ; 180 : 534 – 544 .
Kuruvilla J , Pintilie M , Tsang R , et al. . Salvage chemotherapy and autologous stem cell transplantation are inferior for relapsed or refractory primary mediastinal large B-cell lymphoma compared with diffuse large B-cell lymphoma . Leuk Lymphoma 2008 ; 49 : 1329 – 1336 .
Zinzani PL , Ribrag V , Moskowitz CH , et al. . Safety and tolerability of pembrolizumab in patients with relapsed/refractory primary mediastinal large B-cell lymphoma . Blood 2017 ; 130 : 267 – 270 .
Zinzani PL , Santoro A , Gritt G , et al. . Nivolumab combined with brentuximab vedotin for relapsed/refractory primary mediastinal large B-cell lymphoma: efficacy and safety from the phase II CheckMate 436 study [published online August 9, 2019] . J Clin Oncol . doi: 10.1200/JCO.19.01492
Petrich AM , Gandhi M , Jovanovic B , et al. . Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis . Blood 2014 ; 124 : 2354 – 2361 .
Oki Y , Noorani M , Lin P , et al. . Double hit lymphoma: the MD Anderson Cancer Center clinical experience . Br J Haematol 2014 ; 166 : 891 – 901 .
Dunleavy K , Fanale MA , Abramson JS , et al. . Dose-adjusted EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) in untreated aggressive diffuse large B-cell lymphoma with MYC rearrangement: a prospective, multicentre, single-arm phase 2 study . Lancet Haematol 2018 ; 5 : e609 – 617 .
Savage KJ , Slack GW , Mottok A , et al. . Impact of dual expression of MYC and BCL2 by immunohistochemistry on the risk of CNS relapse in DLBCL . Blood 2016 ; 127 : 2182 – 2188 .
Disclosures: Dr. Advani has disclosed that she has received grant/research support from Agensys, Inc., Celgene Corporation, Forty Seven, Inc., Janssen Pharmaceutica Products, LP, Kura Oncology, Inc., Merck & Co., Inc., Millennium Pharmaceuticals, Inc., Genentech, Inc./Roche Laboratories, Inc., Pharmacyclics, Regeneron Pharmaceuticals, Inc., Seattle Genetics, Inc.; received consulting fees from AstraZeneca Pharmaceuticals LP, Bayer HealthCare, Gilead Sciences, Inc., Kite Pharma, Kyowa Hakko Kirin Co., Ltd., Cell Medica, Genentech, Inc./Roche Laboratories, Inc., Seattle Genetics, Inc., and Takeda Pharmaceuticals North America, Inc.; and is a scientific advisor for AstraZeneca Pharmaceuticals LP, Bayer HealthCare, Gilead Sciences, Inc., Kite Pharma, Kyowa Hakko Kirin Co., Ltd., Cell Medica, Genentech, Inc./Roche Laboratories, Inc., Seattle Genetics, Inc., and Takeda Pharmaceuticals North America, Inc. Dr. Abramson has disclosed that he receives consulting fees from AbbVie, Inc., Bayer HealthCare, Celgene Corporation, EMD Serono, Genentech, Inc., Janssen Pharmaceutica Products, LP, Karyopharm Therapeutics, Kite Pharma, and Roche Laboratories, Inc. Dr. Dutia has disclosed that she has no interests, arrangements, affiliations, or commercial interests with the manufacturers of any products discussed in this article or their competitors. Dr. Fisher has disclosed that he receives consulting fees from Celgene Corporation and PRIME. Dr. Zelenetz has disclosed that he received consulting fees from AbbVie, Inc., Amgen Inc., AstraZeneca Pharmaceuticals LP, Celgene Corporation, Gilead Sciences, Inc., Janssen Pharmaceutica Products, LP, Novartis Pharmaceuticals Corporation, Adaptive Biotechnologies Corporation, Genentech, Inc./Roche Laboratories, Inc., and Pharmacyclics; is a scientific advisor for AbbVie, Inc., AstraZeneca Pharmaceuticals LP, and MorphoSys AG; and receives grant/research support from BeiGene, Gilead Sciences, Inc., MEI Pharma Inc., and Roche Laboratories, Inc.
Article Sections
- View raw image
- Download Powerpoint Slide
Article Information
- Get Permissions
- Similar articles in PubMed
Google Scholar
Related articles.
| All Time | Past Year | Past 30 Days | |
|---|---|---|---|
| Abstract Views | 0 | 0 | 0 |
| Full Text Views | 10616 | 2526 | 211 |
| PDF Downloads | 6141 | 1628 | 157 |
| EPUB Downloads | 0 | 0 | 0 |
- Advertising
- Terms of Use
- Privacy Policy
- Permissions

© 2019-2024 National Comprehensive Cancer Network
Powered by:
- [195.190.12.77]
- 195.190.12.77
Character limit 500 /500
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu
- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Case studies of elderly patients with non-hodgkin's lymphoma.

Share and Cite
Luminari, S.; Federico, M. Case Studies of Elderly Patients with Non-Hodgkin's Lymphoma. Hematol. Rep. 2011 , 3 , e7. https://doi.org/10.4081/hr.2011.s3.e7
Luminari S, Federico M. Case Studies of Elderly Patients with Non-Hodgkin's Lymphoma. Hematology Reports . 2011; 3(s3):e7. https://doi.org/10.4081/hr.2011.s3.e7
Luminari, Stefano, and Massimo Federico. 2011. "Case Studies of Elderly Patients with Non-Hodgkin's Lymphoma" Hematology Reports 3, no. s3: e7. https://doi.org/10.4081/hr.2011.s3.e7
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Case report
- Open access
- Published: 12 August 2021
A case report of COVID-19 in a patient with non-Hodgkin’s lymphoma
- Owrang Eilami 1 ,
- Max Igor Banks Ferreira Lopes 2 ,
- Ronaldo Cesar Borges Gryschek 3 &
- Kaveh Taghipour ORCID: orcid.org/0000-0002-3839-2607 4
BMC Infectious Diseases volume 21 , Article number: 809 ( 2021 ) Cite this article
17k Accesses
1 Citations
8 Altmetric
Metrics details
The current literature is scarce as to the outcomes of COVID-19 infection in non-Hodgkin's lymphoma patients and whether immunosuppressive or chemotherapeutic agents can cause worsening of the patients’ condition during COVID-19 infection.
Case presentation
Our case is a 59-year-old gentleman who presented to the Emergency Department of the Cancer Institute of Hospital das Clínicas da Universidade de São Paulo, São Paulo, Brazil on 10th May 2020 with a worsening dyspnea and chest pain which had started 3 days prior to presentation to the Emergency Department. He had a past history of non-Hodgkin's lymphoma for which he was receiving chemotherapy. Subsequent PCR testing demonstrated that our patient was SARS-CoV-2 positive.
In this report, we show a patient with non-Hodgkin lymphoma in the middle of chemotherapy, presented a mild clinical course of COVID-19 infection.
Peer Review reports
Since the first identification of COVID-19 in an outbreak in Wuhan China in December 2019 COVID-19 has quickly spread worldwide and was declared a worldwide pandemic on 11th March 2020. The clinical presentation of COVID-19 is variable with a clinical spectrum ranging from asymptomatic to life-threatening clinical presentation [ 1 ]. One would expect immunocompromised patients would be at high risk of complications from COVID-19 infection, however, there have been reports of variable clinical presentation and clinical course within this subgroup of patients [ 2 ]. Currently the data regarding risk and outcome of infection by SARS-CoV-2 in lymphoma patients is scarce and variable. Lymphoma patients present an interesting subgroup as they typically receive immunosuppressive and chemotherapy drugs during their treatment. We are presenting a case of symptomatic COVID-19 with comorbid non-Hodgkin's lymphoma who was receiving chemotherapy and subsequently recovered from COVID-19 infection.
Our patient is a 59-year-old gentleman who presented to the Emergency Department of the Cancer Institute of Hospital das Clínicas da Universidade de São Paulo, Brazil on 10th May 2020 with worsening dyspnea and chest pain for the last 3 days. Five months prior to presentation he had been diagnosed with non-Hodgkin's lymphoma and previously, on April 29th during a routine follow-up hospital admission for his lymphoma, he had a routine PET CT (Fig. 1 ) and chest CT scan (Fig. 2 ) performed for lymphoma follow-up showing bilateral ground-glass lung lesions with less than 25% of lung involvement suggestive of COVID-19 infection. Subsequent COVID-19 PCR revealed that the patient was COVID-19 positive, however as he was asymptomatic, he was discharged.
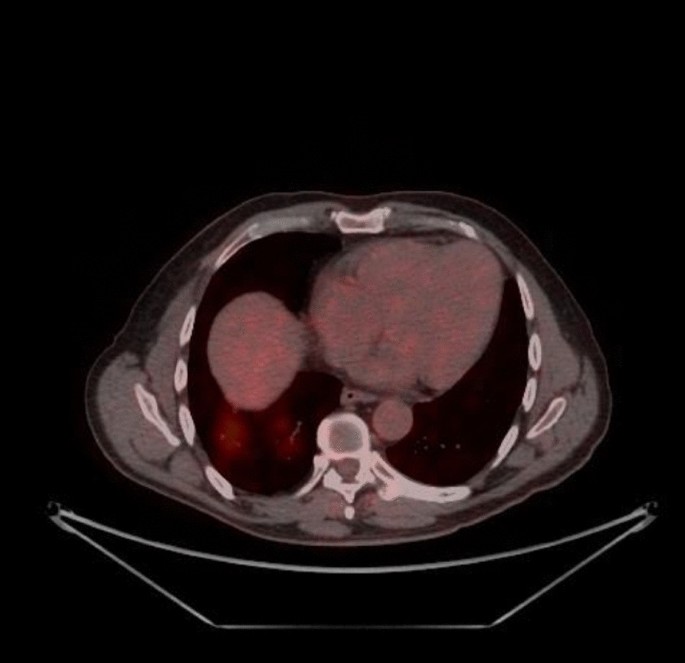
PET-CT 29/04: appearance of multiple areas of discrete opacity bilateral in pulmonary parenchyma, predominating in the base (SUVmax: 3.7-right base. The comparative analysis with a previous examination of 03/18/2020 shows: the degree of glycolytic hypermetabolism persists without significant variation associated with reduced dimensions, in heterogeneous tissue formation. The findings are compatible with uptake above mediastinal, but below or equal to uptake in the liver with nodal or extranodal sites with or without a residual mass indicating a non-progressive disease with a complete metabolic response to lymphoma treatment. The appearance of multiple areas of ground-glass opacities sparse by the bilateral pulmonary parenchyma, predominantly at the right base, suspicious for viral pneumonia
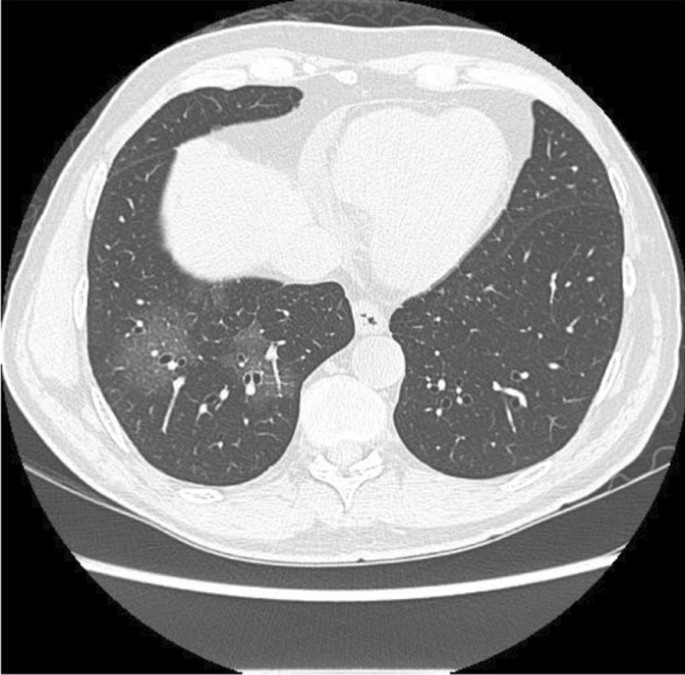
Computed tomography of the chest without the administration of the intravenous contrast medium—pulmonary ground-glass opacities and foci of consolidation, sometimes associated with septal thickening, with multifocal distribution, bilateral and predominantly peripheral. The estimated extent of involvement in pulmonary tomography is less than 50%
Comorbidities presented were systemic arterial hypertension treated with losartan 50 mg bid and non-insulin-dependent diabetes treated with 60 mg of gliclazide per day and metformin 850 mg q8h.
The past medical history of our patient includes the diagnosis of lymphoma on December 1st, 2019, after an exploratory laparotomy due to perforating acute abdomen resulting in enterectomy of the perforated segment (15 cm resection) plus manual end-to-end anastomosis + Barker peritoniostomy (due to hemodynamic instability). On December 5th—a second look abdominal surgery was performed with wall closure and mesh placement. The lymphoma was classified as diffuse large cells non-Hodgkin lymphoma—CD20 negative. The patient started CHOP chemotherapy [cyclophosphamide, doxorubicin, vincristine, prednisolone] with cycles every 21 days last on April 16th and three cycles of intrathecal methotrexate (MTX) chemotherapy last on March 16th.
Eleven days following discharge from the patient's first admission, the patient’s condition worsened. Subsequently on 10th of May 2020, the patient presented with worsening cough, dyspnea and chest pain to the Emergency Department of the Cancer Institute of Hospital das Clínicas da Universidade de São Paulo, Brazil. Due to the patients deteriorating condition the patient was admitted to hospital.
During his latest hospital stay, he was prescribed ceftriaxone 2 g QD for seven days, azithromycin 500 mg QD for five days, enoxaparin 40 mg QD, oseltamivir 75 mg bid for two days (until the result of SARS-CoV-2 RT PCR positive). He received pneumocystis prophylaxis with sulfamethoxazole 400 mg + trimethoprim 80 mg and acyclovir 200 mg QD for herpes simplex prophylaxis. A second chest CT scan was performed (Fig. 3 ) which demonstrated an increase in the extension and attenuation of pulmonary opacities compared with the patient’s previous chest CT scan (Fig. 2 ). The patient’s clinical condition was stable without any worsening of clinical condition and biochemical markers (Table 1 ) during his hospital stay and maximum oxygen intake of 3L/min by nasal cannula. The oxygen supplementation was titrated and interrupted on May 13th. On May 19th, the patient was discharged. At that time, a second nasal SARS-CoV-2 RT PCR was performed and resulted in a negative result.

Computed Tomography of the Chest without the administration of the intravenous contrast medium—these set of findings is suggestive of the inflammatory process, and the viral etiology must be included in the etiological differential, particularly COVID-19. Regarding the PET-CT 29/04/2020 exam, there was an increase in the extension and attenuation of pulmonary opacities
Discussion and conclusion
Non-Hodgkin's lymphoma presents a dilemma to healthcare professionals as there is concern that chemotherapeutic and immunosuppressive treatment which is a pillar of cancer therapy may lead to a worsening of comorbid COVID-19 infections.
The current literature is scarce as to the outcomes of COVID-19 infection in non-Hodgkin's lymphoma patients and whether immunosuppressive or chemotherapeutic agents can cause worsening of the patients’ condition during COVID-19 infection. Our case of a 59-year-old gentleman with non-Hodgkin’s lymphoma presents a glimpse and discussion of current assumptions of this subgroup of patients and comorbid COVID-19 infection because contrary to our expectations the patient had a benign clinical course without any evidence of worsening of symptoms that are contrary to our experience with other infections that are often more frequent and more severe in cancer and hematological malignancy patients.
The clinical presentation of our patient was that he had progressive dyspnea without fever. Only on the 4th day following admission the patient developed fever which is in contrast to a retrospective study by Zhang et al. conducted in Wuhan, China of 28 COVID-19-infected cancer patients which had shown that fever was present in 82.1% of patients followed by dry cough in 81% of patients and dyspnea in 50% of patients [ 3 ]. In another retrospective study by Yang et al. of 52 cancer patients with COVID-19 the common presenting symptoms were: fever (25%), dry cough (17.3%), chest distress (11.5%), and fatigue (9.6%) [ 4 ].
In a study by Chen and colleagues of 128 hospitalized patients with hematological cancer in two centers in Wuhan China it was shown that there was no significant difference in the case rate between in hematological malignancy patients versus non hematological malignancy patients [ 5 ]. Furthermore, patients with hematological malignancy had more severe disease and increase fatality when infected by COVID-19. In a study by Yigenoglu et al. of 740 COVID-19 patients with hematological malignancy it was shown that the length of hospital and ICU admission were higher in patients with hematological malignancy compared to patients without cancer [ 6 ]. However, the length of hospital stays and ICU stay was similar between groups. In a case report of 4 patients by Bellmann-Weiler et al. All 4 patients had COVID-19 infection with comorbid hematological malignancy all recovered from COVID-19 and were discharged. The authors noted that hyperinflammatory associated organ failure may be less pronounced in hematological malignancies due to treatment related immunosuppression [ 7 ]. In an observational study by Norsa et al. of 522 patients with inflammatory bowel disease in Northern Italy it was observed that of these patients none were admitted to hospital with SARS-CoV-2 proven infection and none of the patients with IBD in this study was affected by a complicated SARS-CoV-2–related pneumonia [ 8 ]. The authors concluded that the data suggest that patients receiving immunosuppressive treatments could be at lower risk of developing severe symptomatic SARS-CoV-2 infection.
It is well-known that systemic inflammation and the resulting cytokine cascade is an important pathophysiological mechanism in the development of COVID-19 associated acute respiratory distress [ 9 ]. The resulting therapies for COVID-19 have been aimed at reducing systemic inflammation. In a study by Lee et al. On 800 patients who had a diagnosis of cancer and symptomatic COVID 19 they were unable to find that cancer patients on active cytotoxic chemotherapy were at increased risk of mortality from COVID-19 compared to those cancer patients not on chemotherapy [ 10 ].
Unfortunately, data on COVID-19 among cancer patients is still scarce, with few described cases. Along with the small sample size of only Chinese patients, there is a large amount of heterogeneity due to several cancer types and different oncologic treatments. Despite this, not all cases were fully described, with many of them already in cancer remission with no clear immunosuppression. Most of the studies included patients with a history of negative predictive factors like smoking and older age, which may explain worse outcomes of COVID-19 infection.
In conclusion, although cancer patients with COVID-19 are expected to have a more unsatisfactory outcome, data remains scarce. We are still learning from this outbreak, and international collaboration is necessary to describe better the characteristics and outcomes of COVID-19 disease among cancer patients. In this report, we show a patient with non-Hodgkin lymphoma in the middle of chemotherapy, presented a mild clinical course of COVID-19 infection. More information is still needed concerning specific cancer types and the impact of chemotherapy on COVID-19.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
Corona virus disease 2019
Polymerase chain reaction
Severe acute respiratory syndrome-corona virus-2
Twice daily
Positron emission tomographic computed tomography scan
Cluster of differentiation 20
Cyclophosphamide, doxorubicin, vincristine, prednisolone and methotrexate
Reverse transcriptase polymerase chain reaction
García LF. Immune response, inflammation, and the clinical spectrum of COVID-19. Front Immunol. 2020;11:1441. https://doi.org/10.3389/fimmu.2020.01441 .
Fung M, Babik JM. COVID-19 in immunocompromised hosts: what we know so far. Clin Infect Dis. 2021;72(2):340–50. https://doi.org/10.1093/cid/ciaa863 .
Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31(7):894–901.
Article CAS Google Scholar
Yang F, Shi S, Zhu J, Shi J, Dai K, Chen X. Clinical characteristics and outcomes of cancer patients with COVID-19. J Med Virol. 2020;92:2067–73. https://doi.org/10.1002/jmv.25972 .
He W, Chen L, Chen L, Yuan G, Fang Y, Chen W, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34(6):1637–45.
Yigenoglu TN, Ata N, Altuntas F, Bascı S, Dal MS, Korkmaz S, Namdaroglu S, Basturk A, Hacıbekiroglu T, Dogu MH, Berber İ, Dal K, Erkurt MA, Turgut B, Ulgu MM, Celik O, Imrat E, Birinci S. The outcome of COVID-19 in patients with hematological malignancy. J Med Virol. 2021 Feb;93(2):1099-104. https://doi.org/10.1002/jmv.26404 .
Bellmann-Weiler R, Burkert F, Schwaiger T, Schmidt S, Ludescher C, Oexle H, Wolf D, Weiss G. Janus faced course of COVID-19 infection in patients with hematological malignancies. Eur J Haematol. 2020. https://doi.org/10.1111/ejh.13470 .
Norsa L, Indriolo A, Sansotta N, Cosimo P, Greco S, D’Antiga L. Uneventful course in patients with inflammatory bowel disease during the severe acute respiratory syndrome coronavirus 2 outbreak in Northern Italy. Gastroenterology. 2020;159(1):371–2.
Coperchini F, Chiovato L, Croce L, Magri F, Rotondi M. The cytokine storm in COVID-19: an overview of the involvement of the chemokine/chemokine-receptor system. Cytokine Growth Factor Rev. 2020;53:25–32.
Lee LYW, Cazier J-B, Angelis V, Arnold R, Bisht V, Campton NA, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395(10241):1919–26.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Department of Infectious Diseases and Family Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
Owrang Eilami
Department of Infectious and Parasitic Diseases, Central Institute, Hospital das Clínicas, School of Medicine, University of São Paulo, São Paulo, Brazil
Max Igor Banks Ferreira Lopes
Associate Professor of Infectious Diseases, Hospital das Clínicas,, School of Medicine, University of São Paulo, São Paulo, Brazil
Ronaldo Cesar Borges Gryschek
Department of Family Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
Kaveh Taghipour
You can also search for this author in PubMed Google Scholar
Contributions
Case history, patient data, lab data and radiological images collected by: OE, MIBFL, RCBG; Manuscript written by: OE and KT; Editing: OE and KT; All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Kaveh Taghipour .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
Additional information, publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Eilami, O., Lopes, M.I.B.F., Gryschek, R.C.B. et al. A case report of COVID-19 in a patient with non-Hodgkin’s lymphoma. BMC Infect Dis 21 , 809 (2021). https://doi.org/10.1186/s12879-021-06472-2
Download citation
Received : 16 April 2021
Accepted : 01 July 2021
Published : 12 August 2021
DOI : https://doi.org/10.1186/s12879-021-06472-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Immunosuppressed
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
- Case report
- Open access
- Published: 15 April 2017
Primary adrenal non-Hodgkin lymphoma: a case report and review of the literature
- Nanik Ram 1 ,
- Owais Rashid 1 ,
- Saad Farooq 2 ,
- Imran Ulhaq 1 &
- Najmul Islam 1
Journal of Medical Case Reports volume 11 , Article number: 108 ( 2017 ) Cite this article
5036 Accesses
16 Citations
1 Altmetric
Metrics details
Lymphomas are cancers that arise from the white blood cells and have been traditionally divided into two large subtypes: Hodgkin and non-Hodgkin lymphoma. B-cell lymphoma is the most common subtype of non-Hodgkin lymphoma; almost 85% of patients with lymphoma have this variant. Lymphomas can potentially arise from any lymphoid tissue located in the body; however, primary adrenal non-Hodgkin lymphoma is extremely rare. We report the history, examination findings, and laboratory results of a 50-year-old man diagnosed with a primary left adrenal diffuse large B-cell lymphoma.
Case presentation
A 50-year-old Pakistani man presented to our hospital with progressively increasing pain and fullness in the left upper quadrant of his abdomen, generalized weakness, easy fatigability, and decreased appetite of 1.5 months’ duration. On examination, he had a blood pressure of 140/80 mmHg with no postural drop, a pulse rate of 106 beats/minute, and no fever. His past medical history was significant for pulmonary tuberculosis 2 years earlier, for which he received antituberculous therapy. Computed tomography revealed a heterogeneous enhancing soft tissue density mass in the left adrenal gland. It measured 7.1 × 5.6 × 9.5 cm. Further laboratory workup revealed the following levels: sodium 135 mEq/L, potassium 4.5 mEq/L, lactate dehydrogenase 905 IU/L, renin 364 IU/ml, aldosterone 5.79 ng/dl, dehydroepiandrosterone sulfate 79.20 μg/dl, urinary vanillylmandelic acid 6.4 mg/24 hours, and a low-dose overnight dexamethasone suppression test result of 3.20 μg/dl. The patient underwent left adrenalectomy. Histopathological test results showed a diffuse large B-cell lymphoma. Immunohistochemical stains were strongly positive for CD20 and negative for CD3, CD5, CD10, and cyclin D1. The patient’s Ki-67 (Mib-1) index was approximately 80%. He received a total of six cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy (rituximab was not given, owing to financial constraints) and was routinely followed pre- and postchemotherapy at our hematology clinic with complete blood count and serum lactate dehydrogenase evaluations. The patient responded to chemotherapy and is currently doing well.
Conclusions
Primary adrenal lymphoma is an extremely rare but rapidly progressive disease. It generally carries a poor prognosis, partly because an optimal treatment protocol has not yet been established. Further studies with larger sample sizes are needed to establish the best treatment option and increase overall survival.
Peer Review reports
The American Cancer Society estimated that more than 70,000 new cases of non-Hodgkin lymphoma (NHL) would be diagnosed in 2016 [ 1 , 2 ]. Although lymphomas arise mainly from lymph nodes, primary extranodal NHL occurs in at least 25% of the cases [ 3 ]. The adrenal gland can be secondarily involved in around 4% of the patients; however, primary adrenal NHL is extremely rare and accounts for less than 1% of all NHL cases [ 4 ]. Primary adrenal lymphoma (PAL) is histologically proven lymphoma of one or both adrenal glands in patients with no prior history of lymphoma. If other organs or lymph nodes besides the adrenal glands are involved, the adrenal lesion must be unequivocally dominant [ 5 ].
PAL occurs predominantly in males in the sixth to seventh decades of life. Most commonly, this lymphoma is a nongerminal center-type diffuse large B-cell lymphoma (DLBCL), which is present in 70% to 80% of the patients [ 6 ]. Patients present with abdominal or lumbar pain; fever; weight loss; and signs of adrenal insufficiency such as hypotension, hyponatremia, fatigue, skin hyperpigmentation, and vomiting [ 7 ]. In occasional instances, it may also be an incidental finding on imaging studies obtained for other purposes, and it is frequently bilateral and bulky at the time of presentation. Several etiological factors, such as Epstein-Barr virus infection, genetic defects in p53 and c-kit, and immune dysregulation, have been implicated in the pathogenesis of this disease [ 5 , 7 ]. Laboratory investigations often show elevated lactate dehydrogenase (LDH), β 2 -microglobulin, C-reactive protein, and ferritinemia, which signify high levels of inflammation associated with PAL [ 6 ].
The prognosis of this condition is generally considered to be poor because PAL is an aggressive disease and progresses rapidly. An average 1-year survival as low as 20% has been reported; however, owing to the rare nature of this disease, prognostic factors are difficult to elucidate [ 5 ].
A 50-year-old Pakistani man known to have had diabetes for 21 years presented to our hospital with progressively increasing pain and fullness in the left upper quadrant of his abdomen, generalized weakness, easy fatigability, and decreased appetite of 1.5 months’ duration. He also complained of nausea and early satiety and had a weight loss of 8 kg over this period. On examination, he was found to have a blood pressure of 140/80 mmHg with no postural drop, a pulse rate of 106 beats/minute, and no fever. His physical examination was otherwise unremarkable. His past medical history was significant for pulmonary tuberculosis 2 years earlier, for which he received antituberculous therapy.
The patient had initially presented at another university hospital 3 weeks earlier. At that time, a laboratory workup and computed tomography (CT) of the abdomen with contrast enhancement were done. Although the results of his complete blood count and renal function test were normal, CT of the abdomen showed a heterogeneous enhancing soft tissue density mass in the left adrenal gland. The mass measured 7.1 × 5.6 cm in transverse and anteroposterior diameter, and the craniocaudal extent of the mass was 9.5 cm. Medially, the mass was abutting the celiac and superior mesenteric arteries, and posteroinferiorly, it was bordering the renal vessels. Paraaortic lymphadenopathy was also present, with the largest one measuring 1.6 cm (Fig. 1 ).
Computed tomography of the patient showing a large left adrenal mass
Further laboratory workup revealed the following levels: sodium 135 mEq/L, potassium 4.5 mEq/L, LDH 905 IU/L, renin 364 IU/ml, aldosterone 5.79 ng/dl, dehydroepiandrosterone sulfate 79.20 μg/dl, urinary vanillylmandelic acid 6.4 mg/24 hours, and a low-dose overnight dexamethasone suppression test result of 3.20 μg/dl. The patient was referred to our urology clinic for surgical removal of his mass. He underwent a left adrenalectomy at the urology clinic on 4 March 2016. Histopathological analysis revealed DLBCL (Figs. 2 and 3 ). The results of immunohistochemical stains were strongly positive for CD20 and negative for CD3, CD5, CD10, and cyclin D1. His Ki-67 (Mib-1) index was approximately 80% (Figs. 4 and 5 ).
Low-power view of the lesion showing diffuse sheets of neoplastic cells (hematoxylin and eosin stain)
High-power view of the lesion showing large-sized neoplastic cells with pleomorphic nuclei, variably prominent nucleoli, and scant cytoplasm. Frequent mitotic figures are also noted (hematoxylin and eosin stain)
CD20 immunohistochemical stain (pan-B) is strongly positive for neoplastic cells
Ki-67 immunohistochemical stain highlights a markedly raised proliferative index in the neoplastic lymphoid population
For further management, the patient was referred to our hematology clinic and was planned for a rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) chemotherapy regimen starting on 18 March 2016. He received a total of six cycles of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP; rituximab was not given, owing to financial constraints) and was routinely followed pre- and postchemotherapy at the hematology clinic with complete blood count and serum LDH evaluations. Positron emission tomography (PET) performed on 24 March 2016 showed metabolically active residual disease over the left adrenal bed. Subcentimetric fluorodeoxyglucose (FDG) deposits were seen in the patient’s L5, L2, and T12 vertebrae, suggestive of marrow infiltration. No evidence of hypermetabolic nodal, hepatic, or splenic involvement was appreciated. However, the patient responded to chemotherapy and is currently doing well. He gained around 8 kg of weight and is following his routine daily activities. A recent PET scan revealed that the previously seen hypermetabolic foci along the left crus, left proximal paraaortic region, and foci of FDG uptake in the lumbar and thoracic vertebrae were not appreciable. The patient’s Deauville 5-point scale score was 0 (complete metabolic response).
To the best of our knowledge, this is the first report describing a case of primary adrenal NHL in Pakistan. Our patient was a man in his fifth decade of life, which, on the basis of published literature, is a relatively young age to have this disease. We treated our patient with a regimen of CHOP; rituximab was not included, owing to financial constraints. Even without rituximab, our patient showed a complete response to therapy. Because primary adrenal NHL is a rare disease, optimal treatment has not yet been established. CHOP or CHOP-like regimens were traditionally used before the introduction of rituximab, with generally dismal results (overall survival between 20% and 50%) [ 7 ]. In the largest study to date on PAL, involving 31 patients given an R-CHOP chemotherapy regimen, complete remission and overall response rates were 54.8% and 87.0%, respectively. Surprisingly, no difference was found in overall survival between unilateral and bilateral NHL of the adrenal gland [ 8 ]. Our patient also underwent adrenalectomy; however, the two largest studies to date showed no survival benefit in patients who underwent adrenalectomy as compared with those who were treated with chemotherapy alone [ 6 , 8 ].
In another study involving 28 patients with PAL, 64% of the patients were treated with a CHOP regimen, 50% with an R-CHOP regimen, and 18% had chemotherapy with doxorubicin, cyclophosphamide, vindesine, bleomycin, and prednisone. The overall survival was 61.6%; however, it was 100% for those who received autologous stem cell transplants, which suggests that this may prolong survival [ 6 ]. The Ki-67 index was high in our patient (80%). Ichikawa et al . reported this index to be greater than 70% in seven patients with primary adrenal DLBCL. They treated all of these patients with rituximab-containing chemotherapy and reported a 2-year survival rate of 57%, although none of the patients died as a result of advancement of lymphoma [ 9 ]. These authors suggested that rituximab-containing chemotherapy with central nervous system (CNS) prophylaxis with methotrexate may be a good treatment option for primary adrenal NHL. Kim et al . reported CNS relapses or progression in four patients, none of whom had received intrathecal prophylaxis [ 8 ].
For our patient, we opted for CT as the initial imaging modality and then confirmed the diagnosis via histology of the resected adrenal gland. Grigg et al . suggested that though magnetic resonance imaging and CT findings can be highly suggestive of NHL, a biopsy should be done for diagnosis. Staging should involve a PET or gallium scan, and in patients with elevated LDH levels, a lumbar puncture should also be done [ 7 ].
According to the International Prognostic Index (IPI), our patient was in the low- to intermediate-risk category, which has an estimated 5-year survival of 51%. However, this scoring system is not specific to PAL; thus, it may be inaccurate in predicting overall survival. Kim et al . found that neither high-risk IPI score nor advanced-stage disease according to the Ann Arbor system had any impact on the overall survival; therefore, they suggested a modified IPI scoring system and a revised staging system, which resulted in significantly improved predictability of overall survival [ 9 ]. The modified scoring and staging criteria may prove beneficial in risk stratification of patients with primary adrenal NHL and also guide treatment.
No protocol for specific treatment in cases of a primary adrenal NHL has yet been established, and multiple authors have used a combination of modalities, including surgery and chemotherapy. Ichikawa et al . argued that perhaps one of the reasons for the poor prognosis is that many patients were previously treated with chemotherapy not containing rituximab and did not receive CNS prophylaxis, which may have decreased overall survival [ 9 ].
PAL is a rare but rapidly progressing disease that should be treated aggressively. Rituximab-containing chemotherapy such as R-CHOP has shown promise by increasing the overall survival of patients with this disease. R-CHOP combined with CNS prophylaxis and autologous stem cell transplant may further increase overall survival, but further studies with larger sample sizes are needed to establish the best treatment option and decide whether surgery and radiation have a role in the management of PAL.
Abbreviations
Cyclophosphamide, doxorubicin, vincristine, and prednisone
Central nervous system
Computed tomography
Diffuse large B-cell lymphoma
Fluorodeoxyglucose
International Prognostic Index
Lactate dehydrogenase
- Non-Hodgkin lymphoma
- Primary adrenal lymphoma
Positron emission tomography
Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone
Vinjamaram S, Estrada-Garcia DA, Hernandez-Ilizaliturri FJ. Non-Hodgkin lymphoma: practice essentials [updated 22 Sep 2016]. http://emedicine.medscape.com/article/203399-overview . Accessed 30 Sep 2016.
American Cancer Society. Cancer facts & figures 2016. Atlanta: American Cancer Society; 2016. https://old.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf . Accessed 6 Jul 2016.
Google Scholar
Kashyap R, Mittal B, Manohar K, Harisankar C, Bhattacharya A, Singh B, et al. Extranodal manifestations of lymphoma on [ 18 F]FDG-PET/CT: a pictorial essay. Cancer Imaging. 2011;11:166–74.
Article PubMed PubMed Central Google Scholar
Metser U, Goor O, Lerman H, Naparstek E, Even-Sapir E. PET-CT of extranodal lymphoma. AJR Am J Roentgenol. 2004;182:1579–86.
Article PubMed Google Scholar
Rashidi A, Fisher SI. Primary adrenal lymphoma: a systematic review. Ann Hematol. 2013;92:1583–93.
Article CAS PubMed Google Scholar
Laurent C, Casasnovas O, Martin L, Chauchet A, Ghesquieres H, Aussedat G, et al. Adrenal lymphoma: presentation, management and prognosis. QJM. 2017;110:103–9.
CAS PubMed Google Scholar
Grigg AP, Connors JM. Primary adrenal lymphoma. Clin Lymphoma. 2003;4:154–60.
Kim YR, Kim JS, Min YH, Hyunyoon D, Shin HJ, Mun YC, et al. Prognostic factors in primary diffuse large B-cell lymphoma of adrenal gland treated with rituximab-CHOP chemotherapy from the Consortium for Improving Survival of Lymphoma (CISL). J Hematol Oncol. 2012;5:49.
Article CAS PubMed PubMed Central Google Scholar
Ichikawa S, Fukuhara N, Inoue A, Katsushima H, Ohba R, Katsuoka Y, et al. Clinicopathological analysis of primary adrenal diffuse large B-cell lymphoma: effectiveness of rituximab-containing chemotherapy including central nervous system prophylaxis. Exp Hematol Oncol. 2013;2:19.
Download references
Acknowledgements
We are grateful to Dr. Sabeeh Siddique for providing the histological figures with explanations.
Availability of data and materials
Data sharing is not applicable to this article, because no datasets were generated or analyzed during the present study.
Authors’ contributions
NR conceived of the study and helped to draft the manuscript. OR and SF were involved in patient care and helped write the case presentation. IU and NI also helped to draft the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Department of Medicine, Section of Endocrinology, Aga Khan University, Karachi, Pakistan
Nanik Ram, Owais Rashid, Imran Ulhaq & Najmul Islam
Aga Khan University, Stadium Road, Karachi, Pakistan
Saad Farooq
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Owais Rashid .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Ram, N., Rashid, O., Farooq, S. et al. Primary adrenal non-Hodgkin lymphoma: a case report and review of the literature. J Med Case Reports 11 , 108 (2017). https://doi.org/10.1186/s13256-017-1271-x
Download citation
Received : 10 November 2016
Accepted : 21 March 2017
Published : 15 April 2017
DOI : https://doi.org/10.1186/s13256-017-1271-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adrenal mass
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Clinical analysis of 20 patients with non-Hodgkin lymphoma and autoimmune hemolytic anemia
A retrospective study.
Editor(s): Bush., Eric
Department of Hematology, The First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, PR China.
∗Correspondence: Ji-cheng Zhou, Department of Hematology, The First Affiliated Hospital of Guangxi Medical University, 6 Shuang Yong Road, Nanning 530021, Guangxi, PR China (e-mail: [email protected] ).
Abbreviations: AIHA = autoimmune hemolytic anemia, AIHA/NHL = AIHA associated NHL, AITL = angioimmunoblastic T-cell lymphoma, BCL-U = B-cell lymphoma-unclassified, BMB = bone marrow biopsy, BMS = bone marrow smears, CLL/SLL = chronic lymphocytic leukemia/small lymphocyte lymphoma, CR = complete remission, LBMI = lymphoma bone marrow infiltration, MCL = mantle cell lymphoma, MZBL = marginal zone B-cell lymphoma, NHL = non-Hodgkin's lymphoma, PR = partial remission.
How to cite this article: Zhou Jc, Wu Mq, Peng Zm, Zhao Wh, Bai Zj. Clinical analysis of 20 patients with non-Hodgkin lymphoma and autoimmune hemolytic anemia: a retrospective study. Medicine . 2020;99:7(e19015).
This work was supported by research grants from National Natural science of China (Grant No.81700172), Guangxi Natural Science Foundations (Grant No.2016GXNSFBA380059) and Medical and Health Suitable Technology Development and Application Project of Guangxi (Grant No. S201685).
The authors have no conflicts of interest to disclose.
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial License 4.0 (CCBY-NC), where it is permissible to download, share, remix, transform, and buildup the work provided it is properly cited. The work cannot be used commercially without permission from the journal. http://creativecommons.org/licenses/by-nc/4.0
Non-Hodgkin lymphoma (NHL) can co-exist with autoimmune hemolytic anemia (AIHA), a phenomenon known as AIHA-associated NHL (AIHA/NHL). However, few studies have reported AIHA/NHL incidence or its clinical characteristics. We conducted a retrospective analysis of 20 AIHA/NHL patients treated at our hospital from 2009 to 2018. AIHA/NHL was presented by only 0.91% of the NHL and 9.8% of the AIHA patients. In addition, AIHA occurred most frequently with angioimmunoblastic T-cell lymphoma (AITL) (7.31%), followed by marginal zone B-cell lymphoma (MZBL) (6.25%), B-cell lymphoma-unclassified (BCL-U) (4.25%), chronic lymphocytic leukemia/small lymphocyte lymphoma (CLL/SLL) (2.50%), and mantle cell lymphoma (MCL) (2.30%). In addition to the CLL/SLL patients with impaired bone marrow, 66.7% of the AIHA/NHL patients had lymphoma bone marrow infiltration (LBMI), of which 4 patients presented LBMI in bone marrow smears (BMS) but not in bone marrow biopsy (BMB) and 6 were positive for BMB but not BMS. The 1-, 3- and 5-year survival rates of AIHA/NHL patients were 70%, 30% and 20%, respectively, and they responded poorly to chemotherapy. In conclusion, AIHA can co-exist with various NHLs and the defining clinical characteristic of AIHA/NHL is the high incidence of LBMI. However, both BMS and BMB should be performed to avoid missed diagnosis.
1 Introduction
Autoimmune hemolytic anemia (AIHA) is caused by hyperfunctioning B lymphocytes, which produce large amounts of autoantibodies and/or complement that are adsorbed on red blood cells (RBCs), resulting in their rapid lysis following antigen-antibody reaction. Primary AIHA does not have any underlying diseases, whereas secondary AIHA accompanies immune-related and lymphatic proliferation diseases, measles, EB and cytomegalovirus infections, as well as leukemia, thymoma, and colon cancer. [1–4]
Lymphomas are solid hematological tumors that originate in lymph nodes or lymphoid tissues, and are classified into Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL), depending on the presence or absence of Reed–Sternberg cells. NHLs include diffuse large B cell lymphoma (DLBCL), follicular lymphoma (FL), mucosa-associated lymphoid tissue lymphoma, marginal zone B-cell lymphoma (MZBL), peripheral T-cell lymphoma (PTCL), etc. [5,6] . The etiology and pathogenesis of lymphoma are still unclear, although viral infections, oncogenic mutations, radiation and chemical exposure, and autoimmune diseases have been variously implicated. [7–10]
Roughly one-fifth of AIHA patients develop lymphoma, while 7% to 10% of lymphoma patients have co-existing AIHA, indicating a clinicopathological link between both diseases. [2,3,11,12] The incidence of AIHA/NHL is relatively rare, [3] and few reports are available regarding its clinical characteristics. To this end, we conducted a retrospective study of 20 cases of AIHA/NHL that were diagnosed at our hospital in the last 10 years.
2 Materials and methods
Clinical and laboratory data of the AIHA/NHL patients that were treated at our hospital from January 2009 to December 2018 were retrospectively analyzed. AIHA was diagnosed on the basis of anemia, elevated reticulocyte count, high levels indirect bilirubin, and positive direct antihuman globulin test. Since AIHA usually precedes or occurs during the complete remission (CR) of NHL, patients initially diagnosed with AIHA without any signs of NHL were treated as per the AIHA treatment guidelines. [9,13] In contrast, patients presenting first with NHL with or without accompanying AIHA were treated as per the NCCN treatment guidelines for NHL. [14,15]
NHL was confirmed in all patients of our cohort by bone marrow smears (BMS), bone marrow biopsy (BMB) or lymph node biopsy. In addition, immune-phenotyping was performed for the T cell markers CD2, CD3, CD4, CD5, CD7, CD8, CD30, CD45RO, Cxcl-13, TIA-1, and ALK, B cell markers including CD10, CD19, CD20, CD21, CD79, Pax5, Bcl-2 and Bcl-6, and the NK cell marker CD56. The NHL stage was determined by routine blood tests, liver and kidney function tests, chest CT, and abdominal B-ultrasound. The classification of NHL was based on the WHO 2008 and 2016 lymphoma classification criteria, [16,17] and further staging and subgrouping were based on the Ann Arbor criterion (the staging of CLL/SLL was based on the Rai criterion).
The efficacy of NHL treatment was evaluated after 4 courses of chemotherapy. In case a patient simultaneously presented with AIHA, the efficacy of AIHA treatment was also evaluated. If CR of NHL was obtained, the original chemotherapy regimens would be used to consolidate the chemotherapy 2 courses and ended the treatment. If CR of NHL was not obtained, the efficacy would be re-evaluated after 2 courses of chemotherapy with the original chemotherapy regimens. If CR was obtained, the original chemotherapy regimens would be used to consolidate the chemotherapy 2 courses to end the chemotherapy. Otherwise, radiotherapy or hematopoietic stem cell transplantation would be used.
2.1 Ethics statement
Written informed consents were obtained from all the parents of the patients and their donors in accordance with the Declaration of Helsinki. And it was approved by the ethics committee of the first affiliated hospital of Guangxi Medical University, Guangxi, China.
At total of 2204 NHL and 204 AIHA patients admitted to our hospital in the period between January 2009 and December 2018, of which 20 patients were diagnosed with AIHA/NHL and accounted for 0.91% and 9.8% of the NHL and AIHA cases, respectively. The clinical characteristics of 20 AIHA/NHL patients are summarized in Table 1 . There were 14 males and 6 females in our cohort, with ages ranging from 39 to 85 years and median age 60 years. All patients were at stage III to IV of NHL, and the distribution is shown in Table 2 . The incidence of AIHA was highest in patients with angioimmunoblastic T-cell lymphoma (AITL) (7.31%), followed by MZBL (6.25%), BCL-U (4.25%), chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) (2.50%) and mantle cell lymphoma (MCL) (2.30%). The B-cell lymphoma diagnosed in 47 of the 2204 NHL patients could not be classified further, and the patients were thus grouped under BCL-U. In addition, since CLL and SLL have similar characteristics, patients with either were grouped together as SLL/CLL.

The laboratory characteristics of the AIHA/NHL patients are summarized in Table 3 . Nineteen patients harbored warm-reactive autoantibodies whereas 1 had cold-reactive autoantibodies. In addition, 6 patients each had high levels of C3 or IgG in the sera, and 8 were positive for C3 and IgG. AIHA was diagnosed 0 to 6656 days before NHL diagnosis in 12 patients, and 1 to 2121 days after NHL diagnosis in 8 patients. Among the 5 CLL/SLL cases, patients 9 and 16 were simultaneously diagnosed with AIHA and lymphoma, and patients 18, 19, and 20 were diagnosed with CLL/SLL, respectively, 225, 1619, and 2121 days before AIHA. All patients underwent BMS and BMB, and 10 also underwent lymph node biopsy. In addition to the CLL/SLL patients, 10 others showed lymphoma bone marrow infiltration (LBMI), resulting in a high 66.7% overall incidence in the AIHA/NHL cohort. Among the non-CLL/SLL patients with LBMI, BMS was positive and BMB was negative in 4 cases, including 2 of DLBCL, and 1 each of PTCL and MZBL. In addition, BMB was positive and BMS was negative for LBMI in 6 cases, including 2 of MCL, and 1 each of MZBL, FL, AITL and BCL-U.

During AIHA treatment, patients 1 to 6 (see Table 4 ) were treated with prednisone alone, and the remaining received glucocorticoid and combined chemotherapy for NHL. Patients 1, 2, 8, 13, and 19 achieved CR, and the others showed partial remission (PR) or no remission (NR). Patients 8, 9, 12, 13, 18, 19, and 20 received 4 or more courses of combined chemotherapy, of which only patients 8 and 9 achieved CR. In the follow-up to January 2019, 7 of the 20 patients were still alive. The 1-, 3- and 5-year survival rates were 70%, 30% and 20%, respectively. Among the 4 patients that survived for >5 years, NHL occurred in patients 1 and 2 after 18 and 11 years of AIHA, respectively, and patients 19 and 20 had CLL/SLL, which is an inert lymphoma with a long survival period.

4 Discussion
Lymphomas frequently co-exist with AIHA, [2–4] with 20% of AIHA patients and 7% to 10% of lymphoma patients presenting the other disease. [2,3,11,12] Our cohort of 20 patients accounted, respectively, for 0.91% and 9.8% of the initially diagnosed NHL and AIHA patients. The lower incidence of AIHA/NHL in this cohort could be due to regional and lifestyle factors. Furthermore, AIHA patients often do not seek medical attention due to the mild symptoms, whereas the presence of both AIHA and NHL may make the patient despondent and unwilling to get treatment.
Although AIHA can occur with almost all types of NHLs, [2–4] our cohort mainly included patients with DLBCL, CLL/SLL, MZBL, AITL, MCL, ALCL and PTCL, with the highest incidents in AITL, MZBL, and BCL-U. To the best of our knowledge, this is the first report of AIHA incidence in each NHL subtype. Previous studies have reported AIHA in 5% to 10% CLL/SLL patients, and implicated it as one of the causes of CLL/SLL. [18–20] In our cohort however, AIHA was diagnosed in 3 of the 5 CLL/SLL patients only after multiple courses of chemotherapy, indicating that AIHA was probably the result of chemotherapy. Therefore, we surmise that unlike in Europe and USA where AIHA is often the cause of CLL, it is secondary to CLL/SLL treatment among Chinese patients with no prior history of the disease.
AIHA/NHL is significantly correlated to older median age, tumor stage IV, and multiple NHLs. [3,11] We further detected a 66.7% incidence of LBMI in AIHA/NHL patients, which could be due to the inherently high incidence of LBMI among these patients, simultaneous BMS and BMB that reduces missed diagnosis rate, and the tendency of patients to seek treatment only when their condition aggravates.
At present, PET/CT, BMS, and BMB are used to detect LBMI. PET/CT scan has high sensitivity, but insufficient specificity. In addition, BMB shows better diagnostic results compared to BMS. [21,22] Karak et al [21] proposed PET/CT scan to detect LBMI in DLBCL patients, followed by routine BMS if the scan is diffuse positive, BMB or BMS if it is positive, and neither if the scan is negative. Since only some patients in our cohort underwent PET/CT scans, we focused only on the diagnostic value of BMB and BMS, and observed inconsistent results across 10 patients with LBMI. This strongly suggests that the distribution of NHL lesions in AIHA/NHL patients is uneven, and BMB or BMS alone would result in a relatively higher missed diagnosis rate. Therefore, we recommend the method suggested by Karak et al if PET/CT scans are available; otherwise, BMB and BMS should be performed simultaneously to minimize missed diagnosis of LBMI. The latter approach is particularly suitable for economically underdeveloped areas.
The pathogenesis of AIHA/NHL is still unclear, [2,3,7,8] although recent studies have implicated chronic antigen stimulation and the formation of autoantibodies. [2,3] Drug-induced autoantibody formation is a major factor driving AIHA, [23–25] and likely involves perturbation in the different lymphocyte subtypes. [21–23] Rituximab induces AIHA by destroying the CD20 + B cells, and triggering the release of pro-inflammatory IL-6 and production of autoreactive plasma cells that are resistant to red blood cells. [23,24] Fludarabine mainly targets the CD4+ T cells, and promotes expansion of self-reactive T cells [25] .
The treatment of AIHA/NHL is incumbent on the initial diagnosis. If both are diagnosed at the same time, NHL treatment by chemotherapy and surgery can control the progression of both. [26–28] However, the therapeutic outcomes are at present unsatisfactory for AIHA/NHL patients, [29] and novel methods need to be explored. In our cohort, only 2 of the 7 patients that completed the chemotherapeutic regimen achieved CR. We believe that glucocorticoid administration can be considered for AIHA/NHL patients in the absence of any other options. It is important to devise more individualized chemotherapy regimens against NHL in these patients.
Our study had some limitations that should be addressed. First, 47 NHL patients could only be diagnosed as BCL rather than the exact NHL type, which may have affected the incidence of AIHA/NHL across the different types. Second, only 7 patients received standardized NHL treatment, which makes it impossible to determine the clinical outcome of AIHA/NHL.
5 Conclusions
AIHA can co-exist with various NHLs and the defining clinical characteristic of AIHA/NHL is the high incidence of LBMI. Simultaneous BMS and BMB are recommended to avoid missed diagnosis.
Author contributions
Data curation: Ji-cheng Zhou
Investigation: Zheng-mian Peng, Zhen-jie Bai Funding.
Acquisition: Mei-qing Wu, Wei-hua Zhao.
Methodology: Ji-cheng Zhou, Mei-qing Wu, Zhen-jie Bai.
Resources: Wei-hua Zhao, Zheng-mian Peng.
Software: Zhen-jie Bai.
Supervision: Ji-cheng Zhou.
Validation: Ji-cheng Zhou.
Visualization: Mei-qing Wu, Zhen-jie Bai, Weihua Zhao.
Writing – original draft: Ji-cheng Zhou.
Writing – review & editing: Ji-cheng Zhou.
Jicheng Zhou orcid: 0000-0003-3158-3811.
- Cited Here |
- Google Scholar
autoimmune hemolytic anemia; diagnosis; lymphoma bone marrow infiltration; non-Hodgkin lymphoma; treatment
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Assessment of quality of life and activities of daily living among elderly..., effect assessment of evidence-based nursing in combination with clinical..., nup93</em>: a care case report', 'zhao bo ms; chen, ji-yu ms; liao, ya-bin ms; li, yan-fang ms; jiang, xue-mei ms; bi, xin ms; yang, mi-feng ms; li, li md phd; cui, jing-jing ms', 'medicine', 'february 12, 2021', '100', '6' , 'p e24627');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link">steroid-resistant nephrotic syndrome in infants caused by a novel compound....
- Patient Care & Health Information
- Diseases & Conditions
- Non-Hodgkin's lymphoma
Parts of the immune system
The lymphatic system is part of the body's immune system, which protects against infection and disease. The lymphatic system includes the spleen, thymus, lymph nodes and lymph channels, as well as the tonsils and adenoids.
Non-Hodgkin's lymphoma is a type of cancer that begins in your lymphatic system, which is part of the body's germ-fighting immune system. In non-Hodgkin's lymphoma, white blood cells called lymphocytes grow abnormally and can form growths (tumors) throughout the body.
Non-Hodgkin's lymphoma is a general category of lymphoma. There are many subtypes that fall in this category. Diffuse large B-cell lymphoma and follicular lymphoma are among the most common subtypes. The other general category of lymphoma is Hodgkin's lymphoma.
Advances in diagnosis and treatment of non-Hodgkin's lymphoma have helped improve the prognosis for people with this disease.
Products & Services
- A Book: Living Medicine
- Mayo Clinic Comprehensive Cancer Center
- Chronic lymphocytic leukemia
- Cutaneous B-cell lymphoma
- Cutaneous T-cell lymphoma
- Follicular lymphoma
- Waldenstrom macroglobulinemia
Swollen lymph nodes
One of the most common places to find swollen lymph nodes is in the neck. The inset shows three swollen lymph nodes below the lower jaw.
Signs and symptoms of non-Hodgkin's lymphoma may include:
- Swollen lymph nodes in your neck, armpits or groin
- Abdominal pain or swelling
- Chest pain, coughing or trouble breathing
- Persistent fatigue
- Night sweats
- Unexplained weight loss
When to see a doctor
Make an appointment with your doctor if you have any persistent signs and symptoms that worry you.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get Mayo Clinic cancer expertise delivered to your inbox.
Subscribe for free and receive an in-depth guide to coping with cancer, plus helpful information on how to get a second opinion. You can unsubscribe at any time. Click here for an email preview.
Error Select a topic
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
Your in-depth coping with cancer guide will be in your inbox shortly. You will also receive emails from Mayo Clinic on the latest about cancer news, research, and care.
If you don’t receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
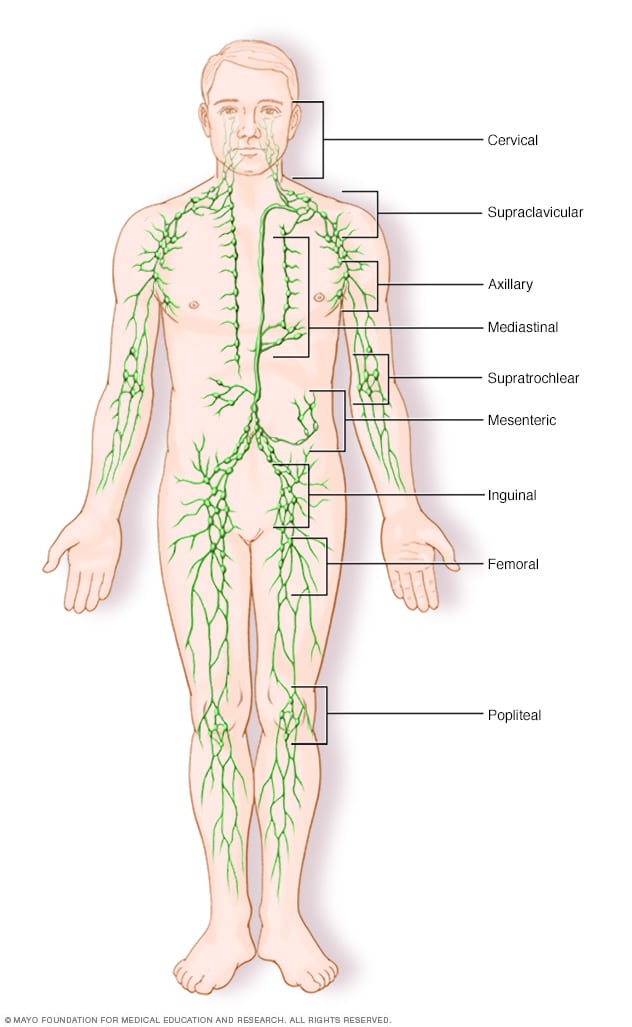
Lymph node clusters
Lymph nodes are bean-sized collections of cells called lymphocytes. Hundreds of these nodes cluster throughout the lymphatic system, for example, near the knee, groin, neck and armpits. The nodes are connected by a network of lymphatic vessels.
In most instances, doctors don't know what causes non-Hodgkin's lymphoma. It begins when your body produces too many abnormal lymphocytes, which are a type of white blood cell.
Normally, lymphocytes go through a predictable life cycle. Old lymphocytes die, and your body creates new ones to replace them. In non-Hodgkin's lymphoma, your lymphocytes don't die, and your body keeps creating new ones. This oversupply of lymphocytes crowds into your lymph nodes, causing them to swell.
B cells and T cells
Non-Hodgkin's lymphoma most often begins in the:
- B cells. B cells are a type of lymphocyte that fights infection by producing antibodies to neutralize foreign invaders. Most non-Hodgkin's lymphoma arises from B cells. Subtypes of non-Hodgkin's lymphoma that involve B cells include diffuse large B-cell lymphoma, follicular lymphoma, mantle cell lymphoma and Burkitt lymphoma.
- T cells. T cells are a type of lymphocyte that's involved in killing foreign invaders directly. Non-Hodgkin's lymphoma occurs much less often in T cells. Subtypes of non-Hodgkin's lymphoma that involve T cells include peripheral T-cell lymphoma and cutaneous T-cell lymphoma.
Whether your non-Hodgkin's lymphoma arises from your B cells or T cells helps to determine your treatment options.
Where non-Hodgkin's lymphoma occurs
Non-Hodgkin's lymphoma generally involves the presence of cancerous lymphocytes in your lymph nodes. But the disease can also spread to other parts of your lymphatic system. These include the lymphatic vessels, tonsils, adenoids, spleen, thymus and bone marrow. Occasionally, non-Hodgkin's lymphoma involves organs outside of your lymphatic system.
Risk factors
Most people diagnosed with non-Hodgkin's lymphoma don't have any obvious risk factors. And many people who have risk factors for the disease never develop it.
Some factors that may increase the risk of non-Hodgkin's lymphoma include:
- Medications that suppress your immune system. If you've had an organ transplant and take medicines that control your immune system, you might have an increased risk of non-Hodgkin's lymphoma.
- Infection with certain viruses and bacteria. Certain viral and bacterial infections appear to increase the risk of non-Hodgkin's lymphoma. Viruses linked to this type of cancer include HIV and Epstein-Barr infection. Bacteria linked to non-Hodgkin's lymphoma include the ulcer-causing Helicobacter pylori.
- Chemicals. Certain chemicals, such as those used to kill insects and weeds, may increase your risk of developing non-Hodgkin's lymphoma. More research is needed to understand the possible link between pesticides and the development of non-Hodgkin's lymphoma.
- Older age. Non-Hodgkin's lymphoma can occur at any age, but the risk increases with age. It's most common in people 60 or over.
Non-Hodgkin's lymphoma care at Mayo Clinic
Living with non-hodgkin's lymphoma?
Connect with others like you for support and answers to your questions in the Blood Cancers & Disorders support group on Mayo Clinic Connect, a patient community.
Blood Cancers & Disorders Discussions

49 Replies Sat, Jun 08, 2024
107 Replies Fri, Jun 07, 2024

90 Replies Wed, Jun 05, 2024
- AskMayoExpert. Diffuse large B-cell lymphoma (adult). Mayo Clinic; 2018.
- B-cell lymphomas. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Feb. 5, 2021.
- T-cell lymphomas. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Feb. 5, 2021.
- Hoffman R, et al. Diagnosis and treatment of diffuse large B-cell lymphoma and Burkitt lymphoma. In: Hematology: Basic Principles and Practice. 7th ed. Elsevier; 2018. https://www.clinicalkey.com. Accessed Feb. 5, 2021.
- Lymphoma — Non-Hodgkin. Cancer.Net. https://www.cancer.net/cancer-types/41246/view-all. Accessed Feb. 11, 2021.
- Laurent C, et al. Impact of expert pathologic review of lymphoma diagnosis: Study of patients from the French Lymphopath Network. Journal of Clinical Oncology. 2017; doi:10.1200/JCO.2016.71.2083.
- Distress management. National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed Feb. 11, 2021.
- Nowakowski GS, et al. Integrating precision medicine through evaluation of cell of origin treatment planning for diffuse large B-cell lymphoma. Blood Cancer Journal. 2019; doi:10.1038/s41408-019-0208-6.
- Lymphoma SPOREs. National Cancer Institute. https://trp.cancer.gov/spores/lymphoma.htm. Accessed Feb. 11, 2021.
- Warner KJ. Allscripts EPSi. Mayo Clinic. Jan. 7, 2021.
- Member institutions. Alliance for Clinical Trials in Oncology. https://www.allianceforclinicaltrialsinoncology.org/main/public/standard.xhtml?path=%2FPublic%2FInstitutions. Accessed Feb. 11, 2021.
- Member institution lists. NRG Oncology. https://www.nrgoncology.org/About-Us/Membership/Member-Institution-Lists. Accessed Feb. 11, 2021.
- Pruthi RK (expert opinion). Mayo Clinic. Feb. 22, 2021.
Associated Procedures
- Bone marrow biopsy
- Bone marrow transplant
- Chemotherapy
- Positron emission tomography scan
- Radiation therapy
News from Mayo Clinic
- All-Star pitcher Liam Hendriks shares how he closed out cancer at Mayo Clinic in Arizona July 21, 2023, 10:08 p.m. CDT
- Mayo Clinic Q and A: What is lymphoma? Nov. 03, 2022, 01:04 p.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Jacksonville, Florida, and Mayo Clinic in Phoenix/Scottsdale, Arizona, have been recognized among the top Cancer hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
We’re transforming healthcare
Make a gift now and help create new and better solutions for more than 1.3 million patients who turn to Mayo Clinic each year.
Hodgkin’s Lymphoma Stories

What is Hodgkin’s lymphoma? Also known as Hodgkin’s Disease, Hodgkin’s lymphoma is a disease in which malignant (cancer) cells form in the lymph system. It may then spread to the liver, lungs, or bone marrow.
Some of the most common first symptoms of Hodgkin’s lymphoma can include:
- Swelling of the lymph nodes (painless), often in the neck, armpits, or groin area
- Fever and chills
- Night sweats
- Weight loss
- Loss of appetite
For an overview of Hodgkin’s lymphoma, check out our Hodgkin’s lymphoma 101 page.
Nodular Lymphocyte Predominant
Hodgkin’s lymphoma patient stories.
Our community members dive deeper into their cancer stories than any others, sharing their first symptoms, different treatment paths and side effects, and reflections on the entire experience. Choose stories based on subtypes below.
A form of blood cancer that develops when lymphocytes, a type of white blood cell, grow out of control.

A form of slow-growing blood cancer that form predominantly in lymph nodes as a result of abnormal growth of B lymphocytes.
No post found
Hodgkin’s Lymphoma Resources
Patient Self-Advocacy: A Conversation on Speaking Up for Ourselves Four incredible Hodgkin lymphoma patients/survivors share how they were able to advocate for themselves throughout their cancer care.
The Latest in Hodgkin Lymphoma with Dr. Matthew Matasar: Dr. Matthew Matasar with Rutgers Cancer Institute discusses emerging and most-promising therapy options for relapsed/refractory Hodgkin lymphoma patients and those newly-diagnosed.
Looking for non-Hodgkin’s lymphoma stories and resources? Visit the non-Hodgkin’s lymphoma stories page.
Hodgkin’s Lymphoma Oncologists & Experts
Read interviews from medical experts who specialize in blood cancers including Hodgkin’s lymphoma.

Navigating Life With Cancer

Reacting to a Cancer Diagnosis

What Does Cancer Feel Like?

Cancer Patient Advocate

What to Say to Someone With Cancer | The Patient Story

How To Tell Your Family and Friends You Have Cancer

My Spouse Was Diagnosed With Cancer | The Patient Story
Join our community.
Get the latest cancer stories, helpful resources, and personalized advice directly to your inbox.
Copyright 2024 © The Patient Story
For cancer patients and caregivers.
Quick Links
Additional Links
CASE REPORT article
A case report of a female patient with hodgkin lymphoma localized in the central nervous system and with concomitant pulmonary lymphomatoid granulomatosis.

- 1 Chair and Department of Neurosurgery and Paediatric Neurosurgery, Medical University of Lublin, Lublin, Poland
- 2 Chair and Department of Clinical Pathomorphology, Medical University of Lublin, Lublin, Poland
- 3 Chair and Department of Haematooncology and Bone Marrow Transplantation, Medical University of Lublin, Lublin, Poland
- 4 Department of Clinical Transplantology, Medical University of Lublin, Lublin, Poland
The involvement of the central nervous system (CNS) in Hodgkin lymphoma (HL) has been rarely reported, especially in its primary isolated form. Herein, we present a case of a 33-year-old woman, who received immunosuppressive treatment due to ulcerative colitis (at the beginning azathioprine and sulfasalazine, changed to mesalazine), with repetitive episodes of loss of consciousness for a few weeks and with no other symptoms. Magnetic resonance imaging scans of the head revealed a tumor in the lateral part of the left temporal lobe and in the cerebellum. Moreover, a subsequent computed tomographic scan of the chest revealed diffuse tumorous lesions in the lungs. The brain tumor was resected and a tumorous lesion resected from the lungs was biopsied. The histopathological analysis confirmed the final diagnosis of HL localized in the CNS with concomitant pulmonary lymphomatoid granulomatosis (LYG) grade 1. After the patient underwent radiotherapy and chemotherapy, the patient showed complete regression of lesions in the CNS and lungs, which was confirmed by positron emission tomographic scan. LYG and CNS-HL are rare proliferative disease derived from lymphocytes B and associated with EBV infections. An association between LYG and other autoimmune disorders has been reported, but to the best of our knowledge, this is the first case of the CNS-HL associated with lymphatoid granulomatosis.
Introduction
The involvement of the CNS in neoplastic lesions of the lymphatic system is most commonly observed in the case of non-Hodgkin lymphoma (NHL). HL localized in the central nervous system (CNS-HL) has been rarely reported, especially in its primary isolated form ( 1 ). It is a specific clinical case to observe the concomitant existence of another rare lymphoproliferative process, such as pulmonary lymphomatoid granulomatosis (LYG). To the best of our knowledge, this is the first case of the CNS-HL associated with lymphatoid granulomatosis.
Case Presentation
A 33-year-old female patient was admitted to the Department of Neurosurgery in September 2013 due to repetitive episodes of loss of consciousness for a few weeks. The patient reported no other symptoms. For the past 6 years, she was on immunosuppressive treatment due to ulcerative colitis (at the beginning azathioprine and sulfasalazine (2 years), and next mesalazine). The magnetic resonance imaging (MRI) scans of the head revealed the tumor present in the lateral part of the left temporal lobe and the cerebellum ( Figure 1 ). After the total resection of the tumor, the samples were histopathologically evaluated. At the same time, a computed tomographic (CT) scan revealed diffuse tumorous lesions in the lungs. After resection, a biopsy was performed on one of the lesions.
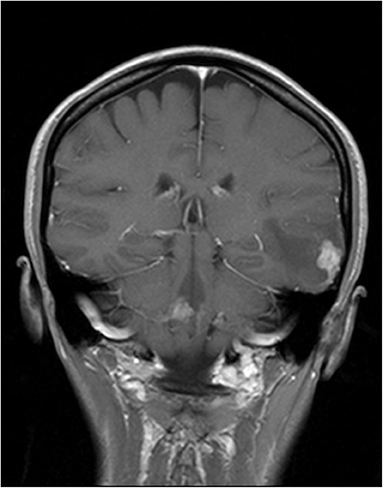
Figure 1 . Tumor in the lateral part of the left temporal lobe and the cerebellum in magnetic resonance imaging (MRI) scans.
Frozen section of the lesion resected from the right lung was examined (No 18502/13). The specimen was measuring 4.5 × 2.5 × 1.5 cm in size, which showed the presence of whitish-gray nodules. The cross-section of the specimen revealed irregular and slightly brown infiltration. On microscopic examination, the specimen revealed bronchopneumonia with focal necrosis and fibrosis of the lung, which raised the suspicion of lymphoma. However, on further evaluation of the formalin-fixed paraffin-embedded sections, we observed many irregular necrotic areas, as well as fibrinous exudate with many macrophages and a few neutrophils in the alveoli ( Figures 2A–C ). We also observed sparse giant multinucleated cells, lymphocytic infiltration around the blood vessel, and necrotic areas together with focal fibrosis. In some blood vessels, thrombi including organized ones were also revealed. Additional staining methods, namely, van Gieson, Warthin–Starry, and azan were performed. Necrotizing pneumonia was ultimately diagnosed.
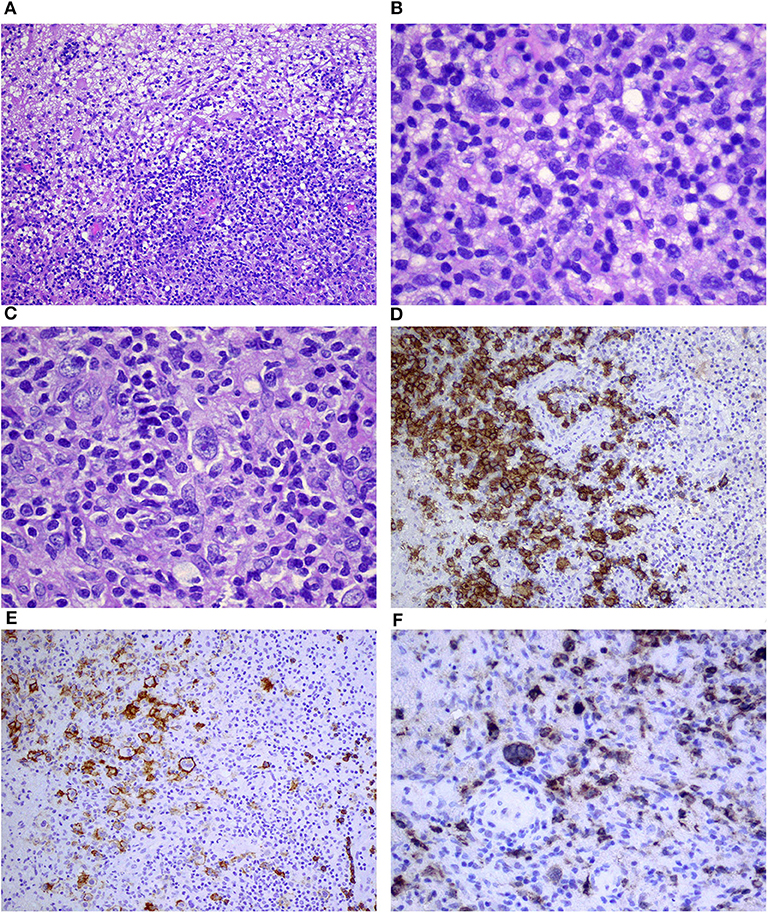
Figure 2 . Necrotic area of the lung surrounded by atypical lymphoid cells (A,B) ; dense lymphocytic infiltration of the wall of the blood vessel (C) ; and positive immunostaining for CD20 (D) , CD30 (E) , and EBV/LMP1 (F) corresponding to grade 1 lymphomatoid granulomatosis (magnification A –10×; B,D–F –20×; C –40×).
Samples obtained from the posterior part of the left temporal lobe of the brain (No: 13727) were small grayish and around 0.5–1 cm in size. On microscopic examination, multiple focal points of infiltrations composed mainly of small T cells (CD3+) and macrophages (CD68+) with dispersed giant cells of Reed–Sternberg morphology were observed ( Figures 3A–C ). The following immunophenotype of the aforementioned cells were revealed: CD45 (+, weaker than in T cells), CD30 (+, strong cytoplasmic and membranous), CD15 (+/–, weak cytoplasmic and in Golgi system in some cells), PAX5 (+, slightly weaker than in B cells), CD20 (+, membranous, weaker than in B cells), OCT (+/–, strong nuclear on the majority of the cells), BOB1 (–/+, trace in single cells), CD10 (–), Bcl6 (–), ALK1 (–), CD3 (–), S100 (–), and CD1a (–). Prognostic markers on Hodgkin and Reed–Sternberg (HRS) cells were as follows: Bcl2 (+, cytoplasmic, weaker than T cells), Ki67 (+, strong in almost all HRS cells), and CD68 (+++) in many concomitant macrophages (category 3) ( Figures 3D,E ). Classical Hodgkin lymphoma (cHL) of the CNS, mixed cellularity subtype (MCcHL) was diagnosed.
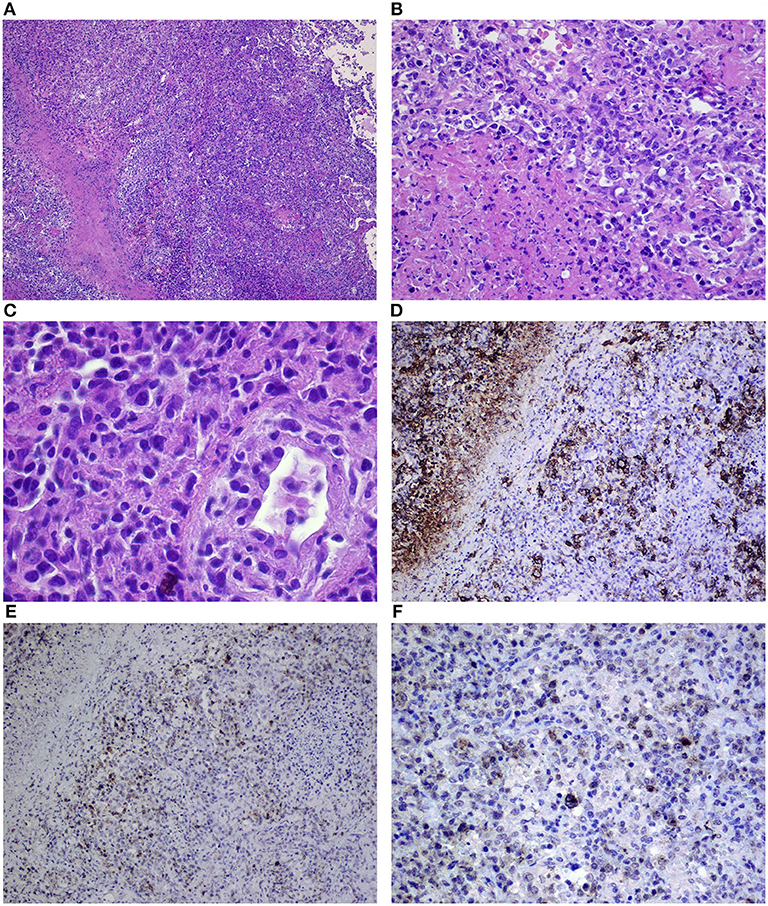
Figure 3 . Dense infiltration of the brain composed of Reed–Sternberg cells, small lymphocytes, and macrophages (A–C) corresponding to the classical Hodgkin lymphoma of the central nervous system, mixed cellularity (MCcHL), and positive immunostaining for CD30 (D) , CD20 (E) , and EBV/LMP1 (F) in Reed–Sternberg cells (objective magnification A –10×; B,C –40×; D–F –20×).
The samples from the brain were consulted and the diagnosis was confirmed. Correlation between the reactivation of Epstein-Barr virus (EBV) with the positive EBV/LMP1 immunostaining was emphasized ( Figure 3F ). Subsequently, the samples from the lung were reevaluated. A few slightly larger B cells (CD20+, CD30+, CD15–, and EBV/LMP1+) admixed with T cells (CD3+) were found ( Figures 2D–F ). The final diagnosis was changed to grade 1 LYG with lung involvement. In trephine biopsy (No: 30601/13) lymphomatous infiltration of the bone marrow was not observed.
Evaluation of the cerebrospinal fluid showed no abnormalities. The patient was HIV negative. The following systemic polychemotherapy was introduced: BEACOPP+ DepoCyte ® 2 courses), radiotherapy (30 Gy), and CHOP (2 courses). Subsequently, complete regression of lesions in the CNS and lungs was confirmed by a positron emission tomographic (PET) scan.
CNS-HL is estimated in only 0.02% of the patients with the systemic form of the disease ( 1 ). It usually takes place either already when stating the diagnosis, or on recurrence or progression of HL ( 2 ). The isolated form of CNS-HL is only reported in the literature as single cases ( 3 ). One of the most complex reports on all primary CNS-HL cases between 1980 and 2013 is the report published by Kresak et al. ( 4 ). The authors showed no correlation between CNS-HL and specific CNS location or neurological symptoms. In six out of seven patients, EBV infection was proven (no such tests were performed in the other nine patients), based on the diagnosis made by histopathological evaluation of the tissue sample and in few cases, by the evaluation of cerebrospinal fluid. Radiotherapy after resection of the lymphoma was the most common treatment modality (12/16 cases) ( 4 ).
Complete resection of the lymphoma was performed and subsequently cytostatic treatment and radiotherapy were administered to the patient. It is noteworthy that complete resection of the lymphoma as a therapeutic modality for primary NHL is controversial and has been rarely performed. The most commonly performed neurosurgical procedure is limited to stereotactic biopsy as a part of the diagnostic process. One of the many arguments that question the relevance of radical surgical procedure is the conclusion of post mortem examinations. These examinations proved leukemic infiltration even in normal brain tissue (whole-brain disease) ( 5 ).
However, so far, there is no data related to the involvement of CNS in HL. The radiological picture of CNS-HL is commonly uncharacteristic. It may sometimes resemble ischemic or inflammatory lesions or even other tumors (i.e., meningioma, glioblastomas, or metastases) ( 6 , 7 ). CNS involvement in HL tends to have less mass effect and edema. In addition, necrosis, hemorrhage, and calcification are rare in these cases ( 7 ). In differentiating other changes in the brain, you can consider expanding diagnostics with single-photon emission computed tomography (SPECT), MR spectroscopy (MRS), or perfusion MRI ( 8 ).
The mechanism that leads to the involvement of CNS in HL is unknown. In the case of coexistence of a systemic disease, a direct transition of neoplastic process from surrounding skull bones or hematogenous dissemination has been suggested ( 9 ). However, large-sized Reed–Sternberg cells effectively restrict their transition into the perivascular spaces of the CNS, which prevents the formation of CNS-HL ( 10 ).
According to the literature, the isolated form of CNS-HL is associated with a better prognosis than that of CNS-HL in the phase of recurrence or HL progression ( 4 ). LYG is a rare proliferative disease derived from lymphocytes B and is associated with EBV infections ( 11 ). It has been most commonly described for the lungs (about 90% of all the cases), followed by the skin (25–50%) and CNS (25–35%). The involvement of lymph nodes, spleen, or bone marrow has been described in the advanced stages of the disease ( 12 ).
An association between LYG and other autoimmune disorders (e.g., Sjogren's syndrome, rheumatoid arthritis, sarcoidosis, and ulcerative colitis), as well as congenital or acquired immunodeficiencies, has been reported. Patients with pulmonary form of LYG usually complain of numerous symptoms (shortness of breath, cough, and chest pain); however, sometimes the diagnosis may be stated when evaluating the lungs due to other reasons (like in our patient). The radiological picture usually shows numerous nodules of different sizes in both lungs ( 13 ).
LYG is an angiocentric and angiodestructive process with the presence of large B cells (EBV+) in the infiltrated tissues. They show the expression of CD20, variably CD30, and no expression of CD15, which leads us to exclude HL. Numerous reactive T cells are characteristic in LYG ( 13 ). In addition, LYG is characterized by foci of necrosis associated with angiogenic ischemic processes. It is thought to be caused by the direct infiltration of blood vessels by T cells. Chemokines IP-10 and Mig induced by EBV have also been suggested to play a role in the aforementioned process ( 14 ). The clinical course of LYG is varied and the method of treatment mainly depends on the stage that is based on the number of atypical EBV+ B cells. Some patients show spontaneous remission or no progression for a long time. However, in the case of an advanced stage of LYG, chemotherapy is required (e.g., CHOP, ICE, or hyperCVAD) in combination with the administration of monoclonal antibodies, anti-CD20 ( 13 ).
In this study, cells with the expression of latent membrane protein 1 (LMP-1; viral protein responsible for oncogenesis) were detected in the tissue samples obtained from the CNS lesion and lungs of the patient. This proves a significant role of EBV in the development of CNS-HL and pulmonary LYG in the presented patient.
LMP-1 is an integral cell membrane protein whose role is to protect infected lymphocytes from apoptosis through the increased expression of some anti-apoptotic genes, such as Bcl-2, Mcl-1, and A20. However, we still do not know why two separate lymphoproliferative processes, triggered most probably by the same factor, developed at the same time in the same patient. The influence of EBV on the expression of receptor proteins, signaling, maturation, and differentiation of the infected cell present only a part of the issues, which requires further investigation ( 14 ).
The lungs, liver, and bone marrow are among the non-lymphatic organs most commonly affected by HL ( 15 ). In the case of diagnosis of HL based on histopathological examination of the lymph node, sometimes changes in the lung are not usually verified (they are thought to be related to HL). It is worth to consider the legitimacy of histopathological assessment in the absence of response to standard HL chemotherapy. It may turn out that the coincidence of HL and LYG occurs more often than it may seem, which would thus allow an in-depth explanation of the etiopathogenesis of the simultaneous occurrence of both conditions. It is very difficult to interpret considering that one case has been described so far ( 16 – 18 ). It is significant, that the MC subtype of HL is the most associated with EBV infection ( 19 ) (such as was present in our patient). There is also indicated impact of immune disorders (e.g., prior immunosuppression) on the development of both disease processes ( 20 ).
The diagnostic process for both the CNS and lung in the patient's work required detailed and complicated diagnostics. In the lungs, the possibility of tuberculosis or other inflammatory processes that excluded intensive chemotherapy could be considered. The simultaneous occurrence of HL and tuberculosis has already been described in the literature ( 16 – 18 ). Jehanno et al. addressed the diagnostic problems of possible coincidence of both conditions using the PET/CT imaging technique ( 21 ). These data indicate the important, clinically important importance of the description of this case.
Ethics Statement
This study was approved by the Ethics Committee of the Medical University of Lublin (KE No. 0254/159/2014). Study was performed in accordance with the ethical standards of the Declaration of Helsinki. There was no additional invasive test or experimental drugs used out of order for the patient. Written informed consent was obtained from the patient for participation and publication of this case report.
Author Contributions
DS, EW-S, JS, FS, ASzy, BJ, ASzc, MH, and TT was responsible for the data collection and analysis, interpreted the results, and contributed to manuscript writing. TT, DS, and EW-S contributed to the interpretation of the data and critical revision of the manuscript for important intellectual content. DS and EW-S designed the study. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Re D, Fuchs M, Schober T, Engert A, Diehl V. CNS involvement of Hodgkin's lymphoma. J Clin Oncol. (2007) 25:3182. doi: 10.1200/JCO.2007.12.5088
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Galan L, Sanchez AC, Cantos B, Provencio M. Central nervous system involvement in Hodgkin's lymphoma. Med Oncol. (2011) 28:505–8. doi: 10.1007/s12032-010-9692-z
3. Sharaf N, Lobo B, Lee J, Prayson RA. Primary Hodgkin lymphoma of the central nervous system. J Clin Neurosci. (2014) 21:1271–3. doi: 10.1016/j.jocn.2013.10.034
4. Kresak JL, Nguyen J, Wong K, Davis R. Primary Hodgkin lymphoma of the central nervous system: two case reports and review of the literature. Neuropathology. (2013) 33:658–62. doi: 10.1111/neup.12035
5. Onda K, Wakabayashi K, Tanaka R, Takahashi H. Intracranial malignant lymphomas: clinicopathological study of 26 autopsy cases. Brain Tumor Pathol. (1999) 16:29–35. doi: 10.1007/BF02478899
6. Gessi M, Kuchelmeister K, Kellner U, Ritter M, Morgner A, Urbach H, et al. Unusual clinico-pathological features in primary Hodgkin's lymphomas of the central nervous system. Acta Neurochir. (2013) 155:19–24. doi: 10.1007/s00701-012-1535-6
7. Gómez Roselló E, Quiles Granado AM, Laguillo Sala G, Pedraza Gutiérrez S. Primary central nervous system lymphoma in immunocompetent patients: spectrum of findings and differential characteristics. Radiologia. (2018) 60:280–9. doi: 10.1016/j.rxeng.2018.04.003
CrossRef Full Text | Google Scholar
8. Tang YZ, Booth TC, Bhogal P. Imaging of primary central nervous system lymphma. Clin Radiol. (2011) 66:768–77. doi: 10.1016/j.crad.2011.03.006
9. Grimm S, Chamberlain M. Hodgkin's lymphoma: a review of neurologic complications. Adv Hematol . (2011) 2011:624578. doi: 10.1155/2011/624578
10. Morawa E, Ragam A, Sirota R, Nabhan C. Hodgkin's lymphoma involving the CNS. J Clin Oncol. (2007) 25:1437–8. doi: 10.1200/JCO.2006.10.1691
11. Pittaluga S, Wilson WH, Jaffe ES. Lymphomatoidgranulomatosis. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, editors. World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues , 4th ed. Lyon: IARC (2008). p. 247–9.
Google Scholar
12. Castrale C, El Haggan W, Chapon F, Reman O, Lobbedez T, Ryckelynck JP, et al. Lymphomatoid granulomatosis treated successfully with rituximab in a renal transplant patient. J Transplant . (2011) 2011:865957. doi: 10.1155/2011/865957
13. Roschewski M, Wilson WH. Lymphomatoid granulomatosis. Cancer J. (2012) 18:469–74. doi: 10.1097/PPO.0b013e31826c5e19
14. Jaffe ES, Wilson WH. Lymphomatoid granulomatosis: pathogenesis, pathology and clinical implications. Cancer Surv. (1997) 30:233–48.
PubMed Abstract | Google Scholar
15. Ansell SM. Hodgkin lymphoma: 2016 update on diagnosis, risk-stratification, and management. Am J Hematol. (2016) 91:434–42. doi: 10.1002/ajh.24272
16. Centkowski P, Sawczuk-Chabin J, Prochorec M, Warzocha K. Hodgkin's lymphoma and tuberculosis coexistence in cervical lymph nodes. Leuk Lymphoma. (2005) 46:471–5. doi: 10.1080/10428190400019891
17. Wang Q, Chen E, Cai Y, Zhang X, Li Q, Zhang X. A case report: systemic lymph node tuberculosis mimicking lymphoma on 18F-FDG PET/CT. Medicine. (2016) 95:e2912. doi: 10.1097/MD.0000000000002912
18. Chen Y, Shen CH, Kao CH. Abnormal FDG PET imaging in tuberculosis appearing like lymphoma. Clin Nucl Med. (2004) 29:124. doi: 10.1097/01.rlu.0000109300.89514.35
19. Piris MA, Medeiros LF, Chang KC. Hodgkin lymphoma: a review of pathological features and recent advances in pathogenesis. Pathology. (2020) 52:154–65. doi: 10.1016/j.pathol.2019.09.005
20. Melani C, Jaffe ES, Wilson WH. Pathobiology and treatment lymphoid granulomatosis, a rare EBV-deriven disorder. Blood. (2020) 135:1344–52. doi: 10.1182/blood.2019000933
21. Jehanno N, Cassou-Mounat T, Vincent-Salomon A, Luporsi M, Bedoui M, Kuhnowski F. PET/CT imaging in management of concomitant Hodgkin lymphoma and tuberculosis – a problem solver tool. Clin Case Rep. (2018) 6:232–4. doi: 10.1002/ccr3.1248
Keywords: primary Hodgkin lymphoma, lymphoma of the central nervous system, pulmonary lymphomatoid granulomatosis, Epstein-Barr virus, latent membrane protein 1
Citation: Szczepanek D, Szumiło J, Stoma F, Szymczyk A, Jarosz B, Szczepanek A, Hus M, Trojanowski T and Wasik-Szczepanek E (2020) A Case Report of a Female Patient With Hodgkin Lymphoma Localized in the Central Nervous System and With Concomitant Pulmonary Lymphomatoid Granulomatosis. Front. Neurol. 11:963. doi: 10.3389/fneur.2020.00963
Received: 02 December 2018; Accepted: 24 July 2020; Published: 08 September 2020.
Reviewed by:
Copyright © 2020 Szczepanek, Szumiło, Stoma, Szymczyk, Jarosz, Szczepanek, Hus, Trojanowski and Wasik-Szczepanek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Agnieszka Szymczyk, agnieszka.szymczyk.med@wp.pl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Advances in Lymphoma Research
Artist’s rendering of T cells (red and blue spheres) attacking cancer cells. T-cell therapy has been effective in treating certain lymphoma patients.
NCI-funded researchers are working to advance our understanding of how to treat lymphoma . All lymphomas start in the cells of the lymph system , which is part of the body’s immune system. Lymphomas are grouped into two main types: Hodgkin lymphoma and non-Hodgkin lymphoma (sometimes called NHL). But more than 70 different subtypes of the disease exist. Advances in understanding the gene changes that can lead to lymphoma are now helping scientists design more personalized treatments for these subtypes.
This page highlights some of the latest lymphoma research, including clinical advances that may soon translate into improved care and research findings from recent studies.
Treatment of Non-Hodgkin Lymphoma (NHL)
Most people diagnosed with lymphoma have a subtype of non-Hodgkin lymphoma. Non-Hodgkin lymphoma can either be aggressive or indolent .
Aggressive non-Hodgkin lymphoma grows and spreads quickly and usually requires immediate treatment. With modern treatment regimens, almost 70% of people with aggressive non-Hodgkin lymphoma will be considered cured. Research is now largely focused on finding better treatments for the minority of people with aggressive lymphoma who are not cured with initial therapy.
Indolent non-Hodgkin lymphoma grows slowly, and in some cases may not cause symptoms for years. People with indolent disease can often postpone treatment until their symptoms worsen, with no negative effects on survival. But sometimes an indolent lymphoma can turn into aggressive lymphoma, which requires immediate treatment.
Indolent non-Hodgkin lymphoma largely cannot be cured. The past two decades have seen improvements in extending the survival of people who are treated for this type of lymphoma. However, researchers are studying how to improve long-term survival further and working toward potentially curative treatments.
Chemotherapy , radiation therapy , targeted therapy , and immunotherapy are all used in the treatment of non-Hodgkin lymphoma. A stem cell transplant is sometimes used for lymphoma that has recurred, but this procedure has serious side effects. Four CAR T-cell therapies have been approved to treat some types of recurrent lymphoma. However, these newer therapies still can't cure many people with recurrent lymphoma.
Most research on treatment for non-Hodgkin lymphoma is now focused on targeted therapy and immunotherapy. Researchers are also trying to identify gene changes in different types of lymphoma that might be targets for new drug development.
For example, in 2018, a study led by NCI researchers identified genetic subtypes of diffuse large B-cell lymphoma (the most common type of non-Hodgkin lymphoma) that could help explain why some patients with the disease respond to treatment and others don’t. Further studies may lead to more tailored treatments for patients with this type of lymphoma.
New targeted therapies
A signaling pathway is a series of chemical reactions that control one or more cell functions. Many types of non-Hodgkin lymphoma are driven by a signaling pathway called the B-cell receptor signaling pathway. A drug called ibrutinib (Imbruvica) has been developed to shut down that pathway. It is being used and tested in a number of ways:
- In the last several years, the drug has been approved for the treatment of small lymphocytic lymphoma and Waldenstrom macroglobulinemia , both indolent non-Hodgkin lymphomas.
- NCI took part in a randomized clinical trial that tested the addition of ibrutinib to chemotherapy and rituximab (Rituxan) in people newly diagnosed with a certain type of diffuse large B-cell lymphoma . People over the age of 60 had worse outcomes with the addition of ibrutinib. However, patients under the age of 60 who were given ibrutinib had substantially improved survival .
- Other studies have suggested that people whose diffuse large B-cell lymphoma has specific genetic characteristics may especially benefit from treatment with ibrutinib .
- An early-phase NCI-sponsored study tested ibrutinib plus chemotherapy in people with primary central nervous system lymphoma , a very aggressive subtype of non-Hodgkin lymphoma. More than half of the patients in this small study went into complete, long-term remission. A larger study is now underway at the National Institutes of Health (NIH) Clinical Center . That study is also testing this combination in people with lymphoma that began elsewhere in the body but has spread to the central nervous system.
The FDA has approved two other drugs that target the B-cell receptor signaling pathway. Acalabrutinib (Calquence) is approved for relapsed mantle cell lymphoma and small lymphocytic lymphoma . An ongoing study at NCI is testing acalabrutinib, in combination with chemotherapy and rituximab , in people with previously untreated diffuse large B-cell lymphoma.
In 2019, zanubrutinib (Brukinsa) was approved for relapsed mantle cell lymphoma. A fourth drug targeting the B-cell receptor signaling pathway, called pirtobrutinib (Jaypirca) , is now being tested in clinical trials for several different types of non-Hodgkin lymphoma. In 2023, it was approved for the treatment of mantle cell lymphoma that has gotten worse after two or more previous treatments.
Many other targeted therapies are being tested in non-Hodgkin lymphoma. Some that are approved for specific subtypes are listed below.
- Polatuzumab vedotin (Polivy) for the treatment of diffuse large B-cell lymphoma . Clinical trials are testing this drug and related drugs for other types of non-Hodgkin lymphoma.
- Venetoclax (Venclexta) for chronic lymphocytic leukemia and small lymphocytic lymphoma.
- Loncastuximab (Zynlonta) for large B-cell lymphoma that has recurred or did not shrink after other treatments .
- Selinexor (Xpovio) for large B-cell lymphoma that has recurred or did not shrink after other treatments .
- The combination of tafasitamab (Monjuvi) and lenalidomide (Revlimid) for people with large B-cell lymphoma who cannot undergo a stem cell transplant .
- Tazemetostat (Tazverik) for some people with follicular lymphoma that has recurred or did not shrink after other treatments .
However, in lymphoma, resistance to a single agent can occur quickly. Researchers are now testing combinations of targeted therapies to treat non-Hodgkin lymphoma to try to overcome this resistance. For example, ongoing trials led by NCI researchers are testing a five-drug regimen and a six-drug regimen in people with aggressive or indolent B-cell lymphomas whose cancer has relapsed or is resistant to treatment.
Researchers are also trying to make standard treatment regimens less toxic for older patients. In one study, NCI researchers found that the intensity of standard chemotherapy could be reduced in older adults with Burkitt lymphoma , an aggressive type of non-Hodgkin lymphoma, without compromising the potential for a cure.
Immunotherapy
Immunotherapy uses substances to stimulate or suppress the immune system to help the body fight cancer. Several immunotherapies have shown promise in treating different types of lymphoma.
CAR T cells. CAR T cells are a type of immunotherapy in which a patient's T cells, a type of immune cell, are changed in the laboratory so they will better attack cancer cells. Four CAR T-cell therapies have been approved for the treatment of non-Hodgkin lymphoma:
- Axicabtagene ciloleucel (Yescarta) for people with large B-cell lymphoma or follicular lymphoma whose cancer has progressed after receiving one prior treatment regimen.
- Tisagenlecleucel (Kymriah) for adults with one of three types of non-Hodgkin lymphoma .
- Lisocabtagene maraleucel (Breyanzi) for people with some types of B-cell non-Hodgkin lymphoma that has relapsed or has not gotten better after at least two other treatments.
- Brexucabtagene autoleucel (Tecartus) for some people with mantle cell lymphoma that has come back or did not get better with other treatments.
To date, CAR T cells have provided long-term remissions for about one third of adults with aggressive lymphoma who receive them. Large randomized trials have been comparing CAR T-cell therapy to autologous stem cell transplantation at first relapse. In one of these trials, more people who received the CAR T-cell therapy were alive four years after treatment compared with those who received chemotherapy followed by stem cell transplantation. Participants in the other trials are still being followed to see if differences in survival emerge over time.
A phase 2 trial tested CAR T cells as initial therapy in people at very high risk of relapse. In early results, over three-quarters of patients had their cancer go into remission. However, long term results are not yet available and CAR T cells are not FDA approved in this setting.
CAR T cells are also being tested in other lymphoma subtypes, both aggressive and indolent, as well as in patients with lymphoma that has spread to the central nervous system.
Immunomodulating drugs . Immunomodulators are drugs that either stimulate or suppress the immune system. One such drug, lenalidomide (Revlimid) , has been approved in combination with targeted therapies for previously treated follicular lymphoma and marginal zone lymphoma . It is also often used to treat diffuse large B-cell lymphoma.
Novel immunotherapies . Researchers are also testing novel ways to stimulate the immune system to fight lymphoma. In 2018, a small trial showed that combining radiation therapy with the injection of a compound that stimulates the immune system could shrink some indolent B-cell lymphomas. In 2019, a trial that used a vaccine to draw immune cells into tumors in people with indolent non-Hodgkin lymphoma also showed promising results . A phase 2 trial testing this strategy in combination with an immune checkpoint inhibitor is currently underway.
Immunotherapy drugs called bispecific antibodies are also under development. These drugs bind to lymphoma cells and the body’s own immune cells at the same time to bring them together. This allows the immune cells to kill the lymphoma cells. Five bispecific antibodies are in clinical trials for various types of lymphoma, including:
- glofitamab (Columvi), which in a phase 1 trial shrank aggressive lymphoma in people who had received several prior treatments
- epcoritamab (Epkinly), which also shrank previously treated aggressive lymphoma in an early-phase clinical trial
- mosunetuzumab (Mosun), which triggered long-lasting remissions in almost 20% of people with aggressive B-cell non-Hodgkin lymphoma and almost 50% of people with indolent B-cell non-Hodgkin lymphoma in an early-phase clinical trial
Glofitamab and epcoritamab have both received accelerated approval from the FDA for the treatment of some lymphomas that have returned or gotten worse after at least two other treatments.
Hodgkin Lymphoma Treatment
Hodgkin lymphoma is much less common than non-Hodgkin lymphoma. It is mostly seen in early adulthood (age 20–39) and in late adulthood (age 65 and older). More than 75% of all adults newly diagnosed with Hodgkin lymphoma can be cured with standard chemotherapy, radiation therapy, or both. Over the last 5 decades, deaths from Hodgkin lymphoma among adults have fallen more rapidly than deaths from any other cancer type.
Researchers are now focusing on adjusting standard treatment regimens to reduce the long-term side effects and improve quality of life for survivors. They are also testing better ways to treat the minority of patients whose cancer does recur.
Targeted therapies
A protein called CD30 is commonly found on the surface of Hodgkin lymphoma cells. A drug called brentuximab vedotin (Adcetris) that targets this protein has been approved as part of initial treatment for people with advanced Hodgkin lymphoma. Use of this new drug may help older patients avoid what had been the standard treatment with an especially toxic chemotherapy drug.
Clinical trials are now testing brentuximab vedotin combined with other chemotherapy drugs and with immunotherapies. The drug has also been approved by the FDA in combination with chemotherapy for some children and adolescents with Hodgkin lymphoma .
Immune checkpoint inhibitors that help T cells to better kill cancer cells have been effective in some people with recurrent Hodgkin lymphoma. Two such drugs— nivolumab (Opdivo) and pembrolizumab (Keytruda) —have been approved for some patients with Hodgkin lymphoma that has recurred after previous treatments. Researchers are now testing these drugs in combination with other therapies, as well as earlier in treatment for some people with cancer that is likely to recur.
NCI-Supported Research Programs
The Lymphoma Specialized Programs of Research Excellence (Lymphoma SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Lymphoma SPOREs support the development of new immunotherapies, novel targeted therapies, and new methods for determining prognosis for individual patients.
The goal of the International Lymphoma Epidemiology Consortium (InterLymph) is to enhance collaboration among epidemiologists studying lymphoma, provide a forum for the exchange of research ideas, and create a framework for collaborating on analyses that compile data from multiple studies.
The Lymphoma Epidemiology of Outcomes (LEO) Cohort Study was established to address the current and long-term health needs of non-Hodgkin lymphoma patients and survivors. The goal is to support a broad research agenda aimed at identifying novel clinical, epidemiologic, host, genetic, tumor, and treatment factors that significantly influence non-Hodgkin lymphoma prognosis and survivorship.
The Cancer Genome Characterization Initiative (CGCI) is supporting research to identify common gene changes in adult and pediatric cancers. Its results are freely available to the wider cancer research community, to spur the development of new targeted drugs. The HIV+ Tumor Molecular Characterization Project (HTMCP) and Burkitt Lymphoma Genome Sequencing Project (BLGSP) are two active CGCI projects.
Within the Center for Cancer Research , the Lymphoid Malignancies Branch focuses on identifying abnormalities in the immune system and looking at molecular disorders that underlie lymphoid malignancies.
The Clinical Trial Sequencing Project (CTSP) promotes the use of genomics in NCI-sponsored clinical trials. CTSP’s goal is to clarify the molecular basis of response and resistance to therapies studied. Diffuse large B-cell lymphoma is one of the cancer types under study, along with breast and renal cell carcinoma.
Lymphoma Research Results
The following are some of NCI's latest news articles on lymphoma research:
- Cholesterol Drug May Help Protect the Heart during Chemotherapy for Lymphoma
- Three-Drug Regimen Improves Protection against GVHD after Stem Cell Transplant
- Trial Confirms CAR T-Cell Therapy Benefits People with Aggressive Lymphomas
- Brentuximab Approved for High-Risk Hodgkin Lymphoma in Children and Adolescents
- Should CAR T Cells Be Used Earlier in People with Non-Hodgkin Lymphoma?
- Ibrutinib Improves Survival for Younger People with Diffuse Large B-cell Lymphoma
View the full list of Lymphoma Research Results and Study Updates .
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Evaluation of clinicians’ knowledge and practice regarding pharmacotherapy of Non-Hodgkin’s lymphoma: A multi-center study in Yemen
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected] (MMB); [email protected] (HZ)
Affiliations Discipline of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia, Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, University of Science and Technology, Sana’a, Yemen
Roles Conceptualization, Methodology, Supervision, Validation, Writing – review & editing
Affiliation Discipline of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, Malaysia
Affiliation Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, University of Science and Technology, Sana’a, Yemen
- Mohammed Mohammed Battah,
- Hadzliana Zainal,
- Doa’a Anwar Ibrahim,
- Nur Hafzan Binti Md Hanafiah,
- Syed Azhar Syed Sulaiman

- Published: June 5, 2024
- https://doi.org/10.1371/journal.pone.0304209
- Reader Comments
Non-Hodgkin lymphoma (NHL) is a hematological malignancy that requires effective pharmacotherapy for optimal management. There is limited information regarding Yemeni clinicians’ knowledge and practice of NHL pharmacotherapy. This study aims to assess the knowledge and practice of physicians and nurses in Yemen regarding pharmacotherapy of NHL. A cross-sectional study was conducted in Sana’a, Yemen, from January 1, 2022, to January 31, 2023. Two self-administrated and validated questionnaires were distributed to 99 physicians and 164 nurses involved in pharmacotherapy for NHL in different oncology centers and units across Yemen. Convenience samples were used to recruit participants. A binary logistic regression analysis was performed to identify factors associated with nurses’ and physicians’ knowledge and practice. The correlation coefficient was used to examine the relationship between knowledge and practice. A total of 77 physicians and 105 nurses completed the questionnaires. The results showed that 54.3% of nurses and 66.2% of physicians had poor knowledge of NHL pharmacotherapy. In terms of practice, 83.8% of nurses and 75.3% of physicians exhibited poor practice regarding NHL pharmacotherapy. Multivariable logistic regression analysis identified that nurses who received sufficient information about chemotherapy displayed a significant association with good knowledge, while nurses working in the chemotherapy administration department were significant predictors of good practice. Among physicians, those working in the National Oncology Center (NOC) in Sana’a demonstrated good practice. Correlation analysis revealed a positive relationship between nurses’ knowledge and their practice. The study’s results confirm deficiencies in knowledge and practice of pharmacotherapy for NHL among physicians and nurses in Yemen. Efforts should be made to enhance their understanding of treatment guidelines and to improve patient care. Improvement in educational programs and training opportunities may contribute to improving patient outcomes in the management of NHL.
Citation: Battah MM, Zainal H, Ibrahim DA, Md Hanafiah NHB, Sulaiman SAS (2024) Evaluation of clinicians’ knowledge and practice regarding pharmacotherapy of Non-Hodgkin’s lymphoma: A multi-center study in Yemen. PLoS ONE 19(6): e0304209. https://doi.org/10.1371/journal.pone.0304209
Editor: Mehmet Baysal, Bursa Ali Osman Sonmez Oncology Hospital, TURKEY
Received: September 9, 2023; Accepted: May 8, 2024; Published: June 5, 2024
Copyright: © 2024 Battah et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Non-Hodgkin lymphoma (NHL) is a hematologic malignancy that arises from immune cells in lymphoid and other lymphoid tissues outside the nodes [ 1 ]. It is the most common type of lymphoma, accounting for about 85% of all lymphomas [ 2 ]. NHL can be classified into two main prognostic groups: aggressive and indolent NHLs [ 3 ]. It is further classified, according to the World Health Organization (WHO), into T-cell, NK-cell, and B-cell subtypes. Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of all NHLs [ 4 ]. NHL treatment strategies vary based on several factors, including the specific subtype, disease stage, affected sites, and individual patient characteristics such as age and comorbidities. These strategies may include chemotherapy, radiation therapy, or a combination of these approaches and may involve only patient observation [ 5 , 6 ].
The most common pharmacotherapeutic agents used in the treatment of NHL include cyclophosphamide, bleomycin, doxorubicin, purine analogs, etoposide, methotrexate, vincristine, and corticosteroids. However, Rituximab-based regimens have shown encouraging outcomes in terms of overall survival rates [ 5 ]. On the other hand, radiation therapy is often reserved as a palliative measure to manage extensive local disease or as a consolidation strategy post-chemotherapy in patients with extranodal large masses [ 5 , 6 ]. The pharmacotherapy process is an essential part of patient care, as it involves the use of medications to manage diseases and symptoms [ 7 ]. However, the complexity of this process introduces the potential for medication errors [ 8 ], which most commonly occur in physicians’ prescriptions (46%) and nurses’ administration (41%) [ 9 , 10 ]. This underscores the importance of the role of clinicians, including physicians and nurses, in prescribing and administering medications, as they have significant impacts on pharmacotherapy outcomes and patients’ recovery [ 7 ].
In cancer pharmacotherapy, physicians and nurses are of utmost importance in the successful implementation of effective anti-cancer measures, particularly in the early detection and management of cases [ 11 ]. Despite this, their knowledge and awareness about pharmacotherapy of cancer, if insufficient, can lead to poor clinical practices, negative attitudes, and, ultimately, worse patient outcomes. This inadequate knowledge also makes it challenging to develop effective cancer prevention and control strategies [ 11 ]. Moreover, clinicians’ adherence to NHL pharmacotherapy guidelines is more likely to provide high-quality patient care. However, their lack of adherence to guidelines can lead to suboptimal care, underscoring the need for interventions to improve adherence and the quality of care [ 12 ].
While few studies have been conducted worldwide to assess physicians’ knowledge and practices in the field of cancer, they have focused primarily on pain control and palliative care areas [ 13 , 14 ]. Studies concerning nurses, in particular, have explored their knowledge and practices regarding the administration of chemotherapy [ 15 , 16 ]. This literature, however, did not address the specific complexities of NHL pharmacotherapy, which represents a significant gap in the current body of literature. According to the WHO: Globocan 2022 in the Yemeni context, NHL accounted for 851 new cases in Yemen, ranking sixth in terms of incidence among both sexes and third among males. It represented 5.2% of all new cancer cases with a cumulative risk of 0.35%. The number of deaths due to NHL was 585 cases, representing 4.9%, ranking as the ninth-highest number of fatalities, with a cumulative risk of 0.25. The 5-year prevalence of NHL cases was 1,829, representing 5.8% of all prevalent cancer cases [ 17 ]. Particularly, in Aden Governorate, in Aden Governorate, NHL emerged as the predominant type of malignant hematological tumors in both 2010 and 2013, according to data from the National Oncology Center (NOC) [ 18 , 19 ]. Lymphomas comprised 9.8% of all cancer cases, with NHL representing 65% of all lymphoma patients [ 19 ].
Despite the alarming prevalence of NHL in Yemen, there is a lack of research focusing on the knowledge and practices of Yemeni clinicians regarding the pharmacotherapy of NHL. Therefore, this study aims to fill this research gap and to assess the knowledge and practice of physicians and nurses regarding pharmacotherapy for NHL in Yemen. Also, to assess the relationship between the knowledge and practice of physicians and nurses regarding pharmacotherapy for NHL.
Ethical approval
The Ethical Committee of the Medical Research, University of Sciences and Technology, Sana’a, Yemen, approved this project, EAC/UST201 (this study is part of a project about Medication Use Evaluation for Non-Hodgkin Lymphoma in Yemen). The ethical committee approved the use of verbal informed consent in this study, as the participants’ identities were kept entirely anonymous, ensuring their privacy, and the study did not involve any risk to the participants. Therefore, clinicians who gave verbal consent and agreed to participate in the study were included. Additionally, all participants received thorough explanations of the study’s aims and objectives, and they were allowed to ask research-related questions.
Study design and setting
A cross-sectional study was conducted to investigate the pharmacotherapy of NHL in Yemen. Structured and validated questionnaires were used to collect data from physicians and nurses involved in the treatment of NHL across various oncology centers and units. Face-to-face interviews were conducted with participants in eight different regions in Yemen, including Sana’a Governorate (the NOC in Al-Jomhouri Teaching Hospital and the Oncology Unit in Al-Kuwait Hospital), Aden Governorate (the NOC in Al-Sadaqah Hospital), Hadramout Governorate (the NOCs in Al-Mukalla, and Hadramout Valley and Desert (Seiyun), Taiz Governorate (Al-Amal Oncology Center), and Ibb and Al-Hudaidah Governorates (Al-Amal Oncology Units). These areas were selected to ensure the representation of oncology centers or units in Yemen’s north and south governorates. The study spanned 13 months, from January 1, 2022, to January 31, 2023.
Study population
The study included all oncology physicians and nurses working in the oncology centers and units in Yemen. Since the overall number of officially registered oncologists in Yemen is few [ 20 ], subjects were enrolled in this study using the entire population, as all physicians and nurses in all oncology centers and units were invited to participate in the study. Those involved in NHL pharmacotherapy and who agreed to participate were included in this study, while physicians and nurses who refused to participate were excluded. The total number of physicians in all large oncology centers in Yemen was 83, and 136 nurses [ 21 ]. However, to broaden the scope of our study, we also collected data from different oncology units in Yemen. After getting the information from these oncology units by personal communication, we found that the actual number across all oncology units in Yemen was 16 physicians and 28 nurses. Taking these additional statistics into account, we found that the final total number across all oncology centers and units in all regions in Yemen was 99 physicians and 164 nurses.
Sample size calculation and participants
Convenience sampling was used to recruit participants for our study [ 11 , 22 ]. Given the descriptive nature of our study and the rarity of NHL, as well as the limited available information on the subject, the sample size was determined by including all physicians and nurses from oncology centers and units [ 11 ]. The targeted physicians were categorized into consultants (those who have a subspecialty), specialists (physicians who completed four or five years of residency program), residents (physicians enrolled in a four or 5-year residency program), and general physicians (GP; licensed physicians who are graduated from an accredited medical school without being enrolled into a residency program).
Study instrument
Two self-administered questionnaires were designed: one for physicians and another for nurses. The questionnaires were developed based on the guidelines’ recommendations, experts’ opinions, and previously published literature [ 23 – 26 ]. Each questionnaire comprises three sections ( S1 and S2 Files ): the first included sociodemographic characteristics, the second contained questions concerning knowledge, and the third included questions concerning practice regarding the pharmacotherapy of NHL.
For physicians, section 1 contained data about age, gender, marital status, specialty and subspecialty, experience years, and working place. Section 2 included eighteen questions designed to assess the participants’ overall knowledge regarding the pharmacotherapy of NHL with three possible responses (agree, disagree, don’t know). Section 3 contained 16 questions that evaluated the physicians’ practices for pharmacotherapy of NHL in Yemen. Eleven questions with responses were measured on a 5-point Likert scale: never, rarely, sometimes, often, always, and the 6 th response was “not applicable”.
For Nurses, section 1 contained data about age, gender, marital status, experience years, professional qualification, and working ward. Furthermore, this section included a question about whether the participants had any chemotherapy training program in the past five years and how many programs if the answer was yes [ 27 ]. The last question in this section was about the adequacy of the information the participants had received on chemotherapy during their studies. Section 2 included fifteen questions designed to assess the participants’ overall knowledge regarding the pharmacotherapy of NHL with three possible responses (agree, disagree, don’t know). Section 3 contained 16 questions that evaluated the nurses’ practices regarding pharmacotherapy of NHL, with responses being measured on a 5-point Likert scale: never, rarely, sometimes, often, always, and the 6 th response was “not applicable”.
Scoring system
The correct answer received one point, while the incorrect or “I do not know” answers were given zero points. Therefore, the highest possible score for nurses’ knowledge is 15, and the lowest is 0. Bloom’s cut-off of 80% was adopted to categorize knowledge, and a score of ≥12 was considered good knowledge. For physicians, the total knowledge score ranged from 0 to 18. The total knowledge score was classified using Bloom’s cut-off point; a score of ≥14.4 was considered good knowledge (14.4–18, 80–100%) [ 28 ]. In the assessment of practices, a scoring system ranging from 1 to 5 was used, where "Never" corresponded to a score of 1, and "Always" represented a score of 5. The negatively worded questions were re-coded so that a higher score indicated higher practice. Nurses’ practices were assessed on a scale of 0 to 72, with higher scores indicating higher practice. The classification for nurses’ practice was defined as good (scores between 57.6 and 72, representing 80–100%) and poor (scores below 57.6, corresponding to ≤79%). Physicians’ practices were evaluated on a scale of 0 to 44, with good practice classified as scores between 35.2 and 44 (80–100%), and poor practice categorized as scores below 35.2 (≤79%) [ 29 ].
For content validation, the questionnaire was distributed to 9 experts from various fields, including clinical pharmacy, community medicine, pharmacy practice, internal medicine, and an oncologist. The experts were asked to assess the relevance and representation of the items within their respective domains. The Scale-Content Validity Index based on the Universal Agreement method (S-CVI/UA) was employed for the knowledge and practices of physicians and nurses’ domains. The results of the S-CVI/UA were 0.78, 0.88, 0.87, and 0.81, respectively, and the Scale-Content Validity Index Average (S-CVI/Ave) were 0.96, 0.98, 0.97, and 0.97, respectively. This indicates a satisfactory level of content validity for the domains [ 30 ].
For face validation, three physicians and four nurses assessed the clarity and comprehension of the questions in each domain. Then, the questionnaire was piloted on ten physicians and ten nurses to evaluate its reliability. Cronbach’s alpha for the physicians’ knowledge and practices was calculated as 0.83 and 0.76, respectively. The calculated Cronbach’s alpha for the nurses’ knowledge and practices were 0.78 and 0.77, respectively, indicating that the questionnaire’ subscales had acceptable internal consistency. Feedback from pilot study participants and face validation helped to improve data collection for the main study.
Procedure of data collection
The questionnaires were sent to the contact persons in all different areas of study with a cover letter written by the primary investigator describing the objectives of the study, and the name of the contact person. The questionnaires were distributed by the principal investigator and a well-trained data collectors’ team, who received adequate training on issues concerning the questionnaire (on the study’s objective, approaching the participants, and how to administer and collect the questionnaire timely). The questionnaires were handed to physicians and nurses in different centers and units after explaining the purpose of the study, and they were given a brief explanation about the study and its purpose after obtaining their verbal informed consent. Physicians and nurses were asked to complete the questionnaire and return it immediately after responding to it. Scoring was performed according to the number of correct answers.
Statistical analysis
The data collected was analyzed statistically using descriptive statistics, namely mean with standard deviation for continuous variables, while the frequency with percentage for categorical variables. Content validity for all questionnaires was conducted using CVI-UA calculation. Cronbach’s alpha test ≥0.7 was used to check the reliability of the study questionnaire instruments and the consistency of the sample’s responses. A scoring system was implemented, wherein a pre-determined set of correct answers was used to assign scores to each category, allowing for quantitative assessment of knowledge and practice. The associations between the physicians’ and nurses’ overall knowledge and practice with their demographic data were analyzed using logistic regression models. Initially, univariate logistic regression was performed, and variables with a significance level ( P -value < 0.25) were selected for inclusion in the multivariate logistic regression analysis. Odds ratios were calculated to determine the effect of each predictor on participants’ knowledge and practice. Correlation coefficients were calculated to assess the strength and direction of the relationship between physicians’ and nurses’ knowledge and practice using bivariate correlations, where strong: |r| ≥ 0.8, moderate: 0.5 < |r| < 0.8, and weak: |r| ≤ 0.5 [ 31 ]. A p-value less than 0.05 was used to indicate statistical significance. All statistical analyses were carried out using SPSS Version 25.0 (IBM Corp., Armonk, NY, USA), a widely used software for statistical analysis, see S3 and S4 Files .
Demographic characteristics of nurses
A total of 105 nurses completed the questionnaire, giving a final response rate of 70%. Table 1 displays the demographic characteristics of the participants. The majority of nurses were male (61.0%), single (54.3%), had 1 to 5 years of experience (59.0%), and held a diploma degree (62.9%). Almost half of them (49.5%) fell within the 20–30 age range, and 34.3% worked in the daily administration ward. Moreover, slightly more than half of the participants (52.4%) had received chemotherapy training in the past five years. Among those, a significant proportion (61.9%) were unsure how many programs they had attended, while only 2.9% reported receiving more than five chemotherapy training programs. Furthermore, the majority of participants (70.5%) believed that the chemotherapy-related information received during their study was insufficient.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0304209.t001
Demographic characteristics of physicians
The questionnaire was completed by 77 physicians, resulting in a final response rate of 89.53%. Table 1 displays the demographic characteristics of the participants. The majority of physicians were male (70.1%), married (55.8%), in the age range of 36–50 (62.3%), and worked in an oncology center (71.4%). Physicians with more than ten years of experience constituted the largest group (36.4%), followed by those with 6–10 years of experience (32.5%). The respondents were mainly specialists (44.2%), followed by consultants (29.9%), while radiation and medical oncology were the most common physicians’ subspecialties, with frequencies of 20.8% and 19.5%, respectively.
Nurses’ knowledge about pharmacotherapy of Non-Hodgkin’s lymphoma
The overall knowledge level of nurses was assessed based on the proportion of correct answers. The results revealed that more than half of nurses (54.3%) demonstrated poor knowledge regarding NHL pharmacotherapy. In terms of the prevalence of NHL compared to HL, 40.0% of nurses incorrectly responded, and almost half of them (49.5%) provided incorrect responses about the hereditary nature of NHL. On the other hand, the majority of nurses (87.6% and 90.5%) correctly responded to the questions “Non-Hodgkin’s lymphoma is not contagious” and “Anti-emetic drugs should be administered 30 to 60min before NHL chemotherapy”, respectively ( Table 2 ).
https://doi.org/10.1371/journal.pone.0304209.t002
Physicians’ knowledge about pharmacotherapy of Non-Hodgkin’s lymphoma
The results of the study showed that physicians demonstrated a high level of knowledge regarding the question of dosage adjustment for NHL patients and the question of assessment of tumor lysis syndrome (TLS) during NHL treatment to prevent acute kidney injury (AKI), showing the highest correct response rates of 94.8% and 93.5%, respectively. However, a considerable percentage of physicians provided incorrect responses to the questions related to the presentation of NHL patients with peripheral lymphadenopathy and the treatment goal for patients diagnosed with aggressive NHL (41.6% and 45.5%), respectively. Surprisingly, the majority of physicians (79.2%) provided incorrect responses to the questions related to the recommended regimens for patients with HIV-related lymphoma and the use of dexamethasone to prevent acute and delayed chemotherapy-induced nausea and vomiting (59.7%), suggesting a knowledge gap in this area ( Table 2 ). Overall, the analysis of physicians’ responses to knowledge questions revealed that 66.2% of physicians demonstrated poor knowledge regarding NHL pharmacotherapy.
Nurses’ practice about pharmacotherapy of Non-Hodgkin’s lymphoma
The results indicated the following findings regarding nurses’ practice of pharmacotherapy of NHL. In terms of overall practice, the majority of nurses (83.8%) were categorized as having poor practice. Surprisingly, the results showed that more than half of nurses (52.4%) stated that they always practice chemotherapy administration before receiving proper training, and 41.9% of them always suggest exclusive treatment with alternative medicine for NHL patients. Moreover, 53.3% of nurses reported that they always substitute supportive care medications based on their availability, and a significant proportion of them (62.9%) never change to the correct way when they encounter medical errors while administering chemotherapy. Additionally, the results showed that the majority of participants (80%) always washed their hands and skin thoroughly after any contact with NHL chemotherapy ( Table 3 ).
https://doi.org/10.1371/journal.pone.0304209.t003
Physicians’ practice about pharmacotherapy of Non-Hodgkin’s lymphoma
In terms of overall practice, only 24.7% of physicians demonstrated good practice, while 75.3% exhibited poor practice regarding pharmacotherapy of NHL. The majority of physicians (81.8%) have participated in different training activities related to NHL pharmacotherapy within the past five years. Among these activities, scientific meetings and medical conferences were reported by (50.6% and 39.0%) of physicians, respectively. However, participation in postgraduate medical research and medical training was only reported by (10.4% and 13.0%) of the physicians, respectively. In addition, a significant proportion of physicians (54.5%) reported that they use paper records and charts as medical record systems. The most common challenges reported by physicians that could significantly affect NHL treatment outcomes are chemotherapy side effects (53.2%), patients’ non-compliance/ignorance (37.7%), and unavailability of chemotherapy medications (35.1%) ( Table 3 ).
Factors associated with nurses’ knowledge and practice
Logistic regression analysis was conducted to examine the relationship between various variables and the likelihood of having good knowledge or practice among nurses in pharmacotherapy for NHL ( Table 4 ). For nurses, both univariate and multivariate logistic regression analyses were performed. The results of the univariate model indicated that nurses who had more than nine years of experience and received enough information about chemotherapy during their study were more likely to have good knowledge compared to the reference group (p = 0.012, OD = 3.571, CI = 1.323–9.639) and (p = 0.002, OD = 8.182, CI = 2.201–30.416), respectively. After adjusting for other factors in the multivariate model, the analysis revealed that only one variable, receiving sufficient information about chemotherapy during their study, remained significantly and independently associated with total knowledge (p = 0.037, AOD = 5.170, CI = 1.105–24.203).
https://doi.org/10.1371/journal.pone.0304209.t004
Regarding total practice among nurses, the univariate analysis model showed that nurses working in the daily administration ward were more likely to have good practice compared to the reference group (p = 0.025, OR = 3.407, CI = 1.170–9.921). Subsequently, multivariate regression analysis was performed to identify the variables significantly and independently associated with practice. The multivariate regression analysis revealed that only working in the daily administration ward fulfilled the criteria, indicating a significant association with good practice (p = 0.033, AOD = 3.234, CI = 1.099–9.515).
Factors associated with physicians’ knowledge and practice
The study indicated the following findings regarding factors associated with physicians’ knowledge about pharmacotherapy for NHL ( Table 5 ). In univariate analysis, the results showed that physicians who were single/divorced were more likely to have good knowledge compared to the reference group (p = 0.031, OD = 2.933, CI = 1.104–7.790). After adjusting for other factors in the multivariate model, the results revealed that being single/divorced was the only variable significantly and independently associated with total knowledge among physicians (p = 0.041, AOD = 2.838, CI = 1.041–7.735). Furthermore, the univariate analysis for physicians demonstrated that physicians over 50 years old and those working in the NOC in Sana’a were more likely to have good practice compared to the reference group (p = 0.034, OD = 3.646, CI = 1.105–12.034) and (p = 0.004, OD = 20.667, CI = 2.585–165.214), respectively. Surprisingly, consultants were less likely to have good practice than specialists, residents, and GP group (p = 0.016, OD = 3.846, CI = 1.291–11.459). After adjusting for other factors in the multivariate model, the multivariate regression analysis identified the working in the NOC in Sana’a as the only variable significantly and independently associated with total practice among physicians (p = 0.009, AOD = 21.961, CI = 2.195–219.758).
https://doi.org/10.1371/journal.pone.0304209.t005
Correlation between nurses’ and physicians’ knowledge and practice
There is a weak significant correlation between nurses’ knowledge and practice (r = 0.343, P-value < 0.001). The correlation coefficient (r) is reported as 0.343, indicating a positive correlation between nurses’ knowledge and their practice. This means that as nurses’ knowledge increases, their practice also tends to improve ( Table 4 ). Based on the results among physicians, there is no significant correlation between physicians’ knowledge and practice (r = 0.205, P-value = .074) ( Table 6 ).
https://doi.org/10.1371/journal.pone.0304209.t006
The results of this study described the knowledge and practice of nurses and physicians regarding the pharmacotherapy of NHL as a multi-center study in eight centers and units in Yemen. Almost half of the nurses have not received chemotherapy training courses within the past five years. This insufficient training often raises concerns about their abilities and skills in administering chemotherapy to cancer patients, as chemotherapy administration is a complex and risky process due to expected high levels of adverse effects, resulting in errors and suboptimal treatment outcomes. This requires continuous training and awareness-raising among healthcare professionals, especially nurses [ 32 ]. Possible reasons for this lack of training may include limited access to training programs, limitations of available resources, and staff shortages [ 20 ]. These findings support a previous study in Bangladesh, which found that most nurses in Bangladesh lack access to chemotherapy training programs. Similarly, another study conducted in Poland highlighted that employers do not provide funding for training nurses for NHL, which may lead to insufficient knowledge and skills in patient care [ 33 , 34 ].
Nurses’ knowledge about pharmacotherapy of NHL
The study proved that the majority of nurses do not have sufficient knowledge regarding the pharmacotherapy of NHL. Such a gap in their knowledge and experience in this field raises doubts about their competence and ability to practice chemotherapy administration effectively. These results contrast with a previous study conducted in Taiz, Yemen, which revealed that half of the nurses had good knowledge regarding the management of side effects of chemotherapy [ 35 ]. The possible explanations for this discrepancy in the knowledge of nurses across Yemen include differences in sample size, nurses’ backgrounds, study locations, and differences in education, training, and resources that may also influence these disparities. On the other hand, this finding is consistent with previous studies conducted in Poland and Pakistan that highlighted insufficient and poor knowledge about NHL among nurses [ 23 , 33 ]. These consistent findings underscore the need for targeted education and training programs to improve nurses’ knowledge and awareness of NHL drug therapy.
Moreover, this study evaluated nurses’ understanding of the hereditary nature of NHL and found that 49.5% of nurses mistakenly believed that NHL is a hereditary disease passed directly from parents to children. However, it is important to clarify that NHL is a malignancy originating from immune cells and is not commonly considered hereditary. While a slightly increased risk is observed in family members, NHL is not classified as a hereditary disorder [ 36 – 38 ]. These findings emphasize the importance of enhancing nurses’ understanding of pharmacotherapy for NHL, similar to a previous study conducted in Poland that emphasized the necessity for education on NHL among nurses [ 33 ]. While nurse-led chemotherapy education is essential for optimal cancer care, current guidelines primarily focus on treatment specifics. Nurses play a vital role in addressing these concerns, answering questions, and providing support, as patients frequently seek guidance on adapting their daily routines for safety and improved well-being during chemotherapy [ 15 ]. In addition, oncology nurses with good knowledge of chemotherapy-induced peripheral neuropathy contribute to improving patients’ quality of life [ 39 ].
The study findings raise significant concerns about the practice of nurses in NHL pharmacotherapy. The majority of nurses showed poor practice, indicating the need to improve their knowledge and implement appropriate protocols of pharmacotherapy. This finding is in agreement with a previous study in Erbil, which revealed that the majority of participants demonstrated poor practice in the safe handling of chemotherapy [ 24 ]. It is alarming to note that a considerable percentage of nurses administer chemotherapy to patients without undergoing proper training. This situation poses potential risks to patient safety and emphasizes the critical need for nurses to receive adequate training before handling chemotherapy medications. Ensuring the appropriate level of nurses’ knowledge is essential for delivering proper nursing care and effective health education [ 33 ].
Another concern in the finding is that a significant proportion of nurses in the study recommended exclusive treatment with alternative medicine for NHL patients. This is consistent with previous studies by Damkier et al. and Fitch et al., which observed that nurses perceive the use of alternative medicine as a personal choice [ 40 , 41 ]. Nurses’ recommendation of exclusive alternative medicine for NHL patients may deviate from evidence-based practice and compromise standard pharmacotherapy effectiveness. This highlights a lack of basic knowledge regarding alternative medicine among nurses, consistent with a previous study in Qatar emphasizing the need to enhance complementary therapy education for oncology nurses [ 42 ]. On the other hand, Canadian oncology nurses acknowledge the importance of complementary and alternative medicine as part of person-centered care, emphasizing its inclusion in the foundations of oncology nursing practice. These findings underscore the need for comprehensive education and integration of complementary therapies into the training and practice of oncology nurses [ 43 ]. In a previous study conducted in Erbil, concerns in practices were observed, including inadequate changing of protective barriers after chemotherapy contact and a lack of knowledge regarding chemotherapy contamination through food [ 24 ]. Similarly, a study in Bangladesh reported inadequate use of specially designed personal protective equipment when handling chemotherapy agents [ 34 ]. In contrast, our study demonstrated positive results. The majority of respondents consistently used personal protective tools, such as gloves and masks, when administering NHL chemotherapy. They also exhibited good hygiene practices by thoroughly washing their hands and skin after any contact with NHL chemotherapy. In Bangladesh, approximately two-thirds of respondents (66.7%) prepared chemotherapeutic agents in a safe environment. Similarly, in our study, most respondents (77.1%) reported always preparing chemotherapy for NHL patients in a safe and appropriate area [ 34 ]. Nurses handling chemotherapy drugs should have appropriate qualifications and training to enhance safety standards. To improve their knowledge, all oncology nurses are required to undergo nursing education. As nurses continuously gain more knowledge, they are more likely to follow safety protocols when dealing with the administration of cancer chemotherapy, which can lead to improved health outcomes [ 34 ].
Overall, these results suggest the need for targeted interventions, including further training, education, and the establishment of clear guidelines, to promote safe and effective pharmacotherapy practices among nurses in NHL treatment. Educational institutions and nursing programs should prioritize providing nurses with a robust understanding of chemotherapy through coursework, practical training, and access to up-to-date resources. Equipping nurses with early education and training enables them to provide effective, evidence-based care to patients [ 44 ].
The study findings demonstrated varying levels of knowledge among physicians regarding the pharmacotherapy of NHL in multi-centers in Yemen. The questions regarding dosage adjustment for NHL patients and the question of assessment of TLS during NHL treatment to prevent AKI showed the highest correct response rates. These findings indicate that the participants have a solid understanding of these critical aspects of NHL management. Such knowledge is crucial for delivering safe and effective care to patients with NHL. The high response rates to these questions indicate that participants have a strong understanding of two critical aspects of managing NHL: dose adjustment and prevention of TLS. Dosage adjustment ensures appropriate chemotherapy dosing for individual patients, considering factors like body surface area and organ dysfunction. TLS prevention involves monitoring for signs and implementing measures to mitigate TLS risks. Participants’ knowledge in these areas reflects their readiness to provide safe and effective care for NHL patients [ 45 , 46 ].
However, physicians had a notable knowledge gap regarding the recommended regimens for treating NHL in patients with HIV-related lymphoma. Managing patients with HIV-related lymphoma poses a challenging situation, especially when many present with high-grade NHL. A typical manifestation involves extranodal disease, often affecting the gastrointestinal tract, central nervous system (CNS), or bone marrow [ 47 ]. Due to the aggressive nature of HIV-related lymphoma, it is recommended to employ intensive chemotherapy protocols such as Hyper-CVAD (hyper-fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) and EPOCH (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin) [ 5 ]. Despite the higher prevalence of non-Hodgkin lymphoma in HIV-infected individuals compared to the general population [ 48 ], physicians’ limited exposure to HIV-related lymphoma cases and their lack of experience and specialized training or education specifically focused on HIV-related lymphoma may contribute to their insufficient understanding of recommended treatment regimens. Surprisingly, a significant proportion of physicians provided incorrect responses regarding the use of dexamethasone to prevent acute and delayed chemotherapy-induced nausea and vomiting (CINV). According to the recommendations issued by the National Comprehensive Cancer Network [ 45 ] and the American Society of Clinical Oncology [ 49 , 50 ], dexamethasone is advised to be used for CINV prophylaxis in the HEC and MEC settings. The lack of awareness of current guidelines among physicians could explain these findings. Consistent with these findings, a previous study has shown that the guideline-recommended triplet of NK1RA–5-HT3RA-dexamethasone was prescribed in only 12.2% of cycles in five European countries: France, Germany, Italy, Spain, and the UK [ 47 ]. Continuing education in the healthcare field is emphasized as vital for healthcare workers to assume responsibility for their development, achieve competence individually and as a team, and enhance their skills and knowledge. Ultimately, this leads to an improved quality of healthcare delivery [ 51 ].
In terms of the overall knowledge assessment, the analysis of physicians’ knowledge regarding NHL pharmacotherapy indicated that a significant proportion of physicians showed good knowledge. Similarly, a study conducted in Bangladesh reported that 54.15% of the participants achieved a good or above-average score in the knowledge section [ 11 ].
The findings in this study indicated that only a small percentage of physicians exhibited good practice, while the majority (75.3%) showed poor practice regarding NHL pharmacotherapy. This emphasizes the need to improve the quality of care physicians provide in this area. In contrast, a study in Bangladesh found that 65.54% of participants scored above average, indicating that community healthcare providers and health assistants effectively fulfilled their roles with good practices [ 11 ]. Regarding training activities, the majority of physicians (81.8%) in this study reported participating in NHL therapy-related training activities within the past five years, primarily through medical conferences and scientific meetings. This demonstrates their commitment to ongoing education. However, over 90% of community healthcare providers and health assistants in Bangladesh did not receive cancer-related training from the government [ 11 ]. In this study, the majority of physicians (71.5%) provide regular follow-up of patients with NHL, even if they were asymptomatic, conducting surveillance and screening tests every six months or yearly. This is consistent with a similar study in Bangladesh, where a majority of community healthcare providers and health assistants (84.25% and 85.35%, respectively) conducted follow-ups for identified cancer patients during fieldwork [ 11 ]. However, contrasting results were observed in a study conducted in Lazio, Italy, where many physicians did not provide follow-up care for patients who tested positive for cancer [ 49 ]. Long-term follow-up care for cancer survivors is critical, as guidelines emphasize continuous follow-up for the first five years after treatment and less frequent follow-up after that [ 52 , 53 ].
Overall, these results suggest that physicians need to improve their practice regarding NHL pharmacotherapy. This could be done through continuous education, addressing side effects and patient compliance, and ensuring medication availability. By improving their practice, physicians can improve treatment outcomes for patients.
Factors associated with the knowledge and practice of nurse
The significant findings of the logistic regression analysis revealed the association between nurses’ receiving sufficient information during their education and their level of knowledge. This relationship remains statistically significant, as indicated by the significantly adjusted odds ratio, even after considering other factors. In the specific context of oncology nursing, previous research supported the importance of acquiring adequate information through continuous educational activities such as seminars and workshops. These activities play a crucial role in increasing knowledge and strengthening competencies, particularly in the safe administration of chemotherapy and adopting a proactive approach to managing side effects. By actively participating in continuous education, oncology nurses can enhance their skills and ultimately contribute to improved patient outcomes [ 16 ]. Moreover, the findings highlighted the complex interplay of various factors in nurses’ practice. Among these factors, years of experience and working ward emerged as influential, where nurses with more experience and those working in the daily administration wards demonstrated a higher percentage of good practice. Several explanations can be attributed to the finding that nurses in the daily administration ward exhibit a higher percentage of good practice than others. One possible reason is their regular involvement in administering chemotherapy to patients, as the daily administration ward in the oncology center is where most chemotherapy treatments are provided to patients, which enhances their understanding and implementation of best practices. Additionally, the work environment in the daily administration ward may also offer more support and resources for nurses to gain experience, enabling them to deliver high-quality care during administration. This underscores the importance of ensuring excellence in nursing practices within this department.
Factors associated with the knowledge and practice of physicians
The logistic regression analysis revealed significant factors associated with physicians having good knowledge and good practice compared to the reference group. Regarding the marital status of physicians, single/divorced physicians showed higher knowledge than married physicians. Single/divorced physicians could have advantages regarding time availability for studies and research, higher motivation to succeed in their careers, and better access to educational resources [ 54 ]. However, they may have less good practice due to increased stress levels and long working hours, which can lead to fatigue and impact patient care. Addressing these challenges can help improve the practice of single/divorced physicians in oncology [ 54 ].
Furthermore, a previous study conducted in Eswatini noted that community health workers in Lubombo, the legislative capital, had slightly lower knowledge scores than their counterparts in Hhohho [ 55 ]. Similarly, our study focused on physicians working on the NOC in Sana’a, the capital of Yemen, and revealed a similar trend. It was found that these physicians are less likely to have good knowledge compared to physicians working in other governorates and different regions across Yemen. This discrepancy in levels of knowledge among physicians may be attributed to various environmental factors, including limited access to educational resources due to the ongoing conflict in Yemen, high staff attrition rates, and potential difficulties in obtaining professional development opportunities. However, despite this relative lack of knowledge, it is important to highlight that these physicians in the NOC appear to have more practical experience than their counterparts in other governorates. The possible explanation for that includes a greater opportunity to deal with various conditions, giving them more hands-on experience, as the NOC in Sana’a treats a higher number of cases than other hospitals.
A correlation coefficient of 0.343 indicates a positive association between nurses’ knowledge and practice. As well-informed nurses, their practices improve accordingly, suggesting that staying up-to-date can positively impact patient care and outcomes, as the more knowledgeable nurses are, the more they use safety measures in their practice and better patient outcomes [ 23 ]. One possible explanation for this positive correlation is that nurses who strongly understand evidence-based medical concepts, procedures, and practices are more likely to apply their knowledge effectively in their daily clinical practice. By keeping abreast of the latest developments in their field, nurses can make informed decisions, provide optimal patient care, and contribute to positive patient outcomes. In contrast to our study, the result of a previous study conducted in Erbil city showed a significant negative association between knowledge and practices among oncology nurses (r = -0.469, p = 0.014) [ 24 ].
Study limitations
First, the convenience sampling method and the small sample size may affect the generalizability of our findings. These limitations can be attributed to the difficulty in obtaining a larger and more representative sample due to the rarity of NHL in Yemen. Additional challenges during the study’s conduct included the complicated treatment regimen for NHL patients and the limited cooperation of some physicians. The study was only conducted in a specific geographic region, Yemen, which may have limited the application of the findings to other contexts and populations. Nevertheless, despite these limitations, our research provides significant relevance since it sheds light on important relationships between physicians’ clinical practice and knowledge of the pharmacotherapy of NHL. It establishes the foundation for ongoing research and serves as a starting point for larger, more varied future investigations intended to both confirm our findings and overcome these acknowledged limitations. Moreover, the multi-center design of the study strengthens the breadth of the data collected and contributes to a richer, more nuanced understanding of the current practices and knowledge gaps in NHL pharmacotherapy in Yemen. Also, the study’s focus on both physicians and nurses provides a more comprehensive view of healthcare providers’ knowledge and practice in this area.
In conclusion, the study revealed alarming knowledge gaps and concerning practices in NHL pharmacotherapy among nurses and physicians in Yemen. While physicians demonstrated high knowledge in certain areas like dosage adjustment, a considerable portion displayed knowledge gaps related to treatment goals and recommended regimens. Nurses exhibited overall poor knowledge, with many lacking recent chemotherapy training and awareness about NHL pharmacotherapy. Targeted educational interventions and continuous training are essential to enhance clinicians’ and nurses’ knowledge and practices, thereby improving patient care.
Supporting information
S1 file. nurses’ questionnaire..
https://doi.org/10.1371/journal.pone.0304209.s001
S2 File. Physicians’ questionnaire.
https://doi.org/10.1371/journal.pone.0304209.s002
S3 File. Nurses’ dataset.
https://doi.org/10.1371/journal.pone.0304209.s003
S4 File. Physicians’ dataset.
https://doi.org/10.1371/journal.pone.0304209.s004
Acknowledgments
The authors would like to thank all physicians and nurses for their participation in this study. The authors would also like to thank all oncology centers and units in Yemen for providing access to the data and facilities.
- View Article
- PubMed/NCBI
- Google Scholar
- 5. DiPiro JT, Yee GC, Posey LM, Haines ST, Nolin TD, Ellingrod V. Pharmacotherapy: A Pathophysiologic Approach. 11th ed. New York: McGraw-Hill Education; 2020. MHID: 1-26-011670-0.
- 6. Chisholm-Burns MA, Schwinghammer TL, Malone PM, Kolesar JM, Bookstaver PB, Lee KC. Pharmacotherapy Principles & Practice. 6th ed. New York: McGraw-Hill Education; 2021. MHID: 1-26-046028-2.
- 20. Bawazir A, Basaleem H, Badheeb A, Abdul Hamid G. General Oncology Care in the Republic of Yemen. In Cancer in the Arab World. Singapore: Springer Singapore; 2022. pp. 321–338. https://doi.org/10.1007/978-981-16-7945-2
- 44. Lubejko BG, Wilson BJ. Oncology nursing: Scope and standards of practice. Pittsburgh, PA, USA: Oncology Nursing Society; 2019.
B–NHL Cases in a Tertiary Pediatric Hematology—Oncology Department: A 20-Year Retrospective Cohort Study
- Kyriakidis, Ioannis
- Pelagiadis, Iordanis
- Stratigaki, Maria
- Katzilakis, Nikolaos
- Stiakaki, Eftichia
Non-Hodgkin lymphoma (NHL) is among the five most common pediatric cancer diagnoses in children and adolescents and consists of a heterogeneous group of lymphoid tissue malignancies –with B-cell-derived NHL accounting for nearly 80% of cases. Novel and high-throughput diagnostic tools have significantly increased our understanding of B-NHL biology and molecular pathogenesis, leading to new NHL classifications and treatment options. This retrospective cohort study investigated 17 cases of both mature B-cell NHL (Burkitt lymphoma or BL; Diffuse large B-cell lymphoma or DLBCL; Primary mediastinal large B-cell lymphoma or PMBCL; Follicular lymphoma or FL) and immature B-cell progenitor NHL (B-lymphoblastic lymphoma or BLL) that were treated in a tertiary Pediatric Hematology-Oncology Department during the last 20 years. Modern NHL protocols for children, adolescents, and young adults, along with the addition of rituximab, are safe and efficient (100% overall survival; one relapse). Elevated ESR was more prevalent than elevated LDH. Analyses have focused on immune reconstitution (grade ≥3 infections, lymphocyte and immunoglobulin levels recovery) and body-mass-index changes post-treatment, late effects (in 53% of patients), and the presence of histology markers BCL2, BCL6, CD30, cMYC, and Ki-67%. One patient was diagnosed with a second malignant neoplasm (papillary thyroid cancer).
- Non-Hodgkin lymphoma;
- Burkitt lymphoma;
- adolescents;
- immune reconstitution;
- drug toxicity;
- second neoplasm;
- biomarkers;
- positron emission tomography computed tomography
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
- DOI: 10.1016/j.htct.2024.02.012
- Corpus ID: 268486450
REALM study: A retrospective evaluation of treatment patterns in patients with mantle cell lymphoma in a routine single private practice in Brazil
- M. Bellesso , Alice Bianco , +3 authors A. Alves
- Published in Hematology, Transfusion and… 1 March 2024
Figures and Tables from this paper

6 References
Efficacy and safety of ibrutinib combined with standard first-line treatment or as substitute for autologous stem cell transplantation in younger patients with mantle cell lymphoma: results from the randomized triangle trial by the european mcl network, zanubrutinib in relapsed/refractory mantle cell lymphoma: long-term efficacy and safety results from a phase 2 study, clinical outcomes of patients with b-cell non-hodgkin lymphoma in real-world settings: findings from the hemato-oncology latin america observational registry study, outcomes in 370 patients with mantle cell lymphoma treated with ibrutinib: a pooled analysis from three open‐label studies, treatment of older patients with mantle-cell lymphoma., chemotherapy plus rituximab versus chemotherapy alone for b-cell non-hodgkin's lymphoma., related papers.
Showing 1 through 3 of 0 Related Papers

Published in Hematology, Transfusion and Cell Therapy 2024
M. Bellesso Alice Bianco R. Santucci R. Centrone Iohanã Gabriely Costa Oliveira A. Alves
- Case Report
- Open access
- Published: 03 June 2024
Next-generation sequencing of primary testicular lymphoma and relapse in the glans penis after prophylactic radiation therapy: a rare case report
- Naoya Ishibashi 1 , 4 ,
- Yoko Nakanishi 2 ,
- Toshiya Maebayashi 1 ,
- Katsuhiro Miura 3 ,
- Sumie Ohni 2 ,
- Shinobu Masuda 2 ,
- Yasuo Amano 4 &
- Masahiro Okada 1
Diagnostic Pathology volume 19 , Article number: 72 ( 2024 ) Cite this article
38 Accesses
Metrics details
Primary testicular lymphoma (PTL) is relatively rare. The contralateral testis is a common site of PTL relapse; therefore, once complete remission is achieved, radiation therapy (RT) is administered to the contralateral testis to prevent relapse.
Case presentation
A 76-year-old man was diagnosed with PTL and received RT as described above. However, despite achieving and maintaining complete remission, a mass diagnosed as diffuse large B-cell lymphoma by tissue biopsy developed in the glans penis 6.5 years after prophylactic RT. We investigated whether the glans penile lymphoma was PTL relapse or a new malignancy by genomic analysis using next-generation sequencing of DNA extracted from two histopathological specimens.
Conclusions
We found the same variant allele fraction in four somatic genes ( MYD88 , IL7R , BLNK , and FLT3 ) at similar frequencies, indicating that the glans penile lymphoma had the same origin as the PTL. To the best of our knowledge, this is the first case report of PTL relapse in the glans penis.
Primary testicular lymphoma (PTL) is a rare disease, accounting for 1–2% of all non-Hodgkin’s lymphomas [ 1 , 2 ]. High orchiectomy of the affected testis is performed to attain the diagnosis, and systemic chemotherapy, such as rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP), is administered after surgery. After complete remission has been achieved, radiation therapy (RT) is administered to the contralateral testis to prevent relapse because the contralateral testis is a common site of PTL relapse [ 1 , 3 , 4 ]. Prophylactic RT significantly reduces the relapse rate in the contralateral testis [ 1 , 5 ]. The central nervous system (CNS) is also a common site of PTL relapse [ 1 , 2 , 3 , 4 , 6 ].
We conducted a comprehensive genomic analysis by targeting the exons of oncogenes and tumor suppressor genes via next-generation sequencing (NGS) of DNA extracted from histopathological samples both at the initial diagnosis and at relapse in the glans penis. We hypothesized that if exactly the same variant allele fraction is detected in some somatic genes at similar frequencies in the two histopathological samples, then the glans penile lymphoma shares the same origin as the initial diffuse large B-cell lymphoma (DLBCL) in the testis, confirming the diagnosis of relapsed PTL.
- Case report
A 76-year-old Japanese man visited our hospital with painless swelling of the right testis. He underwent high orchiectomy for diagnostic purposes. Pathologic examination revealed marked infiltration of atypical lymphocytes extending from the testis to the epididymis, and immunostaining revealed monoclonal proliferation of B cells positive for CD20 and CD79a. These findings led to a diagnosis of DLBCL (Fig. 1 A–D). No infiltration of any other organs was detected by either fluorodeoxyglucose positron emission tomography/computed tomography or bone marrow biopsy. Thereafter, the final diagnosis of the primary testicular DLBCL, Ann Arbor stage I E , was confirmed. The patient’s serum lactate dehydrogenase concentration was elevated, and his International Prognostic Index score was 2 points [ 7 ]. According to this score, he was deemed at low/intermediate risk and received three cycles of the R-CHOP regimen. During R-CHOP therapy, he also received three doses of intrathecal methotrexate at 15 mg for CNS prophylaxis. The penis was lifted and taped to the abdominal wall for exclusion from the irradiation field, and prophylactic RT was delivered to the contralateral testis with an 8-MeV electron beam at a dose of 2 Gy/fraction to a total dose of 30 Gy. Although the patient remained in complete remission after RT, a mass developed in the glans penis 6.5 years after prophylactic RT. The mass grew, and the entire glans penis was swollen. T2-weighted magnetic resonance imaging revealed a large soft tissue mass from the glans penis to the corpus cavernosum (Fig. 2 ). Tissue biopsy of the mass in the glans penis revealed marked infiltration of atypical lymphocytes, and immunostaining revealed monoclonal proliferation of CD20- and CD79a-positive B cells. These findings led to a diagnosis of DLBCL (Fig. 1 E–H). Fluorodeoxyglucose positron emission tomography/computed tomography revealed infiltration of the glans penis (Fig. 3 ) and right inguinal lymph node. Magnetic resonance imaging revealed no infiltration of the CNS or contralateral testis. Because the pain in the glans penis was severe, palliative RT was prioritized over systemic therapy. Three-dimensional conformal RT was delivered to the entire penis and right inguinal lymph node using 6-MV photon beams at a dose of 2 Gy/fraction to a total dose of 40 Gy. The glans penile lymphoma markedly decreased in size after RT. A urinary catheter was placed after RT because the patient exhibited grade 2 urinary retention according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) v5.0 [ 8 ]. Because relapsed DLBCL was considered likely, second-line chemotherapy with polatuzumab vedotin plus bendamustine and rituximab (Pola-BR) was initiated after RT [ 9 ]. CTCAE grade 4 skin rashes subsequently appeared, prompting treatment discontinuation after two cycles of Pola-BR. Computed tomography revealed disappearance of the lesion 199 days after RT, and no relapse was observed up to 549 days after treatment completion.

Histological and immunohistochemical features of the ( A – D ) testicular and ( E – H ) penile samples. Hematoxylin and eosin staining revealed (A) diffuse infiltration of large atypical lymphocytes in the testicular sample and (E) diffuse atypical lymphocytes in the penile sample. The tumor cells in the testicular and penile tissues exhibited diffuse monoclonal expression of ( B , F ) CD20 and ( C , G ) CD79a. ( D , H ) The Ki-67 index was approximately 70–75% in both samples. Each bar represents 50 μm

Magnetic resonance imaging of the glans penile tumor. A T2-weighted image revealed a large soft tissue mass in the glans penis and corpus cavernosum (white arrows)

Sagittal fused fluorodeoxyglucose positron emission tomography/computed tomography image. High fluorodeoxyglucose uptake in the glans penile tumor was confirmed (white arrows; maximum standardized uptake value, 33.3)
- Next-generation sequencing
The site of the relapse in this patient, the glans penis, is an extremely rare site for relapse of PTL and was located close to the primary radiation field in this case. Additionally, a 6.5-year progression-free period is unusual for aggressive lymphomas. Thus, to distinguish relapse of PTL or secondary DLBCL, we performed a comprehensive genomic analysis using NGS of DNA extracted from both histopathological specimens obtained at the initial diagnosis and at relapse after obtaining written informed consent from the patient.
DNA was extracted from both the initial PTL and glans penile lymphoma specimens. NGS was conducted using the Ion AmpliSeq™ Comprehensive Cancer Panel on the Ion Torrent platform (Thermo Fisher Scientific, Waltham, MA, USA). The Ion AmpliSeq™ Comprehensive Cancer Panel provides complete exon coverage of more than 400 cancer-associated genes. The same variant allele fraction in four somatic genes, namely MYD88 , IL7R , BLNK , and FLT3 , was detected in both histopathological specimens at similar frequencies (37.8–54.9%) (Table 1 ). Therefore, the glans penile lymphoma was found to share the same origin as the PTL in this patient, leading to a diagnosis of relapsed PTL. Although these genes are not oncogenic, mutations of these genes have been detected in patients with DLBCL and leukemia [ 10 , 11 , 12 , 13 , 14 ]. In particular, MYD88 encodes for an adaptor protein that mediates Toll-like receptor and interleukin-1 receptor signaling, and mutations in this gene are reportedly important drivers of lymphomagenesis in PTL [ 11 ].
PTL is an aggressive extranodal non-Hodgkin’s lymphoma that relapses in various sites at a high frequency of 52.0–80.0% even after first-line therapy [ 1 , 2 , 3 ]. Common extranodal sites of PTL relapse include the CNS and contralateral testis [ 1 , 2 , 3 ]. The relapse rate in the contralateral testis is 15% at 3 years without prophylactic RT; however, RT significantly reduces the relapse rate [ 1 ]. One study showed that the relapse rate in the contralateral testis was 10% after prophylactic RT [ 4 ], whereas another study showed that no relapse was observed in any patients who received prophylactic RT [ 5 ]. Thus, the National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology and the International Lymphoma Radiation Oncology Group recommend that prophylactic RT should be delivered to the contralateral testis after chemotherapy regimens such as R-CHOP [ 15 , 16 ]. Although prophylactic RT is the standard of care for PTL, statistical data from the US Surveillance, Epidemiology, and End Results program showed that only 35.9% of patients received RT [ 17 ]. However, prophylactic RT to the contralateral testis has also been reported to improve overall survival [ 4 , 17 ]. Although other extranodal sites of relapse reportedly include Waldeyer’s ring and the skin, no report has described relapse in the glans penis [ 1 , 3 , 4 , 6 ]. A rare case of bilateral synchronous testicular involvement of PTL was recently reported, but the spermatic cord and glans penis were intact by surgical examination [ 18 ]. Also in our patient, no infiltration of the spermatic cord by surgical examination at initial high orchiectomy. PTL relapse after first-line therapy occurs relatively early, at a median of 0.8 to 3.0 years. However, relapse in the contralateral testis tends to occur at a median of 45 months after treatment [ 3 , 4 ]. In our patient, PTL relapsed in the glans penis, but not the contralateral testis, 6.5 years after prophylactic RT. In general, the contralateral testis, CNS and skin of the PTL patient should be evaluated carefully for the management of undiagnosed relapse. But we may also need to evaluate the penis henceforth considering our case. Primary penile lymphoma is extremely rare; approximately 30 cases have been reported to date. Although the use of chemotherapy, RT, surgery, or their combination has been reported, no standard of care has been established for primary penile lymphoma [ 19 , 20 , 21 , 22 ]. In our patient, palliative RT was prioritized over systemic therapy because of severe pain in the glans penis, and the glans penile lymphoma lesion markedly decreased in size.
A commonly reported histological subtype of primary penile lymphoma is DLBCL [ 19 , 21 , 22 ]. Because both the PTL and glans penile lymphoma in our patient were histologically diagnosed as DLBCL, we performed a comprehensive genomic analysis by targeting the exons of oncogenes and tumor suppressor genes via NGS of DNA extracted from two histopathological samples to determine whether the glans penile lymphoma shared the same origin as the PTL in this patient or whether it was a new primary lesion such as radiation-induced secondary malignancy. Given the reported association between exposure to radiofrequency waves and testicular cancer [ 23 ], we were concerned about.
unexpected exposure of the glans penis to a very low dose of radiation from the previously prophylactic RT of the contralateral testis. Although the penis was lifted and taped to the abdominal wall for exclusion from the irradiation field, the corpus spongiosum and cavernosum might have been included the irradiation field. We used small electron cones, and the RT dose in these tissues continuous with the glans penis could not be precisely determined. Because identical mutations in four somatic genes were detected from the two histopathological specimens at similar frequencies, the glans penile lymphoma was found to share the same origin as the PTL, leading to a diagnosis of relapsed PTL. In high-grade BCL, gene expressions such as MYC and BCL-6 alterations have been widely known to be associated with poor prognosis and these specific expression patterns were investigated in PTL [ 24 , 25 ]. But in our patient, a comprehensive genomic analysis including MYC and BCL-6 extracted from both histopathological specimens revealed no alterations in MYC and BCL-6 .
In summary, lymphoma developed in the glans penis after a long period following prophylactic RT for PTL. A comprehensive genomic analysis using NGS allowed us to definitively eliminate the possibility of radiation-induced secondary malignancy. To the best of our knowledge, this is the first case report of an NGS-confirmed relapse of PTL in the glans penis.
Data availability
The dataset used during this study are available from the corresponding author on reasonable request.
Abbreviations
- Primary testicular lymphoma
Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone
- Radiation therapy
Central nervous system
Diffuse large B-cell lymphoma
Common Terminology Criteria for Adverse Events
Polatuzumab vedotin plus bendamustine and rituximab
Zucca E, Conconi A, Mughal TI, Sarris AH, Seymour JF, Vitolo U, Klasa R, Ozsahin M, Mead GM, Gianni MA, International Extranodal Lymphoma Study Group, et al. Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the International Extranodal Lymphoma Study Group. J Clin Oncol. 2003;21(1):20–7. https://doi.org/10.1200/JCO.2003.11.141 .
Article CAS PubMed Google Scholar
Hasselblom S, Ridell B, Wedel H, Norrby K, Sender Baum M, Ekman T. Testicular lymphoma–a retrospective, population-based, clinical and immunohistochemical study. Acta Oncol. 2004;43(8):758–65. https://doi.org/10.1080/02841860410002851 .
Article PubMed Google Scholar
Fonseca R, Habermann TM, Colgan JP, O’Neill BP, White WL, Witzig TE, Egan KS, Martenson JA, Burgart LJ, Inwards DJ. Testicular lymphoma is associated with a high incidence of extranodal recurrence. Cancer. 2000;88(1):154–61. https://doi.org/10.1002/(sici)1097-0142(20000101)88:1<154::aid-cncr21>3.0.co;2-t .
Visco C, Medeiros LJ, Mesina OM, Rodriguez MA, Hagemeister FB, McLaughlin P, Romaguera JE, Cabanillas F, Sarris AH. Non-hodgkin’s lymphoma affecting the testis: is it curable with doxorubicin-based therapy? Clin Lymphoma. 2001;2(1):40–6. https://doi.org/10.3816/clm.2001.n.010 .
Vitolo U, Chiappella A, Ferreri AJ, Martelli M, Baldi I, Balzarotti M, Bottelli C, Conconi A, Gomez H, Lopez-Guillermo A, et al. First-line treatment for primary testicular diffuse large B-cell lymphoma with rituximab-CHOP, CNS prophylaxis, and contralateral testis irradiation: final results of an international phase II trial. J Clin Oncol. 2011;29(20):2766–72. https://doi.org/10.1200/JCO.2010.31.4187 .
Cheah CY, Wirth A, Seymour JF, Blood. Prim Testicular Lymphoma. 2014;123(4):486–93. https://doi.org/10.1182/blood-2013-10-530659 .
Article CAS Google Scholar
International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A predictive model for aggressive non-hodgkin’s lymphoma. N Engl J Med. 1993;329(14):987–94. https://doi.org/10.1056/NEJM199309303291402 .
Article Google Scholar
National Cancer Institute Common. Terminology Criteria for Adverse Events (CTCAE) 5.0. Nov 27, 2017.
Sehn LH, Herrera AF, Flowers CR, Kamdar MK, McMillan A, Hertzberg M, Assouline S, Kim TM, Kim WS, Ozcan M, et al. Polatuzumab Vedotin in relapsed or refractory diffuse large B-Cell lymphoma. J Clin Oncol. 2020;38(2):155–65. https://doi.org/10.1200/JCO.19.00172 .
Ngo VN, Young RM, Schmitz R, Jhavar S, Xiao W, Lim KH, Kohlhammer H, Xu W, Yang Y, Zhao H, et al. Oncogenically active MYD88 mutations in human lymphoma. Nature. 2011;470(7332):115–9. https://doi.org/10.1038/nature09671 .
Kraan W, van Keimpema M, HorliMYD HM, Schilder-Tol EJ, Oud ME, Noorduyn LA, Kluin PM, Kersten MJ, Spaargaren M, Pals ST. High prevalence of oncogenic MYD88 and CD79B mutations in primary testicular diffuse large B-cell lymphoma. Leukemia. 2014;28(3):719–20. https://doi.org/10.1038/leu.2013.348 .
Oliveira ML, Veloso A, Garcia EG, Iyer S, Pereira C, Barreto VM, Langenau DM, Barata JT. Mutant IL7R collaborates with MYC to induce T-cell acute lymphoblastic leukemia. Leukemia. 2022;36(6):1533–40. https://doi.org/10.1038/s41375-022-01590-5 .
Article CAS PubMed PubMed Central Google Scholar
Fouquet G, Rossignol J, Ricard L, Guillem F, Couronné L, Asnafi V, Vavasseur M, Parisot M, Garcelon N, Rieux-Laucat F, et al. BLNK mutation associated with T-cell LGL leukemia and autoimmune diseases: Case report in hematology. Front Med (Lausanne). 2022;9:997161. https://doi.org/10.3389/fmed.2022.997161 .
Perl AE, Larson RA, Podoltsev NA, Strickland S, Wang ES, Atallah E, Schiller GJ, Martinelli G, Neubauer A, Sierra J, et al. Outcomes in patients with FLT3-Mutated Relapsed/ refractory Acute myelogenous Leukemia who underwent transplantation in the phase 3 ADMIRAL trial of Gilteritinib versus Salvage Chemotherapy. Transpl Cell Ther. 2022;22S2666–6367. https://doi.org/10.1016/j.jtct.2022.12.006 .
NCCN Clinical Practice. Guidelines in Oncology (NCCN Guidelines®) Version 2.2015 Non-Hodgkin’s Lymphomas.
Yahalom J, Illidge T, Specht L, Hoppe RT, Li YX, Tsang R, Wirth A, International Lymphoma Radiation Oncology Group. Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2015;92(1):11–31. https://doi.org/10.1016/j.ijrobp.2015.01.009 .
Gundrum JD, Mathiason MA, Moore DB, Go RS. Primary testicular diffuse large B-cell lymphoma: a population-based study on the incidence, natural history, and survival comparison with primary nodal counterpart before and after the introduction of Rituximab. J Clin Oncol. 2009;27(31):5227–32. https://doi.org/10.1200/JCO.2009.22.5896 .
Di Domenico D, Barone B, Del Biondo D, Napolitano L, Fusco GM, Cirillo L, Reccia P, De Luca L, Zito AR, Napodano G, et al. Abnormal presentation of a bilateral, synchronous and plurimetastatic medium and large cell testicular lymphoma: a case report. Mol Clin Oncol. 2022;17(2):124. https://doi.org/10.3892/mco.2022.2557 .
Article PubMed PubMed Central Google Scholar
Arena F, di Stefano C, Peracchia G, Barbieri A, Cortellini P. Primary lymphoma of the penis: diagnosis and treatment. Eur Urol. 2001;39(2):232–5. https://doi.org/10.1159/000052441 .
McNab PM, Jukic DM, Mills O, Browarsky I. Primary cutaneous CD30 + T-cell lymphoproliferative disorder presenting as paraphimosis: a case report and review of the literature. Dermatol Online J. 2011;17(7):3.
Hamamoto S, Tozawa K, Nishio H, Kawai N, Kohri K. Successful treatment of primary malignant lymphoma of the penis by organ-preserving rituximab-containing chemotherapy. Int J Clin Oncol. 2012;17(2):181–4. https://doi.org/10.1007/s10147-011-0273-8 .
Stamatiou K, Pierris N. Lymphoma presenting as cancer of the glans penis: a case report. Case Rep Pathol. 2012;2012(948352). https://doi.org/10.1155/2012/948352 .
Yazici S, Del Biondo D, Napodano G, Grillo M, Calace FP, Prezioso D, Crocetto F, Barone B. Risk factors for testicular Cancer: Environment, genes and Infections-Is it all? Medicina (Kaunas). 2023; 59(4): 724. https://doi.org/10.3390/medicina59040724 .
Wang Q, Zheng D, Chai D, Wu S, Wang X, Chen S, Wu L, Cao R, Tao Y. Primary testicular diffuse large B-cell lymphoma: Case series. Med (Baltim). 2020;99(12):e19463. https://doi.org/10.1097/MD.0000000000019463 .
Bruehl FK, Ketterling RP, Rimsza LM, Santos EF, McPhail ED, Bruehl FK, Ketterling RP, Rimsza LM, Santos EF, McPhail ED. J Hematop. 2023;16(3):161–5. https://doi.org/10.1007/s12308-023-00556-5 .
Download references
Acknowledgements
We thank Joe Barber Jr., PhD and Angela Morben, DVM, ELS, from Edanz ( https://jp.edanz.com/ac ) for editing a draft of this manuscript.
No funding was received specifically for this work.
Author information
Authors and affiliations.
Department of Radiology, Nihon University School of Medicine, 30-1, Oyaguchi Kami-cho, Itabashi, 173-8610, Tokyo, Japan
Naoya Ishibashi, Toshiya Maebayashi & Masahiro Okada
Department of Oncologic Pathology, Nihon University School of Medicine, Itabashi, 173-8610, Tokyo, Japan
Yoko Nakanishi, Sumie Ohni & Shinobu Masuda
Division of Hematology and Rheumatology, Department of Medicine, Nihon University School of Medicine, Itabashi, 173-8610, Tokyo, Japan
Katsuhiro Miura
Department of Radiology, Nihon University Hospital, Chiyoda, Tokyo, 101-8309, Japan
Naoya Ishibashi & Yasuo Amano
You can also search for this author in PubMed Google Scholar
Contributions
NI collected the patient’s data, treated the patient, and majorly contributed to the writing of the manuscript. YN, SO, and SM performed the histopathological and molecular analyses. TM and KM treated the patient. YA and MO interpreted the medical images. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Naoya Ishibashi .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent form is available for review by the Editor of this journal. In accordance with local guidelines, ethical approval of this report was not required; the Nihon University Itabashi Hospital Clinical Research Judging Committee has waived the requirement for approval for case reports.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ishibashi, N., Nakanishi, Y., Maebayashi, T. et al. Next-generation sequencing of primary testicular lymphoma and relapse in the glans penis after prophylactic radiation therapy: a rare case report. Diagn Pathol 19 , 72 (2024). https://doi.org/10.1186/s13000-024-01498-x
Download citation
Received : 25 October 2023
Accepted : 21 May 2024
Published : 03 June 2024
DOI : https://doi.org/10.1186/s13000-024-01498-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Glans penis
Diagnostic Pathology
ISSN: 1746-1596
- Submission enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Tislelizumab augment the efficacy of CD19/22 dual-targeted chimeric antigen receptor T cell in advanced stage relapsed or refractory B-cell non-Hodgkin lymphoma
Affiliations.
- 1 National Clinical Research Center for Hematologic Diseases, Jiangsu Institute of Hematology, The First Affiliated Hospital of Soochow University, Suzhou, China.
- 2 Institute of Blood and Marrow Transplantation, Collaborative Innovation Center of Hematology, Soochow University, Suzhou, China.
- 3 Institute of Biomedical Engineering and Technology, Shanghai Engineering Research Center of Molecular Therapeutics and New Drug Development, School of Chemistry and Molecular Engineering, East China Normal University, Shanghai, China.
- PMID: 37776326
- DOI: 10.1002/hon.3227
Dual-targeted chimeric antigen receptor T (CAR-T) cell is an important strategy to improve the efficacy of CD19 CAR-T cell against refractory or relapsed B cell non-Hodgkin lymphoma (R/R B-NHL). However, durable responses are not achieved in most patients, in part owing CAR-T cell exhaustion caused by PD-1/PD-L1 pathway. We conducted a prospective, single-arm study of dual-targeted CD19/22 CAR-T cell combined with anti-PD-1 antibody, tislelizumab, in R/R B-NHL ( NCT04539444 ). Tislelizumab was administrated on +1 day after patients received infusion of CD19/22 CAR-T cell. Responses, survival and safety were evaluated. From 1 August 2020 to 30 March 2023, 16 patients were enrolled. The median follow-up time is 16.0 (range: 5.0-32.0 months) months. Overall response was achieved in 14 of 16 (87.5%) patients, and the complete response (CR) was achieved in 11 of 16 (68.8%) patients. The 1-year progression-free survival and overall survival rates were 68.8% and 81.3%, respectively. Of the 14 patients responded, 9 patients maintained their response until the end of follow-up. Among the 15 out of 16 (93.8%) patients who had extranodal involvement, 14 (93.3%) patients achieved overall response rate with 11 (73.3%) patients achieving CR. Eight (50%) patients experienced cytokine release syndrome. No neurologic adverse events were reported. Gene Ontology-Biological Process enrichment analysis showed that immune response-related signaling pathways were enriched in CR patients. Our results suggest that CD19/22 CAR-T cell combined with tislelizumab elicit a safe and durable response in R/R B-NHL and may improve the prognosis of those patients.
Keywords: CD19/CD22 chimeric antigen receptor T cell; anti-PD-1 antibody; refractory or relapsed B cell non-Hodgkin lymphoma; tislelizumab.
© 2023 John Wiley & Sons Ltd.
PubMed Disclaimer
Similar articles
- CD19/CD22 Chimeric Antigen Receptor T Cell Cocktail Therapy following Autologous Transplantation in Patients with Relapsed/Refractory Aggressive B Cell Lymphomas. Cao Y, Xiao Y, Wang N, Wang G, Huang L, Hong Z, Meng L, Zhou X, Wang J, Yang Y, Xu H, Zhang S, Xiao M, Chen L, Zheng M, Li C, Mao X, Gu C, Zhang T, Zhang Y, Zhou J. Cao Y, et al. Transplant Cell Ther. 2021 Nov;27(11):910.e1-910.e11. doi: 10.1016/j.jtct.2021.08.012. Epub 2021 Aug 20. Transplant Cell Ther. 2021. PMID: 34425260
- Phase I Trial of Fourth-Generation Anti-CD19 Chimeric Antigen Receptor T Cells Against Relapsed or Refractory B Cell Non-Hodgkin Lymphomas. Zhou X, Tu S, Wang C, Huang R, Deng L, Song C, Yue C, He Y, Yang J, Liang Z, Wu A, Li M, Zhou W, Du J, Guo Z, Li Y, Jiao C, Liu Y, Chang LJ, Li Y. Zhou X, et al. Front Immunol. 2020 Nov 27;11:564099. doi: 10.3389/fimmu.2020.564099. eCollection 2020. Front Immunol. 2020. PMID: 33329526 Free PMC article. Clinical Trial.
- Anti-CD19 Chimeric Antigen Receptor T Cells in Combination With Nivolumab Are Safe and Effective Against Relapsed/Refractory B-Cell Non-hodgkin Lymphoma. Cao Y, Lu W, Sun R, Jin X, Cheng L, He X, Wang L, Yuan T, Lyu C, Zhao M. Cao Y, et al. Front Oncol. 2019 Aug 19;9:767. doi: 10.3389/fonc.2019.00767. eCollection 2019. Front Oncol. 2019. PMID: 31482064 Free PMC article.
- Sequential anti-CD19, 22, and 20 autologous chimeric antigen receptor T-cell (CAR-T) treatments of a child with relapsed refractory Burkitt lymphoma: a case report and literature review. Du J, Zhang Y. Du J, et al. J Cancer Res Clin Oncol. 2020 Jun;146(6):1575-1582. doi: 10.1007/s00432-020-03198-7. Epub 2020 Mar 28. J Cancer Res Clin Oncol. 2020. PMID: 32222815 Review.
- Chimeric antigen receptor (CAR) T-cell therapy for people with relapsed or refractory diffuse large B-cell lymphoma. Ernst M, Oeser A, Besiroglu B, Caro-Valenzuela J, Abd El Aziz M, Monsef I, Borchmann P, Estcourt LJ, Skoetz N, Goldkuhle M. Ernst M, et al. Cochrane Database Syst Rev. 2021 Sep 13;9(9):CD013365. doi: 10.1002/14651858.CD013365.pub2. Cochrane Database Syst Rev. 2021. PMID: 34515338 Free PMC article. Review.
- Neelapu SS, Locke FL, Bartlett NL, et al. Comparison of 2-year outcomes with CAR T cells (ZUMA-1) vs salvage chemotherapy in refractory large B-cell lymphoma. Blood Adv. 2021;5(20):4149-4155. https://doi.org/10.1182/bloodadvances.2020003848
- Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377(26):2531-2544. https://doi.org/10.1056/nejmoa1707447
- Locke FL, Ghobadi A, Jacobson CA, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial. Lancet Oncol. 2019;20(1):31-42. https://doi.org/10.1016/s1470-2045(18)30864-7
- Abramson JS, Palomba ML, Gordon LI, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396(10254):839-852. https://doi.org/10.1016/s0140-6736(20)31366-0
- Plaks V, Rossi JM, Chou J, et al. CD19 target evasion as a mechanism of relapse in large B-cell lymphoma treated with axicabtagene ciloleucel. Blood. 2021;138(12):1081-1085. https://doi.org/10.1182/blood.2021010930
- Search in MeSH
Related information
Grants and funding.
- SLT201911/Priority Academic Program Development of Jiangsu Higher Education Institutions Suzhou Science and Technology Program Project
- 82020108003/National Natural Science Foundation of China
- 2022YFC2502700/National Key R & D Program of China
- NCRCH/Translational Research
- 2020WSC03/Translational Research
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Genetic Alliance
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
New Study Highlights Potential Link Between Malignant Lymphoma And Tattoos
A recent study conducted by researchers at Lund University in Sweden suggests a potential association between malignant lymphoma, a form of cancer affecting the lymphatic system, and individuals with tattoos. However, health experts caution that further investigation is needed to establish a definitive link between the two.
Under the leadership of Christel Nielsen, PhD, the research team examined information from 11,905 individuals living in Sweden, sifting through to find patients diagnosed with lymphoma between 2007 and 2017 and individuals of the same age and gender who did not have cancer.
They focused on individuals between the ages of 20 and 60. The research team accessed information from the Swedish National Cancer Register to gather their data. Among the population sample, 2,938 patients aged 20 to 60 were diagnosed with lymphoma.
According to the study, 1,398 patients with lymphoma and 4,193 cancer-free participants were surveyed in 2021. The aim was to gather insights into lifestyle factors that may contribute to the risk of malignant lymphomas, such as smoking and age, and details about their tattoos if they had one or more.
Here are the findings.
Researchers found that 21% of patients with lymphoma and 18% of cancer-free patients had tattoos. Notably, Lund University experts discovered that the risk of developing lymphoma was 21% higher among those who were tattooed. The risk of lymphoma was highest in individuals with less than two years between their first tattoos .
Initially, the researchers speculated that the size of tattoos might impact the risk of lymphoma. They considered that individuals with full-body tattoos might face a higher risk than those with smaller tattoos. However, upon analysis, they found no correlation between the area of the tattooed body surface and the risk of malignant lymphoma.
“We do not yet know why this was the case. [We] can only speculate that a tattoo, regardless of size, triggers a low-grade inflammation in the body, which in turn can trigger cancer. The picture is thus more complex than we initially thought,” Dr. Nielsen said of the Lund University study.
Dr. Nielsen warned that further research is needed to understand tattoos’ potential long-term health implications fully. The team is currently gearing up to conduct a comprehensive assessment to investigate the possible correlations between tattoos, various types of cancer and inflammatory diseases.
“People will likely want to continue to express their identity through tattoos, and therefore, it is vital that we, as a society, can ensure that it is safe. For the individual, it is good to know that tattoos can affect your health and that you should turn to your healthcare provider if you experience symptoms that could be related to your tattoo,” Dr. Nielsen concluded.
Black women may be at risk.
As researchers continue to explore the connection between tattoos and cancer, Black women need to be aware, as they are more inclined to get tattoos compared to other ethnic groups. A 2023 study by Pew Research found that 39% of Black Americans have tattoos, surpassing rates among Hispanic (35%), White (32%) and Asian Americans (14%). The study also highlighted that 38% of women, especially those aged 18 to 49, have tattoos, compared to 27% of men.
The lymphatic system serves as the body’s defense mechanism against diseases. It comprises lymph nodes, spleen, thymus gland, and bone marrow. Per Healthline, malignant lymphoma can spread throughout the lymphatic system, causing serious harm. The two primary types of lymphoma are Hodgkin’s lymphoma and non-Hodgkin’s lymphoma.
While the occurrence of malignant lymphoma in Black women is relatively low , a study from 2017 revealed that they are more prone to displaying high-risk characteristics of follicular lymphoma, a low-grade form of non-Hodgkin’s lymphoma (NHL). Follicular lymphoma manifests when white blood cells clump together to create lumps in lymph glands or organs. This condition frequently emerges in Black women under the age of 45.
However, Black women face a higher risk of developing other forms of cancer, such as breast cancer. According to the American Cancer Society , they are 41% more likely to die of breast cancer than white women, despite being less frequently diagnosed. Additionally, concerning rates of early-onset colorectal and lung cancers are on the rise among Black women, the CDC noted.
RELATED CONTENT: What You Need To Know About Tattoo Removal On Melanin Skin

Dreams And Nightmares! Netherlands Born Singer Sues The Dream For Sexually Abuse And Assault

Amy Robach Says She Gives "Zero F---s" About Her Haters

Unsung: '90s Singer Adina Howard Admits She Fumbled The Bag In Brandy, Wanya Morris Love Triangle

AMC Theatres CEO Admits To Sabotaging Beyoncé’s 'Renaissance' Concert Film While Coveting Taylor Swift's Film

Tahiry Jose Accused Former Lover Joe Budden Of Being Abusive Amid Diddy Debacle, He Responded

Denzel Washington Breaks Down Why 'Fences' Needed A Black Director

Say What?! Chatty Toddler Blabs Out ‘B---h’ After Woman Calls Her A ‘Goofball’

WHO'S THE BIGGEST BULLY? Mike Tyson And Cannon Briggs Reunite In Brownsville In Playful Brawl
We've joined the BHM Digital family of websites and have updated our Terms of Service and Privacy Policy. By continuing to use this site, you agree to our updated Terms of Service and Privacy Policy.
- Entertainment
- Privacy Policy
- COOKIE SETTINGS
- Terms of Service
- Advertising
MadameNoire is a sophisticated lifestyle publication that gives African-American women the latest in fashion trends, black entertainment news, parenting tips and beauty secrets that are specifically for black women. Black women seek information on a wide variety of topics including African-American hair care, health issues, relationship advice and career trends - and MadameNoire provides all of that.
An Urban One Brand
MadameNoire ® Copyright © 2024 BossipMadameNoire, LLC All Rights Reserved | BHM Digital

IMAGES
VIDEO
COMMENTS
Abstract. Lymphomas are solid tumors of the immune system and include 14% of all head and neck malignancies. Non-Hodgkin lymphomas (NHLs) are a heterogeneous group of lymphoproliferative disorders originating in B-, T-, or natural killer T-cells. They have a wide range of histological appearances and clinical features at presentation, which can ...
The patient in the current case study had a CNS-IPI of 3 and an 11% cumulative incidence of CNS relapse at 2 years. Data support some form of CNS prophylaxis, 19 Dr. Advani concluded, but the jury is still out regarding optimal treatment for double-expressor non-Hodgkin's lymphoma.
Dr. Olivia C. Smibert: A 48-year-old man with diffuse large B-cell lymphoma was evaluated in the oncology clinic of this hospital because of abdominal pain. The patient had been generally well ...
myeloma, as well as in patients with non-Hodgkin lymphoma (NHL).3-8 Bendamustine has also shown activity in patients with breast cancer and small cell lung cancer.2 Several clinical trials have assessed the efficacy and safety of BR in patients with relapsed mantle cell and indolent B-cell NHL. In a 2005 study by Rummel and col-
The treatment of patients with non- Hodgkin's lymphoma (NHL) is often the treatment of elderly patients, as most patients are older than 65 years at diagnosis. These elderly patients present particular therapeutic challenges, because they may be more frail and at greater risk of treatment-related toxicity, especially anthracycline-related cardiotoxicity, than younger patients. The following ...
The current literature is scarce as to the outcomes of COVID-19 infection in non-Hodgkin's lymphoma patients and whether immunosuppressive or chemotherapeutic agents can cause worsening of the patients' condition during COVID-19 infection. Our case is a 59-year-old gentleman who presented to the Emergency Department of the Cancer Institute of Hospital das Clínicas da Universidade de São ...
Treatment of aggressive, noncontiguous stage II, III, or IV non-Hodgkin lymphoma may include the following: Monoclonal antibody therapy (rituximab) with combination chemotherapy. Combination chemotherapy. A clinical trial of monoclonal antibody therapy with combination chemotherapy followed by radiation therapy.
The American Cancer Society estimated that more than 70,000 new cases of non-Hodgkin lymphoma (NHL) would be diagnosed in 2016 [1, 2].Although lymphomas arise mainly from lymph nodes, primary extranodal NHL occurs in at least 25% of the cases [].The adrenal gland can be secondarily involved in around 4% of the patients; however, primary adrenal NHL is extremely rare and accounts for less than ...
At total of 2204 NHL and 204 AIHA patients admitted to our hospital in the period between January 2009 and December 2018, of which 20 patients were diagnosed with AIHA/NHL and accounted for 0.91% and 9.8% of the NHL and AIHA cases, respectively. The clinical characteristics of 20 AIHA/NHL patients are summarized in Table 1.
Non-Hodgkin's lymphoma generally involves the presence of cancerous lymphocytes in your lymph nodes. But the disease can also spread to other parts of your lymphatic system. ... Laurent C, et al. Impact of expert pathologic review of lymphoma diagnosis: Study of patients from the French Lymphopath Network. Journal of Clinical Oncology. 2017 ...
A form of blood cancer that develops when lymphocytes, a type of white blood cell, grow out of control. Madi J., Hodgkin's, Stage 1B. Cancer details: Most common and most treatable form of Hodgkin lymphoma. 1st Symptoms: Shortness of breath. Treatment: 3 rounds (6 infusions) of ABVD chemo.
The involvement of the CNS in neoplastic lesions of the lymphatic system is most commonly observed in the case of non-Hodgkin lymphoma (NHL). HL localized in the central nervous system (CNS-HL) has been rarely reported, especially in its primary isolated form . It is a specific clinical case to observe the concomitant existence of another rare ...
The Lymphoma Epidemiology of Outcomes (LEO) Cohort Study was established to address the current and long-term health needs of non-Hodgkin lymphoma patients and survivors. The goal is to support a broad research agenda aimed at identifying novel clinical, epidemiologic, host, genetic, tumor, and treatment factors that significantly influence non ...
Non-Hodgkin lymphoma (NHL) is a hematological malignancy that requires effective pharmacotherapy for optimal management. There is limited information regarding Yemeni clinicians' knowledge and practice of NHL pharmacotherapy. This study aims to assess the knowledge and practice of physicians and nurses in Yemen regarding pharmacotherapy of NHL. A cross-sectional study was conducted in Sana ...
Non-Hodgkin lymphoma (NHL) is among the five most common pediatric cancer diagnoses in children and adolescents and consists of a heterogeneous group of lymphoid tissue malignancies -with B-cell-derived NHL accounting for nearly 80% of cases. Novel and high-throughput diagnostic tools have significantly increased our understanding of B-NHL biology and molecular pathogenesis, leading to new ...
Non-Hodgkin lymphoma, NOS: site: 9591/3: C85.9: 9591/3: T-cell lymphoma, NOS: site: 95913/5: ... We used logistic regression to estimate the association between tattoo exposure and malignant lymphoma. In a case-control study with incidence-density sampling, the odds ratio provides an unbiased estimate of the incidence rate ratio (IRR) in the ...
In non-Hodgkin lymphoma (NHL) radiologic assessment of 18 F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) is a key component of response assessment. 11 The Lugano 2014 classification 10 is the current standard for response assessment in NHL, especially for diffuse large B-cell lymphoma (DLBCL) and follicular ...
Protocol for a prospective feasibility study investigating phenoconversion of CYP3A4, CYP2C19 and CYP2D6 genotype in paeidiatric, adolescent and young adult patients with an acute diagnosis of Hodgkin or Non Hodgkin Lymphoma (PEGASUS) ... If so, please take 10 minutes to fill in our survey, and help us make the case for why sustaining open data ...
@article{Bellesso2024REALMSA, title={REALM study: A retrospective evaluation of treatment patterns in patients with mantle cell lymphoma in a routine single private practice in Brazil}, author={Marcelo Bellesso and Alice Bianco and Rodrigo Santucci and Renato Torrescasana Centrone and Iohan{\~a} Gabriely Costa Oliveira and Adelson Alves ...
Background Primary testicular lymphoma (PTL) is relatively rare. The contralateral testis is a common site of PTL relapse; therefore, once complete remission is achieved, radiation therapy (RT) is administered to the contralateral testis to prevent relapse. Case presentation A 76-year-old man was diagnosed with PTL and received RT as described above. However, despite achieving and maintaining ...
The cancer organization estimates about 80,620 people will be diagnosed with non-Hodgkin lymphoma this year. The new study, published in the eClinicalMedicine journal, spanned a decade and ...
Dual-targeted chimeric antigen receptor T (CAR-T) cell is an important strategy to improve the efficacy of CD19 CAR-T cell against refractory or relapsed B cell non-Hodgkin lymphoma (R/R B-NHL). However, durable responses are not achieved in most patients, in part owing CAR-T cell exhaustion caused by PD-1/PD-L1 pathway.
According to the study, 1,398 patients with lymphoma and ... "We do not yet know why this was the case. ... The two primary types of lymphoma are Hodgkin's lymphoma and non-Hodgkin's lymphoma.