Health literacy and tuberculosis control: systematic review and meta-analysis
Affiliations.
- 1 Public Health Foundation of India, New Delhi, India.
- 2 Country Office for India, World Health Organization, New Delhi, India.
- 3 Indian Council of Medical Research, Regional Medical Research Centre, Chandrasekharpur, Bhubaneswar, Odisha751023, India.
- 4 WHO National Tuberculosis Elimination Programme Technical Support Network, New Delhi, India.
- 5 Department of Psychiatry, Kalinga Institute of Medical Sciences, Bhubaneswar, India.
- PMID: 38812804
- PMCID: PMC11132163
- DOI: 10.2471/BLT.23.290396

Publication types
- Systematic Review
- Meta-Analysis
- Health Knowledge, Attitudes, Practice
- Health Literacy*
- Medication Adherence
- Tuberculosis* / drug therapy
- Tuberculosis* / prevention & control
Grants and funding
- 001/WHO_/World Health Organization/International
Loading metrics
Open Access
Peer-reviewed
Research Article
Functional connectivity changes in the brain of adolescents with internet addiction: A systematic literature review of imaging studies
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Child and Adolescent Mental Health, Department of Brain Sciences, Great Ormond Street Institute of Child Health, University College London, London, United Kingdom
Roles Conceptualization, Supervision, Validation, Writing – review & editing
* E-mail: [email protected]
Affiliation Behavioural Brain Sciences Unit, Population Policy Practice Programme, Great Ormond Street Institute of Child Health, University College London, London, United Kingdom
- Max L. Y. Chang,
- Irene O. Lee

- Published: June 4, 2024
- https://doi.org/10.1371/journal.pmen.0000022
- Peer Review
- Reader Comments
Internet usage has seen a stark global rise over the last few decades, particularly among adolescents and young people, who have also been diagnosed increasingly with internet addiction (IA). IA impacts several neural networks that influence an adolescent’s behaviour and development. This article issued a literature review on the resting-state and task-based functional magnetic resonance imaging (fMRI) studies to inspect the consequences of IA on the functional connectivity (FC) in the adolescent brain and its subsequent effects on their behaviour and development. A systematic search was conducted from two databases, PubMed and PsycINFO, to select eligible articles according to the inclusion and exclusion criteria. Eligibility criteria was especially stringent regarding the adolescent age range (10–19) and formal diagnosis of IA. Bias and quality of individual studies were evaluated. The fMRI results from 12 articles demonstrated that the effects of IA were seen throughout multiple neural networks: a mix of increases/decreases in FC in the default mode network; an overall decrease in FC in the executive control network; and no clear increase or decrease in FC within the salience network and reward pathway. The FC changes led to addictive behaviour and tendencies in adolescents. The subsequent behavioural changes are associated with the mechanisms relating to the areas of cognitive control, reward valuation, motor coordination, and the developing adolescent brain. Our results presented the FC alterations in numerous brain regions of adolescents with IA leading to the behavioural and developmental changes. Research on this topic had a low frequency with adolescent samples and were primarily produced in Asian countries. Future research studies of comparing results from Western adolescent samples provide more insight on therapeutic intervention.
Citation: Chang MLY, Lee IO (2024) Functional connectivity changes in the brain of adolescents with internet addiction: A systematic literature review of imaging studies. PLOS Ment Health 1(1): e0000022. https://doi.org/10.1371/journal.pmen.0000022
Editor: Kizito Omona, Uganda Martyrs University, UGANDA
Received: December 29, 2023; Accepted: March 18, 2024; Published: June 4, 2024
Copyright: © 2024 Chang, Lee. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The behavioural addiction brought on by excessive internet use has become a rising source of concern [ 1 ] since the last decade. According to clinical studies, individuals with Internet Addiction (IA) or Internet Gaming Disorder (IGD) may have a range of biopsychosocial effects and is classified as an impulse-control disorder owing to its resemblance to pathological gambling and substance addiction [ 2 , 3 ]. IA has been defined by researchers as a person’s inability to resist the urge to use the internet, which has negative effects on their psychological well-being as well as their social, academic, and professional lives [ 4 ]. The symptoms can have serious physical and interpersonal repercussions and are linked to mood modification, salience, tolerance, impulsivity, and conflict [ 5 ]. In severe circumstances, people may experience severe pain in their bodies or health issues like carpal tunnel syndrome, dry eyes, irregular eating and disrupted sleep [ 6 ]. Additionally, IA is significantly linked to comorbidities with other psychiatric disorders [ 7 ].
Stevens et al (2021) reviewed 53 studies including 17 countries and reported the global prevalence of IA was 3.05% [ 8 ]. Asian countries had a higher prevalence (5.1%) than European countries (2.7%) [ 8 ]. Strikingly, adolescents and young adults had a global IGD prevalence rate of 9.9% which matches previous literature that reported historically higher prevalence among adolescent populations compared to adults [ 8 , 9 ]. Over 80% of adolescent population in the UK, the USA, and Asia have direct access to the internet [ 10 ]. Children and adolescents frequently spend more time on media (possibly 7 hours and 22 minutes per day) than at school or sleeping [ 11 ]. Developing nations have also shown a sharp rise in teenage internet usage despite having lower internet penetration rates [ 10 ]. Concerns regarding the possible harms that overt internet use could do to adolescents and their development have arisen because of this surge, especially the significant impacts by the COVID-19 pandemic [ 12 ]. The growing prevalence and neurocognitive consequences of IA among adolescents makes this population a vital area of study [ 13 ].
Adolescence is a crucial developmental stage during which people go through significant changes in their biology, cognition, and personalities [ 14 ]. Adolescents’ emotional-behavioural functioning is hyperactivated, which creates risk of psychopathological vulnerability [ 15 ]. In accordance with clinical study results [ 16 ], this emotional hyperactivity is supported by a high level of neuronal plasticity. This plasticity enables teenagers to adapt to the numerous physical and emotional changes that occur during puberty as well as develop communication techniques and gain independence [ 16 ]. However, the strong neuronal plasticity is also associated with risk-taking and sensation seeking [ 17 ] which may lead to IA.
Despite the fact that the precise neuronal mechanisms underlying IA are still largely unclear, functional magnetic resonance imaging (fMRI) method has been used by scientists as an important framework to examine the neuropathological changes occurring in IA, particularly in the form of functional connectivity (FC) [ 18 ]. fMRI research study has shown that IA alters both the functional and structural makeup of the brain [ 3 ].
We hypothesise that IA has widespread neurological alteration effects rather than being limited to a few specific brain regions. Further hypothesis holds that according to these alterations of FC between the brain regions or certain neural networks, adolescents with IA would experience behavioural changes. An investigation of these domains could be useful for creating better procedures and standards as well as minimising the negative effects of overt internet use. This literature review aims to summarise and analyse the evidence of various imaging studies that have investigated the effects of IA on the FC in adolescents. This will be addressed through two research questions:
- How does internet addiction affect the functional connectivity in the adolescent brain?
- How is adolescent behaviour and development impacted by functional connectivity changes due to internet addiction?
The review protocol was conducted in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see S1 Checklist ).
Search strategy and selection process
A systematic search was conducted up until April 2023 from two sources of database, PubMed and PsycINFO, using a range of terms relevant to the title and research questions (see full list of search terms in S1 Appendix ). All the searched articles can be accessed in the S1 Data . The eligible articles were selected according to the inclusion and exclusion criteria. Inclusion criteria used for the present review were: (i) participants in the studies with clinical diagnosis of IA; (ii) participants between the ages of 10 and 19; (iii) imaging research investigations; (iv) works published between January 2013 and April 2023; (v) written in English language; (vi) peer-reviewed papers and (vii) full text. The numbers of articles excluded due to not meeting the inclusion criteria are shown in Fig 1 . Each study’s title and abstract were screened for eligibility.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmen.0000022.g001
Quality appraisal
Full texts of all potentially relevant studies were then retrieved and further appraised for eligibility. Furthermore, articles were critically appraised based on the GRADE (Grading of Recommendations, Assessment, Development, and Evaluations) framework to evaluate the individual study for both quality and bias. The subsequent quality levels were then appraised to each article and listed as either low, moderate, or high.
Data collection process
Data that satisfied the inclusion requirements was entered into an excel sheet for data extraction and further selection. An article’s author, publication year, country, age range, participant sample size, sex, area of interest, measures, outcome and article quality were all included in the data extraction spreadsheet. Studies looking at FC, for instance, were grouped, while studies looking at FC in specific area were further divided into sub-groups.
Data synthesis and analysis
Articles were classified according to their location in the brain as well as the network or pathway they were a part of to create a coherent narrative between the selected studies. Conclusions concerning various research trends relevant to particular groupings were drawn from these groupings and subgroupings. To maintain the offered information in a prominent manner, these assertions were entered into the data extraction excel spreadsheet.
With the search performed on the selected databases, 238 articles in total were identified (see Fig 1 ). 15 duplicated articles were eliminated, and another 6 items were removed for various other reasons. Title and abstract screening eliminated 184 articles because they were not in English (number of article, n, = 7), did not include imaging components (n = 47), had adult participants (n = 53), did not have a clinical diagnosis of IA (n = 19), did not address FC in the brain (n = 20), and were published outside the desired timeframe (n = 38). A further 21 papers were eliminated for failing to meet inclusion requirements after the remaining 33 articles underwent full-text eligibility screening. A total of 12 papers were deemed eligible for this review analysis.
Characteristics of the included studies, as depicted in the data extraction sheet in Table 1 provide information of the author(s), publication year, sample size, study location, age range, gender, area of interest, outcome, measures used and quality appraisal. Most of the studies in this review utilised resting state functional magnetic resonance imaging techniques (n = 7), with several studies demonstrating task-based fMRI procedures (n = 3), and the remaining studies utilising whole-brain imaging measures (n = 2). The studies were all conducted in Asiatic countries, specifically coming from China (8), Korea (3), and Indonesia (1). Sample sizes ranged from 12 to 31 participants with most of the imaging studies having comparable sample sizes. Majority of the studies included a mix of male and female participants (n = 8) with several studies having a male only participant pool (n = 3). All except one of the mixed gender studies had a majority male participant pool. One study did not disclose their data on the gender demographics of their experiment. Study years ranged from 2013–2022, with 2 studies in 2013, 3 studies in 2014, 3 studies in 2015, 1 study in 2017, 1 study in 2020, 1 study in 2021, and 1 study in 2022.
https://doi.org/10.1371/journal.pmen.0000022.t001
(1) How does internet addiction affect the functional connectivity in the adolescent brain?
The included studies were organised according to the brain region or network that they were observing. The specific networks affected by IA were the default mode network, executive control system, salience network and reward pathway. These networks are vital components of adolescent behaviour and development [ 31 ]. The studies in each section were then grouped into subsections according to their specific brain regions within their network.
Default mode network (DMN)/reward network.
Out of the 12 studies, 3 have specifically studied the default mode network (DMN), and 3 observed whole-brain FC that partially included components of the DMN. The effect of IA on the various centres of the DMN was not unilaterally the same. The findings illustrate a complex mix of increases and decreases in FC depending on the specific region in the DMN (see Table 2 and Fig 2 ). The alteration of FC in posterior cingulate cortex (PCC) in the DMN was the most frequently reported area in adolescents with IA, which involved in attentional processes [ 32 ], but Lee et al. (2020) additionally found alterations of FC in other brain regions, such as anterior insula cortex, a node in the DMN that controls the integration of motivational and cognitive processes [ 20 ].
https://doi.org/10.1371/journal.pmen.0000022.g002
The overall changes of functional connectivity in the brain network including default mode network (DMN), executive control network (ECN), salience network (SN) and reward network. IA = Internet Addiction, FC = Functional Connectivity.
https://doi.org/10.1371/journal.pmen.0000022.t002
Ding et al. (2013) revealed altered FC in the cerebellum, the middle temporal gyrus, and the medial prefrontal cortex (mPFC) [ 22 ]. They found that the bilateral inferior parietal lobule, left superior parietal lobule, and right inferior temporal gyrus had decreased FC, while the bilateral posterior lobe of the cerebellum and the medial temporal gyrus had increased FC [ 22 ]. The right middle temporal gyrus was found to have 111 cluster voxels (t = 3.52, p<0.05) and the right inferior parietal lobule was found to have 324 cluster voxels (t = -4.07, p<0.05) with an extent threshold of 54 voxels (figures above this threshold are deemed significant) [ 22 ]. Additionally, there was a negative correlation, with 95 cluster voxels (p<0.05) between the FC of the left superior parietal lobule and the PCC with the Chen Internet Addiction Scores (CIAS) which are used to determine the severity of IA [ 22 ]. On the other hand, in regions of the reward system, connection with the PCC was positively connected with CIAS scores [ 22 ]. The most significant was the right praecuneus with 219 cluster voxels (p<0.05) [ 22 ]. Wang et al. (2017) also discovered that adolescents with IA had 33% less FC in the left inferior parietal lobule and 20% less FC in the dorsal mPFC [ 24 ]. A potential connection between the effects of substance use and overt internet use is revealed by the generally decreased FC in these areas of the DMN of teenagers with drug addiction and IA [ 35 ].
The putamen was one of the main regions of reduced FC in adolescents with IA [ 19 ]. The putamen and the insula-operculum demonstrated significant group differences regarding functional connectivity with a cluster size of 251 and an extent threshold of 250 (Z = 3.40, p<0.05) [ 19 ]. The molecular mechanisms behind addiction disorders have been intimately connected to decreased striatal dopaminergic function [ 19 ], making this function crucial.
Executive Control Network (ECN).
5 studies out of 12 have specifically viewed parts of the executive control network (ECN) and 3 studies observed whole-brain FC. The effects of IA on the ECN’s constituent parts were consistent across all the studies examined for this analysis (see Table 2 and Fig 3 ). The results showed a notable decline in all the ECN’s major centres. Li et al. (2014) used fMRI imaging and a behavioural task to study response inhibition in adolescents with IA [ 25 ] and found decreased activation at the striatum and frontal gyrus, particularly a reduction in FC at inferior frontal gyrus, in the IA group compared to controls [ 25 ]. The inferior frontal gyrus showed a reduction in FC in comparison to the controls with a cluster size of 71 (t = 4.18, p<0.05) [ 25 ]. In addition, the frontal-basal ganglia pathways in the adolescents with IA showed little effective connection between areas and increased degrees of response inhibition [ 25 ].
https://doi.org/10.1371/journal.pmen.0000022.g003
Lin et al. (2015) found that adolescents with IA demonstrated disrupted corticostriatal FC compared to controls [ 33 ]. The corticostriatal circuitry experienced decreased connectivity with the caudate, bilateral anterior cingulate cortex (ACC), as well as the striatum and frontal gyrus [ 33 ]. The inferior ventral striatum showed significantly reduced FC with the subcallosal ACC and caudate head with cluster size of 101 (t = -4.64, p<0.05) [ 33 ]. Decreased FC in the caudate implies dysfunction of the corticostriatal-limbic circuitry involved in cognitive and emotional control [ 36 ]. The decrease in FC in both the striatum and frontal gyrus is related to inhibitory control, a common deficit seen with disruptions with the ECN [ 33 ].
The dorsolateral prefrontal cortex (DLPFC), ACC, and right supplementary motor area (SMA) of the prefrontal cortex were all found to have significantly decreased grey matter volume [ 29 ]. In addition, the DLPFC, insula, temporal cortices, as well as significant subcortical regions like the striatum and thalamus, showed decreased FC [ 29 ]. According to Tremblay (2009), the striatum plays a significant role in the processing of rewards, decision-making, and motivation [ 37 ]. Chen et al. (2020) reported that the IA group demonstrated increased impulsivity as well as decreased reaction inhibition using a Stroop colour-word task [ 26 ]. Furthermore, Chen et al. (2020) observed that the left DLPFC and dorsal striatum experienced a negative connection efficiency value, specifically demonstrating that the dorsal striatum activity suppressed the left DLPFC [ 27 ].
Salience network (SN).
Out of the 12 chosen studies, 3 studies specifically looked at the salience network (SN) and 3 studies have observed whole-brain FC. Relative to the DMN and ECN, the findings on the SN were slightly sparser. Despite this, adolescents with IA demonstrated a moderate decrease in FC, as well as other measures like fibre connectivity and cognitive control, when compared to healthy control (see Table 2 and Fig 4 ).
https://doi.org/10.1371/journal.pmen.0000022.g004
Xing et al. (2014) used both dorsal anterior cingulate cortex (dACC) and insula to test FC changes in the SN of adolescents with IA and found decreased structural connectivity in the SN as well as decreased fractional anisotropy (FA) that correlated to behaviour performance in the Stroop colour word-task [ 21 ]. They examined the dACC and insula to determine whether the SN’s disrupted connectivity may be linked to the SN’s disruption of regulation, which would explain the impaired cognitive control seen in adolescents with IA. However, researchers did not find significant FC differences in the SN when compared to the controls [ 21 ]. These results provided evidence for the structural changes in the interconnectivity within SN in adolescents with IA.
Wang et al. (2017) investigated network interactions between the DMN, ECN, SN and reward pathway in IA subjects [ 24 ] (see Fig 5 ), and found 40% reduction of FC between the DMN and specific regions of the SN, such as the insula, in comparison to the controls (p = 0.008) [ 24 ]. The anterior insula and dACC are two areas that are impacted by this altered FC [ 24 ]. This finding supports the idea that IA has similar neurobiological abnormalities with other addictive illnesses, which is in line with a study that discovered disruptive changes in the SN and DMN’s interaction in cocaine addiction [ 38 ]. The insula has also been linked to the intensity of symptoms and has been implicated in the development of IA [ 39 ].
“+” indicates an increase in behaivour; “-”indicates a decrease in behaviour; solid arrows indicate a direct network interaction; and the dotted arrows indicates a reduction in network interaction. This diagram depicts network interactions juxtaposed with engaging in internet related behaviours. Through the neural interactions, the diagram illustrates how the networks inhibit or amplify internet usage and vice versa. Furthermore, it demonstrates how the SN mediates both the DMN and ECN.
https://doi.org/10.1371/journal.pmen.0000022.g005
(2) How is adolescent behaviour and development impacted by functional connectivity changes due to internet addiction?
The findings that IA individuals demonstrate an overall decrease in FC in the DMN is supported by numerous research [ 24 ]. Drug addict populations also exhibited similar decline in FC in the DMN [ 40 ]. The disruption of attentional orientation and self-referential processing for both substance and behavioural addiction was then hypothesised to be caused by DMN anomalies in FC [ 41 ].
In adolescents with IA, decline of FC in the parietal lobule affects visuospatial task-related behaviour [ 22 ], short-term memory [ 42 ], and the ability of controlling attention or restraining motor responses during response inhibition tests [ 42 ]. Cue-induced gaming cravings are influenced by the DMN [ 43 ]. A visual processing area called the praecuneus links gaming cues to internal information [ 22 ]. A meta-analysis found that the posterior cingulate cortex activity of individuals with IA during cue-reactivity tasks was connected with their gaming time [ 44 ], suggesting that excessive gaming may impair DMN function and that individuals with IA exert more cognitive effort to control it. Findings for the behavioural consequences of FC changes in the DMN illustrate its underlying role in regulating impulsivity, self-monitoring, and cognitive control.
Furthermore, Ding et al. (2013) reported an activation of components of the reward pathway, including areas like the nucleus accumbens, praecuneus, SMA, caudate, and thalamus, in connection to the DMN [ 22 ]. The increased FC of the limbic and reward networks have been confirmed to be a major biomarker for IA [ 45 , 46 ]. The increased reinforcement in these networks increases the strength of reward stimuli and makes it more difficult for other networks, namely the ECN, to down-regulate the increased attention [ 29 ] (See Fig 5 ).
Executive control network (ECN).
The numerous IA-affected components in the ECN have a role in a variety of behaviours that are connected to both response inhibition and emotional regulation [ 47 ]. For instance, brain regions like the striatum, which are linked to impulsivity and the reward system, are heavily involved in the act of playing online games [ 47 ]. Online game play activates the striatum, which suppresses the left DLPFC in ECN [ 48 ]. As a result, people with IA may find it difficult to control their want to play online games [ 48 ]. This system thus causes impulsive and protracted gaming conduct, lack of inhibitory control leading to the continued use of internet in an overt manner despite a variety of negative effects, personal distress, and signs of psychological dependence [ 33 ] (See Fig 5 ).
Wang et al. (2017) report that disruptions in cognitive control networks within the ECN are frequently linked to characteristics of substance addiction [ 24 ]. With samples that were addicted to heroin and cocaine, previous studies discovered abnormal FC in the ECN and the PFC [ 49 ]. Electronic gaming is known to promote striatal dopamine release, similar to drug addiction [ 50 ]. According to Drgonova and Walther (2016), it is hypothesised that dopamine could stimulate the reward system of the striatum in the brain, leading to a loss of impulse control and a failure of prefrontal lobe executive inhibitory control [ 51 ]. In the end, IA’s resemblance to drug use disorders may point to vital biomarkers or underlying mechanisms that explain how cognitive control and impulsive behaviour are related.
A task-related fMRI study found that the decrease in FC between the left DLPFC and dorsal striatum was congruent with an increase in impulsivity in adolescents with IA [ 26 ]. The lack of response inhibition from the ECN results in a loss of control over internet usage and a reduced capacity to display goal-directed behaviour [ 33 ]. Previous studies have linked the alteration of the ECN in IA with higher cue reactivity and impaired ability to self-regulate internet specific stimuli [ 52 ].
Salience network (SN)/ other networks.
Xing et al. (2014) investigated the significance of the SN regarding cognitive control in teenagers with IA [ 21 ]. The SN, which is composed of the ACC and insula, has been demonstrated to control dynamic changes in other networks to modify cognitive performance [ 21 ]. The ACC is engaged in conflict monitoring and cognitive control, according to previous neuroimaging research [ 53 ]. The insula is a region that integrates interoceptive states into conscious feelings [ 54 ]. The results from Xing et al. (2014) showed declines in the SN regarding its structural connectivity and fractional anisotropy, even though they did not observe any appreciable change in FC in the IA participants [ 21 ]. Due to the small sample size, the results may have indicated that FC methods are not sensitive enough to detect the significant functional changes [ 21 ]. However, task performance behaviours associated with impaired cognitive control in adolescents with IA were correlated with these findings [ 21 ]. Our comprehension of the SN’s broader function in IA can be enhanced by this relationship.
Research study supports the idea that different psychological issues are caused by the functional reorganisation of expansive brain networks, such that strong association between SN and DMN may provide neurological underpinnings at the system level for the uncontrollable character of internet-using behaviours [ 24 ]. In the study by Wang et al. (2017), the decreased interconnectivity between the SN and DMN, comprising regions such the DLPFC and the insula, suggests that adolescents with IA may struggle to effectively inhibit DMN activity during internally focused processing, leading to poorly managed desires or preoccupations to use the internet [ 24 ] (See Fig 5 ). Subsequently, this may cause a failure to inhibit DMN activity as well as a restriction of ECN functionality [ 55 ]. As a result, the adolescent experiences an increased salience and sensitivity towards internet addicting cues making it difficult to avoid these triggers [ 56 ].
The primary aim of this review was to present a summary of how internet addiction impacts on the functional connectivity of adolescent brain. Subsequently, the influence of IA on the adolescent brain was compartmentalised into three sections: alterations of FC at various brain regions, specific FC relationships, and behavioural/developmental changes. Overall, the specific effects of IA on the adolescent brain were not completely clear, given the variety of FC changes. However, there were overarching behavioural, network and developmental trends that were supported that provided insight on adolescent development.
The first hypothesis that was held about this question was that IA was widespread and would be regionally similar to substance-use and gambling addiction. After conducting a review of the information in the chosen articles, the hypothesis was predictably supported. The regions of the brain affected by IA are widespread and influence multiple networks, mainly DMN, ECN, SN and reward pathway. In the DMN, there was a complex mix of increases and decreases within the network. However, in the ECN, the alterations of FC were more unilaterally decreased, but the findings of SN and reward pathway were not quite clear. Overall, the FC changes within adolescents with IA are very much network specific and lay a solid foundation from which to understand the subsequent behaviour changes that arise from the disorder.
The second hypothesis placed emphasis on the importance of between network interactions and within network interactions in the continuation of IA and the development of its behavioural symptoms. The results from the findings involving the networks, DMN, SN, ECN and reward system, support this hypothesis (see Fig 5 ). Studies confirm the influence of all these neural networks on reward valuation, impulsivity, salience to stimuli, cue reactivity and other changes that alter behaviour towards the internet use. Many of these changes are connected to the inherent nature of the adolescent brain.
There are multiple explanations that underlie the vulnerability of the adolescent brain towards IA related urges. Several of them have to do with the inherent nature and underlying mechanisms of the adolescent brain. Children’s emotional, social, and cognitive capacities grow exponentially during childhood and adolescence [ 57 ]. Early teenagers go through a process called “social reorientation” that is characterised by heightened sensitivity to social cues and peer connections [ 58 ]. Adolescents’ improvements in their social skills coincide with changes in their brains’ anatomical and functional organisation [ 59 ]. Functional hubs exhibit growing connectivity strength [ 60 ], suggesting increased functional integration during development. During this time, the brain’s functional networks change from an anatomically dominant structure to a scattered architecture [ 60 ].
The adolescent brain is very responsive to synaptic reorganisation and experience cues [ 61 ]. As a result, one of the distinguishing traits of the maturation of adolescent brains is the variation in neural network trajectory [ 62 ]. Important weaknesses of the adolescent brain that may explain the neurobiological change brought on by external stimuli are illustrated by features like the functional gaps between networks and the inadequate segregation of networks [ 62 ].
The implications of these findings towards adolescent behaviour are significant. Although the exact changes and mechanisms are not fully clear, the observed changes in functional connectivity have the capacity of influencing several aspects of adolescent development. For example, functional connectivity has been utilised to investigate attachment styles in adolescents [ 63 ]. It was observed that adolescent attachment styles were negatively associated with caudate-prefrontal connectivity, but positively with the putamen-visual area connectivity [ 63 ]. Both named areas were also influenced by the onset of internet addiction, possibly providing a connection between the two. Another study associated neighbourhood/socioeconomic disadvantage with functional connectivity alterations in the DMN and dorsal attention network [ 64 ]. The study also found multivariate brain behaviour relationships between the altered/disadvantaged functional connectivity and mental health and cognition [ 64 ]. This conclusion supports the notion that the functional connectivity alterations observed in IA are associated with specific adolescent behaviours as well as the fact that functional connectivity can be utilised as a platform onto which to compare various neurologic conditions.
Limitations/strengths
There were several limitations that were related to the conduction of the review as well as the data extracted from the articles. Firstly, the study followed a systematic literature review design when analysing the fMRI studies. The data pulled from these imaging studies were namely qualitative and were subject to bias contrasting the quantitative nature of statistical analysis. Components of the study, such as sample sizes, effect sizes, and demographics were not weighted or controlled. The second limitation brought up by a similar review was the lack of a universal consensus of terminology given IA [ 47 ]. Globally, authors writing about this topic use an array of terminology including online gaming addiction, internet addiction, internet gaming disorder, and problematic internet use. Often, authors use multiple terms interchangeably which makes it difficult to depict the subtle similarities and differences between the terms.
Reviewing the explicit limitations in each of the included studies, two major limitations were brought up in many of the articles. One was relating to the cross-sectional nature of the included studies. Due to the inherent qualities of a cross-sectional study, the studies did not provide clear evidence that IA played a causal role towards the development of the adolescent brain. While several biopsychosocial factors mediate these interactions, task-based measures that combine executive functions with imaging results reinforce the assumed connection between the two that is utilised by the papers studying IA. Another limitation regarded the small sample size of the included studies, which averaged to around 20 participants. The small sample size can influence the generalisation of the results as well as the effectiveness of statistical analyses. Ultimately, both included study specific limitations illustrate the need for future studies to clarify the causal relationship between the alterations of FC and the development of IA.
Another vital limitation was the limited number of studies applying imaging techniques for investigations on IA in adolescents were a uniformly Far East collection of studies. The reason for this was because the studies included in this review were the only fMRI studies that were found that adhered to the strict adolescent age restriction. The adolescent age range given by the WHO (10–19 years old) [ 65 ] was strictly followed. It is important to note that a multitude of studies found in the initial search utilised an older adolescent demographic that was slightly higher than the WHO age range and had a mean age that was outside of the limitations. As a result, the results of this review are biased and based on the 12 studies that met the inclusion and exclusion criteria.
Regarding the global nature of the research, although the journals that the studies were published in were all established western journals, the collection of studies were found to all originate from Asian countries, namely China and Korea. Subsequently, it pulls into question if the results and measures from these studies are generalisable towards a western population. As stated previously, Asian countries have a higher prevalence of IA, which may be the reasoning to why the majority of studies are from there [ 8 ]. However, in an additional search including other age groups, it was found that a high majority of all FC studies on IA were done in Asian countries. Interestingly, western papers studying fMRI FC were primarily focused on gambling and substance-use addiction disorders. The western papers on IA were less focused on fMRI FC but more on other components of IA such as sleep, game-genre, and other non-imaging related factors. This demonstrated an overall lack of western fMRI studies on IA. It is important to note that both western and eastern fMRI studies on IA presented an overall lack on children and adolescents in general.
Despite the several limitations, this review provided a clear reflection on the state of the data. The strengths of the review include the strict inclusion/exclusion criteria that filtered through studies and only included ones that contained a purely adolescent sample. As a result, the information presented in this review was specific to the review’s aims. Given the sparse nature of adolescent specific fMRI studies on the FC changes in IA, this review successfully provided a much-needed niche representation of adolescent specific results. Furthermore, the review provided a thorough functional explanation of the DMN, ECN, SN and reward pathway making it accessible to readers new to the topic.
Future directions and implications
Through the search process of the review, there were more imaging studies focused on older adolescence and adulthood. Furthermore, finding a review that covered a strictly adolescent population, focused on FC changes, and was specifically depicting IA, was proven difficult. Many related reviews, such as Tereshchenko and Kasparov (2019), looked at risk factors related to the biopsychosocial model, but did not tackle specific alterations in specific structural or functional changes in the brain [ 66 ]. Weinstein (2017) found similar structural and functional results as well as the role IA has in altering response inhibition and reward valuation in adolescents with IA [ 47 ]. Overall, the accumulated findings only paint an emerging pattern which aligns with similar substance-use and gambling disorders. Future studies require more specificity in depicting the interactions between neural networks, as well as more literature on adolescent and comorbid populations. One future field of interest is the incorporation of more task-based fMRI data. Advances in resting-state fMRI methods have yet to be reflected or confirmed in task-based fMRI methods [ 62 ]. Due to the fact that network connectivity is shaped by different tasks, it is critical to confirm that the findings of the resting state fMRI studies also apply to the task based ones [ 62 ]. Subsequently, work in this area will confirm if intrinsic connectivity networks function in resting state will function similarly during goal directed behaviour [ 62 ]. An elevated focus on adolescent populations as well as task-based fMRI methodology will help uncover to what extent adolescent network connectivity maturation facilitates behavioural and cognitive development [ 62 ].
A treatment implication is the potential usage of bupropion for the treatment of IA. Bupropion has been previously used to treat patients with gambling disorder and has been effective in decreasing overall gambling behaviour as well as money spent while gambling [ 67 ]. Bae et al. (2018) found a decrease in clinical symptoms of IA in line with a 12-week bupropion treatment [ 31 ]. The study found that bupropion altered the FC of both the DMN and ECN which in turn decreased impulsivity and attentional deficits for the individuals with IA [ 31 ]. Interventions like bupropion illustrate the importance of understanding the fundamental mechanisms that underlie disorders like IA.
The goal for this review was to summarise the current literature on functional connectivity changes in adolescents with internet addiction. The findings answered the primary research questions that were directed at FC alterations within several networks of the adolescent brain and how that influenced their behaviour and development. Overall, the research demonstrated several wide-ranging effects that influenced the DMN, SN, ECN, and reward centres. Additionally, the findings gave ground to important details such as the maturation of the adolescent brain, the high prevalence of Asian originated studies, and the importance of task-based studies in this field. The process of making this review allowed for a thorough understanding IA and adolescent brain interactions.
Given the influx of technology and media in the lives and education of children and adolescents, an increase in prevalence and focus on internet related behavioural changes is imperative towards future children/adolescent mental health. Events such as COVID-19 act to expose the consequences of extended internet usage on the development and lifestyle of specifically young people. While it is important for parents and older generations to be wary of these changes, it is important for them to develop a base understanding of the issue and not dismiss it as an all-bad or all-good scenario. Future research on IA will aim to better understand the causal relationship between IA and psychological symptoms that coincide with it. The current literature regarding functional connectivity changes in adolescents is limited and requires future studies to test with larger sample sizes, comorbid populations, and populations outside Far East Asia.
This review aimed to demonstrate the inner workings of how IA alters the connection between the primary behavioural networks in the adolescent brain. Predictably, the present answers merely paint an unfinished picture that does not necessarily depict internet usage as overwhelmingly positive or negative. Alternatively, the research points towards emerging patterns that can direct individuals on the consequences of certain variables or risk factors. A clearer depiction of the mechanisms of IA would allow physicians to screen and treat the onset of IA more effectively. Clinically, this could be in the form of more streamlined and accurate sessions of CBT or family therapy, targeting key symptoms of IA. Alternatively clinicians could potentially prescribe treatment such as bupropion to target FC in certain regions of the brain. Furthermore, parental education on IA is another possible avenue of prevention from a public health standpoint. Parents who are aware of the early signs and onset of IA will more effectively handle screen time, impulsivity, and minimize the risk factors surrounding IA.
Additionally, an increased attention towards internet related fMRI research is needed in the West, as mentioned previously. Despite cultural differences, Western countries may hold similarities to the eastern countries with a high prevalence of IA, like China and Korea, regarding the implications of the internet and IA. The increasing influence of the internet on the world may contribute to an overall increase in the global prevalence of IA. Nonetheless, the high saturation of eastern studies in this field should be replicated with a Western sample to determine if the same FC alterations occur. A growing interest in internet related research and education within the West will hopefully lead to the knowledge of healthier internet habits and coping strategies among parents with children and adolescents. Furthermore, IA research has the potential to become a crucial proxy for which to study adolescent brain maturation and development.
Supporting information
S1 checklist. prisma checklist..
https://doi.org/10.1371/journal.pmen.0000022.s001
S1 Appendix. Search strategies with all the terms.
https://doi.org/10.1371/journal.pmen.0000022.s002
S1 Data. Article screening records with details of categorized content.
https://doi.org/10.1371/journal.pmen.0000022.s003
Acknowledgments
The authors thank https://www.stockio.com/free-clipart/brain-01 (with attribution to Stockio.com); and https://www.rawpixel.com/image/6442258/png-sticker-vintage for the free images used to create Figs 2 – 4 .
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. 5 ed. Washington, D.C.: American Psychiatric Publishing; 2013.
- 10. Stats IW. World Internet Users Statistics and World Population Stats 2013 [ http://www.internetworldstats.com/stats.htm .
- 11. Rideout VJR M. B. The common sense census: media use by tweens and teens. San Francisco, CA: Common Sense Media; 2019.
- 37. Tremblay L. The Ventral Striatum. Handbook of Reward and Decision Making: Academic Press; 2009.
- 57. Bhana A. Middle childhood and pre-adolescence. Promoting mental health in scarce-resource contexts: emerging evidence and practice. Cape Town: HSRC Press; 2010. p. 124–42.
- 65. Organization WH. Adolescent Health 2023 [ https://www.who.int/health-topics/adolescent-health#tab=tab_1 .

‘Kafka’ Review: The Man Behind ‘The Metamorphosis’
W as Max Brod the Judas Iscariot of 20th-century literature? The wily, six-part “Kafka” suggests as much, though one can regard both figures as paradoxical: If Judas hadn’t sinned, a mission wouldn’t have been fulfilled. If Brod hadn’t ignored his friend Franz’s request—that he burn the author’s unpublished manuscripts after his death—we would never have had “The Trial,” “The Castle” or “Amerika.”
The loss to readers would have been enormous, certainly. But the act of betrayal was also good for the brand: One can imagine Franz Kafka, detached and double-crossed, declaring from the grave that he expected no less.
It is a devoted Brod (David Kross) whom we see cradling Kafka’s papers aboard the last train across the Czech border in 1939, a sequence out of a wartime thriller yet a bit anomalous to the rest of “Kafka.” Co-written by author Daniel Kehlmann (“Measuring the World”) and David Schalko, directed by Mr. Schalko and airing on ChaiFlicks (the “Jewish Netflix”), the series creates a portrait of the artist—who died 100 years ago this week—with a palette of insecurities, perfectionism, hobbled sexuality and tuberculosis. It finds sources of dry comedy in the domestic life of the bourgeois Kafka family in Prague and in Franz’s romantic catastrophes. It reduces complex psychology to amusing tableaux and incorporates references to Kafka’s novels—the thuggish interrogators of “The Trial,” or the castle from “The Castle”—into Kafka’s oft-represented dreamlife.
But it is Brod who provides the necessary setup to this surreal treatment of a problematic subject, a frame for the picture. A successful and prolific writer of the time (among other things, he translated the libretti of Leoš Janáček into German), he is besotted by the idea of the artistic life—he constantly refers to his literary friends as “the Prague Circle,” though there is no circle, only Kafka (Joel Basman). As a failed artist himself, Brod reveres Franz for his purity and standards and acts as a champion and coach. “Write more!” he urges Franz, who answers that his writing isn’t good. “It will be good enough,” Brod responds, and Franz seizes on the thought, that something only “good enough” could enter the realm of his possibilities.
In what one supposes is reverence to the Kafka aesthetic, the filmmakers—with whom Kafka biographer Reiner Stach acted as consultant—combine the fantastical with the incongruously sober, the fictional with fact: Franz, browbeaten by his brutish father, Hermann (Nicholas Ofczarek), signs a contract to be part owner of his brother-in-law’s asbestos factory with no idea of his duties or authority and finds himself in a situation that might be described as, alas, Kafkaesque, an adjective that remains among Kafka’s more popular contributions to language.
The series, aside from the Brod-dominated episode 1, is focused on various aspects of Kafka’s life, which was short—he was only 40 when he died, in obscurity, of tuberculosis in 1924. The approach is wry, the production design is theatrical, the situations are rendered with absurdity front and center: Franz’s on-again, off-again engagement to Felice Bauer (Lia von Blarer), their relationship based almost entirely on correspondence, is a protracted disaster; Franz is quite comfortable in the brothels of Prague, but incapable of consummating beyond their walls, or with someone he cares for. This becomes more painfully apparent during episode 5, which involves Milena Jesenská (Liv Lisa Fries of “Babylon Berlin”), who has translated the Bohemian Kafka’s writing to Czech from German. Per the series (not all of which is to be taken as gospel), she is ready to leave her husband for “Frank,” as she calls him, before he talks her out of it by overthinking passion. (Ms. Fries steals the scene by visibly withering as he speaks; Mr. Basman’s Frank is insistently odd throughout.) This sets up the most electric moment in the entire show, Milena’s excoriation of Kafka for his cultivated alienation, which she interprets, quite convincingly, as narcissism.
ChaiFlicks, per its mission, is interested in Kafka’s Jewishness and his oft-debated devotion to Zionism—he and Felice discuss a trip to Palestine, which like many of Kafka’s promises never comes true. More biting and even haunting, given the pre- and post-World War I era “Kafka” occupies, is episode 3. In it, Kafka attends a performance by a visiting Yiddish theater troupe and is utterly delighted, even as his friends mock what they see as vulgar kitsch. In a gesture of utter blindness (or bile), Franz brings home one of the actors, Jizchak Löwy (Konstantin Frank), to the Kafka dinner table, where Jizchak regales the family in Yiddish and Hermann is disgusted by the “vermin” his son has allowed to enter his home. It is an affront to Hermann’s assimilated self to have a reminder of his roots come into his house. And how ironic, given that three of Franz’s sisters would die in the Holocaust, no distinction having been made between one Jew or the other.
Mr. Anderson is the Journal’s TV critic.

- Scoping Review
- Open access
- Published: 23 September 2022
Interventions pathways to reduce tuberculosis-related stigma: a literature review and conceptual framework
- Charlotte Nuttall 1 na1 ,
- Ahmad Fuady ORCID: orcid.org/0000-0003-0030-0524 2 , 3 , 4 na1 ,
- Holly Nuttall 1 ,
- Kritika Dixit 5 , 6 ,
- Muchtaruddin Mansyur 2 &
- Tom Wingfield ORCID: orcid.org/0000-0001-8433-6887 1 , 5 , 7 , 8
Infectious Diseases of Poverty volume 11 , Article number: 101 ( 2022 ) Cite this article
6173 Accesses
9 Citations
13 Altmetric
Metrics details
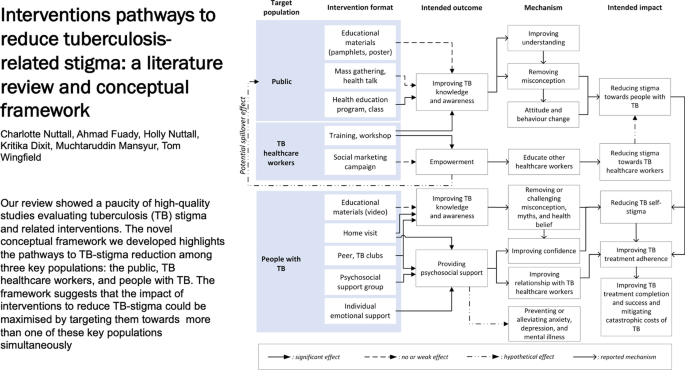
Prevention of tuberculosis (TB)-related stigma is vital to achieving the World Health Organisation’s End TB Strategy target of eliminating TB. However, the process and impact evaluation of interventions to reduce TB-stigma are limited. This literature review aimed to examine the quality, design, implementation challenges, and successes of TB-stigma intervention studies and create a novel conceptual framework of pathways to TB-stigma reduction.
We searched relevant articles recorded in four scientific databases from 1999 to 2022, using pre-defined inclusion and exclusion criteria, supplemented by the snowball method and complementary grey literature searches. We assessed the quality of studies using the Crowe Critical Appraisal Tool, then reviewed study characteristics, data on stigma measurement tools used, and interventions implemented, and designed a conceptual framework to illustrate the pathways to TB-stigma reduction in the interventions identified.
Of 14,259 articles identified, eleven met inclusion criteria, of which three were high quality. TB-stigma reduction interventions consisted mainly of education and psychosocial support targeted predominantly toward three key populations: people with TB, healthcare workers, and the public. No psychosocial interventions for people with TB set TB-stigma reduction as their primary or co-primary aim. Eight studies on healthcare workers and the public reported a decrease in TB-stigma attributed to the interventions. Despite the benefits, the interventions were limited by a dearth of validated stigma measurement tools. Three of eight studies with quantitative stigma measurement questionnaires had not been previously validated among people with TB. No qualitative studies used previously validated methods or tools to qualitatively evaluate stigma. On the basis of these findings, we generated a conceptual framework that mapped the population targeted, interventions delivered, and their potential effects on reducing TB-stigma towards and experienced by people with TB and healthcare workers involved in TB care.
Conclusions
Interpretation of the limited evidence on interventions to reduce TB-stigma is hampered by the heterogeneity of stigma measurement tools, intervention design, and outcome measures. Our novel conceptual framework will support mapping of the pathways to impacts of TB-stigma reduction interventions.
Graphical Abstract
Stigma experienced by people with or affected by tuberculosis (TB)—henceforth termed TB-stigma—remains one of the major challenges in TB control [ 1 , 2 ]. TB-stigma has been shown to delay health-seeking behaviour [ 3 ]. This challenge has been aggravated by the COVID-19 pandemic which has restricted access to healthcare, reduced the number of people notified with TB, and been associated with an increase in TB mortality [ 1 , 4 , 5 ]. TB-stigma has also been shown to reduce treatment compliance, and negatively impact on TB treatment outcomes [ 6 , 7 ]. The prevalence of TB-stigma varies geographically and, in specific subpopulations, has been estimated to affect up to 80% of people with TB [ 8 , 9 ]. Therefore, in the context of TB control, TB-stigma is one of the major social determinants of health and contributes to compounding health inequalities [ 1 , 10 , 11 ].
For these reasons, the Global Fund and UN high-level meeting highlighted TB-Stigma as one of the most significant barriers to reaching the World Health Organization (WHO) End TB goal of eliminating TB by 2050 and called on the international community to “promote and support an end to stigma and all forms of discrimination” [ 12 , 13 , 14 ]. Despite this, few resources have been mobilised to address this issue [ 15 ]. In part, this is due to inherent difficulties in the identification and measurement of TB-Stigma and the complexity and limited evidence base relating to stigma-reduction interventions [ 16 ].
Measuring stigma is vital to understand its determinants, prevalence and assess the effectiveness of stigma-reduction interventions [ 17 ]. Multiple scales and tools exist that assess health-related stigma [ 18 ]. To be robust and reliable, these tools should have been validated in the community or population in which they are to be used and then refined to ensure they are accurate, specific, and reliable. In 2018, the KNCV Tuberculosis Foundation created a TB-Stigma Handbook, which provides examples of how the limited available set of existing tools can best be applied to measure and evaluate stigma [ 19 ]. However, most studies to date have used either disparate, invalidated tools or solely qualitative measures of stigma. This has made it difficult to broaden our understanding of the determinants and consequences of TB-Stigma [ 15 , 20 ] (Box 1 ).
In addition, despite recognition of the global importance of TB-stigma, there has been limited critical appraisal in the literature of the few existing interventions aimed at reducing TB-stigma. The single related systematic review on TB-Stigma by Sommerland et al. focused on the effectiveness of stigma-reduction interventions [ 17 ]. Measuring and reducing TB-Stigma is complex. It involves interrelated, heterogeneous system structures, and multiple approaches from the individual to societal level [ 16 ]. Therefore, it is critical to evaluate not only the scale but also the challenges and successes in the design and implementation processes of interventions to reduce TB-stigma. These evaluations will help identify the weaknesses in current TB-stigma intervention design and delivery in order to refine these interventions for future implementation and scale-up.
We reviewed studies reporting interventions to reduce TB-Stigma. The review appraised the study design and stigma measurement tools, identified their challenges and successes, and evaluated their pathways to impact on TB-Stigma. We then developed a conceptual framework for the TB-Stigma reduction pathway to support researchers to successfully design and deliver impactful TB-stigma reduction interventions.
Box 1 Types of TB-stigma [ 18 ]
Enacted (or experienced) stigma encompasses the range of behaviours directly experienced by a person with TB.
Anticipated stigma is the expectation and fear of discrimination and behaviour of others towards a person if they are diagnosed and/or unwell with TB, which has an impact on health-seeking behaviour, whether enacted stigma occurs or not.
Internalised (or self) stigma is when those diagnosed and/or unwell with TB may accept a negative stereotype about people with TB and potentially act in a way that endorses this stereotype.
Secondary or external stigma is negative attitude towards family members, caregivers, friends, or TB healthcare workers because they are associated with, live with, or have close contact with people with TB.
This study was a systematic literature review. A preliminary scoping search was conducted to ensure that all relevant key terms were identified, and the final search strategy refined.
Search terms and management of search results
The following search terms were used within four databases (CINAHL Complete, Medline Complete, Global Health and PubMed): (TB OR Tubercul* OR “Mycobacterium tuberculosis infections”) AND (stigma* OR discrimin* OR “social stigma” OR barrier* OR attitude* OR “social discrimination” OR marginalisation OR “psychosocial impact” OR “socioeconomic impact” OR shame OR “social isolation” OR “social inclusion” OR prejudice OR perception OR “self-esteem”) AND (interven* OR strateg* OR pathway* OR education OR “psychosocial intervention*” OR “psychoemotional intervention*” OR “socioeconomic intervention*” OR “social support” OR “patient support” OR “training workshop*” OR “counselling”) were searched. In addition, the “snowballing” method of reference tracking and searches of Google Scholar and the WHO database for grey literature were used to identify additional articles that may have been overlooked by the initial search strategy. Searches were limited to December 31, 2021. Citations of the articles identified from the searches were exported into Endnote X9 (Camelot UK Bidco Limited/Clarivate, UK). Duplicates were then identified and removed using the duplicates tool in Endnote X9. The titles and abstracts of the remaining articles were read through and screened for relevance independently by three reviewers (CN, HN, AF). Where there were unresolved disagreements, a fourth senior reviewer finalized screening for inclusion or exclusion (TW). We applied the inclusion and exclusion criteria, documented the reasons for article exclusion, and identified the relevant articles for full-text review. Finally, supplemental manual review of the reference lists of the selected full-text articles was performed to identify any further articles for inclusion.

Selection criteria
Eligible studies included those that reported the implementation and evaluation of TB-stigma reduction interventions amongst people with TB and their households, healthcare workers, and the general public. Included study designs were intervention studies with randomised controlled trials, non-randomised controlled trials, quasi-experimental studies, mixed-methods studies, qualitative studies, cohort studies, case-control studies, and cross-sectional studies. The review was restricted to articles that were written in English. Articles were excluded if they did not report measurement of stigma.
Critical appraisal
Critical appraisal was undertaken by three reviewers (CN, HN, AF) using the “Crowe Critical Appraisal Tool” (CCAT), Version 1.4, to determine the quality of each study [ 21 ]. The CCAT was selected as it has been proven to be reliable and valid for the analysis of multiple studies of heterogenous design and implementation approaches, and can reduce rater bias [ 22 ]. To further reduce researcher bias, each individual assessment was cross-checked. A fourth reviewer (TW) resolved any discrepancies. A priori, and in line with published guidance [ 21 ], a pragmatic decision was taken by the study team that articles with a CCAT score between 75% and 100% would be deemed high quality, 50% and 74% moderate, and below 50% to be low quality.
Data extraction and synthesis
Data on country and region of intervention, target population, type of stigma studied, the scale or tool used to assess stigma, intervention activities, challenges and successes of intervention, the impact of intervention, and reported changes to TB practice and policy were collated and tabulated. Further information on the intervention including format, content, outcomes (both reported and intended if different) and detail on how the intervention reduced TB-stigma (theory explicitly stated in the main text or implied in objectives or methods) were also tabulated. Qualitative details were lifted directly from the text and copied into the data-extraction table. The articles were read carefully for similar and recurring themes and concepts. The concepts were then organised to determine any contradictory concepts, which were then removed. A conceptual framework was then created to organise the variables and concepts perceived by the research team to contribute to the pathways by which an intervention successfully reduced TB-stigma. The intention of the novel conceptual framework was to support researchers to design, develop, and implement a successful and sustainable stigma-reduction intervention in current and future studies [ 23 ]. With respect to stigma measurement tools and scales, these were evaluated through collection of data including: the tool or scale used; implementation methods; methods to reduce bias and ensure validity; internal and external validation and piloting prior to use; comparison of stigma scores before and after the intervention or between study groups; types of stigma assessed; whether the tool was adapted from a previously validated tool; and the described limitations of the tool. Any required data that was missing from the published papers was collected by directly contacting the corresponding author of the paper.
The search yielded 14,244 articles with 15 further articles identified from other sources including grey literature. After removal of duplicate articles, 10,954 were screened, 54 of which met the study inclusion criteria. Following the full-text eligibility assessment, 43 further articles were excluded (Additional file 1 ). The remaining 11 articles were included for critical appraisal in the systematic review (Fig. 1 ).
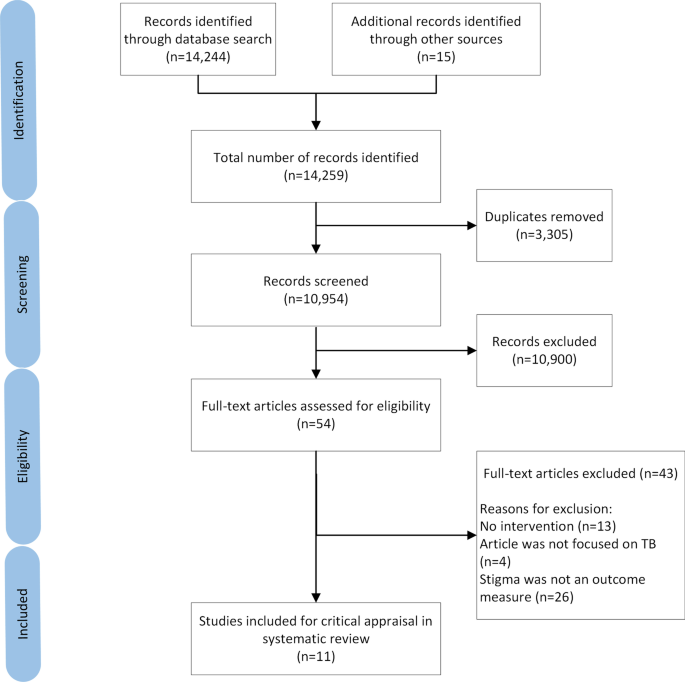
PRISMA flow diagram of study identification, screening, and inclusion in review. Other sources of articles refer to those identified through the Stop TB Partnership website, KNCV Tuberculosis foundation database, and the snowball method
Quality assessment
The median CCAT score for quality of studies was 24/40 (range 15–38) (Additional file 1 ). Three studies were classified as high quality [ 24 , 25 , 26 ]. The predominant reasons for lower quality scoring were lack of details relating to methods and study protocols including sampling frames and ethical approval.
Study characteristics
There was marked heterogeneity in the study characteristics in terms of study aims, designs, population and region/sites, and type of stigma measured (Table 1 ). The studies were conducted in low- ( n = 1) [ 27 ], middle- ( n = 9) [ 24 , 25 , 26 , 28 , 29 , 30 , 31 , 32 , 33 ], and high-income ( n = 1) countries [ 34 ]. Two studies were conducted in the same country (Peru) [ 30 , 31 ], and these studies were linked with some overlap of study team members and co-authors. The studies were targeted at a variety of different populations including people with TB and MDR-TB and their households ( n = 5), HCWs ( n = 3), and the public ( n = 3).
Study population, aims and intervention
Six studies applied interventions targeted towards people with TB. Five of the studies aimed to improve TB treatment compliance and completion through psychosocial support interventions, which were TB clubs or support groups ( n = 3) [ 28 , 29 , 30 ], nurse support ( n = 1) [ 31 ], and household counselling ( n = 1) [ 26 ], while one study focused on improving TB knowledge [ 33 ].
TB clubs involved group meetings of people diagnosed with TB to discuss their experiences and provide mutual support to encourage each other through their illness and treatment. Other studies initiated patient-centred home visits by HCWs to complement the TB clubs [ 30 ], provided individualised emotional support from community nurses who informed and educated people with TB and their households about TB [ 31 ], and implemented a household counselling intervention delivered by nurses and trained counsellors [ 26 ]. All of the studies tailored towards people with TB captured stigma related to being diagnosed with TB. The assessment focused on measuring enacted and internalised stigma and, where possible, the influence of such stigma on TB treatment success rates. Two of the studies also involved family members of people with TB: one to evaluate stigma [ 26 ] and another to evaluate people with TB and their family members’ TB knowledge following delivery of educational videos while waiting at TB outpatient clinic appointments [ 33 ].
Two studies evaluated stigma among HCWs using workshops focused on distinct aspects of stigma [ 24 , 34 ]. One delivered nationwide TB training workshops to educate HCWs on TB, stigma and human rights to improve knowledge on TB and reduce TB-stigma towards people with TB [ 34 ]. In another, there was a focus on healthcare workers who were themselves stigmatised by other HCWs [ 24 ]. This study measured external or secondary stigma, in which HCWs experience negative attitudes or rejection because of the care they have given to people with TB.
Three studies assessed anticipated TB-Stigma among the public: two in an adult population and one in an adolescent population. All the studies measured anticipated TB-stigma using before-after intervention designs. Two studies applied health education programs in the community (mass information programs and health promotion at mass gatherings) [ 27 , 32 ]. Another study delivered training to students and evaluated whether the training reduced their levels of anticipated TB-stigma [ 25 ].
Stigma measurement tools
Eight studies used quantitative questionnaires to measure stigma (Table 2 ) [ 24 , 25 , 26 , 27 , 28 , 32 , 33 , 34 ]. The format of the questionnaires to measure stigma varied widely including the number of questions asked (range 3–14 questions). Three of the questionnaires were adapted from tools that were not specific to any particular disease and had been previously validated but not among people with TB [ 28 , 29 , 34 ]. For example, Macq et al . adapted their questionnaire from the Boyd Ritsher Mental Illness stigma scale and pre-tested it 2 years before the intervention study to improve its internal validity [ 28 ]. One study piloted the tools in six different communities (four Zambian and two South African) with six different languages (Nyanja, Bemba, Tonga, isiXhosa, Afrikaans and English) [ 26 ]. Four other studies piloted their questionnaires in a single population each [ 24 , 25 , 27 , 28 , 35 ].
Most studies ( n = 7) applied the tool before and after a stigma-reduction or related intervention with the time period between the first and second application varying from 4 weeks to 18 months [ 24 , 25 , 26 , 28 , 32 , 33 , 34 ]. One quantitative study did not evaluate stigma before the intervention [ 27 ]. The study was an evaluation of an extensive mass health education programme that was implemented for 2–3 years in one case study area and compared to another control study area with a limited health education programme.
Four studies used qualitative methods, such as focus group discussions, interviews and observation, to evaluate stigma [ 24 , 29 , 30 , 31 ]. No studies used previously validated methods or tools to qualitatively evaluate stigma. However, the qualitative approaches focused less on measurement of stigma and more on exploring how people with TB attempted to combat the stigma perceived by themselves [ 29 ] or by other people [ 30 ], and how HCWs who work with people with TB struggled to deal with stigmatisation from other HCWs [ 24 ].
Challenges, successes, and outcomes
Implementation and delivery challenges and process indicators such as fidelity, acceptability, and feasibility were infrequently measured or reported in the studies. One study caused a positive change to national practice with the production of a manual to expand the intervention to a wider population [ 28 ]. Three studies reported that a success of the intervention was that sustainable changes had been made within the study site communities [ 26 , 29 , 33 ]. However, there was no objective way to measure or verify these changes from the data presented within the study articles.
Four of the studies explicitly stated that their intervention was limited by geographical challenges including some populations not being reached by the intervention [ 25 , 27 , 28 , 32 ]. This limited the external validity of the data. Three studies mentioned challenges concerning maintenance and sustainability of the programmes, including identifying participants to take part in the intervention and motivating people to continue engaging with the intervention [ 30 , 31 , 34 ]. Another study mentioned that inviting all HCWs to participate in a workshop about TB was problematic because hospitals were busy and understaffed [ 24 ]. The intervention itself was also challenged by issues relating to professional rank, position, and social status of different HCWs, which was perceived as limiting open discussion about the optimal ways to address stigma between HCWs (Table 3 ).
Pathways to impact of TB-stigma interventions
Synthesising learning from the interventions and outcomes, we found distinct pathways to reduce stigma depending on the population targeted by the intervention. We created a novel conceptual framework to illustrate these pathways (Fig. 2 ).
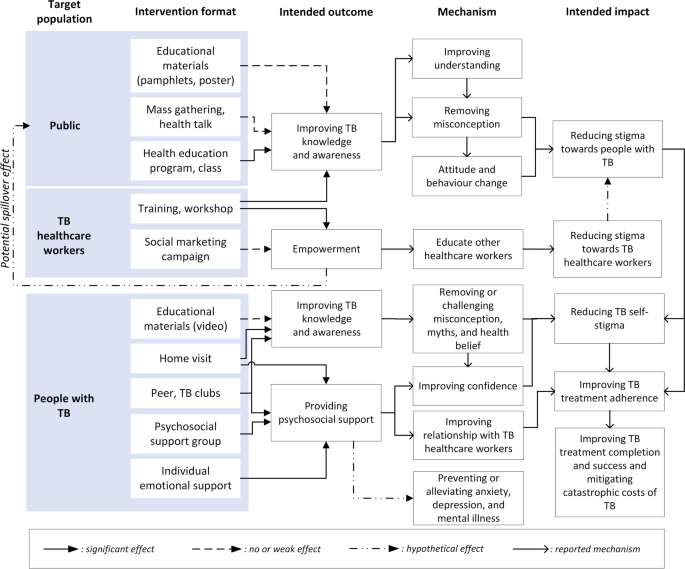
Among people with TB, stigma is a negative effect of being ill with TB, diagnosed with TB, and being on TB treatment. Stigma towards people with TB can develop in three other populations: the public, TB-related HCWs, and other HCWs. The interventions for people with TB improved TB knowledge, reduced myth and misconception related to TB, increased confidence of people with TB, and thereby reduced internalised stigma experienced by people with TB [ 28 , 29 , 30 , 31 , 33 ]. These effects directly supported people with TB to comply with and complete TB treatment. Another study showed that, although household counselling was not specifically designed to, or found to, reduce TB-Stigma [ 26 ], health counsellors can help households manage the consequence of TB-Stigma. The main challenge in providing household counselling, particularly in communities with high levels of TB-stigma, is that the visits themselves may trigger anticipated, internalised, or enacted stigma.
Training to TB HCWs improved the HCWs’ knowledge, attitude, and practice towards people with TB [ 34 ], which may contribute to improved TB care. Conversely, our review found that TB-related HCWs were often stigmatised by other HCWs [ 24 ]. Training HCWs who care for people with TB to educate other HCWs is likely to support dissemination of knowledge and accurate information about TB-Stigma in their workplace. Although the training failed to reduce external or secondary stigma, there was a potential spill over effect that TB-related HCWs could have used the campaign materials to educate people living in their neighbourhood.
Interventions targeted towards the general public had positive impacts on knowledge, attitudes and practice related to TB as measured by knowledge, attitude, and practice (KAP) and stigma scores [ 25 , 27 , 32 ]. Mass TB education to the public was expected to increase TB knowledge and remove TB misconceptions which could result in improved community attitudes and reduced stigma towards people with TB. However, the evidence found in this review suggested that misconceptions about TB persisted, even worsened, if health education through pamphlets or posters were too short and failed to convey accurate public health messages [ 32 ].
This literature review found that, despite the global importance of addressing TB-Stigma, there is a paucity of high-quality studies evaluating interventions to reduce TB-stigma. Intervention design across studies was heterogeneous, but education about TB frequently featured as a core intervention activity. Assessment of the impact of interventions on TB-stigma reduction was limited by a lack of well-validated tools to measure stigma. The novel conceptual framework highlighted that people with TB may experience stigma from three different populations around them: the public, TB HCWs, and other HCWs. The ideal and possibly most synergistic interventions to reduce TB-Stigma would be optimized by delivering interventions targeted towards more than one key populations at the same time.
There has been an increasing awareness of the importance of combatting TB-Stigma in recent years. This study may not have captured stigma-reduction interventions or programs at local, sub-national, or national levels due to such programs not being executed, evaluated, or reported systematically, which makes them difficult to review and compare. Among the limited studies identified, this review found that research on TB-stigma was often hampered by suboptimal design and methods for implementation and evaluation.
This review complements the Sommerland et al . paper[ 17 ] and extends its findings through a specific focus on the tools used to measure stigma reduction, a qualitative evaluation of the potential reasons underlying the success or failure of the interventions, and the creation of a novel conceptual framework of the pathways to intervention impact. By this approach, this review highlights that most TB-stigma intervention studies used tools that lacked appropriate validation. This finding is consistent with other published studies [ 36 , 37 , 38 , 39 ]. Using reliable, validated stigma measurement tools and methods is important and helps measure stigma accurately and consistently. It also enables the comparison of impact evaluation of stigma reduction interventions across studies and contexts. There is a list of available tools that can be used and validated [ 19 ], including Van Rie’s TB-Stigma Scale [ 40 ], one of the most adapted questionnaires to assess stigma [ 38 ], which may support researchers and implementers designing TB-stigma reduction programmes in the future.
Using qualitative approaches to measure TB-stigma has both strengths and limitations. This approach cannot precisely assess the reduction of stigma after the intervention. However, it can help explore more profound dimensions of stigma and its impact on people with TB and their households. For example, qualitative studies have been able to elicit key emotional responses to TB-Stigma, including shock, fear of being isolated or abandoned by a spouse, shame related to becoming weak and incapable of working, worry relating to loneliness, and desperation related to thoughts about TB-related death [ 29 , 30 ]. Therefore, interventions incorporating mixed methods process evaluations would be both prudent and beneficial.
The conceptual framework we have generated can support understanding of the pathways through which interventions successfully reduce stigma and the parties affected. It is notable that interventions rarely have stigma-reduction as a primary aim or objective. Rather, programs often cite stigma reduction as a bridge towards TB treatment compliance, completion, and success. This may be short-sighted: besides improving treatment completion, psychosocial support is also important to prevent or alleviate anxiety, depression, and mental illness, which are well established correlates of being affected by TB [ 41 , 42 ]. Not having stigma reduction as a primary or even co-primary outcome may have contributed to a lack of focus on using validated instruments to measure stigma. Given that global TB policy strongly recommends interventions to reduce TB-stigma [ 43 , 44 ], it is vital that appropriately validated tools be used to measure stigma and that reduction of stigma be considered as a key individual-level outcome for people affected by TB.
The framework shows that the interventions on TB HCWs are also critical and may have potential spill over effects to other healthcare workers and the general public. TB HCWs often face secondary stigma and may be at risk of a psychosocial impact of TB themselves, particularly in areas with high co-prevalence of HIV/AIDS and TB [ 45 , 46 ]. TB-stigma interventions for HCWs can be challenging to implement because they may encounter power structure problems against colleagues with higher professional rank, position, and status [ 24 ]. However, HCWs are well placed to convey anti-stigma messages to their surrounding communities and should be empowered to do so.
The framework also emphasises the potential role for synergy across different pathways of TB-stigma reduction to enhance the effectiveness of interventions. For example, improvements in community and HCWs’ KAP are likely to reduce enacted stigma. Concurrently improving people with TB’s KAP is also expected to mitigate internalised and anticipated stigma. This implies that the ideal and possibly most synergistic intervention would be optimized by delivering interventions to more than one key population. TB clubs, for example, often only benefit people with TB. Stigma-reduction activities and interventions should aim to be more inclusive where possible with HCWS and/or community members being encouraged to attend and participate in TB club meetings, helping to act on all three forms of stigma.
Given that social and economic determinants and consequences of TB are now recognised as significant limiting factors for ending TB, it is notable that there is no recognised national or global indicator for TB-stigma [ 47 ]. Currently, there is a global indicator of TB-related catastrophic costs. This indicator has already proven highly useful within research and National TB Programme activities [ 48 ] and has led to the creation of a WHO database of the financial burden of TB for more than twenty countries [ 1 ]. The same approach should be taken to document the psychosocial burden of TB-stigma across countries. We would strongly advocate for a unified, adaptable global TB-stigma indicator. It could support research and activities to gather data on the prevalence of stigma in different countries or regions. It would also eventually garner further resource investment and scientific interest and heighten much-needed advocacy in this field.
This study has several limitations. First, due to the heterogeneity of study designs, quality, interventions, and tools used, it was not possible to quantitatively determine the effectiveness of interventions. While this was a weakness, the focus was on qualitative assessment of the studies. Second, only articles written in English were included, therefore, some relevant literature may have been missed, particularly of research performed in high TB burden countries in which English is not the first language. Third, paper quality was moderate, and some papers had missing data, which—despite contacting corresponding authors—was not made available for analysis. As our analysis suggested that most papers included were of only low or moderate quality, the power of this review to make conclusions about study impacts is limited [ 49 ]. Fourth, we were not able to include studies of complex interventions that aimed to minimise both the psychosocial (e.g. stigma) and economic (e.g. catastrophic costs) of TB, such as the randomised-controlled HRESIPT and CRESIPT studies in Peru [ 50 , 51 , 52 ]. While TB treatment, prevention, and economic outcomes from these studies are available, the impact of these interventions on stigma is not yet known. While publication bias is a limitation of any review of the published literature, we attempted to mitigate this bias through a comprehensive grey literature review. Despite the comprehensive evaluation of stigma reduction interventions, this review and framework could not capture the complexity of stigma, which—from a social perspective—involves a set of interrelated, heterogeneous system structures [ 16 ].
Despite the global importance of addressing TB-Stigma, there is a paucity of high-quality studies evaluating interventions to reduce TB-stigma. The novel conceptual framework highlighted that people with TB may experience internalized stigma and anticipated or enacted stigma from three different populations around them: the public, TB HCWs, and other HCWs. Interventions for people with TB can effectively provide psychosocial support for treatment completion. Interventions on HCWs can enhance the support provided for people with TB, and interventions for the public have the potential to reduce community-level stigma toward people with TB. The ideal and possibly most synergistic intervention would be optimized by delivering interventions to more than one key population. Finally, our findings reinforce that it is vital to promote stigma as an indicator in national and international TB strategies to strengthen the development and evaluation of stigma-reducing interventions.
Availability of data and materials
Data generated or analysed during this study are included in this published article and its additional information files.
World Health Organization. Global tuberculosis report 2021. Geneva: World Health Organization; 2021.
Google Scholar
Datiko DG, Jerene D, Suarez P. Stigma matters in ending tuberculosis: nationwide survey of stigma in Ethiopia. BMC Public Health. 2020;20(1):190.
Article PubMed PubMed Central Google Scholar
Teo AKJ, Singh SR, Prem K, Hsu LY, Yi S. Duration and determinants of delayed tuberculosis diagnosis and treatment in high-burden countries: a mixed-methods systematic review and meta-analysis. Respir Res. 2021;22(1):251.
Pai M, Kasaeva T, Swaminathan S. COVID-19’s devastating effect on tuberculosis care—a path to recovery. N Engl J Med. 2022;386:1490–3.
Article CAS PubMed Google Scholar
Chapman HJ, Veras-Estévez BA. Lessons learned during the COVID-19 pandemic to strengthen TB Infection control: a rapid review. Glob Health Sci Pract. 2021;9(4):964–77.
Chang SH, Cataldo JK. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. Int J Tuberc Lung Dis. 2014;18(2):168–73.
Article PubMed Google Scholar
Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007;4(7): e238.
Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(4_suppl):34–42.
Chowdhury MRK, Rahman MS, Mondal MNI, Sayem A, Billah B. Social impact of stigma regarding tuberculosis hindering adherence to treatment: a cross sectional study involving tuberculosis patients in Rajshahi City, Bangladesh. Jpn J Infect Dis. 2015;68(6):461–6.
Bonadonna LV, Saunders MJ, Zegarra R, Evans C, Alegria-Flores K, Guio H. Why wait? The social determinants underlying tuberculosis diagnostic delay. PLoS One. 2017;12(9):e0185018.
Craig GM, Daftary A, Engel N, O’Driscoll S, Ioannaki A. Tuberculosis stigma as a social determinant of health: a systematic mapping review of research in low incidence countries. Int J Infect Dis. 2017;56:90–100.
World Health Organization. The end TB strategy. Geneva: World Health Organization; 2015.
The Global Fund. Tuberculosis and human right. In: The UN General Assembly high-level meeting on ending TB. The Global Fund; 2018.
United Nations. United Nations high-level meeting on the fight against tuberculosis. New York: United Nations; 2018.
Macintyre K, Bakker MI, Bergson S, Bhavaraju R, Bond V, Chikovore J, et al. Defining the research agenda to measure and reduce tuberculosis stigmas. Int J Tuberc Lung Dis. 2017;21(11):S87–96.
Article Google Scholar
Pescosolido BA, Martin JK. The stigma complex. Ann Rev Sociol. 2015;41(1):87–116.
Sommerland N, Wouters E, Mitchell EMH, Ngicho M, Redwood L, Masquillier C, et al. Evidence-based interventions to reduce tuberculosis stigma: a systematic review. Int J Tuberc Lung Dis. 2017;21(11):S81–6.
Partnership STB. TB stigma assessment: implementation handbook. Geneva: Stop TB Partnership; 2019.
Challenge TB. TB stigma measurement guidance. Den Haag: KNCV; 2018.
Hartog K, Hubbard CD, Krouwer AF, Thornicroft G, Kohrt BA, Jordans MJD. Stigma reduction interventions for children and adolescents in low- and middle-income countries: systematic review of intervention strategies. Soc Sci Med. 2020;246: 112749.
Crowe M. Crowe Critical Appraisal Tool (CCAT) v 1.4. Queensland; 2013.
Crowe M, Sheppard L. A general critical appraisal tool: an evaluation of construct validity. Int J Nurs Stud. 2011;48(12):1505–16.
Thapa S, Hannes K, Cargo M, Buve A, Aro AR, Mathei C. Building a conceptual framework to study the effect of hiv stigma-reduction intervention strategies on HIV test uptake: a scoping review. J Assoc Nurses AIDS Care. 2017;28(4):545–60.
Sommerland N, Masquillier C, Rau A, Engelbrecht M, Kigozi G, Pliakas T, et al. Reducing HIV- and TB-stigma among healthcare co-workers in South Africa: results of a cluster randomised trial. Soc Sci Med. 2020;266: 113450.
Idris NA, Zakaria R, Muhamad R, Nik Husain NR, Ishak A, Wan Mohammad WMZ. The effectiveness of tuberculosis education programme in Kelantan, Malaysia on knowledge, attitude, practice and stigma towards tuberculosis among adolescents. Malays J Med Sci. 2020;27(6):102–14.
PubMed PubMed Central Google Scholar
Bond V, Floyd S, Fenty J, Schaap A, Godfrey-Faussett P, Claassens M, et al. Secondary analysis of tuberculosis stigma data from a cluster randomised trial in Zambia and South Africa (ZAMSTAR). Int J Tuberc Lung Dis. 2017;21(11):49–59.
Croft RP, Croft RA. Knowledge, attitude and practice regarding leprosy and tuberculosis in Bangladesh. Lepr Rev. 1999;70(1):34–42.
CAS PubMed Google Scholar
Macq J, Solis A, Martinez G, Martiny P. Tackling tuberculosis patients’ internalized social stigma through patient centred care: an intervention study in rural Nicaragua. BMC Public Health. 2008;8:154–154.
Demissie M, Getahun H, Lindtjørn B. Community tuberculosis care through “TB clubs” in rural North Ethiopia. Soc Sci Med. 2003;56(10):2009–18.
Acha J, Sweetland A, Guerra D, Chalco K, Castillo H, Palacios E. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health. 2007;2(4):404–17.
Chalco K, Wu DY, Mestanza L, Muñoz M, Llaro K, Guerra D, et al. Nurses as providers of emotional support to patients with MDR-TB. Int Nurs Rev. 2006;53(4):253–60.
Balogun M, Sekoni A, Meloni ST, Odukoya O, Onajole A, Longe-Peters O, et al. Trained community volunteers improve tuberculosis knowledge and attitudes among adults in a periurban community in southwest Nigeria. Am J Trop Med Hyg. 2015;92(3):625–32.
Wilson JW, Ramos JG, Castillo F, Castellanos EF, Escalante P. Tuberculosis patient and family education through videography in El Salvador. J Clin Tuberc Other Mycobact Dis. 2016;4:14–20.
Wu PS, Chou P, Chang NT, Sun WJ, Kuo HS. Assessment of changes in knowledge and stigmatization following tuberculosis training workshops in taiwan. J Formos Med Assoc. 2009;108(5):377–85.
Wouters E, Rau A, Engelbrecht M, Uebel K, Siegel J, Masquillier C, et al. The development and piloting of parallel scales measuring external and internal HIV and tuberculosis stigma among healthcare workers in the Free State Province, South Africa. Clin Infect Dis. 2016;62(suppl_3):S244–54.
Sommerland N, Wouters E, Mitchell EMH, Ngicho M, Redwood L, Masquillier C, et al. Evidence-based interventions to reduce tuberculosis stigma: a systematic review. Int J Tuberc Lung Dis. 2017;21(11):81–6.
Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–87.
Bergman A, McNabb K, Farley JE. A systematic review and psychometric appraisal of instruments measuring tuberculosis stigma in Sub-Saharan Africa. Stigma Health. 2021. https://doi.org/10.1037/sah0000328 .
MacKenzie SB, Podsakoff PM, Podsakoff NP. Construct measurement and validation procedures in MIS and behavioral research: integrating new and existing techniques. MIS Q. 2011;35(2):293–334.
Van Rie A, Sengupta S, Pungrassami P, Balthip Q, Choonuan S, Kasetjaroen Y, et al. Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: exploratory and confirmatory factor analyses of two new scales. Trop Med Int Health. 2008;13(1):21–30.
Koyanagi A, Vancampfort D, Carvalho AF, DeVylder JE, Haro JM, Pizzol D, et al. Depression comorbid with tuberculosis and its impact on health status: cross-sectional analysis of community-based data from 48 low- and middle-income countries. BMC Med. 2017;15(1):209–209.
Naidu T, Pillay SR, Ramlall S, Mthembu SS, Padayatchi N, Burns JK, et al. Major depression and stigma among individuals with multidrug-resistant tuberculosis in South Africa. Am J Trop Med Hyg. 2020;103(3):1067–71.
Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(Suppl 4):34–42.
Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health. 2007;7(1):211.
Wouters E, Sommerland N, Masquillier C, Rau A, Engelbrecht M, van Rensburg AJ, et al. Unpacking the dynamics of double stigma: how the HIV-TB co-epidemic alters TB stigma and its management among healthcare workers. BMC Infect Dis. 2020;20(1):106.
Rau A, Wouters E, Engelbrecht M, Masquillier C, Uebel K, Kigozi G, et al. Towards a health-enabling working environment—developing and testing interventions to decrease HIV and TB stigma among healthcare workers in the Free State, South Africa: study protocol for a randomised controlled trial. Trials. 2018;19(1):351.
Lönnroth K, Glaziou P, Weil D, Floyd K, Uplekar M, Raviglione M. Beyond UHC: monitoring health and social protection coverage in the context of tuberculosis care and prevention. PLoS Med. 2014;11(9): e1001693.
Viney K, Islam T, Hoa NB, Morishita F, Lönnroth K. The financial burden of tuberculosis for patients in the Western-Pacific region. Trop Med Infect Dis. 2019;4(2):94.
Article PubMed Central Google Scholar
Peters SE, Johnston V, Coppieters MW. Interpreting systematic reviews: looking beyond the all too familiar conclusion. J Hand Ther. 2014;27(1):1–3.
Wingfield T, Tovar MA, Huff D, Boccia D, Montoya R, Ramos E, et al. Socioeconomic support to improve initiation of tuberculosis preventive therapy and increase tuberculosis treatment success in Peru: a household-randomised, controlled evaluation. Lancet. 2017;389:S16.
Wingfield T, Tovar MA, Huff D, Boccia D, Montoya R, Ramos E, et al. A randomized controlled study of socioeconomic support to enhance tuberculosis prevention and treatment, Peru. Bull World Health Organ. 2017;95(4):270.
Wingfield T, Tovar MA, Huff D, Boccia D, Montoya R, Ramos E, et al. The economic effects of supporting tuberculosis-affected households in Peru. Eur Respir J. 2016;48(5):1396–410.
Download references
Acknowledgements
Not applicable.
TW is supported by grants from the Wellcome Trust, UK (209075/Z/17/Z), the Medical Research Council, Department for International Development, and Wellcome Trust (Joint Global Health Trials, MR/V004832/1), and a Dorothy Temple Cross Tuberculosis International Collaboration Grant from the Medical Research Foundation, UK. AF and TW are recipients of a Royal Society of Tropical Medicine and Hygiene early career research grant.
Author information
Charlotte Nuttall and Ahmad Fuady joint first authors with equal contribution
Authors and Affiliations
Department of Clinical Infection, Microbiology and Immunology, University of Liverpool, Liverpool, UK
Charlotte Nuttall, Holly Nuttall & Tom Wingfield
Department of Community Medicine, Faculty of Medicine, Universitas Indonesia, 10310, Jakarta, Indonesia
Ahmad Fuady & Muchtaruddin Mansyur
Department of Public Health, Erasmus MC University Medical Center Rotterdam, 3015GD, Rotterdam, The Netherlands
Ahmad Fuady
Primary Health Care Research and Innovation Center, Indonesian Medical Education and Research Institute, Faculty of Medicine Universitas Indonesia, 10430, Jakarta, Indonesia
Social Medicine, Infectious Diseases, and Migration (SIM) Group, Department of Public Health Sciences, Karolinska Institute, 10653, Stockholm, Sweden
Kritika Dixit & Tom Wingfield
Birat Nepal Medical Trust, Lazimpat Road, Lazimpat, Kathmandu, 44600, Nepal
Kritika Dixit
Departments of International Public Health and Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, L3 5QA, UK
Tom Wingfield
Tropical and Infectious Disease Unit, Liverpool University Hospitals NHS Foundation Trust, Liverpool, L7 8XP, UK
You can also search for this author in PubMed Google Scholar
Contributions
CN and AF led the construction and write-up of the manuscript. TW advised throughout the process of constructing the study and was the lead editor of the manuscript. HN was the second reviewer of papers. KD and MM reviewed the manuscript and provided substantial comments. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Tom Wingfield .
Ethics declarations
Ethics approval and consent to participate.
This review was conducted without patient or public involvement and did not need ethical approval.
Consent for publication
All authors agreed on the final version of the manuscript and gave consent for publication.
Competing interests
The authors declare no conflict of interest.
Supplementary Information
Additional file 1..
Excluded studies reasoning and Crowe Critical Appraisal Tool (CCAT) Score.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nuttall, C., Fuady, A., Nuttall, H. et al. Interventions pathways to reduce tuberculosis-related stigma: a literature review and conceptual framework. Infect Dis Poverty 11 , 101 (2022). https://doi.org/10.1186/s40249-022-01021-8
Download citation
Received : 05 May 2022
Accepted : 01 September 2022
Published : 23 September 2022
DOI : https://doi.org/10.1186/s40249-022-01021-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tuberculosis
- Intervention
- Stigma measurement tool
Infectious Diseases of Poverty
ISSN: 2049-9957
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Tuberculosis.
Ellis H. Tobin ; Debbie Tristram .
Affiliations
Last Update: March 20, 2024 .
- Continuing Education Activity
More lives have been lost as a result of tuberculosis (TB) than any other human disease. The current yearly estimate of worldwide mortality due to TB exceeds 1 million people. TB is a potentially curable disease, yet it is a challenge to diagnose, treat, and prevent. This activity introduces the epidemiology, pathophysiology, diagnostic approaches, and treatments of latent and active TB. It empowers healthcare professionals with an understanding of the myriad symptoms and signs of TB, the limitations in the accuracy of diagnostic modalities, the challenges associated with anti-TB drug treatment, and the limited resources available to prevent transmission. It describes how the landscape of TB has been altered by the advent of HIV, as well as the emergence of drug resistance.
- Screen high-risk populations for tuberculosis infection using evidence-based screening tools and protocols.
- Implement current World Health Organization guidelines for the diagnosis of tuberculosis.
- Assess the effectiveness of tuberculosis treatment regimens through regular monitoring of patient progress and response to therapy.
- Collaborate with an interprofessional healthcare team and public health authorities to ensure timely reporting and management of tuberculosis cases.
- Introduction
Tuberculosis (TB) encompasses a vast amount of information about a common disease that is challenging to diagnose, treat, and prevent. The following quote by S.T. Cole provides a perspective on the importance of this disease: “ More human lives have been lost to tuberculosis than to any other disease .” [1] Before the SARS-CoV-2 pandemic, Mycobacterium tuberculosis ( Mtb ) was the most prevalent human pathogen in the world. Unlike SARS-CoV-2, Mtb has existed as a human pathogen for millennia. Robert Koch reported his discovery of the Mtb bacterium in 1882, and its complete genome sequence was mapped over 100 years later. [2]
The diagnostic Mantoux skin test, developed in 1909, remains in use today with minor modifications in reagents and interpretive criteria. Interferon-gamma release assay (IGRA), developed in 2014, offers another approach to diagnosis. [3] Both tests possess diagnostic, predictive limitations that require a sophisticated understanding of interpretive criteria. The bacterium is slow-growing, frequently sparse, and often difficult to identify in sputum and tissue samples. These historic challenges in confirmatory TB diagnostics have been mitigated somewhat by the recent introduction of molecular nucleic acid amplification tests (NAATs). [4] However, NAATs are not readily available in many parts of the world where TB is most prevalent. Furthermore, when and how to best implement these tests in practice remains a work in progress. New tests that may enhance diagnostic accuracy are gradually emerging. [5]
The regimens required to treat TB are a challenge to administer. The most commonly used anti-TB antibiotics, all developed in the mid-20th century, remain the mainstay of therapy today. For the first time in over 40 years, 2 new anti-TB antibiotics have recently been approved for treatment. [6] Anti-TB regimens will vary depending on the stage and anatomic location of the infection, the immune status of the host, the age of the host, the presence of comorbidities, the development of toxicities, drug-drug interactions, and resistance patterns of the bacterium. Resistance is on the rise and often requires the administration of novel antibiotic combination strategies that have undergone limited testing in clinical trials. The prolonged duration of therapy required to eradicate the organism represents an additional challenge. With respect to latent TB infection, shortened treatment duration strategies have recently been developed to minimize the adverse effects of antibiotics and maximize patient compliance. [7]
TB prevention remains a worldwide challenge. Mtb is easily transmitted, and conditions that favor poverty, overcrowding, and lack of public health infrastructure contribute to its communicability. Moreover, nonspecific symptoms such as persistent cough often go unnoticed, resulting in high transmission rates. In the case of active TB, the multiple antibiotics required to eliminate the disease, along with their prolonged course of administration, represent a challenge even in those regions that possess robust public health infrastructure. Those parts of the world with the highest TB prevalence often lack resources to prevent it. In resource-rich parts of the world where TB is relatively uncommon, many clinicians rarely encounter it, are unfamiliar with its myriad clinical manifestations, and lack experience in approaches to diagnosis and management.
This activity provides an introduction to and overview of TB. Related activities will present details of diagnosis, clinical manifestations, treatment, and prevention.
Members of the Mtb family, also known as the Mtb complex, capable of causing human disease include M tuberculosis ( sensu stricto ), M bovis, M africanum, and M canetii. These are closely related species; M tuberculosis being the predominant human pathogen worldwide. Mtb is aerobic, non–spore-forming, and nonmotile. Its cell wall contains a uniquely high concentration of lipids that confer a characteristic acid-fast staining property and likely contribute to immunomodulation and virulence. [8] Mtb are slow-growing organisms with a generation time of approximately 20 hours. Visible growth on solid media usually takes from 3 to 8 weeks, and this characteristic contributes to the challenge of establishing a diagnosis. Humans are the only known reservoir of M tuberculosis, although other animals can become infected. Genetic variability exists among isolates from around the world and may confer differences in virulence. [9]
Mtb are intracellular pathogens capable of causing subacute and progressive disease, also referred to as active TB. In addition, the bacteria can remain dormant within infected cells where they may or may not cause disease. The molecular and immunologic mechanisms responsible for dormancy and reactivation remain unknown and represent an important area of Mtb research. [2]
- Epidemiology
TB data derived for the year 2022 from the World Health Organization (WHO) includes the following:
- 1.3 million deaths, including 167,000 patients with HIV
- 10.6 million people with active TB
- 5.8 million men
- 3.5 million women
- 1.3 million children
- Approximately 25% of the world’s population is TB-infected
- 5% to 10% will develop active TB disease
- TB is the leading cause of mortality in people with HIV
- The incidence of new TB cases in 2022 was as follows:
- 46% in South-East Asia
- 23% in Africa
- 18% in Western Pacific [10]
Risk factors associated with the development of active TB are as follows:
- Immunocompromise
- Immune senescence of older age
- Genetic diseases causing immunodeficiency
- HIV infection
- Prolonged corticosteroid use
- Cytoreductive chemotherapy
- Transplantation
- Tumor necrosis factor (TNF) antagonists
- Malnutrition
- Diabetes
- Tobacco
- Alcohol abuse
Recent data from the Centers for Disease Control (CDC) provide a perspective on TB in the United States (US):
- 8,300 cases of TB in 2022 (approximately 2.5 cases per 100,000 persons)
- TB cases have been reported in every state
- >80% of reported cases were associated with untreated latent TB or TB reactivation
- 73% of cases were among non–US-born persons
- Highest TB rates occurred in ethnic minorities
- Approximately 5% of persons with TB were HIV co-infected
- Drug-resistant TB is a serious public health concern [11]
- Pathophysiology
TB is spread from person to person by airborne droplet nuclei that can remain suspended in the air for several hours. The fate of the suspended droplet nuclei depends on environmental conditions: the bacilli can be destroyed by exposure to ultraviolet light, the droplet nuclei may innocuously land on inanimate surfaces, or they can be inhaled into a person’s airway, where they may or may not establish infection. The longer one is exposed to an enclosed space where TB droplet nuclei are present, the greater the likelihood of transmission. In modern times, TB is acquired most often via the respiratory route. It can also be acquired via ingestion of contaminated milk, and while this route of infection is of historical importance, it is a rare occurrence today. Also, it is exceedingly rare for TB to be contracted through contact with nonintact skin.
Once inhaled, droplet nuclei can land on upper airway mucosa where infection is unlikely to be established or reach the alveoli where the infectious processes may begin (see Image. Tuberculosis Pathophysiolgy Flow Chart). Depending on complex and poorly understood pathogen virulence factors in concert with host immunomodulatory mechanisms, the bacillus can either be killed, persist in a latent state or progress to active tuberculosis disease. These discreet categorical stages likely represent an oversimplification of a complex and dynamic host-pathogen relationship. [12] [13] Moreover, aspects of the long-held conceptual pathophysiological model, described in some detail below, have been questioned as knowledge about immune mechanisms has evolved. [14]
Alveolar macrophages play a central role in the immunomodulatory process. The bacilli are internalized by the macrophages where they are either killed or establish the primary infection. In the latter case, the bacilli gain access to lung parenchyma and can migrate to pulmonary lymph nodes, where they prime T cells. The primed T cells orchestrate the recruitment of T cells, B cells, monocytes, multinucleated giant cells, dendritic cells, and fibroblasts, forming a granuloma that surrounds infected macrophages within the lung parenchyma. The immunologic mechanisms that govern granuloma formation and the life cycle of the tubercle bacillus within the granuloma are poorly understood and represent areas of intensive research. [15] [16] [17] [13] Occasionally, this primary granuloma, referred to as a Ghon focus, and the associated draining hilar or mediastinal lymph nodes can calcify and reach a size visible on a chest x-ray; this finding is termed the Ranke complex. In children, the intrathoracic lymph nodes can enlarge, obstruct, and erode into bronchi. In immunocompromised adults and immunocompetent children, the Ghon focus may evolve into pneumonia, a form of progressive primary TB disease, primarily in the lower lung zones where cavitation is uncommon. In young children, progressive primary disease can rapidly disseminate within the lung itself and to other organs, most notably the central nervous system, where it can cause life-threatening Mtb meningitis.
In most immunocompetent adults, the bacilli will be contained by the granuloma and establish a latent infection. It may escape immunologic controls and disseminate lymphohematogenously within the lung and to virtually any other organ. Dissemination within the lung favors location in apical posterior segments. The reason for preferential dissemination to apical lung segments is speculative and has been attributed to regional differences in oxygen tension, differences in lymphatic flow, and differences in regional pulmonary immune function. The organs most commonly associated with extrapulmonary dissemination include pleura, lymph nodes, kidneys, long bones, vertebrae, and meninges. [18] Mtb bacilli will grow within the organs to which they have disseminated until cellular immunity or tuberculin reactivity is established, at which time the bacilli become dormant; this is latent TB infection. This occurs 3 to 8 weeks after infection in immunocompetent people. CD4 and CD8 T cells appear to play a central role in latency. [14]
Latent TB is not necessarily synonymous with Mtb dormancy. People labeled as having latent TB may cycle between periods of dormancy and subclinical TB disease. [13] This concept is supported by surveillance studies conducted in regions of high TB endemicity. [19] [20]
If innate and acquired immunity fails to contain Mtb , people will develop active TB disease. Granulomas can undergo caseation necrosis, erode into an airway, and form a cavity within which Mtb bacilli proliferate. [21] The cavity communicates with the airway and is the source of TB transmission. Because of its high concentration of proliferating bacilli and poorly vascularized inner contents, the cavity represents an environment promoting drug resistance development. Areas of cavitation no longer carry out respiratory functions and are a nidus for opportunistic bacteria and fungi. Lung parenchyma adjacent to cavities becomes fibrotic. Pulmonary blood vessels may erode into cavities and cause massive hemoptysis; this clinical finding is termed a Rasmussen aneurysm. Not all granuloma cavitate; they can involute and heal due to poorly understood immunological mechanisms.
Approximately 5% of recently infected people with TB will develop active disease within the first 2 years after infection. An additional 5% will develop active TB at a later time in their lives. Expressed differently, 90% of people infected with TB will not develop active disease. The risk factors associated with the development of active disease are noted above in the epidemiology section.
People with active TB disease can be asymptomatic at 1 end of the clinical spectrum or severely ill at the other end of the spectrum. Specific disease manifestations are a function of the organs involved; the apical posterior segments of the lung are the most commonly involved structures in adults and adolescents. In young children and older individuals, pneumonia involving the lower lobes is common. Constitutional symptoms are nonspecific and often include cough, fever, weight loss, night sweats, and malaise. Asymptomatic TB disease is well described, and prevalence has been reported to be quite high when active case finding is performed among high-risk populations. [22] [12]
Endobronchial TB represents a unique complication resulting from the spread of organisms from a pulmonary cavity, a pneumonic focus, or an adjacent lymph node into the airway. The endobronchial inflammatory process can produce mucosal ulcerations, granulation tissue, edema, and airway narrowing. [23]
Reactivation of a latent focus of infection represents the most common mechanism leading to active disease, and previously infected people are generally immune to exogenous reinfection. However, it is possible to become reinfected when exposed to a large Mtb inocula or if there is significant underlying immunocompromise. [24] This has important therapeutic and epidemiologic implications since it can be a challenge to determine whether a person with a prior history of TB has relapsed due endogenous reinfection, which is failure to eradicate their infection, or due to exogenous reinfection via a newly acquired infection.
Tuberculosis and HIV Coinfection
The HIV epidemic heralded a new era in the long history of TB and deserves a separate discussion of pathogenesis. [25] [26] [13] [27] Data from the WHO indicates that people living with HIV (PLHIV) are approximately 19 times more likely to develop active TB disease than those without HIV. [28] The initiation of antiretroviral therapy (ART) does not completely restore Mtb immunity to baseline. [27] In addition, the return of TB-specific CD4 T cells after initiating ART can lead to TB-immune reconstitution syndrome (IRIS). Globally, TB is the leading cause of death in PLHIV; those in developing countries bear the highest burden. Both increased rates of reactivation and increased susceptibility to Mtb following exposure appear to contribute to the high rate of active TB disease in the HIV population. The risks of developing active TB disease increase as CD4 T lymphocyte counts decline. [13] Within the first year of Mtb primary infection, PLHIV develop significantly higher rates of progressive primary TB disease. Both primary infection and exogenous reinfection appear to contribute to the TB burden in PLHIV. [25]
The underlying alterations in immune function that account for these findings in the HIV-TB co-infected population are not well understood. [26] Several hypotheses exist as follows:
- Selective depletion of Mtb antigen-specific CD4 T cells
- Dysfunction of CD8 T cells
- Increased production of TNF
- HIV alterations in macrophage function
Observational studies suggest that TB infection accelerates the progression from HIV infection to AIDS. [26] [25] Once again, the mechanisms involved are unknown, and several hypotheses exist, including:
- Active TB disease is associated with an accelerated loss of CD4 T cells
- The immune response to TB increases HIV replication in blood and tissues
- Mtb infection induces the production of proinflammatory cytokines that upregulate HIV replication
TB clinical manifestations in PLHIV with high CD4 T lymphocyte counts are similar to those not infected with HIV. Reactivation TB is often associated with upper lobe infiltrates and cavitation. Data suggest a correlation between CD4 T lymphocyte counts and cavitation due to TB; the higher the CD4 T lymphocyte count, the more likely there will be cavitation. [25] Atypical chest x-ray findings are common in people co-infected with TB and HIV when CD4 T lymphocyte counts fall below 200 cells/μL. These findings include:
- Normal chest x-rays
- Interstitial nodules
- Lower and middle lobe infiltrates
- Intrathoracic lymphadenopathy
- Pleural effusions
PLHIV are at greater risk of developing disseminated TB. Moreover, based on postmortem studies, disseminated TB in the HIV population is often undiagnosed. [13] [29] To reduce complications and transmission, it is of paramount importance to promptly identify and treat HIV-TB co-infected individuals. [29]
- Histopathology
Nonspecific appearing necrotizing and non-necrotizing granuloma may be identified in Mtb- infected tissue sections processed by hematoxylin and eosin (H&E) staining. The granuloma consists of an outer rim of lymphocytes and plasma cells surrounding a peripheral rim of epithelioid histiocytes and multinucleated giant cells. A central region of necrosis, if present, can have a caseous consistency on gross inspection. If abundantly present, acid-fast bacilli may be identified using the Ziehl-Neelsen stain. Greater sensitivity in identifying the organisms may be achieved by fluorescent microscopy using the auramine-rhodamine stain.
- History and Physical
Regarding TB, the first rule of taking a history is to think about it. This rule is likely given great consideration in countries with a high prevalence of TB. In those countries where TB is uncommon, it may not be afforded initial consideration by clinicians during the evaluation of patients presenting with nonspecific symptoms such as cough, fever, malaise, or weight loss. The diagnosis is even more challenging when patients present with extrapulmonary TB. Thus, routine exploration of risk factors such as a prior TB history, known TB contacts, country of origin, foreign travel, family history, occupational and residential exposures, immunosuppression, and immunocompromise, are key components of the history. These aspects of history taking should be performed for all initial patient contacts, given the high worldwide prevalence of TB.
Patients with latent TB are asymptomatic, and those with early active TB disease are often asymptomatic and will have no specific physical findings. In the latter instance, as the disease progresses, patients may experience the insidious onset of cough, fever, night sweats, weight loss, and hemoptysis before seeking medical evaluation. Depending on the extent of the disease, the physical findings on lung examination may be normal or demonstrate areas of consolidation, airway inflammation, or the presence of cavities. Those with chronic, extensive, destructive cavities with surrounding fibrosis may develop chest wall deformities due to loss of underlying lung volume. [30]
Since TB can involve any organ, details of the myriad of physical findings are beyond the scope of this introductory activity (see Image. Clinical Features of Extrapulmonary Tuberculosis).
The approach to TB diagnosis depends on whether one is evaluating a patient for latent, active pulmonary, or extrapulmonary TB disease. A combination of immunologic responses to provocative tests, radiology, microbiology, molecular methods, and biomarkers are used to establish a diagnosis. Most importantly, the approach to diagnosis will depend on TB prevalence within a population and the resources available to the public health care system within a specific geographic region. [31] [5] TB is often a diagnostic challenge. Signs and symptoms, if present, are nonspecific. The sensitivity and specificity of existing diagnostic tests can vary significantly depending on several factors that include pre-test probability, immunological status and age of the patient, timing of the test, adherence to proper test procedures, adequacy of specimen collection, and the ability to interpret test results in the context of the patient's risk factors and immune function. Radiological images can range from normal to nonspecific markedly abnormal findings. In the absence of a confirmatory culture or molecular assay, the clinical diagnosis of TB is presumptive and based on the strengths of clinical suspicion in concert with surrogate markers of infection. This can lead to both under- and over-diagnosis depending on the epidemiological setting. In-depth details of TB diagnostic testing are beyond the scope of this article, and the reader is referred to excellent reviews on the topic. [32] [33] [34] [31] [15] [35]
Latent Tuberculosis
Populations that should undergo screening for latent TB infection include the following:
- Contacts of individuals with active TB disease
- Individuals initiating anti-TNF therapy
- Dialysis patients with end-stage renal disease
- Patients anticipating organ or bone marrow transplants
- Patients with silicosis
In low- and middle-income countries (LMIC), the WHO endorses the use of tuberculin skin tests (TSTs) or interferon-gamma release assays (IGRAs). [5] The traditional TSTs, such as the Mantoux or purified protein derivative (PPD), can suffer from low specificity due to the combination of cross-reactivity with the Bacillus Calmette-Guerin (BCG) vaccine and, to a lesser extent, exposure to nontuberculous mycobacteria (NTMB). This is particularly problematic in parts of the world where high TB prevalence has led to the widespread use of BCG vaccination in children. The IGRA possesses greater specificity since it does not cross-react with BCG or most NTMB strains. Recently, TB skin tests have been developed using specific Mtb antigens. [36] The WHO has concluded that these Mtb antigen-based skin tests (TBSTs) have similar diagnostic accuracy to that of IGRAs. [5] Thus, the choice of TST or IGRA for detecting latent TB comes down to resources and ease of use at the point of care.
The IGRA is a blood test that requires the availability of a laboratory and technical personnel; it may be cost-prohibitive in LMIC regions. It does have the advantage of not requiring a return visit for result interpretation. The traditional TST is simple to perform at the point of care and requires fewer resources, but it suffers from less specificity and requires a return visit for interpretation. The new TBSTs are performed similarly but have the advantage of specificity equivalent to that of IGRAs. In the US, if resources allow, IGRAs are the preferred testing modality for the detection of latent TB. [33] TSTs are an acceptable alternative if IGRAs are unavailable or deemed too costly.
TB skin tests have limitations. They can produce false-negative results, particularly in individuals with compromised immunity, including those at the extremes of age, PLHIV, and people receiving immunosuppressive drugs, or those tested within several weeks of TB infection. False-negative results can also occur due to errors made during intradermal injection and in the interpretation of the skin test reaction. False-positive results can be due to prior BCG vaccination, exposure to NTMB, and misinterpretation of the skin test reaction.
While IGRAs are more sensitive than TSTs in individuals co-infected with HIV, false-negative results can occur in those severely immunocompromised. In addition, technical imprecision in processing the blood sample can result in erroneous results. Indeterminate IGRA results may occur more frequently in children younger than 5 years and in PLHIV with CD4 T lymphocyte counts less than 200 cells/μL. [33] Discordant results between skin tests and IGRAs can occur; refer to "BCG Vaccine" in the Treatment/Management section for more information about discordant results. In this case, repeat testing may be considered, and the decision to initiate anti-TB therapy will ultimately depend on the strength of clinical suspicion.
Neither TSTs nor IGRAs can distinguish latent from active TB, nor can they predict who will evolve from latent infection to active disease. When a decision is made to initiate therapy for latent TB, efforts must be made to exclude the presence of active TB disease. Failure to do so will promote the emergence of resistant organisms and result in inadequate treatment outcomes. To further complicate the matter, individuals who have successfully eradicated their TB infection can continue to test positive by TSTs and IGRAs. Conversely, people with a remote history of untreated latent TB can have a false negative test. [37] There are excellent reviews that explore detailed recommendations on latent TB testing strategies in different at-risk populations. [33] [5] In addition, a user-friendly, web-based, interactive program called the Online TST/IGRA Interpreter can provide an individual estimate of the risk of TB infection based on TST and IGRA results. [38] The algorithm incorporates individual parameters and calculates a positive predictive value.
Active Tuberculosis Disease
A diagnosis of active TB is confirmed by culture. However, confirmation is often elusive due to practical difficulties in obtaining adequate sputum, fluid, and tissue specimens, the frequent paucity of organisms present, and their slow growth characteristics. The diagnosis is often presumptive and based on pretest parameters in association with supporting evidence that includes radiological images, molecular assay, and biomarkers.
A helpful way to introduce this topic is to consider imaging techniques in the context of the stage of TB. However, these are dynamic pathological processes with overlapping clinical and radiologic features. Moreover, any single or combination of image findings is possible. Conventional chest x-ray remains the initial modality employed for screening and diagnosis. Computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography–computed tomography (PET-CT) are employed when necessary to better define anatomic involvement with active TB disease. [39] Imaging features of TB are nonspecific and can mimic other diseases. This activity will focus on imaging of the lungs. A detailed presentation of imaging modalities for the evaluation of extrapulmonary TB can be found in excellent reviews. [39] [35]
- Parenchymal infiltrate or atelectasis
- Usually, in middle and lower lungs
- Identified in <10% of cases
- Intrathoracic lymphadenopathy
- Often seen in children and PLHIV
- Ghon focus and Ranke complex
- Often heals with residual calcification
- Pleural effusion (usually unilateral)
- Generally uncommon; seen more commonly in PLHIV
- Miliary pattern (progressive primary disease)
- Uncommon; seen predominantly in infants, older individuals, and severely immunocompromised patients
- Normal chest x-ray
- CT may identify subtle changes not seen on chest x-ray
- Post-primary TB, including reactivation and reinfection
- Patchy consolidation of the apical and posterior upper lobe and superior segments of lower lobe
- Cavitation is seen in 20% to 45% of adult cases but is rare in young children and those who are severely immunocompromised
- Adenopathy is uncommon in adults but common in young children and PLHIV
- Tree-in-bud nodular distribution if endobronchial spread; seen best with CT
- Pleural effusions are uncommon
- Miliary pattern is generally uncommon and seen predominantly in infants, older individuals, and severely immunocompromised patients
- CT may identify subtle changes not seen on chest x-ray
- CD4 T lymphocyte count less than 200 cells/μL
- Intrathoracic lymphadenopathy is common
- Cavitation is uncommon
- Extrapulmonary disease is common
- Bronchiectasis
- Bronchopleural fistula is an uncommon finding
In the majority of primary TB cases, there will be resolution of parenchymal lesions, and occasionally, a Ranke complex will be the only residual clue to a diagnosis of remote TB. Normal chest x-rays can occur in people with active TB disease. When pathologic lung images due to TB are identified with chest x-rays, it is always a challenge to distinguish active from inactive disease. While there are clues such as cavity wall thickness, presence or absence of consolidation, fibrosis, pleural effusion, and calcifications, no definitive findings can exclude active disease. In general, CT images provide significantly improved sensitivity. A small number of reports suggest that fludeoxyglucose F 18 (FDG) PET-CT may be useful in assessing response to therapy. [39]
Microscopy, Culture, and Molecular analysis
Clinical suspicion of active TB requires further microbiological investigation. [40] Analysis of sputum and, if indicated, fluid and tissue samples using staining and culture techniques have, until recently, been the only available confirmatory diagnostic tests. Automated real-time NAATs and biomarker probes have become an important addition to the TB diagnostic landscape. [41] [42] [43]
Acid-Fast Bacilli Smear Microscopy
Sputum smears and culture are the conventional and most commonly applied approach to diagnosis. Not everyone can produce a deep expectorated sputum sample, and the frequent paucibacillary nature of TB limits the sensitivity of this application. It is important to note that sensitivity values are a function of pretest probability; higher sensitivity will be achieved in regions with high TB prevalence. Notably, the application and interpretation of staining methods have not been standardized and are likely subject to significant variations in practice patterns. [44] Improved sensitivity can presumably be achieved by collecting expectorated sputum samples on 3 separate days, although the value of this practice has been debated. [45] Moreover, in resource-poor parts of the world, this practice can be quite burdensome. Staining sensitivity can be increased using fluorochrome stains, specimen concentration techniques, and at least 5 ml of sputum volume. Improved sensitivity may also be achieved when respiratory specimens are obtained by sputum induction and interventional methods such as bronchoscopy and possibly gastric lavage. [40] The sensitivity of sputum acid-fast bacilli (AFB) smears ranges from 34% to 80%. [34]
NAATs should be performed on all AFB smear-positive specimens and smear-negative specimens when the clinical suspicion is intermediate or high. Refer to the "Molecular Detection Methods" for more information. In the latter case, a negative NAAT does not rule out a diagnosis of TB. [33]
Culture sensitivity ranges from 80% to 93%, and specificity is approximately 93%. [34] Broth media can detect growth within 2 weeks, whereas solid media can take up to 8 weeks for visible growth. When Mtb grows in broth media, it can then be subjected to rapid drug susceptibility tests (DSTs) and identification by DNA probe methods. Conventional phenotypic DST methods are time-consuming and resource-intensive.
Molecular Detection Methods
The past 2 decades have experienced a remarkable evolution in the approach to TB diagnosis and drug-resistance detection. Molecular methods using NAATs and lateral flow biomarker detection provide rapid results that impact immediate public health and direct patient care. Several of these tests are capable of simultaneous Mtb detection and drug resistance identification. [28]
The application of these tests continues to evolve; when, where, and how they are best utilized require consideration of several variables that include prevalence of TB and drug resistance, population screening, individual diagnosis of active pulmonary and extrapulmonary cases, applicability to adults, children, and PLHIV, stand-alone testing, follow-on testing, costs, ease of use, and available resources. Moreover, their application must account for pretest probabilities, sensitivity, specificity, and interpretation when there is discordance with conventional methods. In the latter case, repeat testing may or may not resolve the discrepancy, and decisions regarding the presence or absence of active TB must be made on the strength of clinical suspicion. The assays play an important role in complementing conventional smear and culture methods and, in certain circumstances, can stand alone as diagnostic tools. In 2021, the WHO published a detailed, consolidated, evidence-based report that describes the various technologies and provides recommendations for how best to apply them in practice (see Image. Classes of Technologies and Associated Products). [28] The following is a summary of the assays and WHO recommendations; the reader is referred to the WHO report for a detailed discussion. [28]
The Xpert ® MTB/RIF (Xpert ® ) and Xpert ® MTB/RIF Ultra (Xpert Ultra ® ) (Cepheid, Sunnyvale, CA, USA) are automated, cartridge-based NAATs that have gained widespread use. They detect Mtb and rifampin (RIF) resistance mutations directly from specimens within 2 hours; RIF resistance mutations are a surrogate marker for multidrug resistance. The Xpert ® sensitivity for Mtb detection is approximately 70% when a single smear-negative/culture-positive sputum specimen is tested and increases to approximately 90% when 3 consecutive sputum specimens are tested; specificity is approximately 98%. [28] The sensitivity for detecting RIF resistance is approximately 96%, and the specificity for excluding resistance is approximately 98%. [28] The corresponding sensitivity ofXpert Ultra ® increases to approximately 77%, but specificity decreases to approximately 96%. [28] The decrease in specificity is likely due to an increased rate of false positives resulting from the detection of nonviable Mtb that can occur in people treated for TB within 2 to 5 years of Xpert Ultra ® testing. [46] The sensitivity for detecting RIF resistance is approximately 94%, and the specificity for excluding resistance is approximately 99%. [28] The sensitivity of Xpert ® and Xpert Ultra ® assays in detecting pulmonary TB in children is less than that in adults, and this is likely due to the difficulty of obtaining adequate sputum samples in this population.
Both Xpert ® and Xpert Ultra ® assays are valuable in detecting Mtb from samples obtained at extrapulmonary sites, most notably cerebrospinal fluid (CSF) and lymph node aspirates. Details of sensitivity and specificity on various extrapulmonary specimens can be found in the WHO 2021 update document. [28]
The WHO recommends using Xpert ® and Xpert Ultra ® assays as initial tests in adults and children, including PLHIV, with signs and symptoms of pulmonary TB. [28] This includes analysis of gastric aspirate, nasopharyngeal aspirate, and stool specimens in children. The WHO also recommends their use as an initial diagnostic test in adults and children suspected of having extrapulmonary TB. [28] For PLHIV suspected of having disseminated TB, the WHO recommends using Xpert ® and Xpert Ultra ® assays on blood.
The TrueNat ® MTB Plus assay (Molbio Diagnostics, India) is a rapid, automated NAAT endorsed by the WHO in 2020. [47] The NAAT accuracy appears similar to that of Xpert ® and Xpert Ultra ® assays. [28] [47] The TrueNat ® MTB Plus assay is portable and battery-powered, making it advantageous as a point-of-use technology. However, it is a relatively new platform that has not been as extensively evaluated as Xpert ® .
Globally, approximately 13% of new cases and 17% of previously treated cases of TB are isoniazid (INH)-resistant and RIF-susceptible. [28] Several moderate-complexity NAATs are capable of detecting Mtb as well as both INH and RIF resistance. The WHO has endorsed the tests as initial pulmonary TB detection methods, given their speed and relative ease of use compared to conventional culture-based drug susceptibility tests. [28]
TB loop-mediated isothermal amplification (TB-LAMP) is rapid, relatively simple to perform, and can detect Mtb without the need for sophisticated equipment. [48] The WHO endorses using the TB-LAMP assay (Eiken Chemical Company, Tokyo, Japan) as a replacement for sputum-smear microscopy and as a follow-on test for sputum-smear–negative specimens in adults for whom TB is suspected. [28] The assay does not appear to provide added accuracy to sputum-smear microscopy in PLHIV.
Lipoarabinomannan (LAM), a cell wall component of Mtb, is excreted in the urine of people with active TB. [49] The ability to detect LAM in urine samples using a simple lateral flow assay is obviously appealing. In practice, the LAM assay sensitivity is relatively low in the general population. However, sensitivity improves in individuals with HIV infection as immunosuppression increases. The WHO endorses the use of the Determine™ TB LAM lateral flow test (Alere Determine™ TB LAM Ag Alere, MA, USA) for adults and children infected with HIV with CD4 T lymphocyte counts of less than 200 cells/μL and with signs and symptoms of pulmonary or extrapulmonary TB ( see Image. Classes of Technologies and Associated Products). [28] In addition, the WHO endorses its use in PLHIV with CD4 counts of <100 cells/μL irrespective of signs and symptoms of TB. A detailed tabulation of pooled sensitivity and specificity data based on CD4 count is available. [28]
The group of low-complexity NAATs for detecting resistance to isoniazid (INH) and second-line anti-TB agents are used as follow-on assays in settings where multidrug-resistant TB (MDR-TB) is encountered. Compared to conventional culture-based phenotypic DSTs, the NAATs are automated and rapid. They are not currently capable of determining resistance to some of the new and repurposed agents, such as bedaquiline and linezolid. [28] The assays appear to be applicable to sputum and extrapulmonary specimens.
Line probe assays (LPAs) are rapid molecular diagnostic tests that can detect Mtb and resistance to several first- and second-line anti-TB agents ( see Image. Classes of Technologies and Associated Products). [28] [50] LPAs require instrumentation and technical expertise that lend themselves to regional and reference laboratory settings. As reflex tests when RIF resistance is detected, the LPAs are used to identify the presence of resistance genotypes to other anti-TB agents. Compared with the conventional phenotypic culture-based DST, which can take several weeks to perform, the LPAs can obtain a result within several hours. LPAs can be performed on culture isolates as well as sputum specimens. When MDR-TB is potentially identified, the LPAs should be considered initial DST tests and are not meant to replace conventional phenotypic culture-based DST. The strength of the WHO recommendations on using LPAs and all of the molecular detection methods will evolve as more evidence of their utility in many settings is generated.
Tuberculous pleural effusions (TPE) are challenging to diagnose. The detection of adenosine deaminase (ADA) in pleural fluid supports the diagnosis with a pooled sensitivity and specificity of approximately 92% and 90%, respectively. [51] ADA detection is simple and inexpensive to perform and provides a rapid result. Detection of ADA in CSF has been applied to the diagnosis of Mtb meningitis with a pooled sensitivity and specificity of approximately 85% and 90%, respectively. [52] A small number of studies have suggested the value of obtaining ADA levels of peritoneal and pericardial fluid when TB is suspected at these sites. [53]
- Treatment / Management
Latent Infection
TSTs and IGRAs are unable to predict the progression from latent infection to active disease. Several observational studies have demonstrated that the risk of developing active TB is highest during the first 2 years after acquiring infection and that reactivation is rare beyond 10 years after infection. [37] It has been estimated that the number needed to treat (NNT) to prevent 1 case of active TB ranges from 36 in recently infected contacts to 179 in those remotely infected. [37] Thus, while evidence clearly demonstrates that treatment of latent TB reduces the likelihood of developing TB disease in populations at high risk, the evidence is less clear that treatment of those at low or intermediate risk reduces the incidence. [33] The rationale to treat those with latent TB is best defined by the WHO; it is “premised upon the probability that the condition will progress to active TB disease in specific risk groups, on the underlying epidemiology and burden of TB, the feasibility of the intervention, and the likelihood of a broader public health impact.” [54]
The preferred 3-month regimen of once-weekly INH plus rifapentine (3HP) is attractive due to its short duration and decreased incidence of liver toxicity relative to the 6- and 9-month INH regimens (see Image. Recommendations for Regimens to Treat Latent TB infection). Reports of a flu-like syndrome occurring in recipients of the 3HP regimen have raised concerns. [55] However, a large, multinational trial identified that 11% of participants experienced symptoms of a systemic drug reaction (SDR), most frequently within the first month of therapy. Of those experiencing SDR, 48% were able to complete treatment, and serious adverse events were rare. [55]
The WHO guidelines on TB preventive therapy align with those of the CDC. [54] In addition, the WHO guidelines include an alternative regimen consisting of 1 month of daily 3HP plus INH. [54] Moreover, the WHO recommends that “in settings with high TB transmission, adults and adolescents living with HIV who have an unknown or a positive TST or IGRA and are unlikely to have active TB disease should receive at least 36 months of daily INH preventive therapy.” [54] The latter recommendation is made regardless of immune status and whether or not ART is being administered.
Currently, there are no studies providing robust data to help guide TB preventive therapy for individuals having close contact with people infected with MDR-TB. [56] The WHO guidelines suggest a targeted approach based on individual risk assessment. [54] Trials to ascertain the efficacy and safety of fluoroquinolones and delamanid are currently in progress. However, trials will require long follow-ups to assess the absence of disease as the clinical endpoint. It will be challenging to devise TB preventive therapy protocols that can be applied to various drug resistance patterns and assess safety and efficacy in different populations (eg, children, adults, PLHIV, the immunosuppressed, and those with existing comorbidities). [57] [56] [58] See StatPearls' companion topic, "Latent Tuberculosis," for a complete discussion of the treatment of this disease process.
Active Tuberculosis Infection
The goal of anti-TB therapy is to eradicate disease and eliminate transmission in all cases. While the goal seems unambiguous, it has proven exceedingly difficult to achieve in practice. Historically, anti-TB regimens have required many months of treatment and patient adherence has been a challenge. While these challenges exist everywhere, they are particularly problematic in parts of the world with the highest TB prevalence and where public health infrastructure and literacy about TB are lacking. From a global public health perspective, TB treatment guidelines are designed to be straightforward and somewhat standardized. [59] This “one-size-fits-all” approach has been questioned since a standard 6-month regimen may be too long for some and not long enough for others. [60] [59] It is conceivable that in the future, the application of a pretreatment risk stratification algorithm could inform optimized treatment duration schedules on an individualized basis. [60]
Detailed recommendations on dosing, first- and second-line anti-TB drugs, drug-drug interactions, management of treatment interruption, adverse effects of treatment, culture-negative TB, extrapulmonary TB, HIV coinfection, children, advanced age, pregnancy, breastfeeding, and comorbidities are beyond the scope of this activity and may be found in the referenced guidelines (see Image. Drug Regimens for Microbiologically Confirmed Pulmonary TUberculosis Caused by Drug-Susceptible Organisms). [61] In addition, the management of TB is understood to be very complex, and for that reason, the CDC has established an exceptionally useful online resource, TB Centers of Excellence for Training, Education, and Medical Consultation. ( http://www.cdc.gov/tb/education/rtmc/default.htm )
The treatment for drug-susceptible pulmonary TB disease had not, until 2022, changed in 50 years. The long-held standard regimen involves the use of 4 drugs: isoniazid (INH), rifampin (RIF), ethambutol (ETH), and pyrazinamide (PZA). Before the development of that therapeutic combination, the first anti-TB drug, streptomycin, was used as monotherapy in the 1940s. Streptomycin initially provided significant benefit when administered for 6 months but ultimately failed due to the emergence of resistance. [62] The resistance to monotherapy, along with a better understanding of both the pathophysiology of Mtb infection and drug toxicities, informed decisions that led to the current standard of treatment. [61]
There are 2 phases of treatment – an initial intensive phase that provides bactericidal activity directed at rapidly replicating organisms and the continuation phase that is meant to sterilize slowly replicating and dormant tubercle bacilli. [62] The intensive phase of therapy requires the use of INH, RIF, ETH, and PZA, and the continuation phase uses INH and RIF. In treating pulmonary TB, the intensive phase usually extends for 2 months, during which it is hoped that there will be significant reductions in mortality, lung inflammation, rapidly replicating mycobacteria, and transmission. Should drug susceptibility testing indicate that the isolate is sensitive to both INH and RIF, the EMB can be discontinued. In that case, the intensive phase would consist of INH, RIF, and PZA. [61] The continuation phase extends for an additional 4 months. The rationale for the 4-drug combination is that bactericidal killing of rapidly replicating organisms will reduce the chances of emerging resistance. [62]
Patients receiving anti-TB therapy require monitoring to assess the efficacy and safety of the regimens. Sputum smears and cultures should be evaluated monthly until 2 consecutive cultures are negative. In patients with chest x-ray evidence of cavitation and who remain culture positive at 2 months, the recommendation is to extend the continuation phase for an additional 3 months (ie, a total of 9 months of therapy). [62] Extending the continuation phase should also be considered for the following individuals: PLHIV, the malnourished, active smokers, the immunosuppressed, and those with extensive pulmonary disease.
Centers for Disease Control 2022 Interim Guidance
In 2022, the CDC announced interim guidance on a 4-month anti-TB regimen for drug-susceptible pulmonary tuberculosis. [63] The regimen consists of an intensive phase of 8 weeks of daily rifapentine (RPT), INH, PZA, and moxifloxacin (MOX), followed by a continuation phase of 9 weeks of daily RPT, INH, and MOX. [64] This treatment option is available for patients older than 12 years, including PLHIV with CD4 T lymphocyte counts greater than 100 cells/μ L and anticipating an ART regimen that includes efavirenz in the absence of any other known potential drug-drug interaction. Due to a lack of clinical trial data, the regimen is not intended for pregnant or breastfeeding patients, treatment of extrapulmonary TB, those with a history of prolonged QT syndrome or use of QT-prolonging medications, and those with body weight less than 40 kg.
Drug-Resistant Tuberculosis
The vast majority of patients with drug-susceptible pulmonary TB who are able to complete the standard anti-TB regimens will be cured. Unfortunately, drug-resistant TB poses a much greater risk of treatment failure and requires alternative and often more prolonged regimens. [65] There are several categories of drug resistance, including:
- Rifampicin-resistant TB (RR-TB)
- May be resistant to isoniazid
- May be resistant to other TB drugs
- Rifampicin-susceptible, isoniazid-resistant TB
- Multidrug-resistant TB (MDR-TB)
- Resistant to both RIF and INH
- Extensively drug-resistant TB (XDR-TB)
- Resistant to RIF, INH, a fluoroquinolone, and at least 1 of the second-line injectable drugs, such as capreomycin, kanamycin, and amikacin
Drug-resistant TB poses a threat to global public health control efforts. In 2018, the global estimate of MDR-TB was approximately half a million new cases, of which only 30% were started on second-line therapy. The complexity of treatment and management led to the establishment of programmatic strategies to intensify treatment programs. [66] Extended treatment regimens can range from 18 to 21 months and incorporate a variety of first-line, second-line, new, and repurposed agents during both the intensive and continuation phases of therapy. When prolonged regimens and injectable second-line agents are required, the risks of drug toxicities and poor patient compliance are very high. Adherence interventions are being employed and include psychological counseling and patient education, financial and material incentives, and mobile phone text reminders. [66]
New and repurposed agents including but not limited to delamanid, bedaquiline, pretomanid, linezolid, amoxicillin-clavulanate, meropenem-clavulanate, imipenem-cilastatin, cotrimoxazole, and macrolides have recently been employed and may permit shorter durations of treatment in some circumstances. [65] [67] [68] In addition, adjuvant surgical excision may be necessary in efforts to eradicate cavities and nonviable lung tissue. [65] [69]
Details on the management of drug-resistant TB are beyond the scope of this activity and the reader is directed to both WHO and American Thoracic Society/European Respiratory Society/Infectious Diseases Society of America guidelines. [65] [70] Moreover, it is advisable to seek assistance from government health department experts when caring for an individual with suspected or confirmed drug-resistant TB. Experts can be found at ( http://www.cdc.gov/tb/education/rtmc/default.htm ) and ( http://mdrtb.brit-thoracic.org.uk/ ).
Bacille Calmette-Guerin Vaccine
BCG, a live attenuated strain of M bovis, has been recommended by the WHO as a vaccine for infants and children since 1974. [71] It is intended for use in countries with high TB incidence to prevent miliary TB and Mtb meningitis to which infants are most susceptible. It is the most widely used vaccine worldwide. [72] While the vaccine appears somewhat protective when administered to infants and children, its protection wanes over several years. It does not provide significant protection when administered to adults. [73] As previously discussed, BCG vaccine can cause false-positive TSTs.
A commonly encountered clinical question is whether to initiate TB preventive drugs in patients who anticipate anti-TNF therapy or transplantation, have a possible history of having received the BCG vaccine, and are IGRA-negative and TST-positive. This complex scenario becomes particularly troublesome when one considers that the patient comes from a high TB prevalence region, denies a history of known TB infection, lacks radiological signs of latent or active TB, and could be at risk of developing reactivation TB once anti-TNF therapy or transplant commences. Discordant results, such as TST-positive/IGRA-negative, are common in people who received the BCG vaccine. There are no firm cutoff values for the size of TST induration in this particular setting. Moreover, initiating TB preventive therapy is not without risks of adverse drug reactions.
Unfortunately, there is no way to address this clinical situation with absolute certainty. [74] The consensus guidelines approach this scenario somewhat indirectly and state “ Performing a second diagnostic test when the initial test is negative is one strategy to increase sensitivity. While this strategy to increase sensitivity may reduce the specificity of diagnostic testing, this may be an acceptable tradeoff in situations in which it is determined that the consequences of missing latent TB infection (i.e., not treating individuals who may benefit from therapy) exceed the consequences of inappropriate therapy (i.e. hepatotoxicity).” [74] In this complicated situation, the consensus among most experts is to begin a regimen of TB preventive therapy several weeks before the start of the immunosuppressing intervention. [74]
- Differential Diagnosis
As a result of its myriad manifestations over prolonged periods of time, the differential diagnosis of TB is limitless. [31] A list of the more common diseases that TB can easily be confused with is:
- Any infections causing constitutional symptoms
- Fevers of unknown origin
- Pulmonary infections
- Nontuberculous mycobacteria
- Hematologic
- Metastatic tumors
- Renal
- Peritoneal
- Gastrointestinal
- Autoimmune diseases
- Sarcoidosis
- Drug reactions.
- Toxicity and Adverse Effect Management
The anti-TB drugs are associated with potential toxicities ranging from mild to life-threatening. [62] [75] Patients must be educated about early signs and symptoms of drug toxicity, instructed about when to discontinue their use, and seek immediate evaluation should they occur. There are detailed guidelines for assessing treatment responses, patient monitoring, adverse drug reactions, and management. [76] [77] The following is a list of commonly occurring adverse events and their associated anti-TB drugs:
- Hepatitis (malaise, fatigue, fever, anorexia, nausea, dark urine)
- INH; Bedaquiline; RIF; PZA
- Peripheral neuropathy
- INH; Linezolid
- Ocular toxicity
- PZA; ETH; Fluoroquinolones; Amikacin; Beta-lactams; INH; Streptomycin; Para-aminosalicylic acid
- Cranial nerve VIII dysfunction and renal dysfunction
- Amikacin; Streptomycin; Capreomycin; Kanamycin
- Gastrointestinal reactions
- All of the anti-TB drugs are capable of causing gastrointestinal upset
- Myalgias-arthralgias
- Bedaquiline; PZA
- Anxiety, confusion, psychosis
- Cycloserine; Fluoroquinolones
- Hypoglycemia
- Fluoroquinolones
People with TB and HIV coinfection receiving ART present additional management challenges. Both drug-drug interactions, as well as co-administration of anti-TB and antiretroviral agents, can pose significant risks. [78] [79] [80] Rifamycins cause decreased plasma concentrations of protease inhibitors (PIs) and nonnucleoside reverse-transcriptase inhibitors (NNRTIs). Co-administration of anti-TB drugs and ART can cause significant adverse reactions. In those coinfected individuals, the restoration of immunity associated with ART may result in clinical deterioration due to IRIS. A detailed discussion of the management of these pharmacological challenges is beyond the scope of this activity and is presented in excellent references. [78] [25]
More than 80% of TB-associated mortality occurs in LMICs. TB is the leading cause of death in PLHIV. In 2022, the WHO estimated that there were 1.13 million deaths among HIV-negative people and 167,000 deaths among PLHIV. [10] The current estimate of the prognosis of untreated TB is difficult to calculate; it would have to account for regional differences in healthcare resources, those who have either failed or never initiated treatment, those with drug-resistant strains, and people with different underlying comorbidities. [81] Estimates based on prechemotherapy-era data may be unreliable due to heterogeneity in case definition, patient selection, and reporting. The study by Tiemersma et al estimated a 70% lifetime case fatality among untreated HIV-negative individuals. [81]
The following global estimates of successful treatment outcomes derived by WHO in 2018 are:
- 85% success for people with new and relapsed TB
- 76% success for HIV-coinfected people
- 57% success for people with MDR-TB [82]
The WHO estimates that 15% of patients with MDR-TB die of disease, and 26% of those deaths are due to XDR-TB. [65] For those individuals with drug-susceptible TB who adhere to a full therapeutic regimen, the cure rate can exceed 95%. Variables such as extent of disease, presence of comorbidities, age, and adverse drug reactions influence the therapy outcome. Novel regimens will very likely improve outcomes in people treated for drug-resistant TB. [83]
- Complications
Clinical complications of TB and those resulting from adverse drug events have been presented in previous sections of this activity. TB is theoretically a curable and preventable disease for which the WHO has ambitiously established a goal of 90% reduction in incidence between 2015 and 2035. [84] It is this author’s prerogative to use this section to present complications that impede the attainment of that goal.
TB is predominantly a disease associated with poverty, overcrowding, lack of awareness, limitations in public health resources, lack of political commitment, and lack of clinical expertise. None of these complicating factors are easy to remedy. Adherence to multiple-pill, prolonged, and occasionally unpleasant drug regimens often leads to truncated treatment, resulting in failure to eradicate infection and the emergence of drug resistance. Most active TB cases result from the progression of latent infection rather than community transmission. Active community surveillance, interpreting the results of existing testing modalities, and treating latent TB are all very complicated. Outreach and follow-up of patients with latent and active TB are equally very complex. In resource-rich countries, many new cases of TB occur in recent immigrants and marginalized groups; lack of access to expert medical care remains a significant complication in those segments of society. [85] Finding and allocating funds to achieve the WHO global strategy to eliminate TB is perhaps the major complication. TB, a disease of antiquity, continues to be responsible for the death of millions of people each year. Hopefully, the future of TB will be met with robust vaccine technology, sensitive and specific point-of-use diagnostics, safe and highly active anti-TB drugs, and well-funded public health programs across the globe.
- Deterrence and Patient Education
Deterrence to TB eradication includes:
- Social conditions that favor communicability, particularly poverty and overcrowding
- Lack of political commitment
- Nonspecific signs and symptoms of disease
- Asymptomatic disease
- Failure to consider TB in a differential diagnosis
- Diagnostic tests that may lack sensitivity and specificity
- TB illiteracy
- Pill burden, prolonged duration of treatment, adverse drug effects
- Poor adherence to treatment regimens
- Lack of public health resources
- Absence of robust immunizations that prevent TB infection
- Enhancing Healthcare Team Outcomes
TB is a preventable and curable disease that impacts all segments of humankind. Its diagnosis, treatment, and prevention require coordination between front-line public health officials, adult and pediatric primary care physicians, advanced care practitioners, clinical laboratory technologists, pulmonologists, infectious diseases physicians, pharmacists, nurses, and other healthcare professionals. Skillful management of TB demands expertise in history-taking, physical examination, and interpreting diagnostic tests, coupled with proficiency in implementing evidence-based treatment regimens tailored to individual patient needs. The strategy revolves around developing comprehensive care plans integrating TB diagnosis, treatment, and prevention alongside targeted public health interventions to mitigate transmission risks. Ethically, upholding patient autonomy, confidentiality, and principles of beneficence and non-maleficence underpin TB care, ensuring patients are actively involved in decision-making while safeguarding their well-being. Responsibilities are shared among team members, from timely diagnosis to coordinated care transitions and patient education. Effective interprofessional communication fosters collaboration, optimizing care outcomes by exchanging information and promoting shared decision-making. Care coordination, both within healthcare settings and with community resources, ensures seamless continuity of care and addresses patients' psychosocial needs, ultimately enhancing patient-centered care, outcomes, safety, and team performance in managing tuberculosis.
The complexities of TB care and prevention require the expertise of government officials with specific training to help guide front-line health professionals caring for at-risk and affected patients. Efforts are needed to educate clinicians practicing in low TB endemic areas who are unfamiliar with strategies to diagnose and treat patients with TB. Clinics specializing in TB should be made available to marginalized segments of the population who are at the highest risk of having TB.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Clinical Features of Extrapulmonary Tuberculosis Contributed by Dr. Ellis Tobin
Classes of Technologies and Associated Products Adapted from WHO consolidated guidelines on tuberculosis. Module 3: Diagnosis Rapid diagnosis for tuberculosis detection, 2021 update, World Health Organization. [PMID: 34314130]
Recommendations for Regimens to Treat Latent TB Infection Adapted from [PMID: 32053584]
Drug Regimens for Microbiologically Confirmed Pulmonary Tuberculosis Caused by Drug-Susceptible Organisms Adapted from [PMID: 27516382]
Tuberculosis Pathophysiology Flow Chart Contributed and created by Ellis Tobin, MD
Disclosure: Ellis Tobin declares no relevant financial relationships with ineligible companies.
Disclosure: Debbie Tristram declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Tobin EH, Tristram D. Tuberculosis. [Updated 2024 Mar 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Tuberculosis. [Major Infectious Diseases. 2017] Review Tuberculosis. Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, Knight G, Murray M, Nardell E, Rubin E, et al. Major Infectious Diseases. 2017 Nov 3
- Active Tuberculosis. [StatPearls. 2024] Active Tuberculosis. Jilani TN, Avula A, Zafar Gondal A, Siddiqui AH. StatPearls. 2024 Jan
- Review The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. [Lancet Respir Med. 2018] Review The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. Floyd K, Glaziou P, Zumla A, Raviglione M. Lancet Respir Med. 2018 Apr; 6(4):299-314.
- Fighting the tuberculosis epidemic in the Western Pacific region: current situation and challenges ahead. [Kekkaku. 2010] Fighting the tuberculosis epidemic in the Western Pacific region: current situation and challenges ahead. van Maaren PJ. Kekkaku. 2010 Jan; 85(1):9-16.
- Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. [JAMA. 1999] Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. JAMA. 1999 Aug 18; 282(7):677-86.
Recent Activity
- Tuberculosis - StatPearls Tuberculosis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Abstract and Figures. Tuberculosis Is a major bluster to humanity resist to progress in health-care systems and the widespread weapon of TB control programs. The World Health Organization (WHO ...
Introduction. Disseminated tuberculosis (TB) is defined as the presence of two or more noncontiguous sites resulting from hematogenous dissemination of Mycobacterium tuberculosis, occurring as a result of progressive primary infection, reactivation of a latent focus with subsequent spread,[] or rarely through iatrogenic origin.[] Nowadays, the term miliary TB also refers to progressive and ...
The aim of this review was to provide an updated overview of current efforts to optimize classical diagnostic methods, as well as new molecular and other methodologies, for accurate diagnosis of patients with Mtb infection. Keywords: tuberculosis, diagnosis, laboratory methods, innovative techniques. 1.
Treatment regimen for sensitive, drug resistant and extensive drug resistant tuberculosis has been summarized along with newer drugs recommended for multi drug resistant tuberculosis. This review article has been written after extensive literature study in view of better understanding and to increase awareness regarding tuberculosis, as a ...
Tuberculosis (TB) is an airborne infectious disease with high morbidity and mortality rates, especially in low-income countries. ... This is a comprehensive review of the literature on IGRAs for ...
Abstract. Despite being a treatable and preventable disease, tuberculosis will kill an estimated 30 million people during the current decade. Tuberculosis is a global problem, and increases in case rates are occurring not only in the developing countries of the world but also in several industrialized nations, such as the United States ...
Systematic Review. TB. Tuberculosis. WHO. World Health Organization. ... Five potentially relevant publications were retrieved from the grey literature search for full text review. Of these potentially relevant articles, 65 publications were excluded for various reasons, and 9 evidence-based guidelines met the inclusion criteria and were ...
Tuberculosis. Despite the availability of a cheap and effective treatment, tuberculosis still accounts for millions of cases of active disease and deaths worldwide. The disease disproportionately ...
In this study, the researchers have done a systematic review (a study in which the medical literature is surveyed and appraised using defined methods to reach a consensus view on a specific question) of qualitative studies that asked patients, carers, and health workers which factors contributed to adherence to tuberculosis treatment.
80 81 INTRODUCTION 82 Tuberculosis (TB), caused by Mycobacterium tuberculosis (MTB) infection, remains a significant 83 public health threat, with an estimated 10 million new infections annually1.In 2022, it was the 84 second leading cause of mortality among infectious diseases after COVID-192.Though affecting 85 all countries and age groups, TB is most prevalent in low- and middle-income ...
Objective: To identify literature on health literacy levels and examine its association with tuberculosis treatment adherence and treatment outcomes. Methods: Two authors independently searched Pubmed®, Embase, CINAHL, PsycINFO, Scopus, LILACS, Global Health Medicus and ScienceDirect for articles reporting on health literacy levels and tuberculosis that were published between January 2000 and ...
Tuberculosis is a disease of poverty. Although most high-income countries have estimated tuberculosis incidences of less than ten per 100 000 population per year, the 30 high tuberculosis burden countries (which are predominantly low-income and middle-income countries) have an estimated collective tuberculosis incidence of 183 per 100 000 population per year, with the incidence being above 400 ...
There is growing recognition that tuberculosis (TB) infection and disease exists as a spectrum of states beyond the current binary classification of latent and active TB. Our aim was to systematically map and synthesize published conceptual frameworks for TB states. We searched MEDLINE, Embase and EMcare for review articles from 1946 to September 2023. We included 40 articles that explicitly ...
The sources of this review were consulted from the PubMed, Cochrane Library, and Google Scholar data-bases, with the following keywords: Tuberculosis, Epidemiology, Physiopathology, Diagnosis, and Therapy. The Free-text search terms used were: Extrapulmonary Tuberculosis, Diagnosis advances, and Therapeutic advances.
The aim of this review was to provide an updated overview of current efforts to optimize classical diagnostic methods, as well as new molecular and other methodologies, for accurate diagnosis of patients with Mtb infection. Keywords: tuberculosis; diagnosis; laboratory methods; innovative techniques. 1. Introduction.
Tuberculosis. For purposes of this review, we adopted a standard case definition for TB. According to WHO definitions and reporting frameworks for TB, a bacteriologically-diagnosed case of active TB requires detection of Mycobacterium tuberculosis by smear microscopy, culture or a nucleic acid amplification test such as Xpert MTB/RIF (WHO, 2013).
Diagnosis of tuberculosis, and especially the diagnosis of extrapulmonary tuberculosis, still faces challenges in clinical practice. There are several reasons for this. Methods based on the detection of Mycobacterium tuberculosis (Mtb) are insufficiently sensitive, methods based on the detection of Mtb-specific immune responses cannot always differentiate active disease from latent infection ...
This review article has been written after extensive literature study in view of better understanding and to increase awareness regarding tuberculosis, as a sincere effort that will help eliminate ...
Acta Scientific Pharmacology Volume 2 Issue 8 August 2021 Tuberculosis: An Overview and Review of Literature Surya Kant1, Veenita Mitta2, Anil Kumar Mavi3, Rachna Chaturvedi4, Pooja Singh1* 1Department of Respiratory Medicine, KGMU, Lucknow, India 2Department of Microbiology, Ram Manohar Lohiya Institute of Sciences, India 3Amity Institute of Biotechnology, Amity University, Lucknow, Uttar ...
This literature review found that, despite the global importance of addressing TB-Stigma, there is a paucity of high-quality studies evaluating interventions to reduce TB-stigma. Intervention design across studies was heterogeneous, but education about TB frequently featured as a core intervention activity.
Original Article from The New England Journal of Medicine — Review of Recent Literature on Tuberculosis
Abstract. Tuberculosis (TB) is one of the most ancient diseases of mankind, with molecular evidence going back to over 17,000 years. In spite of newer modalities for diagnosis and treatment of TB, unfortunately, people are still suffering, and worldwide it is among the top 10 killer infectious diseases, second only to HIV.
ABSTRACT: This literature review looks at recent research studies that investigate factors involved in successful tuberculosis (TB) interventions, in particular Directly Observed Therapy Short-Course (DOTS), DOTS +, and incentive programs associated with DOTS programs. The review is based on a bibliography complied by Christina Blumel and ...
The World Health Organization (WHO) Global TB Programme (GTB) would like to announce an upcoming Guideline Development Group meeting for the update of the WHO consolidated guidelines on the treatment of drug-resistant tuberculosis, to be held 24-27 June 2024 in Versoix, Switzerland.The current World Health Organization (WHO) recommendations for treating persons with drug resistant TB are ...
Internet usage has seen a stark global rise over the last few decades, particularly among adolescents and young people, who have also been diagnosed increasingly with internet addiction (IA). IA impacts several neural networks that influence an adolescent's behaviour and development. This article issued a literature review on the resting-state and task-based functional magnetic resonance ...
Circumpolar Indigenous People, such as the Sámi, confront significant challenges stemming from environmental shifts and interrelated issues, profoundly affecting their mental health. Nonetheless, they possess invaluable knowledge and capabilities to navigate and adapt to these transformations. This review aims to investigate peer-reviewed scientific literature, exploring the nexus between ...
The series, aside from the Brod-dominated episode 1, is focused on various aspects of Kafka's life, which was short—he was only 40 when he died, in obscurity, of tuberculosis in 1924.
Prevention of tuberculosis (TB)-related stigma is vital to achieving the World Health Organisation's End TB Strategy target of eliminating TB. However, the process and impact evaluation of interventions to reduce TB-stigma are limited. This literature review aimed to examine the quality, design, implementation challenges, and successes of TB-stigma intervention studies and create a novel ...
E-mail: [email protected]. Website: www.menopause.org. symptoms can be bothersome, lasting a mean duration of 7 to. 9 years, and in one-third of women, can last more than 10 years.2 Hormone therapy (HT) remains the most effective treatment and should be considered in menopausal women aged younger than.
Tuberculosis (TB) encompasses a vast amount of information about a common disease that is challenging to diagnose, treat, and prevent. The following quote by S.T. Cole provides a perspective on the importance of this disease: "More human lives have been lost to tuberculosis than to any other disease."[1] Before the SARS-CoV-2 pandemic, Mycobacterium tuberculosis (Mtb) was the most ...