

Case Examples
Examples of recommended interventions in the treatment of depression across the lifespan.

Children/Adolescents
A 15-year-old Puerto Rican female
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. Her more recent episodes related to her parents’ marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT).
Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety , 26, 98-103. https://doi.org/10.1002/da.20457
Sam, a 15-year-old adolescent
Sam was team captain of his soccer team, but an unexpected fight with another teammate prompted his parents to meet with a clinical psychologist. Sam was diagnosed with major depressive disorder after showing an increase in symptoms over the previous three months. Several recent challenges in his family and romantic life led the therapist to recommend interpersonal psychotherapy for adolescents (IPT-A).
Hall, E.B., & Mufson, L. (2009). Interpersonal Psychotherapy for Depressed Adolescents (IPT-A): A Case Illustration. Journal of Clinical Child & Adolescent Psychology, 38 (4), 582-593. https://doi.org/10.1080/15374410902976338
© Society of Clinical Child and Adolescent Psychology (Div. 53) APA, https://sccap53.org/, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Society of Clinical Child and Adolescent Psychology (Div. 53) APA.
General Adults
Mark, a 43-year-old male
Mark had a history of depression and sought treatment after his second marriage ended. His depression was characterized as being “controlled by a pattern of interpersonal avoidance.” The behavior/activation therapist asked Mark to complete an activity record to help steer the treatment sessions.
Dimidjian, S., Martell, C.R., Addis, M.E., & Herman-Dunn, R. (2008). Chapter 8: Behavioral activation for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 343-362). New York: Guilford Press.
Reprinted with permission from Guilford Press.
Denise, a 59-year-old widow
Denise is described as having “nonchronic depression” which appeared most recently at the onset of her husband’s diagnosis with brain cancer. Her symptoms were loneliness, difficulty coping with daily life, and sadness. Treatment included filling out a weekly activity log and identifying/reconstructing automatic thoughts.
Young, J.E., Rygh, J.L., Weinberger, A.D., & Beck, A.T. (2008). Chapter 6: Cognitive therapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 278-287). New York, NY: Guilford Press.
Nancy, a 25-year-old single, white female
Nancy described herself as being “trapped by her relationships.” Her intake interview confirmed symptoms of major depressive disorder and the clinician recommended cognitive-behavioral therapy.
Persons, J.B., Davidson, J. & Tompkins, M.A. (2001). A Case Example: Nancy. In Essential Components of Cognitive-Behavior Therapy For Depression (pp. 205-242). Washington, D.C.: American Psychological Association. http://dx.doi.org/10.1037/10389-007
While APA owns the rights to this text, some exhibits are property of the San Francisco Bay Area Center for Cognitive Therapy, which has granted the APA permission for use.
Luke, a 34-year-old male graduate student
Luke is described as having treatment-resistant depression and while not suicidal, hoped that a fatal illness would take his life or that he would just disappear. His treatment involved mindfulness-based cognitive therapy, which helps participants become aware of and recharacterize their overwhelming negative thoughts. It involves regular practice of mindfulness techniques and exercises as one component of therapy.
Sipe, W.E.B., & Eisendrath, S.J. (2014). Chapter 3 — Mindfulness-Based Cognitive Therapy For Treatment-Resistant Depression. In R.A. Baer (Ed.), Mindfulness-Based Treatment Approaches (2nd ed., pp. 66-70). San Diego: Academic Press.
Reprinted with permission from Elsevier.
Sara, a 35-year-old married female
Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks.
Bleiberg, K.L., & Markowitz, J.C. (2008). Chapter 7: Interpersonal psychotherapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: a treatment manual (4th ed., pp. 315-323). New York, NY: Guilford Press.
Peggy, a 52-year-old white, Italian-American widow
Peggy had a history of chronic depression, which flared during her husband’s illness and ultimate death. Guilt was a driving factor of her depressive symptoms, which lasted six months after his death. The clinician treated Peggy with psychodynamic therapy over a period of two years.
Bishop, J., & Lane , R.C. (2003). Psychodynamic Treatment of a Case of Grief Superimposed On Melancholia. Clinical Case Studies , 2(1), 3-19. https://doi.org/10.1177/1534650102239085
Several case examples of supportive therapy
Winston, A., Rosenthal, R.N., & Pinsker, H. (2004). Introduction to Supportive Psychotherapy . Arlington, VA : American Psychiatric Publishing.
Older Adults
Several case examples of interpersonal psychotherapy & pharmacotherapy
Miller, M. D., Wolfson, L., Frank, E., Cornes, C., Silberman, R., Ehrenpreis, L.…Reynolds, C. F., III. (1998). Using Interpersonal Psychotherapy (IPT) in a Combined Psychotherapy/Medication Research Protocol with Depressed Elders: A Descriptive Report With Case Vignettes. Journal of Psychotherapy Practice and Research , 7(1), 47-55.
Social Work Practice with Carers

Case Study 2: Josef
Download the whole case study as a PDF file
Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently.
This case study looks at the impact of caring for someone with a mental health problem and of being a young carer , in particular the impact on education and future employment .
When you have looked at the materials for the case study and considered these topics, you can use the critical reflection tool and the action planning tool to consider your own practice.
- One-page profile
Support plan
Transcript (.pdf, 48KB)
Name : Josef Mazur
Gender : Male
Ethnicity : White European
Download resource as a PDF file
First language : English/ Polish
Religion : Roman Catholic
Josef lives in a small town with his mother Dorota who is 39. Dorota was diagnosed with Bi-polar disorder seven years ago after she was admitted to hospital. She is currently unable to work. Josef’s father, Stefan, lives in the same town and he sees him every few weeks. Josef was born in England. His parents are Polish and he speaks Polish at home.
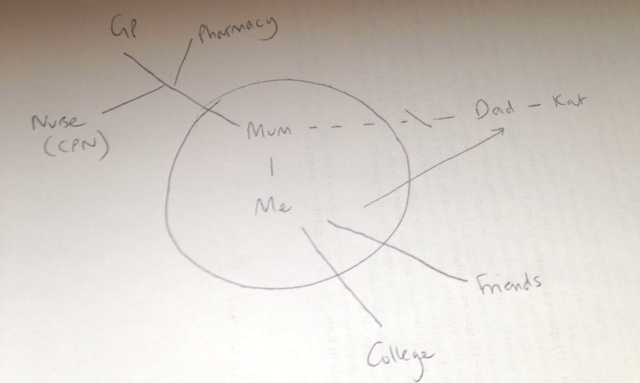
Josef is doing a foundation art course at college. Dorota is quite isolated because she often finds it difficult to leave the house. Dorota takes medication and had regular visits from the Community Psychiatric Nurse when she was diagnosed and support from the Community Mental Health team to sort out her finances. Josef does the shopping and collects prescriptions. He also helps with letters and forms because Dorota doesn’t understand all the English. Dorota gets worried when Josef is out. When Dorota is feeling depressed, Josef stays at home with her. When Dorota is heading for a high, she tries to take Josef to do ‘exciting stuff’ as she calls it. She also spends a lot of money and is very restless.
Josef worries about his mother’s moods. He is worried about her not being happy and concerned at the money she spends when she is in a high mood state. Josef struggles to manage his day around his mother’s demands and to sleep when she is high. Josef has not told anyone about the support he gives to his mother. He is embarrassed by some of the things she does and is teased by his friends, and he does not think of himself as a carer. Josef has recently had trouble keeping up with course work and attendance. He has been invited to a meeting with his tutor to formally review attendance and is worried he will get kicked out. Josef has some friends but he doesn’t have anyone he can confide in. His father doesn’t speak to his mother.
Josef sees some information on line about having a parent with a mental health problem. He sends a contact form to ask for information. Someone rings him and he agrees to come into the young carers’ team and talk to the social worker. You have completed the assessment form with Josef in his words and then done a support plan with him.
Back to Summary
Josef Mazur
What others like and admire about me
Good at football
Finished Arkham Asylum on expert level
What is important to me
Mum being well and happy
Seeing my dad
Being an artist
Seeing my friends
How best to support me
Tell me how to help mum better
Don’t talk down to me
Talk to me 1 to 1
Let me know who to contact if I am worried about something
Work out how I can have some time on my own so I can do my college work and see my friends
Don’t tell mum and my friends
Date chronology completed : 7 March 2016
Date chronology shared with person: 7 March 2016
| 1997 | Josef’s mother and father moved to England from Poznan. | Both worked at the warehouse – Father still works there. |
| 11.11.1999 | Josef born. | Mother worked for some of the time that Josef was young. |
| 2006 | Josef reports that his mother and father started arguing about this time because of money and Josef’s mother not looking after household tasks. | Josef started doing household tasks e.g. cleaning, washing and ironing. |
| 2008 | Josef reports that his mother didn’t get out of bed for a few months. | Josef managed the household during this period. |
| October 2008 | Josef reports that his mother spent lots of money in catalogues and didn’t sleep. She was admitted to hospital. | Mother was in hospital for 6 weeks and was diagnosed with bipolar disorder. Josef began looking after his mother’s medication and says that he started to ‘keep an eye on her.’ |
| May 2010 | Josef’s father moved out to live with his friend Kat. Josef stayed with his mother. | Josef reports that his mother was ‘really sad for a while and then she went round and shouted at them.’ Mother started on different medication and had regular visits from the Community Psychiatric Nurse. Josef said that the CPN told him about his mum’s illness and to let him know if he needed any help but he was managing ok. Josef saw his father every week for a few years and then it was more like every month. Father does not visit Josef or speak to his mother. |
| 2013/14 | Josef reports that his mother got into a lot of debt and they had eviction letters. | Josef’s father paid some of the bills and his mother was referred by the Community Mental Health Team for advice from CAB and started getting benefits. Josef started doing the correspondence. |
| 2015 | Josef left school and went to college. | Josef got an A (art), 4 Cs and 3 Ds GCSE. He says that he ‘would have done better but I didn’t do much work.’ |
| 26 Feb 2016 | Josef got a letter from his tutor at college saying he had to go to a formal review about attendance. | Josef saw information on-line about having a parent with a mental health problem and asked for some information. |
| 2 March 2016 | Phone call from young carer’s team to Josef. | Josef agreed to come in for an assessment. |
| 4 March 2016 | Social worker meets with Josef. | Carer’s assessment and support plan completed. |
| 7 March 2016 | Paperwork completed. | Sent to Josef. |
Young Carers Assessment
Do you look after or care for someone at home?
The questions in this paper are designed to help you think about your caring role and what support you might need to make your life a little easier or help you make time for more fun stuff.
Please feel free to make notes, draw pictures or use the form however is best for you.
What will happen to this booklet?
This is your booklet and it is your way to tell an adult who you trust about your caring at home. This will help you and the adult find ways to make your life and your caring role easier.
The adult who works with you on your booklet might be able to help you with everything you need. If they can’t, they might know other people who can.
Our Agreement
- I will share this booklet with people if I think they can help you or your family
- I will let you know who I share this with, unless I am worried about your safety, about crime or cannot contact you
- Only I or someone from my team will share this booklet
- I will make sure this booklet is stored securely
- Some details from this booklet might be used for monitoring purposes, which is how we check that we are working with everyone we should be
Signed: ___________________________________
Young person:
- I know that this booklet might get shared with other people who can help me and my family so that I don’t have to explain it all over again
- I understand what my worker will do with this booklet and the information in it (written above).
Signed: ____________________________________
Name : Josef Mazur Address : 1 Green Avenue, Churchville, ZZ1 Z11 Telephone: 012345 123456 Email: [email protected] Gender : Male Date of birth : 11.11.1999 Age: 16 School : Green College, Churchville Ethnicity : White European First language : English/ Polish Religion : Baptised Roman Catholic GP : Dr Amp, Hill Surgery
The best way to get in touch with me is:
Do you need any support with communication?
*Josef is bilingual – English and Polish. He speaks English at school and with his friends, and Polish at home. Josef was happy to have this assessment in English, however, another time he may want to have a Polish interpreter. It will be important to ensure that Josef is able to use the words he feels best express himself.
About the person/ people I care for
I look after my mum who has bipolar disorder. Mum doesn’t work and doesn’t really leave the house unless she is heading for a high. When Mum is sad she just stays at home. When she is getting hyper then she wants to do exciting stuff and she spends lots of money and she doesn’t sleep.
Do you wish you knew more about their illness?
Do you live with the person you care for?
What I do as a carer It depends on if my mum has a bad day or not. When she is depressed she likes me to stay home with her and when she is getting hyper then she wants me to go out with her. If she has new meds then I like to be around. Mum doesn’t understand English very well (she is from Poland) so I do all the letters. I help out at home and help her with getting her medication.
Tell us what an average week is like for you, what kind of things do you usually do?
Monday to Friday
Get up, get breakfast, make sure mum has her pills, tell her to get up and remind her if she’s got something to do.
If mum hasn’t been to bed then encourage her to sleep a bit and set an alarm
College – keep phone on in case mum needs to call – she usually does to ask me to get something or check when I’m coming home
Go home – go to shops on the way
Remind mum about tablets, make tea and pudding for both of us as well as cleaning the house and fitting tea in-between, ironing, hoovering, hanging out and bringing in washing
Do college work when mum goes to bed if not too tired
More chores
Do proper shop
Get prescription
See my friends, do college work
Sunday – do paper round
Physical things I do….
(for example cooking, cleaning, medication, shopping, dressing, lifting, carrying, caring in the night, making doctors appointments, bathing, paying bills, caring for brothers & sisters)
I do all the housework and shopping and cooking and get medication
Things I find difficult
Emotional support I provide…. (please tell us about the things you do to support the person you care for with their feelings; this might include, reassuring them, stopping them from getting angry, looking after them if they have been drinking alcohol or taking drugs, keeping an eye on them, helping them to relax)
If mum is stressed I stay with her
If mum is depressed I have to keep things calm and try to lighten the mood
She likes me to be around
When mum is heading for a high wants to go to theme parks or book holidays and we can’t afford it
I worry that mum might end up in hospital again
Mum gets cross if I go out
Other support
Please tell us about any other support the person you care for already has in place like a doctor or nurse, or other family or friends.
The GP sees mum sometimes. She has a nurse who she can call if things get bad.
Mum’s medication comes from Morrison’s pharmacy.
Dad lives nearby but he doesn’t talk to mum.
Mum doesn’t really have any friends.
Do you ever have to stop the person you care for from trying to harm themselves or others?
Some things I need help with
Sorting out bills and having more time for myself
I would like mum to have more support and to have some friends and things to do
On a normal week, what are the best bits? What do you enjoy the most? (eg, seeing friends, playing sports, your favourite lessons at school)
Seeing friends
When mum is up and smiling
Playing football
On a normal week, what are the worst bits? What do you enjoy the least? (eg cleaning up, particular lessons at school, things you find boring or upsetting)
Nagging mum to get up
Reading letters
Missing class
Mum shouting
Friends laugh because I have to go home but they don’t have to do anything
What things do you like to do in your spare time?
Do you feel you have enough time to spend with your friends or family doing things you enjoy, most weeks?
Do you have enough time for yourself to do the things you enjoy, most weeks? (for example, spending time with friends, hobbies, sports)
Are there things that you would like to do, but can’t because of your role as a carer?
Can you say what some of these things are?
See friends after college
Go out at the weekend
Time to myself at home
It can feel a bit lonely
I’d like my mum to be like a normal mum
School/ College Do you think being your caring role makes school/college more difficult for you in any way?
If you ticked YES, please tell us what things are made difficult and what things might help you.
Things I find difficult at school/ college
Sometimes I get stressed about college and end up doing college work really late at night – I get a bit angry when I’m stressed
I don’t get all my college work done and I miss days
I am tired a lot of the time
Things I need help with…
I am really worried they will kick me out because I am behind and I miss class. I have to meet my tutor about it.
Do your teachers know about your caring role?
Are you happy for your teachers and other staff at school/college to know about your caring role?
Do you think that being a carer will make it more difficult for you to find or keep a job?
Why do you think being a carer is/ will make finding a job more difficult?
I haven’t thought about it. I don’t know if I’ll be able to finish my course and do art and then I won’t be able to be an artist.
Who will look after mum?
What would make it easier for you to find a job after school/college?
Finishing my course
Mum being ok
How I feel about life…
Do you feel confident both in school and outside of school?
Somewhere in the middle
In your life in general, how happy do you feel?
Quite unhappy
In your life in general, how safe do you feel?
How healthy do you feel at the moment?
Quite healthy
Being heard
Do you think people listen to what you are saying and how you are feeling?
If you said no, can you tell us who you feel isn’t listening or understanding you sometimes (eg, you parents, your teachers, your friends, professionals)
I haven’t told anyone
I can’t talk to mum
My friends laugh at me because I don’t go out
Do you think you are included in important decisions about you and your life? (eg, where you live, where you go to school etc)
Do you think that you’re free to make your own choices about what you do and who you spend your time with?
Not often enough
Is there anybody who knows about the caring you’re doing at the moment?
If so, who?
I told dad but he can’t do anything
Would you like someone to talk to?
Supporting me Some things that would make my life easier, help me with my caring or make me feel better
I don’t know
Fix mum’s brain
People to help me if I’m worried and they can do something about it
Not getting kicked out of college
Free time – time on my own to calm down and do work or have time to myself
Time to go out with my friends
Get some friends for mum
I don’t want my mum to get into trouble
Who can I turn to for advice or support?
I would like to be able to talk to someone without mum or friends knowing
Would you like a break from your caring role?
How easy is it to see a Doctor if you need to?
To be used by social care assessors to consider and record measures which can be taken to assist the carer with their caring role to reduce the significant impact of any needs. This should include networks of support, community services and the persons own strengths. To be eligible the carer must have significant difficulty achieving 1 or more outcomes without support; it is the assessors’ professional judgement that unless this need is met there will be a significant impact on the carer’s wellbeing. Social care funding will only be made available to meet eligible outcomes that cannot be met in any other way, i.e. social care funding is only available to meet unmet eligible needs.
Date assessment completed : 7 March 2016
Social care assessor conclusion
Josef provides daily support to his mum, Dorota, who was diagnosed with bipolar disorder seven years ago. Josef helps Dorota with managing correspondence, medication and all household tasks including shopping. When Dorota has a low mood, Josef provides support and encouragement to get up. When Dorota has a high mood, Josef helps to calm her and prevent her spending lots of money. Josef reports that Dorota has some input from community health services but there is no other support. Josef’s dad is not involved though Josef sees him sometimes, and there are no friends who can support Dorota.
Josef is a great support to his mum and is a loving son. He wants to make sure his mum is ok. However, caring for his mum is impacting: on Josef’s health because he is tired and stressed; on his emotional wellbeing as he can get angry and anxious; on his relationship with his mother and his friends; and on his education. Josef is at risk of leaving college. Josef wants to be able to support his mum better. He also needs time for himself, to develop and to relax, and to plan his future.
Eligibility decision : Eligible for support
What’s happening next : Create support plan
Completed by Name : Role : Organisation :
Name: Josef Mazur
Address 1 Green Avenue, Churchville, ZZ1 Z11
Telephone 012345 123456
Email [email protected]
Gender: Male
Date of birth: 11.11.1999 Age: 16
School Green College, Churchville
Ethnicity White European
First language English/ Polish
Religion Baptised Roman Catholic
GP Dr Amp, Hill Surgery
My relationship to this person son
Name Dorota Mazur
Gender Female
Date of birth 12.6.79 Age 36
First language Polish
Religion Roman Catholic
Support plan completed by
Organisation
|
|
| |
|
|
| |
|
| ||
|
| ||
Date of support plan: 7 March 2016
This plan will be reviewed on: 7 September 2016
Signing this form
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Josef has given consent to share this support plan with the CPN but does not want it to be shared with his mum.
Mental health
The social work role with carers in adult mental health services has been described as: intervening and showing professional leadership and skill in situations characterised by high levels of social, family and interpersonal complexity, risk and ambiguity (Allen 2014). Social work with carers of people with mental health needs, is dependent on good practice with the Mental Capacity Act where practitioner knowledge and understanding has been found to be variable (Iliffe et al 2015).
- Carers Trust (2015) Mental Health Act 1983 – Revised Code of Practice Briefing
- Carers Trust (2013) The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England
- Mind, Talking about mental health
- Tool 1: Triangle of care: self-assessment for mental health professionals – Carers Trust (2013) The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England Second Edition (page 23 Self-assessment tool for organisations)
Mental capacity, confidentiality and consent
Social work with carers of people with mental health needs, is dependent on good practice with the Mental Capacity Act where practitioner knowledge and understanding has been found to be variable (Iliffe et al 2015). Research highlights important issues about involvement, consent and confidentiality in working with carers (RiPfA 2016, SCIE 2015, Mental Welfare Commission for Scotland 2013).
- Beddow, A., Cooper, M., Morriss, L., (2015) A CPD curriculum guide for social workers on the application of the Mental Capacity Act 2005 . Department of Health
- Bogg, D. and Chamberlain, S. (2015) Mental Capacity Act 2005 in Practice Learning Materials for Adult Social Workers . Department of Health
- Department of Health (2015) Best Interest Assessor Capabilities , The College of Social Work
- RiPfA Good Decision Making Practitioner Handbook
- SCIE Mental Capacity Act resource
- Tool 2: Making good decisions, capacity tool (page 70-71 in good decision making handbook)
Young carers
A young carer is defined as a person under 18 who provides or intends to provide care for another person. The concept of care includes practical or emotional support. It is the case that this definition excludes children providing care as part of contracted work or as voluntary work. However, the local authority can ignore this and carry out a young carer’s need assessment if they think it would be appropriate. Young carers, young adult carers and their families now have stronger rights to be identified, offered information, receive an assessment and be supported using a whole-family approach (Carers Trust 2015).
- SCIE (2015) Young carer transition in practice under the Care Act 2014
- SCIE (2015) Care Act: Transition from children’s to adult services – early and comprehensive identification
- Carers Trust (2015) Rights for young carers and young adult carers in the Children and Families Act
- Carers Trust (2015) Know your Rights: Support for Young Carers and Young Adult Carers in England
- The Children’s Society (2015) Hidden from view: The experiences of young carers in England
- DfE (2011) Improving support for young carers – family focused approaches
- ADASS and ADCS (2015) No wrong doors: working together to support young carers and their families
- Carers Trust, Supporting Young Carers and their Families: Examples of Practice
- Refugee toolkit webpage: Children and informal interpreting
- SCIE (2010) Supporting carers: the cared for person
- SCIE (2015) Care Act Transition from children’s to adults’ services – Video diaries
- Tool 3: Young carers’ rights – The Children’s Society (2014) The Know Your Rights pack for young carers in England!
- Tool 4: Vision and principles for adults’ and children’s services to work together
Young carers of parents with mental health problems
The Care Act places a duty on local authorities to assess young carers before they turn 18, so that they have the information they need to plan for their future. This is referred to as a transition assessment. Guidance, advocating a whole family approach, is available to social workers (LGA 2015, SCIE 2015, ADASS/ADCS 2011).
- SCIE (2012) At a glance 55: Think child, think parent, think family: Putting it into practice
- SCIE (2008) Research briefing 24: Experiences of children and young people caring for a parent with a mental health problem
- SCIE (2008) SCIE Research briefing 29: Black and minority ethnic parents with mental health problems and their children
- Carers Trust (2015) The Triangle of Care for Young Carers and Young Adult Carers: A Guide for Mental Health Professionals
- ADASS and ADCS (2011) Working together to improve outcomes for young carers in families affected by enduring parental mental illness or substance misuse
- Ofsted (2013) What about the children? Joint working between adult and children’s services when parents or carers have mental ill health and/or drug and alcohol problems
- Mental health foundation (2010) MyCare The challenges facing young carers of parents with a severe mental illness
- Children’s Commissioner (2012) Silent voices: supporting children and young people affected by parental alcohol misuse
- SCIE, Parental mental health and child welfare – a young person’s story
Tool 5: Family model for assessment
- Tool 6: Engaging young carers of parents with mental health problems or substance misuse
Young carers and education/ employment
Transition moments are highlighted in the research across the life course (Blythe 2010, Grant et al 2010). Complex transitions required smooth transfers, adequate support and dedicated professionals (Petch 2010). Understanding transition theory remains essential in social work practice (Crawford and Walker 2010). Partnership building expertise used by practitioners was seen as particular pertinent to transition for a young carer (Heyman 2013).
- TLAP (2013) Making it real for young carers
- Learning and Work Institute (2018) Barriers to employment for young adult carers
- Carers Trust (2014) Young Adult Carers at College and University
- Carers Trust (2013) Young Adult Carers at School: Experiences and Perceptions of Caring and Education
- Carers Trust (2014) Young Adult Carers and Employment
- Family Action (2012) BE BOTHERED! Making Education Count for Young Carers

Download The Triangle of Care as a PDF file
The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England
The Triangle of Care is a therapeutic alliance between service user, staff member and carer that promotes safety, supports recovery and sustains wellbeing…

Download the Capacity Tool as a PDF file
Capacity Tool Good decision-making Practitioners’ Handbook
The Capacity tool on page 71 has been developed to take into account the lessons from research and the case CC v KK. In particular:
- that capacity assessors often do not clearly present the available options (especially those they find undesirable) to the person being assessed
- that capacity assessors often do not explore and enable a person’s own understanding and perception of the risks and advantages of different options
- that capacity assessors often do not reflect upon the extent to which their ‘protection imperative’ has influenced an assessment, which may lead them to conclude that a person’s tolerance of risks is evidence of incapacity.
The tool allows you to follow steps to ensure you support people as far as possible to make their own decisions and that you record what you have done.

Download Know your rights as a PDF file
Tool 3: Know Your Rights Young Carers in Focus
This pack aims to make you aware of your rights – your human rights, your legal rights, and your rights to access things like benefits, support and advice.
Need to know where to find things out in a hurry? Our pack has lots of links to useful and interesting resources that can help you – and help raise awareness about young carers’ issues!
Know Your Rights has been produced by Young Carers in Focus (YCiF), and funded by the Big Lottery Fund.
Tool 4: Vision and principles for adults’ and children’s services to work together to support young carers
Download the tool as a PDF file
You can use this tool to consider how well adults’ and children’s services work together, and how to improve this.
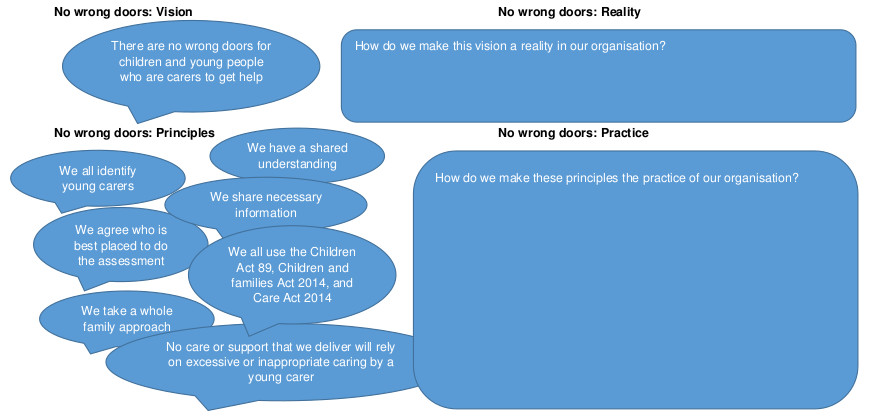
Click on the diagram to open full size in a new window
This is based on ADASS and ADCS (2015) No wrong doors : working together to support young carers and their families
Download the tool as a PDF file
You can use this tool to help you consider the whole family in an assessment or review.
What are the risk, stressors and vulnerability factors?
How is the child/ young person’s wellbeing affected?
How is the adult’s wellbeing affected?

What are the protective factors and available resources?
This tool is based on SCIE (2009) Think child, think parent, think family: a guide to parental mental health and child welfare
Tool 6: Engaging young carers
Young carers have told us these ten things are important. So we will do them.
- Introduce yourself. Tell us who you are and what your job is.
- Give us as much information as you can.
- Tell us what is wrong with our parents.
- Tell us what is going to happen next.
- Talk to us and listen to us. Remember it is not hard to speak to us we are not aliens.
- Ask us what we know and what we think. We live with our parents; we know how they have been behaving.
- Tell us it is not our fault. We can feel guilty if our mum or dad is ill. We need to know we are not to blame.
- Please don’t ignore us. Remember we are part of the family and we live there too.
- Keep on talking to us and keeping us informed. We need to know what is happening.
- Tell us if there is anyone we can talk to. Maybe it could be you.

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Social work practice in community mental health
During the past twenty years, the mental health field has become increasingly cognizant of the interaction between social life and mental status—a relationship that is the basis of traditional social work practice. Social work is committed to improving the interaction among individuals, among institutions, and between people and institutions to enhance the general quality of life. However, in mental health, the major concern (the “dependent variable” in research jargon) is mental status. This article is concerned with social work’s role in community mental health: the activities that enable the social worker to contribute to the improvement of an individual’s mental status while maintaining a commitment to viewing the person in the environment and to improving the overall quality of social life.
As a profession, social work is concerned with all spheres of interaction between people and their environments. Social workers practice in the realm of formal organizations of care and control; are concerned with the social, psychological, and jural dimensions of the family; and have become increasingly interested in the everyday support systems that function among friends and acquaintances. All these concerns have been identified, in one way or another, with the treatment of mental disorders or the promotion of mental health.
To the consternation of many traditional mental health professionals, the field of community mental health has become so elastic that it now includes almost all kinds of ameliorative activity. This expanded purview derives from the association of a myriad of social factors with the development of mental disorders and from the concomitant tendency to equate social well-being with mental well-being. For instance, the relationship between social class and mental illness and the relationship between social stress and mental illness clearly indicate that poor people are at the greatest risk of developing mental disorders.
Because of these relationships, it is tempting to conclude that full employment, better housing for the poor, national health insurance, and an array of poverty programs might be the best means to reduce mental disorders in a society. Unfortunately, there is little evidence to support this conclusion. Such policies and programs are laudable in their own right, but their impact on the mental status of the individual is subject to question. 1 The equation of social well-being and mental well-being is like the Calvinist equation of wealth with salvation: both are nice, but not necessarily related.
What does it mean, then, to “contribute to the improvement of individual mental status” while “maintaining a commitment to improving the overall quality of social life”? The answer depends largely on how a mental health “problem” and a mental health “service” are construed.
INAPPROPRIATE LABELS
As one moves farther from the traditional concerns of mental health (with psychoses, for example), the reliability of the assessment of mental status becomes poorer and the risk of inappropriately labeling “problems of living” as “mental disorders” becomes greater. Similarly, when one approaches human problems whose relationship to discernible mental disorders is ambiguous or distant, the definition of a “mental health service” becomes problematic.
Current empirical understanding does not permit a more elegant solution in either case. Mental disorders are variously defined and diagnosed either in narrow or broad terms. And a mental health service is often what Congress, the National Institute of Mental Health, state legislatures, or local citizens’ advisory boards are willing to pay for.
The clinical risks associated with inappropriate labels make it incumbent on mental health practitioners to be specific and judicious in the use of labels. Further, the treatment of individuals in mental health settings, as opposed to social service or “generic” settings, may discourage potential clients who “know” that only “crazy people” (or members of any devalued group for that matter) go there for help. For this reason, it is often necessary for mental health agencies to assume names that disguise their purpose or spoof the severity of their clients’ problems. (In the past, the authors have been aware of such examples as the Daily Planet in Richmond, Virginia, and the Cabin Fever Clinic in Anchorage, Alaska.) Similarly, in many cases practitioners must allow clients to treat a meaningful diagnosis as a euphemism for problems of living. This obviates the often needless semantic battles over the clinician’s specific meaning and right to pass judgment. Admittedly, these are expedient methods of relieving the dilemma of its horns, but they appear unavoidable in many circumstances and are therefore widely practiced.
Following the same logic of expediency, the authors regard a “mental health service” as whatever service is necessary to improve what clients (except those who are a danger to themselves or others) regard as a less-than-desirable mental status, regardless of the diagnostic description. Although this definition permits a broad interpretation, priorities pertaining to the more reliably assessed mental health problems and to the expenditure of limited funds justifiably narrow the field. That is, mental health services must pay more attention to problems which are derivative of chronic schizophrenia than to those that are only marginally related to mental status.
The following is an example of how broadly the term “mental health service” can be interpreted:
The executive director of a community mental health center (a psychiatrist) was annoyed with the director of the children’s service (a social worker) because she had allowed her staff to provide day care to children of single working mothers whom she believed to be an at-risk population. The executive director informed the children’s service director that no further funds could be expended on this program because it was not a mental health service. She replied that a day care service for children of single mothers who were under stress was a mental health service. Authority prevailed, but the issue was never resolved.
Therefore, the day care service ceased to be a mental health service; it became an “educational supplement.” However, emergency housing was considered an important contribution to mental health and thus became a mental health service. These distinctions came about because the local school district had funds for day care, whereas the mental health system had money for emergency shelter. Subsequently, when the mental health system had fewer funds, shelter became a “social service” and received support from elsewhere.
These are the political concerns that govern the organization and subsidy of mental health care. Such distinctions are authoritative and they are usually arbitrary. Fortunately, the activities of social work transcend their settings. The profession is bigger than the organization of care. The social worker in community mental health is not only concerned with duly sanctioned mental health services but is committed to the application of whatever services can reasonably be expected to improve the mental status of a client over time or to prevent the predictable deterioration of mental status. In the broadest and most important sense, this is what differentiates casework from psychotherapy. If a single mother needs day care for her children to alleviate her anxiety, the case plan should include such services—within the mental health system if they are provided there or within the school system if that is where they are to be found.
Traditional mental health settings are not the only ones that provide mental health services. Family service agencies, youth service bureaus, and many other general social service agencies provide services that are legitimately within the realm of mental health. Many of these agencies provide better services than the traditional agencies. However, in this article, the authors have chosen to focus on the activities of the traditional agencies because these agencies have brought mental health services to the general population, especially to those with discernible mental disorders.
In the past twenty years, two practice models have developed as a result of the community care and community mental health movements. The community care movement has spawned a practice model based primarily on legal and administrative mandates designed to minimize the violation of the patient’s civil rights and to maximize the patient’s right to “fail.” The community mental health movement is based on the epidemiological model. The remainder of this article will be devoted to a discussion of the two models (including their history and problems and the role of the social worker) and to the relationship between the objectives of social work and the practice of community mental health.
COMMUNITY CARE
According to the U.S. General Accounting Office, community care seeks to
(1) Prevent both unnecessary admission to and retention in institutions; (2) Find and develop appropriate alternatives in the community for housing, treatment, training, education, and rehabilitation of the mentally disabled who do not need to be in institutions; (3) Improve conditions, care, and treatment for those who need institutional care …; [(4) Entitle] mentally disabled persons to live in the least restrictive environment necessary and to lead their lives as normally and independently as they can. 2
These principles have been given teeth by administrative codes, state and federal law, and judicial decisions that have formed what amounts to a judicial and statutory model for practice. The U.S. General Accounting Office goes on to say:
Judicially imposed standards in New York and Alabama provide that those states shall make every attempt to move residents of the designated institutions from (1) more to less structured living; (2) larger to smaller facilities; (3) larger to smaller living units: (4) group to individual residences; (5) places segregated from the community to places integrated with community living and programming; (6) dependent to independent living. 3
The Lanterman-Petris-Short Act, passed in California in 1969, is tantamount to a patient’s bill of rights. The act guarantees patients in California the right to a judicial hearing with respect to involuntary confinement and imposes hard evidentiary standards for involuntary admissions. The act also allows patients to refuse certain types of treatment, such as shock treatment and lobotomy. An October 1979 decision in Boston (Rogers et al . v. Okin , U.S. Court, District of Massachusetts, 75–1610–T) allows patients to refuse antipsychotic medication and seclusion unless they are dangerous to themselves or others. Furthermore, the 1972 Wyatt v. Stickney decision in Alabama confirmed that involuntary patients have a right to treatment, not merely custodial care. And there have been other efforts to extend the right-to-treatment principle to community care. 4
Traditionally, social workers have been responsible for managing the patient’s transition from hospital to community. In California, from 1946 until the early 1970s, social workers in the Bureau of Social Work had primary responsibility for community placement and supervision. Although the treatment of psychological disturbance remained within the purview of the medical profession, social workers supervised former patients and, except in acute cases, dealt with the ex-patients’ various psychosocial needs. Ex-patients in family care homes were often on probationary leave from the hospital and could be moved from one family care setting to another or back to the hospital at the discretion of the social worker in charge. To the extent that placements were in good supply, this discretionary power was believed to be an important factor in maintaining high-quality care.
With the growing recognition of patients’ rights, placement workers lost much of the power previously attached to their role. Statutory, judicial, and administrative decisions placed substantial limits on professional discretion and clearly indicated that judgment must err on the side of liberty. Thus, as criteria for involuntary admissions became more stringent, the population of potential clients whose need for institutional care was ambiguous—that group for which the error rate of clinical judgment would be high—was no longer permitted to be admitted involuntarily to mental hospitals. The rationale for this decision was that the benefits of institutional treatment of this group as a whole could not be expected to exceed the therapeutic liabilities of forced treatment or to justify the abrogation of a citizen’s right to liberty. 5
RIGHT TO FAIL
The growing emphasis on the civil rights of patients did more than remove power from placement workers. Mandates for treatment in the least restrictive environment, for the right to treatment rather than mere custodial care, and for the right to refuse treatment have molded the placement worker’s role, providing a framework or model for decision-making and practice. These mandates stimulated the development of a new logic of decision-making, based on the overt consideration of statistical risk. The placement worker must now continually weigh the client’s ability to cope with minimally restrictive environments against the repercussions of failure. This is certainly not a new dilemma in social work practice. However, now the client’s right to fail—and perhaps even his or her right to fail repeatedly—is mandated by law.
Optimally, a placement worker encourages constructive risk-taking while minimizing the impact of failure. To achieve this, systematic attention must be paid to each case, and individualized social support for clients must be developed. Stein, Test, and Marx defined such support as the set of relationships adequate to assure that a client’s needs are addressed without discouraging self-sufficiency. 6 Individualized social support requires a thorough assessment of the client’s current problem-solving capabilities and the existing set of effective and affective relationships, that is, an assessment of the relationship between the client’s mental status and the social context in which the client functions.
Mental status must be assessed in terms of the client’s tolerance of social relationships and the impact of the client’s mental status on those relationships. This assessment ought to include attention to a client’s ability to function within a set of reciprocal relations rather than in a dependent manner. With such an assessment in mind and by monitoring each case, the worker may develop necessary buttresses and change them as necessary to provide either more support or less support, depending on the client’s social situation and mental status.
FOUR ISSUES
In the future, social workers in community care must attend to four salient issues within a minimum treatment or confinement/right-to-fail framework: (1) the burden on the community of a concentrated number of ex-mental patients, (2) matching clients to optimal environments, (3) case management, and (4) medication.
Burden on the Community
Many urban communities have been overwhelmed by an influx of ex-mental patients. Their courts are clogged with disordered petty offenders and their subway stations and doorways are haunted by disheveled, vaguely menacing individuals whose “community care” has been negligible. Although sheltered-care residents pose some burden to local communities, it is the free-living ex-patients that are the most troublesome and threatening.
Elsewhere, the authors have made some specific recommendations for policy and programs with respect to this population that will not be repeated here. 7 The central point, however, is worth repeating: social support must become more than a casework catch-phrase. Social workers must define in more specific operational ways the meaning of social support systems, especially when networks of kin cannot be activated. Developing effective networks of indigenous helpers is crucial to multiply the effect of such helpers and creates a first line of acceptable response to the periodic crises of ex-patients in the community.
It is not enough to define social support systems the way an anthropologist would limn the structure of mutual aid as it naturally occurs. Social workers must learn how to use and develop natural or surrogate helping networks, and this requires more practice-based research designed to yield practice materials. Although much attention has been focused on support systems, on outreach, and on community-building, little has been accomplished. 8 Nor has the profession oriented curricula in schools of social work to reflect interest in these areas. Thus, a commitment to defining, implementing, and teaching methods of social support is an immediate challenge to the profession.
Matching People to Optimal Environments
To date, the placement of former patients in the community has involved a largely unspecified process of finding the best fit between the client and available environmental options. Researchers and practitioners have emphasized that diverse types of individuals fare differently in treatment environments that present various physical and cultural barriers to adjustment and demand either much or little emotional involvement by residents. 9 Little research has been done on the placement process itself, however. Segal and Aviram described the goal of “best available fit” and the political contingencies associated with its achievement, but research on testable placement models is needed. 10 To this end, practitioners must document the placement-decision process in much greater detail.
Much more also needs to be known about the methods by which social workers monitor the progress of ex-patients in community care. To some extent, this is a matter of understanding the impact of mental disorders on social life to achieve greater benefits for clients from programs. However, “burnout” among practitioners may also be reduced through the study of activities constituting the monitoring role and through adjustments to lesser the tedium of routine and the discouragement that results when clients do not improve.
Case Management
By defining and developing the case management role, social work can build a strong base for its future practice in community care. Because there are as yet no specified methods, case management is little more than a goal of coordinated care. Of particular importance is the question of the role of case management in casework settings: Are case managers to be considered specialists who concentrate on coordinating resources and on continuity of care, or should case management be a general activity of casework to be performed by all workers? Further, can difficult problems of case management, such as the tracking of transient clients, be solved without infringing on the rights of ex-patients?
Surber described five functions of the case manager: assessment, planning, linkage, monitoring, and advocacy. 11 Empirical investigation of such procedures and their relationship to established casework methods, the organization of care, and civil rights issues is the next logical step in the development of an effective case management program.
Consequences of Medication
To the degree that the major tranquilizers measure up to their promised performance—inhibiting the symptoms of psychosis without affecting social functioning—they are not the concern of social welfare. Unfortunately, the drugs fail to perform well for some individuals and produce undesired side effects. Moreover, their administration is abused, and there is a notable lack of adequate supervision and follow-up of patients who receive the drugs.
The consequences of medication—its impact on social functioning—are within the purview of social work practice. The authors do not advocate the prescription of drugs by social workers but emphasize that the behavior and side effects associated with medication should be a part of every mental health social worker’s education. Graduate social work curricula are sorely lacking in this area; consequently, many practitioners are not adequately prepared to understand the important role of medication in their clients’ lives.
In a similar vein, social workers must also be able to intervene in the process of self-medication in which many ex-patients are engaged. It is common to find ex-patients medicating themselves with their own or collectively created concoctions of major tranquilizers, opiates, barbiturates, alcohol, marijuana, cocaine, and even LSD. 12 If mental health social workers are to understand the behavior of these clients, they must have some education about the effects of these substances, used alone or in combination.
EPIDEMIOLOGICAL MODEL
To some extent, the community mental health movement grew out of the community care movement and its conflict with advocates of improved care in state mental hospitals. Its emergence is usually traced to the passage of the Community Mental Health Centers Act of 1963 (P.L. 88–164) that provided for the establishment of community mental health centers in “catchment areas” with at least 75,000 but no more than 200,000 residents.
These centers were to be concerned with the mental health of everyone in their designated areas and, to be eligible for construction funds, were required to provide five services: inpatient, outpatient, partial hospitalization, emergency, and consultation and education. The 1975 amendments to the act (P.L. 94–63) increased the number of required services by seven: diagnostic, rehabilitative, precare and aftercare, training, research and evaluation, screening, and provision for community living arrangements. The legislation also required that the full range of twelve services be provided to children, the elderly, drug abusers or addicts, and alcohol abusers or alcoholics.
The community mental health movement’s focus on community-based treatment and its emphasis on the impact of social life on mental status places it squarely within the domain of social welfare. Indeed, despite the greater authority accorded the medical profession, social workers staff more full-time positions and provide more services than any other professional group in community mental health centers. 13
The comprehensive nature of a good community mental health center complements the traditional versatility of social work and offers many roles for practitioners. Social workers may become involved in every dimension of operation—from administration to emergency services. Theoretically, the community mental health center offers social workers the opportunity to address the needs of the “total” individual, rather than administer treatment geared solely to the improvement of mental status.
The traditional role of the epidemiologist has been to discover the causes of a disorder’s appearance in a population. Usually, epidemiologists specify the causal mechanism and public health practitioners then develop the method of attack on the causal chain.
Figure 1 represents a slightly modified epidemiological model derived from the study of infectious diseases. Although the authors do not mean to imply that mental ill-health is infectious or that the problem confronted necessarily has to be a disease, they believe that this model offers a framework for social work practice in community mental health. It is a framework not only for the delivery of direct services, but also for the planning and evaluation of community mental health services.

Epidemiological Framework
At the direct-service level, the model suggests an investigative, empirical approach to ferreting out and detailing material that enables: the worker to understand and have an effect on each component: the host, the contributors, the environmental factors, and the problem itself. (The term “contributors” has been substituted for the epidemiological term “agents,” since, unlike diseases, the causes of most mental disorders are not known.) Figure 1 depicts the interrelations among the four components of the model. As illustrated by the plus and minus poles of each component, influences are variable. Since all components interact, the process described by the model can, in combination with variable influences, be complex.
All models of this sort are liable to appear simple and mechanistic. It is, therefore, important to keep in mind that the purpose of such a model is to illustrate how a case can be analyzed and evaluated. The model does not provide a formula for clinical judgment; nor is it a graphic representation of wisdom. It is simply a useful way of viewing a human dilemma in its proper context. It is a framework for bringing to bear the most complete and complex information possible.
The social worker’s role is that of a detective working with a client to develop the best understanding of each component. Unlike practice models based exclusively on clinical theory, assumptions about discrete “facts” or about the interaction between components of this model must, whenever possible, be validated or tested. The social worker must use the principles of scientific case study (single-subject designs) to assess changes in clients over time. The worker applies the validation and hypothesis-testing techniques of the field researcher, who uses corroboration, multiple observations, and experimental manipulations to achieve a significant degree of empiricism. 14
Perhaps the best way to understand the validation process is by way of example. Let us take the case of an individual with terminal cancer who tells his social worker that he really wishes that someone would tell him what he suffers from. In this situation the social worker seeks to keep the family functioning as a unit while coming to terms with the imminent death of a member and tries to help the dying person cope with the approach of death.
As a first step, the worker speaks to the physician to confirm the patient’s report. The physician may inform the worker that he has communicated the information to the patient several times. The problem thus appears to be denial in the host . Or the physician may indicate that he has not responded to the patient’s questions. The problem thus appears to be avoidance by the physician, a contributor to the host’s anxiety. The worker must also assess the relationship between the patient and his family to determine the strength of environmental factors contributing to denial, for instance. Following such validation, the worker is prepared to plan a strategy that will enable the physician to communicate the information or the patient to hear and understand what is said. The worker must then check the outcomes during the course of the service relationship and after the designated service period has come to an end.
The epidemiological problem-solving framework accommodates various theoretical approaches and, given the assessment of all four components and their interaction, requires the selection of the most useful alternative interventions. The framework accommodates not only a medical model but also a deviance perspective in that the problem, located with the host, is interactive with environmental contingencies. There is always an emphasis on the environmental context and the constraints applied or degrees of freedom allowed by specified components. Problems that appear similar may be treated differently based on the intransigence or tractability of environmental factors.
With respect to planning and evaluation, the epidemiological framework is founded on a preventive model that is concerned with the maximum utility of mental health services for the social group. Outcome is evaluated in relation to changes in rates of occurrence of specific problems within the group and activities are differentiated by the state of the problem in the host. Activities consist of primary, secondary, and tertiary prevention.
Primary Prevention
Primary prevention activities are directed toward populations at risk, that is, those individuals with the highest probability of developing a specific problem but who do not as yet have it. They are evaluated in relation to their efficacy in reducing the incidence or number of new cases of a problem. Although all social work skills are used to implement primary-prevention activities, three (consultation and education, crisis intervention, and community organization) have become the major techniques of primary prevention.
Education and consultation programs of community mental health centers have been the focal point of primary prevention. Such programs have involved family life education and lectures on the impact of stress, retirement, and the benefits of social support. In addition to educating the public, the purpose of consultation and education is to develop further the existing helping systems of lay people in a community. For example, self-help organizations or service programs run by church groups may need consultation from professionals to screen participants with serious psychological problems that require the attention of experts. Bartenders may be trained to provide referrals to problem drinkers, or cab drivers may be taught to refer people in crisis to appropriate programs.
Crisis intervention is usually considered to be a technique of primary prevention when applied to persons in crises caused by such events as a natural disaster or the loss of a spouse. However, it is usually associated with secondary prevention when applied to persons with diagnosable conditions. In these cases the crisis is likely to be the precursor of another acute episode of the condition, for example, schizophrenia.
When no clear point of onset of a mental disorder exists, it is difficult to make a distinction between primary and secondary prevention. For example, when considering services to “troubled youths,” whose problems are invariably diffuse and involve them in several systems of care and control, the distinction between primary and secondary prevention has mostly heuristic value. However they are classed, the activities involved in crisis intervention implement the epidemiological approach through aggressive casework and group work efforts to develop resources, muster social support, and increase the-ego strength of clients to facilitate coping.
As a technique of primary prevention, community organization emphasizes local and democratic control of social institutions as a means of buttressing the individual’s sense of personal control through participation and strengthening social bonds by virtue of reciprocal commitments among participants. Thus, participation is seen to be both health promoting and politically effective, contributing to the well-being of individuals and their communities.
Community mental health centers have sponsored such community-organization activities and have also been the targets of mobilized residents, especially in minority-group communities. Community organization has also been used to foster the development of self-help groups, such as extended “nonfamily” networks capable of lending continuous support to the individual and family in stress.
Secondary Prevention
Secondary prevention activities, such as short-term treatment and crisis intervention, are associated with shortening the duration of a specific problem or treating it before it becomes severe. They are assessed with regard to their effectiveness in decreasing the prevalence of a mental disorder in a community or reducing the total number of cases already suffering from that disorder.
It is in the implementation of secondary prevention activities that the community mental health center has been identified with the less disturbed and more privileged members of a community, and it is in this role that social workers come to be therapists in the narrowest sense of the term. The mandate that community mental health centers serve the total population of a catchment area—and their patent inability to do so—has resulted in the application of resources according to potential demand rather than to severity of need.
Thus, community mental health centers gear their services to middle-class people, whose only previous resource was the mental hospital if they could not afford private psychiatric care. This is an important achievement, but frequently it has come at the expense of the chronically ill, the poor, and ethnic and sexual minorities, who often need different services in alternative settings. This problem is especially important in view of the virtual monopoly that community health centers have on federal mental health funds.
To a great extent, community mental health centers have been the victims of incompatible demands. All the people cannot be pleased all the time—and certainly not under one roof or by one agency. Thus, the last decade has seen the growth of private, usually small, mental health agencies serving groups underserved by community mental health centers. Social workers have been important participants in these alternative efforts as administrators, caseworkers, therapists, and advocates. They have also emerged as the professional links between these agencies and established centers. Thus if a rapprochement is forthcoming, it is likely that social workers will negotiate its terms.
Tertiary Prevention
Tertiary prevention activities are concerned with the reduction of disorder-related problems in a population. They have been largely associated with the care and rehabilitation of the chronically mentally ill and with the deinstitutionalization movement. It appears that shorter hospital stays have reduced the occurrence of the iatrogenic effects of institutional care. However, assumptions that community mental health centers would provide the care necessary to prevent the postinstitutional deterioration of ex-patients have not proved true. Community mental health centers and the social workers practicing in them have been severely criticized for their inattention to the chronically disordered, and statistics have supported these criticisms. 15
Following these criticisms, and in response to the mandates of the 1975 amendments to the Community Mental Health Centers Act, community mental health centers have begun to provide more appropriate services to the chronically mentally ill. Social workers have been outposted or detached to work with ex-patients in single-room occupancy hotels, sheltered-care homes, and private residences. 16 They have also become advocates of patients’ rights. Still, these efforts are far short of what is necessary to prevent the grave consequences of chronic disorders.
SOCIAL WORK OBJECTIVES
The role of social workers in community mental health is embedded in the broader relationship of people to social institutions. Social work’s concern with the quality of life is sanctioned by the social system and involves, of necessity, some commitment to the institutions that organize and govern secular life. This responsibility does not preclude activities directed toward social change. Indeed, to be fully responsible in any society requires a commitment to social change.
However, social workers are creatures of society’s mandate and must keep in mind that the needs of the individual arise in a given social context and must be weighed against the claims of the social group. Social work educators, in particular, must confront the last decade’s fashionable narcissism. Social work’s commitment to equity, social responsibility, relatedness, and sacrifice should be a source of pride for practitioners and should not be dismissed on the road to the practice of psychotherapy.
Social work’s efforts to define and develop its practice in community mental health must address specific and difficult problems currently facing the field, such as violence in families. The profession must also respond to the needs of underserved population groups. In considering the individual’s relationship to the social group, social work must balance primary prevention efforts against services to the chronically ill. The former is an efficient approach to the social group, the latter is a commitment to serving the individual. One should keep in mind these issues and the practice frameworks described in this article in reading the following summary of their relationships to the basic objectives of social work.
Help people enlarge their competence and increase their problem-solving and coping abilities.
The legal/administrative model of community care stresses the first objective of social work practice: to help people enlarge their competence and increase their problem-solving and coping abilities. Emphasis in community care is placed on intervention that provides necessary support without discouraging self-sufficiency. Error in treatment is calculated to occur on the side of the individual’s right to risk failure. Thus the individual is to be served in the least restrictive environment possible and always encouraged to do for himself or herself.
The epidemiological model of community mental health places an emphasis on the host, beginning where he or she is and encouraging the use and development of problem-solving and coping abilities necessary to affect environmental contingencies, contributors to the problem, and the problem itself.
Facilitate interaction between individuals and others in their environment.
The community approach in community care and in community mental health emphasizes the individual’s formal and informal association with groups. It is the “functional community” that most directly affects the individual’s ability to live as an integrated member of society and to achieve a satisfactory state of mental well-being. In describing the individual’s functional community, Caplan referred to the social support system. 17 This system consists of others in the environment who provide help in three ways: (1) They help the individual mobilize psychological resources and master emotional burdens. (2) They share tasks. (3) They provide extra supplies of money, material, tools and cognitive guidance to improve the individual’s situation.
Help people obtain resources.
Segal, Baumohl, and Johnson, drawing on Wiseman, view the function of social support as providing the individual with “social margin”—that leeway for error or disreputability which facilitates survival even in the meanest circumstances. 18 Social margin consists of the relationships, possessions, skills, and personal attributes that can be mortgaged, used, sold, or bartered in return for necessary assistance in prospering or surviving in society. It derives from the interaction among individuals and between individuals and institutions. When the social work profession seeks to improve such interactions, it is trying to increase the social margin of its clients.
Clearly, this improvement may be brought about in numerous ways, including those related to the three remaining objectives of social work: make organizations responsive to people, influence interaction between organizations and institutions, and influence social and environmental policy . In the community mental health field, virtually every activity, from individual casework to community organization, is an attempt to develop the relatedness required to prevent the stresses that seem to forecast the occurrence of a mental disorder or to relieve those which prolong its duration or make its chronic presence more agonizing.
The evaluative component of the epidemiological model emphasizes benefits to the social group, defined in practice as the residents of a particular catchment area. The policies, formal and informal, that govern the organization of care in any area have a substantial impact on the lives of individuals and consequently on the rates of incidence and prevalence of a mental disorder. Criteria for eligibility and barriers to comprehensive or continuous care are, among others, elements of policy and organizational behavior that should be of great concern to social workers in community mental health. These are not simply problems for mental health administrators or for politicians concerned with the formulation of social welfare policy and program. They are issues that affect almost every case.
Aside from organized political activity, which the authors recommend, and in addition to the promotion of more social workers to administrative and policy making positions, the responsiveness of institutions is most affected by the profession through case management, especially through the activities of brokerage and advocacy. As was observed previously in the article, the mental health field is not always or even usually organized in a manner that permits a comprehensive response to those in need. Short of the creation of a mammoth mental health empire, this will always be true. From case management specifically and from good casework generally comes the simultaneous concern for mental and social well-being that forms disparate helping activities into a coherent whole in the service of each client. To see the person in environment obliges social workers to see the person in relation to the organization of care.
The mental health field has moved increasingly into the realm of social welfare, focusing its interventions on the relationship between individuals and institutions. As a result, social work has become the mainstay of mental health’s community-based efforts.
In the future, mental health social workers must develop additional skills to cope with the compound human problems they face daily. They must become adept intervenors in crises, develop a greater awareness of the impact of drugs on social functioning, better define and implement methods of social support and case management, and better describe and evaluate the discrete methods of their profession.
What is most important, though, is that social workers in the mental health field must maintain their commitment to social well-being, even when called on to attend narrowly to the improvement of mental status. In this commitment to the quality of social life—to equity, social responsibility, and relatedness—lies the unique and noble purpose of the profession.
“To the consternation of many traditional mental health professionals, the field of community mental health has become so elastic that it now includes almost all kinds of ameliorative activity.”
Notes and References
- Find a Social Worker
About social work
Where social workers work
What social workers do
How social workers work
How to Find a Social Worker
Seeing a social worker
- Constitution & bylaws
Board of directors
AASW elections
Annual general meetings
Annual Reports
AASW structure
Strategic plan 22-23
Reconciliation action plan
Our history
- Practice & networking groups
Opportunities with AASW
Work with us
Volunteer with us
Employment partnerships
Sponsorships
Advertising
- Awards & grants
- Life Member
- AASW Fellow
Social Policy & Advocacy
Policy positions
Advocacy for the Profession
Registration of social work in Australia
Ethics and Standards
Code of ethics
Practice standards
Ethics consultation service
Making a complaint
Constitution & bylaws
Practice & networking groups
Awards & grants
Life member
AASW fellow
Become a member
- Membership FAQs
Credential Program
Renewal FAQs
Continuing professional development (CPD)
CPD overview
- Specialist learning programs & workshops
On Demand Learning
Live-online Webinars and Workshops
- Branch CPD & events
CPD Newsletter Subscription
Employer partnership program
Become an employer partner
Benefits to employers
Benefits to employees
Practice and careers
- Support & resources
Social work community
Mentoring program
AASW community hub
Credentials Program
- AASW credentials
Find CPD & Events
Specialist learning programs & workshops
Branch CPD & events
Support & resources
AASW Credentials
Higher education providers
Accredited Programs
Accreditation Process
Accreditation Roles
Additional Information
Migration & eligibility assessment (MEA)
Working Overseas
- Migration & eligibility assessment
International qualification recognition
New Zealand Mutual Recognition
International students studying an AASW accredited social work course in Australia
Temporary Graduate Visa Subclass 485
Renewals and reissue of Assessments
Optional migration assessments
Reassessment, internal review and external appeal
Horizon Career Centre
Mea online applications.
Migration & eligibility assessment
News and Media Releases
- News & media releases
- Information for the media
AASW in the media
Newsletters
Publications
Social Work Focus
Australian Social Work
News & media releases
Information for the Media
- Find a social worker
- AASW Accredited Mental Health Social Worker Application Criteria
- Credentials
- Mental Health
- Family Violence
- Child Protection
- Older Persons
In 2004, the Australian Government implemented the Enhanced Primary Care Program under which General Practitioners were able to refer patients with complex care requirements to a range of allied health services. Under this initiative social workers were recognised as one of the group of eligible mental health providers. In 2006, the Government introduced the ‘Better Access to Mental Health Care’ initiative, under which General Practitioners, Paediatricians and Private Psychiatrists could refer to suitably qualified and experienced allied health professionals namely: social workers; psychologists and occupational therapists for the provision of ‘Focussed Psychological Strategies’. This document explains the process which a social worker must undergo, should they wish to be considered by Medicare Australia as ‘suitably qualified and experienced allied health professional’.
Please refer to information below as to the 6 AMHSW criteria that must ALL be met to gain a successful outcome:
- Hold current eligible AASW membership
- Have at least 2 years’ full-time equivalent (FTE) post-qualifying social work experience* in a mental health setting within the last 5 years , totalling a minimum of 3,360 hours. The AASW recognises that full-time employment equates to 35 hours per week, for 48 weeks per year.
- Must be able to articulate your understanding and provide a case example on how your experience meets the AASW Practice Standards for Mental Health Social Workers 2014 . Where applicable, you must demonstrate the use of Focused Psychological Strategies (FPS), within your case example from your mental health practice position/s.
- Demonstrate at least 2 years’ full-time equivalent (FTE) post-qualifying supervision in a mental health setting/field within the last 5 years. You should be able to show that they have been formally supervised, in line with the AASW Supervision Standards . Generally, supervisors should have a higher level of practice experience than their supervisees and should have some training in supervision. For the purposes of this assessment, the supervisor does not necessarily need to have a social work background but should have provided the applicant/supervisee with appraisal and assessment in relation to practice in a mental health field (e.g. psychologist, medical practitioner or a mental health nurse).
- Have met the Continuing Professional Development requirements
- Demonstrate ability and knowledge of clinical Mental Health social work practice through Case study activities. Further information on the case study activity can be found on Case Study Activity
- Curriculum vitae: the CV or resume allows our assessor to get an overall picture of your social work experience. Please ensure the dates align with all the evidence you provide.
- Referee statement: You must provide the official AASW referee statement form completed, signed and dated by an employer or supervisor that validates your work and performance in a mental health setting/field using FPS. For the purposes of this credential, the referee must have appropriate qualifications and experience in mental health in order to provide appropriate assessment and appraisal of an applicants mental health practice and particularly your use of and competence in FPS. The form must also confirm the exact dates and hours per week of employment.
- Position description: an official agency position description on organisation letter head to confirm the key duties and responsibilities of the role.
Note for applicants who are self-employed in private practice
In addition to submitting a referee statement, you will need to provide a signed and declared statutory declaration outlining details of your roles and responsibilities in lieu of a position description. You will need to include the dates and approximate hours per week that you have worked in your private practice role, in particular, your clinical work with mental health clients, utilising FPS, and the percentage of time which is spent in this clinical mental health work.
Why be a member?
When you join the AASW you’ll become part of an active and vibrant community of more than 17,000 social work professionals. As the profession’s peak body, the AASW is committed to maintaining high standards, ethical practice and ongoing professional development.
Access on-demand content, live workshops and events at up to 50% discount as a member
National office
Level 7, 14-20 Blackwood St NORTH MELBOURNE 3051
PO Box 2008 Royal Melbourne Hospital VIC 3050
P: 03 9320 1000
Quick Links
Site information, get the latest cpd news & events, connect with us.
The AASW respectfully acknowledges Aboriginal and/or Torres Strait Islander peoples as the First Australians, and pay our respects to Elders past and present.
© 2023 - AASW Copyright
- Sign up and Get Listed
Be found at the exact moment they are searching. Sign up and Get Listed
- For Professionals
- Worksheets/Resources
Find a Therapist
- Find a Treatment Center
- Find a Marriage Counselor
- Find a Child Counselor
- Find a Support Group
- Find a Psychologist
- If You Are in Crisis
- Self-Esteem
- Sex Addiction
- Relationships
- Child and Adolescent Issues
- Eating Disorders
- How to Find the Right Therapist
- Explore Therapy
- Issues Treated
- Modes of Therapy
- Types of Therapy
- Famous Psychologists
- Psychotropic Medication
- What Is Therapy?
- How to Help a Loved One
- How Much Does Therapy Cost?
- How to Become a Therapist
- Signs of Healthy Therapy
- Warning Signs in Therapy
- The GoodTherapy Blog
- PsychPedia A-Z
- Dear GoodTherapy
- Share Your Story
- Therapy News
- Marketing Your Therapy Website
- Private Practice Checklist
- Private Practice Business Plan
- Practice Management Software for Therapists
- Rules and Ethics of Online Therapy for Therapists
- CE Courses for Therapists
- HIPAA Basics for Therapists
- How to Send Appointment Reminders that Work
- More Professional Resources
- List Your Practice
- List a Treatment Center
- Earn CE Credit Hours
- Student Membership
- Online Continuing Education
- Marketing Webinars
- GoodTherapy’s Vision
- Partner or Advertise
- GoodTherapy Blog >
The Important Role Social Workers Play in Mental Health

Who Are Social Workers?
Social workers are highly trained professionals working to improve the quality of life and well-being of others through direct practice, crisis intervention, research, community organizing, policy change, advocacy, and educational programs. Social workers are dedicated to the pursuit of social justice and strive to help those affected by poverty, disabilities, illnesses , divorce , unemployment, and other personal problems and social disadvantages.
Being a social worker requires extensive knowledge of human behavior and development, as well as social, cultural, and economic institutions and the ways in which they interact. Most social workers will hold at least a bachelor’s degree in social work or related field, though many (especially clinicians) will hold a master’s degree and valid license to practice.
A good social worker will often possess a high degree of compassion and empathy , a passion for helping others, strong interpersonal and problem-solving skills, and good listening and organizational skills.
What Do Social Workers Do?
Social workers fight for social justice, equality , and the overall well-being of people in need. Social workers are responsible for many of the liberties we have today. These include:
- Civil rights for all citizens regardless of race, sexual orientation , gender , faith, etc.
- Medicaid and Medicare programs that provide disadvantaged groups access to health care
- Child abuse and neglect prevention programs
- Unemployment insurance, disability pay, worker’s compensation, and social security
- Humane treatment for those with mental health conditions and developmental issues
Clinical social workers diagnose and treat mental health conditions as well. They provide individual, family, and couples therapy, and they assist with depression , anxiety , family problems , and other mental health or behavioral issues. They may work in private practice or at a mental health or therapeutic facility. Social workers host support groups, create treatment plans, and facilitate interventions when necessary.
Some common duties of a social worker include:
- Identifying and reaching out to those in need.
- Assessing people’s needs and implementing a plan of action.
- Helping people adjust to major life changes .
- Responding to crisis situations.
- Connecting people with important resources and support.
- Evaluating social services and support programs.
- Providing advocacy for people when needed.
- Following up with people to ensure circumstances are improving.
Where Do Social Workers Work?
There are several common areas of focus in the social work industry:
- Administration/supervision
- Alcohol, tobacco, and other drugs
- Children, adolescents , and young adults
- Child welfare
- Physical health
- Mental health
- Private practice
- School social work
- Social and economic justice and peace
- Social work and the courts
A good social worker will often possess a high degree of compassion and empathy, a passion for helping others, strong interpersonal and problem-solving skills, as well as good listening and organizational skills. Social work is unique in the way it can be found in most aspects of community life. Social workers are employed in schools, hospitals, rehabilitation facilities, hospices and nursing homes, private practices , government institutions, correctional facilities, law offices, military organizations, public welfare agencies, nonprofit organizations, and some private businesses and corporations.
Even when social workers are employed in office, they may spend time traveling to visit with people in need. School social workers may also travel from school to school or hospital social workers from hospital to hospital.
Why Social Work Is in Demand
According to the United States Bureau of Labor and Statistics, overall employment of social workers is expected to grow at a rate of 19% between 2012 and 2022. The demand for health care social workers is expected to grow by as much as 27% during this same time period—a rate much higher than the average growth rate for all occupations. One reason for the increase in demand is due to the aging of the baby boomers, who will soon need long-term care and assistance.
Social workers in the mental health and substance abuse fields will also be in high demand, with a 23% increase in employment expected by 2022. More people are expected to seek mental health treatment, and people who have a substance addiction are increasingly sent to treatment programs rather than jails or prisons.
How to Become a Social Worker
Those interested in entering the social work profession should first prepare for admission to the program of their choice by gaining valuable volunteer experience and obtaining professional references in the field.
A bachelor’s degree is the minimum requirement for an entry-level social work position, but most employers prefer a graduate degree. A master’s level education in social work is a requirement for clinical licensure in most states.
An undergraduate degree in social work is not necessary to gain admittance to a master’s program; virtually any bachelor’s degrees will suffice. Upon graduation, a few years of supervised work is necessary to gain licensure.
When to Reach Out to a Social Worker
- You’re seeking therapy or treatment for depression, anxiety, or another mental health condition.
- You’ve recently undergone a major life change (divorce, death of a loved one , etc.) and need support.
- You have witnessed child abuse or neglect.
- You need geriatric assistance for an elderly family member.
- You are coping with a drug or alcohol addiction .
- You are finding it difficult to cover the costs of basic needs (food, shelter, water, or others).
- You or a loved one is battling a major illness.
- You have recently become unemployed or disabled.
- Your child is experiencing behavior problems at school.
References:
- Bureau of Labor Statistics, U.S. Department of Labor, Occupational Outlook Handbook, 2014-15 Edition , Social Workers. Retrieved from http://www.bls.gov/ooh/community-and-social-service/social-workers.htm
- National Association of Social Workers. (NASW). Social Work Profession. Retrieved from https://www.socialworkers.org/pressroom/features/general/profession.asp
- National Association of Social Workers (NASW). Social Work History. Retrieved from http://socialworkers.org/pressroom/features/general/history.asp
- National Association of Social Workers (NASW). Who are Social Workers? We Help. Retrieved from http://www.naswdc.org/pressroom/2011/HSH-FactSheet2011.pdf

© Copyright 2015 GoodTherapy.org. All rights reserved.
The preceding article was solely written by the author named above. Any views and opinions expressed are not necessarily shared by GoodTherapy.org. Questions or concerns about the preceding article can be directed to the author or posted as a comment below.

Please fill out all required fields to submit your message.
Invalid Email Address.
Please confirm that you are human.
- 13 comments
Leave a Comment
These are the people who would be the most responsible with getting people with the resources that they need at any given point in time. They are literally a lifeline for a whole lot of people and yet they get very little praise and recognition overall.
They sure do have a lot of job responsibility without nearly enough in compensation
We do have a lot on our plate. Thanks for posting.
These are the people who advocate for those who tend to not have a voice of their own. I don’t think that we give enough credit to this group of professionals who typically go above and beyond the call of duty if they know that what they are doing is helping and serving another individual.
thanks for your recognition… It means a lot. I’ve been practicing social worker for over 30 years and were recently become an RM.
Think about all of the agencies and resources that they have to keep up with. They have to know where to refer which clients and who could benefit from what service but maybe not that one. I mean, that is a lot!
I do wish that there was a little more understanding about the work that most social workers find themselves engaged in. This is more than just about being a case manager. In many cases you are their link to normalcy, a counselor, and a friend. I think that in many instances families just need someone to talk to who really hears and understands their concerns and they do not get a lot of that. Social workers do a huge amount of work in filling that void for many families.
Good article but you need to be aware that licensure requirements vary from state to state. Some of what you describe here is very specific to “clinical licensure.” But there are other levels of licensure in most states, and those requirements are different from what you describe.
Most of the mass shootings have involved youth or adults with a history of mental illness. Too often families and individuals have fallen between the cracks because of the lack of services available or because there was no one to help them navigate the systems for help. In my former profession I often came in contact with numerous individuals and families who needed help accessing mental services. It was the mental health social workers who I contacted or referred them to. Because of the immense size of our state geographically, the weather barriers in many areas of the state, and number of very rural (Alaskan Bush) communities, it is often impossible for help to be available without a plane or boat ride to a larger community. We have to rely on the social workers in our schools or the village clinics to provide help 24/7. They have a tough job to do but they do it well.
It wasn’t until I looked over this list that I fully realized what kind of role social workers play in the lives of numerous amounts of people. There are those who rely on them for practically every service that they receive, there are those who receive a little help, and then pretty much anything in between. The spectrum that it appears that they deal with is massive and they should be commended much more often for the varying and taxing jobs that they must do.
Social workers are very essential to the growth of a Nation but most leaders fail to recognise that. They are are like a bedrock that should not be under-emphasized especially in Developing countries that’s always faced with series of social problems like poverty,juvenile delinquencydomestic violence to mention but a few. I look uptown that generation when Social work would be accorded the necessary recognition but I pray It comes early. I’m proud to be a social work student.
Hi, Thanks for the article and trying to contribute to the discourse. However, please clarify how could a Clinical/Psychiatric Social Worker diagnose and prescribe treatment? They can support with therapeutic and counselling interventions, yes, but how can they diagnose/treat? Social Worker are para-Health professionals working alongwith other professionals like Psychiatrist, Occupational Therapist, Therapist and so on. Yes, there could be some role overlaps, but certainly not when it comes to diagnosing/prescribing treatment. Social Workers can support the process. I work as a Psychiatric/Mental Health Social Worker in Mumbai, India. Please let me know if you beg to differ or if I have missed out something. Would be glad to recieve and listen:)
Stay safe and take care.
Clinical Social Workers are professionals that can diagnose and treat any mental illnesses. They do have a Master’s Degree in Clinical Social Work Practice and some of them are specialized in Mental Health and Addictions.
By commenting you acknowledge acceptance of GoodTherapy.org's Terms and Conditions of Use .
* Indicates required field.

Search Our Blog
Browse by category.
- Uncategorized
- GoodTherapy.org Announcements
- For Therapists by Therapist
- FAQ/What to Expect in Therapy
- Self-Concept
- Myths in Therapy
- Topic Expert Roundup
- Women's Issues
- Sex/Sexual Concerns
- Grief and Loss
- Separation and Divorce
- social media
Notice to users


|
She has been treated for years with various antidepressants and mood stabilizers but has had only two short inpatient admissions. She has seen numerous therapists since childhood and, for the past five years, has been treated by a respected psychiatrist with a specialty in serious mental illness and psychopharmacology. Symptoms are similar to most major depressions: hopelessness, helplessness, self-directed angry outbursts, worthlessness, poor self-esteem, feelings of guilt, lack of motivation, excessive sleeping, poor hygiene, and tearfulness. She describes herself as a “terrible housekeeper.” She says she never cleans, never opens mail, and rarely eats at home. She once reported with sadness and disdain, “Sometimes, I make a bowl of cold cereal and milk, and I stand in the middle of the dining room and eat it. That’s so pitiful!” Because she is an exceptionally intelligent and articulate person, these negative characterizations are painful to hear—for her therapist, her doctor, and for Taylor.
Taylor’s descriptions of her father have always been more detailed and scathing. She describes her father as harsh and hypercritical with a history of severe teasing. “He never had to raise a hand against me. He is an expert at punishing with words,” Taylor explains. She has reported being called derogatory names critical of her mental health problems and physical appearance. Taylor does understand the connection between these experiences and her problems with depression, self-image, and self-esteem, but this insight does not seem to produce improvement. Unfortunately, due to the repeated episodes of depression, Taylor has had to depend on her father in the past eight years for financial assistance, which she bitterly resents. Periodically, Taylor had problems in school, especially high school. Eventually, her parents enrolled her in a private school that she loved and where she excelled. She was accepted into an Ivy League university but had difficulties due to a combination of social issues, an inability to organize her work, and a serious medical illness that led to a two-month hospitalization. Although she did not finish college, she transferred to a university in France where she stayed for several years, happily studying and traveling to many different countries. One of her major pastimes was mountain climbing, and she has climbed mountains all over Europe, Africa, and the United States. She sometimes talks about living in Europe permanently but has not pursued this beyond the most preliminary steps. Beginning in her mid-40s, Taylor began to suffer multiple health problems, some of which continue but are not life threatening. She has become more hopeless over her impending 50th birthday. The life review that this often engenders in people has become a major crisis for her as she reviews a life she believes to be worthless.
She had an unexpected monetary windfall and decided to reward herself with a three-week trip to Europe. She felt exceptionally energetic and returned to an old love of mountain climbing. On her return to the United States, she resumed treatment. She was full of stories about her trip, quickly found a new job, and felt reasonably content even though she had taken a pay cut. She resumed seeing her friends and talked about returning abroad to live permanently. This improvement was short lived. Over the next year and a half, the depression and its familiar distressing symptoms returned with increasing intensity. Taylor’s doctor actively managed her medications, but she continued to decline. During a session in my office one evening, she was so depressed that she sat practically mute with tears running down her face. She was still able to work but reported that her job was in jeopardy. After much consideration, she decided to try ECT again. However, this trial was unsuccessful, and Taylor had an unfortunate reaction and needed to be hospitalized for a few days. Since her discharge, sessions are dominated by Taylor’s depressive symptoms, self-hatred, and anger. She is frustrated with her inability to manage her home and is increasingly gloomy about her future. During our most recent session, she reported that she had lost her job. Taylor initially presented with a strong desire to get her life together, and she had two specific goals: to feel better about herself and to organize her home. “My doctor recommended you because he said you are a no-nonsense kind of person,” she told me. Taylor comes to therapy regularly, and she has been able to successfully discuss sensitive issues in her past such as a date rape in her late teens. Although she does not have an intimate relationship now and is not dating, she has several close friends with whom she sometimes goes out to dinner or to a movie when she agrees to call them. She often assumes it is their responsibility to call her. She has developed a trusting relationship with me as her therapist and is able to follow some basic cognitive therapy techniques to examine her thinking and structure her day. However, all attempts at permanent change have been met with only temporary success. Homework assignments are done only for a few days, and physical activity has the same duration. Suggestions such as focusing on her beloved Siamese cats, connecting with friends, revisiting former interests, and learning to manage anger and the relationship with her father have all worked for a while but are never entirely successful. There are times when she is able to draw on past accomplishments and see that she has some strengths and has done some positive things. Her life has been adventuresome and somewhat eccentric, but she resists seeing this as a genuine way to live and believes that she is a flawed person without a husband, children, a fine home, and living what she perceives to be a “normal” life. Despite her severe bouts of depression, she does not want to die and firmly states that she would never harm herself. Taylor is wedded to the idea that psychopharmacology or some other yet undiscovered miracle medical procedure will be the answer to her difficulties. She reports that she is more willing to try any medication or procedure (after careful assessment) rather than having to go through the harder, slower process of therapy. Her mantra about any new therapeutic process is “What good will this do?”
Taylor seems to be a study in contradictions. She wants a quick fix for her problems but has stayed in this therapy for at least a year and a half. She shifts from positive to negative feelings about her intelligence, and she sees herself as flawed for not having a “normal” life, though she is quite disparaging of her normal parents. One explanation for these contradictions could be her attachment to her negative feelings about herself, which seem quite profound. Her ability to tolerate positive feelings appears limited, perhaps because it could endanger her negative, but reliable, identity. Despite Taylor’s attachment to her negative persona, she has pursued this therapy, which suggests that there is a role for a therapist to play in helping her find a more self-accepting, positive identity. The key to working with Taylor could be helping her realize that someone understands how much she has suffered but is not empathically overwhelmed and/or emotionally harmed by the suffering she demonstrates in her sessions (i.e., mute despair with weeping and self-punitive comments). Taylor seems to be unaware that the way she treats herself is similar to the way she describes her father treating her, but in an internalized, self-imposed manner. The therapist’s role at this point in the treatment seems to be witnessing Taylor’s intense suffering. The description Taylor was given of her current therapist as “no-nonsense” could be a clue to what she thinks she needs (i.e., a therapist who doesn’t get lost in Taylor’s misery). This could also mean a therapist who sees that the suffering is a crucial part of Taylor’s identity and acknowledges the importance it has to her without seeing it as the only identity she could have. The therapist says, “Something very strong keeps her [Taylor] going in this world, helps her to survive.” I see this comment as encouraging Taylor to see herself as emotionally stronger than she feels, which could be overlooking how psychologically destroyed Taylor can feel at times during what sound like psychotic episodes. The desire to avoid these extremely painful episodes could be what leads Taylor to cling to her very difficult but reliable, negative self-images and to be financially dependent on her demeaning but reliable father. Over time, the therapeutic process could offer Taylor a different experience and new ways to avoid the experience of losing her identity in overwhelming depression. Taylor seems to be nonverbally asking the therapist to take responsibility for her awful feelings, just as she wants her friends to be the ones to reach out to her. Seeing the therapeutic process as a way to begin to own and contain her painful feelings would be a necessary precursor to helping Taylor look at the identity she has constructed and maintains. It would be a good idea for the therapist to explore Taylor’s question, “What good will this do?” and be clear that any change that comes from therapy will likely be a long process, as Taylor and the therapist build new ways for Taylor to own and contain her feelings. Empathizing with the frustration this is likely to cause Taylor would be an important part of building a therapeutic alliance. But simply tolerating the pain Taylor experiences and encouraging her to put it in words when she can, as the therapist seems to be doing, is also a crucial part of helping Taylor. Taylor appears to have built her identity on primarily negative images of herself, her mother, and her father, with little capacity to question the way she now projects these images onto herself and others. Despite her conscious wish to be different from her parents, who she felt were cruel and/or neglectful, Taylor nonetheless continues to expect to be treated in these hurtful ways. In the absence of others doing so, she treats herself cruelly. Her ability to form a connection to the therapist is a good sign, but the miserable internal world she has lived in needs to be identified and discussed, particularly the way it is expressed in the therapy. Managing the feelings Taylor stirs up in the therapist would be a major part of the therapist’s work. My primary goals for working with a patient like Taylor would be to look at her self-punitive comments as a way of avoiding critical comments about the therapist, helping her put her nonverbal anguish into words, and letting her know that this is a difficult process for both Taylor and the therapist but one that can be successful if Taylor is willing to work toward changing her self-punitive identity with the therapist’s help.
I utilize a biopsychosocial/spiritual perspective with most clients. As I explore developmental history, I focus on temperament and particularly on early personality development. Personality begins to show itself around the age of 3 and is thought to be malleable until somewhere in the third decade of life. I am most interested in attachment and bonding dynamics. From my vantage point, Taylor has introjected a “sterile” mother and a “dysfunctional” father in response to the early psychosocial climate and environment during her youth. So her “self” and “other” split object relations are negatively distorted. Through the lens of Erik Erikson, I look at the stages of psychosocial development: trust/mistrust, autonomy/shame or doubt, initiative/guilt, industry/inferiority, and identity and role integration/confusion or what I refer to as diffusion. Taylor has not mastered these opportunities. Drawing from John Bowlby, I look at the common reactions to as serious disruptions or fractures of significant relationships: shock, protest, despair, reattachment, or detachment. I see plenty of evidence of these dynamics, which Taylor projects onto current and future relationships. Taylor shows an insecure attachment with both aggressive/ambivalent and avoidant features. Globally, I consider her to show an “asocial” personality orientation. She likely feels vulnerable and fragile in close, intimate relationships. In my clinical experience, an early childhood onset of depression has been rare. We know that in adolescence and adulthood, women are at great risk of major depression. I am struck by Taylor’s suicide attempt during the latency period. I wonder if the presentation of puberty was a potential trigger. In terms of suicide, women are more likely the attempters and men the completers. What method did she use? I always explore the meaning of these incidents, questioning the client’s reaction to them then and now. I find it remarkable, considering her overall suffering, that she has not attempted again. I am very concerned about her degree of hopelessness. Aaron T. Beck and Judith S. Beck indicate this to be a high risk factor for suicide. I would also examine the degree of helplessness and worthlessness, as I have found this “suicidal triad” to be more predictive of risk. Taylor displays what the Becks refer to as the cognitive triad: negative view of past, self, and future. In addition, she clearly displays an external locus of control that leaves her vulnerable in facing psychosocial stressors. I would like to know more about her sibling position and her current and former connections to her sisters. I am curious about any dynamics related to having a father with no sons. I suspect that her siblings also feel vulnerable about intimacy. With all clients, I conduct a protection/risk inventory. Here is my assessment of Taylor’s: Her intellect and articulate qualities are assets. She has some friends. She used to really enjoy mountain climbing. Her therapy attendance is consistent. She showed a very positive response to her first series of ECT. Her risk factors include the degree of hopelessness she feels, her detachment from others, her persistent dysthymia, her marginal or poor response to appropriate psychotropic medication, and her long-standing negatively distorted self-concept. I am curious about her experiences with previous therapists, and I am especially interested in her transference to her present one. I would like to know more about the clinician’s countertransference to this client. My diagnosis is recurrent major depression with persisting dysthymia. When they occur together, some refer to this as double depression. In fact, some evidence shows that nine of 10 persons with dysthymia experience a major depressive episode. I also see Taylor as evidencing a mixed personality disorder in the “wary cluster (Cluster C), with avoidant and dependent features.” In my experience, persons with disordered personality respond marginally to the use of psychotropics. A course of cognitive behavioral therapy is appropriate for her. I also would consider a course of interpersonal therapy. Both approaches are known to be effective in treating major depression. More importantly for Taylor, I recommend a movement away from individual to group psychotherapy. In group therapy, clinicians have access to various therapeutic factors unique to group, which give them additional leverage to be useful to our clients. I think that it will be important to see her through menopause and beyond. Finally, I inquire about each person’s spiritual beliefs in terms of the meaning it gives to their life in times of suffering and in times of relative well-being. In summary, I see Taylor’s prognosis as guarded with continuing treatment and poor without it.
|
Social Work Today magazine

- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
It’s a New Era for Mental Health at Work
- Kelly Greenwood

Research on how the past 18 months have affected U.S. employees — and how companies should respond.
In 2019, employers were just starting to grasp the prevalence of mental health challenges at work, the need to address stigma, and the emerging link to diversity, equity, and inclusion (DEI). One silver lining amid all the disruption and trauma over the last two years is the normalization of these challenges. In a follow-up study of their 2019 Mental Health at Work Report, Mind Share Partners’ 2021 Mental Health at Work Report, the authors offer a rare comparison of the state of mental health, stigma, and work culture in U.S. workplaces before and during the pandemic. They also present a summary of what they learned and their recommendations for what employers need to do to support their employees’ mental health.
When we published our research on workplace mental health in October 2019, we never could have predicted how much our lives would soon be upended by the Covid-19 pandemic. Then the murders of George Floyd and other Black Americans by the police; the rise in violence against Asian Americans and Pacific Islanders (AAPIs); wildfires; political unrest; and other major stressors unfolded in quick succession, compounding the damage to our collective mental health.
- Kelly Greenwood is the Founder and CEO of Mind Share Partners , a national nonprofit changing the culture of workplace mental health so both employees and organizations can thrive. Through movement building , custom training, and strategic advising, it normalizes mental health challenges and promotes sustainable ways of working to create a mentally healthy workforce. Follow her on LinkedIn and subscribe to her monthly newsletter.
- Julia Anas is the chief people officer at Qualtrics, the world’s #1 Experience Management (XM) provider and creator of the XM category. At Qualtrics, she is responsible for building a talented and diverse organization and driving employee development as well as organizational design, talent, and succession planning.
Partner Center
A sample case study: Mrs Brown
On this page, social work report, social work report: background, social work report: social history, social work report: current function, social work report: the current risks, social work report: attempts to trial least restrictive options, social work report: recommendation, medical report, medical report: background information, medical report: financial and legal affairs, medical report: general living circumstances.
This is a fictitious case that has been designed for educative purposes.
Mrs Beryl Brown URN102030 20 Hume Road, Melbourne, 3000 DOB: 01/11/33
Date of application: 20 August 2019
Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke, which has left her with moderate weakness in her left arm and leg. A diagnosis of vascular dementia was also made, which is overlaid on a pre-existing diagnosis of Alzheimer’s disease (2016). Please refer to the attached medical report for further details.
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job. The eldest daughter Catherine lives on the Gold Coast with her family. Mrs Brown is a retired school teacher and she and both daughters describe her as a very private woman who has never enjoyed having visitors in her home. Mrs Brown took much encouragement to accept cleaning and shopping assistance once a week after her most recent admission; however, she does not agree to increase service provision. Jean has Enduring Power of Attorney (EPOA) paperwork that indicates that Mrs Brown appointed her under an EPOA two years ago. She does not appear to have appointed a medical treatment decision maker or any other decision-supporter.
I also understand from conversations with her daughters that Jean and Mrs Brown have always been very close and that there is a history of long-standing conflict between Catherine and Jean. This was exacerbated by the death of their father. Both daughters state they understand the impact of the stroke on their mother’s physical and cognitive functioning, but they do not agree on a discharge destination. Mrs Brown lacks insight into her care needs and says she will be fine once she gets back into her own home. Repeated attempts to discuss options with all parties in the same room have not resulted in a decision that is agreeable to all parties.
Mrs Brown has a history of Alzheimer’s disease; type II diabetes – insulin dependent; hypertension; high cholesterol and osteoarthritis. She has had two recent admissions to hospital for a urinary tract infection and a fall in the context of low blood sugars. She is currently requiring one to two people to assist her into and out of bed and one person with managing tasks associated with post-toilet hygiene. She can walk slowly for short distances with a four-wheel frame with one person to supervise. She benefits from prompting to use her frame; she needs someone to cut her food and to set her up to eat and drink regularly and to manage her medication routine. She requires one person to assist her to manage her insulin twice daily.
The team believe that Mrs Brown’s capacity for functional improvement has plateaued in the last ten days. They recommend that it is in her best interests to be discharged to a residential care setting due to her need for one to two people to provide assistance with the core tasks associated with daily living. Mrs Brown is adamant that she wants to return home to live with Jean who she states can look after her. Jean, who has a history of chronic back pain, has required several admissions to hospital over the past five years, and states she wants to be able to care for her mother at home. Jean states she is reluctant to agree to extra services as her mother would not want this. Her sister Catherine is concerned that Jean has not been coping and states that given this is the third admission to hospital in a period of few months, believes it is now time for her mother to enter residential care. Catherine states that she is very opposed to her mother being discharged home.
Mrs Brown is at high risk of experiencing falls. She has reduced awareness of the left side of her body and her ability to plan and process information has been affected by her stroke. She is now requiring one to two people to assist with all her tasks of daily living and she lacks insight into these deficits. Mrs Brown is also at risk of further significant functional decline which may exacerbate Jean’s back pain. Jean has stated she is very worried about where she will live if her mother is to enter residential care.
We have convened two family meetings with Mrs Brown, both her daughters and several members of the multi-disciplinary team. The outcome of the first meeting saw all parties agree for the ward to provide personalised carer training to Jean with the aim of trialling a discharge home. During this training Jean reported significant pain when transferring her mother from the bed and stated she would prefer to leave her mother in bed until she was well enough to get out with less support.
The team provided education to both Jean and Catherine about the progressive impact of their mother’s multiple conditions on her functioning. The occupational therapist completed a home visit and recommended that the downstairs shower be modified so that a commode can be placed in it safely and the existing dining room be converted into a bedroom for Mrs Brown. Mrs Brown stated she would not pay for these modifications and Jean stated she did not wish to go against her mother’s wishes. The team encouraged Mrs Brown to consider developing a back-up plan and explore residential care options close to her home so that Jean could visit often if the discharge home failed. Mrs Brown and Jean refused to consent to proceed with an Aged Care Assessment that would enable Catherine to waitlist her mother’s name at suitable aged care facilities. We proceeded with organising a trial overnight visit. Unfortunately, this visit was not successful as Jean and Catherine, who remained in Melbourne to provide assistance, found it very difficult to provide care without the use of an accessible bathroom. Mrs Brown remains adamant that she will remain at home. The team is continuing to work with the family to maximise Mrs Brown’s independence, but they believe that it is unlikely this will improve. I have spent time with Jean to explore her adjustment to the situation, and provided her with information on community support services and residential care services. I have provided her with information on the Transition Care Program which can assist families to work through all the logistics. I have provided her with more information on where she could access further counselling to explore her concerns. I have sought advice on the process and legislative requirements from the Office of the Public Advocate’s Advice Service. I discussed this process with the treating team and we decided that it was time to lodge an application for guardianship to VCAT.
The treating team believe they have exhausted all least restrictive alternatives and that a guardianship order is required to make a decision on Mrs Brown’s discharge destination and access to services. The team recommend that the Public Advocate be appointed as Mrs Brown’s guardian of last resort. We believe that this is the most suitable arrangement as her daughters are not in agreement about what is in their mother’s best interests. We also believe that there is a potential conflict of interest as Jean has expressed significant concern that her mother’s relocation to residential care will have an impact on her own living arrangements.
Mrs Brown’s medical history includes Alzheimer’s disease; type II diabetes; hypertension; high cholesterol and osteoarthritis. She was admitted to Hume Hospital on 3 March 2019 following a stroke that resulted in moderate left arm and leg weakness. This admission was the third hospital admission in the past year. Other admissions have been for a urinary tract infection, and a fall in the context hypoglycaemia (low blood sugars), both of which were complicated by episodes of delirium.
She was transferred to the subacute site under my care, a week post her admission, for slow-stream rehabilitation, cognitive assessment and discharge planning.
Mrs Brown was diagnosed with Alzheimer’s disease by Dr Joanne Winters, Geriatrician, in April 2016. At that time, Mrs Brown scored 21/30 on the Standardised Mini-Mental State Examination (SMMSE). During this admission, Mrs Brown scored 15/30. I have undertaken cognitive assessment and agree with the diagnosis; further cognitive decline has occurred in the context of the recent stroke. There are global cognitive deficits, but primarily affecting memory, attention and executive function (planning, problem solving, mental flexibility and abstract reasoning). The most recent CT-Brain scan shows generalised atrophy along with evidence of the new stroke affecting the right frontal lobe. My assessments suggest moderate to severe mixed Alzheimer’s and vascular dementia.
While able to recall some key aspects of her financial affairs, including the general monetary value of her pension and regular expenses, Mrs Brown was unable to account for recent expenditure (for repairs to her home) or provide an estimate of its value, and had difficulty describing her investments. In addition, I consider that she would be unable to make complex financial decisions due to her level of cognitive impairment. Accordingly, I am of the view that Mrs Brown now lacks capacity to make financial decisions.
Mrs Brown states that she previously made an Enduring Power of Attorney (EPOA) but could no longer recall aspects of the EPOA, such as when it would commence and the nature of the attorney’s powers. Moreover, she confused the EPOA with her will. Her understanding of these matters did not improve with education, and therefore I consider that she no longer has capacity to execute or revoke an EPOA.
Mrs Brown acknowledges that she needs some assistance but lacks insight into the type of assistance that she requires, apart from home help for cleaning and shopping. She does not appreciate her risk of falling. She is unable to get in and out of bed without at least one person assisting her. She frequently forgets to use her gait aid when mobilising and is not able to describe how she would seek help in the event of falling. She is not able to identify or describe how she would manage her blood sugar levels, and this has not improved with education. Accordingly, I consider that she lacks capacity to make decisions about accommodation arrangements and services.
Mrs Brown does not agree with the treating team’s recommendation to move into residential care and maintains her preference to return home. This is in spite of a failed overnight trial at home with both her daughters assisting her. Unfortunately, she was unable to get out of bed to get to the toilet and required two people to assist her to do so in the morning. In light of these matters, and in the context of family disagreement regarding the matter, the team recommends that the Office of the Public Advocate be appointed as a guardian of last resort.
Reviewed 22 July 2022
- Hospitals & health services
- Public hospitals in Victoria
- Patient care
- Ambulance and patient transport
- Non-emergency patient transport
- Non-emergency patient transport review
- NEPT legislation and clinical practice protocols
- Non-emergency patient transport licensing
- NEPT licensing fees
- NEPT services information and guidance
- First Aid Services
- First aid licences
- First aid services information and guidance
- First aid service fees
- Victorian State Trauma System
- Acute medicine
- Emergency care
- Surgical services
- Better at Home
- Critical care
- Hospital in the Home
- Virtual care (Telehealth)
- Perinatal and reproductive services
- Rehabilitation and complex care
- Renal health
- Renal services in Victoria
- Funding for renal services
- Different approaches to haemodialysis
- Specialist clinics
- Access to non-admitted services
- Minimum referral information
- Communication toolkit
- Integrated care
- HealthLinks: Chronic Care
- Community Health Integrated Program (CHIP) guidelines
- Service coordination in Victoria
- Victorian integrated care online resources
- Specialist clinics programs
- Specialist clinics reform
- Specialty diagnostics, therapeutics and programs
- Older people in hospital
- End of life and palliative care in Victoria
- Voluntary assisted dying
- Quality, safety and service improvement
- Planned surgery recovery and reform program
- Digital Health
- Roadmap and Maturity Model
- Standards and guidelines
- Policies and frameworks
- Health Information Sharing Legislation Reform
- My Health Record
- Public hospital accreditation in Victoria
- Credentialing for senior medical staff in Victoria
- Clinical risk management
- Preventing infections in health services
- Healthy choices
- Victorian Perinatal Data Collection
- Rural health
- Improving Access to Primary Care in Rural and Remote Areas Initiative
- Rural x-ray services
- Rural health regions and locations
- Rural and regional medical director role
- Victorian Patient Transport Assistance Scheme
- Rural and isolated practice registered nurses
- Urgent care in regional and rural Victoria
- Private health service establishments
- Private hospitals
- Day procedure centres
- Mobile health services
- Fees for private health service establishments in Victoria
- Design resources for private health service establishments
- Professional standards in private health service establishments
- Legislation updates for private health service establishments
- Complaints about private health service establishments
- Cosmetic procedures
- Guideline for providers of liposuction
- Private hospital funding agreement
- Boards and governance
- About health service boards in Victoria
- Information and education
- Education resources for boards
- Sector leadership
- Data, reporting and analytics
- Health data standards and systems
- Funding, performance and accountability
- Statements of Priorities
- Performance monitoring framework
- Integrity governance framework and assessment tool
- Pricing and funding framework
- Patient fees and charges
- Fees and charges for admitted patients
- Non-admitted patients - fees and charges
- Other services
- Planning and infrastructure
- Sustainability in Healthcare
- Medical equipment asset management framework
- Health system design, service and infrastructure planning
- Complementary service and locality planning
- Primary & community health
- Primary care
- Community pharmacist pilot
- EOI - Victorian Community Pharmacist Statewide Pilot
- Victorian Community Pharmacist Statewide Pilot – Resources for pharmacists
- Emergency Response Planning Tool
- Working with general practice
- Victorian Supercare Pharmacies
- NURSE-ON-CALL
- Priority Primary Care Centres
- Local Public Health Units
- Community health
- Community health services
- Community health pride
- Registration and governance of community health centres
- Community Health Directory
- Community Health Program in Victoria
- Community health population groups
- Dental health
- Access to public dental care services
- Victoria's public dental care fees
- Victoria's public dental care waiting list
- Dental health for SRS residents
- Dental health program reporting
- Smile Squad school dental program
- Maternal and Child Health Service
- Nursery Equipment Program
- Maternal and Child Health Service Framework
- Maternal and Child Health Service resources
- Child Development Information System
- Early parenting centres
- Maternal Child and Health Reporting, Funding and Data
- Baby bundle
- Sleep and settling
- Maternal and Child Health Workforce professional development
- Aboriginal Maternal and Child Health
- Public Dental and Community Health Program funding model review
- Public health
- Women's Health and Wellbeing Program
- Inquiry into Women's Pain
- Inquiry into Women's Pain submissions
- Support groups and programs
- About the program
- Victorian Women's Health Advisory Council
- Cemeteries and crematoria
- Medicines and Poisons Regulation
- Patient Schedule 8 treatment permits
- Schedule 8 MDMA and Schedule 8 psilocybine
- Schedule 9 permits for clinical trials
- Documents and forms to print or download
- Legislation and Approvals
- Frequently Asked Questions - Medicines and Poisons Regulation
- Health practitioners
- Licences and permits to possess (& possibly supply) scheduled substances
- Medicinal cannabis
- Pharmacotherapy (opioid replacement therapy)
- Recent updates
- Environmental health
- Improving childhood asthma management in Melbourne's inner west
- Climate and weather, and public health
- Environmental health in the community
- Environmental health in the home
- Environmental health professionals
- Face masks for environmental hazards
- Human health risk assessments
- Lead and human health
- Per- and poly-fluoroalkyl substances (PFAS)
- Pesticide use and pest control
- Food safety
- Information for community groups selling food to raise funds
- Food businesses
- Food safety information for consumers
- Food regulation in Victoria
- Food safety library
- Food allergens
- Introducing Standard 3.2.2A: Food safety management tools
- Immunisation
- Respiratory syncytial virus (RSV) immunisation
- Seasonal influenza vaccine
- Immunisation schedule and vaccine eligibility criteria
- Ordering vaccine
- Immunisers in Victoria
- Immunisation provider information
- Cold chain management
- Adverse events following immunisation reporting
- Vaccine error management
- Vaccination for infants and children
- Vaccination for adolescents
- Vaccination program for adults
- Vaccination for special-risk groups
- Immunisation resources order form
- Victorian coverage rates for Victoria
- Infectious diseases guidelines & advice
- Infection control guidelines
- Disease information and advice
- Advice to the cruise industry: reporting infections
- Notifiable infectious diseases, conditions and micro-organisms
- Notification procedures for infectious diseases
- Infectious diseases surveillance in Victoria
- Germicidal ultraviolet light
- Protecting patient privacy in Victoria
- Population health systems
- Evidence and evaluation
- Health promotion
- Health status of Victorians
- Municipal public health and wellbeing planning
- Population screening
- Cancer screening
- Conditions not screened
- Improving outcomes in under-screened groups
- Infant hearing screening
- Newborn bloodspot screening
- Prenatal screening
- Screening registers
- Preventive health
- Type 2 diabetes and cardiovascular disease prevention
- Eye health promotion
- Injury prevention
- Healthy eating
- Oral health promotion
- Physical activity
- Sexual health
- Sex worker health
- Decriminalisation of sex work
- Automatic mutual recognition
- Domestic smoke detectors
- Lasers, IPL and LED devices for cosmetic treatments and beauty therapy
- Victoria's regulatory framework for radiation
- Radiation newsletter
- Tobacco reforms
- Tobacco reform legislation and regulations
- E-cigarettes and vaping
- Quitting smoking and vaping
- Smoke-free and vape-free areas
- Building entrances
- Children's indoor play centres
- Public hospitals and health centres
- Children's recreational areas
- Playground equipment
- Skate parks
- Swimming pools
- Under-age sporting events
- Enclosed workplaces
- Government buildings
- Learning environments
- Outdoor dining
- Outdoor drinking areas
- Patrolled beaches
- Train platforms and bus and tram shelters
- Under-age music or dance events
- Tobacco and e-cigarette retailers
- Making a report or complaint
- Resources and factsheets
- Alternative water supplies
- Aquatic facilities
- Blue-green algae (cyanobacteria)
- Drinking water in Victoria
- Legionella risk management
- Private drinking water
- Recreational water use and possible health risks
- Water fluoridation
- Chief Health Officer
- About the Chief Health Officer
- Chief Health Officer publications
- Health alerts and advisories
- Mental health
- Mental Health and Wellbeing Act 2022
- Mental Health and Wellbeing Act 2022 Handbook
- Community information
- Mental Health and Wellbeing Act 2022 in your language
- About Victoria's mental health services
- Area-based services
- Statewide and specialist mental health services
- Mental Health Community Support Services
- Support and intervention services
- Language services - when to use them
- Access to mental health services across areas
- Transport for people in mental health services
- Practice and service quality
- Medical Treatment Planning and Decisions Act
- Service quality
- Specialist responses
- Mental health and wellbeing reform
- Reform activity updates
- Priority areas
- Latest news
- Working with consumers and carers
- Consumer and carer engagement
- Consumer and Carer Experience Surveys
- Family support and crisis plans
- Consumer and carer financial support
- Supporting children whose parents have a mental illness
- Supporting parents with a mental illness
- Prevention and promotion
- Early intervention in mental illness
- Mental health promotion in Victoria
- Suicide prevention in Victoria
- Priorities and transformation
- Supporting the social and emotional wellbeing of Aboriginal and Torres Strait Islander Victorians
- National mental health strategy
- Rights and advocacy
- Making a complaint about a mental health service
- Chief Psychiatrist
- About the Chief Psychiatrist
- Principles in the Mental Health and Wellbeing Act and the Chief Psychiatrist's guidelines
- Obligations under the Mental Health and Wellbeing Act 2022
- Reporting a failure to comply with the Mental Health and Wellbeing Act 2022
- Governance and committees
- Reporting obligations for clinical mental health and wellbeing services
- Mental health and wellbeing support
- Making a complaint and seeking advocacy
- Second psychiatric opinion and process of review by Chief Psychiatrist
- Office of the Chief Psychiatrist's reform activities and news
- Oversight of forensic mental health and wellbeing services
- Resources and reports
- Chief psychiatrist guidelines
- Chief Mental Health Nurse
- About Victoria's Chief Mental Health Nurse
- Best practice
- Reducing restrictive interventions
- Research and reporting
- Mental health performance reports
- Reporting requirements and business rules for clinical mental health services
- Alcohol & drugs
- Alcohol and other drug treatment services
- Overview of Victoria's alcohol and drug treatment system
- Pathways into alcohol and other drugs treatment
- Prevention and harm reduction
- Medically supervised injecting room
- Victoria's Take-Home Naloxone Program
- Community-based AOD treatment services in Victoria
- Residential treatment services
- Mildura statewide alcohol and drug residential treatment service
- Drug rehabilitation plan
- Hospital-based services
- Forensic services
- Pharmacotherapy treatment
- Services for Aboriginal people
- Services for young people
- Statewide and specialist services
- Compulsory treatment
- Family and peer support
- Public intoxication reform
- New public intoxication response services
- Policy, research and legislation
- Alcohol and drug research and data
- Legislation governing alcohol and other drug treatment
- Alcohol and other drug service standards and guidelines
- Alcohol and other drug client charter and resources
- Alcohol and other drug treatment principles
- Service quality and accreditation
- Alcohol and other drug program guidelines
- Maintenance pharmacotherapy
- Specialist Family Violence Advisor capacity building program in mental health and alcohol and other drug services - Victoria
- Alcohol and other drug workforce
- Learning and development
- Alcohol and other drug workforce Minimum Qualification Strategy
- Workforce data and planning
- Funding and reporting for alcohol and other drug services
- Funding of alcohol and other drugs services in Victoria
- Reporting requirements and business rules for alcohol and other drug services
- Drug alerts
- 25C-NBOMe and 4-FA sold as '2C-B'
- Novel stimulants sold as MDMA, cocaine or speed
- Protonitazene sold as ketamine
- High potency benzodiazepine tablets
- MDMA adulterated with PMMA
- 25B-NBOH sold as powdered 'LSD'
- Green 'UPS' pills containing N-ethylpentylone (no MDMA)
- N-ethylpentylone in cocaine
- Ageing & aged care
- Supporting independent living
- Low cost accommodation support programs
- Personal Alert Victoria
- Dementia services
- Victorian Aids and Equipment Program
- Residential aged care services
- Public sector residential aged care services
- Safety and quality in public sector residential aged care
- Physical and social environments
- Emergency preparedness in residential aged care services
- My Aged Care assessment services
- Home and Community Care Program for Younger People
- HACC data reporting
- HACC PYP fees policy and schedule of fees
- Wellbeing and participation
- Age-friendly Victoria
- Healthy ageing
- Seniors participation
- Dementia-friendly environments
- Designing for people with dementia
- Maintaining personal identity
- Personal enjoyment
- Interior design
- Dining areas, kitchens and eating
- Bedrooms and privacy
- Gardens and outdoor spaces
- Assistive technology
- Staff education and support
- Strategies, checklists and tools
- Our Strategic Plan 2023-27
- Our organisation
- Our secretary
- Leadership charter
- Our services
- Our vision and values
- Specialist offices
- Senior officers in health
- Human Research Ethics Committee (HREC)
- Gifts, benefits and hospitality policy
- Information Asset Register
- Health legislation
- Health legislation overview
- Health Complaints legislation
- Health Records Act
- Human Tissue Act 1982
- Public Health and Wellbeing Act 2008
- Voluntary Assisted Dying Act
- Victoria's pandemic management framework
- Independent Pandemic Management Advisory Committee
- Pandemic Order Register
- Our ministers
- Our role in emergencies
- State Health Emergency Response Arrangements
- Emergency type
- Department's responsibilities in emergencies
- Health services’ responsibilities in emergencies
- Aboriginal employment
- Current vacancies
- Employment programs for students and graduates
- Rise program
- Inclusion and diversity at the Department of Health
- Health workforce
- Working in health
- Information sharing and MARAM
- Child Safe Standards
- Regulatory functions
- Reviews of decisions
- Victorian Public Healthcare Awards
- Aboriginal healthcare workers
- Mental health workforce
- Lived and living experience workforces
- Engaging with lived and living experience workforces
- Our workforce, our future
- Nursing and midwifery
- Free nursing and midwifery study
- Additional funding for nursing and midwifery positions
- Becoming a nurse or midwife
- Undergraduate nursing and midwifery scholarships
- Undergraduate student employment programs
- Nursing and midwifery graduates
- Nursing and midwifery graduate sign-on bonus
- Working as a nurse or midwife
- Enrolled nurse to registered nurse transition scholarships
- Support for new nurse practitioners
- Postgraduate scholarships for nurses and midwives
- Nurse practitioners
- Returning to nursing or midwifery
- Refresher pathway for nurses and midwives
- Re-entry pathway scholarships for nurses and midwives
- Nursing and midwifery - legislation and regulation
- Nursing and midwifery program - health sector
- Allied health workforce
- Education and training
- Enterprise agreements
- Worker health and wellbeing
- Working with us
- Grants and programs
- Freedom of Information
- Part II - Information Statements
- Procurement policies
- Protective markings
- Health and medical research
- Sponsorship application information
- Publications
- Annual reports
- Fact sheets
- Strategies, plans and charters
- Policies, standards and guidelines
- Research and reports
- Forms and templates
- Communities
- Designing for Diversity
- Vulnerable children
- Vulnerable children - responsibilities of health professionals
- Identifying and responding to children at risk
- Pathway to good health for children in care
- Older people
- Aboriginal health
- Improving health for Victorians from culturally and linguistically diverse backgrounds
- Asylum seeker and refugee health in Victoria
- News and media hub
- Media releases
- Health alerts
- Feedback and complaints
- Make a payment
- Fees, charges and penalties subject to automatic indexation
- Our campaigns
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window
Share this via Facebook Share this via X Share this via WhatsApp Share this via Email Other ways to share Share this via LinkedIn Share this via Reddit Share this via Telegram Share this via Printer
Download the full report in English
Mental Health Crisis Support Rooted in Community and Human Rights
A Case Study
A Gerstein Crisis Centre Mobile Team responding to a call in Toronto. Crisis teams develop relationships with local communities, providing an alternative to police as first responders in mental health crisis situations. © 2023 Courtesy of Gerstein Crisis Centre
Introduction
Mental health service provision can—and should—respect the human rights of individuals seeking or receiving care. The necessary components of mental health services that respect human rights include informed consent, as well as the availability, accessibility, acceptability, and quality of mental health services. For more than a decade, Human Rights Watch, a global human rights organization, has pushed for a rights-based approach to services and supports for people with a range of disabilities in different settings around the world. [1]
According to the World Health Organization, in 2019, an estimated one in eight people globally—970 million—was living with a mental health condition, and yet, on average only 2 per cent of health budgets were dedicated to mental health. [2] Human Rights Watch research in more than 60 countries has found that mental health services frequently fail to comply with international human rights standards due to stigma related to mental health, the use of coercion, and power imbalances between the service provider and the person seeking or receiving support. [3] In many jurisdictions, inadequate legal and policy protections reinforce discrimination and abusive treatment of people with mental health conditions. The situation is particularly dire for individuals experiencing mental health crises, including in circumstances related to substance use, suicidal thoughts, trauma, housing insecurity, and poverty. Instead of receiving rights-respecting community-based services for their mental health needs, many people face punitive measures by law enforcement and other approaches that may not be suitable, such as in many cases, “wellness checks” by the police. [4] Such crisis responses expose individuals to the risk of police violence, criminalization, involuntary hospitalization, forced treatment, and displacement of unhoused individuals, and this risk is higher for Indigenous and racialized groups. [5]
As part of its growing efforts to promote solutions-oriented approaches, Human Rights Watch is documenting a series on good practices that may serve as useful models for governments and service providers to comply with the principles in the UN’s Convention on the Rights of Persons with Disabilities. As the first part of this series, Human Rights Watch documented the innovative approach of TANDEMplus, a mobile team in Brussels providing mental health services to people with psychosocial disabilities in their homes or a place of their choice, where they work hand-in-hand to find solutions and help the person regain control over their everyday life. [6]
One Canadian initiative, Gerstein Crisis Centre, stood out as a case study for mental health crisis support rooted in community and human rights. For more than 30 years, this community-based service provider has offered communities in Toronto safe, humane, equity-based crisis services. Gerstein Crisis Centre provides free and confidential 24/7 tailored support services to individuals experiencing a mental health and/or substance use crisis, including thoughts of suicide, all of which may be exacerbated by or emanate from trauma, housing insecurity, and poverty, among other things.
In 2021, Human Rights Watch and Gerstein Crisis Centre collaborated to present a snapshot of what a rights-based support service may look like, in contrast to the prevailing forms of mental health crisis responses that predominantly focus on police and/or forced hospitalization. [7] This case study provides a more detailed description of the Centre’s approaches and unpacks lessons learned and good practices emerging from decades of rights-respecting community-based mental health support. These good practices stem from the Centre’s experiences in Canada and are presented as a case study for service providers to consider given each unique context, rather than as a prescriptive guide. Every country and community has different needs that may require a different approach.

Police emergency 378. Do you have an emergency?
Darna Savariu, Crisis Counselor, The Gerstein Crisis Centre
The police is somebody with power, you know with the ability to apprehend somebody and take somebody to the hospital, even against their will.
Elaine Amsterdam, Crisis Service Coordinator, The Gerstein Crisis Centre
If you’ve had poor experience with the police, if you’ve been marginalized, if you come from racialized communities, chances are somebody else could better respond to that community member in need .
Nicki Casseres, Coordinator of Training and Community Education, Gerstein Crisis Centre. And there’s a lot of opportunity that we don’t have to get to that end place where somebody is in such a desperate place that the only thing that they can do is call 911.
Susan Davis, Executive Director, The Gerstein Crisis Centre
Toronto police services respond to about 33,000 mental health crisis calls every year. We need to flip our system as it exists right now from a sort of default position where police are responding to mental health crisis and actually purpose-build a system that allows people to access mental health support when and where they need it.
Kaola Baird, Former Client of the Gerstein Crisis Centre
I’ve been battling chronic depression ever since I can remember. This particular period in life, I was under a lot of stress. I had been working, going to school but I was in the process of losing my apartment. I learned about the Gerstein Centre while I was in counseling. I realize now that I’m lucky enough that at my lowest point, I can reach out for help.
Gerstein Crisis Centre, Darna speaking. How can I help you today?
Gerstein Crisis Centre provides a number of ways in which we respond to individuals in crisis. That includes a telephone crisis line, a mobile team that goes out into the community and sees people where they are, as well as we have a number of crisis beds that offer short stays to people.
My approach to a client in crisis is to listen attentively to what the person is saying…
And this is your first time calling? Yeah?
helping them understand what resources are available
Two of us can come meet you somewhere in the community, if that would be helpful
Gerstein operates in a voluntary nature. Nobody is forced to do anything they don’t want to do .
In the last year, we had 42,000 phone calls and I can tell you that that was double the number of the year before.
Nicki Casseres, Coordinator of Training and Community Education at Gerstein Crisis Centre
And we say, when you are going through a difficult time, you can contact us. You don’t have to wait until it gets so bad that you have to call 911 or you end up in the hospital.
The Toronto police recently started initiated a pilot project with the Gerstein Crisis Centre to co-locate a crisis worker within the 911 call centre.
911 operators transfer callers with non-emergent needs to the crisis worker, diverting the call away from a police reponse.
Nicki Casseres, Coordinator of Training and Community Education, The Gerstein Crisis Centre. And so when people call 911 and then get diverted to talk to a crisis worker, and they can get follow up and we can connect them into the right services.
My first stay at the Gerstein Centre , it didn’t make the immediate crisis go away, but then you can see clearly so you can make decisions. You can make better decisions.
Individuals need a rights-based approach to their health care. They need to be able to have access to the supports and services they need without losing their autonomy. Our commitment at Gerstein Centre is to really listen to and hear the voices of people with lived experience of mental health and substance use. At least 30% of people on our board and our staff are people with lived experience.
My gratitude to those that helped me at Gerstein helped me appreciate what other people are going through.
Kaola Allison Baird, F.R.E.S.H. worker
Today, we’re playing bocce ball. It’s one of the many activities being offered through FRESH. The FRESH program stands for “Finding Recovery through Exercise, Skill and Hope. “ It’s an opportunity for people who’ve had lived experience to come out and learn a skill, be active in a very welcoming, supportive environment.
What we really want to do is to help people develop some strategies that can help them survive the moment and bring them forward because something that works now, may work again.
A non-police non-coercive crisis response is so essential for being able to really provide an option to people that they in that moment make use of and feel like it could be helpful to them.
We’re more than what goes wrong in our life and I feel thankful that I’ve had the experiences I’ve had. Since I've started paddling, I've had a renewed sense of confidence. Realizing your own strength, realizing your own abilities. And every time you go out on the water, it's a test. So it's like a victory every day, every time.
Section I outlines how disability justice and human rights frameworks should inform mental health services. It discusses the importance of rights-based mental health support, built on concepts such as recovery and agency. Section II provides insights into Canada’s mental health care system and the emergence of the Gerstein Crisis Centre more than 30 years ago, against the backdrop of Canada’s wider deinstitutionalization processes. Section III shares key pillars that shape the Centre, formulating the core lessons learned and good practices from the Canadian context. It stresses the importance of centering support around lived experiences and, as such, describes (1) how the Centre addresses power dynamics, including when working with or co-located alongside other actors, and (2) the core services the Centre provides. All sections highlight lessons learned and good practices for service providers to consider in order to promote crisis responses that are community-based and rights-respecting. Each section concludes with the lived experiences of Kaola, a woman who received support at Gerstein Crisis Centre and has continued to work with the organization as a peer to support others experiencing mental health crises.

Human Rights Watch is currently expanding its research on disability rights and mental health service provision, and the issues and good practices discussed here will inform its global research and advocacy on this subject, taking into account the unique specificities of culture, society, and politics.
Human Rights Watch and Gerstein Crisis Centre hope this document inspires action among and across mental health service providers, service users, policymakers, and human rights and mental health advocates on providing community-based and rights-respecting support to people experiencing mental health crises. This document provides examples of how this is being done in Canada, and we invite you to consider their applicability to your current and future work.
I. A Rights-Centered, Holistic Approach
Recent trends in standards and policies on mental health services, such as the Quality Rights guidance developed by the World Health Organization, [8] recommend placing people in mental health crises at the center of decision-making, prioritizing their choices. [9] This person-centered approach highlights agency, choice, and informed consent as the bedrock for the right to health and other human rights.
A human rights-based approach to mental health support also centers on a holistic response to the person’s needs—one that addresses the combined impact of social, physical, emotional, and environmental factors, including discrimination, structural racism, and other forms of exclusion and repression. Such a system should account for the person’s housing, food, and employment situation, among other needs. This also involves crisis responses that go beyond immediate de-escalation and stabilization, to enable people to recover their sense of belonging, inclusion, and connection with others. [10]
Such approaches conform to international human rights law, which has moved away from considering people with psychosocial disabilities as objects of care and instead engaging with them as rightsholders. [11] A one-size-fits-all response is not the solution but, at a minimum, recovery should focus on respect for the person’s own experiences, wishes, coping mechanisms, and choices, including the possibility of not receiving support. [12] Recovery is not about curing people or making them function in a specific way prescribed by society; instead, it should foster a sense of wellbeing that focuses on finding meaning in one’s life and an individual defining for themselves what is desired and hoped for to reduce the harmful effects of their pain and symptoms as much as possible. [13]
Flaws of the Current Approach
There is increasing consensus that people with mental health conditions are crucial contributors to the delivery and transformation of mental health services because they possess relevant knowledge and lived experience. Historically, however, services in many parts of the world rarely center on the person in crisis, meaning they often fail to prioritize the needs, perspectives, expertise, and experiences of individuals seeking mental health support. [14]
Many mental health services continue to have an overreliance on a “medical model,” which often decenters a person’s agency, over-pathologizes the individual, and reduces support to the urgency-driven provision of medication. Many times, the medical model does not focus enough on recovery-oriented approaches that more fully embrace human rights and fails to consider social determinants contributing to mental health crises. [15]

People with mental health conditions (or psychosocial disabilities) around the world often face stigma and prejudice. [16] False perceptions—such as the commonly held belief that people with mental health conditions are incapable of deciding what is best for themselves—pose major barriers to the enjoyment of their human rights. For centuries, professional knowledge regarding the diagnosis and treatment of mental health conditions has been valued over the knowledge and insight of people who live with those conditions. [17] Even today, treatment of mental health conditions can be coercive; for example, forced medication, forced hospitalization, removal from the community, and physical or chemical restraints continue to be used in many countries. [18] Such involuntary treatments can cause or worsen trauma. [19]
Despite significant evidence of its harms, coercion is often justified by classifying the person as a danger to themselves or others. [20] This classification is often vague and open to arbitrary interpretation and application by police officers. Coercion is also often framed as a “last resort” even though it can be—and has been—used as a first or emergency response. [21]
In Canada, as in many countries, police are typically the first responders to mental health crises. [22] When someone is experiencing distress, their emotional state may deteriorate when confronted by police due to power imbalances, fear of violence, and fear of being apprehended. This reaction can be particularly acute for Black, Indigenous, and racialized people who experience higher rates of police violence. [23] In Canada, such incidents too often happen when a concerned person calls the emergency services number (911) seeking help for someone experiencing a mental health crisis. [24] In 2021, four people in Canada were killed during police responses in the course of “wellness checks.” [25] Two-Spirit, lesbian, gay, bisexual, transgender, queer+ ( 2SLGBTQ+) communities have also been historically mistreated by police in Canada, putting them at increased risk when seeking help during a mental health crisis. [26] Any use of force that discriminates against people with disabilities, Indigenous people, racialized groups, and 2SLGBTQ+ communities violates various international treaties and standards. [27]
Governments and other funders have not sufficiently invested in community mental health services. Consequently, the capacity of existing community- and rights-based services is still stretched, often resulting in a mental health crisis response that prioritizes reliance on law enforcement and hospitals. [28]
Barriers to Rights-Respecting Mental Health Crisis Support Services
The establishment of a rights-respecting community -based crisis intervention service can be daunting, especially in environments where medical and psychiatric responses to mental health crises—which can include involuntary detention and treatment, violence, and coercion—continue to dominate and where the government or local authorities tacitly accept human rights violations and abuses. While police involvement in mental health crises has been challenged by communities across North America following incidents of police violence and deaths of individuals in crisis, police remain the first responders to mental health crises in many places. Every person, including anyone who may be struggling with their mental health, deserves to have their rights respected.
Community-based crisis services can improve immediate responses and access to follow-up support. However, long waitlists for housing, lack of culturally relevant counseling and mental health services, as well as insufficient financial assistance, often leave people isolated and unable to access health and social resources in a timely way, which can contribute to escalating and repeated crises.
An overly narrow focus on crisis response without adequate investments in a broader range of community resources to address social determinants of health (such as housing, employment, and income support, and equitable access to rights-based treatment and services) also undermines the government’s obligation to uphold the right to the highest attainable standard of health. In particular, such a narrow focus can undermine the perceived effectiveness of a broader range of community resources, while continuing to obscure under-investment in health services and the social determinants of health. [29]
Mental health support should be available through a low-barrier health support system rather than law enforcement. In particular, the goal of such a low-barrier system is to provide easy, timely, and equitable access to quality health services and support for everyone within the community—with minimal requirements for connection and entry. Marginalized communities, such as 2SLGBTQ+, Black, Indigenous, and racialized people have specific generational and lifelong experiences of discrimination and exclusion in health and social systems that too often resulted in over-policing and over-incarceration. Services should reflect the experiences of the communities served, including those who are often subject to coercive medically-focused responses, racism and other human rights violations such as inequitable access to housing, employment, and education (commonly understood as the social determinants of mental health).
| © 2021 Samer Muscati/Human Rights Watch Kaola Baird, a resident of Toronto, received support at Gerstein Crisis Centre and continues to work as a peer to support others experiencing mental health crises. I don't really see my story as being something so fantastical because I've met a lot of people who have really lived with a lot more challenges than I do. … But I have lived my entire life in absolute fear. I experienced a loss when I was very young—my mother. She was quite ill after she had me and proceeded to just go downhill. She died a couple of days after my second birthday, and apparently, we were just starting to bond. She had a really horrible, painful death. And I did not even really process her death until I was 18. My aunt raised me well; she's my mum. And I knew the story of my mother's death, but it didn't really register. It was just—it was a story. But I had been struggling with depression and it got progressively worse. By the time I turned 16, I was self-medicating, as in reaching into the medicine cabinet, just wanting to go to sleep and hoping that I wouldn't wake up. And I was never sure why I just always felt different and alone. Like I didn't really belong anywhere. And I was not connected to anyone. I realize now that I was lucky enough, when I was at my lowest point, to have a place to reach out to get help and the support I needed. Because even though I feel suicidal, I'm also really, really scared. |
II. The Emergence of Community-Based Mental Health Care in Canada
From the mid-1900s to the early 2000s, psychiatric hospitals gradually closed across Canada. This deinstitutionalization was fueled, among other factors, by provincial governments’ belief that community care would cost less and by the growing awareness of institutionalization’s long-term harms. [31] By 1981, the Province of Ontario saw a 75 percent decrease in bed capacity at psychiatric facilities, and similar changes took place across the country. Nova Scotia Hospital in Dartmouth, for example, reduced its beds from more than 1,000 in the 1960s to fewer than 200 by 2003. [32] The overall reduction of space discharged people from psychiatric hospitals into the community, rendering them reliant on community mental health services that were poorly funded, if they existed at all; in many jurisdictions, they were altogether absent. [33]
Following this process of deinstitutionalization, people in some communities were left unhoused and without access to basic services. In response, in 1983, the mayor of Toronto established a task force to investigate the situation for people who had been discharged from psychiatric hospitals and who were living in the city. [34] The task force’s report and recommendations laid the groundwork for a coordinated community response to address the key issues facing people who were living with mental health conditions, which would bring together the municipal, provincial, and federal governments. One key recommendation was the formation of an independent, community-based, standalone crisis center. [35] This made way for an effort to shift away from the medical model to a community-based approach that puts people with lived experience at its heart, like that of Gerstein Crisis Centre.
Establishment of Gerstein Crisis Centre
In 1989, the chair of the Toronto task force, Dr. Reva Gerstein, in collaboration with community members, including people with lived experience of mental health systems, founded Gerstein Crisis Centre. With funding from Ontario’s Ministry of Health, the Centre started by offering telephone and mobile services. In 1990, the Centre established 10 crisis beds and offered three-day crisis stays. [36]
At that time, the main source of support for people with mental health conditions in the city was a strict medical model centered around hospitals and rife with coercive practices. [37] Many people with mental health conditions, as well as progressive mental health professionals, advocated for a rights-respecting and recovery-based crisis response—one that understood that crises were not inevitable consequences of mental health conditions. They promoted an approach that recognized that crises often resulted from the combined impact of social, physical, emotional, and environmental factors, including a lack of access to essential services and supports, poverty, unstable housing, coexisting substance use, other health conditions, traumatic experience, racism, sexism, and gender discrimination.
More than 30 years later, Gerstein Crisis Centre continues to provide an alternative to hospitals and police stations to support individuals in a mental health crisis. The Centre uses a philosophy of care that centers the lived experiences and safeguards the autonomy of people experiencing mental health distress, enabling them to choose the support they consider is best and connecting them to resources , as needed and desired, to assist in their recovery. To do this well, Gerstein Crisis Centre recognizes the importance of building and strengthening pathways and partnerships that improve access to health and social services for individuals in crisis. Service provision, and its related approaches, should evolve over time to meet current needs and address gaps across systems.
The impact of Gerstein Crisis Centre illustrates the importance of scaling up and expanding such programs, including co-designing such programs in collaboration with local community members and people with lived experience, particularly as law enforcement and involuntary treatment continue to be the primary responses to mental health crises in many jurisdictions around the world, including in Canada.
| © 2021 Samer Muscati/Human Rights Watch I was in the process of rebuilding my life and doing a fairly good job at it, but I’d been battling chronic depression ever since I can remember. I was forced to realize what had been haunting me, holding me back. It just triggered a tsunami, and I was very suicidal. It's not the first time in my life that I experienced that, but it was the first time in many years. And my world was collapsing. I was about to lose everything—I had been working and going to school, but I was in the process of losing my apartment. The things that I needed to do or had wanted to do, I couldn't do because of this desperate fear of—I'm not sure what. But everything came to a head. And I finally did call Gerstein, and so they came out to see me in the community. I was desperate, scared. I knew my life was about to change immensely and I felt I was very alone. I'm not one to talk to people about what's going on in my private life. You know, I have my close friends and they know my general situation, but I never want to be a burden on people. My first stay at the center allowed me to have a good night's sleep. I was still able to work at the time and I could come back, come home, and relax. I think sometimes being out of your regular space, you're forced to just let go. The people were warm and amazing and supportive. And the physical environment for me—that was important. I remember stepping into the house and there was soft jazz in the background and lots of artwork and the lighting … It was very inviting. It was very soothing. And I started to let go and I guess have better perspective on things. It didn't make the immediate crisis go away, but then you can see clearly, so you can make decisions, you can make better decisions. And that was an important first step. When you normalize what a person is feeling, when you can remove that sense of panic and then move to step one and just focus on that step one, and then you deal with step two after—it felt the way I imagined turning to your family for help would feel. … You also have access to resources and it's not crossing any boundaries. So, you still have your independence and your sense of privacy, but there's a warmth and a trust and a normalization of what you're going through. You don't feel like a client or a number or that you're being processed. I shudder to think … Had the police been called for me, I would assume that I would have been taken to a hospital. This is where I feel rather fortunate because I have had experience with self-admittance to hospitals, but I can imagine being scared and being in a different frame of mind that can send you deeper into whatever break you're having. And that wall of fears is a different, difficult one to climb over. So, I would shudder to think what would happen if I were in those shoes. I think when you're going through a crisis, depending on the person and the situation, I think sometimes you lose a sense of who you are. Because everything becomes about this thing that's happening. And as much as you can maybe have a window and see that there are those other things happening in life. And there's more to it than just this cloud. That's going to be different for each and every person, but I think there's always a window somewhere. And I think there's a lot to be said for not wanting to be seen as your crisis because there's still a person underneath. I'm not my illness. I'm not my diagnosis. I'm not whatever crisis I've lived through. |
III. How Can a Rights-Centered Approach Work?
This section provides a case study on lessons learned and good practices, based on Gerstein Crisis Centre’s rights-respecting and community-based approach in Canada. The aim is to assist communities and service providers who are considering how best to establish rights-based, people-centered services for individuals experiencing mental health crises, taking each community’s unique context into account.

Gerstein Crisis Centre provides 24/7 community-based mental health services geared toward diverting individuals aged 16 years and older in mental health crises away from unnecessary interactions with police and hospital emergency rooms. The crisis intervention services include:
- The telephone crisis line team is linked directly to the Centre (at 416 929 5200) and also accessible through a municipal helpline (211) that connects people to social services, programs and community supports;
- A crisis worker is co-located in the 911 Call Centre responding directly to mental health calls that have been diverted away from police dispatch;
- A mobile crisis team that follows up on calls in the community upon request, serving two high-needs neighborhoods;
- Crisis beds in private rooms in two large houses that provide a safe, homey, and supportive environment, staffed around the clock, designed for short-term stays of up to 30 days;
- Short-term follow-up support, including referrals to other beneficial health and social services; and
- Recovery programs, led by individuals with lived experience of mental health, substance use, and the criminal justice system.
The Centre employs about 100 people, the majority of whom have lived or living experience with mental health conditions or substance use. In the fiscal year 2022-2023, 56% of the Centre’s staff, as well as 40% of the Centre’s leadership team and 43% of the Board, had such lived experiences. The phone and mobile crisis workers are experienced intervention specialists, many of whom have lived experience and who reflect the diversity and voices of the communities served. Starting with the initial phone call to the crisis line, the individual in crisis guides what services they would like to receive and tells their story to a crisis worker, whose first step is to listen.
People who seek support from Gerstein Crisis Centre present various concerns that intersect with a mental health crisis. In the fiscal year 2022-2023, according to Centre intake data, 66 per cent of people who engaged with the Centre identified increasing concerns with mental health or substance use as among the reasons for seeking support; in addition, 60 per cent reported issues of isolation, 24 per cent relayed concerns regarding insecure housing, and 20 per cent reported suicidal thoughts. Others reported concerns regarding physical health (25 per cent), family or relationship issues (18 per cent), legal issues (6 per cent), physical or sexual abuse (5 per cent), and employment related issues (3 per cent). The variety of concerns identified by people seeking support at the Centre illustrates the critical importance of person-centered services embedded in a holistic approach that begins with a crisis worker listening.
There are four key components of Gerstein’s person-centered, holistic approach:
- A ddress power imbalances;
- B uild trust;
- L isten to people with lived experience and include those voices in governance and leadership; and
- E ngage partners across diverse sectors.
| Elaine Amsterdam has worked at Gerstein Crisis Centre since 1989 and was part of the first mobile crisis team. Though the organization has grown and evolved, its foundation and the meaning of success has remained consistently rooted in health and social justice: For many folks who are dealing with persistence and intrusive mental health difficulties, success may mean that they feel better and are better valued, that they are less stigmatized and have a sense of their own strength from learning what helps them, what triggers them, what helps them survive. … To be seen not as less than, but equal to. So much of what we see is embedded in loss, pain, forced isolation, as well as all the cross-sectional social determinants of health. And seeing improvement is a success; it’s appreciating what that means in an evolving way for anyone. |
Addressing Power Imbalances
Stigma, marginalization, poverty, and explicit or implicit bias predicated on race, disability, sex, gender identity or expression, language, and/or immigration status, among other things, can influence power dynamics, diagnoses, treatment, and endanger human dignity and even lives.

To reduce power imbalances between the service provider, the service recipient, and the systems and institutions that support them, Gerstein Crisis Centre proactively engages the individual in crisis in the spirit of collaborative interventions rather than coercive ones, and in a safe, unintrusive manner.
For example, the Centre’s Mobile Crisis Intervention Team wears regular clothes rather than uniforms or logoed apparel and uses vehicles with minimal if any markings. The aim of this practice is not only to minimize the experience of power differences that a uniform may promote but also to respect the dignity and privacy of the person in their community by not publicly advertising that the workers or the vehicles are associated with crisis intervention services. Crisis workers carry Gerstein Crisis Centre identification and service materials, as this low-key approach helps create a sense of safety for people they meet in the community. Mobile crisis intervention teams engage in conversation with the person in crisis to learn about the presenting crisis. They listen to the person to learn what is happening with them at the moment and then help identify the immediate needs or concerns, including physical needs and safety risks (e.g., current thoughts of suicide or self-harm).
| Within the mental health or social service context, people using the services depend on staff for their well-being and to receive services. They require the expertise of staff for their treatment and care over which they often have no control. This dependence on staff and lack of control can put them at particularly high risk of coercion and violent and/or abusive treatment. A number of factors can influence and exacerbate the power dynamics in mental health and social services: Given the potential power dynamics in a service, the behaviour of staff towards people using the service has a huge impact on their rights as well as on their well-being and recovery. Identifying and preventing violence, coercion and abuse can happen only when people acknowledge the unequal power dynamics in a service and change their behavior accordingly. A respectful and supportive contact decreases chances of escalation and reduces the risk of violence, abuse and coercion. All people deserve to be treated on an equal basis with others, with dignity and respect. |
Building Trust with Service Users
Trust is at the core of relationships and can lead to quicker de-escalation of crises. To foster trust, the Centre works together with the person in crisis to understand and find the best way forward for them as an individual. The team does this by listening intently to the person, inviting them to share their story from their perspective, acknowledging their feelings, identifying their strengths, providing support networks, and demonstrating a thorough understanding of their situation. The team also reassures the person that their immediate basic needs, such as food, drink, and shelter, will be met, which can greatly promote trust and indicate a genuine recognition of the whole person. As such, crisis intervention is understood as a collaborative process that begins with connecting and rapport building to better understand the individual’s experience and context before co-creating a crisis and safety plan.
Gerstein’s crisis response includes supporting people with complex needs, including suicidal thoughts, substance use, mental health conditions, trauma (including inter-generational trauma associated with discrimination), housing insecurity, and poverty. This requires staff to be nimble and flexible. Responses and service plans are specifically shaped to respect the communication and service needs of each individual and to meet them where they are comfortable engaging: within the context of their unique history, perspective, and quality of life and health goals. Simultaneously, the crisis team assesses the individual’s immediate safety, explores any concerns in this regard, and works with the individual to develop a safety and crisis plan to help mitigate the identified concerns. Sometimes building rapport and connection is immediate; often it builds over multiple interactions across time, where greater trust needs to be established. In some cases, the person prefers to be referred to other alternatives, and the crisis team facilitates this process as well.
| The telephone crisis line is typically how people access support services at Gerstein. An individual experiencing a crisis—or someone else concerned about an individual, such as a friend, family member, service provider, medical professional, doctor, police officer, or a stranger or—can call the crisis line and speak directly to a member of the crisis team. Regardless of the caller, any engagement requires the consent of the person experiencing a crisis. Most often, the crisis worker and the individual concerned address the crisis over the phone by creating and agreeing upon a crisis and safety plan. If more support is needed, and only if the caller consents, that same crisis worker will take a teammate with them to visit the caller in the community on a mobile crisis team visit. No medical professionals or police officers are involved in Mobile Team visits; only trained mental health crisis workers, many of whom have lived experience, respond, and the information they gather remains strictly confidential. Mobile crisis team visits happen anywhere it is safe to meet; for example, someone’s home, a coffee shop, or a park. The Mobile Team can offer the individual concerned a stay at the Centre, one-to-one conversation, crisis counselling, referrals to external resources and follow-up. |
Crisis responses seek to identify and reinforce the personal strengths of the individual in crisis to help them recover from the crisis and protect themselves against further occurrences. This entails inviting the individual to start determining their future based on their strengths; that is, what is “right” in their lives rather than what is “wrong.” This aims to build confidence and comfort, which is especially important in circumstances where there are many uncertainties about basic necessities and ways forward. In this way, the crisis worker helps the individual value themselves and collaborate on developing a crisis plan to address their needs.
| Gerstein Crisis Centre and the person in crisis collaboratively develop an individualized plan that typically includes: |
Service is provided to anyone who calls Gerstein Centre and anyone who is part of the person’s immediate support network, such as a friend, neighbor, or family member. It is important to recognize that, in some circumstances, a person calling about someone they are worried about may also benefit from crisis intervention, support, resources, and referrals.
Gerstein Crisis Centre endeavors to be responsive to the culture, race, age, disability, sexual orientation, gender identity and expression, health literacy, and language needs of the people it serves. The Centre intentionally hires crisis responders who have lived experiences of mental health conditions and substance use, and who reflect the diversity of the communities they serve. Having a team with varied backgrounds and experiences allows people in crisis to see themselves reflected in crisis responders, creating greater opportunities for engagement and connection. It also brings a greater depth of experience and expertise to the Centre’s crisis teams.
Gerstein Crisis Centre values equity and thus its service providers are required to participate in continuous learning and specific trainings, including on anti-racism and anti-oppressive practices. The Centre also encourages its service providers to critically analyze approaches, teachings, research findings, and understandings in the field of crisis intervention that were developed inside and outside Canada. The Centre can refer the individual in crisis to culturally appropriate services, if desired by the individual. In addition, Gerstein Crisis Centre has 24/7 access to interpretation services in more than 180 languages.
Centering Lived Experience in Leadership
The voices of people with lived experience of mental health conditions and substance use should be at the core of rights-based services and support at all levels.
Gerstein Crisis Centre engages people with lived experience in every aspect of its work, including as members of the crisis intervention team and leaders in the organization. The Centre’s governance structure and by-laws require that at least 30 per cent of the Board of Directors are people with lived and living experiences of mental health conditions or substance use.
Engaging with Partners Across Sectors
A key aspect of improving access to health, social, and other support services is engaging in collaborations with individual, community, and governmental partners within and across sectors.
Gerstein Crisis Centre has many partnerships that leverage expertise to better serve client populations, including supports and services for older people, transitional-age youth, Black and Indigenous people, people with disabilities, 2SLGBTQ+ communities, and survivors of trauma. Services are also available to address substance use and harm reduction, food insecurity, and income support, as well as issues related to the justice system, housing insecurity, shelter assistance, and primary care. To that end, the Centre has created pathways and connections to support services that address some of the underlying issues that can contribute to a mental health crisis. This work is ongoing, and new pathways and partnerships are always being formed to address emerging gaps in services.
Avoid Unnecessary Emergency Medical and Police Interactions
Mental health needs are best met with a consent-based health response and quality services that are timely and equitably accessible. Free and informed consent is a human right. Key elements of free and informed consent include prioritizing the autonomy of the individual in crisis in determining next steps. The individual’s wishes are paramount: if they do not want to engage, they can be invited to seek services again if they change their mind. There should be no pressure on the individual to change their mind.
| It is important to be aware of the risk of undue influence due to the power imbalance in relationships that exists within mental health and social services. There is sometimes a fine line between supporting people in making their decision and unduly influencing them. Informed consent means: The right to informed consent also includes the right to refuse treatment. This means that if a person, after being offered information about treatment options, decides they do not want any kind of treatment, this is their right and must be respected. |
In the vast majority of situations, the Centre responds first with trained mental health crisis workers—without engaging emergency medical services or the police—to maximize the participation and choice of the individual in formulating their own crisis plan. Information gathered in the course of providing crisis services remains strictly confidential. This approach addresses crisis situations without the risks of coercion or criminalization. It also ensures that the rights and decisions of service users remain paramount.
In its advocacy to shift mental health crisis responses toward rights-based community support, Gerstein crisis workers participate in various initiatives to divert people away from a criminal justice response. These include weekly “Situation Tables,” co-organized by the City of Toronto, Toronto Police Service and United Way Toronto, where community-based service providers come together to divert people in crisis (that is, people who are at elevated risk of criminality or vulnerable to criminalization) away from law enforcement and refer them to community-based supports through “a targeted, wrap around approach.” [40] These Situation Tables bring together representatives from Gerstein Crisis Centre, as well as representatives of community agencies providing housing support, case management, income, and other beneficial service supports.
Gerstein Crisis Centre also offers short-term residential crisis beds and support in Toronto for individuals who are referred by police or other criminal justice sources. All individuals referred have current involvement with the criminal justice system, are unhoused, and are experiencing mental health conditions and/or substance use. All stays in the crisis beds are consent-based, and Gerstein Crisis Centre does not report to the police any infractions with bail orders. Instead, the Centre works with people on setting goals that are meaningful to them and supports them in pursuing those goals.
In 2021, the Centre expanded its services, piloting a project that places crisis workers at 911 communication centers to provide immediate crisis intervention to callers rather than sending a police response. Crisis workers sit alongside 911 operators to receive calls diverted to their confidential line, and they provide immediate crisis response and intervention, follow-up, and connection to beneficial services as much as possible.
In 2022, Gerstein Crisis Centre expanded again to launch the Toronto Community Crisis Service Team, a non-police response that can be accessed by calling 911 or 211 (a municipal helpline that connects people to social services, programs and community supports). This team of crisis intervention workers is co-located in the call centre where 911 calls are received prior to dispatch to fire, police, or ambulance. The goal is to provide immediate crisis intervention and to help avoid unnecessary interactions with police. Instead of the 911 call taker sending a police officer, the community crisis workers engage with individuals experiencing mental health crises, providing crisis and suicide interventions, de-escalation, connection to health and social services, harm reduction supplies, and other resources, including things like warm coats, water, food, and up to 90 days of follow-up. Once a caller is diverted to a Gerstein crisis worker, the call is forwarded to an independent private Gerstein phone line that is not monitored by police. All services are voluntary and consent-based and divert individuals away from unnecessary police and hospital interactions. In fiscal year 2022-23, almost 2,000 calls were actioned by the Gerstein co-located crisis team, all with the goal of diverting the caller to a mental health, trauma-informed, hard-reduction response and avoiding a police response.
The Centre’s non-medical low-barrier approach, as well as its multiple access points, allow individuals to seek tailored support in the community when and where they need it. Many people who use the Centre’s services value having the choice to get crisis support without going to the hospital or involving law enforcement. They feel they can reach out as soon as they are struggling, not just when it becomes an emergency. Reaching out earlier allows the Centre to provide support, develop strategies, and facilitate community linkages to the resources needed to help prevent crises from escalating or taking place at all. Gerstein Crisis Centre also receives referrals from emergency rooms after the person in crisis has been seen if the hospital believes further crisis support in the community would be beneficial.
| Different actors involved in mental health crisis response, such as the police, emergency medical services, hospitals and abstinence-based services, may use different approaches. In such interactions, it is important for community-based and rights-respecting service providers to uphold fundamental values and maintain integrity while improving coordination and collaboration to better serve individuals and the community. The following are some questions to consider asking when collaborating with actors that have a different focus or approach to mental health crisis response: |
What Are Some Core Elements of a Rights-Based Approach to Crisis Service?
Services such as a 24/7 telephone crisis line, mobile crisis intervention teams, and a house with crisis beds can reflect a rights-centered, non-carceral, holistic approach. Gerstein Crisis Centre’s work offers insights into how this can be done in compliance with international human rights standards.
Involvement with the Centre is completely voluntary and based on free and informed consent. Clients retain autonomy and the ability to continue, end, or reengage with the Centre at any time without fear of recrimination. Other follow-up services and referrals to other community supports can be provided at any juncture.
In the fiscal year 2022-2023, the Centre responded to 38,892 crisis calls, provided 10,828 mobile visits in the community, and hosted 805 house stays in the Centre’s short-term residential accommodation. [41]

Telephone Crisis Line
Individuals experiencing a crisis can call the Centre’s 24/7 telephone crisis line and receive support from skilled and experienced crisis workers, including people with lived experience. Service is provided immediately over the phone, in English, French, and more than 180 other languages using interpretation services.
When someone calls Gerstein Crisis Centre’s telephone line, conversations usually start on a first-name-only basis for both the service user and crisis worker. The Centre respects the choice of anonymity, which may facilitate greater openness and freedom for some callers. First, the crisis worker endeavors to establish connection and build rapport quickly. The crisis worker helps the person share their story and current situation. The crisis worker takes an active, supportive stance, integrated with empathy, active listening, and understanding in order to help define the caller’s concerns, acknowledge their feelings, ensure safety and support for them, clarify choices and alternatives, and collaborate to make a crisis plan that suits the caller.
| Many people using mental health services have experienced trauma in their lives. When violence, coercion and abuses occur in mental health services, not only do the service fail to help people but they compound the original difficulties, by retraumatizing people using the service. When working with a person in distress, a good start may be to ask first what could bring relief (e.g. if there is a preferred person who could be contacted, or if there is a specific need). Since most tension starts from discomfort and powerlessness, listening carefully and reducing powerlessness are key. In addition, responding early reduces the chances that the situation escalates into a conflict. An appropriate and effective response to a tense situation involves: When dealing with tense situations, it may be necessary to think about the safety of all the persons around (e.g. asking people whose presence is not necessary to leave the room or to stay at a safe distance). |
Mobile Crisis Intervention Team
After a call on the Centre’s telephone crisis line, Mobile Crisis Intervention Teams conduct a follow-up in the community upon their caller’s request. This decision is usually made within 10 to 30 minutes over the telephone. Depending on distance, urgency and availability, the team will estimate 40 minutes to 4 hours for arrival. Additional telephone support can be provided in the meantime.
The team focuses on the person in crisis and their expressed immediate needs, taking a collaborative approach that prioritizes informed consent. Situations are addressed in a low-stigma, non-intrusive, and non-threatening manner that uses engagement, listening, and collaborative problem-solving to de-escalate the situation and achieve greater safety for the person and their community. While the focus of engagement is assisting someone to cope more effectively with their immediate stresses, the mobile crisis intervention team understands that the individual exists within a wider context beyond their crisis.
| Darna Savariau-Daley has been a crisis worker at Gerstein Centre for over 30 years, handling the crisis helpline and working as a member of the mobile crisis intervention team. A large portion of the calls the Centre receives come from individuals with suicidal thoughts. Darna described the Centre’s approach to de-escalation and suicide interventions: “We do a lot of listening: we hold your hand and help you through whatever you’re going through. What’s the best course of action we can take you? Part of my job is to give people as much information as possible, give them the choices, and then together we make a decision. Sometimes, it’s a matter of just listening with compassion and saying, ‘hey, it’s okay, we all go through bad times; let’s talk about it and see where we can go with it.’ It’s very low-key and informal.” © 2021 Samer Muscati/Human Rights WatchWhere a caller expresses suicidal thoughts, crisis workers begin with assessing safety to find out whether the person has already hurt themselves, and whether they have a plan and the means to harm themselves or others. “It’s not a one size-fits-all,” according to Darna. “We talk about how they are feeling and what’s behind those thoughts. We focus on their strength base: ‘What has kept you going?’” The Centre only calls 911 in cases involving immediate life-endangering situations. If, for example, a person in crisis has already swallowed a bottle of pills, then the situation turns into a medical emergency and medical intervention is needed. In almost all such cases, the crisis worker informs the person in crisis that paramedics are on the way. The crisis worker helps determine with the person in crisis if there are choices that can be addressed and advocated for with emergency responders. The crisis worker continues to support the person before paramedics arrive and afterwards, once the person has been medically cleared. The only very rare exception to letting the person in crisis know that paramedics are on the way, is if there is indication by the person that disclosing the call to 911 would further endanger their life and/or that of someone else. Every effort is made to preserve a person’s life in a manner that supports their dignity and choice. All crisis workers are trained in suicide intervention and will ensure that each call about suicide begins with exploring why someone feels the way they do that day and ends with a safety plan in which both the caller and crisis worker feel confident. |
Houses with Crisis Beds
Gerstein Crisis Centre operates two houses with crisis beds, providing a safe, supportive environment that is staffed around the clock. One-on-one crisis counselling, referrals, and support are provided. The houses also serve as headquarters for both the telephone crisis line and the Mobile Crisis Intervention Team. In the houses, people can access what they want to take care of their own needs as much as possible. The kitchen is always open, and residents can help themselves to food in the fridge when they would like a snack or a meal. While staff and/or volunteers prepare dinner for the whole house, people are encouraged to make their breakfast and lunch; assistance is available if requested.
| Too frequently services focus on people’s problems and deficits. An essential part of recovery is for people to identify and build on their assets and strengths. This does not mean denying the pain and distress that a person may experience. These feelings should be acknowledged, and the person should be supported to explore them and find ways to overcome them, using their strengths and assets. | |
|
|
|
| Starts with deficiencies and responds to problems. | Starts with assets and identifies opportunities and strengths. |
| Provides support that is limited by the service’s specific mandate or policy rather than focusing on the needs of the individual. | Sees people as experts in their own recovery and acknowledges that people are capable of making decisions. |
| Requires practitioners or other supporters to move from “fixing people” to supporting recovery. | |
| Treats people as passive recipients of care. | Emphasizes collaboration and co-production between the person concerned and practitioners and other supporters in the recovery process and journey. |
| Sees problems or deficits as existing within the person themselves and tries to “fix” or “stabilize” the person. | Views and treats the wider community as assets. |
| Empowers people to better take control of their lives and supports them to develop their potential, with an understanding that they themselves hold the answers and solutions. | |
Spaces within the houses are designed to provide a home-like, healing environment that is respectful and dignified. Space is a major concern for many service users as they often live in congregate environments, such as shelters or supportive housing, where they lack the personal space or privacy they need during a crisis. All crisis beds are in individual private rooms so people can have their own space and the ability to lock their doors to strengthen their feelings of safety and security.
The Centre also pays attention to furnishings and wall colors, intentionally selecting items that appear “non-institutional” and striving to financially support people with lived experience in the process. Social enterprises that employ people with lived experience of mental health crises made a lot of the furniture, people with lived experiences gifted or sold all the art on the walls, and social enterprises provide all cleaning and catering.
| F.R.E.S.H. is a Gerstein Crisis Centre initiative that uses a peer-led model to help people get active, strengthen their community and social connections, develop new skills and knowledge, and have fun. Group activities include yoga, gym groups, bocce ball, boxing, ball hockey, trail hikes, walking groups, and more. For participants who would like to take their fitness to a higher level, individualized one-to-one sessions with a F.R.E.S.H. worker or fitness partner are available. All F.R.E.S.H workers have lived experience of mental health conditions and/or substance use and have navigated many of the issues participants are facing. They all have a passion for physical activity, education, and social/community involvement. |
| Some of the best advice and information I received were from other peers—experiences that they had, things that they did. This definitely allows me to share with other people who are going through things that I went through. I think when you've been through journeys in life, whether it was mental health connected or not, I think when you're able to come out the other side, you really do appreciate things. Whereas before I didn't really feel a purpose in life … it's the little things that I do now that that give me purpose. © 2021 Samer Muscati/Human Rights WatchWhen I meet people now who live with very, very challenging diagnoses, I don't necessarily always know their story. I may never know their story. And that's a good thing because when you meet that person, you just start there, and you don't assume anything of them. And then they will let you in. And they know that their problems haven't been resolved fully. But it's a rejuvenation, and that has a ripple effect. And I've seen it. … I've lived it. Whatever the person's medical health condition is, whatever stage of recovery they're at, that's part of their story. It's not who they are. And I think it's good to remind them and to remind ourselves that we're more than what goes wrong in our life. My gratitude to those that helped me at Gerstein as the years go by—I can look back and think about those times and actually be so thankful and grateful for the opportunities that I've had because of it. Those are things that helped me appreciate what other people are going through. I learn from the people that I work with, but then I can also listen, and we can exchange stories about how an experience feels or what it means. And by going through it myself, I think it just gives you that deeper understanding. … I have a lot of empathy. … I try to give back what I received and still do receive. You just go full circle, but for me, I always think the circle gets larger. Because then you get more tools in your toolbox and hopefully you learn, and you grow. |
IV. Key Recommended Practices for Communities and Service Providers
The following are key recommendations for communities and service providers developing and delivering mental health crisis support services:
Power Dynamics
- Center human dignity and autonomy, a collaborative approach to service provision, and the perspectives of people with lived experience, particularly the individual in crisis.
- Intentionally strive to mitigate power imbalances between service users and service providers.
- Prioritize the autonomy and expressed needs and desires of individuals in crisis to build trust, and tailor strategies to a particular individual in crisis.
Collaborations and Partnerships
- Establish and build strong relationships with individual, community, and governmental actors across diverse sectors while upholding a rights-based approach to crisis support.
- Closely consult and collaborate with individuals and organizations led by people with lived experience.
- Collaborate and partner across sectors to create multiple, intentional access to needed health and social services that direct people to community crisis responses.
- Engage in advocacy on a broader range of community resources to address social determinants of health, including housing, employment, and income support, and equitable access to treatment and services.
- Establish low-barrier, client-driven early access to mental health and crisis support.
- Collaborate with hospitals to create pathways to community-based support.
Crisis Service Provision
- Offer crisis services 24/7 to ensure services are always available when needed.
- Include different methods of immediate crisis responses, such as phone and in-person services.
- Make immediate crisis responses available in the language the person in crisis prefers.
- Be able and willing to meet the individual in crisis where that person is comfortable.
- Prioritize the autonomy of the individual in crisis in determining the next steps, such as whether they want to stay at the Centre. If they do not want to engage, invite them to seek services again if they change their mind, but do not pressure them into doing so.
- Houses with crisis beds should feel home-like and “non-institutional.”
- Establish an independent organization with a governance structure driven by lived experiences, firmly rooted in the mission, vision, and values of the organization.
- Meaningfully include people with lived experience at all levels of the organization, from service provision to leadership roles.
- Ensure that a critical mass of people with lived experiences serve on the board and in other decision-making roles.
- Seek adequate, appropriate, sustainable levels of financial support to ensure stability of operations.
- Urge government entities to support community-based service providers with adequate funding, preferably core funding.
Evaluations and Accountability
- Engage external evaluators to maximize unbiased gathering and analysis of data.
- Involve people with lived experience in leading and facilitating the evaluation to create environments where service participants are comfortable sharing honest information about their experiences.
- Ensure evaluations identify service gaps and make recommendations on improving service provision to better respond to the needs of the communities served.
- Develop a strong accountability framework that combines appropriate and recommended standards of practice with a commitment to inclusivity and social justice practice.
- Solicit the experiences and observations of service users and implement their recommendations for change.
Mental health is receiving unprecedented global political attention, yet in most regions, there continues to be little to no recognition of the social context in which mental distress occurs or what the activism of people with lived experience can offer to promote humane and rights-based approaches. Indeed, too often mental health recovery models and their basic tenets of choice and autonomy are constrained by biomedicalism, over-policing, and deeply engrained stigmatizing and discriminatory attitudes toward people experiencing mental distress. [44] These enforcement models risk overriding people’s rights and perpetuating responses that may be discriminatory, coercive, violent, and traumatic.
Despite these challenges, service users and people with lived experiences around the world have played a key role in resisting marginalization and oppression. This has included questioning the past and present harms of involuntary psychiatric care. It is vital to recognize and elevate the work of organizations like Gerstein Crisis Centre that are grounded in this history and offer an approach to care that is non-medical, trauma-informed, and focused on harm reduction, information, choice, and consent.
For policy writers and legal advocates, this Gerstein Crisis Centre / Human Rights Watch case study offers a viable roadmap to provide safe and humane community-based care through rights-respecting services for individuals experiencing a mental health crisis. In many jurisdictions where under-investment and de-prioritization of rights-based community services are commonplace, this case study offers hope and guidance on transforming theory into practice. The work of Gerstein Crisis Centre foregrounds lived experiences throughout its approach and governance model. The Centre pushes beyond the all-too-familiar rhetorical deployment of “nothing about us without us” by continuously asking what it means to engage with people experiencing mental health crises and to transform the systems that purport to care for them.
This case study strives to do just that. It contains the frameworks, principles, and values needed to mobilize people and bring about fundamental change to mental health crisis care. Above all, it offers concrete guidance for how care practices can respect people’s autonomy and human dignity, as well as follow expertise that is based on lived experiences of mental health crises.
Marina Morrow is a Professor in the School of Health Policy and Management at York University. For over 20 years, she has worked collaboratively with psychiatric survivors, community-based organizations, and policymakers to surface the harms of biomedicalism and how neoliberal regimes reinforce individualist understandings of mental health over social and collective understandings of well-being.
Lucy Costa is the Deputy Executive Director of a rights-based service user-led organization in Toronto, Canada. Her work has involved educating and advocating a wide range of stakeholders, including police services, psychiatry residents, lawyers, and the public. She is the co-editor of Madness, Violence and Power: A Critical Collection .
Related Content
Mental health crisis support rooted in community.
Governments Should Invest in Rights-Respecting Alternatives to Punitive, Involuntary Treatment
- Disability Rights
Protecting Rights, Saving Lives
Human Rights Watch defends the rights of people in close to 100 countries worldwide, spotlighting abuses and bringing perpetrators to justice
share this!
March 1, 2023
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Social workers experienced depression, PTSD, and anxiety at alarming rates during pandemic
by University of Toronto
A new study published in the journal International Social Work has uncovered concerning rates of depression, post-traumatic stress disorder (PTSD) and anxiety among social workers.
Stressors related to COVID-19 were the strongest factors associated with the negative mental health outcomes. Those who experienced a higher number of pandemic-related stressors—such as health concerns , increased caregiving responsibilities, violence in the home, family stress due to confinement, and stress associated with work-life balance —experienced mental health problems at a higher rate compared with those who were not as impacted by pandemic-related hardships.
"Like physicians, nurses and other allied health care providers , social workers are feeling the impact of the pandemic, and it is showing up in their mental health," says lead author Ramona Alaggia, a professor at the University of Toronto's Factor-Inwentash Faculty of Social Work (FIFSW) and the Margaret and Wallace McCain Chair in Child and Family. "As we celebrate Social Work Week in Ontario March 6—12 and National Social Work Month in March, it is important to recognize the stressors that affect social workers and the well-being of those working in this essential field."
An alarming 40% of the sample reported depression—which is four times higher than the general population. The rate of reported depression among social workers is also substantially higher than other health care professionals working in COVID-19 related conditions, where the prevalence rate of depression has been found to be 24%. In total, one fifth of the sample reported PTSD while 15% reported anxiety.
"As personal stressors among social workers have increased, so too have the needs of those they serve," says co-author Esme Fuller-Thomson, FIFSW professor and director of the Institute for Life Course and Aging at the University of Toronto. "With rising rates of domestic violence, child abuse , mental health illnesses and addictions, death rates in long-term care systems, and homelessness, social workers' jobs have become more demanding than ever."
The majority of survey respondents were from Ontario and married or in common law unions. Half of the respondents had children under the age of 18, and 85% were women, which is consistent with the number of women working in the social work field.
"Recent trends clearly indicate women have felt the most negative employment change and job loss during COVID-19," says Carolyn O'Connor, co-author and a doctoral candidate at FIFSW. "Time studies consistently show that women are usually the ones carrying most childcare and domestic responsibilities at home. Meanwhile, COVID lockdowns made working from home even more stressful as parents juggle work demands with home-schooling, while experiencing isolation and fewer supports."
The study also found that the social workers most affected by mental health problems tended to be younger, less experienced and less established in their profession. Levels of resilience were also measured. Those who were older and had higher income had higher resilience scores.
"Job instability is common early in a social worker's career, especially when working within a neo-liberal environment that promotes precarious, contractual work conditions with fewer benefits and lower pay," says co-author and FIFSW Ph.D. candidate Keri West.
Alaggia says that in her work with community-based agencies, she has observed that social workers have been leaving in high numbers since the start of 2022, with some agencies reporting as much as 30% shortfalls in staffing levels and significant problems filling those positions.
"It seems a tipping point has been reached where-by social workers are leaving traditional settings because of low wages, job insecurity and meager benefits," Alaggia says. "Given the essential societal roles that social workers' play, strategies to sustain the profession into the next generation and future generations are urgently needed. These strategies should include a trauma informed approach and strong mental health supports for staff. This may be a defining moment in the social work field and building resilience into social service systems is the way forward."
Provided by University of Toronto
Explore further
Feedback to editors

Genetic algorithm enables precise design of phononic crystals
49 minutes ago

Scientists discover way to 'grow' sub-nanometer sized transistors
3 hours ago

Scientists pinpoint strategies that could stop cats from scratching your furniture
8 hours ago

Two new species of Psilocybe mushrooms discovered in southern Africa
15 hours ago

UV radiation damage leads to ribosome roadblocks, causing early skin cell death
17 hours ago

Dual-laser approach could lower cost of high-resolution 3D printing

Novel method enhances size-controlled production of luminescent quantum dots

Cosmic simulation reveals how black holes grow and evolve
18 hours ago

How climate change is affecting where species live

Human presence shifts balance between leopards and hyenas in East Africa
Relevant physicsforums posts, cover songs versus the original track, which ones are better.
7 hours ago
Who is your favorite Jazz musician and what is your favorite song?
Jul 1, 2024

Biographies, history, personal accounts
Jun 30, 2024
Today's Fusion Music: T Square, Cassiopeia, Rei & Kanade Sato
Jun 29, 2024
The Balinese Alphabet
Jun 27, 2024
History of Railroad Safety - Spotlight on current derailments
Jun 26, 2024
More from Art, Music, History, and Linguistics
Related Stories

Witnessing parental domestic violence in childhood linked to mental illness in adulthood
Apr 20, 2022

Poorer physical health among those who experience discrimination in Canada
Dec 16, 2022

Older adults with asthma at high risk for depression during the COVID-19 pandemic
Jan 19, 2023

The impact of COVID-19 on the mental health of home health care workers in Japan
May 31, 2022

UK railway workers 'did not receive timely advice' on responding to pandemic
Oct 27, 2022

Majority of children who have contact with the child welfare system flourish in adulthood
Jun 15, 2022
Recommended for you

Study: More complaints, worse performance when AI monitors employees
20 hours ago

Watching others' biased behavior unconsciously creates prejudice, finds study
21 hours ago

Understanding the synchronization of physiological states during a live music performance
22 hours ago

The beginnings of fashion: Paleolithic eyed needles and the evolution of dress
Jun 28, 2024

Study finds motivation to compete is stronger with in-group members than with outsiders

We date and marry people who are attractive as we are, new analysis finds
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Phys.org in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
158 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.
Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
July 2, 2024
Walking El Camino de Santiago Helped Me Reconnect With My Authentic Self
“Beneath the outward bravado, I battled with self-doubt and kept wondering why genuine connections seemed beyond my ability. Even though I put out valiant efforts to conceal it, my inner turmoil seeped out, leaving me feeling exposed and vulnerable. And, I knew they could tell.”
Struggled with: Feeling lost People-pleasing Self-doubt
Helped by: Self-acceptance Self-awareness
June 27, 2024
My Journey of Overcoming Heartbreak Thanks to Self-Care and The Support Of Friends
“I’ve learned that finding the right people to confide in, those who offer genuine support and empathy, can make a significant difference in navigating these challenges. It takes time and trust to build those connections, but they are invaluable.”
Struggled with: Breakup
Helped by: Self-Care Social support
June 19, 2024
How Therapy, Self-Help and Medication Help Me Live With Depression and Anxiety
“When the next depressive episode hit in 2018, I was devastated. How could this happen again when I thought I had it all figured out? I experienced some of the darkest moments of my life and a nearly complete loss of hope.”
Struggled with: Anxiety Bipolar Disorder Depression Suicidal
Helped by: Medication Therapy
June 11, 2024
Sharing My Journey From Alcohol and Substance Abuse to Sobriety and Happiness
“I felt prettier, smarter, funnier when alcohol entered my body so I simply continued numbing through the years. The progression of this disease of alcoholism turned into a nasty drug habit and those feelings of insecurity turned into deep darkness when I was “off my meds”. Or in other words, without alcohol or drugs.”
Struggled with: Addiction Depression Suicidal
Helped by: Rehab Therapy
June 4, 2024
Finding Happiness and Self-Love After Escaping Death From Burning 90% Of My Body
“It was like starting life over again, except you know how to do things you physically can’t do, which emotionally drains you. There was definitely a sense of resentment and feeling sorry for myself, I think that is natural. You wonder what you did to deserve that, you wonder if things are ever going to get better, you wonder how people will treat you. When you are confined to a bed for weeks on end, really all you can do is wonder.”
Struggled with: Physical trauma
Helped by: Self-improvement Social support
May 28, 2024
Cognitive Reframing and Mindfulness Helped Me Overcome Depression and Suicidal Ideation
“After exploring ways to end my life, I resolved to slash my wrist. I retrieved a steak knife from the kitchen and pressed it against my skin. Yet, an unexpected sensation washed over me—a profound sense of peace, love, and joy.”
Struggled with: Depression Suicidal
Helped by: Meditation Mindfulness Self-improvement
May 21, 2024
Learning To Live With Postpartum Depression (PPD) Through Self-Acceptance and Coaching
“I absolutely did not want to talk to anyone about this. I found it easier to tell a stranger about my struggles because I knew I would not see them again. I felt that telling family or friends made my struggle real. I felt that they would now be able to hold me accountable.”
Struggled with: Postpartum depression
Helped by: Self-acceptance Social support
May 14, 2024
I’m Finding Luck After Trauma and Abuse Through Mindfulness
“I never mentioned the accident to anyone until I met my future husband at 22. He was sympathetic and supportive, and helped me understand the enormity of what I had been through.I still have not talked to my siblings about it.”
Struggled with: Abuse Depression Eating disorder Suicidal
Helped by: Meditation Mindfulness Reinventing yourself
May 7, 2024
My Journey From Hitting Rock Bottom to Overcoming Abuse, Addiction, and Eating Disorder
“Then something happened. On about day 3 or 4, the group spoke and I realized that their way of thinking around food, their rituals, and their tendencies, were all the same as the things I would do. It was wild because I thought I had made these things up myself and here I was with a room full of people who did the same things.”
Struggled with: Abuse Bullying Depression Divorce Eating disorder PTSD
Helped by: Self-Care Social support Therapy Treatment
May 2, 2024
How Yoga Became My Lifeline in Navigating Depression and Building Self-Love
“My relationship with myself was pretty broken and I had no self-belief, I had low self-esteem and I resented my family. It was through yoga that I found the truest feeling of comfort, self-compassion, and courage to move forward, grow as a person, and fall back in love with myself and life again.”
Struggled with: Depression Insomnia Stress Suicidal
Helped by: Exercise Meditation Mindfulness Self-Care
Certified Peer Support in the Field of Homelessness: Stories Behind the Work
- Original Paper
- Open access
- Published: 02 July 2024
Cite this article
You have full access to this open access article

- Margriet de Zeeuw Wright ORCID: orcid.org/0009-0003-6990-7436 1 &
- Candice Morgan 1
Certified peer support specialists (CPSS) are used as a paraprofessional workforce to engage hard-to-reach populations, including people experiencing homelessness. Thematic analysis was used to explore with CPSS (N = 7) what contributed to their effectiveness when working with this population. Participants were recruited at a HUD lead organization in the southeastern United States. Open-ended semi-structured questions were used in online, synchronous interviews. Themes related to three areas, experience, competence, and the organization, contributed to participants being effective. Specifically, interviewees observed that their lived experiences and abilities to speak a common language with clients contributed to their effectiveness. They identified how personal qualities and unique skillsets suited them for the work. Participants also valued the training they received; certification helped them to develop competencies and to balance vulnerability, empathy, and connection. Finally, participants attributed their effectiveness to clarity about their roles within the organization, supervision, attention to self-care, and co-worker support. Findings from this study may have implications for the value of lived and learned knowledge coexisting in organizations serving those who experience homelessness.
Avoid common mistakes on your manuscript.
Introduction
An individual who lacks a fixed, regular, and adequate nighttime residence may be defined as homeless (de Sousa et al., 2023 ). A recent Point-in-Time count in the United States found that approximately 653,000 people were experiencing homelessness (de Sousa et al., 2023 ). These data reflect an increase of 12%. Six in ten people were experiencing sheltered homelessness, meaning they resided in emergency shelters, transitional housing, or safe havens. Four in ten people were experiencing unsheltered homelessness, meaning they lived in places not meant for human habitation (de Sousa et al., 2023 ). Given its rise, homelessness is a social problem requiring immediate attention.
Homelessness may lead to losses in health, safety, and connectedness. People experiencing homelessness are at risk for acute and chronic health issues (Hwang et al., 2011 ; Krakowsky et al., 2013 ; Raoult et al., 2001 ; Wadhera et al., 2020 ). High rates exist for mental illness (Gutwinski et al., 2021 ), cognitive impairment (Stergiopoulos et al., 2015 ), and drug and alcohol use (Aubry et al., 2012 ). Safety is at risk, hope diminishes, and trust in support services erodes. The result can be isolation and feelings of worthlessness, leading to depression and loneliness (Sanders & Brown, 2015 ). This population has been described as hard to reach (Miler et al., 2020 ) and given the complex, multidimensional aspects of being unsheltered and having substance use and / or health and mental health issues, recovery is difficult to achieve.
It should be noted that “recovery from” is different from being “in recovery.” People may recover from a broken leg, while people who struggle to exit homelessness and overcome substance use or mental health issues, may be in recovery for a lifetime. Kelly and Hoeppner ( 2015 ) sought to clarify recovery as a construct and proposed a bi-axial formulation of recovery for substance use relevant for this discussion of homelessness. According to the authors (Kelly & Hoeppner, 2015 ), there is a reciprocal relationship between remission of a substance use disorder on the one hand, and recovery capital on the other. Recovery capital includes physical and mental health, housing, social relations, education and employment, and meaning and purpose in life (White & Cloud, 2008 ). The bi-axial formulation places remission on one axis and recovery capital on the other (Kelly & Hoeppner, 2015 ). The model proposes that as addiction remission becomes more stable and prolonged, the positive benefits of recovery capital become more evident. From this viewpoint, “recovery is a dynamic process characterized by increasingly stable remission resulting in and supported by increased recovery capital and enhanced quality of life” (Kelly & Hoeppner, 2015 , p. 179).
Kelly and Hoeppner ( 2015 ) suggest that the relationship between remission and recovery capital is mediated by increased coping abilities and decreased experiences of stress. The authors use Lazarus and Folkman’s ( 1984 ) Transactional Model of Stress and Coping to conceptualize these mediating elements. The model suggests that individuals engage in appraisals in the face of stress. A primary appraisal determines if a situation warrants attention. If it is assessed as stressful, a secondary appraisal determines whether the stress exceeds resources and requires strengthened coping. For individuals early in their recovery process, the stress response is more sensitive and may interfere with new learning and increase the risk of relapse (Kelly & Yeterian, 2013 ). Simply stated, managing substance use and accumulating recovery capital hinge on stress appraisal and increased coping; many who succeed do so through the support of their peers.
Peer Support
The history of peer support dates back decades, however, it is best known in the form of the twelve-step model (Alcoholics Anonymous, 2002 ), where sponsors mentor peers who are managing alcohol use. Howard “Howie the Harp” Geld (Harp & Zinman, 1994) was a consumer and consumer rights activist of the 1970’s who believed that “to transform the treatment system, you need to transform its workforce” (Community Access Inc., 2020 para.2) and that “those closest to the problem have a unique part to play in shaping the solution” (Community Access Inc., 2020 para.3). This is supported by a recent report (National Institute for Health and Care Excellence, 2022 ) that recommended that peer workers with lived experience of homelessness be involved in the design and delivery of services, to improve the quality of health and social care to this population. Peer support has grown and developed into a managed resource. As of 2023, 49 of 50 states in America have established programs to train and certify peer support workers Footnote 1 (SAMHSA, 2023 ). Peers assist others with similar challenges, often related to mental health and substance use issues; however, peers support others “in a wide range of nonclinical activities, including advocacy, navigation and linkage to resources, sharing of experience, social support, community and relationship building, group facilitation, skill building, mentoring, goal setting, and more” (SAMHSA, 2023 , p. 7). Training and certification “attest that an individual has the skills and knowledge required for the peer support services profession” (SAMHSA, 2023 , p. 7).
Chinman et al. ( 2016 ) described a wide range of services and activities provided by peer support workers that include “promoting hope, socialization, recovery, self-advocacy and developing natural supports and community living skills” (p. 2). There is consensus that empathy and respect, a nonjudgmental stance, voluntary participation, direct communication, mutual responsibility, shared power, and reciprocal support guide peer support (National Association of State Mental Health Program Directors, n.d.). SAMHSA ( 2018 ) has identified an emerging set of core competencies of peer support workers including: engaging in collaborative and caring relationships; offering not simply support but personalized support; sharing lived experiences of recovery; recovery planning; linking to resources, services and supports; providing information about skills; managing crises; valuing communication; engaging in collegial collaboration and teamwork; promoting leadership and advocacy; and promoting growth and development. Barker and Maguire ( 2017 ) reported that peer support effectively contributed to shared experiences, role modelling, and social support.
Valuing the contribution that peer support workers offer means valuing a non-professional vantage point (Mead & MacNeil, 2006 ). Perceived empathy is one of the key benefits of peer support (Campbell & Leaver, 2003 ). Clay ( 2005 ) described this empathy and respect in terms of safety and acceptance with a focus on an individual’s strengths, noting that the mutual sharing of stories provided encouragement and an opportunity to offer technical support to peers. In this respect, peer support workers function as role models to show that recovery is possible (Clay, 2005 ). The experience of simultaneously being in recovery while assisting others in recovery has proven to be mutually beneficial; however, there are also vulnerabilities contained within this type of relationship that are worth considering. Challenges can be conceptualized as occurring at an individual level and at a system level. Dennis ( 2003 ) identified peer worker stress and over-involvement as potential individual-level challenges. There is also the possibility that peer support workers, in acting as role models, might model negative behaviors (Barker et al., 2019 ). At a system-level, Yuen and Fossey ( 2003 ) noted workload demands as something that required attention. Mowbray et al. ( 1998 ) suggested that professional colleagues may not value the recovery messages offered by peer support workers and may undermine the efforts and confidence of their peers. In their comprehensive review of the literature, Miler et al. ( 2020 ) supported these points and identified five key challenges for peer support workers; this included vulnerability; authenticity; boundaries; stigma; and a lack of recognition of the value of peers. Vulnerability was framed in terms of threats to peer support workers’ own recovery. Maintaining authenticity was a challenge for some peer workers who felt distanced the longer they were in recovery or the more regulated they were as employees. Boundaries were conceptualized as a balance of rapport and self-disclosure, with some limits. Stigma was framed in the literature in a couple of ways, including workplace experiences of discrimination and peer workers stigmatizing their own community. Valuing peer support workers was discussed in terms of respect for the work and adequate compensation. Miler et al. ( 2020 ) recognized the challenging work done by peer support workers and offered guidelines for how this workforce can be integrated effectively into service delivery for those experiencing homelessness. Their review is especially relevant to this study, as it targeted peer support in homelessness.
Focus and Aims of the Study
This pilot study took place with an organization whose mission was to break the cycles of homelessness. The organization was a coordinated entry point serving 13 counties in the southeast region of the United States. Four to five of these counties consistently ranked the lowest on national health outcomes, income, and housing indicators (personal communication A.G.). People with disabilities, veterans, youth, families, and survivors of intimate partner violence were served by the organization. All clients were in housing crises, and depending on their needs, they could also address substance use issues in transitional housing, receive permanent supportive housing assistance, case management, claims support, and homelessness prevention services. The organization grew exponentially in recent years from an annual budget of $140,000 and one full-time employee, to a $10 million annual budget and 54 employees. Organizational funding sources included the U.S. Department of Housing and Urban Development (HUD), the U.S. Department of Veterans Affairs (VA), and private money. Half of the program’s direct service employees, who were called “Team Members,” had lived experiences of homelessness and substance use, and / or mental health issues. Their roles related to intake, housing support, case management, and outreach. These peer support workers inspired and contributed to this study. The study’s aim was to explore what contributes to the effectiveness of Certified Peer Support Specialists (CPSS) in the field of homelessness.
CPSS were involved in the study design and recruitment, data collection, analysis, and reporting. Approval was obtained from the Institutional Review Board (IRB) of the University of South Carolina. Open-ended semi-structured interviews were conducted. An interview guide grew out of Miler’s et al. (2020) systematic review of peer support at the intersection of homelessness and problem substance use. The authors proposed guidelines for how to embed peer workers in services. Furthering their work, this study asked participants to discuss whether and / or how any of the following elements contributed to their effectiveness: (1) the clarity of their role description, (2) the adequacy of their compensation, (3) the degree of support they received, (4) the level of training and development and advancement opportunities, (5) perceptions of their value within the organization, and (6) the degree of flexibility around workplace accommodations, if needed. This qualitative study used a thematic analysis approach, including constructionist, inductive, and latent methods (Boyatzis, 1998 ; Braun & Clark, 2006 ; Burr, 1995 ; Hayes, 1997 ; Rubin & Babbie, 2016 ), to discern and present insights.
Sampling, Study Design, Recruitment, and Data Collection
Seven of a possible 13 CPSS participated in the study. CPSS were recruited through an online information session, multiple emails, and flyers placed at the organization. Participants were required to have received certification as CPSS and to work as CPSS at the time. The seven participants were between the ages of 29 and 42 (mean age 35.3). Of these, five identified as female and two as male. While participants were given the choice whether to self-disclose, 6 explicitly identified that they had experienced homelessness. One reported a history of mental health issues in addition to homelessness. All seven participants reported lived experiences of addiction. Time in recovery ranged from 5 to 16 years (mean time in recovery 9.42 years). Job tenure at the agency varied from 9 months to 5.5 years (mean job tenure 2.5 years). Two longer-serving participants reported earning internal promotions, leading to greater responsibility.
All participants had opportunities to ask questions about the study and gave informed consent to participate. Participants also consented to the publication of results. They were interviewed on average for an hour. Interviews occurred through an online platform and were video and audio recorded. Those who agreed to participate received $20 for completing the interview. We developed a clear policy on payment and recognition prior to involvement. We disclosed that each person would receive $20 cash in the mail to an address of their choosing. The $20 was mailed in a thank you card, detailing why the recipient was receiving the money and thanking them for their time, within a week following the interview. With respect to recognition, we chose to keep the identities of the participants confidential to encourage interviewees currently employed in the agency to be open and honest about their experiences there. We involved one key informant in the decision to provide $20. We sought advice from a supervisor who confirmed this would be comparable to the typical hourly wage at the agency. We also arranged for participants to be allowed to complete the interview while on the clock at the agency, hence receiving double compensation. Participants did not have to take time off to participate.
Data Analysis
Thematic analysis was used to identify, analyze, and report patterns with the data without being tied to any pre-existing theoretical framework (Braun & Clark, 2006 ). Both MW and CM were responsible for the coding. We relied on a constructionist method, “which examines the ways in which events, realities, meanings, experiences, and so on are the effects of a range of discourses operating within society” (Braun & Clark, 2006 , p. 81). We understood that our participants’ experiences and internal constructions of reality form in discourse, which is an understanding held with a social constructionist approach (Gergen, 1999 ). As we conducted and analyzed interviews, we paid close attention to how participants recalled experiences as CPSS and how those recalled experiences formed a reality for them.
An inductive approach was taken to identify themes and patterns. Our goal was to provide a detailed analysis of some aspects of the data, namely what contributes to the effectiveness of CPSS, according to self-report. Focusing on role description, compensation, support, development, value, and accommodations (Miler et al., 2020 ), we took a reflective thematic analysis approach (Braun & Clark, 2006 ). We considered the interview data, as well as our own positionality as social workers and the context of CPSS work within an organization. We chose to identify latent themes and patterns within the data (Boyatzis, 1998 ) ascribed by the participants, as well as by our interpretations. Thematic analysis at the latent level was a good fit with the constructionist approach (Burr, 1995 ).
Thematic analysis was conducted in six phases as depicted in Table 1 . CM and MW worked through the phases separately first, and then together meeting weekly to compare, discuss, and focus our analysis. We strove for consensus rather than compromise during data analysis. To confirm the credibility of our results, we member checked (Birt et al., 2016 ) our data analysis with several participants for accuracy, and resonance with their experiences.

Phase 4 Thematic Map in Response to the Question: What Contributes to the Effectiveness of CPSS in the Field of Homelessness?
The study found that themes broadly related to three areas, namely experience, competence, and the organization, contributed to participants being effective in their jobs. First, their lived experiences and abilities to speak a common language with clients contributed to their effectiveness. They identified that their personal qualities and unique skillset gave them confidence to do the work. Second, participants valued the training they received, as certification helped them to understand and develop competencies to use themselves to offer hope to clients, and to balance vulnerability, empathy, and connection with boundaries. Third, participants in this study spoke about how the organization supported them to be effective in their positions as peer workers. Formally, clarity about their roles, supervision, and attention to self-care were important. Informally, co-worker support was noted as vital to their ability to do the work effectively. There may be reciprocal interaction among factors that made these participants with these competencies at this organization effective in their roles.
Several themes emerged that described what drew these participants to this work. These themes related to their lived experiences of homelessness co-occurring with either substance use or mental health issues, common language, a unique skill set, and confidence in discerning client needs. Nearly all participants explicitly stated that working hard was a part of who they were. They were passionate about their work and internally motivated to not only work at, but work for, the organization.
Lived Experiences Compared with Learned Knowledge
These participants recognized the value of their lived experiences. Participants saw the empathy, skill, and knowledge their co-workers brought to the work. This challenged previously held beliefs for some, who thought that helpers had to have “been there” to appreciate the realities of their experiences of homelessness, mental health issues, or substance use.
And that was probably one of the things I was closed minded to during CPSS (training). I remember going to a rehab and the counselor not being an addict and I immediately had shut down. I didn't want to talk to her. She doesn’t know how I feel. (Participant #2)
Another participant suggested there was a difference between lived and learned knowledge. There was a sense that workers without lived experience could be receptive while those with lived experiences could be perceptive. For participants in substance use recovery, however, the day-to-day work could trigger reminders of their own recovery journeys. For this reason, participants noted that some peer workers return to use or leave their positions.
I think it may be a little more challenging. 'cause it's more … book learned, you know or taught in a training or but it's something very different to know it and genuinely practice it. … There have definitely been times where they'll hand me a nice slice of truth and reality and recovery all at the same time. That'll punch me right in my gut. (Participant #7)
Participants saw the benefits of both lived and learned knowledge being used in services to clients. Some reported that they struggled to understand the professional language of book knowledge but recognized that they contributed important understandings of client language.
Common Language
Participants clearly identified with their clients and noted their skills for connecting with this hard-to-reach population. They spoke a common language, they knew how to complete housing applications because they, themselves, had done so in the past. They understood barriers to being housed and the frustrations associated with engaging with services. Participants knew the community and the experiences intimately because they were part of it.
You know, if you've been out there on the streets for over a year too, you know, you've seen some things you've done some things. … I can’t plant the desire to change, I can only show what change looks like. They have somebody walking right alongside them. … I'm not coming from a place of judgment. I'm trying to come from a place of compassion and understanding. (Participant #5) That experience is going to inform how you talk to others, how you treat others. (Participant #1)
Participants spoke and understood clients’ language. Because they had “been there,” they came from a place of acceptance and compassion, knowing how important this was in their own experiences. The work was meaningful for them.
Personal Qualities, Skillset, and Confidence
These participants found meaning and purpose in their work. Some identified formerly being in jobs with little stimulation and no chance for growth or promotion. Nearly all the participants spoke of their strong work ethic. Because they had worked hard to overcome personal challenges, they were willing to work hard to maintain their growth. They expressed gratitude that the unique skills they possessed, due to their life experiences, could be used to benefit their communities.
So, learning along the way and making a whole bunch of errors and then figuring out how to do it, and you know, it all lined up the way it needed to and for whatever reason the skill set I have was unique for this job and it seemed to be a nice fit. (Participant #6)
Participants expressed confidence in their discernment. They recounted experiences with clients that required judgment, such as when to bend the rules, and how to identify the urgency of some moments for clients to capitalize on their readiness to change. Their instincts and lived experiences enabled them to recognize these moments as client opportunity or opportunism.
OK that’s a crisis … versus an emergency…. Gut instinct… having been a person who manipulated the system, you can tell. Nails done but not paying rent. Lack know-how to budget… Some of this can’t be taught… what works for me is that connection. I’m learning the “correct” language. A lot of it is instinctual. (Participant #5)
These participants that stepped forward to give back to their community, could channel their energy in a meaningful and purpose-filled way. This enhanced their own lives. They saw value in their unique skill set, could speak the language of those they served and had confidence in their ability to discern the needs of clients. This confidence may have come from their own lived experiences, or it may have come from their certification. We turn now to the role of training in participants’ effectiveness.
Participants explicitly discussed their CPSS training in our conversations about their effectiveness. State certification Footnote 2 was a requirement for their roles, to ensure competence to protect vulnerable populations. Training, for these participants, tapped into a willingness and ability to be vulnerable for growth. Participants made decisions about when, or if, to share their own stories with clients. Themes emerged related to hope, use of self in service to others, empathy, and finally the importance of both boundaries and connections.
Vulnerable for Growth
Most participants spoke of their professional growth and development. Growth was often coupled with a willingness to be vulnerable and to ask for help. They identified the learning curve required to be CPSS and were open to seeking and receiving assistance.
If I'm going to work with them and if I can't, then I'm not afraid to cry mercy and ask for some help with some capacity. (Participant #6)
Vulnerability was self-evident for these participants, who implicitly or explicitly linked this to their lived experiences. A sense of pride in their accomplishments was also evident. Participants spoke of desires for promotion and advancement which for almost all of them was unimaginable at some point in their lives. They were hopeful and sought to be a source of hope for their clients.
Many participants voiced gratitude that they had experienced others in their lives who had been further along on the path in some type of recovery (housing, substance use, mental health). They understood firsthand the benefits of peer support. Seeing this had given them some hope, and this was their chance to give that back in some way. Participants wanted clients to know that they would not give up on them and that housing stability was possible.
I went through a long-term place, and it was the women that were further along in the path that I've seen. They were happy and they were truly smiling, and it made all the world to me to see it working for other people. … I give a little hope… I guess I would go back to it being the hope, not ever wanting someone to feel like people had given up on them, or that there's no chance for them. (Participant #2)
Hearing participants speak of their lived experiences, their desire for training, and their willingness to be vulnerable in growth and development; it was clear they had the capacity for self-reflection. Their responses to the study’s questions were honest and introspective.
Use of Self in Service to Others
A significant part of peer support depends on self-disclosure. Participants were mindful that their role was to support clients rather than get their own needs met. They reported being especially effective at engaging clients and getting their buy-in for change. While they acknowledged that sharing their lived experiences and stories of homelessness with clients could be beneficial for themselves, they were clear that their attention needed to focus on the clients they served.
I think it's heavy handed when I'm just like hey, I'm you know I've been homeless before too. Like I said, I only pull that out when it when it feels right, like when it feels like it serves a purpose. When I feel like it will help them internalize some of the things I've said. And then from there you have your buy-in. Now … we're walking right beside each other on a mission and on a journey. (Participant #6)
Determining when to self-disclose and share their lived experiences required participants to effectively read the situation and their clients. This ability revealed participants’ empathy.
Participants demonstrated empathy for their clients. They recalled the challenges and barriers they had faced in seeking and retaining housing or in managing substance use or mental health. Participants acknowledged that training helped open their minds to the idea that there were many paths on a client’s journey. Especially for participants in substance use recovery, training helped to soften the edges on their individual opinions about what clients should be doing.
We just had the lady up there who just got housed yesterday. She hasn't even been in there 12 hours yet and she's really panicked. And you know, a lot of people don't understand that she may not be ready for that right now. She just may not be, you know. (Participant #7) 12-steps taught me absolutes. Peer support is more lenient, meeting you where you’re at versus this is the way you do it. Peer support is, “this is the experience I have, but let’s talk about you though.” (Participant #5)
Empathy came with a risk for overidentification. Participants could see themselves in the lives of clients and while that connection was the strength of their role, there was also the need for boundaries.
Connections and Boundaries
Themes of boundaries and connections were prevalent in interviews. The importance of connection showed up in the meaning participants derived from their work. It was evident in their willingness to be vulnerable and grow. Connections were foundational to participants’ empathy and engagement with those they served. The flipside of connections were boundaries. All participants recognized the importance of boundaries in their effectiveness. Some participants noted that they developed boundaries over time either because their instinct was to save clients and they realized this was neither possible nor their role; or because their boundaries were violated, and they needed to shore them up. Any worker in human services likely understands this. What may be unique to peer support is how to maintain boundaries in a role that depends on personal self-disclosures and identification with clients. An additional complicating factor surfaced when they knew clients from their previous lives.
It's a very fine line to walk… There's not even a whiff of impropriety. And you know, in the job interview they brought up hey, if you know you're going to get approached by people in the rooms about going to the front of the line. And I've had people. I mean my first meeting after getting the job I had someone come up to me and say hey, like I'm on the list. And I’m like, oh man, I know where you live, I can see your house from here, you're not homeless. (Participant #4)
It was evident in interviews with participants that their training contributed to their effectiveness. They presented themselves as lifelong learners. They believed in the power of peer support; some having experienced it themselves. They instilled hope. They showed a willingness to be vulnerable for growth. They demonstrated skills for self-reflection, empathy, and considering boundaries. Their focus was squarely on connection in human relationships and on the needs of their clients. All of this reflects the core competencies of peer support (SAMHSA, 2018 ). Completing the training and being certified did not guarantee longevity or success as a peer support worker. These participants talked about the significant role of the organization in their effectiveness.
Organization
Participants identified the importance of the organization in supporting their effectiveness with clients. Themes emerged related to the clarity of their role within the organization, the value of co-worker support, the promotion of self-care, and regular supervision. These elements of the organization were also highlighted as protective factors against turnover.
Participants spoke about the positive culture of the organization in terms of shared mission and values. They reportedly were valued for their contributions and supported in active engagement. Many participants framed this in terms of belonging, and a family atmosphere, which in this case, led to familiarity and encouragement. Circling back to the unique skill set possessed by these participants, they reported feeling valued (as some were handpicked from the community and asked to consider positions with the organization) and in turn, they valued being in a place where they could be themselves. Their role within the organization was clear, and they did not have to “pretend” to be something they were not.
When I first started here, I was enveloped … I didn't have to conform to a certain ideology that people have when others work for nonprofits. Every single person here is different… And through that uniqueness, it's just this crazy big family and we all offer something unique. (Participant #1)
Being able to show up as their authentic selves contributed to participant self-efficacy. This confidence and competence increased with the support of their co-workers.
Co-worker Support
The skills participants learned in their training such as collaboration, valuing relationships, and communication were reportedly as useful in their interactions with co-workers as they were with clients. Listening skills, empathy, affirmations, and tangible support were reportedly given and received and were viewed as essential ingredients in participants doing their jobs well. Co-worker support was seen as a significant protective factor against turnover.
My coworkers are by my side. People come, you know. I've helped them just as much as they've helped me. We have a very give and take relationship, and that's really across the board now. (Participant #6)
Given the nature of the work, worker turnover was a reality. Participants spoke of risks like burnout or return to use for those in substance use recovery. One participant framed turnover in terms of amateur versus mature recovery. There were some workers who were still journeying on the path towards being ready and able to help others. Not being ready to shoulder the responsibilities of peer support was identified as a barrier to effectiveness.
I did not know how to handle my emotions. Did not know how to be unselfish. I really had no idea what I was doing… And so, that's what I mean by amateur or not ready recovery. (Participant #7)
Organizational administration seemed to recognize the risks of burnout and turnover and offered formal and informal self-care strategies to employees.
Self-care and Supervision
Participants discussed ways the organization supported their self-care. These included informal measures like celebrating milestone anniversaries, encouraging mental health days, time-off to attend the funerals or celebrations of life of clients, on-site book clubs, and yoga, and formal measures like ongoing training and supervision.
(Pay) could be better but self-care perks you can’t put a dollar amount on. (Participant #5)
Participants engaged in regular supervision with a licensed social work supervisor. Several participants reportedly sought and earned promotions within the organization. One participant had the insight that several workers currently in leadership positions at the organization had lived experiences themselves. This offered hope that further advancement was possible. This begs the question whether workers who have “been there” had sought promotion and taken their training and recovery principles with them in a bottom-up movement, or whether there was a conscious top-down promotion of peer worker skillsets and shared values. Regardless, participants appreciated being part of the organization and experiencing the support they received from across the organization to do their jobs well.
(D)efinitely one of our strong suits is the bond that we all share… seeing it, it makes you want to do it, and that's the butterfly effect throughout the organization. …I could think of (the E.D.) doing it for random staff members, random staff members doing it across departments. So yeah, it's pretty ubiquitous. (Participant #4)
Participants identified the importance of the organization in supporting their effectiveness. Themes emerged related to having a clearly identified role, co-worker support, regular supervision, and organization-supported self-care. Participants saw these efforts as protective factors against burnout and turnover and necessary for promotion and advancement. There seemed to be a good fit between these participants with their lived experiences and unique skill sets, the competencies they learned through certification as peer support workers, and the supports found in the organization.
… if you can see it, you can be it.
Homelessness is a complex problem that requires innovative social solutions. One approach taken by the organization in this study was to employ CPSS in their workforce. The question posed in this study was not whether CPSS are effective in their role. Instead, this study explored what contributes to CPSS effectiveness when working with those experiencing homelessness. We asked the people doing the work to self-report on their effectiveness. We will address the limitations of this method in a moment; however, asking CPSS to reflect on the work they did, honored, and included their perspectives in a co-created understanding. Participants in this study saw their work as a way to give back to their community in a meaningful and purpose-filled way. They recognized the value of their unique skill set to reach those experiencing homelessness, they could speak the language of those they served, and had confidence in their ability to discern the needs of clients. These skills contributed to rapport and enabled them to actively engage with the population they served. This is important given how difficult it can be to reach those experiencing homelessness. Not all CPSS workers were ready to assume the role, and some needed time to grow into it. For participants in this study, they made a commitment to seek training and certification, and this clearly contributed to their perceived effectiveness as workers.
Training contributed to competence and effectiveness. Training, for these participants, tapped into a willingness to be vulnerable for growth. Themes related to hope, use of self in service to others, empathy, and finally, the importance of both boundaries and connections were identified. CPSS' attention was squarely on human relationships and on the needs of their clients. The stories shared by these participants were filled with examples of how they applied their training. Reflected in these stories were core competencies of peer support including engaging in collaborative and caring relationships; offering not simply support but personalized support; sharing lived experiences; providing information; managing crises; valuing communication; engaging in collegial collaboration and teamwork; and promoting growth and development (SAMHSA, 2018 ). The training and certification processes were important for shaping role expectations and preparing participants for the work. It is understood that in some settings, peer support workers may not be trained or certified. In this case they were, and often the organization paid for this certification. Participants viewed this as an investment in them, and several wanted the organization to get a return on their investment. Given the importance of training in these participants’ perceived effectiveness, it is recommended that national guidelines (SAMHSA, 2023 ) for peer workers be considered by hiring organizations to safeguard both this workforce and the vulnerable populations with whom they work.
Participants identified the importance of the organization in supporting their effectiveness. Themes related to role clarity, co-worker support along with regular supervision and self-care were identified. Finally, a note was made about the role of organizational leadership in creating and sustaining support for this workforce across the organization. Participants described organizational behaviors and norms in terms of being part of a family. Such norms have the potential to promote shared values, loyalty, and a sense of belonging; on the other hand, this loyalty sometimes leads to workers being exploited by employers for the good of the family (Goffee & Jones, 1998 ). Miler et al. ( 2020 ) cautioned that stigma, workplace experiences of discrimination, and compensation were areas of vulnerability for this workforce. The interview guide contained questions related to these areas. While participants stated that they would appreciate pay raises, stigma and discrimination were not emphasized in what they shared. While workers may have perceived themselves as belonging to an organizational family, another way to frame this is in terms of social innovation. Shier and Handy ( 2016 ) suggested that some direct-practice organizations are responding to community needs by creating an organizational culture oriented toward principles of social innovation. They provided a conceptual framework that included “staff engagement: with issues experienced by service users; with the structure or processes involved in decision making in promoting community engagement; with the initiatives undertaken by the organization; with activities that empower staff to act” (p. 127). Such engagement activities were reflected in the participants’ stories and in the way they were encouraged to be authentic and engage in the work of the organization. Miler et al. ( 2020 ) proposed that role description, support, training and development, and value were areas to be considered when embedding peer workers in organizations. The participants in this study confirmed this. Workers were empowered to use their skills across the organization and felt supported and valued in doing so. As the organization grows, it is unknown if innovation continues or if it moves through a life cycle to a formalization stage (Lester et al., 2003 ). At this moment, there seemed to be a good fit between these participants with their lived experiences and unique skill sets, their competencies, and the organization's culture.
Strengths and Limitations
This study contributes to our understanding of CPSS perceived effectiveness in a community-based organization serving those who experience homelessness. The approach was to assume effectiveness, but questions were posed that identified barriers to providing effective service. The study had some limitations. The first was a small sample size of self-selected participants who may have had more investment in the organization than those who chose to not participate. While we were welcomed into the organization and had key informants collaborating on the design of the study, participants were “hard to reach.” In a similar way that those experiencing homelessness are “hard-to-reach,” recruiting participants with lived experiences of homelessness proved difficult. The second limitation was that data came from self-reports which can invite bias. Chinman et al. ( 2016 ) noted that the peer workers in their review rated themselves higher on tasks than supervisors or clients. Finally, independent coding during the analysis phase sought to ensure intercoder reliability. Threats to validity in qualitative research can arise in description, interpretation, or theory (Maxwell, 1992 ). The debates and discussions that occurred between collaborators during the research process attempted to guard against these threats.
Implications for Policy, Practice, and Future Research
Given the small size of this study, no generalizations can be made for policy, practice, or research. Some insights are worth considering, however, related to the value of lived and learned knowledge coexisting in organizations serving those who experience homelessness. Studies (National Institute for Care and Excellence [NICE], 2022 ) are showing that peer workers can be an important part of multidisciplinary teams, delivering care or support and co-designing services. This is useful not only for the services and the people experiencing homelessness but also for the CPSS themselves. The literature (NICE, 2022) highlights the value of involving people with lived experience in the development of policies, procedures, and protocols. CPSS have skills for engaging hard-to-reach populations, given their empathy and commitment. It is important that this workforce not be exploited due to their willingness to go the extra mile for clients. Training and certification in preparation for the role seem useful to help channel CPSS experiences towards competence. Supervision is needed to ensure ongoing competency and advancement, and to provide an off-ramp as needed. We see this as a pilot study worthy of replication. Future research might ask the clients of CPSS directly about their effectiveness. As former clients themselves, some of the CPSS we spoke with confirmed the value of those who had “been there” in their own journeys out of homelessness.
Peer workers are variously called peer supporters, peer support specialists, peer providers, peer navigators, etc. Peer workers can apply for certification and undergo training. A national model for peer work offers guidance to promote quality for mental health certification, substance use certification, and family peer certification (Substance Abuse and Mental Health Services Administration, 2023 ).
Certification requirements vary by state. For a comparison, see Peer Recovery Center of Excellence ( 2023 )
Alcoholics Anonymous. (2002). Big book (4th edn.). Alcoholics Anonymous World Services.
Aubry, T., Klodawsky, F., & Coulombe, D. (2012). Comparing the housing trajectories of different classes within a diverse homeless population. American Journal of Community Psychology, 49 (1–2), 142–155. https://doi.org/10.1007/s10464-011-9444-z
Article PubMed Google Scholar
Barker, S. L., & Maguire, N. (2017). Experts by experience: Peer support and its use with the homeless. Community Mental Health, 53 , 598–612. https://doi.org/10.1007/s10597-017-0102-2
Article Google Scholar
Barker, S. L., Maguire, N., Bishop, F. L., & Stopa, L. L. (2019). Expert viewpoints of peer support for people experiencing homelessness: A Q sort study. Psychological Services , 16 (3), 402–414. https://doi.org/10.1037/ser0000258 .
Birt, L., Scott, S., Cavers, D., Campbell, C., & Walter, F. (2016). Member checking: A tool to enhance trustworthiness or merely a nod to validation? Qualitative Health Research, 26 (13), 1802–1811. https://doi.org/10.1177/1049732316654870
Boyatzis, R. E. (1998). Transforming qualitative information: Thematic analysis and code development . New York: Sage.
Google Scholar
Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3 (2), 77–101. https://doi.org/10.1191/1478088706qp063oa
Burr, V. (1995). An introduction to social constructionism . Routledge.
Book Google Scholar
Campbell, J. & Leaver, J. (2003). Emerging new practices in organized peer support: Report to the National Technical Assistance Center for State Mental Health Planning. Alexandria, VA: National Association of State Mental Health Program Directors (NASMHPD). https://mdsc.ca/documents/Publications/Emerging%20new%20practices%20in%20organized%20peer%20support.pdf
Chinman, M., McCarthy, S., Mitchell-Miland, C., Daniels, K., Youk, A., & Edelen, M. (2016). Early stages of development of a peer specialist fidelity measure. Psychiatric Rehabilitation Journal, 39 (3), 256–265. https://doi.org/10.1037/prj0000209
Article PubMed PubMed Central Google Scholar
Clay, S. (2005). About us: What we have in common. In S. Clay (Ed.), On our own together: Peer programs for people with mental illness (pp. 3–16). Vanderbilt University Press.
Chapter Google Scholar
Community Access Inc. (2020). Howie the harp: History . https://www.communityaccess.org/our-work/supported-education/howie-the-harp
Dennis, C. L. (2003). Peer support within a health care context: A concept analysis. International Journal of Nursing Studies, 40 , 321–332. https://doi.org/10.1016/s0020-7489(02)00092-5
Gergen, K. (1999). An invitation to social constructionism . Sage.
Goffee, R., & Jones, G. (1998). The character of a corporation. Journal of Business Strategy, 19 (6), 45–48. https://doi.org/10.1108/eb039972
Gutwinski, S., Schreiter, S., Deutscher, K., & Fazel, S. (2021). The prevalence of mental disorders among homeless people in high-income countries: An updated systematic review and meta-regression analysis. PLoS Medicine, 18 (8), e1003750. https://doi.org/10.1371/journal.pmed.1003750
Hayes, N. (1997). Theory-led thematic analysis: Social identification in small companies. In N. Haynes (Ed.), Doing qualitative analysis in psychology (pp. 45–47). Psychology Press.
Hwang, S. W., Gogosis, E., Chambers, C., Dunn, J. R., Hoch, J. S., & Aubry, T. (2011). Health status, quality of life, residential stability, substance use, and health care utilization among adults applying to a supportive housing program. Journal of Urban Health, 88 , 1076–1090. https://doi.org/10.1007/s11524-011-9592-3
Kelly, J. F., & Hoeppner, B. (2015). A biaxial formulation of the recovery construct. Addiction Research & Theory, 23 (1), 5–9. https://doi.org/10.3109/16066359.2014.930132
Kelly, J. F., & Yeterian, J. D. (2013). Mutual-help groups for alcohol and other substance use disorders. In B. S. McCrady & E. E. Epstein (Eds.), Addictions: A comprehensive guidebook (pp. 500–525). Oxford University Press.
Krakowsky, Y., Gofine, M., Brown, P., Danziger, J., & Knowles, H. (2013). Increasing access: A qualitative study of homelessness and palliative care in a major urban center. The American Journal of Hospice & Palliative Care, 30 (3), 268–270. https://doi.org/10.1177/1049909112448925
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal and coping . Springer.
Lester, D. L., Parnell, J. A., & Carraher, S. (2003). Organizational life cycle: A five-stage empirical scale. The International Journal of Organizational Analysis, 11 (4), 339–354. https://doi.org/10.1108/eb028979
Lived Experience Advisory Council. (2016). Nothing about us without us: Seven principles for leadership and inclusion of people with lived experience of homelessness . The Homeless Hub Press. www.homelesshub.ca/NothingAboutUsWithoutUs
Maxwell, J. A. (1992). Understanding and validity in qualitative research. Harvard Educational Review, 62 , 279–300. https://doi.org/10.17763/haer.62.3.8323320856251826
Mead, S., & McNeil, C. (2006). Peer support: What makes it unique? International Journal of Psychosocial Rehabilitation, 10 (2), 29–37.
Miler, J. A., Carver, H., Foster, R., & Parkes, T. (2020). Provision of peer support at the intersection of homelessness and problem substance use services: A systematic ‘state of the art’ review. BMC Public Health, 20 , 641. https://doi.org/10.1186/s12889-020-8407-4
Mowbray, C. T., Moxley, D. P., & Collins, M. E. (1998). Consumers as mental health providers: First person accounts of benefits and limitations. The Journal of Behavioural Health Services & Research, 25 (4), 397–411. https://doi.org/10.1007/BF02287510
Article CAS Google Scholar
National Institute for Health and Care Excellence (NICE): Centre for Homelessness Impact. (2022). Integrated health and social care for people experiencing homelessness. www.nice.org.uk/guidance/ng214
Peer Recovery Center of Excellence. (2023). Comparative analysis of state requirements for peer support specialist training and certification in the United States . https://peerrecoverynow.org/wp-content/uploads/2023-FEB-07-prcoe-comp-analysis.pdf
Raoult, D., Foucault, C., & Brouqui, P. (2001). Infections in the homeless. The Lancet Infectious Diseases, 1 (2), 77–84. https://doi.org/10.1016/S1473-3099(01)00062-7
Article CAS PubMed Google Scholar
Rubin, A., & Babbie, E. R. (2016). Research methods for social work . Cengage Learning.
Sanders, B., & Brown, B. (2015). ‘I was all on my own’: Experiences of loneliness and isolation amongst homeless people. Crisis. www.crisis.org.uk/data/files/publications/LonelinessReport_FINAL.pdf .
Shier, M. L., & Handy, F. (2016). Executive leadership and social innovation in direct-service nonprofits: Shaping the organizational culture to create social change. Journal of Progressive Human Services, 27 (2), 111–130.
de Sousa, T., Andrichik, A., Prestera, E., Rush, K., Tano, C., & Wheeler, M. (2023). The Annual Homeless Assessment Report (AHAR) to Congress: Part 1: Point-in-Time Estimates of Homelessness. The U.S. Department of Housing and Urban Development Office of Community Planning and Development. https://www.huduser.gov/portal/sites/default/files/pdf/2023-AHAR-Part-1.pdf
Stergiopoulos, V., Cusi, A., Bekele, T., Skosireva, A., Latimer, E., Schütz, C., Fernando, I., & Rourke, S. B. (2015). Neurocognitive impairment in a large sample of homeless adults with mental illness. Acta Psychiatrica Scandinavica, 131 (4), 268–356. https://doi.org/10.1111/acps.12391
Substance Abuse and Mental Health Services Administration: Bringing Recovery Supports to Scale Technical Assistance Center Strategy (BRSS TACS). (2018). Core competencies for peer workers in behavioral health services. https://www.samhsa.gov/sites/default/files/programs_campaigns/brss_tacs/core-competencies_508_12_13_18.pdf
Substance Abuse and Mental Health Services Administration. (2023). National model standards for peer support certification . Publication No. PEP23-10-01-001. Office of Recovery, Substance Abuse and Mental Health Services Administration. https://store.samhsa.gov/product/samhsas-national-model-standards-peer-support-certification/pep23-10-01-001
Wadhera, R. K., Khatana, S. A. M., Choi, E., Jiang, G., Shen, C., Yeh, R. W., & Joynt Maddox, K. E. (2020). Disparities in care and mortality among homeless adults hospitalized for cardiovascular conditions. JAMA Internal Medicine, 180 (3), 357–366. https://doi.org/10.1001/jamainternmed.2019.6010
White, W., & Cloud, W. (2008). Recovery capital: A primer for addictions professionals. Counselor, 9 (5), 22–27.
Yuen, M. S. K., & Fossey, E. M. (2003). Working in a community recreation program: A study of consumer-staff perspectives. Australian Occupational Therapy Journal, 50 , 54–63. https://doi.org/10.1046/j.1440-1630.2003.00306.x
Download references
Acknowledgements
We would like to thank our participants for sharing their experiences. We would also like to thank the organization for their collaboration on the project. We appreciate the feedback from reviewers that helped to strengthen the paper.
Open access funding provided by the Carolinas Consortium. No funding was received for conducting this study.
Author information
Authors and affiliations.
College of Social Work, University of South Carolina, Columbia, USA
Margriet de Zeeuw Wright & Candice Morgan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Margriet de Zeeuw Wright .
Ethics declarations
Competing interest.
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
de Zeeuw Wright, M., Morgan, C. Certified Peer Support in the Field of Homelessness: Stories Behind the Work. Community Ment Health J (2024). https://doi.org/10.1007/s10597-024-01315-1
Download citation
Received : 22 November 2023
Accepted : 21 June 2024
Published : 02 July 2024
DOI : https://doi.org/10.1007/s10597-024-01315-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Peer support
- Certified peer support
- Homelessness
- Thematic analysis
- Qualitative research
- Find a journal
- Publish with us
- Track your research

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Part 2 Lucy’s Story
2.4 Lucy case study 3: Mental illness diagnosis
Nicole Graham
Introduction to case study

Lucy has experienced the symptoms of mental illness during her lifespan; however, it was not until her early twenties that she was formally diagnosed with bipolar affective disorder. In the case study below, we explore the symptomology that Lucy experienced in the lead up to and post diagnosis. Lucy needs to consider her mental illness in relation to her work as a Registered Nurse and as she continues to move through the various stages of adulthood.
Learning Objectives
By the end of this case study, you should be able to:
- Identify and consider the symptoms of mental illness.
- Develop an understanding of contributing biopsychosocial stressors that may exacerbate the symptoms of mental illness as experienced by Lucy.
- Critically analyse the professional, ethical, and legal requirements and considerations for a registered health professional living with chronic illness.
Lucy’s small group of friends describe her as energetic and ‘a party person’. Although she sometimes disappears from her social group for periods of time, her friends are not aware that Lucy experiences periods of intense depression. At times Lucy cannot find the energy to get out of bed or even get dressed, sometimes for extended periods. As she gets older, these feelings and moods, as she describes them, get more intense. She loves feeling high on life. This is when she has an abundance of energy, is not worried about what people think of her and often does not need to sleep. These are the times when she feels she can achieve her goals. One of these times is when she decides to become a nurse. She excels at university, loves the intensity of study, practice and the party lifestyle. Emergency Nursing is her calling. The fast pace, the quick turnaround matches her endless energy. The fact that she struggles to stay focused for extended periods of time is something she needs to consider in her nursing career, to ensure it does not impact negatively on her care.
Unfortunately, Lucy has experienced challenges in her career. For example, her manager often comments on her mental illness after she had openly disclosed her diagnosis. It is challenging for her to hear her colleagues speak badly about a person who presents with mental illness. The stigma she hears directed at others challenges her. She is also very aware that it could be her presenting to the Emergency Department when she is unwell and in need of further support. Lucy is constantly worried that her colleagues will read her medical chart and think she is unsafe to practice.
While the symptoms that cause significant distress and disruption to her life began in her late teens, they intensified after she commenced antidepressant medication after the loss of her child. She subsequently ceased taking them due to side effects. These medications particularly impact on her ability to be creative and reduce her libido and energy. By the time she turns 18, she notices more frequent, intense mood swings, often accompanied by intense feelings of anxiety. During her high periods, Lucy enjoys the energy, the feeling of euphoria, the increased desire to exercise, her engagement with people, and being impulsive and creative. Lucas appreciates her increased libido. However, during these periods of high mood, Lucy also has impaired boundaries and is often flirtatious in her behaviour towards both friends and people she doesn’t know. She also increases her spending and has limited sleep. Lucas is often frustrated by this behaviour, leading to fights. On occasion Lucas slaps her and gets into fights with the people she is flirting with. These periods can last days and sometimes weeks, always followed by depressive episodes.
When she is in the low phases of her mood, Lucy experiences an overwhelming sense of hopelessness and emptiness. She is unable to find the energy to get out of bed, shower or take interest in simple daily activities. Lucas gets frustrated and dismisses Lucy’s statements of wanting to end her life as ‘attention seeking’. Lucy often expresses the desire to leave this world when she feels this way. When Lucas seeks support from the local general practitioner, nothing really gets resolved. The GP prescribes the medication; Lucy regains her desire to participate in life; then stops the medication due to side effects which extend to gastrointestinal upsets, on top of the decrease in libido and not feeling like herself. When Lucy is referred to a psychologist, she does not engage for more than one session, saying that she doesn’t like the person and feels they judge her lifestyle. When the psychologist attempts to explore a family history of mental illness, Lucy says no- one in her family has it and dismisses the concept.
The intense ups and downs are briefly interrupted with periods of lower intensity. During these times, Lucy feels worried about various aspects of her life and finds it challenging to let go of her anxious thoughts. There are times when Lucy has symptoms like racing heart, gastrointestinal update and shortness of breath. She spends a great deal of time wanting her life to be better. Her desire to move on from Lucas and to start a new life becomes more intense. Lucy is confident this is not a symptom of depression; it is just that she is unhappy in her relationship. Lucy starts to consider career options, feeling that not working affects her lifestyle, freedom and health. As she explores different options on the internet, Lucy comes across a chat room. Using the chat name ‘Foxy Lady 20’, she develops new friendships. She finds herself talking a lot with a man named Lincoln who lives on the Gold Coast.

After a brief but intense period talking with Lincoln online, Lucy abruptly decides to leave Lucas and her life in Bundaberg to move in with Lincoln. Lincoln, aged 26, 5 years older than Lucy, owns a modest home on the Gold Coast and has stable employment at the local casino. Their relationship progresses quickly and within a month Lincoln has proposed to Lucy. They plan to marry within 12 months.
Lucy is now happy with her life and feels stable. She decides to pursue a degree in nursing at the local university. Lucy enrols and makes many new friends, enjoying the intensity of study and a new social scene. Her fiancé Lincoln also enjoys the social aspects of their relationship. During university examination periods, Lucy experiences strong emotions. At the suggestion of an academic she respects, she makes an appointment with the university counselling service. After the first 3 appointments, Lucy self-discovers, with the support of her counsellor, that she might benefit from a specialist consultation with a psychiatrist. She comes to recognise that her symptoms are not within the normal range experienced by her peers. Lincoln is incredibly supportive and attends the appointments with Lucy, extending on the information she provides. Lucy reveals information about her grandmother, who was considered eccentric, and known for her periods of elevated mood and manic behaviour. The treating psychiatrist suggests Lucy may be living with bipolar affective disorder and encourages her to trial the medication lithium.
Lucy does not enjoy the side effects of decreased energy, nausea and feeling dazed and ceases taking the lithium during the university break period. This causes Lucy to again experience an intense elevation of her mood, accompanied by risk-taking behaviours. Lucy goes out frequently, nightclubbing and being flirtatious with her friends. She becomes aggressive towards a woman who confronts Lucy about her behaviour with her boyfriend in the nightclub. This is the first time Lucy exhibits this type of response, along with very pressured speech, pacing and an inability to calm herself. The police are called. They recommend Lucy gets assessed at the hospital after hearing from Lincoln that she has ceased her medication. Lucy is admitted for a brief period in the acute mental health ward. After stabilising and recommencing lithium, Lucy returns to the care of her psychiatrist in the community. The discharge notes report that Lucy had been previously diagnosed with bipolar disorder, may also be experiencing anxiety related symptoms, and have personality vulnerabilities.
Lucy is in the final year of her university studies when she has a professional experience placement in the emergency ward. Lucy really enjoys the fast pace, as well as the variety of complex presentations. Lucy feels it matches her energy and her desire for frequent change. After she completes her studies, Lucy applies and is successful in obtaining a position at the local hospital. Throughout her initial graduate year, Lucy balances life with a diagnosis of mental illness as well as a program of her own self-care. She finds the roster patterns in particular incredibly challenging and again becomes unwell. She goes through a period of depression and is unable to work. During this period, Lucy experiences an overwhelming sense of hopelessness and considers ending her life. Again, she requires a higher level of engagement from her treating team. Lucy agrees she is not fit to work during this time and has a period of leave without pay to recover. She has disclosed to her manager that she has been diagnosed with a mental illness and later discusses how shift work impacts her sleep and her overall mental wellbeing.
Over time, Lucy develops strategies to maintain wellness. However, she describes her relationship with the Nursing Unit Manager as strained, due to her inability to work night shift as her medical certificate shows. Lucy says she is often reminded of the impact that her set roster has on her colleagues. Lucy also feels unheard and dismissed when she raises workplace concerns, as her manager attributes her feelings to her mental health deteriorating. Lucy has a further period when her mental health deteriorates. However, this time it is due to a change in her medication.
As Lucy and Lincoln have a desire to have a child, Lucy was advised that she cease lithium in favour of lamotrigine, to reduce the risk of harm to the baby. Lucy ceases work during the period when her mental health deteriorates during the initial phase of changing medication. Lucy recommences lithium after she ceases breastfeeding their son at 4 months, with good effect and returns to work.
Case study questions
- Consider the symptoms that Lucy experiences and indicate whether they align with the suggested diagnosis.
- Identify the biopsychosocial contributing factors that could impact mental health and wellness.
- Review and identify the professional disclosure requirements of a Registered Nurse who lives with mental illness in your local area.
- Identify self-care strategies that Lucy or yourself as a health professional could implement to support mental health and wellbeing.
Thinking point
Sometimes people do not agree with a diagnosis of mental illness, which can be incorrectly labelled as ‘denial’ by health professionals. It is possible that the person is unable to perceive or be aware of their illness. This inability of insight is termed anosognosia (Amador, 2023). The cause of anosognosia in simple terms can be due to a non-functioning or impaired part of the frontal lobe of the brain, which may be caused by schizophrenia, bipolar disorder or other diseases such as dementia (Kirsch et al., 2021).
As healthcare workers will likely care for someone who is experiencing anosognosia, it is important to reflect on how you may work with someone who does not have the level of insight you would have hoped. Below is a roleplay activity whereby you can experience what it might be like to communicate with someone experiencing anosognosia. Reflect on your communication skills and identify strategies you could use to improve your therapeutic engagement.
Role play activity – Caring for a person who is experiencing anosognosia
Learning objectives.
- Demonstrate therapeutic engagement with someone who is experiencing mental illness
- Identify effective communication skills
- Reflect on challenges and identify professional learning needs
Resources required
- Suitable location to act out scene.
- One additional person to play the role of service user.
Two people assume role of either service user or clinician. If time permits, switch roles and repeat.
- Lucy has been commenced on lithium carbonate ER for treatment of her bipolar disorder.
- Lucy is attending the health care facility every week, as per the treating psychiatrist’s requests.
- The clinician’s role is to monitor whether Lucy is experiencing any side effects.
Role 1 – Clinician
- Clinician assumes role of health care worker in a health care setting of choice.
- Lucy has presented and your role is to ask Lucy whether she is experiencing any side effects and whether she has noticed any improvements in her mental state.
Role 2 – Lucy who lives with bipolar
- Lucy responds that she does not understand the need for the tablets. She also denies having a mental illness. Lucy says she will do what she is told, but does not think there is anything wrong with her. Lucy thinks she is just an energetic person who at times gets sad, which she describes as ‘perfectly normal.’ Lucy is not experiencing any negative side effects, but says she would like clarification about why the doctor has prescribed this medication.
Post role play debrief
Reflect and discuss your experiences, both as Lucy and as the clinician. Identify and discuss what was effective and what were the challenges.
Identify professional development opportunities and develop a learning plan to achieve your goals.
Additional resources that might be helpful
- Australian Prescriber: Lithium therapy and its interactions
- LEAP Institute: The impact of anosognosia and noncompliance (video)
Key information and links to other resources
Fisher (2022) suggests there are large numbers of health professionals who live with mental illness and recognise the practice value that comes with lived experience. However, the author also notes that as stigma is rife within the health care environment, disclosing mental illness can trigger an enhanced surveillance of the health professional’s practice or impede professional relationships (Fisher, 2022).
It is evident that the case studies derived from Lucy’s life story are complex and holistic care is essential. The biopsychosocial model was first conceptualised in 1977 by George Engel, who suggests it is not only a person’s medical condition, but also psychological and social factors that influence health and wellbeing (Engel,2012).
Below are examples of what you as a health professional could consider in each domain.
- Biological: Age, gender, physical health conditions, drug effects, genetic vulnerabilities
- Psychological: Emotions, thoughts, behaviours, coping skills, values
- Social: Living situation, social environment, work, relationships, finances, education
Developing skills through engaging in reflective practice and professional development is essential. Each person is unique, which requires you as the professional to adapt to their particular circumstances. The resources below can help you develop understanding of both regulatory requirements and the diagnosis Lucy is living with.
Organisations providing information relevant to this case study
- Rethink Mental Illness: Bipolar disorder
- Australian Health Practitioner Regulation Agency (AHPRA): Resources – helping you understand mandatory notifications
- Australian Health Practitioner Regulation Agency (AHPRA): Podcast – Mental health of nurses, midwives and the people they care for
- Black Dog Institute: TEN – The essential network for health professionals
- Borderline Personality Disorder Community
- National Institute of Mental Health (NIMH): Anxiety disorders
Case study 3 summary
In this case study, Lucy’s symptoms of mental illness emerge in her teenage years. Lucy describes periods of intense mood, both elevated and depressed, as well as potential anxiety-related responses. It is not until she develops a therapeutic relationship with a university school-based counsellor that she realises it might be beneficial to engage the services of a psychiatrist. After she is diagnosed with bipolar affective disorder she engages in treatment. Lucy shares her experience of both inpatient and community treatment as well as her professional practice requirements in the context of her mental illness.
Amador, X. (2023). Denial of anosognosia in schizophrenia. Schizophrenia Research , 252 , 242–243. https://doi.org/10.1016/j.schres.2023.01.009
Engel, G. (2012). The need for a new medical model: A challenge for biomedicine. Psychodynamic Psychiatry, 40 (3), 377–396. https://doi.org/10.1521/pdps.2012.40.3.377
Fisher, J. (2023). Who am I? The identity crisis of mental health professionals living with mental illness. Journal of Psychiatric and Mental Health Nursing . Advance online publication. https://doi.org/10.1111/jpm.12930
Kirsch, L. P., Mathys, C., Papadaki, C., Talelli, P., Friston, K., Moro, V., & Fotopoulou, A. (2021). Updating beliefs beyond the here-and-now: The counter-factual self in anosognosia for hemiplegia. Brain Communications , 3 (2), Article fcab098. https://doi.org/10.1093/braincomms/fcab098
Case Studies for Health, Research and Practice in Australia and New Zealand Copyright © 2023 by Nicole Graham is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book

Social Work’s Levone Lee presents at Alliance of Social Workers in Sports 10th Annual Symposium
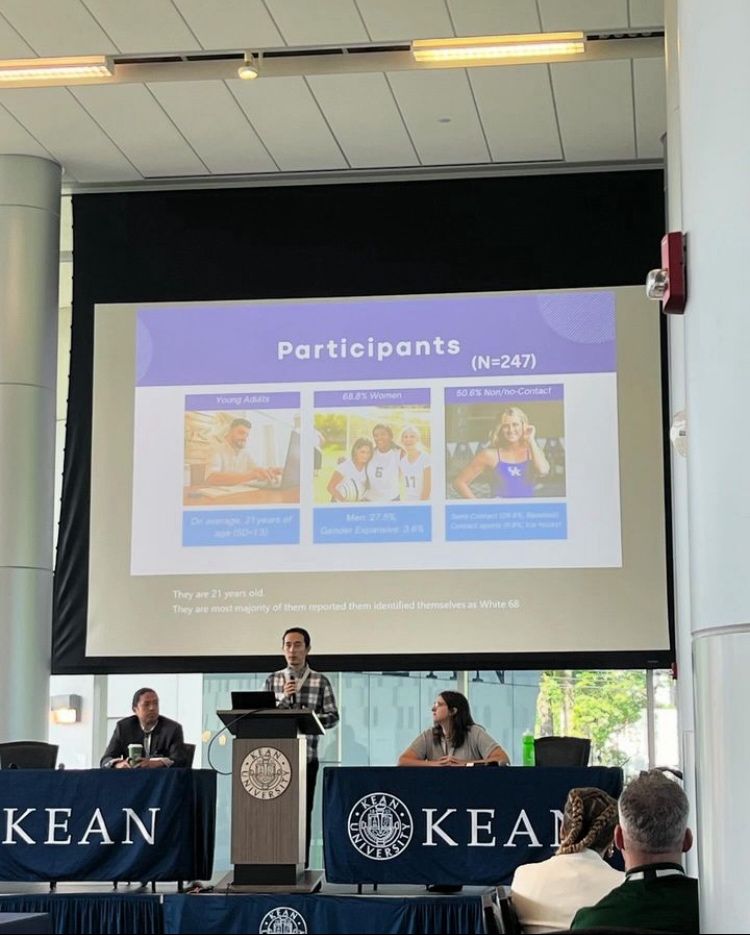
- Published July 2, 2024
- Centers & Labs , College News , Featured News , Student Spotlight
Share news:
UNION, N.J. – Earlier this summer, members of the University of Kentucky College of Social Work’s (CoSW) Sport Social Work Research Lab attended the Alliance of Social Workers in Sports (ASWIS) 10th Annual Symposium. Among those attendees was Ph.D. student Levone Lee, who presented his research at the symposium, marking Lee’s first solo presentation.
ASWIS has been at the forefront of integrating social work principles into sports, promoting the well-being of athletes and supporting professionals who work in the industry. Lee, a researcher in the Sport Social Work Research Lab, presented his study on examining collegiate student-athlete’s comfortability in discussing mental health.
The study focused on the preferences of student-athletes when talking about mental health issues to different social agents like their coaches, teammates, athletic trainers, and mental health professionals.
“In the past, athletes would typically go to their athletic trainers and their coaches more when discussing mental health,” Lee said. “In this study, we found that student-athletes now feel most comfortable discussing their mental health with their teammates and mental health professionals.”
This is due, in part, to new National Collegiate Athletic Association (NCAA) governance that was passed in 2022. Under the NCAA constitution adopted in January 2022 , each Division I member school must facilitate an environment that reinforces physical and mental health within athletics by ensuring access to appropriate resources and open engagement with respect to physical and mental health. Because of this higher exposure to mental health professionals, student-athletes feel more comfortable talking about mental health issues with them.
Lee credits the supportive environment within the CoSW and Sport Social Work Research Lab, as well as the mentorship of Dr. Tarkington Newman, director of the Sport Social Work Research Lab, with the opportunity and platform to pursue his research and build relationships with researchers in the sport social work field.
The intersection of sports and social work has been a passion for Lee, and a unique opportunity to help focus on an athletes’ well-being on and off the playing field.
“Not only are they athletes, but they are also human beings. Their mental health matters,” Lee said. “Their mental health not only affects their performances, but it affects their lifelong happiness. If there are mental health problems that aren’t addressed, especially for young athletes, that will change the trajectory of their life and affect their overall well-being.”
As the sport social work field continues to grow, Lee’s goal is to help others understand that sport social work is important because it’s not just focused on the performance of the athlete. Social workers can help get to the root of the presenting problem, such as generalized anxiety, and address it, which may lead to improved performance.
“We are looking to find positive approaches to address mental health issues within athletes because we do research in theory, but we also want to amplify the practical applications of our research,” Lee said. “We want our research to apply to athletes in the real-world.”
For over 85 years, the College of Social Work (CoSW) at the University of Kentucky has been a leader in education. Our mission is clear: Through rigorous research, excellence in instruction, and steadfast service, the CoSW works to improve the human condition. Always, in all ways.
As the state’s flagship university, our mission is actualized through our deeds. Our faculty are renowned academicians dedicated to fostering the development of high-quality practitioners and researchers. As a college, we promote community and individual well-being through translational research and scholarship, exemplary teaching, and vital community engagement. We are committed to the people and social institutions throughout Kentucky, the nation, and the world.
Recent Articles

The SWAA Alumni-Student Mentoring Program culminates its second year, advancing student futures

Meeting caregivers where they are: Kentucky Kinship Resource Center expands program

Social Work Faculty Advances Research on Digital Postpartum Support Systems
- Search Menu
Sign in through your institution
- Advance articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About The British Journal of Social Work
- About the British Association of Social Workers
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

- < Previous
Social Worker Working Conditions and Psychological Health: A Longitudinal Study
- Article contents
- Figures & tables
- Supplementary Data
J M Ravalier, R Allen, J McGowan, Social Worker Working Conditions and Psychological Health: A Longitudinal Study, The British Journal of Social Work , Volume 53, Issue 8, December 2023, Pages 3818–3837, https://doi.org/10.1093/bjsw/bcad144
- Permissions Icon Permissions
Good social work benefits the recipients of the social worker role, social workers themselves, their employing organisations and society more broadly. However, it is difficult to conduct consistently good social work when social workers have been shown to have chronically poor working conditions. This article, therefore, outlines UK social worker working conditions and well-being from 2022, as well as comparing these results to surveys conducted in 2017 and 2018. We, therefore, report a series of cross-sectional surveys, in addition to open-ended questions, to collect data from 533 respondents in 2022, and compare these to findings from similar surveys in previous years. Results demonstrate that working conditions improved slightly between 2018 and 2022, although these conditions are still very poor compared with other occupations. Qualitative analyses suggest that work-load, resources, lack of respect and lack of consistent and good quality reflective supervision are significant issues for respondents. As such, we argue that policy makers and employers need to provide greater support for social worker working conditions and well-being, and that this support would likely negate current high levels of turnover and sickness absence. Additionally, however, for the first time in these surveys, poor pay also emerged as an issue needing attention.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Short-term Access
To purchase short-term access, please sign in to your personal account above.
Don't already have a personal account? Register
| Month: | Total Views: |
|---|---|
| June 2023 | 186 |
| July 2023 | 53 |
| August 2023 | 25 |
| September 2023 | 24 |
| October 2023 | 43 |
| November 2023 | 37 |
| December 2023 | 49 |
| January 2024 | 55 |
| February 2024 | 39 |
| March 2024 | 72 |
| April 2024 | 40 |
| May 2024 | 49 |
| June 2024 | 15 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1468-263X
- Print ISSN 0045-3102
- Copyright © 2024 British Association of Social Workers
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- As Seen on TV
- Immigration
- Imperial County
- National-World
- Special Reports
- Yuma County
- Local Forecast
- Weather Authority Weather Alert Day
- Weather Authority Insider Blog
- Heat Awareness
- Weather Photos
- College Sports
- High School Sports
- Local Sports
- Noticias CNN
- Noticias de México
- Noticias de Yuma
- Noticias del Valle Imperial
- Programacion
- Telemundo en Vivo
- News 11 Newscast Livestream
- 13 On Your Side Newscast Livestream
- Livestream Special Coverage
- Must See Photo Galleries
- Weekly Health Tips
- Local Health
- The Good Stuff
- Cancer Resources
- Health Connections
- KYMA Careers
- Arizona Careers
- Meet the Team
- TV Listings
- Jobs/Internships
- Advertise With Us
- Closed Captioning
- Download Our Apps
- FCC Public Files
Yuma’s first mental health awareness symposium held this weekend
YUMA, Ariz. (KYMA, KECY) - The first annual Yuma County Mental Health Awareness Symposium took place Saturday afternoon.
The conference aimed to bring mental health providers, students, social workers and others together to share ideas and to learn more about the topic of mental health.
The conference was hosted by Ana Martinez-Celaya in collaboration with the Regional Center for Border Health.
"I wanted to get all the people who work in mental health together to increase mental health awareness," said Martinez-Celaya.
Guest speakers included Francisco Moreno, a Professor of Psychiatry at the University of Arizona and Melissa Waldrip, a licensed clinical social worker in Yuma.
The conference took place from 10:00am to 2:00pm at the Hilton Garden Inn Pivot Point in downtown Yuma.
Jump to comments ↓

Zackary Moran-Norris
Zackary Moran-Norris joined KYMA in July 2023 as a weekend reporter. Send him your story ideas to [email protected].
KYMA KECY is committed to providing a forum for civil and constructive conversation.
Please keep your comments respectful and relevant. You can review our Community Guidelines by clicking here
If you would like to share a story idea, please submit it here .
- Share full article
Advertisement
Supported by
Guest Essay
Surgeon General: Why I’m Calling for a Warning Label on Social Media Platforms

By Vivek H. Murthy
Dr. Murthy is the surgeon general.
One of the most important lessons I learned in medical school was that in an emergency, you don’t have the luxury to wait for perfect information. You assess the available facts, you use your best judgment, and you act quickly.
The mental health crisis among young people is an emergency — and social media has emerged as an important contributor. Adolescents who spend more than three hours a day on social media face double the risk of anxiety and depression symptoms, and the average daily use in this age group, as of the summer of 2023, was 4.8 hours . Additionally, nearly half of adolescents say social media makes them feel worse about their bodies.
It is time to require a surgeon general’s warning label on social media platforms, stating that social media is associated with significant mental health harms for adolescents. A surgeon general’s warning label, which requires congressional action, would regularly remind parents and adolescents that social media has not been proved safe. Evidence from tobacco studies show that warning labels can increase awareness and change behavior. When asked if a warning from the surgeon general would prompt them to limit or monitor their children’s social media use, 76 percent of people in one recent survey of Latino parents said yes.
To be clear, a warning label would not, on its own, make social media safe for young people. The advisory I issued a year ago about social media and young people’s mental health included specific recommendations for policymakers, platforms and the public to make social media safer for kids. Such measures, which already have strong bipartisan support, remain the priority.
Legislation from Congress should shield young people from online harassment, abuse and exploitation and from exposure to extreme violence and sexual content that too often appears in algorithm-driven feeds. The measures should prevent platforms from collecting sensitive data from children and should restrict the use of features like push notifications, autoplay and infinite scroll, which prey on developing brains and contribute to excessive use.
Additionally, companies must be required to share all of their data on health effects with independent scientists and the public — currently they do not — and allow independent safety audits. While the platforms claim they are making their products safer, Americans need more than words. We need proof.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

IMAGES
VIDEO
COMMENTS
Grand Challenges Faculty Development Institute: Eradicate Social Isolation CSWE, Dallas, TX, Oct. 19, 2017 1 Case Studies The following case studies were included to highlight different ways that social workers can assess and intervene with issues of social isolation. These cases are free to you to use, modify, and incorporate into your teaching.
2. Significant impairment in social, occupational, or other important areas of functioning. C. The stress-related disturbance does not meet the criteria for another mental disorder and is not merely an exacerbation of a preexisting mental disorder. D. The symptoms do not represent normal bereavement.
Her more recent episodes related to her parents' marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT). Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response.
The Social Worker explored Foley's thoughts on connecting Monty to mental health service as a support which could be provided at school. Foley reports feeling some anxiety with this as she does not know much about mental health services and fears Monty will simply be medicated "like a Zombie." The Social Worker assures Foley this
Case Study 2: Josef. Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently. This case study looks at the impact of caring for someone with a mental health problem and of being a young carer, in particular the ...
The social workers at the health centers were contacted by a mental health social worker and a case manager nurse working at an urban health center. Both professionals were responsible for providing the health and social care workers with information about the study. ... The social workers in our study considered that the most complex ...
The role of social workers in community mental health is embedded in the broader relationship of people to social institutions. Social work's concern with the quality of life is sanctioned by the social system and involves, of necessity, some commitment to the institutions that organize and govern secular life.
Have at least 2 years' full-time equivalent (FTE) post-qualifying social work experience* in a mental health setting within the last 5 years, totalling a minimum of 3,360 hours. The AASW recognises that full-time employment equates to 35 hours per week, for 48 weeks per year. Must be able to articulate your understanding and provide a case ...
Since 2005 the California Social Work Education Center (CalSWEC) Mental Health Program (MHP) has coor- dinated a stipend program through 17 schools of social work for almost 200 full-time 2nd-year MSW students. In return for their $18,500 stipend, students work for 1 year postgraduation in a county mental health agency or contract community ...
Social workers in the mental health and substance abuse fields will also be in high demand, with a 23% increase in employment expected by 2022. ... This is more than just about being a case ...
This case study portrays issues raised by social work students following a workshop with MHWLE as part of their graduate-level training. A workshop with MHWLE was designed for 24 social work graduate students during a mental health seminar. Following the workshop, a focus group was held.
There were still concerns and risk but holding and working with risk is fundamental to this role. A day in the life of a mental health social worker involves being aware of statutory action that can be taken but also, the need to develop and maintain trusting working relationships so that risk can be worked with and managed collaboratively with ...
July/August 2008 Issue. Therapist's Notebook: Case of Taylor Social Work Today Vol. 8 No. 4 P. 24. Social Work Today presents a case vignette with input from three social workers—a case presenter and two discussants who offer their insights on the presenting problem, background and family history, and the initial phase of treatment.. Case of Taylor
In a follow-up study of their 2019 Mental Health at Work Report, Mind Share Partners' 2021 Mental Health at Work Report, the authors offer a rare comparison of the state of mental health, stigma ...
Depressed; fearful and anxious; acculturation stress. M/67, Born in 1949, African American, Divorcee with one son (deceased). M/55, White, divorced with one son and one daughter. Met with drug cartel leader from Mexican for private interview about drug war policies. Paranoid that Mexican government blamed him for the drug cartel leader's capture.
Mental health social workers remain a minority within a medically dominated workforce (Evans et al., 2012) meaning that when teams and services are faced with managing crises in an increasingly austere environment it might become more difficult for social workers to 'argue the importance of … a person's right to accommodation, building ...
The LKSD school social work program is a long-standing mental health program. Staffed by itinerants and funded by the school district's general funds, the social work team provides each of LKSD's remote school communities with access to in-person supports and services at each tier of the MTSS framework. Community-based partnerships provide ...
Social work report: Background. Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke ...
One Canadian initiative, Gerstein Crisis Centre, stood out as a case study for mental health crisis support rooted in community and human rights. For more than 30 years, this community-based ...
More information: Ramona Alaggia et al, Troubled times: Canadian social workers' early adversities, mental health, and resilience during the COVID-19 pandemic, International Social Work (2023 ...
The following article presents a small-scale qualitative study in which the student learning experiences from service user and carer (SUAC) involvement in social work, mental health nursing and ...
158 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health. At Tracking Happiness, we're dedicated to helping others around the world overcome struggles of mental health. In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year.
Certified peer support specialists (CPSS) are used as a paraprofessional workforce to engage hard-to-reach populations, including people experiencing homelessness. Thematic analysis was used to explore with CPSS (N = 7) what contributed to their effectiveness when working with this population. Participants were recruited at a HUD lead organization in the southeastern United States. Open-ended ...
Lucy ceases work during the period when her mental health deteriorates during the initial phase of changing medication. Lucy recommences lithium after she ceases breastfeeding their son at 4 months, with good effect and returns to work. ... Living situation, social environment, work, relationships, ... In this case study, Lucy's symptoms of ...
Conclusion Community health workers (CHWs) in this study addressed social aspects of mental health, individually, and by engaging with wider structural factors. The micro-innovations of CHWs are dependent on non-linear elements, including local knowledge, time, and relationships.
Lee, a researcher in the Sport Social Work Research Lab, presented his study on examining collegiate student-athlete's comfortability in discussing mental health. The study focused on the preferences of student-athletes when talking about mental health issues to different social agents like their coaches, teammates, athletic trainers, and ...
The number of social workers leaving social work, and high numbers of vacancies/agency social workers, is perhaps not surprising. The Health and Safety Executive statistics (2021) demonstrate that the social work sector has the second highest levels of stress sickness absence in the UK, significantly higher than the UK average.
The conference aimed to bring mental health providers, students, social workers and others together to share ideas and to learn more about the topic of mental health.
The advisory I issued a year ago about social media and young people's mental health included specific recommendations for policymakers, platforms and the public to make social media safer for ...
Background: The COVID-19 pandemic has been linked to stress, anxiety, and depression among college students, with heightened distress tied to greater drinking for some individuals. Emerging research suggests that these associations may differ across race, but few studies use adequate samples to examine this, particularly among college students, an at-risk population for both heavy drinking and ...