Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State

Patient Case Presentation
Mr. E.A. is a 40-year-old black male who presented to his Primary Care Provider for a diabetes follow up on October 14th, 2019. The patient complains of a general constant headache that has lasted the past week, with no relieving factors. He also reports an unusual increase in fatigue and general muscle ache without any change in his daily routine. Patient also reports occasional numbness and tingling of face and arms. He is concerned that these symptoms could potentially be a result of his new diabetes medication that he began roughly a week ago. Patient states that he has not had any caffeine or smoked tobacco in the last thirty minutes. During assessment vital signs read BP 165/87, Temp 97.5 , RR 16, O 98%, and HR 86. E.A states he has not lost or gained any weight. After 10 mins, the vital signs were retaken BP 170/90, Temp 97.8, RR 15, O 99% and HR 82. Hg A1c 7.8%, three months prior Hg A1c was 8.0%. Glucose 180 mg/dL (fasting). FAST test done; negative for stroke. CT test, Chem 7 and CBC have been ordered.
Past medical history
Diagnosed with diabetes (type 2) at 32 years old
Overweight, BMI of 31
Had a cholecystomy at 38 years old
Diagnosed with dyslipidemia at 32 years old
Past family history
Mother alive, diagnosed diabetic at 42 years old
Father alive with Hypertension diagnosed at 55 years old
Brother alive and well at 45 years old
Sister alive and obese at 34 years old
Pertinent social history
Social drinker on occasion
Smokes a pack of cigarettes per day
Works full time as an IT technician and is in graduate school
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Graphical Abstracts and Tidbit
- Author Guidelines
- Submission Site
- Open Access
- About American Journal of Hypertension
- Editorial Board
- Board of Directors
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- AJH Summer School
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Clinical management and treatment decisions, hypertension in black americans, pharmacologic treatment of hypertension in black americans.
- < Previous
- Article contents
- Figures & tables
- Supplementary Data
Suzanne Oparil, Case study, American Journal of Hypertension , Volume 11, Issue S8, November 1998, Pages 192S–194S, https://doi.org/10.1016/S0895-7061(98)00195-2
- Permissions Icon Permissions
Ms. C is a 42-year-old black American woman with a 7-year history of hypertension first diagnosed during her last pregnancy. Her family history is positive for hypertension, with her mother dying at 56 years of age from hypertension-related cardiovascular disease (CVD). In addition, both her maternal and paternal grandparents had CVD.
At physician visit one, Ms. C presented with complaints of headache and general weakness. She reported that she has been taking many medications for her hypertension in the past, but stopped taking them because of the side effects. She could not recall the names of the medications. Currently she is taking 100 mg/day atenolol and 12.5 mg/day hydrochlorothiazide (HCTZ), which she admits to taking irregularly because “... they bother me, and I forget to renew my prescription.” Despite this antihypertensive regimen, her blood pressure remains elevated, ranging from 150 to 155/110 to 114 mm Hg. In addition, Ms. C admits that she has found it difficult to exercise, stop smoking, and change her eating habits. Findings from a complete history and physical assessment are unremarkable except for the presence of moderate obesity (5 ft 6 in., 150 lbs), minimal retinopathy, and a 25-year history of smoking approximately one pack of cigarettes per day. Initial laboratory data revealed serum sodium 138 mEq/L (135 to 147 mEq/L); potassium 3.4 mEq/L (3.5 to 5 mEq/L); blood urea nitrogen (BUN) 19 mg/dL (10 to 20 mg/dL); creatinine 0.9 mg/dL (0.35 to 0.93 mg/dL); calcium 9.8 mg/dL (8.8 to 10 mg/dL); total cholesterol 268 mg/dL (< 245 mg/dL); triglycerides 230 mg/dL (< 160 mg/dL); and fasting glucose 105 mg/dL (70 to 110 mg/dL). The patient refused a 24-h urine test.
Taking into account the past history of compliance irregularities and the need to take immediate action to lower this patient’s blood pressure, Ms. C’s pharmacologic regimen was changed to a trial of the angiotensin-converting enzyme (ACE) inhibitor enalapril, 5 mg/day; her HCTZ was discontinued. In addition, recommendations for smoking cessation, weight reduction, and diet modification were reviewed as recommended by the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). 1
After a 3-month trial of this treatment plan with escalation of the enalapril dose to 20 mg/day, the patient’s blood pressure remained uncontrolled. The patient’s medical status was reviewed, without notation of significant changes, and her antihypertensive therapy was modified. The ACE inhibitor was discontinued, and the patient was started on the angiotensin-II receptor blocker (ARB) losartan, 50 mg/day.
After 2 months of therapy with the ARB the patient experienced a modest, yet encouraging, reduction in blood pressure (140/100 mm Hg). Serum electrolyte laboratory values were within normal limits, and the physical assessment remained unchanged. The treatment plan was to continue the ARB and reevaluate the patient in 1 month. At that time, if blood pressure control remained marginal, low-dose HCTZ (12.5 mg/day) was to be added to the regimen.
Hypertension remains a significant health problem in the United States (US) despite recent advances in antihypertensive therapy. The role of hypertension as a risk factor for cardiovascular morbidity and mortality is well established. 2–7 The age-adjusted prevalence of hypertension in non-Hispanic black Americans is approximately 40% higher than in non-Hispanic whites. 8 Black Americans have an earlier onset of hypertension and greater incidence of stage 3 hypertension than whites, thereby raising the risk for hypertension-related target organ damage. 1 , 8 For example, hypertensive black Americans have a 320% greater incidence of hypertension-related end-stage renal disease (ESRD), 80% higher stroke mortality rate, and 50% higher CVD mortality rate, compared with that of the general population. 1 , 9 In addition, aging is associated with increases in the prevalence and severity of hypertension. 8
Research findings suggest that risk factors for coronary heart disease (CHD) and stroke, particularly the role of blood pressure, may be different for black American and white individuals. 10–12 Some studies indicate that effective treatment of hypertension in black Americans results in a decrease in the incidence of CVD to a level that is similar to that of nonblack American hypertensives. 13 , 14
Data also reveal differences between black American and white individuals in responsiveness to antihypertensive therapy. For instance, studies have shown that diuretics 15 , 16 and the calcium channel blocker diltiazem 16 , 17 are effective in lowering blood pressure in black American patients, whereas β-adrenergic receptor blockers and ACE inhibitors appear less effective. 15 , 16 In addition, recent studies indicate that ARB may also be effective in this patient population.
Angiotensin-II receptor blockers are a relatively new class of agents that are approved for the treatment of hypertension. Currently, four ARB have been approved by the US Food and Drug Administration (FDA): eprosartan, irbesartan, losartan, and valsartan. Recently, a 528-patient, 26-week study compared the efficacy of eprosartan (200 to 300 mg/twice daily) versus enalapril (5 to 20 mg/daily) in patients with essential hypertension (baseline sitting diastolic blood pressure [DBP] 95 to 114 mm Hg). After 3 to 5 weeks of placebo, patients were randomized to receive either eprosartan or enalapril. After 12 weeks of therapy within the titration phase, patients were supplemented with HCTZ as needed. In a prospectively defined subset analysis, black American patients in the eprosartan group (n = 21) achieved comparable reductions in DBP (−13.3 mm Hg with eprosartan; −12.4 mm Hg with enalapril) and greater reductions in systolic blood pressure (SBP) (−23.1 with eprosartan; −13.2 with enalapril), compared with black American patients in the enalapril group (n = 19) ( Fig. 1 ). 18 Additional trials enrolling more patients are clearly necessary, but this early experience with an ARB in black American patients is encouraging.
Efficacy of the angiotensin II receptor blocker eprosartan in black American with mild to moderate hypertension (baseline sitting DBP 95 to 114 mm Hg) in a 26-week study. Eprosartan, 200 to 300 mg twice daily (n = 21, solid bar), enalapril 5 to 20 mg daily (n = 19, diagonal bar). †10 of 21 eprosartan patients and seven of 19 enalapril patients also received HCTZ. Adapted from data in Levine: Subgroup analysis of black hypertensive patients treated with eprosartan or enalapril: results of a 26-week study, in Programs and abstracts from the 1st International Symposium on Angiotensin-II Antagonism, September 28–October 1, 1997, London, UK.
00195-2/2/m_ajh.192S.f1.jpeg?Expires=1719112609&Signature=cvpO6nOV9rurlE9jEgz~8EFmfBlZMmkLnBdQW5bvYyqRvHhRx7M38OoYB63QSNTFir6JYz-NrU5ZSru9g7i-CAAsuY54yxj-Yrc7f8yuJDwf93UghhaPxjy2wb3QxtUezKBjShLhYpqagSXXc2G7aXIXOsp2sEkER2F~jfZ5mgm21qedKErPw5KxlQcQgW4fHR-Bbt5ySRi0tC8Kof3AF4wK09OnHg-0TvgTvwNrmuynf-HpSdFI78JhfZZeDdQqSlub3Sq~-UfCarHvqHEF4u~j32IeHfNjZTfE-cKNgHzMG6va1JqkR1aAFiz0QkfU08WF9RjirZ4zVuMf9ajwTA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Approximately 30% of all deaths in hypertensive black American men and 20% of all deaths in hypertensive black American women are attributable to high blood pressure. Black Americans develop high blood pressure at an earlier age, and hypertension is more severe in every decade of life, compared with whites. As a result, black Americans have a 1.3 times greater rate of nonfatal stroke, a 1.8 times greater rate of fatal stroke, a 1.5 times greater rate of heart disease deaths, and a 5 times greater rate of ESRD when compared with whites. 19 Therefore, there is a need for aggressive antihypertensive treatment in this group. Newer, better tolerated antihypertensive drugs, which have the advantages of fewer adverse effects combined with greater antihypertensive efficacy, may be of great benefit to this patient population.
1. Joint National Committee : The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure . Arch Intern Med 1997 ; 24 157 : 2413 – 2446 .
Google Scholar
2. Veterans Administration Cooperative Study Group on Antihypertensive Agents : Effects of treatment on morbidity in hypertension: Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg . JAMA 1967 ; 202 : 116 – 122 .
3. Veterans Administration Cooperative Study Group on Antihypertensive Agents : Effects of treatment on morbidity in hypertension: II. Results in patients with diastolic blood pressures averaging 90 through 114 mm Hg . JAMA 1970 ; 213 : 1143 – 1152 .
4. Pooling Project Research Group : Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to the incidence of major coronary events: Final report of the pooling project . J Chronic Dis 1978 ; 31 : 201 – 306 .
5. Hypertension Detection and Follow-Up Program Cooperative Group : Five-year findings of the hypertension detection and follow-up program: I. Reduction in mortality of persons with high blood pressure, including mild hypertension . JAMA 1979 ; 242 : 2562 – 2577 .
6. Kannel WB , Dawber TR , McGee DL : Perspectives on systolic hypertension: The Framingham Study . Circulation 1980 ; 61 : 1179 – 1182 .
7. Hypertension Detection and Follow-Up Program Cooperative Group : The effect of treatment on mortality in “mild” hypertension: Results of the Hypertension Detection and Follow-Up Program . N Engl J Med 1982 ; 307 : 976 – 980 .
8. Burt VL , Whelton P , Roccella EJ et al. : Prevalence of hypertension in the US adult population: Results from the third National Health and Nutrition Examination Survey, 1988–1991 . Hypertension 1995 ; 25 : 305 – 313 .
9. Klag MJ , Whelton PK , Randall BL et al. : End-stage renal disease in African-American and white men: 16-year MRFIT findings . JAMA 1997 ; 277 : 1293 – 1298 .
10. Neaton JD , Kuller LH , Wentworth D et al. : Total and cardiovascular mortality in relation to cigarette smoking, serum cholesterol concentration, and diastolic blood pressure among black and white males followed up for five years . Am Heart J 1984 ; 3 : 759 – 769 .
11. Gillum RF , Grant CT : Coronary heart disease in black populations II: Risk factors . Heart J 1982 ; 104 : 852 – 864 .
12. M’Buyamba-Kabangu JR , Amery A , Lijnen P : Differences between black and white persons in blood pressure and related biological variables . J Hum Hypertens 1994 ; 8 : 163 – 170 .
13. Hypertension Detection and Follow-up Program Cooperative Group : Five-year findings of the Hypertension Detection and Follow-up Program: mortality by race-sex and blood pressure level: a further analysis . J Community Health 1984 ; 9 : 314 – 327 .
14. Ooi WL , Budner NS , Cohen H et al. : Impact of race on treatment response and cardiovascular disease among hypertensives . Hypertension 1989 ; 14 : 227 – 234 .
15. Weinberger MH : Racial differences in antihypertensive therapy: evidence and implications . Cardiovasc Drugs Ther 1990 ; 4 ( suppl 2 ): 379 – 392 .
16. Materson BJ , Reda DJ , Cushman WC et al. : Single-drug therapy for hypertension in men: A comparison of six antihypertensive agents with placebo . N Engl J Med 1993 ; 328 : 914 – 921 .
17. Materson BJ , Reda DJ , Cushman WC for the Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents : Department of Veterans Affairs single-drug therapy of hypertension study: Revised figures and new data . Am J Hypertens 1995 ; 8 : 189 – 192 .
18. Levine B : Subgroup analysis of black hypertensive patients treated with eprosartan or enalapril: results of a 26-week study , in Programs and abstracts from the first International Symposium on Angiotensin-II Antagonism , September 28 – October 1 , 1997 , London, UK .
19. American Heart Association: 1997 Heart and Stroke Statistical Update . American Heart Association , Dallas , 1997 .
- hypertension
- blood pressure
- african american
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1941-7225
- Copyright © 2024 American Journal of Hypertension, Ltd.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Newly diagnosed hypertension: case study
Affiliation.
- 1 Trainee Advanced Nurse Practitioner, East Belfast GP Federation, Northern Ireland.
- PMID: 37344134
- DOI: 10.12968/bjon.2023.32.12.556
The role of an advanced nurse practitioner encompasses the assessment, diagnosis and treatment of a range of conditions. This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as hypertension, but using a concordant approach in practice can optimise patient outcomes. This case study outlines a concordant approach to consultations in clinical practice which can enhance adherence in long-term conditions.
Keywords: Adherence; Advanced nurse practitioner; Case study; Concordance; Hypertension.
- Diagnosis, Differential
- Hypertension* / diagnosis
- Hypertension* / drug therapy
- Nurse Practitioners*
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs. Medicine (Baltimore). 2017; 96:(4) https://doi.org/10.1097/MD.0000000000005641
Armitage LC, Davidson S, Mahdi A Diagnosing hypertension in primary care: a retrospective cohort study to investigate the importance of night-time blood pressure assessment. Br J Gen Pract. 2023; 73:(726)e16-e23 https://doi.org/10.3399/BJGP.2022.0160
Barratt J. Developing clinical reasoning and effective communication skills in advanced practice. Nurs Stand. 2018; 34:(2)48-53 https://doi.org/10.7748/ns.2018.e11109
Bostock-Cox B. Nurse prescribing for the management of hypertension. British Journal of Cardiac Nursing. 2013; 8:(11)531-536
Bostock-Cox B. Hypertension – the present and the future for diagnosis. Independent Nurse. 2019; 2019:(1)20-24 https://doi.org/10.12968/indn.2019.1.20
Chakrabarti S. What's in a name? Compliance, adherence and concordance in chronic psychiatric disorders. World J Psychiatry. 2014; 4:(2)30-36 https://doi.org/10.5498/wjp.v4.i2.30
De Mauri A, Carrera D, Vidali M Compliance, adherence and concordance differently predict the improvement of uremic and microbial toxins in chronic kidney disease on low protein diet. Nutrients. 2022; 14:(3) https://doi.org/10.3390/nu14030487
Demosthenous N. Consultation skills: a personal reflection on history-taking and assessment in aesthetics. Journal of Aesthetic Nursing. 2017; 6:(9)460-464 https://doi.org/10.12968/joan.2017.6.9.460
Diamond-Fox S. Undertaking consultations and clinical assessments at advanced level. Br J Nurs. 2021; 30:(4)238-243 https://doi.org/10.12968/bjon.2021.30.4.238
Diamond-Fox S, Bone H. Advanced practice: critical thinking and clinical reasoning. Br J Nurs. 2021; 30:(9)526-532 https://doi.org/10.12968/bjon.2021.30.9.526
Donnelly M, Martin D. History taking and physical assessment in holistic palliative care. Br J Nurs. 2016; 25:(22)1250-1255 https://doi.org/10.12968/bjon.2016.25.22.1250
Fawcett J. Thoughts about meanings of compliance, adherence, and concordance. Nurs Sci Q. 2020; 33:(4)358-360 https://doi.org/10.1177/0894318420943136
Fisher NDL, Curfman G. Hypertension—a public health challenge of global proportions. JAMA. 2018; 320:(17)1757-1759 https://doi.org/10.1001/jama.2018.16760
Green S. Assessment and management of acute sore throat. Pract Nurs. 2015; 26:(10)480-486 https://doi.org/10.12968/pnur.2015.26.10.480
Harper C, Ajao A. Pendleton's consultation model: assessing a patient. Br J Community Nurs. 2010; 15:(1)38-43 https://doi.org/10.12968/bjcn.2010.15.1.45784
Hitchings A, Lonsdale D, Burrage D, Baker E. The Top 100 Drugs; Clinical Pharmacology and Practical Prescribing, 2nd edn. Scotland: Elsevier; 2019
Hobden A. Strategies to promote concordance within consultations. Br J Community Nurs. 2006; 11:(7)286-289 https://doi.org/10.12968/bjcn.2006.11.7.21443
Ingram S. Taking a comprehensive health history: learning through practice and reflection. Br J Nurs. 2017; 26:(18)1033-1037 https://doi.org/10.12968/bjon.2017.26.18.1033
James A, Holloway S. Application of concepts of concordance and health beliefs to individuals with pressure ulcers. British Journal of Healthcare Management. 2020; 26:(11)281-288 https://doi.org/10.12968/bjhc.2019.0104
Jamison J. Differential diagnosis for primary care. A handbook for health care practitioners, 2nd edn. China: Churchill Livingstone Elsevier; 2006
History and Physical Examination. 2021. https://patient.info/doctor/history-and-physical-examination (accessed 26 January 2023)
Kumar P, Clark M. Clinical Medicine, 9th edn. The Netherlands: Elsevier; 2017
Matthys J, Elwyn G, Van Nuland M Patients' ideas, concerns, and expectations (ICE) in general practice: impact on prescribing. Br J Gen Pract. 2009; 59:(558)29-36 https://doi.org/10.3399/bjgp09X394833
McKinnon J. The case for concordance: value and application in nursing practice. Br J Nurs. 2013; 22:(13)766-771 https://doi.org/10.12968/bjon.2013.22.13.766
McPhillips H, Wood AF, Harper-McDonald B. Conducting a consultation and clinical assessment of the skin for advanced clinical practitioners. Br J Nurs. 2021; 30:(21)1232-1236 https://doi.org/10.12968/bjon.2021.30.21.1232
Moulton L. The naked consultation; a practical guide to primary care consultation skills.Abingdon: Radcliffe Publishing; 2007
Medicine adherence; involving patients in decisions about prescribed medications and supporting adherence.England: NICE; 2009
National Institute for Health and Care Excellence. How do I control my blood pressure? Lifestyle options and choice of medicines patient decision aid. 2019. https://www.nice.org.uk/guidance/ng136/resources/patient-decision-aid-pdf-6899918221 (accessed 25 January 2023)
National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. NICE guideline NG136. 2022. https://www.nice.org.uk/guidance/ng136 (accessed 15 June 2023)
Nazarko L. Healthwise, Part 4. Hypertension: how to treat it and how to reduce its risks. Br J Healthc Assist. 2021; 15:(10)484-490 https://doi.org/10.12968/bjha.2021.15.10.484
Neighbour R. The inner consultation.London: Radcliffe Publishing Ltd; 1987
The Code. professional standards of practice and behaviour for nurses, midwives and nursing associates.London: NMC; 2018
Nuttall D, Rutt-Howard J. The textbook of non-medical prescribing, 2nd edn. Chichester: Wiley-Blackwell; 2016
O'Donovan K. The role of ACE inhibitors in cardiovascular disease. British Journal of Cardiac Nursing. 2018; 13:(12)600-608 https://doi.org/10.12968/bjca.2018.13.12.600
O'Donovan K. Angiotensin receptor blockers as an alternative to angiotensin converting enzyme inhibitors. British Journal of Cardiac Nursing. 2019; 14:(6)1-12 https://doi.org/10.12968/bjca.2019.0009
Porth CM. Essentials of Pathophysiology, 4th edn. Philadelphia: Wolters Kluwer; 2015
Rae B. Obedience to collaboration: compliance, adherence and concordance. Journal of Prescribing Practice. 2021; 3:(6)235-240 https://doi.org/10.12968/jprp.2021.3.6.235
Rostoft S, van den Bos F, Pedersen R, Hamaker ME. Shared decision-making in older patients with cancer - What does the patient want?. J Geriatr Oncol. 2021; 12:(3)339-342 https://doi.org/10.1016/j.jgo.2020.08.001
Schroeder K. The 10-minute clinical assessment, 2nd edn. Oxford: Wiley Blackwell; 2017
Thomas J, Monaghan T. The Oxford handbook of clinical examination and practical skills, 2nd edn. Oxford: Oxford University Press; 2014
Vincer K, Kaufman G. Balancing shared decision-making with ethical principles in optimising medicines. Nurse Prescribing. 2017; 15:(12)594-599 https://doi.org/10.12968/npre.2017.15.12.594
Waterfield J. ACE inhibitors: use, actions and prescribing rationale. Nurse Prescribing. 2008; 6:(3)110-114 https://doi.org/10.12968/npre.2008.6.3.28858
Weiss M. Concordance, 6th edn. In: Watson J, Cogan LS Poland: Elsevier; 2019
Williams H. An update on hypertension for nurse prescribers. Nurse Prescribing. 2013; 11:(2)70-75 https://doi.org/10.12968/npre.2013.11.2.70
Adherence to long-term therapies, evidence for action.Geneva: WHO; 2003
Young K, Franklin P, Franklin P. Effective consulting and historytaking skills for prescribing practice. Br J Nurs. 2009; 18:(17)1056-1061 https://doi.org/10.12968/bjon.2009.18.17.44160
Newly diagnosed hypertension: case study
Angela Brown
Trainee Advanced Nurse Practitioner, East Belfast GP Federation, Northern Ireland
View articles · Email Angela

The role of an advanced nurse practitioner encompasses the assessment, diagnosis and treatment of a range of conditions. This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as hypertension, but using a concordant approach in practice can optimise patient outcomes. This case study outlines a concordant approach to consultations in clinical practice which can enhance adherence in long-term conditions.
Hypertension is a worldwide problem with substantial consequences ( Fisher and Curfman, 2018 ). It is a progressive condition ( Jamison, 2006 ) requiring lifelong management with pharmacological treatments and lifestyle adjustments. However, adopting these lifestyle changes can be notoriously difficult to implement and sustain ( Fisher and Curfman, 2018 ) and non-adherence to chronic medication regimens is extremely common ( Abegaz et al, 2017 ). This is also recognised by the National Institute for Health and Care Excellence (NICE) (2009) which estimates that between 33.3% and 50% of medications are not taken as recommended. Abegaz et al (2017) furthered this by claiming 83.7% of people with uncontrolled hypertension do not take medications as prescribed. However, leaving hypertension untreated or uncontrolled is the single largest cause of cardiovascular disease ( Fisher and Curfman, 2018 ). Therefore, better adherence to medications is associated with better outcomes ( World Health Organization, 2003 ) in terms of reducing the financial burden associated with the disease process on the health service, improving outcomes for patients ( Chakrabarti, 2014 ) and increasing job satisfaction for professionals ( McKinnon, 2013 ). Therefore, at a time when growing numbers of patients are presenting with hypertension, health professionals must adopt a concordant approach from the initial consultation to optimise adherence.
Great emphasis is placed on optimising adherence to medications ( NICE, 2009 ), but the meaning of the term ‘adherence’ is not clear and it is sometimes used interchangeably with compliance and concordance ( De Mauri et al, 2022 ), although they are not synonyms. Compliance is an outdated term alluding to paternalism, obedience and passivity from the patient ( Rae, 2021 ), whereby the patient's behaviour must conform to the health professional's recommendations. Adherence is defined as ‘the extent to which a person's behaviour, taking medication, following a diet and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider’ ( Chakrabarti, 2014 ). This term is preferred over compliance as it is less paternalistic ( Rae, 2021 ), as the patient is included in the decision-making process and has agreed to the treatment plan. While it is not yet widely embraced or used in practice ( Fawcett, 2020 ), concordance is recognised, not as a behaviour ( Rae, 2021 ) but more an approach or method which focuses on the equal partnership between patient and professional ( McKinnon, 2013 ) and enables effective and agreed treatment plans.
NICE last reviewed its guidance on medication adherence in 2019 and did not replace adherence with concordance within this. This supports the theory that adherence is an outcome of good concordance and the two are not synonyms. NICE (2009) guidelines, which are still valid, show evidence of concordant principles to maximise adherence. Integrating the theoretical principles of concordance into this case study demonstrates how the trainee advanced nurse practitioner aimed to individualise patient-centred care and improve health outcomes through optimising adherence.
Patient introduction and assessment
Jane (a pseudonym has been used to protect the patient's anonymity; Nursing and Midwifery Council (NMC) 2018 ), is a 45-year-old woman who had been referred to the surgery following an attendance at an emergency department. Jane had been role-playing as a patient as part of a teaching session for health professionals when it was noted that her blood pressure was significantly elevated at 170/88 mmHg. She had no other symptoms. Following an initial assessment at the emergency department, Jane was advised to contact her GP surgery for review and follow up. Nazarko (2021) recognised that it is common for individuals with high blood pressure to be asymptomatic, contributing to this being referred to as the ‘silent killer’. Hypertension is generally only detected through opportunistic checking of blood pressure, as seen in Jane's case, which is why adults over the age of 40 years are offered a blood pressure check every 5 years ( Bostock-Cox, 2013 ).
Consultation
Jane presented for a consultation at the surgery. Green (2015) advocates using a model to provide a structured approach to consultations which ensures quality and safety, and improves time management. Young et al (2009) claimed that no single consultation model is perfect, and Diamond-Fox (2021) suggested that, with experience, professionals can combine models to optimise consultation outcomes. Therefore, to effectively consult with Jane and to adapt to her individual personality, different models were intertwined to provide better person-centred care.
The Calgary–Cambridge model is the only consultation model that places emphasis on initiating the session, despite it being recognised that if a consultation gets off to a bad start this can interfere throughout ( Young et al, 2009 ). Being prepared for the consultation is key. Before Jane's consultation, the environment was checked to minimise interruptions, ensuring privacy and dignity ( Green, 2015 ; NMC, 2018 ), the seating arrangements optimised to aid good body language and communication ( Diamond-Fox, 2021 ) and her records were viewed to give some background information to help set the scene and develop a rapport ( Young et al, 2009 ). Being adequately prepared builds the patient's trust and confidence in the professional ( Donnelly and Martin, 2016 ) but equally viewing patient information can lead to the professional forming preconceived ideas ( Donnelly and Martin, 2016 ). Therefore, care was taken by the trainee advanced nurse practitioner to remain open-minded.
During Jane's consultation, a thorough clinical history was taken ( Table 1 ). History taking is common to all consultation models and involves gathering important information ( Diamond-Fox, 2021 ). History-taking needs to be an effective ( Bostock-Cox, 2019 ), holistic process ( Harper and Ajao, 2010 ) in order to be thorough, safe ( Diamond-Fox, 2021 ) and aid in an accurate diagnosis. The key skill for taking history is listening and observing the patient ( Harper and Ajao, 2010 ). Sir William Osler said:‘listen to the patient as they are telling you the diagnosis’, but Knott and Tidy (2021) suggested that patients are barely given 20 seconds before being interrupted, after which they withdraw and do not offer any new information ( Demosthenous, 2017 ). Using this guidance, Jane was given the ‘golden minute’ allowing her to tell her ‘story’ without being interrupted ( Green, 2015 ). This not only showed respect ( Ingram, 2017 ) but interest in the patient and their concerns.
Once Jane shared her story, it was important for the trainee advanced nurse practitioner to guide the questioning ( Green 2015 ). This was achieved using a structured approach to take Jane's history, which optimised efficiency and effectiveness, and ensured that pertinent information was not omitted ( Young et al, 2009 ). Thomas and Monaghan (2014) set out clear headings for this purpose. These included:
- The presenting complaint
- Past medical history
- Drug history
- Social history
- Family history.
McPhillips et al (2021) also emphasised a need for a systemic enquiry of the other body systems to ensure nothing is missed. From taking this history it was discovered that Jane had been feeling well with no associated symptoms or red flags. A blood pressure reading showed that her blood pressure was elevated. Jane had no past medical history or allergies. She was not taking any medications, including prescribed, over the counter, herbal or recreational. Jane confirmed that she did not drink alcohol or smoke. There was no family history to note, which is important to clarify as a genetic link to hypertension could account for 30–50% of cases ( Nazarko, 2021 ). The information gathered was summarised back to Jane, showing good practice ( McPhillips et al, 2021 ), and Jane was able to clarify salient or missing points. Green (2015) suggested that optimising the patient's involvement in this way in the consultation makes her feel listened to which enhances patient satisfaction, develops a therapeutic relationship and demonstrates concordance.
During history taking it is important to explore the patient's ideas, concerns and expectations. Moulton (2007) refers to these as the ‘holy trinity’ and central to upholding person-centredness ( Matthys et al, 2009 ). Giving Jane time to discuss her ideas, concerns and expectations allowed the trainee advanced nurse practitioner to understand that she was concerned about her risk of a stroke and heart attack, and worried about the implications of hypertension on her already stressful job. Using ideas, concerns and expectations helped to understand Jane's experience, attitudes and perceptions, which ultimately will impact on her health behaviours and whether engagement in treatment options is likely ( James and Holloway, 2020 ). Establishing Jane's views demonstrated that she was eager to engage and manage her blood pressure more effectively.
Vincer and Kaufman (2017) demonstrated, through their case study, that a failure to ask their patient's viewpoint at the initial consultation meant a delay in engagement with treatment. They recognised that this delay could have been avoided with the use of additional strategies had ideas, concerns and expectations been implemented. Failure to implement ideas, concerns and expectations is also associated with reattendance or the patient seeking second opinions ( Green, 2015 ) but more positively, when ideas, concerns and expectations is implemented, it can reduce the number of prescriptions while sustaining patient satisfaction ( Matthys et al, 2009 ).
Physical examination
Once a comprehensive history was taken, a physical examination was undertaken to supplement this information ( Nuttall and Rutt-Howard, 2016 ). A physical examination of all the body systems is not required ( Diamond-Fox, 2021 ) as this would be extremely time consuming, but the trainee advanced nurse practitioner needed to carefully select which systems to examine and use good examination technique to yield a correct diagnosis ( Knott and Tidy, 2021 ). With informed consent, clinical observations were recorded along with a full cardiovascular examination. The only abnormality discovered was Jane's blood pressure which was 164/90 mmHg, which could suggest stage 2 hypertension ( NICE, 2019 ; 2022 ). However, it is the trainee advanced nurse practitioner's role to use a hypothetico-deductive approach to arrive at a diagnosis. This requires synthesising all the information from the history taking and physical examination to formulate differential diagnoses ( Green, 2015 ) from which to confirm or refute before arriving at a final diagnosis ( Barratt, 2018 ).
Differential diagnosis
Hypertension can be triggered by secondary causes such as certain drugs (non-steroidal anti-inflammatory drugs, steroids, decongestants, sodium-containing medications or combined oral contraception), foods (liquorice, alcohol or caffeine; Jamison, 2006 ), physiological response (pain, anxiety or stress) or pre-eclampsia ( Jamison, 2006 ; Schroeder, 2017 ). However, Jane had clarified that these were not contributing factors. Other potential differentials which could not be ruled out were the white-coat syndrome, renal disease or hyperthyroidism ( Schroeder, 2017 ). Further tests were required, which included bloods, urine albumin creatinine ratio, electrocardiogram and home blood pressure monitoring, to ensure a correct diagnosis and identify any target organ damage.
Joint decision making
At this point, the trainee advanced nurse practitioner needed to share their knowledge in a meaningful way to enable the patient to participate with and be involved in making decisions about their care ( Rostoft et al, 2021 ). Not all patients wish to be involved in decision making ( Hobden, 2006 ) and this must be respected ( NMC, 2018 ). However, engaging patients in partnership working improves health outcomes ( McKinnon, 2013 ). Explaining the options available requires skill so as not to make the professional seem incompetent and to ensure the patient continues to feel safe ( Rostoft et al, 2021 ).
Information supported by the NICE guidelines was shared with Jane. These guidelines advocated that in order to confirm a diagnosis of hypertension, a clinic blood pressure reading of 140/90 mmHg or higher was required, with either an ambulatory or home blood pressure monitoring result of 135/85 mmHg or higher ( NICE, 2019 ; 2022 ). However, the results from a new retrospective study suggested that the use of home blood pressure monitoring is failing to detect ‘non-dippers’ or ‘reverse dippers’ ( Armitage et al, 2023 ). These are patients whose blood pressure fails to fall during their nighttime sleep. This places them at greater risk of cardiovascular disease and misdiagnosis if home blood pressure monitors are used, but ambulatory blood pressure monitors are less frequently used in primary care and therefore home blood pressure monitors appear to be the new norm ( Armitage et al, 2023 ).
Having discussed this with Jane she was keen to engage with home blood pressure monitoring in order to confirm the potential diagnosis, as starting a medication without a true diagnosis of hypertension could potentially cause harm ( Jamison, 2006 ). An accurate blood pressure measurement is needed to prevent misdiagnosis and unnecessary therapy ( Jamison, 2006 ) and this is dependent on reliable and calibrated equipment and competency in performing the task ( Bostock-Cox, 2013 ). Therefore, Jane was given education and training to ensure the validity and reliability of her blood pressure readings.
For Jane, this consultation was the ideal time to offer health promotion advice ( Green, 2015 ) as she was particularly worried about her elevated blood pressure. Offering health promotion advice is a way of caring, showing support and empowerment ( Ingram, 2017 ). Therefore, Jane was provided with information on a healthy diet, the reduction of salt intake, weight loss, exercise and continuing to abstain from smoking and alcohol ( Williams, 2013 ). These were all modifiable factors which Jane could implement straight away to reduce her blood pressure.
Safety netting
The final stage and bringing this consultation to a close was based on the fourth stage of Neighbour's (1987) model, which is safety netting. Safety netting identifies appropriate follow up and gives details to the patient on what to do if their condition changes ( Weiss, 2019 ). It is important that the patient knows who to contact and when ( Young et al, 2009 ). Therefore, Jane was advised that, should she develop chest pains, shortness of breath, peripheral oedema, reduced urinary output, headaches, visual disturbances or retinal haemorrhages ( Schroeder, 2017 ), she should present immediately to the emergency department, otherwise she would be reviewed in the surgery in 1 week.
Jane was followed up in a second consultation 1 week later with her home blood pressure readings. The average reading from the previous 6 days was calculated ( Bostock-Cox, 2013 ) and Jane's home blood pressure reading was 158/82 mmHg. This reading ruled out white-coat syndrome as Jane's blood pressure remained elevated outside clinic conditions (white-coat syndrome is defined as a difference of more than 20/10 mmHg between clinic blood pressure readings and the average home blood pressure reading; NICE, 2019 ; 2022 ). Subsequently, Jane was diagnosed with stage 2 essential (or primary) hypertension. Stage 2 is defined as a clinic blood pressure of 160/100 mmHg or higher or a home blood pressure of 150/95 mmHg or higher ( NICE, 2019 ; 2022 ).
A diagnosis of hypertension can be difficult for patients as they obtain a ‘sick label’ despite feeling well ( Jamison, 2006 ). This is recognised as a deterrent for their motivation to initiate drug treatment and lifestyle changes ( Williams, 2013 ), presenting a greater challenge to health professionals, which can be addressed through concordance strategies. However, having taken Jane's bloods, electrocardiogram and urine albumin:creatinine ratio in the first consultation, it was evident that there was no target organ damage and her Qrisk3 score was calculated as 3.4%. These results provided reassurance for Jane, but she was keen to engage and prevent any potential complications.
Agreeing treatment
Concordance is only truly practised when the patient's perspectives are valued, shared and used to inform planning ( McKinnon, 2013 ). The trainee advanced nurse practitioner now needed to use the information gained from the consultations to formulate a co-produced and meaningful treatment plan based on the best available evidence ( Diamond-Fox and Bone, 2021 ). Jane understood the risk associated with high blood pressure and was keen to begin medication as soon as possible. NICE guidelines ( 2019 ; 2022 ) advocate the use of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin-receptor blockers in patients under 55 years of age and not of Black African or African-Caribbean origin. However, ACE inhibitors seem to be used as the first-line treatment for hypertensive patients under the age of 55 years ( O'Donovan, 2019 ).
ACE inhibitors directly affect the renin–angiotensin-aldosterone system which plays a central role in regulation of blood pressure ( Porth, 2015 ). Renin is secreted by the juxtaglomerular cells, in the kidneys' nephrons, when there is a decrease in renal perfusion and stimulation of the sympathetic nervous system ( O'Donovan, 2018 ). Renin then combines with angiotensinogen, a circulating plasma globulin from the liver, to form angiotensin I ( Kumar and Clark, 2017 ). Angiotensin I is inactive but, through ACE, an enzyme present in the endothelium of the lungs, it is transformed into angiotensin II ( Kumar and Clark, 2017 ). Angiotensin II is a vasoconstrictor which increases vascular resistance and in turn blood pressure ( Porth, 2015 ) while also stimulating the adrenal gland to produce aldosterone. Aldosterone reduces sodium excretion in the kidneys, thus increasing water reabsorption and therefore blood volume ( Porth, 2015 ). Using an ACE inhibitor prevents angiotensin II formation, which prevents vasoconstriction and stops reabsorption of sodium and water, thus reducing blood pressure.
When any new medication is being considered, providing education is key. This must include what the medication is for, the importance of taking it, any contraindications or interactions with the current medications being taken by the patient and the potential risk of adverse effects ( O'Donovan, 2018 ). Sharing this information with Jane allowed her to weigh up the pros and cons and make an informed choice leading to the creation of an individualised treatment plan.
Jamison (2006) placed great emphasis on sharing information about adverse effects, because patients with hypertension feel well before commencing medications, but taking medication has the potential to cause side effects which can affect adherence. Therefore, the range of side effects were discussed with Jane. These include a persistent, dry non-productive cough, hypotension, hypersensitivity, angioedema and renal impairment with hyperkalaemia ( Hitchings et al, 2019 ). ACE inhibitors have a range of adverse effects and most resolve when treatment is stopped ( Waterfield, 2008 ).
Following discussion with Jane, she proceeded with taking an ACE inhibitor and was encouraged to report any side effects in order to find another more suitable medication and to prevent her hypertension from going untreated. This information was provided verbally and written which is seen as good practice ( Green, 2015 ). Jane was followed up with fortnightly blood pressure recordings and urea and electrolyte checks and her dose of ramipril was increased fortnightly until her blood pressure was under 140/90 mmHg ( NICE, 2019 ; 2022 ).
Conclusions
Adherence to medications can be difficult to establish and maintain, especially for patients with long-term conditions. This can be particularly challenging for patients with hypertension because they are generally asymptomatic, yet acquire a sick label and start lifelong medication and lifestyle adjustments to prevent complications. Through adopting a concordant approach in practice, the outcome of adherence can be increased. This case study demonstrates how concordant strategies were implemented throughout the consultation to create a therapeutic patient–professional relationship. This optimised the creation of an individualised treatment plan which the patient engaged with and adhered to.
- Hypertension is a growing worldwide problem
- Appropriate clinical assessment, diagnosis and management is key to prevent misdiagnosis
- Long-term conditions are associated with high levels of non-adherence to treatments
- Adopting a concordance approach to practice optimises adherence and promotes positive patient outcomes
CPD reflective questions
- How has this article developed your assessment, diagnosis or management of patients presenting with a high blood pressure?
- What measures can you implement in your practice to enhance a concordant approach?
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 6: 10 Real Cases on Hypertensive Emergency and Pericardial Disease: Diagnosis, Management, and Follow-Up
Niel Shah; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Clinical Symptoms
- Diagnostic Evaluation
- Full Chapter
- Supplementary Content
Case 1: Management of Hypertensive Encephalopathy
A 45-year-old man with a 2-month history of progressive headache presented to the emergency department with nausea, vomiting, visual disturbance, and confusion for 1 day. He denied fever, weakness, numbness, shortness of breath, and flulike symptoms. He had significant medical history of hypertension and was on a β-blocker in the past, but a year ago, he stopped taking medication due to an unspecified reason. The patient denied any history of tobacco smoking, alcoholism, and recreational drug use. The patient had a significant family history of hypertension in both his father and mother. Physical examination was unremarkable, and at the time of triage, his blood pressure (BP) was noted as 195/123 mm Hg, equal in both arms. The patient was promptly started on intravenous labetalol with the goal to reduce BP by 15% to 20% in the first hour. The BP was rechecked after an hour of starting labetalol and was 165/100 mm Hg. MRI of the brain was performed in the emergency department and demonstrated multiple scattered areas of increased signal intensity on T2-weighted and fluid-attenuated inversion recovery (FLAIR) images in both the occipital and posterior parietal lobes. There were also similar lesions in both hemispheres of the cerebellum (especially the cerebellar white matter on the left) as well as in the medulla oblongata. The lesions were not associated with mass effect, and after contrast administration, there was no evidence of abnormal enhancement. In the emergency department, his BP decreased to 160/95 mm Hg, and he was transitioned from drip to oral medications and transferred to the telemetry floor. How would you manage this case?
The patient initially presented with headache, nausea, vomiting, blurred vision, and confusion. The patient’s BP was found to be 195/123 mm Hg, and MRI of the brain demonstrated scattered lesions with increased intensity in the occipital and posterior parietal lobes, as well as in cerebellum and medulla oblongata. The clinical presentation, elevated BP, and brain MRI findings were suggestive of hypertensive emergency, more specifically hypertensive encephalopathy. These MRI changes can be seen particularly in posterior reversible encephalopathy syndrome (PRES), a sequela of hypertensive encephalopathy. BP was initially controlled by labetalol, and after satisfactory control of BP, the patient was switched to oral antihypertensive medications.
Hypertensive emergency refers to the elevation of systolic BP >180 mm Hg and/or diastolic BP >120 mm Hg that is associated with end-organ damage; however, in some conditions such as pregnancy, more modest BP elevation can constitute an emergency. An equal degree of hypertension but without end-organ damage constitutes a hypertensive urgency, the treatment of which requires gradual BP reduction over several hours. Patients with hypertensive emergency require rapid, tightly controlled reductions in BP that avoid overcorrection. Management typically occurs in an intensive care setting with continuous arterial BP monitoring and continuous infusion of antihypertensive agents.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

- Previous Article
- Next Article
Presentation
Clinical pearls, case study: treating hypertension in patients with diabetes.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Evan M. Benjamin; Case Study: Treating Hypertension in Patients With Diabetes. Clin Diabetes 1 July 2004; 22 (3): 137–138. https://doi.org/10.2337/diaclin.22.3.137
Download citation file:
- Ris (Zotero)
- Reference Manager
L.N. is a 49-year-old white woman with a history of type 2 diabetes,obesity, hypertension, and migraine headaches. The patient was diagnosed with type 2 diabetes 9 years ago when she presented with mild polyuria and polydipsia. L.N. is 5′4″ and has always been on the large side,with her weight fluctuating between 165 and 185 lb.
Initial treatment for her diabetes consisted of an oral sulfonylurea with the rapid addition of metformin. Her diabetes has been under fair control with a most recent hemoglobin A 1c of 7.4%.
Hypertension was diagnosed 5 years ago when blood pressure (BP) measured in the office was noted to be consistently elevated in the range of 160/90 mmHg on three occasions. L.N. was initially treated with lisinopril, starting at 10 mg daily and increasing to 20 mg daily, yet her BP control has fluctuated.
One year ago, microalbuminuria was detected on an annual urine screen, with 1,943 mg/dl of microalbumin identified on a spot urine sample. L.N. comes into the office today for her usual follow-up visit for diabetes. Physical examination reveals an obese woman with a BP of 154/86 mmHg and a pulse of 78 bpm.
What are the effects of controlling BP in people with diabetes?
What is the target BP for patients with diabetes and hypertension?
Which antihypertensive agents are recommended for patients with diabetes?
Diabetes mellitus is a major risk factor for cardiovascular disease (CVD). Approximately two-thirds of people with diabetes die from complications of CVD. Nearly half of middle-aged people with diabetes have evidence of coronary artery disease (CAD), compared with only one-fourth of people without diabetes in similar populations.
Patients with diabetes are prone to a number of cardiovascular risk factors beyond hyperglycemia. These risk factors, including hypertension,dyslipidemia, and a sedentary lifestyle, are particularly prevalent among patients with diabetes. To reduce the mortality and morbidity from CVD among patients with diabetes, aggressive treatment of glycemic control as well as other cardiovascular risk factors must be initiated.
Studies that have compared antihypertensive treatment in patients with diabetes versus placebo have shown reduced cardiovascular events. The United Kingdom Prospective Diabetes Study (UKPDS), which followed patients with diabetes for an average of 8.5 years, found that patients with tight BP control (< 150/< 85 mmHg) versus less tight control (< 180/< 105 mmHg) had lower rates of myocardial infarction (MI), stroke, and peripheral vascular events. In the UKPDS, each 10-mmHg decrease in mean systolic BP was associated with a 12% reduction in risk for any complication related to diabetes, a 15% reduction for death related to diabetes, and an 11% reduction for MI. Another trial followed patients for 2 years and compared calcium-channel blockers and angiotensin-converting enzyme (ACE) inhibitors,with or without hydrochlorothiazide against placebo and found a significant reduction in acute MI, congestive heart failure, and sudden cardiac death in the intervention group compared to placebo.
The Hypertension Optimal Treatment (HOT) trial has shown that patients assigned to lower BP targets have improved outcomes. In the HOT trial,patients who achieved a diastolic BP of < 80 mmHg benefited the most in terms of reduction of cardiovascular events. Other epidemiological studies have shown that BPs > 120/70 mmHg are associated with increased cardiovascular morbidity and mortality in people with diabetes. The American Diabetes Association has recommended a target BP goal of < 130/80 mmHg. Studies have shown that there is no lower threshold value for BP and that the risk of morbidity and mortality will continue to decrease well into the normal range.
Many classes of drugs have been used in numerous trials to treat patients with hypertension. All classes of drugs have been shown to be superior to placebo in terms of reducing morbidity and mortality. Often, numerous agents(three or more) are needed to achieve specific target levels of BP. Use of almost any drug therapy to reduce hypertension in patients with diabetes has been shown to be effective in decreasing cardiovascular risk. Keeping in mind that numerous agents are often required to achieve the target level of BP control, recommending specific agents becomes a not-so-simple task. The literature continues to evolve, and individual patient conditions and preferences also must come into play.
While lowering BP by any means will help to reduce cardiovascular morbidity, there is evidence that may help guide the selection of an antihypertensive regimen. The UKPDS showed no significant differences in outcomes for treatment for hypertension using an ACE inhibitor or aβ-blocker. In addition, both ACE inhibitors and angiotensin II receptor blockers (ARBs) have been shown to slow the development and progression of diabetic nephropathy. In the Heart Outcomes Prevention Evaluation (HOPE)trial, ACE inhibitors were found to have a favorable effect in reducing cardiovascular morbidity and mortality, whereas recent trials have shown a renal protective benefit from both ACE inhibitors and ARBs. ACE inhibitors andβ-blockers seem to be better than dihydropyridine calcium-channel blockers to reduce MI and heart failure. However, trials using dihydropyridine calcium-channel blockers in combination with ACE inhibitors andβ-blockers do not appear to show any increased morbidity or mortality in CVD, as has been implicated in the past for dihydropyridine calcium-channel blockers alone. Recently, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) in high-risk hypertensive patients,including those with diabetes, demonstrated that chlorthalidone, a thiazide-type diuretic, was superior to an ACE inhibitor, lisinopril, in preventing one or more forms of CVD.
L.N. is a typical patient with obesity, diabetes, and hypertension. Her BP control can be improved. To achieve the target BP goal of < 130/80 mmHg, it may be necessary to maximize the dose of the ACE inhibitor and to add a second and perhaps even a third agent.
Diuretics have been shown to have synergistic effects with ACE inhibitors,and one could be added. Because L.N. has migraine headaches as well as diabetic nephropathy, it may be necessary to individualize her treatment. Adding a β-blocker to the ACE inhibitor will certainly help lower her BP and is associated with good evidence to reduce cardiovascular morbidity. Theβ-blocker may also help to reduce the burden caused by her migraine headaches. Because of the presence of microalbuminuria, the combination of ARBs and ACE inhibitors could also be considered to help reduce BP as well as retard the progression of diabetic nephropathy. Overall, more aggressive treatment to control L.N.'s hypertension will be necessary. Information obtained from recent trials and emerging new pharmacological agents now make it easier to achieve BP control targets.
Hypertension is a risk factor for cardiovascular complications of diabetes.
Clinical trials demonstrate that drug therapy versus placebo will reduce cardiovascular events when treating patients with hypertension and diabetes.
A target BP goal of < 130/80 mmHg is recommended.
Pharmacological therapy needs to be individualized to fit patients'needs.
ACE inhibitors, ARBs, diuretics, and β-blockers have all been documented to be effective pharmacological treatment.
Combinations of drugs are often necessary to achieve target levels of BP control.
ACE inhibitors and ARBs are agents best suited to retard progression of nephropathy.
Evan M. Benjamin, MD, FACP, is an assistant professor of medicine and Vice President of Healthcare Quality at Baystate Medical Center in Springfield, Mass.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Loading metrics
Open Access
Learning Forum
Learning Forum articles are commissioned by our educational advisors. The section provides a forum for learning about an important clinical problem that is relevant to a general medical audience.
See all article types »
A 21-Year-Old Pregnant Woman with Hypertension and Proteinuria
- Andrea Luk,
* To whom correspondence should be addressed. E-mail: [email protected]
- Ching Wan Lam,
- Wing Hung Tam,
- Anthony W. I Lo,
- Enders K. W Ng,
- Alice P. S Kong,
- Wing Yee So,
- Chun Chung Chow
- Andrea Luk,
- Ronald C. W Ma,
- Ching Wan Lam,
- Wing Hung Tam,
- Anthony W. I Lo,
- Enders K. W Ng,
- Alice P. S Kong,
- Wing Yee So,

Published: February 24, 2009
- https://doi.org/10.1371/journal.pmed.1000037
- Reader Comments
Citation: Luk A, Ma RCW, Lam CW, Tam WH, Lo AWI, Ng EKW, et al. (2009) A 21-Year-Old Pregnant Woman with Hypertension and Proteinuria. PLoS Med 6(2): e1000037. https://doi.org/10.1371/journal.pmed.1000037
Copyright: © 2009 Luk et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The authors received no specific funding for this article.
Competing interests: RCWM is Section Editor of the Learning Forum. The remaining authors have declared that no competing interests exist.
Abbreviations: CT, computer tomography; I, iodine; MIBG, metaiodobenzylguanidine; MRI, magnetic resonance imaging; SDH, succinate dehydrogenase; SDHD, succinate dehydrogenase subunit D
Provenance: Commissioned; externally peer reviewed
Description of Case
A 21-year-old pregnant woman, gravida 2 para 1, presented with hypertension and proteinuria at 20 weeks of gestation. She had a history of pre-eclampsia in her first pregnancy one year ago. During that pregnancy, at 39 weeks of gestation, she developed high blood pressure, proteinuria, and deranged liver function. She eventually delivered by emergency caesarean section following failed induction of labour. Blood pressure returned to normal post-partum and she received no further medical follow-up. Family history was remarkable for her mother's diagnosis of hypertension in her fourth decade. Her father and five siblings, including a twin sister, were healthy. She did not smoke nor drink any alcohol. She was not taking any regular medications, health products, or herbs.
At 20 weeks of gestation, blood pressure was found to be elevated at 145/100 mmHg during a routine antenatal clinic visit. Aside from a mild headache, she reported no other symptoms. On physical examination, she was tachycardic with heart rate 100 beats per minute. Body mass index was 16.9 kg/m 2 and she had no cushingoid features. Heart sounds were normal, and there were no signs suggestive of congestive heart failure. Radial-femoral pulses were congruent, and there were no audible renal bruits.
Baseline laboratory investigations showed normal renal and liver function with normal serum urate concentration. Random glucose was 3.8 mmol/l. Complete blood count revealed microcytic anaemia with haemoglobin level 8.3 g/dl (normal range 11.5–14.3 g/dl) and a slightly raised platelet count of 446 × 10 9 /l (normal range 140–380 × 10 9 /l). Iron-deficient state was subsequently confirmed. Quantitation of urine protein indicated mild proteinuria with protein:creatinine ratio of 40.6 mg/mmol (normal range <30 mg/mmol in pregnancy).
What Were Our Differential Diagnoses?
An important cause of hypertension that occurs during pregnancy is pre-eclampsia. It is a condition unique to the gravid state and is characterised by the onset of raised blood pressure and proteinuria in late pregnancy, at or after 20 weeks of gestation [ 1 ]. Pre-eclampsia may be associated with hyperuricaemia, deranged liver function, and signs of neurologic irritability such as headaches, hyper-reflexia, and seizures. In our patient, hypertension developed at a relatively early stage of pregnancy than is customarily observed in pre-eclampsia. Although she had proteinuria, it should be remembered that this could also reflect underlying renal damage due to chronic untreated hypertension. Additionally, her electrocardiogram showed left ventricular hypertrophy, which was another indicator of chronicity.
While pre-eclampsia might still be a potential cause of hypertension in our case, the possibility of pre-existing hypertension needed to be considered. Box 1 shows the differential diagnoses of chronic hypertension, including essential hypertension, primary hyperaldosteronism related to Conn's adenoma or bilateral adrenal hyperplasia, Cushing's syndrome, phaeochromocytoma, renal artery stenosis, glomerulopathy, and coarctation of the aorta.
Box 1: Causes of Hypertension in Pregnancy
- Pre-eclampsia
- Essential hypertension
- Renal artery stenosis
- Glomerulopathy
- Renal parenchyma disease
- Primary hyperaldosteronism (Conn's adenoma or bilateral adrenal hyperplasia)
- Cushing's syndrome
- Phaeochromocytoma
- Coarctation of aorta
- Obstructive sleep apnoea
Renal causes of hypertension were excluded based on normal serum creatinine and a bland urinalysis. Serology for anti-nuclear antibodies was negative. Doppler ultrasonography of renal arteries showed normal flow and no evidence of stenosis. Cushing's syndrome was unlikely as she had no clinical features indicative of hypercortisolism, such as moon face, buffalo hump, violaceous striae, thin skin, proximal muscle weakness, or hyperglycaemia. Plasma potassium concentration was normal, although normokalaemia does not rule out primary hyperaldosteronism. Progesterone has anti-mineralocorticoid effects, and increased placental production of progesterone may mask hypokalaemia. Besides, measurements of renin activity and aldosterone concentration are difficult to interpret as the renin-angiotensin-aldosterone axis is typically stimulated in pregnancy. Phaeochromocytoma is a rare cause of hypertension in pregnancy that, if unrecognised, is associated with significant maternal and foetal morbidity and mortality. The diagnosis can be established by measuring levels of catecholamines (noradrenaline and adrenaline) and/or their metabolites (normetanephrine and metanephrine) in plasma or urine.
What Was the Diagnosis?
Catecholamine levels in 24-hour urine collections were found to be markedly raised. Urinary noradrenaline excretion was markedly elevated at 5,659 nmol, 8,225 nmol, and 9,601 nmol/day in repeated collections at 21 weeks of gestation (normal range 63–416 nmol/day). Urinary adrenaline excretion was normal. Pregnancy may induce mild elevation of catecholamine levels, but the marked elevation of urinary catecholamine observed was diagnostic of phaeochromocytoma. Conditions that are associated with false positive results, such as acute myocardial infarction, congestive heart failure, acute cerebrovascular event, withdrawal from alcohol, withdrawal from clonidine, and cocaine abuse, were not present in our patient.
The working diagnosis was therefore phaeochromocytoma complicating pregnancy. Magnetic resonance imaging (MRI) of neck to pelvis, without gadolinium enhancement, was performed at 24 weeks of gestation. It showed a 4.2 cm solid lesion in the mid-abdominal aorto-caval region, while both adrenals were unremarkable. There were no ectopic lesions seen in the rest of the examined areas. Based on existing investigation findings, it was concluded that she had extra-adrenal paraganglioma resulting in hypertension.
What Was the Next Step in Management?
At 22 weeks of gestation, the patient was started on phenoxybenzamine titrated to a dose of 30 mg in the morning and 10 mg in the evening. Propranolol was added several days after the commencement of phenoxybenzamine. Apart from mild postural dizziness, the medical therapy was well tolerated during the remainder of the pregnancy. In the third trimester, systolic and diastolic blood pressures were maintained to below 90 mmHg and 60 mmHg, respectively. During this period, she developed mild elevation of alkaline phosphatase ranging from 91 to 188 IU/l (reference 35–85 IU/l). However, liver transaminases were normal and the patient had no seizures. Repeated urinalysis showed resolution of proteinuria. At 38 weeks of gestation, the patient proceeded to elective caesarean section because of previous caesarean section, and a live female baby weighing 3.14 kg was delivered. The delivery was uncomplicated and blood pressure remained stable.
Following the delivery, computer tomography (CT) scan of neck, abdomen, and pelvis was performed as part of pre-operative planning to better delineate the relationship of the tumour to neighbouring structures. In addition to the previously identified extra-adrenal paraganglioma in the abdomen ( Figure 1 ), the CT revealed a 9 mm hypervascular nodule at the left carotid bifurcation, suggestive of a carotid body tumour ( Figure 2 ). The patient subsequently underwent an iodine (I) 131 metaiodobenzylguanidine (MIBG) scan, which demonstrated marked MIBG-avidity of the paraganglioma in the mid-abdomen. The reported left carotid body tumour, however, did not demonstrate any significant uptake. This could indicate either that the MIBG scan had poor sensitivity in detecting a small tumour, or that the carotid body tumour was not functional.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1000037.g001
https://doi.org/10.1371/journal.pmed.1000037.g002
In June 2008, four months after the delivery, the patient had a laparotomy with removal of the abdominal paraganglioma. The operation was uncomplicated. There was no wide fluctuation of blood pressures intra- and postoperatively. Phenoxybenzamine and propranolol were stopped after the operation. Histology of the excised tumour was consistent with paraganglioma with cells staining positive for chromogranin ( Figures 3 and 4 ) and synaptophysin. Adrenal tissues were notably absent.
The tumour is a well-circumscribed fleshy yellowish mass with maximal dimension of 5.5 cm.
https://doi.org/10.1371/journal.pmed.1000037.g003
The tumour cells are polygonal with bland nuclei. The cells are arranged in nests and are immunoreactive to chromogranin (shown here) and synaptophysin.
https://doi.org/10.1371/journal.pmed.1000037.g004
The patient was counselled for genetic testing for hereditary phaeochromocytoma/paraganglioma. She was found to be heterozygous for c.449_453dup mutation of the succinate dehydrogenase subunit D (SDHD) gene ( Figure 5 ). This mutation is a novel frameshift mutation, and leads to SDHD deficiency (GenBank accession number: 1162563). At the latest clinic visit in August 2008, she was asymptomatic and normotensive. Measurements of catecholamine in 24-hour urine collections had normalised. Resection of the left carotid body tumour was planned for a later date. She was to be followed up indefinitely to monitor for recurrences. She was also advised to contact family members for genetic testing. Our patient gave written consent for this case to be published.
https://doi.org/10.1371/journal.pmed.1000037.g005
Phaeochromocytoma in Pregnancy
Hypertension during pregnancy is a frequently encountered obstetric complication that occurs in 6%–8% of pregnancies [ 2 ]. Phaeochromocytoma presenting for the first time in pregnancy is rare, and only several hundred cases have been reported in the English literature. In a recent review of 41 cases that presented during 1988 to 1997, maternal mortality was 4% while the rate of foetal loss was 11% [ 3 ]. Antenatal diagnosis was associated with substantial reduction in maternal mortality but had little impact on foetal mortality. Further, chronic hypertension, regardless of aetiology, increases the risk of pre-eclampsia by 10-fold [ 1 ].
Classically, patients with phaeochromocytoma present with spells of palpitation, headaches, and diaphoresis [ 4 ]. Hypertension may be sustained or sporadic, and is associated with orthostatic blood pressure drop because of hypovolaemia and impaired vasoconstricting response to posture change. During pregnancy, catecholamine surge may be triggered by pressure from the enlarging uterus and foetal movements. In the majority of cases, catecholamine-secreting tumours develop in the adrenal medulla and are termed phaeochromocytoma. Ten percent of tumours arise from extra-adrenal chromaffin tissues located in the abdomen, pelvis, or thorax to form paraganglioma that may or may not be biochemically active. The malignant potential of phaeochromocytoma or paraganglioma cannot be determined from histology and is inferred by finding tumours in areas of the body not known to contain chromaffin tissues. The risk of malignancy is higher in extra-adrenal tumours and in tumours that secrete dopamine.
Making the Correct Diagnosis
The diagnosis of phaeochromocytoma requires a combination of biochemical and anatomical confirmation. Catecholamines and their metabolites, metanephrines, can be easily measured in urine or plasma samples. Day collection of urinary fractionated metanephrine is considered the most sensitive in detecting phaeochromocytoma [ 5 ]. In contrast to sporadic release of catecholamine, secretion of metanephrine is continuous and is less subjective to momentary stress. Localisation of tumour can be accomplished by either CT or MRI of the abdomen [ 6 ]. Sensitivities are comparable, although MRI is preferable in pregnancy because of minimal radiation exposure. Once a tumour is identified, nuclear medicine imaging should be performed to determine its activity, as well as to search for extra-adrenal diseases. I 131 or I 123 MIBG scan is the imaging modality of choice. Metaiodobenzylguanidine structurally resembles noradrenaline and is concentrated in chromaffin cells of phaeochromocytoma or paraganglioma that express noradrenaline transporters. Radionucleotide imaging is contraindicated in pregnancy and should be deferred until after the delivery.
Treatment Approach
Upon confirming the diagnosis, medical therapy should be initiated promptly to block the cardiovascular effects of catecholamine release. Phenoxybenzamine is a long-acting non-selective alpha-blocker commonly used in phaeochromocytoma to control blood pressure and prevent cardiovascular complications [ 7 ]. The main side-effects of phenoxybenzamine are postural hypotension and reflex tachycardia. The latter can be circumvented by the addition of a beta-blocker. It is important to note that beta-blockers should not be used in isolation, since blockade of ß2-adrenoceptors, which have a vasodilatory effect, can cause unopposed vasoconstriction by a1-adrenoceptor stimulation and precipitate severe hypertension. There is little data on the safety of use of phenoxybenzamine in pregnancy, although its use is deemed necessary and probably life-saving in this precarious situation.
The definitive treatment of phaeochromocytoma or paraganglioma is surgical excision. The timing of surgery is critical, and the decision must take into consideration risks to the foetus, technical difficulty regarding access to the tumour in the presence of a gravid uterus, and whether the patient's symptoms can be satisfactorily controlled with medical therapy [ 8 , 9 ]. It has been suggested that surgical resection is reasonable if the diagnosis is confirmed and the tumour identified before 24 weeks of gestation. Otherwise, it may be preferable to allow the pregnancy to progress under adequate alpha- and beta-blockade until foetal maturity is reached. Unprepared delivery is associated with a high risk of phaeochromocytoma crisis, characterised by labile blood pressure, tachycardia, fever, myocardial ischaemia, congestive heart failure, and intracerebral bleeding.
Patients with phaeochromocytoma or paraganglioma should be followed up for life. The rate of recurrence is estimated to be 2%–4% at five years [ 10 ]. Assessment for recurrent disease can be accomplished by periodic blood pressure monitoring and 24-hour urine catecholamine and/or metanephrine measurements.
Genetics of Phaeochromocytoma
Approximately one quarter of patients presenting with phaeochromocytoma may carry germline mutations, even in the absence of apparent family history [ 11 ]. The common syndromes of hereditary phaeochromocytoma/paraganglioma are listed in Box 2 . These include Von Hippel-Lindau syndrome, multiple endocrine neoplasia type 2, neurofibromatosis type 1, and succinate dehydrogenase (SDH) gene mutations. Our patient has a novel frameshift mutation in the SDHD gene located at Chromosome 11q. SDH is a mitochondrial enzyme that is involved in oxidative phosphorylation. Characteristically, SDHD mutation is associated with head or neck non-functional paraganglioma, and infrequently, sympathetic paraganglioma or phaeochromocytoma [ 12 ]. Tumours associated with SDHD mutation are rarely malignant, in contrast to those arisen from mutation of the SDHB gene. Like all other syndromes of hereditary phaeochromocytoma, SDHD mutation is transmitted in an autosomal dominant fashion. However, not all carriers of the SDHD mutation develop tumours, and inheritance is further complicated by maternal imprinting in gene expression. While it may not be practical to screen for genetic alterations in all cases of phaeochromocytoma, most authorities advocate genetic screening for patients with positive family history, young age of tumour onset, co-existence with other neoplasms, bilateral phaeochromocytoma, and extra-adrenal paraganglioma. The confirmation of genetic mutation should prompt evaluation of other family members.
Box 2: Hereditary Phaeochromocytoma/Paraganglioma Syndromes
- Von Hippel-Lindau syndrome
- Multiple endocrine neoplasia type 2A and type 2B
- Neurofibromatosis type 1
- Mutation of SDHB , SDHC , SDHD
- Ataxia-telangiectasia
- Tuberous sclerosis
- Sturge-Weber syndrome
Key Learning Points
- Hypertension complicating pregnancy is a commonly encountered medical condition.
- Pre-existing chronic hypertension must be considered in patients with hypertension presenting in pregnancy, particularly if elevation of blood pressure is detected early during pregnancy or if persists post-partum.
- Secondary causes of chronic hypertension include renal artery stenosis, renal parenchyma disease, primary hyperaldosteronism, phaeochromocytoma, Cushing's syndrome, coarctation of the aorta, and obstructive sleep apnoea.
- Phaeochromocytoma presenting during pregnancy is rare but carries high rates of maternal and foetal morbidity and mortality if unrecognised.
- Successful outcomes depend on early disease identification, prompt initiation of alpha- and beta-blockers, carefully planned delivery, and timely resection of the tumour.
Phaeochromocytoma complicating pregnancy is uncommon. Nonetheless, in view of the potential for catastrophic consequences if unrecognised, a high index of suspicion and careful evaluation for secondary causes of hypertension is of utmost importance. Blood pressure should be monitored in the post-partum period and persistence of hypertension must be thoroughly investigated.
Author Contributions
All authors participated in the management of the patient or writing of the article. AL and RCWM wrote the article, with contributions from all the authors.
- View Article
- Google Scholar
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Next Generation Research Uses Real-World Data to Identify Most Effective Hypertension Drugs for Patients
Listen to "next generation research uses real-world data to identify most effective hypertension drugs for patients".
More than 100 million U.S. adults have been diagnosed with hypertension , one of the leading risk factors for cardiovascular disease. While more than 70% of people with hypertension cannot achieve adequate blood pressure control with just one drug, current guidelines only make recommendations for first-line therapy.
“The question is: when the first drug is not enough, what is the optimal second drug to add?” said Yuan Lu, ScD , assistant professor of medicine (cardiology) and assistant professor of biomedical informatics and data science and of epidemiology (chronic disease). “There are more than 50 drugs across five major classes available for treating hypertension. Conducting clinical trials to compare every possible drug and combination thereof is impractical; it would be incredibly time-consuming and costly. Consequently, this creates a significant gap in evidence.”
Lu recently received a Research Project Grant (R01) from the National Institutes of Health (NIH) for the project, “Real-World Evidence to Inform Decisions for Hypertension Treatment Escalation,” to help address this question.
Lu and her team will analyze real-world data that is routinely collected by clinicians in health care settings to compare the effectiveness of second antihypertensive agents on major cardiovascular events as well as their comparative risk on potential drug-related adverse events. This study will also look at the effectiveness and safety of each second hypertensive agent when used in different patient subgroups defined by age, sex, race, ethnicity, and comorbidities, which Lu hopes will help address disparities for patients with hypertension. This is the first research study of its kind that uses real-world data assets and reproducible methods to comprehensively evaluate the safety and effectiveness of second anti-hypertensive drugs added after monotherapy.
“Clinicians often face this important patient scenario and lack comprehensive, high-quality evidence on how best to guide the implementation of the available drug options for patients into real-world practice,” said Eric Velazquez, MD , Robert W. Berliner Professor of Medicine and chief of Yale Cardiovascular Medicine. “Hypertension impacts nearly every family in the world. It has been a substantial frustration for me that randomized clinical trials such as ACCOMPLISH , which we completed over 15 years ago, have not been adequately integrated into everyday care. Yuan’s work is pivotal to ensure our research meets its potential to improve the lives of millions of people living with hypertension.”
The study will analyze data from more than 100 million patients in the United States in five electronic health record (EHR) databases. Lu and her team are collaborating with the Observational Health Data Science and Informatics (OHDSI) , a multi-stakeholder, international organization that aims to use systematic approaches to improve observational study. OHDSI created the OMOP Common Data Model , which is an open community data standard that allows institutions to efficiently share data for analysis.
“By mapping EHR data into a common data model, we can now combine the power of computing, data science, and clinical knowledge to generate new evidence to address these important clinical questions,” said Lu. “We hope our research will inform the prioritization of future clinical trials, assisting investigators in selecting the most promising drug combinations for testing.”
Lu joined Yale in 2015 after receiving her ScD in Global Health and Population at the Harvard School of Public Health. “I was intrigued by this area of study because instead of a doctor, who can only treat 20 or 30 patients a day, I would have the opportunity to impact health at the population level,” she said.
She hopes that this research will inform the development of clinical guidelines. Even though clinical trials provide the highest quality of evidence, real-world data from observational studies can provide important evidence to complement clinical trials and support guideline development, especially when clinical trials are too expensive or unethical to conduct.
“Physicians can’t just wait for clinical trials to end before they help their patients. They need to keep treating people using the best available information and practices,” said Lu.
Eventually, Lu and her team plan to develop a clinical decision support tool that would incorporate the knowledge gained from this project. The tool would help doctors quickly and easily see recommendations about the types of combination therapies that may work best for their individual patients. “It’s often said that it takes about 17 years to translate about 14% of research findings to be implemented into routine clinical practice. It’s a long time. I want to try to reduce the time it takes to get research into clinical practice and increase the percentage of knowledge translation," she said.
The research team is beginning to refine their protocol for the study, which they aim to publish online via GitHub so that anyone interested in this work can read the proposal and provide feedback to help make improvements. Lu sees tremendous potential for this type of study in other areas of medicine, including diabetes, obesity, and other common health conditions. She and other team members are already beginning work on other projects using real-world data.
For example, Lu, along with other researchers from Yale and colleagues at Sentara Health, recently published a paper in the Journal of the American Heart Association (JAHA) , which used real-world EHR data to identify the prevalence, control rates, and diagnostic codes used in a large patient population. The study found that prevalence is increasing, a quarter of patients’ hypertension was not controlled, and there were marked disparities between non-Hispanic Black patients and other racial and ethnic groups. Lu and the study authors say other regional health systems could emulate this study to better understand their hypertension prevalence and control rates and to inform strategies to improve hypertension care. Other study authors include: Yuntian Liu, MPH , Shu-Xia Li, PhD , Mitsuaki Sawano, MD , Patrick Young, PhD , Wade Schulz, MD , and Harlan Krumholz, MD, SM , from Yale, and John E. Brush, Jr., MD, Jordan R. Asher, MD, MS, Mark Anderson, AS, and John S. Burrows, MBA.
“I feel so fortunate that I decided to come to Yale. As an investigator, it can sometimes seem like the only deliverable is a paper. But at Yale, I’m able to work closely with clinicians and see how this knowledge can inform their clinical practice or help them do their job better,” Lu said. “I’m excited to come to work every day.”
- National Institutes of Health (NIH)
- Internal Medicine
- Cardiovascular Medicine

Featured in this article
- Yuan Lu, ScD Assistant Professor of Medicine (Cardiology) and of Biomedical Informatics and Data Science and of Epidemiology (Chronic Diseases)
- Yuntian Liu Statistician I
- Shu-Xia Li, PhD Staff Affiliate - YNHH; Associate Director, Data Management & Analytics, Center for Outcomes Research & Evaluation (CORE)
- Mitsuaki Sawano, MD, PhD Associate Research Scientist
- Wade Schulz, MD, PhD Assistant Professor; Director of Informatics, Laboratory Medicine; Director, CORE Center for Computational Health, Center for Outcomes Research & Evaluation (CORE)
- Patrick Young, PhD Associate Research Scientist
- Harlan Krumholz, MD, SM Harold H. Hines, Jr. Professor of Medicine (Cardiology) and Professor in the Institute for Social and Policy Studies, of Investigative Medicine and of Public Health (Health Policy); Founder, Center for Outcomes Research and Evaluation (CORE)
- Eric Velazquez, MD Robert W. Berliner Professor of Medicine (Cardiology); Chief, Cardiovascular Medicine; Chief, Cardiovascular Medicine, Yale New Haven Hospital; Physician-in-Chief, Heart and Vascular Center, Yale New Haven Health System; Deputy Director, Clinical Trials Innovation, Yale Center for Clinical Investigation (YCCI); Co-Chair, Clinical and Translational Research Oversight Committee; President’s contingency planning committee, Clinical Practice/Clinical Research Subcommittee
Related Links
- Digital Health Tools Help Manage Hypertension for Populations Experiencing Health Disparities
- Enhancing Treatment for Persistent Hypertension: Unleashing the Power of Actionable Taxonomy from EHR Data for Precision Medicine
- The Unmet Potential of Clinical Decision Support Tools in Cardiology
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 27 May 2024
Hemodynamic parameters and diabetes mellitus in community-dwelling middle-aged adults and elders: a community-based study
- Tzu-Wei Wu 1 ,
- Yih-Jer Wu 1 , 2 , 3 , 4 ,
- Chao-Liang Chou 1 , 5 ,
- Chun-Fang Cheng 6 ,
- Shu-Xin Lu 5 &
- Li-Yu Wang 1
Scientific Reports volume 14 , Article number: 12032 ( 2024 ) Cite this article
Metrics details
- Prognostic markers
Hemodynamic parameters have been correlated with stroke, hypertension, and arterial stenosis. While only a few small studies have examined the link between hemodynamics and diabetes mellitus (DM). This case-control study enrolled 417 DM patients and 3475 non-DM controls from a community-based cohort. Peak systolic velocity (PSV), end-diastolic velocity (EDV), blood flow velocity (MFV), pulsatility index (PI), and the resistance index (RI) of the common carotid arteries were measured by color Doppler ultrasonography. Generalized linear regression analyses showed that as compared to the non-DM controls, the age-sex-adjusted means of PSV, EDV, and MFV were − 3.28 cm/sec, − 1.94 cm/sec, and − 2.38 cm/sec, respectively, lower and the age-sex-adjusted means of RI and PI were 0.013 and 0.0061, respectively, higher for the DM cases (all p -values < 0.0005). As compared to the lowest quartiles, the multivariable-adjusted ORs of DM for the highest quartiles of PSV, EDV, MFV, RI, and PI were 0.59 (95% confidence interval [CI] 0.41–0.83), 0.45 (95% CI 0.31–0.66), 0.53 (95% CI 0.37–0.77), 1.61 (95% CI 1.15–2.25), and 1.58 (95% CI 1.12–2.23), respectively. More importantly, the additions of EDV significantly improved the predictabilities of the regression models on DM. As compared to the model contained conventional CVD risk factors alone, the area under the receiver operating curve (AUROC) increased by 1.00% (95% CI 0.29–1.73%; p = 0.0059) and 0.80% (95% CI 0.15–1.46%; p = 0.017) for models that added EDV in continuous and quartile scales, respectively. Additionally, the additions of PSV and MFV also significantly improved the predictabilities of the regression models (all 0.01 < p -value < 0.05). This study reveals a significant correlation between DM and altered hemodynamic parameters. Understanding this relationship could help identify individuals at higher risk of DM and facilitate targeted preventive strategies to reduce cardiovascular complications in DM patients.
Similar content being viewed by others
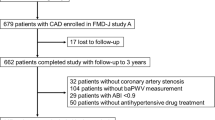
Increased arterial stiffness and cardiovascular risk prediction in controlled hypertensive patients with coronary artery disease: post hoc analysis of FMD-J (Flow-mediated Dilation Japan) Study A

Left ventricular mass versus pulse wave velocity as predictors of coronary artery disease in hypertensive patients: data from a 6-year-follow-up study

Relationship between arterial stiffness and chronic kidney disease in patients with primary hypertension
Atherosclerosis is a chronic disease that causes the occlusion of arteries by the accumulation of plaques within the arterial intima 1 . These plaques consist of lipids, predominantly low-density lipoprotein (LDL), and inflammatory cells, such as macrophages that transform into foam cells after phagocytosing lipids 2 , 3 . Atherosclerosis advances gradually and often asymptomatically, but it can be aggravated by other factors such as hypertension 4 . As the plaques enlarge, they can impair blood flow and induce shear stress in the vessel wall. This can provoke the erosion of vulnerable plaques and the generation of thrombi that can occlude the artery or embolize other organs 5 . Atherosclerosis can result in severe cardiovascular complications such as myocardial infarction and stroke, which are among the leading causes of mortality worldwide 6 , 7 . Atherosclerosis is especially common in developed countries, but it is also increasing in developing countries 8 . In Taiwan, for instance, five of the top ten causes of mortality are associated with atherosclerosis 9 .
Hemodynamics is the study of blood flow and the forces acting on the blood vessels and the heart. The relationship between atherosclerosis and hemodynamics is complex and bidirectional. On one hand, hemodynamic shear stress can influence the development and progression of atherosclerosis by modulating the phenotype and function of endothelial cells and smooth muscle cells, and by promoting or inhibiting inflammation, oxidative stress, lipid accumulation, and matrix remodeling in the arterial wall 10 , 11 , 12 . On the other hand, atherosclerosis can alter the geometry and elasticity of the arteries, which can affect the hemodynamic patterns and parameters such as pressure, flow, velocity, and shear stress 13 . These changes can further influence the stability and rupture risk of atherosclerotic plaques. Key hemodynamic parameters include peak systolic velocity (PSV), end-diastolic velocity (EDV), and mean blood flow velocity (MFV) measured by Doppler ultrasonography. Pulsatility index (PI) and resistance index (RI) were secondary parameters calculated from velocities 14 , 15 and were accepted as methods of examing microcirculation with a variety of clinical applications 16 . PI is defined as the difference between PSV and EDV, divided by MFV, and RI is defined as the difference between PSV and EDV, divided by PSV.
Diabetes mellitus (DM) is a metabolic disorder characterized by chronic hyperglycemia that induces polyuria, polydipsia, and polyphagia. DM results from inadequate insulin secretion and/or impaired insulin action in the target tissues 17 . There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease that causes β-cell destruction in the pancreatic islets. It typically manifests in children and adolescents and necessitates exogenous insulin therapy. Type 2 diabetes is more prevalent and involves insulin resistance that exacerbates as the β-cell function deteriorates 18 . DM affects over 450 million people worldwide and accounts for 4.2 million deaths annually 19 . DM is diagnosed by assessing fasting and post-load plasma glucose levels.
Clinically, DM is associated with increased risks of vascular events, including carotid artery diseases 20 , 21 . Our previous study demonstrated the prevalence of DM is significantly associated with the development and severity of carotid atherosclerosis 22 . Later we identified 9 DM SNPs showing promising associations with the presence of carotid plaque in a community-based case-control study 23 . The associations of hemodynamics and carotid pulsatility with DM were noted in a few studies previously 24 , 25 , 26 . However, this clinical correlation is not fully explored. In this community-based case-control study, the relationship between DM and hemodynamic parameters was investigated in more than 3800 subjects, including 417 DM patients and 3475 non-DM controls, from the Northern coast of Taiwan.
Study subjects
The study subjects were recruited from our two previous community-based cohort studies that enrolled 40–74-year-old middle-aged adults and elders residing in the five districts in the northern coastal area of Taiwan for at least six months 22 , 27 . Cohort I and II enrolled study subjects from September 2010 to May 2011 and from September 2014 to May 2020, respectively. During each period, well-informed invitation letters describing the objective and protocols of the study were sent to households with eligible subject(s), and recruitment sites were set up at the local health stations, schools, or community activity centers. Residents who were willing to complete a structured questionnaire regarding personal health information and willing to provide blood samples were recruited. A total of 4102 residents voluntarily provided informed consent and were enrolled. Subjects who had a positive history of physician-diagnosed myocardial infarction or had ever received a cardiac catheter or stent (n = 165) and who were without a proper flow pattern sample (n = 45) were excluded, leaving a total of 3892 middle-aged adults and elders in this study. The study complied with the 1975 Helsinki Declaration on ethics in medical research and was reviewed and approved by the institutional review boards of MacKay Medical College (No. P990001) and MacKay Memorial Hospital (No. 14MMHIS075).
Anthropometric and biochemical measurements
The measurements of baseline anthropometric and clinical characteristics were described previously 27 , 28 . In brief, blood pressure was measured three times by a digital system (UDEX-Twin; ELK Co., Daejon, Korea) in the morning after 10 min of rest. Three blood pressure measurements, with an interval of ≥ 3 minutes, were made for each participant. The averages of repeated measurements of systolic blood pressure (SBP) and diastolic blood pressure (DBP) were used for analyses.
A venous blood sample was collected from each participant for blood lipids and glucose analyses after at least 10 hours of fasting. We used an autoanalyzer (Toshiba TBA c16000; Toshiba Medical System, Holliston, MA, USA) to determine the blood levels of lipids, including total cholesterol (TCHO), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglycerides (FTG), and glucose (FPG) with commercial kits (Denka Seiken, Tokyo, Japan).
In this study, DM was defined as FPG ≥ 126 mg/dL or the use of insulin or other hypoglycemic agents. Hypertension was defined as SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, or a history of taking antihypertensive medications. Current cigarette smoking was defined as having smoked cigarettes at least 4 days per week during the past month before enrollment. Current alcohol drinking was defined as having drunk alcohol-containing beverages at least 4 days per week during the past month before enrollment.
Ultrasonographic measurements of carotid blood flow
In the study, blood flows, including PSV, EDV, and MFV, of extracranial carotid arteries, were measured at the middle segment of the bilateral common carotid arteries by color Doppler ultrasonography. The ultrasonographic systems (GE Healthcare Logie E, Vivid 7, and Vivid E9; General Electric Company, Milwaukee, USA), which were equipped with a multi-frequency linear array transducer, were operated by two experienced technicians who were blind to patients’ clinical profiles. Each participant was examined in the supine position with his/her head turned 45° from the site being measured. An insonation angle equal to or less than 60° and a sample volume size covering 1/2–2/3 of the arterial lumen were maintained for all Doppler measurements. In the study, a proper flow pattern sample was defined as subjects with at least 3 waveforms with similar patterns. The subject’s PI and RI were calculated as (PSV-EDV)/MFV and (PSV-EDV)/PSV, respectively. In the study, the averages of the measurements of the right and left common carotid arteries were used for statistical analyses.
Statistical analyses
In this study, the student t-test and one-way analysis of variance were used to test the significance of means of continuous measurements among groups. Logarithmic transformation was performed for continuous random variables with positive skewness. The Chi-square test was used to test the significance of the associations between DM status and categorical variables. The effects of age, sex, and DM on the carotid hemodynamic parameters were assessed by the generalized linear regression analyses. The odds ratio (OR), which was estimated by the unconditional logistic regression model, was used as the indicator of the strength of association between carotid hemodynamic parameters and DM status. To assess the independent effects of carotid hemodynamic parameters on DM, we used multivariable logistic regression analyses to control for the confounding effects of other conventional cardiovascular risk factors. The area under the receiver operating curve (AUROC) was used as the indicator of the predictability of the regression model on DM. To explore whether there were interactions between hemodynamic biomarkers and other significant factors on the likelihoods of having DM, we carried out stratified analyses. For continuous variables, the values close to the medians in the non-DM subjects were used as the cut-points. We used the statistical method proposed by Clogg et al. 29 to test the significance in the regression coefficients between two groups. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics approval and consent to participate
The study complied with the 1975 Helsinki Declaration on ethics in medical research and was reviewed and approved by the institutional review boards of MacKay Medical College (No. P990001, granted date: 2010/7/5) and MacKay Memorial Hospital (No. 14MMHIS075, Granted date: 2014/5/23).
Among 3892 participants, 417 (10.7%) of them fulfilled the DM definition and were regarded as cases. Table 1 shows that all baseline anthropometric and biochemical measurements, except for alcohol drinking, were significantly different between DM cases and non-DM controls. As compared to the non-DM controls, DM cases had significantly higher means of age, body mass index (BMI), waist circumference (WC), hip circumference (HIP), waist-to-hip ratio (WHR), blood pressure, and Log (TG) and higher proportions of the male sex, hypertension, schooling years < 12 years, and cigarette smoking. The means of TCHO, LDL-C, and HDL-C of DM cases were significantly lower than those of the non-DM controls.
Multivariable logistic regression analyses of the conventional cardiovascular risk factors showed that older age, hypertension, fewer schooling years, cigarette smoking, higher BMI, higher WHR, and higher TG were correlated with significantly higher ORs of having DM (Table 2 ). The multivariable-adjusted ORs of having DM with TCHO and HDL-C levels were significantly inverse. The multivariable-adjusted ORs for per 1.0 SD increases in BMI, WHR, TCHO, HDL-C, and log(TG) were 1.24 (95% CI 1.11–1.40), 1.30 (95% CI 1.14–1.48), 0.77 (95% CI 0.67–0.87), 0.84 (95% CI 0.71–0.99), and 1.98 (95% CI 1.56–2.51) respectively.
The effects of age, sex, and DM on carotid blood flows, RI, and PI are shown in Table 3 . As compared to female subjects, male subjects had significantly higher means of PSV, PI, and RI and significantly lower means of EDV and MFV (all p -values < 0.0001). The means of these five carotid hemodynamic parameters were all significantly different among seven age groups (all p -values < 0.0001). The means (SD) of PSV, EDV, and MFV for subjects aged 40–44 years were 95.1 (17.6) cm/sec, 26.1 (5.6) cm/sec, and 44.4 (8.0) cm/sec, respectively, for subjects aged 55–59 years were 84.5 (17.4) cm/sec, 24.4 (5.4) cm/sec, and 41.4 (7.9) cm/sec, respectively, and for subjects aged 70–74 years were 75.9 (16.7) cm/sec, 18.2 (4.6) cm/sec, and 34.5 (7.2) cm/sec, respectively. The means of RI and PI were lower for subjects aged 45–54 years and were higher for elderly subjects. Table 3 also shows that DM cases had significantly lower means of PSV, EDV, and MFV and significantly higher means of RI and PI as compared to the non-DM controls (all p -values < 0.0001).
The results of generalized linear regression analyses were also shown in Table 3 . The age trends for PSV, EDV, and MFV were significantly negative while for RI and PI were significantly positive. The adjusted regression coefficients of PSV, EDV, MFV, RI, and PI per 5.0 years increase in age at enrollment were − 3.17 cm/sec, − 1.17 cm/sec, − 1.51 cm/sec, 0.0038, and 0.0079, respectively (all p -values < 0.005). As compared to female subjects, male subjects had significantly higher adjusted means for PSV, RI, and PI, while exhibiting significantly lower adjusted means for EDV and MFV (all p -values < 0.0001). After adjustment for the effects of age and sex, the effects of DM status on all five carotid hemodynamic parameters remained statistically significant. As compared to the non-DM controls, the adjusted means of PSV, EDV, and MFV were − 3.28 cm/sec ( p = 0.0003), − 1.94 cm/sec ( p < 0.0001), and − 2.38 cm/sec ( p < 0.0001), respectively, lower for the DM cases. The age-sex-adjusted means of RI and PI of DM cases were 0.013 and 0.0061 (both p -values < 0.0001), respectively, higher than those of the non-DM controls.
Table 4 shows that the prevalence rates of DM were negatively correlated with increased levels of PSV, EDV, and MFV and were positively correlated with increased levels of RI and PI. The prevalence rates of DM for subjects whose carotid blood flows were of the lowest quartile (Q1) and the highest quartile (Q4) ranged from 14.1 to 17.5% and from 4.9 to 5.1%, respectively. The prevalence rates of DM for subjects who had Q1 levels of RI or PI were approximately 7.0% and for Q4 levels of RI or PI were approximately 16.0%. As compared to subjects who had Q1 levels of carotid blood flows, subjects who had Q4 levels of PSV, EDV, and MFV had significantly decreased ORs of having DM. The corresponding age-sex-adjusted ORs were 0.51 (95% CI 0.37–0.72), 0.37 (95% CI 0.26–0.54), and 0.40 (95% CI 0.28–0.57), respectively. The age-sex-adjusted ORs were significantly increased for subjects who had Q3 and Q4 levels of RI and PI as compared to those who had Q1 levels of RI and PI.
The results of multivariable analyses showed that the multivariable-adjusted ORs of having DM remained statistically significant for subjects who had Q4 levels of PSV, EDV, MFV, RI, and PI, relative to those with Q1 levels (Table 4 ). The corresponding multivariable-adjusted ORs of having DM were 0.59 (95% CI 0.41–0.83), 0.45 (95% CI 0.31–0.66), 0.53 (95% CI 0.37–0.77), 1.61 (95% CI 1.15–2.25), and 1.58 (95% CI 1.12–2.23), respectively. As compared to those who had a Q1 level of EDV, subjects who had a Q3 level of EDV also had a significantly lower OR (0.63; 95% CI 0.46–0.87). The multivariable-adjusted ORs of having DM per 5.0 cm/sec increase in PSV, EDV, and MFV were 0.95 (95% CI 0.92–0.98), 0.74 (95% CI 0.66–0.83), and 0.86 (95% CI 0.80–0.93), respectively. Increased PI and RI were significantly positively correlated with the likelihood of DM. The multivariable-adjusted ORs of having DM per 0.1 increases in RI was 1.52 (95% CI 1.21–1.91) and for per 1.0 increase in PI was 1.49 (95% CI 1.05–2.12).
The comparisons of the predictabilities of the regression models that contained different carotid hemodynamic parameters are shown in Table 5 . The AUROC for the basic model, i.e., the most predictive model selected from the regression analyses which contained all significantly conventional cardiovascular risk factors, was 0.7578 (95% CI 0.7346–0.7809). The results of multivariable logistic regression analyses showed that EDV was the most significantly independent predictor of DM. The AUROC were 0.7658 (95% CI 0.7430–0.7885) and 0.7678 (95% CI 0.7453–0.7904) for models adding EDV as a continuous or a categorical variable, respectively. The additions of PSV and MFV also significantly increased the predictabilities of DM status but with smaller added AUROC (Table 5 ).
To explore whether there were interactive effects between EDV and conventional CVD risk factors on the likelihoods of having DM, we carried out stratified analyses. Table 6 shows that increased EDV were correlated with significantly decreased ORs of having DM in all strata. The regression coefficient (SE) for per 5 cm/sec increase in EDV for subjects aged < 55 year was non-significantly different that of subjects aged ≥ 55 years (− 0.229 (0.096) vs. − 0.414 (0.069), p = 0.12). Similarly, there was no significant difference in the regression coefficients between two strata of other factors.
In this study, we conducted a community-based case-control study, in which we enrolled approximately 4000 subjects aged 40–74 residing in the northern coastal area of Taiwan. In the case-control study, large numbers of DM cases and non-DM controls received color Doppler ultrasonographic measurements, including PSV, EDV, MFV, PI, and RI. We found significant age and sex effects on these hemodynamic parameters. After adjustment for the effects of age and sex, all these five carotid hemodynamic parameters remained significantly influenced by DM status. As compared to the non-DM controls, the adjusted means of PSV, EDV, and MFV were significantly lower and the adjusted means of RI and PI were significantly higher for the DM cases. We also found that after controlling for the effects of other conventional CVD risk factors, the multivariable-adjusted ORs of having DM were negatively correlated with PSV, EDV, and MFV and were positively correlated with PI and RI. More importantly, the additions of PSV, EDV, and MFV, either in categorical or continuous scales, significantly improved the predictabilities of the regression models on DM status and among them EDV was the most significantly independent predictor.
Pulsatility is a crucial aspect of the cardiovascular system, linked to artery elasticity. The natural pressure pulsations from each left ventricle contraction are reduced by the elasticity of large arteries. The aorta's expansion stores part of the stroke volume, lessening pulsatile stress on microvasculature 30 . However, with the loss of elastic fiber with age and disorders of metabolism, such as hyperlipidemia or DM, arterial walls continually increase their stiffness resulting in a gradual increase in blood pressure and, eventually affecting global cardiovascular health 16 . Pulsatile hemodynamics can be measured with invasive or non-invasive methods. Inserting an intraarterial catheter is the most accurate method of assessing pulsatile hemodynamics, however, multiple studies indicated that non-invasive methods could be reasonable surrogates for invasive ones 31 , 32 , 33 . Hemodynamic parameters including blood velocities such as PSV, EDV, and MFV as well as PI and RI were used to study their clinical correlation with different cardiovascular conditions including but not limited to stroke 34 , 35 , 36 , 37 , 38 , 39 , hypertension 40 , 41 , 42 , arterial stenosis 43 , 44 , 45 , 46 .
Prolonged hyperglycemia in patients with DM can damage the vascular endothelium leading to an increase in vascular stiffness and likely a change in hemodynamics 47 . The increase in the stiffness of large vessels can result in increased pulsation and microvascular complications 48 . Several studies have shown possible applications of hemodynamic parameters in predicting and preventing microvascular complications. In 2000, Lee et al. first studied 56 type 2 DM patients and 70 controls and measured their flow velocities and PI of the middle cerebral artery (MCA), extracranial internal carotid artery (ICA), and basilar artery (BA) 25 . They found that PIs of the MCA and ICA were closely correlated with the duration of DM. Some of these studies were lack of sex and age-matched controls 49 , 50 , 51 , 52 while some studies were designed to test the effect of drugs with only DM patients 53 , 54 . In studies with sex and age-matched controls, Agha et al. measured the velocity and PI of BA, ICA, and MCA in 141 DM patients and 132 controls 55 ; Dikanovic et al. measured the velocity and PI of MCA in 100 type 2 DM patients and 100 controls 26 ; Park et al. measured the velocity and PI of MCA in 90 type 2 DM patients and 45 controls 56 ; Zou et al. measured the velocity, PI and RI of dorsalis pedis artery and plantar digital artery in 56 type 2 DM patients and 50 controls 57 . All of these studies came to the same conclusion as we did that hemodynamic parameters including velocities, PI, and RI can be useful indicators and predictors of DM. However, none of them perform their studies at the same large scale as we did.
In a previous study, we included 4073 participants from the same study area, with prevalence rates of carotid plaque and DM at 35.4% and 11.3%, respectively 22 . The study found statistically significant linear trends between the likelihood of having DM and the total number of carotid plaques, maximum carotid stenosis, or severity of carotid atherosclerosis. The multivariate-adjusted odds ratio (OR) for DM was 1.57 (1.25–1.98), indicating a significantly higher risk for subjects with carotid plaques compared to those without observable plaque images. Furthermore, a greater number of carotid plaques, increased maximum carotid atherosclerosis, and more severe carotid atherosclerosis were associated with significantly higher ORs for DM. The prevalence rate of carotid plaque in the prevalent DM group was also significantly higher than in the incident DM group. In our most recent case-control study, we enrolled 309 carotid plaque-positive subjects and 439 carotid plaque-negative subjects from a community-based cohort 23 . Multivariable analyses of anthropometric attributes and biochemical profiles revealed that DM was a significant independent predictor in the best-fit regression model for the presence of carotid plaque. Among the 43 tested DM SNPs, 9 showed promising associations with carotid atherosclerosis, controlling for age, cigarette smoking, and hypertension. Although not all of these promising SNPs demonstrated significant independent effects in the multivariable analyses, a notable linear trend between their composite indicator 9-GCS and the risks of carotid atherosclerosis was observed. We identified four SNPs (rs9937354, rs10842993, rs7180016, and rs4383154) that exhibited significant independent effects with carotid atherosclerosis. Genes that are closely associated with these SNPs include FTO, PRC1, GP2, and KLHL42.
Several potential mechanisms of increased arterial stiffness and altered hemodynamics in DM have been implicated including the formation of advanced glycation endproducts (AGEs) and the dysregulation of nitric oxide (NO) 58 . The formation of AGE involves multiple reversible and irreversible steps, ultimately leading to the pathological binding of collagen molecules within the arterial vessel wall 59 . Numerous studies have linked AGEs to the acceleration of age-related vascular changes and the development of cardiovascular events in both diabetic and non-diabetic populations 60 . The presence of AGE-induced cross-links can make collagen highly resistant to enzymatic breakdown, resulting in a reduced degradation rate. This, in turn, contributes to the increased collagen content observed in arterial walls, which is a characteristic of aging and is further accelerated in conditions such as DM 61 . Research has shown a positive correlation between carotid-femoral pulse wave velocity and collagen crosslinking 62 . Moreover, the levels of specific AGEs in aortic tissue have been found to correlate with aortic stiffness in individuals with and without DM 63 . NO possesses various beneficial properties, including vasodilation, anti-platelet activity, anti-inflammatory effects, and antioxidant properties 64 . However, in the state of insulin resistance, the activation of NO synthase is impaired, and there is an increase in the production of superoxide. These factors together contribute to a decrease in the availability of NO 65 . In individuals with diabetes, particularly those with microvascular disease, basal levels of NO are reduced compared to those without such complications. Furthermore, the severity of microvascular disease correlates with a further decline in NO levels 66 . Further mechanical studies including gene-association studies based on our current findings will provide insight into finding therapeutic targets for atherosclerosis and related complications in DM patients.
The findings of this study highlight a noteworthy association between DM and changes in hemodynamic parameters. Adding hemodynamic parameters enhanced the predictabilities of the regression models on DM status. Gaining a deeper understanding of this relationship can aid in identifying individuals who are at a heightened risk of DM. Future follow-up and mechanical studies will enlighten us on factors that contribute to the development of vascular complications in DM patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Area under the receiver operating curve
Body mass index
Common carotid artery
Coronary heart disease
Total cholesterol
Confidence interval
Diastolic blood pressure
- Diabetes mellitus
End-diastolic velocity
Fasting plasma glucose
Fasting triglycerides
High-density lipoprotein cholesterol
Hip circumference
Low-density lipoprotein cholesterol
Mean blood flow velocity
- Pulsatility index
Peak systolic velocity
- Resistance index
Systolic blood pressure
Standard deviation
Standard error
Waist circumference
Waist-to-hip ratio
Wohlschlaeger, J., Bertram, S., Theegarten, D., Hager, T. & Baba, H. A. Coronary atherosclerosis and progression to unstable plaques : Histomorphological and molecular aspects. Herz 40 (6), 837–844 (2015).
Article PubMed Google Scholar
Falk, E. Pathogenesis of atherosclerosis. J. Am. Coll. Cardiol. 47 (8 Suppl), C7-12 (2006).
Article CAS PubMed Google Scholar
Summerhill, V. I., Grechko, A. V., Yet, S. F., Sobenin, I. A. & Orekhov, A. N. The atherogenic role of circulating modified lipids in atherosclerosis. Int. J. Mol. Sci. 20 (14), 3561 (2019).
Article CAS PubMed PubMed Central Google Scholar
Vasdev, S., Gill, V. & Singal, P. Role of advanced glycation end products in hypertension and atherosclerosis: Therapeutic implications. Cell Biochem. Biophys. 49 (1), 48–63 (2007).
Galis, Z. S., Sukhova, G. K., Lark, M. W. & Libby, P. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J. Clin. Invest. 94 (6), 2493–2503 (1994).
Robinson, J. G., Fox, K. M., Bullano, M. F., Grandy, S. & Group, S. S. Atherosclerosis profile and incidence of cardiovascular events: A population-based survey. BMC Cardiovasc. Disord. 9 , 1–8 (2009).
Article Google Scholar
Mozaffarian, D. et al. Executive summary: Heart disease and stroke statistics–2016 update: A report from the American heart association. Circulation 133 (4), 447–454 (2016).
Bortnick, A. E. et al. Biomarkers of mineral metabolism and progression of aortic valve and mitral annular calcification: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis 285 , 79–86 (2019).
Li, Y. H. et al. 2017 Taiwan lipid guidelines for high risk patients. J. Formos. Med. Assoc. 116 (4), 217–248 (2017).
Hastings, N. E., Simmers, M. B., McDonald, O. G., Wamhoff, B. R. & Blackman, B. R. Atherosclerosis-prone hemodynamics differentially regulates endothelial and smooth muscle cell phenotypes and promotes pro-inflammatory priming. Am. J. Physiol. Cell Physiol. 293 (6), C1824-1833 (2007).
Glagov, S., Zarins, C., Giddens, D. P. & Ku, D. N. Hemodynamics and atherosclerosis. Insights and perspectives gained from studies of human arteries. Arch. Pathol. Lab. Med. 112 (10), 1018–1031 (1988).
CAS PubMed Google Scholar
Malek, A. M., Alper, S. L. & Izumo, S. Hemodynamic shear stress and its role in atherosclerosis. JAMA 282 (21), 2035–2042 (1999).
Wong, K. K. L., Wu, J., Liu, G., Huang, W. & Ghista, D. N. Coronary arteries hemodynamics: Effect of arterial geometry on hemodynamic parameters causing atherosclerosis. Med. Biol. Eng. Comput. 58 (8), 1831–1843 (2020).
Gosling, R. G. & King, D. H. Arterial assessment by doppler-shift ultrasound. Proc. R. Soc. Med. 67 (6 Pt 1), 447–449 (1974).
CAS PubMed PubMed Central Google Scholar
George, P., Pourcelot, L., Fourcade, C., Guillaud, C. & Descotes, J. The Doppler effect and measurement of the blood flow. C R Acad. Hebd. Seances Acad. Sci. D 261 (1), 253–256 (1965).
Wielicka, M., Neubauer-Geryk, J., Kozera, G. & Bieniaszewski, L. Clinical application of pulsatility index. Med. Res. J. 5 (3), 201–210 (2020).
Kharroubi, A. T. & Darwish, H. M. Diabetes mellitus: The epidemic of the century. World J. Diabetes 6 (6), 850–867 (2015).
Article PubMed PubMed Central Google Scholar
Stancakova, A. et al. Changes in insulin sensitivity and insulin release in relation to glycemia and glucose tolerance in 6414 Finnish men. Diabetes 58 (5), 1212–1221 (2009).
Saeedi, P. et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 157 , 107843 (2019).
Grant, P. J. & Cosentino, F. The 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 40 (39), 3215–3217 (2019).
Katsiki, N. & Mikhailidis, D. P. Diabetes and carotid artery disease: A narrative review. Ann. Transl. Med. 8 (19), 1280 (2020).
Wu, T. W., Chou, C. L., Cheng, C. F., Lu, S. X. & Wang, L. Y. Prevalences of diabetes mellitus and carotid atherosclerosis and their relationships in middle-aged adults and elders: A community-based study. J. Formos. Med. Assoc. 121 (6), 1133–1140 (2022).
Wu, T. W. et al. Associations of genetic markers of diabetes mellitus with carotid atherosclerosis: A community-based case-control study. Cardiovasc. Diabetol. 22 (1), 51 (2023).
Lau, K. K. et al. Age and sex-specific associations of carotid pulsatility with small vessel disease burden in transient ischemic attack and ischemic stroke. Int. J. Stroke 13 (8), 832–839 (2018).
Lee, K. Y., Sohn, Y. H., Baik, J. S., Kim, G. W. & Kim, J. S. Arterial pulsatility as an index of cerebral microangiopathy in diabetes. Stroke 31 (5), 1111–1115 (2000).
Dikanovic, M. et al. Transcranial Doppler ultrasound assessment of intracranial hemodynamics in patients with type 2 diabetes mellitus. Ann. Saudi Med. 25 (6), 486–488 (2005).
Wu, T. W. et al. Differential patterns of effects of age and sex on metabolic syndrome in Taiwan: implication for the inadequate internal consistency of the current criteria. Diabetes Res. Clin. Pract. 105 (2), 239–244 (2014).
Chou, C. L. et al. Segment-specific prevalence of carotid artery plaque and stenosis in middle-aged adults and elders in Taiwan: A community-based study. J. Formos Med. Assoc. 118 (1 Pt 1), 64–71 (2019).
Clogg, C. C., Petkova, E. & Haritou, A. Statistical methods for comparing regression coefficients between models. Am. J. Sociol. 100 (5), 1261–1293 (1995).
Climie, R. E. et al. Measuring the interaction between the macro- and micro-vasculature. Front. Cardiovasc. Med. 6 , 169 (2019).
Kang, J. et al. Relationship between brachial-ankle pulse wave velocity and invasively measured aortic pulse pressure. J. Clin. Hypertens (Greenwich) 20 (3), 462–468 (2018).
Weber, T., Wassertheurer, S., Hametner, B., Parragh, S. & Eber, B. Noninvasive methods to assess pulse wave velocity: Comparison with the invasive gold standard and relationship with organ damage. J. Hypertens. 33 (5), 1023–1031 (2015).
Yamashina, A. et al. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens. Res. 25 (3), 359–364 (2002).
Chuang, S. Y. et al. Blood pressure, carotid flow pulsatility, and the risk of stroke: A community-based study. Stroke 47 (9), 2262–2268 (2016).
van Sloten, T. T. et al. Carotid stiffness is associated with incident stroke: A systematic review and individual participant data meta-analysis. J. Am. Coll. Cardiol. 66 (19), 2116–2125 (2015).
Chuang, S. Y. et al. Common carotid end-diastolic velocity and intima-media thickness jointly predict ischemic stroke in Taiwan. Stroke 42 (5), 1338–1344 (2011).
Chuang, S. Y. et al. Common carotid artery end-diastolic velocity is independently associated with future cardiovascular events. Eur. J. Prev. Cardiol. 23 (2), 116–124 (2016).
Asil, T., Uzunca, I., Utku, U. & Berberoglu, U. Monitoring of increased intracranial pressure resulting from cerebral edema with transcranial Doppler sonography in patients with middle cerebral artery infarction. J. Ultrasound Med. 22 (10), 1049–1053 (2003).
Hitsumoto, T. Relationships between the cardio-ankle vascular index and pulsatility index of the common carotid artery in patients with cardiovascular risk factors. J. Clin. Med. Res. 11 (8), 593–599 (2019).
Cho, S. J., Sohn, Y. H., Kim, G. W. & Kim, J. S. Blood flow velocity changes in the middle cerebral artery as an index of the chronicity of hypertension. J. Neurol. Sci. 150 (1), 77–80 (1997).
Bardelli, M., Jensen, G., Volkmann, R. & Aurell, M. Non-invasive ultrasound assessment of renal artery stenosis by means of the Gosling pulsatility index. J. Hypertens. 10 (9), 985–989 (1992).
Sasaki, N., Yamamoto, H., Ozono, R., Maeda, R. & Kihara, Y. Association of common carotid artery measurements with n-terminal pro b-type natriuretic peptide in elderly participants. Intern. Med. 59 (7), 917–925 (2020).
Rustempasic, N. & Gengo, M. Assesment of carotid stenosis with CT angiography and color doppler ultrasonography. Med. Arch. 73 (5), 321–325 (2019).
Vigen, T. et al. Carotid atherosclerosis is associated with middle cerebral artery pulsatility index. J. Neuroimaging 30 (2), 233–239 (2020).
Wong, N. D. et al. Atherosclerotic cardiovascular disease risk assessment: An American Society for Preventive Cardiology clinical practice statement. Am. J. Prev. Cardiol. 10 , 100335 (2022).
Bytyci, I., Shenouda, R., Wester, P. & Henein, M. Y. Carotid atherosclerosis in predicting coronary artery disease: A systematic review and meta-analysis. Arterioscler. Thromb. Vasc. Biol. 41 (4), e224–e237 (2021).
Dec-Gilowska, M. et al. Circulating endothelial microparticles and aortic stiffness in patients with type 2 diabetes mellitus. Medicina 55 (9), 596 (2019).
Climie, R. E. D. et al. Pulsatile interaction between the macro-vasculature and micro-vasculature: Proof-of-concept among patients with type 2 diabetes. Eur. J. Appl. Physiol. 118 (11), 2455–2463 (2018).
Soyoye, D. O. et al. Relationship between renal doppler indices and biochemical indices of renal function in type 2 diabetes mellitus. West Afr. J. Med. 35 (3), 189–194 (2018).
Fukuhara, T. & Hida, K. Pulsatility index at the cervical internal carotid artery as a parameter of microangiopathy in patients with type 2 diabetes. J. Ultrasound Med. 25 (5), 599–605 (2006).
Janssen, A. Pulsatility index is better than ankle-brachial doppler index for non-invasive detection of critical limb ischaemia in diabetes. Vasa 34 (4), 235–241 (2005).
Kozera, G. M. et al. Cerebral and skin microcirculatory dysfunction in type 1 diabetes. Postepy Dermatol. Alergol. 36 (1), 44–50 (2019).
Onmez, A., Gokosmanoglu, F., Baycelebi, G. & Arikan, A. A. Carotid Doppler ultrasonographic findings of dapagliflozin use in type 2 diabetic patients. Aging Male 23 (5), 1246–1250 (2020).
Park, J. S. et al. The effects of pioglitazone on cerebrovascular resistance in patients with type 2 diabetes mellitus. Metabolism 56 (8), 1081–1086 (2007).
Agha, M. S. & Alboudi, A. Arterial pulsatility as an index of cerebral microangiopathy in diabetes type 2. East Mediterr. Health J. 19 (Suppl 3), S198-203 (2014).
PubMed Google Scholar
Park, J. S. et al. Cerebral arterial pulsatility and insulin resistance in type 2 diabetic patients. Diabetes Res. Clin. Pract. 79 (2), 237–242 (2008).
Zou, C. et al. Differences between healthy adults and patients with type 2 diabetes mellitus in reactivity of toe microcirculation by ultrasound combined with a warm bath test. Med. (Baltimore) 96 (22), e7035 (2017).
Prenner, S. B. & Chirinos, J. A. Arterial stiffness in diabetes mellitus. Atherosclerosis 238 (2), 370–379 (2015).
Powell, J. T., Vine, N. & Crossman, M. On the accumulation of D-aspartate in elastin and other proteins of the ageing aorta. Atherosclerosis 97 (2–3), 201–208 (1992).
Sell, D. R. & Monnier, V. M. Molecular basis of arterial stiffening: role of glycation - a mini-review. Gerontology 58 (3), 227–237 (2012).
Schnider, S. L. & Kohn, R. R. Effects of age and diabetes mellitus on the solubility and nonenzymatic glucosylation of human skin collagen. J. Clin. Invest. 67 (6), 1630–1635 (1981).
Monnier, V. M. et al. Relation between complications of type I diabetes mellitus and collagen-linked fluorescence. N. Engl. J. Med. 314 (7), 403–408 (1986).
Sims, T. J., Rasmussen, L. M., Oxlund, H. & Bailey, A. J. The role of glycation cross-links in diabetic vascular stiffening. Diabetologia 39 (8), 946–951 (1996).
Kawashima, S. The two faces of endothelial nitric oxide synthase in the pathophysiology of atherosclerosis. Endothelium 11 (2), 99–107 (2004).
Du, X. et al. Insulin resistance reduces arterial prostacyclin synthase and eNOS activities by increasing endothelial fatty acid oxidation. J. Clin. Invest. 116 (4), 1071–1080 (2006).
Brillante, D. G., O’Sullivan, A. J., Johnstone, M. T. & Howes, L. G. Arterial stiffness and haemodynamic response to vasoactive medication in subjects with insulin-resistance syndrome. Clin. Sci. (Lond) 114 (2), 139–147 (2008).
Download references
Acknowledgements
We thank the staff in the district health station of Tamsui District, Sanzhi District, and Shimen District, New Taipei City, for their administrative support.
This work was supported by research grants from the Council of Science and Technology of Taiwan (MOST 111-2314-B-715-007 & NSTC 112-2314-B-715-007-MY3) and MacKay Medical College (MMC-RD-110-1B-P010 & MMC-RD-111-1B-P007). The funding agencies played no role in the research.
Author information
Authors and affiliations.
Department of Medicine, MacKay Medical College, No. 46, Sec. 3, Jhong-Jheng Rd., San-Jhih District, New Taipei City, Taiwan
Tzu-Wei Wu, Yih-Jer Wu, Chao-Liang Chou & Li-Yu Wang
Institute of Biomedical Sciences, MacKay Medical College, New Taipei City, Taiwan
Cardiovascular Center, Department of Internal Medicine, MacKay Memorial Hospital, Taipei, Taiwan
Department of Medical Research, MacKay Memorial Hospital, Taipei, Taiwan
Department of Neurology, MacKay Memorial Hospital, New Taipei City, Taiwan
Chao-Liang Chou & Shu-Xin Lu
Tamsui Health Station, Department of Health, New Taipei City Government, New Taipei City, Taiwan
Chun-Fang Cheng
You can also search for this author in PubMed Google Scholar
Contributions
T.W.W. developed the study design, analyzed and interpreted data, and wrote the manuscript. Y.J.W. interpreted the results, contributed to the discussion, and revised the manuscript. C.L.C., C.F.C., and S.X.L. contributed to the study design, interpreted results, and discussion. L.Y.W. developed the study design, analyzed data, interpreted data, wrote the manuscript, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Tzu-Wei Wu or Li-Yu Wang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wu, TW., Wu, YJ., Chou, CL. et al. Hemodynamic parameters and diabetes mellitus in community-dwelling middle-aged adults and elders: a community-based study. Sci Rep 14 , 12032 (2024). https://doi.org/10.1038/s41598-024-62866-7
Download citation
Received : 11 February 2024
Accepted : 22 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1038/s41598-024-62866-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Carotid blood flow
- Case-control study
- Community-based
- Hemodynamics
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Assessment of Deafness in Term Infants with Birth Asphyxia with Otoacoustic Emission and Brain Stem Evoked Response Audiometry: A Prospective Observational Study
- Original Article
- Published: 22 May 2024
Cite this article

- Reshma P. Chavan ORCID: orcid.org/0000-0002-4267-7285 1 ,
- Sujit M. Shivsharan 1 &
- Akshay B. Nalte 1
19 Accesses
Explore all metrics
To assess deafness in term infant with birth asphyxia by otoacoustic emission and brain stem evoked response audiometry. A Prospective observational study was done at Tertiary care government hospital from 15/02/2021 to 15/10/2022.Total 130 patients were included in the study by consecutive sampling method. All the patients fulfilling the inclusion criteria during the study period were included. After explaining the aims, objectives and methods of study, written informed consent was obtained from the parents to undergo Otoacoustic Emission (OAE) and Brain Stem Evoked Response Audiometry Test (BERA). Data was entered in case record form. Collected data was analysed by appropriate statistical methods. Hearing impairment was present in eight (6.15%) asphyxiated term infants. A mild degree of hearing loss was seen in three (37.5%), a moderate degree of hearing loss was seen in four (50%), severe degree of hearing loss was seen in one (12.5%) asphyxiated term infant. In asphyxiated term infants, no significant difference in hearing loss was seen with respect to gender, Obstetrics history, and type of delivery. Significant difference in hearing loss was seen in antenatal Diabetes mellitus, hypertension, family history of SNHL and APGAR Score less than 6. Severe degree of hearing loss was seen in prolonged labour and HTN mother. Significant difference in hearing loss was seen in antenatal Diabetes mellitus, hypertension, family history of SNHL and APGAR Score less than 4 and 6 in one and five minutes respectively. Severe degree of hearing loss was seen in prolonged labour and HTN mother.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
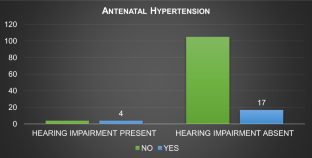
Similar content being viewed by others
Hearing impairment and its risk factors by newborn screening in north-western india.
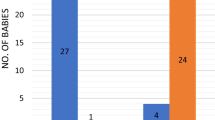
Assessment of Otoacoustic Emissions (OAE) in Birth Asphyxiated Neonates

The Hearing Status of Preterm Infant’s ≤ 34 Weeks as Revealed by Otoacoustic Emissions (OAE) Screening and Diagnostic Brainstem Evoked Response Audiometry (BERA): A Tertiary Center Experience
Mishra G, Sharma Y, Mehta K, Patel G (2013) Efficacy of distortion product oto-acoustic emission (OAE)/auditory brainstem evoked response (ABR) protocols in universal neonatal hearing screening and detecting hearing loss in children <2 years of age. Indian J Otolaryngol Head Neck Surg 65(2):105–110
Article PubMed Google Scholar
Sachdeva K, Sao T (2017) Outcomes of newborn hearing screening program: a hospital based study. Indian J Otolaryngol Head Neck Surg 69(2):194–198
Article PubMed PubMed Central Google Scholar
Wroblewska-Seniuk KE, Dabrowski P, Szyfter W, Mazela J (2016) Universal newborn hearing screening: methods and results, obstacles, and benefits. Pediatr Res 81(3):415–422. https://doi.org/10.1038/pr.2016.250
Parving A (1993) Congenital hearing disability: epidemiology and identification: a comparison between two health authority districts. Int J Pediatr Otorhinolaryngol 27:29–46
Article CAS PubMed Google Scholar
Kim SY, Bothwell NE, Backous DD (2002) The expanding role of the otolaryngologist in managing infants and children with hearing loss. Otolaryngol Clin N Am 35(4):699–710
Article Google Scholar
White KR, Maxon AB (1995) Universal screening for infant hearing impairment: simple, beneficial, and presently justified. Int J Pediatric Otorhinolaryngol 32(3):201–211. https://doi.org/10.1016/0165-5876(95)01165-8
Article CAS Google Scholar
Aradhana A, Sarangi G, Saboth P, Tripathy R (2020) Assessment of hearing impairment in NICU graduates by otoacoustic emission and brainstem evoked response audiometry tests. J Neonatol 34(3):109–117
Wilson DF, Hodgson RS, Gustafson MF, Hogue S, Mills L (1992) The sensitivity of auditory brainstem response testing in small acoustic neuromas. Laryngoscope 102(9):961–964
Sharma P, Chhangani NP, Meena KR et al (2006) Brainstem evoked response audiometry (BAER) in infants with hyperbilirubinemia. Indian J Pediatr 73(5):413–416
Yousefi J, Ajalloueyan M, Amirsalari S, Hassanali Fard M (2013) The specificity and sensitivity of transient otoacustic emission in neonatal hearing screening compared with diagnostic test of auditory brain stem response in tehran hospitals. Iran J Pediatr 23(2):199–204
PubMed PubMed Central Google Scholar
Amini E, Kasheh Farahani Z, Rafiee Samani M et al (2014) Assessment of hearing loss by OAE in asphyxiated newborns. Iran Red Crescent Med J 16(1):e6812. https://doi.org/10.5812/ircmj.6812
Singh R, Vates E. Brainstem Auditory Evoked Response Test. [Updated 2023 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK597358
Eiserman WD, Hartel DM, Shisler L, Buhrmann J, White KR, Foust T (2008) Using otoacoustic emissions to screen for hearing loss in early childhood care settings. Int J pediatr otorhinolaryngol 72(4):475–482
Davis A, Wood S (1992) The epidemiology of childhood hearing impairment: factors relevant to planning of services. Br J Audiol 26(2):77–90
Pourarian S, Khademi B, Pishva N, Jamali A (2012) Prevalence of hearing loss in newborns admitted to neonatal intensive care unit. Iran J otorhinolaryngol 24(68):129
Kilickan L, Gürkan Y, Aydin Ö, Etiler N (2003) The effect of combined spinal-epidural (CSE) anaesthesia and size of spinal needle on postoperative hearing loss after elective caesarean section. Clin Otolaryngol Allied Sci 28(3):267–272
Ohl C, Dornier L, Czajka C, Chobaut JC, Tavernier L (2009) Newborn hearing screening on infants at risk. Int J Pediatr Otorhinolaryngol 73(12):1691–1695
Thornberg E, Thiringer K, Odeback A, Milsom I (1995) Birth asphyxia: incidence, clinical course and outcome in a Swedish population. Acta Paediatr 84(8):927–932
Alfirevic Z, Devane D, Gyte GM, Cuthbert A (2017) Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labor. Cochrane Database Syst Rev, 2: CD006066.
Bahl R (2010) Newborn and infant hearing screening. In: Kocur I (ed) Current issues and guiding principles for action. WHO Press, Geneva
Google Scholar
World Health Organization (WHO). Situation review and update on deafness, hearing loss and intervention programs proposed plans of action for prevention and alleviation of hearing impairment in countries of the South East Asia Region. New Delhi WHO Regional Office for South East Asia; 2007.
Yoshinaga Itano C, Sedey AL, Coulter DK, Mehl AL (1998) Language of early and later identified children with hearing loss. Pediatrics 102(5):1161–1171
Yoshinaga-Itano C (1995) Efficacy of early identification and intervention. Semin Hear 16:115–120
Martines F, Porrello M, Ferrara M, Martines M, Martines E (2007) Newborn hearing screening project using transient evoked otoacoustic emissions: western sicily experience. Int J Pediatr Otorhinolaryngol 71(1):107–112
Martines F, Bentivegna D, Ciprì S, Costantino C, Marchese D, Martines E (2012) On the threshold of effective well infant nursery hearing screening in Western Sicily. Int J Pediatr Otorhinolaryngol 76(3):423–427
Salvago P, Martines E, Martines F (2013) Prevalence and risk factors for sensorineural hearing loss: western sicily overview. Eur Arch Otorhinolaryngol 270(12):3049–3056
Pawar R, Illalu S, Fattepur SR (2019) A study on prevalence of hearing impairment in newborns with birth asphyxia admitted to neonatal intensive care unit. Int J Pediatr Res 6(1):42–49
Meqbel AL, AS, Al BAGHLI HA, (2015) The prevalence of hearing impairment in high-risk infants in Kuwait. Aud Vest Res 24(1):11–16
Bakhshaee M, Boskabadi H, Hassanzadeh M, Nourizadeh N, Ghassemi MM, Khazaeni K, Moghiman T, Tale MR (2008) Hearing impairment in the neonate of preeclamptic women. Otolaryngol Head Neck Surg 139(6):846–849
Amini E, Kasheh Farahani Z, Rafiee Samani M, Hamedi H, Zamani A, Karimi Yazdi A, Nayeri F, Nili F, Rezaeizadeh G (2014) Assessment of hearing loss by OAE in asphyxiated newborns. Iran Red Crescent Med J 16(1):e6812
Stanton SG, Ryerson E, Moore SL, Sullivan-Mahoney M, Couch SC (2005) Hearing screening outcomes in infants of pregestational diabetic mothers. Am J Audiol 14(1):86–93
Zhou JH, Yu K, Ding H, Zhu ZH, Han LH, Zhang T (2021) A clinical study on gestational diabetes mellitus and the hearing of newborns. Diabet Metab Syndr Obes Targets Ther 14:2879
Kountakis SE, Skoulas I, Phillips D, Chang CJ (2002) Risk factors for hearing loss in neonates: a prospective study. Am J Otolaryngol 23(3):133–137
Ewart-Toland A, Yankowitz J, Winder A, Imagire R, Cox VA, Aylsworth AS et al (2000) Oculoauriculovertebral abnormalities in children of diabetic mothers. Am J Med Genet 90(4):303–309
Alan C, Alan MA (2021) Maternal hypertension, pre-eclampsia, eclampsia and newborn hearing: a retrospective analysis of 454 newborns. Int J Pediatr Otorhinolaryngol 146:110748
Kattah AG, Garovic VD (2013) The management of hypertension in pregnancy. Adv Chronic Kidney Dis 20(3):229–239. https://doi.org/10.1053/j.ackd.2013.01.014
Berg CJ, Callaghan WM, Syverson C, Henderson Z (2010) Pregnancy-related mortality in the United States, 1998 to 2005. Obstet Gynecol 9(3):1302–1309
Tabrizi AG, Asadi M, Naini AS (2016) Preeclamsia: A New Risk Factor for Hearing Loss. Biomed Pharmacol J 9(3):1135–1138
Bakhshaee M, Hassanzadeh M, Nourizadeh N, Karimi E, Moghiman T, Shakeri M (2008) Hearing impairment in pregnancy toxemia. Otolaryngol Head Neck Surg 139(2):298–300. https://doi.org/10.1016/j.otohns.2008.04.016
Kunnath AZ, Aboobakker ASC, Kunjimon BN, Sreedhar S (2021) Hearing impairment among high risk neonates born in a tertiary care hospital in north Kerala–a cross sectional study. Int J Otorhinolaryngol Head Neck Surg 7:452–458
Gouri ZU, Sharma D, Berwal PK, Pandita A, Pawar S (2015) Hearing impairment and its risk factors by newborn screening in north-western India. Matern health, neonatol perinatol 1(1):1–7
Binay C, Kavuncuoglu S, Fidan V, Binay O, Altuncu E, Taskin U (2016) Screening for abnormal hearing in newborns and assessment of high-risk group. Austin J Otolaryngol. 3(2):1073
Regina M, Moideen SP, Mohan M, Mohammed MT, Afroze KH (2017) Audiological screening of high risk infants and prevalence of risk factors. Int J Contemp Pediatr. 4(2):507–511
Sun P, Liang Y, Tan M, Yuan Y, Yang C, Liu Y et al (2015) Correlation between risk factors of hearing lose and results of initial hearing screening in 1021 neonates. J Clinical Otorhinolaryngology Head Neck Surg 29(10):893–898
American Academy of Paediatrics (2007) Years 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Paediatrics 120(4):898
Beswick R, Driscoll C, Kei J (2012) Monitoring for postnatal hearing loss using risk factors: a systematic literature review. Ear Hearing 33(6):745–756
Güven SG (2019) The effect of mode of delivery on newborn hearing screening results. Turk Arch Otolaryngol 57(1):19–23
Shahid R, Vigilante M, Deyro H, Reyes I, Gonzalez B, Kliethermes S (2016) Risk factors for failed newborn otoacoustic emissions hearing screen. Clin Pediatr 55(12):1138–1142
Olusanya BO (2009) Newborns at risk of sensorineural hearing loss in low-income countries. Arch Dis Child 94(3):227–230
Xiao T, Li Y, Xiao L, Jiang L, Hu Q (2015) Association between mode of delivery and failure of neonatal acoustic emission test: a retro-spective analysis. Int J Pediatr Otorhinolaryngol 79(4):516–519
Roth DA, Hildesheimer M, Maayan-Metzger A, Muchnik C, Hamburger A, Mazkeret R, Kuint J (2006) Low prevalence of hearing impairment among very low birthweight infants as detected by universal neonatal hearing screening. Arch Dis Child Fetal Neonatal Ed 91(4):F257–F262
Article PubMed Central Google Scholar
Poonual W, Navacharoen N, Kangsanarak J, Namwongprom S (2016) Risk factors for hearing loss in infants under universal hearing screening program in Northern Thailand. J Multidiscip Healthc 9:1–5
PubMed Google Scholar
Joint Committee on Infant Hearing, American Academy of Audiology, American Academy of Pediatrics et al (2000) position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics 106(4):798–817
Baradaranfar M, Mehrparvar A, Mostagahci M, Mollasadeghi A, Naghshineh E, Davari M (2014) Hearing abnormality in neonate intensive care unit (NICU). Yazd-Iran Int J Pediatr 2(2):113–117
Nagapoornima P, Ramesh A, Rao S et al (2007) Universal hearing screening. Indian J Pediatr 74(6):545–549
John M, Balraj A, Kurien M (2009) Neonatal screening for hearing loss: pilot study from a tertiary care centre. Indian J Otolaryngol Head Neck Surg 61(1):23–26
Article CAS PubMed PubMed Central Google Scholar
Rance G (2005) Auditory neuropathy/dys-synchrony and its perceptual consequences. Trends in Amplif 9(1):1–43
Vare R et al (2022) Neonatal hearing screening programme-efficacy of otoacoustic emissions in detecting hearing loss. Int J Recent Sci Res 13(04):984–988
Heikkinen T (2001) The role of respiratory viruses in otitis media. Vaccine 19:S51–S55
Sano S, Kamide Y, Schachern PA, Paparella MM (1994) Micropathologic changes of pars tensa in children with otitis media with effusion. Arch Otolaryngol Head Neck Surg 120:815–819
Heikkinen T, Thint M, Chonmaitree T (1999) Prevalence of various respiratory viruses in the middle ear during acute otitis media. N Engl J Med 340:260–264
Olusanya BO, Davis AC, Hoffman HJ (2019) Hearing loss grades and the International classification of functioning, disability and health. Bull World Health Organ 97(10):725–728. https://doi.org/10.2471/BLT.19.230367
Ramanjaneyulu J, Kumar SR, Chaitanya VK, Kusumanjali A (2021) Oto acoustic emissions in early detection of sensorineural hearing loss in high-risk neonates. Int J Otorhinolaryngol Head Neck Surg 7:1794–1798
Labaeka AA, Tongo OO, Ogunbosi BO, Fasunla JA (2018) Prevalence of hearing impairment among high-risk newborns in Ibadan. Nigeria Frontiers in pediatrics 6:194
Hess M, Finckh-Krumer U, Bartsch M, Kewitz G, Versmold H, Gross M (1998) Hearing screening in at-risk neonate cohort. Int J Pediatr Otorhinolaryngol 46(1–2):81–89
Download references
Author information
Authors and affiliations.
Department of ENT, GMC Miraj, Miraj, Maharashtra, India
Reshma P. Chavan, Sujit M. Shivsharan & Akshay B. Nalte
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Reshma P. Chavan .
Ethics declarations
Conflict of interest.
Ethical Approval
Ethical Approval was taken by Institutional Ethical Board as per ICMR guidelines by letter no. GMCM/IEC-C/7/2021.
Human and Animal Rights
This article is a retrospective analysis of data and does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed Consent was obtained from parents of all Infants included in the study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (XLSX 32 KB)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Chavan, R.P., Shivsharan, S.M. & Nalte, A.B. Assessment of Deafness in Term Infants with Birth Asphyxia with Otoacoustic Emission and Brain Stem Evoked Response Audiometry: A Prospective Observational Study. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-04736-2
Download citation
Received : 01 January 2024
Accepted : 29 April 2024
Published : 22 May 2024
DOI : https://doi.org/10.1007/s12070-024-04736-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Otoacoustic emission
- Brain stem evoked response audiometry
- Hearing loss
- Hearing assessment
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World J Cardiol
- v.15(6); 2023 Jun 26
- PMC10308268
Virtual patient education for hypertension: The truth about behavioral change
Zeynep yukselen.
Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States
School of Public Health and Health Sciences, University of Massachusetts, Amherst, MA 01003, United States. ude.ssamu@neleskuyz
Yuvaraj Singh
Sarat malempati, mahati dasari, pramukh arun kumar, eddison ramsaran.
Department of Cardiovascular Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States
Corresponding author: Zeynep Yukselen, BSc, MD, Doctor, Department of Internal Medicine, Saint Vincent Hospital, 123 Summer St., Worcester, MA 01608, United States. ude.ssamu@neleskuyz
Anti-hypertensive education is an important public health intervention to decrease the mortality and burden of the disease. Using digital technologies for education as a part of preventive measures for hypertension is a cost-effective approach and helps low-income communities and vulnerable populations overcome barriers to healthcare access. The coronavirus disease 19 pandemic further highlighted the need of new health interventions to address health inequalities. Virtual education is helpful to improve awareness, knowledge, and attitude toward hypertension. However, given the complexity of behavioral change, educational approaches do not always provide a change in behavior. Some of the obstacles in online hypertensive education could be time limitations, not being tailored to individual needs and not including the different elements of behavioral models to enhance behavior change. Studies regarding virtual education should be encouraged and involve lifestyle modifications emphasizing the importance of Dietary Approaches to Stop Hypertension diet, salt restriction, and exercise and should be used adjunct to in-person visits for the management of hypertension. Additionally, to stratify patients according to hypertension type (essential or secondary) would be useful to create specific educational materials. Virtual hypertension education is promising to increase awareness regarding risk factors and most importantly motivate patients to be more compliant with management helping to decrease hypertension related complications and hospitalizations.
Core Tip: Online anti-hypertensive education can play an important role in preventing and managing hypertension by providing individuals with the knowledge and resources they need to make lifestyle changes. Hypertensive management and education can be difficult in certain populations due to lack of access to healthcare, lack of information, and social determinants of health. Virtual education would promote health in those vulnerable populations.
TO THE EDITOR
In a recent article titled “Impact of the virtual anti-hypertensive educational campaign towards knowledge, attitude, and practice of hypertension management during the COVID-19 pandemic”, Andrianto et al [ 1 ] emphasized the importance of online education in patients with hypertension[ 1 ]. Given the burden of hypertension, we found this article very interesting and promising for health promotion. Hypertension has been described as the "largest epidemic ever known to mankind"[ 2 ]. In the United States, nearly half of the adults have hypertension, and only 25% are under control[ 3 ]. Being an epidemic globally, it’s not surprising that the economic burden of hypertension is enormous. In the United States itself, hypertension costs about $131 billion each year[ 4 ]. From the public health intervention perspective, Andrianto et al 's study is brilliant as we believe that one of the ways to cut the cost of hypertension is community-based interventions, such as health education and support groups, which can help reduce the cost of hypertension by providing individuals with the information and resources they need to manage their condition effectively[ 1 ].
As highlighted by the authors, overall, the coronavirus disease 19 (COVID-19) pandemic has had a significant impact on health disparities and healthcare access[ 5 ]. Even in the non-COVID era, patients with low economic status have been disproportionately affected by hypertension. The Prospective Urban Rural Epidemiology study, including patients from 17 countries on five continents, showed that awareness, diagnosis, and control of hypertension were lower in low-income countries compared with other countries and in rural settings compared with urban areas[ 6 ]. Considering the disadvantages of the vulnerable population, the COVID-19 pandemic highlighted the importance of addressing health disparities to ensure that all individuals have access to the care they need. Some of the difficulties in the population-level management of hypertension for minorities are barriers to healthcare, awareness, and understanding of the importance of monitoring, which is often linked to social determinants of health such as poverty, cultural beliefs, illiteracy, discrimination, and language barriers[ 7 ].
In the current era, the increasing use of mobile applications and telemedicine for communication has the potential to bridge disparities and play a significant role in managing hypertension in outpatient settings. A study by Freund et al [ 8 ] suggests that even elderly patients can effectively use online interventions as an inexpensive way to find answers to their health-related questions and improve their medical knowledge[ 8 ]. To address the global burden of hypertension, the Lancet commission encourages governments, pharmaceutical companies, healthcare professionals, and professional societies to develop simple mobile apps and online education programs to provide equal basic health access to people in low-income and middle-income countries[ 9 ]. In sync with this concept, the study conducted by Andrianto et al [ 1 ] reveals the importance of anti-hypertensive education in lower-middle-income countries. They found that virtual anti-hypertensive educational campaign implementation led to a significant improvement in the knowledge and attitude of patients with hypertension; however, it did not reflect a change in patient practice in taking measures against hypertension[ 1 ].
We are curious as to why a prospective study such as this with robust methodology could detect an improvement in facets of hypertension management but could not alter patient behavior. The education provided by Andrianto et al [ 1 ] was mainly directed toward the Dietary Approaches to Stop Hypertension (DASH), which is known as one of the most effective dietary interventions to lower blood pressure (BP)[ 1 , 10 ]. While dietary changes constitute a part of the non-pharmacologic therapy of hypertension, trials have shown that DASH dietary pattern reduced BP by 6/4 mmHg compared to a typical American-style diet[ 11 ]. Interestingly, and contrary to popular belief, dietary salt restriction is not a constituent of the original DASH dietary approach. In a systematic review of well-controlled randomized control trials, sodium restriction was associated with a reduction of BP by 4.8/2.5 mmHg in hypertensive and 1.9/1.1 mmHg in normotensive patients, respectively[ 12 ]. The benefits of dietary sodium restriction coupled with the DASH approach were only later studied[ 10 ]. Given the heterogeneity in the approach, we would like to know how much emphasis was placed on salt restriction education in the population. Further, the authors set the level of significance for practice-changing reduction of systolic BP at 10 mmHg. It is possible that since the primary education was directed at dietary changes amongst the non-pharmacologic measures, this reduction was not detected due to a higher set threshold. Upon reviewing Table 1 of the study, it appears that the intervention did not educate heavily on the importance of physical activity and weight loss. Multiple studies have shown that weight loss effectively reduces systolic blood pressure (SBP) and diastolic BP, and 10 kg of weight loss may lower SBP by 5 to 20 mmHg[ 13 , 14 ]. Integrating this could have potentially led to detecting a significant change in behavior. This is important, especially since a sedentary lifestyle is a well-known contributor to hypertension, accelerated due to the restrictions and lockdown measures during the COVID-19 pandemic.
The other reason could be a limited time of education and a lack of other intervention components. According to the behavior change wheel model, ten different intervention functions have been suggested, some of them being education, incentivization, persuasion, training, and enablement[ 15 ]. Given the complexity of behavior change required in hypertension; applying those intervention elements, such as providing patient-centered, tailored information and feedback by the healthcare professionals, would be required. Virtual education can also be tailored to an individual's specific needs and preferences. For example, some virtual programs may offer personalized meal and exercise plans, while others may provide resources and support for stress management or medication management. Although the study by Andrianto et al [ 1 ] did not show a major behavior change, it greatly impacted the patient’s perception towards not stopping medications when the BP is under control. This is another achievement of this study, as patients obtained that awareness after education.
Lastly, we noticed that the inclusion criteria were all patients with a diagnosis of hypertension. Did the authors sub-stratify their findings for the etiology of hypertension (essential vs secondary)? It would be valuable to learn how many patients amongst the included 110 participants had secondary/renovascular etiology of hypertension, especially since Table 2 indicates that 30 participants were < 40 years, which is when secondary hypertension is more prevalent. Both pharmacologic and non-pharmacologic measures differ for secondary hypertension and could be a reason for not reflecting in the behavioral change of patients.
To conclude, this randomized clinical trial has nicely addressed the importance of virtual hypertension education in the current pandemic, showing an impact on knowledge and attitude specifically. Future studies could focus on the effect of behavior coaching and personalized interventions such as texting patients or following up via telemedicine by healthcare providers to change behavior on medication adherence, lifestyle, and BP monitoring. These interventions would make an impactful effect on health promotion when used as an adjunct to management of hypertension and reduce the risk of complications and hospitalizations.
Conflict-of-interest statement: The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: March 19, 2023
First decision: April 28, 2023
Article in press: May 22, 2023
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Freund O, Israel; Tostes RC, Brazil S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
Contributor Information
Zeynep Yukselen, Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States. School of Public Health and Health Sciences, University of Massachusetts, Amherst, MA 01003, United States. ude.ssamu@neleskuyz .
Yuvaraj Singh, Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States.
Sarat Malempati, Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States.
Mahati Dasari, Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States.
Pramukh Arun Kumar, Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States.
Eddison Ramsaran, Department of Cardiovascular Medicine, Saint Vincent Hospital, Worcester, MA 01608, United States.

IMAGES
VIDEO
COMMENTS
A 45-year-old woman presented with hypertension, fatigue, and episodic confusion. After medications were administered, the blood pressure decreased but fatigue and confusion persisted. Four ...
Patient Case Presentation. Mr. E.A. is a 40-year-old black male who presented to his Primary Care Provider for a diabetes follow up on October 14th, 2019. The patient complains of a general constant headache that has lasted the past week, with no relieving factors. He also reports an unusual increase in fatigue and general muscle ache without ...
Case study. Ms. C is a 42-year-old black American woman with a 7-year history of hypertension first diagnosed during her last pregnancy. Her family history is positive for hypertension, with her mother dying at 56 years of age from hypertension-related cardiovascular disease (CVD). In addition, both her maternal and paternal grandparents had CVD.
Hypertension. 2018; 71:1269-1324. doi: 10.1161/HYP.0000000000000066 Link Google Scholar; 14. Khera R, Lu Y, Lu J, Saxena A, Nasir K, Jiang L, Krumholz HM. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ.
A Worrying and Puzzling Case of Hypertension Presenting to the Emergency Department. A 29-year-old man presented at another hospital with a blood pressure (BP) of 240/140 mmHg and rhythmic tachycardia (heart rate, 114 bpm). One week before, he reported red urines for 1 day without stones emission for which he had received ciprofloxacin with ...
Editorial on the Research Topic Case reports in hypertension: 2022. 1. Introduction. Clinical guidelines for the management of hypertension are regularly updated, and the whole community of hypertension specialists is longing for the promised new guidelines of the ESH/ESC expected to be released in June 2023.
From Framingham Heart Study displays, about 17% of women and 19% of men with hypertension had this as their only CVD risk factor, while 32% of women and 30% of men with this hypertension had 3 or more additional risk factors. 9 Therefore, the main goal of this study was to identify those risk factors that lead hypertensive patients to CVD at ...
In a randomized study of hypertension patients, ... J Med Case Rep. 2021;15:622. Article PubMed PubMed Central Google Scholar Tsai WC, Lee WH, Chen YC, Liu YH, Chang CT, Hsu PC, et al. Combination ...
This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as ...
DR DELBANCO: Mr R is a 41-year-old African-American man with a long history of hypertension, first discovered in the early 1990s. Over the years, Mr R has had difficulty adhering to suggested medication regimens, and his blood pressure has been poorly controlled, despite the efforts of multiple doctors at a number of different institutions ...
Definitions used in these clinical case scenarios. Definitions Stage 1 hypertension Clinic blood pressure is 140/90 mmHg or higher and. subsequent ambulatory blood pressure monitoring (ABPM) daytime average or home blood pressure monitoring (HBPM) average blood pressure is 135/85 mmHg or higher. Stage 2 hypertension Clinic blood pressure is 160 ...
Case Presentation. The patient was a 17-year-old male who was admitted to our hospital in May 2020 due to uncontrolled hypertension for 6 months and weakness of limbs for 20 days. Six months prior to admission, blood pressure of the patient was found to have increased to 200/120 mmHg during the physical examination.
This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as ...
He had significant medical history of hypertension and was on a β-blocker in the past, but a year ago, he stopped taking medication due to an unspecified reason. The patient denied any history of tobacco smoking, alcoholism, and recreational drug use. The patient had a significant family history of hypertension in both his father and mother.
This case study describes the effective treatment of a hypertensive crisis in a 63 year old woman with special reference to relevant, optimal, physical exercise and psychophysiological, heart ...
Studies that have compared antihypertensive treatment in patients with diabetes versus placebo have shown reduced cardiovascular events. The United Kingdom Prospective Diabetes Study (UKPDS), which followed patients with diabetes for an average of 8.5 years, found that patients with tight BP control (< 150/< 85 mmHg) versus less tight control (< 180/< 105 mmHg) had lower rates of myocardial ...
Recent observational studies have suggested potential harms associated with treating asymptomatic elevated inpatient BP, which brings current practice into question. Despite the ubiquity of elevated inpatient BPs, few position papers, guidelines, or consensus statements have focused on improving BP management in the acute care setting ...
Over a billion people near about 1 in 4 men and 1 in 5 women having hypertension. In this case study 60 years old women with Hypertension was identified in community remote area and checked the ...
Abstract. Objective: To explore the effect of management of nursing case on blood pressure control in hypertension patients. Method: This is a randomized controlled study which will be carried out from May 2021 to May 2022. The experiment was granted through the Research Ethics Committee of the People's Hospital of Chengyang District (03982808).
Description of Case. A 21-year-old pregnant woman, gravida 2 para 1, presented with hypertension and proteinuria at 20 weeks of gestation. She had a history of pre-eclampsia in her first pregnancy one year ago. During that pregnancy, at 39 weeks of gestation, she developed high blood pressure, proteinuria, and deranged liver function.
Lu and the study authors say other regional health systems could emulate this study to better understand their hypertension prevalence and control rates and to inform strategies to improve hypertension care. Other study authors include: Yuntian Liu, MPH, Shu-Xia Li, PhD, Mitsuaki Sawano, MD, Patrick Young, PhD, Wade Schulz, MD, and Harlan ...
Study with Quizlet and memorize flashcards containing terms like How should the student nurse respond?, What significant risk factors for hypertension does the student nurse identify for George, according to this health history? (Select all that apply.), According to the assessment of this client, which recommendation is most important for the student nurse to provide George? and more.
Several studies have reported the correlation between pediatric hypertension and family H/O hypertension, low birth weight, excess body weight [6,7]. Here we describe a 13 year old girl presenting with epistaxis, headache and uncontrolled hypertension despite poly drug therapy, abnormal peripheral pulses and unequal blood pressure in upper limbs.
Hemodynamic parameters have been correlated with stroke, hypertension, and arterial stenosis. While only a few small studies have examined the link between hemodynamics and diabetes mellitus (DM).
We thank Songtao Cai and colleagues for their Correspondence. Our study's aim was to compare integrated management with standard vertical management, with both models of care delivered by health services staff in close to normal conditions. We showed that integrated management resulted in a very high level of retention in care for participants living with diabetes, hypertension, or both, which ...
Labs and Diagnostics: For this patient with suspected hypertension, anticipated labs and diagnostics may include blood tests, urinalysis, electrocardiogram (ECG or EKG), echocardiogram, ambulatory blood pressure monitoring (ABPM) or home blood pressure monitoring, imaging studies, and specialized tests.
In another study, 4,396 patients aged 65 to 74 years with mild to moderate hypertension were randomly assigned to receive diuretic, β blocker, or placebo. 3 Patients in the treatment group had a 25% reduction in stroke and a 19% reduction in coronary artery events.
A study conducted by Kunnath et al. found that pregnancy induced hypertension was significantly associated with hearing impairment. Bakhshaee et al. [ 29 ] and Alan et al. [ 35 ] reported transient effects of preeclampsia on neonatal hearing scan results and the study showed higher failure rates in the first TEOAE in the preeclampsia group ...
The Prospective Urban Rural Epidemiology study, including patients from 17 countries on five continents, showed that awareness, diagnosis, and control of hypertension were lower in low-income countries compared with other countries and in rural settings compared with urban areas. Considering the disadvantages of the vulnerable population, the ...