Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 19, Issue 6
- Assessing quality of care from hospital case notes: comparison of reliability of two methods
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- A Hutchinson 1 ,
- J E Coster 1 ,
- K L Cooper 1 ,
- A McIntosh 1 ,
- S J Walters 2 ,
- P A Bath 3 ,
- M Pearson 4 ,
- K Rantell 2 ,
- M J Campbell 2 ,
- J Nicholl 2 ,
- 1 Section of Public Health, ScHARR, University of Sheffield, Sheffield, UK
- 2 Section of Health Services Research, ScHARR, University of Sheffield, Sheffield, UK
- 3 Department of Information Studies, University of Sheffield, Sheffield, UK
- 4 Clinical Effectiveness and Evaluation Unit, Royal College of Physicians, London, UK
- Correspondence to Allen Hutchinson, Section of Public Health, ScHARR, Regent Court, 30 Regent Street, Sheffield S1 4DA, UK; allen.hutchinson{at}sheffield.ac.uk
Objectives To determine which of the two methods of case note review provide the most useful and reliable information for reviewing quality of care.
Design Retrospective, multiple reviews of 692 case notes were undertaken using both holistic (implicit) and criterion-based (explicit) review methods. Quality measures were evidence-based review criteria and a quality of care rating scale.
Setting Nine randomly selected acute hospitals in England.
Participants Sixteen doctors, 11 specialist nurses and three clinically trained audit staff, and eight non-clinical audit staff.
Analysis Methods Intrarater consistency, inter-rater reliability between pairs of staff using intraclass correlation coefficients (ICCs), completeness of criterion data capture and between-staff group comparison.
Results A total of 1473 holistic reviews and 1389 criterion-based reviews were undertaken. When the three same staff types reviewed the same record, holistic scale score inter-rater reliability was moderate within each group (ICC 0.46 to 0.52). Inter-rater reliability for criterion-based scores was moderate to good (ICC 0.61 to 0.88).
Comparison of holistic review score and criterion-based score of case notes reviewed by doctors and by non-clinical audit staff showed a reasonable level of agreement between the two methods.
Conclusions Using a holistic approach to review case notes, same staff groups can achieve reasonable repeatability within their professional groups. When the same clinical record was reviewed twice by the doctors, and by the non-clinical audit staff, using both holistic and criterion-based methods, there are close similarities between the quality of care scores generated by the two methods. When using retrospective review of case notes to examine quality of care, a clear view is required of the purpose and the expected outputs of the project.
- Medical records
- quality of care
- reliability
- implicit review
- explicit review
- healthcare quality
- criterion-based review
- holistic review
https://doi.org/10.1136/qshc.2007.023911
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Quality of care is assessed from clinical records using two principal approaches: holistic (implicit) and criterion-based (explicit) review. Both approaches have strengths and weaknesses, whether they are used for performance monitoring, assessment or research.
Clinical staff are accustomed to reviewing patient records to judge the quality of care. This holistic approach uses professional judgement and requires no prior assumptions about the individual case, can be applied to any condition, can extend to examining any aspect of care and may be relatively quick. However, the standards against which quality is judged holistically are implicit, being dependent on the reviewer's personal knowledge and perspective, and therefore subjective.
Semistructured holistic review methods have therefore been developed to determine standards of hospital, outpatient and nursing care. 1–3 These methods ask specific questions about phases and aspects of care and may use scales to rate quality.
Nevertheless, despite attempts to reduce levels of subjectivity in holistic review by providing extensive training for physician reviewers, concerns remain about review methods based principally on professional judgement. There are concerns about inter-rater reliability, 4 choice of methods of assessing reliability, 5 consistency, 6 bias towards harshness or leniency, 7 hindsight bias 8 and reviewer idiosyncrasy. 9 Moreover, lower levels of inter-rater reliability have been found for holistic review than for criterion-based review. 9 Criterion-based review has therefore been proposed as a more effective means of assessing quality. 10 , 11
Criterion-based review allows comparison of care against explicit standards (eg, from national clinical guidelines), where unambiguous questions are defined to construct variables with good reproducibility, for retrieval from case notes. Clinical audit in the UK has adopted these objective, criterion-based, approaches, 12–14 using explicit standards, independent of profession. These have been used to identify substantial variations in organisation and clinical care between hospitals. 12
However, criterion-based review has been criticised as being insensitive 15 and may not identify unexpected factors influencing outcomes of care. 16 Mixed methods are an alternative, 17 , 18 whereby nurses use criterion-based review to identify a subset of problematic cases for subsequent holistic review by doctors; however, prior selection may lead to hindsight bias among the physician reviewers who may judge selected cases more harshly. 8 , 11 Moreover, nurses and doctors may use different information to judge care quality (and may make different judgements about an individual case). 18
It is therefore not clear which review method provides more reliable and useful information or how relatively reliable and reproducible are the different methods when carried by different healthcare professionals. Our study compares the results of three different professional groupings when evaluating quality of care from the same set of case notes, using both holistic review using quality of care rating scales and criterion-based review.
Setting and reviewer professional background
Data were collected from nine acute hospitals in England, selected randomly from 136 that met high patient-throughput criteria for the two study conditions. In each hospital, staff were recruited to undertake reviews of cases of an admission for an exacerbation of either chronic obstructive pulmonary disease (COPD) or heart failure. Three staff types were recruited: 16 doctors in specialist training, 14 other clinical staff (11 of whom were nurses specialising in the review condition) and 8 non-clinical audit staff.
Training and data collection
Reviewers received a 1-day joint training session on holistic and criterion-based review methods. Clinical scenarios were used and reviewers were provided with copies of national clinical guidelines for COPD and heart failure care. 19 , 20 Data collection software was demonstrated. Reviewers evaluated the records within their own hospital, similar to local clinical audit, and no patient-identifiable data were used in the analysis.
Review methods
Different combinations of reviewers from the three staff types were used at each hospital to compare their effectiveness in carrying out holistic and criterion-based case note reviews. In each hospital, case notes of 50 consecutive admissions of COPD or heart failure were sought and reviewed by staff type combinations of one to four staff ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Overview of selection and review process.
Each reviewer evaluated care on the same case notes using both review methods, holistic and then criterion-based review, holistic being used first to reduce potential hindsight bias 8 , 11 caused by finding a low criterion-based score first. Using their own implicit standards, reviewers rated the reported quality of care provided to each patient for three structured phases of care (admission/investigations, initial management and predischarge care). Each phase was rated on a 1 to 6 scale (1=unsatisfactory, 6=very best care). Overall quality of care for each review was rated on a 1 to 10 scale (1=unsatisfactory, 10=very best care).
Reviewers then undertook a criterion-based review on the same case notes. Criteria development used established methods for constructing explicit evidence-based review criteria 4 , 12 , 13 , 21 (COPD, n=37; heart failure, n=33) derived from national clinical guidelines recommendations and expert opinion. 19 , 20
Criterion-based data were used to assess each reviewer's effectiveness at abstracting data from clinical records and completing the data collection form; an “effectiveness of reviewer” score was calculated and converted to a percentage for each record review (one point per data field completed by the reviewer; one point subtracted per data field left blank). Quality of care scores were calculated for each record, comprising the percentage of the criteria identified by the reviewer as having been met.
Analysis methods
Holistic review.
Intrarater and inter-rater reliability was calculated for holistic quality of care scores. Robust standard errors (STATA V.9, College Station, Texas, USA) 22 were used to allow for clustering of scores around each reviewer when calculating confidence intervals and p values for the mean overall scores by reviewer type.
Intrarater consistency for each review was assessed by calculating Pearson's correlation coefficient between the mean rating of the three phases of care and the rating of overall care.
To assess inter-rater reliability between ratings of the same record by different reviewers, raw ratings were converted to ranks to adjust for variation in the range of scores used by different reviewers. Intraclass correlation coefficients (ICCs) were calculated on these ranks. 4 , 23 The ICC is the correlation between two measurements or quality of care ratings in the same patient, using randomly chosen reviewers.
Criterion-based review
Mean criterion-based quality of care scores were compared across the three staff types using a one-way analysis of variance, taking account of clustering by staff type.
Inter-rater reliability for overall quality of care scores by pairs/triplets of staff reviewing the same records was estimated using ICCs. Pooled ICC estimates from the different combinations of reviewers used a weighting that was inversely proportional to the variance of the estimate. 23
Inter-rater reliability results for the two review methods were compared.
Across nine acute hospitals, 38 reviewers undertook 1473 holistic reviews and 1389 criterion-based reviews (total=692 case notes). The number of case notes reviewed by each individual ranged from 9 to 50 (see electronic table E1). This variation was due to the effect of job rotations, workload pressures and difficulties in obtaining clinical records.
Intrarater consistency in holistic reviews
For all three staff types ( table 1 ), there were statistically significant correlations (r>0.71, p<0.001) between the mean scale score ratings that reviewers assigned to the individual phases of care and their rating of the overall quality of care for the same set of case notes, indicating a fair to good level of intrarater consistency in rating the quality of care using holistic review scale scores.
- View inline
Intrarater consistency between holistic scale score ratings for phases of care and for overall care
Criterion-based reviewer effectiveness
Effectiveness in capturing criterion-based data was high and similar across all staff types ( table 2 ), with mean scores approximately 95% (approximately 1.5 data items missing per review).
Criterion-based reviewer effectiveness scores
Inter-rater reliability for holistic review
Holistic review reliability between scale score ratings of the same record by pairs of reviewers was moderate within all three staff types, although it varied between reviewer pairs and was sometimes very poor ( table 3 ).
Inter-rater reliability between holistic overall ratings of the same record by paired reviewers of different staff types
The overall weighted mean ICC was moderate across all three reviewer types, with overlapping 95% confidence intervals (CIs) indicating no significant differences between staff types.
Comparisons between professional groups
Where reviewers from different staff types used holistic scale score methods to review the same record, inter-rater reliability was assessed between staff groups for all phases of care and overall care ( table 4 ). For the holistic phase of care findings within staff groups, there was generally modest to fair agreement within pairs, particularly among doctors, although the range is large even among them (eg, initial management results). However, where staff from different groups reviewed the same record, agreement between the different professional groups on their assessment of the quality of care was poor to non-existent.
Within-staff-type ICC and between-staff-type group ICC comparisons of holistic scale score reliability for phases of care and overall score
Analysis of variance between the holistic overall scale ratings of the three staff types show that the nurse/other clinical group scores were significantly lower than the doctor (p<0.001) and non-clinical audit groups (p<0.001). The comparison of the latter two groups showed no significant differences (p=0.352).
Inter-rater reliability for criterion-based review
Inter-rater reliability between criterion-based scores (ie, the percentage of criteria recorded as being met) for the same record by different reviewers ranged from moderate to good within all staff types. Doctors showed a significantly higher level of reliability ( table 5 ).
Inter-rater reliability between criterion-based scores (proportion of criteria stated as being met) for the same record by different reviewers
Comparison of holistic and criterion-based methods
Inter-rater reliability results for the two review methods were compared. In addition, an estimate of the within-staff-type consistency across both review methods was calculated using p value for difference between the overall holistic quality of care ratings (percentage) and the percentage of criteria recorded as being met.
Table 6 shows that the mean overall “quality of care” scores across the 692 patient records were similar for holistic and criterion-based methods and for all three staff types (70% to 79%, where 100%=excellent care).
Mean ratings/scores of overall quality of care: comparison of two review methods
Estimation of the level of quality of care score agreement between the two methods for an individual record, using p value for difference, shows that there was no significant difference between the holistic and criterion-based assessments when undertaken by the doctors (mean difference −1.9, p value for difference 0.406) and by the non-clinical audit staff (mean difference 3.1, p value for difference 0.223).
A non-significant p value for difference indicates that there is some association between the scores derived from the two review methods. These results suggest that for the doctors and the non-clinical audit staff the two methods are giving, on average, a somewhat similar result. The pooled results for all staff showed a small mean difference (−2.6) that bordered on statistical significance, possibly influenced by the highly significant results from the nurse/other clinical group (39% of all of the reviews).
Retrospective assessment of the quality and safety of care can be performed from the clinical record using holistic or criterion-based review methods: both have methodological constraints. Studies mostly compare different professional groups using different methods. Thus, Weingart et al 18 compared explicit (criterion-based) review undertaken by nurses with implicit review of the same record undertaken by physicians, and found that “nurse and physician reviewers often came to substantially different conclusions”. This is the first UK study to contrast the two methods of review systematically and also across three different professional groups.
We investigated the level of agreement between healthcare professionals, from different backgrounds, when they review the same record. This agreement, or reliability, relates to the repeatability of the results from the review—whether a different reviewer would come to the same conclusion about the quality of care from the same data source, using the same method. This is clearly a practical question for those reviewing quality of care in clinical audit or performance review.
Reviewers undertaking holistic review, using scale scores, were relatively consistent in the scores allocated to care quality across the individual phases of care and overall for the entire episode of care. All three staff groups had moderate within-group inter-rater reliability, ranging from 0.46 (95% CI 0.34 to 0.59) to 0.52 (95% CI 0.41 to 0.62), with the doctor reviewers faring best. These were rather higher values than the average found in a systematic review by Lilford et al , 5 in which implicit structured case note review studies concerned with causality and process of care had mean κ values <0.4 (causality; κ 0.39 (SD 0.19), process; κ 0.35 (SD 0.19)). Our study results are also somewhat similar to those of Hofer et al 4 who used ICCs to examine repeatability and found a reliability of 0.46 for a structured holistic review of diabetes and heart failure case notes by physician reviewers (although only 0.26 for case notes of patients with COPD). By comparison, a recent holistic assessment of patients dying in UK hospitals achieved a κ score of 0.39 on the key indicator of quality of medical care. 24
Criterion-based review demonstrated that all reviewers could identify relevant data (the effectiveness of reviewer scores were around 95%). There were moderate (0.61 for non-clinical audit staff) to quite high levels of inter-rater reliability (clinical staff 0.74, doctors 0.88)—similar to those found in large UK national clinical audit programmes of stroke 25 , 26 and continence, 27 and reflecting the trend to higher values for explicit reviews found in other studies. 5 Our study confirms the findings of the UK stroke care audit, 25 , 26 that criterion-based record review can be undertaken by staff from different backgrounds.
Case note review can only consider what has been recorded, and incomplete records do not mean that an event did not occur. If a practitioner considered something too trivial to record, then it is doubtful that any consequential actions would have occurred. However, some significant events will remain unrecorded and thus unreviewed. Direct observation of care delivery overcomes the problem of missing information, and is an alternative approach, 17 although too expensive as a standard procedure. Hindsight bias in case note review is an acknowledged challenge. 28 We tried to minimise any effect by undertaking holistic review before criterion review.
The overall results of care quality assessment were similar with both methods from our review and all rated care quality reasonably highly (between 70% and 79%, where 100% represents excellent care). But the weak inter-group reliability for holistic scores has implications when choosing how to evaluate the care quality from case notes. Performing as a screening tool, criterion-based review produces sufficient information to judge the overall quality of care, provided that appropriate review criteria are chosen. A structured form of holistic review also gives a reliable picture of the quality of care in the right hands, yet can also pick up extra nuances of quality variation.
Our medical reviewers were relatively inexperienced but with audit training were able to use both criterion-based and holistic review effectively. It would be interesting to explore whether senior clinicians' greater clinical experience would produce different holistic assessments. We hypothesise that it would useful to explore further the expertise of specialist nurses in holistic review because they have particular skills in helping patients with adherence to care pathways.
So which method of review would be best used for clinical audit and performance review, and by which professional groups? All three professional groups performed well when using criterion-based review, so the decision on who should undertake reviews depends mainly on cost and availability of staff.
On the other hand, the decision on who should undertake structured holistic review is more complex. The method can deliver more than just the sum of the results of collecting a set of review criteria. Although all groups can use the method of holistic scale scoring, our data suggest that, for the more technical phases of care, the three groups interpreted the same records differently despite considerable training in the review method. To some extent this probably reflects their background knowledge of clinical care delivery. It is unrealistic to expect non-clinical audit staff to fully appreciate the details of the medical care, let alone judge when care has deviated from best practice.
Although nurses are much closer to the medical care process, the limited agreement between the doctors and the nurses may reflect different internal professional standards for assessing quality and safety of care. Weingart et al 18 conjectured that nurses and doctors reviewed in different ways, that nurses sought data on the routines of care while doctors looked for a wider picture and that neither group considered both dimensions. Analysis of textual commentary on quality of care available from each holistic review will throw further light on this question.
Conclusions
There is modest agreement between the holistic and criterion-based quality assessment scores of the same record by the same reviewer. However, for holistic review, different staff groups are implicitly using different care standards in their assessment of quality. Large-scale criterion-based audits, such as those promoted by the English Healthcare Commission, 29 may miss the richer information provided by holistic review. A mixed holistic and criterion-based approach may be a solution 5 and has been subsequently used in this study to investigate the relationship between care process and outcome.
Acknowledgments
Karen Beck has provided administrative support throughout the project and her contribution has been exceptionally helpful.
The research team would like to thank all of those NHS staff who so generously contributed to the successful completion of this study. We also wish to thank staff at the Royal College of Physicians Clinical Effectiveness and Evaluation Unit for their help in selecting research sites and methods development.
- ↵ Agency for Health Care Policy and Research . Using clinical practice guidelines to evaluate quality of care . Vol 2 . Rockville (MD) : US Department of Health and Human Services, Public Health Service , 1995 .
- Rubenstein LR ,
- Harris ER ,
- Pearson M ,
- Hayward RA ,
- Lilford R ,
- Edwards A ,
- Girling A ,
- Parkerson GR ,
- McMahon LF ,
- Kuykendall D ,
- Johnson ML ,
- Localio RA ,
- Weaver SL ,
- Hutchinson A ,
- McIntosh A ,
- Anderson J ,
- ↵ The North of England Study of Standards and Performance in General Practice . Medical audit in general practice. I: Effects on doctors' clinical behaviour for common childhood conditions . BMJ 1992 ; 304 : 1480 – 4 . OpenUrl Abstract / FREE Full Text
- Camacho LA ,
- Mohammed MA ,
- Bentham L ,
- Thomas EJ ,
- Studdert DM ,
- Weingart SN ,
- Palmer RH ,
- ↵ National Institute for Clinical Excellence . Chronic obstructive pulmonary disease. Management of chronic obstructive pulmonary disease in adults in primary and secondary care . London : National Institute for Clinical Excellence , 2004 .
- ↵ National Institute for Clinical Excellence . Chronic heart failure: management of chronic heart failure in adults in primary and secondary care. Clinical Guideline 5 . London : National Institute for Clinical Excellence , 2003 .
- Hadorn DC ,
- Kamberg CJ ,
- ↵ StataCorp . Stata statistical software: release 9 . College Station (TX) : StataCorp LP , 2005 .
- Wardle TD ,
- Burnham R ,
- Gompertz PH ,
- Gompertz P ,
- Hopkins A ,
- Lilford RJ ,
- Brauholtz D ,
- ↵ http://www.healthcarecommission.org.uk/national clinical audit/ (accessed 28 Nov 2008).
Funding DoH Methodology Research Programme c/o Department of Epidemiology and Public Health, University of Birmingham, Edgbaston, Birmingham, UK. The project was funded by the Department of Health for England Methodology Research Programme.
Competing interests None.
Ethics approval An opinion was sought from the Trent Multiple Research Ethics Committee and the project was deemed not to require formal ethical review because no identifiable individual patient data were seen by the research team.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Search Menu
- Ageing - Other
- Bladder and Bowel Health
- Cardiovascular
- Community Geriatrics
- Dementia and Related Disorders
- End of Life Care
- Ethics and Law
- Falls and Bone Health
- Frailty in Urgent Care Settings
- Gastroenterology and Clinical Nutrition
- Movement Disorders
- Perioperative Care of Older People Undergoing Surgery
- Pharmacology and therapeutics
- Respiratory
- Sarcopenia and Frailty Research
- Telemedicine
- Advance articles
- Editor's Choice
- Supplements
- Themed collections
- The Dhole Eddlestone Memorial Prize
- 50th Anniversary Collection
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Publish
- Advertising and Corporate Services
- Journals Career Network
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- About Age and Ageing
- About the British Geriatrics Society
- Editorial Board
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Patients and methods.
- < Previous
Differences in care received by patients with and without dementia who died during acute hospital admission: a retrospective case note study
- Article contents
- Figures & tables
- Supplementary Data
Elizabeth L. Sampson, Vivienne Gould, Dan Lee, Martin R. Blanchard, Differences in care received by patients with and without dementia who died during acute hospital admission: a retrospective case note study, Age and Ageing , Volume 35, Issue 2, March 2006, Pages 187–189, https://doi.org/10.1093/ageing/afj025
- Permissions Icon Permissions
SIR—Dementia is a malignant and ultimately fatal condition, yet may not be viewed as such [ 1 ]. One-third of patients aged between 75 and 84 years with Mini Mental State Examination (MMSE) [ 2 ] scores of 19–23 will die within a year [ 3 ]. The acute admission of a person with dementia to the general hospital setting increases mortality even further and over half of patients with moderately severe dementia (MMSE cutoff 17/18) admitted with hip fracture or pneumonia will die within 6 months [ 4 ]. The incidence of dementia from all causes increases with age, the number of older people is increasing and therefore more patients with dementia will be admitted to, and die on, acute hospital wards. Little is known about the experience of dying dementia patients in the acute hospital setting, although a recent Royal Commission report suggested that they receive sub-optimal care [ 5 ] and their religious and spiritual needs are neglected [ 6 ].
The aim of this study was to retrospectively examine the care received by dying patients with and without dementia on acute medical wards and to identify differences between them. Our hypothesis was that patients who were documented in their medical notes as having dementia would receive similar end-of-life care to those who were not.
We examined the case notes of patients aged 70 or over who died whilst an inpatient on an acute medical ward from 1 April 2002 to 31 March 2003. One hundred and fifty sets of notes were selected by hospital numbers (using random number tables). Of these, 122 sets of notes were available and used for the study. Dementia caseness was defined as having a formal diagnosis of dementia (of any type) written in the medical notes. From the notes, we collected demographic information including age at death, gender, type and severity of dementia and religious faith. Abbreviated Mental Test Scores (AMTS) [ 7 ] or MMSE scores were noted if they had been performed at any time during admission. We documented the use of painful invasive procedures such as arterial blood sampling and urinary catheterisation using a checklist developed by Morrison et al . [ 8 ].
End-of-life care was assessed using items from the Liverpool Care Pathway for the Dying Patient [ 9 ]; this includes diagnosing that the patient is dying, limiting unnecessary procedures and interventions, and prescribing appropriate palliative medications. It specifically notes the prescription of medications for certain indications such as pain, nausea, vomiting and excessive respiratory secretions. We also noted whether patients were referred to the palliative care team and whether there was any indication that the patients’ spiritual needs were assessed by any member of hospital staff during the admission.
Statistical analysis was performed using SPSS (version 11.0). The relationship between dementia status and dichotomous variables was investigated using Fisher’s exact test. The Mann–Whitney U test was used for continuous variables. The study was approved by the hospital ethics committee.
Of the 122 patients with available notes, 35 (28%) had a diagnosis of ‘dementia’ documented, 65 (53%) were described as cognitively intact and 22 (18%) had no mention of the patient’s cognitive status. Further analysis was conducted on the 100 sets of notes where cognitive status was documented.
There were no significant differences in terms of age, gender and length of hospital admission between patients with and without dementia. Of the patients whose dementia status was documented in the notes, 44 (44%) had an AMTS performed during their admission and three patients (3%) had an MMSE. Patients with dementia had significantly lower AMTS scores. Of the 35 patients noted as having dementia, nine (26%) had Alzheimer’s disease, 10 (29%) vascular dementia, 1 (2%) Lewy body disease and 15 (43%) had no specific diagnosis made. Significantly fewer patients who were documented as having dementia had any mention of their religious faith (40 versus 63%; P = 0.023) (Table 1 ).
Demographic data on patients with ( n = 35) and without ( n = 65) dementia who died on acute medical wards
Data only available on 44 of a total of 100 subjects, 16 with dementia and 28 without dementia
Regarding medical management (Table 2 ), significantly fewer patients who were recorded as having dementia had a central line inserted (3% with dementia versus 20% without dementia). Two patients with dementia received mechanical ventilation. The measurement of blood gases was more frequent among patients who were documented as having dementia (80 versus 58%; P = 0.024) as was the use of urinary catheters (77 versus 57%; P = 0.035) and nasogastric tubes (40 versus 23%; P = 0.062). Discussions regarding resuscitation status and limiting procedures (amongst professionals and with family members) occurred with equal frequency in both patient groups. However, referral to palliative care and the prescription of palliative medications was significantly less frequent in patients who were documented as having dementia. Only three patients (3% of the total cohort) had any assessment of their spiritual needs prior to their death documented.
Management of patients with ( n = 35) and without ( n = 65) dementia prior to death
Our results suggest that patients who are noted to have dementia may be receiving different end-of-life care to those who are cognitively intact. Although some of this may be related to associated physical problems—incontinence and dysphagia are common in end-stage dementia [ 10 ]—other differences are more difficult to explain.
The diagnosis of imminent death, documentation of resuscitation status and discussions regarding limiting medical procedures occurred with similar frequency in both groups. Although there is some evidence that invasive procedures were limited in patients with dementia, i.e. less use of mechanical ventilation and central lines, and therefore that the poor prognosis of patients with dementia was realised to a degree, this did not appear to influence other aspects of the quality of end-of-life care. It was interesting that significantly more patients documented as having dementia had blood gases measured. This may have occurred because these patients are more vulnerable to developing pneumonia secondary to aspiration or malnutrition [ 11 ]. Patients with documented dementia received significantly fewer referrals to specialist palliative care and less palliative medication.
This may occur because there are no validated prognostic indicators for patients with end-stage dementia who are suffering from acute physical illness [ 12– 14 ]. Dementia does not appear to be viewed as a ‘terminal’ disease by carers [ 1 ] nor health professionals [ 15 ]. This is despite the facts that the mortality risk ratio of mild/moderate dementia is 3.61 compared to 2.01 for neoplastic disease [ 15 ], and in older women, dementia carries a relative risk of death greater than that of carcinoma of the gastrointestinal tract [ 16 ]. Although there are worthy calls to increase palliative care provision in dementia [ 17 ], any development would be based upon a very limited evidence base; a recent systematic review [ 18 ] found only one randomised controlled trial.
A large part of good end-of-life care is control of pain; however, pain is poorly managed in patients with dementia. Cognitively impaired patients with fractured neck of femur are prescribed only one-third of the analgesia compared with cognitively intact controls [ 19 ]. Untreated pain and discomfort causes unnecessary suffering and behavioural problems. The latter may in turn lead to the inappropriate use of neuroleptic medication and may engender negative attitudes towards patients with dementia from staff [ 20– 22 ].
Our results indicate that the recording of patients’ cognitive function during admission was inadequate and this is in keeping with previous studies [ 21 , 22 ]. The admission of an acutely unwell person with dementia to hospital is a critical event. In a recent study, 53% of patients with severe dementia admitted with hip fracture or pneumonia died within 6 months [ 2 ]. Thus, it is a vital part of management that cognitive function is recorded.
Very few patients had their spiritual needs assessed or addressed while they were dying, and it was of note that fewer patients with dementia had information documented regarding their religious beliefs. They may be unable to give details regarding their faith [ 23 ], and this should be actively sought from relatives or carers on admission.
The methodology used for this study (retrospective case note review) may have lead to some bias, as it relies on the quality of documentation in patient case notes. We have no reason to believe that the quality of note keeping may be different if a patient has dementia. The quality of end-of-life care was not rated blind to the presence or absence of dementia. However, evidence of care, decided a priori on the factors described in the methods section, was either written in the notes or absent. Dementia is under-diagnosed in patients admitted to the acute hospital sector, and some of those in our non-dementia group could well have been ‘missed’ cases. However, our intention was to investigate whether the perception that a patient has ‘dementia’ influences the end-of-life care that they receive.
Standard 2 of the English National Service Framework for Older People supports the use of better quality end-of-life care for older people, noting that ‘many older people and their carers have also found that palliative care services have not been available to them’ [ 24 ]. This study illustrates that patients who die with dementia in the acute hospital sector, have poor access to palliative care and that research in to service provision is urgently needed to remedy this situation.
There is increasing awareness of the need to provide good quality palliative care to older people, but those with dementia have particular difficulty in accessing services.
Older people, who died whilst admitted to acute hospital wards and who were documented in their medical notes as having dementia, received significantly fewer palliative medications or referrals to palliative care teams prior to death.
In those patients where dementia was noted, there was less attention to spiritual needs and religious background.
McCarthy M , Addington-Hall J, Altmann D. The experience of dying with dementia: a retrospective study. Int J Geriatr Psychiatry 1997 ; 12 : 404 –9.
Folstein MF , Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975 ; 12 : 189 –98.
Neale R , Brayne C, Johnson AL. Cognition and survival: an exploration in a large multicentre study of the population aged 65 years and over. Int J Epidemiol 2001 ; 30 : 1383 –8.
Morrison RS , Siu AL. Survival in end-stage dementia following acute illness. JAMA 2000 ; 284 : 47 –52.
House of Commons Health Committee. Palliative Care. Fourth Report of Session 2003–04, Volume 1. London: The Stationery Office, 2005 .
Everett D. Forget me not: the spiritual care of people with Alzheimer’s Disease. J Health Care Chaplain 1999 ; 8 : 77 –88.
Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing 1972 ; 1 : 233 –8.
Morrison RS , Ahronheim JC, Morrison GR et al. Pain and discomfort associated with common hospital procedures and experiences. J Pain Symptom Manage 1998 ; 15 : 91 –101.
Ellershaw J , Ward C. Care of the dying patient: the last hours or days of life. BMJ 2003 ; 326 : 30 –4.
Molaschi M , Ponzetto M, Ferrario E, Scarafiotti C, Fabris F. Health and functional status in elderly patients living in nursing homes. Arch Gerontol Geriatr 1995 ; 21 : 267 –76.
Olichney JM , Hofstetter CR, Galasko D, Thal LJ, Katzman R. Death certificate reporting of dementia and mortality in an Alzheimer’s disease research center cohort. J Am Geriatr Soc 1995 ; 43 : 890 –3.
Maletta GJ. Access to hospice programs in end-stage dementia. J Am Geriatr Soc 1995 ; 43 : 1174 –5.
Ahronheim JC , Morrison RS, Morris J, Baskin S, Meier DE. Palliative care in advanced dementia: a randomized controlled trial and descriptive analysis. J Palliat Med 2000 ; 3 : 265 –73.
Hanrahan P , Luchins DJ. Feasible criteria for enrolling end-stage dementia patients in home hospice care. Hosp J 1995 ; 10 : 47 –54.
Baldereschi M , Di Carlo A, Maggi S et al. Dementia is a major predictor of death among the Italian elderly. ILSA Working Group. Italian Longitudinal Study on Aging. Neurology 1999 ; 52 : 709 –13.
Aevarsson O , Skoog I. A population-based study on the incidence of dementia disorders between 85 and 88 years of age. J Am Geriatr Soc 1996 ; 44 : 1455 –60.
Hughes JC , Robinson L, Volicer L. Specialist palliative care in dementia. BMJ 2005 ; 330 : 57 –8.
Sampson EL , Ritchie CW, Lai R, Blanchard MR, Raven PW. A systematic review of the scientific evidence for the efficacy of a palliative care approach in advanced dementia. Int Psychogeriatr 2005 ; 17 : 31 –40.
Morrison RS , Siu AL. A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage 2000 ; 19 : 240 –8.
Marshall M. ‘ They should not really be here’ – people with dementia in the acute sector. Age Ageing 1999 ; 28 (Suppl. 2): 9 –11.
Laurila JV , Pitkala KH, Strandberg TE, Tilvis RS. Detection and documentation of dementia and delirium in acute geriatric wards. Gen Hosp Psychiatr 2004 ; 26 : 31 –5.
Mayou R , Hawton K, Feldman E, Ardern M. Psychiatric problems among medical admissions. Int J Psychiatry Med 1991 ; 21 : 71 –84.
Aminoff BZ , Adunsky A. Dying dementia patients: too much suffering, too little palliation. Am J Alzheimers Dis Other Demen 2004 ; 19 : 243 –7.
Department of Health. National Service Framework for Older People, London, 2001 .
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1468-2834
- Copyright © 2024 British Geriatrics Society
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Retrospective case...
Retrospective case note review of acute and inpatient stroke outcomes
- Related content
- Peer review
- Nabil Aly , specialist registrar ,
- Kevin McDonald , research associate ,
- Michael Leathley , research fellow ,
- Anil Sharma , consultant physician ( aksharma{at}aintreestar.u-net.com ) ,
- Caroline Watkins , honorary research fellow
- Aintree Stroke Unit, Department of Medicine for the Elderly, University Hospital Aintree, Liverpool L9 7AL
- Correspondence to: A Sharma
- Accepted 5 April 2000
The annual incidence of stroke in the community is about 2 per 1000 population, 1 whereas among hospital inpatients it is 11 per 1000. 2 However, a study that systematically and simultaneously identifies all inpatients experiencing stroke and all patients admitted with stroke does not exist. Previous work on stroke among inpatients has excluded some patients—for example, those with 3 or without 2 obvious iatrogenic predisposing factors. Similarly, although risk factors for stroke have been used as predictors of an event in the context of a study, 3 these are often not documented clinically. Secondary prevention is dependenton identification and documentation of risk factors.
We compared outcomes and the identification and documentation of known risk factors in a cohort of patients admitted with a stroke or having had a stroke while in hospital (having been admitted to hospital with a primary diagnosis other than stroke).
Subjects, methods, and results
University Hospital Aintree serves a predominantly urban population of 250 000 and admits about 32 000 patients annually. Its stroke unit has 18 acute and 25 rehabilitation beds. Guidelines for the management of acute stroke are available throughout the hospital.
We identified all patients with a primary diagnosis of stroke (excluding transient ischaemic attacks and subarachnoid haemorrhages) on a stroke register. From October 1994 to March 1997, 100 inpatients with stroke and 1274 patients admitted with stroke were identified prospectively by a 24 hour, on-call stroke research team or retrospectively from the hospital discharge coding. Data collection was by retrospective review of case notes.
Median ages were 75 (interquartile range 67-82) years for inpatients and 74 (66-81) years for admitted patients. Fifty four (54%) inpatients and 647 (51%) admitted patients were female. Forty seven (47%) inpatients and 537 (42%) admitted patients were managed in the stroke unit.
The table shows the numbers of patients for whom known risk factors for stroke were clearly documented and the numbers for whom no documentation existed. According to documentation, cardiovascular risk factors were significantly higher in inpatients whereas previous strokes or transient ischaemic attacks were more common among admitted patients. Documentation was less complete for inpatients than for admitted patients.
Identification and documentation of known stroke risk factors among patients who had a stroke while in hospital and among patients who were admitted with stroke. Values are numbers (percentages) of patients
- View inline
Of the 80 (80%) inpatients and 1092 (86%) admitted patients who had computed tomography, 5 (6%) and 144 (13%) respectively had a primary intracerebral haemorrhage χP>0.05).
The inpatients remained in hospital longer after stroke (median 31 (interquartile range 13-59) days) than the admitted patients (16 (6-43) days). Twenty four (24%) inpatients returned to their previous residence, compared with 799 (63%) admitted patients (odds ratio 0.19, 95% confidence interval 0.11 to 0.31). Sixteen (16%) inpatients were newly discharged to an institution, compared with 124 (10%) admitted patients (1.77, 95% confidence interval 0.93 to 3.16), which may partly account for the longer stay for inpatients. Sixty (60%) inpatients died in hospital, compared with 351 (28%) admitted patients (3.94, 95% confidence interval 2.55 to 6.15); stroke was the primary or secondary cause of death for 51 (85%) inpatients and 301 (86%) admitted patients.
Although the inpatients and the admitted patients were similar in terms of age and sex, inpatients stayed in hospital longer, were more likely to die in hospital, and had less well documented risk factors. Improving staff awareness on medical and surgical wards regarding the importance of the early identification and documentation of known risk factors for stroke may improve outcome.
Acknowledgments
We thank Liz Lightbody, Hazel Dickinson, and Dimitrios Theofanidis, who collected data from the European stroke database, and the BMJ reviewers (Gord Gubitz and M J Campbell) for their comments.
Contributors: NA contributed to the interpretation of the results and to writing the paper. KMcD analysed the data and contributed to writing the paper. ML advised on and contributed to the statistical analysis and interpretation of the results and to writing the paper. AS contributed to the interpretation of the results and to writing the paper and will act as guarantor for the paper. CW advised on the results, analysis, and interpretation and contributed to writing the paper.
Funding None.
Competing interests None declared.
- Bamford J ,
- Sandercock P ,
- McPherson K ,
- Azzimondi G ,
- Fiorani L ,
- Vignatelli L ,
- Stracciari A ,
- Pazzaglia P ,
- Mahaffey KW ,
- Granger CB ,
- Thompson TD ,
- Weaver WD ,
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 8, Issue 8
- Escalation-related decision making in acute deterioration: a retrospective case note review
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Natasha Campling 1 , 2 ,
- Amanda Cummings 1 , 2 ,
- Michelle Myall 1 , 2 ,
- Susi Lund 1 , 2 ,
- Carl R May 1 , 2 , 3 ,
- Neil W Pearce 3 ,
- Alison Richardson 1 , 3 , 2
- 1 School of Health Sciences , University of Southampton , Southampton , UK
- 2 NIHR CLAHRC Wessex , University of Southampton , Southampton , UK
- 3 University Hospital Southampton NHS Foundation Trust , Southampton , UK
- Correspondence to Dr Natasha Campling; N.C.Campling{at}soton.ac.uk
Aim To describe how decision making inter-relates with the sequence of events in individuals who die during admission and identify situations where formal treatment escalation plans (TEPs) may have utility.
Design and methods A retrospective case note review using stratified sampling. Two data analysis methods were applied concurrently: directed content analysis and care management process mapping via annotated timelines for each case. Analysis was followed by expert clinician review (n=7), contributing to data interpretation.
Sample 45 cases, age range 38–96 years, 23 females and 22 males. Length of admission ranged from <24 hours to 97 days.
Results Process mapping led to a typology of care management, encompassing four trajectories: early de-escalation due to catastrophic event; treatment with curative intent throughout; treatment with curative intent until significant point; and early treatment limits set. Directed content analysis revealed a number of contextual issues influencing decision making. Three categories were identified: multiple clinician involvement, family involvement and lack of planning clarity; all framed by clinical complexity and uncertainty.
Conclusions The review highlighted the complex care management and related decision-making processes for individuals who face acute deterioration. These processes involved multiple clinicians, from numerous specialities, often within hierarchical teams. The review identified the need for visible and clear management plans, in spite of the frame of clinical uncertainty. Formal TEPs can be used to convey such a set of plans. Opportunities need to be created for patients and their families to request TEPs, in consultation with the clinicians who know them best, outside of the traumatic circumstances of acute deterioration.
- decision-making
- treatment escalation
- de-escalation
- resuscitation
- goals of care
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/bmjopen-2018-022021
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
There is a lack of description of escalation-related decision making in the context of deterioration outside of the critical care environment. Our study setting was the comprehensive hospital environment and individuals who were facing acute deterioration that led to death.
The study explored clinical decision-making processes: the types and range of decisions made, the involvement of families in these processes and the interaction between clinical teams. Care management trajectories provoked by acute deterioration were characterised via typology, including points of significance in the sequence of events. Contextual issues influencing decision making were described: multiple clinician involvement, family involvement and lack of planning clarity; all framed by clinical complexity and uncertainty.
While the sample was stratified, it was small, selected from a single acute hospital trust. However, two data analysis methods were applied concurrently (followed by expert clinician review): directed content analysis and care management process mapping via annotated timelines.
Examination of decision-making processes highlighted areas for improvement and the potential impact of formal treatment escalation plans through pre-emptive decision making and patient involvement outside of crisis situations.
Background
Clinical decision making in the context of acute deterioration during hospital admission is complex. Such decisions are frequently made in the face of uncertainty, characterised by: lack of underpinning information or diagnostic clarity, necessity for rapid decision making and the inability of patients to collaborate in discussions and decisions because of the acuity of their condition. 1
Previous research has focused on the illness trajectories of deteriorating patients or on clinical decision making in the specific context of critical care. The wider context of care management and related decision making remains an unresearched area. Murray et al 2 highlighted the value of awareness of illness trajectories as a mechanism for clinicians to help plan care to meet patients’ needs and for families to cope. More recently, Etkind and colleagues 3 defined trajectories of final illness among patients who died while inpatients. These were defined a priori to their case note review as: predictable (gradual deterioration during admission); predictable (rapid deterioration during admissions); unpredictable course during hospital admission; and sudden death. One hundred and forty-nine cases were examined (all deaths over 11 months on five inpatient wards where the AMBER care bundle was implemented) and characterised according to one of four trajectories.
Our study progresses the above, which focused exclusively on illness trajectories by expanding the focus to care management and understanding of the associated decision-making processes to inform clinical practice. Higginson and colleagues 4 explored this area by examining patterns of decision making, but their work was specific to critical care. Only 16 cases were examined (in combination with interviews and non-participant observation), and four trajectories with different patterns of clinical decision making were identified: curative care from admission (to critical care); oscillating curative and comfort care; shift to comfort care; and comfort care from admission. They emphasised that ‘conflict’ in decision making could occur between relatives and staff and between and within clinical teams.
Given the complexity of clinical decision making related to acuity and deterioration, and perhaps the likelihood for ‘conflict’, 4 there has been a move nationally and internationally to develop and implement formal treatment escalation plans (TEPs). Structured, procedure-specific TEPs are proposed as a mechanism by which to improve understanding and communication when escalation-related decisions need to be made and acted on. 5 They provide a framework on which to base a conversation and document treatment options that are appropriate if a patient were to become acutely unwell. They vary in both design and use. 5–7 Notable examples include: Universal Form of Treatment Options, 8 Deciding Right ( http://www.nescn.nhs.uk/common-themes/deciding-right/) and Physician Orders for Life Sustaining Treatment. 9 In the UK, there is growing interest in the national initiative, instigated in 2014, led by the Resuscitation Council and the Royal College of Nursing, which generated the Recommended Summary Plan for Emergency Care and Treatment ( http://www.respectprocess.org.uk/).
Despite this increasing awareness, little work has examined the implementation of TEPs. This study is part of a wider programme of work to inform the implementation and evaluation of TEPs as part of the Complexity, Patient Experience and Organisational Behaviour theme of the National Institute for Health Research Collaboration for Applied Health Research and Care Wessex. Additionally, the team has undertaken a review of communication and decision-making interventions directed at goals of care via a theory-led scoping review. 10
Aims/objectives
The study explored the care management of those who deteriorate and die during hospital admission, characterising the resources mobilised, in as much detail as could be tracked through recourse to case notes. The aims were: to describe how decision-making processes inter-relate with the sequence of events for individuals who die during inpatient admission and to identify situations where treatment escalation plans may have had utility.
The objectives were:
To identify and characterise, via the generation of a typology, the care management trajectories of hospital inpatients facing acute pathophysiological deterioration that ultimately leads to death.
To map clinical decision-making processes, including the involvement of patients and families in decisions, identifying what leads to and triggers changes in management.
To identify the potential role of treatment escalation plans in providing a framework to support discussions and recording of decisions.
Methodology and methods
Study design.
A retrospective case note review exploring the care management of those who die during hospital admission.
Sampling strategy
The case note review followed an initial audit of death certificate review forms (DCRFs) from all deaths at a single acute hospital trust in England (n=911) within a 6-month period (January–July 2015). Case notes of a 5% sample (45 sets of notes) of patients, aged over 18 years were reviewed. The DCRF data enabled stratified sampling, ensuring appropriate representation across groups. Thirty-two mutually exclusive strata were created based on whether cases had all possible combinations of the following: do not attempt cardiopulmonary resuscitation (DNACPR), palliative care team involvement, intensive care/high dependency management, evidence of escalation/de-escalation decision and unpredictable illness trajectory. 3 Proportionate allocation was used to sample the same fraction from each strata, with a check that the total sample size was calculated as expected (ie, not affected by rounding of the numbers for each strata to integers).
Data collection
Data were collected from case notes only. Data collection tracked the period from admission to hospital through to each patient’s death to identify: (1) when decisions to escalate or de-escalate treatment were made, (2) how those decisions were made and (3) who was involved in these decisions. For those with a prolonged admission (>30 days), data collection was limited to the last 30 days of admission (but included social and clinical data regarding their admission). The following data were extracted:
Clinical and demographic information regarding admission to hospital, including but not limited to, comorbidities and admitting specialism.
End-of-life care (EOLC) and DNACPR information, including but not limited to, whether CPR was attempted.
Nature of any events leading to a discussion or decision regarding levels of care, who recognised and responded to the event, actions taken, further detail on escalation or de-escalation of care and outcomes from this. Here, ‘event’ referred to episodes such as clinical deterioration, ward rounds, specialist review or emergence of new clinical findings.
How decisions were documented, including clarity of documentation and use of care plans.
Evidence of patient and/or family involvement in decision making and how patient preferences and those of others are taken into account, including whether patient wishes were known in advance.
Ward movements.
Date and cause of death.
Data extraction was undertaken by two clinically qualified researchers (NC and AC) and data recorded using an Excel spreadsheet pro forma (see online supplementary file 1 ). The pro forma was piloted on a set of notes and based on this changes to the form were made to facilitate usability and increase reliability of data extraction. This resulted in: inclusion of all causes of death (not just cause 1a but also underlying causes 1b and 1c), and enabling of free-text entry for avoidable EOLC admission and failed EOLC discharge. The revised pro forma was tested by NC and AC on an initial sample of case notes (n=8) to assess utility and consistency of data entry. No further changes were required. At the end of data collection, a process of cross-checking by both researchers helped to mitigate against errors, ensure accuracy and consistency.
Supplemental material
Data analysis.
Two methods of data analysis were applied concurrently. First, case notes were treated as qualitative data and analysed using directed content analysis. 11 The data within the pro forma were analysed using this method and directed towards: the event leading to the decision or discussion and the action taken and resulting outcomes and details regarding involvement and discussion with the patient and family. Data comprised verbatim transcription of relevant entries in the case notes to the pro forma. Additionally, field notes were analysed to capture limitations of case notes as a data source and recurrent issues (sequence of events and triggers for decision making) across cases.
Second, care management process mapping via annotated timelines involving key events were developed for each case. 12 These timelines included: escalation and de-escalation related decisions; involvement of patient and family in decision-making; clinical treatment plans made; investigations undertaken and treatment received; and key clinical information to inform probability of outcomes and prompt decisions.
Timelines were drawn for each case (NC and AC) and then grouped independently by NC and AC (double screened) into one of four care management trajectories, which became apparent during analysis. Categorisation of cases by the researchers were compared, with input from two additional clinical members of the research team (SL and AR). Where there was initial disagreement, the pro formas were revisited in a team discussion to agree final categorisation (n=11).
Diagrams were subsequently drawn to represent the group experience of the four care management trajectories. These were iteratively refined (NC, AC, SL and AR). They were combined with tabulated data representing the cases within each trajectory and a case exemplar (case study) and sent to a group of expert clinicians (representing a wide range of specialities) for review. They were asked to consider:
Do the four care management trajectories capture the sequence of events and decision-making processes involved?
Do the trajectories apply to patients you have seen recently who have then gone on to die while in hospital? Could you consider how they do or do not apply?
Do these data demonstrate potential triggers for decision making or treatment escalation planning that you would like to see put into practice?
Is there anything in the data you are surprised by or any other comments you would like to make?
Out of 13 experts approached, seven commented in detail on the data either face-to-face or via telephone/email. Their feedback verified: the care management trajectories reflected what clinicians encounter in practice and were described in a way they could identify with; the classification of cases to the trajectories; and the authenticity of the case exemplars. They contributed to the overall interpretation of data.
Ethical and research governance considerations
As access to patient identifiable data (case notes) was required without consent, support under section 251 of the National Health Service Act (2006) was sought and obtained via the Health Research Authority’s Confidentiality Advisory Group. 13
Patient and public involvement (PPI)
A PPI champion worked closely with the research team on this study, and the wider programme, informing all study processes. Involvement led to the recommendation that the team solely access paper-based notes (to restrict the amount of data accessed) and not electronic medical records as originally planned.
Sample characteristics
The age range of patients included (in the review of the 45 sets of notes) was 38–96 years, with 23 female and 22 male. The length of admission ranged from <24 hours to 97 days. Thirty-five patients had a DNACPR in place at time of death. Fifteen patients had palliative care team involvement.
A typology of care management
Analysis via process mapping led to the development of a typology of care management, encompassing four distinct trajectories. The trajectories characterised the sequence of events and decision-making processes through acute pathophysiological deterioration leading to death. They were:
Early de-escalation (within 24–48 hours of admission) due to catastrophic event — clinically observable signs and symptoms ± observable on imaging.
Treatment with curative intent throughout (no de-escalation) ± cardiopulmonary resuscitation.
Treatment with curative intent until significant point.
Early treatment limits set (within 48 hours of admission).
Table 1 displays the key characteristics of the cases represented by each trajectory. Each care management trajectory is described in sequence below, including a diagrammatic representation of the respective trajectory. Exemplar case studies for each trajectory are included in online supplementary file 2 . The process of reviewing the data with expert clinicians added a valuable dimension to data interpretation. The depth and range of their feedback, via their experiential knowledge, is summarised in online supplementary file 3 .
- View inline
Key characteristics of cases within the trajectories
Early de-escalation due to catastrophic event
This trajectory was characterised by hospital admission due to ‘catastrophic’ events ( figure 1 ). The event had occurred outside of hospital, was evident at the point of admission and referenced individuals who were in danger of dying on admission (eg, patients who were moribund secondary to shock) or those admitted with severe, critical illnesses (eg, major cerebrovascular accidents).
- Download figure
- Open in new tab
- Download powerpoint
Early de-escalation due to catastrophic event.
Following admission, there was a period of initial escalation, with accompanying imaging, diagnostic investigations such as blood tests or ECGs and treatment with intravenous antibiotics or fluids. This escalation also encompassed senior or specialist (eg, surgical and intensive care) review.
A key feature of this trajectory was the early (within 24–48 hours) recognition of an unsurvivable or irreversible event. All cases had at least one factor that identified this including: imaging results, clinically observable diagnoses, reduced level of consciousness and/or consultant review. Following recognition of futility, discussions with family and next of kin preceded palliation in all cases bar one. In this case, deterioration and death were so rapid as to prevent timely palliation. This trajectory was generally defined by short admissions, on average, patients died within 3 days.
Treatment with curative intent throughout
Trajectory 2 was characterised by treatment with curative intent for the duration of hospital admission ( figure 2 ). Individuals were admitted with a variety of diagnoses, and admissions were characterised by ongoing care at ward or high dependency unit/intensive care unit (HDU/ICU) level for multiple issues. These included fluid balance management associated with cardiorenal failure or acute kidney injury, treatment of infections and management of ischaemic or arrhythmic cardiac disease.
Treatment with curative intent throughout.
This trajectory was also characterised by the development of new diagnoses (eg, sepsis) or sudden, unpredictable events (eg, pulmonary embolism), which ultimately led to death. However, in these cases, such events did not trigger de-escalation (as in trajectory 3); patients were actively treated until death. In five of the eight cases, unsuccessful cardiopulmonary resuscitation occurred prior to death. In the three remaining individuals, DNACPR orders had been stimulated by senior clinician reviews and/or family discussions.
The reasons underlying a lack of de-escalation related to patient characteristics, individual preferences and the delivery or focus of healthcare. Some individuals were younger or normally fit and well with minimal comorbidities, while others expressed a preference for active treatment. For some, a recent intervention with curative intent, or the fact that they were awaiting discharge or transfer to alternative settings, meant that de-escalation was not a consideration. In others, the involvement of multiple specialist teams meant that the leading specialism (and thus the team who might be expected to make de-escalation decisions) was not clear.
Treatment with curative intent until significant point
Trajectory 3 was characterised by curative intent treatment until a significant point, triggering de-escalation of care ( figure 3 ). These triggers included significant deterioration in the patient’s current condition (in the absence of a new diagnosis), for example, a reduction in consciousness level or patient agitation/distress, and new diagnoses (eg, infection or malignancy), which led to deterioration in the patient’s condition. A third trigger involved a new clinical specialism or out-of-hours review recognising poor prognosis and the futility of current treatment, prompting de-escalation.
All triggers for de-escalation prompted discussions with next of kin, family and the patient or other clinical teams (if under shared-care management). Following these discussions, multistaged de-escalation ensued. The first stage involved the setting of ceilings of care and DNACPR orders. This first stage at times occurred prior to family discussion, but such discussion always preceded the second stage, which included stopping vital sign observations, early-warning activation scores and invasive investigations/treatments. In some cases, a time and intensity limited trial of treatment (eg, antibiotics) preceded a third stage of de-escalation, palliation. For patients receiving HDU/ICU level care, the latter stages of de-escalation involved the withdrawal of treatment. There was usually some degree of treatment provided in parallel to multistaged de-escalation, although this was limited, typically involving antibiotics and intravenous fluids. The time between the significant point, which triggered de-escalation and patient death, was between 0–10 days; however, this trajectory was characterised by the longest and most varied admission length, 3–97 days.
Early treatment limits set
Trajectory 4 was characterised by the presence of early treatment limits, set within 48 hours of admission ( figure 4 ). The triggers for setting limits included patient refusal of treatment, discussions with family, senior clinician review and marked deterioration in the patients’ condition. Crucially, these triggers occurred against backgrounds of: history of recent deterioration, frailty, underlying diagnoses of dementia or malignancy and the presence of pre-existing DNACPR orders and palliative care involvement. In line with this, the patients in this trajectory had the highest average comorbidity scores and ages.
Early treatment limits set.
Early treatment limits formed the start of a multistaged de-escalation process, which occurred across the duration of admission. This de-escalation started with treatment limits (DNACPR, not for intubation/dialysis/ICU care and ward-based care) before progressing to more active de-escalation (ceasing early warning scores, ceasing antibiotics/intravenous fluids/regular medications, palliation and commencement of an individualised end of life care plan).
Key to this trajectory was the level of ongoing treatment in parallel with the staged de-escalation. Despite early treatment limits being set, ongoing treatment involved a far more extensive range of treatment (interventions, therapy and medications) than in trajectory 3. Interventions included catheterisation, nasogastric tubes and blood transfusions. There was therapy input from physiotherapists, speech and language therapists, dietitians and occupational therapy teams, and medications included diuretics and antibiotics. Nonetheless, ongoing treatment was restricted to a ward environment as clinical history meant these individuals were not candidates for intensive treatment.
The categories
In addition to the care management typology, our directed content analysis revealed a number of contextual issues, which influenced decision making. We identified three interlinked categories consisting of: multiple clinician involvement, family involvement and lack of planning clarity. The categories were framed by clinical complexity and uncertainty.
Clinical complexity and uncertainty
The cases demonstrated clinical complexity caused in the main by multiple comorbidities, new diagnoses or undiagnosed conditions and challenging management, for example, of sepsis, kidney injury and frailty. Challenging management of fluid balance issues associated with multiple concurrent comorbidities, and the onset of new infections, were a frequent occurrence. A lack of clarity surrounding definitive diagnoses often meant that clinicians were ‘working in the dark’ trying to maximise management despite ongoing uncertainty. Although there were some more clearly defined diagnoses and management paths evidenced (such as stroke), with greater clinical predictability, these cases were in the minority.
Decision making was complicated by frequently changing clinical situations, particularly in relation to new findings or diagnoses. Escalation-related decisions were required that could adapt to these changing situations, where previous management plans were rapidly rendered inappropriate.
Multiple clinician involvement
Clinical management via multiple specialities, therapy and outreach teams could preclude sight of the patient’s prognosis. This was evidenced by treatment decisions and therapy involvement that did not always reflect an individual’s prognosis. Likewise, the practicalities of input from multiple specialisms, including numerous repeat reviews and interplay between different teams, often acted to elongate decision-making processes, and added complexity when no-one team took responsibility for leading decisions.
There was evidence of a hierarchy in decision making, with senior clinicians most often instigating decisions. Junior doctors were less likely to make escalation-related decisions, especially concerning placing limitations on, or removal of, treatments. Junior doctors, when required to make decisions alone (particularly those working out of hours), were more likely to continue treatment escalation, especially in the absence of prespecified escalation plans. As such, there was a clear role for senior review, with registrars and consultants instigating the majority of decisions regarding treatment limits and withdrawal of treatment.
The transfer of patients between wards and clinical teams added complexity to decision processes. There was evidence of transfers resulting in de-escalation plans being overlooked; however, in other circumstances, ward or team moves prompted new reviews and the initiation of appropriate planning. The positive influence of new perspectives or ‘fresh eyes’ on escalation-related decision making was apparent, especially via out-of-hours clinicians. It appeared that individuals not caught up in the day-to-day management of patient care were able to see the ‘bigger picture’ regarding care management, often initiating ceilings of care, or prompting escalation plans.
Family involvement
The role and influence of the family was often central in the decision-making process. It was apparent that escalation-related decisions (ie, whether to continue to increase the intensiveness of treatment, for example, dialysis, intubation and ventilation or maintain treatment at ward level) were often established and actioned before discussions with the family took place, whereas, de-escalation-related decisions (such as ceasing treatments and commencing palliation) were postponed until after discussions with family. Family involvement and consensus agreement always preceded the withdrawal of treatment (eg, organ support and ventilation). This reflects the moral imperative to discuss such decisions with family. Additionally, family were involved in the decision-making process for DNACPR orders where there was any concern about patient competency. Families also played an important role in providing collateral histories for clinicians, enabling decision making to be placed in the context of an individual’s recent health. This was particularly the case with older patients where families could highlight weeks or months of recent deterioration or recurrent infections, aiding the admission clerking, and facilitating early treatment limits being set (trajectory 4).
The impact of the familial role was most apparent when absent. In a few cases, where patients had limited or no family involvement, or lacked the physical presence of family members to prompt discussions, de-escalation decisions were not made (those in trajectory 2). In contrast, where families were engaged, they were frequently involved in consultative decision making with clinical teams. These families were often able to provide clear instructions to clinicians because of their knowledge of patients’ prior wishes. For example, relatives were recorded as stating that the ‘ patient wouldn’t want to live like this ’ and were therefore more likely to endorse clinician recommendations for treatment withdrawal. Additionally, families often agreed with recommendations that if the patient did not respond to treatment, then a move to focus on palliation should occur. The converse did apply, although only in a few cases, whereby families stated that the patient would ‘ want all done ’. In situations where families were unsure of the patient’s wishes, further team meetings with the family were always undertaken.
Lack of planning clarity
The data revealed a general lack of clarity and visibility regarding management plans in the case notes. However, the clinical complexity of these cases at times precluded the making of escalation-related plans or led to them being held in a type of uncommitted management ‘status’ until certainty was gained. Even where cogent management plans were made, they may not have been followed because there were no effective methods for signposting clinicians to plans buried in subsequent pages of notes. In addition, where management plans involved clear de-escalation, these were not always followed. This was sometimes more than just due to the lack of visibility in the notes and also due to clinical complexity and unpredictability of deterioration, with fluctuations leading to patients temporarily improving or stabilising.
Initial clerking and history taking was paramount to the quality of decision making throughout admission. This was particularly apparent where clerking histories appeared ‘lost’, with key factors not carrying through into decisions made. Where an important comorbidity was not acknowledged during the admission clerking, this could continue to influence care over the length of admission.
This case note review and qualitative analysis, identified four care management trajectories, defining and mapping clinical decision-making processes in the context of acute pathophysiological deterioration. All trajectories from admission through to death were framed by clinical complexity and related uncertainty. In general, such complexity confounded decision-making processes. Nonetheless, in a minority of profoundly complex cases (eg, older age, associated frailty and comorbid and premorbid statuses), complexity could encourage escalation-related decision making. This was apparent in the fourth trajectory, where early treatment limits were set based on patients’ preadmission morbidity. This concurs with Fritz et al 14 who in a retrospective case note review found a lower threshold for completing DNACPR orders in patients with multiple co-morbidities.
The trajectories identified here expand those previously described by Higginson et al , which were exclusive to critical care, as they are applicable to hospital inpatients irrespective of care setting. 4 Consequently, our trajectories highlight: (a) significant points in care trajectories where senior secondary review and re-evaluation of management plans would be valuable and (b) groups of patients for whom a formal TEP would be of particular benefit, as a framework to support discussions and the recording of decisions.
Our findings display significant points in care management trajectories (1 and 3). These included the recognition of irreversibility, deterioration in current condition, new diagnoses leading to deterioration and new clinical or out-of-hours team involvement. It was these points that triggered discussions around escalation and ultimately decision making. We propose that while acting as triggers, these points in trajectory 3 cases also present missed opportunities, for earlier, timely decision making. It was frequent for deterioration to occur out of hours, with important decisions left to on-call teams and sometimes more junior clinicians. As previous studies have shown, this can preclude decisions that reflect the best interests and preferences of the patient. 12 Here, clear management plans are required that pre-empt the possibility of deterioration and outline the patients’ wishes in such circumstances, as well as realistic parameters of care.
The absence of significant points in some cases by which to trigger decision making, such as those in trajectory 2, leads to a proposition made by the study’s expert clinical reviewers that strategic senior reviews are required. It is possible that earlier senior review secondary to a postadmission review may enable appropriate re-evaluation and alter management plans. Nevertheless, a lack of recognition of the dying phase, even by senior clinicians, highlighted the role and contribution of palliative care teams in questioning ongoing investigations or treatment and stimulating appropriate symptom control.
It is known that formal TEPs are helpful in stimulating discussions, formulating clear plans, ensuring patient preferences are considered 5 15 and perceived as a good idea by patients, families and healthcare professionals. 5 15–17 In addition, they help healthcare professionals structure their discussions with patients and families, and record their decisions, improving documentation clarity 18 and escalation-related communication within clinical teams. 16 19 Despite this, in the case notes reviewed, there were no recorded instances of a formal TEP being used to aid decision making. Four patients held pre-existing DNACPR orders, but none had evidence of an advance care plan or formal TEP. Despite the small number of pre-existing DNACPR orders in the review, their existence led clinicians to have wider escalation-related discussions with patients and families. There is also a pragmatic argument that documenting a DNACPR decision should trigger consideration of a TEP, as a logical continuation of the resuscitation discussion. However, based on our care trajectories, treatment escalation decision making must account for premorbid status, which may, if possible, be best assessed outside of crisis situations and acute deterioration. To incorporate patient preferences, completion of formal TEPs in primary care would enable patients who might be too acutely unwell on admission to hospital to participate in such discussions (of particular relevance to trajectories 1 and 4). Although it is impossible to anticipate the catastrophic events that occurred for individuals in trajectory 1, it is contended that those individuals who have significant comorbidities and resulting premorbid dependencies (such as those in trajectory 4) should be party to sensitive discussion and documentation of a TEP in primary and community care settings.
In summary, this review has highlighted a number of clinically relevant findings, with resulting recommendations, which the authors contend might represent best practice:
Accurate history taking surrounding premorbid functional status, comorbidity and level of dependency is vital for establishing ceilings of care.
Regular senior clinician involvement results in ongoing review of prognosis and facilitates effective decision making in complex patients where there is significant clinical uncertainty.
Awareness of a patient’s premorbid wishes and, where possible, discussion with the patient, should be a priority in deciding ceilings of care.
Discussion with family around prognosis should complement discussions with the patient.
‘Fresh eyes’ are a valuable tool for reassessing patients’ prognosis and should be used more widely for complex patients with significant clinical uncertainty, not responding to treatment.
A senior clinician with overall responsibility for the patient should facilitate multidisciplinary discussion of patients with multiple team involvement.
Earlier involvement of palliative care specialists in patient assessment would aid decision making and recognition of those who are at the end of life.
Formal TEPs do not preclude active management of reversible conditions but would aid decision making and need to be introduced and adopted by clinical teams.
Patients with TEPs need these to be readily visible to teams providing ongoing care to ensure they are followed.
This review highlighted the complex care management and related decision-making processes of individuals who face acute pathophysiological deterioration leading to death in hospital. Such decision-making processes involve multiple layers of clinicians, from numerous specialities, within often hierarchical teams. Families were involved in contributing to decision making; in these circumstances, patients themselves were frequently too acutely unwell to contribute to all stages of the process. The review identified the need for visibility and clarity of management plans, in spite of the surrounding frame of clinical uncertainty. Even where clear plans were documented they could be buried by subsequent pages of notes, with no effective signposting, a particular problem when further deterioration occurred out of hours. Therefore, the review suggests that there is a clear role for formal TEPs to be introduced more widely into routine practice. Opportunities need to be created for patients and their families to be able to ask for such plans to be made, in consultation with clinicians who know them best, outside of the circumstances of acute deterioration.
Acknowledgments
The authors would like to thank Dr Marion Penn for her assistance with stratification of the sample. The authors would also like to thank Mrs Sally Dace for her patient and public focused involvement and the expert clinicians who reviewed the analysis and contributed to the overall interpretation of the data.
- Murray SA ,
- Kendall M ,
- Boyd K , et al
- Etkind SN ,
- Edmonds PM , et al
- Higginson IJ ,
- Shipman C , et al
- Obolensky L ,
- Matthew G , et al
- Frankau JM , et al
- Clements M ,
- Hickman SE ,
- Keevern E ,
- Cummings A ,
- Campling N , et al
- Trebble TM ,
- Hydes T , et al
- 13. ↵ National Health Services Act . Chapter 41 . London : The Stationery Office , 2006 .
- Heywood RM ,
- Moffat SC , et al
- Nelson CA ,
- Moss AH , et al
- Chidgey-Clark J , et al
- Brimblecombe C ,
- Crosbie D ,
- Lim WK , et al
- Newport KB ,
- Lyckholm L , et al
- Charlson M ,
- Szatrowski TP ,
- Peterson J , et al
Contributors All authors designed the review. NC applied for the necessary approvals. NC and AC extracted the data. NC and AC analysed the data with assistance from SL, NWP and AR. NC and AC drafted the manuscript with assistance from SL, MM, CRM, NWP and AR. All authors critically reviewed the manuscript for intellectual content and approved the final version of the paper.
Funding This work was supported by the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care (NIHR CLAHRC) Wessex, which is a partnership between Wessex NHS organisations and partners, including the NIHR Southampton Biomedical Research Centre, and the University of Southampton.
Disclaimer Funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Competing interests None declared.
Patient consent Not required.
Ethics approval Health Research Authority and Research Ethics Committee South Central – Hampshire A.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The datasets generated and analysed during this study are not available due to the nature of approval for the study. Support under section 251 of the NHS Act (2006) was obtained via the Health Research Authority’s Confidentiality Advisory Group as access to patient identifiable data was required without consent; therefore, no additional data can be made available.
Read the full text or download the PDF:
To read this content please select one of the options below:
Please note you do not have access to teaching notes, referrals of older adults to forensic and psychiatric intensive care services: a retrospective case‐note study in scotland.
The British Journal of Forensic Practice
ISSN : 1463-6646
Article publication date: 1 March 2008
The aim was to determine the number of referrals of people aged 55 and over to three forensic and psychiatric intensive care unit (PICU) services in Scotland, and to describe their demographic, criminological and psychiatric characteristics. Of a total of 1838 referrals, 63 (3.4%) were aged 55 and over. Of these, 35 were referred for court reports or prison assessment and half had been charged with violent or sexual offences. Most were diagnosed as suffering from a psychiatric disorder at the time of assessment, 11 (31.4%) were admitted for further assessment. There were a further 28 admissions to PICU beds. Older adults form a small but important minority of referrals to forensic and PICU services. A single case register would aid further study in this area. Further exploration of the clinical needs of these patients would be useful.
- Elderly offender
- Forensic psychiatry
- Psychiatric services
McLeod, C. , Yorston, G. and Gibb, R. (2008), "Referrals of older adults to forensic and psychiatric intensive care services: a retrospective case‐note study in Scotland", The British Journal of Forensic Practice , Vol. 10 No. 1, pp. 36-43. https://doi.org/10.1108/14636646200800006
Emerald Group Publishing Limited
Copyright © 2008, Emerald Group Publishing Limited
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
Behavioral Sleep Interventions for Children with Rare Genetic Neurodevelopmental Conditions: A Retrospective Analysis of Overall Outcomes for 26 Cases
- ORIGINAL PAPER
- Open access
- Published: 07 May 2024
Cite this article
You have full access to this open access article

- Emma C. Woodford ORCID: orcid.org/0000-0001-9596-8636 1 ,
- Karyn G. France ORCID: orcid.org/0000-0002-6943-5390 1 ,
- Neville M. Blampied ORCID: orcid.org/0000-0002-0158-4904 2 ,
- Ursula Hanning ORCID: orcid.org/0009-0009-8906-8303 1 ,
- Catherine E. Swan 3 &
- Laurie K. McLay ORCID: orcid.org/0000-0001-7002-3695 1 , 4
36 Accesses
Explore all metrics
Sleep difficulties are highly prevalent among children with rare genetic neurodevelopmental conditions (RGNC) such as Angelman and Smith-Magenis syndromes. Behavioral interventions are commonly used in the treatment of sleep difficulties in children; however, research is limited in children with RGNC. This study evaluated the overall effectiveness and acceptability of function-based behavioral sleep interventions for children with RGNC.
Data was collated from a series of experimental single-case research studies with 26 children (18 months to 19 years of age) with a range of RGNC, who received a behavioral sleep intervention. Intervention strategies included circadian (e.g., sleep/wake rescheduling), antecedent (e.g., sleep hygiene), and/or consequence (e.g., positive reinforcement of sleep-conducive behavior and modified extinction) modifications implemented by parents. Clinicians provided support for parents mostly via telehealth methods. Overall outcomes were examined using modified Brinley plots and effect size estimates. The effect of age, gender, and a range of psychological variables on intervention response was also examined.
Improvements in sleep problem severity were observed for 24/26 participants, and gains were maintained at long-term follow-up for 13/16. Interestingly, 50% of the children achieved clinically significant change with less restrictive strategies (e.g., circadian, antecedent and positive reinforcement strategies), suggesting extinction procedures may be used as the last option in a sequence of interventions. Parents generally perceived interventions to be acceptable. There was minimal evidence of any differential response to intervention as a function of age, gender, or psychological variables.
Conclusions
Results suggest function-based behavioral interventions offer an effective and socially valid method for treating sleep disturbance in children with RGNC.
Similar content being viewed by others
The Lighter Touch: Less-Restriction in Sequentially Implemented Behavioral Sleep Interventions for Children with Rare Genetic Neurodevelopmental Conditions

Less Restrictive Behavioral Interventions for Sleep Problems in Children with Neurodevelopmental Disorders: A Single Case Feasibility Study
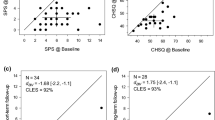

Function-Based Behavioral Interventions for Sleep Problems in Children and Adolescents with Autism: Summary of 41 Clinical Cases
Avoid common mistakes on your manuscript.
Rare genetic neurodevelopmental conditions (RGNC) are group of heterogeneous syndromes characterized by differences in the number and/or structure of chromosomes, which affect < 1:2000 of the general population (European Commission, 2021 ; Rare Diseases International, 2023 ). Phenotypic presentations often include physiological, intellectual, and developmental differences, typically manifested before 22 years of age. Examples of RGNC include Angelman, Prader-Willi, Fragile X, and Smith-Magenis syndromes (McLay et al., 2019 ; Neo et al., 2021 ).
Along with the phenotypic characteristics described, sleep difficulties are prevalent in children (encompassing children and adolescents) with RGNC compared to neurotypical children, with substantial variability depending on the type of sleep difficulty and RGNC (Agar et al., 2021 ; Annaz et al., 2011 ; Kronk et al., 2010 ; Veatch et al., 2021 ). Sleep difficulties experienced may include circadian rhythm disturbances, prolonged sleep onset latency (SOL), night wakings (NWs), unwanted bed-sharing, excessive daytime sleepiness, and early morning waking (EMW). These can have significant adverse short- and long-term effects on learning, behavior, and cognitive development (Kronk et al., 2010 ), as well as parent and family quality of life and physical and mental health (Annaz et al., 2011 ; Chu & Richdale, 2009 ; Kronk et al., 2010 ; Shochat et al., 2014 ; Mörelius & Hemmingsson, 2014 ). Thus, sleep disturbance may further compound the immense challenges already faced by children with RGNC and their families.
Research on the etiology of sleep difficulties associated with RGNC is scarce and mostly focused on biomedical causes (e.g., irregular melatonin production and/or co-occurring medical conditions; Agar et al., 2020 ; Stores, 2016 ; Woodford et al., 2021 ). Consequently, interventions are predominantly pharmacological, most commonly melatonin (e.g., Bailey et al., 2012 ; Braam et al., 2008 ). While melatonin is often effective (Bailey et al., 2012 ; Braam et al., 2008 ), it is not universally funded, many parents have general concerns about chronic use of medication, and problems that are not always associated with melatonin dysregulation (e.g., unwanted bed-sharing, NW and bedtime resistance) often persist (Blampied, 2013 ; McLay et al., 2022 ).
In children with neurodevelopmental conditions (e.g., autism, RGNC), sleep difficulties are generally understood to be the result of a complex interaction between biopsychosocial and behavioral variables (Richdale & Schreck, 2009 ; Veatch et al., 2021 ). Specifically, the behavioral model of sleep disturbance posits that sleep onset occurs at the end of a behavior chain, motivated by sleep pressure, that starts with a bedtime routine and ends with the behavioral quietude necessary for sleep to occur (Blampied, 2013 ; Blampied & van Deurs, 2022 ). Antecedent variables (i.e., variables that precede and/or regulate a behavior) can affect this behavior chain by altering motivation and cues for sleep (Loring & Malow, 2022 ). Homeostatic sleep pressure arising from sleep deprivation, delayed bedtime, or excessive daytime activity can increase an individual’s motivation to sleep and, thus, the reinforcing value of sleep (Borbély et al., 2016 ; Laraway et al., 2003 ). Further, each step in the behavior chain leading up to sleep onset is under stimulus control whereby each sequential step provides the discriminative stimulus for the step that follows (Blampied, 2013 ; Blampied & van Deurs, 2022 ). When discriminative stimuli are absent (e.g., because of a variable bedtime routine) or insufficiently salient, the behavior chain is disrupted. Moreover, when discriminative stimuli are consistently experienced at sleep onset, these cues may become required for sleep onset. Thus, some discriminative stimuli (e.g., a regularly available soft toy) can support, while others (e.g., the absence of parental presence following NWs when otherwise present at initial sleep onset) can interfere with sleep onset both at the start of the night and following NWs (Blampied & van Deurs, 2022 ). Furthermore, reinforcement contingencies also play a critical role in sleep. Consequences that occur immediately following a behavior may increase or decrease the future likelihood of that behavior (Cooper et al., 2020 ). If sleep-conducive (e.g., lying quietly in bed) or sleep-interfering (e.g., calling out) behaviors are reinforced (e.g., by some parental response), this is likely to result in continuation of that behavior (Blampied & van Deurs, 2022 ; McLay & Lang, 2022 ).
To effectively treat sleep difficulties that are underpinned by behavioral factors, it is essential to identify and address the contributing antecedent and consequence variables (Blampied & van Deurs, 2022 ; Jin et al., 2013 ; McLay et al., 2022 ). Functional Behavioral Assessment (FBA) guides the identification of relevant antecedents, contingencies of reinforcement, and other contextual factors to inform the development of individualized interventions for a range of behavioral difficulties including sleep disturbance (Blampied, 2013 ; Jin et al., 2013 ). Interventions may be based on the topography (i.e., presentation) or diagnostic classification of the behavior alone, but such an approach has many conceptual limitations (e.g., the lack of individualization and understanding of mechanisms; Ingram et al., 2005 ). Consequently, FBA-informed interventions are strongly recommended for children with neurodevelopmental conditions such as autism, attention-deficit hyperactivity disorder (ADHD), and intellectual disability (Soorya et al., 2018 ), with increased evidence to support their use in the treatment of sleep disturbance for these populations (e.g., Curfs et al., 1999 ; Didden et al., 1998 ; Jin et al., 2013 ; McLay et al., 2020 ; Weiskop et al., 2005 ).
Given the evidence supporting function-based interventions for children with higher incidence neurodevelopmental conditions such as autism, and the similarities in the type and topography of presenting sleep difficulties, such interventions merit investigation of their effectiveness for sleep difficulties in children with RGNC. Existing research is limited to individual case studies or small N projects (Curfs et al., 1999 ; Didden et al., 1998 ; Woodford et al., 2022 ) and has rarely included adolescents, and interventions have typically been generic rather than being individualized for each case (Allen et al., 2013 ; Weiskop et al., 2005 ). The current study is a retrospective review of 26 participants with RGNC who received function-based behavioral sleep interventions evaluated with experimental, single-case research designs (e.g., Woodford et al., 2022 ; 2024a ). Overall outcomes, possible moderators of intervention response (demographic and child characteristics) and the social validity of the interventions were examined.
The University of Canterbury research team has been investigating the effectiveness of behavioral sleep interventions for children with RGNC since 2018. For each participant, we used FBA to inform the design of individualized, parent-implemented interventions.
Participants and Recruitment
Participants were recruited from throughout New Zealand via service providers for children with RGNC. Between 2018 and 2022, approximately 50 families were screened for the sleep program. Of those screened, 26 families provided consent/assent and met criteria for inclusion in this study. Inclusion criteria were the child (a) was between 18 months and 21 years of age; (b) had or were likely to have a diagnosis of a RGNC, as defined above; (c) had parent-reported sleep difficulties (e.g., prolonged SOL, NWs, unwanted bed-sharing), verified during assessment using sleep diaries and/or video recordings; and (d) had at least commenced the intervention phase of the program and had provided at least one week of intervention data. If the child had a co-occurring condition not currently managed or that might interfere with the implementation of intervention (e.g., epilepsy, tube feeding), approval was obtained from the child’s primary physician; otherwise, they were excluded for safety reasons. Other reasons for exclusion included unstable medication use or withdrawal between the assessment phase and commencement of intervention.
Of the 26 participants (16 males; 10 females), 13 were aged ≤ 6 years, 9 were between 6 and 12 years, and 4 were > 12 years ( M = 7.0, SD = 4.2). This included 13 participants from previously published studies (Woodford et al., 2022 ; 2024a ) and 13 participants who did not meet the specific study criteria of these previous studies ( N = 6) and/or who withdrew during intervention ( N = 9). Inclusion of all participants regardless of whether they adhered to or completed intervention was important for determining the overall, relatively unbiased clinical effectiveness of behavioral sleep intervention (Lachin, 2000 ). Participant details are summarized in Table 1 . In summary, children presented with a range of RGNC. Four cases did not have a confirmed RGNC: Two had a primary diagnosis of cerebral palsy, one had cerebral maldevelopment with cleft frontal lobe and ventriculomegaly and one had a diagnosis of autism and a suspected genetic condition. However, these four children were included due to similarities with those with RGNC (i.e., developmental delay, confirmed neurological alterations and/or were awaiting genetic testing results). All participants had at least one parent-reported co-occurring condition.
Study Design
This study is a retrospective analysis of case data collected within a series of single case experimental studies (e.g., Woodford et al., 2022 ; 2024a ), similar to that conducted by McLay et al. ( 2020 ). Case data was gathered in the context of non-concurrent, multiple-baseline across participants experimental designs wherein all participants were randomly allocated pre-determined baseline lengths (namely, 7, 14, or 21 days). Such random allocation ensured that extraneous factors that may have affected response to intervention (e.g., researcher biases) were controlled for, while the assigned lengths were minimally sufficient to permit stability to be observed (Barlow et al., 2009 ; Christ, 2007 ; Cooper, et al., 2020 ; Kratochwill et al., 2010 ). Given the lack of prior research into the treatment of sleep disturbance with this population, constraints of time and financial support, the disruptions caused by COVID-19, and that by definition RGNC are rare, this N (26) is considered sufficient for research to be informative (Lakens, 2022 ).
All therapeutic support was provided remotely via email, phone, and video conferencing for all participants, except for seven who had in-person meetings in the family home or the university clinic. Sleep interventions were implemented by parents, in the family home, with the support of the research team through digital means.
Each family progressed through the following phases (a) assessment including FBA; (b) baseline; (c) behavioral case formulation and intervention; and (d) maintenance, including short-term (STFU) and long-term (LTFU) follow-up.
As part of the assessment, parents completed a clinical interview (conducted by the first author [EW] or a licensed psychologist or intern psychologist within the research team), at least three nights of parent-reported sleep diaries and/or video recording, and questionnaires (described under “ Measures ” section). The interview provided information about demographic characteristics, presenting sleep difficulties, goals for sleep, child developmental history, and parents’ motivation to engage in a sleep intervention. The Sleep Assessment Treatment Tool (SATT; Hanley, 2005 ), used extensively in prior research including neurodivergent children (e.g., Jin et al., 2013 ; McLay et al., 2020 ; Woodford et al., 2022 ), was used to guide interviewing around sleep.
FBAs for each participant considered data from the SATT (Hanley, 2005 ), sleep diaries, and video (for cases where data patterns were unclear), which were coded according to Antecedent, Behavior, Consequence event recording procedures (ABC recording; Cooper et al., 2020 ). Patterns that suggested potential behavioral (i.e., operant) functions, including (a) sleep/wake schedules that interfered with motivation for sleep; (b) other sleep-interfering antecedent variables (e.g., sleep hygiene, inappropriate discriminative stimuli for sleep, other environmental factors); and (c) reinforcement contingencies maintaining the sleep difficulties, were then identified by the research team.
Baseline data were collected using sleep diaries and video for a randomly assigned baseline length of 7, 14, or 21 days. If visual analysis indicated baseline trends were unstable, or there were threats to internal validity (e.g., unforeseen circumstances such as illness), additional data were collected until baseline stability was achieved (Kazdin, 2011 ). During baseline, parents maintained typical routines throughout the night.
Behavioral Case Formulation and Intervention
Behavioral case formulation and intervention planning as outlined in Blampied ( 2013 ) was undertaken with parents within the framework of the guided participation model (Sanders & Burke, 2014 ). This was done to individualize intervention for each participant to suit the child’s FBA and accommodate factors such as the child’s developmental status, physical functioning, co-occurring conditions, and family preferences (e.g., the number of verbal prompts, steps taken in modified extinction, or rewards chosen differed depending on such factors). Intervention plans typically included three components: (1) circadian modifications (i.e., sleep/wake scheduling); (2) antecedent modifications; and/or (3) consequence-based modifications.
Circadian modifications were designed to increase motivation for sleep in consideration of the National Sleep Foundation Guidelines for age-appropriate sleep durations (Hirshowitz et al., 2015 ) and family routines and preferences. Procedures included restricting/eliminating daytime naps, faded bedtime (see Schreck, 2022 for a discussion of faded bedtime), and establishing consistent sleep/wake schedules.
Antecedent modifications included changes to the sleep environment to minimize precipitants of the sleep difficulties, for example, physical environmental (e.g., the addition of light switch coverings), discriminative stimuli (i.e., consistent sleep setting, visual supports, and use of discriminative stimuli for sleep/wake times), and sleep hygiene modifications (i.e., a consistent bedtime routine, sleep-conducive environment) (Loring & Malow, 2022 ). In addition, visual prompts (e.g., Gro-clocks™, Social Stories™; Gray, 2010 ) were used to facilitate sleep conducive behavior.
Consequence-based modifications included reinforcement of sleep-conducive behavior (i.e., by social and tangible rewards) and modification of contingencies of reinforcement maintaining sleep-interfering behavior (i.e., by extinction and modified extinction). Extinction procedures involved immediate withdrawal of reinforcement for sleep-incompatible behaviors (e.g., digital device use). Modified extinction procedures included faded parental presence and minimal check (see Carnett & McLay, 2022 for a discussion of extinction procedures).
All strategies were parent-implemented. Parent-clinician contact (mostly by digital means) was frequent (i.e., daily in the early stages of implementing strategies and at least once a week at other times), to obtain updated information and provide guidance. Parents were also able to contact the researchers for ad hoc advice as required. The principle of less restriction (Johnston & Sherman, 1993 ) was used to guide intervention planning in most cases, so that consequence modifications were the last option in the sequence of interventions given their complexity and difficulty (Woodford et al., 2022 , 2024a ). Parents were provided revised recommendations both verbally and in written format via email, with systematic formative evaluation of intervention progress. Intervention continued until the parent-clinician determined goals had been met, the family withdrew, or the research team determined that further support would not be beneficial. Intervention duration (including baseline) ranged from 21 to 250 nights ( M = 112). See Table 2 for a summary of intervention procedures and the number of participants who received each intervention.
Maintenance and Follow-Up
On conclusion of intervention, parents moved to the maintenance phase where there was no more nightly sleep data recording or researcher-initiated contact, except for an interview with an independent interviewer to gather program feedback. Parents also completed post-intervention questionnaires before STFU. STFU and LTFU data (available for 17 and 16 families, respectively) were collected via seven nights of video and/or sleep diary recordings commencing at 4–6 and 10–14 weeks after the final day of intervention.
Primary sleep outcome measures included time-series parent-reported sleep diary data and Sleep Problem Severity (SPS) scoring of the diaries. Secondary sleep outcome measures included the Children’s Sleep Habits Questionnaire (Owens et al., 2000 ) global scores and video recording. The CSHQ was completed at pre-intervention (assessment phase) and post-intervention (maintenance phase, before STFU). Other measures included the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001 ), Strengths and Difficulties Questionnaire (SDQ; Goodman, 2001 ), and the Communication domain of the Vineland Adaptive Behavior Scale, Third Edition Parent/Caregiver comprehensive form (VABS-III; Sparrow et al., 2016 ). These were completed by parents’ pre-intervention to assess for potential moderators of intervention response.
Sleep Outcome Measures
Parent-reported sleep diaries.
Sleep diaries, in paper or digital format, were provided to parents via post or email and completed daily, across study phases (Horne & Biggs, 2013 ). Parents’ recorded information regarding their child’s (a) sleep setting; (b) frequency, duration (minutes), and timing of daytime naps and NW; (c) SOL (minutes); (d) frequency of curtain calls (CCs, i.e., bids for parent attention during sleep onset); (e) onset and offset times of bed-sharing with parent(s); (f) and morning wake time. Parents also described occurrences of sleep interfering behavior and their responses to these, as well as disruptions such as illness and family events.
Video Recording
Swann Advanced-Series DVR4-1200 night-time, infrared video cameras, D-Link HD Cloud cameras, or TP-Link Tapo C100 cameras and recording hardware were posted to parents to set up where the child slept (e.g., their bedroom). Video recordings were used to provide a direct measure of children’s sleep (i.e., from the child’s bedtime to morning waketime) where necessary (including providing data on nights in which sleep diaries were incomplete), as well as for interobserver agreement (IOA) calculations (described below). Videos were coded to align with sleep diary data (bedtime, sleep onset time, time and duration of NWs, etc.). Coding was completed by the lead author (EW), a research assistant or the primary clinician for at least 20% of nights across phases, for whom sufficient video was available. All who coded video footage were blinded to the sleep diaries.
Sleep Problem Severity
Sleep Problem Severity (SPS) composite scores were calculated using coded sleep diary data averaged across the final seven nights of each of baseline, intervention, and STFU and LTFU, as in previous studies conducted by the research team (e.g., McLay et al., 2020 ; Clarke et al., 2024 ; Woodford et al., 2022 ; 2024a ). Missing sleep diary information was supplemented with video data, as required. Each child received a single (average) severity score per phase (range 0–22). Scoring code criteria were established based on previously published research defining adequate sleep quality and quantity for preschool (2–4 years 11 months), childhood (5–12 years 11 months), and adolescent (13–18 years) age groups (e.g., Crowley et al., 2014 ; Hirshkowitz et al., 2015 ; Mindell & Moore, 2014 ; Ohayon et al., 2017 ). An average score of > 2 indicates the presence of clinically significant sleep disturbance, i.e., severe disturbance in one sleep domain or moderate disturbance in two sleep domains (e.g., SOL, NWs) per night. SPS scoring criteria are outlined in Online Resource 1.
Children’s Sleep Habits Questionnaire
The CSHQ (Owens et al., 2000 ) is a 45-item parent-report measure of the frequency of specific sleep behaviors over the past seven nights in children 4–10 years of age. The CSHQ yields eight subscale scores and a total sleep disturbance score (range 33–99), with a clinical cutoff > 41 based on a neurotypical sample. This measure has acceptable sensitivity (0.80), specificity (0.72), internal consistency ( α = 0.68–0.78) and test–retest reliability ( r = 0.62–0.79) based on a neurotypical sample (Owens et al., 2000 ). Consequently, it has been rated by the American Psychological Association’s Evidence-based Assessment Task Force as “well-established” (Lewandowski et al., 2011 ). Although not validated for use with children with RGNC, it is widely used in research and practice as a measure of sleep disturbance among children both with and without neurodevelopmental conditions. The CSHQ was completed by parents of all children including those outside of the recommended age range (10/26 participants). This is not uncommon among children with neurodevelopmental conditions (Goodlin-Jones et al., 2008 ; Moss et al., 2014 ) and there was no alternative parent-report measure allowing for comparison across ages (Owens et al., 2000 ).
Treatment Acceptability
The Treatment Acceptability Rating Form-Revised (TARF-R; Reimers et al., 1992 ) is a 20-item parent-report measure given to parents to complete in the maintenance phase to evaluate their perceptions of the effectiveness and acceptability of intervention. Responses are provided on a 7-point Likert scale; 17 items rate treatment acceptability, and three items assess problem severity and parents’ understanding of the intervention process. Higher scores indicate greater acceptability.
Other Measures
Communication domain of the vabs-iii.
The Communication domain of the VABS-III is a parent-report measure of children’s communication level used primarily to inform intervention planning. The Communication domain has three sub-domains, namely expressive, receptive, and written language. Item scores per sub-domain are summed and then converted to standardized age equivalence scores to determine the child’s communicative level relative to developmental norms (Pepperdine & McCrimmon, 2018 ; Sparrow et al., 2016 ). The VABS-III domains have good psychometric properties (e.g., internal consistency, α = 0.94–0.99, and test–retest reliability, r = 0.64–0.94; Pepperdine & McCrimmon, 2018 ) and have been frequently used to assess a range of adaptive behaviors in neurodivergent children (e.g., De Bildt et al., 2005 ).
Child Behavior Checklist
The CBCL (Achenbach & Rescorla, 2001 ) is a parent-report measure of internalizing and externalizing symptoms in children and adolescents between 1.5 and 18 years of age. Specific item ratings are summed to provide internalizing and externalizing problem scale scores and a total score, with higher scores indicating greater symptom severity. These are converted to t -scores to determine whether the child meets criteria for classifying symptom severity as “normal” (non-clinical; t- score < 65), “borderline” (at-risk: t -score 65–69), or “clinical” ( t -score > 70). The CBCL has good psychometric properties based on a neurotypical sample (e.g., internal consistency, α = 0.63–0.90; Achenbach & Rescorla, 2001 ) and sample of pre-schoolers with RGNC (e.g., internal consistency, α = 0.82–0.94; Neo et al., 2021 ). Although not validated for use with children with RGNC > 5 years of age, Glasson et al. ( 2020 ) found it was the most used measure of internalizing and externalizing symptoms in this population.
Strengths and Difficulties Questionnaire
The SDQ is a 25-item parent-report measure of behavioral strengths and difficulties in young people 4–17 years of age (Goodman, 2001 ). It has five subscales: emotional symptoms, conduct problems, hyperactivity-inattention, peer problems, and prosocial behavior. Subscale scores (excluding prosocial behavior) are summed to give a total difficulties score, with higher scores indicating greater difficulty, and score ranges for classifying symptom severity as “normal” (0–13), “borderline” (14–16), and “abnormal” (i.e., clinical, 17–40). The SDQ has adequate psychometric properties based on a neurodiverse sample (e.g., internal consistency [ α = 0.71]; Emerson, 2005 ).
Summary of Measures
The measures described contributed to varying components of data analysis for the 26 participants. In summary, data from sleep diaries and the derived SPS scores were used as the primary outcome measures, while CSHQ global scores were used as a secondary outcome measure in this study; data from sleep diaries and video recordings were the primary measures used for individual time-series analyses such as in (Woodford et al., 2022 ; 2024a ) and interobserver agreement and treatment fidelity calculations; and data from the questionnaires assessing child psychological variables were used for analysis of potential moderators of intervention response in this study and for the analysis of collateral effects in a separate study (Woodford et al., 2024b ).
Data Analysis
For the purposes of tracking outcome data for each case, individual time-series data was analyzed visually accompanied by percentage below the median (Parker et al., 2011 ) calculations as an individual effect size measure (see Woodford et al., 2022 ; 2024a ). For this study, i.e., the purposes of the retrospective analysis of overall outcome, changes in participant SPS and CSHQ scores from pre-intervention to the end of intervention phases (i.e., the final week of intervention, STFU and LTFU for SPS; post-intervention for CSHQ) were examined via modified Brinley plots created using SigmaPlot 14 software (systatsoftware.com). These are a type of scatterplot that displays an individual’s response to intervention within the context of group data (Blampied, 2017 ). Data for each individual is represented as a coordinate pair, with baseline/pre-intervention data on the X axis and data from any subsequent time point on the Y axis. Individual data points that lie on or near the 45° diagonal line show minimal or no therapeutic benefit (Blampied, 2017 ), while points that fall below the diagonal line indicate a reduction in SPS and CSHQ scores (i.e., the direction of therapeutic change). A cross gives the coordinates of the X and Y means and the length of each arm reflects the standard deviation of the respective mean.
Cohen’s d (the standardized mean difference; d av = within-subjects and d s = between-subjects; Lakens, 2013 ) and the percent superiority effect size (PSES; the probability that a randomly selected participant has an improved score at time two relative to time one; McGraw & Wong, 1992 ) were both calculated using Lakens ( 2013 ) calculator. Negative d values indicate clinically desirable change (i.e., improvement on a measure). Interpretation of small ( d ≤ 0.2), medium ( d = ~ 0.5), and large ( d ≥ 0.8) effect sizes were based tentatively on Cohen ( 1988 ) criteria. Confidence intervals (95% CI) about d were used to classify d as reliably different from zero ( p < 0.05) and were calculated using the exploratory software for confidence intervals (ESCI) package by Cumming ( 2012 ).
A separate analysis was conducted to evaluate the possible impact of age, gender, and psychological variables on intervention outcome measured by the primary dependent variable (SPS scores) following the procedure of McLay et al. ( 2020 ). Psychological variables included VABS expressive and receptive language age equivalence scores, CBCL internalizing and externalizing symptom t -scores, and the SDQ total score. Gender was compared as natural groups, while the sample was split at the median score of the variables of interest to create groups (above or below the median) whose SPS scores could then be compared. First, Cohens d s was calculated to compare the groups’ SPS scores at baseline to see if the variable was associated with different SPS levels pre-intervention. Second, Cohens d av was calculated for each group to separately examine the response of the groups to intervention. A d value of at least medium size (≈0.5) on the SPS scores would indicate that the variable of interest either might be influencing baseline levels of severity and or response to intervention.
Interobserver Agreement and Treatment Fidelity
IOA and treatment fidelity were calculated for at least 20% and 30% of nights, respectively, across study phases for all participants for whom sufficient data were available, to determine the reliability of the parent-reported sleep diary data and parent adherence to intervention strategies, respectively. These percentage aims (≥ 20% and 30%) align with that of other sleep treatment evaluation studies (e.g., Kuhn et al., 2020 ; McLay et al., 2020 ) as well as research quality evaluation guidelines (e.g., Reichow et al., 2008 ).
To calculate IOA (%), participant data for all dependent variables (e.g., SOL, frequency and duration of NWs) from sleep diaries and video footage were compared (where variables were detectable by parents) and the formula (agreement/[agreement + disagreement]) × 100 was used. To calculate treatment fidelity (%), information regarding the intervention components implemented by parents as noted in sleep diaries, video coding and case notes were compared to the intervention protocol and the formula (number of intervention components implemented/total recommended components) × 100 was used.
Results are presented in the following order. First, the outcomes of FBA across participants are described. Second, the intervention outcomes, i.e., changes in the sleep measures (SPS and CSHQ scores), are presented, comparing baseline/pre-intervention to post-intervention, STFU and LTFU. Third, possible moderating effects on intervention outcomes of (a) demographic variables and (b) selected psychological variables are presented. Fourth, a summary is provided regarding participant withdrawal. Fifth, data on IOA, treatment fidelity and acceptability are summarized.
FBA Outcomes
All participants had more than one type of parent-reported sleep difficulty (range = 2–6). Sleep difficulties included bedtime resistance, problematic sleep setting, prolonged SOL, CCs, frequent and prolonged NWs, EMW (i.e., time awake prior to goal waketime), unwanted bed-sharing, and/or parental involvement (i.e., the presence and/or support) during sleep onset and NWs. The most common sleep difficulties were prolonged SOL and NWs, present for 23/26 (88%) children. Interestingly, unwanted bed-sharing and parental involvement during sleep onset and NWs was also common, occurring for 14 (54%) and 6 (23%) participants, respectively. Difficulties related to bedtime resistance (6 participants; 23%), sleep setting (5 participants; 19%), CCs (6 participants; 23%) and EMW (9 participants; 35%) were less common.
There was a range of functions underpinning sleep difficulties. Insufficient sleep pressure related to inconsistent and/or developmentally inappropriate sleep/wake times was common (22 participants; 85%). Parent attention related to unwanted bed-sharing or parent involvement in the night was also common (20 participants; 77%). Other functions included escape from the bedroom (12 participants; 46%) and access to tangible items that competed with sleep, such as digital devices (12 participants; 46%), food/drink (8 participants; 31%), toys (7 participants; 27%), and earmuffs (1 participant; 4%). Automatic reinforcement of stereotypy (e.g., repeated vocalizations or physical movements) in the sleep context was identified for six participants (23%). Other factors that contributed to sleep difficulties included toileting issues (3 participants; 12%), caffeine consumption (1 participant; 4%), and co-occurring medical/physical issues (e.g., reflux, colds, allergies, headlice) that either were not known by the researcher pre-intervention or arose during intervention (11 participants; 42%).
Intervention Outcomes
Group pre- and post-intervention SPS and CSHQ data are summarized in Table 3 and displayed in Fig. 1 . Mean SPS and CSHQ scores at baseline were 7.81 (SD = 2.83) and 57.29 (SD = 8.86), respectively, both above the respective clinical cut-offs. For SPS, all but three participants showed a reduction in scores from pre- to post-intervention. Of these three, one boy showed a slight deterioration, while the other two participant scores remained stable. The post-intervention scores of 13 participants fell on or below the clinical cut-off. Although nine participants dropped out in intervention or maintenance phases and do not have follow-up data, this pattern of improvement was maintained. For the CSHQ ( N = 21), all but two participants showed a reduction in scores with intervention; however, the mean score remained above the cut-off ( M = 47, SD = 7.92). Post-intervention scores fell on or below the clinical cut-off for five participants. Cohen’s d av values were − 1.26 (95%CI = − 1.83, − 0.67) and − 1.35 (95%CI = − 1.88, − 0.81) for the pre- to post-intervention CSHQ and SPS, respectively, indicating a large effect. The effect was also large for SPS from pre-intervention to STFU ( d av = − 1.69; 95%CI = − 2.80, − 1.00; PSES = 93%) and LTFU ( d av = − 1.69; 95%CI = − 2.43, − 0.94; PSES = 96%). All the 95% confidence intervals did not include zero, with the upper limits (the smallest probable effect given the negative range) consistently being either in the large or moderate effect range (− 0.67 to − 1.0).
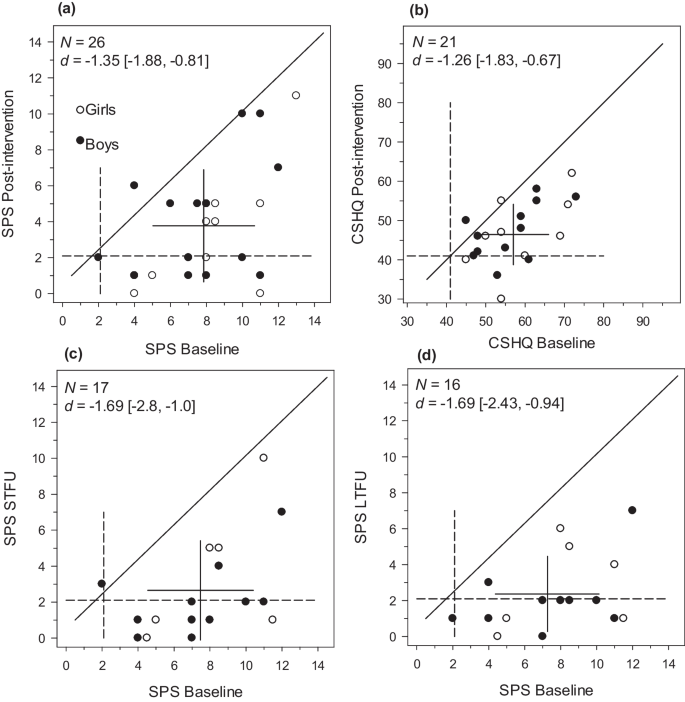
Modified Brinley plots showing individual participants’ change for Sleep Problem Severity (SPS) scores from pre- to post-intervention and short-term (STFU) and long-term follow-up (LTFU) ( a , c , and d ) and for the Children’s Sleep Habits Questionnaire (CSHQ) total scores from pre- to post-intervention ( b ). Note. Filled and unfilled data points represent boys and girls, respectively. The 45° diagonal line (i.e., where X = Y ) represents “no-change.” The dashed lines represent the measure’s clinical cut-off. The means and standard deviations are displayed as a cross, with the mean at the center and the cross arms = ± 1 SD
Analysis of Potential Moderator Variables
Summary data for the potential moderators of age, gender, and selected psychological variables are shown in Table 4 . The outcomes of the analysis of the impact of these potential moderators on intervention outcome are shown in Table 5 . Older children had somewhat lower SPS scores than younger children, suggesting older children had fewer sleep difficulties. Those above the median on the SDQ also had reduced SPS scores, suggesting those with greater social, behavioral, and emotional difficulties had fewer sleep difficulties. The associated effect size was large for both age and SDQ, but none of the other effect sizes were statistically significantly different from zero. All groups showed a consistently large response to intervention (range − 0.96 to − 2.15) with older age, being female, and having higher receptive and expressive language and lower CBCL internalizing symptoms associated with substantially better response to intervention than the respective comparison groups.
Participant Withdrawal
Of the 26 participants, nine (35%) withdrew at varying stages part way through intervention. Withdrawals included participant-initiated discontinuation of intervention prior to meeting parent-clinician determined goals. Reasons for withdrawal reported by parents included family stressors ( N = 4), lack of parental readiness ( N = 4), and/or child medical concerns ( N = 6). The lack of parental readiness (i.e., ambivalence about the proposed intervention, or low motivation) was associated with concerns about the suitability of consequence modifications, which were recommended for some families as a last option in the sequence of interventions.
Data suggests that families who withdrew (i.e., non-completers), compared with those who completed intervention (i.e., completers), had a child younger in age ( M = 3.8 versus 8.8 years) with greater sleep difficulties as measured by the baseline CSHQ ( M = 60.2 versus 55) and SPS ( M = 8.4 versus 7.5). Interestingly, these participants also had generally fewer reported co-occurring conditions ( M = 2.9 versus 3.9) and took fewer medications ( M = 1.2 versus 2.3). There were negligible differences between completers and non-completers in communication level and daytime functioning as measured by the VABS-III and CBCL, respectively.
Interobserver Agreement
IOA was calculated for 72% of cases. The remaining 28% did not have video recordings due to an equipment malfunction, or video was their primary data source (i.e., difficulties were undetectable to parents) meaning IOA was unable to be calculated. IOA was calculated for 15–34% of nights across all phases per participant. IOA was between 72 and 98% ( M = 89%) for observed children, across all study phases and behaviors, suggesting parent-reported diary data were generally reliable.
Treatment Fidelity
Treatment fidelity was calculated over 32–66% of nights across intervention and follow-up phases, for 23 participants who had sufficient data available. Mean treatment fidelity overall was 78% (range 29–100%). Treatment fidelity declined across study phases with a mean of 80% (range 29–100%), 66% (range 43–100%), and 61% (29–100%) across intervention, STFU and LTFU, respectively.
The TARF-R was completed by 19 mothers and 9 fathers for 20/26 participants. The maximum possible total score and subscale scores differ; therefore, the percentage of the possible maximum score was calculated. Mean total TARF-R scores were 100.03 and 102.67 for mothers and fathers, respectively. There were negligible differences between mothers and fathers across subscales. Overall, taking 75% as the lower threshold of a highly acceptable rating, both mothers and fathers rated almost all aspects of intervention (except for disruptiveness) as highly acceptable. TARF-R results are detailed in Table 6 .
This study aimed to evaluate the overall effectiveness of parent-implemented, function-based sleep interventions for 26 children with RGNC. The results of the FBA across children identified a variety of co-occurring sleep difficulties, most commonly prolonged SOL and NWs, maintained by a combination of antecedent and consequence variables. At baseline, 77% of children required parental intervention (i.e., parental presence or bed-sharing) to manage prolonged SOL and NWs, suggesting social attention was a common function. However, sleep difficulties were often multi-functional; that is, they were maintained by social attention, insufficient sleep pressure, escape (i.e., avoidance of bed), automatic (i.e., sensory reinforcement), and/or tangible (e.g., access to devices, toys, and/or food and drink) functions. As a result, the function-based parent-implemented interventions consisted of a range of circadian, antecedent, and consequence modifications.
Results showed that behavioral sleep interventions were somewhat effective for 24/26 children, as reflected in reduced SPS scores and were maintained at follow-up (up to 14 weeks post-intervention). Interestingly, for approximately half, simple modifications to the sleep/wake schedule, sleep environment, and/or reinforcement of target behavior(s) were sufficient to reduce sleep disturbance. For one child, a faded bedtime procedure (Schreck, 2022 ) alone was sufficient to reduce NW and EMW to a clinically meaningful level. This suggests homeostatic sleep pressure may be used to promote sleep onset and maintenance as well as recalibrate the circadian rhythm (Deboer, 2018 ; Laraway et al., 2003 ; Woodford et al., 2022 ) even when behaviors are maintained by other functions (e.g., social, tangible, escape). For the remaining 13 participants, parents implemented an extinction or modified extinction procedure. For ten, addressing socially maintained difficulties, this involved faded parental presence or minimal check, with high rates of success.
Although highly effective for reducing sleep difficulties, particularly those maintained by parent attention, the finding that 50% of children did not require implementation of extinction-based procedures suggests that, for many, such procedures might not be needed. The principle of less restriction advises that practitioners should commence intervention using minimally sufficient and less intrusive strategies (Johnston & Sherman, 1993 ). In the sleep context, less restrictive strategies might comprise circadian and antecedent modifications, preliminary to consequence modifications involving extinction (Blampied & van Deurs, 2022 ; Woodford et al., 2022 ; 2024a ). This study suggests staggering intervention components starting with those that are less restrictive (Johnston & Sherman, 1993 ) may facilitate change using less restrictive methods (Woodford et al., 2022 ; 2024a ). Such an approach is particularly important for children with RGNC and their families, due to the high demands associated with the range and severity of co-occurring conditions or symptoms. In such cases, the need to minimize stress is important for the wellbeing of both the child and parents, as well as the child’s safety (Stores, 2016 ).
Given the range of needs with which children with RGNC present, it is also important that parents feel comfortable implementing behavioral sleep interventions. Only a few studies have evaluated the social validity of such interventions for parents of children with RGNC (Allen et al., 2013 ; McLay et al., 2020 ; Woodford et al., 2022 ), and our finding that these interventions were viewed as reasonable and effective is promising. Given the impact of child sleep disturbance on parents (Mörelius & Hemmingsson, 2014 ) and the acceptability of intervention being a moderator of intervention response (Miller & Rollnick, 2014 ), further research should continue to explore this area.
The influence of age, gender and child psychological variables on the response to behavioral intervention was also considered. Previous research has noted that a range of variables may influence children’s sleep and responses to intervention including behavioral difficulties and low communicative abilities and intellectual functioning (McLay et al., 2020 ; Stores, 2016 ). Interestingly, the present study found children who were younger in age, female and had fewer emotional and behavioral difficulties had slightly greater SPS at baseline. However, there was minimal evidence of any differential response to intervention as a function of those variables. While those with lower internalizing difficulties and greater communicative abilities responded better to intervention, the difference was small, and most children responded positively. Although these results are preliminary, they suggest sleep difficulties may be amenable to change, regardless of the presence and severity of co-occurring factors (France et al., 2022 ).
Furthermore, although physician approval and/or appropriate management of co-occurring medical and/or physical conditions were part of the inclusion criteria for this study, symptoms associated with these conditions likely still played a role in the presenting difficulties for some cases. In addition, alterations to biological sleep processes (e.g., altered melatonin regulation; Woodford et al., 2021 ) may have also played a role. The presence of such factors may explain why some children’s sleep difficulties did not fully resolve and provides context to working with children with RGNC in a clinical setting, i.e., behavioral sleep interventions must be applied in consideration of these (Hamilton et al., 2023 ).
Limitations and Future Research
There are several study limitations which should be considered. First, although the sample size was larger than most current studies that include children with RGNC ( N = 1–66; M = 13.44; McLay et al., 2019 ), it is small relative to the population of children with RGNC, especially given the heterogeneity of that population. The small N reduces confidence in the reliability of the effect size estimates and in the generality of our findings to particular sub-samples of the RGNC population. However, given that RGNC are by definition rare, any evidence of therapeutic effects may be useful, and it should be noted that many of the effect sizes reported were clearly not zero (as shown by their 95%CI). Second, some participants ( N = 9) withdrew during intervention and did not complete follow-up, and so results regarding treatment acceptability gathered post-intervention are limited. Interestingly, however, outcomes suggest positive changes are possible without fully completing intervention. Third, assessment of treatment acceptability was also relatively limited (TARF-R; Reimers et al., 1992 ). A more extensive investigation of parents’ expectations, experiences, resource-limitations, and stress would be desirable. Fourth, IOA could not be calculated for all participants due mostly to technical issues and thus the reliability of parent-report is not known for all participants. Given the measures were based primarily on parent-report, they are susceptible to bias (e.g., halo effect, social desirability bias). Fifth, most of the measures used have not yet been validated for use with children with RGNC. Consequently, there is potential for type one or two errors (Hamrick et al., 2020 ; Neo et al., 2021 ). However, these measures have been widely used in sleep research with neurodivergent children (e.g., Glasson et al., 2020 ; Goodlin-Jones et al., 2008 ; Moss et al., 2014 ). Therefore, they were used for consistency with extant research and because there was a lack of alternative measures. Sixth, although an analysis of potential moderators was completed one variable of interest at a time, information regarding parent variables and the cumulative impact of multiple child and parent variables as potential moderators is lacking. Future research should evaluate the complex interplay of a range of variables simultaneously. Finally, the effectiveness and acceptability of individual intervention components were not evaluated in this study. Future research should continue to implement behavioral strategies in a sequential fashion or evaluate individual strategies, to determine what is minimally sufficient for these children. This is particularly important, since multi-component interventions often require substantial clinical support, which is not always readily available in clinical settings.
In conclusion, this study shows that behavioral interventions are a feasible option for a wide variety of families and children affected by RGNC, the challenges posed by their co-occurring conditions notwithstanding. Although internalizing symptoms and communicative abilities might play a small role in determining intervention response, further research into factors that might moderate the response to intervention is needed. It emphasizes the importance of conducting a comprehensive functional assessment considering behavioral, environmental, developmental, and biological factors. Sound clinical judgment is then required to determine how a behavioral intervention is best implemented for each individual child. Within this, it is important to consider whether parents might or might not need to implement extinction procedures to resolve, or at the very least improve children’s sleep difficulties. Finally, and importantly, this study also provides preliminary evidence to suggest that telehealth individualized sleep support is feasible, having been delivered completely remotely for 22 participants during the peak of the COVID-19 pandemic.
Data Availability
The data that support the findings of this study are available on request from the corresponding author (EW).
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles: Child behavior checklist for ages 6–18, teacher’s report form, youth self-report: An integrated system of multi-informant assessment . University of Vermont, Research Center for Children Youth & Families.
Google Scholar
Agar, G., Brown, C., Sutherland, D., Coulborn, S., Oliver, C., & Richards, C. (2021). Sleep disorders in rare genetic syndromes: A meta-analysis of prevalence and profile. Molecular Autism, 12 (1), 18–18. https://doi.org/10.1186/s13229-021-00426-w
Article PubMed PubMed Central Google Scholar
Agar, G., Oliver, C., Trickett, J., Licence, L., & Richards, C. (2020). Sleep disorders in children with Angelman and Smith-Magenis syndromes: The assessment of potential causes of disrupted settling and night time waking. Research in Developmental Disabilities, 97 , 103555. https://doi.org/10.1016/j.ridd.2019.103555
Article PubMed Google Scholar
Allen, K. D., Kuhn, B. R., DeHaai, K. A., & Wallace, D. P. (2013). Evaluation of a behavioral treatment package to reduce sleep problems in children with Angelman syndrome. Research in Developmental Disabilities, 34 (1), 676–686. https://doi.org/10.1016/j.ridd.2012.10.001
Annaz, D., Hill, C. M., Ashworth, A., Holley, S., & Karmiloff-Smith, A. (2011). Characterisation of sleep problems in children with Williams syndrome. Research in Developmental Disabilities, 32 (1), 164–169. https://doi.org/10.1016/j.ridd.2010.09.008
Bailey, D. B., Raspa, M., Bishop, E., Olmsted, M., Mallya, U. G., & Berry-Kravis, E. (2012). Medication utilization for targeted symptoms in children and adults with Fragile X syndrome: US survey. Journal of Developmental and Behavioral Pediatrics, 33 (1), 62–69. https://doi.org/10.1097/DBP.0b013e318236c0e1
Barlow, D. H., Nock, M., & Hersen, M. (2009). Single case experimental designs: Strategies for studying behavior for change (3rd ed.). Pearson Education.
Blampied, N. M. (2013). Functional behavioral analysis of sleep in infants and children. In A. R. Wolfson & H. E. Montgomery-Down (Eds.), The Oxford handbook of infant, child, and adolescent sleep and behavior. Oxford University Press. https://doi.org/10.1093/oxfordhb/9780199873630.013.0013
Chapter Google Scholar
Blampied, N. M. (2017). Analyzing therapeutic change using modified Brinley plots: History, construction, and interpretation. Behavior Therapy, 48 (1), 115–127. https://doi.org/10.1016/j.beth.2016.09.002
Blampied, N. M., & van Deurs, J. R. (2022). A conceptual framework for understanding and designing behavioral interventions for sleep problems in children on the autism spectrum. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 59–74). Springer International Publishing AG.
Borbély, A. A., Daan, S., Wirz-Justice, A., & Deboer, T. (2016). The two-process model of sleep regulation: A reappraisal. Journal of Sleep Research, 25 (2), 131–143. https://doi.org/10.1111/jsr.12371
Braam, W. J., Didden, H. C. M., Smits, M. G., & Curfs, L. M. G. (2008). Melatonin for chronic insomnia in Angelman syndrome: A randomized placebo-controlled trial. Journal of Child Neurology, 23 (6), 649–654. https://doi.org/10.1177/0883073808314153
Carnett, A., & McLay, L. K. (2022). Behavioral extinction as a treatment for sleep problems in children on the autism spectrum. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 177–191). Springer.
Christ, T. J. (2007). Experimental control and threats to internal validity of concurrent and nonconcurrent multiple baseline designs. Psychology in the Schools, 44 (5), 451–459. https://doi.org/10.1002/pits.20237
Article Google Scholar
Chu, J., & Richdale, A. L. (2009). Sleep quality and psychological wellbeing in mothers of children with developmental disabilities. Research in Developmental Disabilities, 30 (6), 1512–1522. https://doi.org/10.1016/j.ridd.2009.07.007
Clarke, M. A. C., McLay, L. K., France, K. G., & Blampied, N. M. (2024). An evaluation of a stepped-care telehealth program for improving the sleep of autistic children. Research in Autism Spectrum Disorders , 112 . https://doi.org/10.1016/j.rasd.2024.102356
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum.
Cooper, J. O., Heron, T. E., & Heward, W. L. (2020). Applied behavior analysis (3rd ed.). Pearson.
Book Google Scholar
Crowley, S. J., Tarokh, L., & Carskadon, M. A. (2014). Sleep during adolescence. In S. H. Sheldon, R. Ferber, M. H. Kryger, & D. Gozal (Eds.), Principles and practice of pediatric sleep medicine (2nd ed., pp. 45–5). W.B. Saunders. https://doi.org/10.1016/B978-1-4557-0318-0.00006-1
Cumming, G. (2012). Understanding the new statistics: Effect sizes, confidence intervals, and meta-analysis . Routledge. https://doi.org/10.4324/9780203807002
Curfs, L. M., Didden, R., Sikkema, S. P., & De Die-Smulders, C. E. (1999). Management of sleeping problems in Wolf-Hirschhorn syndrome: A case study. Genetic Counseling, 10 (4), 345.
PubMed Google Scholar
De Bildt, A., Sytema, S., Kraijer, D., Sparrow, S., & Minderaa, R. (2005). Adaptive functioning and behaviour problems in relation to level of education in children and adolescents with intellectual disability. Journal of Intellectual Disability Research, 49 (9), 672–681. https://doi.org/10.1111/j.1365-2788.2005.00711.x
Deboer, T. (2018). Sleep homeostasis and the circadian clock: Do the circadian pacemaker and the sleep homeostat influence each other’s functioning? Neurobiology of Sleep and Circadian Rhythms, 5 , 68–77. https://doi.org/10.1016/j.nbscr.2018.02.003
Didden, R., Curfs, L. M., Sikkema, S. P., & de Moor, J. (1998). Functional assessment and treatment of sleeping problems with developmentally disabled children: Six case studies. Journal of Behavior Therapy and Experimental Psychiatry, 29 (1), 85–97.
Emerson, E. (2005). Use of the strengths and difficulties questionnaire to assess the mental health needs of children and adolescents with intellectual disabilities. Journal of Intellectual & Developmental Disability, 30 (1), 14–23. https://doi.org/10.1080/13668250500033169
European Commission. (2021). Rare diseases: Commission activities in the area of rare diseases. European Commision. https://ec.europa.eu/info/research-and-innovation_en?pg=area&areaname=rare
France, K. G., McLay, L. K., Blampied, N. M., Chow, Y. W. Y., & Pin, N. I. (2022). Intervening in cases with clinical complexity. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 59–74). Springer International Publishing AG.
Glasson, E. J., Buckley, N., Chen, W., Leonard, H., Epstein, A., Skoss, R., Jacoby, P., Blackmore, A. M., Bourke, J., & Downs, J. (2020). Systematic review and meta-analysis: Mental health in children with neurogenetic disorders associated with intellectual disability. Journal of the American Academy of Child and Adolescent Psychiatry, 59 (9), 1036–1048. https://doi.org/10.1016/j.jaac.2020.01.006
Goodlin-Jones, B. L., Sitnick, S. L., Tang, K., Liu, J., & Anders, T. F. (2008). The children’s sleep habits questionnaire in toddlers and preschool children. Journal of Developmental and Behavioral Pediatrics, 29 (2), 82–88.
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 40 (11), 1337–1345. https://doi.org/10.1097/00004583-200111000-00015
Gray, C. A. (2010). Social stories™10.1 definition, criteria, & sample stories. Retrieved from http://blogs.4j.lane.edu/communityaccess/files/2013/05/Social-Story-Criteria.pdf
Hamilton, A., Joyce, A., & Spiller, J. (2023). Recommendations for assessing and managing sleep problems in children with neurodevelopmental conditions. Current Developmental Disorders Reports, 10 (4), 274–285. https://doi.org/10.1007/s40474-023-00283-7
Hamrick, L. R., Haney, A. M., Kelleher, B. L., & Lane, S. P. (2020). Using generalizability theory to evaluate the comparative reliability of developmental measures in neurogenetic syndrome and low–risk populations. Journal of Neurodevelopmental Disorders, 12 (1), 16–16. https://doi.org/10.1186/s11689-020-09318-1
Hanley, G. P. (2005). Sleep assessment and treatment tool [Measurement instrument]. Retrieved May 26, 2017, from https://practicalfunctionalassessment.files.wordpress.com/2015/06/satt.pdf
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., DonCarlos, L., Hazen, N., Herman, J., Adams Hillard, P. J., Katz, E. S., Kheirandish-Gozal, L., Neubauer, D. N., O’Donnell, A. E., Ohayon, M., Peever, J., Rawding, R., Sachdeva, R. C., Setters, B., Vitiello, M. V., & Ware, J. C. (2015). National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health, 1 (4), 233–243. https://doi.org/10.1016/j.sleh.2015.10.004
Horne, S. C., & Biggs, S. N. (2013). Actigraphy and sleep/wake diaries. In A. R. Wolfson & H. E. Montgomery-Downs (Eds.), The Oxford handbook of infant, child, and adolescent sleep and behavior (pp. 189–203). Oxford University Press.
Ingram, K., Lewis-Palmer, T., & Sugai, G. (2005). Function-based intervention planning: Comparing the effectiveness of FBA function-based and non—function-based intervention plans. Journal of Positive Behavior Interventions, 7 (4), 224–236. https://doi.org/10.1177/10983007050070040401
Jin, C. S., Hanley, G. P., & Beaulieu, L. (2013). An individualized and comprehensive approach to treating sleep problems in young children. Journal of Applied Behavior Analysis, 46 (1), 161–180. https://doi.org/10.1002/jaba.16
Johnston, J. M., & Sherman, R. A. (1993). Applying the least restrictive alternative principle to treatment decisions: A legal and behavioral analysis. The Behavior Analyst, 16 (1), 103–115. https://doi.org/10.1007/BF03392615
Kazdin, A. E. (2011). Single-case research designs: Methods for clinical and applied settings (2nd ed.). Oxford University Press. https://go.exlibris.link/WsvCgmqY .
Kratochwill, T. R., Hitchcock, J., Horner, R. H., Levin, J. R., Odom, S. L., Rindskopf, D. M. & Shadish, W. R. (2010). Single–case design technical documentation (Version 1.0 [Pilot]). What Works Clearinghouse. https://ies.ed.gov/ncee/wwc/Docs/ReferenceResources/wwc_scd.pdf
Kronk, R., Bishop, E. E., Raspa, M., Bickel, J. O., Mandel, D. A., & Bailey, D. B. (2010). Prevalence, nature, and correlates of sleep problems among children with Fragile X syndrome based on a large scale parent survey. Sleep: Journal of Sleep and Sleep Disorders Research, 33 (5), 679–687. https://doi.org/10.1093/sleep/33.5.679
Kuhn, B. R., LaBrot, Z. C., Ford, R., & Roane, B. M. (2020). Promoting independent sleep onset in young children: Examination of the excuse me drill. Behavioral Sleep Medicine, 18 (6), 730–745. https://doi.org/10.1080/15402002.2019.1674852
Lachin, J. M. (2000). Statistical considerations in the intent-to-treat principle. Controlled Clinical Trials, 21 (3), 167–189. https://doi.org/10.1016/S0197-2456(00)00046-5
Lakens, D. (2022). Sample size justification. Collabra: Psychology , 8(1). https://doi.org/10.1525/collabra.33267
Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Frontiers in Psychology, 4 , 1–12. https://doi.org/10.3389/fpsyg.2013.00863
Laraway, S., Snycerski, S., Michael, J., & Poling, A. (2003). Motivating operations and terms to describe them: Some further refinements. Journal of Applied Behavior Analysis, 36 (3), 407–414.
Lewandowski, A. S., Toliver-Sokol, M., & Palermo, T. M. (2011). Evidence-based review of subjective pediatric sleep measures. Journal of Pediatric Psychology, 36 (7), 780–793.
Loring, W., & Malow, B. (2022). Sleep Hygiene and related interventions: Their impact on sleep. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 127–136). Springer International Publishing AG.
McGraw, K. O., & Wong, S. P. (1992). A common language effect size statistic. Psychological Bulletin, 111 (2), 361–365. https://doi.org/10.1037/0033-2909.111.2.361
McLay, L. K., Carnett, A., & Sigafoos, J. (2022). Functional behavior assessment of sleep problems in children on the autism spectrum. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 77–91). Springer International Publishing AG.
McLay, L. K., France, K. G., Blampied, N. M., van Deurs, J. R., Hunter, J. E., Knight, J., Hastie, B., Carnett, A., Woodford, E., Gibbs, R., & Lang, R. (2020). Function-based behavioral interventions for sleep problems in children and adolescents with autism: Summary of 41 clinical cases. Journal of Autism and Developmental Disorders, 51 (2), 418–432. https://doi.org/10.1007/s10803-020-04548-7
McLay, L. K., & Lang, R. (2022). The role of reinforcement in the treatment of sleep problems. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 161–177). Springer International Publishing AG.
McLay, L., Roche, L., France, K. G., Blampied, N. M., Lang, R., France, M., & Busch, C. (2019). Systematic review of the effectiveness of behaviorally-based interventions for sleep problems in people with rare genetic neurodevelopmental disorders. Sleep Medicine Reviews, 46 , 54–63. https://doi.org/10.1016/j.smrv.2019.04.004
Miller, W. R., & Rollnick, S. (2014). The effectiveness and ineffectiveness of complex behavioral interventions: Impact of treatment fidelity. Contemporary Clinical Trials, 37 (2), 234–241. https://doi.org/10.1016/j.cct.2014.01.005
Mindell, J. A., & Moore, M. (2014). Bedtime problems and night wakings. In S. H. Sheldon, R. Ferber, M. H. Kryger, & D. Gozal (Eds.), Principles and Practice of Pediatric Sleep Medicine (2nd ed., pp. 105–109). W.B. Saunders. https://doi.org/10.1016/B978-1-4557-0318-0.00014-0
Mörelius, E., & Hemmingsson, H. (2014). Parents of children with physical disabilities - perceived health in parents related to the child’s sleep problems and need for attention at night. Childcare, Health & Development, 40 (3), 412–418. https://doi.org/10.1111/cch.12079
Moss, A. H. B., Gordon, J. E., & O’Connell, A. (2014). Impact of sleepwise: An intervention for youth with developmental disabilities and sleep disturbance. Journal of Autism and Developmental Disorders, 44 (7), 1695–1707. https://doi.org/10.1007/s10803-014-2040-y
Neo, W. S., Suzuki, T., & Kelleher, B. L. (2021). Structural validity of the child behavior checklist (CBCL) for preschoolers with neurogenetic syndromes. Research in Developmental Disabilities, 109 , 103834–103834. https://doi.org/10.1016/j.ridd.2020.103834
Ohayon, M., Wickwire, E., Hirshkowitz, M., Albert, S., Avidan, A., Daly, F., Dauvilliers, Y., Ferri, R., Fung, C., Gozal, D., Hazen, N., Krystal, A., Lichstein, K., Mallampalli, M., Plazzi, G., Rawding, R., Scheer, F., Somers, V., & Vitiello, M. (2017). National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health, 3 (1), 6–19. https://doi.org/10.1016/j.sleh.2016.11.006
Owens, J. A., Spirito, A., & McGuinn, M. (2000). The children’s sleep habits questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep, 23 (8), 1043–1049. https://doi.org/10.1093/sleep/23.8.1d
Parker, R. I., Vannest, K. J., & Davis, J. L. (2011). Effect size in single-case research: A review of nine nonoverlap techniques. Behavior Modification, 35 (4), 303–322. https://doi.org/10.1177/0145445511399147
Pepperdine, C. R., & McCrimmon, A. W. (2018). Test review: Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2016), “Vineland adaptive behavior scales, third edition” ("vineland-3") San Antonio, TX: Pearson. Canadian Journal of School Psychology, 33 (2), 157. https://doi.org/10.1177/0829573517733845
Rare Diseases International. (2023). Operational description of rare diseases . Rare Diseases International. https://www.rarediseasesinternational.org/description-for-rd/ .
Reichow, B., Volkmar, F. R., & Cicchetti, D. V. (2008). Development of the evaluative method for evaluating and determining evidence-based practices in autism. Journal of Autism and Developmental Disorders , 38(7), 1311–1319. https://doi.org/10.1007/s10803-007-0517-7
Reimers, T. M., Wacker, D. P., Cooper, L. J., & Deraad, A. O. (1992). Clinical evaluation of the variables associated with treatment acceptability and their relation to compliance. Behavioral Disorders, 18 (1), 67–76. https://doi.org/10.1177/019874299201800108
Richdale, A. L., & Schreck, K. A. (2009). Sleep problems in autism spectrum disorders: Prevalence, nature, & possible biopsychosocial aetiologies. Sleep Medicine Reviews, 13 (6), 403–411.
Sanders, M. R., & Burke, K. (2014). The “Hidden” technology of effective parent consultation: A guided participation model for promoting change in families. Journal of Child and Family Studies, 23 (7), 1289–1297. https://doi.org/10.1007/s10826-013-9827-x
Schreck, K. A. (2022). Bedtime fading and bedtime fading with response cost. In L. K. McLay, K. G. France, & N. M. Blampied (Eds.), Clinical handbook of behavioral sleep treatment in children on the autism spectrum (pp. 137–150). Springer International Publishing AG.
Shochat, T., Cohen–Zion, M., & Tzischinsky, O. (2014). Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Medicine Reviews, 18(1), 75–87. https://doi.org/10.1016/j.smrv.2013.03.005
Soorya, L., Leon, J., Trelles, M. P., & Thurm, A. (2018). Framework for assessing individuals with rare genetic disorders associated with profound intellectual and multiple disabilities (PIMD): The example of Phelan McDermid syndrome. Clinical Neuropsychologist, 32 (7), 1226–1255. https://doi.org/10.1080/13854046.2017.1413211
Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2016). Vineland adaptive behavior scales, third edition (Vineland-3) . Pearson.
Stores, G. (2016). Multifactorial influences, including comorbidities, contributing to sleep disturbance in children with a neurodevelopmental disorder. CNS Neuroscience & Therapeutics, 22 (11), 875–879. https://doi.org/10.1111/cns.12574
Veatch, O. J., Malow, B. A., Lee, H., Knight, A., Barrish, J. O., Neul, J. L., Lane, J. B., Skinner, S. A., Kaufmann, W. E., Miller, J. L., Driscoll, D. J., Bird, L. M., Butler, M. G., Dykens, E. M., Gold, J., Kimonis, V., Bacino, C. A., Tan, W., Kothare, S. V., . . . Glaze, D. G. (2021). Evaluating sleep disturbances in children with rare genetic neurodevelopmental syndromes. Pediatric Neurology, 123 , 30–37. https://doi.org/10.1016/j.pediatrneurol.2021.07.009
Weiskop, S., Richdale, A., & Matthews, J. (2005). Behavioral treatment to reduce sleep problems in children with autism or fragile X syndrome. Developmental Medicine and Child Neurology, 47 (2), 94–104. https://doi.org/10.1017/S0012162205000186
Woodford, E. C., McLay, L., France, K. G., Blampied, N. M., Gibbs, R., Swan, C. E., & Eggleston, M. (2021). Endogenous melatonin and sleep in individuals with rare genetic neurodevelopmental disorders (RGNC): A systematic review. Sleep Medicine Reviews, 57 , 101433–101433. https://doi.org/10.1016/j.smrv.2021.1014
Woodford, E. C., McLay, L., Blampied, N. M., France, K. G., Gibbs, R., Whitaker, C., & McCaughan, E. (2022). Less restrictive behavioral interventions for sleep problems in children with neurodevelopmental disorders: A single case feasibility study. Journal of Developmental and Physical Disabilities , 1–36. https://doi.org/10.1007/s10882-022-09872-7
Woodford, E. C., McLay, L. K., France, K. G., & Blampied, N. M. (2024a). The lighter touch: Less-restriction in sequentially implemented behavioral sleep interventions for children with rare genetic neurodevelopmental conditions. Journal of Autism and Developmental Disorders , 1–22. https://doi.org/10.1007/s10803-024-06234-4
Woodford, E., McLay, L., France, K. G., Blampied, N. M., & Catherine, S. (2024b). Collateral child and parent effects of behavioral sleep interventions for children with rare genetic neurodevelopmental conditions. Advances in Neurodevelopmental Disorders. https://doi.org/10.1007/s41252-024-00399-w
Download references
Open Access funding enabled and organized by CAUL and its Member Institutions. This research was supported by funding from the Royal Society of New Zealand Marsden Fund Fast-Start Grant (#M1211).
Author information
Authors and affiliations.
Te Kaupeka Oranga Faculty of Health, University of Canterbury, Private Bag 4800, Christchurch, New Zealand
Emma C. Woodford, Karyn G. France, Ursula Hanning & Laurie K. McLay
School of Psychology, Speech, and Hearing, Te Kura Mahi ā-Hirikapo, University of Canterbury, Private Bag 4800, Christchurch, New Zealand
Neville M. Blampied
Department of Paediatrics, Te Whatu Ora, Christchurch, New Zealand
Catherine E. Swan
Child Wellbeing Research Institute, University of Canterbury, Private Bag 4800, Christchurch, New Zealand
Laurie K. McLay
You can also search for this author in PubMed Google Scholar
Contributions
EW designed and executed the study, completed assessment and intervention with most participants (EW was enrolled in a licensure-track Child and Family Psychology training program at the time of the project), conducted the data analyses, and wrote the paper. LM provided clinical supervision and collaborated with the design and execution of the study and writing of the paper. KF provided clinical supervision and collaborated with the design of the study and editing of the final manuscript. NB collaborated with the design of the study, data analyses, and the editing of the final manuscript. UH collaborated with data collation and editing of references. CS collaborated with editing the manuscript. All authors approved the final version of the manuscript for submission.
Corresponding author
Correspondence to Emma C. Woodford .
Ethics declarations
Ethics approval.
This research was approved by the relevant university Human Ethics Committee (HEC 2018–48) and has been conducted in accordance with the tenets of the declaration of Helsinki and its later amendments.
Consent to Participate
Informed consent was obtained from all parent participants, and assent was provided by most children (in cases with an adequate level of comprehension determined in collaboration with parents, interaction with the child, and in consideration of the Communication domain Vineland Adaptive Behavior Scales, Third Edition [VABS-III; Sparrow et al., 2016 ] results) for both participation in the study and publishing of results.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 19 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Woodford, E.C., France, K.G., Blampied, N.M. et al. Behavioral Sleep Interventions for Children with Rare Genetic Neurodevelopmental Conditions: A Retrospective Analysis of Overall Outcomes for 26 Cases. Adv Neurodev Disord (2024). https://doi.org/10.1007/s41252-024-00403-3
Download citation
Accepted : 09 April 2024
Published : 07 May 2024
DOI : https://doi.org/10.1007/s41252-024-00403-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Behavioral interventions
- Neurodevelopmental disorders
- Rare genetic syndromes
- Find a journal
- Publish with us
- Track your research
- Biomarker-Driven Lung Cancer
- HER2-Positive Breast Cancer
- Chronic Lymphocytic Leukemia
- Small Cell Lung Cancer
- Renal Cell Carcinoma

- CONFERENCES
- PUBLICATIONS
Retrospective Data Highlight Impact of Dose Escalation of Regorafenib in mCRC
During a Case-Based Roundtable® event, Madappa Kundranda, MD, PhD, discussed recent retrospective studies that looked at outcomes of dose optimization of regorafenib for patients with relapsed/refractory advanced colorectal cancer in the first article of a 2-part series.

Madappa Kundranda, MD, PhD
Gastrointestinal Medical Oncologist
Banner MD Anderson Cancer Center Clinic
Gilbert, AZ

TARGETED ONCOLOGY: How did investigators optimize the dose of regorafenib (Stivarga) in patients with refractory metastatic colorectal cancer?
MADAPPA KUNDRANDA, MD, PHD : This was [shown in] the ReDOS trial [NCT02368886]…. In essence, there were 2 arms. [One] was the dose escalation arm [giving regorafenib] from 80 mg to 120 mg to 160 mg [daily]. [The other arm] was a standard group [who received 160 mg of regorafenib daily]. Within that, there were these subgroups of patients wherein they received the steroid cream preemptively vs those who were reactively treated [for a hand-foot skin reaction]. Although the primary end point of the study was the number of patients getting to the third [cycle of treatment], and it was not powered to look for overall survival, [benefit to dose escalation] was seen in the small subset of patients [HR, 0.72; 95% CI, 0.47-1.10; log-rank P = .12]. 1 This is to be taken with a grain of salt, when you look at the number [of patients], because this wasn’t powered for this, and was not statistically significant. But what it did establish was the fact that with ReDOS, we realized that starting with 160 mg of regorafenib was not the way to dose these patients.
The other thing we realized with ReDOS, and that the subsequent [studies] will indicate, is that getting the 160 mg as the total cumulative dose is not the optimal dose, and we realized that…keeping patients on treatment for longer [leads to] having a prolonged exposure to a lower dose, and the sweet spot is probably somewhere between 120 mg to 140.
The toxicities were significantly higher with the standard dose as opposed to the dose escalation across the board, whether it was the skin toxicities, or whether it was the diarrhea. This is not surprising, but this was one of the studies that first demonstrated that.
What did the presentation on the European patient population at the 2024 American Society of Clinical Oncology Gastrointestinal Cancers Symposium [ASCO GI] show about the use of regorafenib?
In terms of looking at this real-world evidence of the European patient population at 3 years [2019-2022] of looking at the patients who received regorafenib, the key part of this to remember is that when these patients were looked at, [it was] all of these patients who [received] regorafenib irrespective of the line of therapy. It wasn’t a line of therapy study; when they looked at it, it was just the European experience with any line of therapy, and this was presented at ASCO GI this year. 2
Within this patient population, they looked at the ‘ReDOs-like’ [regimen]: dose adjusted [vs] the standard regimen of 160 mg. The ‘dose-adjusted’ [regimen] for patients who started off at 160 mg had dose reductions based on toxicities and how they did. The ‘ReDOS-like’ was exactly what [the study did], which was the 80 mg and 120 mg [dose escalation]. That’s why they call it ‘ReDos-like’, and the standard was still the 160 mg dose.
When we look at these 2 parameters, in terms of the patients who had more lines [of therapy] and at least got past the third cycle of treatment, the ones who did the best were the ones who were dose adjusted. And to a certain degree it reflects what we saw even prior to the ReDOS data, [which was] we stopped them at a dose and then dose deescalated very quickly. This goes to the point of saying that the exposure to a certain degree makes a lot more difference than trying to push for a higher dose. The [mean] duration of treatment across the board is in the magnitude of [2.2 months in the overall population, 2.0 months for ‘ReDos-like’, 2.0 months for dose-adjusted, and 1.7 months for the standard]. This reiterated what we’ve always seen with these drugs, [which was] getting that exposure for a prolonged period of time helps in getting these patients to have a better outcome.
In terms of the reasons for discontinuation, most of it is because of disease progression, which is not unusual.2 But I’m impressed with the fact that quite a few of the patients within the standard arm made [disease progression], whereas, the patients who discontinued within the European population was not as high as I thought it would be.
REFERENCES:
1. bekaii-saab ts, ou fs, ahn dh, et al. regorafenib dose-optimisation in patients with refractory metastatic colorectal cancer (redos): a randomised, multicentre, open-label, phase 2 study. lancet oncol . 2019;20(8):1070-1082. doi:10.1016/s1470-2045(19)30272-4, 2. peeters m, chibaudel b, barzi a, et al. real world (rw) use and outcomes of regorafenib (reg) flexible dosing in patients (pts) with metastatic colorectal cancer (mcrc) in europe. j clin oncol . 2024;42(suppl_3):47. doi:10.1200/jco.2024.42.3_suppl.47.

EP: 1 . Regorafenib Continues to Benefit Patients With Advanced CRC

EP: 2 . Retrospective Data Demonstrates Efficacy of Regorafenib in mCRC
Ep: 3 . retrospective data highlight impact of dose escalation of regorafenib in mcrc.

Behind the FDA Approval of Fruquintinib for Previously Treated mCRC
In season 4, episode 18 of Targeted Talks, Arvind Dasari, MD, MS, dives into the recent approval of fruquintinib for patients with metastatic colorectal cancer.

FDA Oks ColoSense, a Stool Test for Early Colorectal Cancer Detection
The FDA has approved ColoSense, a stool screening test with 93% accuracy for colon cancer in average-risk adults over the age of 45. This noninvasive option may boost early detection rates.

Special Episode: Insight on Targeting Rare Genomic Alterations in Colorectal Cancers
In season 2, episode 6 of Targeted Talks, Dr. Michael J. Overman, joins Targeted Oncology for a special discussion around rare genomic alterations in colorectal cancer

NGS and ctDNA Considered in Advanced Breast Cancer After Progression
During a Case-Based Roundtable® event, Ruth M. O'Regan, MD, led a discussion on whether to order next-generation sequencing and/or circulating tumor DNA testing for a patient with hormone receptor–positive breast cancer after progression in the first article of a 2-part series.

Comparing Choices for IO/TKI Combinations in Advanced RCC
During a Case-Based Roundtable® event, Shilpa Gupta, MD, led a discussion on the combination of immunotherapy and tyrosine kinase inhibitors for patients with advanced renal cell carcinoma in the second article of a 2-part series.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Perkins E, Gambles M, Houten R, et al. The care of dying people in nursing homes and intensive care units: a qualitative mixed-methods study. Southampton (UK): NIHR Journals Library; 2016 Jun. (Health Services and Delivery Research, No. 4.20.)

The care of dying people in nursing homes and intensive care units: a qualitative mixed-methods study.
Appendix 13 retrospective case note analysis form (final version).
(PDF download)
Included under terms of UK Non-commercial Government License .
- Cite this Page Perkins E, Gambles M, Houten R, et al. The care of dying people in nursing homes and intensive care units: a qualitative mixed-methods study. Southampton (UK): NIHR Journals Library; 2016 Jun. (Health Services and Delivery Research, No. 4.20.) Appendix 13, Retrospective case note analysis form (final version)
- PDF version of this title (105M)
Other titles in this collection
- Health Services and Delivery Research
Recent Activity
- Retrospective case note analysis form (final version) - The care of dying people... Retrospective case note analysis form (final version) - The care of dying people in nursing homes and intensive care units: a qualitative mixed-methods study
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Open access
- Published: 10 May 2024
Discharge within 24 h, transvaginal natural orifice transluminal endoscopic surgery- more suitable for ambulatory surgery in gynecology procedures: a retrospective study
- Fangyuan Zhong 1 na1 ,
- Yueyu Dai 2 na1 ,
- Xiaoyan Liao 1 ,
- Wei Cheng 1 ,
- Ying Liu 1 ,
- Yan Liu 1 ,
- Ziru Yan 1 ,
- Yonghong Lin 1 &
- Xiaoqin Gan 1
BMC Women's Health volume 24 , Article number: 283 ( 2024 ) Cite this article
Metrics details
Natural orifice transluminal endoscopic surgery (NOTES) is an achievement in the field of minimally invasive surgery. However, the vantage point of vaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologicalprocedures remains unclear. The main purpose of this study was to compare vNOTES with laparo-endoscopic single-site surgery, and to determine which procedure is more suitable for ambulatory surgery in gynecologic procedures.
This retrospective observational study was conducted at the Department of Gynecology, Chengdu Women’s and Children’s Central Hospital. The 207 enrolled patients had accepted vNOTES and laparo-endoscopic single-site surgery in gynecology procedures from February 2021 to March 2022. Surgically relevant information regarding patients who underwent ambulatory surgery was collected, and 64 females underwent vNOTES.
Multiple outcomes were analyzed in 207 patients. The Wilcoxon Rank-Sum test showed that there were statistically significant differences between the vNOTES and laparo-endoscopic single-site surgery groups in terms of postoperative pain score (0 vs. 1 scores, p = 0.026), duration of anesthesia (90 vs. 101 min, p = 0.025), surgery time (65 vs. 80 min, p = 0.015), estimated blood loss (20 vs. 40 mL, p < 0.001), and intestinal exhaustion time (12.20 vs. 17.14 h, p < 0.001). Treatment with vNOTES resulted in convenience, both with respect to time savings and hemorrhage volume in surgery and with respect to the quality of the prognosis.
These comprehensive data reveal the capacity of vNOTES to increase surgical efficiency. vNOTES in gynecological procedures may demonstrate sufficient feasibility and provide a new medical strategy compared with laparo-endoscopic single-site surgery for ambulatory surgery in gynecological procedures.
Peer Review reports
NOTES focuses on the natural orifices of the body, known as the mouth, anus, umbilicus, urethra, and vagina [ 1 ]. It was first performed in 2004 in a porcine model by researchers at Johns Hopkins University [ 2 ]. Since 2007, as a less invasive procedure, vNOTES has been performed in gynecology practice for the surgical treatment of ovarian cysts, intramural uterine fibroids, ectopic pregnancies, adnexal masses, and pelvic organ prolapse [ 3 , 4 , 5 , 6 ]. Minimally invasive surgeries such as vNOTES are frequently performed [ 7 , 8 ].
Laparoscopic skills allow minimally invasive surgical procedures to be performed in many gynecological procedures. Laparo-endoscopic single-site surgery has advantages over conventional multiple-port laparoscopic practice, on behave of cosmetic appearance, decreased port site pain, and less duration of surgeries [ 9 ]. Advances in technology and laparoscopic techniques have enabled a shift in gynecological surgery from inpatient to more time-efficient settings. Ambulatory surgery, also known as same-day discharge, refers to an operation in which the patient is admitted and discharged within 24 h; in special cases, it should not exceed 48 h [ 10 ]. The growing relevance of the Enhanced Recovery after Surgery (ERAS) concept requires surgeons to continuously refine their surgical skills to ensure less surgery-related damage and pain, shorter hospital stays, and earlier return to normal life [ 11 , 12 ]. After the concept of ambulatory surgery was first proposed in 1909, it has rapidly developed in patients undergoing laparoscopic procedures for benign indications. Ambulatory surgery has been demonstrated to be safe, money-saving, and acceptable to patients [ 13 , 14 ].
This study aimed to determine which vNOTES and laparo-endoscopic single-site surgery are more suitable for Ambulatory surgery in gynecological practice.
This study was conducted at the Department of Gynecology, Chengdu Women’s and Children’s Central Hospital and School of Medicine, University of Electronic Science and Technology. Patients were enrolled if they underwent laparo-endoscopic single-site surgery and vNOTES between February 1, 2021, and March 31, 2022, with one of four attending surgeons who were members of the Department of Gynecology at Chengdu Women’s and Children’s Central Hospital. Patients with poorly controlled medical comorbidities were not eligible for same-day discharge. Patients with advanced (≥ 65 years), congestive heart failure, hepatic disease, history of cerebrovascular accidents, and poorly managed sleep apnea were excluded from the study. Patients were excluded if the pathological analysis of a biopsy revealed malignancy. Patients who required conversion to laparotomy were excluded from the study.
All patients were treated during the course of surgery with ERAS. Patients received preoperative education, urinary catheters and drainage tubes were not placed during surgery, and patients were encouraged to eat and get out of bed as soon as possible after surgery to achieve rapid recovery.
All data were extracted from the patients’ medical records. Four gynecologic surgeons performed vNOTES or laparo-endoscopic single-site (LESS) surgery in the patients included in this study. Laparoscopic instrumentation was performed according to surgeon preference. Complications that occurred within 30 days of surgery were abstracted and categorized by type. The clinical characteristics analyzed included age, body mass index, prior medical or surgical history; postoperative complications such as mortality, unplanned reoperation, delayed discharge, readmission, duration of anesthesia, execution time of surgery, estimated blood loss, postoperative pain score, infection (urinary tract infection, pneumonia), nausea and vomiting, venous thromboembolism, and patient satisfaction within 30 days. Postoperative bleeding that required readmission or blood transfusion was classified as a hemorrhagic complication.
SPSS 22.0 statistical software was used for statistical analysis. The measurement data were expressed as mean and median such as age, BMI. The measurement data of non-normal distribution were described by the median. The Wilcoxon Rank-Sum test was used for comparisons between two groups. All statistical analyses in this study were conducted by two-sided tests, and P < 0.05 was indicative of statistical significance.
Multiple outcomes of 207 patients were analyzed; of these, 39 patients had uterine fibroids (2 vNOTES, 37 LESS), 51 underwent tubal surgery for ectopic pregnancy (36 vNOTES, 15 LESS), six patients were treated for the presence of an ovarian mass (23 vNOTES, 40 LESS), 20 underwent tubal sterilization (20 LESS), and fivepatients underwent hysterectomy (5 LESS) (due to endometrioma, uterine myoma, and CIN endometrial disease). In addition, 29 patients underwent surgery for endometriosis, cervical intraepithelial lesions, endometrial disease, or diseases. After completion of the Wilcoxon Rank-Sum test, especially for the median, there were statistically significant differences between the vNOTES and laparo-endoscopic single-site surgery groups.
As shown in Table 1 , BMI, time spent getting out of bed, urination, and bowel movement were not significantly different between the two groups. Only 3 patients with unplanned reoperation and readmission were included in both the vNOTES and LESS groups. Two of them underwent tubal fenestration surgery but unfortunately had persistent ectopic pregnancy and reoperation for salpingectomy. NOTES assisted vaginal myomectomy was performed to address a 7 cm intramural uterine fibroid located in the posterior uterine wall. The procedure lasted 107 min. However, due to postoperative hematoma formation, the patient required readmission for further treatment. Nine patients (1 vNOTES, 8 LESS) had delayed discharge. One patient in the vNOTES group refused to be discharged the day after surgery for personal reasons. In the LESS group, two patients had fever after surgery, four had hysterectomies, and one had severe anemia and have to stay in the hospital for a blood transfusion. Four patients had delayed discharge due to intestinal exhaust. None of the patients had venous thromboembolism.
As shown in Table 2 , the postoperative pain score (0 vs. 1, p = 0.026), duration of anesthesia (90 vs. 101 min, p = 0.025), duration of surgery (65 vs. 80 min, p = 0.015), estimated blood loss (20 vs. 40 mL, p < 0.001), and intestinal exhaust time (12.20 vs. 17.14 h, p < 0.001) were significantly different. Some patients may require pain relief through oral pain relievers (such as ibuprofen) or intramuscular injections (e.g., pethidine), particularly in the evening after surgery. In this study, the postoperative pain score (vNOTES, 0 vs. LESS, 1) indicated that vNOTES may result in less pain in patients undergoing surgery. The overall duration of the surgical procedures ranged from 55 to 215 min, indicating variability based on factors such as the size and complexity of the mass being treated. In this study, vNOTES procedures were used to treat various pathologies, with a mean surgery duration of approximately 65 min, which is comparable to that of LESS procedures (80 min). Surgeries involving endometrioma and dense pelvic adhesions tended to increase operative time. These studies were conducted primarily using the LESS approach. The comparison between vNOTES and LESS procedures revealed that vNOTES surgery, with an anesthesia duration of 90 min, is more time efficient than LESS surgery. LESS surgery requires 101 min of anesthesia. The comparison of estimated blood loss between vNOTES and LESS highlights another advantage of vNOTES. vNOTES resulted in only 20 mL of blood loss compared with 40 mL with LESS.
Discussions
Ambulatory surgery offers significant advantages by enhancing patient convenience and optimizing the utilization of hospital resources. Additionally, it contributes to substantial cost savings in healthcare and reduces the incidence of nosocomial infections [ 15 ]. Advanced laparoscopic gynecologic surgery is safe and effective in ambulatory surgery centers. As the foundations of laparoscopic surgery in gynecology have expanded, it has become the standard of care. Moreover, the skills of individual surgeons and the availability of advanced instrumentation continue to improve. This minimally invasive approach offers the advantage of minimal abdominal wall trauma.
Minimally invasive surgeries such as vNOTES are frequently performed [ 7 , 8 ]. Baekelandt et al. reported the feasibility of NOTES for treating uterine fibroids in eight cases. All patients were successfully treated without complications and required conversion to standard laparoscopy. Based on their findings, they concluded that vNOTES could serve as a minimally invasive approach for the treatment of uterine fibroids [ 4 ]. Another area in which NOTES is useful is the treatment of ectopic pregnancies. Baekelandt et al. conducted a study focusing on the treatment of pregnancies with unknown locations in 15 patients [ 5 ]. Their approach involved initiating transvaginal hydro-laparoscopy and subsequently performing salpingectomies using the vNOTES technique in 12 patients, with successful outcomes. Kaya et al. reported that vNOTES is a feasible technique for obese women who require a hysterectomy. It provides favorable outcomes, including a shorter surgery duration and postoperative hospitalization. Additionally, patients experienced lower pain scores [ 6 ]. Huang had a study of 1147 patients underwent vNOTES of adnexal surgery, myomectomy, hysterectomy, pelvic floor reconstruction surgery, and malignant tumor surgery, and found that the application of vNOTES is safe and feasible for most gynecological surgeries [ 16 ].
The advantage of magnifying the surgical area with optical systems is that it decreases the umbilical or port-site hernia rates. The NOTES procedure has better outcomes than conventional laparoscopic and open surgeries [ 9 , 17 ]. Potential advantages of vNOTES compared to traditional laparoscopic and robotic approaches include the potential for less pain, decreased operative time, improved cosmesis, and decreased risks [ 18 , 19 ]. Karakaş recently reported the compare of vNOTES with conventional laparoscopy regarding pre-/intra-/postoperative outcomes. In the study, the women who were operated on for emergency indications such as ectopic pregnancy, ovarian torsion, ovarian cyst rupture and acute abdominal pain were evaluated, suggesting that vNOTES could serve as an alternative to conventional laparoscopy. They offer advantages such as shorter surgery duration, lower postoperative pain scores, shorter hospital stays, and better cosmetic outcomes [ 20 ], mirroring the results of the current study. Cihan Kaya et al. reported that hysterectomy performed using vNOTES had a shorter mean operation duration compared to both standard laparoscopy and laparotomy [ 21 ]. They also compared the results of conventional laparoscopic and vNOTES techniques for the treatment of benign adnexal pathologies. The study consisted of 114 patients for oophorectomy, ovarian cystectomy, or ectopic pregnancies, showed that the duration of surgery was significantly shorter in the vNOTES group compared to the conventional laparoscopy group, postoperative hospital stay was significantly shorter in the vNOTES group, Postoperative 6th- and 24th-hour VAS pain scores were significantly lower in the vNOTES group [ 22 ].
Recent studies also have assessed the feasibility of NOTES procedures. These studies found that NOTES procedures were associated with shorter hospital stays, shorter duration of surgery, and reduced total use of analgesics compared to LESS [ 23 ]. vNOTES was equally safe and effective for ovarian cystectomy compared to LESS. vNOTES aligned with the concept of the day-care procedure due to its reduced postoperative pain, shorter exhaust time, and absence of scarring. However, surgeons should conduct a comprehensive preoperative evaluation and exclude patients suspected to have severe pelvic adhesions [ 24 ]. vNOTES can shorten the exhaust time and duration of hospitalization, reduce postoperative pain, and avoid surface surgical scars in tubal pregnancy surgeries, consistent with the ERAS concept [ 25 ].
In Karakaş’ study [ 20 ], vNOTES group had lower VAS scores after 6 h than the conventional laparoscopy group. In our study, the postoperative pain score (vNOTES, 0 vs. LESS, 1) indicated that vNOTES may result in less pain in patients undergoing surgery. However, the necessity for postoperative analgesia depends on an individual patient’s pain tolerance, leading to highly subjective data. The vagina is relatively less sensitive than the abdominal nerves, resulting in less pain when an incision is made in the posterior fornix of the Patients who underwent vNOTES, as opposed to LESS, reported less pain and required fewer painkillers. This advantage allows patients to mobilize sooner after surgery, thereby facilitating recovery of intestinal function.
The surgical execution time (vNOTES 65 min vs. LESS 80 min) suggests that the vNOTES procedure is more time efficient, which is the same with Karakaş’ study [ 20 ]. vNOTES reducing the duration of surgery, the day surgery mode becomes more efficient, facilitating the effective utilization of surgeons, nursing staff, and operating room resources.
This time-saving aspect of vNOTES not only reduces the duration of anesthesia but also minimizes the number of anesthetic drugs administered. Consequently, vNOTES can effectively alleviate postoperative gastrointestinal reactions such as nausea and vomiting as well as mitigate discomforts such as dizziness and headaches. Moreover, vNOTES facilitated swift restoration of gastrointestinal function by minimizing the inhibition of intestinal peristalsis. In the present study, patients undergoing vNOTES exhibited shorter intervals to intestinal exhaust, leading to fewer instances of delayed discharge than those undergoing LESS. This observation underscores the advantages of vNOTES in promoting quicker postoperative recovery and optimizing patient outcomes.
The lower blood loss in patients treated with vNOTES contributed to the expedited postoperative recovery and faster restoration of normal vital signs. Additionally, it reduces the likelihood of postoperative blood transfusion. Based on clinical experience, researchers have observed that patients with higher postoperative hemoglobin levels have a decreased risk of developing complications such as postoperative infections. Therefore, minimizing blood loss during surgery, as achieved with vNOTES, may help mitigate these potential complications and improve the overall patient outcomes.
This study has several limitations. The retrospective nature of the study may have been constrained by inherent selection bias. Additionally, limitations related to the availability of medical records and the possibility of transcription errors could affect the accuracy. Moreover, the number of postoperative complications may be underreported as patients may have sought care at their physician’s office or a different hospital. Furthermore, while much of the focus has been on outcomes and costs, it is crucial to include discussions that compare measures of patient experience. This encompasses experiences from the waiting room to the care received pre- and post-operatively.
These comprehensive data revealed the capacity of vNOTES to enhance surgical efficiency in ambulatory surgery. Treatment with vNOTES not only saves time and reduces hemorrhage volume during surgery but also improves the quality of prognosis. Similar findings have been reported in other studies, suggesting that vNOTES could serve as an alternative to conventional laparoscopy. They offer advantages such as shorter surgery duration, lower postoperative pain scores, shorter hospital stays, and better cosmetic outcomes [ 20 ], mirroring the results of the current study. vNOTES procedures in gynecology have demonstrated sufficient feasibility and provide a new medical strategy compared with laparo-endoscopic single-site surgery in ambulatory surgery in the ERAS mode.
In conclusion, vNOTES procedures showed promising results in treating various gynecological diseases and may be more suitable than LESS procedures in ambulatory surgery centers. However, further investigation is warranted to validate these findings and achieve better surgical outcomes in the near future.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy restricions.
Kale A, Sarıibrahim B. Bas¸ Ol, Hysterectomy and salphingoopherectomy by Transvaginal Natural Orifice Transluminal endoscopic surgery (NOTES): Turkish surgeons’ initial experience. Int J Surg. 2017;47(November):62–8.
Article PubMed Google Scholar
Kalloo AN, Singh VK, Jagannath SB, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–7.
Zorron R, Filgueiras M, Maggioni LC, Pombo L, Lopes Carvalho G. Lacerda Oliveira, NOTES. Transvaginal cholecystectomy: report of the first case. Surg Innov. 2007;14:279–83.
Baekelandt J. Transvaginal naturalorifice transluminal endoscopic surgery: a new approach to myomectomy. Fertil Steril. 2018;109:179.
Baekelandt J, Vercammen J. IMELDA transvaginal approach to ectopic pregnancy: diagnosis by transvaginal hydrolaparoscopy and treatment by transvaginal natural orifice transluminal endoscopic surgery. Fertil Steril. 2017;107:e1–2.
Kaya C. The comparison of Surgical outcomes following laparoscopic hysterectomy and vNOTES hysterectomy in obese patients. J Invest Surg. 2022;35(4):862–7.
Naoyuki, Yoshiki. Review of transvaginal natural orifice transluminal endoscopic surgery in gynecology. Gynecol Minim Invasive Ther. 2017;6:1–5. (February (1)).
Article Google Scholar
Li CB, Hua KQ. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologic surgeries: a systematic review. Asian J Surg. 2020;43:44–51.
Article CAS PubMed Google Scholar
Baekelandt J, De Mulder PA, Le Roy I, Mathieu C, Laenen A, Enzlin P, et al. Postoperative outcomes and quality of life following hysterectomy by natural orifice transluminal endoscopic surgery (NOTES) compared to laparoscopy in women with a non-prolapsed uterus and benign gynaecological disease: a systematic review and metaanalysis. Eur J Obstet Gynecol Reprod Biol. 2017;208:6–15.
International Association for Ambulatory. Surgery (IAAS)ambulatory surgery handbook. London, UK: International Association for Ambulatory Surgery; 2013.
Google Scholar
Ripolles-Melchor J. Association between use of enhanced recovery after surgery protocols and postoperative complications after gastric surgery for cancer (POWER 4): a nationwide, prospective multicentre study. Cir. Esp. (Engl. Ed.). 2023.
Nelson G. Enhanced recovery after surgery (ERAS(R)) society guidelines for gynecologic oncology: addressing implementation challenges – 2023 update. Gynecol Oncol. 2023;173:58–67.
Nahas S, Feigenberg T, Park S. Feasibility and safety of same-day discharge after minimally invasive hysterectomy in gynecologic oncology: a systematic review of the literature. Gynecol Oncol. 2016;143:439–42.
Gien LT, Kupets R, Covens A. Feasibility of same-day discharge after laparoscopic surgery in gynecologic oncology. Gynecol Oncol. 2011;121:339–43.
Hurt WG. Outpatient gynecologic procedures. Surg Clin North Am. 1991;71:1099–110.
Huang L. Transvaginal natural orifice transluminal endoscopic surgery in gynecological procedure: experience of a women’s and children’s medical center from China. J Obstet Gynaecol Res. 2022;48:2926–34.
Lee CL, Wu KY, Su H, Wu PJ, Han CM, Yen CF. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery (NOTES): a series of 137 patients. J Minim Invasive Gynecol. 2014;21:818–24.
Lerner VT, May G, Iglesia CB. Vaginal natural orifice transluminal endoscopic surgery revolution: the next frontier in gynecologic minimally invasive surgery. J Soc Laparoendosc Surg. 2023;27(1).
Chaccour C, Giannini A, Golia D’Augè T, et al. Hysterectomy using vaginal natural orifice transluminal endoscopic surgery compared with classic laparoscopic hysterectomy: a new advantageous approach? A systematic review on surgical outcomes. Gynecol Obstet Invest. 2023;88:187–96.
Karakaş S. Comparison of vNOTES technique with conventional laparoscopy in gynecological emergency cases. Minim Invasive Ther Allied Technol. 2022;31(5):803–9.
Kaya C. Hysterectomy by vaginal-assisted natural orifice transluminal endoscopic surgery: initial experience with twelve cases. J Turk Ger Gynecol Assoc. 2018;19(1):34–8.
Article PubMed PubMed Central Google Scholar
Kaya C. Conventional laparoscopy or vaginally assisted natural orifice transluminal endoscopic surgery for Adnexal pathologies: a paired sample cross-sectional study. J Invest Surg. 2021;34(11):1185–90.
Baekelandt JF, De Mulder PA, Le Roy I, Mathieu C, Laenen A, Enzlin P, et al. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery versus laparoscopy as a day-care procedure: a randomised controlled trial. BJOG. 2019;126:105–13.
Xie A. Transvaginal natural orifice endoscopic surgery for ovarian cystectomy: a more suitable surgical approach for the day-care procedure. Front Med (Lausanne). 2023;10:1164970.
Liu Y. Transvaginal natural orifice endoscopic surgery for tubal ectopic pregnancy: a more suitable surgical approach for enhanced recovery after surgery. Heliyon. 2024;10(2):e24945.
Download references
Acknowledgements
Not applicable.
Author information
Fangyuan Zhong and Yueyu Dai contributed equally to this work.
Authors and Affiliations
Department of Gynecology and Obstetrics, School of Medicine, Chengdu Women’s and Children’s Central Hospital, University of Electronic Science and Technology of China, 1617 Riyue Avenue, Chengdu, Sichuan, 610073, China
Fangyuan Zhong, Xiaoyan Liao, Wei Cheng, Ying Liu, Yan Liu, Ziru Yan, Yonghong Lin & Xiaoqin Gan
The Second Affiliated Hospital of Chongqing Medical University, Chongqing, 400042, China
You can also search for this author in PubMed Google Scholar
Contributions
ZFY: study concept, data verification, literature review, manuscript writing, and manuscript revision. DYY: data verification, statistical analysis, manuscript revision. GXQ: data verification, literature review, and manuscript revision. LXY, CW: preparation of data for statistical analysis, approval of statistical results and outcomes. LL (Ying Liu), LL (Yan Liu), YZR : manuscript revision, data verification for revised manuscript. LYH: final approval of the manuscript. All authors reviewed the manuscript.
Corresponding author
Correspondence to Xiaoqin Gan .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of Chengdu Women’s and Children’s Central Hospital (No: [2023]106). All participants provided written informed consent after enrollment. All methods were carried out in accordance with relevant institutional guidelines and regulations.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhong, F., Dai, Y., Liao, X. et al. Discharge within 24 h, transvaginal natural orifice transluminal endoscopic surgery- more suitable for ambulatory surgery in gynecology procedures: a retrospective study. BMC Women's Health 24 , 283 (2024). https://doi.org/10.1186/s12905-024-03132-w
Download citation
Received : 06 November 2023
Accepted : 06 May 2024
Published : 10 May 2024
DOI : https://doi.org/10.1186/s12905-024-03132-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Laparo-endoscopic single-site surgery
- Ambulatory surgery
- Gynecology procedures
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Retrospective delirium ascertainment from case notes: a retrospective cohort study
Collaborators.
- Geriatric Medicine Research Collaborative : Abigail Wrathall , Aidan Ryan , Al Wakkass Mahmood , Alexander Harbinson , Alice Wheeler , Amr Bazaraa , Amy Walter , Anekea Ross , Anna Reay , Benjamin Jelley , Carly Welch , Chenxian Wu , Chioma Iwu , Christopher Miller , Daisy Wilson , Dhruv Sarma , Elisabeth Hunter , Elizabeth J Ellis , Elizabeth Lonsdale-Eccles , Emily McNicholas , Fiona E Macdonald , Fiona Herbert , Gerry McGonigal , Hannah J Robinson , Hannah Watson , Hussun-Ara Shah , Ijeoma T Obi , Imola Bargaoanu , James E Lucocq , Jane Giddings , Jane Masoli , Jenni Burton , Joanne Taylor , Jodie Crofts , John Headlam , Kelli Torsney , Kumudhini Giridharan , Lahiru Satharasinghe , Laura J Beeley , Lauren McCluskey , Liji Ng , Lindsay Jones , Mary Ni Lochlainn , Michael Sj Wilson , Minal D Patel , Mustafa Alsahab , Nader Nashed , Natalie Cox , Oliver Todd , Olivia Handley , Olugbenro Akintade , Philip Nwabufor , Philippa K Traill , Phillipa Adams , Qurrat Ul Ain , Rinata Farah , Robert Grange , Roisin Healy , Ruth Willott , Sarah Jagdeo , Sarah Richardson , Shonit Nagumantry , Simon M Stapley , Sophie J Irwin , Sophie Wright , Srividya Sundara , Swetha Byravan , Tarunya Vedutla , Thomas A Jackson , Thomas Arkle , Thyn Thyn , Vee-Han Lim , Victoria Gaunt , Yathu Matheswaran , Zeinab Majid , Carly Welch
- PMID: 34049901
- PMCID: PMC8166612
- DOI: 10.1136/bmjopen-2020-042440
Objectives: This study sets out to ascertain if recognition of delirium impacts on patient outcomes.
Design: Retrospective cohort study.
Setting: Unscheduled admissions to acute care trust/secondary care UK hospitals.
Participants: Six hundred and fifty-six older adults aged ≥65 years admitted on 14 September 2018.
Measurements: Delirium was ascertained retrospectively from case notes using medical notes. Documented delirium was classified as recognised delirium and retrospectively ascertained delirium was classified as unrecognised delirium.
Primary and secondary outcome measures: Primary outcome measure: inpatient mortality.
Secondary outcome measures: length of stay, discharge destination.
Results: Delirium was present in 21.1% (132/626) of patients at any point during admission. The presence of delirium was associated with increased mortality (HR 2.65, CI 1.40 to 5.01). Recognition of delirium did not significantly impact on outcomes.
Conclusions: Delirium is associated with adverse outcomes in hospitalised older adults. However, there is insufficient evidence that recognition of delirium affects outcomes. However, delirium recognition presents an opportunity to discuss a person's overall prognosis and discuss this with the patient and their family. Further research is needed to assess the pathophysiology of delirium to enable development of targeted interventions towards improved outcomes in patients with delirium.
Keywords: delirium & cognitive disorders; geriatric medicine; medical education & training.
© Author(s) (or their employer(s)) 2021. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ.
Publication types
- Research Support, Non-U.S. Gov't
- Delirium* / diagnosis
- Delirium* / epidemiology
- Hospitalization
- Patient Discharge
- Retrospective Studies
Grants and funding
- RTF107/0117/DMT_/The Dunhill Medical Trust/United Kingdom
CORRECTION article
Corrigendum: second malignant neoplasms within 5 years from first primary diagnosis in pediatric oncology patients in canada: a population-based retrospective cohort study.
This article is a correction to:
Second malignant neoplasms within 5 years from first primary diagnosis in pediatric oncology patients in Canada: a population-based retrospective cohort study
- Read original article

- 1 Lifespan Chronic Disease and Conditions Division, Public Health Agency of Canada, Ottawa, ON, Canada
- 2 Department of Pediatrics, Division of Hematology-Oncology, Izzak Walton Killam (IWK) Health Centre, Halifax, NS, Canada
- 3 Faculty of Medicine, Dalhousie University, Halifax, NS, Canada
- 4 Surveillance Systems and Data Management Division, Public Health Agency of Canada, Ottawa, ON, Canada
- 5 Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 6 Centre for Health Sciences Research, University of Queensland, Brisbane, QLD, Australia
- 7 Division of Pediatric Hematology-Oncology, CHU de Québec-Centre Mère-Enfant Soleil, Quebec City, QC, Canada
- 8 Research Centre of the CHU de Québec, Axe Reproduction, Santé de la Mère et de l’Enfant, Quebec City, QC, Canada
- 9 C17 Research Network, C17 Council, Edmonton, AB, Canada
- 10 Department of Pediatrics and Child Health, University of Manitoba, Winnipeg, MB, Canada
- 11 Department of Pediatrics, Division of Pediatric Hematology-Oncology, Charles-Bruneau Cancer Center, Centre Hospitalier Universitaire (CHU) Sainte-Justine, Montréal, QC, Canada
- 12 Immune Diseases and Cancers Axis, CHU Sainte-Justine Research Center, Montréal, QC, Canada
- 13 Department of Pediatric Hematology-Oncology, CancerCare Manitoba, Winnipeg, MB, Canada
- 14 Division of Hematology Oncology, The Hospital for Sick Children, Toronto, ON, Canada
- 15 Department of Anesthesia and Intensive Care, IRCCS San Raffaele Scientific Institute, Milan, Italy
- 16 Department of Pharmacy, Izzak Walton Killam (IWK) Health, Halifax, NS, Canada
- 17 Faculty of Health Professions, Dalhousie University, Halifax, NS, Canada
- 18 Child Health Evaluative Sciences, Research Institute, The Hospital for Sick Children, Toronto, ON, Canada
A Corrigendum on Second malignant neoplasms within 5 years from first primary diagnosis in pediatric oncology patients in Canada: a population-based retrospective cohort study
By Ricci C, Subburaj D, Lim K, Shukla N, Kaur J, Xie L, Laverty M, Zakaria D, Pole J, Pelland-Marcotte M-C, Barber R, Israels SJ, Tran T-H, Oberoi S, Renzi S, MacDonald T, Sung L and Kulkarni K (2024). Front. Oncol. 14:1376652. doi: 10.3389/fonc.2024.1376652
In the published article, there was an error in the legend for Figure 5 to 7 as published. Currently it stated “This hazard ratio has been suppressed because less than 5 patients have the characteristic.” The corrected legend appears below.
“ƚ indicates this hazard ratio has been suppressed because less than 5 patients have the characteristic.”
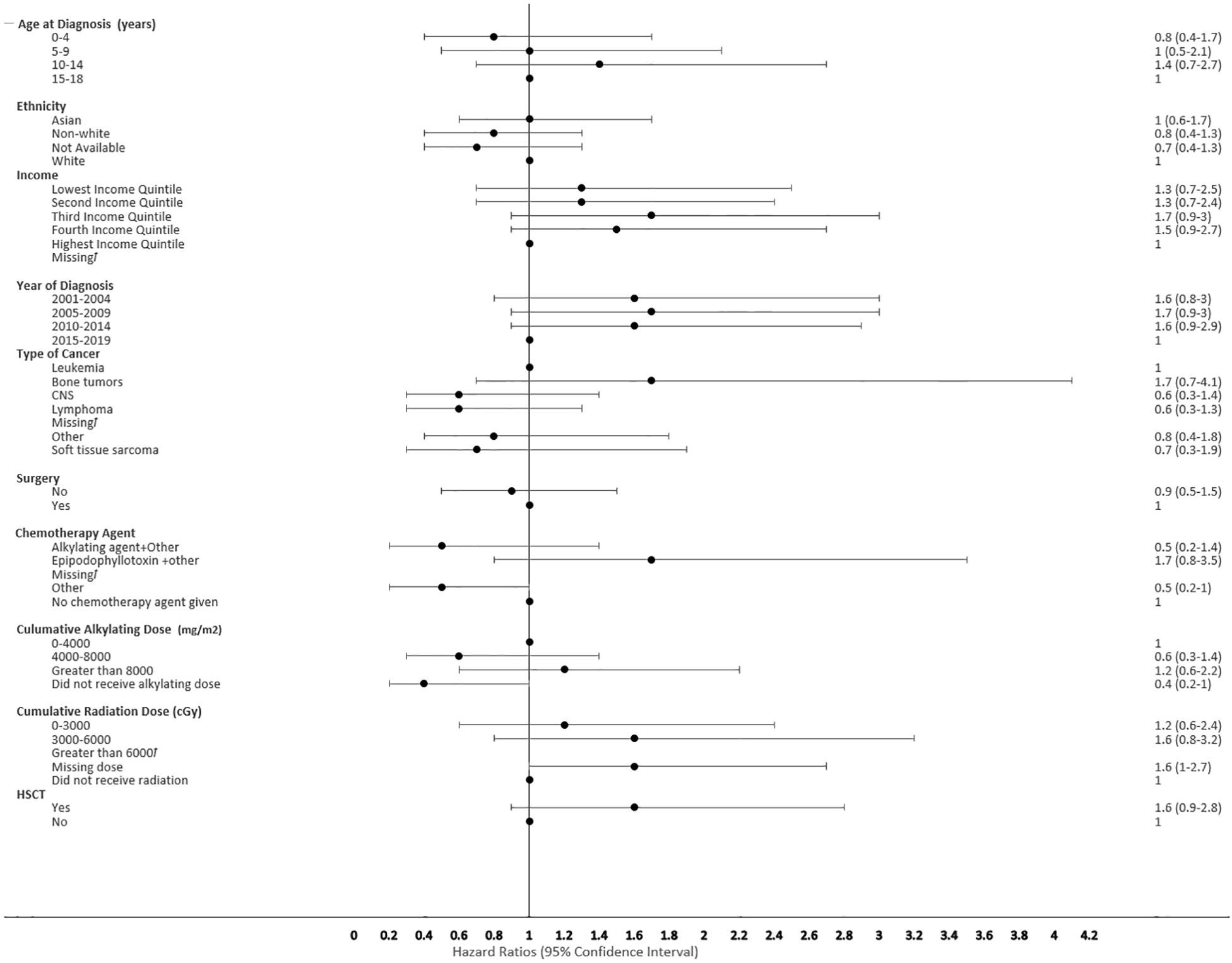
Figure 5 Forest plot depicting the variables and adjusted hazard ratio for SMN. ƚ indicates this hazard ratio has been suppressed because less than 5 patients have the characteristic.
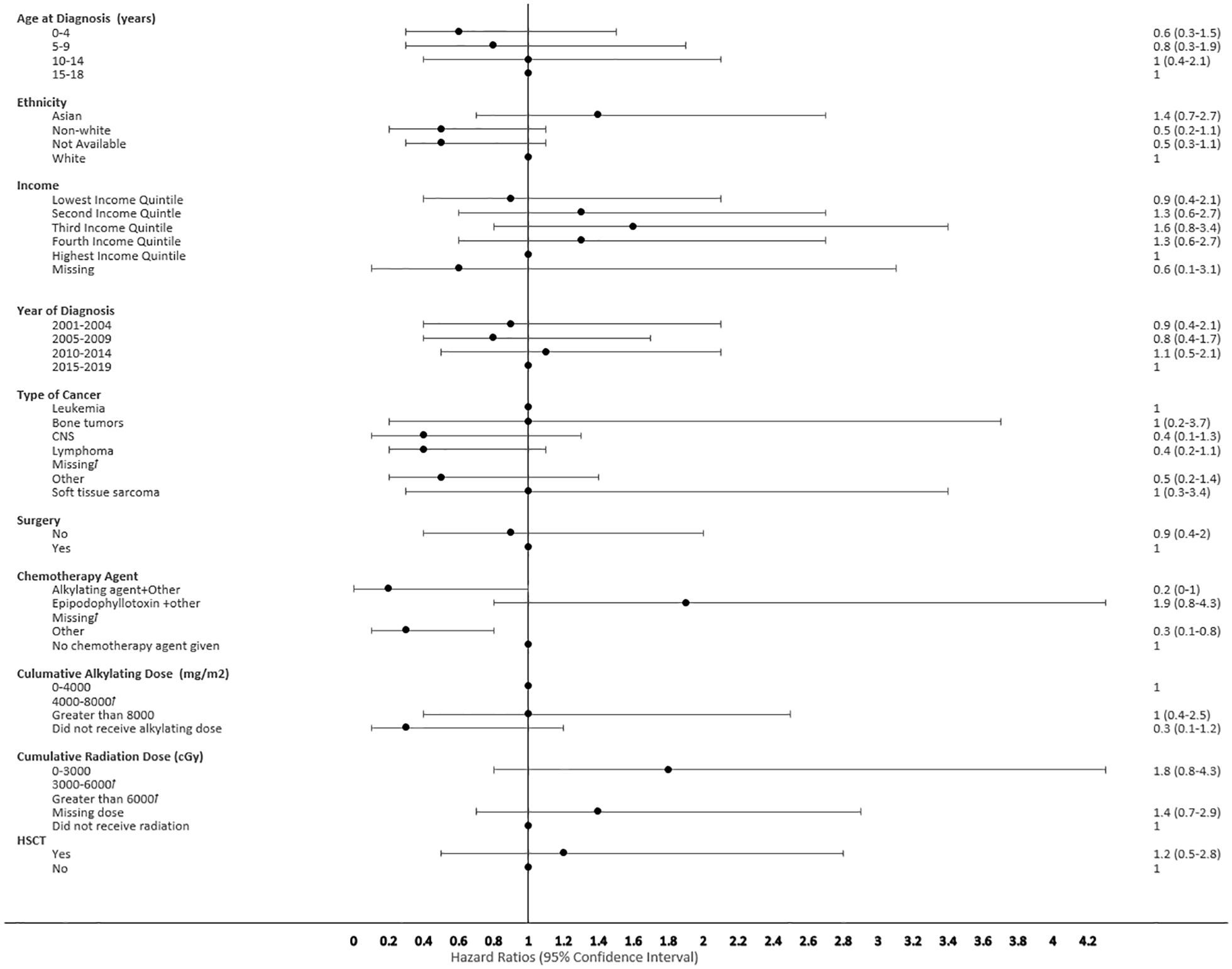
Figure 6 Forest plot depicting the variables and adjusted hazard ratio for SMN developed within 0-2 years. ƚ indicates this hazard ratio has been suppressed because less than 5 patients have the characteristic.
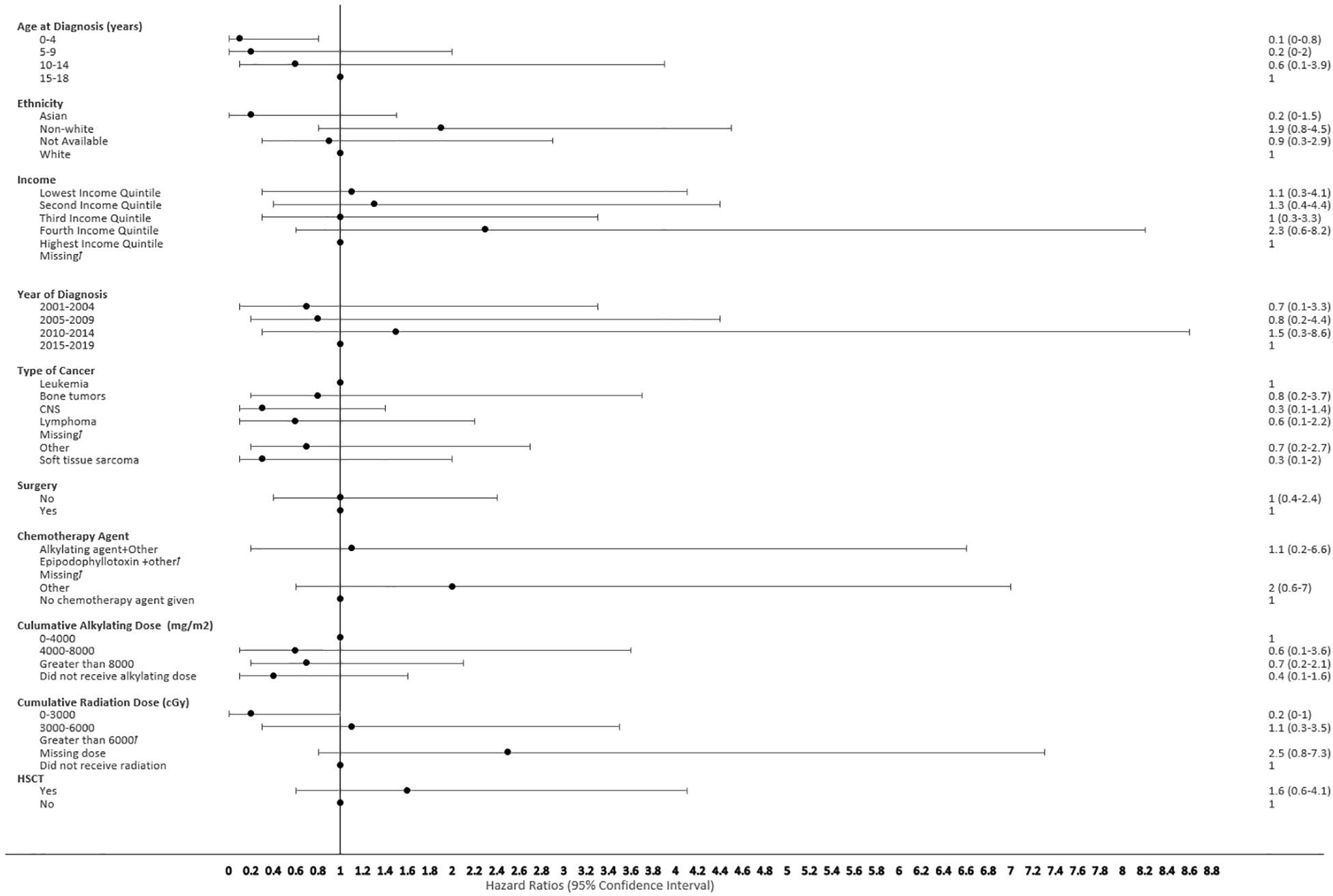
Figure 7 Forest plot depicting the variables and adjusted hazard ratio for SMN developed within 2-5 years. ƚ indicates this hazard ratio has been suppressed because less than 5 patients have the characteristic.
The authors apologize for this error and state that this does not change the scientific conclusions of the article in any way. The original article has been updated.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Keywords: oncology, pediatrics, risk factors, early second malignant neoplasm (early SMN), Canada, surveillance
Citation: Ricci C, Subburaj D, Lim K, Shukla N, Kaur J, Xie L, Laverty M, Zakaria D, Pole J, Pelland-Marcotte M-C, Barber R, Israels SJ, Tran T-H, Oberoi S, Renzi S, MacDonald T, Sung L and Kulkarni K (2024) Corrigendum: Second malignant neoplasms within 5 years from first primary diagnosis in pediatric oncology patients in Canada: a population-based retrospective cohort study. Front. Oncol. 14:1418512. doi: 10.3389/fonc.2024.1418512
Received: 16 April 2024; Accepted: 22 April 2024; Published: 10 May 2024.
Approved by:
Copyright © 2024 Ricci, Subburaj, Lim, Shukla, Kaur, Xie, Laverty, Zakaria, Pole, Pelland-Marcotte, Barber, Israels, Tran, Oberoi, Renzi, MacDonald, Sung and Kulkarni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kate Lim, [email protected] ; Ketan Kulkarni, [email protected]
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
The retrospective chart review (RCR), also known as a medical record review, is a type of research design in which pre-recorded, patient-centered data are used to answer one or more research questions [ 1 ]. The data used in such reviews exist in many forms: electronic databases, results from diagnostic tests, and notes from health service ...
Objectives To determine which of the two methods of case note review provide the most useful and reliable information for reviewing quality of care. Design Retrospective, multiple reviews of 692 case notes were undertaken using both holistic (implicit) and criterion-based (explicit) review methods. Quality measures were evidence-based review criteria and a quality of care rating scale. Setting ...
The methodology used for this study (retrospective case note review) may have lead to some bias, as it relies on the quality of documentation in patient case notes. We have no reason to believe that the quality of note keeping may be different if a patient has dementia. The quality of end-of-life care was not rated blind to the presence or ...
Retrospective case note review of acute and inpatient stroke outcomes. The annual incidence of stroke in the community is about 2 per 1000 population, 1 whereas among hospital inpatients it is 11 per 1000. 2 However, a study that systematically and simultaneously identifies all inpatients experiencing stroke and all patients admitted with ...
This was a multicentre retrospective cohort study within the UK using case notes review. Patients were identified through consult with site patient record and informatics teams. We included patients aged 65 years and older, who were admitted on 14 September 2018 across all sites as unscheduled admissions, with lengths of stay of 2 days or greater.
At follow-up, 8 to 11 months later, only two of 19 (11 %) patients were still taking risperidone. We suggest that risperidone does have a role in a minority of TS sufferers but it is not suggested as the first line treatment. More placebo-controlled studies using risperidone are clearly indicated.
Aim To describe how decision making inter-relates with the sequence of events in individuals who die during admission and identify situations where formal treatment escalation plans (TEPs) may have utility. Design and methods A retrospective case note review using stratified sampling. Two data analysis methods were applied concurrently: directed content analysis and care management process ...
A retrospective case note audit of older patients dying on an acute medical ward in a London hospital in 2002/2003 reports that there is no sign that the number of empirical studies in this field is increasing and a number of barriers will need to be overcome if high-quality end-of-life care for people with dementia is to permeate clinical ...
In a replication of an earlier published study, case notes of 75 elderly in-patients with bipolar affective disorder were examined. Few of the patients had experienced a manic episode before the age of 40. Mean age of onset of affective disorder was 46 years, and first manic episode at 60 years.
A retrospective naturalistic case note study to determine the frequency, co-morbidity and treatment-response of body dysmorphic disorder (BDD). Methods. Records from 280 patients attending a highly specialised obsessive-compulsive disorder (OCD)/BDD service were analysed. The clinical outcome was measured either through scoring of the Yale ...
This study aimed to determine the prevalence of childhood trauma in patients in the UK Early Intervention Service based on a case note review. Methods: This is a retrospective case note study of 296 patients in an UK Early Intervention Service. Trauma history obtained on service entry was reviewed and trauma experienced categorized.
In each of the sites in this study case notes of deceased patients were analysed to gain an insight into how care in different settings was documented and described in the very last hours or days of life. The case notes provide a written record of demographic information about each patient as well as information about decisions made, conversations held and care delivered in the last hours or ...
Case notes of 33 patients between 4 and 14 years of age, seen in two clinics over a 4-year-period were studied, finding that children suffered from anxiety, obsessive compulsive symptoms, both food and non-food related and often had social and school difficulties. The literature on children who present with selective eating is limited to single case studies. This study aims to provide a ...
2007. TLDR. This study examined the sleep of patients with OCD prospectively to establish the frequency of DSPS in this population and any associated clinical or demographic factors which might be implicated in its aetiology. Expand. 58. Semantic Scholar extracted view of "P.3.020 A retrospective case note study of sleep inobsessive compulsive ...
Objectives: A retrospective naturalistic case note study to determine the frequency, co-morbidity and treatment-response of body dysmorphic disorder (BDD). Methods: Records from 280 patients ...
Most were diagnosed as suffering from a psychiatric disorder at the time of assessment, 11 (31.4%) were admitted for further assessment. There were a further 28 admissions to PICU beds. Older adults form a small but important minority of referrals to forensic and PICU services. A single case register would aid further study in this area.
Study Design. This study is a retrospective analysis of case data collected within a series of single case experimental studies (e.g., Woodford et al., 2022; 2024a), similar to that conducted by McLay et al. . Case data was gathered in the context of non-concurrent, multiple-baseline across participants experimental designs wherein all ...
EP: 3. Retrospective Data Highlight Impact of Dose Escalation of Regorafenib in mCRC. During a Case-Based Roundtable® event, Madappa Kundranda, MD, PhD, discussed recent retrospective studies that looked at outcomes of dose optimization of regorafenib for patients with relapsed/refractory advanced colorectal cancer in the first article of a 2 ...
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Retrospective case note analysis form (final version) - The care of dying people in nursing homes and intensive care units: a qualitative mixed-methods study Your browsing activity is empty. Activity recording is turned off.
Background Natural orifice transluminal endoscopic surgery (NOTES) is an achievement in the field of minimally invasive surgery. However, the vantage point of vaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologicalprocedures remains unclear. The main purpose of this study was to compare vNOTES with laparo-endoscopic single-site surgery, and to determine which ...
Design: Retrospective cohort study. Setting: Unscheduled admissions to acute care trust/secondary care UK hospitals. Participants: Six hundred and fifty-six older adults aged ≥65 years admitted on 14 September 2018. Measurements: Delirium was ascertained retrospectively from case notes using medical notes. Documented delirium was classified ...
Sporadic human infections with highly pathogenic avian influenza (HPAI) A(H5N1) virus, with a wide spectrum of clinical severity and a cumulative case fatality of more than 50%, have been reported ...
Second malignant neoplasms within 5 years from first primary diagnosis in pediatric oncology patients in Canada: a population-based retrospective cohort study By Ricci C, Subburaj D, Lim K, Shukla N, Kaur J, Xie L, Laverty M, Zakaria D, Pole J, Pelland-Marcotte M-C, Barber R, Israels SJ, Tran T-H, Oberoi S, Renzi S, MacDonald T, Sung L and ...
Please note: AP coordinators should order alternate (late-testing) exams for students who would like to take exams that are scheduled for the same time. Schools must begin the morning exam administration between 8 and 9 a.m. local time and the afternoon exam administration between 12 and 1 p.m. local time.