Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Center for Bloodless Medicine and Surgery
Case study: gastroenterology, severe gastrointestinal (gi) bleed secondary to xarelto with a hemoglobin-based oxygen carrier (sanguinate) available as precautionary measure.
A 78-year old man who is one of Jehovah’s Witnesses presented with fatigue and weakness along with a 4-week history of maroon colored stools. He was recently admitted to another hospital for a pulmonary infection, where he was found to be in atrial fibrillation (AF) and diagnosed with a non-ischemic cardiomyopathy. He was placed on Xarelto, one of the newer anticoagulants, as a preventative measure, due to his AF. His past medical history included hypertension, type-2 diabetes mellitus, mild aortic stenosis, hematuria, and arterio-venous malformations in the gastrointestinal tract.
His hemoglobin upon admission was 4.1 g/dL, which decreased to 3.1 on the 3rd day after admission. Xarelto was discontinued upon admission and he was placed on aspirin 325 mg/day. An upper GI endoscopy, was normal. A colonoscopy revealed a transverse colon polyp but no active bleeding. He also had a video capsule endoscopic exam where a small “pill camera” is swallowed and video pictures of the entire GI tract are recorded. This exam was significant for an arterial-venous malformation (AVM) in the proximal small bowel, which was not actively bleeding at that time. An echocardiogram showed a left-ventricular ejection fraction of 40%, which was much improved over a prior exam at an outside hospital showing a 10% ejection fraction.
His treatment plan included the following regimen given daily: folate 1 mg IV, vitamin B12 1,000mcg SQ, iron sucrose 200 mg IV, and erythropoietin 40,000 units IV. Phlebotomy blood loss was minimized using neonatal tubes, which require about 10% of the blood volume compared to the full adult sized tubes.
Given his very low hemoglobin, and his risk factors for coronary artery disease, our team decided to obtain a hemoglobin-based oxygen carrier (Sanguinate), in case he developed congestive heart failure or symptomatic myocardial ischemia. This was procured within 24 hours after the necessary FDA phone calls and paperwork, along with the Johns Hopkins IRB emergency applications. These measures were required given that Sanguinate (and all other hemoglobin based oxygen carriers) are not yet FDA approved, and are only available for “compassionate use”. Since the half-life of these compounds is relatively short, the concept is to use them as a temporary measure while the erythropoietic regimen is given to promote red blood cell production. Although the Sanguinate was obtained, its use was not necessary since the patient did not exhibit symptoms, despite severe anemia, and responded well to the erythropoietic therapy.
The hemoglobin level upon discharge on day #7 was 5.1 g/dL. He was not symptomatic from this anemia (his heart rate was 50 bpm). He was sent home on all his prior medications except for Xarelto. Aspirin 325 mg/day, and iron sulfate 325 mg/day were recommended upon discharge. He visited the infusion clinic three times in three weeks, where iron dextran 1 gram IV, and erythropoietin 40,000 units IV, were given during each visit. His last hemoglobin was 11.1 g/dL after these three treatments. He is being followed up by Cardiology, Gastroenterology and Hematology.
- Dermatology
- Gastroenterology
- Geriatric Medicine and Gerontology
- Gynecology and Obstetrics
- Heart and Vascular
- Neurology and Neurosurgery
- Ophthalmology
- Orthopaedics
- Otolaryngology–Head and Neck Surgery
- Physical Medicine and Rehabilitation
- Plastic and Reconstructive Surgery
- Psychiatry and Behavioral Sciences
- Pediatric Specialties
- Pediatric Diabetes and Endocrinology
- Pediatrics Florida
- Pediatric Gastroenterology and GI Surgery
- Pediatric Heart
- Pediatrics Maryland/DC
- Pediatric Neurology & Neurosurgery
- Pediatric Orthopaedics
- Physician Affiliations
- Health Care Technology
- High-Value Health Care
- Clinical Research Advancements
- Precision Medicine Excellence
- Patient Safety
Bariatric Surgery Case Study – Gastric Bypass with ICG Leak Test

Johns Hopkins Center for Bariatric Surgery, National Capital Region
Patient presentation
- A 38-year-old female with a history of class 3 obesity (BMI 45.9), gastroesophageal reflux disease (GERD), hypertension and sleep apnea presented with multiple failed attempts at medical weight-loss. She was initially interested in a minimally invasive sleeve gastrectomy, but a gastric bypass was recommended due to her history of GERD. A sleeve gastrectomy can worsen heartburn postoperatively, but a gastric bypass is a surgical treatment for both morbid obesity as well as GERD. The patient was evaluated by the bariatric multidisciplinary team at Sibley Memorial Hospital and approved for surgery.
Treatments received
- The patient underwent a minimally invasive Roux-en-Y gastric bypass using the latest camera technology. After her procedure, a new technique was used to test the gastro-jejunal anastomosis for any signs of a leak. A novel fluid solution containing indocyanine green dye was instilled into the stomach, and a laparoscopic camera with near-infrared fluorescence visualization was used to transilluminate the anastomosis. It gave real-time feedback and confirmed no leak was present.
Patient outcome after surgery
- The patient was kept overnight and discharged the following day after passing an oral fluid challenge. She was seen two weeks later and was feeling well, tolerating a soft diet and already beginning to see weight loss results.
Johns Hopkins Center for Bariatric Surgery at Sibley Memorial Hospital in Washington, D.C., is accredited from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) as a Comprehensive Center with Adult Qualifications. The team performs open and minimally invasive surgery using state-of-the art equipment. In addition to surgery, the multidisciplinary team provides nutrition counseling, exercise training and close follow-up after surgery.

- About Johns Hopkins Medicine
- Contact Johns Hopkins Medicine
- Centers & Departments
- Maps & Directions
- Find a Doctor
- Patient Care
- Terms & Conditions of Use
- Privacy Statement
Connect with Johns Hopkins Medicine
Join Our Social Media Communities >
Clinical Connection
- Otolaryngology—Head and Neck Surgery
- Contact Johns Hopkins
© The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System. All rights reserved.
Privacy Policy and Disclaimer
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Presentation
The condition, lessons for the clinician, poster presentations:, section editor’s note, suggested readings, case 5: a 13-year-old boy with abdominal pain and diarrhea.
AUTHOR DISCLOSURE
Drs Sudhanthar, Okeafor, and Garg have disclosed no financial relationships relevant to this article. This commentary does not contain a discussion of an unapproved/investigative use of a commercial product/device.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Anjali Garg , Sathyan Sudhanthar , Chioma Okeafor; Case 5: A 13-year-old Boy with Abdominal Pain and Diarrhea. Pediatr Rev December 2017; 38 (12): 572. https://doi.org/10.1542/pir.2016-0223
Download citation file:
- Ris (Zotero)
- Reference Manager
A 13-year-old boy presents to his primary care provider with a 5-day history of abdominal pain and a 2-day history of diarrhea and vomiting. He describes the quality of the abdominal pain as sharp, originating in the epigastric region and radiating to his back, and exacerbated by movement. Additionally, he has had several episodes of nonbloody, nonbilious vomiting and watery diarrhea. His mother discloses that several family members at the time also have episodes of vomiting and diarrhea.
He admits to decreased oral intake throughout the duration of his symptoms. He denies any episodes of fever, weight loss, fatigue, night sweats, or chills. He also denies any hematochezia or hematemesis. His medical history is significant for a ventricular septal defect that was repaired at a young age, but otherwise no other remarkable history.
During the physical examination, the adolescent is afebrile and assessed to be well hydrated. Examination of the abdomen reveals tenderness in the epigastric region and the right lower quadrant on light to deep palpation, with radiation to his back on palpation. There are no visible marks or lesions on his abdomen. Physical examination is negative for rebound tenderness, rovsing sign, or psoas sign. The remainder of the examination findings are negative.
Complete blood cell count, liver enzyme levels, pancreatic enzyme levels, and urinalysis results are all within normal limits.
Our patient was asked to observe his hydration status and pain at home and to report any changes. However, he arrived at the emergency department the next day due to increased severity of abdominal pain. The pain had localized into the right lower quadrant. Further imaging revealed the diagnosis.
The differential diagnosis for an adolescent who presents with abdominal pain is broad, including gastrointestinal causes such as gastroenteritis, appendicitis, or constipation and renal causes such as nephrolithiasis or urinary tract infections. With our patient, the more plausible answers were ruled out through laboratory studies and physical examination, and he was assumed to have gastroenteritis based on the history of similar symptoms in his family members. However, with the worsening of his abdominal pain, further diagnostic study became imperative and a computed tomographic (CT) scan of the abdomen was obtained to assess for appendicitis or nephrolithiasis.
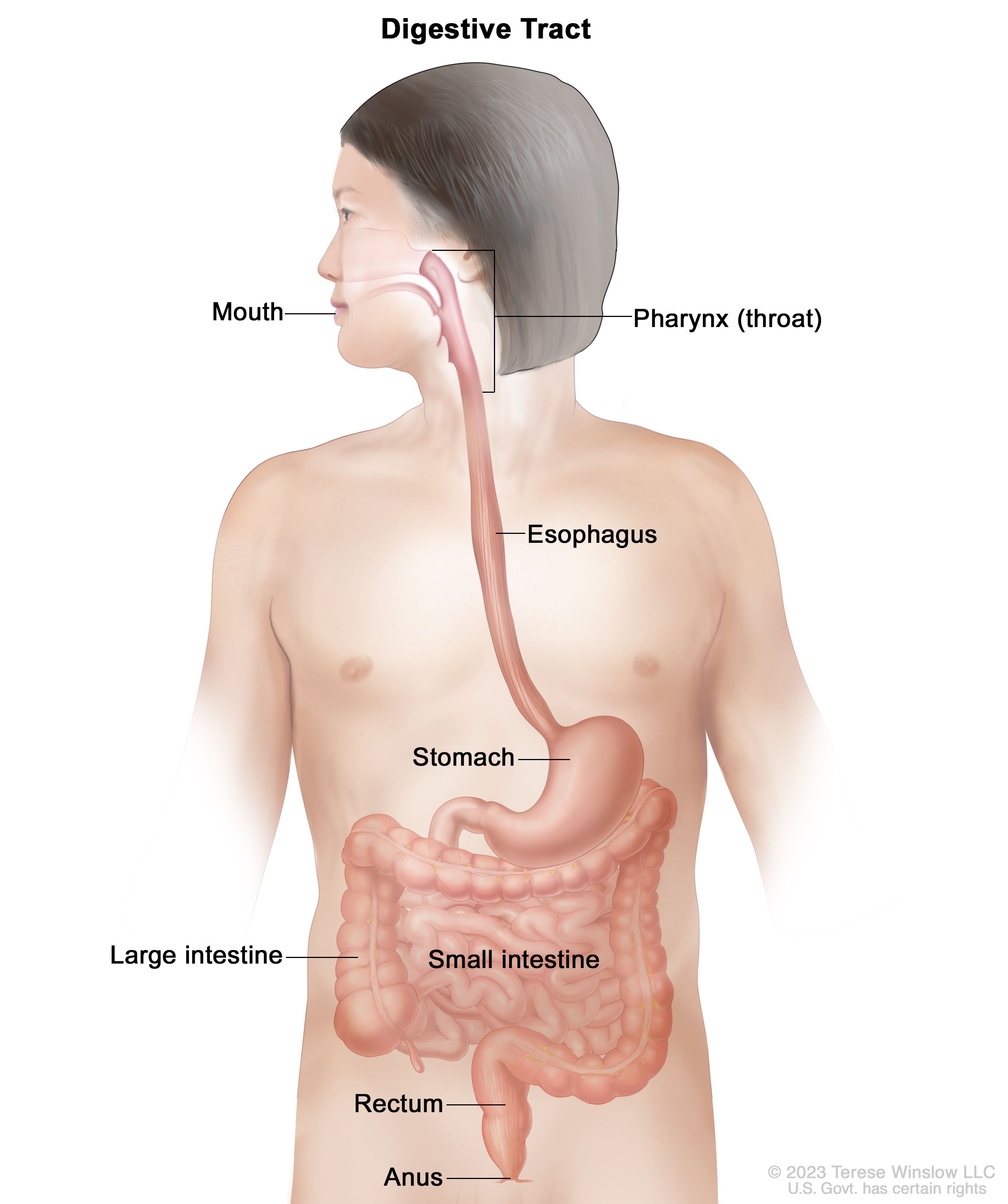
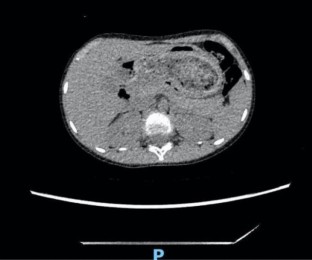
The CT scan showed a cecum located midline; the large intestine was on the left side of the abdomen, and the small intestine was on the right ( Figs 1 and 2 ). The appendix was buried deep in the right pelvis, and there was no indication of appendicitis. These findings were consistent with intestinal malrotation. Intestinal malrotation is rare beyond the first year of life. Maintaining a higher index of suspicion in any patient with an acute presentation of severe abdominal pain is imperative because of the severity of potential complications such as bowel obstruction, volvulus, and eventual necrosis. Our patient’s pain is assumed to have been due to compressive effects of the peritoneal bands (Ladd bands), which were irritated by an initial gastroenteritis. He did not have the signs or symptoms of a more severe complication, such as bowel obstruction or volvulus.

Computed tomographic scan of the abdomen showing intestinal malrotation, specifically of the subtype nonrotation. The small bowel is present in the right hemi-abdomen and the large bowel in the left hemi-abdomen. The cecum is midline in the pelvis. Haustra are still present, excluding any sign of obstruction.

Swirling appearance of the mesentery is known as the whirl sign, which is also indicative of malrotation. This computed tomographic scan shows the superior mesenteric vein wrapped around the superior mesenteric artery.
Owing to the severity of the pain, our patient was taken for surgery, specifically, a Ladd procedure and a prophylactic appendectomy. Ladd bands were seen to extend from the cecum to above the duodenum. During the procedure, these bands were lysed, then the mesentery was spread out, and the bowels were rearranged. He tolerated the surgery well and was discharged 3 days after the operation.
His abdominal pain improved after surgery, and he has been doing well at his postoperative checks.
Intestinal malrotation is when the intestines fail to rotate properly in utero. From the fifth to 10th weeks of embryologic development, the small intestine lies in the right aspect of the abdomen, with the ileocecal junction midline, and the large intestine in the left hemi-abdomen. The segments are then pushed out of the abdomen into the umbilical cord. Both segments grow in the first stage of rotation. During the second stage of rotation, the small intestine rotates counterclockwise 270 degrees around the superior mesenteric artery. The remaining intestine is pulled into the abdomen, and the mesentery is fixed to the retroperitoneal space. The large intestine comes in last, with the final segment of the cecum lying anterior to the small intestine in the right lower quadrant.
Nonrotation is the most frequent cause of intestinal malrotation. Nonrotation occurs when the 270-degree rotation does not occur and, thus, the mesentery is not fixed to the retroperitoneal space. Derangements of the second stage of rotation are defined as having the small intestine in the right hemi-abdomen, with the cecum midline in the pelvis, and the large intestine in the left hemi-abdomen.
One percent of the population has intestinal rotation disorders. The incidence decreases with age. Approximately 90% of patients are diagnosed within the first year of their life, with 80% among them within the first month after birth. Due to a delay in diagnosis, the 10% of patients who present beyond that first year after birth can have severe complications.
Symptoms of malrotation are different in infants compared with adolescents. Neonates typically will have bilious emesis. In contrast, children and adults commonly exhibit acute abdominal pain. Some older patients have had chronic abdominal pain that goes unnoticed; others may be asymptomatic before diagnosis. The co-occurrence of intestinal malrotation with congenital cardiac anomalies is a common finding. Twenty-seven percent of intestinal malrotation patients were found to have a concurrent cardiovascular defect such as ventricular septal defect or another minor/major abnormality.
The diagnostic modality of choice is an upper gastrointestinal tract contrast study. This study modality shows any obstruction and depicts the malrotation through contrast media. Sometimes a contrast medium is not needed for diagnosis, as in the case of our patient, where CT scanning was enough to diagnose the malrotation.
Asymptomatic neonates and all symptomatic individuals, regardless of age, go through the Ladd procedure to correct the abnormality. However, the guidelines are not as clear for treatment of children older than 1 year who are asymptomatic. Currently, there is some consensus for performance of the procedure regardless of symptom status because of the severity of the complications or mortality that can occur due to malrotation. The narrow pedicle of the mesentery that forms in malrotation is prone to volvulus and ischemia, leading to complications at any point in an individual’s life. A diagnostic laparoscopy should be performed at the very least and can be therapeutic as well. Removal of the appendix has been suggested to prevent any diagnostic complications on future presentation. Additionally, the Ladd procedure can lyse Ladd bands, which are abnormal fibrous adhesions from the cecum that also arch over the duodenum. Removal of these bands is imperative because they can cause intestinal obstruction and ischemia as well.
Diagnosis of intestinal malrotation should be considered in a patient presenting acutely with severe abdominal pain, especially in a patient with known cardiac anomalies.
Often the symptoms of intestinal malrotation can be vague, and a patient can be asymptomatic for years before presentation.
The diagnostic modality of choice is an upper gastrointestinal tract series, but other imaging, such as computed tomographic scan, can help diagnose the presence of malrotation in emergency situations.
A Ladd procedure should be conducted on a patient even if he/she does not have current symptoms of obstruction due to increased risk of obstruction or complications such as volvulus and gut necrosis with this disease.
This case is based on a presentation by Ms Anjali Garg and Drs Sathyan Sudhanthar and Chioma Okeafor at the 39th Annual Michigan Family Medicine Research Day Conference in Howell, MI, May 26, 2016.
Poster Session: Student and Resident Case Report Poster Presentation
Poster Number: 23
This case is based on a presentation by Ms Anjali Garg and Drs Sathyan Sudhanthar and Chioma Okeafor at the 2016 AAP National Conference and Exhibition in San Francisco, CA, October 22-25, 2016.
Poster Session: Section on Pediatric Trainees Clinical Case Competition
Abdominal Pain in Children: https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Abdominal-Pain-in-Children.aspx
Diarrhea: https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/Diarrhea.aspx
For a comprehensive library of AAP parent handouts, please go to the Pediatric Patient Education site at http://patiented.aap.org .
This case was selected for publication from the finalists in the 2016 Clinical Case Presentation program for the Section on Pediatric Trainees of the American Academy of Pediatrics (AAP). Ms Anjali Garg, BS, was a medical student from Michigan State University College of Human Medicine, East Lansing, MI, when she wrote this case report, and she now is a medical resident at Rainbow Babies and Children's Hospital in Cleveland, OH. Choosing which case to publish involved consideration of not only the teaching value and excellence of writing but also the content needs of the journal. Other cases have been chosen from the finalists presented at the 2017 AAP National Conference and Exhibition and will be published in 2018.
Competing Interests
Advertising Disclaimer »
Citing articles via
Email alerts.
Affiliations
- Editorial Board
- ABP Content Spec Map
- Pediatrics On Call
- Online ISSN 1526-3347
- Print ISSN 0191-9601
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Gastrointestinal Case Studies
Gastrointestinal (GI) disorders refer to conditions affecting the digestive system, including the esophagus, stomach, small and large intestines, liver, pancreas, and gallbladder.
Source: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/gastrointestinal-tract
Common GI disorders
- Gastroesophageal reflux disease (GERD)
- Peptic ulcer disease
- Inflammatory bowel disease (IBD)
- Irritable bowel syndrome (IBS)
- Celiac disease
- Colorectal cancer
- Gallbladder disease
- Pancreatitis
- Gastrointestinal infections (e.g., gastroenteritis)
Symptoms and signs
Symptoms and signs of GI disorders vary depending on the specific condition. Common symptoms may include abdominal pain, bloating, nausea, vomiting, diarrhea, constipation, difficulty swallowing, heartburn, and rectal bleeding.
Diagnostic Investigation
Diagnostic tests for GI disorders may include imaging studies such as endoscopy, colonoscopy, CT scan, MRI, and ultrasound, as well as blood tests, stool tests, and breath tests.
Options for GI disorders may include lifestyle modifications such as dietary changes and exercise, medications, and surgery. Examples of treatment modalities for specific conditions include:
- GERD: proton pump inhibitors (PPIs), H2 receptor blockers, antacids
- Peptic ulcer disease: antibiotics to eradicate H. pylori bacteria, PPIs, H2 receptor blockers, antacids
- IBD: immunomodulators, biologics, corticosteroids, aminosalicylates
- IBS: dietary changes, probiotics, antispasmodics, fiber supplements
- Celiac disease: gluten-free diet
- Colorectal cancer: surgery, radiation therapy, chemotherapy
- Gallbladder disease: surgery to remove the gallbladder (cholecystectomy)
- Pancreatitis: supportive care, pain management, enzyme supplements
- Hepatitis: antiviral medications, liver transplant
- Gastrointestinal infections: antibiotics, anti-diarrheal medications, fluid replacement therapy
Treatment plans are individualized based on the patient’s specific condition and medical history, and may involve a combination of different therapies.
HEALTH & MEDICAL CASE STUDIES (V1.01) Copyright © by Dr. Tranum Kaur is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License , except where otherwise noted.
Share This Book
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Gastroenterology
- Immune checkpoint inhibitor associated diarrhoea Amin Al-Hussainy , Joss Adams , Jon Simmons , James Kennedy BMJ Case Reports CP May 2024, 17 (5) e259057; DOI: 10.1136/bcr-2023-259057
- Extensive retroperitoneal lymphangiectasia presenting as inguinal swelling Deepthi Arun Kumar , Senthil Kumar Aiyappan , Kshitija Narayan Vinchurkar , Revathi Rajagopal BMJ Case Reports CP May 2024, 17 (5) e260193; DOI: 10.1136/bcr-2024-260193
- Chronic diarrhoea, weight loss and a positive anti-tissue transglutaminase antibody: A case report of olmesartan-induced enteropathy Rachel Sheppard , Benjamin Evanson , Iona Campbell , Alan Shand BMJ Case Reports CP May 2024, 17 (5) e255407; DOI: 10.1136/bcr-2023-255407
- Cannabinoid hyperemesis syndrome Ali Elnagar , Mpho Kgomo , Modise Mokone , Badreldin Yousif BMJ Case Reports CP Apr 2024, 17 (4) e256921; DOI: 10.1136/bcr-2023-256921
- Colonoscopy-assisted laparoscopic wedge resection for a large symptomatic colonic lipoma Julia Hanevelt , Wouter Hugo de Vos Tot Nederveen Cappel , Fiebo Johannes Cornelis ten Kate , Henderik Leendert van Westreenen BMJ Case Reports CP Apr 2024, 17 (4) e258947; DOI: 10.1136/bcr-2023-258947
- Iatrogenic immunodeficiency-associated lymphoproliferative disorder presenting as small bowel perforation Rathnayaka Mudiyanselage Kalpanee Dhanushika Gunasingha , Kayleigh Herrick-Reynolds , Jeffrey A Sanford , Jason Radowsky BMJ Case Reports CP Mar 2024, 17 (3) e257148; DOI: 10.1136/bcr-2023-257148
- Simultaneous Presentation of Takayasu Arteritis and Crohn’s Disease in a Middle-Aged Patient: Are they two sides of the same coin? Swathi Suyamburajan , Rama Bhat , Raghavendra Rao , Srilatha Srilatha Parampalli BMJ Case Reports CP Mar 2024, 17 (3) e259110; DOI: 10.1136/bcr-2023-259110
- Blue rubber bleb nevus syndrome in a patient on anticoagulation: a management dilemma Aditya Mithanthaya , Ali Galalah Mostafa Ismail , Niroshan Muwanwella , Kannan Venugopal BMJ Case Reports CP Nov 2023, 16 (11) e256702; DOI: 10.1136/bcr-2023-256702
- Atypical hypertrophy of retinal pigment epithelium manifesting as the first sign of familial adenomatous polyposis João Ponces Ramalhão , Miguel Afonso , Mafalda Macedo , Maria Araújo BMJ Case Reports CP Nov 2023, 16 (11) e254350; DOI: 10.1136/bcr-2022-254350
- Primary anorectal amelanotic melanoma with liver, lungs and lymph nodal metastases James R Marak , Gaurav Raj , Shivam Dwivedi , Ariba Zaidi BMJ Case Reports CP Nov 2023, 16 (11) e257510; DOI: 10.1136/bcr-2023-257510
- Anaesthesia (209)
- Cardiovascular medicine (985)
- Complementary medicine (6)
- Dentistry and oral medicine (211)
- Dermatology (538)
- Clinical diagnostic tests (50)
- Radiology (diagnostics) (146)
- Surgical diagnostic tests (23)
- Diagnostics
- Drugs and medicines (1781)
- Ear, nose and throat/otolaryngology (452)
- Disaster response
- Poisoning (49)
- Resuscitation (57)
- Trauma (160)
- Emergency medicine (474)
- Adrenal disorders (118)
- Calcium and bone (97)
- Diabetes (127)
- Drugs: endocrine system (25)
- Lipid disorders (26)
- Metabolic disorders (89)
- Pituitary disorders (57)
- Thyroid disease (118)
- Endocrinology (652)
- Changing physician behavior
- Effectiveness of care
- Gastroenterology (913)
- Drugs: gastrointestinal system (44)
- Endoscopy (165)
- GI bleeding (99)
- Infection (gastroenterology) (107)
- Inflammatory bowel disease (72)
- Liver disease (186)
- Neurogastroenterology
- Oesophagus (55)
- Pancreas and biliary tract (100)
- Pancreatitis (61)
- Portal hypertension (16)
- Small intestine (76)
- Stomach and duodenum (85)
- General practice / family medicine (242)
- Clinical genetics
- Cytogenetics
- Genetic screening / counselling (92)
- Molecular genetics
- Genetics (291)
- Elder abuse
- End of life decisions (geriatric medicine) (2)
- Long term care (18)
- Psychogeriatrics
- Geriatric medicine (65)
- Haematology (incl blood transfusion) (531)
- HIV/AIDS (80)
- Immunology (including allergy) (56)
- Infectious diseases (1322)
- Adult intensive care (301)
- Mechanical ventilation (19)
- Neonatal intensive care (90)
- Paediatric intensive care (69)
- Intensive care (560)
- Brain stem / cerebellum (85)
- Cerebral palsy (6)
- Clinical neurophysiology (40)
- Coma and raised intracranial pressure (29)
- Cranial nerves (107)
- Dementia (7)
- Drugs: CNS (not psychiatric) (33)
- Epilepsy and seizures (116)
- Headache (including migraine) (9)
- Hydrocephalus (22)
- Infection (neurology) (166)
- Motor neurone disease (14)
- Movement disorders (other than Parkinsons) (63)
- Multiple sclerosis (19)
- Muscle disease (40)
- Neuroimaging (396)
- Neurological injury (71)
- Neuromuscular disease (77)
- Neurooncology (116)
- Neuroophthalmology (8)
- Pain (neurology) (47)
- Parkinson's disease (7)
- Peripheral nerve disease (84)
- Sleep disorders (neurology) (8)
- Spinal cord (105)
- Stroke (239)
- Trauma CNS / PNS (40)
- Variant Creutzfeld-Jakob Disease (2)
- Neurology (1609)
- Nursing (36)
- Childhood nutrition (5)
- Malnutrition (24)
- Obesity (nutrition) (17)
- Vitamins and supplements (46)
- Nutrition and metabolism (118)
- Obstetrics and gynaecology (589)
- Oncology (1477)
- Ophthalmology (763)
- Orthopaedics (371)
- Adolescent health
- Bilirubin disorders (9)
- Child abuse (6)
- Child and adolescent psychiatry (paedatrics) (9)
- Child health
- Childhood nutrition (paediatrics) (7)
- Congenital disorders (280)
- Developmental paediatrics (4)
- Failure to thrive (19)
- Infant health (32)
- Infant nutrition (including breastfeeding) (5)
- Materno-fetal medicine (72)
- Neonatal and paediatric intensive care (96)
- Neonatal health (93)
- Paediatrics (878)
- End of life decisions (palliative care) (14)
- Pain (palliative care) (8)
- Palliative care (37)
- Chemical pathology
- Cytopathology
- Histopathology
- Inflammation
- Microbiology
- Molecular biology
- Morbid anatomy / surgical pathology
- Neuropathology
- Pathology (572)
- Drug misuse (including addiction) (33)
- Medicines regulation
- Toxicology (56)
- Unwanted effects / adverse reactions (311)
- Pharmacology and therapeutics (477)
- Prison medicine (1)
- Adjustment disorders
- Alcohol-related disorders (4)
- Anxiety disorders (including OCD and PTSD) (18)
- Child and adolescent psychiatry (11)
- Delirium (17)
- Drugs misuse (including addiction) (27)
- Drugs: psychiatry (29)
- Eating disorders (7)
- Impulse control disorders (6)
- Memory disorders (psychiatry) (22)
- Mood disorders (including depression) (33)
- Personality disorders (2)
- Psychiatry of old age (8)
- Psychotherapy (14)
- Psychotic disorders (incl schizophrenia) (37)
- Sexual and gender disorders (2)
- Sleep disorders (2)
- Somatoform disorders (6)
- Suicide (psychiatry) (7)
- Psychiatry (221)
- Radiology (871)
- Continuing medical education
- Disability (17)
- Other rehabilitative therapies
- Physiotherapy (41)
- Rehabilitation medicine (84)
- Acute renal failure (107)
- Chronic renal failure (49)
- Dialysis (61)
- Fluid electrolyte and acid-base disturbances (78)
- Nephrotic syndrome (29)
- Proteinurea (29)
- Renal transplantation (48)
- Renal medicine (369)
- Respiratory medicine (615)
- Ankylosing spondylitis (2)
- Biological agents (37)
- Connective tissue disease (97)
- Degenerative joint disease (9)
- Drugs: musculoskeletal and joint diseases (26)
- Fibromyalgia (2)
- Musculoskeletal syndromes (71)
- Osteoarthritis (13)
- Osteoporosis (11)
- Rheumatoid arthritis (40)
- Sjogren's syndrome (3)
- Systemic lupus erythematosus (60)
- Vascularitis (161)
- Rheumatology (569)
- Sexual health (102)
- Sports and exercise medicine (123)
- Breast surgery (69)
- Cardiothoracic surgery (205)
- Gastrointestinal surgery (432)
- General surgery (457)
- Neurosurgery (204)
- Oral and maxillofacial surgery (142)
- Orthopaedic and trauma surgery (235)
- Otolaryngology / ENT (246)
- Plastic and reconstructive surgery (177)
- Surgical oncology (230)
- Transplantation (61)
- Urological surgery (183)
- Vascular surgery (192)
- Surgery (2573)
- Urology (273)
- Communication
- Clinical trials (epidemiology)
- Epidemiologic studies
- Population trends
- Screening (epidemiology)
- Survey techniques
- Therapeutic trials
- Time-to-event methods
- Artificial and donated transplantation
- Assisted dying
- Clinical ethics
- Codes of professional ethics
- Competing interests (ethics)
- Confidentiality
- Drug issues
- End of life decisions (ethics)
- Ethics of abortion
- Ethics of reproduction
- Experiments in vivo
- Informed consent
- Research and publication ethics
- Sexuality / gender
- Ethics (16)
- Ethnic studies (2)
- Health economics (7)
- Information management
- Telemedicine
- Health policy
- Health service research
- Journalology
- Legal and forensic medicine
- Choosing / changing career
- Combining life and work
- Continuous professional development
- Flexible training
- Getting and changing jobs
- Getting and changing jobs (including job descriptions and contracts)
- Leaving medicine
- Medical careers
- Organise and prepare your CV
- Organise working abroad
- Pay, working conditions, and health
- Personal development
- Portfolio development
- Prepare for appraisal
- Prepare for interview
- Professional conduct and regulation
- Professional regulation and standards
- History taking and the physical examination
- Postgraduate
- Undergraduate
- Medical education (108)
- Doctors' morale and well being
- Medical error/ patient safety
- Quality improvement
- Medical management (208)
- Occupational and environmental medicine (141)
- Abuse (child, partner, elder)
- Air pollution
- Drug misuse
- Environmental issues
- Health education
- Health of indigenous peoples
- Health promotion
- Housing and health
- Human rights
- Obesity (public health) (5)
- Screening (public health)
- Sexual health (public health)
- Social conditions and disease
- Suicide (public health)
- Urban health
- Vaccination programs
- Violence (other)
- Violence against women
- Public health (68)
- Smoking and tobacco (16)
- Sociology (1)
- Comparative effectiveness research
- Qualitative research
- Quantitative research
- Statistics and research methods (1)
- 10-Minute Consultation
- Assessment of older adults
- BMJ clinical evidence summaries
- Care of older people
- Change page
- Clinical evidence
- Clinical governance in primary care
- Clinical guidelines (the theory)
- Clinical Update
- Competent novice
- Complexity science
- Conflict and health
- Coping with loss
- Data campaign
- Diagnosis in general practice
- Digital theme issue: Overdiagnosis
- Drug points
- E-cigarettes
- Easily missed
- Economics notes
- Ethical debates
- Evidence base of clinical diagnosis
- Evidence based case report
- Evidence based management of hypertension
- Evidence based paediatrics
- Extracts from BestTreatments
- For and against (controversies in management)
- Getting research findings into practice
- Guideline summaries
- Health needs assessment
- How does it work?
- If I ruled the NHS
- Improving the quality of health care
- Interactive case reports
- Investigation
- Lesson of the week
- Making a difference
- Managing demand
- Maternal, child, and adolescent health
- Measuring quality of life
- Methods in health services research
- Mid Staffordshire Inquiry
- Modernising the NHS
- Multimorbidity
- Narrative based medicine
- Non-communicable diseases
- Patient authored
- Patient journeys
- Pharmacology
- Practice pointer
- Pregnancy plus
- Primary care groups
- Qualitative research in health care
- Quality improvement report
- Rapid Recommendation
- Rational imaging
- Rational testing
- Regulating nursing homes
- Research pointers
- Safety alerts
- Science, medicine, and the future
- Scrap the Cap
- Seven day NHS
- Shared decision making
- Spotlight on climate change
- State of the Art
- Statistics notes
- Systematic reviews in health care
- Teaching rounds
- The BMJ Awards 2015
- The World Bank and world health
- Theories in health care and research
- Therapeutics
- Too much medicine
- UK general election 2015
- Uncertainties page
- Understanding controlled trials
- What the educators are saying
- What your patient is thinking
- What's new this month in BMJ Journals
- When I use a word
- Access to health care (9)
- Adverse drug reactions and complications (328)
- Corrections
- Determinants of health (2)
- Findings that shed new light on the possible pathogenesis of a disease or an adverse effect (256)
- Global health (71)
- Health in vulnerable communities (12)
- Images in... (2251)
- Learning from errors (76)
- Learning from unexpected outcome (positive or negative) (146)
- Medical student electives
- Medicine in the humanitarian sector
- Myth exploded
- New disease (44)
- Novel diagnostic procedure (55)
- Novel treatment (new drug/intervention; established drug/procedure in new situation) (393)
- Other full case
- Rare disease (2616)
- Reminder of important clinical lesson (714)
- Rural medicine
- Unexpected outcome (positive or negative) including adverse drug reactions (219)
- Unusual association of diseases/symptoms (708)
- Unusual presentation of more common disease/injury (792)
- Video reports
- COVID-19 (548)
- Editor's choice (66)
- Anaesthetics and ITU
- Anatomy quiz
- Case report
- Case Review
- Case scenario
- Drugs and therapeutics
- Emergency medicine
- Endocrinology
- General practice
- Haematology
- Histopathology/cytology/pathology/autopsy
- Infectious diseases
- Law and ethics
- Learning disabled
- Obstetrics and gynaecology
- onExamination questions
- Ophthalmology
- Orthopaedics and trauma
- Paediatrics
- Picture quiz
- Renal medicine
- Respiratory
- Rheumatology
- Spot Diagnosis
- GUT Recent advances in clinical practice
- GUT Snapshot
- IP Cochrane corners
- JCP Education
- JECH Gallery
- JMG Online mutation reports
- Open access (794)
- Animal Models
- Biomarker Studies
- Childhood Lupus
- Clinical Trials and Drug Discovery
- Co-morbidities
- Cutaneous Lupus
- Epidemiology and Outcomes
- Immunology and Inflammation
- Lupus Nephritis
- Reproductive Health and APS
- Quality Improvement Reports
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 13 July 2020
Gastrointestinal surgery and the gut microbiome: a systematic literature review
- Suzie Ferrie 1 , 2 ,
- Amy Webster 1 ,
- Betty Wu 3 ,
- Charis Tan 2 &
- Sharon Carey ORCID: orcid.org/0000-0003-4155-5240 1 , 2
European Journal of Clinical Nutrition volume 75 , pages 12–25 ( 2021 ) Cite this article
1387 Accesses
12 Citations
3 Altmetric
Metrics details
- Translational research
Background/objectives
The impact of gastrointestinal surgery on the profile of the human gut microbiome is not fully understood. This review aimed to identify whether there is a change to the profile of the gut microbiome as a result of gastrointestinal surgery.
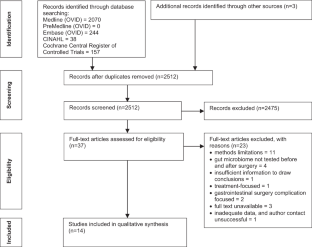
Subjects/methods
In August 2018, a systematic literature search was conducted in Medline, PreMedline, Embase, CINAHL and The Cochrane Register of Clinical Trials, identifying and critically appraising studies which investigated changes to gut microbiome pre- and post-gastrointestinal surgery.
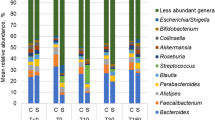
Of 2512 results, 14 studies were included for analysis. All studies reported post-surgical change to the microbiome. In 9 of the 14 studies, prevalence of specific bacteria had significantly changed after surgery. Improved outcome was associated with higher levels of beneficial bacteria and greater microbiome diversity post-surgery.
There were methodological limitations in the included studies leading to uncertainty regarding the impact of gastrointestinal surgery alone on the microbiome profile. An ideal future model for research should encompass case-controlled or cohort design with longer term follow-up in a homogeneous patient group. Future research should seek to clarify the gold standard testing method and standardised timing for post-surgical microbiome sample collection. It is imperative that controls for confounders be put in place to attempt to identify the true association between gastrointestinal surgery and changes to gut microbiome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Intestinal dysbiosis as an intraoperative predictor of septic complications: evidence from human surgical cohorts and preclinical models of peritoneal sepsis
A pilot study demonstrating the impact of surgical bowel preparation on intestinal microbiota composition following colon and rectal surgery

Peri-operative antibiotics acutely and significantly impact intestinal microbiota following bariatric surgery
Whelan K. Modification of the gastrointestinal microbiota and its application to clinical nutrition. J Hum Nutr Diet. 2012;25:297–9.
PubMed Google Scholar
Peat CM, Kleiman SC, Bulik CM, Carroll IM. The intestinal microbiome in bariatric surgery patients. Eur Eat Disord Rev. 2015;23:496–503.
PubMed PubMed Central Google Scholar
Singh RK, Chang H-W, Yan D, Lee KM, Ucmak D, Wong K, et al. Influence of diet on the gut microbiome and implications for human health. J Transl Med. 2017;15:73.
Sidhu M, van der Poorten D. The gut microbiome. Aust Fam Physician 2017;46:206–11.
Bäckhed F, Fraser Claire M, Ringel Y, Sanders ME, Sartor RB, Sherman PM, et al. Defining a healthy human gut microbiome: current concepts, future directions, and clinical applications. Cell Host Microbe 2012;12:611–22.
Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–14.
Google Scholar
Hollister EB, Gao C, Versalovic J. Compositional and functional features of the gastrointestinal microbiome and their effects on human health. Gastroenterology. 2014;146:1449–58.
Zheng S, Shao S, Qiao Z, Chen X, Piao C, Yu Y, et al. Clinical parameters and gut microbiome changes before and after surgery in thoracic aortic dissection in patients with gastrointestinal complications. Sci Rep. 2017;7:15228.
Zhang Y-J, Li S, Gan R-Y, Zhou T, Xu D-P, Li H-B. Impacts of gut bacteria on human health and diseases. Int J Mol Sci. 2015;16:7493–519.
CAS PubMed PubMed Central Google Scholar
McIlroy J, Ianiro G, Mukhopadhya I, Hansen R, Hold GL. Review article: the gut microbiome in inflammatory bowel disease—avenues for microbial management. Aliment Pharmacol Ther. 2018;47:26–42.
CAS PubMed Google Scholar
Wexler HM. Bacteroides: the good, the bad, and the nitty-gritty. Clin Microbiol Rev. 2007;20:593–621.
Duvallet C, Gibbons SM, Gurry T, Irizarry RA, Alm EJ. Meta-analysis of gut microbiome studies identifies disease-specific and shared responses. Nat Commun. 2017;8:1784.
Guyton K, Alverdy JC. The gut microbiota and gastrointestinal surgery. Nat Rev Gastroenterol Hepatol. 2016;14:43–54.
Scotti E, Boué S, Lo Sasso G, Zanetti F, Belcastro V, Poussin C, et al. Exploring the microbiome in health and disease: implications for toxicology. Toxicol Res Appl. 2017;1:1–37.
Galperin MY. Genome diversity of spore-forming firmicutes. Microbiol Spectr. 2013; 1: TBS-0015-2012. https://doi.org/10.1128/microbiolspectrum.TBS-0015-2012 .
Mizuta M, Endo I, Yamamoto S, Inokawa H, Kubo M, Udaka T, et al. Perioperative supplementation with bifidobacteria improves postoperative nutritional recovery, inflammatory response, and fecal microbiota in patients undergoing colorectal surgery: a prospective, randomized clinical trial. Biosci Microbiota Food Health. 2016;35:77–87.
Neut C, Guillemot F, Colombel JF. Nitrate-reducing bacteria in diversion colitis: a clue to inflammation? Dig Dis Sci. 1997;42:2577–80.
Ventura M, Canchaya C, Tauch A, Chandra G, Fitzgerald GF, Chater KF, et al. Genomics of actinobacteria: tracing the evolutionary history of an ancient phylum. Microbiol Mol Biol Rev. 2007;71:495–548.
Barka EA, Vatsa P, Sanchez L, Gaveau-Vaillant N, Jacquard C, Klenk HP, et al. Taxonomy, physiology, and natural products of actinobacteria. Microbiol Mol Biol Rev. 2015;80:1–43.
Stavrou G, Kotzampassi K. Gut microbiome, surgical complications and probiotics. Ann Gastroenterol. 2017;30:45–53.
Chen YPL. Bioinformatics for whole-genome shotgun sequencing of microbial communities. PLoS Comput Biol. 2005;1:e24.
PubMed Central Google Scholar
Morgan XC, Huttenhower C. Meta’omic analytic techniques for studying the intestinal microbiome. Gastroenterology. 2014;146:1437–48.e1.
Valdes AM, Walter J, Segal E, Spector TD. Role of the gut microbiota in nutrition and health. Br J Med. 2018;361(Supp 1):36–44.
Joanna Briggs Institute. Critical appraisal tools. 2018. http://joannabriggs.org/research/critical-appraisal-tools.html . Accessed 2 Oct 2018.
Joanna Briggs Institute. The JBI approach. 2018. http://joannabriggs.org/jbi-approach.html#tabbed-nav=Levels-of-Evidence . Accessed 2 Oct 2018.
Almeida MG, Kiss DR, Zilberstein B, Quintanilha AG, Teixeira MG, Habr-Gama A. Intestinal mucosa-associated microflora in ulcerative colitis patients before and after restorative proctocolectomy with an ileoanal pouch. Dis Colon Rectum. 2008;51:1113–9.
Neut C, Bulois P, Desreumaux P, Membre JM, Lederman E, Gambiez L, et al. Changes in the bacterial flora of the neoterminal ileum after ileocolonic resection for Crohn’s disease. Am J Gastroenterol. 2002;97:939–46.
Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux JJ, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA. 2008;105:16731–6.
Marteau P, Lémann M, Seksik P, Laharie D, Colombel JF, Bouhnik Y, et al. Ineffectiveness of Lactobacillus johnsonii LA1 for prophylaxis of postoperative recurrence in Crohn’s disease: a randomised, double blind, placebo controlled GETAID trial. Gut. 2006;55:842–7.
De Cruz P, Kang S, Wagner J, Buckley M, Sim WH, Prideaux L, et al. Association between specific mucosa-associated microbiota in Crohn’s disease at the time of resection and subsequent disease recurrence: a pilot study. J Gastroenterol Hepatol. 2015;30:268–78.
Dey N, Soergel DA, Repo S, Brenner SE. Association of gut microbiota with postoperative clinical course in Crohn’s disease. BMC Gastroenterol. 2013;13:131.
Laffin M, Perry T, Park H, Gillevet P, Sikaroodi M, Kaplan GG, et al. Endospore-forming bacteria are associated with maintenance of remission following intestinal resection in Crohn’s disease. Gastroenterology. 2017;152:S192–3.
Wright EK, Kamm MA, Wagner J, Teo SM, De Cruz P, Hamilton AL, et al. Microbial factors associated with postoperative Crohn’s disease recurrence. J Crohns Colitis. 2017;11:191–203.
Mondot S, Lepage P, Seksik P, Allez M, Tréton X, Bouhnik Y, et al. The GETAID group. Structural robustness of the gut mucosal microbiota is associated with Crohn’s disease remission after surgery. Gut. 2016;65:954–6.
Feng X, Su Y, Jiang J, Ning L, Weiwei D, Zhiming W, et al. Changes in fecal and colonic mucosal microbiota of patients with refractory constipation after a subtotal colectomy. Am J Surg. 2015;81:198–206.
Ohigashi S, Sudo K, Kobayashi D, Takahashi T, Nomoto K, Onodera H. Significant changes in the intestinal environment after surgery in patients with colorectal cancer. J Gastrointest Surg. 2013;17:1657–64.
Mangell P, Thorlacius H, Syk I, Ahrne S, Molin G, Olsson C, et al. Lactobacillus plantarum 299v does not reduce enteric bacteria or bacterial translocation in patients undergoing colon resection. Dig Dis Sci. 2012;57:1915–24.
Guimaraes Quintanilha AG, Azevedo dos Santos MA, Avila-Campos MJ, Saad WA, Pinotti HW, Zilberstein B. Chagasic megacolon and proximal jejunum microbiota. Scandanivian J Gastroenterol. 2000;35:632–6.
CAS Google Scholar
Mariat D, Firmesse O, Levenez F, Guimaraes VD, Sokol H, Dore J, et al. The Firmicutes/Bacteroidetes ratio of the human microbiota changes with age. BMC Microbiol. 2009;9:123.
Kabeerdoss J, Sankaran V, Pugazhendhi S, Ramakrishna BS. Clostridium leptum group bacteria abundance and diversity in the fecal microbiota of patients with inflammatory bowel disease: a case-control study in India. BMC Gastroenterol. 2013;13:20
Toprak NU, Gulluoglu BM, Cakici O, Akin LM, Demirkalem P, Celenk T, et al. Do antimicrobial susceptibility patterns of colonic isolates of Bacteroides species change after antibiotic prophylaxis with cefoxitine during elective abdominal surgery? World J Surg. 2005;29:1311–5.
Okazaki M, Matsukuma S, Suto R, Miyazaki K, Hidaka M, Matsuo M, et al. Perioperative synbiotic therapy in elderly patients undergoing gastroenterological surgery: a prospective, randomized control trial. Nutrition. 2013;29:1224–30.
Vaughn BP, Moss AC. Prevention of post-operative recurrence of Crohn’s disease. World J Gastroenterol. 2014;20:1147–54.
Vuik FER, Dicksved J, Lam SY, Fuhler GM, van der Laan LJW, van de Winkel A, et al. Composition of the mucosa-associated microbiota along the entire gastrointestinal tract of human individuals. United Eur Gastroenterol J. 2019;7:897–907.
Conlon MA, Bird AR. The impact of diet and lifestyle on gut microbiota and human health. Nutrients. 2014;7:17–44.
Vandeputte D, Tito RY, Vanleeuwen R, Falony G, Raes J. Practical considerations for large-scale gut microbiome studies. FEMS Microbiol Rev. 2017;41(Supp 1):S154–67.
Wu GD, Lewis JD, Hoffmann C, Chen YY, Knight R, Bittinger K, et al. Sampling and pyrosequencing methods for characterizing bacterial communities in the human gut using 16S sequence tags. BMC Microbiol. 2010;10:206.
Bahl MI, Bergström A, Licht TR. Freezing fecal samples prior to DNA extraction affects the Firmicutes to Bacteroidetes ratio determined by downstream quantitative PCR analysis. FEMS Microbiol Lett. 2012;329:193–7.
Cowan ST. SK. Manual for idenfication of medical bacteria 2nd ed. New York: Cambridge University Press; 1974.
Sutter VLCD, Finegold SM. Wadsworth anaerobic bacteriology manual. 3rd ed. St. Louis: Mosby; 1980.
Holdeman LVCE, Moore WE. Anaerobic laboratory manual. 4th ed. Blacksburg: Virginia Polytechnics Institute and State University; 1977.
Kang S, Denman SE, Morrison M, Yu Z, McSweeney C. An efficient RNA extraction method for estimating gut microbial diversity by polymerase chain reaction. Current Microbiology. 2009;58:464–71.
Zoetendal EG, Akkermans AD, De Vos WM. Temperature gradient gel electrophoresis analysis of 16S rRNA from human fecal samples reveals stable and host-specific communities of active bacteria. Appl Environ Microbiol. 1998;64:3854–9.
Quednau M, Ahrne S, Petersson AC, Molin G. Identification of clinically important species of Enterococcus within 1 day with randomly amplified polymorphic DNA (RAPD). Curr Microbiol. 1998;36:332–6.
Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11:589–603.
Wagner J, Short K, Catto-Smith AG, et al. Identification and characterisation of Pseudomonas 16S ribosomal DNA from ileal biopsies of children with Crohn’s disease. PLoS ONE. 2008;3:e3578.
Hudault S, Guignot J, Servin AL. Escherichia coli strains colonising the gastrointestinal tract protect germfree mice against Salmonella typhimurium infection. Gut.2001;49:47–55.
Yoshida N, Emoto T, Yamashita T, Watanabe H, Hayashi T, Tabata T, et al. Bacteroides vulgatus and Bacteroides dorei reduce gut microbial lipopolysaccharide production and inhibit atherosclerosis. Circulation. 2018;138:2486–98.
Hehemann JH, Kelly AG, Pudlo NA, Martens EC, Borastona AB. Bacteria of the human gut microbiome catabolize red seaweed glycans with carbohydrate-active enzyme updates from extrinsic microbes. Proc Natl Acad Sci USA. 2012;109:19786–91.
Slattery C, Cotter PD, O’Toole PW. Analysis of health benefits conferred by Lactobacillus species from kefir. Nutrients. 2019;11:1252–76.
CAS PubMed Central Google Scholar
Cools P, Melin P. Group B Streptococcus and perinatal mortality. Res Microbiol. 2017;168:793–801.
NB Corrêa, LA Filho Péret, Penna FJ, Lima FM, Nicoli JR. A randomized formula controlled trial of Bifidobacterium lactis and Streptococcus thermophilus for prevention of antibiotic-associated diarrhea in infants. J Clin Gastroenterol. 2005;39:385–9.
Eberhard J, Stumpp N, Winkel A, Schrimpf C, Bisdas T, Orzak P, et al. Streptococcus mitis and Gemella haemolysans were simultaneously found in atherosclerotic and oral plaques of elderly without periodontitis-a pilot study. Clin Oral Investig. 2017;21:447–52.
Adam EL, Siciliano RF, Gualandro DM, Calderaro D, Issa VS, Rossi F, et al. Case series of infective endocarditis caused by Granulicatella species. Int J Infect Dis. 2015;31:56–58.
Cuiv PO, Klaassens ES, Durkin AS, Harkins DM, Foster L, McCorrison J, et al. Draft genome sequence of Turicibacter sanguinis PC909 , isolated from human feces. J Bacteriol. 2011;193:1288–9.
Bibbò S, Riccardo Lopetuso L, Ianiro G, Di Rienzo T, Gasbarrini A, et al. Role of microbiota and innate immunity in recurrent Clostridium difficile infection. J Immunol Research. 2014;2014:462740.
Kanauchi O, Matsumoto Y, Matsumura M, Fukuoka M, Bamba T. The beneficial effects of microflora, especially obligate anaerobes, and their products on the colonic environment in inflammatory bowel disease. Curr Pharm Des. 2005;11:1047–53.
de la Cuesta-Zuluaga J, Mueller NT, Corrales-Agudelo V, Velásquez-Mejía EP, Carmona JA, Abad JM, et al. Metformin is associated with higher relative abundance of mucin-degrading Akkermansia muciniphila and several short-chain fatty acid–producing microbiota in the gut. Diabetes Care. 2017;40:54–62.
Workneh M, Wang F, Romagnoli M, Simner PJ, Carroll K. Bypass graft infection and bacteremia caused by Anaerostipes caccae : First report of human infection caused by a recently described gut anaerobe. Anaerobe. 2016;42:98–100.
Schwiertz A, Hold GL, Duncan SH, Gruhl B, Collins MD, Lawson PA, et al. Anaerostipes caccae gen. nov., sp. nov., a new saccharolytic, acetate-utilising, butyrate-producing bacterium from human faeces. Syst Appl Microbiol. 2002;25:46–51.
Ahn J, Sinha R, Pei Z, Dominianni C, Wu J, Shi J, et al. Human gut microbiome and risk for colorectal cancer. J Natl Cancer Inst. 2013;105:1907–11.
Linares DM, Ross P, Stanton C. Beneficial microbes: the pharmacy in the gut. Bioengineered. 2015;7:11–20.
Buchanan M. Sizing up bacteria. Nat Phys. 2014;10:788.
Download references
Author information
Authors and affiliations.
University of Sydney, Sydney, NSW, Australia
Suzie Ferrie, Amy Webster & Sharon Carey
Royal Prince Alfred Hospital, Sydney, NSW, Australia
Suzie Ferrie, Charis Tan & Sharon Carey
St George Hospital, Sydney, NSW, Australia
You can also search for this author in PubMed Google Scholar
Contributions
SC was responsible for conceptualisation of the study. AW, SF and SC were responsible for designing study. SC, SF and AW conducted the search, quality assessments and analysis of results. BW, SF and CT were responsible for reviewing the analysis. SF led the interpretation of results with all authors having involvement. AW and SF drafted the paper and all authors contributed to reviewing the paper.
Corresponding author
Correspondence to Sharon Carey .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Ferrie, S., Webster, A., Wu, B. et al. Gastrointestinal surgery and the gut microbiome: a systematic literature review. Eur J Clin Nutr 75 , 12–25 (2021). https://doi.org/10.1038/s41430-020-0681-9
Download citation
Received : 31 October 2019
Revised : 09 June 2020
Accepted : 01 July 2020
Published : 13 July 2020
Issue Date : January 2021
DOI : https://doi.org/10.1038/s41430-020-0681-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 8, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
Road of recovery in gastrointestinal surgery: From ERAS to FRAS
by KeAi Communications Co., Ltd.
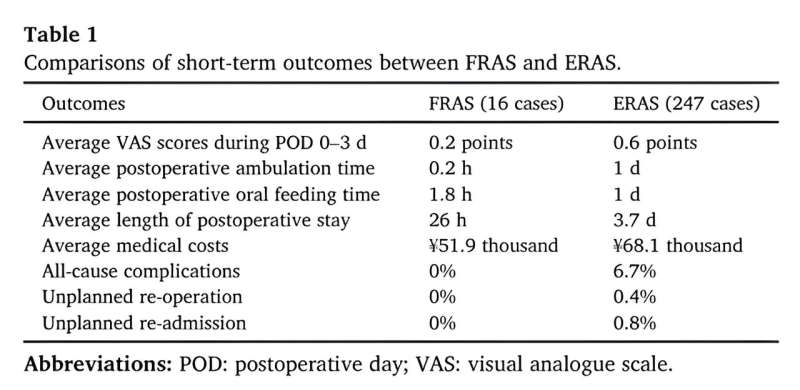
In the 1990s, Dr. Henrik Kehlet introduced the concept of enhanced recovery after surgery (ERAS), pioneering multimodal surgical care. Initially applied to patients undergoing colonic surgery, ERAS has also been dedicated to developing multimodal perioperative care to improve patients' recovery after major surgery through research, education, audit and implementation of evidence-based practice, aiming to close the "knowing-doing" gap.
Representing a paradigm shift in perioperative care, ERAS challenges traditional practices, replacing them with evidence-based best practices in perioperative care.
Currently, the debate has shifted away from whether colorectal surgery following ERAS principles or traditional care is superior, towards enhancing the approach and streamlining its implementation. One such improvement involves transitioning patients from a surgical procedure requiring a 3–4 day hospital stay to a 1–2 day, or even same-day outpatient visit.
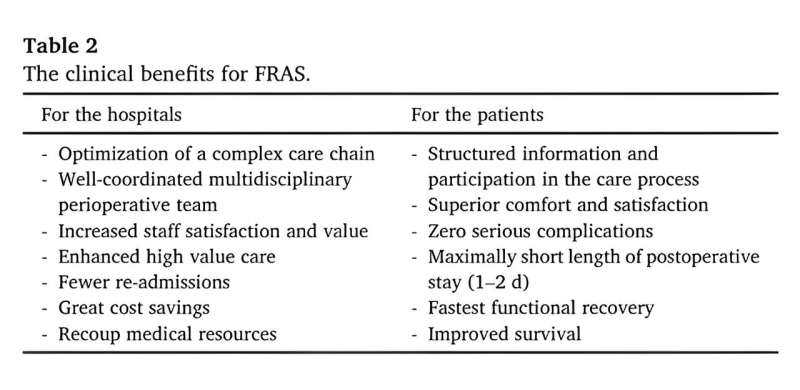
To this end, a team of researchers from China proposed a new concept called fastest recovery after surgery (FRAS) and implemented it in clinical practice to expedite recovery in patients undergoing elective major gastrointestinal surgery, building upon existing ERAS protocols.
"FRAS is a series of strengthened multimodal perioperative care pathways to optimize physiologic function, minimize surgical stress response, improve response to stress, and facilitate fastest postoperative recovery with improving comfort and satisfaction," explains Xiaohuang Tu, co-corresponding author of the study.
The researchers conducted pilot studies comparing short-term outcomes between FRAS and ERAS, and found that FRAS demonstrated "zero" complications, significantly reduced hospital stay duration, substantial cost savings and notably superior perioperative comfort and satisfaction.
The team reported their study in the journal Gastroenterology & Endoscopy .
"Considering the evidence underpinning the recommendations is continuously evolving, clinical guidelines need to be challenged and updated on a regular basis. More clinical evidence from high quality of randomized controlled trials or real-world medical data with large sample size are needed," notes Tu.
Explore further
Feedback to editors

Study suggests two copies of APOE4 gene behind up to 20% of Alzheimer's cases
19 hours ago

Researchers show genetic variant common among Black Americans contributes to large cardiovascular disease burden
22 hours ago

First person to receive a genetically modified pig kidney transplant dies nearly 2 months later

New vaccine could protect against coronaviruses that haven't even emerged yet
May 11, 2024


Study links organization of neurotypical brains to genes involved in autism and schizophrenia

Study traces an infectious language epidemic

Visual experiences unique to early infancy provide building blocks of human vision, study finds
May 10, 2024

Study points to personalized treatment opportunities for glioblastoma

Research team introduces new tool to boost battle against childhood undernutrition

How herpes hijacks a ride into cells
Related stories.

Enhanced recovery protocols improve patient outcomes in minimally invasive gynecologic surgery
Oct 14, 2022

Patient engagement and surgical outcomes improved by digital health platform
Apr 4, 2024
Colorectal surgery patients use fewer opioids, report less pain with enhanced recovery after surgery
Oct 19, 2019

Recovery protocol cuts opioid use after elective neurosurgery
Aug 27, 2020

Opioid use down with 'enhanced recovery after surgery' program
Oct 4, 2018

New approach to managing surgery will speed patient recovery but challenges current practices
Apr 29, 2019
Recommended for you

Autism's missing microbes may influence social behavior by protecting the gut

ERR-gamma 'trains' stomach stem cells to become acid-producing cells

Study shows damaging impact of heat waves on vital organs

A potential treatment for inflammatory bowel disease: Engineered yeast can transport medicines and lower inflammation
May 7, 2024

Researchers suggest B-cells may play role in lung transplant rejection
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
CASE REPORT article
This article is part of the research topic.
Changing Backgrounds and Groundbreaking Changes: Gynecological surgery in the third decade of the 21st century Volume II
A rare case of Malacoplakia resembling a malignant tumor of the cervix: a case report and review of the literature Provisionally Accepted

- 1 Department of gynecology, Ningbo No. 2 Hospital, China
The final, formatted version of the article will be published soon.
Malacoplakia is a rare chronic granulomatous disease that mostly affects the gastrointestinal tract and urinary tract of immunocompromised patients; malacoplakia rarely effects the female reproductive tract. Here, we report a 56-year-old patient who underwent thymectomy for thymoma and myasthenia gravis prior to developing cervical and vaginal malacoplakia. The patient presented with recurrent vaginal bleeding.. We discovered that there were alterations in the cervical cauliflower pattern during colposcopy, which is suggestive of cervical cancer. Pathological examination of the lesion tissue showed that a large number of macrophages aggregated, and M-G bodies with concentric circles and refractive properties were observed between cells.Immunostaining for CD68 and CD163 was positive, and special staining for D-PAS and PAS was positive. The discovery of Escherichia coli in bacterial culture can aid in the diagnosis of malacoplakia. Following surgery, we performed vaginal lavage with antibiotics in addition to resection of local cervical and vaginal lesions. This study provides a fresh perspective on the management of genital malacoplakia.
Keywords: Malacoplakia, malignant tumor of the cervix, Pathology, Vaginal bleeding, case report
Received: 29 Mar 2024; Accepted: 13 May 2024.
Copyright: © 2024 Li, Mi, Wang and ZHUO. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: PhD. Zhihong ZHUO, Department of gynecology, Ningbo No. 2 Hospital, Ningbo, China
People also looked at
Rapunzel syndrome in children: a retrospective review of ten cases combined with literature review in a tertiary referral center
- Original Article
- Published: 04 May 2024
- Volume 40 , article number 121 , ( 2024 )
Cite this article

- Yiyuan Liang 1 ,
- Liuming Huang 1 ,
- Dayong Wang 1 ,
- Tingting Liu 1 ,
- Xianling Li 1 ,
- Wei Wang 1 ,
- Qiulong Shen 1 ,
- Jinbao Han 1 ,
- Shuanling Li 1 ,
- Li Wang 1 &
- Long Chen 1
68 Accesses
Explore all metrics
Rapunzel syndrome is an uncommon condition in children, and its clinical features remain unclear. This study presents the largest single-center series of pediatric cases to date, with the objective of documenting the clinical characteristics and treatment approaches for children with Rapunzel syndrome.
A retrospective study was conducted in children with Rapunzel syndrome from 2019 to 2023. We recorded age, gender, symptoms, locations of bezoar, complications, and treatment options.
Ten patients with Rapunzel syndrome were included. The median age was 9.1 years, with all of whom were female. The most common clinical symptoms were upper abdominal mass (90%), abdominal pain (80%), and nausea and vomiting (50%). Complications occurred in six cases (60%), including small bowel obstruction (20%), severe gastric dilatation (10%), intestinal perforation (10%), choledochodilation (10%), acute pancreatitis with cholecystitis (10%). Preoperative ultrasonography suggested low-echoic foreign bodies continuing to the jejunum or ileocecal region in five cases (50%). Preoperative gastroscopy attempted in four cases (40%) to remove the foreign bodies, all of which failed. All patients underwent surgical treatment, with nine cases undergoing gastric incision foreign body removal, and one case undergoing gastric incision foreign body removal combined with intestinal perforation repair. All patients recovered well. No recurrence was observed during follow-up.
The accuracy of ultrasound diagnosis in identifying Rapunzel syndrome is high; however, it may lead to misdiagnosis if not complemented with the patient’s medical history. Endoscopic presents a heightened treatment risk and a reduced success rate. The condition commonly presents with severe complications, thus making laparotomy a safe and effective option for intervention.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Gastrointestinal trichobezoars in the pediatric population: a retrospective study
The role of endoscopic ultrasound in children with pancreatobiliary and gastrointestinal disorders: a single center series and review of the literature.

Gastrointestinal Tract Duplications
Data availability.
Original data are available on request.
Muhammad BM, Nabila T, Muhammad S (2020) Gastrointestinal trichobezoar: an experience with 17 cases. J Pediatr Surg 55(11):2504–2509. https://doi.org/10.1016/j.jpedsurg.2020.04.020
Article Google Scholar
Ivar S, Emily JR, Aliza TS, Thamrin H et al (2022) Sex differences in age at onset and presentation of trichotillomania and trichobezoar: a 120-year systematic review of cases. Child Psychiatr Hum Dev 53(1):165–171. https://doi.org/10.1007/s10578-020-01117-y
Paschos KA, Chatzigeorgiadis A (2019) Pathophysiological and clinical aspects of the diagnosis and treatment of bezoars. Ann Gastroenterol 32:224–232
PubMed PubMed Central Google Scholar
Mustafa ED, Tansel G, Mehmet Ç (2023) Saime Shermatova; Bezoar types in children and aetiological factors affecting bezoar formation: a single-centre retrospective study. Afr J Paediatr Surg 20(1):8–11. https://doi.org/10.4103/ajps.ajps_70_21
Catalina M, Bogdan M, Vasile D, Cristina CP (2013) Gastric bezoars—diagnostic and therapeutic challenges. J Gastrointest Liver Dis 224(1):111
Google Scholar
Kumble SM, Manas V, Danny J (2022) Rapunzel syndrome. J Gastrointest Surg 26(5):1111–1112. https://doi.org/10.1007/s11605-021-05239-z
Veena G, Divya-Devi J (2009) Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res 7(3):99–102. https://doi.org/10.3121/cmr.2009.822
Vaughan ED, Sawyers JL, Scott HW (1968) The Rapunzel syndrome: an unusual complication of intestinal bezoar. Surgery 63(2):339–343
PubMed Google Scholar
Dolores EB (2013) American Psychiatric Association Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Publishing, Philadelphia
Marta GS, Marek W, Andrzej K, Piotr A, Tomasz W (2016) Trichotillomania and trichophagia—diagnosis, treatment, prevention. Psychiatr Pol 50(1):127–143. https://doi.org/10.12740/PP/59513
Swedo SE, Leonard HL, Lenane MC, Rettew DC (1992) Trichotillomania: a profile of the disorder from infancy through adulthood. Int Pediatrics 7:114–150
Swedo SE, Rapoport JL (1991) Annotation: trichotillomania. J Child Psychol Psychiatry 32:401–409
Article CAS PubMed Google Scholar
Bloch MH, Craiglow BG, Landeros-Weisenberger A, Dombrowski PA, Panza KE, Peterson BS, Leckman JF (2009) Predictors of early adult outcome in pediatric-onset obsessive-compulsive disorder. Pediatrics 124:1085–1093
Article PubMed Google Scholar
Marek W, Marta GS, Michał G, Tomasz W, Piotr A, Andrzej K (2016) Trichotillomania, trichophagia, trichobezoar—summary of three cases. Endoscopic follow up scheme in trichotillomania. Psychiatr Pol 50(1):145–152. https://doi.org/10.12740/PP/43636
Besma H, Saida H, Amine K, Meriem O, Sana M, Marwa M, Sabrine BY, Lassaad S, Mongi M, Mohsen B, Abdellatif N (2022) Management of trichobezoar: about 6 cases. Afr J Paediatr Surg 19(2):102–104. https://doi.org/10.4103/ajps.AJPS_110_20
Erica YK, Nicholas JS, Gregory RD, Sarah NB (2015) Trichobezoar causing airway compromise during esophagogastroduodenoscopy. Case Rep Med 2015:806857. https://doi.org/10.1155/2015/806857
Xinlin C, Jessica YN (2021) Acute presentation of Rapunzel syndrome and a review of bezoars. Cureus 13(12):e20785. https://doi.org/10.7759/cureus.20785
Andreia FN, Chris JH, Richard ML, Sean SM, Mike AT (2020) Human and Doll’s hair in a gastric trichobezoar, endoscopic retrieval hazards. J Pediatr Gastroenterol Nutr 71(2):163–170. https://doi.org/10.1097/MPG.0000000000002779
Hanna C, Aleksandra K, Ewa P, Marta S, Adam R (2018) Trichotillomania and trichophagia: modern diagnostic and therapeutic methods. Dermatol Ther 8(3):389–398. https://doi.org/10.1007/s13555-018-0256-z
Lyons R, Ismaili G, Devine M, Malik H (2020) Rapunzel syndrome causing partial gastric outlet obstruction requiring emergency laparotomy. BMJ Case Rep 13:e232904. https://doi.org/10.1136/bcr-2019-232904
Article PubMed PubMed Central Google Scholar
Darwish AA, Abdelgawad AE, Platt E, Garrett-Cox R (2019) Formation of a temporary gastrostomy to aid delivery of gastric trichobezoar and decrease incidence of wound infection. BMJ Case Rep 12:e228660. https://doi.org/10.1136/bcr-2018-228660
Maarten JO, Ayoub C, Lucia ED (2020) Small-bowel obstruction secondary to a trichobezoar in a Meckel’s diverticulum in a patient with Rapunzel syndrome. J Gastrointest Surg 24(5):1220–1221. https://doi.org/10.1007/s11605-019-04448-x
Islam N, Mona AA, Ahmed M, Sohier Y, Yahya W, Abd ES (2019) Rapunzel syndrome (gastric trichobezoar), a rare presentation with generalised oedema: case report and review of the literature. Paediatr Int Child Health 39(1):76–78. https://doi.org/10.1080/20469047.2017.1389809
Appak YC, Ertan D, Karakoyun M, Ozyurt G, Ozdemir T, Baran M (2019) The cause of abdominal mass in a child with celiac disease: Rapunzel syndrome. A case report. Sao Paulo Med J 137:292–294
Bargas Ochoa M, Xacur Hernandez M, Espadas Torres M, Quintana Gamboa A, Tappan Lavadores I, Mendez Dominguez N (2018) Rapunzel syndrome with double simultaneous trichobezoar in a teenager: clinical case report. Rev Chil Pediatr 89:98–102
Cannalire G, Conti L, Celoni M, Grassi C, Cella A, Bensi G, Capelli P, Biasucci G (2018) Rapunzel syndrome: an infrequent cause of severe iron deficiency anemia and abdominal pain presenting to the pediatric emergency department. BMC Pediatr 18:125
Frey AS, Mckee M, King RA, Martin A (2005) Hair apparent: Rapunzel syndrome. Am J Psychiatry 162:242–248
Naik S, Gupta V, Naik S, Rangole A, Chaudhary AK, Jain P, Sharma AK (2007) Rapunzel syndrome reviewed and redefined. Dig Surg 24:157–161
Nour I, Abd Alatef M, Megahed A, Yahia S, Wahba Y, Shabaan AE (2019) Rapunzel syndrome (gastric trichobezoar), a rare presentation with generalised oedema: case report and review of the literature. Paediatr Int Child Health 39:76–78
Kohler JE, Millie M, Neuger E (2012) Trichobezoar causing pancreatitis: first reported case of Rapunzel syndrome in a boy in North America. J Pediatr Surg 47:e17–e19
Jain M, Solanki SL, Bhatnagar A, Jain PK (2011) An unusual case report of rapunzel syndrome trichobezoar in a 3-year-old boy. Int J Trichology 3:102–104
Hirugade ST, Talpallikar MC, Deshpande AV, Gavali JS, Borwankar SS (2001) Rapunzel syndrome with a long tail. Indian J Pediatr 68:895–896
Sarin YK (1998) Rapunzel syndrome. Indian Pediatr 35:682–683
CAS PubMed Google Scholar
Gonuguntla V, Joshi DD (2009) Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res 7:99–102
Mateju E, Duchanova S, Kovac P, Moravansky N, Spitz DJ (2009) Fatal case of Rapunzel syndrome in neglected child. Forensic Sci Int 190:e5-7
Hassan AA, Panesar KJ (1989) The Rapunzel syndrome: a rare presentation of trichobezoar. Ulster Med J 58:94–96
CAS PubMed PubMed Central Google Scholar
Bahk E, Ulman I, Taneli C, Demircan M (1993) The Rapunzel syndrome: a case report and review of the literature. Eur J Pediatr Surg 3:171–173
Seker B, Dilek ON, Karaayvaz M (1996) Trichobezoars as a cause of gastrointestinal obstructions: the Rapunzel syndrome. Acta Gastroenterol Belg 59:166–167
Pul N, Pul M (1996) The Rapunzel syndrome (trichobezoar) causing gastric perforation in a child: a case report. Eur J Pediatr 155:18–19
Bonnet JP, El Arbi N, Chelly D, Girodet D (1996) The Rapunzel syndrome: case report and review of the literature. Pediatr Surg Int 11:493–495
Senapati MK, Subramanian S (1997) Rapunzel syndrome. Trop Doct 27:53–54
West WM, Duncan ND (1998) CT appearances of the Rapunzel syndrome: an unusual form of bezoar and gastrointestinal obstruction. Pediatr Radiol 28:315–316
Singla SL, Rattan KN, Kaushik N, Pandit SK (1999) Rapunzel syndrome—a case report. Am J Gastroenterol 94:1970–1971
Dalshaug GB, Wainer S, Hollaar GL (1999) The Rapunzel syndrome (trichobezoar) causing atypical intussusception in a child: a case report. J Pediatr Surg 34:479–480
Faria AP, Silva IZ, Santos A, Avilla SG, Silveira AE (2000) The Rapunzel syndrome - a case report: trichobezoar as a cause of intestinal perforation. J Pediatr (Rio J) 76:83–86
Uckun A, Sipahi T, Igde M, Uner C, Cakmak O (2001) Is it possible to diagnose Rapunzel syndrome pre-operatively? Eur J Pediatr 160:682–683
Memon SA, Mandhan P, Qureshi JN, Shairani AJ (2003) Recurrent Rapunzel syndrome—a case report. Med Sci Monit 9:CS92–CS94
Klipfel AA, Kessler E, Schein M (2003) Rapunzel syndrome causing gastric emphysema and small bowel obstruction. Surgery 133:120–121
Perez E, Santana JR, Garcia G, Mesa J, Hernandez JR, Betancort N, Nunez V (2005) Gastric perforation due to trichobezoar in an adult (Rapunzel syndrome). Cir Esp 78:268–270
Mathai J, Chacko J, Kumar TS, Scott JX, Agarwal I, Varkki S (2007) Rapunzel syndrome: a diagnosis overlooked. Acta Paediatr 96:135–137
Henry PY, Nair PM, Jemila J, Krishna HR (2007) Rapunzel syndrome. Indian J Pediatr 74:872–873
Rabie ME, Arishi AR, Khan A, Ageely H, Seif El-Nasr GA, Fagihi M (2008) Rapunzel syndrome: the unsuspected culprit. World J Gastroenterol 14:1141–1143
Western C, Bokhari S, Gould S (2008) Rapunzel syndrome: a case report and review. J Gastrointest Surg 12:1612–1614
Anzieta VJ, Felmer EO, Gabrielli NM, Venturelli MF, Sánchez CG, Torrijos CC (2008) Intestinal obstruction due to a trichobezoar or Rapunzel syndrome: report of one case. Rev Med Chil 136:1027–1030
Al Wadan AH, Al Kaff H, Al Senabani J, Al Saadi AS (2008) ‘Rapunzel syndrome’ trichobezoar in a 7-year-old girl: a case report. Cases J 1:205
Mehta P, Bhutiani R (2009) The Rapunzel syndrome: is it an Asian problem? (case report and review of literature). Eur J Gastroenterol Hepatol 21:937–940
Agrawal V, Joshi MK, Jain BK, Gupta A (2009) Plasticobezoar—another new entity for Rapunzel syndrome. Indian J Pediatr 76:229–230
Vila S, Garcia C, Piscoya A, De Los RR, Pinto JL, Huerta-Mercado J, Bussalleu A (2009) Giant gastroduodenal trichobezoar: Rapunzel syndrome. Am J Gastroenterol 104:2864–2865
Koc O, Yildiz FD, Narci A, Sen TA (2009) An unusual cause of gastric perforation in childhood: trichobezoar (Rapunzel syndrome). A case report. Eur J Pediatr 168:495–497
Hernandez-Peredo-Rezk G, Escarcega-Fujigaki P, Campillo-Ojeda ZV, Sanchez-Martinez ME, Rodriguez-Santibanez MA, Angel-Aguilar AD, Rodriguez-Gutierrez C (2009) Trichobezoar can be treated laparoscopically. J Laparoendosc Adv Surg Tech A 19:111–113
Rajakannu M, Venkateshwarlu (2010) Rapunzel syndrome: report of a case with review of treatment. Trop Gastroenterol 31:133–134
Raikar S, Wali P, Khan S (2010) Recurrence of Rapunzel syndrome. J Pediatr 157(343–43):e1
Chogle A, Bonilla S, Browne M, Madonna MB, Parsons W, Donaldson J, Alonso E (2010) Rapunzel syndrome: a rare cause of biliary obstruction. J Pediatr Gastroenterol Nutr 51:522–523
Fernandes SV (2010) Re: Chappel v Hart res judicata? ANZ J Surg 80:568–569; author reply 76
Gorter RR, Kneepkens CM, Mattens EC, Aronson DC, Heij HA (2010) Management of trichobezoar: case report and literature review. Pediatr Surg Int 26:457–463
Article CAS PubMed PubMed Central Google Scholar
Dorn HF, Gillick JL, Stringel G (2010) Laparoscopic intragastric removal of giant trichobezoar. JSLS 14:259–262
Bashir EA, Samiullah SMA, Yusuf O, Karim K (2010) Rapunzel syndrome. J Ayub Med Coll Abbottabad 22:218–220
Tiwary SK, Kumar S, Khanna R, Khanna AK (2011) Recurrent Rapunzel syndrome. Singapore Med J 52:e128–e130
Singh S, Wakhlu A, Pandey A, Gupta A, Ahmed I, Chandra N (2011) Complicated Rapunzel syndrome mimicking intussusception. BMJ Case Rep 2011: bcr0820103277
Cook SL, Beaver B, Brislin R, Elitsur Y (2011) Rapunzel syndrome: not just a “hairy tail.” Clin Pediatr (Phila) 50:372–374
Kawoosa NU, Zargar BR (2011) A giant Trichobezoar causing Rapunzel syndrome in a 12-year-old female. Indian J Psychol Med 33:77–79
Ozdemir H, Ozdemir ZU, Sahiner IT, Senol M (2012) Rapunzel syndrome case report: a 13-year-old girl. Int J Trichol 4:275–277
Phavichitr N, Vathanasanti C (2012) Rapunzel syndrome in a Thai girl with an asymptomatic abdominal mass: a case report. J Med Assoc Thai 95(Suppl 5):S177–S180
Germani M, Beltra Pico R, Hernandez Castello C (2014) Rapunzel syndrome: laparoscopic treatment. An Pediatr (Barc) 80:e33–e34
Islek A, Sayar E, Yilmaz A, Boneval C, Artan R (2014) A rare outcome of iron deficiency and pica: Rapunzel syndrome in a 5-year-old child iron deficiency and pica. Turk J Gastroenterol 25:100–102
Marwah S, Pandey S, Raj A, Jangra MS, Sharma H (2015) Rapunzel syndrome presenting as jejuno-jejunal intussusception. Clin J Gastroenterol 8:202–206
Zeraatian S, Ameri S, Tabesh H, Kamalzadeh N (2015) Uncommon presentation of gastric trichobezoar: a case report. Iran J Public Health 44:1008–1011
Czerwinska K, Bekiesinska-Figatowska M, Brzewski M, Gogolewski M, Wolski M (2015) Trichobezoar, rapunzel syndrome, tricho-plaster bezoar—a report of three cases. Pol J Radiol 80:241–246
Wolski M, Gawlowska-Sawosz M, Gogolewski M, Wolanczyk T, Albrecht P, Kaminski A (2016) Trichotillomania, trichophagia, trichobezoar—summary of three cases. Endoscopic follow up scheme in trichotillomania. Psychiatr Pol 50:145–152
Kim SC, Kim SH, Kim SJ (2016) A case report: large trichobezoar causing Rapunzel syndrome. Medicine (Baltimore) 95:e3745
Rojas PG, Paredes EB, Reto CP (2016) Rapunzel syndrome as a cause of obstruction and intestinal perforation. Acta Gastroenterol Latinoam 46:114–117
Ahmed N, Baloch MA, Baber KM, Ahmed J (2016) A rare variant of Rapunzel syndrome-acute small bowel obstruction caused by ball of hairs in distal ileum with its tail extending in caecum and ascending colon. J Pak Med Assoc 66:761–764
Kumar Bn A, Kumar LN, Thippeswamy J, Rangaswamaiah LN (2016) Trichobezoar (Rapunzel syndrome) in an adolescent patient with Trichotillomania and generalized anxiety disorder: a case report. Asian J Psychiatr 23:44–45
Caiazzo P, Lascio PD, Crocoli A, Prete ID (2016) The Rapunzel syndrome. Report of a case. G Chir 37:90–94
Beristain-Silva JL, Cordero-Barberena R, Beristain-Hernandez JL (2016) Rapunzel syndrome: a rare cause of abdominal pain. Rev Gastroenterol Mex 81:178–179
Yik YI, How AK (2016) Stomach trichobezoar (rapunzel syndrome) with iatrogenic intussusception. Med J Malaysia 71:74–76
Nwankwo E, Daniele E, Woller E, Fitzwater J, McGill T, Brooks SE (2017) Trichobezoar presenting as a gastric outlet obstruction: a case report. Int J Surg Case Rep 34:123–125
Lalith S, Gopalakrishnan KL, Ilangovan G, Jayajothi A (2017) Rapunzel syndrome. J Clin Diagn Res 11:TD01–TD02
Iwama I, Nambu R, Hara T (2018) A novel finding of Rapunzel syndrome. Clin J Gastroenterol 11:19–22
Hamid M, Chaoui Y, Mountasser M, Sabbah F, Raiss M, Hrora A, Alaoui M, Ahallat M, Chaouch S, Ouazzani H (2017) Giant gastric trichobezoar in a young female with Rapunzel syndrome: case report. Pan Afr Med J 27:252
Alcívar MS, Ruiz MB, Gusñay MM, Almeida JC, Rendón FA, Robles-Medranda C (2019) Giant Rapunzel syndrome with atypical complication. Report of a case. Rev Gastroenterol Peru 39:74–77
Tripodi V, Caruso A, Luraghi M, Armao FT, Bisagni P, Romano S, Scagnelli P, Giacchero R, Gendarini A, Leoni P (2020) Paediatric gastric trichobezoar: the Rapunzel syndrome. A report of two cases. Ann Ital Chir 9
Antunes H, Barroso C, Faria C, Correia-Pinto J (2020) Images in paediatrics: Rapunzel syndrome: the pathway for a prompt diagnosis. Arch Dis Child 105:298
Kumar M, Maletha M, Bhuddi S, Kumari R (2020) Rapunzel syndrome in a 3-year-old boy: a menace too early to present. J Indian Assoc Pediatr Surg 25:112–114
Vellaisamy R, Iyer S, Chandramohan SM, Harikrishnan S (2020) Rapunzel syndrome with cholangitis and pancreatitis—a rare case report. Open Med (Wars) 15:1137–1142
Otten MJ, Charehbili A, Duinhouwer LE (2020) Small-bowel obstruction secondary to a Trichobezoar in a Meckel’s diverticulum in a patient with Rapunzel syndrome. J Gastrointest Surg 24:1220–1221
Jackman J, Nana GR, Catton J, Christakis I (2021) Gastric perforation secondary to Rapunzel syndrome. BMJ Case Rep 14:e240100
Madhusudhan KS, Vaishnav M, Joy D (2022) Rapunzel Syndrome. J Gastrointest Surg 26:1111–1112
Haggui B, Hidouri S, Ksia A, Oumaya M, Mosbahi S, Messaoud M, Youssef SB, Sahnoun L, Mekki M, Belghith M, Nouri A (2022) Management of trichobezoar: about 6 cases. Afr J Paediatr Surg 19:102–104
Pegues JN, Lucas ED, Morris M (2023) Recurrent Rapunzel syndrome in an adolescent female. Am Surg 89:3665–3667
Kumar D, Pandey V, Nandan R (2023) Rapunzel syndrome: a concealed tale of the misleading tail. J Indian Assoc Pediatr Surg 28:69–71
Trinh NB, Nguyen MT, Nguyen TGH (2023) Sepsis secondary to Rapunzel syndrome. Indian J Dermatol Venereol Leprol 89:334
Eddin AS, Amarneh M, Goetz S, Donato F Jr (2023) Successful endovascular treatment of superior mesenteric artery-duodenal fistula secondary to Rapunzel syndrome. Radiol Case Rep 18:2689–2691
Nasri S, Ammor A, Bendaoud M, Diouri L, Tayeb B, Driss EA, Kamaoui I, Aichouni N, Skiker I (2023) Rapunzel syndrome: an infrequent cause of paediatric mechanical occlusion. Afr J Paediatr Surg 20:71–73
Kyin C, Patel P, Casas-Melley A, Abdalla WM, Westmoreland T (2023) Acute case of trichobezoar diagnosed from computed tomography and 3D images: Rapunzel syndrome re-examined. Cureus 15:e35597
Piras GN, Tomassini L, Bottoni E, Di Gioia C, Ciallella C (2023) An atypical death from Rapunzel syndrome: a case report. Forensic Sci Med Pathol 19:207–214
Zyla AA, Jacques R (2023) Fatal Rapunzel syndrome: gastric and intestinal trichobezoars in a child with trichotillomania. Am J Forensic Med Pathol. https://doi.org/10.1097/PAF.0000000000000849
Download references
Author information
Authors and affiliations.
Department of Emergency Surgery, National Center for Children’s Health, Beijing Children’s Hospital, Capital Medical University, Beijing, China
Yiyuan Liang, Liuming Huang, Dayong Wang, Tingting Liu, Xianling Li, Wei Wang, Qiulong Shen, Jinbao Han, Shuanling Li, Li Wang & Long Chen
You can also search for this author in PubMed Google Scholar
Contributions
Yiyuan Liang: Visualization; writing – original draft. Dayong Wang,Tingting Liu,Xianling Li: Data curation;resources; software. Wei Wang,Qiulong Shen,Jinbao Han: Data curation; formal analysis;resources. Shuanling Li , Li Wang,Long Chen: Data curation; formal analysis; visualization; Liuming Huang: Conceptualization; project administration;supervision. All authors reviewed the manuscript
Corresponding author
Correspondence to Liuming Huang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Liang, Y., Huang, L., Wang, D. et al. Rapunzel syndrome in children: a retrospective review of ten cases combined with literature review in a tertiary referral center. Pediatr Surg Int 40 , 121 (2024). https://doi.org/10.1007/s00383-024-05705-0
Download citation
Accepted : 21 April 2024
Published : 04 May 2024
DOI : https://doi.org/10.1007/s00383-024-05705-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rapunzel syndrome
- Trichotillomania
- Trichobezoar
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Meckel's diverticulum is a true diverticulum comprised of all 3 layers of the gastrointestinal (GI) tract, including mucosa, ... and if found during surgery, removal is typically up to the discretion of the surgeon. ... Case Study: 32-Year-Old Male Presenting with Right Lower Quadrant Abdominal Pain - StatPearls ...
PRESENTATION OF CASE. A 76-year-old woman was seen in our multidisciplinary gastrointestinal oncology clinic for further management of an adenocarcinoma of the body of the stomach. The patient presented to her primary care physician with a four-week history of intermittent chest pressure radiating to her back. Extensive evaluation for a cardiac ...
A 29-year-old woman was evaluated at a primary care clinic affiliated with this hospital because of nausea, vomiting, and diarrhea. She reported a history of nonprescribed oxycodone use and request...
His past medical history included hypertension, type-2 diabetes mellitus, mild aortic stenosis, hematuria, and arterio-venous malformations in the gastrointestinal tract. His hemoglobin upon admission was 4.1 g/dL, which decreased to 3.1 on the 3rd day after admission. Xarelto was discontinued upon admission and he was placed on aspirin 325 mg/day.
Clinical Case, February 05, 2008. Gastroparesis -- Current Concepts and Considerations Gastroparesis presents with symptoms of gastric retention and nongastrointestinal manifestations, with ...
The patient was evaluated by the bariatric multidisciplinary team at Sibley Memorial Hospital and approved for surgery. The patient underwent a minimally invasive Roux-en-Y gastric bypass using the latest camera technology. After her procedure, a new technique was used to test the gastro-jejunal anastomosis for any signs of a leak.
Results included studies assessing microbiome in surgery for IBD (n = 8), in colorectal surgery (n = 4) and in non-specified gastrointestinal surgery (n = 2). Inflammatory bowel diseases
Case study. GISTs are rare, accounting for 0.1-3% of all malignancies of the gastrointestinal tract. 1 They can present with a number of local and systemic symptoms including acute or chronic blood loss. A previously fit and healthy 35-year-old woman was airlifted to A&E after her husband found her collapsed and bleeding heavily on the bathroom floor.
D.N. AssisN Engl J Med 2024;390:853-854. Primary biliary cholangitis is a chronic cholestatic, autoimmune disease characterized by the destruction of small, intrahepatic biliary epithelial cells ...
This journal's articles appear in a wide range of abstracting and indexing databases, and are covered by numerous other services that aid discovery and access. Find out more about where and how the content of this journal is available. Case Reports in Gastrointestinal Medicine publishes case reports and case series focusing on gastroenterology ...
Gastrointestinal stromal tumors (GISTs) are soft tissue sarcomas that can occur anywhere in the GI tract. There are roughly 4,000 to 6,000 cases diagnosed in the United States annually. GISTs are often asymptomatic early on and can evade detection, occasionally resulting in malignancy. Due to their insidious growth and location, it is suspected ...
A 13-year-old boy presents to his primary care provider with a 5-day history of abdominal pain and a 2-day history of diarrhea and vomiting. He describes the quality of the abdominal pain as sharp, originating in the epigastric region and radiating to his back, and exacerbated by movement. Additionally, he has had several episodes of nonbloody, nonbilious vomiting and watery diarrhea. His ...
Gastrointestinal Case Studies Gastrointestinal (GI) disorders refer to conditions affecting the digestive system, including the esophagus, stomach, small and large intestines, liver, pancreas, and gallbladder. ... and surgery. Examples of treatment modalities for specific conditions include: GERD: proton pump inhibitors (PPIs), H2 receptor ...
BMJ Case Reports CP Nov 2023, 16 (11) e256702; DOI: 10.1136/bcr-2023-256702 . ... Gastrointestinal surgery (432) General surgery (457) Neurosurgery (204) ... Epidemiologic studies. Population trends. Screening (epidemiology) Survey techniques. Therapeutic trials. Time-to-event methods.
Background Current evidence on the surgical rate, indication, procedure, risk factors, mortality, and postoperative rebleeding for acute lower gastrointestinal bleeding (ALGIB) is limited. Methods We constructed a retrospective cohort of 10,342 patients admitted for acute hematochezia at 49 hospitals (CODE BLUE J-Study) and evaluated clinical data on the surgeries performed. Results Surgery ...
Gastrointestinal surgery represents the largest field in General Surgery. In the last years, several new techniques have been introduced, sometimes with low-evidence to justify a wider adoption, sometimes improving postoperative outcomes and adding a further help for a tailored approach to a specific disease (e.g. TaTME in the surgery of rectal cancer, CME in right hemicolectomy, Mini-invasive ...
gastrointestinal surgery alone on the microbiome profile. An ideal future model for research should encompass case- controlled or cohort design with longer term follow-up in a homogeneous patient ...
Gastrointestinal Endoscopy publishes original, peer-reviewed articles on endoscopic procedures used in the study, diagnosis, and treatment of digestive diseases. Articles report on outcomes research, prospective studies, and controlled trials of new endoscopic instruments and treatment methods. Online features include full text of all articles ...
Current recommendations on EPM after gastrointestinal surgery basically refer to a systematic review of trials involving early mobilization and published up to 2015, ... Three prospective studies (one case control, two RCTs) assessed short-term pulmonary function after EPM by measuring oxygenation (for example oxygen saturation (SaO 2)), ...
Gastrointestinal surgery is commonly performed for various indications in the upper gastrointestinal tract. There are a number of unique complications that arise in this patient population and require specific knowledge for proper management. ... Surgical resection of the redundant limb provided 94-100% success rate in case series studies [67 ...
Road of recovery in gastrointestinal surgery: From ERAS to FRAS. by KeAi Communications Co., Ltd. Comparisons of short-term outcomes between FRAS and ERAS. Credit: Huanghui Wu, et al. In the 1990s ...
A case control study by Zhang et al. analyzed 206 patients who had GI complications following CPB surgery from 2000 to 2007 compared to 206 matched control patients. The results of this study suggested that GI complications could be reduced by maintaining a higher perfusion pressure and shortening the time on CPB and ventilation .
While in the ED, the nurse inserted an 18-gauge intravenous (IV) to the left antecubital fossa (AC) and administered a 1 L normal saline (NS) bolus. Mary's labs (CBC, CMP, cultures) were drawn, an x-ray and abdominal CT scan were performed, and a stool sample was ordered. She was administered 1 mg of morphine sulfate IV push at 1115 for her pain.
Malacoplakia is a rare chronic granulomatous disease that mostly affects the gastrointestinal tract and urinary tract of immunocompromised patients; malacoplakia rarely effects the female reproductive tract. Here, we report a 56-year-old patient who underwent thymectomy for thymoma and myasthenia gravis prior to developing cervical and vaginal malacoplakia. The patient presented with recurrent ...
This work points out the need for a prospective, large study comparing the diagnostic yield of enteroscopy vs EGD in patients with upper GI bleeding status post RYGB surgery. Peer-review The authors report two cases with acute UGIB following Roux-en-Y gastric bypass where the diagnosis and treatment were performed successfully with enteroscopy.
Purpose Rapunzel syndrome is an uncommon condition in children, and its clinical features remain unclear. This study presents the largest single-center series of pediatric cases to date, with the objective of documenting the clinical characteristics and treatment approaches for children with Rapunzel syndrome. Methods A retrospective study was conducted in children with Rapunzel syndrome from ...