- FCUS Courses
- Register for FCUS Course

- What is the ICN?
- The ICN Story
- ICN Hot cases
- Semantic sMatter
- ECG Proving Ground
- ICU Radiology Cases
- Game Changing Evidence
- Pharmacology
- Past Papers
- Approaches to Questions
- Clinical Exam
- Clinical Governance
- Past Papers with Answers
- The ICN meta feed
- Conferences
- Websites & Blogs
- Books & Journals
- Clinical Calculators

Clinical Cases
This section is a collection of critical care clinical cases to test yourself and hopefully get some new ideas.
Please leave feedback and comments, and if you want to put your own hot cases up, please get in touch and we can make it happen.

Can you work out the cause of this DVT?

Pulmonary Artery Catheters: PAC traps for young snake charmers

End-o-bed-o-gram – Case 3

Spot Diagnosis #2
End-o-bed-o-gram – case 2.

The NEJM Critical Care Challenge: Case 11 (Answer)
Spot diagnosis #1, the nejm critical care challenge: case 11 (end of life care), nejm critical care challenge case 10 (sdh) answer, the nejm critical care challenge: case 10 (acute sdh), icu-acquired weakness: nejm critical care challenge case 9 (question and answer).
Nutrition: NEJM Critical Care Challenge Case 8 Answer
End-o-bed-o-gram 1, the nejm critical care challenge: case 8, coagulopathy: nejm critical care challenge case 7 answer, coagulopathy: nejm critical care challenge case 7, icu sedation: nejm critical care challenge case 6 answer, icu sedation: nejm critical care challenge case 6, acute liver failure: nejm critical care challenge case 5 answer, acute liver failure: nejm critical care challenge case 5, ventilation: nejm critical care challenge case 4 answer.
Haemodynamic Monitoring: NEJM Critical Care Challenge Case 3 ANSWER
Haemodynamic monitoring: the nejm critical care challenge case 3, resuscitation fluid: nejm critical care challenge case 2 answer.

The NEJM Critical Care Challenge: Case 2
Septic shock: nejm critical care challenge case 1 answer, septic shock: nejm critical care challenge case 1.

The NEJM Critical Care Challenge: Case 1

Hot Case #14 – I’m pregnant … HELLP!
Hot Case #13 – To bust or not to bust?

ICN Hot Case #12 – Pull my finger!
Hot Case #11 – Testing testing

ICN Hot Case #10

ICN Hot Case #9

ICN Hot Case #8

ICN Hot Case #7

ICN Hot Case # 6
The nejm critical care challenge: case 4.
ICN Hot Case #5

September Case of the month

ICN Hot Case #4

ICN Hot Case #3

- What is ICN
- The Team
- ICN NSW
- ICN QLD
- ICN VIC
- ICN WA
- ICN NZ
- ICN UK
- Lung US
- Exam Help
- Clinical Cases
- Echo Cases
- Echo Guide
- ICU Radiology
- Game Changing Evidence
- ICN Metafeed
- Simulation Resouces
- SMACC Posters
- Audio
- Video
- Pecha Kuchas
- End-o-Bed-o-Gram
- ICU Primary Exam
- CICM Fellowship
- ANZCA Fellowship
- Paeds Fellowship
- Emergency Primary
- Anaesthetics Primary
® 2024 The Intensive Care Network || All rights reserved || Disclaimer || Site Map || Contact ICN Support
Log in with your credentials
or Create an account
Forgot your details?
Create account.

- Medical Books
Fulfillment by Amazon (FBA) is a service we offer sellers that lets them store their products in Amazon's fulfillment centers, and we directly pack, ship, and provide customer service for these products. Something we hope you'll especially enjoy: FBA items qualify for FREE Shipping and Amazon Prime.
If you're a seller, Fulfillment by Amazon can help you grow your business. Learn more about the program.

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player

Case Studies in Critical Care Nursing: A Guide for Application and Review 3rd Edition
- Each chapter contains the case presentation, questions and answers, and references.
- Each case study includes patient assessment and history of the disorder, laboratory observations and results, and pharmacological options for the patient.
- Comprehensive discussion and evaluation of the critical thinking questions follow each case study.
- Internet resources are included throughout the case studies to further the user's access to information on a variety of disorders.
- Contains an all-inclusive glossary of key critical care abbreviations.
- ISBN-10 0721603440
- ISBN-13 978-0721603445
- Edition 3rd
- Publisher Saunders
- Publication date March 5, 2004
- Language English
- Dimensions 8.5 x 1 x 10.5 inches
- Print length 528 pages
- See all details

Customers who viewed this item also viewed

Editorial Reviews
About the author, product details.
- Publisher : Saunders; 3rd edition (March 5, 2004)
- Language : English
- Paperback : 528 pages
- ISBN-10 : 0721603440
- ISBN-13 : 978-0721603445
- Item Weight : 2.87 pounds
- Dimensions : 8.5 x 1 x 10.5 inches
- #278 in Nursing Critical & Intensive care
- #341 in Critical Care
- #5,113 in Core
Customer reviews
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
- Sort reviews by Top reviews Most recent Top reviews
Top reviews from the United States
There was a problem filtering reviews right now. please try again later..
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell on Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Become an Amazon Hub Partner
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
Book review Previous Next
Case studies in critical care nursing, maureen eby.
Case Studies in Critical Care Nursing is an exciting book for the critical care nurse who is striving to develop skills in analysing the complex needs of the critically ill patient. It will enable nurses to play a vital role in co-ordinating and focusing the efforts of the many health care workers toward realistic patient-orientated goals.
Nursing Standard . 5, 45, 43-43. doi: 10.7748/ns.5.45.43.s58
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

31 July 1991 / Vol 5 issue 45
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Case Studies in Critical Care Nursing
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Innovative solutions: using case studies to generate increased nurse's clinical decision-making ability in critical care
Affiliation.
- 1 Family Nurse Practitioner Specialty, Fairfield University School of Nursing, Fairfield, CT 06824, USA. [email protected]
- PMID: 20395734
- DOI: 10.1097/DCC.0b013e3181d24d86
Learning to care for critically ill patients requires a high level of critical thinking, clinical decision-making ability, and a substantial knowledge base. At this nursing school, an elective Critical Care Nursing course for last-semester seniors was designed to include active learning strategies, focusing on the use of case studies to facilitate learning. Results indicate significantly improved final examination scores for those involved with the case-study pedagogy. In addition, students identified enhanced communication skills. Two complex cases are presented for others to use with their educational programs.
Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study
Hye jin yoo.
1 Department of Nursing, Asan Medical Center, Seoul, South Korea
Oak Bun Lim
Jae lan shim.
2 College of Medicine, Department of Nursing, Dongguk University, Gyeongju, South Korea
Associated Data
All relevant data are within the manuscript.
This study evaluated the communication experiences of critical care nurses while caring for patients in an intensive care unit setting. We have collected qualitative data from 16 critical care nurses working in the intensive care unit of a tertiary hospital in Seoul, Korea, through two focus-group discussions and four in-depth individual interviews. All interviews were recorded and transcribed verbatim, and data were analyzed using the Colaizzi’s method. Three themes of nurses’ communication experiences were identified: facing unexpected communication difficulties, learning through trial and error, and recognizing communication experiences as being essential for care. Nurses recognized that communication is essential for quality care. Our findings indicate that critical care nurses should continuously aim to improve their existing skills regarding communication with patients and their care givers and acquire new communication skills to aid patient care.
Introduction
Critical care nurses working in intensive care units (ICUs) care for critically-ill patients, and their work scope can include communicating with patients’ loved ones and care givers [ 1 ]. In such settings, nurses must make timely judgments based on their expertise, and this requires a high level of communication competency to comprehensively evaluate the needs of patients and their families [ 2 , 3 ]. The objective of nurses’ communication is to optimize the care provided to patients [ 4 ]. Therapeutic communication, a fundamental component of nursing, involves the use of specific strategies to encourage patients to express feelings and ideas and to convey acceptance and respect. In building an effective therapeutic relationship, a focus on the patient and a genuine display of empathy is required [ 5 ]. Empathy is the ability to understand and share another person’s emotions. To convey empathy towards a patient, one must accurately perceive the patient’s situation, communicate that perception to the patient, and act on the perception to help the patient [ 6 ]. Effective communication based on empathy not only contributes greatly to the patient's recovery [ 3 , 5 – 7 ], but also has a positive effect of improving job satisfaction by nursing with confidence [ 8 ] In contrast, inefficient communication leads to complaints and anxiety in patients and can also lead to other negative outcomes, such as extended hospital stays, increased mortality, burnout, job stress, and turnover [ 9 , 10 ].
Therefore, communication experiences need investigation since effective communication is an essential for critical care nurses. Nurses use curative communication skills to provide new information, encourage understanding of patient’s responses to health troubles, explore choices for care, help in decision making, and facilitate patient wellbeing [ 11 ]. Particularly, patient- and family-centered communication contributes to promoting patient safety and improving the quality of care [ 12 , 13 ]. However, communication skills are relatively poorly developed among critical care nurses compared to nurses in wards and younger and less experienced nurses than in their older and more experienced counterparts [ 3 , 7 , 14 – 16 ]. This calls for an examination of the overall communication experiences of critical care nurses.
To date, most studies on the communication of critical care nurses have been quantitative and have evaluated work performance, association with burnout, and factors that hinder communication [ 2 – 4 , 7 ]. A qualitative study has examined communications with families of ICU patients in Korea [ 17 ], while an international study has identified factors that promote or hinder communication between nurses and families of ICU patients [ 16 , 18 ]; however, few studies have been conducted on participant-oriented communication (including patients and families). Nurses’ communication with patients and their families in a clinical setting is complex and cannot be understood solely on the basis of questionnaire surveys; therefore, these communication experiences must be studied in depth.
This study explored critical care nurses’ communication experiences with patients and their families using an in-depth qualitative research methodology. This study will help to enhance communication skills of critical care nurses, thereby improving the quality of care in an ICU setting.
Materials and methods
This study employed a qualitative descriptive design using focus-group interviews (FGIs) and in-depth individual interviews and was performed according to the consolidated criteria for reporting qualitative research (COREQ) checklist [ 19 ]. An FGI is a research methodology in which individuals engage in an intensive and in-depth discussion of a specific topic to explore their experiences and identify common themes based on the interactions among group members [ 20 ]. Individual in-depth interviews were also conducted to complement the content identified in FGIs and further explore the deeper information developed based on experiences at the individual level.
Participants
Sixteen critical care trained nurses providing direct care to patients in an ICU of a tertiary hospital in Seoul were included in this study. The purpose of this study and the contents of the questionnaire were explained to them, and they voluntarily agreed to participate and complete the questionnaire. The exclusion criteria were as follows: 1) nurses with a hearing problem; 2) nurses with less than 1 year of clinical experience; and 3) nurses diagnosed with psychiatric disorders.
Snowball sampling—in which participants recruit other participants who can vividly share their experiences regarding the topic under investigation—was used. Six participants for the first FGI, six for the second FGI, and four for the individual in-depth interviews were recruited. All participants were women (mean age = 29.0 years old; mean nursing experience = 4.5 years). Their characteristics are listed in Table 1 .
Data collection
Developing interview questions.
The interview questions were structured according to the guidelines developed for the focus-group methodology [ 21 ]: 1) introductory questions, 2) transitional questions, 3) key questions, and 4) ending questions. The questions were reviewed by a nursing professor with extensive experience in qualitative research and three critical care nurses with more than 10 years of ICU experience ( Table 2 ). These questions were also used for individual face-to-face in-depth interviews.
Conducting FGIs and individual interviews
The two FGIs and four individual interviews were conducted between July 20, 2019 and September 30, 2019. The FGIs were moderated by the principal female investigator and were conducted in a quiet conference room where participants were gathered around a table to encourage them to talk freely. The FGIs were audio-recorded with the participants’ consent, and the recordings were transcribed and analyzed immediately after. Similar content was observed from the two rounds of FGIs, and we continued the discussion until no new topics emerged.
To complement the FGIs and verify the results of the analysis, we also conducted individual interviews of four participants. One assistant helped in facilitating the interviews and took notes. The duration of each interview was about 60–90 minutes.
Ethical considerations and investigator training and preparation
This study was approved by the institutional review board of the Asan Medical Center (approval no. 2019–0859). Prior to data collection, participants provided written informed consent and were informed in advance that the interviews would be audio-recorded, their participation would remain confidential, the recordings and transcripts would only be used for research purposes, the data would be securely stored under a double lock and would be accessed by the investigators only, and personal information would be deleted upon the completion of the study to eliminate any possibility of a privacy breach. The collected data were coded and stored to be accessed by the investigators only to prevent leakage of any personal information.
The authors of this study are nurses with more than 10 years of ICU experience and a deep understanding of critical care. The principal investigator took a qualitative research course in graduate school and has conducted multiple qualitative studies to enhance her qualitative research experience.
Data analysis
We utilized Colaizzi’s [ 22 ] method of phenomenological analysis to understand and describe the fundamentals and meaning of nurses’ communication experiences with patients and families. Data analysis was conducted in seven steps: 1) Recording and transcription of the in-depth interviews (all authors read the transcripts repeatedly to better understand the participants’ meaning); 2) Collection of meaningful statements from phrases and sentences containing phenomena relating to the communication experiences in the ICU. We extracted statements overlapping with statements of similar meaning—taking representative ones of similar statements—and omitted the rest; 3) Searching for other interpretations of participant statements using various contexts; 4) Extraction of themes from relevant meanings and development of a coding tree, with the meanings organized into themes; 5) Organization of similar topics into a more general and abstract collection of themes; 6) Validation of the collection of themes by cross-checking and comparing with the original data; 7) After integrating the analyzed content into one technique, the overall structure of the findings was described.
During data analysis, we received advice on the use of language or result of analyzing from a nursing professor with extensive experience in qualitative research and had the data verified by three participants to establish the universality and validity of the identified themes.
Establishing precision
The credibility, fittingness, auditability, and confirmability of the study were evaluated to analyze our findings [ 23 ]. To increase credibility, we conducted the interviews in a quiet place to focus on participants’ statements and help participants feel comfortable during interviews; to establish the universality and validity of the identified themes, data verification was performed by three participants. To ensure uniformity in data, participants who could provide detailed accounts of their experiences were selected, and the data were collected and analyzed until saturation was achieved (i.e., no new content emerged). To ensure auditability, the raw data for the identified themes were presented in the results, such that the readers could understand the decision-making process. To ensure confirmability, our preconceptions or biases regarding the participants’ statements were consistently reviewed to minimize the impact of bias and maintain neutrality.
After analyzing the communication experiences of 16 critical care nurses, three major themes emerged: facing unexpected communication difficulties, learning through trial and error, and recognizing communication experiences as being essential for care. The results are summarized in Table 3 .
The results of this study are schematized based on Travelbee's Human-to-Human Relationship Model [ 24 , 25 ] ( Fig 1 ), which suggests that human-to-human interaction is at a developmental stage. In this study, communication between patients and their families and experienced nurses in ICUs promotes human-to-human connections, leading to a genuine caring relationship through interaction, empathy, listening, sharing, and respect, which are all therapeutic communication skills.

Theme 1: Facing unexpected communication difficulties
Nurses experienced more difficulties in communicating with patients and their families and caregivers than in performing essential nursing activities (e.g., medication administration, suction, and various mechanical operations) The communication difficulties they experienced were either nurse-, patient- and family-, or system-related. Distinct problems in an ICU are related to urgency; for example, hemodynamically unstable patients or patients with respiratory failure or those suffering from a cardiac arrest may be prioritized.
Nurse-related factor: True intentions were not conveyed as wished
Although nurses intend to treat patients and their families with empathy, they frequently lead one-way conversations when pressed for time in the ICU. In addition, their usual way of talking, such as their dialect and intonation, can sometimes be misunderstood and cause offense. Participants experienced difficulties communicating their sincerity to patients and their families.
“Oftentimes, I only say what I have to say instead of what the caregivers really want to know when I’m pressed for time to convey my thoughts and go on to the next patient to explain things to the other patient.” (Participant 2)
“I usually speak loudly, and I speak in dialect; so, things I say are not delivered gently…I try to be careful because my dialect can seem more aggressive than the Seoul dialect; but it’s not easy to fix what I have used for all my life at once.” (Participant 3)
Nurse-related factor: Hesitant to provide physical comfort
Participants were not familiar with using non-verbal communication. The participants realized the importance of both verbal communication and physical contact in providing care, but the application of both these communication styles was not easy in clinical practice.
“I want to console the caregivers of patients who pass away; but I just can’t because I get shy. I feel like I’m overstepping, and when I’m contemplating whether I can really speak to their emotions, the caregiver has already left the ICU in many cases.” (Participant 6)
“I’m really bad at physical contact even with my close friends; but I’m even worse when it comes to patients and caregivers. Because of my tendency, there are times when I hesitate to touch patients while providing care.” (Participant 7)
Patient- and family-related factor: Mechanical ventilation hindering communication with the patient
Mechanical ventilators were the greatest obstruction to communication in ICU. Although it is normal for patients on a mechanical ventilator to lose the ability to speak, patients and their families did not understand how mechanical ventilators work and were frustrated that they could not communicate freely with the patient. Participants expressed difficulty in communicating with patients in ways other than verbal communication as well.
“Patients who are on mechanical ventilation can’t talk as they want and do not have enough strength in their hands to write correctly; so, even if I try to listen to them, I just can’t understand what they are saying. You know in that game where people wear headphones playing loud music and try to communicate with one another—words completely deviant from the original word are conveyed. It just feels like that.” (Participant 9)
“Patients on mechanical ventilation and who thus cannot communicate are the most difficult. The patient keeps talking; so, it hinders respiration—the ventilator alarm keeps going off, the stomach becomes gassy, and the patient has to take the tube off and vomit later. No matter how much I explain, there are patients or caregivers who tell me that the tube in the throat is making [it] hard [for them] to breathe or [they] ask me to take it off just once and put it back on, and these patients are really difficult. There is no way to communicate if they cannot accept mechanical ventilators even if I explain.” (Participant 8)
Patient- and family-related factor: Caregivers’ negative responses to nurses
It was also burdensome for nurses to communicate with extremely stressed caregivers and loved ones, especially when patients were in a critical state. Despite the role of nurses in helping patients during health recovery, caregivers’ negative responses to nurses, such as blaming them and speaking and behaving aggressively, intimidated the participants and ultimately discouraged conversations.
“I can manage the patients’ poor vital signs by working hard but communicating with sensitive caregivers who project their anxiety about the patient’s state onto nurses doesn’t go as I wish, so, it’s really difficult and burdensome.” (Participant 6)
“When the patient is in a bad state, caregivers sometimes want to not accept it and project their feelings onto the nurses, and in such cases, there are no words that can console them. Even approaching the caregivers is a burden, and I get kind of intimidated.” (Participant 5)
System-related factor: Lack of experience and a mismatch between theory and practice
Participants have learned the importance of communication during training; however, they had trouble appropriately applying the learned concepts in their workplace. Participants in this study were in their 20s and 30s, with limited life and social experiences, and felt the gap between theory and practice in communicating with patients and families in ICU.
“Talking to the patient or caregiver was the most challenging thing when I was new…it is impossible for nurses with not much life experience to communicate skillfully.” (Participant 10)
“It would be nice if the real-world conversation proceeds in the way shown in our textbook; but it doesn’t in most cases. So, it is more practical to observe and learn from what other nurses do in the actual field.” (Participant 2)
System-related factor: Intense visiting hours in limited time
The 30-minute ICU visiting period is the only time when patients and families can talk to one another. Although nurses are well trained to care for the patients to the best of their ability, caregivers distrust the nurses’ ability to care for patients since caregivers only have a limited amount of visiting time, thus hindering effective communication. Some participants even experienced mental trauma following short but unforgettable interactions with caregivers.
“…the caregiver browbeat me and intimidated me for doing so. This gave me a mental trauma for visiting hours…I didn’t know how to start a conversation and the visiting hours were really stressful for me.” (Participant 3)
“The caregivers don’t stay in the ICU for 24 hours; so, once they begin to doubt our nursing practice, we cannot continue our conversation with them…” (Participant 11)
System-related factor: Urgent workplace that deprioritizes communication
The ICU is a unit for treating critically-ill patients; therefore, ICU nurses were more focused on tasks directly linked to maintaining patients’ health, such as stabilizing vital signs, than on communication. Participants frequently encountered emergency situations, in which they could not idly stay around to communicate with one patient because another required immediate assistance, i.e., they faced a reality in which they had to prioritize another patients’ health over communication with one.
“…I’m really pressed for time when the patient keeps writing things I can’t understand with their weak hands…I don’t have time to spare even if I want to listen to them.” (Participant 12)
“Vital signs are the utmost priority in [the] ICU. I’m on my feet the entire shift and don’t even have time to go to the restroom…During early ICU treatment, there are a lot of emergency situations; so, communication is way down in the priority list.” (Participant 5)
Theme 2: Learning through trial and error
The negative experiences arising from communicating with various individuals sometimes forced nurses to think twice about their vocation; however, due to a sense of responsibility, they tried to engage in therapeutic communication and to overcome difficulties.
Fundamental doubts about the nursing profession
Experiencing unfriendly and confrontational conversations with patients and caregivers was intolerable for participants. These experiences were shocking enough to make them fundamentally question their decision to choose and stay in the nursing profession.
“I felt so disappointed and frustrated when patients or caregivers bombard[ed] rude comments at me with complete disregard of what I have done over a long period…I can’t sleep well at night and my values as [a] nurse are shaken from their root.” (Participant 14)
“It becomes so difficult the moment communication fails and mutual trust is lost. Maybe I could survive if this is just with one patient or caregiver; but the afterimage lingers with me persistently while I’m working…I came to think whether I could continue nursing.” (Participant 7)
Finding out which communication style is better suited for patients and their families
Nurses learned how to resolve communication-related difficulties that they encountered from their seniors and mentors and tried to communicate better from their position at the nursing station.
“A senior nurse of mine was talking to a caregiver who was really concerned, and she was using affirmations like ‘Oh, really’ and ‘I see’ with a relaxed facial expression, and the caregiver would spill her heart out to her. That’s when I thought that empathy is to express responses to what the other person is saying.” (Participant 10)
“I can feel that I am able to bond with patients’ families when I tell them about the patient’s daily living, such as how much the patient had slept, eaten, and whether the patient was not in pain, during visiting hours.” (Participant 13)
Knowhow learned through persistent effort
Nursing activities, such as taking vital signs and performing aspiration and intravenous injection, are learned over time; however, it is impossible to acquire therapeutic communication skills without personal effort and interactive experiences in the field.
“I’m reading a book about conversation and am learning about how to express empathy and understand other people…Nursing skills are developed and improved over time; but it’s not easy to enhance communication without personal effort or change in perception.” (Participant 16)
“Communication is an indispensable part of nursing. If you want to provide high-quality care, you need to enhance your communication skills first.” (Participant 15)
Theme 3: Recognizing communication experiences as being essential for care
Nursing and communication are inseparable. Although communication is a challenge while caring for ICU patients, therapeutic communication is important for the patients’ and their families’ overall wellbeing. In an ICU, communication based on empathy and experience is a significant component that helps patients perceive their illnesses more positively.
Empathy garnered through various clinical experiences
Since participants met many patients and their families in the ICU, they were able to communicate. Participants understood patients’ discomfort and learn why it was difficult for them to communicate and to comfort and assure unease families who could not observe the patient's condition. However, it was a necessary communication method in the ICU. Participants realized the value and importance of their words.
“…his endotracheal tube was touching his throat and was so uncomfortable: his mouth was dry, he couldn’t talk, and his arms were tied; so, he thought the only way to communicate was to use his legs and that’s why he was kicking. I felt really sorry…” (Participant 7)
“I gave a little detailed explanation to the caregiver during visiting hours and she thanked me overwhelmingly. I feel that, because this is the ICU, patients and caregivers can be encouraged and discouraged by the words of the medical professionals.” (Participant 9)
The power of active listening
Although the ability to handle tasks promptly is important, listening to patients amid the hectic work schedule in the ICU is also an important nursing skill. Critical care nurses realized that listening to patients and caregivers without saying anything is also meaningful and therapeutic.
“I was listening to the caregiver the entire duration of the visiting hour…She said that she just had to open up to someone to talk about her frustrations, and that my listening to her was a huge consolation for her.” (Participant 12)
“While listening to the caregiver and showing empathy every day at the same time, I was able to witness that the caregiver who had been aggressive and edgy changed in a way to trust in and depend on the nurse more.” (Participant 16)
Mediator between physicians, patients, and caregivers
Participants were at the center of communication, serving as the bridge connecting physicians to patients and patients to caregivers. They served as mediators, explaining the doctors’ comments to the caregivers, and providing details regarding the patients’ state to families. Participants helped maintain a close and balanced relationship between the doctor, the patients, and their families by conveying messages not effectively communicated by the doctor or patients.
“Caregivers would not ask any questions to the doctor in the ICU and would ask me instead once the doctor is gone. They would ask, ‘what did the doctor say?’ and ask me for an explanation.” (Participant 4)
“The patients can’t say everything they want; so, as nurses, we are the mediators between patients and caregivers…Tell[ing] the family about things that happened when they were not around the patient is meaningful.” (Participant 14)
Expressing warmth and respect
Participants have experienced sharing emotions with the patient's family as well as with the patient during disease improvement and exacerbation.
In particular, sincere actions, such as staying with the families of patients who died or those whose condition was deteriorating, led to more genuine relationships, as respect for human life was expressed.
“When patients whom we have spent a long time [with] are about to pass away, we cry for them and we stay beside them in their final moments…Showing respect for a person’s final moments of life and expressing our hearts is meaningful, and it is something critical care nurses must do.” (Participant 16)
“When the patient’s state worsened and…his daughter was sobbing next to him…I softly touched her shoulder, and she really thanked me. As I saw the patient’s family grieve, I just expressed how I felt, and, fortunately, my intention was well conveyed” (Participant 4)
This study evaluated critical care nurses’ communication skills and experiences with patients and their caregivers. Based on the two FGIs and four individual in-depth interviews, three themes have been identified: 1) facing unexpected communication difficulties; 2) learning through trial and error; and 3) recognizing communication experiences as being essential for care
For theme 1, we examined nurse-, patient-, family-, and system-related (i.e., pertaining to hospital resources and education) factors. Theme 1 can be considered as the communication involving human-to-human interaction, as mentioned in Travelbee [ 24 , 25 ], that takes place at an incomplete stage. First, critical care nurses struggled with balancing their heavy workload and communicating with patients and their families. In Korea, an ICU nurse, on an average, cares for two to four patients, which is higher than in some other countries, wherein an ICU nurse cares for one or two patients at the most; thus, the Korean work environment for ICU nurses is more stressful [ 26 ]. This limits the amount of time nurses may have to communicate and interact with their patients and caregivers. Misunderstandings are also common owing to the patients’ inability to speak while intubated and to use of regional dialects. Patients and caregivers want to hear specific and comprehensible information from health professionals regarding the treatment procedures in the ICU [ 17 , 27 ]. However, previous studies [ 4 , 28 ] have reported that critical care nurses experience communication difficulties due to high mental pressure due to work, time constraints, and the inability to use their own language; these are consistent with our findings. As nurses are required to interact with patients having various needs, they need to learn how to communicate verbally and nonverbally in a sophisticated manner [ 27 ], and hospital managers should implement practical communication programs in the ICU.
Communication between nurses and their patients in the ICU is also often adversely affected by the therapeutic environment, such as patient emergencies and the use of mechanical ventilation [ 27 , 28 ]. Mechanical ventilators are one of the greatest obstacles to communication. Although they are essential for critically-ill patients who are incapable of spontaneous breathing, they affect their ability to speak [ 29 ]; therefore, these patients need to employ other strategies for communication, such as using facial expressions and lip movements, which make communication extremely difficult [ 27 , 30 ]. Our participants strived to understand the needs of critically-ill patients through verbal and nonverbal communication, such as writing and body language. However, when the intentions were not conveyed properly, some patients responded aggressively, hindering respiratory treatment and ultimately prolonging treatment. This is in line with many previous findings [ 29 , 31 , 32 ] indicating that patients’ failure to effectively express their needs to nurses or their family members triggers negative emotions. In addition, participants had trouble interacting with caregivers who were extremely tense and sensitive. According to Lee and Yi [ 17 ], families of critically-ill patients experience fear and anxiety regarding the patients’ health state and strive to save the patient. Thus, nurses must consider this when addressing vulnerable patients and their families and must actively identify and resolve causes of discomfort in patients on mechanical ventilation (i.e., by using appropriate analgesics/sedatives and removing the ventilator). Further, considering a systematic review revealing that electronic communication devices enable efficient communication with critically-ill patients through touch or eye blinks [ 33 ], Korea should also keep abreast with technological advances in communication technology.
Concerning theme 2, as participants experienced emotional exhaustion from being misunderstood or unfairly criticized by patients and their families, they contemplated and doubted the occupational values of nursing. Park and Lee [ 7 ] found that higher job satisfaction for ICU nurses is associated with better communication. This is consistent with our participants’ doubt for choosing the nursing profession. However, instead of giving up on this profession, they closely observed the effective communication skills of more experienced nurses, actively learned about therapeutic communication through books and videos, and applied their learnings during practice. Similar results were reported by Park and Oh [ 3 ] that patient-centered communication competency among critical care nurses was the highest when a biopsychosocial perspective, focused on delivery of factual information, was followed and the lowest in the therapeutic alliance domain, which is required for performing cooperative care with patients. Therapeutic communication provided by nurses to patients and their families in the ICU effectively diminished their psychological burden and fostered positive responses from families [ 34 ]. Currently, ICUs implement a systematic education system for nurses that focuses on therapeutic techniques, such as hemodynamic monitoring, mechanical ventilation care, aspiration, and extracorporeal membrane oxygenation; however, they lack a program targeting effective therapeutic communication with patients and caregivers. The communication difficulties experienced by nurses will persist without this additional program; thus, its implementation is critical to improve patient satisfaction and nursing quality of care. Further, instead of coercing unilateral effort from critical care nurses, nurse managers should pay attention to nurses’ emotional wellbeing and promptly develop systems to offset potential burnout, such as voluntary counseling systems or measures to “refresh” nurses.
Concerning theme 3, participants learned that communication is a challenging but essential aspect of critical care. The concept of communication resonates through Travelbee’s model [ 24 , 25 ]. Getting to know another human being is as important as performing procedures. A nurse must establish a rapport with the patient and the patient’s caregivers, otherwise he or she will not know the patient’s needs. As a place where life-and-death decisions are made, the ICU induces anxiety in critically-ill patients and their caregivers. Hence, nurses should fully empathize with patients and their caregivers [ 4 , 5 , 17 ].
Travelbee [ 24 , 25 ] emphasized the relationship between the nurse and the patient by establishing the Human-to-Human relationship model, which gives meaning to disease and suffering based on empathy, compassion, and rapport building. In addition, it presents concepts, such as disease, hope, human-to-human relations, communication, interaction, patient’s needs, perception, pain, finding meaning, therapeutic use of communication, and self-actualization. The participants cultivated empathy and active listening skills when speaking with patients and their families, and, as they spend more time doing so, their quality of care and nonverbal communication skills (such as eye contact, soft touch, and tears) improve and became more genuine. Our findings are consistent with the meaning of human-centered care suggested by Jang and Kim [ 35 ], which involves paying close attention to and protecting patients’ lives, deeply empathizing with patients from a humanistic perspective, and being sincere. The experience of nursing, including active interaction, has a positive impact on establishing the roles and caring attitudes of professional nurses [ 36 ], which is significant for critical care nurses. Patient-family-centered care, which has been confirmed to positively promote critically-ill patients’ recovery worldwide [ 1 ], is possible when nurses engage in therapeutic communication with patients and their families through dynamic interactions [ 34 , 37 ]. Therefore, critical care nurses and nurse managers should pay attention to communication and develop an effective communication course that can be applied in clinical practice. To do this, first, it is necessary to hire appropriate nursing personnel for active therapeutic communication with the patients and their families in an ICU. Second, continuous, and diverse educational opportunities should be provided to critical care nurses, along with policy strategies. For example, at the organizational level, it is necessary to develop manuals on how to deal with difficult situations by gathering challenging communication cases from actual clinical practice. Simulation education for communication is an important component of the nursing curriculum.

Limitations
First, this study included a small number of participants; however, we ensured that the maximum data was collected from these participants. Second, specific information was collected from only those nurses who provided direct care in the ICU of a general hospital in a large city in Korea. The homogeneity and dynamics of the focus groups may have resulted in congruent opinions. Third, because the experiences of nurses from only one hospital were analyzed, caution should be exercised in generalizing our results and applying them to other hospitals in Korea. Therefore, follow-up studies with larger sample sizes and more representative participants are warranted.
This qualitative study explored critical care nurses’ communication skills and experiences with patients and caregivers from various perspectives. Although these nurses felt discouraged by the unexpected communication difficulties with patients and their families, they recognized that they could address these difficulties by improving their communication skills over time through experience and learning. They realized that empathy, active listening, and physical interaction with patients and their families enabled meaningful communication and have gradually learned that effective communication is an indispensable tool in providing nursing care to critically-ill patients.
Supporting information
Acknowledgments.
The authors would like to thank all the participants for their time and contribution in this study.
Funding Statement
This work was supported by the Dongguk University Nursing Academy-Industry Cooperation Research Fund of 2018.The funder had no role in study design, data collectionand analysis, decision to publish, or preparation of the manuscript
Data Availability
LOGIN
Annual Report
- Board of Directors
- Nomination Process
- Organizational Structure
- ATS Policies
- ATS Website
- MyATS Tutorial
- ATS Experts
- Press Releases
Member Newsletters
- ATS in the News
- ATS Conference News
- Embargo Policy
ATS Social Media
Breathe easy podcasts, ethics & coi, health equity, industry resources.
- Value of Collaboration
- Corporate Members
- Advertising Opportunities
- Clinical Trials
- Financial Disclosure
In Memoriam
Global health.
- International Trainee Scholarships (ITS)
- MECOR Program
- Forum of International Respiratory Societies (FIRS)
- 2019 Latin American Critical Care Conference
Peer Organizations
Careers at ats, affordable care act, ats comments and testimony, forum of international respiratory societies, tobacco control, tuberculosis, washington letter.
- Clinical Resources
- ATS Quick Hits
- Asthma Center
Best of ATS Video Lecture Series
- Coronavirus
- Critical Care
- Disaster Related Resources
- Disease Related Resources
- Resources for Patients
- Resources for Practices
- Vaccine Resource Center
- Career Development
- Resident & Medical Students
- Junior Faculty
- Training Program Directors
- ATS Reading List
- ATS Scholarships
- ATS Virtual Network
ATS Podcasts
- ATS Webinars
- Professional Accreditation
Pulmonary Function Testing (PFT)
- Calendar of Events
Patient Resources
- Asthma Today
- Breathing in America
- Fact Sheets: A-Z
- Fact Sheets: Topic Specific
- Patient Videos
- Other Patient Resources
Lung Disease Week
Public advisory roundtable.
- PAR Publications
- PAR at the ATS Conference
Assemblies & Sections
- Abstract Scholarships
- ATS Mentoring Programs
- ATS Official Documents
- ATS Interest Groups
- Genetics and Genomics
- Medical Education
- Terrorism and Inhalation Disasters
- Allergy, Immunology & Inflammation
- Behavioral Science and Health Services Research
- Clinical Problems
- Environmental, Occupational & Population Health
- Pulmonary Circulation
- Pulmonary Infections and Tuberculosis
- Pulmonary Rehabilitation
- Respiratory Cell & Molecular Biology
- Respiratory Structure & Function
- Sleep & Respiratory Neurobiology
- Thoracic Oncology
- Joint ATS/CHEST Clinical Practice Committee
- Clinicians Advisory
- Council of Chapter Representatives
- Documents Development and Implementation
- Drug/Device Discovery and Development
- Environmental Health Policy
- Ethics and Conflict of Interest
- Health Equity and Diversity Committee
- Health Policy
- International Conference Committee
- International Health
- Members In Transition and Training
- View more...
- Membership Benefits
- Categories & Fees
- Special Membership Programs
- Renew Your Membership
- Update Your Profile
- ATS DocMatter Community
- Respiratory Medicine Book Series
- Elizabeth A. Rich, MD Award
- Member Directory
- ATS Career Center
- Welcome Trainees
- ATS Wellness
- Thoracic Society Chapters
- Chapter Publications
- CME Sponsorship
Corporate Membership
Clinical cases, professionals.
- Respiratory Health Awards
- Clinicians Chat
- Ethics and COI
- Pulmonary Function Testing
- ATS Resources
- Live from the CCD
- Pediatric Division Directors

Massive Pulmonary Embolism
Claire L. Keating, M.D.
Jennifer A. Cunningham, M.D.
Columbia University College of Physicians and Surgeons
HISTORY: 55-year-old female nursing home resident with past medical history of AIDS, dilated cardiomyopathy (estimated left ventricular ejection fraction 15% on a previous transthoracic echocardiogram), and prior deep venous thrombosis (DVT) was found to be hypotensive and in respiratory distress while at her skilled nursing facility.
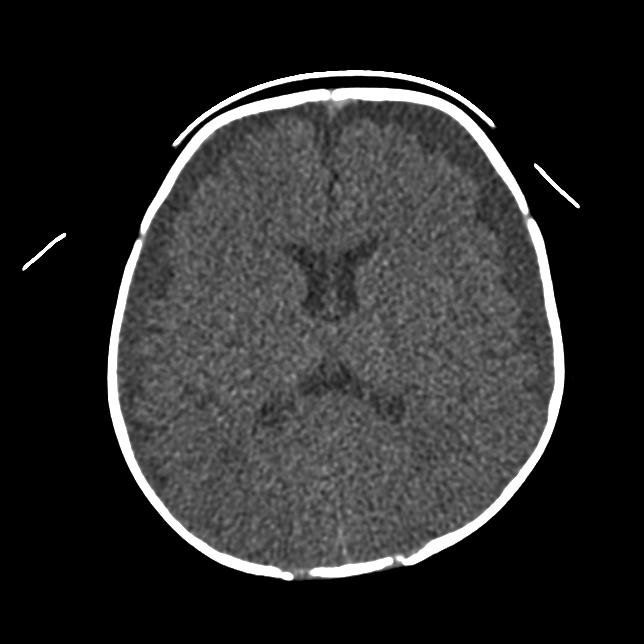
She was brought to the emergency department, where vital signs were notable for temperature of 100.9ºF, HR=142/min, BP=90/60 mmHg after intravenous fluids, with oxygen saturation of 99% while breathing 100% oxygen via non-rebreather mask. Computed tomography of the chest with pulmonary angiogram protocol (Figure 1) revealed large, thrombi in the right main and left main pulmonary arteries with incomplete occlusion, in addition to multiple segmental thrombi in right upper, middle and lower lobes. No lower extremity deep vein thromboses were noted on venogram. Anticoagulation was initiated and the patient was transferred to the intensive care unit (ICU) for further management.
FIGURE 1: CT scan of the chest demonstrating pulmonary emboli in bilateral main pulmonary artery

What distinguishes massive from submassive pulmonary embolism?
- the presence of hypoxemia
- the presence of right ventricular dysfunction
- the presence of shock
- the presence of pulmonary hypertension
- the presence of concurrent deep venous thrombosis
Answer to Question 1
Correct answer: C
The main criteria defining a massive pulmonary embolism are signs of hemodynamic compromise [1]. These include:
-Arterial hypotension defined as systolic arterial blood pressure <90mmHg or a drop in systolic arterial blood pressure of at least 40mmHg for at least 15 minutes (mortality 15%) -Cardiogenic shock as manifested by tissue hypoperfusion and hypoxia, altered level of consciousness, oliguria, or cool, clammy extremities (mortality 25%) -Circulatory collapse requiring cardiopulmonary resuscitation (mortality 65%)
Patients with submassive pulmonary emboli are normotensive with signs of right ventricular dysfunction present (see below).
PAST MEDICAL HISTORY: AIDS (CD4+ cell count=20/mm3) Multiple cerebrovascular infarcts with residual expressive aphasia and hemiparesis Dilated cardiomyopathy (presumed HIV-related) Hypertension Chronic kidney disease with baseline serum creatinine of 1.5 mg/dL Past DVT (not on anticoagulation for unclear reasons)
MEDICATIONS: Clopidogrel ASA Enalapril Furosemide Levetiracetam Abacavir Lamivudine Zidovudine Efavirenz
PHYSICAL EXAM: Upon admission to ICU Vitals: T=100.1ºF, HR=112/min, BP=91/63 mmHg, RR=28/min, SpO2=96% on 100% oxygen via nonrebreather mask General: awake, nonverbal, dyspneic and diaphoretic HEENT: Eyes deviated left, pupils 3mm and reactive, JVP estimated at 8cm H2O Heart: tachycardic, regular with frequent ectopy, grade 3/6 holosystolic murmur and S3 gallop present, point of maximal impulse displaced laterally Lungs: coarse breath sounds bilaterally Abdomen: soft, nontender, hypoactive bowel sounds, pulsatile liver, brown guaiac negative stool Extremities: right upper extremity with decreased tone, 1+ edema in lower extremities bilaterally, all extremities cool to touch Neurologic: withdrawal to pain in all extremities, spontaneous eye opening, non-attentive, nonverbal and not following commands.
ADMISSION LABORATORY VALUES: White blood count 14,600/mm3 Hemoglobin 10.6 g/dL Platelets 125,000/ mm3
Sodium 134 mmol/L Potassium 4.6 mmol/L Chloride 107 mmol/L Bicarbonate 13 mmol/L Blood urea nitrogen 45 mg/dL Creatinine 2.8 mg/dL (baseline 1.5) Serum glucose 102 mg/dL Troponin 2.7 ng/mL (upper limit normal = 0.08) BNP 1,944 pg/mL (upper limit normal = 100-400)
Arterial Blood Gases: Emergency Room (on 100% oxygen via non-rebreather mask): pH=7.32 PaCO2=25 mmHg PaO2=250 mmHg
ICU (prior to intubation, on 100% oxygen via non-rebreather mask): pH=7.04 PaCO2=38 mmHg PaO2=71 mmHg
What echocardiogram findings are seen in submassive and massive pulmonary embolism?
- right ventricular dilation
- right ventricular hypokinesis with sparing of the right ventricular apex (McConnell sign)
- loss of inspiratory collapse on inferior vena cava
- paradoxical septal wall motion
- all of the above
Answer to Question 2
Correct answer: E
Doppler echocardiogram can be useful in supporting the diagnosis of submassive and massive pulmonary embolism, especially in the cases where a contrast chest CT cannot be performed immediately. Findings on Doppler echocardiogram demonstrate acute right ventricular pressure overload in the absence of left ventricular or mitral valve disease with or without increased pulmonary artery pressures. These findings typically occur only after >30% of the pulmonary vascular cross-sectional area is impaired and include [2]:
- right ventricular dilatation (larger than the left ventricle from the apical or subcostal view) and hypertrophy (about 6 mm; normal <4mm)
- right pulmonary artery dilatation
- paradoxical septal wall motion (interventricular septum bulges towards the left ventricle)
- loss of inspiratory collapse of inferior vena cava
- elevated pulmonary artery systolic pressure as estimated by the gradient across the tricuspid valve
- small difference in LV area during diastole and systole (low cardiac output)
- patent foramen ovale
What is the preferred hemodynamic support for hypotension in massive pulmonary embolism?
- intravenous fluids
- norepinephrine
- inotropic agents, such as isoproteronol
- vasopressin
- intra-aortic balloon counter-pulsation device (IABP)
Answer to Question 3
Correct answer: B
Norepinephrine is the preferred agent for hemodynamic support in massive pulmonary embolism with hypotension. This is based on several studies using canine models of pulmonary embolism [4-6], where isoproterenol or norepinephrine were administered for hemodynamic support in acute pulmonary embolism. Success in achieving hemodynamic stability and improvement in ventricular wall function was higher in dogs receiving infusions of norepinephrine. The effect is hypothesized to be due to increased systemic pressures, resulting in improved coronary perfusion and improved right ventricular function. In patients with less severe hypotension and more severe cardiac dysfunction, inotropic agents may be considered as an adjunct or alternative to norepinephrine [6-11]. Newer inotropic agents, such as amrinone, which act as both inotropic agent and pulmonary vasodilator have shown promise in animal studies and case reports [12,13].
A number of detrimental effects of intravenous fluids have been documented in animal studies, including decreased cardiac output and diminished right coronary artery blood flow due to increased right ventricular dilation [4-9]. In the face of diminished right coronary artery flow, worsening right ventricular ischemia can lead to diminished RV systolic function, establishing a vicious cycle of auto-aggravation. One study in humans [14], however, suggested that a 500 ml fluid load may initially improve cardiac output among patients with massive PE, although the long-term effects of fluid administration on cardiac function and hemodynamics are unclear. Most authors would agree that intravenous fluids must be used with caution in patients with massive PE [15-17].
HOSPITAL COURSE After admission to the ICU, the patient received an intravenous infusion of unfractionated heparin drip and an intravenous infusion of norepinephrine at 5 micrograms/minute for hemodynamic support. A Foley catheter was placed with urine output remaining <0.5 mL/kg/hour despite a trial of intravenous fluid resuscitation. Bedside transthoracic echocardiogram was performed and demonstrated a dilated left ventricle with depressed systolic function with an estimated left ventricular ejection fraction of 15% (unchanged from baseline echo), in addition to a new finding of moderate right ventricular and right atrial dilatation with a calculated RV systolic pressure of 58mmHg (increased RV dysfunction from the prior study). There was moderate tricuspid regurgitation and a dilated inferior vena cava noted. Consideration was given to systemic thrombolysis due to the presence of persistent hypotension and end organ dysfunction, however, with a therapeutic partial thromboplastin time (PTT) on heparin, massive hemoptysis (>250 cc with >2g/dL hemoglobin drop) developed. The trachea was urgently intubated and heparin was discontinued. Interventional radiology was consulted for catheter thrombectomy and inferior vena caval (IVC) filter placement.
In cases of massive pulmonary embolism, what options remain when systemic thrombolysis cannot be performed safely?
- surgical embolectomy
- catheter-directed thrombolysis
- percutaneous embolectomy
- percutaneous thrombus fragmentation
Answer to Question 4
Correct answer: E
Surgical embolectomy: Surgical embolectomy involves transection of the main pulmonary artery via sternotomy incision with manual extraction of thromboembolism. Although in the past, peri-operative mortality was a high as 57%, some experienced centers now report peri-operative mortality of approximately 6% [33]. However, with the use of cardiopulmonary bypass and increasing surgical expertise, mortality and morbidity from surgical embolectomy can be minimized,[18,19] and may offer benefit particularly to those patients with evidence of pulmonary hypertension [18].
Historically, surgical embolectomy was the only available option for patients who fail or who have contraindications to systemic thrombolysis. It is not clear what role it will play in the future given the advent of other interventional options (listed below).
Catheter-directed thrombolysis: This technique requires placement of an intra-arterial catheter to the site of the embolus with bolus and infusion of a thrombolytic agent [20]. Catheter-directed thrombolysis usually requires concurrent intravenous unfractionated heparin administration.
Small studies, including case series and controlled trials, have evaluated the efficacy of intrapulmonary thrombolysis [21-23]. Although clinical endpoints such as mortality were not evaluated, these studies suggest equivalent or superior radiographic resolution of thrombolysis compared to systemic thrombolysis. Bleeding complication rates were low following intrapulmonary thrombolysis, suggesting that catheter-directed thrombolysis may be possible even in patients who have contraindications to systemic thrombolysis [29]. It is noteworthy, however, that these regimens also utilized systemic anticoagulation. Therefore, caution must be exercised in extrapolating the results of these small studies to patients with contraindications to systemic thrombolysis or anticoagulation. Further investigation into the safety of this technique in high risk patient populations is needed.
Percutaneous aspiration thrombectomy or fragmentation: When systemic or intrapulmonary thrombolysis and surgical embolectomy are not possible, there are a number of interventional options available that aim to rapidly relieve central obstruction and restore hemodynamic stability [20].
Greenfield embolectomy catheter [20] : This catheter (Boston Scientific/Meditech; Watertown, MA) is inserted into the site of the thrombus, and with manual suction using a large syringe retrieves the clot, which is then removed en bloc through the venotomy site or vascular sheath.
Rotatable pigtail catheter [20] : The pigtail tip of this catheter (Cook Europe; Bjaeverskov, Denmark) is rotated either by hand or by an attachable low-speed electric catheter to disrupt the intrapulmonary clot into smaller fragments which then migrate into the distal pulmonary circulation. The catheter can be advanced into peripheral pulmonary branches and manually rotated to further clot fragmentation.
Rheolytic thrombectomy catheters [20] : The Angiojet system (Possis; Minneapolis, MN) uses the Venturi effect to perform thrombectomy. This is a double lumen catheter, of which the inner smaller catheter directs a high-velocity stream of saline. The high-pressure generated by the smaller lumen catheter creates a low pressure state in the larger catheter resulting in a vortex and promotion of fragmentation and aspiration of the thrombus.
What are the most recent American College of Chest Physicians (ACCP) guidelines on placement of IVC filters in pulmonary embolism?
- routine use of retrievable IVC filter in patients with PE
- use of IVC filter among patients with a contraindication to anticoagulation
- use of IVC filter among patients with recurrent PE despite adequate anticoagulation
Answer to Question 5
Correct answer: D
The official recommendation from the 7th ACCP conference on Antithrombotic and Thrombolytic Therapy [30] is as follows: “In pulmonary embolism patients with a contraindication for, or a complication of anticoagulant therapy as well in those with recurrent thromboembolism despite adequate anticoagulation, we suggest placement of an IVC filter.”
Although this received only a Grade 2C recommendation (with low or very low evidence), there is general consensus within the pulmonary community that a patient at high risk for death due to recurrent pulmonary embolism may also benefit from placement of an IVC filter. This is based on a clinical trial of 400 patients with known deep vein thrombosis (with or without concomitant pulmonary embolism) randomized to IVC filter placement or anticoagulation alone. Concurrent placement of an IVC filter lowered the rate of new pulmonary embolism at day 12. There was no difference in PE rates at 2 years, although there was a higher incidence of DVT in the IVC filter group [31]. Although there was no difference in short-term mortality observed, patients with massive PE were not included in this study. Therefore, the use of a retrievable IVC filter [32] is a reasonable option among patients with severe hemodynamic compromise due to PE to prevent a recurrent catastrophic thromboembolism.
The patient required mechanically-assisted ventilation with a fraction of inspired oxygen (FiO2) of 0.6 and positive end-expiratory pressure (PEEP) of 10 cmH20 to maintain the arterial oxygen saturation >90%. Due to persistent hypotension after a trial of fluid resuscitation, norepinephrine was continued. A trial infusion of dobutamine was limited by prolonged runs of non-sustained ventricular tachycardia (NSVT). The patient’s urine output remained minimal. Interventional radiology placed an IVC filter but declined to perform a catheter thrombectomy due to the patient’s baseline depressed cardiac function.
Norepinephrine was discontinued by ICU day 6 and the patient’s oxygenation slowly improved, and mechanical ventilation was successfully discontinued on ICU day 8. Renal function improved without need for dialysis. Heparin was reintroduced before patient was discharged from the ICU without recurrence of hemoptysis. The patient recovered to her baseline status and was discharged on hospital day 39.
REFERENCES:
1. Kucher N and Goldhaber SZ. Management of massive pulmonary embolism. Circulation 2005; 112: e28-e32.
2. Goldhaber SZ. Echocardiography in the management of pulmonary embolism. Ann Intern Med 2002; 136: 691–700.
3. Kasper W et al . Distinguishing between acute and subacute massive pulmonary embolism by conventional and Doppler echocardiography. Br. Heart J . 1993; 70: 352-6.
4. Molloy WD et al. Treatment of shock in a canine model of pulmonary embolism. Am Rev Respir Dis 1984; 130: 870-4.
5. Rosenberg JC et al. Isoproterenol and norepinephrine therapy for pulmonary embolism shock. J Thorac Cardiovasc Surg 1971; 62: 144-58.
6. Imamoto et al. Treatment of canine acute pulmonary embolic shock – effects of isoproterenol and norepinephrine on hemodynamics and ventricular wall motion. Jpn Circ J 1990; 54: 1246-57.
7. Manier G and Castaing Y. Influence of cardiac output on oxygen exchange in acute pulmonary embolism. Am Rev Respir Dis 1992; 145: 130-6.
8. Ducas J et al. Pulmonary vascular pressure-flow characteristics. Effects of dopamine before and after pulmonary embolism. Am Rev Respir Dis 1992; 145: 307-12.
9. Ghigone M et al. Volume expansion versus norepinephrine in treatment of a low cardiac output complicating an acute increase in right ventricular afterload in dogs. Anesthesiology 1984; 60: 132-5.
10. Jardin F et al. Dobutamine: a hemodynamic evaluation in pulmonary embolism shock. Crit Care Med 1985; 13: 1009-12.
11. Prewitt RM. Hemodynamic management in pulmonary embolism and acute hypoxemic respiratory failure. Crit Care Med 1990; 18: S61-9.
12. Wolfe MW et al. Hemodynamic effects of amrinone in a canine model of massive pulmonary embolism. Chest 1992; 102: 274-8.
13. Spence TH et al. Pulmonary embolism: improvement in hemodynamic function with amrinone therapy. South Med J 1989; 82: 1267-8.
14. Mercat A et al. Hemodynamic effects of fluid loading in acute massive pulmonary embolism. Crit Care Med 1999; 11: 339-45.
15. Piazza G and Goldhaber SZ. The acutely decompensated right ventricle. Chest 2005; 128: 1836-52.
16. Mebazaa A et al. Acute right ventricular failure – from pathophysiology to new treatments. Intensive Care Med 2004; 30: 185-96.
17. Layish DT and Tapson VF. Pharmacologic hemodynamic support in massive pulmonary embolism. Chest 1997; 111: 218-24.
18. Jamieson SW et al. Experience and results of 150 pulmonary thromboendarterectomy operations over a 29 month period. J Thorac Cardiovasc Surg 1993; 106: 116-27.
19. Gulba DC et al. Medical compared with surgical treatment for massive pulmonary embolism. Lancet 1994; 114: 576-7.
20. Uflacker, R. Interventional Therapy for Pulmonary Embolism . J Vasc Interv Radiol. 2001; 12:147-164
21. Gonzalez-Juanatey J et al. Treatment of massive pulmonary thromboembolism with low intrapulmonary dosages of urokinase. Chest 1992; 102: 341-6.
22. Verstaete M et al. Intravenous and intrapulmonary recombinant tissue-type plasminogen activator in the treatment of acute massive pulmonary embolism. Circulation 1998; 77: 353-60.
23. McCotter CJ et al. Intrapulmonary artery infusion of urokinase for treatment of massive pulmonary embolism: a review of 26 patients with and without contraindications to systemic thrombolytic therapy. Clin Cardiol 1999; 22: 661-4.
24. Kucher, N. Catheter embolectomy for acute pulmonary embolism . Chest 2007; 132: 657-663.
25. Greenfield LJ et al. Long-term experience with transvenous catheter pulmonary embolectomy. J Vasc Surg 1993; 18: 450-8.
26. Murphy JM et al. Percutaneous catheter and guidewire fragmentation with local administration of recombinant tissue plasminogen activator as a treatment for massive pulmonary embolism. Eur Radiol 1999; 9: 959-64.
27. Stock KW et al. Massive pulmonary embolism: treatment with thrombus fragmentation and local fibrinolysis with recombinant human-tissue plasminogen activator. Cardiovasc Intervent Radiol 1997; 20: 364-8.
28. Schmitz-Rode T et al. Fragmentation of massive pulmonary embolism using a pigtail rotation catheter. Chest 1998; 114: 1427-36.
29. Cela MC et al. Nonsurgical pulmonary embolectomy. In : Cope C, ed. Current Techniques in Interventional Radiology. Philadelphia: Current Medicine, 1994; 12: 2-8.
30. Buller HR et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126(3 Suppl):401S-428S.
31. Decousus H. et al . A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. N Engl J Med. 1998; 338(7):409-15.
32. Mismetti P et al. A prospective long-term study of 220 patients with a retrievable vena cava filter for secondary prevention of venous thromboembolism. Chest 2007; 131: 223-9.
33. Leacche M et al. Modern surgical treatment of massive pulmonary embolism: results in 47 consecutive patients after rapid diagnosis and aggressive surgical approach. J Thorac Cardiovasc Surg 2005; 129:1018-23.

The American Thoracic Society improves global health by advancing research, patient care, and public health in pulmonary disease, critical illness, and sleep disorders. Founded in 1905 to combat TB, the ATS has grown to tackle asthma, COPD, lung cancer, sepsis, acute respiratory distress, and sleep apnea, among other diseases.
AMERICAN THORACIC SOCIETY 25 Broadway New York, NY 10004 United States of America Phone: +1 (212) 315-8600 Fax: +1 (212) 315-6498 Email: [email protected]
Privacy Statement | Term of Use | COI Conference Code of Conduct


Nursing Case Study Examples and Solutions
- Premium Academia
- August 17, 2023
- Nursing Essay Examples
NursingStudy.org is your ultimate resource for nursing case study examples and solutions. Whether you’re a nursing student, a seasoned nurse looking to enhance your skills, or a healthcare professional seeking in-depth case studies, our comprehensive collection has got you covered. Explore our extensive category of nursing case study examples and solutions to gain valuable insights, improve your critical thinking abilities, and enhance your overall clinical knowledge.
Comprehensive Nursing Case Studies
Discover a wide range of comprehensive nursing case study examples and solutions that cover various medical specialties and scenarios. These meticulously crafted case studies offer real-life patient scenarios, providing you with a deeper understanding of nursing practices and clinical decision-making processes. Each case study presents a unique set of challenges and opportunities for learning, making them an invaluable resource for nursing education and professional development.
- Nursing Case Study Analysis [10 Examples & How-To Guides] What is a case study analysis? A case study analysis is a detailed examination of a specific real-world situation or event. It is typically used in business or nursing school to help students learn how to analyze complex problems and make decisions based on limited information.
- State three nursing diagnoses using taxonomy of North American Nursing Diagnosis Association (NANDA) that are appropriate, formatted correctly, prioritized, and are based on the case study. NUR 403 Week 2 Individual Assignment Case Study comprises: Resources: The case study found on p. 131 in Nursing Theory and the Case Study Grid on the Materials page of the student website Complete the Case Study Grid. List five factors of patient history that demonstrates nursing needs.
- Neuro Case Study
- Endocrine Case Study
- Anxiety & Depression Case Study
- Ethical dilemma
- A Puerto Rican Woman With Comorbid Addiction
- Tina Jones Comprehensive SOAP Note
- Insomnia 31 year old Male
- Chest Pain Assessment
Pediatric Nursing Case Studies

In this section, delve into the world of pediatric nursing through our engaging and informative case studies. Gain valuable insights into caring for infants, children, and adolescents, as you explore the complexities of pediatric healthcare. Our pediatric nursing case studies highlight common pediatric conditions, ethical dilemmas, and evidence-based interventions, enabling you to enhance your pediatric nursing skills and deliver optimal care to young patients.
- Case on Pediatrics : Part 1& 2 Solutions
- Pediatric Infant Reflux : History and Physical – Assignment 1 Solution
- Otitis Media Pediatrics Toddler – NSG 5441 Reflection Assignment/Discussion – Solution
- Pediatric Patient With Strep – NSG 5441 Reflection Assignment/Discussion
- Pediatric Urinary Tract infections (UTI) -NSG 5441 Reflection Assignment/Discussion – Solution
- Week 3 discussion-Practical Application in critical care/pediatrics
- Cough Assessmen t
Mental Health Nursing Case Study Examples
Mental health nursing plays a crucial role in promoting emotional well-being and providing care for individuals with mental health conditions. Immerse yourself in our mental health nursing case studies, which encompass a wide range of psychiatric disorders, therapeutic approaches, and psychosocial interventions. These case studies offer a holistic view of mental health nursing, equipping you with the knowledge and skills to support individuals on their journey to recovery.
- Psychiatric Nursing: Roles and Importance in Providing Mental Health Care
- Mental Health Access and Gun Violence Prevention
- Fundamentals of neurotransmission as it relates to prescribing psychotropic medications for clients with acute and chronic mental health conditions – Unit 8 Discussion – Reflection
- Unit 7 Discussion- Complementary and Alternative Medicine in Mental Health Care – Solution
- Ethical and Legal Foundations of PMHNP Care Across the Lifespan Assignment – Analyze salient ethical and legal issues in psychiatric-mental health practice | Solution
- Pathways Mental Health Case Study – Review evaluation and management documentation for a patient and perform a crosswalk of codes – Solution
- Analyze salient ethical and legal issues in psychiatric-mental health practice
- SOAP notes for Mental Health Examples
- compare and contrast two mental health theories
- Environmental Factors and Health Promotion Presentation: Accident Prevention and Safety Promotion for Parents and Caregivers of Infants
Geriatric Nursing Case Studies
As the population ages, the demand for geriatric nursing expertise continues to rise. Our geriatric nursing case studies focus on the unique challenges faced by older adults, such as chronic illnesses, cognitive impairments, and end-of-life care. By exploring these case studies, you’ll develop a deeper understanding of geriatric nursing principles, evidence-based gerontological interventions, and strategies for promoting optimal health and well-being in older adults.
- M5 Assignment: Elderly Driver
- HE003: Delivery of Services – Emmanuel is 55-year-old man Case – With Solution The Extent of Evidence-Based Data for Proposed Interventions – Sample Assignment 1 Solution
- Planning Model for Population Health Management Veterans Diagnosed with Non cancerous chronic pain – Part 1 & 2 Solutions
- PHI 413 Case Study Fetal Abnormality Essay
- Insomnia Response and Insomnia
- Analysis of a Pertinent Healthcare Issue: Short Staffing
- Paraphrenia as a Side of the Schizophrenia – Week 4 Solution
- Module 6 Pharm Assignment: Special Populations
- Public Health Nursing Roles and Responsibilities in Disaster Response – Assignment 2 Solution
- Theory Guided Practice – Assignment 2 Solution
- How can healthcare facilities establish a culture of safety – Solution
- Discuss the types of consideration a nurse must be mindful of while performing a health assessment on a geriatric patient as compared to a middle-aged adult – Solution
- Promoting And Protecting Vulnerable Populations – Describe what is meant by vulnerable populations and explain strategies you, as the public health nurse, could use to best facilitate the achievement of healthful outcomes in this population?
Community Health Nursing Case Studies
Community health nursing plays a vital role in promoting health, preventing diseases, and advocating for underserved populations. Dive into our collection of community health nursing case studies, which explore diverse community settings, public health issues, and population-specific challenges. Through these case studies, you’ll gain insights into the role of community health nurses, interdisciplinary collaboration, health promotion strategies, and disease prevention initiatives.
- Community and Target Aggregate: Residents of the community health center, particularly those aged 65 and above Topic: Secondary Prevention/Screenings for a Vulnerable Population
- Tools For Community Health Nursing Practice2
- 5 Theories in Community Health Nursing: A Complete Guide
- Role of community health nursing and community partnerships as they apply to the participating family’s community – Assignment 1 Solution
- Community/Public Health Nursing DQ2
- CSU-Community healthcare Presentation – Assignment 1 Solution
- Community Healthcare Presentation – Domestic Violence And Level Of Prevention – Solution
Critical Care Nursing Case Study Examples
Critical care nursing demands swift decision-making, advanced technical skills, and the ability to provide intensive care to acutely ill patients. Our critical care nursing case studies encompass a range of high-acuity scenarios, including trauma, cardiac emergencies, and respiratory distress. These case studies simulate the fast-paced critical care environment, enabling you to sharpen your critical thinking skills, enhance your clinical judgment, and deliver exceptional care to critically ill patients.
- Nursing Case Study Parkinsons Disease
- Nursing Case Study: Patient with Drug and Alcohol Induced Paranoid Schizophrenia
- Neonatal Hypothermia and Neonatal Sepsis: Nursing Case Study
- Chronic Obstructive Pulmonary Disease Nursing Case Study
Maternal and Child Health Nursing Case Study Examples
The field of maternal and child health nursing requires specialized knowledge and skills to support the health and well-being of women and children throughout their lifespan. Explore our collection of maternal and child health nursing case studies, which encompass prenatal care, labor and delivery, postpartum care, and pediatric nursing. These case studies provide a comprehensive view of maternal and child health, allowing you to develop expertise in this essential area of nursing practice.
You can also check out Patient Safety in High-Tech Settings PICOT Questions Examples
Surgical Nursing Case Studies
Surgical nursing involves caring for patients before, during, and after surgical procedures. Our surgical nursing case studies cover a wide range of surgical specialties, including orthopedics, cardiovascular, and gastrointestinal surgeries. Delve into these case studies to gain insights into preoperative assessment, perioperative management, and postoperative care. By examining real-life surgical scenarios, you’ll develop a comprehensive understanding of surgical nursing principles and refine your skills in providing exceptional care to surgical patients.
- Discuss DI in relation to a postoperative neurosurgical patient – Week 2, 3, 4 Solution
- DISCUSSION WK 3
- Career Planning & Professional Identity Paper
- N ursing Case Analysis
- Ethical Dilemma on Robotic Surgery and ACS Codes of Ethics – Post 2
- NURS – 6521C Advanced Pharmacology
- Essay on Alterations in Neurological and Endocrine Functions
- Clinical Preparation Tool – Child and Adolescent Symptom Inventory – Unit
- Initial Psychiatric Interview/SOAP Note – Assignment 1 Solution
- Current Trends in Nursing Practice: Electronic Prescriptions for Opioids – Week 4 Solution
- Nurse-Sensitive Indicators -Week 3 Solution
- Theory–Practice Gap in Jean Watson Theory of Human Caring – Assignment 1 Solution
- Bowel Obstruction Case Video Presentation – Week 4 Solution
- Appendicitis SOAP Note – Sample SOAP Solution 1
- Week 4: GERD SOAP Note Assignment Solution
Obstetric Nursing Case Study
Obstetric nursing focuses on providing care to women during pregnancy, childbirth, and the postpartum period. Our obstetric nursing case studies explore various aspects of prenatal care, labor and delivery, and postpartum recovery. Gain valuable knowledge about common obstetric complications, evidence-based interventions, and strategies for promoting maternal and fetal well-being. These case studies will enhance your obstetric nursing skills and prepare you to deliver compassionate and competent care to expectant mothers.
- Capstone Proposal: Postpartum Hemorrhage Education To Nursing Students
- Progress Evaluation Telecommunication: Teleconference on Post-Partum Hemorrhage
- Case Study 5.2 the Moral and Ethical Questions of Aborting an Anencephalic Baby
- Holistic intervention plan design to improve the quality of outcomes – Problem Statement (PICOT)
- ADV HEALTH ASSESSMENT: TJ a 32-year-old pregnant lesbian, is being seen for an annual physical exam and has been having vaginal discharge – Solution
- Facilitative Communication and Helping Skills in Nursing & Decision Making Assignment Solution
- Benchmark – Evidence-Based Practice Proposal Paper Example
- Three nursing diagnoses for this client based on the health history and screening (one actual nursing diagnosis, one wellness nursing diagnosis, and one “risk for” nursing diagnosis)
- Identify two or more issues with the existing system
- Differences between inpatient and outpatient coding
Nursing Ethics Case Study
Ethical dilemmas are an inherent part of nursing practice. Our nursing ethics case studies shed light on complex ethical issues that nurses encounter in their daily work. Explore thought-provoking scenarios involving patient autonomy, confidentiality, end-of-life decisions, and resource allocation. By examining these case studies, you’ll develop a deeper understanding of ethical principles, ethical decision-making frameworks, and strategies for navigating ethical challenges in nursing practice.
- Ethics in Complementary Therapies
- Ethics Case Study Analysis
- Ethics in Practice
- Ethical Dilemma on Robotic Surgery and ACS Codes of Ethics – Post 1
- Case Study on Biomedical Ethics in the Christian Narrative
- Academic Success and Professional Development Plan Part 2: Strategies to Promote Academic Integrity and Professional Ethics
- Week 9 Assignment 9.1: Mercy Killing Ethics – Using one theory that you have studied that you agree with and one theory that you disagree with, describe how Officer Jones would act in each case – Solution
- Deliverable 4 – Code of Ethics Intake Packet
- Ethics in the Workplace
- code of ethics for nurses
- Applying the ANA Code of Ethics
Health Promotion Case Study
Community health promotion plays a crucial role in improving the health and well-being of populations. Our community health promotion case studies highlight successful initiatives aimed at preventing diseases, promoting healthy lifestyles, and addressing social determinants of health. Explore strategies for community engagement, health education, and collaborative interventions that make a positive impact on the well-being of individuals and communities.
- Health Promotion in Minority Populations
- Environmental Factors and Health Promotion Presentation: Accident Prevention and Safety Promotion for Parents and Caregivers of Infants
- Health Education And Current Challenges For Family-Centered Health Promotion
- Cultural Competence And Nutrition In Health Promotion
- Why is the concept of family health important? Consider the various strategies for health promotion.
- levels of health promotion
- Integrate evidence from research and theory into discussions of practice competencies, health promotion and disease prevention strategies, quality improvement, and safety standards.
- Discuss various theories of health promotion, including Pender’s Health Promotion Model, the Health Belief Model, the Transtheoretical Theory, and the Theory of Reasoned Action.
- What strategies, besides the use of learning styles, can a nurse educator consider when developing tailored individual care plans, or for educational programs in health promotion?
- Describe health promotion for Pregnant women
- Identify a health problem or need for health promotion for a particular stage in the life span of a population from a specific culture in your area. Choose one of the Leading Health Indicators (LHI) priorities from Healthy People 2020: https://www.healthypeople.gov/2020/Leading-Health-Indicators
- A description of a borrowed theory (expectancy-value theory and social cognitive theory) that could be applied to improve health promotion patient education in primary care clinic. Is this borrowed theory appropriate?
- How has health promotion changed over time
- Primary Prevention/Health Promotion
- Health Risk Assessment and Health Promotion Contract
Nursing Leadership Case Studies
Nursing leadership is essential for driving positive change and ensuring high-quality patient care. Our nursing leadership case studies examine effective leadership strategies, change management initiatives, and interprofessional collaboration in healthcare settings. Gain insights into the qualities of successful nurse leaders, explore innovative approaches to leadership, and learn how to inspire and motivate your team to achieve excellence in nursing practice.
- Part 3: Nursing Leadership – Childbearing after menopause – Assignment Solution
- Capstone Project Ideas for Nursing Leadership
- The purpose of this assignment is to examine the impact of contemporary challenges in care delivery facing nursing leadership. Select and research a major issue in the delivery of care facing nurse leaders today and write a 1,250-1,500 word paper addressing the following:
- One nursing theory will be presented as a framework to resolve a problem occurring within one of the professional areas of leadership, education, informatics, healthcare policy or advance clinical practice. The same nursing theory selected in Assignment One may be used to resolve the identified problem.
- Module 6: Change and Leadership in Nursing Education – Professional Development
- Module 6: Change and Leadership in Nursing Education – Critical Thinking
- Module 6: Change and Leadership in Nursing Education – Discussion
- Analyze one of the following concepts: “Advanced Practice Nursing,” “Leadership in Nursing Practice” or “Holistic Nursing Practice”
- Nursing Administration Function: A Comprehensive Guide for Nursing Students
- Theory and Leadership
- NUR-514: Organizational Leadership and Informatics
- Leadership: Workplace Environment Assessment
- Professional Development in Nursing – Topic 3 Assignment Solution
- Leadership Change Framework – Week 8 Assignment Solution
At NursingStudy.org, we strive to provide you with a comprehensive collection of nursing case study examples and solutions that align with the best practices recommended by YOAST and RankMath. By exploring these diverse case studies, you’ll enhance your clinical knowledge, critical thinking abilities, and overall understanding of nursing practice. Take advantage of this valuable resource and elevate your nursing skills to new heights.
Remember, success in nursing begins with knowledge and continues with lifelong learning. Explore our nursing case study examples and solutions today and embark on a journey of professional growth and excellence.
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Paper Examples
Related Posts
- Personal Philosophy Statement Example for a PMHNP
- Leadership Strategies for Success-Nursing Paper Examples
- Applying the Scientific Method-Nursing Paper Examples
Important Links
Knowledge base, paper examples, nursing writing services.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org
- Open access
- Published: 14 May 2024
Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study
- Jocelyn Schroeder 1 ,
- Barbara Pesut 1 , 2 ,
- Lise Olsen 2 ,
- Nelly D. Oelke 2 &
- Helen Sharp 2
BMC Nursing volume 23 , Article number: 326 ( 2024 ) Cite this article
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada’s legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses’ (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education; and bereavement care for family. Nurses have a right under the law to conscientious objection to participating in MAiD. Therefore, it is essential to prepare nurses in their entry-level education for the practice implications and moral complexities inherent in this practice. Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context.
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
During phase 1, a 56-item survey was developed from existing literature that included demographic items and items designed to measure experience with death and dying (including MAiD), education and preparation, attitudes and beliefs, influences on those beliefs, and anticipated future involvement. During phase 2, an expert faculty panel reviewed, modified, and prioritized the items yielding 51 items. During phase 3, a sample of nursing students further evaluated and modified the language in the survey to aid readability and comprehension. The final survey consists of 45 items including 4 case studies.
Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students’ attitudes toward MAiD in a Canadian context.
The survey is appropriate for use in education and research to measure knowledge and attitudes about MAiD among nurse trainees and can be a helpful step in preparing nursing students for entry-level practice.
Peer Review reports
Medical Assistance in Dying (MAiD) is permitted under an amendment to Canada’s Criminal Code which was passed in 2016 [ 1 ]. MAiD is defined in the legislation as both self-administered and clinician-administered medication for the purpose of causing death. In the 2016 Bill C-14 legislation one of the eligibility criteria was that an applicant for MAiD must have a reasonably foreseeable natural death although this term was not defined. It was left to the clinical judgement of MAiD assessors and providers to determine the time frame that constitutes reasonably foreseeable [ 2 ]. However, in 2021 under Bill C-7, the eligibility criteria for MAiD were changed to allow individuals with irreversible medical conditions, declining health, and suffering, but whose natural death was not reasonably foreseeable, to receive MAiD [ 3 ]. This population of MAiD applicants are referred to as Track 2 MAiD (those whose natural death is foreseeable are referred to as Track 1). Track 2 applicants are subject to additional safeguards under the 2021 C-7 legislation.
Three additional proposed changes to the legislation have been extensively studied by Canadian Expert Panels (Council of Canadian Academics [CCA]) [ 4 , 5 , 6 ] First, under the legislation that defines Track 2, individuals with mental disease as their sole underlying medical condition may apply for MAiD, but implementation of this practice is embargoed until March 2027 [ 4 ]. Second, there is consideration of allowing MAiD to be implemented through advanced consent. This would make it possible for persons living with dementia to receive MAID after they have lost the capacity to consent to the procedure [ 5 ]. Third, there is consideration of extending MAiD to mature minors. A mature minor is defined as “a person under the age of majority…and who has the capacity to understand and appreciate the nature and consequences of a decision” ([ 6 ] p. 5). In summary, since the legalization of MAiD in 2016 the eligibility criteria and safeguards have evolved significantly with consequent implications for nurses and nursing care. Further, the number of Canadians who access MAiD shows steady increases since 2016 [ 7 ] and it is expected that these increases will continue in the foreseeable future.
Nurses have been integral to MAiD care in the Canadian context. While other countries such as Belgium and the Netherlands also permit euthanasia, Canada is the first country to allow Nurse Practitioners (Registered Nurses with additional preparation typically achieved at the graduate level) to act independently as assessors and providers of MAiD [ 1 ]. Although the role of Registered Nurses (RNs) in MAiD is not defined in federal legislation, it has been addressed at the provincial/territorial-level with variability in scope of practice by region [ 8 , 9 ]. For example, there are differences with respect to the obligation of the nurse to provide information to patients about MAiD, and to the degree that nurses are expected to ensure that patient eligibility criteria and safeguards are met prior to their participation [ 10 ]. Studies conducted in the Canadian context indicate that RNs perform essential roles in MAiD care coordination; client and family teaching and support; MAiD procedural quality; healthcare provider and public education; and bereavement care for family [ 9 , 11 ]. Nurse practitioners and RNs are integral to a robust MAiD care system in Canada and hence need to be well-prepared for their role [ 12 ].
Previous studies have found that end of life care, and MAiD specifically, raise complex moral and ethical issues for nurses [ 13 , 14 , 15 , 16 ]. The knowledge, attitudes, and beliefs of nurses are important across practice settings because nurses have consistent, ongoing, and direct contact with patients who experience chronic or life-limiting health conditions. Canadian studies exploring nurses’ moral and ethical decision-making in relation to MAiD reveal that although some nurses are clear in their support for, or opposition to, MAiD, others are unclear on what they believe to be good and right [ 14 ]. Empirical findings suggest that nurses go through a period of moral sense-making that is often informed by their family, peers, and initial experiences with MAID [ 17 , 18 ]. Canadian legislation and policy specifies that nurses are not required to participate in MAiD and may recuse themselves as conscientious objectors with appropriate steps to ensure ongoing and safe care of patients [ 1 , 19 ]. However, with so many nurses having to reflect on and make sense of their moral position, it is essential that they are given adequate time and preparation to make an informed and thoughtful decision before they participate in a MAID death [ 20 , 21 ].
It is well established that nursing students receive inconsistent exposure to end of life care issues [ 22 ] and little or no training related to MAiD [ 23 ]. Without such education and reflection time in pre-entry nursing preparation, nurses are at significant risk for moral harm. An important first step in providing this preparation is to be able to assess the knowledge, values, and beliefs of nursing students regarding MAID and end of life care. As demand for MAiD increases along with the complexities of MAiD, it is critical to understand the knowledge, attitudes, and likelihood of engagement with MAiD among nursing students as a baseline upon which to build curriculum and as a means to track these variables over time.
Aim, design, and setting
The aim of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. We sought to explore both their willingness to be involved in the registered nursing role and in the nurse practitioner role should they chose to prepare themselves to that level of education. The design was a mixed-method, modified e-Delphi method that entailed item generation, item refinement through an expert faculty panel [ 24 , 25 , 26 ], and initial item validation through a cognitive focus group interview with nursing students [ 27 ]. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
Participants
A panel of 10 faculty from the two nursing education programs were recruited for Phase 2 of the e-Delphi. To be included, faculty were required to have a minimum of three years of experience in nurse education, be employed as nursing faculty, and self-identify as having experience with MAiD. A convenience sample of 5 fourth-year nursing students were recruited to participate in Phase 3. Students had to be in good standing in the nursing program and be willing to share their experiences of the survey in an online group interview format.
The modified e-Delphi was conducted in 3 phases: Phase 1 entailed item generation through literature and existing survey review. Phase 2 entailed item refinement through a faculty expert panel review with focus on content validity, prioritization, and revision of item wording [ 25 ]. Phase 3 entailed an assessment of face validity through focus group-based cognitive interview with nursing students.
Phase I. Item generation through literature review
The goal of phase 1 was to develop a bank of survey items that would represent the variables of interest and which could be provided to expert faculty in Phase 2. Initial survey items were generated through a literature review of similar surveys designed to assess knowledge and attitudes toward MAiD/euthanasia in healthcare providers; Canadian empirical studies on nurses’ roles and/or experiences with MAiD; and legislative and expert panel documents that outlined proposed changes to the legislative eligibility criteria and safeguards. The literature review was conducted in three online databases: CINAHL, PsycINFO, and Medline. Key words for the search included nurses , nursing students , medical students , NPs, MAiD , euthanasia , assisted death , and end-of-life care . Only articles written in English were reviewed. The legalization and legislation of MAiD is new in many countries; therefore, studies that were greater than twenty years old were excluded, no further exclusion criteria set for country.
Items from surveys designed to measure similar variables in other health care providers and geographic contexts were placed in a table and similar items were collated and revised into a single item. Then key variables were identified from the empirical literature on nurses and MAiD in Canada and checked against the items derived from the surveys to ensure that each of the key variables were represented. For example, conscientious objection has figured prominently in the Canadian literature, but there were few items that assessed knowledge of conscientious objection in other surveys and so items were added [ 15 , 21 , 28 , 29 ]. Finally, four case studies were added to the survey to address the anticipated changes to the Canadian legislation. The case studies were based upon the inclusion of mature minors, advanced consent, and mental disorder as the sole underlying medical condition. The intention was to assess nurses’ beliefs and comfort with these potential legislative changes.
Phase 2. Item refinement through expert panel review
The goal of phase 2 was to refine and prioritize the proposed survey items identified in phase 1 using a modified e-Delphi approach to achieve consensus among an expert panel [ 26 ]. Items from phase 1 were presented to an expert faculty panel using a Qualtrics (Provo, UT) online survey. Panel members were asked to review each item to determine if it should be: included, excluded or adapted for the survey. When adapted was selected faculty experts were asked to provide rationale and suggestions for adaptation through the use of an open text box. Items that reached a level of 75% consensus for either inclusion or adaptation were retained [ 25 , 26 ]. New items were categorized and added, and a revised survey was presented to the panel of experts in round 2. Panel members were again asked to review items, including new items, to determine if it should be: included, excluded, or adapted for the survey. Round 2 of the modified e-Delphi approach also included an item prioritization activity, where participants were then asked to rate the importance of each item, based on a 5-point Likert scale (low to high importance), which De Vaus [ 30 ] states is helpful for increasing the reliability of responses. Items that reached a 75% consensus on inclusion were then considered in relation to the importance it was given by the expert panel. Quantitative data were managed using SPSS (IBM Corp).
Phase 3. Face validity through cognitive interviews with nursing students
The goal of phase 3 was to obtain initial face validity of the proposed survey using a sample of nursing student informants. More specifically, student participants were asked to discuss how items were interpreted, to identify confusing wording or other problematic construction of items, and to provide feedback about the survey as a whole including readability and organization [ 31 , 32 , 33 ]. The focus group was held online and audio recorded. A semi-structured interview guide was developed for this study that focused on clarity, meaning, order and wording of questions; emotions evoked by the questions; and overall survey cohesion and length was used to obtain data (see Supplementary Material 2 for the interview guide). A prompt to “think aloud” was used to limit interviewer-imposed bias and encourage participants to describe their thoughts and response to a given item as they reviewed survey items [ 27 ]. Where needed, verbal probes such as “could you expand on that” were used to encourage participants to expand on their responses [ 27 ]. Student participants’ feedback was collated verbatim and presented to the research team where potential survey modifications were negotiated and finalized among team members. Conventional content analysis [ 34 ] of focus group data was conducted to identify key themes that emerged through discussion with students. Themes were derived from the data by grouping common responses and then using those common responses to modify survey items.
Ten nursing faculty participated in the expert panel. Eight of the 10 faculty self-identified as female. No faculty panel members reported conscientious objector status and ninety percent reported general agreement with MAiD with one respondent who indicated their view as “unsure.” Six of the 10 faculty experts had 16 years of experience or more working as a nurse educator.
Five nursing students participated in the cognitive interview focus group. The duration of the focus group was 2.5 h. All participants identified that they were born in Canada, self-identified as female (one preferred not to say) and reported having received some instruction about MAiD as part of their nursing curriculum. See Tables 1 and 2 for the demographic descriptors of the study sample. Study results will be reported in accordance with the study phases. See Fig. 1 for an overview of the results from each phase.
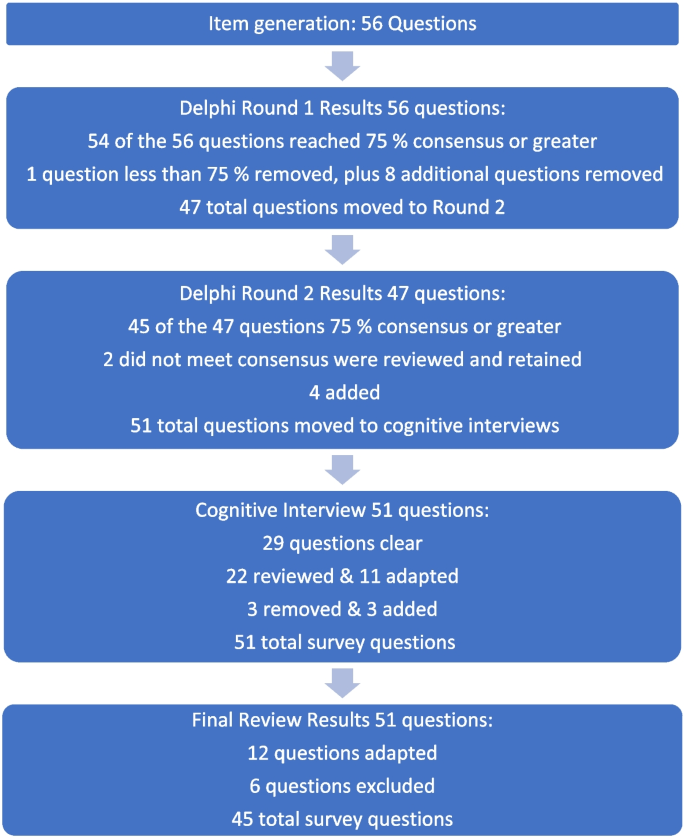
Fig. 1 Overview of survey development findings
Phase 1: survey item generation
Review of the literature identified that no existing survey was available for use with nursing students in the Canadian context. However, an analysis of themes across qualitative and quantitative studies of physicians, medical students, nurses, and nursing students provided sufficient data to develop a preliminary set of items suitable for adaptation to a population of nursing students.
Four major themes and factors that influence knowledge, attitudes, and beliefs about MAiD were evident from the literature: (i) endogenous or individual factors such as age, gender, personally held values, religion, religiosity, and/or spirituality [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], (ii) experience with death and dying in personal and/or professional life [ 35 , 40 , 41 , 43 , 44 , 45 ], (iii) training including curricular instruction about clinical role, scope of practice, or the law [ 23 , 36 , 39 ], and (iv) exogenous or social factors such as the influence of key leaders, colleagues, friends and/or family, professional and licensure organizations, support within professional settings, and/or engagement in MAiD in an interdisciplinary team context [ 9 , 35 , 46 ].
Studies of nursing students also suggest overlap across these categories. For example, value for patient autonomy [ 23 ] and the moral complexity of decision-making [ 37 ] are important factors that contribute to attitudes about MAiD and may stem from a blend of personally held values coupled with curricular content, professional training and norms, and clinical exposure. For example, students report that participation in end of life care allows for personal growth, shifts in perception, and opportunities to build therapeutic relationships with their clients [ 44 , 47 , 48 ].
Preliminary items generated from the literature resulted in 56 questions from 11 published sources (See Table 3 ). These items were constructed across four main categories: (i) socio-demographic questions; (ii) end of life care questions; (iii) knowledge about MAiD; or (iv) comfort and willingness to participate in MAiD. Knowledge questions were refined to reflect current MAiD legislation, policies, and regulatory frameworks. Falconer [ 39 ] and Freeman [ 45 ] studies were foundational sources for item selection. Additionally, four case studies were written to reflect the most recent anticipated changes to MAiD legislation and all used the same open-ended core questions to address respondents’ perspectives about the patient’s right to make the decision, comfort in assisting a physician or NP to administer MAiD in that scenario, and hypothesized comfort about serving as a primary provider if qualified as an NP in future. Response options for the survey were also constructed during this stage and included: open text, categorical, yes/no , and Likert scales.
Phase 2: faculty expert panel review
Of the 56 items presented to the faculty panel, 54 questions reached 75% consensus. However, based upon the qualitative responses 9 items were removed largely because they were felt to be repetitive. Items that generated the most controversy were related to measuring religion and spirituality in the Canadian context, defining end of life care when there is no agreed upon time frames (e.g., last days, months, or years), and predicting willingness to be involved in a future events – thus predicting their future selves. Phase 2, round 1 resulted in an initial set of 47 items which were then presented back to the faculty panel in round 2.
Of the 47 initial questions presented to the panel in round 2, 45 reached a level of consensus of 75% or greater, and 34 of these questions reached a level of 100% consensus [ 27 ] of which all participants chose to include without any adaptations) For each question, level of importance was determined based on a 5-point Likert scale (1 = very unimportant, 2 = somewhat unimportant, 3 = neutral, 4 = somewhat important, and 5 = very important). Figure 2 provides an overview of the level of importance assigned to each item.
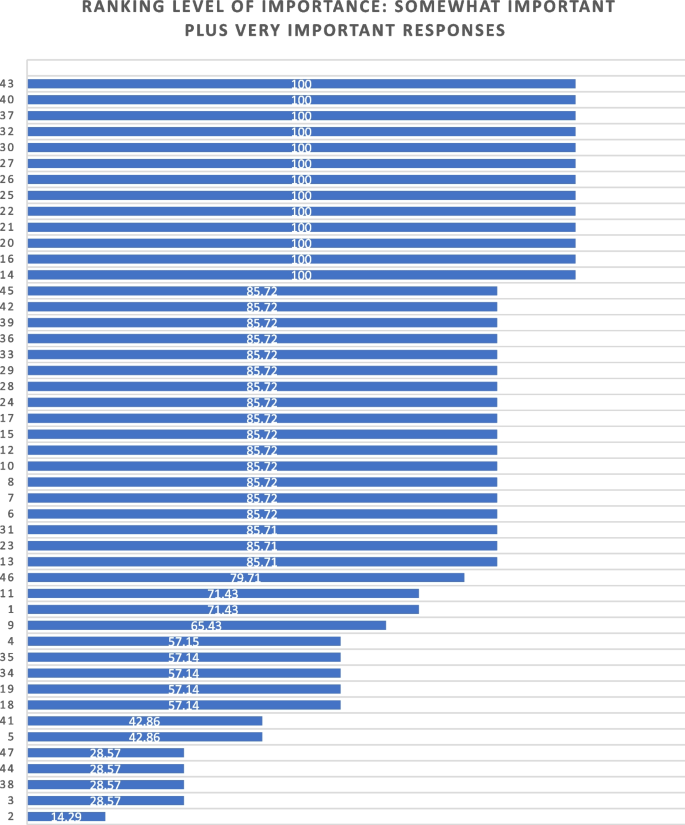
Ranking level of importance for survey items
After round 2, a careful analysis of participant comments and level of importance was completed by the research team. While the main method of survey item development came from participants’ response to the first round of Delphi consensus ratings, level of importance was used to assist in the decision of whether to keep or modify questions that created controversy, or that rated lower in the include/exclude/adapt portion of the Delphi. Survey items that rated low in level of importance included questions about future roles, sex and gender, and religion/spirituality. After deliberation by the research committee, these questions were retained in the survey based upon the importance of these variables in the scientific literature.
Of the 47 questions remaining from Phase 2, round 2, four were revised. In addition, the two questions that did not meet the 75% cut off level for consensus were reviewed by the research team. The first question reviewed was What is your comfort level with providing a MAiD death in the future if you were a qualified NP ? Based on a review of participant comments, it was decided to retain this question for the cognitive interviews with students in the final phase of testing. The second question asked about impacts on respondents’ views of MAiD and was changed from one item with 4 subcategories into 4 separate items, resulting in a final total of 51 items for phase 3. The revised survey was then brought forward to the cognitive interviews with student participants in Phase 3. (see Supplementary Material 1 for a complete description of item modification during round 2).
Phase 3. Outcomes of cognitive interview focus group
Of the 51 items reviewed by student participants, 29 were identified as clear with little or no discussion. Participant comments for the remaining 22 questions were noted and verified against the audio recording. Following content analysis of the comments, four key themes emerged through the student discussion: unclear or ambiguous wording; difficult to answer questions; need for additional response options; and emotional response evoked by questions. An example of unclear or ambiguous wording was a request for clarity in the use of the word “sufficient” in the context of assessing an item that read “My nursing education has provided sufficient content about the nursing role in MAiD.” “Sufficient” was viewed as subjective and “laden with…complexity that distracted me from the question.” The group recommended rewording the item to read “My nursing education has provided enough content for me to care for a patient considering or requesting MAiD.”
An example of having difficulty answering questions related to limited knowledge related to terms used in the legislation such as such as safeguards , mature minor , eligibility criteria , and conscientious objection. Students were unclear about what these words meant relative to the legislation and indicated that this lack of clarity would hamper appropriate responses to the survey. To ensure that respondents are able to answer relevant questions, student participants recommended that the final survey include explanation of key terms such as mature minor and conscientious objection and an overview of current legislation.
Response options were also a point of discussion. Participants noted a lack of distinction between response options of unsure and unable to say . Additionally, scaling of attitudes was noted as important since perspectives about MAiD are dynamic and not dichotomous “agree or disagree” responses. Although the faculty expert panel recommended the integration of the demographic variables of religious and/or spiritual remain as a single item, the student group stated a preference to have religion and spirituality appear as separate items. The student focus group also took issue with separate items for the variables of sex and gender, specifically that non-binary respondents might feel othered or “outed” particularly when asked to identify their sex. These variables had been created based upon best practices in health research but students did not feel they were appropriate in this context [ 49 ]. Finally, students agreed with the faculty expert panel in terms of the complexity of projecting their future involvement as a Nurse Practitioner. One participant stated: “I certainly had to like, whoa, whoa, whoa. Now let me finish this degree first, please.” Another stated, “I'm still imagining myself, my future career as an RN.”
Finally, student participants acknowledged the array of emotions that some of the items produced for them. For example, one student described positive feelings when interacting with the survey. “Brought me a little bit of feeling of joy. Like it reminded me that this is the last piece of independence that people grab on to.” Another participant, described the freedom that the idea of an advance request gave her. “The advance request gives the most comfort for me, just with early onset Alzheimer’s and knowing what it can do.” But other participants described less positive feelings. For example, the mature minor case study yielded a comment: “This whole scenario just made my heart hurt with the idea of a child requesting that.”
Based on the data gathered from the cognitive interview focus group of nursing students, revisions were made to 11 closed-ended questions (see Table 4 ) and 3 items were excluded. In the four case studies, the open-ended question related to a respondents’ hypothesized actions in a future role as NP were removed. The final survey consists of 45 items including 4 case studies (see Supplementary Material 3 ).
The aim of this study was to develop and validate a survey that can be used to track the growth of knowledge about MAiD among nursing students over time, inform training programs about curricular needs, and evaluate attitudes and willingness to participate in MAiD at time-points during training or across nursing programs over time.
The faculty expert panel and student participants in the cognitive interview focus group identified a need to establish core knowledge of the terminology and legislative rules related to MAiD. For example, within the cognitive interview group of student participants, several acknowledged lack of clear understanding of specific terms such as “conscientious objector” and “safeguards.” Participants acknowledged discomfort with the uncertainty of not knowing and their inclination to look up these terms to assist with answering the questions. This survey can be administered to nursing or pre-nursing students at any phase of their training within a program or across training programs. However, in doing so it is important to acknowledge that their baseline knowledge of MAiD will vary. A response option of “not sure” is important and provides a means for respondents to convey uncertainty. If this survey is used to inform curricular needs, respondents should be given explicit instructions not to conduct online searches to inform their responses, but rather to provide an honest appraisal of their current knowledge and these instructions are included in the survey (see Supplementary Material 3 ).
Some provincial regulatory bodies have established core competencies for entry-level nurses that include MAiD. For example, the BC College of Nurses and Midwives (BCCNM) requires “knowledge about ethical, legal, and regulatory implications of medical assistance in dying (MAiD) when providing nursing care.” (10 p. 6) However, across Canada curricular content and coverage related to end of life care and MAiD is variable [ 23 ]. Given the dynamic nature of the legislation that includes portions of the law that are embargoed until 2024, it is important to ensure that respondents are guided by current and accurate information. As the law changes, nursing curricula, and public attitudes continue to evolve, inclusion of core knowledge and content is essential and relevant for investigators to be able to interpret the portions of the survey focused on attitudes and beliefs about MAiD. Content knowledge portions of the survey may need to be modified over time as legislation and training change and to meet the specific purposes of the investigator.
Given the sensitive nature of the topic, it is strongly recommended that surveys be conducted anonymously and that students be provided with an opportunity to discuss their responses to the survey. A majority of feedback from both the expert panel of faculty and from student participants related to the wording and inclusion of demographic variables, in particular religion, religiosity, gender identity, and sex assigned at birth. These and other demographic variables have the potential to be highly identifying in small samples. In any instance in which the survey could be expected to yield demographic group sizes less than 5, users should eliminate the demographic variables from the survey. For example, the profession of nursing is highly dominated by females with over 90% of nurses who identify as female [ 50 ]. Thus, a survey within a single class of students or even across classes in a single institution is likely to yield a small number of male respondents and/or respondents who report a difference between sex assigned at birth and gender identity. When variables that serve to identify respondents are included, respondents are less likely to complete or submit the survey, to obscure their responses so as not to be identifiable, or to be influenced by social desirability bias in their responses rather than to convey their attitudes accurately [ 51 ]. Further, small samples do not allow for conclusive analyses or interpretation of apparent group differences. Although these variables are often included in surveys, such demographics should be included only when anonymity can be sustained. In small and/or known samples, highly identifying variables should be omitted.
There are several limitations associated with the development of this survey. The expert panel was comprised of faculty who teach nursing students and are knowledgeable about MAiD and curricular content, however none identified as a conscientious objector to MAiD. Ideally, our expert panel would have included one or more conscientious objectors to MAiD to provide a broader perspective. Review by practitioners who participate in MAiD, those who are neutral or undecided, and practitioners who are conscientious objectors would ensure broad applicability of the survey. This study included one student cognitive interview focus group with 5 self-selected participants. All student participants had held discussions about end of life care with at least one patient, 4 of 5 participants had worked with a patient who requested MAiD, and one had been present for a MAiD death. It is not clear that these participants are representative of nursing students demographically or by experience with end of life care. It is possible that the students who elected to participate hold perspectives and reflections on patient care and MAiD that differ from students with little or no exposure to end of life care and/or MAiD. However, previous studies find that most nursing students have been involved with end of life care including meaningful discussions about patients’ preferences and care needs during their education [ 40 , 44 , 47 , 48 , 52 ]. Data collection with additional student focus groups with students early in their training and drawn from other training contexts would contribute to further validation of survey items.
Future studies should incorporate pilot testing with small sample of nursing students followed by a larger cross-program sample to allow evaluation of the psychometric properties of specific items and further refinement of the survey tool. Consistent with literature about the importance of leadership in the context of MAiD [ 12 , 53 , 54 ], a study of faculty knowledge, beliefs, and attitudes toward MAiD would provide context for understanding student perspectives within and across programs. Additional research is also needed to understand the timing and content coverage of MAiD across Canadian nurse training programs’ curricula.
The implementation of MAiD is complex and requires understanding of the perspectives of multiple stakeholders. Within the field of nursing this includes clinical providers, educators, and students who will deliver clinical care. A survey to assess nursing students’ attitudes toward and willingness to participate in MAiD in the Canadian context is timely, due to the legislation enacted in 2016 and subsequent modifications to the law in 2021 with portions of the law to be enacted in 2027. Further development of this survey could be undertaken to allow for use in settings with practicing nurses or to allow longitudinal follow up with students as they enter practice. As the Canadian landscape changes, ongoing assessment of the perspectives and needs of health professionals and students in the health professions is needed to inform policy makers, leaders in practice, curricular needs, and to monitor changes in attitudes and practice patterns over time.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to small sample sizes, but are available from the corresponding author on reasonable request.
Abbreviations
British Columbia College of Nurses and Midwives
Medical assistance in dying
Nurse practitioner
Registered nurse
University of British Columbia Okanagan
Nicol J, Tiedemann M. Legislative Summary: Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying). Available from: https://lop.parl.ca/staticfiles/PublicWebsite/Home/ResearchPublications/LegislativeSummaries/PDF/42-1/c14-e.pdf .
Downie J, Scallion K. Foreseeably unclear. The meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhousie Law J. 2018;41(1):23–57.
Nicol J, Tiedeman M. Legislative summary of Bill C-7: an act to amend the criminal code (medical assistance in dying). Ottawa: Government of Canada; 2021.
Google Scholar
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf .
Council of Canadian Academies. The state of knowledge on advance requests for medical assistance in dying. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2019/02/The-State-of-Knowledge-on-Advance-Requests-for-Medical-Assistance-in-Dying.pdf .
Council of Canadian Academies. The state of knowledge on medical assistance in dying for mature minors. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-for-Mature-Minors.pdf .
Health Canada. Third annual report on medical assistance in dying in Canada 2021. Ottawa; 2022. [cited 2023 Oct 23]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2021.html .
Banner D, Schiller CJ, Freeman S. Medical assistance in dying: a political issue for nurses and nursing in Canada. Nurs Philos. 2019;20(4): e12281.
Article PubMed Google Scholar
Pesut B, Thorne S, Stager ML, Schiller CJ, Penney C, Hoffman C, et al. Medical assistance in dying: a review of Canadian nursing regulatory documents. Policy Polit Nurs Pract. 2019;20(3):113–30.
Article PubMed PubMed Central Google Scholar
College of Registered Nurses of British Columbia. Scope of practice for registered nurses [Internet]. Vancouver; 2018. Available from: https://www.bccnm.ca/Documents/standards_practice/rn/RN_ScopeofPractice.pdf .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Global Qual Nurs Res. 2020;7:2333393620938686. https://doi.org/10.1177/2333393620938686 .
Article Google Scholar
Pesut B, Thorne S, Schiller CJ, Greig M, Roussel J. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs. 2020;19:12. https://doi.org/10.1186/s12912-020-0404-5 .
Pesut B, Greig M, Thorne S, Burgess M, Storch JL, Tishelman C, et al. Nursing and euthanasia: a narrative review of the nursing ethics literature. Nurs Ethics. 2020;27(1):152–67.
Pesut B, Thorne S, Storch J, Chambaere K, Greig M, Burgess M. Riding an elephant: a qualitative study of nurses’ moral journeys in the context of Medical Assistance in Dying (MAiD). Journal Clin Nurs. 2020;29(19–20):3870–81.
Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2018;26(5):1337–49.
Wright DK, Chan LS, Fishman JR, Macdonald ME. “Reflection and soul searching:” Negotiating nursing identity at the fault lines of palliative care and medical assistance in dying. Social Sci & Med. 2021;289: 114366.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;54(4):511–20.
Bruce A, Beuthin R. Medically assisted dying in Canada: "Beautiful Death" is transforming nurses' experiences of suffering. The Canadian J Nurs Res | Revue Canadienne de Recherche en Sci Infirmieres. 2020;52(4):268–77. https://doi.org/10.1177/0844562119856234 .
Canadian Nurses Association. Code of ethics for registered nurses. Ottawa; 2017. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics .
Canadian Nurses Association. National nursing framework on Medical Assistance in Dying in Canada. Ottawa: 2017. Available from: https://www.virtualhospice.ca/Assets/cna-national-nursing-framework-on-maidEng_20170216155827.pdf .
Pesut B, Thorne S, Greig M. Shades of gray: conscientious objection in medical assistance in dying. Nursing Inq. 2020;27(1): e12308.
Durojaiye A, Ryan R, Doody O. Student nurse education and preparation for palliative care: a scoping review. PLoS ONE. 2023. https://doi.org/10.1371/journal.pone.0286678 .
McMechan C, Bruce A, Beuthin R. Canadian nursing students’ experiences with medical assistance in dying | Les expériences d’étudiantes en sciences infirmières au regard de l’aide médicale à mourir. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2019;5(1). https://doi.org/10.17483/2368-6669.1179 .
Adler M, Ziglio E. Gazing into the oracle. The Delphi method and its application to social policy and public health. London: Jessica Kingsley Publishers; 1996
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–12.
Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and health research. 1st ed. City: Wiley; 2011.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 1st ed. Thousand Oaks, Calif: Sage; 2005. ISBN: 9780761928041
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood EW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2017;26(1):37–49.
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood K. Nurses’ use of conscientious objection and the implications of conscience. J Adv Nurs. 2018;75(3):594–602.
de Vaus D. Surveys in social research. 6th ed. Abingdon, Oxon: Routledge; 2014.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149 .
Puchta C, Potter J. Focus group practice. 1st ed. London: Sage; 2004.
Book Google Scholar
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. Oxford: Oxford University Press; 2015.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Adesina O, DeBellis A, Zannettino L. Third-year Australian nursing students’ attitudes, experiences, knowledge, and education concerning end-of-life care. Int J of Palliative Nurs. 2014;20(8):395–401.
Bator EX, Philpott B, Costa AP. This moral coil: a cross-sectional survey of Canadian medical student attitudes toward medical assistance in dying. BMC Med Ethics. 2017;18(1):58.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53(4):511–20.
Brown J, Goodridge D, Thorpe L, Crizzle A. What is right for me, is not necessarily right for you: the endogenous factors influencing nonparticipation in medical assistance in dying. Qual Health Res. 2021;31(10):1786–1800.
Falconer J, Couture F, Demir KK, Lang M, Shefman Z, Woo M. Perceptions and intentions toward medical assistance in dying among Canadian medical students. BMC Med Ethics. 2019;20(1):22.
Green G, Reicher S, Herman M, Raspaolo A, Spero T, Blau A. Attitudes toward euthanasia—dual view: Nursing students and nurses. Death Stud. 2022;46(1):124–31.
Hosseinzadeh K, Rafiei H. Nursing student attitudes toward euthanasia: a cross-sectional study. Nurs Ethics. 2019;26(2):496–503.
Ozcelik H, Tekir O, Samancioglu S, Fadiloglu C, Ozkara E. Nursing students’ approaches toward euthanasia. Omega (Westport). 2014;69(1):93–103.
Canning SE, Drew C. Canadian nursing students’ understanding, and comfort levels related to medical assistance in dying. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2022;8(2). https://doi.org/10.17483/2368-6669.1326 .
Edo-Gual M, Tomás-Sábado J, Bardallo-Porras D, Monforte-Royo C. The impact of death and dying on nursing students: an explanatory model. J Clin Nurs. 2014;23(23–24):3501–12.
Freeman LA, Pfaff KA, Kopchek L, Liebman J. Investigating palliative care nurse attitudes towards medical assistance in dying: an exploratory cross-sectional study. J Adv Nurs. 2020;76(2):535–45.
Brown J, Goodridge D, Thorpe L, Crizzle A. “I am okay with it, but I am not going to do it:” the exogenous factors influencing non-participation in medical assistance in dying. Qual Health Res. 2021;31(12):2274–89.
Dimoula M, Kotronoulas G, Katsaragakis S, Christou M, Sgourou S, Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurs Educ Today. 2019;74:7–14.
Matchim Y, Raetong P. Thai nursing students’ experiences of caring for patients at the end of life: a phenomenological study. Int J Palliative Nurs. 2018;24(5):220–9.
Canadian Institute for Health Research. Sex and gender in health research [Internet]. Ottawa: CIHR; 2021 [cited 2023 Oct 23]. Available from: https://cihr-irsc.gc.ca/e/50833.html .
Canadian Nurses’ Association. Nursing statistics. Ottawa: CNA; 2023 [cited 2023 Oct 23]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics .
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47. https://doi.org/10.1007/s11135-011-9640-9 .
Ferri P, Di Lorenzo R, Stifani S, Morotti E, Vagnini M, Jiménez Herrera MF, et al. Nursing student attitudes toward dying patient care: a European multicenter cross-sectional study. Acta Bio Medica Atenei Parmensis. 2021;92(S2): e2021018.
PubMed PubMed Central Google Scholar
Beuthin R, Bruce A. Medical assistance in dying (MAiD): Ten things leaders need to know. Nurs Leadership. 2018;31(4):74–81.
Thiele T, Dunsford J. Nurse leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics. 2019;26(4):993–9.
Download references
Acknowledgements
We would like to acknowledge the faculty and students who generously contributed their time to this work.
JS received a student traineeship through the Principal Research Chairs program at the University of British Columbia Okanagan.
Author information
Authors and affiliations.
School of Health and Human Services, Selkirk College, Castlegar, BC, Canada
Jocelyn Schroeder & Barbara Pesut
School of Nursing, University of British Columbia Okanagan, Kelowna, BC, Canada
Barbara Pesut, Lise Olsen, Nelly D. Oelke & Helen Sharp
You can also search for this author in PubMed Google Scholar
Contributions
JS made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. JS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. BP made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. BP has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. LO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. LO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. NDO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. NDO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HS made substantial contributions to drafting and substantively revising the work. HS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
JS conducted this study as part of their graduate requirements in the School of Nursing, University of British Columbia Okanagan.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Selkirk College Research Ethics Board (REB) ID # 2021–011 and the University of British Columbia Behavioral Research Ethics Board ID # H21-01181.
All participants provided written and informed consent through approved consent processes. Research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schroeder, J., Pesut, B., Olsen, L. et al. Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study. BMC Nurs 23 , 326 (2024). https://doi.org/10.1186/s12912-024-01984-z
Download citation
Received : 24 October 2023
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12912-024-01984-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying (MAiD)
- End of life care
- Student nurses
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

521 S. Main, Moscow, Idaho 83843 | (208) 882-2669 | [email protected] | 10am - 6pm Mon-Sat, 10am - 4pm Sun

Critical Care Nursing Demystified (Paperback)

- Description
- About the Author
- Reviews & Media
A fun, streamlined way to learn the major concepts and theories of critical care nursing - and how to apply them to real-world patient situations
Whether you're a professional nurse who wants to transition into critical care nursing or a student seeking to excel in your advanced studies, Critical Care Nursing Demystified is the book you need to quickly and easily understand the key concepts and advanced trends of this specialty.
In order to make the learning process as quick and effective as possible, each chapter contains lesson objectives, key terms, NCLEX(R)-style Q&A, and vignettes of nursing situations you're likely to encounter in the workplace. You'll also find a comprehensive final exam and coverage that includes overviews of basic anatomy and physiology of target organ systems, detailed health assessments using the body systems approach, diagnostic studies utilized to confirm an illness, common critical procedures performed, current medications used in the treatment of the critical care patient, and implementation of the nursing process to identify and solve patient concerns.
Learn how to care for patients with:
- Critical respiratory needs
- Critical cardiac and vascular needs
- Critical cardiac rhythm disturbance needs
- Neurological needs
- Endocrine disorders
- Critical renal needs
- Critical hematologic needs
Simple enough for students but challenging enough for professional nurses considering a switch from their current field to this specialty, Critical Care Nursing Demystified is the book you need to make your transition or entry into the field as smooth and painless as possible.
- Nursing - Critical & Intensive care
- Education & Training
- Emergency Medicine
- Kobo eBook (June 16th, 2011): $30.00

IMAGES
VIDEO
COMMENTS
Critical Care Nursing: Scenarios & Case Studies. Lesson Transcript. Instructor Jennifer Mitchell. Jennifer is a clinical professor for nursing students in critical care and has several years of ...
This section is a collection of critical care clinical cases to test yourself and hopefully get some new ideas. Please leave feedback and comments, and if you want to put your own hot cases up, please get in touch and we can make it happen. ... The NEJM Critical Care Challenge: Case 11 (End of Life Care) Lachlan Donaldson, 15/06/14 16/07/14 ...
A nursing case study can be described as a student-learning activity that tells a story about a patient/family (clinical ... Phase 1: Critical Care A 24-year old woman, Cheryl, was admitted to the trauma unit following a motor vehicle accident as a front-seat passenger. She does not have any apparent brain, spinal cord, or internal organ injury.
I see you: a Chaplain case study on existential distress and transdisciplinary support, ... Reflections on Medical Futility From an Ancient Intensivist, Critical Care Medicine, 49, 1, (1-6), ...
This case study explores the . Early Recognition and Management of Sepsis in the Elderly: A Case Study : Critical Care Nursing Quarterly ... Critical Care Nursing Quarterly 44(2):p 175-181, April/June 2021. | DOI: 10.1097/CNQ.0000000000000351. Buy; Metrics Abstract.
Nursing Care of a Child With Delirium Receiving Venoarterial Extracorporeal Membrane Oxygenation: A Case Report ... American Association of Critical-Care Nurses 27071 Aliso Creek Road Aliso Viejo, CA 92656. Tel: (800) 899-1712; Tel: (949) 362-2000; Facebook;
Nursing in Critical Care is a peer-reviewed international journal publishing articles on all aspects of critical care nursing practice, research, education and ... including research, quality improvement, service evaluation, education projects, case studies, literature reviews and critical commentaries. Deadline for Submissions: 1 December 2023 ...
Case Studies in Critical Care Nursing contains detailed and up-to-date case studies on critical care conditions with accompanying questions and answers for applied learning of the practice of critical care nursing. The organization of the book has been changed to mirror that of Thelan's Critical Care Nursing, 4th Edition; the chapters in this ...
BOOKS Case Studies in Critical Care Nursing: A Guide for Application and Review third edition Sheila Drake Melander 2004, 506 pages $39.95 softcover. This book contains 33 nursing case studies about issues commonly seen in intensive care units (eg, acute renal failure, respiratory distress, neurotrauma). The patient scenarios increase knowledge ...
Case Studies in Critical Care Nursing is an exciting book for the critical care nurse who is striving to develop skills in analysing the complex needs of the critically ill patient. It will enable nurses to play a vital role in co-ordinating and focusing the efforts of the many health care workers toward realistic patient-orientated goals.
At this nursing school, an elective Critical Care Nursing course for last-semester seniors was designed to include active learning strategies, focusing on the use of case studies to facilitate learning. Results indicate significantly improved final examination scores for those involved with the case-study pedagogy.
Case Studies in Critical Care Nursing contains detailed and up-to-date case studies on critical care conditions with accompanying questions and answers for applied learning of the practice of critical care nursing. The organization of the book has been changed to mirror that of Thelan's Critical Care Nursing, 4th Edition; the chapters in this 3rd edition are grouped according to body systems.
AORN Journal is a perioperative nursing journal providing evidence-based practice information to help meet the physiological, behavioral, and safety needs of patients. Case Studies in Critical Care Nursing: A Guide for Application and Review, Sheila Drake Melander, third edition, 2004, softcover, 506 pages $39.95 Skip to Article Content ...
A CASE STUDY OF CRITICAL CARE NURSES' ENTERAL FEEDING DECISIONS Andrea Marshall RN, BN, MN A thesis submitted in fulfilment of the requirements for the degree of Doctor of Philosophy The University of Sydney 2008 View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Sydney eScholarship
Introduction. Critical care nurses working in intensive care units (ICUs) care for critically-ill patients, and their work scope can include communicating with patients' loved ones and care givers [].In such settings, nurses must make timely judgments based on their expertise, and this requires a high level of communication competency to comprehensively evaluate the needs of patients and ...
The nursing role during end-of-life care in the intensive care unit related to the interaction between patient, family and professional: an integrative review. Scand J Caring Sci 2016; 30: 645-661.
Correct answer: C. The main criteria defining a massive pulmonary embolism are signs of hemodynamic compromise [1]. These include: -Arterial hypotension defined as systolic arterial blood pressure <90mmHg or a drop in systolic arterial blood pressure of at least 40mmHg for at least 15 minutes (mortality 15%) -Cardiogenic shock as manifested by ...
Our critical care nursing case studies encompass a range of high-acuity scenarios, including trauma, cardiac emergencies, and respiratory distress. These case studies simulate the fast-paced critical care environment, enabling you to sharpen your critical thinking skills, enhance your clinical judgment, and deliver exceptional care to ...
Student Resources on Evolve NEW! 10 Next Generation NCLEX ® Exam-style case studies for student practice 25 animations 15 videos 5 review questions per chapter for the NCLEX, CCRN ® , and PCCN ® exams Free access to selected Elsevier Clinical Skills Audio glossary ... Critical Care Nursing - Elsevier eBook on VitalSource. Elsevier eBook on ...
The World Medical Association (WMA) defines "clinical independence" as the "assurance that individual physicians have the freedom to exercise their professional judgment in the care and treatment of their patients without undue influence by outside parties or individuals," and it "is a critical component of high quality medical care and an essential principle of health care ...
This chapter explores risk assessment and management, highlighting the need to prevent or minimise risks within the nursing process of providing care. Risk assessment and management is everybody's business; it is a major component of daily living and nursing practice. Risk assessment is simply an assessment or calculation of risk or potential ...
Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students' knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. ... The final survey consists of 45 items including 4 case studies ...
In 2017, the department allocated educational premises at the address: ul. 1st Borodino, house 2. Since January 31, 2018, the Department of Nursing Year is part of the Medical and Preventive Faculty (MPF). Scientific work of the department: Complex scientific theme of the department "Psychovegetative correlations in patients with coronary ...
521 S. Main, Moscow, Idaho 83843 | (208) 882-2669 | [email protected] | 10am - 6pm Mon-Sat, 10am - 4pm Sun