- Open access
- Published: 09 August 2022

Risk factors for missed abortion: retrospective analysis of a single institution’s experience
- Wei-Zhen Jiang 1 ,
- Xi-Lin Yang 2 &
- Jian-Ru Luo 1
Reproductive Biology and Endocrinology volume 20 , Article number: 115 ( 2022 ) Cite this article
14k Accesses
3 Citations
Metrics details
To explore the risk factors including the difference between mean gestational sac diameter and crown-rump length for missed abortion.
Hospitalized patients with missed abortion and patients with continuing pregnancy to the second trimester from Chengdu Women's and Children's Central Hospital from June 2018 to June 2021 were retrospectively analyzed. The best cut-off value for age and difference between mean gestational sac diameter and crown-rump length (mGSD-CRL) were obtained by x-tile software. Univariate and multivariate logistic regression analysis were adopted to identify the possible risk factors for missed abortion.
Age, gravidity, parity, history of cesarean section, history of recurrent abortion (≥ 3 spontaneous abortions), history of ectopic pregnancy and overweight or obesity (BMI > 24 kg/m 2 ) were related to missed abortion in univariate analysis. However, only age (≥ 30 vs < 30 years: OR = 1.683, 95%CI = 1.017–2.785, P = 0.043, power = 54.4%), BMI (> 24 vs ≤ 24 kg/m 2 : OR = 2.073, 95%CI = 1.056–4.068, P = 0.034, power = 81.3%) and mGSD-CRL (> 20.0vs ≤ 11.7 mm: OR = 2.960, 95% CI = 1.397–6.273, P = 0.005, power = 98.9%; 11.7 < mGSD-CRL ≤ 20.0vs > 20.0 mm: OR = 0.341, 95%CI = 0.172–0.676, P = 0.002, power = 84.8%) were identified as independent risk factors for missed abortion in multivariate analysis.
Patients with age ≥ 30 years, BMI > 24 kg/m 2 or mGSD-CRL > 20 mm had increasing risk for missed abortion, who should be more closely monitored and facilitated with necessary interventions at first trimester or even before conception to reduce the occurrence of missed abortion to have better clinical outcomes.
Missed abortion was a special type of spontaneous abortion that the embryo or fetus has already died but remained in the uterus for days or weeks and with a closed cervical ostium [ 1 ]. Patients might present with or without subtle clinical symptoms such as vaginal bleeding or abdominal pain. Missed abortion, occuring in approximately 8–20% of clinically confirmed intrauterine pregnancies [ 2 ], was often confirmed using ultrasonography.
Missed abortion was undoubtedly a huge physical and psychological setback for women with fertility requirements. Therefore, early identification of women at high risk of missed abortion was pivotal, which might aid in providing possible theoretical basis for implementing clinical measures to prevent missed abortion. Previous studies have revealed that Human Chorionic Gonadotropin(HCG), Estradiol(E2), progesterone, gestational sac diameter(GSD), Crown-Rump Length(CRL), fetal heart rate and yolk sac diameter might be predictive for early pregnancy loss [ 3 , 4 , 5 ] . In addition, the predictive value of mGSD-CRL for early pregnancy outcome in in vitro fertilization(IVF) treatment has been established [ 6 ]. However, most of the current studies have performed univariate analysis to identify the risk factors for early pregnancy loss [ 3 , 4 , 5 , 6 ].
Therefore, we conducted this study to more comprehensively explore the possible high risk factors relating to developing of missed abortion using multivariate logistic regression analysis, hopefully it could be of great help to identification and intervention.
Materials and methods
Data sources.
We reviewed patients from Chengdu Women's and Children's Central Hospital from June 2018 to June 2021. Inclusion criteria of missed abortion group were listed as follows: (1) Not more than 12 weeks gestation; (2) Crown-rump length ≥ seven mm without heartbeat or (3) mean sac diameter ≥ 25 mm without embryo or (4) absence of embryo with heartbeat ≥ two weeks after a scan that showed a gestational sac without a yolk sac or (5) absence of embryo with heartbeat ≥ 11 days after a scan that showed a gestational sac with a yolk sac [ 7 ]. Exclusion criteria of missed abortion group were listed as follows: (1) Incomplete information; (2) multiple pregnancy. Patients with the following inclusion and exclusion criteria were enrolled as control group: (1) Patients continued pregnancy to the second trimester were included; (2) Incomplete information and multiple pregnancy were excluded. After excluding patients with incomplete information, 307 patients were finally included with 160 patients having missed abortion and 147 with continuing pregnancy to second trimester. Due to the retrospective nature of the study, informed consent was waived, but this study was granted by the ethics committee of Chengdu Women's and Children's Central Hospital and the ethics approval number was B2021(26).
Collection of data
Patients’ information regarding age, gravidity, parity, history of vaginal delivery, history of cesarean delivery, history of recurrent abortion (≥ 3 spontaneous abortions), history of induced abortion, history of medication abortion, history of midtrimester induction, history of ectopic pregnancy, history of smoking, history of alcohol consumption, history of other uterine operations, mode of conception, BMI, mGSD-CRL not more than 12 weeks with live embryo were collected.
Statistical analysis
Categorical variables were described as percentages or frequencies and compared using Pearson χ2 test; continues variables were described as medians with interquartile range (IQR) and compared with t test. We identified the cut-off value for age and mGSD-CRL via X-tile software (version 3.6.1; Yale University, New Haven, CT, USA) once maximal chi-square value reached, which was considered to represent the greatest difference in outcomes prediction among the subgroups [ 8 ].
Logistic regression was used to determine independent risk factors for missed abortion. Statistically significant variables from univariate logistic regression analysis ( P < 0.1) were included in the multivariate analysis. Pearson χ2 test, t test and logistic regression were performed using SPSS (version 25.0, SPSS, Chicago, IL, USA), X-tile software was uesed to calculate cut-off value. G*Power Analysis program (version 3.1, The G*Power Team, Belgium) was used for power calculation. A two-tailed P < 0.05 was recognized as statistically significant.
Study cohort
A total of 307 patients were finally included in the study with 160 cases having missed abortion and 147 with continuing pregnancy to second trimester (Supplementary Fig. 1 ). The characteristics was listed in Supplementary Table 1 . As a result, 30 years old was the cut-off value for age via X-tile software. Therefore, age was split as age ≥ 30 years and age < 30 years. Similarl y , mGSD-CRL was divided into three subgroups: GSD-CR < 11.7 mm, 11.7 mm ≤ mGSD-CRL ≤ 20.0 mm, GSD-CR > 20.0 mm (Fig. 1 ). Nearly half of the patients were over 30 years old (49.2%). 38.4% of the patients were having first pregnancy, and the majority of the patients had never delivered (71.0%). 11.1% of the patients had a history of vaginal delivery, however, 18.2% of the patients had a history of cesarean section. Of note, 16% of the patients had a BMI > 24 kg/m 2 , 29.6% of the patients had a mGSD-CRL < 11.7 mm and 18.9% had a mGSD-CRL > 20 mm. Moreover, 2.6% of the patients suffering from recurrent abortion and 4.2% had a history of ectopic pregnancy. Besides, 39.1% of the patients had a history of curettage. In total, 52.1% of the patients developed missed abortion (Table 1 ).
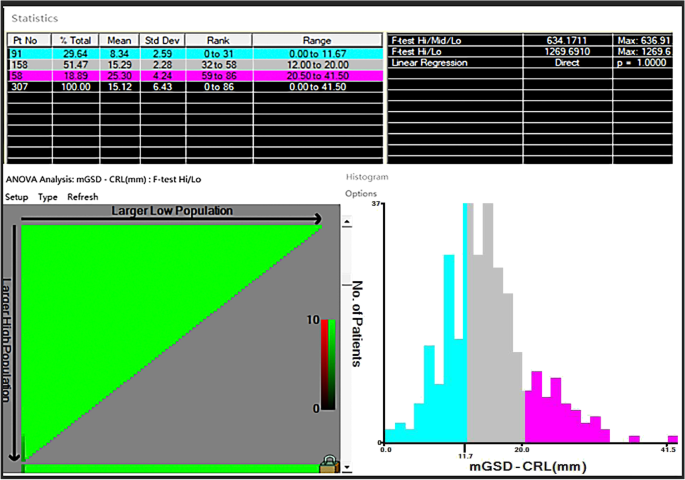
mGSD-CRL at diagnosis stratification by X-tile software
Risk factors for missed abortion
In the univariate logistic regression analysis, Age, gravidity, parity, history of cesarean section, history of recurrent abortion, history of ectopic pregnancy, overweight or obesity (BMI > 24 kg/m 2 ) and mGSD-CRL were significantly related to increased risk factors for missed abortion. Furthermore, risk factors identified in the univariate logistic regression analysis were included in the multivariate analysis, which revealed that Age (≥ 30 vs < 30 years: OR = 1.683, 95%CI = 1.017–2.785, P = 0.043, power = 54.4%), BMI (> 24 vs ≤ 24 kg/m 2 : OR = 2.073, 95%CI = 1.056–4.068, P = 0.034, power = 81.3%), mGSD-CRL (> 20.0vs ≤ 11.7 mm: OR = 2.960, 95% CI = 1.397–6.273, P = 0.005, power = 98.9%; 11.7 < mGSD-CRL ≤ 20.0vs > 20.0 mm: OR = 0.341, 95%CI = 0.172–0.676, P = 0.002, power = 84.8%) were independent risk factors for missed abortion (Table 2 ).
Missed abortion, normally presenting without symptoms of threatened abortion such as abdominal pain and vaginal bleeding, was a kind of spontaneous abortion, which were frequently diagnosed using ultrasonography. In this study, we retrospectively analyzed the data of 160 missed abortion patients and 147 pregnant women who didn’t have abortion in the first trimester in order to fully establish the possible risk factors for missed abortion, and provide evidence for early identification and intervention for patients with high risk of missed abortion.
In previous studies, it was believed that advanced age was a high risk factor for missed abortion, which might result from the decline of ovarian function and corpus luteum function as age accrued [ 1 , 9 ]. However, previous study also showed that advanced age was not a high risk factor for spontaneous abortion [ 10 ], in which age was divided into advanced age group (> 35 years) and non-advanced age group (≤ 35 years old). Therefore, we hypothesized that there might be a more meaningful cutoff value other than 35 years old to divide the age into two subgroups. As a result, 30 years old, calculated via x-tile, showed significant value in the final multivariate logistic analysis (OR = 1.683, 95%CI = 1.017–2.785, P = 0.043). As controversial regarding age existed in previous studies, our result showing that age > 30 was an independent risk factor for missed abortion seemed solid. And the dropping from 35 to 30 in terms of cut-off value for age might be related to factors like increasing pressure, unhealthy living habits and environmental pollution resulting from social developing [ 2 , 11 ]. Although the cut-off value in our study were not consistent with previous ones, the consensus on older age was a high risk factor for missed abortion was basically reached.
A meta-analysis including 16 studies demonstrated that BMI > 25 kg/m 2 was a high risk factor for abortion [ 12 ], which reported that the missed abortion rate of overweight or obese women was as high as 25–37% [ 13 ]. The participants from our study were childbearing age women from China, so the definition of overweight or obese as BMI > 24 kg/m 2 was used for grouping though the World Health Organization(WHO) defined overweight or obesity as BMI > 25 kg/m 2 [ 14 ]. And the result showed that patients with BMI > 24 kg/m 2 were more likely to have missed abortion than BMI ≤ 24 kg/m 2 (OR = 2.073, 95% CI = 1.056–4.068, P = 0.034), which was consistent with previous studies [ 11 , 12 ]. Therefore, weight control before pregnancy was usually recommended.
Although the effect of mGSD and CRL on missed abortion had been reported [ 3 , 4 , 15 , 16 , 17 , 18 ], there was few studies working on the relationship between mGSD-CRL and missed abortion. Bromley et al.firstly proposed the concept of "small gestational sac" [ 19 ]. And their work revealed that mGSD-CRL < 5 mm in the first trimester was a high risk factor for missed abortion. However, the extremely limited number of included patients in their study might impede the generalization of the conclusion. Similarly, the research from Kapfhamer el also showed that mGSD-CRL < 5 mm was a high risk factor for early pregnancy loss, and further demonstrated that mGSD-CRL > 10 mm was a protective factor for early pregnancy loss [ 6 ]. However, Zhao et al. believed that "large gestational sac"(mGSD-CRL ≥ 18 mm) was related to increasing risk for spontaneous abortion [ 20 ]. Therefore, we used x-tile to find the two optimal cutoff values for mGSD-CRL, which showed that patients with mGSD-CRL > 20 mm was more more likely to have missed abortion than patients with mGSD-CR ≤ 20 mm. And there was no statistical difference between mGSD-CRL < 11.7 mm group and 11.7 ≤ mGSD-CRL ≤ 20.0 mm group. In summary, we were inclined to believe that increasing mGSD-CRL was associated with increasing risk of missed abortion, which should be further validated in the future due to the differences in sample size from previous studies [ 6 , 19 , 20 ].
Age, gravidity, parity, history of cesarean section, history of recurrent abortion, history of ectopic pregnancy, BMI and mGSD-CRL were identified in the univariate analysis. However, only age, BMI and mGSD-CRL were still meaningful in multivariate analysis. What was inconsistent with previous studies in our study was that recurrent abortion was not a high risk factor for missed abortion [ 21 ], which might result from the low incidence of recurrent abortion (missed abortion group vs non-missed abortion group: 7 vs 1) in our study.
One major strength of this study was that stratifying age by x-tile rather than 35 years were firstly recognized for high risk of missed abortion. Other strengths included that mGSD-CRL were analyzed instead of mGSD or CRL independently. On the contrary, This study was inevitably limited by the retrospective nature. In addition, the pathogenic factors for missed abortion was complicated, and some possible high risk factors like immunological or genetic factors could not be obtained.
It is well known that missed abortion is a special type of spontaneous abortion and the ultimate outcome is embryonic arrest. The current knowledge of the missed abortion mostly relates to prevention and treatment, but the classification and severity have not been covered yet according to existing literature and guidelines. The purpose of this paper is to explore the high-risk factors of missed abortion, therefore treatment was barely involved, and we will do more research on the treatment of missed abortion in future work. Overall, We hope that the present study could aid in abortion prediction and treatment decision-making for clinicians.
Conclusions
This study demonstrated that age ≥ 30 years old, BMI > 24 kg/m 2 and mGSD-CRL > 20 mm were independent risk factors for missed abortion. This study provided a theoretical basis for clinicians to deliver prompt interventions in childbearing age women during the first trimester or even before pregnancy, so as to reduce the incidence of missed abortion.
Availability of data and material
All data that support the findings of this study were available from the corresponding author via E-mail due to appropriate request.
Cunningham FG, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Casey BM, et al. Williams Obstetrics. 25nd ed. New York: McGraw-Hill; 2018.
Google Scholar
Fang J, Xie B, Chen B, et al. Biochemical clinical factors associated with missed abortion independent of maternal age: A retrospective study of 795 cases with missed abortion and 694 cases with normal pregnancy. Medicine (Baltimore). 2018;97(50):e13573.
Article Google Scholar
Altay MM, Yaz H, Haberal A. The assessment of the gestational sac diameter, crown-rump length, progesterone and fetal heart rate measurements at the 10th gestational week to predict the spontaneous abortion risk. J Obstet Gynaecol Res. 2009;35(2):287–92.
Article CAS Google Scholar
Papaioannou GI, Syngelaki A, Maiz N, et al. Ultrasonographic prediction of early miscarriage. Hum Reprod. 2011;26(7):1685–92.
Puget C, Joueidi Y, Bauville E, et al. Serial hCG and progesterone levels to predict early pregnancy outcomes in pregnancies of uncertain viability: A prospective study. Eur J Obstet Gynecol Reprod Biol. 2018;220:100–5.
Kapfhamer JD, Palaniappan S, Summers K, et al. Fertil Steril. 2018;109(1):130–6.
Doubilet PM, Benson CB, Bourne T, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369(15):1443–51.
Zhuang W, Chen J, Li Y, et al. Valuation of lymph node dissection in localized high-risk renal cell cancer using X-tile software. Int Urol Nephrol. 2020;52(2):253–62.
Guifang G, Caixin Y, Yanqing H, et al. A survey of influencing factors of missed abortion during the two-child peak period. J Obstet Gynaecol. 2020;undefined:1–4.
Yavuz P, Taze M, Salihoglu O. The effect of adolescent and advanced-age pregnancies on maternal and early neonatal clinical data. J Matern Fetal Neonatal Med. 2021;undefined:1–7.
Wu J, Hou H, Ritz B, et al. Exposure to polycyclic aromatic hydrocarbons and missed abortion in early pregnancy in a Chinese population. Sci Total Environ. 2010;408(11):2312–8.
Metwally M, Ong KJ, Ledger WL, et al. Does high body mass index increase the risk of miscarriage after spontaneous and assisted conception? A meta-analysis of the evidence. Fertil Steril. 2008;90(3):714–26.
Hamilton-Fairley D, Kiddy D, Watson H, et al. Association of moderate obesity with a poor pregnancy outcome in women with polycystic ovary syndrome treated with low dose gonadotrophin. Br J Obstet Gynaecol. 1992;99(2):128–31.
WHO. Obesity: preventing and managing the global epidemic. World Health Organ Tech Rep Ser. 2000;894:1–253.
Pexsters A, Luts J, Van Schoubroeck D, et al. Clinical implications of intra- and interobserver reproducibility of transvaginal sonographic measurement of gestational sac and crown-rump length at 6–9 weeks’ gestation. Ultrasound Obstet Gynecol. 2011;38(5):510–5.
Preisler J, Kopeika J, Ismail L, et al. Defining safe criteria to diagnose miscarriage: prospective observational multicentre study. BMJ. 2015;351:4579.
Ouyang Y, Qin J, Lin G, et al. Reference intervals of gestational sac, yolk sac, embryonic length, embryonic heart rate at 6–10 weeks after in vitro fertilization-embryo transfer. BMC Pregnancy Childbirth. 2020;20(1):533.
Papaioannou GI, Syngelaki A, Poon LCY, et al. Normal ranges of embryonic length, embryonic heart rate, gestational sac diameter and yolk sac diameter at 6–10 weeks. Fetal Diagn Ther. 2010;28(4):207–19.
Bromley B, Harlow BL, Laboda LA, et al. Small sac size in the first trimester: a predictor of poor fetal outcome. Radiology. 1991;178(2):375–7.
Xuan Z, Liu Lu, Haiqian Li. Clinical Analysis of the Impact of Corpus Luteum, Gestational Sac and Embryo in Early Pregnancy on the Pregnant Outcomes. J Pract Obstetr Gynecolo. 2013;08:595–8.
Li H, Qin S, Xiao F, et al. Predicting first-trimester outcome of embryos with cardiac activity in women with recurrent spontaneous abortion. J Int Med Res. 2020;48(6):300060520911829.
CAS PubMed Google Scholar
Download references
Acknowledgements
The authors wish to thank the participants, Chengdu Women's and Children's Central Hospital hospital staff, and whoever contributed to this study.
Not applicable.
Author information
Authors and affiliations.
Department of Gynaecology and Obstetrics, Chengdu Women’s and Children’s Central Hospital, School of Medicine, University of Electronic Science and Technology of China, No.1617 of Riyue Avenue, Qingyang District, Chengdu, 611731, China
Wei-Zhen Jiang & Jian-Ru Luo
Department of Radiation Oncology, Chengdu Women’s and Children’s Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, 611731, China
Xi-Lin Yang
You can also search for this author in PubMed Google Scholar
Contributions
Conception/design: Wei-Zhen Jiang. Provision of study material or patients: Wei-Zhen Jiang. Collection and/or assembly of data: Wei-Zhen Jiang, Xi-Lin Yang. Data analysis and interpretation: Wei-Zhen Jiang, Xi-Lin Yang. Manuscript writing: Wei-Zhen Jiang. Manuscript revision: Jian-Ru Luo. Final approval of manuscript: All authors.
Corresponding author
Correspondence to Jian-Ru Luo .
Ethics declarations
Ethics approval and consent to participate.
Due to the retrospective nature of the study, informed consent was waived, but this study was granted by the ethics committee of Chengdu Women's and Children's Central Hospital and the ethics approval number was B2021(26).
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
The authors have declared that there is on potential conflicts of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: supplementary figure 1..
Flow chart depicting for inclusion of studysubjects. Supplementary Table1. Clinical characteristicsof participants.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jiang, WZ., Yang, XL. & Luo, JR. Risk factors for missed abortion: retrospective analysis of a single institution’s experience. Reprod Biol Endocrinol 20 , 115 (2022). https://doi.org/10.1186/s12958-022-00987-2
Download citation
Received : 09 January 2022
Accepted : 03 August 2022
Published : 09 August 2022
DOI : https://doi.org/10.1186/s12958-022-00987-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- First trimester pregnancy
- Missed abortion
- Gestational sac
- Crown-rump length
Reproductive Biology and Endocrinology
ISSN: 1477-7827
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 10 May 2017
Misoprostol for medical treatment of missed abortion: a systematic review and network meta-analysis
- Hang-lin Wu ORCID: orcid.org/0000-0001-7882-3072 1 ,
- Sheeba Marwah 2 ,
- Pei Wang 1 ,
- Qiu-meng Wang 1 &
- Xiao-wen Chen 1
Scientific Reports volume 7 , Article number: 1664 ( 2017 ) Cite this article
27k Accesses
42 Citations
44 Altmetric
Metrics details
- Drug therapy
- Reproductive disorders
The efficacy and safety of misoprostol alone for missed abortion varied with different regimens. To evaluate existing evidence for the medical management of missed abortion using misoprostol, we undertook a comprehensive review and meta-analysis. The electronic literature search was conducted using PubMed, the Cochrane Library, Embase, EBSCOhost Online Research Databases, Springer Link, ScienceDirect, Web of Science, Ovid Medline and Google Scholar. 18 studies of 1802 participants were included in our analysis. Compared with vaginal misoprostol of 800 ug or sublingual misoprostol of 600 ug, lower-dose regimens (200 ug or 400 ug) by any route of administration tend to be significantly less effective in producing abortion within about 24 hours. In terms of efficacy, the most effective treatment was sublingual misoprostol of 600 ug and the least effective was oral misoprostol of 400 ug. In terms of tolerability, vaginal misoprostol of 400 ug was reported with fewer side effects and sublingual misoprostol of 600 ug was reported with more side effects. Misoprostol is a non-invasive, effective medical method for completion of abortion in missed abortion. Sublingual misoprostol of 600 ug or vaginal misoprostol of 800 ug may be a good choice for the first dose. The ideal dose and medication interval of misoprostol however needs to be further researched.
Similar content being viewed by others

Early pregnancy ultrasound measurements and prediction of first trimester pregnancy loss: A logistic model

Pre-eclampsia

Male delayed orgasm and anorgasmia: a practical guide for sexual medicine providers
Introduction.
Missed abortion is defined as unrecognized intrauterine death of the embryo or fetus without expulsion of the products of conception. It constitutes approximately 15% of clinically diagnosed pregnancies 1 . Women experiencing a missed abortion may have no self-awareness due to the lack of obvious symptoms.
With around 95% success rate, surgical evacuation is regarded as the standard treatment for missed abortion, which had been widely performed all over the world in the past 50 years 2 . However, the costs of surgery and hospitalization, as well as the complications associated with surgery and anaesthesia are a major unresolved concern. Besides infection and bleeding, decreased fertility caused by intrauterine adhesions may be unacceptable for women with missed abortion, who have not yet fulfilled their motherhood desires. Some studies have thus suggested that expectant or medical management might be more suitable instead of surgical evacuation 3 , 4 .
Expectant management has been reported with unpredictable success rate ranging from 25–76% 5 , 6 , 7 . Waiting for spontaneous expulsion of the products of conception would waste much time, during which women may suffer uncertainty and anxiety 5 . When additional surgical evacuation is needed owing to failure, they may suffer from an emotional breakdown. It is thus not recommended for missed early miscarriage due to the risks of emergency surgical treatment and blood transfusion 8 .
Misoprostol is a synthetic prostaglandin E1 analogue which was originally developed to prevent non-steroidal anti-inflammatory drugs related gastric ulcers. However it has been used for various other indications in obstetrics and gynaecology. Medical management using misoprostol or combined with mifepristone for missed abortion had been widely researched 9 , 10 , 11 , 12 , 13 . Some studies have reported that medical treatment with mifepristone and misoprostol in women with missed abortion would increase the incidence of excessive bleeding 11 , 12 , 13 . Apart from this, mifepristone is more expensive which will add to unnecessary expenses.
The efficacy and safety of misoprostol alone for missed abortion was established in many studies 14 , 15 , 16 , 17 . However, route of administration of misoprostol and success rates varied among the studies. It could be given by oral, sublingual or vaginal, while the doses ranged from 100 micrograms to 800 micrograms 14 , 15 , 16 , 17 , 18 , 19 . The most suitable route and dose of misoprostol for missed abortion is not yet clear. A single dose of 800 micrograms of misoprostol by vaginal or oral for missed abortion was recommended by National Institute for Health and Care Excellence (NICE) 20 . However some studies reported converse opinion, by pointing out that a lower dose or different routes of misoprostol may be equally effective 21 , 22 .
So we evaluated the existing evidence for the medical management of missed abortion using misoprostol, with the hope of finding alternate suitable management strategies for surgical termination, which must be highly effective and with fewer side effects.
Literature Search
Overall, 1735 articles were identified by the search and 48 potentially eligible articles were retrieved in full text. Of these articles, 35 were excluded for reasons shown in Fig. 1 . The remaining 13 articles met our predefined inclusion criteria. Most of studies compared vaginal route of misoprostol with sublingual or oral route while only one study compared sublingual route with oral route (Fig. 2A ). When it turned to a network meta-analysis, another five articles which compared misoprostol with different doses in the same route were also included in our work. The network diagram of all included studies is shown in Fig. 2B .
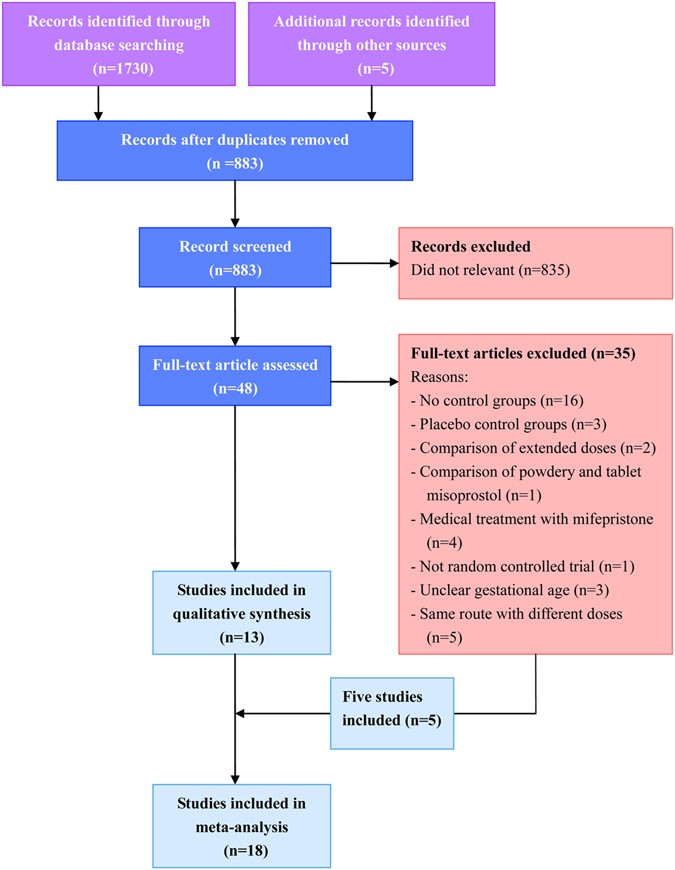
Article retrieval and screening.
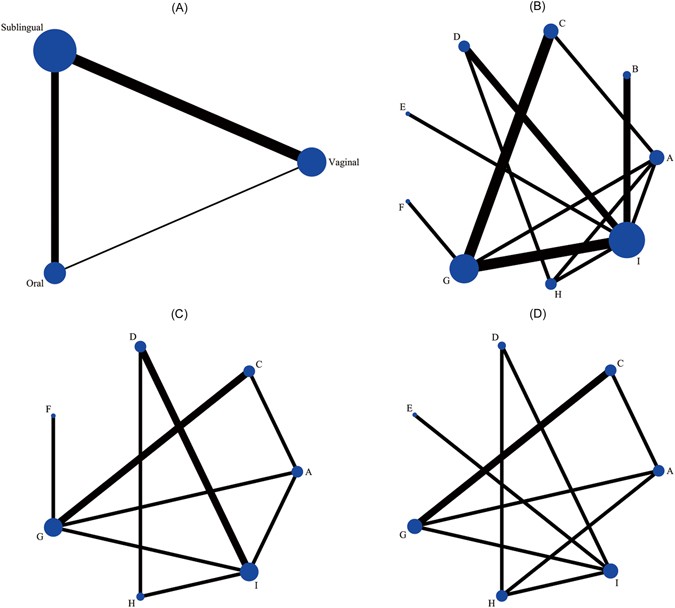
Network diagram of all studies and studies included in analyses of complete abortion rate within about 24 hours and main side effects. ( A ) Studies comparing different routes of misoprostol. ( B ) Studies comparing different routes or doses of misoprostol. ( C ) Complete abortion rate within about 24 hours. ( D ) Main side effects totally. Studies are classified according to the first dose of misoprostol in both groups; The width of the lines is proportional to the number of trials directly comparing each pair of interventions; The size of each node is proportional to the number of trails comparing a single intervention totally. Interventions are sequenced as follows: A. Oral 400 ug; B. Oral 800 ug; C. Sublingual 400 ug; D. Sublingual 600 ug; E. Sublingual 800 ug; F. Vaginal 200 ug; G. Vaginal 400 ug; H. Vaginal 600 ug; I. Vaginal 800 ug.
Study Characteristics
In all, 18 studies of 1802 participants, published between 1999 and 2016, were included in our analysis. The primary characteristics of the studies are tabulated in Supplementary Table S1 . Most of the studies were form India and Thailand. The maximum gestational age of participants in all the studies ranged from 8 weeks to 13 weeks, except one study which reported the outcomes separately according to different trimesters 23 . Interventions in the groups varied in terms of routes, doses and medication intervals and we used the first dose to classify them. In most of studies, complete abortion was defined as complete expulsion of the products of conception without surgical intervention. However in four studies, a less than 15 mm intrauterine tissue diameter on ultrasound scan was taken as the cutof f 24 , 25 , 26 , 27 , while one research adopted the criterion for endometrial thickness less than 10 mm 28 . Not all trials reported the same outcomes, especially for the follow-up time. A complete abortion rate within about 24 hours (24 to 28 hours) was mostly mentioned. We calculated it as our primary outcome. There was insufficient data to evaluate for complete abortion rate within 12 hours, 48 hours or 7 days.
For the reported side effects, we could only compare the incidence of nausea or vomiting, diarrhoea and fever. There was insufficient data to analyze other side effects. The mean time taken to abortion was difficult to evaluate due to different follow-up time. For each outcome we have indicated the number of trials contributing data to the network meta-analysis (Fig. 2C and D ). Complete abortion rate within about 24 hours of any intervention and side effects of all the interventions in the analysis are presented in Supplementary Table S2 .
Risk of bias was summarized in Supplementary Table S3 . It was categorized the risk of bias as unclear when no related information reported could be used. Most of the included trials described adequate randomization processes; however most of them were assessed as having an unclear risk of bias for allocation concealment and blinding.
Meta-analysis
The results of the network meta-analysis for the outcomes are presented as forest plots in Fig. 3 . Compared with vaginal misoprostol of 800 ug, lower-dose regimens (200 ug or 400 ug) by any route of administration tend to be significantly less effective in producing abortion within about 24 hours. Similar results can be seen in another comparison with sublingual misoprostol of 600 ug. For the comparison between the two regimens, there is no significant difference (RR 1.01, 95% CI 0.86 to 1.19). For the same dose of 600 ug, administration by vaginal route seems to be less effective than sublingual route, however it is not significant (RR 0.81, 95% CI, 0.65 to 1.01). For vaginal misoprostol, doses of 600 ug and 800 ug have no significant differences in producing miscarriage within about 24 hours (RR 0.82, 95% CI 0.63 to 1.07). In the analysis of main side effects, significant difference could be seen only in the comparison of vaginal and sublingual misoprostol of 400 ug (RR 0.54, 95% CI 0.32 to 0.90). For the same dose of 600 ug, administration by vaginal route seems to accompany with fewer side effects than sublingual route, which is not significant again (RR 0.49, 95% CI, 0.22 to 1.06). In detailed comparison for nausea or vomiting, there were no significant differences observed amongst all the regimens (Supplementary Figure S1 ). For the incidence of diarrhoea, sublingual route seems to be more common than vaginal route with same doses of 600 ug and 400 ug (Supplementary Figure S2 ). For the incidence of fever, sublingual route also seems to be more common than vaginal or oral route with a same dose of 400 ug (Supplementary Figure S3 ).
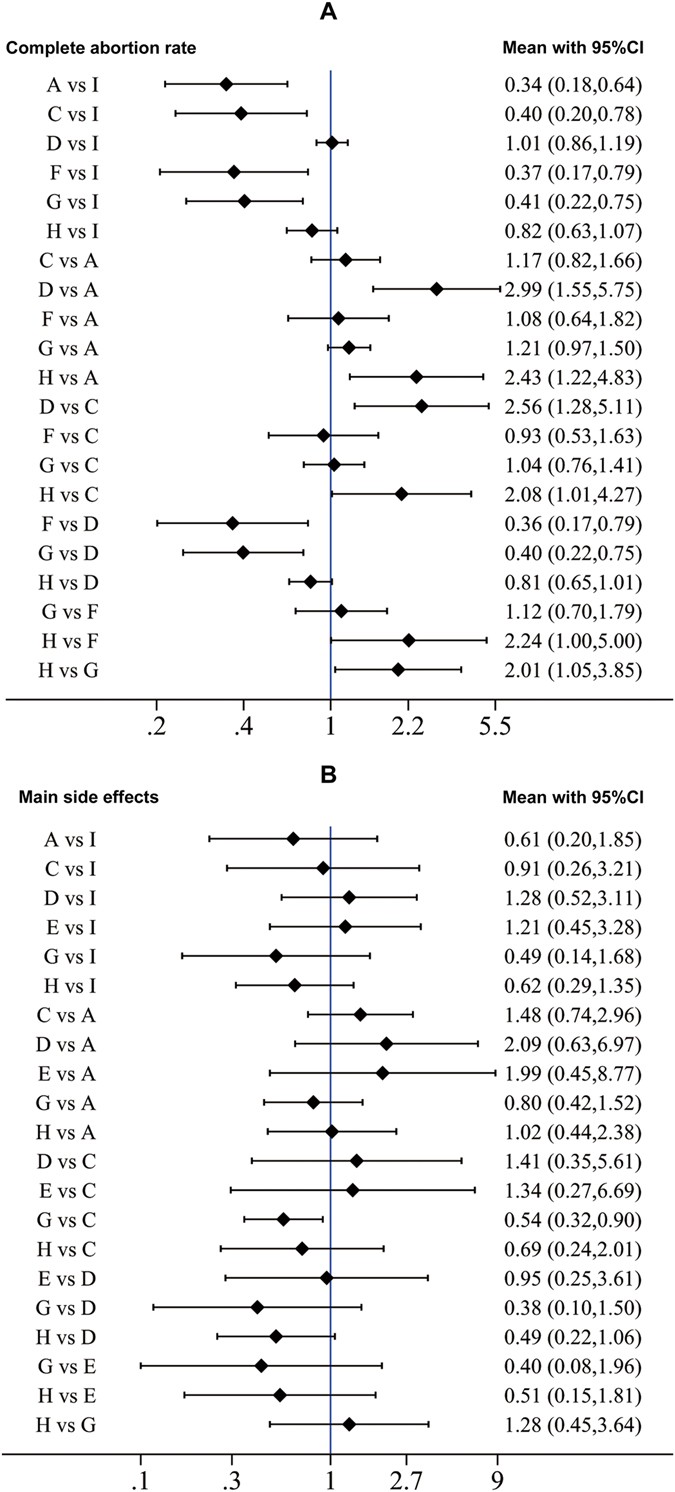
Network meta-analysis of complete abortion rate within about 24 hours and main side effects. Interventions are sequenced as follows: A. Oral 400 ug; C. Sublingual 400 ug; D. Sublingual 600 ug; E. Sublingual 800 ug; F. Vaginal 200 ug; G. Vaginal 400 ug; H. Vaginal 600 ug; I. Vaginal 800 ug.
Tests of consistency showed that there was no difference between the direct and indirect estimates in all close loops in the analysis of complete abortion rate (Supplementary Figure S4 ). The comparison-adjusted funnel plots of the network meta-analysis for complete abortion rate were not suggestive of any publication bias or small study effect (Supplementary Figure S5 ). The percentage contribution of each direct and indirect comparisons is presented as a table in Supplementary Figure S6 . Inconsistency could be seen in a close loop (sublingual misoprostol of 600 ug, vaginal misoprostol of 600 ug and 800 ug) in the analysis of main side effects (Supplementary Figure S7 ). It was due to the inconsistency in the analysis of nausea or vomiting (Supplementary Figure S8 ). No publication bias or small study effect was found in the analysis of main side effects (Supplementary Figure S9 ).
The results of sensitivity analyses of complete abortion rate were shown in Supplementary Table S4 . In the first sensitivity analysis we excluded one study in which gestational age of the participants was below 8 weeks while in the second we excluded another study in which complete abortion was defined as complete expulsion of the products of conception and endometrial thickness <10 mm. The results were robust for the two sensitivity analyses. When we excluded studies in which only single dose of misoprostol was used in both groups, pre-existed significantly differences disappeared and some of the confidence intervals were wide and across the null line. We reviewed studies related in the close loop with inconsistency, it was impossible to exclude any study for a reasonable argument. In the sensitivity analysis excluding studies with only single dose of misoprostol, the significant difference between vaginal and sublingual misoprostol of 400 ug still existed (Supplementary Table S5 ).
The ranking of interventions based on cumulative probability plots and surfaces under the cumulative ranking curve (SUCRAs) is presented in Fig. 4 . In terms of efficacy, the most effective treatment was sublingual misoprostol of 600 ug and the least effective was oral misoprostol of 400 ug. In terms of tolerability, vaginal misoprostol of 400 ug was reported with fewer side effects and sublingual misoprostol of 600 ug was reported with more side effects.
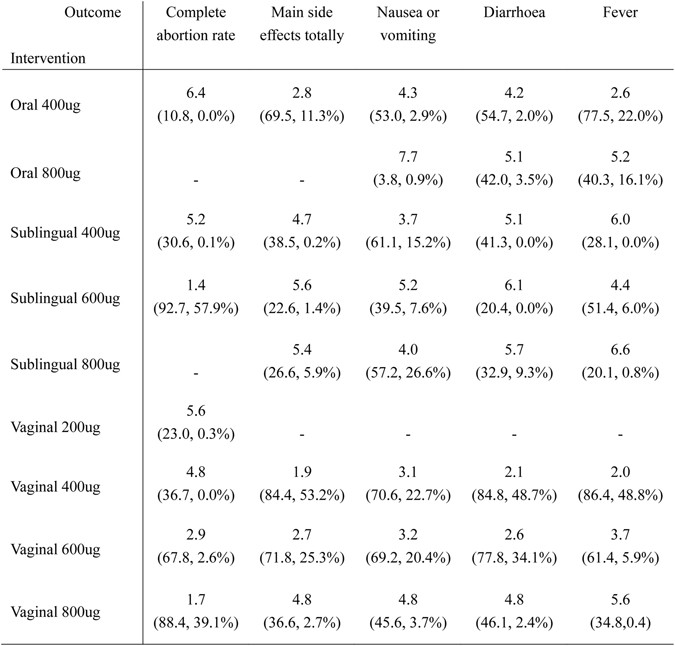
Ranking of all the interventions in network meta-analysis. Information of ranking is located at the intersection of the column-defining outcome and the row-defining intervention; The number in the first row is the ranking of all the interventions; The first number below in brackets is the surface under the cumulative ranking curve (SUCRA) while the second is the probability of the intervention to be the best.
This network meta-analysis represents the most comprehensive synthesis of data for medical treatment using misoprostol for missed abortion. It was found that higher-dose regimens were associated with higher complete abortion rate and more sides effects. Sublingual misoprostol of 600 ug or vaginal misoprostol of 800 ug as the first dose was more effective in producing complete abortion within about 24 hours. However the superiority decreased with multiple doses. It could be explained that a single high-dose of misoprostol might have produced complete abortion in most of women 29 , 30 , 31 . If multiple doses were given, more women with lower-dose misoprostol would convert into complete abortion, which was confirmed by Kovavisarach 30 . We found that the least effective treatment was the oral misopristol of 400 ug. It was due to the liver first-pass effect which greatly reduced the bioavailability of the drug. Alternative routes of administration like vaginal and sublingual avoid the liver first-pass effect because they allow drugs to be absorbed directly into the systemic circulation.
Side effects were most likely to appear in sublingually or orally administered misoprostol. A low dose vaginal misoprostol was reported with the fewest side effects, accompanied by low complete abortion rate 32 . Compared with vaginally or orally administered misoprostol, sublingual misoprostol of 600 ug or 400 ug was associated with more frequent diarrhoea and fever. It was due to the pharmacokinetics of misoprostol, which showed that sublingual misoprostol had the shortest onset of action, the highest peak concentration and greatest bioavailability among the routes of administration 33 .
Vaginal misoprostol of 800 ug was recommend for missed abortion by National Institute for Health and Care Excellence(NICE) and some clinical guidelines 8 , 20 . The results of our meta-analysis lead support to this regimen for medical treatment of missed abortion, however the question of whether sublingual misoprostol of 600 ug is better raises. Apart from this, the incidence of side effects reported was still higher than we expected for these regimens. A variety of methods were researched to increase the efficacy of misoprostol in order to reduce the dose. Some studies discussed the administration of different types of misoprostol, such as gel form and powder form, however the efficacy was not improved 34 , 35 . Some studies discussed the efficacy of moistened misoprostol by acetic acid or normal saline, conclusion was made that vaginal misoprostol either moistened with normal saline or acetic acid was comparable in terms of efficacy and adverse effects 36 , 37 , 38 . Some studies reported different methods to combine misoprostol with laminaria tents or castor oil, however these studies did not focus on the efficacy of these methods to produce abortion for women with missed abortion 39 , 40 .
Limited articles could be found about the efficacy and tolerability of sublingual or oral misoprostol of 800 ug which made us difficult to evaluate. Only in one study it was compared with vaginal misoprostol of 800 ug, the authors found that sublingual misoprostol was as effective as vaginal misoprostol and most side effects were similar in both groups, but heavy bleeding was more common in the sublingual group 41 . Two studies reported that oral misoprostol or vaginal of 800 ug was comparable in terms of efficacy while more side effects were reported in oral misoprostol of 800 ug in one study 42 , 43 . Further research on the efficacy and tolerability of sublingual or oral misoprostol of 800 ug is needed. At present, these regimens should not be regarded as the first-line of medical treatment of missed abortion.
In our work, complete abortion rate was calculated within about 24 hours. Seldom studies reported complete abortion rate within longer follow-up time, they suggested follow-up care to be offered one week following drug administration to ensure the highest success rate 43 , 44 , 45 . Due to the limited amounts of studies, it is difficult to draw any conclusions. The security of waiting at home needs further researched, especially for the incidence of excessive bleeding. For women needed emergency operation, cervical ripening was prepared due to the medical treatment and it is convenient to perform dilatation and curettage 24 , 26 .
Despite the foregoing advantages, serious consideration should be given to the contraindication before planning for medical treatment for women with missed abortion. A missed early miscarriage (<14 weeks of gestation) should be defined by ultrasound findings and suspected ectopic pregnancy must be excluded. Women with unstable hemodynamics, signs of pelvic infections or sepsis also need to be excluded. Detailed medical histories, including the distance between home and hospital, past medical history, previous surgical history, allergic history, medication history, should be recorded. Medical treatment can only be considered in women without following contraindications: known allergy to misoprostol, previous caesarean section, mitral stenosis, hypertension, glaucoma, bronchial asthma, use of non-steroidal drugs and remote areas without hospital around.
All women must be informed of the advantages and disadvantages of surgical and medical treatment. For women who choose medical treatment, hospitalization is not necessary, but the follow-up period will be more important. Pain killers and anti-emetics, such as paracetamol and metoclopramide, should be offered to them as needed 20 . All women should be advised to contact the doctor in case of heavy bleeding or signs of infection. A follow-up visit is recommended to perform within 2 weeks after treatment. Pregnancy test, physical examination of the uterus, and ultrasound should be performed to confirm the status of abortion. In the event of failure, surgical management maybe needed.
One of the strengths of our study is the inclusion of only randomized clinical trial data in a specific population (i.e., women with missed abortion of no more than 14 weeks of gestation). Our meta-analysis included all studies published so far on this topic and statistical tests showed no significant potential publication biases. The protocol of this review was registered on the International Prospective Register of Systematic Reviews before the selection of articles.
Limitations of this analysis are obvious. For a net-work meta-analysis, only 18 studies were included in this analysis which might affect the accuracy of the results. For this reason, comparisons could not be performed for some results. Most of the included studies were not double blind. This was therefore a considerable source of bias that may have affected treatment or performance of these women. We classified the interventions according to the first dose, however it is obvious that different max doses or medication intervals will affect the results.
The relation between max doses or medication intervals with complete abortion rate or side effects need to be further researched. Another remaining question is whether there are methods to reduce the incidence of side effects when treated with misoprostol. Further studies should focus on the quality of trails, especially for the blinding of participants and researchers.
In conclusion, misoprostol is a non-invasive, effective medical method for completion of abortion in missed abortion. Sublingual misoprostol of 600 ug or vaginal misoprostol of 800 ug may be a good choice for the first dose. The ideal dose and medication interval of misoprostol however needs to be further researched.
Search strategy and selection criteria
For this meta-analysis, we searched PubMed, the Cochrane Library, Embase, EBSCOhost Online Research Databases, Springer Link, ScienceDirect, Web of Science, Ovid Medline and Google Scholar for randomized controlled trials (RCTs) published from the date of database inception to August 15th, 2016, comparing different routes of administration of misoprostol in the medical management of missed abortion. We also searched some related journals. No language or publication type limits were applied. The reference lists of selected articles were hand searched to identify any relevant articles. Study authors were contacted to supplement incomplete reports of the original papers. Detailed search strategy can be found in Supplementary Table S6 .
Considering the gestational weeks available for surgical evacuation, women with missed abortion of no more than 14 weeks of gestation who received misoprostol treatment were assessed for inclusion into our meta-analysis. Women with incomplete abortion, threatened abortion or excessive uterine bleeding were excluded. Studies involving medical management with both mifepristone and misoprostol were also excluded.
We considered complete abortion rate for our primary analyses. Complete abortion was defined as complete expulsion of the products of conception without surgical intervention. Our secondary outcome was the side effects of misoprostol reported. The mean induction-abortion time would be also analyzed, if applicable.
Data extraction and quality assessment
Two researchers (H-L.W. and P.W.) performed their own search independently. Data extraction and check for accuracy were resolved by other two researchers (Q-M.W. and X.-W.C.). Duplicate or irrelevant articles were excluded by screening of titles and abstracts. All remaining articles were screened in full text. Relevant information from the included trials was extracted with a predefined data extraction sheet. All researchers assessed the risk of bias independently according to the Cochrane Handbook for Systematic Reviews of Interventions 46 . Specifically, attention was focused on seven domains, i.e., random sequence generation, allocation concealment blinding of participants and personnel, blinding of the outcome assessments, incomplete outcome data, selective reporting and other biases. The review authors’ judgments were categorized as low risk, high risk, or unclear risk of bias. We categorized the risk of bias as unclear when no reported information could be used. The article was reviewed and revised by another researcher (S.M.). Any discrepancies were resolved by discussion within the review team.
Statistical analysis
This study was registered with PROSPERO, number CRD42016046221. The full dataset is available online. After screening of the articles, we found the interventions in included articles were so varied in both the routes and doses of misoprostol that we could not carry out a direct comparison. We chose to perform a network meta-analysis instead. The strategies for data synthesis remained unchanged and the predefined analysis of subgroups with different doses was cancelled.
This network meta-analysis used all the available evidence, both direct and indirect, to evaluate relative effects of different routes or doses of misoprostol 47 , 48 . Statistical analysis was performed with STATA (version 12.0). We used a continuity correction for studies with no events by adding 0.5 to both the events count and the total sample size. We presented results as summary risk ratio (RR) for dichotomous data and the mean difference (MD) for continuous data, both with 95% confidence intervals (CIs). Inconsistency between direct and indirect sources of evidence was statistically assessed by calculation of the difference between direct and indirect estimates in all closed loops in the network. Random effects models were used to estimate the inconsistency. If there was no inconsistency between direct and indirect sources of evidence, fixed effects models would be used in further analysis, otherwise random effects models would still be used and sensitivity analyses would be performed to exclude studies with possibilities of causing bias in the close loops. A comparison-adjusted funnel plot was used to detect publication bias and small study effect. We estimated the ranking probabilities for all treatments of being at each possible rank for each intervention and the treatment hierarchy was summarized and presented as surface under the cumulative ranking curve 49 .
Wood, S. L. & Brian, P. H. Medical management of missed abortion: a randomized clinical trial. Obstet Gynecol. 99 , 563–566 (2002).
CAS PubMed Google Scholar
Joint study of Royal College of general practitioner and Royal College of obstetrician and gynaecologist. Induced abortion operations and their early sequelae. J R Coll Gen Pract . 35 , 175–180 (1985).
Chia, K. V. & Ogbo, V. I. Medical termination of missed abortion. J Obstet Gynaecol. 22 , 184–186, doi: 10.1080/01443610120113382 (2002).
Article CAS PubMed Google Scholar
Petrou, S., Trinder, J., Brocklehurst, P. & Smith, L. Economic evaluation of alternative management methods of first-trimester miscarriage based on results from the MIST trial. BJOG. 113 , 879–889, doi: 10.1111/j.1471-0528.2006.00998.x (2006).
Jukovic, D., Ross, J. A. & Nicoladies, K. H. Expectant management of missed miscarriage. Br J Obstet Gynaecol. 105 , 670–671, doi: 10.1111/bjo.1998.105.issue-6 (1998).
Article Google Scholar
Neilsen, S. & Hahlin, M. Expectant management of first-trimester spontaneous abortion. Lancet. 345 , 84–86, doi: 10.1016/S0140-6736(95)90060-8 (1995).
Luise, C. et al . Outcome of expectant management of spontaneous first trimester miscarriage: observational study. BMJ. 324 , 873–875, doi: 10.1136/bmj.324.7342.873 (2002).
Article PubMed PubMed Central Google Scholar
Huchon, C. et al . Pregnancy loss: French clinical practice guidelines. European Journal of Obstetrics & Gynecology and Reproductive Biology. 201 , 18–26, doi: 10.1016/j.ejogrb.2016.02.015 (2016).
Article CAS Google Scholar
Anderson, J. et al . A randomised controlled trial of oral versus vaginal misoprostol for medical management of early fetal demise. International Journal of Gynecology and Obstetrics. 107 , S533–S533, doi: 10.1016/S0020-7292(09)61912-3 (2009).
Kushwah, D. S., Kushwah, B., Salman, M. T. & Verma, V. K. Acceptability and safety profile of oral and sublingual misoprostol for uterine evacuation following early fetal demise. Indian J Pharmacol. 43 , 306–310, doi: 10.4103/0253-7613.81513 (2011).
Article CAS PubMed PubMed Central Google Scholar
Leladier, C. et al . Mifepristone (RU 486) induces embryo expulsion in first trimester non-developing pregnancies: a prospective randomised trial. Hum Reprod. 8 , 492–495, doi: 10.1093/oxfordjournals.humrep.a138078 (1993).
Gronlund, A. et al . Management of missed abortion: comparison of medical treatment with either mifepristone misoprostol or misoprostol alone with surgical evacuation. A multi-center trial in Copenhagen county, Denmark. Acta Obstet Gynecol Scand. 81 , 1060–1065, doi: 10.1034/j.1600-0412.2002.811111.x (2002).
Article PubMed Google Scholar
Nielsen, S., Hahlin, M. & Platz-Christensen, J. J. Unsuccessful treatment of missed abortion with a combination of an antiprogesterone and a prostaglandine E1 analogue. Br J Obstet Gynaecol. 104 , 1094–1096, doi: 10.1111/bjo.1997.104.issue-9 (1997).
Tasnee, S., Gul, M. S., Navid, S. & Alam, K. Efficacy and safety of misoprostolin missed miscarriage in terms of blood loss. Rawal Medical Journal 39 , 314–318 (2014).
Google Scholar
Seyam, Y. S., Flamerzi, M. A., Abdallah, M. M. & Ahmed, B. Vaginal misoprostol in the management of first trimester non-viable pregnancy. Qatar Medical Journal. 17 , 14–19 (2007).
Poveda, C. et al . Intrauterine misoprostol: a new high effective treatment of missed abortion. Fertility and Sterility. 76 , S96, doi: 10.1016/S0015-0282(01)02284-1 (2001).
Sharma, D., Singhal, S. R. & Rani, X. X. Sublingual misoprostol in management of missed abortion in India. Trop Doct. 37 , 39–40, doi: 10.1258/004947507779952023 (2007).
EI-Sokkary, H. H. Comparison Between Sublingual and Vaginal Administration of Misoprostol in Management of Missed Abortion. J Obstet Gynaecol India. 66 , 24–29, doi: 10.1007/s13224-015-0757-y (2016).
Haberal, A., Celikkanat, H. & Batioglu, S. Oral misoprostol use in early complicated pregnancy. Adv Contracept. 12 , 139–143, doi: 10.1007/BF01849635 (1996).
National Institute for Health and Care Excellence guidelines. Ectopic pregnancy and miscarriage: diagnosis and initial management. www.nice.org.uk/guidance/cg154 (2012).
Prasartsakulchai, C. & Tannirandorn, Y. A comparison of vaginal misoprostol 800 microg versus 400 microg in early pregnancy failure: a randomized controlled trial. J Med Assoc Thai. 87 , S18–23 (2004).
PubMed Google Scholar
Seervi, N. et al . Comparison of different regimes of misoprostol for the termination of early pregnancy failure. Medical Journal Armed Forces India. 70 , 360–363, doi: 10.1016/j.mjafi.2014.08.012 (2014).
Shah, N., Azam, S. I. & Khan, N. H. Sublingual versus vaginal misoprostol in the management of missed miscarriage. J Pak Med Assoc. 60 , 113–116 (2010).
Marwah, S. et al . A Comparative Study to Evaluate the Efficacy of Vaginal vs Oral Prostaglandin E1 Analogue (Misoprostol) in Management of First Trimester Missed Abortion. J Clin Diagn Res. 10 , Qc14–18, doi: 10.7860/JCDR/2016/18178.7891 (2016).
CAS PubMed PubMed Central Google Scholar
Akanksha, L., Ramanjeet, K. & Priya, S. A study to compare the clinical outcome of sublingual and vaginal misoprostol in the medical management. Int J Reprod Contracept Obstet Gynecol. 5 , 491–494 (2016).
Tanha, F. D., Feizi, M. & Shariat, M. Sublingual versus vaginal misoprostol for the management of missed abortion. J Obstet Gynaecol Res. 36 , 525–532, doi: 10.1111/j.1447-0756.2010.01229.x (2010).
Rita, G. S. & Kumar, S. A randomised comparison of oral and vaginal misoprostol for medical management of first trimester missed abortion. JK Science 8 , 35–38 (2006).
Ayudhaya, O. P., Herabutya, Y., Chanrachakul, B. & Ayuthaya, N. I. O-Prasertsawat,P. A comparison of the efficacy of sublingual and oral misoprostol 400 microgram in the management of early pregnancy failure: a randomized controlled trial. J Med Assoc Thai. 89 (Suppl 4), S5–10 (2006).
Hombalegowda, R. B., Samapthkumar, S., Vana, H., Jogi, P. & Ramaiah, R. A randomized controlled trial comparing different doses of intravaginal misoprostol for early pregnancy failure. Contraception. 92 , 364–365, doi: 10.1016/j.contraception.2015.06.051 (2015).
Srikhao, N. & Tannirandorn, Y. A comparison of vaginal misoprostol 800 microg versus 400 microg for anembryonic pregnancy: a randomized comparative trial. J Med Assoc Thai. 88 (Suppl 2), S41–47 (2005).
Kovavisarach, E. & Jamnansiri, C. Intravaginal misoprostol 600 microg and 800 microg for the treatment of early pregnancy failure. Int J Gynaecol Obstet. 90 , 208–212, doi: 10.1016/j.ijgo.2005.04.016 (2005).
Suchonwanit, P. Comparative study between vaginal misoprostol 200 mg and 400 mg in first trimester intrauterine fetal death and anembryonic gestation. Thai Journal of Obstetrics and Gynaecology. 11 , 263 (1999).
Tang, O. S., Schweer, H., Seyberth, H. W., Lee, S. W. & Ho, P. C. Pharmacokinetics of different routes of administration of misoprostol. Hum Reprod. 17 , 332–336, doi: 10.1093/humrep/17.2.332 (2002).
Pongsatha, S. & Tongsong, T. Randomized comparison of dry tablet insertion versus gel form of vaginal misoprostol for second trimester pregnancy termination. J Obstet Gynaecol Res. 34 , 199–203, doi: 10.1111/j.1447-0756.2008.00757.x (2008).
Saichua, C. & Phupong, V. A randomized controlled trial comparing powdery sublingual misoprostol and sublingual misoprostol tablet for management of embryonic death or anembryonic pregnancy. Arch Gynecol Obstet. 280 , 431–435, doi: 10.1007/s00404-009-0947-x (2009).
Bhattacharjee, N. et al . A randomized comparative study on vaginal administration of acetic acid-moistened versus dry misoprostol for mid-trimester pregnancy termination. Arch Gynecol Obstet. 285 , 311–316, doi: 10.1007/s00404-011-1949-z (2012).
Pongsatha, S. & Tongsong, T. Randomized controlled study comparing misoprostol moistened with normal saline and with acetic acid for second-trimester pregnancy termination. Is it different? J Obstet Gynaecol Res. 37 , 882–886, doi: 10.1111/jog.2011.37.issue-7 (2011).
Creinin, M. D., Carbonell, J. L., Schwartz, J. L., Varela, L. & Tanda, R. A randomized trial of the effect of moistening misoprostol before vaginal administration when used with methotrexate for abortion. Contraception. 59 , 11–16, doi: 10.1016/S0010-7824(98)00142-5 (1999).
Jain, J. K. & Mishell, D. R. A comparison of misoprostol with and without laminaria tents for induction of second-trimester abortion. Am J Obstet Gynecol. 175 , 173–177, doi: 10.1016/S0002-9378(96)70270-3 (1996).
Jmylyan, M. & Hydry, M. Comparison of the Efficacy of Castor Oil and Vaginal Misoprostol With Vaginal Misopostol Alone for Treatment of Missed Abortion. Arak Medical University Journal. 18 , 30–38 (2015).
Areerat, S. & Teerapat, C. Comparison of sublingual and vaginal misoprostol for termination of early pregnancy failure. Thai J Obstet Gynaecol. 22 , 128–136 (2014).
Mohammed, S. Oral versus vaginal misoprostol for termination of frist trimester missed abortion. MSc for Cairo University . http://www.erepository.cu.edu.eg/index.p-hp/cuth eses/thesis/view/13990 (2013).
Ngoc, N. T., Blum, J., Westheimer, E., Quan, T. T. & Winikoff, B. Medical treatment of missed abortion using misoprostol. Int J Gynaecol Obstet. 87 , 138–142, doi: 10.1016/j.ijgo.2004.07.015 (2004).
Tang, O. S., Lau, W. N., Ng, E. H., Lee, S. W. & Ho, P. C. A prospective randomized repeated doses of vaginal study to compare the use of with sublingual misoprostol in the management of first trimester silent miscarriages. Hum Reprod. 18 , 176–81, doi: 10.1093/humrep/deg013 (2013).
Tang, O. S. et al . A randomized trial to compare the use of sublingual misoprostol with or without an additional 1 week course for the management of first trimester silent miscarriage. Hum Reprod. 21 , 189–92, doi: 10.1093/humrep/dei303 (2006).
Higgins, J. G. S. Cochrane Handbook for Systematic reviews of Interventions (v5.1.0). http://handbook.cochrane.org/ (2011).
Caldwell, D. M., Ades, A. E. & Higgins, J. P. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 331 , 897–900, doi: 10.1136/bmj.331.7521.897 (2005).
Dias, S., Ades, A., Sutton, A. & Welton, N. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making. 33 , 607–617, doi: 10.1177/0272989X12458724 (2013).
Salanti, G., Ades, A. E. & Ioannidis, J. P. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 64 , 163–171, doi: 10.1016/j.jclinepi.2010.03.016 (2011).
Download references
Acknowledgements
We would like to thank all authors who shared their valuable data for the purpose of this meta-analysis.
Author information
Authors and affiliations.
Department of Obstetrics and Gynaecology, Hangzhou Women’s Hospital, Hangzhou, 310008, Zhejiang, China
Hang-lin Wu, Pei Wang, Qiu-meng Wang & Xiao-wen Chen
Department of Obstetrics and Gynaecology, VMMC and Safdarjung Hospital, New Delhi, 110029, India
Sheeba Marwah
You can also search for this author in PubMed Google Scholar
Contributions
H.-L.W. designed the study, conducted the article searching, and drafted the paper. P.W. conducted the article searching. Q.-M.W. and X.-W.C. analyzed and interpreted the data. S.M. revised the paper. All researchers reviewed the manuscript and participated the discussion within the review team.
Corresponding author
Correspondence to Hang-lin Wu .
Ethics declarations
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wu, Hl., Marwah, S., Wang, P. et al. Misoprostol for medical treatment of missed abortion: a systematic review and network meta-analysis. Sci Rep 7 , 1664 (2017). https://doi.org/10.1038/s41598-017-01892-0
Download citation
Received : 27 October 2016
Accepted : 05 April 2017
Published : 10 May 2017
DOI : https://doi.org/10.1038/s41598-017-01892-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The relationship between heavy metals and missed abortion: using mediation of serum hormones.
Biological Trace Element Research (2023)
Effect of obesity on the time to a successful medical abortion with misoprostol in first-trimester missed abortion
- Zekiye Soykan Sert
- Mete Bertizlioğlu
Archives of Gynecology and Obstetrics (2022)
Therapie der „missed abortion“ – wo stehen wir?
- Alexander Freis
Gynäkologische Endokrinologie (2021)

Efficacy and safety of myrrh in patients with incomplete abortion: a randomized, double-blind, placebo-controlled clinical study
- Homeira Vafaei
- Sara Ajdari
- Shohreh Roozmeh
BMC Complementary Medicine and Therapies (2020)
Serum Levels of Collectins Are Sustained During Pregnancy: Surfactant Protein D Levels Are Dysregulated Prior to Missed Abortion
- Kavita Kale
- Pallavi Vishwekar
- Taruna Madan
Reproductive Sciences (2020)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Abortion policy is changing every day. Minors are the most vulnerable– and the least understood
Youth Reproductive Equity kicks off a new research agenda today on minor abortion access
ANN ARBOR – Time magazine ran a profile last summer about “Ashley,” a 13-year-old girl who went nearly mute after she was raped outside of her home in Mississippi: For weeks, she didn’t tell anyone what had happened, and with state abortion bans set into motion following the Supreme Court’s Dobbs decision, she had no practical options but to deliver the baby before she started seventh grade. The story was one of many that have surfaced to show the human impacts of Dobbs, the U.S. Supreme Court decision that overturned the nationwide right to abortion– but how many teens are in the position of seeking abortions they can’t obtain? How do minors learn about abortion access or decide whether and how to seek reproductive healthcare? How are they navigating and experiencing the changing landscape of abortion access, and restrictions that accrue to minors in particular? We don’t know– because those data do not exist.
Research Gap
Abortion access policy disproportionately affects adolescents, but we know strikingly little about this population. Next month will mark two years since the U.S. Supreme Court’s Dobbs decision, and an ocean of research has investigated the impacts of legislation that is changing every day as states press for new policies to restrict or protect abortion access. More than 14,000 articles on “abortion after Dobbs” can be found today on Google Scholar . But the impact of these changes on minors–teens aged 17 or younger with often different legal rights – is a critical area of focus that has been largely overlooked, according to Youth Reproductive Equity, a national collaborative of researchers and clinician-scientists that today launched a report aimed to address this gap.
“Minors are a marginalized group who already face additional barriers to abortion access, have fewer protections, and receive differential treatment under the law,” said lead author Julie Maslowsky, an affiliate of the University of Michigan School of Nursing and the Population Studies Center at the Institute for Social Research. “This is a problem of equity because all people, regardless of age, are entitled to the right of bodily autonomy. It is an issue of scientific rigor because we are systematically excluding one part of the population who are impacted by changing abortion laws from our studies.”
A Research Agenda for Adolescents and Abortion
The new report, “ Adolescence Post-Dobbs: A Policy-Driven Research Agenda for Minor Adolescents and Abortion ,” presents an overview of today’s policy landscape, principles and questions for future research, and recommendations to overcome challenges that limit research and policy change for minors. The report is derived from the proceedings of an expert consensus panel representing key constituencies: Researchers, reproductive health organization leaders, clinicians, law and policy experts, and a group that is not often at the table– young people themselves.
Minors aged 17 or younger account for about 4 percent of all abortions in the formal healthcare system. We know that some 25,000 minors received abortion care each year, prior to Dobbs – but we don’t know how many were unable to obtain a wanted abortion. We know that more than two-thirds of pregnancies to minors are unintended– more than other groups, and that minors’ pregnancies were more likely to end in abortion than adults’ pregnancies, prior to Dobbs . Post- Dobbs , adolescents living in states with severe abortion restrictions or bans are expected to be less likely to access abortion than adults. Adults are more likely to be able to travel to another state or access care through telehealth or online options. In Texas– one of the first states to enact a 6-week abortion ban– adolescents showed the largest decrease in their abortion rate compared to other age groups. In the rapidly shifting state policy environment, minors are often targeted by restrictive policies – like parental consent requirements or new “abortion trafficking” laws that criminalize helping minors cross state lines for abortion access – and they are often left out of protective ones, Maslowsky said. Further, adolescents also face particular barriers to pregnancy prevention– including access to contraception and to comprehensive sex education that includes information about pregnancy prevention and abortion.
The Post- Dobbs Landscape
The Guttmacher Institute yesterday identified “attacks on youth reproductive autonomy” as a key trend in its first quarterly report on state reproductive health policy. Its recent study out last month on the characteristics of adolescents obtaining abortions in the US concluded that this population is “more vulnerable” than adults, and that adolescents navigate unique barriers to both information and logistics to access care. Multiple factors delay abortion care for this age group– including mandated counseling and waiting periods, mandated ultrasound viewing, parental involvement laws, financial barriers, transportation challenges, and limited availability of care. Compared to adults, adolescents are more likely to report not knowing they are pregnant– as some may not recognize signs of pregnancy or have more irregular cycles that make a missed period less concerning. Compared to adults, the Guttmacher study found, adolescents were more likely to report not knowing they were pregnant (57% vs. 43%), not knowing where to obtain an abortion (19% vs. 11%), or that they were looking into insurance (12% vs. 5%). The report was based on Guttmacher’s 2021-22 Abortion Patient Survey, with 6,698 respondents – but because they represent only a small percentage of the population, only 156 minors were included. In reporting the study limitations, the authors acknowledged the data were not nationally representative, the sample included too few minors to do a more comprehensive analysis of the population, and the study did not capture people who wanted abortions but were unable to travel to a facility. While important, this report showcases the prevailing challenge– there is not enough data about adolescents and abortion to provide needed information and perspectives.
Meanwhile, more than half of American adolescents, aged 13 to 19, now live in states with severely restricted or no legal abortion access.
The details of cases involving minors can be found in testimonies provided to lawmakers and in news stories that paint a picture of a policy landscape that may be confusing, hostile, frightening, and dangerous to navigate. Abortion restrictions have impacted women and girls seeking interventions for life-threatening conditions and medications used to make miscarriages safer. In a post- Dobbs case in Florida, a judge denied a 17-year-old a parental consent waiver for an abortion, citing her C-average grades. A highly publicized case just days after the SCOTUS ruling involved a rape victim who fled Ohio to seek an abortion at six-and-a-half weeks in Indianapolis; she was 10 years old .
But while experiences and anecdotes like these accumulate, researchers face particular barriers to gathering evidence about minors and struggle to gather data at scales that are sufficient for robust insights.
Research Challenges
“Minors are a major blindspot in abortion research that need to be addressed,” said Laura Lindberg of the Rutgers School of Public Health, a co-author of the Youth Reproductive Equity report. “We need research that incorporates minors’ experiences, corrects the misperception that minors aren’t competent to make decisions, and guides funders and Institutional Review Boards about feasibility and best practices to break through challenges we face in efforts to conduct needed research.”
Those challenges include small samples of minors in abortion surveillance efforts, age groupings in national data that combine minors and non-minors, research gaps on the systems and contexts involved in minor abortion information, access, and care, and limited focus on the unique experiences of minors and parents navigating those systems, according to Youth Reproductive Equity. Their report includes recommendations and research questions in four areas of policy: access to abortion, access to abortion information, parental/adult involvement, and privacy and confidentiality, a category that includes electronic record sharing and criminalization of self-managed abortion.
Implications
Filling these research gaps may help guide practitioners and policymakers in an era of legislative flux. As of February, 14 states have enacted near-total abortion bans, three states have bans under litigation, and seven have lowered their gestational threshold for abortion to 20 weeks or less. The Supreme Court will rule this year on the closely-watched case that would restrict access to the “abortion pill” mifepristone, and the invocation of 19th-century Comstock Laws in that case by conservative justices was concerning to advocates of reproductive rights. Those laws– which were inactionable under Roe– banned the mailing of “lewd” content and materials for abortion or contraception. Several states– including Oklahoma , Tennessee , Idaho , and Alabama – have moved to consider bills banning minors from crossing state lines to seek abortions without parental consent. A TV response ad entitled “ The Fugitive ,” running in Alabama, includes a scene reminiscent of A Handmaid’s Tale : A highway patrolman pulls over two frightened young women, tapping the driver-side window with a home pregnancy test. Several states will vote on abortion in the upcoming election, and reproductive rights will figure as a top issue.
“It would be useful to have a larger body of research about adolescents and minors who get abortion care in all different kinds of contexts, and all different kinds of policy environments,” said Rachel Jones, a principal research scientist at Guttmacher who focuses on domestic abortion research. Most young people do involve their parents in making decisions about pregnancy, said Jones, but it would help legislators to understand the circumstances of those who don’t. Jones said the Guttmacher study suggested minors may be less likely to opt for medication abortion, but that further research would be needed to understand the replicability and implications of that finding. Given their vulnerability, it would benefit the field if foundations were more proactive about supporting research on minors who have abortions, and the barriers they face, she said.
“Historically, young people have always been the first people dismissed when it comes to reproductive care, including abortion care,” said Kylee Sunderlin of the reproductive justice organization If/When/How , whose role as a Michigan judicial bypass lawyer is to represent pregnant minors who must ask a judge to grant the right to obtain an abortion without state-mandated parental involvement. We see this reflected in the maze of laws around the country requiring parental involvement or judicial bypass, in state bills seeking to block young people’s access to abortion, as well as in ballot measures that focus on increasing abortion access but have negotiated young people out of the expansions– as we saw in the Michigan Reproductive Health Act, she said.
“As a lawyer who relies on research for amicus briefs and policy change, I have a front row seat to the ways that the absence of impactful research on sexual and reproductive health for young people has resulted in profound harm,” said Sunderlin. “The Youth Reproductive Equity report not only shows why, in stark terms, we cannot continue to ignore young people, but it also creates a clear roadmap for equitable and actionable research to remedy this gap.”
“If we understand parent perspectives, we can better inform policies about parental involvement that are often a barrier to adolescents’ desired pregnancy outcomes and result in delays in care,” said Maslowsky. “With young people’s perspectives, we will be able to counter restrictions that are based on a non-evidence based narrative that minors aren’t mature enough to make decisions. There are many questions that need to be asked to support stakeholders, make timely decisions, and understand the long-term impacts of these new restrictions.”
“The most consequential data for the work I do supporting young people is about the harms of forced parental involvement laws, the judicial bypass process, and ultimately, what it means to force a young person into birth. Because without a supportive parent or a judicial bypass, then the state is forcing young people into the incredible trauma of forced birth,” said Sunderlin. “Restricting young people’s bodily autonomy is affirmatively harmful. I hope that by hearing this—either directly from young people or indirectly through research—that the people making decisions about young people’s lives will actually start caring about them.”
With Maslowsky and Lindberg, Emily Mann of the University of South Carolina co-authored the Youth Reproductive Equity report.
This post was written by Tevah Platt of the University of Michigan Population Studies Center at the Institute for Social Research.

- Missed miscarriage
- Report problem with article
- View revision history
Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
At the time the article was last revised Yuranga Weerakkody had no recorded disclosures.
- Missed abortion
- Early fetal demise
- Early intrauterine fetal demise
- Early loss of pregnancy
A missed miscarriage , sometimes termed a missed abortion 3 , is a situation when there is a non-viable fetus within the uterus , without symptoms of a miscarriage .
Radiographic features
Ultrasound diagnosis of miscarriage should only be considered when either a mean gestation sac diameter is ≥25 mm with no obvious yolk sac or a fetal pole with a crown rump length of ≥7 mm without evidence of fetal cardiac activity.
Transvaginal ultrasound is the mainstay in the diagnosis of miscarriage. Once the diagnosis of miscarriage is made based on the above ultrasound criteria, the patient can then be offered different types of management depending on their clinical status and patient's choice.
Treatment and prognosis
Expectant management is possible, with a "wait and watch" approach can be offered after careful counseling to women who have met the inclusion criteria:
- patient's preference once miscarriage is diagnosed based on ultrasound findings
- incomplete miscarriage
For medical management, misoprostol is the drug of choice. Surgical management is dilatation and curettage. Inclusion criteria:
- patient's preference
- haemodynamically unstable
- persistent excessive bleeding
- evidence of infected retained tissue
- suspected gestational trophoblastic disease
- unsuccessful expectant or medical management
- recurrent miscarriage, to assess for cytogenetics
- 1. Bernard K & Cooperberg P. Sonographic Differentiation Between Blighted Ovum and Early Viable Pregnancy. AJR Am J Roentgenol. 1985;144(3):597-602. doi:10.2214/ajr.144.3.597
- 2. Harris R & Barth R. Sonography of the Gravid Uterus and Placenta: Current Concepts. AJR Am J Roentgenol. 1993;160(3):455-65. doi:10.2214/ajr.160.3.8430536
- 3. Trinder J, Brocklehurst P, Porter R, Read M, Vyas S, Smith L. Management of Miscarriage: Expectant, Medical, or Surgical? Results of Randomised Controlled Trial (Miscarriage Treatment (MIST) Trial). BMJ. 2006;332(7552):1235-40. doi:10.1136/bmj.38828.593125.55
Incoming Links
- Differential diagnosis for PV bleeding in pregnancy
- Miscarriage
- Mean sac diameter
- Early pregnancy
- Crown rump length
- Threatened miscarriage
- Partial hydatidiform mole
- DCDA pregnancy co-twin demise and ovarian torsion
- Failed early pregnancy
- Cervical ectopic pregnancy
- Failed early pregnancy - missed miscarriage
Related articles: Pathology: Genitourinary
- mean sac diameter (MSD)
- empty gestational sac
- crown rump length (CRL)
- fetal tachycardia
- fetal bradycardia
- fetal bradyarrhythmia(s)
- gestational age
- physiologic gut herniation
- embryonic rhombencephalon
- beta-hCG levels
- double decidual sac sign
- intradecidual sign
- double bleb sign
- pregnancy of unknown location (PUL)
- pseudogestational sac
- decidual cast
- eccentric gestational sac
- interstitial line sign
- ovarian ectopic
- cervical ectopic
- scar ectopic
- abdominal ectopic
- live ectopic pregnancy
- heterotopic pregnancy
- tubal rupture
- pregnancy of uncertain viability (PUV)
- irregular gestational sac
- missed miscarriage
- inevitable miscarriage
- complete miscarriage
- anembryonic pregnancy in the exam
- irregular yolk sac
- calcified yolk sac
- echogenic yolk sac
- small yolk sac
- large yolk sac
- gestational trophoblastic disease
- subchorionic hemorrhage
- monochorionic monoamniotic twin pregnancy
- monochorionic diamniotic twin pregnancy
- dichorionic diamniotic twin pregnancy
- twin peak sign
- demise of a twin
- implantation bleeding
- early structural scan
- 11-13 weeks antenatal scan
- nuchal translucency
- biparietal diameter (BPD)
- head circumference (HC)
- abdominal circumference (AC)
- femur length (FL)
- amniotic fluid index
- maximal vertical pocket method
- two diameter pocket method
- polyhydramnios
- oligohydramnios sequence
- four chamber view (fetal)
- LVOT view (fetal)
- RVOT view (fetal)
- non-visualization of the fetal stomach
- nuchal fold thickness
- ventriculomegaly
- hypoplastic nasal bone
- echogenic intracardiac focus
- choroid plexus cysts
- enlarged cisterna magna
- shortened femur
- shortened humerus
- echogenic fetal bowel
- aberrant right subclavian artery
- fetal pyelectasis / fetal renal pelvic dilatation
- sandal gap toes
- amnioreduction
- single umbilical artery
- absent umbilical arterial end diastolic flow
- reversal of umbilical arterial end diastolic flow
- fetal MCA pulsatility index (PI)
- fetal MCA peak systolic velocity (PSV)
- fetal MCA systolic/diastolic (S/D) ratio
- abnormal ductus venosus waveforms
- umbilical venous flow assessment
- uterine artery flow notching
- chorionic villus sampling (CVS) and amniocentesis
- fetal death in utero
- retained products of conception
- small placenta
- placentomegaly
- placental calcification
- placental venous lakes
- bilobed placenta
- succenturiate lobe
- circumvallate placenta
- circummarginate placenta
- placenta membranacea
- placenta fenestrata
- horse shoe shaped placenta
- low-lying placenta
- marginal previa
- partial previa
- complete previa
- placenta accreta
- placenta increta
- placenta percreta
- variation in cord insertion
- velamentous insertion of the cord
- marginal insertion of the cord
- vasa previa
- marginal placental abruption
- preplacental abruption
- retroplacental abruption
- traumatic abruptio placental scale (for CT)
- retroplacental hemorrhage
- placental infarction
- placental hemorrhage
- chorioamnionitis
- subchorionic cyst
- placental septal cyst
- placental chorioangioma
- placental chorioangiomatosis
- placental site trophoblastic tumor
- placental teratoma
- hydropic degeneration of placenta
- partial mole
- complete mole
- invasive mole
- choriocarcinoma
- dizygotic twin pregnancy
- monozygotic twin pregnancy
- placental fusion
- placental mosaicism
- placental trophotropism
- acute pelvic pain
- chronic pelvic pain
- abnormal endometrial thickness (differential)
- endometrial hyperplasia
- endometrioid carcinoma
- serous type adenocarcinoma of the endometrium
- clear cell type adenocarcinoma of the endometrium
- mucinous type adenocarcinoma of the endometrium
- endometrial polyp
- endometrial fluid
- tamoxifen-associated changes
- endometritis
- tubal occlusion device
- IUD perforation
- sonohysterography
- intramural leiomyoma
- subserosal leiomyoma
- submucosal leiomyoma
- adenomyosis
- lipoleiomyoma
- leiomyosarcoma
- c-section scar
- Mullerian agenesis or hypoplasia
- unicornuate uterus
- uterus didelphys
- bicornuate uterus
- septate uterus
- arcuate uterus
- DES-related uterine abnormalities
- cumulus oophorus
- ovarian torsion
- tubo-ovarian abscess complex
- ovarian cyst
- corpus luteum
- hemorrhagic ovarian cyst
- ruptured ovarian cyst
- endometrioma
- serous cystadenoma / serous cystadenofibroma
- borderline cystadenoma
- serous cystadenocarcinoma
- ovarian mucinous cystadenoma
- ovarian borderline mucinous tumor
- ovarian mucinous cystadenocarcinoma
- fibrothecoma
- granulosa cell tumors of the ovary
- Krukenberg tumor
- paraovarian cyst
- polycystic ovaries
- ovarian hyperstimulation syndrome
- post-hysterectomy ovary
- cervical stenosis
- cervical polyp
- cervical cancer
- cervical fibroid
- hydrosalpinx
- hematosalpinx
- pelvic congestion syndrome
- peritoneal inclusion cyst
- prostate biopsy
- extracapsular extension
- prostate peripheral zone T2 hypointensity
- dynamic contrast enhancement
- MR spectroscopy
- Gleason score
- prostate sarcoma
- acute bacterial prostatitis
- chronic bacterial prostatitis
- chronic prostatitis and chronic pelvic pain syndrome (CPPS)
- asymptomatic inflammatory prostatitis
- prostatic tuberculosis
- emphysematous prostatitis
- prostatic abscess
- benign prostatic hypertrophy
- prostatic utricle cyst
- prostatic cystadenoma
- prostatic calcification
- prostatic infarction
- testicular torsion-detorsion syndrome
- testicular fracture
- testicular dislocation
- intratesticular hematoma
- testicular seminoma
- mixed germ cell tumor
- yolk sac tumor (endodermal sinus tumor)
- embryonal cell carcinoma
- testicular teratoma
- testicular epidermoid (teratoma with ectodermal elements only)
- burned out testis tumor
- Leydig cell tumor of the testis
- Sertoli cell tumor of the testis
- juvenile granulosa cell tumor of the testis
- fibroma-thecoma cell tumor of the testis
- gonadoblastoma
- testicular cyst
- testicular lymphoma
- testicular microlithiasis
- metastases to the testis
- spermatocele
- scrotoliths
- cyst of the tunica albuginea
- indirect inguinal hernia
- epididymo-orchitis
- epididymal abscess
- epididymal masses
- epididymal head cyst
- torsion of the epididymal appendix
- adenomatoid tumor
- epididymal leiomyoma
- polyorchidism
- cryptorchidism
- tubular ectasia of the rete testis
- cystadenoma of the rete testis
- testicular sarcoidosis
- testicular tuberculosis
- spermatic cord lipoma
- spermatic cord liposarcoma
- spermatic cord leiomyosarcoma
- fibrous pseudotumor of the scrotum
- scrotal leiomyosarcoma
- testicular adrenal rest tumors (TARTs)
- tunica vaginalis testis mesothelioma
- splenogonadal fusion
- testicular vasculitis
- abnormal testicular Doppler flow (differential)
- Peyronie's disease
- normal renal anatomy
- hydronephrosis
- urolithiasis
- clear cell renal cell carcinoma
- papillary renal cell carcinoma
- chromophobe renal cell carcinoma
- renal lymphoma
- renal angiomyolipoma
- simple renal cyst
- autosomal dominant polycystic kidney disease (ADPKD)
- autosomal recessive polycystic kidney disease (ARPKD)
- acquired renal cystic disease
- multicystic dysplastic kidney
- lithium-induced renal disease
- renal abscess
- xanthogranulomatous pyelonephritis
- emphysematous pyelonephritis
- renal tuberculosis
- renal artery stenosis
- renal vein thrombosis
- renal arteriovenous fistula
- renal trauma assessment
- normal ureter anatomy
- urothelial cell carcinoma
- tuberculous involvement of the urethra
- eosinophilic ureteritis
- vesico-urethral reflux (VUR)
- ectopic ureter
- ureteral duplication
- ureteral tumors
- ureteral trauma
- ureteral pseudodiverticulosis
- ureteritis cystica
- bladder diverticulum
- urothelial carcinoma of the bladder
- bladder outlet obstruction
- neurogenic bladder
- infectious cystitis
- cystitis following radiation or chemotherapy
- drug-induced bladder calculi
- pseudoureterocele
- cystitis cystica / cystitis glandularis
- interstitial cystitis
- emphysematous cystitis
- bladder urothelial cell carcinoma
- bladder adenocarcinoma
- bladder squamous cell carcinoma
- bladder small cell carcinoma
- patent urachus
- urachal cyst
- umbilical-urachal sinus
- vesicourachal diverticulum
- schistosomiasis
Promoted articles (advertising)
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

The independent source for health policy research, polling, and news.
Key Facts on Abortion in the United States
Usha Ranji , Karen Diep , and Alina Salganicoff Published: Nov 21, 2023
Note: This brief was updated on January 4, 2024 to correct the description of the data collected by the federal CDC Abortion Surveillance System. On June 24, 2022, the Supreme Court issued a ruling in Dobbs v. Jackson Women’s Health Organization that overturned the constitutional right to abortion as well as the federal standards of abortion access, established by prior decisions in the cases Roe v. Wade and Planned Parenthood v. Casey . Prior to the Dobbs ruling, the federal standard was that abortions were permitted up to fetal viability. That federal standard has been eliminated, allowing states to set policies regarding the legality of abortions and establish limits. Access to and availability of abortions varies widely between states , with some states banning almost all abortions and some states protecting abortion access.
This issue brief answers some key questions about abortion in the United States and presents data collected before and new data that was published shortly after the overturn of Roe v. Wade .
What is abortion?
How safe are abortions, how often do abortions occur, who gets abortions, at what point in pregnancy do abortions occur, where do people get abortion care, how much do abortions cost, does private insurance or medicaid cover abortions, what are public opinions about abortion.
Abortion is the medical termination of a pregnancy. It is a common medical service that many women obtain at some point in their life. There are different types of abortion methods, which the National Academy of Sciences, Engineering, and Medicine (NASEM ) places in four categories:
- Medication Abortion – Medication abortion, also known as medical abortion or abortion with pills, is a pregnancy termination protocol that involves taking oral medications. There are two widely accepted protocols for medication abortion. In the U.S., the most common protocol involves taking two different drugs, Mifepristone and Misoprostol. Typically, an individual using medication abortion takes Mifepristone first, followed by misoprostol 24-48 hours later. In the U.S., the Food and Drug Administration (FDA) has approved this protocol of medication abortion for use up to the first 70 days (10 weeks) of pregnancy, and its use has been rising for years. Another medication abortion protocol uses misoprostol alone . Patients can take 800 µg (4 pills) of misoprostol sublingually or vaginally every three hours for a total of 12 pills. The regimen is also recommended for up to 70 days (10 weeks) of pregnancy, but it is not currently approved by the FDA and is more commonly used in other countries.
Guttmacher Institute estimates that in 2020, medication was used for more than half (53%) of all abortions. While medication abortion has been available in the U.S. for more than 20 years, studies have found that many adults and women of reproductive age have not heard of medication abortion. Many have confused emergency contraception ( EC ) pills with medication abortion pills, but EC does not terminate a pregnancy. EC works by delaying or inhibiting ovulation and will not affect an established pregnancy.
- Aspiration , a minimally invasive and commonly used gynecological procedure, is the most common form of procedural abortion. It can be used to conduct abortions up to 14-16 weeks of gestation. Aspiration is also commonly used in cases of early pregnancy loss (miscarriage).
- Dilation and evacuation abortions (D&E) are usually performed after the 14th week of pregnancy. The cervix is dilated, and the pregnancy tissue is evacuated using forceps or suction.
- Induction abortions are rare and conducted later in pregnancy. They involve the use of medications to induce labor and delivery of the fetus.
( Back to top )
Decades of research have shown that abortion is a very safe medical service.
Despite its strong safety profile, abortion is the most highly regulated medical service in the country and is now banned in several states. In addition to bans on abortion altogether and telehealth, many states impose other limitations on abortion that are not medically indicated, including waiting periods, ultrasound requirements, gestational age limits, and parental notification and consent requirements. These restrictions typically delay receipt of services.
- NASEM completed an exhaustive review on the safety and effectiveness of abortion care and concluded that complications from abortion are rare and occur far less frequently than during childbirth.
- NASEM also concluded that safety is enhanced when the abortion is performed earlier in the pregnancy. State level restrictions such as waiting periods, ultrasound requirements, and gestational limits that impede access and delay abortion provision likely make abortions less safe.
- When medication abortion pills, which account for the majority of abortions, are administered at 9 weeks’ gestation or less, the pregnancy is terminated successfully 99.6% of the time, with a 0.4% risk of major complications, and an associated mortality rate of less than 0.001 percent (0.00064%).
- Medication abortion pills can be provided in a clinical setting or via telehealth (without an in-person visit). Research has found that the provision of medication abortion via telehealth is as safe and effective as the provision of the pills at an in person visit.
- Studies on procedural abortions, which include aspiration and D&E, have also found that they are very safe. Research on aspiration abortions, the most common procedural method, have found the rate of major complications of less than 1%.
There are three major data sources on abortion incidence and the characteristics of people who obtain abortions in the U.S: the Centers for Disease Control and Prevention (CDC), the Guttmacher Institute, and most recently, the Society of Family Planning’s (SFP) #WeCount project.
The federal CDC Abortion Surveillance System requests data from the central health agencies of the 50 states, DC, and New York City to document the number and characteristics of women obtaining abortions. Most states collect data from facilities where abortions are provided on the demographic characteristics of patients, gestational age, and type of abortion procedure. Reporting these data to the CDC is voluntary and not all states participate in the surveillance system. Notably, California, Maryland, and New Hampshire have not reported data on abortions to the CDC system for years. CDC publishes available data from the surveillance system annually.
Guttmacher Institute , an independent research and advocacy organization, is another major source of data on abortions in the U.S. Prior to the Dobbs ruling, Guttmacher conducted the Abortion Provider Census (APC) periodically which has provided data on abortion incidence, abortion facilities, and characteristics of abortion patients. Data from this Census are based primarily on questionnaires collected from all known facilities that provide abortion in the country, information obtained from state health departments, and Guttmacher estimates for a small portion of facilities. The most recent APC reports data from 2020.
The CDC and Guttmacher data differ in terms of methods, timeframe, and completeness, but both have shown similar trends in abortion rates over the past decade. One notable difference is that Guttmacher’s study includes continuous reporting from California, D.C., Maryland, and New Hampshire, which explains at least in part the higher number of abortions in their data.
Since the Dobbs ruling, the Guttmacher Institute has established the Monthly Abortion Provision Study to track abortion volume within the formal United States health care system. This ongoing effort collects data on and provides national and state-level estimates on procedural and medication abortions while also tracking the changes in abortion volume since 2020. The Monthly Abortion Provision Study was designed to complement Guttmacher’s APC along with other data collection efforts to allow for quick snapshots of the changing abortion landscape in the United States.
Society of Family Planning’s (SFP) #WeCount is another national reporting effort that measures changes in abortion access following the Dobbs ruling. The project reports on the number of abortions per month by state and includes data on abortions provided through clinics, private practices, hospitals, and virtual-only providers. The report does not include data on self-managed abortions that are performed without clinical supervision. The most recent #WeCount report analyzes data from April 2022 to data from June 2023, marking one full year of abortion data since Dobbs. The effort represents 83% of all providers known to #WeCount who agreed to participate in their research.
This KFF issue brief uses data from the CDC, Guttmacher, and SFP as well as other research organizations.
How has the abortion rate changed over time?
For most of the decade prior to the Dobbs ruling, there was a steady decline in abortion rates nationally, but there was a slight increase in the years just before the ruling.
In their most recent national data, Guttmacher Institute reported 930,160 abortions in 2020 and a rate of 14.4 per 1,000 women. CDC reported 622,108 abortions in 2021 and a rate of 11.6 abortions per 1,000 women (excludes CA, DC, MD, NH). Guttmacher’s study showed an upward trend in abortion from 2017 to 2020 whereas CDC’s report showed an increase in abortions from 2017 to 2021 except for a slight decrease in 2020.
While most attribute the long-term decline in abortion rates to increased use of more effective methods of contraception , several states had reduced access to low- or no-cost contraceptive care as a result of reductions in the Title X network under the Trump Administration, which may have contributed to the slight rise in abortions prior to the Dobbs ruling. Other factors that may have contributed to the increase could include greater coverage under Medicaid that subsequently made abortions more affordable in some states and broader financial support from abortion funds to help individuals pay for the costs of abortion care.
Even prior to the Dobbs ruling, abortion rates varied widely between states.
National averages can mask local and more granular differences. Lower state-level abortion rates do not reflect less need. Some of the variation has been due to the wide differences in state policies, with some states historically placing restrictions on abortion that make access and availability to nearly out of reach and, on the other side, some states enshrining protections in state Constitutions and legislation.
- In 2020, the abortion rate (per 1,000 women ages 15-44) ranged from 0.1 in Missouri to 48.9 in the District of Columbia (DC). Trends also varied between states. While the national rate of abortion increased between 2017 and 2019, some states saw declines, with particularly sharp drops in states where heavy restrictions were put into place.
While the number of abortions in the U.S. dropped immediately following the Dobbs decision, new data show that the number of abortions increased overall one year following the ruling. However, the upswing obscures the declines in abortion care in states with bans.
SFP’s #WeCount estimates there were 2,200 cumulative more abortions in the year following Dobbs (July 2022 to June 2023) compared to the pre- Dobbs period (April 2022 and May 2022). Nationally, the number of abortions varied month-by-month, with the largest decrease observed in November 2022 (73,930 abortions; 8,185 fewer abortions than pre- Dobbs period ) and the largest increase in March 2023 (92,680 abortions; 10,565 more abortions than pre- Dobbs period). The states with the largest cumulative increases in the total number of abortions provided by a clinician during the 12-month period include Illinois, Florida, North Carolina, California, and New Mexico. States with abortion bans experienced the largest cumulative decreases in the number of abortions, including Texas, Georgia, Tennessee, and Louisiana (data varies by month in each state; data not shown).
States without abortion bans experienced an increase of abortions following the Dobbs ruling likely due to a combination of reasons: increased interstate travel for abortion access, expanded in-person and virtual/telehealth capacity to see patients, increased measures to protect and cover abortion care for residents and out-of-state patients, and potentially reduced abortion-related stigma as a result of community mobilization around abortion care.
However, the overall national increase in the number of abortions masks the absence and/or scarcity of abortion care in states with total abortion bans or severe restrictions. States with total bans experienced observed 94,930 fewer clinician-provided abortions a year following the ruling (data not shown). Note, this figure is an underestimate due several state policies that restricted abortion access during the pre- Dobbs period. These estimates do not include abortions that may have been performed through self-managed means.
Most of the information about people who receive abortions comes from data prior to the Dobbs ruling. In 2021, women across a range of age groups, socioeconomic status, and racial and ethnic backgrounds obtained abortions, but the majority were obtained by women who were in their twenties, low-income, and women of color.
- Women in their twenties accounted for more than half (57%) of abortions. Nearly one-third (31%) were among women in their thirties and a small share were among women in their 40s (4%) and teens (8%).
- Seven in ten abortion patients were of women of color. Black women comprised 42% of abortion recipients, White women 30% , Hispanic women 22%, and 7% women of other races/ethnicities.
- Many women who sought abortions have children. More than six in 10 (61%) abortion patients in 2021 had at least one previous birth.
The vast majority (94%) of abortions occur during the first trimester of pregnancy according to data available from before the Dobbs decision.
Before the 2022 ruling in Dobbs, there was a federal constitutional right to abortion before the pregnancy is considered to be viable, that is, can survive outside of a pregnant person’s uterus. Viability is generally considered around 24 weeks of pregnancy. Most abortions, though, occur well before the point of fetal viability.
- Data from 2021 found that more than four in ten (45%) abortions occurred by six weeks of gestation, a third (36%) occurred between seven and nine weeks, and 13% at 10-13 weeks. Just 7% of abortions occurred after the first trimester.
- Prior to the decision in the Dobbs case, almost half of states (22) had enacted laws that ban abortion at a certain gestational age. Most of these limits are in the second trimester, but some are in the first trimester, well before fetal viability. Many of these laws were blocked because they violated the federal standard established by Roe v Wade. Some states have enacted laws banning abortions after fetal cardiac activity can be detected, or around 6 weeks of pregnancy, which is often before a person knows they are pregnant. In addition to banning abortion, states can now establish pre-viability gestational restrictions because the federal standard has been overturned.
Just over half of abortions were provided at clinics that specialize in abortion care in 2020. Others were provided at clinics that offer abortion care in addition to other family planning services.
Guttmacher Institute estimated that 96% of abortions were provided at clinics and just 4% were provided in doctors’ offices or hospitals in 2020. Most clinic-based abortions were provided at clinics that specialize in providing abortion care, but many were provided at clinics that offer a wide range of other sexual and reproductive health services like contraception and STI care. Most abortions are provided by physicians. However, in 19 states and D.C., Advanced Practice Clinicians (APCs) such as Nurse Practitioners and midwives may provide medication abortions. Conversely, 31 states prohibit clinicians other than physicians from providing abortion care.
Even prior to the ruling in Dobbs , access to abortion services was very uneven across the country though. The proliferation of restrictions in many states, particularly in the South, had greatly shrunk the availability of services in some areas. In the wake of overturning Roe v. Wade , these geographic disparities are likely to widen as more states ban abortion services altogether.
Telehealth has grown as a delivery mechanism for abortion services.
While procedural abortions must be provided in a clinical setting, medication abortion can be provided in a clinical setting or via telehealth. Access to medication abortion via telehealth had been limited for many years by a Food and Drug Administration (FDA) restriction that had permitted only certified clinicians to dispense mifepristone in a health care setting. The drug could not be mailed or picked up at a retail pharmacy. However, in December 2021, the FDA permanently revised its policy and no longer requires clinicians to dispense the drug in person. Additionally, in January 2023, the FDA finalized a change that allows retail pharmacies to dispense medication abortion pills to patients with a prescription.
While some states are regulating the use of mifepristone as an abortion method, the Biden Administration has asserted that the FDA has regulatory power over all drugs, including mifepristone. This could result in future legal action as the authority of the state to regulate health care will be pitted against the authority of the federal government to regulate drugs through the FDA will be contested.
- In a telehealth abortion, the patient typically completes an online questionnaire to assess (1) confirmation of pregnancy, (2) gestational age and (3) blood type. If determined eligible by a remote clinician, the patient is mailed the medications. This model does not require an ultrasound for pregnancy dating if the patient has regular periods and is sure of the date of their last menstrual period (in line with ACOG ’s guidelines for pregnancy dating). If the patient has irregular periods or is unsure how long they have been pregnant, they must obtain an ultrasound to confirm gestational age and rule out an ectopic pregnancy 3 and send in the images for review before receiving their medications. If the patient does not know their blood type or has Rh negative blood, the provider may prompt the patient to visit a nearby clinic for an injection to prevent adverse reactions between maternal and fetal blood ( RhoGAM ), The follow-up visit with a clinician can also happen via a telehealth visit.
- However, even in some of the states that have not banned abortion altogether, telehealth may not be available. Many states had established restrictions prior to the Dobbs ruling that limit the use of telehealth abortions by either requiring abortion patients to take the pills at a physical clinic, require ultrasounds for all abortions, set their own policies regarding the dispensing of the medications used for abortion care, or directly ban the use of telehealth for abortion care. As of November 2022, of the 33 states that have not banned abortion, eight had at least one of these restrictions, effectively prohibiting telehealth for medication abortion.
- Medication abortion has emerged as a major legal front in the battle over abortion access across the nation. Multiple cases have been filed in federal courts regarding aspects of the FDA’s regulation of medication abortion as well as the mailing of medications. One notable ongoing case is Alliance for Hippocratic Medicine v. FDA , where the plaintiffs are challenging the FDA’s authority and approval process for mifepristone. The plaintiffs also contend that an 1873 anti-obscenity law, the Comstock Act, prohibits the mailing of any medication used for abortion. In April 2023, a US Supreme Court ruling allowed current FDA rules to remain in effect as the case proceeds through the courts. This means that mifepristone remains available for medication abortion either in a clinic or via telehealth where state law permits.
Data from SFP’s October 2023 #WeCount report show that abortions provided by virtual-only clinics represent approximately 5% of all abortions post- Roe . The number of telehealth abortions increased 72% from a monthly average of 4,045 abortions in April and May 2022 to 6,950 abortions per month in the 12 months post- Dobbs . Nearly all of these abortions occurred in states that permit abortions.
Self-managed abortions are provided without a clinician visit.
Self-managed abortions typically involve obtaining medication abortion pills from an online pharmacy that will send the pills by mail or by purchasing the pills from a pharmacy in another country. This does not typically involve a direct consultation with a clinician either in person or via telehealth.
Research has found that prior to Dobbs , more than one in ten patients who obtained abortions at clinics had considered self-managing their abortions. This is likely to increase going forward since abortion care is not available in many states, and there have already been reports of people ordering pills from online markets outside the U.S. medical system. Tracking information on these online orders can help fill in gaps in abortion count estimates but can also be difficult. Some companies may not share data on purchases, and it would also be unclear whether patients take the abortion medication after receiving it in the mail.
The median costs of abortion services exceed $500.
Obtaining an abortion can be costly. On average, the costs are higher for abortions in the second trimester than in the first trimester. State restrictions can also raise the costs, as people may have to travel if abortions are prohibited or not available in their area. Many people pay for abortion services out of pocket, but some people can obtain assistance from local abortion funds.
- In 2021, the median costs for people paying out of pocket in the first trimester were $568 for a medication abortion and $625 for a procedural abortion. The Federal Reserve estimates that nationally about one-third of people do not have $400 on hand for unexpected expenses. For low-income people, who are more likely to need abortion care, these costs are often unaffordable.
- The costs of abortion are higher in the second trimester compared to the first, with median self-pay of $775. In the second trimester, more intensive procedures may be needed, more are likely to be conducted in a hospital setting (although still a minority), and local options are more limited in many communities that have fewer facilities. This results in additional nonmedical costs for transportation, childcare, lodging, and lost wages. nonmedical costs for transportation, childcare, lodging, and lost wages.
- Abortion funds are independent organizations that help some people pay for the costs of abortion services. Most abortion funds are regional and have connections to clinics in their area. Funds vary, but they typically provide assistance with the costs of medical care, travel, and accommodations if needed. However, they do not reach all people seeking services, and many people are not able to afford the costs of obtaining an abortion because they cannot pay for the abortion itself or cover the costs of travel, lodging or missed work.
Insurance coverage for abortion services is heavily restricted in certain private insurance plans and public programs like Medicaid and Medicare.
Private insurance covers most women of reproductive age, and states have the responsibility to regulate fully insured private plans in their state, whereas the federal government regulates self-funded plans under the Employee Retirement Income Security Act (ERISA). States can choose whether abortion coverage is included or excluded in private plans that are not self-insured.
- Prior to the Dobbs ruling, several states had enacted private plan restrictions and banned abortion coverage from ACA Marketplace plans. Currently, there are 11 states that have policies restricting abortion coverage in private plans and 26 that ban coverage in any Marketplace plans. Since the Dobbs ruling, some of these states have also banned the provision of abortion services altogether.
- A handful of states ( 9 ), however, have enacted laws that require private plans to cover abortion.
- The Medicaid program covers approximately one in five women of reproductive age and four in ten who are low-income. For decades, the Hyde Amendment has banned the use of federal funds for abortion in Medicaid and other public programs unless the pregnancy is a result of rape, incest, or it endangers the woman’s life.
- States have the option to use state-only funds to cover abortions under other circumstances for women on Medicaid, which 16 states do currently. However, more than half (56% ) of women covered by Medicaid live in Hyde states.
- According to a Guttmacher Institute survey of patients in the year prior to the Dobbs ruling, a quarter (26%) of abortion patients in the study used Medicaid to pay for abortion services, 11% used private insurance, and 60% paid out of pocket. People in states with more restrictive abortion policies were less likely to use Medicaid or private insurance and more likely to pay out of pocket compared to people living in less restrictive states.
- Federal law also restricts abortion funding under the Indian Health Service, Medicare, and the Children’s Health Insurance Program. Over the years, language similar to that in the Hyde Amendment has been incorporated into a range of other federal programs that provide or pay for health services to women including: the military’s TRICARE program, federal prisons, the Peace Corps, and the Federal Employees Health Benefits Program.
National polls have consistently found that a majority of the public did not want to see Roe v . Wade overturned and that most people feel that abortion is a personal medical decision. The public also strongly opposes the criminalization of abortion both among people who get abortion and the clinicians who provide abortion services. Nearly three quarters of adults (74%) and 79% of reproductive age women say that obtaining an abortion should be a personal choice rather than regulated by law (data not shown). For example, two-thirds of the public are concerned that bans on abortion may lead to unnecessary health problems for people experiencing pregnancy complications.
Additional KFF resources:
Abortion in the US Dashboard
Access and Coverage of Abortion Services
Issue Brief: Abortion at SCOTUS: Dobbs v. Jackson Women’s Health
Issue Brief: State Actions to Protect and Expand Access to Abortion Services
Policy Watch: A Year After Dobbs: Policies Restricting Access to Abortion in States Even Where It’s Not Banned
Policy Watch: Employer Coverage of Travel Costs for Out-of-State Abortion
Issue Brief: Exclusion of Abortion Coverage from Employer-Sponsored Health Plans
Interactive: How State Policies Shape Access to Abortion Coverage
Medication Abortion
Issue Brief: Legal Challenges to the FDA Approval of Medication Abortion Pills
Infographic: The Availability and Use of Medication Abortion Care
Fact Sheet: The Availability and Use of Medication Abortion
Issue Brief: The Intersection of State and Federal Policies on Access to Medication Abortion Via Telehealth
Public Opinion on Abortion
Web Event: Americans’ Knowledge and Attitudes About Abortion Access and The Pending Supreme Court Ruling
KFF Health Tracking Poll: Early 2023 Update On Public Awareness On Abortion and Emergency Contraception
KFF Health Tracking Poll: Views on and Knowledge about Abortion in Wake of Leaked Supreme Court Opinion
Other Resources on Women’s Health
Interactive: State Profiles for Women’s Health
Interactive: State Health Facts on Women’s Health Indicators
Homepage: Women’s Health Policy
- Women's Health Policy
- Access to Care
Also of Interest
- The Availability and Use of Medication Abortion
- State Actions to Protect and Expand Access to Abortion Services
- Legal Challenges to State Abortion Bans Since the Dobbs Decision
- Legal Challenges to the FDA Approval of Medication Abortion Pills
- Employer Coverage of Travel Costs for Out-of-State Abortion
- Abortion in the United States Dashboard

Texas maternal death task force can’t review abortion cases, contrary to CDC guidance
S ince 2013, one Texas task force has analyzed hundreds of pregnancy-related death cases and released dozens of recommendations for their prevention — helping shape policy and best practices for lawmakers, health care providers and residents across the state.
Now that Texas has had abortion bans in place for more than two years, the task force believed it could help answer a question that has long divided abortion rights advocates and anti-abortion groups in Texas: What effect do those restrictions have on women's health?
Then the panel realized it can't answer that question. State law prohibits it.
For more than a decade, a Texas law — Senate Bill 495 — has blocked the state's Maternal Mortality and Morbidity Review Committee from reviewing cases of women whose pregnancies ended in abortion, the group's chair, Dr. Carla Ortique, said at a public meeting March 22.
“When asked by many how the Texas MMMRC would gauge the impact of recent national and state legislative changes, we were confident when we responded that we review maternal deaths regardless of pregnancy outcome, and, as such, would be able to identify differences in case cohorts by comparative analysis over time,” said Ortique, an OB-GYN from Houston. “We're now aware that that will not be the case.”
Dr. Charlie Brown, a maternal-fetal medicine specialist and former chair of the Texas chapter of the American College of Obstetricians and Gynecologists, said he was “flabbergasted” that state law would keep cases in which a woman had an abortion from the committee’s review.
“Of course, abortion is related to pregnancy and (so are) deaths from an abortion," he told the American-Statesman in a phone interview. “I can't think of any reason why they would exclude that.”
The exclusion of abortion cases from the committee's review goes against recommendations from the Centers for Disease Control and Prevention , which establishes standards for maternal mortality review committees around the country, the federal agency told the Statesman.
“CDC guidance is that Maternal Mortality Review Committees review all deaths that occurred during pregnancy through the year after the end of pregnancy,” CDC spokesperson Nick Spinelli wrote in an email. “This includes pregnancies that ended in abortion.”
Though the group's name includes the word "maternal," the Texas Maternal Mortality and Morbidity Review Committee is a task force charged with reviewing and making recommendations for the prevention of “pregnancy-related deaths" — a term defined in state law and federal guidance to include patients whose pregnancies didn't end in delivery, such as those who died before their pregnancy ended or those whose pregnancies ended in miscarriage.
As per SB 495, which established the committee in 2013, pregnancy-related deaths are deaths “from any cause related to a woman’s pregnancy” that occur while she is pregnant “or within one year of delivery or end of pregnancy, regardless of the duration and site of the pregnancy." The bill also authorizes the group to study severe maternal morbidities, which are near-death events caused by a pregnancy-related condition.
But a provision tucked into the end of the 14-page bill , now enshrined in Chapter 34 of the Texas Health and Safety Code , specifies that the law does not apply to “disclosure of records pertaining to voluntary or therapeutic termination of pregnancy."
The provision means that the group cannot review cases like that of Amanda Zurawski , an aspiring mother who was forced to wait until she nearly died of septic shock for a hospital to terminate her nonviable pregnancy. The committee also is prohibited from examining any instances in which the state's medical emergency exceptions to its abortion bans were applied — 71 such cases have been reported to Health and Human Services since July 2022.
While state law has since 2018 required Texas doctors to report abortion-related health complications, including deaths, SB 495 prevents that data from being shared with the committee.
The Department of State Health Services confirmed to the Statesman that, in compliance with state law , the agency does not provide mortality or mortality records from pregnancies that ended in abortion to the committee. In fact, the agency does not maintain those case records, the department's media relations director, Chris Van Deusen, said .
The department is responsible for identifying cases that could be pregnancy-related, removing identifying details, and then presenting them to the review committee. Together, they produce a biennial report.
“The committee was set up to determine the causes of preventable maternal deaths and make recommendations about systemic changes to prevent them, not to look into elective or medically necessary abortions," Van Deusen wrote in an email to the Statesman.
He also said that each committee member receives a briefing and a copy of the group’s legislative mandate from the department, so the abortion records provision "is not something anyone was trying to hide from them."
Language in several of the review committee’s joint reports , however, could mislead the public into thinking that deaths related to any pregnancy, regardless of outcome, are included in the group’s data.
“The (committee) studies conditions around each pregnancy-associated case to determine pregnancy-relatedness by answering the question, ‘If she had not been pregnant, would she have died?’” reads the 2022 joint report from the state health department and the committee.
What the Texas panel may have missed — and could miss in the future
Data from the the state health department and the CDC indicate that the number of abortion-related cases that eluded the committee's review might not have been enough to sound an alarm, but some predict they could increase.
An average of 53,000 pregnancies were legally terminated in Texas each year between 2014 and 2020. Fewer than two women per year — 20 in total — were reported to have died from abortion-related causes during that period, according to CDC data taken from Texas death certificates, as the Austin Chronicle first reported. Roughly 100 reports of abortion-related complications have been filed each year since 2018, as per state health departement data.
Scientific studies have also shown that women whose pregnancies end before delivery generally have a far lower rate of maternal mortality and morbidity than those who carry to term. A 2017 CDC and Johns Hopkins University study of more than 2,000 pregnancy-related deaths in the U.S. found that 2.4% occurred for women who miscarried or had induced abortions, while 56.4% occurred after a live birth or stillbirth. Roughly 2.7% had ectopic pregnancies, and slightly more than one-fourth (26.4%) did not deliver. The outcomes of roughly 10% of the pregnancies studied were not known among cases in the study's cohort.
However, some researchers have predicted that new prohibitions could drive up deaths and near-deaths from unsafe abortions . Texas women and OB-GYNs have also filed lawsuits and have testified before the Texas Medical Board that uncertainty and fear around narrow medical emergency exceptions to Texas' abortion bans — which allow physicians to terminate pregnancies in cases in which a woman risks death or seriously risks "substantial impairment of a major bodily function" — have led physicians to delay or deny medical care to women experiencing severe pregnancy complications.
State Rep. Donna Howard, D-Austin, expressed concern about the provision and what it says about the state's views on women who have therapeutic or elective abortions.
"The Legislature’s decision to keep this data from the Maternal Mortality and Morbidity Review Committee perpetuates the idea that the state does not value the lives of women who terminate their pregnancies," Howard wrote in an email to the Statesman. "From my understanding, the potential abortion-related data would not have been statistically significant, but that does not mean their deaths should not have been considered in the Committee’s review."
The past and future of Texas' law prohibiting abortion review
Of the six authors and sponsors of SB 495 that the Statesman contacted for this article, only Rep. Armando Walle, D-Houston, who sponsored but did not author the bill, answered the Statesman's questions.
Walle said abortion cases were excluded during negotiations for the bill because they were not the legislation's primary focus. Given the changes in Texas abortion laws, Walle said he would be open to amending the review committee's current mandate to allow review of those records.
"We're talking about a review board that was created well before the overturning of Roe. But now with the overturning of Roe, it's obviously a much more pronounced issue," Walle told the Statesman. "The world has completely changed for women."
But Walle, who is known for facilitating bipartisan legislation in the House, wasn't optimistic that the change would succeed in the Legislature because it's "an environment that is hostile as it relates to abortion," he said in a phone interview May 8.
But he could have some unexpected allies. Two of the most influential anti-abortion lobbying groups in the state — Texas Alliance for Life and Texas Right to Life — also told the Statesman that they would support striking the provision excluding abortion records data.
"We would support allowing the MMMRC to review cases of pregnancy-related death or morbidity in which a woman's pregnancy ended in abortion," Texas Right to Life Director Rebecca Weaver wrote in a statement. "This is an important data point that is currently ignored in trying to address maternal mortality and morbidity in our state.”
Brown, the maternal-fetal medicine specialist who spoke on behalf of the Texas chapter of the American College of Obstetricians and Gynecologists, said the group would support efforts to lift the provision.
"From the perspective of wanting as complete a data set as possible, ACOG would certainly support (abortion records) being in there," he told the Statesman.
SB 495's authors — Sen. Joan Huffman, R-Houston, and Sen. Royce West, D-Dallas — declined to comment in response to repeated inquiries by phone and email over several weeks.
Read part two of this story: Abortion foes, supporters say Texas maternal death task force should review abortion cases
Correction: This story previously misstated the number of cases of pregnancy-related near-deaths that the committee has analyzed; while state law allows DSHS to provide such cases to the MMMRC, past reports have not included case studies of these incidents .
This article originally appeared on Austin American-Statesman: Texas maternal death task force can’t review abortion cases, contrary to CDC guidance

A pilot study on environmental and behavioral factors related to missed abortion
Affiliation.
- 1 Department of Occupational and Environmental Health, Peking University, Beijing, 100191, China.
- PMID: 21431815
- PMCID: PMC3117210
- DOI: 10.1007/s12199-010-0196-4
Objective: The purpose of this study was to investigate the environmental and behavioral factors associated with the induction of missed abortion, with a particular focus on the relationship between job stress and missed abortion.
Methods: This was a case-control study in which 552 women participated (267 cases, 285 controls). Job stress was measured using the Job Content Questionnaire 1.0 (JCQ1.0).
Results: The case and control groups were significantly different for many factors, including age, physical exercise, exposure time to cell phone and computer, home refurbishment, ventilation, folic acid supplements, preference for fried food, reproductive knowledge, premarital health screening, parity, and supervisor support (P < 0.05). For job stress, the univariate analysis revealed that there was no significant difference between cases and controls. Logistic analysis revealed that physical exercise (2-3 times per week or >3 times per week) [odds ratio (OR) 0.433, 95% confidence interval (CI) 0.213-0.881 or OR 0.268, 95% CI 0.106-0.680, respectively], ventilation (OR 0.415, 95% CI 0.251-0.685), folic acid supplements (OR 0.409, 95% CI 0.265-0.633), age (OR 1.102, 95% CI 1.033-1.174), and supervisor support (OR 0.870, 95% CI 0.768-0.986) were the significant factors contributing to the missed abortion (P < 0.05).
Conclusions: Physical exercise, ventilation, folic acid supplements, and supervisor support were identified as protective factors for the prevention of missed abortion. Advanced age at pregnancy was a risk factor for missed abortion.
- Abortion, Missed / epidemiology*
- Age Factors
- Case-Control Studies
- China / epidemiology
- Dietary Supplements*
- Folic Acid / administration & dosage*
- Logistic Models
- Pilot Projects
- Risk Factors
- Stress, Psychological*
- Ventilation*
- Newsletters
- Account Activating this button will toggle the display of additional content Account Sign out
Trump Inadvertently Said Something Honest About Abortion
He’s been trying to have it both ways on the issue, but this freudian slip gives away the game..
This is Totally Normal Quote of the Day , a feature highlighting a statement from the news that exemplifies just how extremely normal everything has become.
“We’re, like, the party of fertilization because we are for the women.” —Donald Trump, speaking about abortion following a rally in Michigan earlier this month
Over the past week, Trump has been all over the headlines, between Stormy Daniels’ testimony in his hush money trial and the news that Trump’s mysterious, yearslong IRS audit could result in his owing $100 million in back taxes. But the Trump news I can’t stop thinking about is a baffling—and accidentally quite telling—interview the former president gave to a local news station about reproductive rights. It was mostly a bunch of word vomit that got very little attention, but it contained a damning Freudian slip that encapsulates the party’s views on abortion and what rights, if any, should be afforded to women.
Following a rally in Saginaw County, a Fox 2 Detroit anchor asked Trump how abortion would affect the November election. Trump, regurgitating some of his favorite lines of late, claimed that all legal scholars wanted Roe v. Wade overturned—a feat he managed to achieve. Now that abortion is a state issue, he said, “it’s working out” and “people are satisfied with it.” (Trump also seemed not to know that Michigan voters already passed a ballot measure to protect abortion.) This is all a bunch of nonsense, but it’s not the part that’s stuck with me.
Trump then appeared to reference the Alabama Supreme Court ruling declaring that embryos created for in vitro fertilization were legally human beings under wrongful-death statutes. The February decision halted IVF treatments in the state and sent GOP members of Congress into a tailspin about whether they support the fertility treatment’s legality. (Shocker: They blocked a Senate bill that would have protected it.) In the interview, Trump tried to claim that the GOP supports IVF more than Democrats do, and made a glaring slip-up (starting around 6:30 into this clip):
We’re, like, the party of fertilization because we are for the women. We wanna help the women. Because they were gonna end fertilization, which is where the IVF—where women go to the clinics and they get help in having a baby, and that’s a good thing, not a bad thing. And we’re for it 100 percent. [Democrats] tried to say that [Republicans] weren’t for it. They actually weren’t for it and aren’t for it as much as us, but women see that.
Trump saying that Republicans are “the party of fertilization” is inadvertently one of the most honest things he’s ever said about abortion. He can swear up and down that he believes it’s now an issue for the states, but anti-abortion activists and the current GOP have been extremely clear that their end goal is full legal rights for fertilized eggs—rights that necessarily come at the expense of the living, breathing people with said eggs inside them.
A month after the Alabama IVF dust-up, the influential Republican Study Committee endorsed the Life at Conception Act, a House bill that would give embryos legal rights from “ the moment of fertilization .” If that fetal personhood bill became law, it would not only nationalize the Alabama Supreme Court decision—it would also ban abortion in all 50 states. The RSC comprises nearly 80 percent of House Republicans. Days after that bill endorsement, Alliance Defending Freedom CEO Kristen Waggoner told Politico that the legal juggernaut hopes to one day get the Supreme Court to uphold a federal abortion ban based on personhood: “We do believe at ADF that the Constitution protects the life of an unborn child and that that is in the 14 th Amendment.” The ADF helped write the Mississippi law the court used to overturn Roe and ostensibly send abortion back to the states, but it’s not stopping there.
Another ADF case horrifically illustrates what it means to be the party of fertilization—and how legal rights during pregnancy can become a zero-sum game. In Moyle v. United States , the legal advocacy group is helping Idaho defend its near-total abortion ban, which has exceptions only to prevent death, not threats to health. The Biden administration says the ban conflicts with a federal law that requires hospitals to stabilize all emergency room patients whose health or organ function is in jeopardy , even if that care is abortion. Idaho’s argument was, essentially, that a miscarrying woman on the verge of losing her uterus may not be entitled to an abortion because the state has acted to protect fetal life—even though, in many of these cases, the fetus won’t survive. Responding to hypotheticals from Justice Elena Kagan, Idaho’s lawyer said, “There are two patients to consider in those circumstances,” and “the two-patient scenario is tough.” (If the justices side against the Biden administration, it could mean that pregnant women in Idaho and other states with abortion bans will face dangerous discrimination in ERs.)
Trump’s “fertilization” interview reminded me of another recent pile of abortion gibberish that contained a kernel of honesty: his early April video on Truth Social in which he claimed he wants to leave abortion to the states but that the issue isn’t as important as winning in November . He previewed his video by saying that Republicans “have an obligation to the salvation of our Nation … TO WIN ELECTIONS.” He reiterated this sentiment on camera: “You must follow your heart on this issue. But remember, you must also win elections to restore our culture and, in fact, to save our country.”
Trump implying that he can’t endorse a national ban now because it’s so unpopular is the most believable thing he said. It was also a wink and a nod to conservatives that he’s doing what it takes to regain power: They can simply revisit the issue later. And we know exactly what they’ll do.
The Kentucky 2024 legislative session is over. Here's what you missed on its final night

FRANKFORT— The final day of the Kentucky legislative session was marked by what didn't happen rather than what did.
On the Republican side, several bills reflecting key party priorities failed to get final passage, allaying the fears of diversity and open government advocates.
On the Democratic side, a last-minute procedural maneuver that would have opened the door to adding exceptions to the state's near-total abortion ban also failed.
And both sides turned to legislative procedure to save the day for a bill aimed at improving health care for pregnant women in Kentucky.
'Momnibus' passes at last minute
An omnibus maternal health bill with bipartisan support almost foundered on the shoals of abortion politics but managed to get final passage on Monday night.
House Bill 10 , dubbed the "Momnibus," started its legislative career with all signs pointing toward passage : A bipartisan group of female legislators put aside their differences on abortion and crafted a bill aimed at improving maternal and child health in Kentucky.
That bill sailed through the House with unanimous approval but stalled when a Senate committee passed a version that would have required certain health care facilities to provide "perinatal palliative care" that included services for women who gave birth to nonviable fetuses or babies who die shortly after birth. The proposal included language that defined a "baby" as an "unborn child."
Democrats said the measure , initially proposed by Rep. Nancy Tate , R-Brandenburg, reinforced the state's anti-abortion stance and doubled down on Kentucky women with difficult pregnancies who may have preferred an abortion.
The addition of Tate's controversial proposal to the original Momnibus appeared to halt its progress. But at the last minute, legislative procedure saved it: The original bill was added as an amendment to a separate maternal health care bill , and it gained final passage with just hours left on the legislative clock.
Among other things, the Momnibus will change state law so that newly pregnant women can qualify for health insurance in Kentucky and establish a “Lifeline for Moms” to help health care providers find services for mothers with mental illness or intellectual disability.
Abortion-ban exceptions fails
Near the start of the session, Sen. David Yates, D-Louisville , proposed a bill to add exceptions to the state's abortion ban in the case of incest, rape, a nonviable fetus or to protect the health of a mother to Kentucky's near-total abortion ban.
Despite a Senate rule requiring all bills to be assigned to committee for consideration, Yates' bill never got a committee assignment. At the end of the session, he made an unusual procedural move , filing a "discharge petition" to dislodge the bill in hopes of a possible Senate vote on the matter.
"Kentuckians deserve to know where their elected leaders stand on this issue," Yates told reporters about his reason for filing the petition.
But the petition failed on Monday night, with Senate leadership saying the motion was order during a heated, if somewhat arcane, procedural deliberation on the Senate floor.
Floor Majority Leader Damon Thayer, R-Georgetown, said Yates' move was a political stunt on the last day of the legislative session because he could have raised the issue earlier.
Yates has vowed to introduce the bill again next year.
Anti-DEI and open records bills falter
It looked like lawmakers were going to resurrect Kentucky’s “anti-DEI” bill, but despite being posted on the Senate agenda, the chamber did not consider it on the last day of the session.
Despite Republican agreement that diversity, equity and inclusion initiatives are a problem, the party lacked consensus about a solution, resulting in dueling House and Senate versions of bills that took aim at DEI.
The Senate bill would have prohibited state universities from requiring students or employees to endorse a specific ideology or viewpoint to receive admission, employment, promotions or graduation. The House version went much further, requiring Kentucky's public colleges to dismantle on all diversity, equity, and inclusion programs and banning race-based scholarships at Kentucky’s public colleges.
Last month, the House gutted the Senate version and replaced it with its own, much-tougher version.
GOP Senators felt it best to work on the bill during the interim rather than vote for a House version not all caucus members agreed with, Senate President Robert Stivers, R-Manchester, told reporters Monday night.
“I think that was something that the caucus had a long debate and discussion about, and it wasn't a matter of not doing something versus doing something … but what should something be,” Stivers told reporters last week.
Government transparency advocates were also deeply concerned about a bill sponsored by Rep. John Hodgson, R-Fisherville , that would have created a loophole for public officials' text messages about official business if sent on privately owned devices . That bill failed to get a vote in the Senate on Monday night, and Stivers said it would be considered during the interim.
Lawmakers override Beshear vetoes, including Safer Kentucky Act, JCPS 'split' study, more
Hodgson said the bill was motivated by the desire to protect the private lives of officials , while critics said it opened the door for officials to conduct public business outside the purview of the state's open records law, which allows members of the public to view documents that shed light on the workings of government.
Gov. Andy Behsear had expressed support for the bill, which also required government bodies to create official emails for official business. Ultimately, though, the governor will not be forced to make a decision because the measure did not advance to the Senate floor.
Reach Rebecca Grapevine at [email protected] or follow her on X, formerly known as Twitter, at @RebGrapevine. Reach reporter Hannah Pinski at @[email protected] or follow her on X, formerly known as Twitter, at @hannahpinski.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.6(10); 2016

Estimating the visibility rate of abortion: a case study of Kerman, Iran
Maryam zamanian.
1 Modeling in Health Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
Mohammad Reza Baneshi
Aliakbar haghdoost.
2 HIV/STI Surveillance Research Center, and WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
Farzaneh Zolala
Abortion is a sensitive issue; many cultures disapprove of it, which leads to under-reporting. This study sought to estimate the rate of abortion visibility in the city of Kerman, Iran—that is, the percentage of acquaintances who knew about a particular abortion. For estimating the visibility rate, it is crucial to use the network scale-up method, which is a new, indirect method of estimating sensitive behaviours more accurately.
Materials and methods
This cross-sectional study was conducted in Kerman, Iran using various methods to ensure the cooperation of clinicians and women. A total of 222 women who had had an abortion within the previous year (74 elective, 74 medical and 74 spontaneous abortions) were recruited. Participants were asked how many of their acquaintances were aware of their abortion. Abortion visibility was estimated by abortion type. 95% CIs were calculated by a bootstrap procedure. A zero-inflated negative binomial regression analysis was conducted to assess the variables related to visibility.
The visibility (95% CI) of elective, medical and spontaneous abortion was 8% (6% to 10%), 60% (54% to 66%) and 50% (43% to 57%), respectively. Women and consanguineal family were more likely to be aware of the abortion than men and affinal family. Non-family members had a low probability of knowing about the abortion, except in elective cases. Abortion type, marital status, sex of the acquaintance and closeness of the relationship were the most important determinants of abortion visibility in the final multifactorial model.
Conclusions
This study shows the visibility rate to be low, but it does differ among social network members and by the type of abortion in question. This difference might be explained through social and cultural norms as well as stigma surrounding abortion. The low visibility rate might explain the low estimates of abortion rates found in other studies.
Strengths and limitations of this study
- This is a rare study estimating abortion visibility in Iran—as well as in the rest of the world; the results could draw policy makers' attention to appropriate policies by providing a more realistic picture of abortion.
- The most important challenge faced in this study was low participation from women who had abortions and reproductive health providers because of stigma and severe legal restrictions. As a result, we tried to encourage their participation using different strategies.
- We were unable to assess other cases of abortion (eg, women who used traditional and herbal medicines, as well as cases performed by non-medical providers or the woman herself). The visibility of abortion in such cases may be different from the cases we considered.
Introduction
Self-reporting and direct methods of measuring health events are prone to high levels of under-reporting bias. This bias is much more common for behaviours that are sensitive or subject to social disapproval, occurring more often among women. 1 2 Abortion can be classified as a sensitive issue because of the high level of stigma related to it and legal restrictions in many communities. 3
Abortion can be divided into two overarching categories, spontaneous and induced, with the latter further divided into two types, medical and elective. 4 Medical abortion is performed in cases of fetal anomaly or to safeguard the mother's health, whereas elective abortion is performed at the request of the mother for other than therapeutic reasons. Elective abortion, which has also been called intentional, criminal or illegal abortion, garners greater stigma in many societies. 3 5 Stigma causes women to hide their experience of abortion from acquaintances and healthcare providers. 6 Even in communities where abortion is legal, a comparison of medical records and self-reported abortion rates shows a high discrepancy of ∼70%. 7 This rate may be much higher in societies where abortion is illegal, which results in under-reporting and unsafe abortions that can jeopardise the mother's life. 8
Iran—a Middle Eastern country governed by the Islamic state—culturally, religiously and legally prohibits elective abortion. Because of these conditions, many elective abortions are performed at home or under unsafe conditions, 9 which could lead to the mother's death or irreparable complications. 3 These abortions can never be registered if they are performed successfully, and, in cases of referral to a hospital for a critical complication endangering the mother's health, the mothers often report spontaneous abortion rather than elective. 9 In addition, a new population growth policy in Iran is encouraging families to have more children, as the Iranian population has declined in recent years. 10 This, in turn, could increase legal restrictions and ultimately lead to even more under-reporting of abortion. Last but not least, not all cases of spontaneous abortion are recorded in the registration system. 5
While the data derived from direct survey methods and from the registration system represent just the tip of the iceberg, an accurate estimate of abortion is necessary to inspire more effective planning and policymaking to reduce unsafe abortion and to improve maternal health. Such an estimate is also needed for purposes such as accurate estimation of pregnancy rates, levels of unintended pregnancy (UP) (UP itself includes two main categories: unwanted pregnancy and mistimed pregnancy) and contraceptive failure rate. 11
How can better estimates for sensitive issues be obtained? An effective alternative method to self-reporting and direct techniques is the network scale-up (NSU) method, an indirect technique. In this method, a representative sample of the general population is questioned about the number of the target population in their active social network—it does not require direct questioning of the target population. 12 For example, the participants are asked, ‘among your acquaintances, how many women have had abortion experiences?’ This indirect and anonymous question could desensitise the respondents to the topic and increase response rates and accuracy for two reasons: first, the question is not directly about the respondents themselves but about other people; second, they are not required to name those acquaintances or their relation to them; they merely provide the number. 12 13 The NSU method is based on the idea that the proportion of individuals known by participants is linearly proportional to the real size of the same subpopulation in the society. 12 However, one of the basic NSU assumptions, perfect awareness of their acquaintances' behaviours, is often not met; hence, visibility bias remains a major source of bias in estimations of hard-to-count populations. 14
Visibility bias describes respondents not being aware of all the behaviours among their active social network. This occurs more often for stigmatised or illegal behaviours. For example, respondents may not be aware of abortions that have happened in their network. 15 In the case of the NSU method, the obtained crude estimate should be adjusted accordingly. For example, if the visibility of a hidden behaviour was estimated at 50%, the NSU method's crude estimate should be doubled. Thus far, visibility rates have been estimated for hidden populations such as men who have sex with men (MSM), injection drug users (IDUs) and commercial sex workers (CSWs), as well as for certain types of cancer. 12 16–18 Only one study has estimated the visibility of abortion by asking gynaecologists and midwives to guess the visibility rate of abortion. 19 However, to the best of our knowledge, no study has used the standard method to estimate the abortion visibility (AV) rate. Therefore, in this study, we sought to estimate the visibility rate and its determinants for all types of abortion in an Iranian population to provide a more accurate estimate of abortion.
Study setting and study population
This cross-sectional study was part of a larger ongoing study in Kerman, Iran in 2015, the primary aim of which was to estimate the frequency of abortion. Kerman is the capital of the largest province of Iran and is located in the southeastern part of the country. Eligible participants were female residents of Kerman over the past 5 years who had a history of abortion during the previous year. A total of 222 women who had an abortion of any type within the previous year (74 elective, 74 medical and 74 spontaneous) were recruited. To obtain the study sample, both private and public centres were approached, including referral hospitals, private offices of gynaecologists and midwives. The critical factor in this study was gaining the trust of the reproductive health providers, so that they felt comfortable cooperating with data collection for elective abortion cases. This was difficult owing to the severe legal restrictions on abortions in Iran. Therefore, we held several meetings to explain the study method and assure them that their confidentiality and anonymity were paramount. They were also provided with financial incentives. Subsequently, these providers introduced us to women who had had an abortion and consented to be interviewed. Most participants were interviewed in person, but 33 (∼15%) were interviewed on the phone to further protect their privacy. After explaining the purpose of the study to the participants, reassuring them of their anonymity and the confidentiality of information, and obtaining verbal informed consent, we were permitted to collect data.
To obtain a sample of non-elective abortions—participants whose medical records listed a medical or spontaneous abortion within the previous year—we sought the help of gynaecologists and midwives in referral hospitals throughout the city. These participants were interviewed after they provided verbal consent. Written consent forms were not used owing to the cultural sensitivity of this topic and to help increase both participation and accuracy of responding. 20 All interviews were conducted in a private room at the same centre. Despite all these safeguards, the participation rates for elective, medical and spontaneous abortions were 39%, 70% and 62%, respectively. We are cognisant that non-random sampling and the relatively low response rate for elective cases, which were almost unavoidable, could affect the generalisability of the results; therefore, the estimated AV rate cannot be generalised to the whole population of women living in Kerman. The data were collected using a structured interview instrument administered by a trained female interviewer. The study protocol was approved by the ethics committee of Kerman University of Medical Sciences (ir.kmu.rec.1394.223).
Data collection
The interview form included four sections. The first provided an overview of the study and its objectives. In the second, a table listed the participant's active social network relationships in the rows. In the NSU method, the standard definition of an active social network is ‘people whom you know and who know you by name, with whom you can interact, if needed, and with whom you have had contact over the last two years personally, or by telephone or e-mail’. 12 13 For ease of recall and therefore increased accuracy, we divided the entire active social network into a list of comprehensive relationships and two main categories: family and non-family. The family group included consanguineal 1 and affinal 2 family. Both consanguineal and affinal family included two subgroups: immediate family (sometimes known as first-degree relatives, including parents, siblings and children) and extended family (including grandparents, aunts, uncles, cousins, nieces, nephews, etc). The non-family group included male and female friends from school, friends from university, friends from their neighbourhood, acquaintances from work, acquaintances from their husband's work, friends of their husband and other friends or acquaintances. The table included three columns (A, B and C). The first (column A) tallied the total number of persons from each relationship. The next column (B) indicated the number of adults (persons 18 years old and over) from each relationship, and the last (column C) indicated the number of adults who were aware of the abortion. (Participants were not asked about the awareness of those under 18 years old because any lack of knowledge on their part is more likely due to their age than to a low visibility rate.) Participants were prompted with questions such as ‘How many cousins do you have? How many of them are adults? And how many of these adults are aware of your abortion?’.
The third section assessed the abortion type. In addition, participants were asked whether their pregnancy was intended (planned), why the pregnancy was unintended, the number of children they already have, any previous pregnancies, age, marriage age, marital status, career, husband's career, and their level of education.
The last section included more sensitive questions. This section included questions to be completed in cases of elective abortion (such as the reason for the abortion, whether the man involved in the pregnancy (MIP) was aware and consented to the abortion, and what their marital status was at the time of the abortion). A self-completion form and a ballot box were used for this section in order to maintain the participant's privacy and to improve the accuracy of the data. The form was piloted in two studies and revised accordingly to increase acceptability and comprehension.
Data analysis
We estimated AV using formula (1):

AV and 95% CI were estimated for each type of abortion and by different subgroups divided by abortion type ( table 1 and figure 1 ). The 95% CIs were computed by a bootstrapping procedure, drawing 1000 independent samples with replacement. The calculations for AV and 95% CI were performed separately for different demographic characteristics.
Table 1
Abortion visibility by demographic characteristics
*Immediate family of consanguineal and affinal family.
†Extended family of consanguineal and affinal family.
AV, abortion visibility.

Abortion visibility in the city of Kerman, in 2015, divided by abortion type. (A) Abortion visibility, divided by abortion type. (B) Comparison of abortion visibility among women's husbands and female and male members of their social network, divided by abortion type. (C) Comparison of abortion visibility among women's consanguineal family, affinal family and non-family, divided by abortion type. (D) Comparison of abortion visibility among women's immediate and extended consanguineal family, divided by abortion type. The y axis shows abortion visibility as a percentage, which is calculated by dividing the number of adults who were aware of the abortion by the total number of adults listed in any given category. E, elective; M, medical; S, spontaneous; H, husband; F, females; M, males; CF, consanguineal family; AF, affinal family; NF, non-family; ICF, immediate consanguineal family; ECF, extended consanguineal family.
A zero-inflated negative binomial regression analysis was used to model the potential determinants of AV because so many acquaintances were not aware of the abortion, generating excess zero responses, and because of the large difference between the mean and variance of the data. To adjust for the correlation between each participant's responses about the members of her network, each participant was defined as a cluster layer, and cluster robust SE was used. Potential determinants of AV were tested in univariate analyses, and those with p values less than 0.2 were entered into a multifactorial model using backward elimination variable selection. We performed these analyses for each type of abortion separately; the results were similar in terms of effect sizes and levels of significance. Hence, we performed one regression for all of the data (including all types of abortion). The analyses were performed using Stata software (V.11.2) and Microsoft Excel (2007).
In this study, 222 women with a history of abortion in the previous year, including elective, medical and spontaneous abortions (74 cases of each type), were recruited. The mean (SD) age of elective, medical and spontaneous abortion cases was 31.4 (7.8), 29.0 (5.1) and 29.1 (6.5), respectively, and the respondents' mean years of education were 13.9, 12.6 and 11.8 years, respectively. The employment percentages were 31.1, 23.0 and 14.9 for respondents who had had elective, medical and spontaneous abortions, respectively. While all of the women with medical and spontaneous abortions were married, the corresponding figure was 82.4% for elective abortions; 9.5% of these participants were single, and 8.1% were divorced or widowed. While pregnancies ending in spontaneous and medical abortions were mainly intended (90.5% and 81.1%, respectively), most pregnancies terminated by elective abortion were unintended, with some of those being unwanted (31.1%) and mistimed (27.1%) pregnancies ( table 2 ). Elective abortions were conducted mainly with the agreement of both parents (66.2%). However, 31.1% were undertaken based only on the mother's wishes, and, in one-third of these cases, the MIP was not informed about the abortion. The remainder of the abortions were performed based only on the wish of the MIP (2.7%).
Table 2
Elective abortion visibility divided by the reason for abortion
*Unintended pregnancy.
†Pregnancy outside of marriage.
‡Pregnancy in girls whose marriages are legally recorded but they do not yet share accommodation with their husbands.
§Intended pregnancy.
¶Not calculated because of small sample size.
The number of family members in the participants' social networks totalled 25 974, consisting of 60% adults. Of the adults, 20% were immediate family members and 80% were extended family members. The corresponding figure for non-family adults was 6609. The average percentage of each subgroup in a participant's active social network was husband 1%, consanguineal family 42%, affinal family 27%, and non-family members 30%. The sex ratio of the participants' active social network was 48% male to 52% female ( table 1 ).
The visibility (95% CI) of elective, medical and spontaneous abortion was 8% (6% to 10%), 60% (54% to 66%) and 50% (43% to 57%), respectively ( figure 1 A). All abortion types were much more visible to husbands than to other members of the active social network (in the case of elective abortion, the difference between husbands and other members of the network was much higher than for the other two types of abortion) ( figure 1 B). The visibility of all abortion types was lower for non-family than for family, except for elective abortions, which were more visible to non-family than to family ( figure 1 C). The visibility of all types of abortion was higher for consanguineal family than for affinal family (although this difference was smaller for spontaneous abortion) ( figure 1 C); among consanguineal family members, all abortion types were more visible to immediate family than to extended family (but in elective cases, this difference was much higher than for the other two types) ( figure 1 D). With the exception of the husband, abortion was always more visible to women than to men in participants' networks ( figure 1 B). The difference in visibility between women and men who were immediate consanguineal family was not sizable for medical and spontaneous abortions, but the difference was high for elective abortion (55% for women vs 13% for men), meaning mothers and sisters were more likely to know about elective abortions than fathers and brothers.
In the univariate analysis, the visibility of abortion was not significantly (at the 0.2 level) associated with the participant's age and education or with the husband's occupation and education (results not shown). Therefore, these variables were not included in the multifactorial analysis. The number of children did not remain significant after adjustment for other variables in the multifactorial analysis.
The final multivariate model—after being adjusted for potential factors and backward elimination—showed that non-elective abortions were approximately twice as visible as elective ones (medical abortion was 98% (95% CI 1.58 to 2.48) and spontaneous abortion 96% (95% CI 1.56 to 2.46) more visible than elective abortion). In addition, the abortions of unmarried women were 66% (95% CI 0.22 to 0.52) less visible than those of married women. The abortions of self-employed women were 14% (95% CI 1.03 to 1.27) more visible than those of housewives. Abortions of intended pregnancies were 17% (95% CI 0.70 to 0.98) less visible than those of UPs, yet increasing the number of UPs decreased visibility (1 UP vs 0 UPs was 17% (95% CI 0.72 to 0.95) less visible and two or more UPs vs 0 UPs was 30% (95% CI 0.57 to 0.88) less visible).
Among acquaintances, compared with men, women were 19% (95% CI 1.13 to 1.26) more informed about abortions. Compared with non-family members in active social networks, the husband, immediate family members and extended family members were 91% (95% CI 1.69 to 2.18), 47% (95% CI 1.34 to 1.62) and 13% (95% CI 1.03 to 1.24) more informed about abortions ( table 3 ).
Table 3
Determinants of abortion visibility
AV, abortion visibility; RR, rate ratio; Unmarried, single/divorced/widowed.
This study found that the visibility of abortion, particularly elective abortion, was very low in Kerman in 2015. Of all members of the participants' active social networks, their husbands had a very high probability of being informed about the abortion. In addition, women and consanguineal family were more likely to be informed of the abortion than men and affinal family. Non-family members had a low probability of being informed, yet non-family had the highest possibility of being informed of elective abortions. Other factors affecting visibility were marital and employment status, as well as the type of pregnancy and frequency of UPs.
To the best of our knowledge, only one study in the world has estimated the visibility of abortion, but it used a different method: Rastegari and coworkers 19 used gynaecologists’ and midwives' guesses to calculate the visibility rate of abortion in Iran. Their study estimated visibility at 20–34% for elective abortion (termed abortions without medical indications), which was higher than our estimate, and 43–75% for other types of abortion (termed abortions with medical indications), which was similar to our estimate but had wide variability and did not differentiate between spontaneous and medical abortions. Although that study was the first attempt to estimate AV, it is reasonable to suppose that this issue is best sourced not from clinicians but by the woman herself, as she knows far more about her own pattern of disclosure. Another study in Iran used a method similar to that used in this study to estimate the visibility of cancer, finding a cancer visibility rate of 86%. 18 Other studies have estimated visibilities of 1.4 for MSM in Japan, 76 for IDUs in Brazil, and 24, 57 and 34 for MSM, IDUs and CSWs, respectively, in Ukraine. 12 16 17 The observed differences in these visibility rates indicate variation in the stigma of each behaviour in different cultures. The visibility rate of abortion in this study was similar to, or even lower than, those of other stigmatised behaviours, which highlights that abortion is highly stigmatised in the study setting.
The rest of the literature has mainly compared self-reporting and medical record data, and they have also concluded that abortions are under-reported. 21 22 These studies have shown that most women who have a history of abortion (listed in their medical records) did not self-report the abortion. This is the case even in countries where there are no legal restrictions for abortion. 7 Abortion under-reporting, which could be an indicator of low AV, in addition to the sensitive nature of sexual matters such as abortion, is also due to social, cultural, religious and legal factors that are more pertinent in traditional, religious countries such as Iran. In Iran, sexual relationships outside marriage are highly stigmatised, particularly for women. 9 Hence, the stigma related to abortion differs by marital status. Married women are stigmatised for elective abortion because it is against religious law. 9 However, women who experience non-elective abortions could be labelled infertile or could be blamed by others. 23 24 In Iran, the expression ‘ojagh koor’ (which has a negative meaning and is pejorative) is applied to both men and women who are unable to have children. ‘This metaphoric expression is according to popular belief in Iran that an infertile couple will never have a house with a ‘warm kitchen’ (ojaghe koor)’. 23 As a result, many women hide their abortions from acquaintances. This might also explain the low visibility of intended pregnancies leading to abortion compared with UPs. On the other hand, a higher number of previous UPs decreased the level of visibility. Recently, Iranian families have tended to consider fewer children as a sign of higher social class; 10 therefore, informing others about repeated UPs could decrease their social standing and lead to humiliation for violating childbearing norms.
Unmarried women (single, divorced and widowed) tell a very different story; having sexual relationships outside marriage is the main reason for the stigma attached to abortions, regardless of the type. This stigma can be very devastating and can disrupt a person's life. For example, a pregnant single woman may lose the chance to be married and have a normal social life. This could even disgrace her family name. She is very likely to be blamed, rejected and subjected to physical or mental punishment by acquaintances. 9 The social stigma of abortion for unmarried women is much heavier than for married women, which explains the lower visibility in these women. Severe social stigma exists even for girls whose marriages are legally recorded but who do not yet share accommodation with their husbands and during which they still live with their parents (the ‘Aghd’ period). In this period, there is no legal restriction against having a sexual relationship with her husband and getting pregnant; however, from a traditional point of view, they should abstain from sexual activity until they share accommodation. 9 These norms could explain the low visibility observed for this group. Furthermore, current Iranian rules based on Islamic laws prohibit elective abortion, and there are legal penalties for reproductive health providers who perform abortions. 3 9 A new Iranian population growth policy 10 could enforce such restrictions, which could ultimately decrease AV further.
The visibility of abortion was significantly higher among self-employed women, those with no affiliation with the government. As abortion is unlawful, women who have government jobs might perceive it as a threat to their job, which would lead them not to disclose it and be more conservative than self-employed women. Moreover, in self-employed professions, such as hair styling, women might have more opportunities to speak with other women and to talk about personal issues 25 than do women in government jobs.
The highest AV was observed for husbands. This is due to his special position as the MIP and the provider of support for the woman in such a situation. 9 However, ∼10% of elective abortions were performed without informing the MIP. This could be explained by the father's religious prejudice or by different levels of involvement in the tasks of childbearing: in many societies, such as Iran, women are more often thought to be solely responsible for this task. 9 Other studies conducted in Iran have also found that men were less satisfied with their wives' terminating UPs and that women who had failed to gain their husband's consent were likely to obtain an abortion without. 9 With the exception of their husband, the women in this study were more likely to disclose their abortion to women than men. Other studies report that, in general, female-to-female disclosure is higher than female-to-male disclosure. 26 Moreover, the shame of disclosing sexual and reproductive issues to members of the opposite gender contributes to different levels of disclosure between men and women. Furthermore, the women disclosed their abortions to more consanguineal family members than affinal family members, which might be due to women being more likely to be blamed by affinal families than by consanguineal families. 24 27 However, in the case of elective abortions, the participants were more likely to disclose their abortion to non-family members than to family members, even consanguineal family members (which are the closest family members). This difference may be because women trust their peers and very close friends enough to disclose sensitive personal issues; 28 29 in addition, family members might be more likely than non-family members to want to prevent women from obtaining an elective abortion.
Strengths and limitations
We acknowledge that our study has several limitations; the most important challenge in this study was the low participation rates of women who had had abortions and reproductive health providers. Reproductive health providers were often unwilling to cooperate because of the severe legal restrictions on abortion in Iran. As a result, we tried to encourage their participation using different strategies, such as holding meetings to explain the study method, assuring them of confidentiality and anonymity protection, and providing financial incentives. We also had difficulty obtaining women's consent to participate, particularly in cases of elective abortion and for unmarried women. Sometimes women who had been introduced by the midwife or gynaecologist as a patient who had obtained an elective abortion denied the intentionality of the abortion; the midwife or gynaecologist had to reassure them of the confidentiality of the study.
Furthermore, it is very common in Iranian society to use herbal medicines that do not require prescriptions. We have not assessed these traditional methods of abortion, nor have we considered abortions performed by non-medical providers or by the woman herself. The visibility of abortion in such cases might differ from that of other cases, perhaps affected by factors such as low socioeconomic status because of the high costs of elective abortion services.
We also note two points for consideration, although they do not affect the level of visibility. The first is the possibility of recording elective abortions as non-elective (if the physician and patient agree to do so). 9 However, this did not affect our results for visibility because these women pretended their abortion was medical, and their disclosing behaviour is similar to that of women who had had a medical abortion. The second point is that some married women who became pregnant outside of marriage and thus obtained an elective abortion may have reported it as an unwanted or mistimed pregnancy. This could affect the classification of the reasons for abortion but not the visibility.
Despite these limitations, this is one of the rare studies estimating AV in Iran, or even the world. It can be considered a first step in highlighting the extent of the problem in a developing and traditional society, and even beyond such societies; the results could direct policymakers to appropriate policies by providing a more realistic picture of abortion.
In this study, AV was low, but differed among social network members and by the type of abortion. This difference might be explained by social and cultural norms and the stigma surrounding abortion. The low visibility rate that we observe might explain the low estimates of abortion rates found in other studies, and this issue should be considered by policymakers when planning women's healthcare services.
Contributors: MZ collected the data. MZ, MRB and AAH analysed the data. MZ and FZ wrote the manuscript. All the authors approved the final version of the manuscript.
Competing interests: None declared.
Ethics approval: Ethics committee of Kerman University of Medical Sciences.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
1 Blood-related family.
2 Marriage-related family, also called in-laws—that is, the husband's relatives.

IMAGES
VIDEO
COMMENTS
Study cohort. A total of 307 patients were finally included in the study with 160 cases having missed abortion and 147 with continuing pregnancy to second trimester (Supplementary Fig. 1).The characteristics was listed in Supplementary Table 1.As a result, 30 years old was the cut-off value for age via X-tile software.
Pregnancy loss, also referred to as miscarriage or spontaneous abortion, is generally defined as a nonviable intrauterine pregnancy up to 20 weeks of gestation. Early pregnancy loss, which occurs in the first trimester (ie, up to 12+6 weeks gestation), is the most common type. Individuals experiencing pregnancy loss are evaluated for conditions ...
Missed abortion is defined as unrecognized intrauterine death of the embryo or fetus without expulsion of the products of conception. ... Seldom studies reported complete abortion rate within longer follow-up time, ... All women should be advised to contact the doctor in case of heavy bleeding or signs of infection. A follow-up visit is ...
The terminology used to describe the loss of an intrauterine pregnancy before fetal viability (ie, a fetus likely to survive outside of the uterus) is inconsistent in the literature and has varied over time.[1][2] Traditionally, spontaneous abortion referred to a natural pregnancy loss before 20 weeks of gestation; however, more recently, the medical literature has been transitioning away from ...
One of the strengths of our study is the inclusion of only randomized clinical trial data in a specific population (i.e., women with missed abortion of no more than 14 weeks of gestation).
1 Introduction. Missed abortion (MA), also known as silent miscarriage, usually occurs when an embryo or fetus dies, but the body does not recognize the pregnancy loss and continues to release hormones. MA is very common complication, which affects ∼15% of all clinically recognized pregnancies. The loss of a pregnancy is often distressing for women and their partners, with adverse effects on ...
weeks, and four days (Figure 2), compared to the previous ultrasound study a month prior, showed GA of 10 weeks and one day, indicating an interval missed abortion. 1 1 Open Access Case Report DOI: 10.7759/cureus.7499 How to cite this article Suwanwongse K, Shabarek N (April 01, 2020) Missed Abortion Presented with Worsening Hyperemesis Gravidarum.
A series of 18 cases of missed abortion is presented where the dead ovum was retained for at least twenty-eight days and up to one hundred and ninety-six days.No patient, in the series reported, presented alarming symptoms of retention, as toxemia, hemorrhage, or infection.Conservative management was employed.There was no maternal mortality and in only one case was there any morbidity.The ...
Missed abortion with negative biomarkers Am J Emerg Med. 2022 Jul:57:236.e5-236.e6. doi: 10.1016/j.ajem.2022.04.028. Epub 2022 Apr 25. Authors ... We report a case of a 34-year-old woman who presented to an emergency department with vaginal bleeding and abdominal pain and was found to have negative urine and serum markers of pregnancy. A ...
Relational Dialectics Theory (RDT) Because talking about one's abortion experience remains stigmatized and muted (Cockrill & Nack, Citation 2013), examining women's stories after having had a medication abortion may illuminate the competing discourses surrounding this debated moral and social issue (e.g., largely evident in the two polarized movements: Right to Choice v.
Miscarriage is generally defined as the loss of a pregnancy before viability. An estimated 23 million miscarriages occur every year worldwide, translating to 44 pregnancy losses each minute. The pooled risk of miscarriage is 15·3% (95% CI 12·5-18·7%) of all recognised pregnancies. The population prevalence of women who have had one miscarriage is 10·8% (10·3-11·4%), two miscarriages ...
Univariate and multivariate logistic regression analysis were adopted to identify the possible risk factors for missed abortion. Results: Age, gravidity, parity, history of cesarean section, history of recurrent abortion (≥ 3 spontaneous abortions), history of ectopic pregnancy and overweight or obesity (BMI > 24 kg/m 2) were related to ...
The aim of this study was to identify related factors for missed abortion through a retrospective study of serum indices.A total of 795 cases of women with missed abortion and 694 cases of women with normal pregnancy between March 2014 and March 2017 were included in the present study. The diagnosis of missed abortion was based on clinical ...
ultrasound. Intrauterine gestational sac is seen measured about 3 cm (8 w 1 d) showing non-viable fetal pole measured ~9 mm (6 w 6 d) with no fetal pulsations could be detected. The cervix shows a simple cyst measured 0.9 x 0.7 cm (nabothian cyst). Left ovary shows a cystic lesion with clear central contents and hypoechoic periphery, measured 2 ...
In a post-Dobbs case in Florida, a judge denied a 17-year-old a parental consent waiver for an abortion, citing her C-average grades. A highly publicized case just days after the SCOTUS ruling involved a rape victim who fled Ohio to seek an abortion at six-and-a-half weeks in Indianapolis; she was 10 years old.
A missed miscarriage, sometimes termed a missed abortion 3, is a situation when there is a non-viable fetus within the uterus, without symptoms of a miscarriage.. Radiographic features Ultrasound. Ultrasound diagnosis of miscarriage should only be considered when either a mean gestation sac diameter is ≥25 mm with no obvious yolk sac or a fetal pole with a crown rump length of ≥7 mm ...
Black women comprised 42% of abortion recipients, White women 30% , Hispanic women 22%, and 7% women of other races/ethnicities. Many women who sought abortions have children. More than six in 10 ...
In this study, we retrospectively analyzed the data of 160 missed abortion patients and 147 pregnant women who didn't have abortion in the first trimester in order to fully establish the possible risk factors for missed abortion, and provide evidence for early identification and intervention for patients with high risk of missed abortion. In ...
Mifepristone was first marketed in Canada in January 2017 as a 200-mg tablet combined with 800 μg of misoprostol. 10 Approval came more than 15 years after approval in the United States and more ...
The aim of this study was to identify related factors for missed abortion through a retrospective study of serum indices. A total of 795 cases of women with missed abortion and 694 cases of women with normal pregnancy between March 2014 and March 2017 were included in the present study. The diagnosis of missed abortion was based on clinical ...
Then they realized: They can't possibly answer that question. For more than a decade, state law has prohibited the state's Maternal Mortality and Morbidity Review Committee from reviewing cases of ...
Mifepristone (Mifeprex) and Misoprostol, the two drugs used in a medication abortion, are seen at the Women's Reproductive Clinic, which provides legal medication abortion services, in Santa ...
That made it more likely that any differences before and after the abortion would be missed due to the smaller number of cases examined. But when Reardon reanalyzed the data to examine the cumulative rates of mental health disorders over identical periods of time, nine months before and nine months after the abortion, the differences were ...
What you may have missed ... study finds. — Moderna wins patent case in Europe against Pfizer, BioNTech over COVID shot. — Americans divided as Supreme Court weighs abortion pill access, ...
Objective: The purpose of this study was to investigate the environmental and behavioral factors associated with the induction of missed abortion, with a particular focus on the relationship between job stress and missed abortion. Methods: This was a case-control study in which 552 women participated (267 cases, 285 controls). Job stress was measured using the Job Content Questionnaire 1.0 ...
It was mostly a bunch of word vomit that got very little attention, but it contained a damning Freudian slip that encapsulates the party's views on abortion and what rights, if any, should be ...
Near the start of the session, Sen. David Yates, D-Louisville, proposed a bill to add exceptions to the state's abortion ban in the case of incest, rape, a nonviable fetus or to protect the health ...
The visibility (95% CI) of elective, medical and spontaneous abortion was 8% (6% to 10%), 60% (54% to 66%) and 50% (43% to 57%), respectively. Women and consanguineal family were more likely to be aware of the abortion than men and affinal family. Non-family members had a low probability of knowing about the abortion, except in elective cases.