- Open access
- Published: 16 March 2006

Revision of visual impairment definitions in the International Statistical Classification of Diseases
- Lalit Dandona 1 &
- Rakhi Dandona 1
BMC Medicine volume 4 , Article number: 7 ( 2006 ) Cite this article
26k Accesses
141 Citations
6 Altmetric
Metrics details
The existing definitions of visual impairment in the International Statistical Classification of Diseases are based on recommendations made over 30 years ago. New data and knowledge related to visual impairment that have accumulated over this period suggest that these definitions need to be revised.
Three major issues need to be addressed in the revision of these definitions. First, the existing definitions are based on best-corrected visual acuity, which exclude uncorrected refractive error as a cause of visual impairment, leading to substantial underestimation of the total visual impairment burden by about 38%. Second, the cut-off level of visual impairment to define blindness in the International Statistical Classification of Diseases is visual acuity less than 3/60 in the better eye, but with increasing human development the visual acuity requirements are also increasing, suggesting that a level less than 6/60 be used to define blindness. Third, the International Statistical Classification of Diseases uses the term 'low vision' for visual impairment level less than blindness, which causes confusion with the common use of this term for uncorrectable vision requiring aids or rehabilitation, suggesting that alternative terms such as moderate and mild visual impairment would be more appropriate for visual impairment less severe than blindness. We propose a revision of the definitions of visual impairment in the International Statistical Classification of Diseases that addresses these three issues. According to these revised definitions, the number of blind persons in the world defined as presenting visual acuity less than 6/60 in the better eye would be about 57 million as compared with the World Health Organization estimate of 37 million using the existing International Statistical Classification of Diseases definition of best-corrected visual acuity less than 3/60 in the better eye, and the number of persons in the world with moderate visual impairment defined as presenting visual acuity less than 6/18 to 6/60 in the better eye would be about 202 million as compared with the World Health Organization estimate of 124 million persons with low vision defined as best-corrected visual acuity less than 6/18 to 3/60 in the better eye.
Our suggested revision of the visual impairment definitions in the International Statistical Classification of Diseases takes into account advances in the understanding of visual impairment. This revised classification seems more appropriate for estimating and tracking visual impairment in the countries and regions of the world than the existing classification in the International Statistical Classification of Diseases.
Peer Review reports
The currently available version of the tenth revision of the International Statistical Classification of Diseases and Related Health Problems (ICD) defines visual impairment categories primarily on the basis of recommendations made by a World Health Organization (WHO) Study Group in 1972 [ 1 ]. Since these recommendations of over three decades ago, there have been substantial studies on the distribution of blindness and less severe visual impairment in populations worldwide. These studies have incrementally suggested a more nuanced understanding of visual impairment and of how it should be defined to comprehend its actual burden, as revealed by recent reviews [ 2 – 6 ]. As ICD is considered the standard worldwide classification, the ICD definitions of visual impairment are used most often for worldwide estimates of visual impairment [ 4 , 5 ]. However, several issues with these ICD definitions need to be addressed for better clarity and utilisation, including some that have been referred to previously in the literature [ 2 – 5 , 7 – 10 ]. In this paper, we bring together the major issues regarding the ICD definitions of visual impairment that would benefit from revision. On the basis of current understanding of visual impairment, we propose modifications in the ICD definitions that might enable their better practical utilisation for classification and estimation of the different levels of visual impairment worldwide.
The current categories of visual impairment in ICD are shown in Table 1 , and their use to classify different levels of visual impairment is shown in Table 2 . We identified three major issues in this ICD classification that need to be addressed: use of best-corrected or presenting visual acuity, cut-off level to define blindness, and appropriateness of the term 'low vision'.
Best-corrected or presenting visual acuity
There is increasing consensus that the use of best-corrected visual acuity to assess the burden of visual impairment in a population is inappropriate as it misses visual impairment caused by uncorrected refractive error [ 2 , 3 , 5 – 7 ]. The use of presenting visual acuity, that is acuity with whatever refractive correction the person is using, is more appropriate as it enables uncorrected refractive error to be included as a cause of visual impairment. Our review of the published data suggests that there may be about 98 million persons with visual impairment due to uncorrected refractive error worldwide [ 6 ], in addition to the 161 million persons estimated by WHO to have visual impairment with best-corrected visual acuity [ 5 ]. This implies that of the estimated total 259 million persons worldwide with visual impairment, 38% would be erroneously excluded with the best-corrected acuity definition of visual impairment. This is particularly ironic as uncorrected refractive error is the most easily treatable cause of visual impairment, usually with a simple pair of spectacles. Perhaps because it is so easily treatable, it was not initially considered worthy of qualifying as a "cause" of visual impairment in the ICD definition based on recommendations made over 30 years ago [ 1 ]. However, the assumption in the ICD definition – that persons with poor vision due to uncorrected refractive error are not visually impaired because they could have better vision if they had simple refractive correction with spectacles – seems misplaced, as they have poor vision as long as they do not get refractive correction. If extended to cataract, this anomalous assumption could imply that because most persons visually impaired due to cataract could potentially have their vision restored with cataract surgery, they are not visually impaired because best correction (in this case cataract surgery) would probably restore their vision. A recent estimate suggests that uncorrected refractive error is the most common cause of visual impairment in the world [ 6 ], emphasising the urgent need to replace best-corrected visual acuity with presenting visual acuity for defining visual impairment in the ICD classification. This will avoid the huge underestimation of the actual visual impairment burden that occurs with the existing ICD definition.
For perspective, it is interesting to note that a historical analysis has suggested that the invention of eye glasses to improve vision was one of the few most important contributors to human development over the past several centuries [ 11 ]. This further underscores the need not to overlook uncorrected refractive error in the definition of visual impairment.
Since definitions of visual impairment are based on distance visual acuity, it is important to note certain features of visual impairment related to uncorrected refractive error. First, a portion of the persons who qualify as visually impaired due to uncorrected refractive error would have good near vision. Such impairment may be less disabling than the visual impairment that causes poor vision at both distance and near. More needs to be understood about the extent to which the disabling effects of these two types of visual impairment differ. Second, blindness due to uncorrected natural refractive error sets in at a young age, resulting in many more blind years suffered per person than with most other major causes of blindness that usually set in at a later age [ 12 ]. Third, disability also occurs due to uncorrected refractive error related to aging that causes difficulty in seeing at near, which usually sets in around the age of 40 years and is referred to as presbyopia. But adequate data are not available yet to suggest how this could be included in the visual impairment definitions. This deficiency would need to be addressed in the future. The first of these three features of visual impairment due to uncorrected refractive error would suggest a relatively lower disability, whereas the latter two would suggest higher unaccounted disability. Clearly, it would be useful to generate further knowledge indicating how these features could be taken into account while assessing visual impairment due to uncorrected refractive error.
Visual acuity level to define blindness
Because the ICD definition and WHO recommend use of a visual acuity level less than 3/60 to define blindness [ 1 ], many population-based surveys from less developed countries have reported blindness rates with this definition in the past [ 4 ]. There are exceptions such as India, where a visual acuity level less than 6/60 is used to define blindness [ 12 ], and recent reports from other less developed countries covering African and Chinese populations that have used visual acuity less than 6/60 to define blindness [ 13 – 16 ]. The more developed countries have often used visual acuity level less than 6/60 to define blindness [ 17 , 18 ]; the United States uses visual acuity less than or equal to 6/60 for this definition [ 19 ]. The level of human development in less developed countries has been increasing over the past few decades, as indicated by increases in life expectancy, literacy and income [ 20 ]. Since the recommendation to use visual acuity level less than 3/60 to define blindness some three decades ago [ 1 ], higher levels of vision are now required for optimal functioning even in less developed countries because of the increasing complexity of daily tasks, prompting suggestions for using a less severe level of visual impairment to define blindness [ 8 ]. We therefore suggest that a uniform definition of blindness for both the less and more developed countries as presenting visual acuity less than 6/60 is now more appropriate than the 3/60 acuity level used by the ICD definition (Table 3 ). In the existing ICD visual impairment categories, there is no visual field loss corresponding to visual acuity less than 6/60 to 3/60 (Table 1 ) [ 1 ]. It has previously been suggested that for visual acuity level of 6/60 the equivalent central visual field of 20° seems appropriate [ 21 , 22 ], and we propose this for inclusion in the ICD classification (Table 3 ).
Additionally, visual acuity less than 6/12 is often used in more developed countries to define visual impairment, as this level of vision is considered necessary for daily tasks [ 18 , 19 ]. Using logic similar to that used above for blindness, the increasing complexity of daily tasks even in less developed countries would require better vision with the passage of time. We therefore suggest that it would be useful to have a category of mild visual impairment in the ICD classification for presenting visual acuity less than 6/12 to 6/18 (Table 3 ).
The term 'low vision'
A WHO consultation has suggested "a person with low vision as one who has impairment of visual functioning even after treatment and/or refractive correction, and has a visual acuity of less than 6/18 to light perception, or a visual field of less than 10° from the point of fixation, but who uses, or is potentially able to use, vision for the planning and/or execution of a task" [ 9 ]. This definition of 'low vision' identifies persons who have poor vision after therapy and would potentially benefit from special low vision aids or rehabilitation to enhance their quality of life [ 10 ]. This seems a more appropriate use of the term 'low vision', which is evident from the common use of the term 'Low vision clinics' around the world for clinics that provide aids and rehabilitative services to such patients. In the ICD classification, the term 'low vision' is used for visual acuity less than 6/18 to 3/60 after refractive correction, which includes treatable causes such as cataract and others [ 1 , 5 ]. This causes confusion with the more apt use of the term 'low vision' for persons with untreatable visual impairment of a certain level who would benefit from low vision aids or rehabilitation. We therefore suggest that the term 'moderate visual impairment' be used in the ICD classification for presenting visual acuity less than 6/18 to 6/60 instead of 'low vision' for best-corrected visual acuity less than 6/18 to 3/60 (Table 3 ). The prefix "moderate" in this term denotes visual impairment less severe than blindness, and allows use of the term 'mild visual impairment' for presenting visual acuity less than 6/12 to 6/18.
Implications of the suggested ICD revision
We suggest revision of the ICD classification for visual impairment to reflect the modifications in the definitions suggested above and to indicate combinations of visual impairment in the two eyes of a person that are most commonly used in practical assessments of visual impairment (Table 4 ). The existing ICD classification includes two combinations of binocular visual impairment that are rarely if ever used (Table 2 ). First, blindness in one eye and low vision in the other eye (ICD code H54.1) is not needed, as this level and low vision in both eyes (ICD code H54.2) denote the same visual impairment level in the better eye of the person, and are not used separately in practical assessments of visual impairment. Second, unspecified visual loss (H54.7) is also not needed, as unqualified visual loss in both eyes (H54.3) and unqualified visual loss in one eye (H54.6) are already covered.
Although the revision we suggest for the ICD definitions seems more consistent with current understanding of visual impairment, it is important to recognise how the new estimates of visual impairment with these revised estimates could be compared with past estimates that have used the existing definitions. For this, the following issues would have to be taken into account:
Defining visual impairment as presenting visual acuity less than 6/18 in the better eye would increase the number of visually impaired persons in the world to about 259 million, compared with the WHO estimate of 161 million based on the best-corrected acuity definition, an increase of 61% [ 6 ]. This increase, indicating the true burden of visual impairment less than 6/18, would vary in magnitude in different regions of the world [ 6 ].
Changing the definition of blindness to presenting visual acuity less than 6/60 from best-corrected visual acuity 3/60 would increase the number of blind persons. We have estimated that the number of persons worldwide with presenting visual acuity less than 3/60 in the better eye would be about 42 million, which is 14% more than the 37 million estimated by WHO with best-corrected visual acuity less than 3/60 in the better eye [ 6 ]. Data from a few recent population-based studies that reported presenting visual acuity for both the less than 6/60 and less than 3/60 levels, and which enabled these two levels to be compared clearly, suggest that there could be an increase of 34–37% for less developed countries and even higher for more developed countries, in the number of persons with presenting visual acuity less than 6/60 as compared with presenting visual acuity less than 3/60 [ 12 , 23 , 24 ]. Based on this, the number of blind persons in the world as defined by presenting visual acuity less than 6/60 in the better eye can be roughly estimated at about 57 million (Table 5 ).
The proposed moderate visual impairment, defined as presenting visual acuity less than 6/18 to 6/60, would have estimates different from the existing low vision, defined in the ICD classification as best-corrected visual acuity less than 6/18 to 3/60. We have estimated an increase of about 75% worldwide for visual acuity level of less than 6/18 to 3/60 if presenting visual acuity were used instead of best-corrected acuity [ 6 ]. On the other hand, there would be a decrease due to exclusion of the less than 6/60 to 3/60 slab from the less than 6/18 to 3/60 range, estimated to be about 6% for less developed countries and larger for more developed countries based on the limited data available from the few studies using presenting visual acuity and allowing this distinction [ 12 , 23 – 25 ]. Overall, these two opposing effects would result in a rough estimate of about 202 million persons in the world with moderate visual impairment defined as presenting visual acuity less than 6/18 to 6/60 in the better eye, compared with the WHO estimate of 124 million persons with low vision defined as best-corrected acuity less than 6/18 to 3/60 in the better eye (Table 5 ).
Very few data are available for the proposed category of mild visual impairment defined as presenting visual acuity less than 6/12 to 6/18. In a national sample of adults aged 30 years or older in Bangladesh, the prevalence of mild visual impairment was 6.46%, which would add 65% to the 9.97% prevalence of all other levels of visual impairment (presenting visual acuity less than 6/18) [ 23 ]. In a sample of adults aged 40 years or older in Victoria, Australia, the prevalence of mild visual impairment was 2.51%, which would add 146% to the 1.72% prevalence of all other levels of visual impairment [ 24 ]. In these studies, mild visual impairment in a large proportion of the persons could be improved with refractive correction.
The calculations presented above should be considered as only indicative, as they are based on limited available data. However, keeping the above issues in mind would enable informed comparisons to be made between past estimates of visual impairment and the new estimates using the proposed revised ICD classification, for assessing the changes in trends of visual impairment in countries and regions of the world.
The ICD classification has provisions for an updating and revision process when the need arises [ 26 ]. It would seem to be useful for the ICD Updating and Revision Committee to consider the update/revision suggested in this manuscript, which is based on current understanding of visual impairment, as the existing classification is based on recommendations made over three decades ago.
New understanding of visual impairment has become available since the recommendations made some three decades ago, on which the existing classification of visual impairment in the International Statistical Classification of Diseases is based, suggesting that this classification must be revised.
We propose that the visual impairment definitions in the International Statistical Classification of Diseases be based on presenting visual acuity instead of best-corrected visual acuity, the visual acuity cut-off level for blindness be changed from less than 3/60 to less than 6/60, the low vision category be modified to moderate visual impairment defined as presenting visual acuity less than 6/18 to 6/60, and the category of mild visual impairment be added defined as presenting visual acuity less than 6/12 to 6/18.
According to these revised definitions, the number of blind persons in the world defined as presenting visual acuity less than 6/60 in the better eye would be about 57 million as compared with the estimate of 37 million using the current International Statistical Classification of Diseases definition of best-corrected visual acuity less than 3/60 in the better eye, and the number of persons in the world with moderate visual impairment defined as presenting visual acuity less than 6/18 to 6/60 in the better eye would be about 202 million as compared with the estimate of 124 million persons with low vision defined as best-corrected visual acuity less than 6/18 to 3/60 in the better eye.
The Updating and Revision Committee of the International Statistical Classification of Diseases could consider the update/revision of the classification of visual impairment suggested in this manuscript, as this seems more appropriate than the existing classification for estimating and tracking visual impairment in the countries and regions of the world.
World Health Organization: International Statistical Classification of Diseases and Related Health Problems. 10th revision. Current version. Version for. 2003, [ http://www.who.int/classifications/icd/en/ ] . Chapter VII. H54. Blindness and low vision
Google Scholar
Dandona R, Dandona L: Refractive error blindness. Bull World Health Organ. 2001, 79: 237-243.
CAS PubMed PubMed Central Google Scholar
Dandona L, Foster A: Patterns of blindness. Duane's Clinical Ophthalmology. Edited by: Tasman W, Jaeger EA. 2002, Philadelphia: Lippincott Williams & Wilkins, Chapter 53
Pascolini D, Mariotti SP, Pokharel GP, Pararajasegaram R, Etya'ale D, Negrel AD, Resnikoff S: 2002 global update of available data on visual impairment: a compilation of population-based prevalence studies. Ophthalmic Epidemiol. 2004, 11: 67-115. 10.1076/opep.11.2.67.28158.
Article CAS PubMed Google Scholar
Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP: Global data on visual impairment in the year 2002. Bull World Health Organ. 2004, 82: 844-851.
PubMed PubMed Central Google Scholar
Dandona L, Dandona R: What is the global burden of visual impairment?. BMC Med. 2006, 4 (1): 6-10.1186/1741-7015-4-6.
Article PubMed PubMed Central Google Scholar
Taylor H: Refractive errors: magnitude of the need. Community Eye Health. 2000, 13: 1-2.
West S, Sommer A: Prevention of blindness and priorities for the future. Bull World Health Organ. 2001, 79: 244-248.
World Health Organization: The Management of Low Vision in Children – Report of a WHO Consultation, Bangkok, 23–24 July 1992. 1993, Geneva: World Health Organization, WHO/PBL/93.27, [ http://whqlibdoc.who.int/hq/1993/WHO_PBL_93.27.pdf ]
Dandona R, Dandona L, Srinivas M, Giridhar P, Nutheti R, Rao GN: Planning low vision services in India: a population-based perspective. Ophthalmology. 2002, 109: 1871-1878. 10.1016/S0161-6420(02)01183-1.
Article PubMed Google Scholar
Landes DS: The Wealth and Poverty of Nations. 1999, New York: W.W. Norton & Company
Dandona L, Dandona R, Srinivas M, Giridhar P, Vilas K, Prasad MN, John RK, McCarty CA, Rao GN: Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci. 2001, 42: 908-916.
CAS PubMed Google Scholar
Courtright P, Hoechsmann A, Metcalfe N, Chirambo M, Noertjojo K, Barrows J, Katz J, Chikwawa Survey Team: Changes in blindness prevalence over 16 years in Malawi: reduced prevalence but increased numbers of blind. Br J Ophthalmol. 2003, 87: 1079-1082. 10.1136/bjo.87.9.1079.
Article CAS PubMed PubMed Central Google Scholar
Fouad D, Mousa A, Courtright P: Sociodemographic characteristics associated with blindness in a Nile Delta governorate of Egypt. Br J Ophthalmol. 2004, 88: 614-618. 10.1136/bjo.2003.026997.
Li S, Xu J, He M, Wu K, Munoz SR, Ellwein LB: A survey of blindness and cataract surgery in Doumen county, China. Ophthalmology. 1999, 106: 1602-1608. 10.1016/S0161-6420(99)90459-1.
Dunzhu S, Wang FS, Courtright P, Liu L, Tenzing C, Noertjojo K, Wilkie A, Santangelo M, Bassett KL: Blindness and eye diseases in Tibet: findings from a randomised, population based survey. Br J Ophthalmol. 2003, 87: 1443-1448. 10.1136/bjo.87.12.1443.
Laitinen A, Koskinen S, Harkanen T, Reunanen A, Laatikainen L, Aromaa A: A nationwide population-based survey on visual acuity, near vision, and self-reported visual function in the adult population in Finland. Ophthalmology. 2005, 112: 2227-2237. 10.1016/j.ophtha.2005.09.010.
Taylor HR, Keeffe JE, Vu HT, Wang JJ, Rochtchina E, Pezzullo ML, Mitchell P: Vision loss in Australia. Med J Aust. 2005, 182: 565-568.
PubMed Google Scholar
Congdon N, O'Colmain B, Klaver CC, Klein R, Munoz B, Friedman DS, Kempen J, Taylor HR, Mitchell P, Eye Diseases Prevalence Research Group: Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004, 122: 477-485. 10.1001/archopht.122.4.477.
United Nations Development Programme: Human Development Reports. 1990, [ http://hdr.undp.org/reports/view_reports.cfm?type=1 ] –2005
Taylor HR, Livingston PM, Stanislavsky YL, McCarty CA: Visual impairment in Australia: distance visual acuity, near vision, and visual field findings of the Melbourne Visual Impairment Project. Am J Ophthalmol. 1997, 123: 328-337.
Dandona L, Dandona R, Naduvilath TJ, McCarty CA, Nanda A, Srinivas M, Mandal P, Rao GN: Is current eye-care-policy focus almost exclusively on cataract adequate to deal with blindness in India?. Lancet. 1998, 351: 1312-1316. 10.1016/S0140-6736(97)09509-3.
Dineen BP, Bourne RR, Ali SM, Huq DM, Johnson GJ: Prevalence and causes of blindness and visual impairment in Bangladeshi adults: results of the National Blindness and Low Vision Survey of Bangladesh. Br J Ophthalmol. 2003, 87: 820-828. 10.1136/bjo.87.7.820.
VanNewkirk MR, Weih L, McCarty CA, Taylor HR: Cause-specific prevalence of bilateral visual impairment in Victoria, Australia: the Visual Impairment Project. Ophthalmology. 2001, 108: 960-967. 10.1016/S0161-6420(01)00554-1.
Dandona R, Dandona L, Srinivas M, Giridhar P, Prasad MN, Vilas K, McCarty CA, Rao GN: Moderate visual impairment in India: the Andhra Pradesh Eye Disease Study. Br J Ophthalmol. 2002, 86: 373-377. 10.1136/bjo.86.4.373.
World Health Organization: International Statistical Classification of Diseases and Related Health Problems. Updating process. [ http://www.who.int/classifications/icd/updates/en/index.html ]
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1741-7015/4/7/prepub
Download references
Author information
Authors and affiliations.
Health Studies Area, Centre for Human Development, Administrative Staff College of India, Hyderabad, India
Lalit Dandona & Rakhi Dandona
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Lalit Dandona .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
LD conceived this report, reviewed the literature and wrote the initial draft of the manuscript. RD contributed to the ideas presented and the writing of this manuscript. Both authors approved the final version of the manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Dandona, L., Dandona, R. Revision of visual impairment definitions in the International Statistical Classification of Diseases. BMC Med 4 , 7 (2006). https://doi.org/10.1186/1741-7015-4-7
Download citation
Received : 01 December 2005
Accepted : 16 March 2006
Published : 16 March 2006
DOI : https://doi.org/10.1186/1741-7015-4-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Visual Acuity
- Visual Impairment
- International Statistical Classification
- Blind Person
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Visual Acuity Scores

In this article
Visual acuity refers to the sharpness of your vision at a certain distance (typically 20 feet). Visual acuity is expressed as a fraction. When people say they have 20/20 vision, they’re talking about their visual acuity.
Visual acuity is one factor that contributes to your overall vision. Others include:
- Depth perception
- Color vision
- Peripheral awareness (side vision)
- Eye coordination
Most of the time, people with low visual acuity must wear corrective lenses like glasses or contact lenses. Refractive eye surgery , such as LASIK, can also help.
What Is 20/20 Vision?
Having 20/20 vision means you can see the same level of detail from a distance of 20 feet as an average person.
20/25 vision means that you need to be 20 feet away to see clearly what a person with normal eyesight can see from 25 feet away.
What Contributes to Visual Acuity?
Visual acuity is dependent on a combination of optical and neural elements. These include:
- The health and functionality of the retina
- How sharply the retina forms images
- How well your brain can interpret sensory inputs
What Is a Visual Acuity Test?
A visual acuity test is a type of eye examination that measures your ability to see details at a specific distance.
Optometrists use visual acuity tests to help determine the level of vision correction required for your eyeglasses or contact lens prescription.
Visual acuity is measured by charts, optical instruments, or computerized tests during an eye exam. Visual acuity tests are noninvasive and don’t involve any risks or special preparation.
Where to Buy Glasses + Contacts
Best Overall: Warby Parker
Fastest Delivery: EyeBuyDirect
Also Great: Liingo
Best Place to Buy Contacts: Discount Contacts
What Are the Types of Visual Acuity Tests?
Eye charts are the most common type of visual acuity test. They show several rows of optotypes (letters, numbers, or symbols) progressively smaller towards the bottom.

The most frequently used visual acuity tests are the Snellen Eye Chart (left) and the Random E Chart (right).
Snellen Test
The Snellen test is the visual acuity test most people are familiar with. It uses the Snellen chart, which contains many rows of different letters that become increasingly smaller. The letters on a Snellen chart are large at the top, with the smallest line at the bottom.
Your eye care provider will ask you to read lines on the Snellen chart until you can’t make the letters out anymore. Some Snellen charts are projected onto the wall.
Random E Test
The random E test is similar to the Snellen test but only uses the capital letter E. The letters on the random E chart are flipped (rotated) in various directions. Like the Snellen test, the random E test has letters that get smaller toward the bottom.
Your eye care specialist will ask you to read lines on the random E chart until you can’t tell which way the letter E is facing.
Visual Acuity Tests for Children
Because young children may not yet be able to name letters, they have special visual acuity tests.
A pediatric eye care specialist may have an eye chart containing symbols children can easily identify.
What Does a Visual Acuity Score Mean?
A visual acuity score results from a visual acuity test performed by an optometrist or ophthalmologist during an eye exam.
Visual acuity scores are usually written as a fraction. These test results describe your ability to see an object 20 feet away compared to a person with normal vision.
For example, 20/20 vision means seeing an object clearly from 20 feet away. The medical term for this is emmetropia .
What Vision Problems Affect Visual Acuity Scores?
Various eye conditions can affect visual acuity, including refractive errors and neural factors. A comprehensive eye exam by an eye care specialist can help diagnose these problems.
Refractive Errors
Refractive errors or neural factors usually cause poor visual acuity. A refractive error is a visual impairment that affects the way light is bent, or refracted, in your eyeball.
Common refractive errors include:
- Hyperopia (farsightedness). This is blurry near vision but clear distance vision.
- Myopia (nearsightedness). This is blurry distance vision while close objects are clear.
- Presbyopia (age-related farsightedness). A loss of focusing ability on near objects that occurs with age.
- Astigmatism. Irregular curvature of the eyeball that causes blurred vision for objects up close and far away.
Neural Factors
Neural factors occur in the retina, brain, or the pathway between the two. Examples include:
- Age-related macular degeneration (AMD)
- Detached retina
- Amblyopia ( lazy eye )
- Brain injuries
What Is the Purpose of a Visual Acuity Test?
A visual acuity test will help assess your visual function and diagnose common vision problems, such as refractive errors. It’s a key part of a comprehensive eye exam.
Children frequently get their visual acuity tested to detect potential vision problems early on, while they’re easiest to treat.
You will likely need to take a corrected visual acuity test (wearing your glasses or contacts, if you use them) to get a driver’s license.
How Is a Visual Acuity Test Performed?
An optometrist or ophthalmologist typically performs a visual acuity test as part of a comprehensive eye exam. Opticians, technicians, and nurses can also perform a visual acuity test.
You’ll be seated a certain distance from the visual acuity chart during the eye exam. Elements such as distance from the test chart and lighting conditions must be standardized.
You’ll cover one eye and read the chart with the uncovered eye. You’ll start at the top and proceed downwards until you can’t distinguish the letters.
Then you’ll switch to the other eye and repeat the process from the same viewing distance. The doctor will use the smallest visible letter size line to determine your results.
Visual Acuity Test Interpretation
Visual acuity is typically measured as a fraction or decimal number. The first is the testing distance, and the second refers to the distance from which the average person could see the same details. The higher the second fraction number, the lower the visual acuity.
Most vision testing in the United States uses the Snellen chart, which requires a test distance of 20 feet. In other countries, visual acuity is expressed using the metric system. Because 20 feet is equivalent to 6.096 meters, 20/20 vision is equal to 6/6 vision.
For example, 6/12 is a metric measurement on the Snellen test. It’s equivalent to 20/40 in feet, .50 in decimal, and .30 on the LogMAR scale.
20/20 vision means that a person can see an object, as does anyone with normal vision from 20 feet.
LogMAR Chart
The National Vision Research Institute of Australia developed the LogMAR chart (Logarithm of the Minimum Angle of Resolution) in 1976.
The Bailey-Lovie chart and ETDRS chart (Early Treatment Diabetic Retinopathy Study) are two charts that use the LogMAR scale.
Its design provides a more accurate visual acuity score than other charts. With a LogMAR chart, your visual acuity score is measured in reference to the minimum angle of resolution.

Visual Acuity Scale
| 20/200 | 6/60 | 0.10 | 1.00 |
| 20/160 | 6/48 | 0.125 | 0.90 |
| 20/125 | 6/38 | 0.16 | 0.80 |
| 20/100 | 6/30 | 0.20 | 0.70 |
| 20/80 | 6/24 | 0.25 | 0.60 |
| 20/63 | 6/19 | 0.32 | 0.50 |
| 20/50 | 6/15 | 0.40 | 0.40 |
| 20/40 | 6/12 | 0.50 | 0.30 |
| 20/32 | 6/9.5 | 0.63 | 0.20 |
| 20/25 | 6/7.5 | 0.80 | 0.10 |
| 20/20 | 6/6 | 1.00 | 0.00 |
| 20/16 | 6/4.8 | 1.25 | −0.10 |
| 20/12.5 | 6/3.8 | 1.60 | −0.20 |
| 20/10 | 6/3 | 2.00 | −0.30 |
Visual acuity refers to your ability to see details at a specific distance. Most of the time, visual acuity is expressed as a fraction, such as 20/20 vision.
An eye care specialist will perform a visual acuity test during a routine eye exam. This helps detect vision problems and determine the level of vision correction needed for your eyeglass prescription.
The most common types of visual acuity tests use the Snellen chart or the random E chart.
Best Places to Buy Glasses

Best Overall
Warby Parker has stylish, high-quality frames at affordable prices.

Liingo Eyewear is another great option to buy glasses online.

Best on a Budget
EyeBuyDirect has a wide variety of budget frames starting at $6.
Best Places to Buy Contacts

Discount Contacts is our #1 recommendation to buy contacts online.

GlassesUSA has a huge selection of contacts, glasses, & sunglasses.
Related Articles

Visual Acuity: What is 20/20 Vision?
by Dr. Melody Huang, O.D.

Is 1.25 Eye Prescription Bad?
Medically Reviewed by Dr. Melody Huang, O.D.

How to Know if Your Eye Prescription is Bad

What Does Axis Mean for Glasses Prescriptions?

20/25 Vision: Understanding What It Means

Dominant Eye Test and Meaning
- Kniestedt, C., and Stamper, R.L. “ Visual acuity and its measurement .” Ophthalmology Clinics of North America, 2003
- Bailey, I.L., and Lovie, J.E. “New design principles for visual acuity letter charts. American Journal of Optometry and Physiological Optics .” American Journal of Optometry and Physiological Optics, 1976.
- Raasch et al. “ Repeatability of visual acuity measurement .” Optometry and Vision Science: Official Publication of the American Academy of Optometry, 1998.
- Lovie-Kitchin, JE. “ Validity and reliability of visual acuity measurements .” Ophthalmic & Physiological Optics: The Journal of the British College of Ophthalmic Opticians (Optometrists), 1988.
- Marsden et al. “ How to measure distance visual acuity .” Community Eye Health, 2014.
- “ Visual acuity test .” UCSF Health, 2019.

- Find a Lasik Surgeon Near You
- Find Optometrist Near You
- Contact Lenses
Other Links
- Advertise With Us
- Privacy Policy
- Listen to the Podcast
Social Links

- For Ophthalmologists
- For Practice Management
- For Clinical Teams
- For Public & Patients
Museum of the Eye
- Eye Health A-Z
- Glasses & Contacts
- Tips & Prevention
- Ask an Ophthalmologist
- Patient Stories
- No-Cost Eye Exams
- For Public & Patients /
- Eye Exam and Vision Testing Basics
- Get an Eye Disease Screening at 40
- Home Vision Tests for Children and Adults
- Eye Pressure Testing
Visual Field Test
Visual Acuity
All About the Eye Chart
- What Does 20/20 Vision Mean?

What is visual acuity?
Visual acuity measures how sharp your vision is at a distance. It is usually tested by reading an eye chart.
How is visual acuity tested?
- The Snellen eye chart , with its familiar rows of letters in decreasing sizes, is the most common visual acuity test. While standing or sitting 20 feet from the chart, you are instructed to read each row until you no longer can.
- The Random E test uses a capital letter E that gets smaller in size and also changes direction (up, down, left, right). The test is completed when you can’t tell which direction the E is facing.
- Simplified testing for children. The child is given cards with symbols or letters, which are matched to those on the chart.
You can also test visual acuity at home . But home tests are not meant to replace an exam given by an eye care professional. Your ophthalmologist tests visual acuity as part of a comprehensive eye exam , but others may perform the test, including:
- a pediatrician or other doctor
- a technician or medical assistant
- an optician
Visual acuity can also be tested at schools and most states require testing before issuing a driver’s license.
What do my test results mean?
The results of a visual acuity test are written as a fraction in the U.S. The top number is always the same and signifies the distance between you and the chart, 20 feet. The bottom number is the last line read correctly. For example, a result of “20/20” —normal visual acuity—means you read the line that those with normal vision can read . Visual acuity decreases as the bottom number gets larger. A result of 20/40 means you can see at 20 feet what those with normal vision can see from 40 feet away.
Why would I not have 20/20 vision?
Visual acuity less than 20/20 is common. In most cases, blurry vision from a refractive error ( nearsightedness , farsightedness or astigmatism ) is to blame. The good news is that glasses, contact lenses or surgery can likely improve your vision to 20/20 or close to it.
Sometimes eye disease, infection or other health problems reduce your visual acuity. In this case, you and your doctor can discuss next steps and what treatment may be needed.
Visual acuity isn’t everything…
We all want uncorrected 20/20 vision, but remember, visual acuity is just one facet of your eye health. With regular eye exams, your ophthalmologist can monitor the entire range of your visual function, including:
- best corrected (with glasses or contact lenses) visual acuity
- peripheral (side) vision
- depth perception (seeing objects in three dimensions)
- eye movement
- binocular (two-eye) function
- the health of the retina, in the back of your eye
- Find an Ophthalmologist Search Advanced Search

Free EyeSmart Newsletter
All content on the Academy’s website is protected by copyright law and the Terms of Service . This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
- About the Academy
- Jobs at the Academy
- Financial Relationships with Industry
- Medical Disclaimer
- Privacy Policy
- Terms of Service
- Statement on Artificial Intelligence
- For Advertisers
- Ophthalmology Job Center
FOLLOW THE ACADEMY
Medical Professionals
Public & Patients
- Vision Test
- How is near vision measured?
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- HIV and AIDS
- Hypertension
- Mental disorders
- Top 10 causes of death
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
Blindness and vision impairment
- Globally, at least 2.2 billion people have a near or distance vision impairment. In at least 1 billion of these, vision impairment could have been prevented or is yet to be addressed.
- The leading causes of vision impairment and blindness at a global level are refractive errors and cataracts.
- It is estimated that globally only 36% of people with a distance vision impairment due to refractive error and only 17% of people with vision impairment due to cataract have received access to an appropriate intervention.
- Vision impairment poses an enormous global financial burden, with the annual global cost of productivity estimated to be US$ 411 billion.
- Vision loss can affect people of all ages; however, most people with vision impairment and blindness are over the age of 50 years.
Vision, the most dominant of our senses, plays a critical role in every facet and stage of our lives. We take vision for granted, but without vision, we struggle to learn, to walk, to read, to participate in school and to work.
Vision impairment occurs when an eye condition affects the visual system and its vision functions. Everyone, if they live long enough, will experience at least one eye condition in their lifetime that will require appropriate care.
Vision impairment has serious consequences for the individual across the life course. Many of these consequences can be mitigated by timely access to quality eye care. Eye conditions that can cause vision impairment and blindness – such as cataract or refractive error – are, for good reasons, the main focus of eye care strategies; nevertheless, the importance of eye conditions that do not typically cause vision impairment – such as dry eye or conjunctivitis – must not be overlooked. These conditions are frequently among the leading reasons for presentation to eye care services.
Globally, the leading causes of vision impairment and blindness are:
- refractive errors
- diabetic retinopathy
- age-related macular degeneration.
There is substantial variation in the causes of vision impairment between and within countries according to the availability of eye care services, their affordability, and the education of the population. For example, the proportion of vision impairment attributable to unoperated cataract is higher in low- and middle-income countries. In high income countries, diseases such as glaucoma and age-related macular degeneration are more common.
Among children, congenital cataract is a leading cause of vision impairment in low-income countries, whereas in middle-income countries it is more likely to be retinopathy of prematurity.
Uncorrected refractive error remains a leading cause of vision impairment in all countries amongst children and adult populations.
Globally, at least 2.2 billion people have a near or distance vision impairment. In at least 1 billion – or almost half – of these cases, vision impairment could have been prevented or has yet to be addressed.
Among this 1 billion people, the main conditions causing distance vision impairment or blindness are cataract (94 million), refractive error (88.4 million), age-related macular degeneration (8 million), glaucoma (7.7 million), diabetic retinopathy (3.9 million) (1) . The main condition causing near vision impairment is presbyopia (826 million) (2) .
In terms of regional differences, the prevalence of distance vision impairment in low- and middle-income regions is estimated to be 4 times higher than in high-income regions (1) . With regards to near vision, rates of unaddressed near vision impairment are estimated to be greater than 80% in western, eastern and central sub-Saharan Africa, while comparative rates in high-income regions of North America, Australasia, western Europe, and of Asia-Pacific are reported to be lower than 10% (2) .
Population growth and ageing are expected to increase the risk that more people acquire vision impairment.
Impact of vision impairment
Personal impact.
Young children with early onset irreversible severe vision impairment can experience delayed motor, language, emotional, social and cognitive development, with lifelong consequences. School-age children with vision impairment can also experience lower levels of educational achievement.
Vision impairment severely impacts quality of life among adult populations. Adults with vision impairment can experience lower rates of employment and higher rates of depression and anxiety.
In the case of older adults, vision impairment can contribute to social isolation, difficulty walking, a higher risk of falls and fractures, and a greater likelihood of early entry into nursing or care homes.
Economic impact
Vision impairment poses an enormous global financial burden with an estimate annual global productivity loss of about US$ 411 billion purchasing power parity (3) . This figure far outweighs the estimated cost gap of addressing the unmet need of vision impairment ( estimated at about US$ 25 billion ).
Strategies to address eye conditions to avoid vision impairment
There are effective interventions covering promotion, prevention, treatment and rehabilitation which address the needs associated with eye conditions and vision impairment. While many vision loss cases can be prevented (such as those due to infections, trauma, unsafe traditional medicines, perinatal diseases, nutrition-related diseases, unsafe use or self-administration of topical treatment), this is not possible for all. For many eye conditions, e.g. diabetic retinopathy, early detection and timely treatment are crucial to avoid irreversible vision loss. Spectacle correction for refractive error and surgery for cataract are among the most cost-effective of all health-care interventions. Yet, globally only 36% of people with a distance vision impairment due to refractive error have received access to an appropriate pair of spectacles and only 17% of people with vision impairment or blindness due to cataract have received access to quality surgery.
Treatment is also available for many eye conditions that do not typically cause vision impairment, such as dry eye, conjunctivitis and blepharitis, but generate discomfort and pain. Treatment of these conditions is directed at alleviating the symptoms and preventing the evolution towards more severe stages of those diseases.
Vision rehabilitation is very effective in improving functioning for people with an irreversible vision loss that can be caused by eye conditions such as diabetic retinopathy, glaucoma, consequences of trauma, and age-related macular degeneration.
WHO response
WHO’s work is guided by the recommendations of the WHO World report on vision (2019) and the resolution on "integrated, people-centred eye care, including preventable blindness and vision impairment" adopted at the Seventy-third World Health Assembly in 2020. The key proposal is to make integrated people-centred eye care (IPEC) the care model of choice and to ensure its widespread implementation. It is expected that by shaping the global agenda on vision and eye care, the report and resolution will assist Member States and their partners in their efforts to reduce the burden of eye conditions and vision.
Some of WHO’s key areas of work and activities in the prevention of blindness include:
- Developing reports of the effective coverage of eye care indicators to monitor progress towards the 2030 global targets .
- Developing resources and technical tools to support the integration of eye care into health information systems .
- Observing and promoting World Sight Day as an annual advocacy event.
- The Eye care in health systems: Guide for action .
- The Package of eye care interventions (PECI) .
- The Eye care competency framework (ECCF) .
- The Eye care situation analysis tool
- The Tool for the assessment of diabetic retinopathy and diabetes management services.
- The Tool for the assessment of glaucoma services.
- The Tool for the assessment of refractive services.
- The Tool for the assessment of rehabilitation services and systems.
- The MyopiaEd: a mobile health toolkit for myopia to increase health literacy .
- A population-facing app for near and distance visual acuity testing.
- Graphics promoting healthy eye habits .
1. GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021 Feb;9(2):e144-e160. doi: 10.1016/S2214-109X(20)30489-7.
2. Fricke, TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Suit MH, Naduvilath T, Naidoo K, Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling, Ophthalmology. 2018 May 9.
3. Burton MJ, Ramke J, Marques AP, Bourne RR, Congdon N, Jones I, et al. The Lancet Global Health commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021; 9(4):e489–e551.
Health topic page
- WHO’s work on eye care, vision impairment and blindness (who.int)
Related links
- Report of the 2030 targets on effective coverage of eye care (who.int)
- Eye care in health systems: guide for action (who.int)
- World report on vision (who.int)
- Blurry Vision
- Conjunctivitis - Pink Eye
- Corneal Abrasions
- Eye Discharge
- Dilated Pupils
- Eye Infections
- Eye Twitching
- Ocular Migraines
- Swollen Eyelids
- How to Get Rid of a Stye
- Blepharitis
- Eye Floaters
- Myopia in Children
- Myopia (nearsightedness)
- Astigmatism
- Contrast sensitivity testing
- Refractive errors and refraction
- Visual Acuity: 20/20 Vision
- Hyperopia (farsightedness)
- Digital Eye Strain
- Computer Glasses
- Kids & Screen Time
- Blue Light and Vision
- Blue Light Glasses
- How to Choose Eyeglass Lenses
- Anti-reflective Lenses
- Progressive Lenses
- Eyeglass Lens Coatings
- Photochromic Lenses
- Multi-focal Lenses
- Eyeglass Frame Materials
- How to Clean Your Glasses
- What do the numbers on your eyeglass frames mean?
- Eyeglass temples: How do you know if they're the right length?
- Can you be allergic to eyeglasses?
- The Best Glasses for Your Face Shape
- Pupillary Distance
- Glasses for Round Faces
- Glasses for Small Faces
- Glasses for Long Faces
- Sunglasses for Oval Faces
- How Much Do Glasses Cost?
- Cheap Glasses
- Choosing Eyeglasses
- Best Places to Buy Glasses
- How to Solve Problems with New Glasses
- Styles: Trends in Men's Glasses
- Polarized Lenses
- Prescription Sunglasses Guide
- Ray-Ban Wayfarer Guide
- Performance Sunglasses
- Are Designer Shades Worth It?
- How to Spot Fake Wayfarer Sunglasses
- Guide to High-Quality Sunglasses
- Tint Guide for Sports Sunglasses
- UV Radiation and Your Eyes
- Contact Lens Basics
- Reading a Contact Lens Prescription
- Soft Contact Lens Care
- Daily Disposable Contacts
- Buying Contacts Without a Prescription?
- Bifocal Contacts
- Toric Contact Lenses
- Colored Contacts
- Multifocal Contacts
- Gas Permeable Contact Lenses
- Scleral GP Contact Lenses
- What is vision insurance?
- How to Use Vision Insurance Benefits
- Check Your Vision Insurance Benefits
- EyeMed Vision Insurance
- VSP Vision Insurance
- Vision Insurance or Vision Benefits Plan
- Vision Insurance Provider List
- Provider Networks and Vision Insurance
- What is Covered by Vision Insurance?
- Medicare & Medicaid Vision Benefits
- Medicare Advantage Plans (Part C Plans)
- Medicaid: Eligibility and Vision Benefits
- How to Get Free Eye Exams and Glasses
- LASIK Eye Surgery Guide
- Cost of LASIK
- LASIK Risks
- How Long Does LASIK Last?
- Does LASIK Hurt?
- Do I Have To Be Awake During LASIK?
- PRK Surgery
- SMILE Laser Surgery
- Epi-LASIK Surgery
- Lens Replacement Surgery
- LASEK Eye Surgery
- PresbyLASIK
- Cataract Surgery
- Laser Cataract Surgery
- Cataract Surgery Video
- Cataract Surgery Recovery
- Cataract Surgery Complications
- Cataract Surgery Cost
- What to Expect During Eye Exams
- Free Eye Exams
- What is an Eye Test?
- How to Read Your Eyeglass Prescription
- How to Choose an Eye Doctor
- Infant vision development
- Are contact lenses a good choice for kids?
- Reading glasses: Tips before you buy
- How older drivers can improve their driving at night
- Lutein & Zeaxanthin
- Eye Vitamins and Supplements
- Omega-3 Fatty Acids
- Safety Glasses
- Sports Glasses & Goggles
- Eye Safety Basics
- Contact Lenses for Sports
- Shooting Glasses and Hunting Eyewear
- Ski Goggles
- Eye Diagram
- Baby's Eye Colors
- Dominant Eye Test
- Color Blindness
- Color Blind Tests
Trusted Content
This article was written or reviewed by an All About Vision expert contributor, a partner medical reviewer or a member of our medical advisory board.
Sources used at the time of publication are provided in the Notes and References section. These may include peer-reviewed scientific research, data from government health authorities, and other trusted sources of information.
Visual acuity and visual acuity tests
By Sonia Kelley, OD, MS
What is visual acuity?
How is visual acuity measured, what are common distance visual acuity tests, what are common near visual acuity tests, how is visual acuity measured in infants, why are visual acuity tests useful, is there more to vision than visual acuity, can kids have perfect visual acuity and still have vision problems, how can i get my visual acuity tested.
Visual acuity is the ability to see distinct figures and fine detail with clarity. With good visual acuity, the outline of an object is sharp and easily detectable.
Visual acuity tests measure how well a person sees fine details at distance and near.
Doctors test visual acuity by using eye charts. They measure how well a person can see fine detail at a specific distance. High contrast figures (for example, black letters on a white chart) are used in visual acuity tests.
Visual acuity tests provide information about how clearly a person is seeing. For example, the ability to see street signs, the front of a classroom or words in a book depends on good visual acuity.
There are many types of visual acuity tests . These tests are designed for different ages and levels. For example, a small child who cannot speak yet will need a different visual acuity test than a college student.
Distance visual acuity tests are usually done at 20 feet or 6 meters. “Perfect vision” is considered to be 20/20 vision .
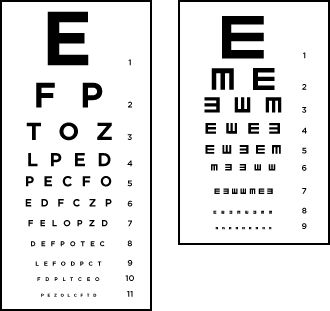
How a Snellen chart and a "tumbling E" chart might look at your eye doctor's office.
The most commonly used tests to measure distance visual acuity are:
Snellen Chart – A chart with rows of capital letters, with each row decreasing in size. Usually used for older children and adults
Random E Chart – A chart with rows of a “tumbling” E facing different directions. Each row decreases in size, similar to the Snellen chart. Usually used for young children who can point in the direction that the E is facing.
Near vision tests are usually done at 16 inches or 40 cm. The most common near visual acuity tests are:
Reduced Snellen – A miniature Snellen test. “Perfect” vision is the ability to read the 20/20 line.
Jaeger – Paragraphs of text increasing in size. “Perfect” vision is the ability to read the J-1 line.
Infant visual acuity is measured by a technique called “ preferential looking .” The most common type of preferential looking test is with the use of Teller Acuity Cards .
Preferential looking tests do not need a person to respond. They are performed using the following technique:
The tester holds up a blank, gray card with no pattern and a card with a pattern that is “more interesting” to look at.
The person being tested turns their head to look at the “more interesting” card with a pattern.
As the test progresses, sharper visual acuity is needed to see the markings on the patterned card.
When the patterns on the card become too difficult to see, both cards look alike. There is no head turn due to “preferential looking.”
Doctors use visual acuity tests to determine the correct prescription for glasses or contact lenses.
Visual acuity tests can also determine whether:
An infant or child has proper visual development .
A person has the required visual acuity to get a drivers license .
A person qualifies for special services due to decreased visual acuity.
A disease has progressed and caused changes in vision.
A medication is effective in stabilizing vision or preventing vision loss.
Yes. The brain gets many different signals that contribute to vision. A visual acuity test measures one aspect of vision: how clearly a person sees a high contrast object.
Driving in rainy weather, keeping your eye on a soccer ball or chopping vegetables all require more than just good visual acuity. Many components of vision work together to give “good vision.”
Some components that contribute to good vision include :
Contrast sensitivity – The ability to discern a figure from its background.
Color – The ability to perceive different colors (see color blindness ).
Depth perception – The ability to judge the distance of an object, 3D vision.
Glare sensitivity – A decrease in visual acuity due to bright lighting.
Visual fields – Your field of vision when your eyes are focused ahead.
Binocular vision – The ability to clearly focus on a single target with both eyes.
Visual tracking – The ability to track moving objects.
Yes. Good visual acuity does not guarantee that a child has all the visual skills needed to perform well academically and outside the classroom.
Some kids who have “perfect” visual acuity may still need visual therapy to address other visual problems.
READ MORE: Vision therapy for kids
Vision issues that may require visual therapy are:
Amblyopia – “Lazy eye” due to improper vision development in childhood.
Strabismus – “Crossed eyes” due to eyes not lining up and working together.
Binocular vision disorders – Double vision due to the eyes not being able to focus together and see a single image.
Tracking difficulty – A decreased ability to visually track moving objects.
Accommodative disorders – A decreased ability to focus on near objects.
A comprehensive eye exam , including visual acuity testing, can be performed at an eye doctor’s office.
Keeping your eyes healthy by eating nutrient rich foods , exercising and spending time outdoors will help to maintain good visual acuity throughout life.
Notes and References
How to measure distance visual acuity . Community Eye Health . June 2014.
‘ Preferential looking’ for monocular and binocular acuity testing of infants . British Journal of Ophthalmology . April 1982.
Teller acuity cards reference and instruction manual . Stereo Optical Co. 2005.
Distance and near visual acuity, contrast sensitivity, and visual fields of 10-year-old children . JAMA Ophthalmology. January 1999.
Page published on Tuesday, July 20, 2021

Schedule an exam
What your eye doctor can tell about your heart health
How the covid-19 omicron and delta variants could affect your eyes, how to limit your child’s screen time with digital apps, eye symptoms commonly seen in multiple sclerosis, ray-ban stories: features, pros and cons.

How to find the best computer glasses in 2024
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 18 October 2023
Associations of presenting visual acuity with morphological changes on OCT in neovascular age-related macular degeneration: PRECISE Study Report 2
- Shruti Chandra ORCID: orcid.org/0000-0002-2634-9775 1 , 2 ,
- Sarega Gurudas 2 ,
- Benjamin J. L. Burton ORCID: orcid.org/0000-0001-9579-9078 3 ,
- Geeta Menon 4 ,
- Ian Pearce 5 ,
- Martin Mckibbin ORCID: orcid.org/0000-0003-4388-243X 6 ,
- Ajay Kotagiri 7 ,
- James Talks 8 ,
- Anna Grabowska ORCID: orcid.org/0000-0002-3053-2142 9 ,
- Faruque Ghanchi ORCID: orcid.org/0000-0002-4448-8162 10 ,
- Richard Gale 11 ,
- Andrea Giani 12 ,
- Victor Chong ORCID: orcid.org/0000-0002-7693-522X 2 ,
- Taffeta Ching Ning Yamaguchi 12 ,
- Bishwanath Pal 1 ,
- Sridevi Thottarath 1 ,
- Raheeba Muhamed Pakeer 1 ,
- Swati Chandak 1 ,
- Andrea Montesel 1 &
- Sobha Sivaprasad 1 , 2
Eye volume 38 , pages 757–765 ( 2024 ) Cite this article
279 Accesses
1 Altmetric
Metrics details
- Business and industry
- Predictive markers
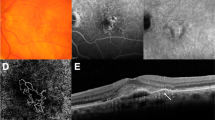
To study associations of optical coherence tomography (OCT) features with presenting visual acuity (VA) in treatment naive neovascular age-related macular degeneration (nAMD).
Patients with nAMD initiated on aflibercept therapy were recruited from December 2019 to August 2021. Demographic and OCT (Spectralis, Heidelberg Engineering) features associated with good VA (VA ≥ 68 ETDRS letters, Snellen ≥ 6/12) and poor VA (VA < 54 letters, Snellen < 6/18) were analysed using Generalised Estimating Equations to account for inter-eye correlation.
Of 2274 eyes of 2128 patients enrolled, 2039 eyes of 1901 patients with complete data were analysed. Mean age was 79.4 (SD 7.8) years, female:male 3:2 and mean VA 58.0 (SD 14.5) letters. On multivariable analysis VA < 54 letters was associated with increased central subfield thickness (CST) (OR 1.40 per 100 µm; P < 0.001), foveal intraretinal fluid (OR 2.14; P < 0.001), polypoidal vasculopathy (PCV) relative to Type 1 macular neovascularisation (MNV) (OR 1.66; P = 0.049), presence of foveal subretinal hyperreflective material (SHRM) (OR 1.73; P = 0.002), foveal fibrosis (OR 3.85; P < 0.001), foveal atrophy (OR 5.54; P < 0.001), loss of integrity of the foveal ellipsoid zone (EZ) or external limiting membrane (ELM) relative to their preservation (OR 3.83; P < 0.001) and absence of subretinal drusenoid deposits (SDD) (presence vs absence; OR 0.75; P = 0.04). These features were associated with reduced odds of VA ≥ 68 letters except MNV subtypes and SDD.
Presence of baseline fovea-involving atrophy, fibrosis, intraretinal fluid, SHRM, PCV EZ/ELM loss and increased CST determine poor presenting VA. This highlights the need for early detection and treatment prior to structural changes that worsen baseline VA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
251,40 € per year
only 13,97 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Association between visual acuity, lesion activity markers and retreatment decisions in neovascular age-related macular degeneration

Baseline predictors for subretinal fibrosis in neovascular age-related macular degeneration
Characterisation of macular neovascularisation subtypes in age-related macular degeneration to optimise treatment outcomes
Data availability.
The anonymised PRECISE clinical database analysed during the current study is available from author SS on approval of a data sharing agreement. Sharing of retinal images requires patient consent and sponsor approval.
Rahman F, Zekite A, Bunce C, Jayaram H, Flanagan D. Recent trends in vision impairment certifications in England and Wales. Eye. 2020;34:1271–8.
Article PubMed Central PubMed Google Scholar
Ying GS, Maguire MG, Daniel E, Ferris FL, Jaffe GJ, Grunwald JE, et al. Association of baseline characteristics and early vision response with 2-year vision outcomes in the comparison of AMD treatments trials (CATT). Ophthalmology. 2015;122:2523–31.e1.
Article PubMed Google Scholar
Ying GS, Huang J, Maguire MG, Jaffe GJ, Grunwald JE, Toth C, et al. Baseline predictors for one-year visual outcomes with ranibizumab or bevacizumab for neovascular age-related macular degeneration. Ophthalmology. 2013;120:122–9.
Ho AC, Albini TA, Brown DM, Boyer DS, Regillo CD, Heier JS. The potential importance of detection of neovascular age-related macular degeneration when visual acuity is relatively good. JAMA Ophthalmol. 2017;135:268–73.
Diabetic Retinopathy Clinical Research, N, Wells JA, Glassman AR, Ayala AR, Jampol LM, Aiello LP, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372:1193–203.
Article Google Scholar
Ho AC, Kleinman DM, Lum FC, Heier JS, Lindstrom RL, Orr SC, et al. Baseline visual acuity at wet AMD diagnosis predicts long-term vision outcomes: an analysis of the IRIS registry. Ophthalmic Surg Lasers Imaging Retina. 2020;51:633–9.
Chae B, Jung JJ, Mrejen S, Gallego-Pinazo R, Yannuzzi NA, Patel SN, et al. Baseline predictors for good versus poor visual outcomes in the treatment of neovascular age-related macular degeneration with intravitreal Anti-VEGF therapy. Invest Ophthalmol Vis Sci. 2015;56:5040–7.
Article CAS PubMed Google Scholar
Rao P, Lum F, Wood K, Salman C, Burugapalli B, Hall R, et al. Real-world vision in age-related macular degeneration patients treated with single anti-VEGF Drug Type for 1 Year in the IRIS Registry. Ophthalmology. 2018;125:522–8.
Fragiotta S, Rossi T, Cutini A, Grenga PL, Vingolo EM. Predictive factors for development of neovascular age-related macular degeneration: a spectral-domain optical coherence tomography study. Retina. 2018;38:245–52.
Naysan J, Jung JJ, Dansingani KK, Balaratnasingam C, Freund KB. Type 2 (Subretinal) neovascularization in age-related macular degeneration associated with pure reticular pseudodrusen phenotype. Retina. 2016;36:449–57.
Schlanitz FG, Baumann B, Kundi M, Sacu S, Baratsits M, Scheschy U, et al. Drusen volume development over time and its relevance to the course of age-related macular degeneration. Br J Ophthalmol. 2017;101:198–203.
Hu X, Waldstein SM, Klimscha S, Sadeghipour A, Bogunovic H, Gerendas BS, et al. Morphological and functional characteristics at the onset of exudative conversion in age-related macular degeneration. Retina. 2020;40:1070–8.
Roberts PK, Schranz M, Motschi A, Desissaire S, Hacker V, Pircher M, et al. Baseline predictors for subretinal fibrosis in neovascular age-related macular degeneration. Sci Rep. 2022;12:88.
Article ADS PubMed Central PubMed Google Scholar
Foss A, Rotsos T, Empeslidis T, Chong V. Development of macular atrophy in patients with wet age-related macular degeneration receiving anti-VEGF Treatment. Ophthalmologica. 2022;245:204–17.
Schmidt-Erfurth U, Bogunovic H, Sadeghipour A, Schlegl T, Langs G, Gerendas BS, et al. Machine learning to analyze the prognostic value of current imaging biomarkers in neovascular age-related macular degeneration. Ophthalmol Retina. 2018;2:24–30.
Jaffe GJ, Ying GS, Toth CA, Daniel E, Grunwald JE, Martin DF, et al. Macular morphology and visual acuity in year five of the comparison of age-related macular degeneration treatments trials. Ophthalmology. 2019;126:252–60.
Waldstein SM, Simader C, Staurenghi G, Chong NV, Mitchell P, Jaffe GJ, et al. Morphology and visual acuity in aflibercept and ranibizumab therapy for neovascular age-related macular degeneration in the VIEW Trials. Ophthalmology. 2016;123:1521–9.
Rim TH, Lee AY, Ting DS, Teo K, Betzler BK, Teo ZL, et al. Detection of features associated with neovascular age-related macular degeneration in ethnically distinct data sets by an optical coherence tomography: trained deep learning algorithm. Br J Ophthalmol. 2021;105:1133–9.
von der Emde L, Pfau M, Dysli C, Thiele S, Möller PT, Lindner M, et al. Artificial intelligence for morphology-based function prediction in neovascular age-related macular degeneration. Sci Rep. 2019;9:11132.
Moraes G, Fu DJ, Wilson M, Khalid H, Wagner SK, Korot E, et al. Quantitative analysis of OCT for neovascular age-related macular degeneration using deep learning. Ophthalmology. 2021;128:693–705.
Golbaz I, Ahlers C, Stock G, Schütze C, Schriefl S, Schlanitz F, et al. Quantification of the therapeutic response of intraretinal, subretinal, and subpigment epithelial compartments in exudative AMD during anti-VEGF therapy. Invest Ophthalmol Vis Sci. 2011;52:1599–605.
Abbas A, O'Byrne C, Fu DJ, Moraes G, Balaskas K, Struyven R, et al. Evaluating an automated machine learning model that predicts visual acuity outcomes in patients with neovascular age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2022;260:2461–73.
PubMed Central PubMed Google Scholar
Yeh TC, Luo AC, Deng YS, Lee YH, Chen SJ, Chang PH, et al. Prediction of treatment outcome in neovascular age-related macular degeneration using a novel convolutional neural network. Sci Rep. 2022;12:5871.
Article ADS CAS PubMed Central PubMed Google Scholar
Spaide RF, Jaffe GJ, Sarraf D, Freund KB, Sadda SR, Staurenghi G, et al. Consensus nomenclature for reporting neovascular age-related macular degeneration data: consensus on neovascular age-related macular degeneration nomenclature study group. Ophthalmology. 2020;127:616–36.
Sadda SR, Guymer R, Holz FG, Schmitz-Valckenberg S, Curcio CA, Bird AC, et al. Consensus definition for atrophy associated with age-related macular degeneration on OCT: classification of atrophy report 3. Ophthalmology. 2018;125:537–48.
Cheung CMG, Lai T, Teo K, Ruamviboonsuk P, Chen SJ, Kim JE, et al. Polypoidal choroidal vasculopathy: consensus nomenclature and non-indocyanine green angiograph diagnostic criteria from the Asia-Pacific Ocular Imaging Society PCV Workgroup. Ophthalmology. 2021;128:443–52.
Spaide RF, Ooto S, Curcio CA. Subretinal drusenoid deposits AKA pseudodrusen. Surv Ophthalmol. 2018;63:782–815.
Wu Z, Fletcher EL, Kumar H, Greferath U, Guymer RH. Reticular pseudodrusen: a critical phenotype in age-related macular degeneration. Prog Retin Eye Res. 2022;88:101017.
Hardin, JW, Hilbe JM, Generalized estimating equations. 1st ed. New York: Chapman and Hall/CRC; 2002.
Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22.
Article MathSciNet Google Scholar
Team, RC, R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. http://www.R-project.org/ .
Talks JS, Lotery AJ, Ghanchi F, Sivaprasad S, Johnston RL, Patel N, et al. First-year visual acuity outcomes of providing aflibercept according to the VIEW study protocol for age-related macular degeneration. Ophthalmology. 2016;123:337–43.
Mehta H, Kim LN, Mathis T, Zalmay P, Ghanchi F, Amoaku WM, et al. Trends in real-world neovascular AMD treatment outcomes in the UK. Clin Ophthalmol. 2020;14:3331–42.
Ohji M, Okada AA, Sasaki K, Moon SC, Machewitz T, Takahashi K, et al. Relationship between retinal fluid and visual acuity in patients with exudative age-related macular degeneration treated with intravitreal aflibercept using a treat-and-extend regimen: subgroup and post-hoc analyses from the ALTAIR study. Graefes Arch Clin Exp Ophthalmol. 2021;259:3637–47.
Article CAS PubMed Central PubMed Google Scholar
Guymer RH, Markey CM, McAllister IL, Gillies MC, Hunyor AP, Arnold JJ, et al. Tolerating subretinal fluid in neovascular age-related macular degeneration treated with ranibizumab using a treat-and-extend regimen: FLUID Study 24-month results. Ophthalmology. 2019;126:723–34.
Kim KT, Lee H, Kim JY, Lee S, Chae JB, Kim DY. Long-term visual/anatomic outcome in patients with fovea-involving fibrovascular pigment epithelium detachment presenting choroidal neovascularization on optical coherence tomography angiography. J Clin Med. 2020;9:1863.
Haj Najeeb B, Deak G, Schmidt-Erfurth U, Gerendas BS. THE RAP STUDY, REPORT TWO: The regional distribution of macular neovascularization type 3, a novel insight into its etiology. Retina. 2020;40:2255–62.
Haj Najeeb B, Schmidt-Erfurth U. Do patients with unilateral macular neovascularization type 3 need AREDS supplements to slow the progression to advanced age-related macular degeneration? Eye (Lond). 2023;37:1751–3.
Fasler K, Moraes G, Wagner S, Kortuem KU, Chopra R, Faes L, et al. One- and two-year visual outcomes from the Moorfields age-related macular degeneration database: a retrospective cohort study and an open science resource. BMJ Open. 2019;9:e027441.
Download references
Acknowledgements
The research was funded by Boehringer Ingelheim and supported by the NIHR Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology and the NIHR Moorfields Clinical Research Facility. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Author information
Authors and affiliations.
National Institute of Health Research Moorfields Biomedical Research Centre, Moorfields Eye Hospital, London, UK
Shruti Chandra, Bishwanath Pal, Sridevi Thottarath, Raheeba Muhamed Pakeer, Swati Chandak, Andrea Montesel & Sobha Sivaprasad
Institute of Ophthalmology, University College, London, UK
Shruti Chandra, Sarega Gurudas, Victor Chong & Sobha Sivaprasad
James Paget University Hospitals NHS Foundation Trust, Norfolk, UK
Benjamin J. L. Burton
Frimley Health NHS Foundation Trust, Surrey, UK
Geeta Menon
The Royal Liverpool and Broadgreen University Hospitals NHS Foundation Trust, Liverpool, UK
Leeds Teaching Hospitals NHS Trust, Leeds, UK
Martin Mckibbin
South Tyneside and Sunderland NHS Foundation Trust, Sunderland, UK
Ajay Kotagiri
Newcastle Hospitals NHS Foundation Trust, Newcastle, UK
James Talks
King’s College Hospital NHS Foundation Trust, London, UK
Anna Grabowska
Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK
Faruque Ghanchi
Hull York Medical School and York, University of York and Scarborough Teaching Hospital NHS Foundation Trust, York, UK
Richard Gale
Boehringer Ingelheim, Binger Str. 173, 55216, Ingelheim am, Rhein, Germany
Andrea Giani & Taffeta Ching Ning Yamaguchi
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: ShC and SS; Data curation: ShC, ST, RMP, SC, and AM; Formal analysis: SG and SS; Funding acquisition: AGi, VC and SS; Investigation: ShC, SG and SS; Methodology: ShC, SG, and SS; Project administration: AGi. and SS; Resources: ShC, GM, BJB, IP, MM, ST, SC, RPM, AM, AK, JT, AGr, FG, RG, BP and SS; Supervision: AGi, VC and SS; Visualisation: SG and ShC; Writing – original draft: ShC, SG and SS; Writing - review & editing: AGi, VC and SS Review and approval of final manuscript: ShC, SG., AGi, VC, SS, GM, BJB, IP, MM, ST, RPM, SC, AM, AK, JT, AGr, CC, FG, RG, and BP.
Corresponding author
Correspondence to Sobha Sivaprasad .
Ethics declarations
Competing interests.
SS received consultancy fees from Bayer, Allergan, Novartis Pharma AG, Roche, Boehringer Ingelheim, Optos, Apellis, Oxurion, Oculis and Heidelberg Engineering. VC is an employee of Janssen R&D and previously of Boehringer Ingelheim. AGi is an employee of Boehringer Ingelheim. TCNY is an employee of Boehringer Ingelheim. BB is in the advisory board and received international conference attendance sponsored by Novartis and Bayer; GM has conducted consultancy-advisory boards for Novartis, Bayer and Allergan, received educational travel grants from Novartis, Bayer, Allergan; IP has received lecture fees from Allergan, Bayer, Heidelberg and Novartis, consultancy fees from Allergan, Alimera, Bayer and Novartis and travel fees from Allergan, Bayer and Novartis. FG has received honorarium for consultancy-advisory boards from Alimera, Allergan, Bayer, Novartis, Oxford BioElectronics, Roche; educational travel grants from Allergan, Bayer, Novartis. MM has received lecture and advisory board honoraria from Bayer and Novartis and an educational travel grant from Bayer. RG has conducted consultancy-advisory boards for Novartis, Bayer and Allergan, Alimera, Santen, received educational travel grants from Novartis, Bayer, Allergan, Heidelberg Engineering. JT is a consultant for Bayer and Novartis, received grant support from Bayer, Novartis and Heidelberg Engineering, and is involved in research for Allergan, Roche, Bayer, Novartis and Boehringer Ingelheim. AK received travel support from Novartis, Bayer, and Allergan, and speaker fees from Allergan and Bayer. Bishwanath Pal received travel support and received advisory boards honoraria from Novartis and Bayer. ShC, SG, ST, RMP, SC and AM have no financial disclosures. SS, FG, and ShC are members of the Eye editorial board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2023_2769_moesm1_esm.docx.
Table S1. Ocular and OCT characteristics associated with VA>=68 ETDRS letters and VA<54 ETDRS letters – Odds Ratios (95% CI) and P-values from univariate and multivariable analysis using Generalised E
41433_2023_2769_MOESM2_ESM.docx
Table S2. Ocular and OCT characteristics associated with moderate VA comparing moderate (VA 54-67) vs good VA (VA>=68) and moderate (VA 54-67) vs poor VA (VA<54) – univariate and multivariable analysi
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Chandra, S., Gurudas, S., Burton, B.J.L. et al. Associations of presenting visual acuity with morphological changes on OCT in neovascular age-related macular degeneration: PRECISE Study Report 2. Eye 38 , 757–765 (2024). https://doi.org/10.1038/s41433-023-02769-5
Download citation
Received : 08 April 2023
Revised : 04 September 2023
Accepted : 21 September 2023
Published : 18 October 2023
Issue Date : March 2024
DOI : https://doi.org/10.1038/s41433-023-02769-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Article Information
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Lopes MS , Zayit-Soudry S , Moshiri A , Bressler SB , Bressler NM. Understanding and Reporting Visual Acuity Measurements in Publications of Clinical Research. Arch Ophthalmol. 2011;129(9):1228–1229. doi:10.1001/archophthalmol.2011.248
Manage citations:
© 2024
- Permissions
Understanding and Reporting Visual Acuity Measurements in Publications of Clinical Research
Author Affiliations: Universidade Nove de Julho, São Paulo, Brazil (Dr Lopes); and Retina Division, Wilmer Eye Institute, Johns Hopkins University School of Medicine and Hospital, Baltimore, Maryland (Drs Zayit-Soudry, Moshiri, S. B. Bressler, and N. M. Bressler).
Visual acuity is an important measure for assessment of visual function. While there are many charts available to test visual acuity, 1 , 2 there is lack of consistency 3 in the methods of testing 4 and methods of reporting 5 visual acuity that may make comparisons difficult between visual outcomes among different published studies. In our opinion, most US ophthalmologists are familiar with the Snellen notation of visual acuity but have limited understanding of how other notations of visual acuity translate into Snellen notation. While some journals such as the American Journal of Ophthalmology provide charts to facilitate this translation, if the chart is not available at the time one is reading an article or listening to a presentation, understanding the level of visual acuity or changes in visual acuity may be limited.
The method of reporting visual acuity in clinical research in retina in 2008 was reviewed systematically to determine how frequently each method of acuity reporting was used among all retina articles published during the 2008 calendar year in 4 ophthalmology journals, including the American Journal of Ophthalmology , Archives of Ophthalmology , Ophthalmology , and Retina . Articles regarding case reports, intraocular tumors, and pediatric retina were excluded.
In addition, a survey to assess understanding of different visual acuity measurements was designed for 5 ophthalmology residents, 4 individuals obtaining advanced specialty training in retina following completion of an ophthalmology residency, and 5 faculty within a retina division at an academic medical center following approval of the study by the medical center's institutional review board and after an oral consent process approved by the institutional review board. The questionnaire was proctored to ensure that the participants provided the answers without reference to other materials. Each participant was asked to give the Snellen equivalent (within 1 line) of various visual acuity measurements that were in non-Snellen formats, including a fraction of 10 notation (eg, 5/10), decimal notation (eg, 0.2), logMAR (eg, 0.1), letter count on an Early Treatment Diabetic Retinopathy Study (ETDRS) chart (eg, letter score of 65), and a fraction based on readings at 6 m (eg, 6/60).
Among 356 articles identified in the 4 journals that were in the retina field, 206 reported visual acuity results. Methods used to report the visual acuity among these 206 articles included Snellen equivalent in 175 (85.0%), logMAR in 106 (51.5%), ETDRS letter scores in 67 (32.5%), decimal notation in 13 (6.3%), and metric fractional notation in 1 (0.5%). The 206 publications included 66 (32.0%) using Snellen notation only, 109 (52.9%) using a non-Snellen format and providing a Snellen equivalent, and 31 (15.0%) using non-Snellen notation alone. Among the 140 articles reporting acuity in non-Snellen systems, 83 of the 106 articles (78.3%) reporting logMAR and 54 of the 67 articles (80.6%) reporting an ETDRS letter score also provided a Snellen equivalent. Results were similar among the 172 publications specifying visual acuity as an outcome measure (data not shown).
Fourteen ophthalmologists among 14 volunteers completed the survey. No participants were able to interpret all 5 methods of visual acuity reporting correctly. Two participants (1 resident and 1 attending) demonstrated the ability to interpret 4 of the 5 methods assessed, while most other participants could not correctly interpret logMAR or letter score values within 2 lines of the Snellen equivalent. Ten participants (71.4%) were able to interpret visual acuity in the form of a fraction taken from an ETDRS chart read at 6 m (eg, 6/24). Eight participants (57.1%) correctly converted decimal notation into the appropriate Snellen equivalent. Seven participants (50.0%) correctly converted a fraction of 10 notation (eg, 4/10). Three participants (21.4%) were able to interpret logMAR acuity correctly, and none were able to interpret an ETDRS letter score correctly.
Uniformity in reporting visual acuity measurements in retina peer-reviewed published articles is currently lacking. Almost 1 in 6 articles did not provide Snellen equivalent values when visual acuity was an outcome, but our survey suggests that when an article provides visual acuity as an ETDRS letter score or logMAR, many ophthalmologists, regardless of their level of training, may not understand the Snellen equivalent level of visual acuity.
While the scope of this study is limited (only 14 participants were included in the survey, and all participants were from one academic institution) and the results do not necessarily mean that the individuals would not understand the results of the articles reviewed in their context or would not reference other materials to translate the results of visual acuity outcomes not provided as Snellen equivalents, the results bring into question whether ophthalmologists might understand rapid oral presentations at professional meetings that use letter scores or logMAR without Snellen equivalent information. Based on our findings, ophthalmic journals and organizers of oral presentations of ophthalmic studies might consider requiring approximate Snellen equivalents when visual acuity outcomes are provided using other notations, especially when letter scores or logMAR values are provided.
Correspondence: Dr N. M. Bressler, Wilmer Eye Institute, Maumenee 752, Johns Hopkins Hospital, 600 N Wolfe St, Baltimore, MD 21287-9227 ( [email protected] ).
Author Contributions: All authors had full access to all of the data in the study, and Dr N. M. Bressler takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure: None reported.
Funding/Support: This work was supported by unrestricted research gifts to the Retina Division, Wilmer Eye Institute, Johns Hopkins University, the Julia G. Levy, PhD, Professorship (Dr S. B. Bressler), the Research to Prevent Blindness Senior Scientific Investigator Award (Dr N. M. Bressler), and the James P. Gills Professorship (Dr N. M. Bressler).
Role of the Sponsor: Johns Hopkins University had no role in the design and conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Retinoblastoma treatment in a Brazilian population. Presentation and long-term results
Affiliations.
- 1 Division of Ophthalmology, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil.
- 2 Laboratory for Investigation in Ophthalmology (LIM-33), Faculdade de Medicina FMUSP, Universidade de São Paulo, São Paulo, Brazil.
- 3 ITACI (Treatment of Children with Cancer Institute) and Children's Institute, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil.
- PMID: 38243643
- PMCID: PMC10905530
- DOI: 10.1002/cam4.6683
Introduction: Retinoblastoma is a malignant tumor with a high cure potential when proper therapy is used. The purpose of this paper is to report the clinical features and outcomes of patients with retinoblastoma who were treated with a combination of local and systemic chemotherapy-based protocols.
Method: We retrospectively studied patients treated with systemic chemotherapy plus local treatment between 2003 and 2015 with a follow-up ≥2 years. We correlated clinical and pathological characteristics with decimal visual acuity (VA) and death.
Results: Among 119 patients, 60% had unilateral disease (UNI), and 52% were male. The median presentation age was 19.5 months, 10% had a positive family history, and the most frequent sign was leukocoria (68.8%). Advanced disease was more frequent in eyes with UNI (98.4%) than in eyes with bilateral retinoblastoma (BIL: 55.3%). Enucleation was performed in 97% of UNI eyes and in 55.8% of BIL eyes. The overall globe salvage was 26.6%, 44.25% of BIL eyes. Bilateral enucleation was required in 5%. High-risk pathologic features occurred in 50% and 37% of eyes enucleated without and with neoadjuvant chemotherapy, respectively. High-risk features were related to the presence of goniosynechiae in the pathologic specimen and were more frequent in children younger than 10 months or older than 40 months. Extraocular disease was present in 5% of patients, and the death rate related to metastasis of the tumor was 8%. The final VA was ≥ 0.7 in 72.8% and ≥0.1 in 91% of BIL patients.
Conclusions: Treatment of retinoblastoma with conservative systemic-based chemotherapy was associated with an excellent survival rate (92%). Albeit the low overall globe salvage rate, in BIL patients, approximately half the eyes were conserved, and a satisfactory functional visual result was achieved The evaluated protocol is an important treatment option, especially in developing countries.
Keywords: chemotherapy; eye enucleation; neoplasm staging; retinoblastoma; survival; treatment outcome; visual acuity.
© 2023 The Authors. Cancer Medicine published by John Wiley & Sons Ltd.
PubMed Disclaimer
Right (only) eye of a…
Right (only) eye of a bilateral retinoblastoma with final vision 0.5, 15 years…
Similar articles
- Retinoblastoma in Asia: Clinical Presentation and Treatment Outcomes in 2112 Patients from 33 Countries. Kaliki S, Vempuluru VS, Mohamed A, Al-Jadiry MF, Bowman R, Chawla B, Hamid SA, Ji X, Kapelushnik N, Kebudi R, Sthapit PR, Rojanaporn D, Sitorus RS, Yousef YA, Fabian ID; Global Retinoblastoma Study Group. Kaliki S, et al. Ophthalmology. 2024 Apr;131(4):468-477. doi: 10.1016/j.ophtha.2023.10.015. Epub 2023 Oct 13. Ophthalmology. 2024. PMID: 37839559
- Impact of Systemic Chemotherapy and Delayed Enucleation on Survival of Children with Advanced Intraocular Retinoblastoma. Zhao J, Feng ZX, Wei M, Liu G, Solarte CE, Li B, Wang Y, Zhang C, Gallie BL. Zhao J, et al. Ophthalmol Retina. 2020 Jun;4(6):630-639. doi: 10.1016/j.oret.2020.02.015. Epub 2020 Mar 4. Ophthalmol Retina. 2020. PMID: 32387053
- [Retinoblastoma update]. Aerts I, Lumbroso-Le Rouic L, Gauthier-Villars M, Brisse H, Doz F. Aerts I, et al. Arch Pediatr. 2016 Jan;23(1):112-6. doi: 10.1016/j.arcped.2015.09.025. Epub 2015 Dec 8. Arch Pediatr. 2016. PMID: 26679524 Review. French.
- Retinoblastoma. Ortiz MV, Dunkel IJ. Ortiz MV, et al. J Child Neurol. 2016 Feb;31(2):227-36. doi: 10.1177/0883073815587943. Epub 2015 May 28. J Child Neurol. 2016. PMID: 26023180 Review.
- Retinoblastoma in Turkey: results from a tertiary care center in Ankara. Gündüz K, Köse K, Kurt RA, Süren E, Taçyildiz N, Dinçaslan H, Ünal E, Erden E, Heper AO. Gündüz K, et al. J Pediatr Ophthalmol Strabismus. 2013 Sep-Oct;50(5):296-303. doi: 10.3928/01913913-20130730-02. Epub 2013 Aug 6. J Pediatr Ophthalmol Strabismus. 2013. PMID: 23937863
- Dimaras H, Corson TW, Cobrinik D, et al. Retinoblastoma. Nat Rev Dis Primers. 2015;1:15021. doi:10.1038/nrdp.2015.21 - DOI - PMC - PubMed
- Stacey AW, Bowman R, Foster A, et al. Incidence of retinoblastoma has increased: results from 40 European countries. Ophthalmology. 2021;128(9):1369‐1371. doi:10.1016/j.ophtha.2021.01.024 - DOI - PubMed
- Barbosa AC, de Magalhães‐Barbosa MC, Moreira JPL, Colombini GNUI, Prata‐Barbosa A. Incidence of retinoblastoma in children and adolescents in Brazil: a population‐based study. Front Pediatr. 2022;10:1048792. doi:10.3389/fped.2022.1048792 - DOI - PMC - PubMed
- Kaliki S, Patel A, Iram S, Ramappa G, Mohamed A, Palkonda VAR. RETINOBLASTOMA IN INDIA: clinical presentation and outcome in 1,457 patients (2,074 eyes). Retina. 2019;39(2):379‐391. doi:10.1097/IAE.0000000000001962 - DOI - PubMed
- Chawla B, Hasan F, Azad R, et al. Clinical presentation and survival of retinoblastoma in Indian children. Br J Ophthalmol. 2016;100(2):172‐178. doi:10.1136/bjophthalmol-2015-306672 - DOI - PubMed
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Europe PubMed Central
- PubMed Central
- Genetic Alliance

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Ophthalmol
- v.13(12); 2020
Frequency of presenting visual acuity and visual impairment in Chinese college students
Co-first authors: Jia-Min Cai and Ye Ye
To obtain the baseline data on presenting visual acuity (PVA) and evaluate the prevalence and associated factors for visual impairment based on PVA in 9070 Chinese college students.
The freshmen at a university in southern China, including 6527 undergraduate students and 2543 graduate students, were investigated for some socio-demographic characteristics and underwent routine medical examination, including measuring PVA, height, and weight. Visual impairment was defined according to the new World Health Organization criteria for blindness and visual impairment.
In 9070 college students, the mean PVA in the better eye was 0.094±0.163 logMAR. The prevalence of visual impairment based on PVA was 2.7%. Only 38.3% college students had normal visual acuity [PVA equal to 0 logMAR (20/20) in both eyes]. There were 69.8% of students wearing spectacles. Logistic regression showed that home region (non-Guangdong provinces, P <0.0001, OR=1.70) was risk factor for visual impairment while BMI ( P =0.001, OR=0.92) was protective factor from visual impairment. Ethnicity (Han Chinese, P <0.0001, OR=3.17) was risk factor for wearing spectacles while age ( P =0.01, OR=0.90) was protective factor from wearing spectacles.
This study provides the baseline data on PVA and the prevalence of visual impairment in Chinese college students. Our analyses reveal that BMI and home region are associated factors for visual impairment based on PVA, while age and ethnicity are associated factors for wearing spectacles.
INTRODUCTION
The eye is an important sensory organ of the human body, and more than 80% of the information entering the brain is gained by visual system [1] . Visual impairment is a serious global public health problem. According to the latest estimates on distance vision by World Health Organization (WHO), 188 million people had mild visual impairment, 217 million people had moderate to severe visual impairment, and 36 million people were blind. More than 80% of visual impairment can be prevented or cured. Uncorrected refractive error is the main cause of moderate and severe visual impairment [2] . In 2003, WHO proposed the use of presenting visual acuity (PVA) for estimating visual impairment and blindness [3] . PVA is defined as the uncorrected visual acuity of those who do not wear corrective spectacles, or the corrected visual acuity of those who wear spectacles in their daily life. With the introduction of PVA by WHO and the implementation of new standards for blindness and visual impairment in various countries, there have been several studies to evaluate the prevalence of visual impairment in various populations using PVA in recent years [4] – [7] .
The VISION 2020 Global Initiative emphasizes the priority of prevention and treatment of refractive error, and recommends all countries to collect data on the prevalence of visual impairment and its associated factors in order to provide scientific basis for further improvement of eye health [8] . However, only a few surveys on visual acuity have been conducted in Chinese college students in recent years. Moreover, the participants in most studies were examined for uncorrected visual acuity or best corrected visual acuity instead of PVA [9] – [11] , which did not well represent the visual quality of students' daily life. Surveys on PVA can indirectly represent the screening status of visual impairment in a region, the intensity of efforts to popularize the knowledge and acceptance of wearing spectacles, and the level of medical services of ophthalmology. In the present study, we investigated the status of PVA and evaluated the prevalence and associated factors for visual impairment based on PVA in 9070 Chinese first-year college students, hoping to provide the baseline data on PVA and new reference data for prevention and control of visual impairment as a real-world study.
The study was conducted in Guangdong Province, a coastal province in south China on the north shore of South China Sea. According to the data from the National Bureau of Statistics of China, Guangdong is the 4 th largest sub-national economy in the world with a GDP size of 1.47 trillion US dollars in 2018. It has also developed rapidly in terms of medical treatment. Therefore, the Guangdong study was motivated by interest in obtaining data on PVA and factors associated with visual impairment in a large urban setting for comparison with that obtained from surveys in other region.
SUBJECTS AND METHODS
Ethical approval.
This study followed the tenets of the Declaration of Helsinki and was approved by the Ethical Committee of Shenzhen Eye Hospital, China. The data used in this study were retrieved from electronic medical records of the study participants, and informed consent was waived.
This is a cross-sectional study on first-year college students admitted in fall 2018 at a university in southern China, who participated in the admission physical examination, including undergraduate students and graduate students. Taking into account the age gap between undergraduate and graduate students, the difference in their education level and understanding of eye care, we defined undergraduates as group I and graduates as group II for the comparisons in the following study. The student health information was de-identified by removing the identifiable individual information such as name and identity number.
Physical Examination
Physical examination was performed at the university hospital for all the freshmen. Demographic information including gender, age, ethnicity, home region, and clinical information including PVA, height and weight, were collected. Students who didn't wear spectacles were examined for uncorrected visual acuity, and those who wore spectacles were examined for corrected visual acuity and inquired for their eyeglass prescriptions. The visual acuity examination was strictly performed in accordance with the standard operation guidelines [12] . Under the standard illumination conditions, the E-type standard logarithmic visual chart light box was used at 5 m of distance. Visual acuity was recorded at a decimal scale, and then converted to the logarithm of MAR (logMAR) for data analysis. According to the new WHO classification for blindness and visual impairment [3] , [13] , PVA in the better eye was categorized into 4 groups: 1) mild or no visual impairment: PVA≤0.5 logMAR (20/63); 2) moderate visual impairment: 0.5 logMAR (20/63)<PVA≤1.0 logMAR (20/200); 3) severe visual impairment: 1.0 logMAR (20/200)<PVA≤1.3 logMAR (20/400); and 4) blindness: PVA>1.3 logMAR (20/400). The better eye was defined as the eye with superior vision on the visual acuity examination. Moderate and severe visual impairment were defined as low vision. Visual impairment included low vision and blindness. To facilitate the comparison of our results with those of other studies, the prevalence of visual impairment was calculated according to published evaluation criterion for visual impairment (PVA≥0.3 logMAR (20/40) in the better eye) [14] – [16] . Undercorrection was defined as abnormal corrected visual acuity in the better eye of students wearing their own spectacles [PVA equal to 0 logMAR (20/20)]. Height and body weight with bare feet and light clothing were measured using standardized methods to nearest 0.1 cm or 0.1 kg. The body mass index (BMI) was calculated by dividing body weight (kg) by height squared (m 2 ).
Statistical Analysis
Statistical analysis was performed using the statistical software package (SPSS version 20.0, SPSS Inc., Chicago, IL, USA). Chi-square test or rank sum test was used to compare the PVA and wearing spectacles between undergraduate and graduate students. Logistic regression was used to evaluate the associated factors for visual impairment and wearing spectacles. Odds ratio (OR) and 95% confidence intervals (CIs) were calculated for each independent variables. P values of less than 0.05 were considered to indicate statistical significance.
Background Characteristics of the Study Subjects
A total of 9070 first-year college students were investigated, including 6527 undergraduate students in group I and 2543 graduate students in group II. All students included 4792 (52.83%) males and 4278 (47.17%) females. The average age was 20.01±2.69y, ranging from 15 to 42y. There were 8843 (97.50%) students who were Han Chinese and 6009 (66.25%) students lived in Guangdong Province and the rest were from other provinces in China. The average BMI was 20.79±3.15 kg/m 2 , ranging from 13.44 to 46.28 kg/m 2 ( Table 1 ).
| Parameters | Overall students | Group I | Group II | ||||||
| All ( ) | Visual impairment, (%) | Wearing spectacles, (%) | All ( ) | Visual impairment, (%) | Wearing spectacles, (%) | All ( ) | Visual impairment, (%) | Wearing spectacles, (%) | |
| No. of students | 9070 | 249 (2.7) | 6336 (69.8) | 6527 | 174 (2.7) | 4557 (69.8) | 2543 | 75 (2.9) | 1778 (69.9) |
| Age (y) | 20.01±2.69 | 18.58±0.68 | 25.68±2.46 | ||||||
| Range | 15-42 | 15 to 23 | 18 to 42 | ||||||
| Gender | |||||||||
| Male | 4792 | 123 (2.5) | 3308 (69.0) | 3385 | 83 (2.5) | 2327 (68.7) | 1407 | 40 (2.8) | 980 (69.7) |
| Female | 4278 | 126 (2.9) | 3028 (70.7) | 3142 | 91 (2.9) | 2230 (71.0) | 1136 | 35 (3.1) | 798 (70.3) |
| Ethnicity | |||||||||
| Han | 8843 | 243 (2.7) | 6232 (70.4) | 6336 | 169 (2.7) | 4477 (70.7) | 2507 | 74 (3.0) | 1754 (70.0) |
| Non-Han | 227 | 6 (2.6) | 104 (45.8) | 191 | 5 (2.6) | 80 (41. 9) | 36 | 1 (2.8) | 24 (66.7) |
| BMI (kg/m ) | 20.79±3.15 | 20.60±3.15 | 21.31±3.07 | ||||||
| Range | 13.44-46.28 | 13.44-45.55 | 14.24-46.28 | ||||||
| Home region | |||||||||
| Guangdong Province | 6009 | 139 (2.3) | 4248 (70.6) | 5033 | 122 (2.4) | 3550 (70.5) | 976 | 17 (1.7) | 698 (71.5) |
| Non-Guangdong provinces | 3061 | 110 (3.5) | 2088 (68.2) | 1494 | 52 (3.5) | 1007 (67.4) | 1567 | 58 (3.7) | 1080 (68.9) |
BMI: Body mass index.
The group I included 3385 (51.86%) males and 3142 (48.14%) females. The average age was 18.58±0.68y, ranging from 15 to 23y. There were 6336 (97.07%) undergraduate students who were Han Chinese and 5033 (77.11%) undergraduate students lived in Guangdong Province and the rest were from other provinces in China. The average BMI was 20.60±3.15 kg/m 2 , ranging from 13.44 to 45.55 kg/m 2 . The group II included 1407 (55.33%) males and 1136 (44.67%) females. The average age was 25.68±2.46y, ranging from 18 to 42y. There were 2507 (98.58%) graduate students who were Han Chinese and 976 (38.38%) graduate students lived in Guangdong Province and the rest were from other provinces in China. The average BMI was 21.31±3.07 kg/m 2 , ranging from 14.24 to 46.28 kg/m 2 ( Table 1 ).
PVA, Prevalence of Visual Impairment and Wearing Spectacles
In overall college students, the mean PVA in the better eye was 0.094±0.163 ( Figure 1A ). There were 38.3% ( n =3472) students who had PVA equal to 0 logMAR (20/20) in both eyes. There were 97.3% ( n =8821) students without visual impairment, and 2.7% ( n =249) students had visual impairment, including 2.6% ( n =240) students with moderate visual impairment, 0.09% ( n =8) students with severe visual impairment, and 0.01% blind student ( n =1). A total of 69.8% ( n =6335) students wore spectacles, and of them, 35.5% ( n =2248) students were undercorrected ( Table 2 ).

A: Overall students ( n =9070): the mean PVA in the better eye was 0.094±0.163; B: Undergraduate students ( n =6527): the mean PVA in the better eye was 0.089±0.159; C: Graduate students ( n =2543): the mean PVA in the better eye was 0.107±0.173.
| Factor | Overall students | Group I | Group II | |
| PVA≤0 logMAR (20/20) both eyes | 38.3 (3472) | 39.7 (2592) | 34.6 (880) | <0.0001 |
| PVA≤0 logMAR (20/20) one eye only | 23.0 (2090) | 23.2 (1512) | 22.7 (578) | 0.66 |
| PVA≤0.5 logMAR (20/63) (mild or no visual impairment) | 97.3 (8821) | 97.3 (6353) | 97.1 (2468) | 0.46 |
| Low vison and blindness | 2.7 (249) | 2.7 (174) | 2.9 (75) | 0.46 |
| 0.5 logMAR (20/63)<PVA≤1.0 logMAR (20/200) (moderate visual impairment) | 2.6 (240) | 2.6 (169) | 2.8 (71) | 0.34 |
| 1.0 logMAR (20/200)<PVA≤1.3 logMAR (20/400) (severe visual impairment) | 0.09 (8) | 0.06 (4) | 0.16 (4) | 0.21 |
| PVA>1.3 logMAR (20/400) (blindness) | 0.01 (1) | 0.015 (1) | 0 | 0.40 |
| PVA≥0.3 logMAR (20/40) | 12.7 (1151) | 11.8 (769) | 15.0 (382) | <0.0001 |
| Wearing spectacles | 69.8 (6335) | 69.8 (4557) | 69.9 (1778) | 0.93 |
| Undercorrection | 35.5 (2248) | 34.2 (1557) | 38.9 (691) | <0.0001 |
PVA: Presenting visual acuity. a P <0.05.
In group I, the mean PVA in the better eye was 0.089±0.159 ( Figure 1B ). There were 39.7% ( n =2592) students who had PVA equal to 0 logMAR (20/20) in both eyes and it was significantly higher in males (42.7%) than females (36.4%; P <0.0001), while 23.2% ( n =1512) students had PVA equal to 0 logMAR (20/20) in one eye only with no significant difference between male and female students ( P =0.85). There were 97.3% ( n =6353) students without visual impairment, and 2.7% ( n =174) students had visual impairment, including 2.6% ( n =169) students with moderate visual impairment, 0.06% ( n =4) students with severe visual impairment, and 1 blind student (0.015%). A total of 69.8% ( n =4557) students wore spectacles, and of them, 34.2% ( n =1557) students were undercorrected ( Table 2 ).
In group II, the mean PVA in the better eye was 0.107±0.173 ( Figure 1C ). There were 34.6% ( n =880) students had PVA equal to 0 logMAR (20/20) in both eyes and it was significantly higher in males (36.6%) than females (32.1%; P <0.0001), while 22.7% ( n =578) students had PVA equal to 0 logMAR (20/20) in one eye only and there was no remarkable gender difference ( P =0.22). There were 97.1% ( n =2468) students without visual impairment, and 2.9% ( n =75) students had visual impairment, including 2.8% ( n =71) students with moderate visual impairment, 0.16% ( n =4) students with severe visual impairment, and no blind students. A total of 1778 (69.9%) students wore spectacles, and of them, 38.9% ( n =691) students were undercorrected ( Table 2 ).
The mean PVA in the better eye of group I was significantly better than that of group II (0.089 vs 0.107; P <0.0001). The rate of PVA equal to 0 logMAR (20/20) in both eyes in group I was higher than that in group II (39.7% vs 34.6%; P <0.0001). The prevalence of visual impairment (PVA≥0.3 logMAR in the better eye) in group I was significantly lower than that in group II (11.8% vs 15.0%; P <0.0001). The rate of undercorrection in group I was significantly lower than that in group II (34.2% vs 38.9%; P <0.0001). There was no significant difference in the rate of PVA equal to 0 logMAR (20/20) in one eye only, mild or no visual impairment, low vision and blindness, wearing spectacles and between group I and group II (all P >0.05; Table 2 ).
Associated Factors for Visual Impairment and Wearing Spectacles
In overall students, multivariate Logistic regression showed that home region (non-Guangdong provinces, P <0.0001, OR=1.70, 95%CI: 1.28-2.26) was risk factor for visual impairment while BMI ( P =0.001, OR=0.92, 95%CI: 0.88-0.97) was protective factor from visual impairment. Ethnicity (Han Chinese, P <0.0001, OR=3.17, 95%CI: 2.04-3.53) was risk factor for wearing spectacles while age ( P =0.01, OR=0.90, 95%CI: 0.93-0.99) was protective factor from wearing spectacles ( Table 3 ).
| Parameters | Overall students | Group I | Group II | |||||||||
| Visual impairment | Wearing spectacles | Visual impairment | Wearing spectacles | Visual impairment | Wearing spectacles | |||||||
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |||||||
| Age (y) | 0.96 (0.87-1.07) | 0.50 | 0.90 (0.93-0.99) | 0.01 | 1.05 (0.91-1.20) | 0.51 | 0.90 (0.83-0.97) | 0.01 | 0.97 (0.82-1.07) | 0.33 | 0.97 (0.94-1.01) | 0.10 |
| Gender | ||||||||||||
| M | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| F | 1.02 (0.79-1.31) | 0.89 | 1.09 (0.99-1.20) | 0.05 | 1.09 (0.90-1.32) | 0.37 | 1.11 (0.99-1.24) | 0.05 | 0.89 (0.55-1.46) | 0.65 | 1.03 (0.86-1.24) | 0.75 |
| Ethnicity | ||||||||||||
| No-Han Chinese | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| Han Chinese | 1.35 (0.58-3.15) | 0.48 | 3.17 (2.04-3.53) | <0.0001 | 1.19 (0.66-2.13) | 0.56 | 3.17 (2.31-4.33) | <0.0001 | 1.21 (1.63-8.99) | 0.85 | 1.13 (0.56-2.27) | 0.74 |
| BMI (kg/m ) | 0.92 (0.88-0.97) | 0.001 | 1.00 (0.99-1.02) | 0.99 | 0.94 (0.91-0.97) | <0.0001 | 0.99 (0.98-1.02) | 0.87 | 0.97 (1.86-1.02) | 0.14 | 0.99 (0.97-1.03) | 1.00 |
| Home region | ||||||||||||
| Guangdong Province | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) | ||||||
| Non-Guangdong Provinces | 1.70 (1.28-2.26) | <0.0001 | 0.94 (0.84-1.04) | 0.22 | 1.25 (1.00-1.56) | 0.04 | 0.99 (0.87-1.14) | 0.92 | 2.13 (1.23-3.71) | 0.007 | 0.86 (0.72-1.03) | 0.10 |
| Graduation | 1.05 (0.91-1.20) | 0.51 | 0.90 (0.83-0.97) | 0.01 | 0.97 (0.82-1.07) | 0.33 | 0.97 (0.94-1.01) | 0.10 | ||||
| Undergraduate | 1.00 (ref.) | 1.00 (ref.) | ||||||||||
| Graduate | 1.13 (0.62-2.07) | 0.70 | 0.96 (0.93-1.99) | 0.27 | ||||||||
OR: Odds ratio; CI: Confidence interval; ref.: Reference; BMI: Body mass index. a P <0.05.
In group I, multivariate Logistic regression showed that home region (non-Guangdong provinces, P =0.04, OR=1.25, 95%CI: 1.00-1.56) was risk factor for visual impairment while BMI ( P <0.0001, OR=0.94, 95%CI: 0.91-0.97) was protective factor from visual impairment. Ethnicity (Han Chinese, P <0.0001, OR=3.17, 95%CI: 2.31-4.33) was risk factor for wearing spectacles while age ( P =0.01, OR=0.90, 95%CI: 0.83-0.97) was protective factor from wearing spectacles ( Table 3 ).
In group II, multivariate Logistic regression showed that home region (non-Guangdong provinces, P =0.007, OR=2.13, 95%CI: 1.23-3.71) was risk factor for visual impairment, while no factors were associated with wearing spectacles ( P >0.05; Table 3 ).
For most of the previous studies focused on children or older adults, our findings provided supplemental information for the baseline data on PVA and the prevalence of visual impairment in Chinese college students. In this study, of the overall students examined, although 97.3% students didn't have visual impairment, only 3472 out of 9070 (38.3%) had normal visual acuity [PVA equal to 0 logMAR (20/20) in both eyes], while fewer students had normal visual acuity in the group II (34.6%) compared with group I (39.7%). The mean PVA in the better eye of group I was lower than that of group II ( Figure 1 ), suggesting that undergraduate students had better PVA than graduate students. PVA is an important factor that affects the quality of vision, and the degree of vision diminution causes a considerable impact on the quality of life. Although visual impairment was defined as PVA worse than 0.5 logMAR (20/63) in the better eye by WHO, clinical experience points to the fact that students with mild or no visual impairment can experience symptomatic difficulties in reading at distance. Therefore, it should be considered to offer suitable diagnostic and therapeutic services or appropriate eye care services for college students to obtain good PVA.
In this study, the undercorrection rate in both group I and group II exceeded 30% ( Table 2 ), which was higher than that in two previous studies of children wearing spectacles in China (26.1% [17] and 30% [18] ). The remarkable undercorrection rate may be due to the failure to update eyeglass prescriptions in time or the poor quality of spectacles. Not only that, another study in China reported that 36.07% college students wore spectacles only when they needed in the specific circumstance [19] . Improper habits of wearing spectacles would lead to worse PVA of students; thus their daily activities can be affected to some extent. It has been reported that people with undercorrection were more likely to encounter difficulties in their daily life activities [20] , and undercorrection might aggravate visual impairment [21] – [22] . Therefore, everyone with ametropia should be checked regularly so that appropriate spectacles can be fitted in time for better PVA.
Based on the WHO standards, most of the first-year undergraduate and graduate students in this study had mild or no visual impairment in their daily life, with only 2.7% and 3.0% visual impairment, respectively, which was a little lower than the prevalence of visual impairment in first-year undergraduate students at Tianjin Medical University from north China (3.2%) [19] . In previous studies among old adults (usually 40y and older), the rates of visual impairment were higher than our results, like the survey conducted in nine provinces in China (10.71% [23] ) and the Iranian survey (6.43% [4] ). In this study, according to the visual impairment defined as PVA ≥ 0.3 logMAR (20/40) in the better eye, the prevalence of visual impairment in group I was lower than that in group II (11.8% vs 15.0%; Table 2 ), which were higher than other studies of Chinese children in different regions (7.70% [14] and 10.3% [15] ). These differences are probably due to the differences in age and region. In developed countries, visual acuity>0.3 logMAR (20/40) is the most common requirement for obtaining a driver's license, and studies have shown that the degree of visual impairment is related to the increase of social isolation [24] – [25] . The visual impairment information of young adults that was not much involved in previous studies was provided in the present study. Collectively, these findings suggest that the quality of daily life of Chinese undergraduate and graduate students should be concerned.
Generally, it was observed in previous studies among older adults (usually 40y and older) in China that gender and age were risk factors for visual impairment [9] , [26] – [27] , while the Beijing Eye Study reported that visual impairment was not associated with gender [28] . In this study, Logistic regression analysis showed that gender and age were not associated with the prevalence of visual impairment in first-year college students ( Table 3 ). For most of the previous studies focused on adults aged 40y and older, further studies are needed to determine whether gender and age are associated factors for visual impairment in college students. Uniquely, our study showed that lower BMI was a risk factor for visual impairment in all students and group I ( Table 3 ), suggesting that poor diet might affect visual acuity. Studies have shown that the lack of certain vitamins and trace elements such as zinc, copper and selenium could affect normal development of the eye [29] . Previous studies have reported that high BMI in older adults was associated with prevalence of visual impairment [30] – [31] , which was not consistent with our result probably due to different populations.
Our results suggest that home region in non-Guangdong provinces was a risk factor for visual impairment ( Table 3 ) and no studies have been reported that. Regardless of undergraduate or graduate students, the prevalence of visual impairment in students outside Guangdong Province was higher than that in students from Guangdong Province. This geographical difference may be related to local education, eye care promotion and the ability to provide services. Apparently, large disparities in healthcare exist across geographical localities and socioeconomic groups. Due to the poor economic situation in some regions, the authorities provide fewer and lower quality services. Guangdong Province is responsible for 11 percent of the China' $14.4 trillion GDP and its economy is larger than that of any other province in the nation according to the data from the National Bureau of Statistics of China. The lower rate of visual impairment among students in Guangdong Province in our study may be related to the better economy and eye health care in Guangdong Province. However, given the lack of more direct information, further studies and evidences on the regional differences in visual impairment especially among the young adults are needed. Understanding the prevalence and associated factors related to visual impairment will be conducive to the prevention and control of visual impairment.
In this study, younger age and Han ethnicity were associated with wearing spectacles in all students and group I ( Table 3 ), indicating that the prevalence of refractive error in younger students and Han Chinese might be higher. But a 5-year longitudinal study in Taiwan University and a 3-year longitudinal studies in Norway reported that older students were more myopic than younger ones [32] – [33] . Studies have shown that the prevalence of myopia increases with age before adulthood [34] . We supposed that these longitudinal studies were better in showing this progression pattern than the cross-sectional design of our study which might cause the result different. In addition, our results are consistent with previous studies in which the rate of myopia in non-Han Chinese was lower than that in Han Chinese [35] – [37] . It is unclear if this difference is due to genetic difference or different lifestyles between these ethnic groups. It has been reported that non-Han Chinese may spend more time outdoors in childhood than Han Chinese [37] .
According to the data from the National Bureau of Statistics of China, there were 27.53 million undergraduate students and 2.63 million graduate students in 2017 in China. The data on the PVA and wearing spectacles in daily life of these college students are limited. Previous definition for visual impairment was based on best-corrected visual acuity, but there has been an increasing consensus that this is inappropriate because it may underestimate visual impairment caused by uncorrected refractive error [38] – [39] . However, surveys based on PVA can avoid the underestimation of the actual visual impairment, which not only allows us to know the true state of visually impaired patients in daily life, but also provides a more accurate estimate of prevalence. We investigated 9070 Chinese first-year college students, including 6527 undergraduate students and 2543 graduate students, for their PVA and factors associated with visual impairment. As a real-world study, the data from this study showed the visual status for undergraduate and graduate students at a university in southern China in their daily life, and to some extent reflected their visual quality. To the best of our knowledge, this is the largest study of Chinese college students on PVA and visual impairment based on PVA to date. In addition, our study showed that lower BMI and home region in non-Guangdong province were associated with visual impairment in undergraduate students, which were not investigated in other relevant studies of college students. Our findings provides further epidemiologic data on the PVA in college students population in south China which can be used by health policy planners, low vision rehabilitation providers, and eye care professionals to plan for the future eye care needs of college students.
However, there were several limitations in this study. First, we did not acquire more socio-demographic characteristics that might be associated with visual impairment, such as family income and visual impairment in their parents. Second, we did not perform accurate refractive examinations to diagnose refractive errors, which may lead to an underestimation of the actual prevalence of refractive errors in this study. Third, the eyeglass prescriptions provided by the students were not verified so that the myopia rates at all levels might have been biased. Finally, we did not further study the causes of visual impairment. If the main causes of visual impairment in college students can be clarified, it will be more helpful for the prevention and control of visual impairment in young people. Future studies may focus on PVA in other populations and explore the causes of visual impairment in college students and the causes behind the excess in prevalence of visual impairment among students with lower BMI and students in Guangdong province. Large-scale study and wide age range will contribute to more accurate PVA in the population.
In summary, we provided the baseline data on PVA in 9070 Chinese college students. More than 60% of all students didn't have normal visual acuity in both eyes, while no more than 3% of them had visual impairment based on PVA in the better eye according to the new criteria of WHO. Our analyses suggest that lower BMI and home region in non-Guangdong provinces are risk factors for visual impairment, while younger age and Han ethnicity are risk factors for wearing spectacles. These findings can help public and policy makers aware and concern about the vision of college students in their daily life. Effective and systematic comprehensive prevention and treatment measures should be taken to further reduce the prevalence of visual impairment and improve the rate of appropriate correction to achieve better PVA, thus improving the quality of visual function of college students.
Acknowledgments
Authors' contributions: Conceptualization (Zhao J); Data curation, formal analysis (Cai JM, Ye Y, Zhang T, Zheng JH); Methodology (Zhao J, Cai JM, Ye Y, Liang P); Investigation (Cai JM, Ye Y, Wang J); Funding acquisition, supervision, validation (Zhao J); Resources (Liang R); Writing–original draft (Cai JM, Ye Y); Writing–review & editing (Zhao J).
Foundations: Supported by Science, Technology and Innovation Commission of Shenzhen Municipality (No.GJHZ20180420180937076; No.JCYJ20180228164400218); Sanming Project of Medicine in Shenzhen Grant (No.SZSM201812090).
Conflicts of Interest: Cai JM, None; Ye Y, None; Liang P, None; Zhang T, None; Zheng JH, None; Wang J, None; Zhao J, None.

IMAGES
VIDEO
COMMENTS
The current categories of visual impairment in ICD are shown in Table 1, and their use to classify different levels of visual impairment is shown in Table 2.We identified three major issues in this ICD classification that need to be addressed: use of best-corrected or presenting visual acuity, cut-off level to define blindness, and appropriateness of the term 'low vision'.
Visual acuity is the clarity or sharpness of vision. Visual acuity assessment is a crucial aspect of ophthalmic examination. The loss of visual acuity can significantly impact an individual's quality of life. Vision loss may be due to ocular disease, systemic disease, or diseases of other organ systems, including the central nervous system.
A visual acuity score results from a visual acuity test performed by an optometrist or ophthalmologist during an eye exam. Visual acuity scores are usually written as a fraction. These test results describe your ability to see an object 20 feet away compared to a person with normal vision. For example, 20/20 vision means seeing an object ...
Visual acuity estimates the level of finest detail that can be detected or identified, and remains a very important measure of visual function in both clinical evaluation and research. ... 6/18, severe visual impairment is acuity worse than 6/60, and profound visual impairment (or blindness) is defined with presenting visual acuity worse than 3 ...
It is the spatial resolving capacity of the visual system and measures the sharpness of vision. Visual acuity is usually measured using a Snellen's chart at a distance of 6 metres or 20 feet. Several other charts are available for specialised conditions. Normal vision is denoted as a visual acuity of 6/6 or 20/20.
Visual acuity measures how sharp your vision is at a distance. It is usually tested by reading an eye chart. How is visual acuity tested? The Snellen eye chart, with its familiar rows of letters in decreasing sizes, is the most common visual acuity test. While standing or sitting 20 feet from the chart, you are instructed to read each row until ...
Visual acuity (VA) commonly refers to the clarity of vision, ... Variables such as pupil size, background adaptation luminance, duration of presentation, type of optotype used, interaction effects from adjacent visual contours (or "crowding") can all affect visual acuity measurement.
Assessment of presenting visual acuity demonstrated that 28.7% of patients had moderate-severe visual impairment (MSVI) in both eyes at presentation while 10.3% were bilaterally blind. Increasing ...
Globally, at least 2.2 billion people have a near or distance vision impairment. In at least 1 billion of these, vision impairment could have been prevented or is yet to be addressed. The leading causes of vision impairment and blindness at a global level are refractive errors and cataracts. It is estimated that globally only 36% of people with ...
10°, in the better eye with the available correction. "Severe visual impairment" is defined as a presenting visual acuity of between less than 6/60 and 3/60 and "moderate visual impairment" as a presenting visual acuity of less than 6/18 to 6/60. In this document "visual impairment" includes both severe and moderate visual impairment.
Near vision tests are usually done at 16 inches or 40 cm. The most common near visual acuity tests are: Reduced Snellen - A miniature Snellen test. "Perfect" vision is the ability to read the 20/20 line. Jaeger - Paragraphs of text increasing in size. "Perfect" vision is the ability to read the J-1 line.
Presenting visual acuity is not refracted visual acuity as this is not routine practice in the UK [33, 39]. The VA categories are pragmatically defined as the ICD-10 or WHO criteria of visual ...
A visual acuity test is an eye examination that measures your eyes' ability to read or see small details. In simple terms, a visual acuity test determines how sharp and clear your vision is. The Snellen chart is the most common eye chart for the test. You can also use the jaeger and tumbling charts to perform visual acuity testing.
Blindness - presenting visual acuity worse than 3/60; Near vision impairment: Presenting near visual acuity worse than N6 or M.08 with existing correction. A person's experience of vision impairment varies depending upon many different factors. This includes for example, the availability of prevention and treatment interventions, access to ...
A visual acuity test is only one part of a comprehensive ophthalmologic examination. The goal of the visual acuity test is to determine clarity or sharpness of vision. Visual acuity testing examines a patient's ability to distinguish different optotypes (recognizable letters or symbols) at a standard distance. This process requires many functioning pathways, including light reaching the retina ...
Visual acuity is an important measure for assessment of visual function. While there are many charts available to test visual acuity, 1,2 there is lack of consistency 3 in the methods of testing 4 and methods of reporting 5 visual acuity that may make comparisons difficult between visual outcomes among different published studies. In our opinion, most US ophthalmologists are familiar with the ...
This includes 42 million persons with blindness defined as presenting visual acuity less than 3/60 in the better eye, and 217 million persons with less severe visual impairment level defined as presenting visual acuity less than 6/18 to 3/60 in the better eye, 14% and 75% higher, respectively, than the WHO estimates based on best-corrected ...
Download Table | Presenting visual acuity and best corrected visual acuity (better eye) from publication: Prevalence of visual impairment, cataract surgery and awareness of cataract and glaucoma ...
Visual acuity is tested using a standardized chart during a routine eye exam, but may also be performed in a doctor's office or school setting, during a vision screening. What is the Snellen visual acuity test? The Snellen test is a visual acuity chart that consists of 11 rows of capital letters, with one large letter at the top of the chart.
Aim: To obtain the baseline data on presenting visual acuity (PVA) and evaluate the prevalence and associated factors for visual impairment based on PVA in 9070 Chinese college students. Methods: The freshmen at a university in southern China, including 6527 undergraduate students and 2543 graduate students, were investigated for some socio-demographic characteristics and underwent routine ...
Presentation and long-term results Cancer Med. 2024 Feb;13 ... We correlated clinical and pathological characteristics with decimal visual acuity (VA) and death. Results: Among 119 patients, 60% had unilateral disease (UNI), and 52% were male. The median presentation age was 19.5 months, 10% had a positive family history, and the most frequent ...
Digital health company Luminopia Inc. announced real-world data from the Patients Using Prescription Luminopia Registry, which demonstrated the efficacy of its binocular, virtual reality-based ...
Keywords: presenting visual acuity, prevalence, visual impairment, China, college student. INTRODUCTION. The eye is an important sensory organ of the human body, and more than 80% of the information entering the brain is gained by visual system [1]. Visual impairment is a serious global public health problem. According to the latest estimates ...
• Normal or corrected to normal visual and hearing acuity, hand and eye coordination, and manual dexterity. • Full range of motion including the capacity to sit for long periods in the classroom. • The ability to assist patients in range of motion. • The ability to stand and walk for long periods of time in hospital or clinic settings.
Operator: Good morning, and welcome to the Acuity Brands Fiscal 2024 Third Quarter Earnings Call. At this time, all participants are in a listen-only mode. After the speakers' presentation, the ...
vision, defined as losing fewer than 15 letters of visual acuity at week 52 compared to baseline. Both aflibercept 2Q8 and aflibercept 2Q4 groups were shown to have efficacy that was clinically equivalent to the ranibizumab 0.5 mg Q4 group in year 1. Detailed results from the analysis of the VIEW1 and VIEW2 studies are shown in Table 4 and