
- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons

Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

8.1: Case Study: Genes and Inheritance
- Last updated
- Save as PDF
- Page ID 16760

- Suzanne Wakim & Mandeep Grewal
- Butte College
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Case Study: Cancer in the Family
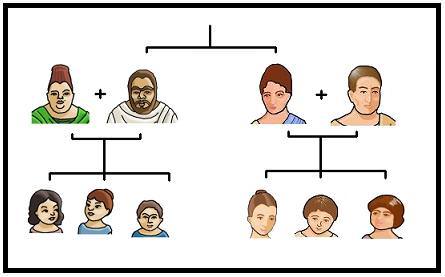
People tend to look similar to their biological parents, as illustrated by the family tree in Figure \(\PageIndex{1}\). But, you can also inherit traits from your parents that you can’t see. Rebecca becomes very aware of this fact when she visits her new doctor for a physical exam. Her doctor asks several questions about her family's medical history, including whether Rebecca has or had relatives with cancer. Rebecca tells her that her grandmother, aunt, and uncle, who have all passed away, all had cancer. They all had breast cancer, including her uncle, and her aunt additionally had ovarian cancer. Her doctor asks how old they were when they were diagnosed with cancer. Rebecca is not sure exactly, but she knows that her grandmother was fairly young at the time, probably in her forties.
Rebecca’s doctor explains that while the vast majority of cancers are not due to inherited factors, a cluster of cancers within a family may indicate that there are mutations in certain genes that increase the risk of getting certain types of cancer, particularly breast and ovarian cancer. Some signs that cancers may be due to these genetic factors are present in Rebecca’s family, such as cancer with an early age of onset (e.g. breast cancer before age 50), breast cancer in men, and breast cancer and ovarian cancer within the same person or family.
Based on her family medical history, Rebecca’s doctor recommends that she see a genetic counselor because these professionals can help determine whether the high incidence of cancers in her family could be due to inherited mutations in their genes. If so, they can test Rebecca to find out whether she has the particular variations of these genes that would increase her risk of getting cancer.
When Rebecca sees the genetic counselor, he asks how her grandmother, aunt, and uncle with cancer are related to her. She says that these relatives are all on her mother’s side — they are her mother’s mother and siblings. The genetic counselor records this information in the form of a specific type of family tree, called a pedigree, indicating which relatives had which type of cancer and how they are related to each other and to Rebecca. He also asks her ethnicity. Rebecca says that her family, on both sides, are Ashkenazi Jews, meaning Jews whose ancestors came from central and eastern Europe. “But what does that have to do with anything?” she asks. The counselor tells Rebecca that mutations in two tumor-suppressor genes called BRCA1 and BRCA2, located on chromosome 17 and 13, respectively, are particularly prevalent in people of Ashkenazi Jewish descent and greatly increase the risk of getting cancer. About 1 in 40 Ashkenazi Jewish people have one of these mutations, compared to about 1 in 800 in the general population. Her ethnicity, along with the types of cancer, age of onset, and the specific relationships between her family members who had cancer indicate to the counselor that she is a good candidate for genetic testing for the presence of these mutations.
Rebecca says that her 72-year-old mother never had cancer, and nor had many other relatives on that side of the family, so how could the cancers be genetic? The genetic counselor explains that the mutations in the BRCA1 and BRCA2 genes, although dominant, are not inherited by everyone in a family. Also, even people with mutations in these genes do not necessarily get cancer — the mutations simply increase their risk of getting cancer. For instance, 55 to 65% of women with a harmful mutation in the BRCA1 gene will get breast cancer before age 70, compared to 12% of women in the general population who will get breast cancer sometime over the course of their lives.
Rebecca is not sure she wants to know whether she has a higher risk of cancer. The genetic counselor understands her apprehension but explains that if she knows that she has harmful mutations in either of these genes, her doctor will screen her for cancer more often and at earlier ages. Therefore, any cancers she may develop are likely to be caught earlier when they are often much more treatable. Rebecca decides to go through with the testing, which involves taking a blood sample, and nervously waits for her results.
Chapter Overview: Genetics
At the end of this chapter, you will find out Rebecca ’s test results. By then, you will have learned how mutations in genes such as BRCA1 and BRCA2 can be passed down and cause disease. Especially, you will learn about:
- How Gregor Mendel discovered the laws of inheritance for certain types of traits.
- The science of heredity, known as genetics, and the relationship between genes and traits.
- Simple and more complex inheritance of some human traits.
- Genetic Disorders.
As you read this chapter, keep Rebecca’s situation in mind and think about the following questions:
- What do the BRCA1 and BRCA2 genes normally do? How can they cause cancer?
- Are BRCA1 and BRCA2 considered linked genes? And are they on autosomes or sex chromosomes?
- After learning more about pedigrees, draw the pedigree for cancer in Rebecca’s family. Use the pedigree to help you think about why it is possible that her mother does not have one of the BRCA gene mutations, even if her grandmother, aunt, and uncle did have it.
- Why do you think certain gene mutations are prevalent in certain ethnic groups?
Attributions
- Caelius and Valerius family tree by Ann Martin , licensed CC BY 2.0 via Flickr
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
5.1 Case Study: Genes and Inheritance
Created by: CK-12/Adapted by Christine Miller
Case Study: Cancer in the Family
People tend to carry similar traits to their biological parents, as illustrated by the family tree. Beyond just appearance, you can also inherit traits from your parents that you can’t see.
Rebecca becomes very aware of this fact when she visits her new doctor for a physical exam. Her doctor asks several questions about her family medical history, including whether Rebecca has or had relatives with cancer. Rebecca tells her that her grandmother, aunt, and uncle — who have all passed away — had cancer. They all had breast cancer, including her uncle, and her aunt also had ovarian cancer. Her doctor asks how old they were when they were diagnosed with cancer. Rebecca is not sure exactly, but she knows that her grandmother was fairly young at the time, probably in her forties.
Rebecca’s doctor explains that while the vast majority of cancers are not due to inherited factors, a cluster of cancers within a family may indicate that there are mutations in certain genes that increase the risk of getting certain types of cancer, particularly breast and ovarian cancer. Some signs that cancers may be due to these genetic factors are present in Rebecca’s family, such as cancer with an early age of onset (e.g., breast cancer before age 50), breast cancer in men, and breast cancer and ovarian cancer within the same person or family.
Based on her family medical history, Rebecca’s doctor recommends that she see a genetic counselor, because these professionals can help determine whether the high incidence of cancers in her family could be due to inherited mutations in their genes. If so, they can test Rebecca to find out whether she has the particular variations of these genes that would increase her risk of getting cancer.
When Rebecca sees the genetic counselor, he asks how her grandmother, aunt, and uncle with cancer are related to her. She says that these relatives are all on her mother’s side — they are her mother’s mother and siblings. The genetic counselor records this information in the form of a specific type of family tree, called a pedigree, indicating which relatives had which type of cancer, and how they are related to each other and to Rebecca.
He also asks her ethnicity. Rebecca says that her family on both sides are Ashkenazi Jews (Jews whose ancestors came from central and eastern Europe). “But what does that have to do with anything?” she asks. The counselor tells Rebecca that mutations in two tumor-suppressor genes called BRCA1 and BRCA2 , located on chromosome 17 and 13, respectively, are particularly prevalent in people of Ashkenazi Jewish descent and greatly increase the risk of getting cancer. About one in 40 Ashkenazi Jewish people have one of these mutations, compared to about one in 800 in the general population. Her ethnicity, along with the types of cancer, age of onset, and the specific relationships between her family members who had cancer, indicate to the counselor that she is a good candidate for genetic testing for the presence of these mutations.
Rebecca says that her 72-year-old mother never had cancer, nor had many other relatives on that side of the family. How could the cancers be genetic? The genetic counselor explains that the mutations in the BRCA1 and BRCA2 genes, while dominant, are not inherited by everyone in a family. Also, even people with mutations in these genes do not necessarily get cancer — the mutations simply increase their risk of getting cancer. For instance, 55 to 65 per cent of women with a harmful mutation in the BRCA1 gene will get breast cancer before age 70, compared to 12 per cent of women in the general population who will get breast cancer sometime over the course of their lives.
Rebecca is not sure she wants to know whether she has a higher risk of cancer. The genetic counselor understands her apprehension, but explains that if she knows that she has harmful mutations in either of these genes, her doctor will screen her for cancer more often and at earlier ages. Therefore, any cancers she may develop are likely to be caught earlier when they are often much more treatable. Rebecca decides to go through with the testing, which involves taking a blood sample, and nervously waits for her results.
Chapter Overview: Genetics
At the end of this chapter, you will find out Rebecca’s test results. By then, you will have learned how traits are inherited from parents to offspring through genes, and how mutations in genes such as BRCA1 and BRCA2 can be passed down and cause disease. Specifically, you will learn about:
- The structure of DNA.
- How DNA replication occurs.
- How DNA was found to be the inherited genetic material.
- How genes and their different alleles are located on chromosomes.
- The 23 pairs of human chromosomes, which include autosomal and sex chromosomes.
- How genes code for proteins using codons made of the sequence of nitrogen bases within RNA and DNA.
- The central dogma of molecular biology, which describes how DNA is transcribed into RNA, and then translated into proteins.
- The structure, functions, and possible evolutionary history of RNA.
- How proteins are synthesized through the transcription of RNA from DNA and the translation of protein from RNA, including how RNA and proteins can be modified, and the roles of the different types of RNA.
- What mutations are, what causes them, different specific types of mutations, and the importance of mutations in evolution and to human health.
- How the expression of genes into proteins is regulated and why problems in this process can cause diseases, such as cancer.
- How Gregor Mendel discovered the laws of inheritance for certain types of traits.
- The science of heredity, known as genetics, and the relationship between genes and traits.
- How gametes, such as eggs and sperm, are produced through meiosis.
- How sexual reproduction works on the cellular level and how it increases genetic variation.
- Simple Mendelian and more complex non-Mendelian inheritance of some human traits.
- Human genetic disorders, such as Down syndrome, hemophilia A, and disorders involving sex chromosomes.
- How biotechnology — which is the use of technology to alter the genetic makeup of organisms — is used in medicine and agriculture, how it works, and some of the ethical issues it may raise.
- The human genome, how it was sequenced, and how it is contributing to discoveries in science and medicine.
As you read this chapter, keep Rebecca’s situation in mind and think about the following questions:
- BCRA1 and BCRA2 are also called Breast cancer type 1 and 2 susceptibility proteins. What do the BRCA1 and BRCA2 genes normally do? How can they cause cancer?
- Are BRCA1 and BRCA2 linked genes? Are they on autosomal or sex chromosomes?
- After learning more about pedigrees, draw the pedigree for cancer in Rebecca’s family. Use the pedigree to help you think about why it is possible that her mother does not have one of the BRCA gene mutations, even if her grandmother, aunt, and uncle did have it.
- Why do you think certain gene mutations are prevalent in certain ethnic groups?
Attributions
Figure 5.1.1
Family Tree [all individual face images] from Clker.com used and adapted by Christine Miller under a CC0 1.0 public domain dedication license (https://creativecommons.org/publicdomain/zero/1.0/).
Figure 5.1.2
Rebecca by Kyle Broad on Unsplash is used under the Unsplash License (https://unsplash.com/license).
Wikipedia contributors. (2020, June 27). Ashkenazi Jews. In Wikipedia. https://en.wikipedia.org/w/index.php?title=Ashkenazi_Jews&oldid=964691647
Wikipedia contributors. (2020, June 22). BRCA1. In Wikipedia . https://en.wikipedia.org/w/index.php?title=BRCA1&oldid=963868423
Wikipedia contributors. (2020, May 25). BRCA2. In Wikipedia. https://en.wikipedia.org/w/index.php?title=BRCA2&oldid=958722957
Human Biology Copyright © 2020 by Christine Miller is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

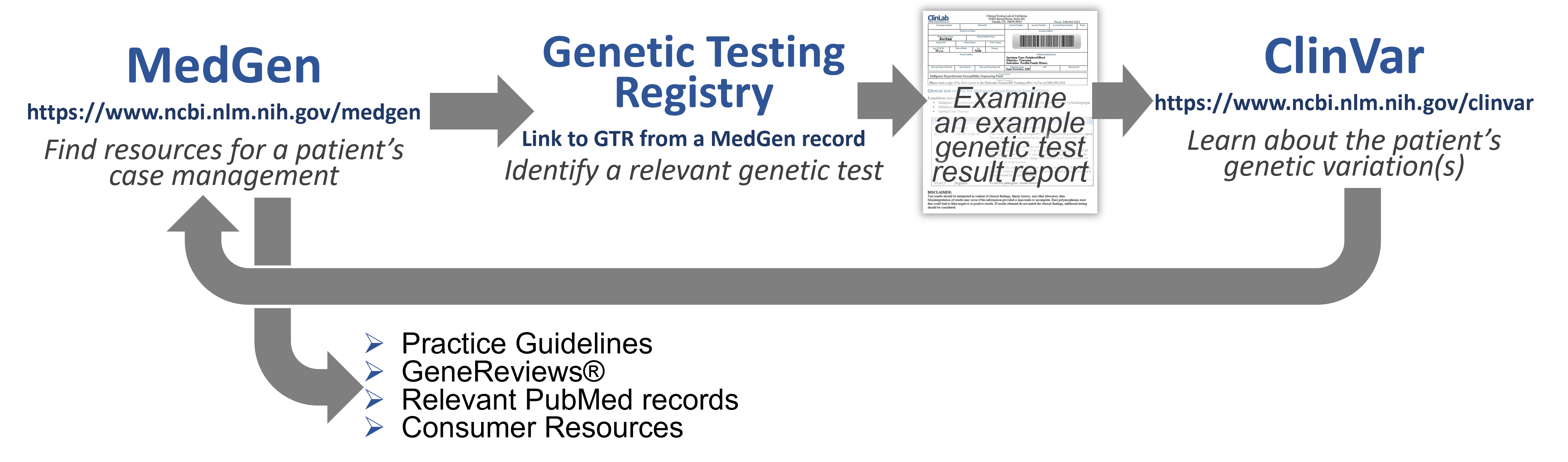
Case 1: Genetic testing to support disorder diagnosis
Welcome to Your Patient!
(P.S. He's now in his mid-30s and doing well!)
Learn more about Jordan's proposed diagnosis
- To learn more about the proposed diagnosis of Malignant Hyperthermia, search MedGen ( https://www.ncbi.nlm.nih.gov/medgen/ ) with:
- Relevant publications available in PubMed.
- Clinical Trials in ClinicalTrials.gov .
- Genetic tests are decreasing in cost & are not particularly invasive.
- A well-known genetic lesion can sometimes help in diagnosis and/or drug/therapy selection - may provide actionable information.
- A finding may predict disorders before symptoms begin for proactive & preventative care.
- We are early in our understanding of genes, gene variants and disease: Failure to detect a pathogenic variant does not rule out the diagnosis.
- Prediction isn’t guaranteed - as pathogenic variants sometimes do not have consistent phenotypic impact in all patients (penetrance, severity, multi-genic & environmental influences).
- Lack of coverage by some insurance companies…
Find a genetic test to order and examine the results
4. In the Genetic Testing Registry section of the MedGen record (on the right), click on the See all link to retrieve information on all of the genetic test information that has been submitted to us by providers for this disorder or condition.
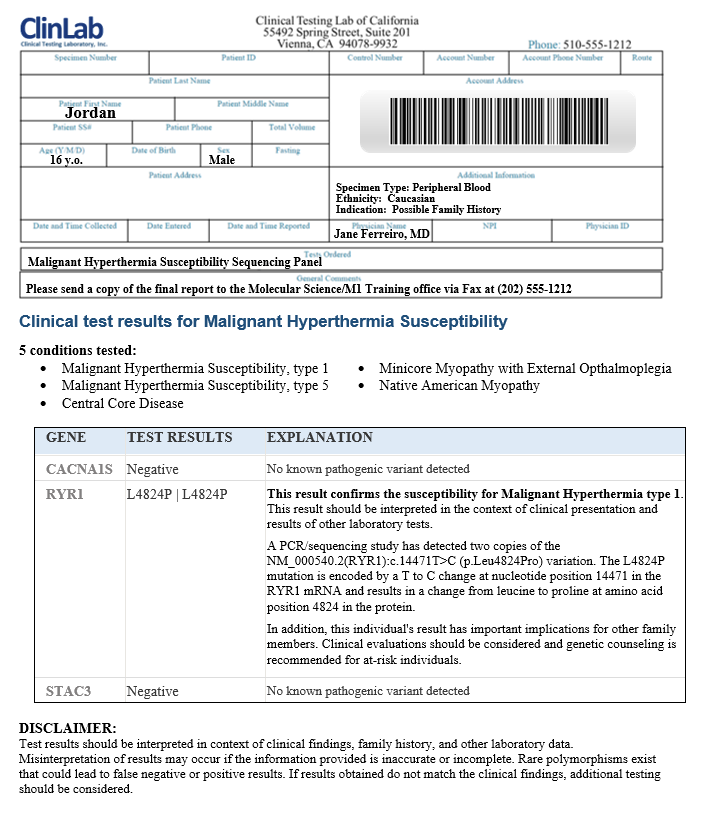
- Hopefully, you already knew what to do with the information (potential impact of a genetic variant on the patient’s physiology and phenotype and how this relates to your choice of case management) – before the test was ordered.
- A patient may ask: “ What is wrong with me and how can we fix it?" A great reason to consult with a Genetic Counselor!
- Implications for the patient - beyond this particular surgery: Consider having them discuss this with their primary care physician, dentist, and any other clinical professionals who may need to know for their care.
- Implications for the patient’s family members: Should they tell others?
Validate the genetic test result assertion and find more information about a genetic variant
- To validate what is asserted by this clinical testing laboratory, search NCBI’s ClinVar database ( https://www.ncbi.nlm.nih.gov/clinvar/ ) with:
Important! Assertions about the clinical significance or interpretation are provided to NCBI by submitters. All those who have provided information are listed in the Submitted interpretations and evidence section of the record, so that you can look at them all and learn more about what each submitter provided.
Find a practice guideline to identify actionable recommendations
Find patient education materials to share with the patient and his family.
- Professional literature such as a the full GeneReviews Chapter on the NCBI Bookshelf , OMIM or one of the Reviews in PubMed .
- For a more lay audience, you could find information in MedlinePlus or MedlinePlus Genetics (GHR) or NIH's NCATS Genetic and Rare Diseases Information Center
- Halogenated volatile anesthetics, such as enflurane, methoxyflurane, desflurane, halothane, isoflurane, sevoflurane.
- The depolarizing neuromuscular blocker succinylcholine.
- Anesthetics such as propofol supplemented by benzodiazepines, opioids, nitrous oxide, or regional anesthetic techniques. Amide and ester local anesthetic agents can also be used in these patients.
- Non-depolarizing neuromuscular blockers such as mivacurium, atracurium, rocuronium, pancuronium, cisatracurium, and vecuronium.
- Jordan may want to inform other healthcare practicioners, in case they need to do procedures involving triggering agents, such as his dentist.
- Because of a possible risk for exposure to non-anesthetic triggering conditions, such as Exertional heat stroke or Exertional rhabdomyolysis, Jordan may want to discuss that mid-summer athletic camp with his care team.
Take-away Message!
This case study was an example of how genetic testing for diagnosis of a disorder might impact the optimal case management plan for a particular patient based on their genetics. It also showed that understanding a patient's particular risk may have wide implications for both themselves and their families and could help to inform health and medical care beyond one incident.
Last Reviewed: April 18, 2023
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Case Reports
Sex-determining region y (sry) in a patient with 46,xx true hermaphroditism.
- Akito Tanoue
- Toshiro Nakamura
- Ichiro Matsuda
Direct insertion of euchromatic material from chromosome y in the x-chromosome in hypogonadotropic hypogonadisms with crohn’s disease
- K. H. Ramesh
- Ram S. Verma
Mevalonic acidemia: First case of Japan
- Nobuhiko Okamoto
- Mashiro Nakayama
- Soichiro Toda
Megalocornea-mental retardation syndrome: An additional case report
- Kenji Naritomi
- Yasutsugu Chinen
- Takaya Tohma
An azoospermic male with an unbalanced autosomal-Y translocation
- Atsumi Yoshida
- Yutaka Nakahori
- Masafumi Shirai
A nager acrofacial dysostosis syndrome patient with severe respiratory distress syndrome (RDS)
- Tatsuro Kondoh
- Yoshiro Tsuji
The cohen syndrome: Report of a case
Small interstitial deletion of the long arm of chromosome 2 (2q24.3): further delineation of 2q medial monosomy syndrome, interstitial deletion of the short arm of chromosome 10: report of a case and review of the literature.
- Zenichiro Kato
- Tomomi Kato
A japanese patient with X-linked α-thalassemia/mental retardation syndrome: An additional case report
- Kenji Kurosawa
- Masako Asoh
- Kihei Maekawa
Retrieval of aneuploidy by fish-technique in a case with 46,XX/47,XXX/47,XX,+8
- Swarna K. Gogineni
- David N. Mann
Missense mutation of rhodopsin gene codon 15 found in Japanese autosomal dominant retinitis pigmentosa
- Keiko Fujiki
- Yoshihiro Hotta
- Atsushi Kanai

Chromosome 1q terminal deletion resulting from de novo translocation with an acrocentric chromosome
- Shuichi Nishimura
- Tatsuro Ikeuchi
Paracentric inversion of chromosome 14: A case report
- Shigeki Uehara
- Shingo Tanigawara
- Akira Yajima
Asphyxiating thoracic dystrophy: Surgical correction and 2-year follow-up in a girl
- Fumio Takada
- Koh-ichi Hiroki
- Yoshikazu Kuroki
Cytogenetic study of a severe case of Pallister-Killian syndrome using fluorescence in situ hybridization
- Sahar M. Gamal
- Tomoko Hasegawa
- Yasuhisa Satoh
A family with pericentric inversion of chromosome 12
Familial hyperextensible proximal interphalangeal joints.
- Masato Tsukahara
- Isabel Fernandez G.
The costello syndrome: Report of a case and review of the literature
- Ikuko Kondo
- Koichiro Tamanaha
- Kaoru Ashimine
The Costello syndrome: Are nasal papillomata essential?
- Reiko Yoshida
- Yoshimitsu Fukushima
- Yukio Fukuyama
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- MedEdPORTAL

A Case-Based Active Learning Session for Medical Genetics Resources
Hana anderson.
1 Associate Professor, Department of Internal Medicine and Department of Cell Biology and Human Anatomy, University of California Davis School of Medicine
Amy C. Studer
2 Health Science Librarian, Blaisdell Medical Library, University of California Davis School of Medicine
Katharine N. Holm
3 Research Associate, Department of Biochemistry and Molecular Medicine, University of California Davis
Ayaka Suzuki
4 Licensed and Certified Genetics Counselor, Division of Genomic Medicine, Department of Pediatrics, University of California Davis
Associated Data
- Syllabus Introduction.docx
- Student Preclass Hands-on Exercise.docx
- Session Timetable.docx
- Didactic In-class Discussion.docx
- Students In-class Activity.docx
- Faculty Preclass Hands-on Exercise.docx
- Faculty Guide In-class Activity.docx
- Postsession Survey.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Introduction
As the clinical applications of medical genetics and genomics continue to expand, nongenetics professionals increasingly find themselves in the position of managing patients with genetic conditions. To prepare medical students to handle this future practice demand, it is imperative that they obtain skills and confidence in utilizing credible medical genetics resources to care for patients with genetic conditions. To this end, we developed active learning materials to introduce first-year medical students to these resources.
This approximately 2-hour session targeted first-year medical students (123 students) and combined flipped classroom and small-group collaborative case-based learning models. Students first completed a hands-on preclass exercise, which guided them in navigating the Online Mendelian Inheritance in Man website, and then attended an in-person small-group classroom activity, which provided the opportunity to apply information obtained from credible medical genetics resources to a patient case. At the conclusion of the classroom activity, students voluntarily completed an anonymous survey.
Results of student postsession surveys showed that, regardless of previous exposure to medical genetics resources, this session increased both confidence in skills and future intention to use medical genetics resources.
Since the majority of students were unfamiliar with using specialized medical genetics resources prior to this educational intervention, the session functioned as a practical introduction to these essential resources. We propose that equipping medical students with skills that support inquiry-oriented learning, particularly in the early stage of training, can cultivate the practice of lifelong learning in medical genetics.
Educational Objectives
By the end of this activity, learners will be able to:
- 1. Identify clinical questions relevant to a patient with a possible genetic condition, guided by an established framework.
- 2. Utilize credible, specialized medical genetics resources (e.g., Online Mendelian Inheritance in Man and GeneReviews) to acquire information related to a clinical genetics case.
- 3. Apply the information gathered using specialized medical genetics resources to answer various types of questions generated during a medical genetics case (e.g., differential diagnosis, genotype-phenotype relationships, genetic testing, patient management, patient advocacy and support, family counseling, and clinical trials).
- 4. Apply basic genetics concepts and tools to clinical genetics cases (e.g., phenotypic heterogeneity, allelic heterogeneity, locus heterogeneity, and family pedigree).
- 5. Describe the value of collaborations with genetic counselors in the care of patients and families with suspected genetic conditions.
The application of genetics and genomic medicine to clinical practice has been steadily expanding, owing to rapid advances in the knowledge of the genetic basis for a broad range of human diseases and the increased use of genetic testing. 1 For example, the recent expansion in applications of genomic medicine in cancer diagnosis and treatment 2 and clinical utility of whole exome sequencing 3 epitomize the trajectory of genomic medicine in practice. However, the number of genetics professionals (e.g., medical geneticists, genetic counselors) is not keeping pace with the growing demand. 4 , 5 Increasingly, nongenetics professionals are placed in the position of providing care for patients with genetic conditions, creating an urgent need for genetics curricula to adapt. 6 – 8 As the clinical importance of medical genetics continues to grow, there is a compelling need to educate today's health professions students with the essential knowledge and skills that will allow them to adapt to the fast-paced progress of genetics and genomic medicine. 9
Considering that there are over 5,000 monogenic disorders 10 and the fields of genetics and genomic medicine are constantly evolving, 11 it is critical that clinicians be able to identify and effectively use credible medical genetics resources at the point-of-care. To this end, undergraduate medical genetics education should support the development of inquiry-oriented critical thinking skills and lifelong learning practice beyond the memorization of factual knowledge. Indeed, the Association of Professors of Human and Medical Genetics’ Medical School Genetics Competencies address the importance of these skills as a component of practice-based learning and improvement. They propose that students should be able to: (1) use information technology to obtain reputable current information about genetics, and (2) demonstrate skills required to stay abreast of advances in genetics that relate to medical practice. To achieve these competencies, it is required that medical students become proficient in utilizing medical genetics resources, such as Online Mendelian Inheritance in Man (OMIM) and GeneReviews. 12
At the University of California (UC) Davis School of Medicine, we observed that first-year medical students typically do not have prior exposure to these resources, thereby presenting a skills gap that needed to be addressed. To this end, we developed an active learning session to introduce first-year medical students to credible medical genetics resources. This learning session combined a preclass individual hands-on guided exercise and an in-class small-group collaborative learning activity. The preclass exercise was based on a hypothetical clinical vignette to guide students in learning basic navigation of the OMIM website. The in-class session was developed around a patient case, which allowed students to learn how to apply medical genetics resources in solving questions presented by real-life situations. Case-based learning has been proven to enhance students’ learning by aiding them in linking theory to clinical practice. 13 The positive learning effects of using a case-based approach in preclinical curriculum to stimulate students’ engagement has been clearly demonstrated. 14 – 16
In medical education literature, a few learning modules combining online medical genetics resources and patient vignettes have been published. 17 – 19 Two studies from the Johns Hopkins School of Medicine described how incorporating asynchronous OMIM training modules into a preclerkship genetics course was regarded positively by students and was associated with increased confidence in clinical genetics skills. 17 , 20 In our session, we built on the basic formula used in these previous reports and significantly expanded the student learning experience as described above. Our work makes a unique contribution to the literature by offering preclerkship students highly structured learning materials for introducing medical genetics resources, thereby providing know-how of genetic investigation in a time-efficient manner. This module could serve as a foundation for further genetics skills training during clerkship, such as reported by Hoffman et al. 21 Either in conjunction with clerkship modules or as a standalone activity, the resource presented here will encourage students to use specialized medical genetics resources as a lifelong learning practice in clinical genetics.
Curricular Context
At UC Davis School of Medicine, preclinical courses are currently offered during the first 2 years, including foundational science courses covering basic science principles of human health (first year), followed by pathophysiology and organ-based courses (second year). Genetics instruction is part of the foundational sciences at UC Davis. Within our competency-based curriculum framework, the genetics course supports graduation milestones in the knowledge competency, such that students will be able to apply current fundamental genetics knowledge to problem solving, as well as identify credible medical genetics resources and critically appraise information in the practice of lifelong learning and evidence-based medicine (EBM).
We designed this resource for first-year medical students as the first genetics active learning session during the 2019–2020 academic year. To receive full credit for this learning session, students needed to complete the preclass hands-on exercise (half credit) and attend the in-class active learning session (half credit). Our goals were to provide students with the opportunity to become familiar with specialized medical genetics resources, so that they could utilize these resources to practice EBM. In lectures prior to this session, students learned basic genetics concepts, such as human genome structure, genetic diversity in human populations, cytogenetics, mode of inheritance, population genetics, molecular tools for genetic testing, and molecular bases of genetic diseases. Students also had an active learning session in their epidemiology course that introduced them to credible medical resources in the context of beginning EBM instruction.
Preclass Individual Activities
A week prior to the in-class session, we provided students with the session syllabus ( Appendix A ) and guided hands-on exercise assignment ( Appendix B ). The syllabus included a list of recommended medical genetics resources and a framework of clinical questions for patients with possible genetic conditions. The question framework was based on the list previously published by Diehl et al. 17 The goal of the preclass hands-on exercise was to familiarize students with specialized medical genetics resources, with an emphasis on OMIM. To this end, we constructed a clinical vignette of a hypothetical Marfan syndrome patient and five associated questions modeling after an OMIM tutorial exercise published by Diehl et al. 17 To support asynchronous learning, we supplemented the assignment with detailed instructions for the relevant search and analysis functions available on the OMIM website ( Appendix B ). Students completed the preclass exercise individually and submitted their answers to the genetics course website prior to the in-class session. The correct responses are included for facilitators in Appendix F .
In-Class Session
The in-class session was held in an active learning classroom with small-group tables, each equipped with a large monitor, but can also be convened in a lecture hall. We divided the class (123 students) into 18 groups of six to seven students, assigned in alphabetical order. The in-class session was 110 minutes long and the time allotted to each activity was summarized in Appendix C . When conducting this learning activity using small-group rooms, we recommend limiting the group size to a maximum of 10 students, if possible, to encourage student participation.
Supplemental didactic discussion
At the beginning of the in-class session, we spent approximately 10 minutes exploring the clinical resources external links accessible from the OMIM website (e.g., GeneReviews, ClinicalTrials, MedlinePlus Genetics). 22 The genetics course instructor led this free-form didactic portion using three questions provided in Appendix D .
Case-based group learning activity
The in-class session was based on the case of a patient diagnosed with hereditary diffuse gastric cancer caused by a germline pathogenic variant in the cadherin-1 gene ( Appendix E ). Students were encouraged to use the medical genetics resources listed in the syllabus ( Appendix A ) to answer eight case-related questions. The first three questions were made available at the beginning of the in-class session and students were given 25 minutes to draw a pedigree using the patient's family history, propose possible diagnoses based on the family history, and discuss the appropriate type of genetic testing for the patient. A question and answer period (15 minutes) immediately followed, during which we randomly selected a student group to present an answer. After the question and answer session, a genetic counselor (one of the facilitators) shared a 10-minute informal introduction ( Appendix G ) on the role of a genetic counselor and how physicians and genetic counselors collaborate to manage patients. The patient's genetic testing result and the remaining five questions were then made available to students on the course website. With this final set of questions, students interpreted the genetic testing result, and explored the implications of the diagnosis for the patient and her family as well as resources to support and answer patient's questions. Twenty-five minutes were allotted for working on these questions and 20 minutes for the question and answer session that followed.
Facilitation of the in-class session
Four facilitators were present and circulated the room including two preclinical basic science faculty (PhD with background in human genetics), one genetic counselor, and one medical librarian. Facilitators answered students’ questions and provided pointers to keep students on track. The presence of a genetic counselor and a librarian allowed us to model interprofessional teamwork for students. In preparation for the session, facilitators reviewed the syllabus and faculty guides ( Appendices A , F , and G ), which were provided to them 1 week prior. We also had a 30-minute presession meeting to discuss any questions. The two question-and-answer sessions at the in-class session were led by the instructor of the genetics course, who was also one of the facilitators.
We distributed anonymous survey sheets ( Appendix H ) to each table at the beginning of the in-class session and collected them after the session. We designed the survey questions to collect: (1) students’ prior experience with medical genetics resources before the session and students’ intended use of the resources after the session, (2) students’ comfort levels in using newly introduced medical genetics resources at the conclusion of the session, and (3) narrative responses to the session as a whole.
Preclass Hands-On Exercise
All 123 first-year students completed all five questions of the required preclass hands-on exercise however time logs for nine students were not fully recorded and, therefore, they were excluded from time calculation. The average time taken by students to finish the exercise was 32 ± 24 minutes ( n = 114). Students’ answers indicated that they followed the instructions closely and navigated the OMIM site as intended. Five students gave answers other than Marfan syndrome; however, these alternatives were phenotypically similar connective tissue disorders such as Marfanoid-Progeroid-Lipodystrophy syndrome and Loeys-Dietz syndrome type 1.
Postsession Survey Results
The voluntary postsession survey response rate was 46% (57 of the 123 students). Of the respondents, 30 students indicated they had done online searches on genetic conditions before this session and 27 had not. Figure 1 summarizes the reported usage of online resources by students while searching for information about genetic conditions prior to and after this session. Among the students with prior search experience, the most frequently used online sites before the session were PubMed, UpToDate, and Google. Only a small fraction of these students indicated that they had used OMIM and/or GeneReviews. After the session, the vast majority of students, independent of the prior search experience, said their choice of online resource for searching genetic conditions would be OMIM.

To the Likert-scale (1 = strongly disagree , 5 = strongly agree ) question, “After this session, I feel more confident in using medical genetics resources to investigate genetic conditions” most students with prior search experience (96%) responded strongly agree or agree , as did most students without prior search experience (89%; Figure 2 ). In narrative responses regarding the session, students commented positively on the: (1) effectiveness of the preclass hands-on exercise, (2) value of learning experience using a patient case, (3) usefulness of OMIM, and (4) value of interacting with a genetic counselor and a medical librarian as facilitators. The representative narrative excerpts were:
- • “The preclass assignment was very helpful—I was not aware of lots of the more nuanced functions of OMIM like ‘compare selected,’ tables, etc.”
- • “The questions were realistic. I wish we could have more specific case-based work like this.”
- • “I loved the OMIM website—it's tough to navigate at first, but so cool when you get used to it— will definitely use in future. I have it bookmarked on my computer!”
- • “I found it helpful to hear from the genetic specialist and search experts. It was nice having to navigate the website on our own. Interesting discussion questions; I liked thinking about all aspects of care, including useful legal and support info.”

Critical comments suggested that the in-class session could be shortened and that the class cover more than one genetic condition; a representative excerpt was, “Timeframe was a little long. Could have been interesting to investigate more than one condition instead of one condition in depth.”
We developed this session to provide practical knowledge and skills that enabled students to obtain reputable information on genetic conditions and apply it to clinical cases. We envisioned that the learning experience gained in the early stage of medical education will foster students’ practice of EBM and lifelong learning in genetics and genomic medicine. The structure of our session was a combination of a flipped classroom and small-group collaborative case-based learning activity. At the end of the in-class session, we conducted a voluntary survey to assess perceived changes in attitudes, future intention to use medical genetic resources, and confidence levels in using these resources. Narrative survey responses helped to identify what worked and what can be improved. Having two opportunities to practice using the medical genetics resources—first as an individual assignment then as a group assignment—was received favorably by students. Specifically, they indicated that the preclass hands-on exercise oriented them in the basic functions of OMIM and the group activity allowed them to focus on obtaining germane information for solving the patient case. This was reflected by a narrative response such as, “I found utilizing these resources as a group was helpful, especially OMIM.”
Our survey showed that about a half of the responding students had never searched for information on genetic conditions and the vast majority of them had never used OMIM before ( Figure 1 ). Despite the fact that this session was their first encounter with OMIM, the students followed the hands-on exercise instructions closely and applied the learned skills successfully to the in-class patient case. In addition, regardless of prior search experience, a significant proportion of the students expressed their intention of using OMIM after the session ( Figure 1 ) and increased confidence in medical genetics databases ( Figure 2 ). The significant preference for OMIM demonstrated by students likely stemmed from the hands-on exercise which focused on the use of OMIM, even though we described the utility of other resources such as GeneReviews and ClinVar whose links are listed at the OMIM site as clinical resources. These results indicate that students become motivated to use specialized genetics resources when they acquired skills through active learning. We think adopting multiple instructional methods in the session also maximized learning by supporting various learning preferences of individual students. 23
Lessons Learned and Implementation Challenges
We noticed that even though other useful resources such as GeneReviews were referred to in the students’ materials ( Appendices A , B , D , and E ), they ranked low in the resource list of future intended use ( Figure 1 ). This result revealed to us that tailoring exercise questions to different resources would be necessary to increase students’ comfort level for using them. During the in-class session, progress varied among groups, leaving some fast-paced students unoccupied. This is a common challenge in dealing with multiple student groups and providing additional cases for extra credit could keep more advanced students engaged. Additional challenges with implementation may include recruiting a sufficient number of facilitators to support small-group learning.
Limitations
We have identified the following limitations in our analysis. First, results reported here were based on one class of students; therefore, conducting an analysis based on data from multiple classes of students would make our assessment more robust and reproducible. Second, observing the long-term effect of the session on students’ behavior is desirable. Evaluating students’ habits for medical genetics resources usage throughout the clinical curriculum would provide an appropriate outcome assessment. For example, at UC Davis, third-year students shadow genetic counselors counseling familial cancer cases during the OB/GYN clerkship. As Hoffman et al. 21 successfully delivered genetics cases during the third-year pediatrics clerkship, revisiting evidence-based genetics learning could provide a suitable opportunity to reevaluate and reinforce the use of medical genetics resources.
Future Directions
Currently, at UC Davis School of Medicine, we are redesigning our curriculum to be a patient- and learner-centered curriculum. To enhance the clinical relevance of basic science education, it is important to teach students not simply factual knowledge, but also skills in identifying and validating current information so they can practice evidence-based patient care. To this end, we will continue to provide opportunities for student skill development in the effective use of medical genetics resources in the medical school curriculum. The resource presented here functions as an introductory module to essential skills for lifelong learning in managing patients with genetic conditions.
Disclosures
None to report.
Funding/Support
Ethical approval.
Reported as not applicable.

IMAGES
VIDEO
COMMENTS
How Gregor Mendel discovered the laws of inheritance for certain types of traits. The science of heredity, known as genetics, and the relationship between genes and traits. Simple and more complex inheritance of some human traits. Genetic Disorders.
Chapter Overview: Genetics. At the end of this chapter, you will find out Rebecca’s test results. By then, you will have learned how traits are inherited from parents to offspring through genes, and how mutations in genes such as BRCA1 and BRCA2 can be passed down and cause disease. Specifically, you will learn about:
Case Reports in Genetics publishes case reports and case series focusing on diseases caused by hereditary predisposition or genetic variation in individuals and families.
This is a case report of presumed non-accidental injury that had an underlying medical condition of congenital insensitivity to pain with anhidrosis (CIPA). CIPA is a rare autosomal recessive genetic disease caused by certain gene mutations. CIPA, also known as hereditary sensory and autonomic neuropathy type IV, is a rare genetic condition [1 ...
The goal of this case study is to show you how to perform research to support a disorder diagnosis and to identify information suitable for optimizing a specific patient's case management based on the results of their genetic test results.
Cytogenetic study of a severe case of Pallister-Killian syndrome using fluorescencein situ hybridization. Sahar M. Gamal; Tomoko Hasegawa; Yasuhisa Satoh
Case study: Testing for genetic disorders. Purpose: A genetic disorder is a disorder that is caused by an abnormality (or several abnormalities) in a person’s genome. Genetic disorders are often hereditary, which means they are passed down to a child from its parents.
Genetics in Practice: Five Case Studies. Case 1: No News Is Good News–A Family History of Intellectual Disability. Nathan, aged 30 years, and his wife Natalie, aged 28 years, are planning a pregnancy in the next year. They are concerned because Nathan’s 36-year-old brother, Billy, has mild intellectual disability. The Medical-Family History.
A recent study suggested that it was possible to use genome editing to correct a dominant mutation in embryos fertilised by sperm from a man with cardiomyopathy.
Apply the information gathered using specialized medical genetics resources to answer various types of questions generated during a medical genetics case (e.g., differential diagnosis, genotype-phenotype relationships, genetic testing, patient management, patient advocacy and support, family counseling, and clinical trials).