- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

An Overview of Histopathology
Also Known as a Biopsy or Pathology Report
What Is Histopathology?
- How It's Performed
- Report Components
- Interpretation
Other Sampling Techniques
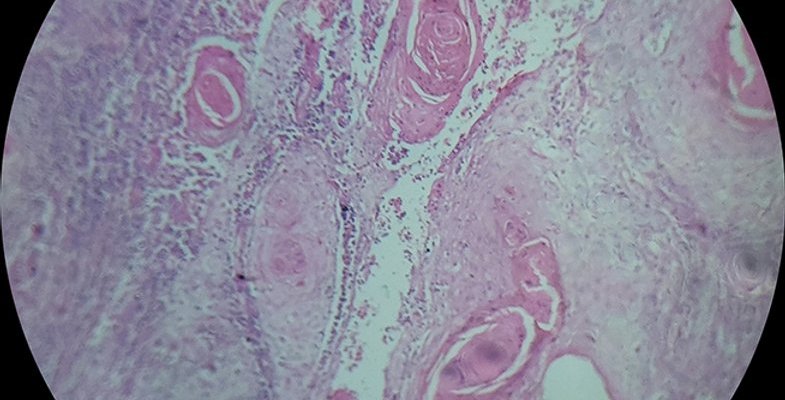
Histopathology involves using a microscope to look at human tissue to check for signs of disease. The term is derived from "histology" (meaning the study of tissues), and "pathology" (meaning the study of disease).
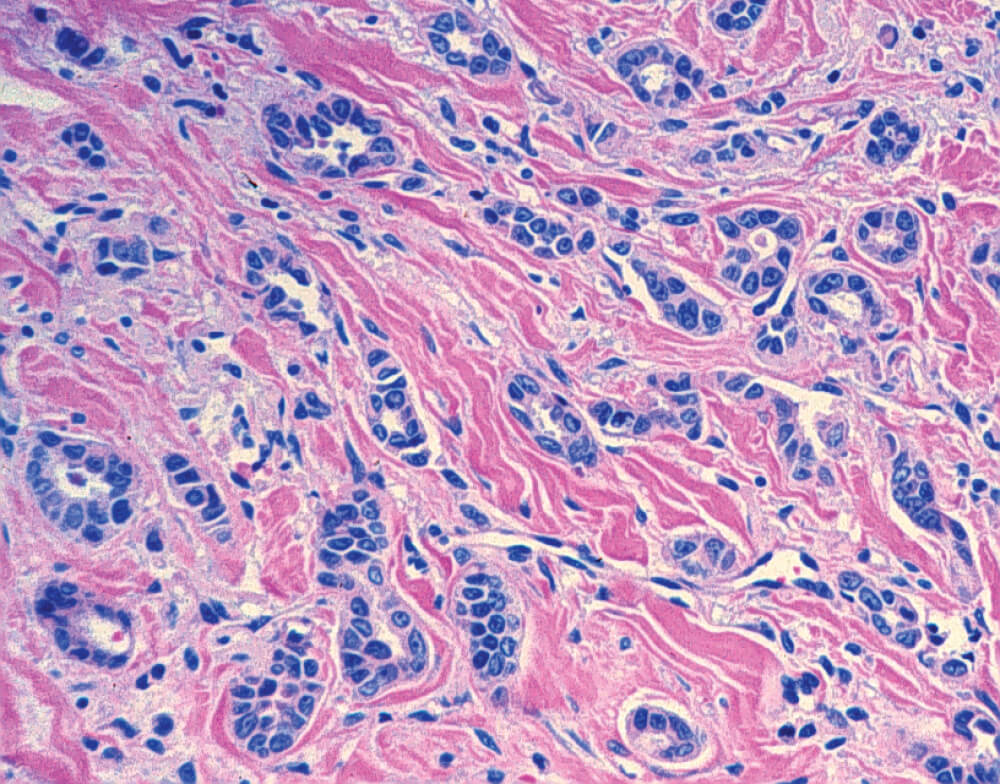
A histopathology report describes the findings of a specialist known as a medical pathologist . Examples include the accumulation of white blood cells seen with infections, crystallized deposits that occur with gout , granular lumps characteristic of tuberculosis or sarcoidosis , or abnormal cell formations seen with cancer .
This article explains the purpose of histopathology, what's in a histopathology report, and reasons why a histopathology test may be done. It also details how pathology results are interpreted.
In clinical practice, histopathology refers to the examination of tissues obtained by biopsy or the surgical removal of an organ. It is a form of anatomical pathology that looks specifically at tissues and organs as opposed to clinical pathology which looks at bodily fluids.
Histopathology is performed by a lab-based pathologist who, with the assistance of a medical technologist , prepares the tissues by sectioning them and placing them on a glass slide. The sample can then be exposed to dyes and other techniques to highlight, segregate, or remove cells so they are better viewed under the microscope.
Histopathology is not the same thing as cytopathology which looks at individual cells. With histopathology, the pathologist not only evaluates cell structure but also how cells are grouped.
Why Is Histopathology Important?
Without histopathology, it would be difficult, if not impossible, to diagnose many diseases. It is essential to the diagnosis of many conditions, chief of which includes cancer .
Along with a biopsy (the extraction of tissues for lab evaluation), histopathology remains the gold standard for diagnosing many solid-tumor cancers. Histopathology can differentiate benign tumors from cancerous ones and is also central to cancer staging (determining how advanced a cancer is) and cancer grading (determining how aggressive a cancer is).
Other diseases for which histopathology is central to the diagnosis include:
- Infectious diseases like disseminated tuberculosis , tropical parasitic infections , H. pylori , and necrotizing fasciitis
- Inflammatory diseases like sarcoidosis , Crohn's disease , ulcerative colitis , and vasculitis
- Autoimmune diseases like celiac disease , psoriasis , scleroderma , autoimmune hepatitis , and lupus nephritis
- Organ-specific diseases like endometriosis , uterine fibroids , and peptic ulcers
Histopathology is also important for the management of diseases. It can help monitor for organ rejection after transplant surgery or check for the response to treatment of inflammatory bowel disease (IBD) .
Histopathology also contributes to advances in our understanding of diseases, leading to the development of new treatments. It can also look for new genetic or immunological biomarkers for diseases so that they can diagnosed earlier when they are most treatable.
How Is Histopathology Performed?
Histopathology is performed by pathologists who process and cut tissue into very thin layers, called sections. Then, they stain and examine it with a microscope. Using a microscope, they can observe and document the tissue's details.
Histopathology relies on samples of tissue obtained through procedures such as endoscopy , colonoscopy , and colposcopy , or by doing surgical procedures such as a breast biopsy .
Click Play to Learn All About Histopathology
This video has been medically reviewed by Anju Goel, MD, MPH .
Frozen Section
For some diseases, a sample of the tissue can be interpreted very quickly using frozen sections (also called a cryosection) that are obtained during surgery. Frozen sections are examined immediately in the lab to provide a result within about 20 minutes.
This type of pathology is most commonly used to evaluate tumor margins during surgery so that a surgeon can decide if more tissue should be removed for the full removal of cancer. The use of frozen sections during surgery depends on the type of cancer being removed and other factors.
Lymph and Blood Cancers
Lymph nodes are often biopsied to evaluate for certain types of blood cancer and to identify metastases of solid tumors (such as breast cancer and lung cancer). A bone marrow biopsy may also be required for a definitive diagnosis of many types of blood cancers.
Components of a Histopathology Report
Histopathology reports on surgical cancer specimens can be complex. They may include:
- A description of the appearance of the involved tissue
- A diagnosis
- A synoptic report detailing the findings of the case
- Pathologist's comments
Histopathology reports can be challenging to understand, so it's essential to go over them with a healthcare provider. Knowing which components are going to be included in your report may help you prepare for your appointment.
Interpreting the Results
Many of the pathologist's findings are used to help determine prognosis , especially in cases of cancer. Prognosis is the prediction or estimate of survival or recovery from a disease.
Prognostic indicators may include:
- Size and severity of the disease
- Tumor grade
- Indications that cancer has spread and the extent of spread
Grading systems differ depending on the kind of cancer. In general, the cells are scored based on how abnormal they appear under the microscope. The more abnormal the cells look, the higher the grade.
For example, Grade 1 tumors appear nearly normal, whereas Grade 4 tumors reflect more abnormalities.
In addition to histopathology, pathologists may use other techniques to assess the presence of cancer in the tissues.
Molecular Techniques
Molecular techniques refer to the ability to analyze cells and tissues at the molecular level, which is at the level of proteins, receptors, and genes.
Pathologists diagnose cancer, such as leukemia , through a combination of techniques, including:
- Cytochemistry : How the sampled cells take up certain stains
- Immunophenotype : Looks for unique surface proteins
- Karyotype : Chromosomal changes
- Morphology : How the cells look
Immunohistochemistry
Often in lymphomas and other cancers, pathologists use immunohistochemistry to help assess the tumor type, prognosis, and treatment.
Immunohistochemistry involves using antibodies to stick to particular tags or markers outside the cancer cells. These markers that the antibodies attach to often have "CD" in their name, which stands for "cluster of differentiation." CDs identify cell phenotypes, which identify different cancers.
For example, if CD23 and CD5 are present in the cancer cells, it might support the notion that chronic lymphocytic leukemia (CLL) is a possible diagnosis.
However, these same markers are also present in other malignancies. So pathologists use this method in combination with other identifying features.
Chromosomal Studies
Pathologists may perform molecular and chromosomal studies to look at gene rearrangements and specific changes to the chromosomes. Sometimes inserted or deleted genes correlate to prognosis. Genetic changes present in a cancer tissue sample may be hereditary or acquired.
For instance, in CLL, a specific piece of a chromosome (17p) is lost. Along with the missing chromosome, a gene that helps suppress cancer is often lost.
The 17p deletion is found in about 5% to 10% of people with CLL overall. The 17p deletion CLL is a form of CLL that is harder to treat with conventional chemotherapy.
Putting It Together
Pathologists may use additional pathology techniques to diagnose cancer. For example, molecular techniques look at proteins, receptors, and genes, which help identify cancer subtypes. Immunohistochemistry looks for markers on cancer cells to narrow down what type of cancer a person has and chromosomal studies look at gene differences to develop a prognosis.
Histopathology is the study of tissue to look for disease. Pathologists perform histopathology in a lab. They examine tissue under a microscope and develop a report of their findings.
Histopathology reports can include descriptions of the tissue, diagnosis, and prognosis. In addition to evaluating the shape and structure of cells, pathologists may also use other techniques to assess and diagnose cancer.
National Cancer Institute. NCI dictionary of cancer terms.
Royal College of Pathologists. Histopathology .
Underwood JCE. More than meets the eye: the changing face of histopathology . Histopathology. 2017;70:4–9. doi:10.1111/his.13047
University of California Davis. Best practices in frozen section analysis .
Dogan NU, Dogan S, Favero G, Kohler C, Dursun P. The basics of sentinel lymph node biopsy: anatomical and pathophysiological considerations and clinical aspects . J Oncol. 2019;2019:3415630. doi:10.1155/2019/3415630
Tomasian A, Jennings JW. Bone marrow aspiration and biopsy: techniques and practice implications . Skeletal Radiol . 2022;51(1):81-88. doi:10.1007/s00256-021-03882-w
College of American Pathologists. How to read your pathology report .
Schafer KA, Eighmy J, Fikes JD, et al. Use of severity grades to characterize histopathologic changes . Toxicol Pathol . 2018;46(3):256-265. doi:10.1177/0192623318761348
Salto-Tellez M, James JA, Hamilton PW. Molecular pathology – the value of an integrative approach . Mol Oncol. 2014 Oct;8(7):1163–1168. doi:1016/j.molonc.2014.07.0211
Ho C, Rodig SJ. Immunohistochemical markers in lymphoid malignancies: Protein correlates of molecular alterations . Semin Diagn Pathol . 2015;32(5):381-91. doi:10.1053/j.semdp.2015.02.016
Shadman M. Diagnosis and treatment of chronic lymphocytic leukemia: a review . JAMA . 2023;329(11):918-932. doi:10.1001/jama.2023.1946
Yu L, Kim HT, Kasar S, et al. Survival of Del17p CLL depends on genomic complexity and somatic mutation . Clin Cancer Res . 2017;23(3):735-745. doi:10.1158/1078-0432.CCR-16-0594
Taylor J, Xiao W, Abdel-wahab O. Diagnosis and classification of hematologic malignancies on the basis of genetics . Blood . 2017;130(4):410-423.
By Indranil Mallick, MD Indranil Mallick, MD, DNB, is a radiation oncologist with a special interest in lymphoma.
You are using an outdated browser. Please upgrade your browser or activate Google Chrome Frame to improve your experience.
- Discover pathology
Histopathology
What is histopathology.
Histopathology is the diagnosis and study of diseases of the tissues, and involves examining tissues and/or cells under a microscope. Histopathologists are responsible for making tissue diagnoses and helping clinicians manage a patient’s care.
Why is histopathology important?
Histopathologists are doctors who work closely with other clinical specialties. They can reach a diagnosis by examining a small piece of tissue from the skin, liver, kidney or other organ. This is called a biopsy.
They examine the tissue carefully under a microscope, looking for changes in cells that might explain what is causing a patient’s illness. Around 20 million histopathology slides are examined in the UK each year.
Cancer Diagnosis
Histopathologists provide a diagnostic service for cancer; they handle the cells and tissues removed from suspicious ‘lumps and bumps’, identify the nature of the abnormality and, if malignant, provide information to the clinician about the type of cancer, its grade and, for some cancers, its responsiveness to certain treatments.
With the help of sophisticated imaging techniques, biopsy tissue can now be obtained from previously inaccessible sites such as the pancreas or retroperitoneum (behind the peritoneum, the membrane lining the abdominal cavity). Tissue is then processed, usually overnight, before being examined under a microscope. In certain limited circumstances using special techniques, the specimen can be examined immediately.
With rapidly changing developments in molecular pathology, pathologists are leading the way with new techniques such as fluorescence in-situ hybridization (FISH) and polymerase chain reaction (PCR), to map the genetic material in tissues or tumours, which are essential in the management of many cancers.
Find out what a histopathologist does, by hearing from Dr Mark Howard
The role of the histopathologist.
Many histopathologists specialise in specific organs such as the liver or skin, dissecting (‘cutting up’ or ‘trimming’) tissues for viewing under the microscope on a daily basis. For large specimens, such as samples of bowel or breast following surgery, these are dissected to select the most appropriate areas to examine under microscope. Histopathologists write reports on specimens, consult literature (past and current research findings), and many also have teaching and research responsibilities.
They will also attend multi-disciplinary meetings so their findings can be discussed with other clinicians. Treatments are then planned in detail and tailored to each individual patient.
Histopathologists also work directly with patients, for example, they may carry out procedures such as fine needle aspiration in head and neck or breast clinics. They increasingly have key responsibilities for cancer screening, at the moment for breast, bowel and cervical cancer, with other programmes expected in the near future.
Histopathologists also examine cells in smears, aspirates or bodily fluids (cytopathology), for example in urine or cervical smears. Other subspecialties include forensic pathology, neuropathology and paediatric pathology.


Dr Rachel Brown, Histopathologist
At my desk I do some cases at the microscope dictating reports as I go. I usually do some trimming in the morning. My areas of interest are liver/pancreas and head and neck pathology so I might be looking at a liver removed at transplantation or a partial liver resection or pancreatic resection for tumour.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Biopsy Report
What is a biopsy report.
A biopsy report is also known as a histopathology report or a surgical pathology report. For many health problems, a diagnosis is made by removing a piece of tissue for study in the pathology lab. The piece of tissue may be called the sample or specimen. A pathologist looks at the specimen. A pathologist is a doctor who specializes in diagnosing what type of disease is found in tissue samples or specimens taken from your body. The biopsy report describes what the pathologist finds out about the specimen. Biopsy report information may differ somewhat, but all reports contain important details that your healthcare provider needs to diagnose and manage your condition or disease.
What happens to the specimen after the biopsy is done?
After the specimen is removed from the patient, it's put in a container with a special type of liquid to preserve the sample. The pathologist or trained lab assistant reviews the specimen by the naked eye. This means without using a microscope. The pathologist looks at, measures, feels, or takes pictures of the specimen. This type of exam helps the pathologist determine which part of the specimen is the most important. That part will be looked at under a microscope to help diagnose a disease or condition.
Next, the pathologist or a trained lab assistant gets the specimen ready to look at under a microscope. Specimens are processed based on the type of sample sent to the pathology lab. They can be prepared as a histologic section or a smear, as described below.
Histologic sections are very thin slices of the specimen that are stained, placed on a glass slide, and then covered with a thin piece of glass called a coverslip.
Smears are done when the specimen is a liquid or there are small, solid chunks suspended in a liquid. These are "smeared" onto a slide. They are then allowed to dry or are fixed. The fixed smears are stained, covered with a coverslip, and then examined under a microscope
Routine processing and histology can take one day or more. Sometimes information about a tissue sample is needed during surgery to make immediate decisions. A pathology consult can be done during surgery if the surgeon can't wait for routine processing and histology. This is often called a frozen section exam and usually takes 10 to 20 minutes.
What is the purpose of a biopsy?
A biopsy report describes the findings of the specimen. Most reports contain the following information:
Identification and clinical information. This information includes your name, medical record number, date of the procedure, and the unique identifier of the specimen. The clinical information is your medical information and the special request from the healthcare provider who provided the sample.
Gross description. A gross description describes how it looks to the naked eye and where the biopsy was taken from. It may include a description of the color, size, weight, and texture of the specimen.
Microscopic exam. A microscopic exam is a description of what the findings of the slides showed under a microscope. It's usually technical and not in simple language.
Diagnosis. This is usually considered the "bottom line." Although the format varies, often the diagnosis is expressed as: organ or tissue, site from which the biopsy was obtained, type of surgical procedure used to obtain the biopsy, and then diagnosis.
Comment. This section is used by the pathologist to address or clarify concerns of your healthcare provider or to recommend additional tests you may need.
Summary (also called a synoptic report). This section consists of a summary of the pathologist's findings. For example: colon, sigmoid, endoscopic biopsy, tubular adenoma. In other words, you had a biopsy of the sigmoid portion of the colon by endoscopy, and a benign tumor was found.
The name of the pathologist and the name and address of the pathology lab is included in the report.
Find a Doctor
Specializing In:
- Renal Pathology
- Kidney biopsy
- Kidney Cysts
- Cervical Dysplasia
- Biomedical Engineering
- Dermatopathology
- Cutaneous Surgery
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
Find Additional Treatment Centers at:
.png?h=123&iar=0&w=200&hash=434ACD5D3D5A5BC3DC4CE91A7A90C040)
Request an Appointment
.png?h=123&iar=0&mh=260&mw=380&w=200&hash=590CFDA013DBA7BA4BFC7F4E2DE1E0FC)
Prostate Biopsy
Surgical Pathology
Related Topics

Understanding Your Pathology Report
If you have had a biopsy or surgery that removes tissue from your body, in almost all cases a sample will be sent to a pathology lab for examination. Pathologists, who specialize in looking at microscopic tissue samples, will look for signs of disease.
Their findings will be detailed in a pathology report. The first section will contain their overall diagnosis. The rest of the document will provide details.
In the US, a patient will receive the pathology report as soon as the pathologist files it, so you might see it before your physician does. It’s important to know a few things about pathology reports before you look.
Pathologist Stuart Schnitt, MD , has one piece of advice: “If a patient doesn’t understand something in the report, they should talk to their doctor about it. Don’t try consulting the internet. It’s too easy to be misled and jump to conclusions that cause unnecessary anxiety.”
Are there parts of the pathology report that I should look at?
If the pathologist found disease in your tissues, a Final Diagnosis section, typically at the top, will describe the disease.
Please note that the report will provide many details whether there is a diagnosis of cancer or not. The terms used may be technical and difficult to understand without context or expertise.
The best practice is to review your report with your doctor. If you do receive a cancer diagnosis, your doctor will help you understand the important details, such as the origin of the cancer in your body, its size, type, and any biomarkers that can be used to guide the selection of treatments.
Receiving a cancer diagnosis is emotionally difficult. There is a lot of information to take in, and it can be hard to comprehend all at once. If you realize that you didn’t understand everything in your report during the first review, don’t hesitate to ask to review it again. A social worker can also help you through the process.
Learn more about Dana-Farber’s Adult Social Work Program .
Which doctor do I ask about my pathology report?
The most appropriate doctor to talk to varies depending on where you are in the process of diagnosis and treatment.
- If your pathology report details the results of a biopsy to investigate a possible new cancer, the physician who performed your biopsy can help you understand the results.
- If your report provides an analysis after surgery performed to remove cancer, the surgeon who performed the excision can help you understand the results.
- If you have been diagnosed with metastatic cancer and have received a report from a biopsy or removal of metastatic tissue, your medical oncologist will be a good resource.
To avoid confusion, focus on:
- Understanding where you are in the process of diagnosis or treatment.
- Connecting with the right expert who can help you understand your report.
- Making sure you get all your questions answered about your diagnosis and what your care team recommends for next steps.
How do I know if my pathology report is right?
Pathologists often consult with one another to validate their findings before finalizing a report. Large cancer centers like Dana-Farber/Brigham and Women’s Cancer Center will review findings submitted for a second opinion.
“As part of my job, I do consultations on challenging cases from pathologist all around the world,” says Schnitt.
Learn about Dana-Farber’s Second Opinion Program .
How do I learn more about the details in the pathology report?
Pathology reports typically contain the following detailed sections.
Patient and specimen identifiers
This information includes the patient’s name, birth date, and other personal information. It also details clinical history, the type of biopsy or procedure, and the type of tissue being analyzed.
Some surgical procedures generate multiple specimens that are submitted together to the pathologist. For instance, a colonoscopy might generate multiple specimens. Information about each sample will be labelled so that the clinician knows which location each sample came from.
Gross description
The gross description details the size and appearance of the sample on the outside. This section will also include an index of samples prepared by the pathologist for microscopy.
Microscopic description
Each sample is sliced, stained, and mounted on a glass slide for a pathologist to examine under a microscope. For surgical specimens involving cancer, pathologists will create a separate report, called a synoptic report, for each specimen examined.
These reports will include details that can help guide treatment options. Details include:
- Histologic type – The type of cancer based on how the cells and tissues look under the microscope. Histologic types can vary even within a given organ.
- Tumor grade – The grade measures how abnormal the cells look. A higher number means the cells are more abnormal.
- Margins – A negative margin means the resected cancer is completely contained within the surgically removed specimen. A positive margin means that the surgeon couldn’t remove all the cancer. Margins aren’t measured when a sample is a biopsy which is a just small piece of the tumor.
- Mitotic rate – This is a measure of how quickly cells are dividing and may give a sense of how quickly the cancer is growing.
- Invasiveness – Your surgeon may have removed lymph nodes or other tissues for inspection to see if the cancer has spread.
- Biomarkers – For certain forms of cancer, samples are studied in ways that highlight cancer cells that have certain flags. Those flags can indicate if a specific type of targeted medicine or immunotherapy might be effective. Some biomarker readouts are supplied later.
Some details in a pathology report might be alarming. Please work with your care team to understand how they can help guide your treatment. There are many different treatment options and clinical trials to consider, and those details, though scary, could be the key to knowing the best next steps.
For some forms of cancer, your doctor might also order genetic testing of the tumor to understand the mutations driving its growth or germline genetic testing to determine if you have inherited cancer risk genes. The results of these tests can help your care team select the best treatment options.
If you need additional support to help you cope with or understand your results, Dana-Farber has programs such as the Patient Navigator Program and the Adult Social Work Program that can help.
About the Medical Reviewer

Stuart J. Schnitt, M.D. is the Chief of Breast Oncologic Pathology for the Dana-Farber Brigham Cancer Center, Associate Director of the Dana-Farber Cancer Institute/Brigham and Women’s Hospital Breast Oncology Program, co-leader of the Dana-Farber Harvard Cancer Center Breast Program, Senior Pathologist at Brigham and Women’s Hospital, a Professor of Pathology at Harvard Medical School and an internationally recognized expert in breast pathology. Dr. Schnitt did his internship and residency in Anatomic and Clinical Pathology at Beth Israel Hospital in Boston followed by a fellowship in surgical pathology, also at Beth Israel Hospital. He was a faculty member in the Beth Israel Hospital/Beth Israel Deaconess Medical Center Department of Pathology from 1984-2017, including 11 years as Director of Anatomic Pathology and subsequently Vice Chair for Anatomic Pathology. He has published over 340 original articles, review articles, editorials, commentaries, and book chapters, primarily in the area of breast diseases. He has authored a popular breast pathology textbook entitled “Biopsy Interpretation of the Breast”, now its third edition. The first two editions of this book were also published in Chinese. In addition, he is one of the editors of the 4th Edition of the “World Health Organization Classification of Tumours of the Breast”, published in 2012. Dr. Schnitt is a Past President of the United States and Canadian Academy of Pathology (2010-2011). Other notable honors include the Arthur Purdy Stout Society of Surgical Pathologists Annual Prize (1999), the Albany Medical College Distinguished Alumnus award (2014), the Lynn Sage Distinguished Lecturer (2014) and the Maude Abbot Lecture at the United States and Canadian Academy of Pathology Annual Meeting (2016). He is particularly proud to have been involved in the training of 35 breast pathology fellows since 1995. He has lectured extensively around the world. His research interests and contributions to our understanding of benign breast diseases and breast cancer have been broad, but have largely focused on risk factors for local recurrence in patients with invasive breast cancer and ductal carcinoma in situ treated with breast conserving therapy, benign breast disease and breast cancer risk, and stromal-epithelial interactions in breast tumor progression.
1 thought on “Understanding Your Pathology Report”
Nicely done! Thank you!
Comments are closed.

IMAGES
VIDEO
COMMENTS
What Is Histopathology? In clinical practice, histopathology refers to the examination of tissues obtained by biopsy or the surgical removal of an organ. It is a form of anatomical pathology that looks specifically at tissues and organs as opposed to clinical pathology which looks at bodily fluids.
Specifically, in clinical medicine, histopathology refers to the examination of a biopsy or surgical specimen by a pathologist, after the specimen has been processed and histological sections have been placed onto glass slides.
What is Histopathology? Histopathology is the diagnosis and study of diseases of the tissues, and involves examining tissues and/or cells under a microscope. Histopathologists are responsible for making tissue diagnoses and helping clinicians manage a patient’s care.
A biopsy report is also known as a histopathology report or a surgical pathology report. For many health problems, a diagnosis is made by removing a piece of tissue for study in the pathology lab. The piece of tissue may be called the sample or specimen. A pathologist looks at the specimen.
Published: July 17, 2019. Updated: March 11, 2024. Medically Reviewed By: Stuart J. Schnitt, MD. If you have had a biopsy or surgery that removes tissue from your body, in almost all cases a sample will be sent to a pathology lab for examination. Pathologists, who specialize in looking at microscopic tissue samples, will look for signs of disease.