- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

4 Home Remedies for Stomach Flu
What is stomach flu.
- Home Remedies
Medical Treatment
When to seek medical attention, frequently asked questions.
If you’ve ever had the stomach flu, known as gastroenteritis , you’re far from alone. Infection with norovirus , the most common cause, is the second most common illness in the US. Occurring due to infection and inflammation of the intestines and stomach, typical symptoms include fever, diarrhea , abdominal pain, and vomiting.
In most cases, stomach flu resolves without medical management, and there’s no outright cure for it. Ensuring you get rest, staying hydrated, and making dietary changes are among the strategies to help you manage stomach flu. It’s important to understand the symptoms and causes of this common condition as well as what home remedies and medical approaches look like.
Stomach flu symptoms arise due to an inflammation of the tissues of your intestines and stomach (parts of the gastrointestinal tract ). It arises due to infection, most often with the norovirus,a type of viral gastroenteritis. Despite being called "stomach flu," it’s not actually caused by the influenza (flu) virus virus; however, both diseases can be very contagious. As an acute condition, this illness that causes diarrhea generally affects you for a short time and resolves within a week.
At-Risk Groups
Gastroenteritis tends not to be severe in healthy adults, though it can be fatal in infants, people over age 65, and those with weakened immune systems. People who are immunocompromised (have weakened immune systems) include those who have existing health conditions, are taking certain medications that lower their immunity, or undergoing chemotherapy.
The most common symptoms of gastroenteritis are:
- Watery diarrhea
- Cramping and pain in the abdomen
- Vomiting and nausea
- Fever, in some cases
The most significant complication of stomach flu is dehydration as this can become dangerous, or even fatal. In adults, this can cause an array of additional signs, including:
- Dry mouth and thirst
- Less urine than normal
- Dark-colored urine
- Loss of energy, fatigue
- Sagging eyes and cheeks
- No tears when crying
- Reduced skin elasticity , or turgor (skin not returning into position after a pinch)
Parents of infants should also recognize the signs their child is dehydrated. These include:
- Less urine in their diapers
- Extra thirst
- Loss of energy
- Lack of tears
- Sunken cheeks or eyes
- Fussiness and restlessness
Causes of the Stomach Flu
Fundamentally, stomach flu symptoms are the result of inflammation in the gastrointestinal system. This can be caused by viruses (viral gastroenteritis), bacteria, parasites, or chemicals.
Viral Gastroenteritis
Viral forms of stomach flu are highly contagious as the virus spreads through contact with an infected person’s stool or vomit. It can be picked up from direct contact with that person, contaminated food, or after touching a surface and then your mouth without washing your hands.
Most gastroenteritis cases are caused by three viruses, which are:
- Norovirus : By far the most common form of stomach flu is norovirus infection, which causes inflammation of the stomach and intestines. Symptoms set on within 24 to 48 hours of exposure and usually resolve within 24 to 72 hours. It can affect people of all ages.
- Rotavirus : Primarily affecting infants and children under age 5 (though adults also catch milder forms), rotavirus causes vomiting and diarrhea for three to eight days. This type of gastroenteritis is vaccine-preventable .
- Adenovirus : The highly contagious adenovirus causes mild cold and flu symptoms three days after infection; they last up to two weeks. Most at risk are people with weaker immune systems, such as younger children and infants, older people, and those with existing conditions
- Astrovirus : As with some others, being older, a child or infant, or having compromised immunity makes you more likely to become infected with astrovirus . Stomach flu due to astrovirus arises four to five days after infection, resolving within one to four days.
Seasonal Outbreaks
In the United States, most viral gastroenteritis outbreaks are due to norovirus, rotavirus, and astrovirus and occur during the winter months. This is because most spend more time indoors and in close quarters to others when it’s colder, increasing the chances of transmission.
Bacterial Gastroenteritis
Certain bacterial infections can also cause stomach flu, though this type of gastroenteritis is rarer than viral types. The bacteria causing food poisoning grow on foods like meat, fruits, and vegetables, as well as other food; water and liquids can also be contaminated. Primarily, three types of bacteria cause bacterial gastroenteritis:
- Campylobacter
Parasites and Contaminants
Gastroenteritis may also arise due to infection with microorganisms, as in giardiasis . This is an infection of the Giardia duodenalis parasite, often referred to as giardia. Following contact, these microbes reside in the intestines and pass through the feces.
Another parasite that causes gastroenteritis is Cryptosporidium , infections that lead to cryptosporidiosis, commonly known as crypto. Like giardia, this parasite survives in the intestines and spreads via contact with human or animal feces.
Lastly, exposure to certain chemicals and contaminants can cause diarrhea, vomiting, and other gastroenteritis symptoms. As with the others, transmission is often through contaminated food or drink.
Food Poisoning
When what you eat or drink is contaminated with viruses, bacteria, contaminants, or parasites, you contract food poisoning . This is a type of gastroenteritis.
Home Remedies for the Stomach Flu
In most cases, stomach flu resolves on its own, without the need for medications or medical treatments. Healing from the condition primarily means managing the symptoms, getting rest, staying hydrated, and boosting electrolyte intake. Treating gastroenteritis primarily involves dietary restrictions, drinking water, and getting rest.
There’s much you can do to prevent the infections that cause this condition.
Since stomach flu causes nausea and vomiting, eating and getting enough nutrients can be challenging. Making dietary changes is a cornerstone of gastroenteritis treatment.
The BRAT (bananas, rice, applesauce, and toast) diet is designed to ease the symptoms of stomach flu, diarrhea, and nausea. It consists of foods that are low in protein, fiber, and fat, which are easier to digest. These are foods that are bland and easy to chew. There is, however, limited evidence of its efficacy.
It is recommended to choose soft, low residue/low fiber foods, unseasoned lean protein sources (poultry/eggs), tea, broth, and hydration fluid, such as Pedialyte, and avoiding dairy.
It is best to start with a liquid-based diet and work up to more solid foods.
Bouillon or broth
Apple or cranberry juice
Popsicles (ice pops) and hard candies
Saltines or white bread
Toast, plain pasta, or rice
Mashed potatoes
Lean protein (poultry/eggs)
Spicy or fried foods
Caffeinated beverages
Dried peas or beans
Raw or dried fruits and vegetables (bananas are recommended)
Whole grain cereals or breads
Milk and dairy products, like cheeses, butter, etc.
Seeds, nuts, popcorn, and coconut
Drink Water
The primary focus of treatment for gastroenteritis involves ensuring you don’t become dehydrated. Central to management is fluid and electrolyte intake. This may involve:
- Drinking water
- Eating saltine crackers (a source of electrolytes)
- Drinking beverages with electrolytes, such as Gatorade or Pedialyte
- Drinking broth
Additionally, a provider may recommend oral rehydration therapy. This requires drinking a preformulated solution of water, bicarbonate, glucose, and sodium chloride (electrolytes) throughout the day.
One of the most important things your body needs to fight off infection is plenty of rest. Take time off of work, keep your child out of school or daycare if they're infected, and make sure you and your child is getting enough sleep . This will help strengthen the immune system and allow you time to recoup.
Gastroenteritis is highly communicable; the viruses, bacteria, and other pathogens that cause it are often resilient and able to survive on surfaces or foods. Ways to prevent infection include:
- Proper handwashing : Give your hands a thorough cleaning after going to the bathroom and changing diapers; make sure you’ve done so prior to and after handling any food.
- Cleaning surfaces : If surfaces have come into contact with vomit or feces, they need to be fully cleaned and sanitized. Use a solution of 5 to 25 tablespoons of bleach to 1 gallon of hot water. Dirty clothing should be washed at the longest possible cycle with detergent.
- Washing food items : Contaminated foods can be vectors (transmitters) for infections that cause gastroenteritis. Make sure to thoroughly wash fruits and vegetables and cook meats, shellfish, and clams all the way through.
Safe Food Handling
If you’re sick, you can spread gastroenteritis by handling food. Make sure to very thoroughly wash your hands or put on rubber gloves before touching anything you’ll be eating.
In some cases, home management of stomach flu isn’t enough to stop nausea, diarrhea, and other symptoms. You may be prescribed:
- Antibiotics, such as Cipro ( ciprofloxacin ), may help in cases of bacterial gastroenteritis but not if it’s viral or due to a parasite.
- Imodium (loperamide), Pepto-Bismol (bismuth subsalicylate), or Lomotil ( diphenoxylate ) may help with loose stools and diarrhea.
- Daily probiotics , such as Lactobacillus, may also be recommended to aid digestion.
- Over-the-counter (OTC) oral rehydration solutions, such as Pedialyte
- Intravenous (IV) rehydration in cases of severe dehydration
- Rotavirus vaccine, administered to infants at two, four, and sometimes six months
Medicate With Care
If you’re taking prescribed or OTC medications for gastroenteritis, do so with care. Be mindful of your condition and use them only as directed. Let your healthcare provider know if you’re experiencing debilitating side effects or worsening symptoms.
Gastroenteritis symptoms can be especially dangerous for certain populations, prompting a call to your provider. These include:
- Children born prematurely
- Pregnant women
- People with a weakened immune system (due to illness, autoimmune conditions, etc.)
- People undergoing chemotherapy
- People over 65 years old
In addition, if an infant is not drinking or has had diarrhea for two days, you should seek immediate medical attention.
Furthermore, the following symptoms warrant medical help:
- Irritability, lack of energy, or altered mental state
- Diarrhea for more than two days
- Frequent vomiting
- Six or more loose stools (bouts of watery diarrhea) in one day
- Severe pain in the abdomen or rectum (the lowermost part of the intestines)
- Blood and pus in the stool; stool with a black or tarry appearance
- Dehydration symptoms
Stomach flu, or gastroenteritis , is an inflammation of the intestines and stomach that causes diarrhea, vomiting, nausea, and sometimes fever. Symptoms typically resolve within two weeks—often within one to three days—without medical treatment. Gastroenteritis symptoms can cause severe dehydration.
While this condition is often viral in origin, with most cases arising due to norovirus infection, it can also be the result of exposure to bacteria, such as E. coli , parasites like giardia, or chemicals. Stomach flu can be highly contagious. Infants and children, older people, and those with compromised immunity are more likely to develop stomach flu.
The goals of treatment for gastroenteritis are to prevent dehydration, get rest, manage symptoms, and employ a restricted diet. This may involve drinking water or drinks with electrolytes, prioritizing sleep and rest throughout recovery, and taking OTC medications, such as Imodium (loperamide) and probiotics. Signs of dehydration prompt immediate medical attention.
A Word From Verywell
Whether you’re experiencing the symptoms of stomach flu or your child or loved one, it’s important to take the condition seriously. As you go through home management by rehydrating, treating symptoms, resting, and following a restricted diet, remember to be vigilant. A careful and deliberate approach—one that’s informed and focused—will go a long way in ensuring a successful recovery.
If you’re concerned about stomach flu symptoms or are seeing signs of dehydration, don’t hesitate to call your healthcare provider or even emergency medical help.
Many types of stomach flu, or gastroenteritis, are highly contagious. The amount of time that you’re contagious depends on the specific virus or other pathogens that are causing the symptoms.
For norovirus—the most common type—you’re usually contagious anywhere from two days to two weeks after symptoms have resolved.
People with rotavirus are contagious before you feel sick, about one to two days as well as up to two weeks after recovery.
The duration of stomach flu symptoms, or gastroenteritis, depends on the underlying viral, bacterial, or parasitic infection. Most recover without medical help anywhere from a couple of days to two weeks.
With norovirus infection—the most common type—symptoms arise within two days of exposure, and last 24 to 72 hours.
Rotavirus tends to last longer, anywhere from three to eight days, and adenovirus can last up to two weeks.
To manage the diarrhea and vomiting associated with stomach flu, it’s often recommended that you stick to a restricted diet focused on bland and soft foods. Generally, you should be able to start reincorporating fruits and vegetables and getting back to normal as your symptoms subside.
Most cases of stomach flu resolve within two to three days.
National Institutes of Health. Definition & facts for viral gastroenteritis (“stomach flu”) . U.S. Department of Health and Human Services.
National Institutes of Health. Viral gastroenteritis (“stomach flu”) . U.S. Department of Health and Human Services.
Centers for Disease Control and Prevention. About norovirus .
Centers for Disease Control and Prevention. Rotavirus clinical information .
Jeong HS, Jeong A, Cheon DS. Epidemiology of astrovirus infection in children . Korean J Pediatr . 2012;55(3):77–82. doi:10.3345/kjp.2012.55.3.77
Johns Hopkins Medicine. Bacterial gastroenteritis .
Centers for Disease Control and Prevention. Giardia: General information .
Centers for Disease Control and Prevention. Parasites: Cryptosporidium (also known as “Crypto”) .
Centers for Disease Control and Prevention. Treatment of viral gastroenteritis (“stomach flu”) .
Barr W, Smith A. Acute diarrhea in adults . Am Fam Physician. 2014;89(3):180-189.
Brown University Health Services. Viral gastroenteritis .
Graves N. Acute Gastroenteritis . Prim Care . 2013;40(3):727-741. doi:10.1016/j.pop.2013.05.006
National Institutes of Health. Definition & facts for viral gastroenteritis (“stomach flu”) .
By Mark Gurarie Gurarie is a freelance writer and editor. He is a writing composition adjunct lecturer at George Washington University.
Viral gastroenteritis (stomach flu)
On this page, when to see a doctor, risk factors, complications.
Viral gastroenteritis is an intestinal infection that includes signs and symptoms such as watery diarrhea, stomach cramps, nausea or vomiting, and sometimes fever.
The most common way to develop viral gastroenteritis — often called stomach flu — is through contact with an infected person or by consuming contaminated food or water. If you're otherwise healthy, you'll likely recover without complications. But for infants, older adults and people with compromised immune systems, viral gastroenteritis can be deadly.
There's no effective treatment for viral gastroenteritis, so prevention is key. Avoid food and water that may be contaminated and wash your hands thoroughly and often.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Although it's commonly called stomach flu, gastroenteritis isn't the same as influenza. The flu (influenza) affects only your respiratory system — your nose, throat and lungs. Gastroenteritis, on the other hand, attacks your intestines, causing signs and symptoms such as:
- Watery, usually nonbloody diarrhea — bloody diarrhea usually means you have a different, more severe infection
- Nausea, vomiting or both
- Stomach cramps and pain
- Occasional muscle aches or headache
- Low-grade fever
Depending on the cause, viral gastroenteritis symptoms may appear within 1-3 days after you're infected and can range from mild to severe. Symptoms usually last just a day or two, but occasionally they may last up to 14 days.
Because the symptoms are similar, it's easy to confuse viral diarrhea with diarrhea caused by bacteria, such as Clostridioides difficile, salmonella and Escherichia coli, or parasites, such as giardia.

- Viral gastroenteritis
The stomach, small intestine and large intestine (colon) are part of your digestive tract, which processes the foods you eat. Viral gastroenteritis is an inflammation of these organs caused by a virus.
If you're an adult, call your health care provider if:
- You're not able to keep liquids down for 24 hours
- You've been vomiting or having diarrhea for more than two days
- You're vomiting blood
- You're dehydrated — signs of dehydration include excessive thirst, dry mouth, deep yellow urine or little or no urine, and severe weakness, dizziness or lightheadedness
- You notice blood in your bowel movements
- You have severe stomach pain
- You have a fever above 104 F (40 C)
For infants and children
See your child's health care provider right away if your child:
- Has a fever of 102 F (38.9 C) or higher
- Seems tired or very irritable
- Is in a lot of discomfort or pain
- Has bloody diarrhea
- Seems dehydrated — watch for signs of dehydration in sick infants and children by comparing how much they drink and urinate with how much is normal for them, and watching for signs such as a dry mouth, thirst and crying without tears
If you have an infant, remember that while spitting up may be an everyday occurrence for your baby, vomiting is not. Babies vomit for a variety of reasons, many of which may require medical attention.
Call your baby's doctor right away if your baby:
- Has vomiting that is frequent
- Hasn't had a wet diaper in six hours
- Has bloody stools or severe diarrhea
- Has a sunken soft spot (fontanel) on the top of his or her head
- Has a dry mouth or cries without tears
- Is unusually sleepy, drowsy or unresponsive
From Mayo Clinic to your inbox
You're most likely to get viral gastroenteritis when you eat or drink contaminated food or water. You may also be likely to get gastroenteritis if you share utensils, towels or food with someone who has one of the viruses that cause the condition.
Many viruses can cause gastroenteritis, including:
Noroviruses. Both children and adults are affected by noroviruses, the most common cause of foodborne illness worldwide. Norovirus infection can sweep through families and communities. It's especially likely to spread among people in confined spaces.
In most cases, you pick up the virus from contaminated food or water. But it can also spread between people who are in close contact or who share food. You can also get the virus by touching a surface that's been contaminated with norovirus and then touching your mouth.
Rotavirus. Worldwide, this is the most common cause of viral gastroenteritis in children, who are usually infected when they put their fingers or other objects contaminated with the virus into their mouths. It can also spread through contaminated food. The infection is most severe in infants and young children.
Adults infected with rotavirus may not have symptoms, but can still spread the illness. This is of particular concern in institutional settings such as nursing homes because adults with the virus unknowingly can pass the virus to others. A vaccine against viral gastroenteritis is available in some countries, including the United States, and appears to be effective in preventing the infection.
Some shellfish, especially raw or undercooked oysters, also can make you sick. Contaminated drinking water is a cause of viral diarrhea. But in many cases the virus is passed when someone with a virus handles food you eat without washing his or her hands after using the toilet.
Gastroenteritis occurs all over the world and can affect people of all ages.
People who may be more susceptible to gastroenteritis include:
- Young children. Children in child care centers or elementary schools may be especially vulnerable because it takes time for a child's immune system to mature.
- Older adults. Adult immune systems tend to become less efficient later in life. Older adults in nursing homes are vulnerable because their immune systems weaken. They also live in close contact with others who may pass along germs.
- Schoolchildren or dormitory residents. Anywhere that groups of people come together in close quarters can be an environment for an intestinal infection to get passed.
- Anyone with a weakened immune system. If your resistance to infection is low — for instance, if your immune system is compromised by HIV/AIDS, chemotherapy or another medical condition — you may be especially at risk.
Each gastrointestinal virus has a season when it's most active. If you live in the Northern Hemisphere, for instance, you're more likely to have rotavirus or norovirus infections in the winter and spring.
The main complication of viral gastroenteritis is dehydration — a severe loss of water and essential salts and minerals. If you're healthy and drink enough to replace fluids you lose from vomiting and diarrhea, dehydration shouldn't be a problem.
Infants, older adults and people with weakened immune systems may become severely dehydrated when they lose more fluids than they can replace. Hospitalization might be needed so that lost fluids can be replaced through an IV in their arms. Dehydration can rarely lead to death.
The best way to prevent the spread of intestinal infections is to follow these precautions:
- Get your child vaccinated. A vaccine against gastroenteritis caused by the rotavirus is available in some countries, including the United States. Given to children in the first year of life, the vaccine appears to be effective in preventing severe symptoms of this illness.
Wash your hands thoroughly. And make sure your children do, too. If your children are older, teach them to wash their hands, especially after using the toilet.
Wash your hands after changing diapers and before preparing or eating food, too. It's best to use warm water and soap and to rub hands well for at least 20 seconds. Wash around cuticles, beneath fingernails and in the creases of the hands. Then rinse thoroughly. Carry sanitizing wipes and hand sanitizer for times when soap and water aren't available.
- Use separate personal items around your home. Avoid sharing eating utensils, drinking glasses and plates. Use separate towels in the bathroom.
- Prepare food safely. Wash all your fruits and vegetables before eating them. Clean kitchen surfaces before preparing food on them. Avoid preparing food if you're sick.
- Keep your distance. Avoid close contact with anyone who has the virus, if possible.
- Disinfect hard surfaces. If someone in your home has viral gastroenteritis, disinfect hard surfaces, such as counters, faucets and doorknobs, with a mixture of 5-25 tablespoons (73 to 369 milliliters) of household bleach to 1 gallon (3.8 liters) of water.
- Avoid touching laundry that may have been exposed to a virus. If someone in your home has viral gastroenteritis, wear gloves while touching laundry. Wash clothing and bedding in hot water and dry them on the hottest setting. Wash your hands well after touching laundry.
- Check out your child care center. Make sure the center has separate rooms for changing diapers and preparing or serving food. The room with the diaper-changing table should have a sink as well as a sanitary way to dispose of diapers.
Take precautions when traveling
When you're traveling in other countries, you can become sick from contaminated food or water. You may be able to reduce your risk by following these tips:
- Drink only well-sealed bottled or carbonated water.
- Avoid ice cubes because they may be made from contaminated water.
- Use bottled water to brush your teeth.
- Avoid raw food — including peeled fruits, raw vegetables and salads — that has been touched by human hands.
- Avoid undercooked meat and fish.
More Information
- Flu shot: Will it prevent the stomach flu?
- Stomach flu: How long am I contagious?
Jan 18, 2022
- Alexandraki I, et al. Acute viral gastroenteritis in adults. https://www.uptodate.com/contents/search. Accessed Aug. 16, 2021.
- Norovirus. Centers for Disease Control and Prevention. https://www.cdc.gov/norovirus/. Accessed Aug. 16, 2021.
- Rotavirus. Centers for Disease Control and Prevention. https://www.cdc.gov/rotavirus/index.html. Aug. 16, 2021.
- Viral gastroenteritis ("stomach flu"). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/viral-gastroenteritis/definition-facts. Accessed Aug. 16, 2021.
- O'Ryan MG. Acute viral gastroenteritis in children in resource-rich countries: Management and prevention. https://www.uptodate.com/contents/search. Accessed Aug. 16, 2021.
- Choose safe food and drinks when traveling. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/food-water-safety. Accessed Aug. 16, 2021.
- Diseases & Conditions
- Viral gastroenteritis (stomach flu) symptoms & causes
News from Mayo Clinic

CON-XXXXXXXX
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Search the site GO Please fill out this field.
- Newsletters
- Health Conditions A-Z
- Digestive Disorders
7 Effective Stomach Flu Remedies
Several at-home remedies may help quickly alleviate your unpleasant symptoms.
:max_bytes(150000):strip_icc():format(webp)/MaxineLipnerheadshot-MaxineLipner-12a4b5b02d154e2394160631b5b94630.jpeg)
1. Drink Fluids
2. follow a brat diet, 3. avoid certain foods, 4. get adequate rest, 5. try medications, 6. take probiotics, 7. experiment with acupressure.
- Causes and Prevention of the Stomach Flu
When To Contact a Healthcare Provider
A quick review, frequently asked questions.
Gastroenteritis, commonly known as the " stomach flu ," is a highly contagious illness that causes unpleasant symptoms like diarrhea, cramps, fever, nausea, and vomiting. People with the stomach flu typically recover on their own with remedies like eating bland foods, getting plenty of rest, and staying hydrated.
Some evidence suggests that probiotics help get rid of stomach flu symptoms, like diarrhea, quicker than other remedies. More research is needed to know the effects of probiotics on stomach flu symptoms.
Read on to learn how to ease your symptoms and improve your chances of quickly recovering if you have the stomach flu.
Prostock-Studio / Getty Images
Focus on getting plenty of fluids to avoid dehydration if you have the stomach flu. Dehydration can be a concern if you cannot replenish fluids and electrolytes, like potassium and sodium. Severe dehydration from the stomach flu is most common in infants, children, older adults, and people with weak immune systems.
Adults with the stomach flu can replenish lost fluids by consuming liquids like:
- Sports drinks with electrolytes
Children, people with severe diarrhea and vomiting, and older adults with weak immune systems may require a rehydration solution containing electrolytes and glucose (sugar). Rehydration solutions include CeraLyte and Pedialyte.
Food may seem unappealing if you have the stomach flu, but replenishing your body with nutrients is essential. Fueling your body with certain foods may improve stomach flu symptoms. Bland foods, like those in the BRAT diet, are easy on your digestive system and may treat diarrhea by firming up loose stools.
The BRAT diet includes:
Other bland foods that may quell nausea if you have the stomach flu include clear broths or soups and oatmeal. Eating salty, easy-to-digest foods like saltine crackers can also help replace lost electrolytes like sodium and give you a bit of energy.
Research has found that following the BRAT diet for long periods may be unsafe. Eating bland foods for one or two days while treating your symptoms is probably OK. Make sure you gradually reintroduce a balanced diet of carbs, healthy fats, and lean proteins once you start feeling better.
Some foods may worsen stomach flu symptoms. For example, the bland diet advises against fried, high-fiber, spicy, and raw foods. Alcoholic and caffeinated beverages, including coffee, soft drinks, and tea, may also aggravate your symptoms.
Other foods that you might avoid until your symptoms resolve:
- Cured or smoked tough meats
- Dairy products containing lactose, a sugar
- Dried fruits
- Fermented foods (e.g., pickles and sauerkraut)
- High-fat foods (e.g., fast foods, fried foods, and pizza)
- High-fiber vegetables (e.g., broccoli, cabbage, and corn)
- Nuts and seeds
- Raw vegetables
- Sugary foods
- Whole grains, which often have a lot of fiber
Stomach flu symptoms generally resolve on their own with plenty of rest. Sleep supports your immune system by helping get rid of bacteria and reducing inflammation. In contrast, poor sleep may increase inflammation and worsen infectious illnesses like stomach flu.
Over-the-counter medications (OTC), including Imodium (loperamide) and Pepto-Bismol (bismuth subsalicylate), may help alleviate diarrhea. Do not give those medications to children or use them if you have blood diarrhea or a fever.
Imodium helps treat diarrhea by slowing gut movement. You may develop mild side effects, such as constipation and fatigue. Imodium may cause severe side effects like changes in heart rhythm, which can be life-threatening.
Do not take Imodium without consulting a healthcare provider if you have:
- An irregular or slow heartbeat
- Issue with fainting
- Low potassium levels
Do not use Imodium if you take amiodarone, which treats irregular heart rhythms, or methadone, an opioid. Imodium may adversely interact with those medications. Imodium may also be unsafe for children younger than 2.
Pepto-Bismol
Pepto-Bismol typically treats digestive symptoms like heartburn and indigestion. Pepto-Bismol may treat mild diarrhea symptoms by reducing the severity of gas and nausea.
Pepto-Bismol alleviates diarrhea by:
- Boosting electrolyte and fluid reabsorption
- Decreasing inflammation in your gut
- Preventing bacteria from binding and growing on the walls of your stomach
- Reducing intestinal secretion
Pepto-Bismol is safe for most people if used correctly. Some people may develop minor side effects like black poop or nausea, which usually goes away once you stop taking the medication.
Do not take Pepto-Bismol if you are pregnant or breastfeeding, have an allergy to the ingredients, or have diabetes or gout. Speak with a healthcare provider if you are unsure whether Pepto-Bismol is safe for you and before giving it to children.
A healthcare provider may advise taking probiotics to treat the stomach flu. Probiotics are live microbes in your gut and certain foods. Some probiotic supplements help ease stomach flu-related symptoms like diarrhea.
Some evidence suggests that probiotic supplements help shorten the duration of diarrhea. Probiotics that may help treat the stomach flu include Bifidobacterium infantis and Lactobacillus rhamnosus .
Note that the Food and Drug Administration does not evaluate the efficacy of supplements before they are on the market. Talk to a healthcare provider before starting a new supplement.
Acupressure is a type of complementary and alternative medicine in which you apply pressure to different body parts to alleviate symptoms. According to ancient Chinese medicine, acupressure helps intercede pain messages that your nerve cells send to your brain.
For example, you might alleviate nausea by pressing your middle and index fingers to the inside of your wrist, near your palm. A study published in 2022 looked at 90 women with hyperemesis gravidarum, or severe nausea and vomiting during pregnancy, split into acupressure and control groups. The acupressure group wore a wristband that applied pressure to their inner wrists.
The study found that the acupressure had significantly decreased nausea and vomiting. You can purchase similar wristbands to help apply pressure to your inner wrist and possibly decrease nausea.
Causes and Prevention of the Stomach Flu
Viruses most commonly cause the stomach flu. Despite the name, influenza viruses do not cause the stomach flu. Instead, norovirus is the most common cause of the stomach flu. Other viruses that cause the stomach flu include adenovirus, astrovirus, and rotavirus, which are more common in children than adults. Some bacteria, chemicals, and parasites may also cause symptoms.
The viruses may spread through contact with infected stool or vomit. An infected person may spread viral particles by preparing drinks and foods, shaking hands, and touching objects without washing their hands.
You may contract stomach flu viruses by consuming food or drinks made with contaminated water. Bacteria, chemicals, or parasites may infect food and cause food poisoning , a type of gastroenteritis. Swimming in contaminated water may increase your risk of the stomach flu.
The stomach flu is highly contagious and not always preventable, but you can significantly lower your risk by:
- Cleaning commonly touched objects and surfaces
- Getting vaccinated (i.e., some vaccines protect infants against rotavirus)
- Properly washing your hands
- Safely preparing food
Most cases of the stomach flu resolve on their own within a few days. In contrast, you or someone you are caring for may require medical attention for dehydration or severe symptoms.
Consult a healthcare provider right away if you have:
- Black, tar-like stool that contains blood or pus
- Changes in your mental state
- Diarrhea that lasts two days or longer
- Frequent vomiting that does not improve or worsens
- A high fever
- Loose stools more than six times per day
- Severe abdominal or rectal pain
- Signs of dehydration (e.g., fainting, feeling dizzy, and rapid heart rate)
Older adults, pregnant people, and those with weak immune systems may see a healthcare provider if they develop stomach flu symptoms to prevent severe illness.
Seek immediate medical attention if an infant or young child with the stomach flu develops signs of dehydration, such as becoming irritable, crying without tears, and having no wet diapers for three hours or longer.
You can help reduce stomach flu symptoms at home by eating bland foods, getting plenty of rest, and taking medications like Imodium or Pepto-Bismol. Make sure that you replace lost electrolytes and fluids by staying hydrated.
Most people recover from the stomach flu within one to two days, but some may develop severe symptoms. Contact a healthcare provider if you have a high fever, develop severe diarrhea and vomiting, or show signs of dehydration. Avoid making or sharing food with others for at least two days after your symptoms resolve to avoid spreading the stomach flu.
How long the stomach flu lasts may depend on the virus that causes it:
- Adenovirus: One to two weeks
- Astrovirus: One to four days
- Norovirus: One to three days
- Rotavirus: Three to eight days
Bacterial gastroenteritis may resolve within a few days with at-home treatments. Parasitic gastroenteritis may last as long as two weeks and require medical attention.
The stomach flu is contagious for as long as you have symptoms and for some time before and after you are no longer sick. Norovirus, the most common cause of the stomach flu, may persist in stool before you develop symptoms and for two weeks after.
National Institute of Diabetes and Digestive and Kidney Diseases. Definition and facts for viral gastroenteritis ("stomach flu") .
Can probiotics help against diarrhea? Institute for Quality and Efficiency in Health Care (IQWiG); 2019.
Kluijfhout S, Trieu TV, Vandenplas Y. Efficacy of the probiotic probiotical confirmed in acute gastroenteritis . Pediatr Gastroenterol Hepatol Nutr . 2020;23(5):464-471. doi:10.5223/pghn.2020.23.5.464
MedlinePlus. Gastroenteritis .
National Institute of Diabetes and Digestive and Kidney Diseases. Treatment of viral gastroenteritis ("stomach flu") .
National Institute of Diabetes and Digestive and Kidney Diseases. Eating, diet, & nutrition for viral gastroenteritis ("stomach flu") .
Nemeth V, Pfleghaar N. Diarrhea . In: StatPearls . StatPearls Publishing; 2023.
Carson RA, Mudd SS, Madati PJ. Clinical practice guideline for the treatment of pediatric acute gastroenteritis in the outpatient setting . J Pediatr Health Care . 2016;30(6):610-616. doi:10.1016/j.pedhc.2016.04.012
MedlinePlus. Bland diet .
Garbarino S, Lanteri P, Bragazzi NL, et al. Role of sleep deprivation in immune-related disease risk and outcomes . Commun Biol . 2021;4(1):1304. doi:10.1038/s42003-021-02825-4
MedlinePlus. Loperamide .
MedlinePlus. Bismuth subsalicyclate .
Ansari F, Pashazadeh F, Nourollahi E, et al. A systematic review and meta-analysis: The effectiveness of probiotics for viral gastroenteritis . Curr Pharm Biotechnol . 2020;21(11):1042-1051. doi:10.2174/1389201021666200416123931
Kluijfhout S, Trieu TV, Vandenplas Y. Efficacy of the probiotic Probiotical confirmed in acute gastroenteritis . Pediatr Gastroenterol Hepatol Nutr . 2020;23(5):464-471. doi:10.5223/pghn.2020.23.5.464
Office of Dietary Supplements. Dietary supplements: What you need to know - consumer .
MedlinePlus. Nausea and acupressure .
Khanijow V, Prakash P, Emsellem HA, et al. Sleep dysfunction and gastrointestinal diseases . Gastroenterol Hepatol (N Y) . 2015;11(12):817-825.
National Institute of Diabetes and Digestive and Kidney Diseases. Symptoms & causes of viral gastroenteritis ("stomach flu") .
American Academy of Family Physicians. Dehydration .
MedlinePlus. Dehydration .
MedlinePlus. Bacterial gastroenteritis .
Halliez MC, Buret AG. Gastrointestinal parasites and the neural control of gut functions . Front Cell Neurosci . 2015;9:452. doi:10.3389/fncel.2015.00452
Related Articles
- Português Br
- Journalist Pass
Home Remedies: Struggling with stomach flu
Dana Sparks
Share this:

What some people commonly refer to as stomach flu is also known as viral gastroenteritis . It's an intestinal infection marked by watery diarrhea, abdominal cramps, nausea or vomiting, and sometimes fever.
The most common way to develop viral gastroenteritis is through contact with an infected person or by ingesting contaminated food or water. If you're otherwise healthy, you'll likely recover without complications. But for infants, older adults and people with compromised immune systems, viral gastroenteritis can be deadly.
Symptoms include:
- Watery, usually nonbloody diarrhea — bloody diarrhea usually means you have a different, more severe infection
- Abdominal cramps and pain
- Nausea, vomiting or both
- Occasional muscle aches or headache
- Low-grade fever
There's no effective treatment for viral gastroenteritis, so prevention is key. In addition to avoiding food and water that may be contaminated, thorough and frequent hand-washing can be your best defense. If you get the stomach flu, staying hydrated is extremely important.
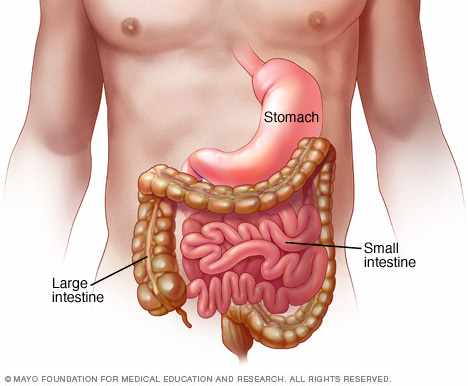
The stomach, small intestine and large intestine (colon) are part of your digestive tract, which processes foods you eat. Viral gastroenteritis is an inflammation of these organs caused by a virus.
To help keep yourself more comfortable and prevent dehydration while you recover, try the following:
- Let your stomach settle. Stop eating solid foods for a few hours.
- Try sucking on ice chips or taking small sips of water. You might also try drinking clear soda, clear broths or noncaffeinated sports drinks. Drink plenty of liquid every day, taking small, frequent sips.
- Ease back into eating. Gradually begin to eat bland, easy-to-digest foods, such as soda crackers, toast, gelatin, bananas, rice and chicken. Stop eating if your nausea returns.
- Avoid certain foods and substances until you feel better. These include dairy products, caffeine, alcohol, nicotine, and fatty or highly seasoned foods.
- Get plenty of rest. The illness and dehydration may have made you weak and tired.
- Be cautious with medications. Use many medications, such as ibuprofen (Advil, Motrin IB, others), sparingly if at all. They can make your stomach more upset. Use acetaminophen (Tylenol, others) cautiously; it sometimes can cause liver toxicity, especially in children. Don't give aspirin to children or teens because of the risk of Reye's syndrome, a rare, but potentially fatal disease. Before choosing a pain reliever or fever reducer discuss with your child's pediatrician.
For infants and children
When your child has an intestinal infection, the most important goal is to replace lost fluids and salts. These suggestions may help:
- Help your child rehydrate. Give your child an oral rehydration solution, available at pharmacies without a prescription. Talk to your doctor if you have questions about how to use it. Don't give your child plain water — in children with gastroenteritis, water isn't absorbed well and won't adequately replace lost electrolytes. Avoid giving your child apple juice for rehydration — it can make diarrhea worse.
- Get your child back to a normal diet slowly. Gradually introduce bland, easy-to-digest foods, such as toast, rice, bananas and potatoes.
- Avoid certain foods. Don't give your child dairy products or sugary foods, such as ice cream, sodas and candy. These can make diarrhea worse.
- Make sure your child gets plenty of rest. The illness and dehydration may have made your child weak and tired.
- Avoid giving your child over-the-counter anti-diarrheal medications, unless advised by your doctor. They can make it harder for your child's body to eliminate the virus.
If you have a sick infant, let your baby's stomach rest for 15 to 20 minutes after vomiting or a bout of diarrhea, then offer small amounts of liquid. If you're breast-feeding, let your baby nurse. If your baby is bottle-fed, offer a small amount of an oral rehydration solution or regular formula. Don't dilute your baby's already-prepared formula.
The Mayo Clinic Book of Home Remedies provides answers you need to take care of common health problems on your own. This reference covers 120 of today’s common health problems in an easy-to-follow, A-to-Z format. Learn what you can do for yourself and when to seek medical attention.
- Mayo Clinic Minutes of 2016: A few of our favorite things Paired Kidney Donation Offers a Unique Way Forward for Transplant Recipient
Related Articles

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Entire Site
- Research & Funding
- Health Information
- About NIDDK
- Digestive Diseases
- Viral Gastroenteritis (“Stomach Flu”)
- Español
Treatment of Viral Gastroenteritis (“Stomach Flu”)
How can i treat viral gastroenteritis.
In most cases, people with viral gastroenteritis get better on their own without medical treatment. You can treat viral gastroenteritis by replacing lost fluids and electrolytes to prevent dehydration . In some cases, over-the-counter medicines may help relieve your symptoms.
Research shows that following a restricted diet does not help treat viral gastroenteritis. When you have viral gastroenteritis, you may vomit after you eat or lose your appetite for a short time. When your appetite returns, you can most often go back to eating your normal diet, even if you still have diarrhea . Find tips on what to eat when you have viral gastroenteritis .
If your child has symptoms of viral gastroenteritis, such as vomiting or diarrhea, don’t hesitate to call a doctor for advice.
Replace lost fluids and electrolytes
When you have viral gastroenteritis, you need to replace lost fluids and electrolytes to prevent dehydration or treat mild dehydration. You should drink plenty of liquids. If vomiting is a problem, try sipping small amounts of clear liquids.
Most adults with viral gastroenteritis can replace fluids and electrolytes with liquids such as
- fruit juices
- sports drinks
Eating saltine crackers can also help replace electrolytes.
If your child has viral gastroenteritis, you should give your child an oral rehydration solution—such as Pedialyte, Naturalyte, Infalyte, and CeraLyte—as directed to replace lost fluids and electrolytes. Oral rehydration solutions are liquids that contain glucose and electrolytes. Talk with a doctor about giving these solutions to your infant. Infants should drink breast milk or formula as usual.
Older adults, adults with a weakened immune system , and adults with severe diarrhea or symptoms of dehydration should also drink oral rehydration solutions.
Over-the-counter medicines
In some cases, adults can take over-the-counter medicines such as loperamide (Imodium) and bismuth subsalicylate (Pepto-Bismol, Kaopectate) to treat diarrhea caused by viral gastroenteritis.
These medicines can be unsafe for infants and children. Talk with a doctor before giving your child an over-the-counter medicine.
If you have bloody diarrhea or fever—signs of infections with bacteria or parasites —don’t use over-the-counter medicines to treat diarrhea. See a doctor for treatment.
How do doctors treat viral gastroenteritis?
Your doctor may prescribe medicine to control severe vomiting. Doctors don’t prescribe antibiotics to treat viral gastroenteritis. Antibiotics don’t work for viral infections.
In some cases, your doctor may recommend probiotics . Probiotics are live microbes, most often bacteria, that are like the ones you normally have in your digestive tract . Studies suggest that some probiotics may help shorten a case of diarrhea. Researchers are still studying the use of probiotics to treat viral gastroenteritis. For safety reasons, talk with your doctor before using probiotics or any other complementary or alternative medicines or practices .
Anyone with signs or symptoms of dehydration should see a doctor right away. Doctors may need to treat people with severe dehydration in a hospital.
How can I prevent viral gastroenteritis?
You can take several steps to keep from getting or spreading infections that cause viral gastroenteritis. Wash your hands thoroughly with soap and water
- after using the bathroom
- after changing diapers
- before and after handling, preparing, or eating food
You can clean surfaces that may have come into contact with infected stool or vomit, such as countertops and changing tables, with a mixture of 5 to 25 tablespoons of household bleach and 1 gallon of water. 7 If clothes or linens may have come into contact with an infected person’s stool or vomit, you should wash them with detergent for the longest cycle available and machine dry them. To protect yourself from infection, wear rubber gloves while handling the soiled laundry and wash your hands afterward. 7
If you have viral gastroenteritis, avoid handling and preparing food for others while you are sick and for 2 days after your symptoms stop. 7 People who have viral gastroenteritis may spread the virus to any food they handle, especially if they do not thoroughly wash their hands. Contaminated water may also spread a virus to foods before they are harvested. For example, contaminated fruits, vegetables, and oysters have been linked to norovirus outbreaks. Wash fruits and vegetables before using them, and thoroughly cook oysters and other shellfish. 7 Find tips to help keep food safe .
The flu vaccine does not protect against viral gastroenteritis. Although some people call viral gastroenteritis “stomach flu,” influenza (flu) viruses do not cause viral gastroenteritis. However, rotavirus vaccines can prevent viral gastroenteritis caused by rotavirus.
Rotavirus Vaccines
Two vaccines, which infants receive by mouth, are approved to protect against rotavirus infections 8
- RotaTeq: Infants receive three doses, at ages 2 months, 4 months, and 6 months
- Rotarix: Infants receive this vaccine in two doses, at ages 2 months and 4 months
For the rotavirus vaccine to be most effective, infants should receive the first dose by 15 weeks of age. Infants should receive all doses by 8 months of age.
If you have a baby, talk with your baby’s doctor about rotavirus vaccination .
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.

Set My Location
Providing your location allows us to show you nearby providers and locations.
Have the Stomach Flu? 4 Ways to Treat Symptoms at Home
There’s almost nothing worse than being bent over a toilet throwing up. And, sadly, it can be hard to know what caused you to be there in the first place. Kelli Miller, ANP, UnityPoint Health, lists the symptoms of the stomach flu and how long it lasts, plus ways to feel better, so you can get out of the bathroom and get back to normal.
Stomach Flu Symptoms
Miller says it’s easy to get confused about the difference between influenza, or “the flu,” and gastroenteritis, better known as “the stomach flu.” The stomach flu is caused by a number of viruses, mainly norovirus, which accounts for more than 50 percent of all cases, and others, like rotavirus. Bacteria, such salmonella and E. coli, can also be to blame. Getting the flu shot does not prevent you from getting the stomach flu, but it does prevent you from getting influenza. “Stomach flu symptoms include stomach pain, nausea, vomiting and diarrhea,” Miller says. “A low-grade fever, chills and muscle aches aren’t uncommon to experience as well. Symptoms can start as little as 12 hours after exposure.” These symptoms can last anywhere from one to 14 days, and unfortunately, the stomach flu is extremely contagious. “The stomach flu is spread by the fecal-oral route, which means the viruses from infected feces or vomit find their way into our mouths from either touching a contaminated surface and then touching your face or eating/drinking contaminated foods and/or water. Compared to other viruses, noroviruses can live for days on household surfaces, which is why they spread easily,” Miller says.
- Influenza - Primary symptoms can include fever, chills, cough, congestion and fatigue. Influenza symptoms typically appear suddenly and last between 2-10 days. Prevention includes getting an annual flu shot .
- Stomach flu - Primary symptoms can include stomach pain, nausea, vomiting and diarrhea. Stomach flu symptoms can appear in as little as 12 hours after exposure and last 1-14 days. Prevention includes washing your hands with soap and water.
- 24-hour flu - Primary symptoms can include stomach pain, nausea, vomiting and diarrhea. 24-hour flu symptoms last only between 12-60 hours total. Prevention includes washing your hands with soap and water.
- Food poisoning - Primary symptoms can include stomach pain, nausea, vomiting and diarrhea. Food poisoning symptoms begin within a few hours of eating. Prevention includes preparing food safely and not eating expired items.
Stomach Flu vs. Food Poisoning
Miller says the clinical symptoms of the stomach flu and food poisoning overlap quite a bit, as you can have vomiting, diarrhea, abdominal discomfort and fever with either one. She says the easiest way to determine the cause of your discomfort is to look back at your recent history. “If your symptoms are caused by food poisoning, they tend to occur within hours after eating something. If you can recall eating something questionable, or if others who ate the same thing as you and have similar symptoms, you probably have food poisoning. If you are the only one who got sick, you more than likely picked up a viral illness,” Miller says.
Stomach Flu vs. COVID-19
To make matters even more confusing, some people with COVID-19 (about 20% according to studies ) experience stomach issues including nausea, vomiting and/or diarrhea. Most people with those symptoms usually report developing them in the first couple of days and then go on to experience other respiratory or cold-like symptoms like fever, headache, cough and fatigue.
If you experience nausea, vomiting and/or diarrhea, keep an eye out for other symptoms that may follow. If you notice a progression in the illness, talk with your doctor about getting tested for COVID-19 . Remember, if you’re feeling sick, stay home and continue to wash your hands frequently.
How to Treat the Stomach Flu at Home
Miller says there's often no specific medical treatment for viral gastroenteritis. Antibiotics aren't effective against viruses and overusing them can contribute to the development of antibiotic-resistant strains of bacteria. She recommends treating the stomach flu with the following self-care steps:
- Keep drinking the right fluids. You’ll need to drink enough fluids to prevent dehydration. In addition to water, older children and adults can drink sports drinks, like Gatorade, Power Aid, while babies and young children can have an oral rehydration solution, such as Pedialyte. If your child is vomiting, you can try to give your child a few teaspoons of fluid every few minutes. Babies who breastfeed can continue to breastfeed. But, you should avoid drinks with increased sugar content, such as juices or sodas, which can make diarrhea worse.
- Eat the right foods. If you don’t have an appetite, you should resort to drinking only liquids for a short period of time. Boiled starches (potatoes, noodles, rice, wheat and oats) and plain cereals with salt are recommended, if you have watery diarrhea. You may also try crackers, bananas, soup and boiled vegetables.
- Avoid heavy foods. On the other hand, you should avoid certain foods until you are feeling better. These include dairy products, caffeine, alcohol, nicotine and fatty or highly-seasoned foods.
- Get plenty of rest. The illness or dehydration can make you feel tired.
“Adults under 65 years old with a new bout of diarrhea, with no fever or blood in bowel movements, can take medicine to stop diarrhea, such as loparmide (Imodium) or bismuth subsalicyclate (Pepto Bismal) for one to two days, if they’re not allergic to these medications. Children and adults over the age of 65 should check with their health care provider before taking any over-the-counter medicines,” Miller says.
As contagious as it is, keeping your family from catching the stomach flu can be tricky. Miller offers these tips to protect against the viral infections that cause gastroenteritis:
- Immunize little ones. Infants can be immunized with the rotavirus vaccine. This is offered at 2, 4 and 6 months old during well-child visits.
- Simply wash your hands. Wash your hands often to stop the spread of germs. Hand sanitizer works after being in public as well.
- Give your home the once-over. Use household cleaning products to disinfect surfaces and objects, like countertops, doorknobs, handles, sinks, toilets, computer keyboards and phones.
- Separate your laundry loads. Wash laundry of those recovering from the stomach flu in different loads than the rest of your family.
- Keep your distance. Try to keep your children, especially newborns, away from anyone who is sick. If someone in your family is sick, stay home and do not go to work, school or day care. You should be symptom-free for 48 hours before returning.
When the Stomach Flu Requires a Doctor
While most stomach illnesses pass on their own, there are cases when medical attention is necessary. Miller recommends watching for signs of severe dehydration:
- Increased thirst
- Increased heart rate over 100 beats per minute
- Increased breathing rate
- Dizziness, including when standing from a sitting or laying position
- Passing out
- Dark yellow or amber colored urine
- No urination within the past six to eight hours (during the day)
In addition to severe dehydration, Miller also says the following are causes for concern, and if you experience these, contact your provider:
- Bloody stool /rectal bleeding or blood in vomit
- Vomiting for more than 24 hours
- Fever greater than 104 degrees
- Weight loss
- Severe abdominal pain
- Prolonged symptoms lasting more than a week
- Are currently pregnant
Lastly, call your baby's doctor right away if your baby:
- Has vomiting lasting several hours
- Hasn't had a wet diaper in six hours
- Has bloody stools or severe diarrhea
- Has a sunken soft spot (fontanel) on the top of his or her head
- Has a dry mouth or cries without tears
- Is unusually sleepy, drowsy or unresponsive
If any of these symptoms are present, evaluation by a health care professional is needed right away, and IV hydration may need to be administered or possible admission to the hospital.
Virtual and Urgent Care for Stomach Flu
If your stomach flu symptoms aren’t severe but are making you miserable, consider visiting one of our walk-in clinics near your home. It’s a good idea to save your spot online first as some clinics require it. Don’t want to leave home? We get it. Smart Exam and virtual urgent care are also available for patients ages two and up who live in Iowa. Just log-in to your patient app, MyUnityPoint , to set up your appointment.
Same-day appointments may also be available with your provider, or their care team, if it’s a weekday. Just look in the app , or call the clinic, to see if something’s available.
Get Care Now
Related Content
Phlegm Cheat Sheet: Recognizing Normal and Concerning Colors and Consistencies
Swollen Lymph Nodes: Causes, Treatments and When to Go to the Doctor
How Do Antibiotics Work and When Should I Take Them?
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
- Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skin, nail and hair health
Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
- Abdominal pain
Advice for recovering from gastroenteritis

Peer reviewed by Dr Krishna Vakharia, MRCGP Last updated by Matt Binny Last updated 5 Apr 2023
Gastroenteritis is an intestinal infection that causes vomiting, diarrhoea, abdominal cramps, and other symptoms. These symptoms usually aren't harmful but can be debilitating, so self-care is essential during recovery. Here we look at the best ways to recover from gastroenteritis.
In this article :
What causes gastroenteritis, symptoms of gastroenteritis, how to recover from gastroenteritis, further reading.
Continue reading below
Gastroenteritis , sometimes called stomach flu, is commonly caused by noroviruses and adenoviruses, but other viruses can also be responsible. Bacterial gastroenteritis is caused by common bacteria such as salmonella , E. coli , and c ampylobacter . It can also be caused by contaminated food and drinks 1 .
Symptoms can vary in severity, from a few days of mild tummy upset with vomiting and diarrhoea to severe sickness and diarrhoea for several days. It's mostly harmless, especially if you are otherwise in good health. However, there can be cause for concern if young children, the elderly, pregnant people, and those with compromised immune systems experience severe or persistent symptoms.
The most common symptoms are vomiting and diarrhoea, but abdominal cramps and fever may also occur. While it's very unpleasant, most people recover in a few days. With that said, it's essential to take care of yourself while recovering from gastroenteritis and prevent prolonging or worsening your symptoms.
Stay at home and rest
Staying home and resting until you're better are important. Leaving your house risks your own health and that of anyone you come into close contact with, as gastroenteritis is contagious. The official advice is to stay away from people or work until you are 48 hours free of any bouts of vomiting or diarrhoea, to avoid passing it on to others 2 .
Vomiting and diarrhoea both cause dehydration, especially if you are unable to keep food and fluids down. Signs of dehydration include dizziness , headaches , and other symptoms that make everyday tasks strenuous and even exhausting.
Overexerting yourself can make you feel worse and slow the recovery period. It can also be unsafe for you to leave the house when suffering from severe dehydration, as it may affect factors such as your decision-making and balance.
Drink plenty of fluids
Repeated vomiting and diarrhoea make it difficult to give your body what it needs, fluids being one of them. Whether you are unable to keep fluids down or feel too unwell to drink at all, dehydration makes you feel worse and can cause additional symptoms. Symptoms of mild dehydration include dizziness and headaches, dry mouth and tongue, dark urine, and fatigue.
If you suspect you or someone you're caring for is severely dehydrated, you should seek medical advice.
People should drink two to three litres of water daily. If you have gastroenteritis, drink more water than usual or consider using oral rehydration solutions to prevent dehydration. A rough guide for increasing water intake is an extra glass of water following bouts of diarrhoea.
Vomiting makes it difficult to keep down fluids and stay hydrated. If you've been sick, wait around 5-10 minutes before drinking again, and start by drinking small amounts every few minutes. This will help your body get used to drinking without overdoing it and causing you to be sick again.
Ease back into eating
You should try to eat as normally as possible. This can be difficult as you may not have an appetite or are still vomiting. Adults can handle a day or two without food, but when you start eating again, you should ease yourself back with small, light, plain meals and foods that are easy to digest - such as bread, rice, pasta, and sugar-free cereals. Try to avoid dairy products if you have an upset tummy as they can be more difficult for your body to digest.
The key is to go with your appetite - if you're hungry, try to eat. Even small amounts of food will help your intestinal lining heal and provide the energy to regain your strength and recover. However, if you begin to feel nauseous or vomit, you should ease back on your food intake. Here's a guide for eating when you have gastroenteritis .
Note : even if you stop eating for a few days, you should never stop drinking. This causes dehydration because you won't replace the fluids lost through vomiting, diarrhoea, and sweating if you have a fever.
Patient picks for Abdominal pain

What causes appendicitis?

Right upper quadrant pain
Avoid spreading infection at home.
An important part of recovering from gastroenteritis is ensuring it doesn't spread to other people. Hygiene precautions help to prevent others getting sick and you experiencing repeat bouts of gastroenteritis.
Here are some good hygiene practices to keep in mind when you or someone else at home has gastroenteritis:
Stay at home until you haven't vomited or had an episode of diarrhoea for at least 48 hours.
Thoroughly wash your hands with soap and water after using the toilet. Dry your hands properly.
Using disinfectant, clean the toilet and any surfaces that may have been touched, including larger surfaces as well as small surfaces, such as taps and door handles.
Don't share towels.
Don't make or serve food for other people.
Monitor medications
If you take daily medications, it's crucial to monitor your intake, as bouts of sickness could mean you're not getting the right dosage. Generally, if you're sick more than 20 minutes after taking medication, it's unlikely you'll need to take more. But to be safe, contact your doctor for advice as all medications vary with regard to dosage and side-effects.
It's better to take paracetamol for pain relief, as ibuprofen can irritate your stomach.
When to call a doctor
Most cases of gastroenteritis clear up after a few days. Contact your doctor for advice if:
You suspect that you are becoming severely dehydrated.
You have extreme abdominal pain .
There is blood in your vomit or stool (poo).
You have a continuous high temperature ( fever ) lasting more than five days or not responding to paracetamol.
You are elderly or have an underlying health condition such as epilepsy , diabetes , or kidney disease .
You are pregnant.
Your immune system is weakened by long-term medical treatments, such as chemotherapy .
Stuempfig et al: Viral gastroenteritis .
UKHSA: Norovirus: What to do if you catch it and helping to stop the spread .
Article history
The information on this page is peer reviewed by qualified clinicians.
5 Apr 2023 | Latest version
Last updated by
Peer reviewed by
5 Apr 2023 | Originally published
Authored by:

Feeling unwell?
Assess your symptoms online for free
Welcome to your journey for creating a healthier you

- Our Services
- Departments
- Brain & Spine
- Cold & Flu
- Heart & Vascular
- Infectious Diseases
- Mental Health
- Orthopedics & Sports Medicine
- ExpressCare
- Weight Management
- Alternative Medicine
- Regional News
- Community Involvement
- Family Wellness
- Tweens & Teens
- Clinical Care
- CEO Insights
- Our Annual Report
- Values in Action
- Diversity, Equity & Inclusion
- Environmental Stewardship
- Perspectives
- Digital Innovation
- Distributed care
- Personalization
- Health equity
- Behavioral health
- Innovation @ scale
- Industry disruption
Understanding your stomach pain: When to worry
- Share this Article

[5 MIN READ]
In this article: , stomach pain is a common complaint, but it can be a sign of something more serious., stomach pain can be an early sign of emergency conditions like appendicitis or a heart attack., when in doubt about your abdominal pain, it’s important to see your doctor or go to the emergency room..
Everyone experiences stomach pain at some point in their life. Whether you ate something that didn’t agree with you or you suffer from a virus, stomach pain is often a normal, but aggravating, complaint. However, sometimes stomach pain can be cause for concern.
The Centers for Disease Control and Prevention (CDC) reports that 45.1 million people each year visit their doctor or emergency room because of stomach pain. There are many causes of abdominal pain. The severity of your pain and the location within your abdominal area may provide important clues about the cause of your pain and whether you should see a doctor.
What causes stomach pain?
There are many reasons you may experience stomach pain. The cause of your stomach pain may be from an illness or injury. Stomach pain is often referred to as discomfort in any part of your abdominal area between your ribs and pelvis. However, the pain can be associated with other organs located in the same region, including your:
- Gallbladder
- Large intestine
- Small intestine
Stomach pain is subjective, which means only you can describe your symptoms. Many common complaints of stomach pain are:
- Intermittent
According to Hardeep Singh, M.D. , a gastroenterologist from Providence St. Joseph Hospital in Orange, CA, it’s important to accurately describe your pain to your health care provider.
“Your doctor will be able to help confirm the severity of your condition and what tests you may need based on your description of the pain,” he says.
Normal stomach pain vs. something more serious
Most stomach pain is temporary and not the result of a serious condition. But in some cases, stomach pain can be a cause for serious concern. Dr. Singh says knowing the difference could save your life.
Symptoms of everyday stomach pain
Normal stomach pain is often mild to moderate and resolves within a few days. In many cases, it is the result of a digestive issue, menstrual pain, virus or infection. Pain and discomfort from this type of stomach pain can generally be treated with over-the-counter medications.
Some common digestive system-related stomach pain include:
- Constipation
- Food allergies
- Food poisoning
- Indigestion
- Lactose intolerance
Inflammation is another common cause of stomach pain. Stomach possible causes of abdominal inflammation may include:
- Gastroesophageal acid reflux disease (GERD) also known as heartburn
- Inflammatory bowel disease
- Pancreatitis
- Peptic ulcer disease
- Stomach virus
- Urinary tract infection
Serious stomach symptoms
In some cases, stomach pain may be a sign of a serious issue that requires medical attention. Dr. Singh says there are certain symptoms you should never ignore. “Anytime you have severe, sudden onset of abdomen pain, you should contact your doctor immediately,” he says.
Other signs of a serious stomach issue are:
- Abdomen tenderness or swelling
- Blood in your poop, urine or vomit
- Persistent fever
- Persistent vomiting
- Shortness of breath
- Severe abdominal pain
- Vomiting blood
Specific stomach pain and what it may mean
With so many causes of stomach pain, it may be difficult to tell what’s serious. There are several warning signs Dr. Singh says you should never ignore.
Severe stomach pain after eating a fatty meal
If you find yourself doubled over after eating a high-fat meal, you may be experiencing a gallbladder attack. “Women are especially prone to gallbladder disease,” says Singh. “Overweight women in their 40s are at highest risk.” When you experience a gallbladder attack, the pain becomes worse after eating, lasts 30 to 60 minutes, and may come and go, becoming more constant and severe over time, says Singh.
You can help prevent gallbladder attacks with a diet that’s rich in nutrients and fiber and low in fatty foods.
Crampy pain with diarrhea or constipation
Lower “crampy” abdominal pain accompanied by bloating and diarrhea, or constipation can be signs of irritable bowel syndrome (IBS), says Singh. “It’s exceptionally common and affects 15% of the U.S. population, particularly younger women, although it can happen at any age.” Symptoms of IBS can usually be controlled by managing diet , lifestyle and stress. Medication and counseling may be needed in some cases.
Upper abdominal pain between the rib cage
Aching or stabbing pain or pressure in the upper abdominal area just under the ribs may indicate a heart-related problem. Heart issues may be accompanied by chest pain, shortness of breath and are concerning if the pain persists. You could mistake this type of pain for indigestion, and while that may be the case, if you have risk factors such as diabetes or hypertension, you should see a doctor as soon as possible.
If you do struggle with acid reflux, you may want to talk to a gastroenterologist . They can help you manage your symptoms through medications, lifestyle changes and diet. In some cases, antacids can help you minimize symptoms.
Severe, acute pain in the lower right side of the abdomen
Sudden pain in the lower part of the abdomen may be a sign of appendicitis. You may also experience a fever. Pain often begins around the belly button area and becomes worse with time. Vomiting, constipation or diarrhea along with the pain also indicate it’s time to go to the emergency room.
Appendicitis mostly affects kids and teens between the ages of 5 and 20. While many digestive health issues can cause stomach pain in kids , it’s important to talk to your child’s doctor immediately if you suspect appendicitis — especially if the pain comes on suddenly over several hours or is persistent. Appendicitis requires immediate medical attention and often leads to surgery. If left untreated, a ruptured appendix can be deadly.
Vague upper abdominal pain associated with nausea and belching
Sometimes stomach pain is hard to identify or comes with multiple symptoms. Vague pain in the upper and mid-abdominal area that is accompanied by nausea, burping or belching could be signs of a heart attack, particularly in older individuals. Tests like an ECG or cardiac markers can be lifesaving. Symptoms such as vomiting along with back or jaw pain and shortness of breath can also be a sign of a life-threatening emergency.
Women are more likely to experience abdominal pain or digestive issues during a heart attack. It’s important to learn how heart disease, including heart attacks, can affect women differently .
Sudden and severe onset stomach pain
When mid-abdominal pain occurs suddenly — especially in people with a history of peptic ulcer disease or in those who take excessive amounts of aspirin or NSAIDs — it may be a sign of a tear that could require emergency surgery. A tear could leak air and gastric content which can lead to a condition called peritonitis, and eventually, septic shock. Surgery would be required to seal the perforation.
If you’re experiencing chronic stomach pain, take steps now to head off any bigger problems down the road. Your primary care provider can help determine what’s causing your issues and create a plan to help improve your gut health. Your plan may include medication, lifestyle changes, a healthier diet and stress management techniques .
Right or left lower abdominal pain in women
Sudden onset of right lower abdominal pain or left lower abdominal pain can indicate a ruptured ovarian cyst in a woman who is in the middle of her menstrual cycle. This kind of pain could also be a sign of ovarian torsion, which is the rotation of the ovary and part of the fallopian tube, or possibly a twisting of the ovary due to reduced blood supply. Seek treatment immediately at the nearest emergency department. Surgery to remove the ovary may be necessary.
Knife-like pain in the lower abdomen
Pain that wraps around the lower stomach area, commonly accompanied by nausea, vomiting, fever and chills, could be a sign of kidney stones or kidney infection. Kidney stones are diagnosed by ultrasound or CT scans and NSAIDs are often recommended for pain relief. In cases of persistent pain, rescue narcotics may be prescribed for immediate relief or alpha-blockers which can relax blood vessels allowing larger stones to pass.
Belly pain in the lower left side that’s worse when you move
Abdominal pain in the left lower area of the abdomen may be a sign of diverticulitis , small pockets in the colon that can become obstructed and tear. Traditional treatment includes antibiotics and stool softeners to reduce the risk of abscess formation. According to research , antibiotics may no longer be needed in this scenario, and doctors recommend acetaminophen instead.
Contributing caregiver
Hardeep Singh, M.D. , is a gastroenterologist from Providence St. Joseph Hospital in Orange, CA.
Find a doctor
If you are looking for a Providence gastroenterologist or primary care physician, you can search for one who’s right for you in our provider directory .
Download the Providence app
We’re with you, wherever you are. Make Providence’s app your personalized connection to your health. Schedule appointments, conduct virtual visits, message your doctor, view your health records and more. Learn more and download the app .
Related resources
Maintain a healthy gut: Three reasons to see a gastroenterologist
When should you be concerned about your child’s stomach pain?
Coping with diverticulitis
This information is not intended as a substitute for professional medical care. Always follow your health care professional’s instructions.
About the Author The Providence Body & Mind Team is dedicated to providing medically-sound, data-backed insights and advice on how to reach and maintain your optimal health through a mixture of exercise, mindfulness, preventative care and healthy living in general. More Content by Providence Body & Mind Team
Previous Article

The Better Birthing Project honors tribal cultures by using native doulas, creating birth plans that respec...
Next Article

Your culture plays an important role in shaping your pregnancy experience. Here are five tips for voicing y...
Most Recent Articles
The better birthing project honors tribal cultures by using native doulas, creating birth plans that respect traditions, and ensuring follow-up care., your culture plays an important role in shaping your pregnancy experience. here are five tips for voicing your cultural preferences during your pregnancy and delivery..

A Providence allergist and immunologist shares tips for people living with food allergies on how to stay safe and avoid severe reactions.

Discover essential skin cancer prevention tips from the experts at Providence, and learn how to protect your skin effectively.

A Providence expert explains the different types of strokes, how to quickly identify stroke symptoms using the BE FAST acronym and ways to prevent strokes.

Recovery from addiction is hard, but it’s especially difficult when you’re pregnant. Caregivers talk about how they help at Addiction Recovery Services.

Learn to prioritize mental health with our guide. Find essential tips for all ages that cover awareness, support and managing mental health conditions.

A child or teen’s mental health is important to their quality of life. Learn the symptoms to watch for and when to see your pediatrician.

Discover the truth about Parkinson's Disease, from myths debunked to the latest treatment advancements. Learn key facts and figures at Providence.

Hospitals use a lot of energy. Providence is finding ways to cut that use with efficient, renewable alternatives that enhance patient care and comfort.

Colville resident Mary Selecky needed wound care. Thanks to Providence Mount Carmel Hospital, she received quality health care close to home.

Do you have high blood pressure, or hypertension? If so, you may need medication, but there are also lifestyle changes you can make to get healthier.

If you live long enough, you will eventually develop cataracts. A Providence ophthalmologist debunks some of the most common myths about cataracts.

When you’re pregnant, it can be difficult to keep all the different roles straight — midwife, doula or obstetrician. Here’s how to tell them apart.

Learn key strategies for managing epilepsy from the doctors at Providence. Understand triggers, treatments and lifestyle tips to manage epilepsy effectively.

Many of the medications in your medicine cabinet may be expired, but some are safer than others to take past their expiration date.

If you are a man between the ages of 20 and 35, you should be performing testicular self-examinations to look for cancer. Here, we teach you what to look for.

The last week of April is World Immunization Week 2024. Here, a Providence family medicine doctor discusses some common myths about vaccines.

Discover the fastest ways to get rid of allergies. Our guide offers effective tips and remedies for quick allergy relief from the experts at Providence.

A Providence gastroenterologist shares what you need to know about lower abdominal pain, including common causes and signs you should seek medical care.
- Share this Hub
Gastroenteritis
Gastroenteritis is a very common condition that causes diarrhoea and vomiting. It’s usually caused by a bacterial or viral tummy bug.
It affects people of all ages, but is particularly common in young children.
Most cases in children are caused by a virus called rotavirus. Cases in adults are usually caused by norovirus (the ‘winter vomiting bug’) or bacterial food poisoning .
Gastroenteritis can be very unpleasant, but it usually clears up by itself within a week. You can normally look after yourself or your child at home until you’re feeling better.
Try to avoid going to your GP, as gastroenteritis can spread to others very easily. Phone 111 or your GP if you’re concerned or need any advice.
Symptoms of gastroenteritis
The main symptoms of gastroenteritis are:
- sudden, watery diarrhoea
- feeling sick
- vomiting, which can be projectile
- a mild fever
Some people also have other symptoms, such as a loss of appetite, an upset stomach , aching limbs and headaches.
The symptoms usually appear up to a day after becoming infected. They typically last less than a week, but can sometimes last longer.
What to do if you have gastroenteritis
If you experience sudden diarrhoea and vomiting, the best thing to do is stay at home until you’re feeling better. There’s not always a specific treatment, so you have to let the illness run its course.
You don’t usually need to get medical advice, unless your symptoms don’t improve or there’s a risk of a more serious problem.
There are things you can do to help ease your symptoms.
- drink plenty of fluids to avoid dehydration; you need to drink more than usual to replace the fluids lost from vomiting and diarrhoea – water is best, but you could also try fruit juice and soup
- take paracetamol for any fever or aches and pains
- get plenty of rest
- if you feel like eating, try small amounts of plain foods, such as soup, rice, pasta and bread
- use special rehydration drinks made from sachets bought from pharmacies if you have signs of dehydration, such as a dry mouth or dark urine
- take anti-vomiting medication (such as metoclopramide) and/or antidiarrhoeal medication (such as loperamide) if you need to – some types are available from pharmacies, but check the leaflet that comes with the medicine; you can also ask your pharmacist or GP for advice about whether they’re suitable
Read further information about treating dehydration
Gastroenteritis can spread very easily. You should wash your hands regularly while you’re ill and stay off work or school until at least 48 hours after your symptoms have cleared, to reduce the risk of passing it on.
When to get medical advice
You don’t normally need to see your GP if you think you have gastroenteritis, as it should get better on its own.
Visiting your GP practice can put others at risk, so it’s best to phone 111 or your GP if you’re concerned or feel you need advice.
Phone 111 or your GP practice if:
- you have symptoms of severe dehydration , such as persistent dizziness , only passing small amounts of urine or no urine at all, or if you’re losing consciousness
- you have bloody diarrhoea
- you’re vomiting constantly and are unable to keep down any fluids
- you have a fever over 38C (100.4F)
- your symptoms haven’t started to improve after a few days
- in the last few weeks you’ve returned from a part of the world with poor sanitation
- you have a serious underlying condition, such as kidney disease , inflammatory bowel disease or a weak immune system, and have diarrhoea and vomiting
Your GP may suggest sending off a sample of your poo to a laboratory to check what’s causing your symptoms. Antibiotics may be prescribed if this shows you have a bacterial infection.
Looking after a child with gastroenteritis
You can look after your child at home if they have diarrhoea and vomiting. There’s not usually any specific treatment and your child should start feeling better in a few days.
You don’t normally need to get medical advice unless their symptoms don’t improve or there’s a risk of a more serious problem.
There are things you can do to help ease your child’s symptoms.
- encourage them to drink plenty of fluids as they need to replace the fluids lost from vomiting and diarrhoea – water is generally best; avoid giving them fizzy drinks or fruit juice, as they can make their diarrhoea worse
- babies should continue to feed as usual, either with breast milk or other milk feeds
- make sure they get plenty of rest
- let your child eat if they’re eating solids and feel hungry – try small amounts of plain foods, such as soup, rice, pasta and bread
- give them paracetamol if they have an uncomfortable fever or aches and pains – young children may find liquid paracetamol easier to swallow than tablets
- use special rehydration drinks made from sachets bought from pharmacies if they’re dehydrated – your GP or pharmacist can advise on how much to give your child
Don’t give your child antidiarrhoeal and anti-vomiting medication, unless advised to by your GP or pharmacist.
Make sure you and your child wash your hands regularly while your child is ill. Keep them away from school or nursery until at least 48 hours after their symptoms have cleared.
Getting medical advice for your child
You don’t usually need to see your GP if you think your child has gastroenteritis, as it should get better on its own, and taking them to a GP practice can put others at risk.
You’re concerned about your child, or they:
- have symptoms of dehydration , such as passing less urine than normal, being unusually irritable or unresponsive, pale or mottled skin, or cold hands and feet
- have blood in their poo or green vomit
- are vomiting constantly and are unable to keep down any fluids or feeds
- have had diarrhoea for more than a week
- have been vomiting for 3 days or more
- have signs of a more serious illness, such as a high fever (over 38C or 100.4F), shortness of breath, rapid breathing, a stiff neck, a rash that doesn’t fade when you roll a glass over it or a bulging fontanelle (the soft spot on a baby’s head)
- have a serious underlying condition, such as inflammatory bowel disease or a weak immune system, and have diarrhoea and vomiting
Your GP may suggest sending off a sample of your child’s poo to a laboratory to confirm what’s causing their symptoms. Antibiotics may be prescribed if this shows they have a bacterial infection.
How gastroenteritis is spread
The bugs that cause gastroenteritis can spread very easily from person to person.
You can catch the infection if small particles of vomit or poo from an infected person get into your mouth, such as through:
- close contact with someone with gastroenteritis – they may breathe out small particles of vomit
- touching contaminated surfaces or objects
- eating contaminated food – this can happen if an infected person doesn’t wash their hands before handling food, or you eat food that has been in contact with contaminated surfaces or objects, or hasn’t been stored and cooked at the correct temperatures
A person with gastroenteritis is most infectious from when their symptoms start until 48 hours after all their symptoms have passed, although they may also be infectious for a short time before and after this.
Preventing gastroenteritis
It’s not always possible to avoid getting gastroenteritis, but following this advice can help stop it spreading.
- stay off work, school or nursery until at least 48 hours after the symptoms have passed – you or your child should also avoid visiting anyone in hospital during this time
- ensure you and your child wash your hands frequently and thoroughly with soap and water, particularly after using the toilet and before preparing food – don’t rely on alcohol hand gels, as they’re not always effective
- disinfect any surfaces or objects that could be contaminated – it’s best to use a bleach-based household cleaner
- wash contaminated items of clothing or bedding separately on a hot wash
- flush away any poo or vomit in the toilet or potty and clean the surrounding area
- practice good food hygiene: make sure food is properly refrigerated, always cook your food thoroughly, and never eat food that is past its use-by date
Don’t
- do not rely on alcohol hand gels, as they’re not always effective
- don’t share towels, flannels, cutlery or utensils while you or your child is ill
Take extra care when travelling to parts of the world with poor sanitation, as you could pick up a stomach bug. For example, you may need to boil tap water before drinking it.
Young children can have the rotavirus vaccination when they’re 2 to 3 months old, which can reduce their risk of developing gastroenteritis.
Source: NHS 24 - Opens in new browser window
Last updated: 29 May 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
- Self-help guide: Diarrhoea
- Self-help guide: Abdominal pain
- Dehydration
- Preparing and cooking food safely
Other health sites
- fitfortravel: Norovirus
- Conditionally
- Newsletter Signup
Health Conditions Chevron
Autoimmune Diseases Chevron
6 Signs of an Autoimmune Disease That Can Be Easy to Miss
By Julia Sullivan
Medically reviewed by Kristin Sokol, MD, MS
Think of your immune system like a hardworking security team: Day and night, with zero breaks, it’s scanning for potentially dangerous intruders. And while you mindlessly scroll your social feeds and munch on chips, it might be waging a battle against harmful bacteria and viruses without you even realizing it. But those defenses can occasionally glitch and mistake the very things it’s designed to protect—your own bodily tissues—for foreign invaders. When this happens, you might have what’s called an autoimmune disease , Konstantin Balashov, MD, PhD , the director of the Boston Medical Center Multiple Sclerosis Center, tells SELF.
But accurately diagnosing this problem can be so tricky. There are more than 80 types of autoimmune diseases (also called disorders or conditions) that researchers know of, and, frustratingly, it can sometimes take years to figure out what’s going on. A big reason for this? There’s no single test that can easily confirm a diagnosis, so doctors often have to rely on other markers, like symptoms, to try to put the puzzle pieces together. But the list of possible symptoms associated with autoimmune diseases is enormous, and they can feel a bit vague or be easily mistaken for another health problem. Plus symptoms might pop up in a lot of different places (or even move around) in your body. They can also wax and wane, worsening during flare-ups and then subsiding into relatively calm periods—and even disappearing by the time you get in to see a doctor—before ramping up again.
Most autoimmune diseases are chronic conditions, meaning they don’t have a cure. However, they are usually very treatable; an effective medication plan, physical therapy, and certain surgical procedures can help slow down or prevent severe complications or even permanent damage down the road. That’s why seeing a doctor about your symptoms early on is so important. Here are six signs you might have an autoimmune disease.
1. You’re ridiculously fatigued or constantly feel like you’re coming down with the flu.
When you’ve got an infection, your body funnels a ton of your energy into fighting it off. This is why you might feel particularly drained if you have a cold, the flu, or some other bug. “Your body works so hard to build an inflammatory response to fight infections, but that inflammation itself can cause fatigue,” Roshini Rajapaksa, MD , a gastroenterologist who treats autoimmune disorders that affect the digestive system, like Crohn’s and celiac disease , says. And because most autoimmune conditions cause widespread and chronic inflammation, feeling persistently worn down is a symptom doctors tend to see across the board, Dr. Rajapaksa adds.
Though every person that Lindsay McAlpine, MD , a neurologist at the Yale School of Medicine, treats has varying descriptions of fatigue, she’s noticed a few common patterns in folks with autoimmune diseases. “You’ll often hear patients say that when they first get up in the morning they’re doing okay, and then in the afternoon they hit a wall ,” she tells SELF. “Or somebody takes a 20-minute walk around the neighborhood with their dog, and then 12 to 24 hours later, they crash and can’t function for a day or two.”

By Katie Camero

By Kathleen Felton
There are lots of reasons why you might be tired all the time , but Dr. Rajapaksa likens autoimmune-related fatigue, in particular, to a deep, whole-body ache: “You feel it in your bones and muscles,” she describes. “It’s not like you just didn’t get enough sleep last night.” Dr. Rajapaksa understands this on a personal level: She has Hashimoto’s thyroiditis , an autoimmune condition that causes the body to attack healthy thyroid cells, and fatigue is a major issue for her. “When I had a toddler and a newborn, I found myself extremely exhausted all the time,” Dr. Rajapaksa recalls. She initially attributed that fatigue to parenthood, but when it didn’t dissipate as her kids got older, she knew something bigger was happening. “I can personally attest to the fact that fatigue with an autoimmune condition profoundly affects your ability to function,” she says.
It’s one of Jennifer Graves’s most frustrating symptoms too. The 41-year-old lives in Gilbert, Arizona, and has both multiple sclerosis (MS) and rheumatoid arthritis (RA). “[The fatigue] can get so bad that I have no other choice but to stop whatever I’m doing and rest ,” she tells SELF. “I could be in the middle of grocery shopping and I have to go home and sleep.” (FYI: Research suggests that one in four people with an autoimmune disease develop another one, like Graves did.)
2. You have unexplained pain or swelling in your joints or muscles.
Again, a wonky immune system often goes after certain body parts, and for a lot of people that inflammation settles in certain joints, per Dr. Rajapaksa. RA symptoms, for example, are often symmetrical , so you might feel aches in your wrists, fingers, toes, knees, shoulders, elbows, or ankles on both sides of your body, as SELF has previously reported. And like fatigue, autoimmune-related joint pain can seriously affect your day-to-day life, per Dr. Rajapaksa—something Graves knows all too well. “My RA makes my joints super swollen, sometimes I can barely move,” she explains, noting that her shoulders are hot spots. “I can recall times the pain would be so horrific that I would need to roll up towels and put them in my armpits to ‘separate’ the shoulder joint and relieve pressure.”
A few other notable autoimmune conditions that can cause joint issues? Lupus (one type that attacks a bunch of different parts of the body rather than a certain area), psoriatic arthritis (which typically manifests alongside psoriasis , another autoimmune condition), and Sjögren’s syndrome (a condition that triggers inflammation in the glands that produce moisture in your eyes and mouth).
What’s more, Dr. McAlpine says that chronic muscle pain or weakness, particularly in the legs, can sometimes signal things like MS. Actor Jamie-Lynn Sigler , who has been open about living with the condition, used to have symptoms so severe that she could barely stand. “I had to try so hard to look like an able-bodied person that I could barely concentrate on the scene I was in,” Sigler previously told SELF. “I was getting away with surface-level performances because I was just worried about physically holding myself up and trying to walk normally.”
3. Rashes or other strange skin issues are popping up.
There could be any number of reasons for a weird itchy spot or sudden rash . Perhaps you encountered an irritating detergent or a tick out in the woods . Often, skin symptoms gradually disappear with time or treatment (say, you stopped using the detergent or got an antibiotic for said tick bite). But it’s important to point out that some skin conditions defined by rashes are also autoimmune diseases, Dr. Rajapaksa says. She notes psoriasis as a really common one; it causes skin cells to multiply way too quickly, resulting in scaly skin, often on the scalp, knees, or elbows.
In other autoimmune diseases, skin issues can be a secondary symptom. For example, lupus sometimes presents with a butterfly-shaped rash on the cheeks after immune cells in your skin react to UV light. The rash can also flare up for no reason at all. Even some gastrointestinal conditions can cause skin problems too. “With celiac disease , an intestinal autoimmune disorder, you can get a characteristic skin rash,” Dr. Rajapaksa explains. That’s because if you have the disorder, your immune system sees the gluten protein in wheat and other foods as an invader. So when you consume it, your immune system goes a bit haywire and attacks healthy parts of your body—and yep, that can include your skin. All of this spurs inflammation that might lead to well-known GI symptoms, like bloating , diarrhea , and constipation, but also itchy, blistery rashes on the elbows, knees, butt, scalp, or back.
4. Your gut is seriously struggling.
Nobody over the age of 15 is going to feel amazing after downing a Chili’s sampler plate with spicy margs, but recurring bowel problems can sometimes mean your immune system is going into attack mode on your digestive tract, Dr. Rajapaksa says. Again, this could be related to something like celiac disease—she notes that a big chunk of people don’t even realize they have it, mistaking constant constipation or diarrhea for normal bathroom pains.
Ulcerative colitis (UC), which causes chronic inflammation and sores (most often in the rectum and colon), and Crohn’s disease, which can affect any part of the intestines, are two other autoimmune-related biggies, per Dr. Rajapaksa. Both UC and Crohn’s are inflammatory bowel diseases that can cause debilitating fatigue, diarrhea, abdominal pain or cramping, bloody poop , and sometimes weight loss.
It’s important to note that a lot of things can cause gut problems (like said sampler plate and even irritable bowel syndrome , which isn’t autoimmune-related). But if you’re sprinting to the bathroom and it’s seriously messing with your quality of life, it’s worth flagging to a doc.
5. You’re having trouble processing information, you have recurring headaches, or your vision seems off.
According to Dr. McAlpine, when your immune system attacks your nervous system (as is the case with MS), it can cause some pretty unsettling neurological effects. You might feel a little foggy in general: Research shows that people with MS are more likely to have difficulty processing information and have a harder time remembering things. The condition can also make you prone to chronic migraine or frequent tension headaches , studies suggest . Non-neurological autoimmune diseases, like lupus, psoriasis, and rheumatoid arthritis, can also cause cognitive issues.
Another hot spot for autoimmune attacks is the eyes. If your vision starts to change suddenly or for seemingly no reason—particularly if it’s blurry or you’re seeing double—that’s a symptom to flag to your doctor, Dr. McAlpine says. Super dry eyes can signal something is wrong too: It’s something 66-year-old Eileen Bailey from Pottstown, Pennsylvania, experienced before she was diagnosed with Sjögren’s syndrome. “I had dry eyes and a dry mouth, but I just drank water and used eye drops. I didn’t connect it to a medical problem,” she tells SELF. But when Bailey would lift her arm, she’d often wince with pain. When she flagged this issue to a doctor, the connection to her other symptoms finally surfaced.
6. You experience any of these symptoms in an on-again, off-again way.
Beyond the constellation of symptoms, there’s often one major defining feature among a lot of autoimmune diseases, Dr. McAlpine says: flare-ups. It’s common to go through periods when you feel totally fine, and then have weeks or months with symptoms. “That relapsing-remitting pattern is common across a lot of [these diseases],” she says. For example, in a Crohn’s disease flare-up , you might suddenly get painful gastrointestinal issues (urgent bowel movements or cramps) that pop up for seemingly no reason at all. Meanwhile, if your autoimmune disease predominantly causes pain (like in RA), your joints might get inexplicably swollen or stiff even if you felt totally fine a few weeks prior.
Try to remember when your first flare-up might have happened too. Dr. McAlpine says a bacterial or viral infection can sometimes “trigger” an autoimmune reaction in some people, so it’s worth bringing up to your doctor if you’re trying to solidify a diagnosis: “It really depends on the specific disease, but the onset of symptoms within [several] weeks of a viral infection is always kind of a clue. We’ve diagnosed quite a bit of new autoimmune diseases after COVID-19, for example.” Researchers have noted this trend among other infections too, like Epstein-Barr (EBV), a super common virus that can sometimes lead to mono, and cytomegalovirus (CMV), which is particularly a concern for pregnant people and newborns, since it can be transmitted during gestation and while breastfeeding. (Both EBV and CMV are in the herpes family, similar to the virus that causes chicken pox.)
Dr. Rajapaksa says it’s important to seek out a health care provider any time you have symptoms that affect your ability to live your life. If they suspect an autoimmune disease could be at play, they will refer you to a specialist, like a rheumatologist, who can do more testing. “If you’re fatigued to the point where you’re having trouble going to work or going to school, or you have abdominal pain to the point you can’t eat properly or you’re losing weight, it’s better to err on the side of caution.” You might be told that you’re dealing with an issue that’ll pass soon, or you might learn something new about your health. Either way, a doc can give you clear direction on next steps—and if you do have an autoimmune disease, they’ll get you situated with treatment ASAP.
- Here’s When Getting Sick a Lot Can Signal a Major Immune System Issue
- My ‘Flu’ Symptoms Turned Out to Be Early Signs of a Stroke
- 7 Digestive Symptoms You Should Definitely Tell Your Doctor About

SELF does not provide medical advice, diagnosis, or treatment. Any information published on this website or by this brand is not intended as a substitute for medical advice, and you should not take any action before consulting with a healthcare professional.

How long does it take for Pepto Bismol to work?
Medically reviewed by Kristianne Hannemann, PharmD . Last updated on May 22, 2024.
Official answer
Pepto-Bismol (also known as the “pink stuff”) is a medication that is commonly used to treat diarrhea and upset stomach. It is available over the counter as an oral liquid, capsules, and chewable tablets. Pepto-Bismol usually works within 30 to 60 minutes.
What is Pepto-Bismol used for?
The active ingredient in Pepto-Bismol, bismuth subsalicylate, works to relieve upset stomach and is also an antidiarrheal. Pepto-Bismol can be taken for the following stomach problems:
- Traveler’s diarrhea
- Indigestion
How often can you take Pepto-Bismol?
Adults and children 12 years and older can take one dose of Pepto-Bismol every 30 to 60 minutes until symptoms improve. Do not take more than 8 doses in 24 hours, and do not take Pepto-Bismol for more than 2 days to treat your symptoms without consulting your doctor.
Make sure to read the instructions on the packaging, since Pepto-Bismol comes as a liquid, capsules, and chewable tablets. This means the amount you need to take for each dose varies.
Pepto-Bismol may not be the best option for everyone. It is not recommended for the following situations:
- People with an active stomach ulcer, a bleeding problem, or who have bloody or black stools
- Children or teens who are recovering from chickenpox or flu-like symptoms because of the risk of a serious illness called Reye’s syndrome
- Pregnant women
Additionally, if you have a fever or mucus in your stool, ask your doctor before using Pepto-Bismol.
Related Questions
- Why does Pepto-Bismol turn your tongue black?
- Can you give Pepto Bismol to kids?
- Does Pepto-Bismol help with diarrhea?
Can you take Pepto-Bismol for stomach pain?
Yes. Pepto-Bismol can be used for an upset stomach that is due to eating too much food or drink. However, if your stomach symptoms are not going away after taking Pepto-Bismol or are severe, you should get medical attention.
Pepto-Bismol [package insert]. Revised 10/2023. The Procter & Gamble Manufacturing Company - https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=67006e82-870d-8d63-e053-2991aa0a02d1
Centers for Disease Control and Prevention. (Updated June 2022). Pregnant Travelers. Available from: https://wwwnc.cdc.gov/travel/page/pregnant-travelers
Pepto-bismol.com. When and How to Take Pepto Bismol. Accessed May 22, 2024 at https://pepto-bismol.com/en-us/faq/dosage
What causes black hairy tongue?
Black hairy tongue is often caused by an overgrowth of papillae (taste buds) on the tongue. It results in a dark, furry appearance of dead skin cells on the surface of the tongue that can be stained from bacteria, food, or tobacco. Although it may be unpleasant, it doesn't usually require medical treatment and it's temporary and harmless. Continue reading
Should you take probiotics with antibiotics?
There is controversy about whether you should routinely take probiotics with antibiotics and the question cannot be answered with a straight yes or no. Evidence for taking probiotics with antibiotics includes a Cochrane review which reported that children who were given a course of probiotics after antibiotics had less diarrhea. Evidence against taking probiotics with antibiotics includes a 2019 Italian study that reported that the gut microbiome of people given probiotics after antibiotics took six months to return to its normal state compared to only three weeks for those not given any probiotics. More studies are needed before a definite statement can be made. Continue reading
What to eat when you have a stomach virus?
When you have a stomach virus, it is best to eat bland and easy to-digest foods until your symptoms improve, such as:
- soda crackers (“saltines”)
- plain toast
- gelatin (“jello”)
- plain chicken
It’s best to stay away from caffeine, dairy, alcohol, high amounts of sugar, and fried or spicy foods until you feel better. Continue reading
Related medical questions
- Pepto-Bismol - How long will your stool be dark for?
- How to stop diarrhea - any medicine or remedy suggestions?
- My stool has changed color. What does it mean?
- Is using expired Pepto-Bismol a hazard or health risk?
- Over the Counter Medication for Pets
- How long does the flu last for?
- Can antibiotics cause diarrhea?
- What type of diarrhea does Aemcolo (rifamycin) treat?
- Why does metformin cause diarrhea?
- How long does Imodium stop diarrhea for?
- Can you take metformin without food?
- Can Flagyl be used to treat diarrhea?
- Does Flagyl cause diarrhea?
- Why is my poop green? What does this mean?
- Why does Ofev cause diarrhea?
- What type of pain does fibromyalgia cause?
- If I am Lactose Intolerant or Lactose Allergic, are there Medications I should Avoid?
- I think I have an allergy to my antibiotic! What can I do to treat my infection?
- What's the buzz on Ozempic and Wegovy?
- When does diarrhea start when taking Nerlynx?
- What OTC drugs relieve tripledemic symptoms in kids?
- What are some tips for treating diarrhea?
- What do I need to know about Medications/Vaccinations before I Travel?
- Oral Chemotherapy at Home
Drug information
- Pepto-Bismol Information for Consumers
- Side Effects of Pepto-Bismol (detailed)
Related support groups
- Pepto-Bismol (29 questions, 16 members)
- Diarrhea (208 questions, 393 members)
- Indigestion (44 questions, 87 members)
- Traveler's Diarrhea (9 questions, 5 members)
Medical Disclaimer
- What are the new treatment options for migraines?
- CGRP Inhibitors - what are they?
- How quickly can acute migraines be treated?

Symptoms of virus sweeping the UK after 'do not go to work' warning
T he UK Health Security Agency has issued an alert after thousands of cases of norovirus - 75% higher than would normally be found at this time of year. The agency said anyone who catches it should stay home, in a bid to stop the spread.
Amy Douglas, Norovirus Epidemiologist at UKHSA said: “Norovirus levels were higher in April than we would usually see at this time of year and have been increasing. This is likely due to a combination of factors, but the colder weather we have had won’t have helped.
“Norovirus can cause dehydration, especially in vulnerable groups such as young children and older or immunocompromised people, so if you do get ill it is important to drink plenty of fluids. If you have got diarrhoea and vomiting, you can take steps to avoid passing the infection on. Do not return to work, school or nursery until 48 hours after your symptoms have stopped and don’t prepare food for others in that time either."
Norovirus is a highly contagious virus that causes gastroenteritis, which is an inflammation of the stomach and intestines. The symptoms of norovirus typically include:
Nausea : A feeling of discomfort in the stomach that may be accompanied by an urge to vomit.
Vomiting : Often sudden and profuse, vomiting is a common and prominent symptom.
Diarrhoea : Watery and often frequent bowel movements are a hallmark of norovirus infection.
Stomach Cramps : Abdominal pain or cramps can occur and may range from mild to severe.
Low-Grade Fever : Some individuals may experience a slight fever.
Muscle Pain : Generalized body aches or muscle pain can occur, although it is less common.
Fatigue : The infection can lead to a feeling of overall weakness and tiredness.
Headache : Some individuals may experience a headache during the course of the infection.
Symptoms usually develop 12 to 48 hours after exposure to the virus and typically last for 1 to 3 days. In some cases, especially in young children, older adults, and individuals with weakened immune systems, symptoms can be more severe and last longer.
Norovirus is highly contagious and spreads easily through contaminated food, water, surfaces, and close contact with infected individuals. Good hygiene practices, such as frequent handwashing and proper food handling, are crucial in preventing the spread of norovirus.


IMAGES
VIDEO
COMMENTS
Norovirus: By far the most common form of stomach flu is norovirus infection, which causes inflammation of the stomach and intestines. Symptoms set on within 24 to 48 hours of exposure and usually resolve within 24 to 72 hours. It can affect people of all ages. Rotavirus: Primarily affecting infants and children under age 5 (though adults also catch milder forms), rotavirus causes vomiting and ...
Diagnosis. Your doctor will likely diagnose viral gastroenteritis (stomach flu) based on symptoms, a physical exam and sometimes on the presence of similar cases in your community. A rapid stool test can detect rotavirus or norovirus, but there are no quick tests for other viruses that cause gastroenteritis.
The flu (influenza) affects only your respiratory system — your nose, throat and lungs. Gastroenteritis, on the other hand, attacks your intestines, causing signs and symptoms such as: Watery, usually nonbloody diarrhea — bloody diarrhea usually means you have a different, more severe infection. Nausea, vomiting or both. Stomach cramps and ...
Adults with the stomach flu can replenish lost fluids by consuming liquids like: Broth. Juice. Sports drinks with electrolytes. Water. Children, people with severe diarrhea and vomiting, and older ...
Diarrhea. Nausea and vomiting. Loss of appetite. Abdominal pain and cramping. These symptoms come from inflammation in your stomach and intestines. (Although the name, gastroenteritis, refers to your stomach and small intestine, inflammation can spread to your large intestine, too). Inflammation is your immune system activating to fight the virus.
This can cause belly pain, cramping, nausea, vomiting, and diarrhea. The cause is typically inflammation triggered by your immune system's response to a viral or bacterial infect ion. However ...
Read the script. Dr. Allen says if you experience nausea and vomiting, diarrhea and stomach pain — all symptoms of norovirus — drink lots of fluids and follow a bland diet like crackers, or broth or flavored water. This bland diet is well-tolerated by some people. For the first couple of days, you may not feel like eating or drinking, and ...
To help keep yourself more comfortable and prevent dehydration while you recover, try the following: Let your stomach settle. Stop eating solid foods for a few hours. Try sucking on ice chips or taking small sips of water. You might also try drinking clear soda, clear broths or noncaffeinated sports drinks.
Some may also help ease stomach upset from other sources, such as irritable bowel syndrome. 1. Drinking water. The body needs water to efficiently digest and absorb nutrients from foods and ...
When you have viral gastroenteritis, you need to replace lost fluids and electrolytes to prevent dehydration or treat mild dehydration. You should drink plenty of liquids. If vomiting is a problem, try sipping small amounts of clear liquids. Most adults with viral gastroenteritis can replace fluids and electrolytes with liquids such as.
To help prevent the spread of stomach flu, the Centers for Disease Control and Prevention (CDC) recommends the following: thoroughly washing hands with soap and water. cleaning and disinfecting ...
Getting the flu shot does not prevent you from getting the stomach flu, but it does prevent you from getting influenza. "Stomach flu symptoms include stomach pain, nausea, vomiting and diarrhea," Miller says. "A low-grade fever, chills and muscle aches aren't uncommon to experience as well. Symptoms can start as little as 12 hours after ...
Rice. Graham crackers. Wheat toast. Oats. Advertisement. This is sometimes referred to as the BRAT (bananas, rice, applesauce, toast) diet. And it's important to note that the BRAT diet should ...
Drink adequate fluids to prevent dehydration. Adults and older children can drink sports drinks. Young children and babies can drink an oral rehydration solution such as Pedialyte. Avoid drinks with a lot of sugar, such as juices and sodas, which can worsen diarrhea. If you can keep food down:
Summary. Stomach pain and cramps are common symptoms of viral gastroenteritis, or stomach flu. Symptoms typically last around 1-3 days but may persist longer, depending on the cause. The above ...
Gastroenteritis, sometimes called stomach flu, is commonly caused by noroviruses and adenoviruses, but other viruses can also be responsible. Bacterial gastroenteritis is caused by common bacteria such as salmonella, E. coli, and c ampylobacter. It can also be caused by contaminated food and drinks 1. Symptoms of gastroenteritis
Supplements and medications may help. If you have post-infectious IBS, your doctor may recommend probiotics. These supplements help repopulate the small intestine with healthy flora, Dr. Kirsh ...
Exercise. Working out can help prevent constipation and gas pain. Even just getting up and walking about can help. The body retains more gas when supine (lying face upwards). Stomach Massage. A ...
Dr. Singh says there are certain symptoms you should never ignore. "Anytime you have severe, sudden onset of abdomen pain, you should contact your doctor immediately," he says. Other signs of a serious stomach issue are: Abdomen tenderness or swelling. Blood in your poop, urine or vomit. Persistent fever.
IBD can cause intestinal spasms that lead to stomach cramping, diarrhea, weight loss, and fatigue. Diverticulitis. is inflammation or infection of the diverticula (small pouches in the large ...
Symptoms of gastroenteritis. The main symptoms of gastroenteritis are: sudden, watery diarrhoea. feeling sick. vomiting, which can be projectile. a mild fever. Some people also have other symptoms, such as a loss of appetite, an upset stomach, aching limbs and headaches. The symptoms usually appear up to a day after becoming infected.
Here are six signs you might have an autoimmune disease. 1. You're ridiculously fatigued or constantly feel like you're coming down with the flu. When you've got an infection, your body ...
People with an active stomach ulcer, a bleeding problem, or who have bloody or black stools; Children or teens who are recovering from chickenpox or flu-like symptoms because of the risk of a serious illness called Reye's syndrome; Pregnant women; Additionally, if you have a fever or mucus in your stool, ask your doctor before using Pepto-Bismol.
Stomach Cramps: Abdominal pain or cramps can occur and may range from mild to severe. Low-Grade Fever : Some individuals may experience a slight fever. Muscle Pain : Generalized body aches or ...