161 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.

Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
July 23, 2024
Surviving The Boston Marathon Bombings While Facing TBI and Medical Gaslighting
“As I literally lived on his couch, with my port-a-potty in his living room, my partner eventually applied for permanent disability status for me. But, even then doctor gaslighted me, told me I was physically able to work, and reported the same to the government. In reality, I was so dizzy with vertigo, this same doctor refused to let me walk to and from our car, by myself, fearing I’d fall and sue!”
Struggled with: CPTSD Traumatic Brain Injury
Helped by: Treatment
July 16, 2024
Somatic Therapy Helped Me Heal From CPTSD After Years of Childhood Abuse
“At 22 years old, I knew that I was dying of alcoholism. I accepted that. The trauma symptoms I experienced were too overwhelming to stop drinking. When I was sober, I would sometimes experience 30 to 40 body memories of being sexually assaulted–again and again in succession. I drank to feel numb.”
Struggled with: Abuse Addiction CPTSD Suicidal
Helped by: Social support Therapy
July 9, 2024
Learning To Live With Irritable Bowel Syndrome With Therapy And A Positive Mindset
“Raising four young children and battling a chronic illness with no cure was challenging for me. On the outside, I looked OK. But I wasn’t and in some ways today still have flare-ups and struggles, the difference is, I now know how to maintain it, especially knowing this will be the rest of my life regardless!”
Struggled with: Irritable Bowel Syndrome
Helped by: Therapy Treatment
July 4, 2024
How A Rescue Dog Helped Me Overcome TBI, Depression and Suicidal Ideation
“I sat on the summer-hot pavement, and no one stopped or asked me if I was okay. No one called the police. People walked around me as quickly as possible. When I was all cried out, I walked home to my empty house. I bought a set of knives, ostensibly for cooking, but that was not the reason. I had thought about pills, and every day I researched how many of each prescription drug I was on would I need to take to die. Using a sharp knife seemed so much easier.”
Struggled with: Depression Suicidal Traumatic Brain Injury
Helped by: Medication Pets Volunteering
July 2, 2024
Walking El Camino de Santiago Helped Me Reconnect With My Authentic Self
“Beneath the outward bravado, I battled with self-doubt and kept wondering why genuine connections seemed beyond my ability. Even though I put out valiant efforts to conceal it, my inner turmoil seeped out, leaving me feeling exposed and vulnerable. And, I knew they could tell.”
Struggled with: Feeling lost People-pleasing Self-doubt
Helped by: Self-acceptance Self-awareness
June 27, 2024
My Journey of Overcoming Heartbreak Thanks to Self-Care and The Support Of Friends
“I’ve learned that finding the right people to confide in, those who offer genuine support and empathy, can make a significant difference in navigating these challenges. It takes time and trust to build those connections, but they are invaluable.”
Struggled with: Breakup
Helped by: Self-Care Social support
June 19, 2024
How Therapy, Self-Help and Medication Help Me Live With Depression and Anxiety
“When the next depressive episode hit in 2018, I was devastated. How could this happen again when I thought I had it all figured out? I experienced some of the darkest moments of my life and a nearly complete loss of hope.”
Struggled with: Anxiety Bipolar Disorder Depression Suicidal
Helped by: Medication Therapy
June 11, 2024
Sharing My Journey From Alcohol and Substance Abuse to Sobriety and Happiness
“I felt prettier, smarter, funnier when alcohol entered my body so I simply continued numbing through the years. The progression of this disease of alcoholism turned into a nasty drug habit and those feelings of insecurity turned into deep darkness when I was “off my meds”. Or in other words, without alcohol or drugs.”
Struggled with: Addiction Depression Suicidal
Helped by: Rehab Therapy
June 4, 2024
Finding Happiness and Self-Love After Escaping Death From Burning 90% Of My Body
“It was like starting life over again, except you know how to do things you physically can’t do, which emotionally drains you. There was definitely a sense of resentment and feeling sorry for myself, I think that is natural. You wonder what you did to deserve that, you wonder if things are ever going to get better, you wonder how people will treat you. When you are confined to a bed for weeks on end, really all you can do is wonder.”
Struggled with: Physical trauma
Helped by: Self-improvement Social support
May 28, 2024
Cognitive Reframing and Mindfulness Helped Me Overcome Depression and Suicidal Ideation
“After exploring ways to end my life, I resolved to slash my wrist. I retrieved a steak knife from the kitchen and pressed it against my skin. Yet, an unexpected sensation washed over me—a profound sense of peace, love, and joy.”
Struggled with: Depression Suicidal
Helped by: Meditation Mindfulness Self-improvement

Case Examples
Examples of recommended interventions in the treatment of depression across the lifespan.

Children/Adolescents
A 15-year-old Puerto Rican female
The adolescent was previously diagnosed with major depressive disorder and treated intermittently with supportive psychotherapy and antidepressants. Her more recent episodes related to her parents’ marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT).
Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response. Depression and Anxiety , 26, 98-103. https://doi.org/10.1002/da.20457
Sam, a 15-year-old adolescent
Sam was team captain of his soccer team, but an unexpected fight with another teammate prompted his parents to meet with a clinical psychologist. Sam was diagnosed with major depressive disorder after showing an increase in symptoms over the previous three months. Several recent challenges in his family and romantic life led the therapist to recommend interpersonal psychotherapy for adolescents (IPT-A).
Hall, E.B., & Mufson, L. (2009). Interpersonal Psychotherapy for Depressed Adolescents (IPT-A): A Case Illustration. Journal of Clinical Child & Adolescent Psychology, 38 (4), 582-593. https://doi.org/10.1080/15374410902976338
© Society of Clinical Child and Adolescent Psychology (Div. 53) APA, https://sccap53.org/, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of the Society of Clinical Child and Adolescent Psychology (Div. 53) APA.
General Adults
Mark, a 43-year-old male
Mark had a history of depression and sought treatment after his second marriage ended. His depression was characterized as being “controlled by a pattern of interpersonal avoidance.” The behavior/activation therapist asked Mark to complete an activity record to help steer the treatment sessions.
Dimidjian, S., Martell, C.R., Addis, M.E., & Herman-Dunn, R. (2008). Chapter 8: Behavioral activation for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 343-362). New York: Guilford Press.
Reprinted with permission from Guilford Press.
Denise, a 59-year-old widow
Denise is described as having “nonchronic depression” which appeared most recently at the onset of her husband’s diagnosis with brain cancer. Her symptoms were loneliness, difficulty coping with daily life, and sadness. Treatment included filling out a weekly activity log and identifying/reconstructing automatic thoughts.
Young, J.E., Rygh, J.L., Weinberger, A.D., & Beck, A.T. (2008). Chapter 6: Cognitive therapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: A step-by-step treatment manual (4th ed., pp. 278-287). New York, NY: Guilford Press.
Nancy, a 25-year-old single, white female
Nancy described herself as being “trapped by her relationships.” Her intake interview confirmed symptoms of major depressive disorder and the clinician recommended cognitive-behavioral therapy.
Persons, J.B., Davidson, J. & Tompkins, M.A. (2001). A Case Example: Nancy. In Essential Components of Cognitive-Behavior Therapy For Depression (pp. 205-242). Washington, D.C.: American Psychological Association. http://dx.doi.org/10.1037/10389-007
While APA owns the rights to this text, some exhibits are property of the San Francisco Bay Area Center for Cognitive Therapy, which has granted the APA permission for use.
Luke, a 34-year-old male graduate student
Luke is described as having treatment-resistant depression and while not suicidal, hoped that a fatal illness would take his life or that he would just disappear. His treatment involved mindfulness-based cognitive therapy, which helps participants become aware of and recharacterize their overwhelming negative thoughts. It involves regular practice of mindfulness techniques and exercises as one component of therapy.
Sipe, W.E.B., & Eisendrath, S.J. (2014). Chapter 3 — Mindfulness-Based Cognitive Therapy For Treatment-Resistant Depression. In R.A. Baer (Ed.), Mindfulness-Based Treatment Approaches (2nd ed., pp. 66-70). San Diego: Academic Press.
Reprinted with permission from Elsevier.
Sara, a 35-year-old married female
Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks.
Bleiberg, K.L., & Markowitz, J.C. (2008). Chapter 7: Interpersonal psychotherapy for depression. In D.H. Barlow (Ed.) Clinical handbook of psychological disorders: a treatment manual (4th ed., pp. 315-323). New York, NY: Guilford Press.
Peggy, a 52-year-old white, Italian-American widow
Peggy had a history of chronic depression, which flared during her husband’s illness and ultimate death. Guilt was a driving factor of her depressive symptoms, which lasted six months after his death. The clinician treated Peggy with psychodynamic therapy over a period of two years.
Bishop, J., & Lane , R.C. (2003). Psychodynamic Treatment of a Case of Grief Superimposed On Melancholia. Clinical Case Studies , 2(1), 3-19. https://doi.org/10.1177/1534650102239085
Several case examples of supportive therapy
Winston, A., Rosenthal, R.N., & Pinsker, H. (2004). Introduction to Supportive Psychotherapy . Arlington, VA : American Psychiatric Publishing.
Older Adults
Several case examples of interpersonal psychotherapy & pharmacotherapy
Miller, M. D., Wolfson, L., Frank, E., Cornes, C., Silberman, R., Ehrenpreis, L.…Reynolds, C. F., III. (1998). Using Interpersonal Psychotherapy (IPT) in a Combined Psychotherapy/Medication Research Protocol with Depressed Elders: A Descriptive Report With Case Vignettes. Journal of Psychotherapy Practice and Research , 7(1), 47-55.
Social Work Practice with Carers

Case Study 2: Josef
Download the whole case study as a PDF file
Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently.
This case study looks at the impact of caring for someone with a mental health problem and of being a young carer , in particular the impact on education and future employment .
When you have looked at the materials for the case study and considered these topics, you can use the critical reflection tool and the action planning tool to consider your own practice.
- One-page profile
Support plan
Transcript (.pdf, 48KB)
Name : Josef Mazur
Gender : Male
Ethnicity : White European
Download resource as a PDF file
First language : English/ Polish
Religion : Roman Catholic
Josef lives in a small town with his mother Dorota who is 39. Dorota was diagnosed with Bi-polar disorder seven years ago after she was admitted to hospital. She is currently unable to work. Josef’s father, Stefan, lives in the same town and he sees him every few weeks. Josef was born in England. His parents are Polish and he speaks Polish at home.
Josef is doing a foundation art course at college. Dorota is quite isolated because she often finds it difficult to leave the house. Dorota takes medication and had regular visits from the Community Psychiatric Nurse when she was diagnosed and support from the Community Mental Health team to sort out her finances. Josef does the shopping and collects prescriptions. He also helps with letters and forms because Dorota doesn’t understand all the English. Dorota gets worried when Josef is out. When Dorota is feeling depressed, Josef stays at home with her. When Dorota is heading for a high, she tries to take Josef to do ‘exciting stuff’ as she calls it. She also spends a lot of money and is very restless.
Josef worries about his mother’s moods. He is worried about her not being happy and concerned at the money she spends when she is in a high mood state. Josef struggles to manage his day around his mother’s demands and to sleep when she is high. Josef has not told anyone about the support he gives to his mother. He is embarrassed by some of the things she does and is teased by his friends, and he does not think of himself as a carer. Josef has recently had trouble keeping up with course work and attendance. He has been invited to a meeting with his tutor to formally review attendance and is worried he will get kicked out. Josef has some friends but he doesn’t have anyone he can confide in. His father doesn’t speak to his mother.
Josef sees some information on line about having a parent with a mental health problem. He sends a contact form to ask for information. Someone rings him and he agrees to come into the young carers’ team and talk to the social worker. You have completed the assessment form with Josef in his words and then done a support plan with him.
Back to Summary
Josef Mazur
What others like and admire about me
Good at football
Finished Arkham Asylum on expert level
What is important to me
Mum being well and happy
Seeing my dad
Being an artist
Seeing my friends
How best to support me
Tell me how to help mum better
Don’t talk down to me
Talk to me 1 to 1
Let me know who to contact if I am worried about something
Work out how I can have some time on my own so I can do my college work and see my friends
Don’t tell mum and my friends
Date chronology completed : 7 March 2016
Date chronology shared with person: 7 March 2016
| 1997 | Josef’s mother and father moved to England from Poznan. | Both worked at the warehouse – Father still works there. |
| 11.11.1999 | Josef born. | Mother worked for some of the time that Josef was young. |
| 2006 | Josef reports that his mother and father started arguing about this time because of money and Josef’s mother not looking after household tasks. | Josef started doing household tasks e.g. cleaning, washing and ironing. |
| 2008 | Josef reports that his mother didn’t get out of bed for a few months. | Josef managed the household during this period. |
| October 2008 | Josef reports that his mother spent lots of money in catalogues and didn’t sleep. She was admitted to hospital. | Mother was in hospital for 6 weeks and was diagnosed with bipolar disorder. Josef began looking after his mother’s medication and says that he started to ‘keep an eye on her.’ |
| May 2010 | Josef’s father moved out to live with his friend Kat. Josef stayed with his mother. | Josef reports that his mother was ‘really sad for a while and then she went round and shouted at them.’ Mother started on different medication and had regular visits from the Community Psychiatric Nurse. Josef said that the CPN told him about his mum’s illness and to let him know if he needed any help but he was managing ok. Josef saw his father every week for a few years and then it was more like every month. Father does not visit Josef or speak to his mother. |
| 2013/14 | Josef reports that his mother got into a lot of debt and they had eviction letters. | Josef’s father paid some of the bills and his mother was referred by the Community Mental Health Team for advice from CAB and started getting benefits. Josef started doing the correspondence. |
| 2015 | Josef left school and went to college. | Josef got an A (art), 4 Cs and 3 Ds GCSE. He says that he ‘would have done better but I didn’t do much work.’ |
| 26 Feb 2016 | Josef got a letter from his tutor at college saying he had to go to a formal review about attendance. | Josef saw information on-line about having a parent with a mental health problem and asked for some information. |
| 2 March 2016 | Phone call from young carer’s team to Josef. | Josef agreed to come in for an assessment. |
| 4 March 2016 | Social worker meets with Josef. | Carer’s assessment and support plan completed. |
| 7 March 2016 | Paperwork completed. | Sent to Josef. |
Young Carers Assessment
Do you look after or care for someone at home?
The questions in this paper are designed to help you think about your caring role and what support you might need to make your life a little easier or help you make time for more fun stuff.
Please feel free to make notes, draw pictures or use the form however is best for you.
What will happen to this booklet?
This is your booklet and it is your way to tell an adult who you trust about your caring at home. This will help you and the adult find ways to make your life and your caring role easier.
The adult who works with you on your booklet might be able to help you with everything you need. If they can’t, they might know other people who can.
Our Agreement
- I will share this booklet with people if I think they can help you or your family
- I will let you know who I share this with, unless I am worried about your safety, about crime or cannot contact you
- Only I or someone from my team will share this booklet
- I will make sure this booklet is stored securely
- Some details from this booklet might be used for monitoring purposes, which is how we check that we are working with everyone we should be
Signed: ___________________________________
Young person:
- I know that this booklet might get shared with other people who can help me and my family so that I don’t have to explain it all over again
- I understand what my worker will do with this booklet and the information in it (written above).
Signed: ____________________________________
Name : Josef Mazur Address : 1 Green Avenue, Churchville, ZZ1 Z11 Telephone: 012345 123456 Email: [email protected] Gender : Male Date of birth : 11.11.1999 Age: 16 School : Green College, Churchville Ethnicity : White European First language : English/ Polish Religion : Baptised Roman Catholic GP : Dr Amp, Hill Surgery
The best way to get in touch with me is:
Do you need any support with communication?
*Josef is bilingual – English and Polish. He speaks English at school and with his friends, and Polish at home. Josef was happy to have this assessment in English, however, another time he may want to have a Polish interpreter. It will be important to ensure that Josef is able to use the words he feels best express himself.
About the person/ people I care for
I look after my mum who has bipolar disorder. Mum doesn’t work and doesn’t really leave the house unless she is heading for a high. When Mum is sad she just stays at home. When she is getting hyper then she wants to do exciting stuff and she spends lots of money and she doesn’t sleep.
Do you wish you knew more about their illness?
Do you live with the person you care for?
What I do as a carer It depends on if my mum has a bad day or not. When she is depressed she likes me to stay home with her and when she is getting hyper then she wants me to go out with her. If she has new meds then I like to be around. Mum doesn’t understand English very well (she is from Poland) so I do all the letters. I help out at home and help her with getting her medication.
Tell us what an average week is like for you, what kind of things do you usually do?
Monday to Friday
Get up, get breakfast, make sure mum has her pills, tell her to get up and remind her if she’s got something to do.
If mum hasn’t been to bed then encourage her to sleep a bit and set an alarm
College – keep phone on in case mum needs to call – she usually does to ask me to get something or check when I’m coming home
Go home – go to shops on the way
Remind mum about tablets, make tea and pudding for both of us as well as cleaning the house and fitting tea in-between, ironing, hoovering, hanging out and bringing in washing
Do college work when mum goes to bed if not too tired
More chores
Do proper shop
Get prescription
See my friends, do college work
Sunday – do paper round
Physical things I do….
(for example cooking, cleaning, medication, shopping, dressing, lifting, carrying, caring in the night, making doctors appointments, bathing, paying bills, caring for brothers & sisters)
I do all the housework and shopping and cooking and get medication
Things I find difficult
Emotional support I provide…. (please tell us about the things you do to support the person you care for with their feelings; this might include, reassuring them, stopping them from getting angry, looking after them if they have been drinking alcohol or taking drugs, keeping an eye on them, helping them to relax)
If mum is stressed I stay with her
If mum is depressed I have to keep things calm and try to lighten the mood
She likes me to be around
When mum is heading for a high wants to go to theme parks or book holidays and we can’t afford it
I worry that mum might end up in hospital again
Mum gets cross if I go out
Other support
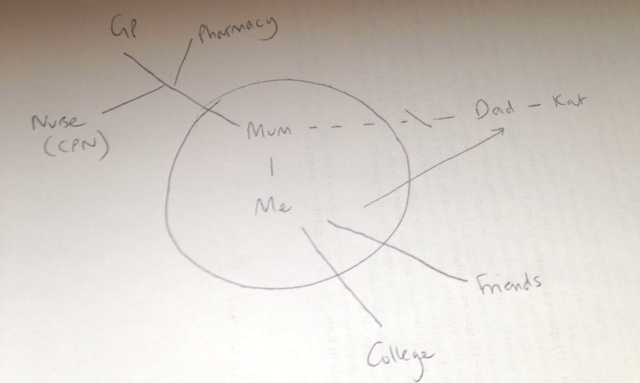
Please tell us about any other support the person you care for already has in place like a doctor or nurse, or other family or friends.
The GP sees mum sometimes. She has a nurse who she can call if things get bad.
Mum’s medication comes from Morrison’s pharmacy.
Dad lives nearby but he doesn’t talk to mum.
Mum doesn’t really have any friends.
Do you ever have to stop the person you care for from trying to harm themselves or others?
Some things I need help with
Sorting out bills and having more time for myself
I would like mum to have more support and to have some friends and things to do
On a normal week, what are the best bits? What do you enjoy the most? (eg, seeing friends, playing sports, your favourite lessons at school)
Seeing friends
When mum is up and smiling
Playing football
On a normal week, what are the worst bits? What do you enjoy the least? (eg cleaning up, particular lessons at school, things you find boring or upsetting)
Nagging mum to get up
Reading letters
Missing class
Mum shouting
Friends laugh because I have to go home but they don’t have to do anything
What things do you like to do in your spare time?
Do you feel you have enough time to spend with your friends or family doing things you enjoy, most weeks?
Do you have enough time for yourself to do the things you enjoy, most weeks? (for example, spending time with friends, hobbies, sports)
Are there things that you would like to do, but can’t because of your role as a carer?
Can you say what some of these things are?
See friends after college
Go out at the weekend
Time to myself at home
It can feel a bit lonely
I’d like my mum to be like a normal mum
School/ College Do you think being your caring role makes school/college more difficult for you in any way?
If you ticked YES, please tell us what things are made difficult and what things might help you.
Things I find difficult at school/ college
Sometimes I get stressed about college and end up doing college work really late at night – I get a bit angry when I’m stressed
I don’t get all my college work done and I miss days
I am tired a lot of the time
Things I need help with…
I am really worried they will kick me out because I am behind and I miss class. I have to meet my tutor about it.
Do your teachers know about your caring role?
Are you happy for your teachers and other staff at school/college to know about your caring role?
Do you think that being a carer will make it more difficult for you to find or keep a job?
Why do you think being a carer is/ will make finding a job more difficult?
I haven’t thought about it. I don’t know if I’ll be able to finish my course and do art and then I won’t be able to be an artist.
Who will look after mum?
What would make it easier for you to find a job after school/college?
Finishing my course
Mum being ok
How I feel about life…
Do you feel confident both in school and outside of school?
Somewhere in the middle
In your life in general, how happy do you feel?
Quite unhappy
In your life in general, how safe do you feel?
How healthy do you feel at the moment?
Quite healthy
Being heard
Do you think people listen to what you are saying and how you are feeling?
If you said no, can you tell us who you feel isn’t listening or understanding you sometimes (eg, you parents, your teachers, your friends, professionals)
I haven’t told anyone
I can’t talk to mum
My friends laugh at me because I don’t go out
Do you think you are included in important decisions about you and your life? (eg, where you live, where you go to school etc)
Do you think that you’re free to make your own choices about what you do and who you spend your time with?
Not often enough
Is there anybody who knows about the caring you’re doing at the moment?
If so, who?
I told dad but he can’t do anything
Would you like someone to talk to?
Supporting me Some things that would make my life easier, help me with my caring or make me feel better
I don’t know
Fix mum’s brain
People to help me if I’m worried and they can do something about it
Not getting kicked out of college
Free time – time on my own to calm down and do work or have time to myself
Time to go out with my friends
Get some friends for mum
I don’t want my mum to get into trouble
Who can I turn to for advice or support?
I would like to be able to talk to someone without mum or friends knowing
Would you like a break from your caring role?
How easy is it to see a Doctor if you need to?
To be used by social care assessors to consider and record measures which can be taken to assist the carer with their caring role to reduce the significant impact of any needs. This should include networks of support, community services and the persons own strengths. To be eligible the carer must have significant difficulty achieving 1 or more outcomes without support; it is the assessors’ professional judgement that unless this need is met there will be a significant impact on the carer’s wellbeing. Social care funding will only be made available to meet eligible outcomes that cannot be met in any other way, i.e. social care funding is only available to meet unmet eligible needs.
Date assessment completed : 7 March 2016
Social care assessor conclusion
Josef provides daily support to his mum, Dorota, who was diagnosed with bipolar disorder seven years ago. Josef helps Dorota with managing correspondence, medication and all household tasks including shopping. When Dorota has a low mood, Josef provides support and encouragement to get up. When Dorota has a high mood, Josef helps to calm her and prevent her spending lots of money. Josef reports that Dorota has some input from community health services but there is no other support. Josef’s dad is not involved though Josef sees him sometimes, and there are no friends who can support Dorota.
Josef is a great support to his mum and is a loving son. He wants to make sure his mum is ok. However, caring for his mum is impacting: on Josef’s health because he is tired and stressed; on his emotional wellbeing as he can get angry and anxious; on his relationship with his mother and his friends; and on his education. Josef is at risk of leaving college. Josef wants to be able to support his mum better. He also needs time for himself, to develop and to relax, and to plan his future.
Eligibility decision : Eligible for support
What’s happening next : Create support plan
Completed by Name : Role : Organisation :
Name: Josef Mazur
Address 1 Green Avenue, Churchville, ZZ1 Z11
Telephone 012345 123456
Email [email protected]
Gender: Male
Date of birth: 11.11.1999 Age: 16
School Green College, Churchville
Ethnicity White European
First language English/ Polish
Religion Baptised Roman Catholic
GP Dr Amp, Hill Surgery
My relationship to this person son
Name Dorota Mazur
Gender Female
Date of birth 12.6.79 Age 36
First language Polish
Religion Roman Catholic
Support plan completed by
Organisation
|
|
| |
|
|
| |
|
| ||
|
| ||
Date of support plan: 7 March 2016
This plan will be reviewed on: 7 September 2016
Signing this form
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Josef has given consent to share this support plan with the CPN but does not want it to be shared with his mum.
Mental health
The social work role with carers in adult mental health services has been described as: intervening and showing professional leadership and skill in situations characterised by high levels of social, family and interpersonal complexity, risk and ambiguity (Allen 2014). Social work with carers of people with mental health needs, is dependent on good practice with the Mental Capacity Act where practitioner knowledge and understanding has been found to be variable (Iliffe et al 2015).
- Carers Trust (2015) Mental Health Act 1983 – Revised Code of Practice Briefing
- Carers Trust (2013) The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England
- Mind, Talking about mental health
- Tool 1: Triangle of care: self-assessment for mental health professionals – Carers Trust (2013) The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England Second Edition (page 23 Self-assessment tool for organisations)
Mental capacity, confidentiality and consent
Social work with carers of people with mental health needs, is dependent on good practice with the Mental Capacity Act where practitioner knowledge and understanding has been found to be variable (Iliffe et al 2015). Research highlights important issues about involvement, consent and confidentiality in working with carers (RiPfA 2016, SCIE 2015, Mental Welfare Commission for Scotland 2013).
- Beddow, A., Cooper, M., Morriss, L., (2015) A CPD curriculum guide for social workers on the application of the Mental Capacity Act 2005 . Department of Health
- Bogg, D. and Chamberlain, S. (2015) Mental Capacity Act 2005 in Practice Learning Materials for Adult Social Workers . Department of Health
- Department of Health (2015) Best Interest Assessor Capabilities , The College of Social Work
- RiPfA Good Decision Making Practitioner Handbook
- SCIE Mental Capacity Act resource
- Tool 2: Making good decisions, capacity tool (page 70-71 in good decision making handbook)
Young carers
A young carer is defined as a person under 18 who provides or intends to provide care for another person. The concept of care includes practical or emotional support. It is the case that this definition excludes children providing care as part of contracted work or as voluntary work. However, the local authority can ignore this and carry out a young carer’s need assessment if they think it would be appropriate. Young carers, young adult carers and their families now have stronger rights to be identified, offered information, receive an assessment and be supported using a whole-family approach (Carers Trust 2015).
- SCIE (2015) Young carer transition in practice under the Care Act 2014
- SCIE (2015) Care Act: Transition from children’s to adult services – early and comprehensive identification
- Carers Trust (2015) Rights for young carers and young adult carers in the Children and Families Act
- Carers Trust (2015) Know your Rights: Support for Young Carers and Young Adult Carers in England
- The Children’s Society (2015) Hidden from view: The experiences of young carers in England
- DfE (2011) Improving support for young carers – family focused approaches
- ADASS and ADCS (2015) No wrong doors: working together to support young carers and their families
- Carers Trust, Supporting Young Carers and their Families: Examples of Practice
- Refugee toolkit webpage: Children and informal interpreting
- SCIE (2010) Supporting carers: the cared for person
- SCIE (2015) Care Act Transition from children’s to adults’ services – Video diaries
- Tool 3: Young carers’ rights – The Children’s Society (2014) The Know Your Rights pack for young carers in England!
- Tool 4: Vision and principles for adults’ and children’s services to work together
Young carers of parents with mental health problems
The Care Act places a duty on local authorities to assess young carers before they turn 18, so that they have the information they need to plan for their future. This is referred to as a transition assessment. Guidance, advocating a whole family approach, is available to social workers (LGA 2015, SCIE 2015, ADASS/ADCS 2011).
- SCIE (2012) At a glance 55: Think child, think parent, think family: Putting it into practice
- SCIE (2008) Research briefing 24: Experiences of children and young people caring for a parent with a mental health problem
- SCIE (2008) SCIE Research briefing 29: Black and minority ethnic parents with mental health problems and their children
- Carers Trust (2015) The Triangle of Care for Young Carers and Young Adult Carers: A Guide for Mental Health Professionals
- ADASS and ADCS (2011) Working together to improve outcomes for young carers in families affected by enduring parental mental illness or substance misuse
- Ofsted (2013) What about the children? Joint working between adult and children’s services when parents or carers have mental ill health and/or drug and alcohol problems
- Mental health foundation (2010) MyCare The challenges facing young carers of parents with a severe mental illness
- Children’s Commissioner (2012) Silent voices: supporting children and young people affected by parental alcohol misuse
- SCIE, Parental mental health and child welfare – a young person’s story
Tool 5: Family model for assessment
- Tool 6: Engaging young carers of parents with mental health problems or substance misuse
Young carers and education/ employment
Transition moments are highlighted in the research across the life course (Blythe 2010, Grant et al 2010). Complex transitions required smooth transfers, adequate support and dedicated professionals (Petch 2010). Understanding transition theory remains essential in social work practice (Crawford and Walker 2010). Partnership building expertise used by practitioners was seen as particular pertinent to transition for a young carer (Heyman 2013).
- TLAP (2013) Making it real for young carers
- Learning and Work Institute (2018) Barriers to employment for young adult carers
- Carers Trust (2014) Young Adult Carers at College and University
- Carers Trust (2013) Young Adult Carers at School: Experiences and Perceptions of Caring and Education
- Carers Trust (2014) Young Adult Carers and Employment
- Family Action (2012) BE BOTHERED! Making Education Count for Young Carers

Download The Triangle of Care as a PDF file
The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England
The Triangle of Care is a therapeutic alliance between service user, staff member and carer that promotes safety, supports recovery and sustains wellbeing…

Download the Capacity Tool as a PDF file
Capacity Tool Good decision-making Practitioners’ Handbook
The Capacity tool on page 71 has been developed to take into account the lessons from research and the case CC v KK. In particular:
- that capacity assessors often do not clearly present the available options (especially those they find undesirable) to the person being assessed
- that capacity assessors often do not explore and enable a person’s own understanding and perception of the risks and advantages of different options
- that capacity assessors often do not reflect upon the extent to which their ‘protection imperative’ has influenced an assessment, which may lead them to conclude that a person’s tolerance of risks is evidence of incapacity.
The tool allows you to follow steps to ensure you support people as far as possible to make their own decisions and that you record what you have done.

Download Know your rights as a PDF file
Tool 3: Know Your Rights Young Carers in Focus
This pack aims to make you aware of your rights – your human rights, your legal rights, and your rights to access things like benefits, support and advice.
Need to know where to find things out in a hurry? Our pack has lots of links to useful and interesting resources that can help you – and help raise awareness about young carers’ issues!
Know Your Rights has been produced by Young Carers in Focus (YCiF), and funded by the Big Lottery Fund.
Tool 4: Vision and principles for adults’ and children’s services to work together to support young carers
Download the tool as a PDF file
You can use this tool to consider how well adults’ and children’s services work together, and how to improve this.
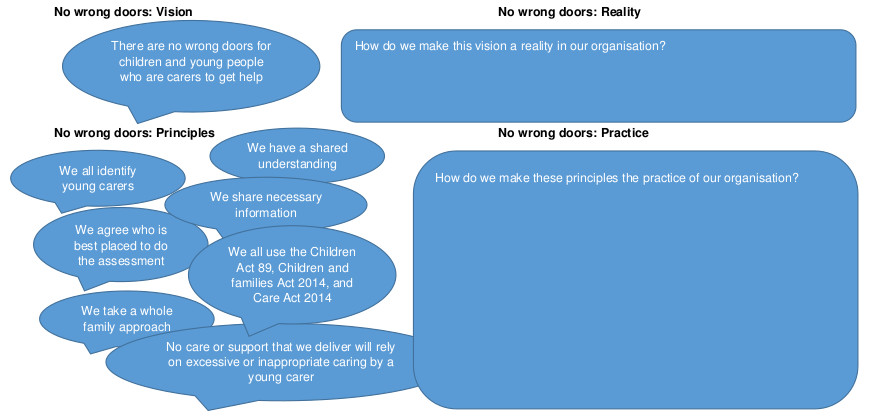
Click on the diagram to open full size in a new window
This is based on ADASS and ADCS (2015) No wrong doors : working together to support young carers and their families
Download the tool as a PDF file
You can use this tool to help you consider the whole family in an assessment or review.
What are the risk, stressors and vulnerability factors?
How is the child/ young person’s wellbeing affected?
How is the adult’s wellbeing affected?

What are the protective factors and available resources?
This tool is based on SCIE (2009) Think child, think parent, think family: a guide to parental mental health and child welfare
Tool 6: Engaging young carers
Young carers have told us these ten things are important. So we will do them.
- Introduce yourself. Tell us who you are and what your job is.
- Give us as much information as you can.
- Tell us what is wrong with our parents.
- Tell us what is going to happen next.
- Talk to us and listen to us. Remember it is not hard to speak to us we are not aliens.
- Ask us what we know and what we think. We live with our parents; we know how they have been behaving.
- Tell us it is not our fault. We can feel guilty if our mum or dad is ill. We need to know we are not to blame.
- Please don’t ignore us. Remember we are part of the family and we live there too.
- Keep on talking to us and keeping us informed. We need to know what is happening.
- Tell us if there is anyone we can talk to. Maybe it could be you.

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility


A two-way street: Mental health can’t be ignored during work injury recovery
Assistant Professor, John Molson School of Business, Concordia University
Professor of Organizational Behaviour and Future Fund Chair in Leadership, Haskayne School of Business, University of Calgary
Disclosure statement
Steve Granger receives research funding from the Social Sciences and Humanities Research Council of Canada.
Nick Turner currently receives research funding from Cenovus Energy Inc., Mitacs, and the Social Sciences and Humanities Research Council of Canada.
Concordia University and University of Calgary provide funding as founding partners of The Conversation CA.
Universitié Concordia provides funding as a founding partner of The Conversation CA-FR.
University of Calgary provides funding as a member of The Conversation CA-FR.
View all partners
Discussions about mental health in the workplace have surged lately, driven by growing awareness of its impact on employee and organizational success . As occupational health researchers, these discussions have helped us shed light on the precursors and consequences of mental health challenges.
One such critical but often overlooked aspect is the relationship between mental health challenges and work injuries — a relationship that goes in both directions : struggling with mental health can increase the risk of work injuries, and work injuries can give rise to, or worsen, mental health challenges.
We aimed to shed light on this crucial bidirectional relationship because it undermines the sustainability of an organization’s most crucial asset: its people.
Mental health and work injuries
Mental health challenges and work injuries result in significant costs for organizations and society, and tremendous suffering among individuals and their families, workplaces and wider support systems.
While the costs for work injuries and mental health challenges vary widely, evidence indicates that experiencing both together can multiply medical expenses and time loss from two to 10 times.
Despite their impact, the critical relationship between work injuries and mental health challenges has only been examined sporadically across diverse disciplines, which rarely communicate with each other — until now.

Our comprehensive meta-analysis , involving a worldwide sample of more than 1.4 million participants across 147 studies conducted since 1988, highlights the need for integrated approaches to address physical and psychological well-being in the workplace.
Meta-analytical studies like ours are valuable because they involve systematically gathering and summarizing all existing quantitative research. This approach helps us consolidate and distil the findings from multiple studies, providing a clearer picture of what we currently understand.
Our findings reveal that the relationship between work injuries and mental health depends on whether someone expriences mental health challenges or workplace injuries first. A stronger, more robust relationship emerges when work injuries precede mental health challenges, while a smaller, but still significant, association exists when mental health challenges precede work injuries.
The hidden toll of work injuries
When a work injury occurs, the immediate focus is on physical recovery. However, the psychological impact of injuries shouldn’t be neglected.
The sudden disruption caused by a work injury can lead to increased stress, anxiety and depression. This psychological distress can stem from various factors, including pain, stigma and uncertainty about one’s ability to continue earning a living.
Our analysis indicates that negative thoughts, such as rumination, commonly arise after work injuries. They play a significant role in the development of mental health challenges. These negative thoughts can lead to a downward spiral, mentally trapping an injured individual in their situation and further hindering their recovery process.
Interestingly, the relationship is not one-way. Our research also shows that mental health challenges are associated with an increased likelihood of sustaining a work injury.
Individuals struggling with mental health often experience reduced cognitive functioning, increased distractibility and impaired decision-making abilities, making regular job duties increasingly overwhelming and difficult to manage. These factors can lead to a higher risk of injuries at work.
For example, an employee dealing with severe depression might have difficulty concentrating on tasks, increasing the risk of overlooking emerging hazards or misjudging dangerous situations.
The stigma associated with their mental health condition might also prevent the employee from seeking the help or accommodations they need, further increasing their vulnerability to work injuries.
Breaking the vicious cycle
The interconnected nature of work injuries and mental health challenges highlights the need for comprehensive rehabilitation approaches. Integrating psychological care into the rehabilitation process is crucial for promoting overall well-being and preventing the recurrence of injuries.
Employers and policymakers should consider implementing programs that address both the physical and mental health needs of employees. This includes providing access to and awareness of mental health services , promoting a safe and supportive work environment and implementing strategies to reduce workplace stress.

By taking a human sustainability approach that emphasizes physical, psychological and social health through prevention rather than reaction, it’s possible to break the cycle of work injuries and mental health challenges. This could ultimately lead to healthier and more productive workplaces.
Improving human sustainability
Our study paves the way for future research and interventions aimed at mitigating the impact of work injuries on mental health and vice versa. Recognizing this bidirectional relationship is the first step towards creating more effective interventions and support systems.
Understanding the underlying mechanisms, such as negative thoughts and perceived job demands, can help when designing targeted interventions that address the root causes of these issues.
Additionally, understanding factors that influence the connection between work injuries and mental health — like how severe or often injuries occur, the types of mental health challenges that may arise and specific vulnerable groups — can provide valuable insights for developing tailored strategies.
By integrating physical and psychological care, we can ensure both aspects receive the attention they rightfully deserve in promoting human sustainability and enhancing the quality of life for workers across all industries.
- Mental health
- Employee health
- workplace injuries
- Health and well-being

Educational Designer

Lecturer, Small Animal Clinical Studies (Primary Care)

Organizational Behaviour – Assistant / Associate Professor (Tenure-Track)

Apply for State Library of Queensland's next round of research opportunities

Associate Professor, Psychology
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Burnout in Mental Health Services: A Review of the Problem and Its Remediation
Places for People: Community Alternatives for Hope, Health and Recovery
Michelle P. Salyers
Center of Excellence on Implementing Evidence-Based Practice, Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (VA HSR&D); Associate Professor, Department of Psychology, IUPUI; Co-Director, ACT Center of Indiana
Angela L. Rollins
Center of Excellence on Implementing Evidence-Based Practice, VA HSR&D; Assistant Research Professor, Department of Psychology, IUPUI; Research Director, ACT Center of Indiana
Maria Monroe-DeVita
Psychiatry and Behavioral Sciences, University of Washington
Corey Pfahler
Social Work, IUPUI
Staff burnout is increasingly viewed as a concern in the mental health field. In this article we first examine the extent to which burnout is a problem for mental health services in terms of two critical issues: its prevalence and its association with a range of undesirable outcomes for staff, organizations, and consumers. We subsequently provide a comprehensive review of the limited research attempting to remediate burnout among mental health staff. We conclude with recommendations for the development and rigorous testing of intervention approaches to address this critical area. Keywords: burnout, burnout prevention, mental health staff
Introduction
Burnout has been defined a number of ways ( Burke & Richardsen, 1993 ; Chemiss, 1980 ; Pines & Aronson, 1988 ; Stalker & Harvey, 2002 ), but most researchers favor a multifaceted definition developed by Maslach and colleagues (1993 ; 1996) that encompasses three dimensions: emotional exhaustion, depersonalization, and reduced personal accomplishment. The dimension of emotional exhaustion refers to feelings of being depleted, overextended, and fatigued. Depersonalization (also called cynicism) refers to negative and cynical attitudes toward one’s consumers or work in general. A reduced sense of personal accomplishment (or efficacy) involves negative self-evaluation of one’s work with consumers or overall job effectiveness ( Stalker & Harvey, 2002 ). Many researchers consider burnout to be a job-related stress condition or even a “work-related mental health impairment” (( Awa, Plaumann, & Walter, 2010 ), p. 184); in fact, burnout closely resembles the ICD-10 diagnosis of job-related neurasthenia ( Maslach, Schaufeli, & Leiter, 2001 ; Organization, 1992 ). Although burnout is correlated with other mental health conditions, such as anxiety and depression, research also supports that burnout is a construct distinct from these other mental health disorders, from a general stress reaction, and from other work phenomena such as job dissatisfaction ( Awa, et al., 2010 ; Maslach, et al., 2001 ). Burnout is also distinct from secondary traumatization, vicarious traumatization, and compassion fatigue ( Canfield, 2005 ; Dunkley & Whelan, 2006 ; Figley, 1995 ).
Since burnout was first described in the early 1970s, thousands of conceptual papers and empirical studies have focused on this complex phenomenon. As research has burgeoned over the past three decades, it has become clear that burnout, which occurs cross culturally, is prevalent across a variety of occupations, including teachers, managers and clerical workers, and in a variety of fields, including education, business, criminal justice, and computer technology ( Leiter & Schaufeli, 1996 ; Stalker & Harvey, 2002 ). Not surprisingly, burnout is also thought to be common among mental health service providers and administrators, and to be increasing for employees in public service systems ( Awa, et al., 2010 ). In public mental health, burnout is considered to be costly and “economically wasteful”, especially given the expense of recruiting and training staff (p. 7, ( Gilbody et al., 2006 ). Recently, the United States federal government also identified burnout as one key factor driving the “major problem” of retaining competent staff in “treatment organizations and state behavioral health systems” (p. 16, ( Hoge et al., 2007 )). Some studies have examined limited aspects of burnout among mental health providers, but there have been relatively few systematic attempts to better understand or ameliorate burnout in mental health; this is both surprising and ironic, given the goals of mental health organizations for improving the behavioral health of individuals and the fact that burnout is a stress-related psychological condition that arises within the workplace.
Given the complexity of the topic and the vast prior work on burnout, this review is not meant to be exhaustive; instead, we focus on two key questions: 1) To what extent is burnout a problem for mental health staff and the service delivery system? 2) What can — and should — be done to address burnout among mental health providers? We build upon a prior review of burnout and mental health ( Leiter & Harvie, 1996 ) while also incorporating key issues and findings from other reviews and empirical studies in the general field of burnout. Throughout the paper, we seek to identify areas important for further research and intervention, before making final conclusions and recommendations for research and practice. While another useful review of mental health and burnout was recently published ( Paris & Hoge, 2010 ), our review is different in that it emphasizes the full range of problems associated with burnout, a comprehensive review of the intervention literature, and new research and development strategies for remediating burnout.
Burnout: The Scope of the Problem for the Mental Health Field
We will examine the extent to which burnout is a problem in the mental health field in terms of two key areas: 1) the prevalence of burnout among mental health providers, and 2) the association of burnout with other problems for mental health staff and service delivery. Prevalence
Across several studies, it appears that 21-67% of mental health workers may be experiencing high levels of burnout. In a study of 151 community mental health workers in Northern California, Webster and Hackett (1999) found that 54% had high emotional exhaustion and 38% reported high depersonalization rates, but most reported high levels of personal accomplishment as well. In Rohland’s (2000) sample of 29 directors of community mental health centers in Iowa, over two-thirds reported high emotional exhaustion and low personal accomplishment. Further, almost half reported high levels of depersonalization. Siebert (2005) surveyed a state chapter of social workers, and of the 751 respondents, 36% scored in the high range of emotional exhaustion. The investigators also used a single item burnout measure and 18% of the sample endorsed the statement: “I currently have problems with burnout.” Oddie and colleagues (2007) examined 71 forensic mental health workers in the UK, and 54% reported high rates of emotional exhaustion. Prior United Kingdom studies reviewed by Oddie and colleagues (2007) also reported a range of 21% to 48% of general mental health workers as having high emotional exhaustion.
Differences in burnout between various mental health occupational types have yielded some evidence for higher burnout among community social workers compared to nurses and psychiatrists in one study in two European cities ( Priebe, Fakhoury, Hoffmann, & Powell, 2005 ), with an exception noted in an older study in Great Britain ( Onyett, Pillinger, & Muijen, 1997 ) where emotional exhaustion on the Maslach Burnout Inventory (MBI; Maslach, Jackson, & Leiter, 1996 ) —the most frequently used measure of burnout--was relatively high across the entire sample. Some research has noted lower job satisfaction for social workers compared to psychiatrists ( Prosser et al., 1997 ), but most mental health burnout studies have not compared rates of burnout across professions or disciplines. For instance, many studies either focus on burnout rates for single professional groups of interest (e.g., nurses, psychologists, social workers) or aggregate burnout findings across a wider swath of disciplines working within a single service type (e.g, psychosocial rehabilitation workers or staff of an intensive case management team; see studies in ( Leiter & Harvie, 1996 ; Taris, 2006 )). Prosser et al. (1997) found some differences in burnout and related factors between inpatient and community-based work settings, with inpatient staff experiencing lower levels of burnout and work stress compared to community-based staff. Rupert and Kent (2007) found higher levels of personal accomplishment for psychologists working independently or in group practices compared to psychologists working in “agency” settings, such as hospitals or community-based programs. Comparative rates of problematic burnout could give helpful clues on whether and/or how to target and package burnout interventions for various disciplines or program types.
Even though burnout is frequently mentioned as a problem in the mental health field (e.g., ( Edwards, Burnard, Coyle, Fothergill, & Hannigan, 2000 ), the construct is typically measured as a continuous variable so that the actual prevalence of “burnout” is difficult to quantify. In order to help address this issue, Maslach, Jackson, and Leiter (1996) presented score ranges on the MBI to conceptualize low, average, and high levels of burnout based on large normative samples for various occupations. For mental health workers, high levels of burnout included emotional exhaustion scores of at least 21, depersonalization scores of at least 8, and personal accomplishment scores of 28 or below; note, however, that these cut-off scores for “high” burnout in mental health workers are relatively low compared to other occupational groups. Research shows that continuous data scores on the MBI are predictive of other problems (see Maslach et al., 2001 ), but empirical validation of the cut-points for “high” burnout on the MBI is lacking. Therefore, literature using these cut-offs should be evaluated with some skepticism, namely that the low cut-off scores for “high” burnout in mental health may inflate the prevalence of burnout in some studies. On the other hand, one could argue that lower rates of burnout still deserve attention, since even “mild” burnout has been associated with increased risk for mental health problems ( Ahola et al., 2005 ). Either way, external validation studies with strong methodologies (e.g. representative sampling, higher response rates, longitudinal designs) are sorely needed for determining problematic levels of burnout. For instance, validation studies might determine what levels of burnout are associated with poor staff performance measures, staff intentions to leave the organization, staff health problems, or poor consumer outcomes.
Stability of the burnout construct is another area of need in future research. Burke and Richardsen (1993) reviewed several studies in the general literature which suggest that the level of burnout remains fairly stable across time if untreated. Of particular interest is Burke and Richardsen’s conclusion that burnout often becomes a chronic condition, and that after one year, about 40% of workers remain in the same stage of burnout, about 30% become more burned out, and about another 30% become less burned out. The lack of longitudinal research in the mental health field makes this topic another important area for further study.
Although methodological problems are common in many prevalence studies, the rates across studies indicate that burnout may indeed be widespread among mental health workers, and there is reason to believe that rates will continue to increase. As public sector funding for mental health is either constant or reduced (see California’s recent state budget cuts to social services, e.g., ( Goldmacher, 2009 ) and the costs for employee healthcare benefits and other expenses continue to rise, some mental health agencies are increasing staff “productivity” standards for billable services. In an already stressful work domain, the added pressures and responsibilities are likely to be triggers for greater levels of burnout.
Associated Problems for the Mental Health Field
Burnout has been associated with a large number of negative conditions affecting different types of employees, their organizations, and the consumers they serve. These undesirable situations are briefly highlighted below. We refer the reader to reviews in the general literature and larger population-based studies, and highlight studies specifically addressing mental health workers where data are available. One important caveat – we refer to consequences or outcomes of burnout, although many of these findings are derived from cross-sectional studies, making it difficult to firmly conclude whether the conditions are the outcomes of burnout rather than noncausal correlates or even antecedents.
The empirical and theoretical literature suggests that the consequences of burnout can be severe and far-reaching. Employees who experience burnout often experience impaired emotional and physical health and a diminished sense of well-being ( Stalker & Harvey, 2002 ). Some population-based studies, not specifically focused on mental health workers, have shown correlations between burnout and aspects of physical and mental health. For example, Peterson and colleagues (2008) studied a sample of service workers in a Swedish city (N = 1252) including nurses, physicians, social workers, occupational therapists, physiotherapists, dentists, dental hygienists, administrators, teachers, and technicians. Burnout was associated with increased depression, anxiety, sleep problems, impaired memory, neck and back pain, and alcohol consumption. Ahola and colleagues (2005) investigated the relationship between job-related burnout and depressive disorders in 3,276 workers in Finland. Based on a standardized clinical interview, individuals with mild burnout were at 3.3 times more risk of having major depressive disorder, and those with severe burnout were 15 times more likely to have major depressive disorder. The risk of having a major depressive disorder with severe burnout was greater for men than for women, with the risk of a major depressive disorder 10.2 fold for women and 29.5 fold for men.
Health issues have also been linked to mental health provider burnout. In a study of 591 social workers in NY, Acker (2010) found that high levels of burnout, particularly emotional exhaustion and depersonalization, were related to greater reports of flu-like symptoms and symptoms of gastroenteritis. Notably, social workers with greater levels of involvement with consumers with severe mental illness reported higher levels of burnout. Burnout has also been correlated with increased substance use in directors of mental health agencies ( Rohland, 2000 ).
Employee burnout has been correlated with a number of negative organizational measures, including reduced commitment to the organization ( Burke & Richardsen, 1993 ), negative attitudes ( Chemiss, 1980 ), and often absenteeism and turnover ( Schwab, Jackson, & Schuler, 1986 ; Smoot & Gonzolas, 1995 ; Stalker & Harvey, 2002 ). Not surprising, burnout is related to job dissatisfaction ( Maslach, et al., 2001 ; Prosser, et al., 1997 ; Schulz, Greenley, & Brown, 1995 ) and burnout may also damage the morale of other employees and lead to staff turnover ( Stalker & Harvey, 2002 ). In a longitudinal study of 3,895 employees (non mental health workers) who worked in a large industry corporation, Toppinen-Tanner and colleagues (2005) found that burnout predicted future sick leave, even after controlling for the effects of age, gender, occupation, and previous absence. High levels of burnout increased the risk of absence related to mental and behavioral disorders, as well as diseases of the circulatory, respiratory, and musculoskeletal systems. In mental health, staff absences and turnover are correlated with reduced fidelity to evidence-based practices ( Mancini et al., 2009 ; Rollins, Salyers, Tsai, & Lydick, 2010 ) and increase the costs of recruiting and training new staff.
Over time, the cumulative effects of managing a consumer caseload can lead to fatigue, exhaustion and burnout ( Ducharme, Knudsen, & Roman, 2008 ). In turn, burnout may also impact care provided to mental health service consumers. Although few studies have actually examined the relationship of burnout to quality of care, burnout and staff turnover are believed to disrupt the continuity of mental health care ( Boyer & Bond, 1999 ) and to undermine the quality of services provided ( Carney, Donovan, Yurdin, & Starr, 1993 ; Hoge, et al., 2007 ; Maslach & Pines, 1979 ). High levels of burnout signify that workers possess insufficient resources to deal with the demands of their jobs, leading to impaired job performance. Employees with high levels of burnout may not be willing to expend effort, leading to suboptimal functioning at work ( Taris, 2006 ). In addition, burned out workers may be less able to be empathic, collaborative, and attentive -- characteristics that have been associated with higher consumer satisfaction ( Corrigan, 1990 ). In the general burnout literature, Taris (2006) performed a systematic literature review on burnout and objective performance, subsequently reviewing 16 articles. In 5 articles, high levels of exhaustion were associated with low levels of role performance, and in three articles examining consumer satisfaction, higher levels of exhaustion resulted in lower customer service ratings. Indeed, burnout among nurses and general medicine physicians has been found to be related to decreased patient satisfaction ( Halbesleben & Rathert, 2008 ; Leiter, Harvie, & Frizzell, 1998 ).
Burnout has also been empirically associated with negative feelings about mental health consumers. A study of 510 psychiatric workers in 28 different units ( Holmqvist & Jeanneau, 2006 ) found that high levels of emotional exhaustion and depersonalization were correlated with negative attitudes (e.g., distant, rejecting) toward consumers on their ward. Negative staff attitudes, in turn, have been linked with poorer outcomes among consumers with severe mental illness ( Gowdy, Carlson, & Rapp, 2003 ). In a study empirically linking burnout to poor consumer satisfaction, Garman and colleagues (2002) surveyed 333 mental health staff on 31 different teams serving people with severe mental illness. Team level emotional exhaustion, but not depersonalization, was significantly related to average consumer satisfaction scores for those teams.
Overall, burnout has been associated with a variety of other negative conditions at the level of the individual, organization, and to some extent, quality of services provided. The vast majority of these studies, however, have been cross-sectional and correlational. So, the idea of “burnout consequences” may not accurately capture the direction of relationships. For example, staff who are already experiencing high levels of physical health problems may feel added work pressure and report high levels of emotional exhaustion as a result of their pre-existing health problem. Conversely, a third variable, for example, underlying depression or anxiety, could manifest in both high levels of burnout and greater preoccupation with physical health concerns. As well, associated problems may moderate burnout through complex, multivariate pathways. For example, in research on 43 mental health organizations in Wisconsin, Schulz, Greenley, and Brown (1995) found that a number of organizational, management, and job variables predicted job satisfaction, not burnout directly, but job satisfaction moderated employees’ levels of burnout. In addition to the lack of clear directionality, we found only a handful of studies specifically assessing potential consequences of burnout in mental health workers. However, there is little reason to believe that burnout would affect mental health workers differently than nurses, teachers, or other professional groups where additional research describes strong relationships between burnout and a range of associated problems. Nonetheless, future research should include mental health workers and use larger samples, longitudinal designs, and multivariate models to better examine the relationship between burnout and associated problems.
Reducing Burnout
Mental health staff.
Despite its prevalence and association with a number of negative outcomes, little attention has been directed toward reducing or preventing burnout among mental health professionals. The need for burnout prevention and interventions for mental health providers has been highlighted by researchers for decades ( Pines & Maslach, 1978 ), but few such programs have actually been implemented and evaluated. At the time of their review, Leiter and Harvie (1996) reported only one intervention study specific to mental health workers. We conducted an updated review of this literature for this paper. Specifically, we ran computerized literature searches using the terms burnout, mental health professionals and personnel using the PsychInfo database from 1987 through 2010. In addition, we manually examined citations and reference lists in original articles on burnout and in reviews in overlapping areas (e.g., ( Awa, et al., 2010 ; Gilbody, et al., 2006 ; Paris & Hoge, 2010 )) to identify other studies of burnout interventions for mental health staff. To be included in the present paper, the intervention study must have included (a) a planned method or strategy designed to reduce or prevent burnout, (b) sample participants who met the inclusion criteria as mental health staff (related disciplines, such as substance abuse counselors, were excluded) and who served persons with mental health disorders (one study with staff serving primary dementia, was excluded); (c) an outcome variable specifically measuring burnout; and (d) a quasi-experimental or experimental research design. Prior to summarizing these approaches, it is important to note that most studies in any occupational field have not differentiated between programs designed to prevent burnout from those developed to help employees recover from burnout. To some extent, this tendency may arise from theorists conceptualizing burnout along a continuum. It remains to be seen, however, whether the same strategies are effective for both reducing as well as preventing burnout. Regardless, intervention programming and research could benefit from further specification and clarity on this issue.
Our search identified eight studies, which are described in detail in Table 1 . Perhaps the most striking observations concerned the settings of the studies. As shown, six (75%) of the eight studies were conducted in European countries, while only two were conducted in the United States. Further, at least five (62.5%) of the eight studies involved staff working in psychiatric inpatient settings, and only one study clearly evaluated burnout prevention in a community mental health setting. Four (50%) of the studies were conducted with psychiatric nurses exclusively.
Controlled Intervention Studies to Improve Burnout Among Mental Health Staff
| Study | Participants | Setting | Design | Intervention | Results |
|---|---|---|---|---|---|
| Halberg 1994 | 11 nurses (Sweden) | Psychiatric inpatient (child/adol escent) | Quasi-exp Pre-Post: Baseline, 6 and 12 month | Group psycho-dynamic clinical supervision for emotional reactions (14 2-hour sessions over 1 year) | NS changes for burnout; Significant decrease for tedium |
| 326 nurses (Netherlands) | Psychiatric inpatient | Quasi-exp 2 Pretest, 1 Post, nonequivalent groups | Primary nursing model plus special supervisor feedback vs usual treatment | NS changes for burnout; Trend toward less turnover; However, attrition >50%, problems with treatment diffusion. | |
| 35 direct care and clinical staff | Psychiatric residential program | Pre-Post | Staff training needs assessment, planning and training on psychiatric rehabilitation. 90 minute trainings for 8 months | Significant reduction on EE for direct care but not clinical staff; NS on DP and PA; Significant improved attitudes about behavioral interventions, satisfaction with staff support | |
| 352 “direct care professionals” (Netherlands) | Not specified | Quasi exp Pre-Post for Exp and 2 nonequivalent comparisons | Cognitive behavioral training (1/2 day per week for 5 weeks to improve equity; 3 sessions for supervisors, to improve communication & social skills | EE reduced at 6 months, but NS at 12 months; NS change in DP; PA significant at 6 mos vs. external comparison group but NS at 12 mos, and NS vs. internal comparison group; Absences | |
| Carson et al., 1999 | 53 nurses (UK) | Psychiatric inpatient | RCT | Social support group vs feedback-only on stress level plus stress management handout; 2 hours × 5 weeks | NS change for EE and DP PA, Control improved at post-test, NS at 6 months; 36% attrition at 6 months |
| 20 forensic nurses (UK) | Psychiatric inpatient | RCT | Psychosocial intervention training (6 weeks) vs waiting list control | Significant decrease in EE and DP, and increased PA; significantly improved knowledge, attitudes re: SMI | |
| 25 mental health staff (14 direct care, 11 managers) | Psychiatric inpatient, residential, day programs, (Italy) | Quasi-exp (pretest, post-test, follow-up) | Assertiveness training (3 hr workshops monthly for 5 mos) plus one additional workshop: CBT for handling emotions while serving consumers (direct care) or task planning, leadership style, supporting staff (managers) | NS change in EE; DP decreased at post-test and 18 mos; PA worse at post-test; NS at 18 mos | |
| 84 mental health staff | Communit y mental health | Quasi-exp 2 pre-test, post test (6 weeks) | Day workshop to improve awareness and skills (contemplative, cognitive, social, etc.) | EE reduced; DP reduced; NS change in PA Improved optimism re: consumers |
NS = Not significant; EE= Emotional Exhaustion; DP = Depersonalization; PA=Personal Accomplishment
In terms of research design, two studies conducted randomized controlled trials (RCTs) while the remainder employed quasi-experimental designs, such as nonequivalent control groups or simple pre-post designs (sometimes using multiple pretests or multiple posttests). Follow-up periods ranged from a simple post-test at the completion of the intervention to one-year follow-ups. Three of the studies experienced high rates of research attrition and four studies used small samples. The types of interventions also ranged widely. Most of the intervention programs involved multiple training and/or supervision sessions spread over a period of weeks or months, although one program involved a single day workshop.
In terms of results, five (62.5%) programs resulted in significant reductions in mental health staff burnout. Corrigan and colleagues (1997) used a staff needs assessment and program development committee to identify training needs, which were then addressed by behavioral rehabilitation training. After eight months of meetings and trainings, the program reduced emotional exhaustion at the post-test among “direct care staff” but not for “clinical staff” working in psychiatric rehabilitation programs. Ewers and colleagues (2002) also provided training in psychosocial interventions to improve nurses’ coping skills and attitudes and found significant reductions in all three components of burnout at post-test for inpatient forensic psychiatric nurses. Their training program included educational information about severe mental health disorders and intervention strategies (e.g., engagement skills, interventions for hallucinations). Meanwhile, van Dierendonck and colleagues (1998) sought to reduce staff burnout by reducing feelings of inequity in workers via improving the congruence between workers’ “motives, needs, and capacities and the organizational demands and provisions” (p. 395). The program incorporated cognitive behavioral interventions (cognitive restructuring, relaxation training) for individual staff, and supervisors were also trained in communication and social skills. The investigators reported reduced burnout, absenteeism, and feelings of being deprived over one year among the intervention group in a quasi-experimental design; however, research attrition was very high (58 percent). Scarnera, Bosco, Soleti, and Lacioni (2009) provided assertiveness training to mental health staff in Italy. In addition, they provided direct care staff with additional cognitive restructuring training for managing emotions while working with consumers with severe mental illness; managers, meanwhile, received additional training on task planning, leadership styles, and supporting staff. This study reported decreased depersonalization at post-test and 18 months after baseline (interestingly, personal accomplishment worsened at post-test but was not significant at 18 months). A recent program for community mental health staff combined cognitive-behavioral coping skills with other strategies, including mindfulness, meditation, the identification of personal meaning, and the development of practices of gratitude in a one-day training intervention ( Salyers et al., 2011 ). Results showed a reduction in emotional exhaustion and depersonalization, as well as an increase in positive perceptions of consumers six weeks later. Both of these recent intervention studies ( Salyers, et al., 2011 ; Scarnera, et al., 2009 ) also included participant time to develop personal strategies for coping with their own individual stressors.
The small number of intervention studies and the methodological problems present in the prior studies make conclusions difficult, but the literature does suggest that interventions can reduce burnout among mental health staff. The limited existing literature also clearly suggests the need for developing additional interventions and using more controlled research to evaluate these programs. Before discussing recommendations and future directions for burnout prevention programming and research, however, it is useful, given the small number of mental health studies, to consider findings from the broader literature on burnout reduction across other fields and disciplines than mental health.
Burnout Reduction Studies in Other Fields
Several earlier reviews within the general field of burnout reached a similarly disturbing conclusion as we have for mental health: despite the high prevalence of burnout, relatively few intervention or prevention programs have been implemented, and very few of these have been adequately evaluated ( Burke & Richardsen, 1993 ; Halbesleben & Buckley, 2004 ; Stalker & Harvey, 2002 ). Over the past decade, however, there has been an increasing number of burnout reduction programs more rigorously evaluated. For example, in their recent review, Awa, Plaumann & Walter (2010) identified 25 controlled (quasi-experimental or randomized control trial) studies of burnout reduction programs across various fields and occupations. An inspection of the studies in their review indicates that 21 (84%) of these studies were published in or after 2000 (and 12 or 48% were published after 2004). Although the occupations varied widely in these studies, a cross-cultural trend was also evident: specifically, only four (16%) of these studies were conducted in the United States while 72% of the studies were in Europe (including 48% of the total in the Netherlands).
An important conceptual issue in the burnout prevention literature concerns the target of the intervention. Earlier reviewers ( Burke & Richardson, 1993 ; Halbesleben & Buckley 2004 ; Maslach et al., 2001 ) conceptualized intervention strategies within two broad categories: programs designed to improve burnout by targeting change strategies at individual workers, and those that are designed to change the work environment. We prefer a three-component categorization, also used by Awa and colleagues (2010) , which also includes programs that combine individual and environmental interventions.
Programs for Individuals
As others have noted ( Awa, et al., 2010 ; Halbesleben & Buckley, 2004 ; Maslach, et al., 2001 ; van Dierendonck, et al., 1998 ), most burnout programs have focused on changing the individual to improve burnout, typically with the goal of reducing work stress by improving the person’s coping skills or social support. A variety of different techniques have been tried, ranging from making recreational music ( Bittman, Bruhn, Stevens, Westengard, & Umbach, 2003 ), to psychosynthesis, a humanistic therapy with spiritual emphasis ( van Dierendonck, Garssen, & Visser, 2005 ). Most of the interventions, however, fall within the broad category of cognitive-behavioral interventions, including providing educational information, cognitive restructuring, progressive muscle relaxation, social skills training, communication skills training, and skills to enhance social support ( Murphy, 1996 ; van Dierendonck, et al., 1998 ). Evaluations of individual-level interventions suggest that coping skills programs are often effective for reducing burnout, especially emotional exhaustion, and some of these programs also have led to positive physiological results (e.g., lower blood pressure) for employees (see ( Awa, et al., 2010 ; Halbesleben & Buckley, 2004 ; van Dierendonck, et al., 1998 ). Awa and colleagues also concluded, however, that the significant improvements in burnout that accrued from individual-focused interventions often disappeared six to 12 months after the completion of the intervention, unless booster sessions were included in the program.
In addition to general coping skills, an interesting and emerging set of strategies falls within the broad rubric of “third generation cognitive behavioral” interventions ( Hayes, Follette, & Linehan, 2004 ), which often incorporate methods derived in part from spiritual practices or Eastern religions, such as meditation and mindfulness. In a review of work-based stress management programs, Murphy (1996) found that meditation programs (and programs that offered a combination of intervention strategies) tended to be the most effective. Two intervention studies are of particular interest. Using a randomized controlled trial, Hayes, Bisset, Padilla et al., (2004) found that a one-day workshop of acceptance and commitment therapy reduced burnout for substance abuse counselors at post-training and after a three month follow-up. Most recently, Krasner and colleagues ( Krasner et al., 2009 ) developed a continuing medical education program for primary care physicians that used mindfulness practices, appreciative inquiry, and narrative exercises to help physicians increase awareness and communication skills. Using a pre- and post-test design with multiple follow-up assessments over 15 months, Krasner et al. (2009) reported significant reductions in all facets of burnout as well as improvements in mood. This study also illustrates another important issue: that while improving coping skills for stress is an important element for reducing burnout, very few studies attempt to prevent burnout by increasing other positive human qualities and abilities, such as increasing a sense of meaning and purpose, which were critical elements in the Krasner program (see also ( Salyers, et al., 2011 )). Similarly, developing a sense of personal (and organizational) meaning was the focus of the program by Robey, Ramsland, and Castelbaum (1991) which improved the related outcome of job satisfaction.
Organizational Strategies
Despite a number of studies finding positive results for interventions targeting individual staff, some researchers have criticized or minimized individual-based interventions in favor of environmental or organizational-level changes ( Burke & Richardsen, 1993 ; Halbesleben & Buckley, 2004 ; Maslach, et al., 2001 ; Stalker & Harvey, 2002 ). Researchers advocating this approach argue that organizational-environmental factors are antecedents to individual burnout and should therefore be the appropriate targets for intervention rather than individuals. Indeed, research on the correlates and antecedents of burnout suggest that a number of organizational-environmental variables are related to burnout, including an excessive workload, time pressure, role conflict, role ambiguity, an absence of job resources (especially supervisory and coworker social support), limited job feedback, limited participation in decision-making in matters affecting the employee, a lack of autonomy, unfairness or inequity in the workplace, and insufficient rewards (including social recognition) ( Maslach, et al., 2001 ; Paris & Hoge, 2010 ; van Dierendonck, Schaufeli, & Buunk, 2001 ). Moreover, organizational-environmental variables tend to be more potent predictors of burnout than individual characteristics.
Prior researchers have suggested a number of possible changes in organizational practices that may help decrease or prevent burnout, including increasing social support for employees, especially by teaching communication and social skills to supervisors ( Burke & Richardsen, 1993 ; Halbesleben & Buckley, 2004 ); increasing individual employee autonomy and involvement in decision-making (see ( Burke & Richardsen, 1993 ); reducing role ambiguity and conflicts for employees ( Stalker & Harvey, 2002 ); providing regular supervision, including peer supervision ( Feingold, 2005 ); and decreasing workloads and promoting self-care as a value within the organizational culture ( Feingold, 2008 ). Not all of these recommendations, however, have been implemented and evaluated.
Despite strong recommendations from past researchers for organizational interventions, there have been very few studies of organizational-level intervention programs to reduce burnout, and those that have been implemented tend to be limited by major methodological weaknesses. Awa and colleagues (2010) identified only two controlled studies of organizational interventions for burnout, one of which reported significant findings for reducing the emotional exhaustion and depersonalization of fire department workers ( Halbesleben, Osburn, & Mumford, 2006 ). Three other studies (not included in Awa and colleagues’ review) also show positive support for organizational interventions for reducing burnout. The program by Corrigan and colleagues (1997) , described earlier in the section on mental health interventions, represents an organizational development strategy. More recently, Glisson, Dukes, and Green (2006) tested the Availability, Responsiveness, and Continuity (ARC) organizational intervention model in an RCT study of child welfare and juvenile justice system case management programs. Results showed a number of positive outcomes for ARC, including improvements in the burnout components of emotional exhaustion and depersonalization (as well as for staff turnover, role conflict, and role overload). Leiter, Laschinger, Day and Oore (in press) tested the Civility, Respect, and Engagement at Work (CREW) social relationship intervention in a quasi-experimental study involving 41 hospital units. Outcomes included significant improvements for depersonalization, but not emotional exhaustion or personal achievement; positive improvements also occurred for job satisfaction, absences, civility, respect and trust of management. In summary, organizational interventions appear to show considerable promise for reducing burnout, but the field lacks a breadth of intervention models and sufficient controlled research. Unfortunately, however, some factors in burnout (e.g., workload) may be more influenced by environmental factors out of the organization’s immediate control that stem from larger systems (e.g., paperwork requirements for Medicaid reimbursement). In such cases, compensatory interventions may need to be directed at the individual or organization, unless system-level interventions are developed. Given the nature of environmental interventions, researchers will also need to overcome greater logistic problems in conducting intervention research, as the unit for experimental manipulation (and potentially for data analysis) may involve teams, units, departments or organizations rather than individuals.
Combined Person and Organizational Interventions
A small number of studies have examined interventions that either used multiple or complex interventions targeted at both the individual and the organizational levels. Awa and colleagues (2010) categorized six controlled burnout studies in this area and reported positive effects for reducing burnout in all six studies. However, our examination of one of these studies ( Melchior et al., 1996 ) revealed that the intervention was not successful for reducing burnout after the intervention; a reduction in burnout occurred for the intervention group between the first and second pretest, prior to the implementation of the burnout reduction program. Still, the overall rate of effectiveness of these combined interventions reported by Awa and colleagues remains high, with five of six (83%) programs showing positive outcomes. In addition, two mental health interventions, van Dierendonck and colleagues’ (1998) and Scarnera and colleagues (2009) , both showed positive effects for reducing burnout. Both programs can be considered combined interventions, because supervisors also received training to improve their ability to communicate and provide support to staff, in addition to direct care staff receiving cognitive behavioral interventions.
Conclusions and Future Directions
Ironically, the mental health field has paid relatively little attention to the health and well-being of its own workers. Relatively few well-designed, empirical studies have examined burnout in mental health. Many prior studies are plagued by significant methodological weaknesses, including small samples, samples of convenience, high attrition rates, cross-sectional rather than longitudinal designs, and bivariate rather than multivariate models. Despite these frequent methodological limitations, it is clear that burnout is a significant problem in mental health, both in its prevalence and its association with a wide range of other problems for individual staff persons, for the organizations that employ them, and likely for the people with mental health disorders whom they serve.
There is a pressing need for additional, basic research on mental health and burnout. As Paris and Hoge (2010) put it, “a primary challenge for the mental health field is to . . . build a more robust knowledge base about the prevalence, causes, and effects of burnout in this field” (p. 526). In particular, our ability to understand burnout will improve as researchers use representative samples and multivariate and longitudinal designs in future studies. Problematic levels of burnout should also be defined and validated to determine whether interventions can reduce burnout to sub-threshold levels. Important and under-studied topics include the consequences of burnout on consumers of mental health services, the role of organizational and other environmental factors in causing burnout, and models and theories of burnout. Further, additional attention should focus on the positive aspects of working, such as the process by which mental health workers experience compassion, joy, meaning, and fulfillment in their jobs.
The existing research does currently provide some support for the notion that burnout among mental health workers can be significantly improved. However, the number of controlled studies is very limited, especially in mental health, and particularly for community mental health workers in the United States. Further, conclusions about the effectiveness of burnout interventions are weakened by a number of methodological problems, including the paucity of experimental designs, limited follow-up periods, high research attrition rates, and a lack of replication studies for well-specified intervention models. Given the prevalence and consequences of burnout among mental health workers, there is a great need for additional, future development and research of burnout prevention and intervention programs.
Researchers and administrators can draw upon findings and strategies from the existing literature in mental health and other fields while developing and testing new burnout reduction programs. In particular, for individual-level interventions, various cognitive-behavioral strategies appear useful for improving coping skills and reducing burnout. Rather than relying on a single technique, however, the use of multiple intervention strategies is often helpful ( Murphy, 1996 ) —see Table 2 for a listing of possible intervention target areas and strategies. In order to develop potentially more effective burnout prevention programs, however, it is important that researchers and program developers experiment with new and more innovative methods. Third-generation cognitive-behavioral methods, especially meditation and mindfulness practices, also appear promising. Burnout prevention programs that help individuals to not only cope with stress but to develop more positive qualities —such as a sense of meaning, gratitude, and fulfillment in work — are especially important areas for further research. Regardless of the type of intervention strategy, given the complexity of burnout, it is likely that the most effective programs for sustaining long-term results will need to be delivered over time rather than in a single day and to incorporate booster sessions ( Awa, et al., 2010 ). The use of technology to supplement the delivery of burnout reduction methods may be one innovative means of supplementing interventions and providing follow-up boosters —just as technology is being developed to improve care between mental health providers and the people they serve. For example, Common Ground is a shared decision-making tool that collects information about the consumer’s goals, current condition, and care, and reports progress over time for the treating provider and consumer ( Deegan, Rapp, Holter, & Riefer, 2008 ). We envision similar tools, whereby mental health providers could track their own level of burnout and the interventions they have used while also being able to electronically access additional strategies to remediate burnout.
Targets and Strategies for Future Intervention Studies on Burnout
| INDIVIDUAL LEVEL | |
|---|---|
| Target | Strategy |
| Increase Positive Stress Coping Skills (e.g., ) | Various Cognitive Behavioral Stress Reduction and Coping Skills (See Awa et al.) |
| Increase Social Support ( ; ) | Teach Social Support Enhancement Skills, Especially Toward Co-Workers and Supervisors |
| Increase Internal Sense of Reward and Satisfaction ( ) | Training to Recognize and Celebrate Recovery, Consumer Strengths, Small Steps in Progress |
| Increase a Sense of Gratitude in Work and Life (Geller et al., 2008) | Teach Gratitude Perspective and Skills ( ) |
| Increase Sense of Meaning and Purpose in Work (Geller et al., 2008) | Appreciate Inquiry, Narrative Exercises ( ) |
| Increase Awareness/Reduce Numbing | Teach Mindfulness Skills ( ) |
| Reduce Employee Work Overload ( ; ) | Create Organizational/Unit Goals, Priorities. ARC ( ) Collaborative and Supervisor-Employee Goal and Priority Setting |
| Reduce Role Ambiguity ( ; ) | Develop Clear, Accurate Job Descriptions and Provide Necessary Training ( ) |
| Reduce Role Conflict ( ; ) | ARC ( ); CREW ( ) |
| Increase Job Resources/ Increase Positive Feedback/External Rewards ( ) | Provide Regular, Collaborative, Quality Supervision ( ; Knudsen et al., 2008); Train Supervisors to Provide Positive Social Support ( ) and Express Gratitude ( ) Provide Competitive Compensation ( ) |
| Increase Employee Involvement in Relevant Decision Making and Problem Solving ( ) | Collaborative Team Meetings Use of Problem Solving and Continuous Quality Improvement, e.g., -ARC ( ) |
| Increase Employee Autonomy ( ) | Decentralize Decision Making |
| Create Shared Values ( )/Positive Work Culture/Sense of Community ( ) that Support Employee Wellness | Develop Interlocking Individual/Team/Agency Mission and Value Statements ( ) ARC ( ), Administrative Policies ( ) |
Organizational-level interventions also appear promising for reducing staff burnout, though the paucity of existing controlled studies in this area is problematic. The shortage of organizational interventions may stem in part from research challenges (gaining the cooperation of a number of organizations or units that is necessary for controlled study), in part from biases in the human service and mental health fields to focus change on the individual rather than systems, and also from uncertainty about possible intervention targets and strategies. Table 2 also highlights possible organizational-level targets and change strategies, drawing from the literature that has identified organizational antecedents of burnout, from selected intervention studies, and from our own recommendations. As shown, some organizational interventions such as ARC ( Glisson, et al., 2006 ) are multifaceted and address multiple organizational factors that correlate with staff burnout. Other promising strategies include the development of a sense of shared meaning between the organization and employees through interlocking mission statements ( Robey, et al., 1991 ), working with administrators to develop organizational policies and practices that promote staff wellness ( Fallot & Harris, 2008 ), and training managers to regularly express gratitude at work ( Kerns, 2006 ).
It is likely that the most effective programs for reducing burnout in the future will be those that combine individual and organizational interventions. This does not mean that researchers and administrators should necessarily attempt to design and test comprehensive interventions that incorporate all possible strategies. However, the use of individual intervention strategies, in combination with some type of organization intervention, appears feasible, promising, and worthy of further experimentation and study.
Future intervention studies should be improved by stronger research designs, especially the use of RCTs, longer follow-up periods, and assertive methods to improve participant retention over time. While burnout should remain a central outcome variable, future knowledge will also be enhanced as researchers include an expanded set of outcome variables. Core outcome variables should include measures of interest to employers (e.g., employee turnover, absences, and positive work engagement —see ( Maslach, et al., 2001 )), employee work variables (e.g., job satisfaction), employee health and stress outcomes (e.g., depression), and, ultimately, measures of positive employee states (e.g., growth in personal meaning, compassion, fulfillment). Most importantly, research on reducing staff burnout should also examine the effects on consumers, with the hope that burnout reduction programs will improve the quality, quantity, and outcomes of services to people with mental health disorders.
Contributor Information
Gary Morse, Places for People: Community Alternatives for Hope, Health and Recovery.
Michelle P. Salyers, Center of Excellence on Implementing Evidence-Based Practice, Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (VA HSR&D); Associate Professor, Department of Psychology, IUPUI; Co-Director, ACT Center of Indiana.
Angela L. Rollins, Center of Excellence on Implementing Evidence-Based Practice, VA HSR&D; Assistant Research Professor, Department of Psychology, IUPUI; Research Director, ACT Center of Indiana.
Maria Monroe-DeVita, Psychiatry and Behavioral Sciences, University of Washington.
Corey Pfahler, Social Work, IUPUI.
- Acker G. The challenges in providing services to clients with mental illness: Managed care, burnout and somatic symptoms among social workers. Community Mental Health Journal. 2010; 46 (6):591–600. [ PubMed ] [ Google Scholar ]
- Ahola K, Honkonen T, Isometsä E, Kalimo R, Nykyri E, Aromaa A, Lönnqvist J. The relationship between job-related burnout and depressive disorders--results from the Finnish Health 2000 Study. Journal of Affective Disorders. 2005; 88 (1):55–62. [ PubMed ] [ Google Scholar ]
- Awa WL, Plaumann M, Walter U. Burnout prevention: a review of intervention programs. Patient Educ Couns. 2010; 78 (2):184–190. [ PubMed ] [ Google Scholar ]
- Bittman B, Bruhn KT, Stevens C, Westengard J, Umbach PO. Recreational music-making: a cost-effective group interdisciplinary strategy for reducing burnout and improving mood states in long-term care workers. Adv Mind Body Med. 2003; 19 (3–4):4–15. [ PubMed ] [ Google Scholar ]
- Boyer SL, Bond GR. Does assertive community treatment reduce burnout? A comparison with traditional case management. Mental Health Services Research. 1999; 1 (1):31–45. [ Google Scholar ]
- Burke RJ, Richardsen AM. Psychological burnout in organizations. In: Golembiewski RT, editor. Handbook of organizational behavior. New York: Marcel Dekker; 1993. [ Google Scholar ]
- Canfield J. Secondary Traumatization, Burnout, and Vicarious Traumatization: A Review of the Literature as It Relates to Therapists Who Treat Trauma. Smith College Studies in Social Work. 2005; 75 (2):81–101. [ Google Scholar ]
- Carney J, Donovan R, Yurdin M, Starr R. Incidence of burnout among New York City intensive case managers: Summary of findings. Psychosocial Rehabilitation Journal. 1993; 16 (4):25–38. [ Google Scholar ]
- Chemiss C. Staff burnout: Job stress in the human services. Beverly Hills, CA: Sage; 1980. [ Google Scholar ]
- Corrigan PW. Consumer satisfaction with institutional and community care. Community Mental Health Journal. 1990; 26 (2):151–165. [ PubMed ] [ Google Scholar ]
- Corrigan PW, McCracken SG, Edwards M, Kommana S, Simpatico T. Staff training to improve implementation and impact of behavioral rehabilitation programs. Psychiatr Serv. 1997; 48 (10):1336–1338. [ PubMed ] [ Google Scholar ]
- Deegan PE, Rapp C, Holter M, Riefer M. Best practices: a program to support shared decision making in an outpatient psychiatric medication clinic. Psychiatr Serv. 2008; 59 (6):603–605. [ PubMed ] [ Google Scholar ]
- Ducharme LJ, Knudsen HK, Roman PM. Emotional exhaustion and turnover intention in human service occupations: the protective role of coworker support. Sociological Spectrum. 2008; 28 (1):81–104. [ Google Scholar ]
- Dunkley J, Whelan TA. Vicarious traumatisation: Current status and future directions. British Journal of Guidance & Counselling. 2006; 34 (1):107–116. [ Google Scholar ]
- Edwards D, Burnard P, Coyle D, Fothergill A, Hannigan B. Stress and burnout in community mental health nursing: A review of the literature. Journal of Psychiatric and Mental Health Nursing. 2000; 7 :7–14. [ PubMed ] [ Google Scholar ]
- Emmons RA, Shelton CM. Gratitude and the science of positive psychology. In: Snyder C, Lopez S, editors. Handbook of positive psychology. New York: Oxford University Press; 2001. pp. 459–471. [ Google Scholar ]
- Ewers P, Bradshaw T, McGovern J, Ewers B. Does training in psychosocial interventions reduce burnout rates in forensic nurses? J Adv Nurs. 2002; 37 (5):470–476. [ PubMed ] [ Google Scholar ]
- Fallot RD, Harris M. Trauma informed approaches to systems of care. Trauma Psychology Newsletter. 2008; 3 (1):6–7. [ Google Scholar ]
- Feingold A. Sustaining stamina at the interface of HIV and mental health practice. Mental Health AIDS. 2005; 6 (2) [ Google Scholar ]
- Feingold A. Kicking it upstairs. Mental Health AIDS. 2008; 9 (2) [ Google Scholar ]
- Figley CR. Compassion fatigue as secondary traumatic stress disorder: An overview. In: Figley CR, editor. Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. Philadelphia, PA US: Brunner/Mazel; 1995. pp. 1–20. [ Google Scholar ]
- Garman AN, Corrigan PW, Morris S. Staff burnout and patient satisfaction: evidence of relationships at the care unit level. J Occup Health Psychol. 2002; 7 (3):235–241. [ PubMed ] [ Google Scholar ]
- Gilbody S, Cahill J, Barkham M, Richards D, Bee P, Glanville J. Can we improve the morale of staff working in psychiatric units? A systematic review. Journal of Mental Health. 2006; 15 (1):7–17. [ Google Scholar ]
- Glisson C, Dukes D, Green P. The effects of the ARC organizational intervention on caseworker turnover, climate, and culture in children's service systems. Child Abuse Negl. 2006; 30 (8):855–880. discussion 849–854. [ PubMed ] [ Google Scholar ]
- Goldmacher S. California's budget woes will continue for years, report says. The Los Angeles Times; 2009. Nov 19, Retrieved from www.latimes.com/news/local/la-me-budget-deficit19-2009nov19,0,433593.story . [ Google Scholar ]
- Gowdy EA, Carlson LS, Rapp CA. Practices differentiating high-performing from low-performing supported employment programs. Psychiatric Rehabilitation Journal. 2003; 26 :232–239. [ PubMed ] [ Google Scholar ]
- Halbesleben JR, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Management Review. 2008; 33 (1):29–39. [ PubMed ] [ Google Scholar ]
- Halbesleben JRB, Buckley MR. Burnout in organizational life. Journal of Management. 2004; 30 (6):859–879. [ Google Scholar ]
- Halbesleben JRB, Osburn HK, Mumford MD. Action Research as a Burnout Intervention: Reducing Burnout in the Federal Fire Service. Journal of Applied Behavioral Science. 2006; 42 (2):244–266. [ Google Scholar ]
- Hayes SC, Bissett R, Roget N, Padilla M, Kohlenberg BS, Fisher G, Niccolls R. The Impact of Acceptance and Commitment Training and Multicultural Training on the Stigmatizing Attitudes and Professional Burnout of Substance Abuse Counselors. Behavior Therapy. 2004; 35 (4):821–835. [ Google Scholar ]
- Hayes SC, Follette VM, Linehan MM. Mindfulness and acceptance: expanding the cognitive-behavioral tradition. New York, New York: Guilford Publications Guilford Press; 2004. [ Google Scholar ]
- Hoge MA, Morris JA, Daniels AS, Stuart GW, Huey LY, Adams N. An Action Plan for Behavioral Health Workforce Development: A Framework for Discussion. Rockville, MD: 2007. [ Google Scholar ]
- Holmqvist R, Jeanneau M. Burnout and psychiatric staff's feelings towards patients. Psychiatry Res. 2006; 145 (2–3):207–213. [ PubMed ] [ Google Scholar ]
- Kerns CD. Gratitude at work: Counting your blessings will benefit yourself and your organization. Graziado Business Review. 2006; 9 (4) Retrieved from http://gbr.pepperdine.edu/2010/08/gratitude-at-work/ [ Google Scholar ]
- Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, Quill TE. Association of an Educational Program in Mindful Communication With Burnout, Empathy, and Attitudes Among Primary Care Physicians. JAMA: Journal of the American Medical Association. 2009; 302 (12):1284–1293. [ PubMed ] [ Google Scholar ]
- Leiter MP, Harvie P, Frizzell C. The correspondence of patient satisfaction and nurse burnout. Social Science & Medicine. 1998; 47 (10):1611–1617. [ PubMed ] [ Google Scholar ]
- Leiter MP, Harvie PL. Burnout among mental health workers: A review and research agenda. International Journal of Social Psychology. 1996; 42 :90–101. [ PubMed ] [ Google Scholar ]
- Leiter MP, Laschinger HKS, Day A, Oore DG. The impact of civility interventions on employee social behavior, distress, and attitudes. Journal of Applied Psychology (in press) [ PubMed ] [ Google Scholar ]
- Leiter MP, Schaufeli WB. Consistency of the burnout construct across occupations. Anxiety, Stress & Coping: An International Journal. 1996; 9 (3):229–243. [ Google Scholar ]
- Mancini AD, Moser LL, Whitley R, McHugo GJ, Bond GR, Finnerty MT, Burns BJ. Assertive community treatment: Facilitators and barriers to implementation in routine mental health settings. Psychiatric Services. 2009; 60 (2):189–195. [ PubMed ] [ Google Scholar ]
- Maslach C. Burnout: A multidimensional perspective. In: Schaufeli WB, Maslach C, Marek T, editors. Professional burnout: Recent developments in theory and research. Washington, DC: Taylor & Francis; 1993. pp. 19–32. [ Google Scholar ]
- Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3. Palo Alto, California: Consulting Psychologists Press; 1996. [ Google Scholar ]
- Maslach C, Pines A. Burnout, the loss of human caring. In: Pines A, Maslach C, editors. Experiencing social psychology. New York: Random House; 1979. [ Google Scholar ]
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001; 52 :397–422. [ PubMed ] [ Google Scholar ]
- Melchior ME, Philipsen H, Abu-Saad HH, Halfens RJ, van de Berg AA, Gassman P. The effectiveness of primary nursing on burnout among psychiatric nurses in long-stay settings. J Adv Nurs. 1996; 24 (4):694–702. [ PubMed ] [ Google Scholar ]
- Murphy LR. Stress management in work settings: a critical review of the health effects. American Journal Of Health Promotion: AJHP. 1996; 11 (2):112–135. [ PubMed ] [ Google Scholar ]
- Oddie S, Ousley L. Assessing burn-out and occupational stressors in a medium secure service. The British Journal of Forensic Practice. 2007; 9 (2):32–48. [ Google Scholar ]
- Onyett S, Pillinger T, Muijen M. Job satisfaction and burnout among members of community mental health teams. Journal of Mental Health. 1997; 6 (1):55–66. [ Google Scholar ]
- Organization, WH. The ICD-10 Classification of Mental and Behavioral Disorders. Geneva: World Health Organization; 1992. [ Google Scholar ]
- Paris M, Jr, Hoge MA. Burnout in the mental health workforce: a review. J Behav Health Serv Res. 2010; 37 (4):519–528. [ PubMed ] [ Google Scholar ]
- Peterson U, Demerouti E, Bergström G, Samuelsson M, Åsberg M, Nygren Å. Burnout and physical and mental health among Swedish healthcare workers. Journal of Advanced Nursing. 2008; 62 (1):84–95. [ PubMed ] [ Google Scholar ]
- Pines A, Aronson E. Career burnout: Causes and cures. New York, NY US: Free Press; 1988. [ Google Scholar ]
- Pines A, Maslach C. Characteristics of staff burnout in mental health settings. Hospital & Community Psychiatry. 1978; 29 (4):233–237. [ PubMed ] [ Google Scholar ]
- Priebe S, Fakhoury WKH, Hoffmann K, Powell RA. Morale and job perception of community mental health professionals in Berlin and London. Social Psychiatry and Psychiatric Epidemiology. 2005; 40 (3):223. [ PubMed ] [ Google Scholar ]
- Prosser D, Johnson S, Kuipers E, Szmukler G, Bebbington P, Thornicroft G. Perceived sources of work stress and satisfaction among hospital and community mental health staff, and their relation to mental health, burnout and job satisfaction. Journal of Psychosomatic Research. 1997; 43 (1):51–59. [ PubMed ] [ Google Scholar ]
- Robey K, Ramsland SE, Castelbaum K. Alignment of agency and personal missions: An evaluation. Administration and Policy in Mental Health. 1991; 19 (1):39–45. [ Google Scholar ]
- Rohland BM. A survey of burnout among mental health center directors in a rural state. Administration & Policy in Mental Health. 2000; 27 (4):221–237. [ PubMed ] [ Google Scholar ]
- Rollins A, Salyers M, Tsai J, Lydick J. Staff Turnover in Statewide Implementation of ACT: Relationship with ACT Fidelity and Other Team Characteristics. Administration and Policy in Mental Health and Mental Health Services Research. 2010; 37 (5):417–426. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rupert PA, Kent JS. Gender and work setting differences in career-sustaining behaviors and burnout among professional psychologists. Professional Psychology: Research and Practice. 2007; 38 (1):88–96. [ Google Scholar ]
- Salyers MP, Hudson C, Morse G, Rollins AL, Monroe-DeVita M, Wilson C, Freeland L. BREATHE: A pilot study of a one-day retreat to reduce burnout among mental health professionals. Psychiatr Serv. 2011; 62 (2):214–217. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scarnera P, Bosco A, Soleti E, Lancioni GE. Preventing burnout in mental health workers at interpersonal level: an Italian pilot study. Community Ment Health J. 2009; 45 (3):222–227. [ PubMed ] [ Google Scholar ]
- Schulz R, Greenley JR, Brown R. Organization, management, and client effects on staff burnout. Journal of Health & Social Behavior. 1995; 36 (4):333–345. [ PubMed ] [ Google Scholar ]
- Schwab RL, Jackson SE, Schuler RS. Educator burnout: Sources and consequences. Educational Research Quarterly. 1986; 10 :15–30. [ Google Scholar ]
- Siebert DC. Personal and occupational factors in burnout among practicing social workers: Implications for research, practitioners, and managers. Journal of Social Service Research. 2005; 32 (2):25–44. [ Google Scholar ]
- Smoot SL, Gonzolas JL. Cost-effective communication skills training for state hospital employees. Psychiatric Services. 1995; 46 :819–822. [ PubMed ] [ Google Scholar ]
- Stalker C, Harvey C. Partnerships for Children and Families Project. Wilfrid Laurier University; 2002. Professional burnout: A review of theory, research, and prevention. [ Google Scholar ]
- Taris TW. Is there a relationship between burnout and objective performance? A critical review of 16 studies. Work & Stress. 2006; 20 (4):316 – 334. [ Google Scholar ]
- Toppinen-Tanner S, Ojajärvi A, Väänänen A, Kalimo R, Jäppinen P. Burnout as a predictor of medically certified sick-leave absences and their diagnosed causes. Behavioral Medicine. 2005; 31 (1):18–27. [ PubMed ] [ Google Scholar ]
- van Dierendonck D, Garssen B, Visser A. Burnout Prevention Through Personal Growth. International Journal of Stress Management. 2005; 12 (1):62–77. [ Google Scholar ]
- van Dierendonck D, Schaufeli WB, Buunk BP. The evaluation of an individual burnout intervention program: The role of inequity and social support. Journal of Applied Psychology. 1998; 83 (3):392–407. [ Google Scholar ]
- van Dierendonck D, Schaufeli WB, Buunk BP. Burnout and inequity among human service professionals: A longitudinal study. Journal of Occupational Health Psychology. 2001; 6 (1):43–52. [ PubMed ] [ Google Scholar ]
- Webster L, Hackett RK. Burnout and leadership in community mental health systems. Adm Policy Ment Health. 1999; 26 (6):387–399. [ PubMed ] [ Google Scholar ]
- Application for guardianship
On this page
Application processes and the roles of the organisations involved, who is involved in the application process, vcat hearing, office of the public advocate, advocate guardian, making an application and supplying supporting information for the appointment of a guardian of last resort, the application process, the application.
Before seeking appointment of a guardian of last resort for an older person in hospital, you should explore all least restrictive options. This is in the best interests of the patient, and it is a legal requirement. The Victorian Civil and Administrative Tribunal (VCAT) will need to be satisfied that the treating team has worked with the older person and their family and carers to rule out least restrictive alternatives.
If you are satisfied that seeking guardianship is the most appropriate option, familiarise yourself with the roles of each organisation and the terminology used, to ensure you approach the formal application process in the best possible way. This page provides information about who is involved in the process when applying on behalf of an older person in hospital. You should also follow your health service’s policies and procedures, and consult the Office of the Public Advocate (OPA) website, the VCAT website and the OPA advice service for guidance on the process.
The following table outlines a list of common terms and their meanings.
| Proposed represented person | Older person who needs a guardian. |
| Applicant | Person who submits the guardianship application (you or your health service). |
| Registry VCAT Guardianship List | Receives and processes applications; appoints hearing time, place and person to decide it. |
| VCAT member | Person who hears the case and makes the decision. |
| Office of the Public Advocate | Organisation that provides guardians of last resort. Also provides advice and sometimes investigates before an application is heard by VCAT. |
| Advocate guardian | An employee of the OPA to whom the Public Advocate delegates their powers and duties in the guardianship order, when appointed as guardian by VCAT. |
Proposed represented person
This term is used by VCAT to describe the older person for whom you are making the application. Making an application has the potential to remove an older person’s rights to exercise decisions about their life and can be extremely stressful for them, their family and carers. We all play a role in providing support and empathy throughout this process.
In many Victorian hospitals, social workers coordinate and complete the application forms for guardianship. However, they can be completed by any clinician who knows the proposed represented person. Whoever completes the application becomes known by VCAT as the applicant. The applicant must explain the process to the older person and their family or carers and keep them informed throughout the process. The applicant can complete and lodge the application form online, or download it from the VCAT website. It can be lodged by email, in person or by post. Some hospitals in Victoria have an internal system for lodging applications. The applicant is expected to attend the hearing, or delegate the task to a colleague who can adequately speak to the person’s situation. As the applicant, if you believe that the matter should be heard urgently, seek advice from the OPA advice service. If the risk is unmanageable you may have to apply for a temporary order; speak to the advice service about this. By law, the applicant must provide a copy of the application to the older person and any other interested parties. Interested parties can include the person’s family and carers. The applicant must also supply VCAT with a medical report and any other supporting documents (such as a social work report or a neuropsychological report ) prior to the hearing date. The medical report must indicate what disability the proposed represented person has, how this was diagnosed, if the person is incapable of making reasonable judgement and how this has been assessed. The application may also be supported by additional clinical reports from physiotherapists, occupational therapists, and speech therapists as required. These reports should provide a context for the application and outline all least restrictive options that have been proposed and trialled. Be mindful that any individual party to the proceedings may apply to VCAT for a copy of these reports. In some circumstances, especially where a professional is feeling threatened by a person, a report may be provided under the name of the hospital rather than an individual.
Registry VCAT Guardianship List
The VCAT Guardianship List receives applications for guardianship or administration, hears the matter and makes orders appointing a guardian or administrator for a person with a disability (who is 18 years of age or over) when there is a need and it is in that person's best interests to do so. VCAT is like a court but less formal. The Tribunal members listen to the legal cases, facilitate the proceeding and decide whether an order for guardianship is required. Applications must be heard within 30 days of VCAT receiving the application; the applicant can assist to streamline this process by ensuring all relevant contact details are included on the application form. VCAT will inform all interested parties that are listed on the application of the date and venue of the hearing.
VCAT member
A VCAT member will manage all aspects of the hearing and make a decision which could include appointing a guardian or requesting OPA investigate the matter before an appointment of a guardian can be determined.
Who attends the hearing
The applicant or their delegate must attend the hearing and bring copies of relevant evidence. The person about whom the application has been made should be encouraged to attend, particularly if the hearing is on-site at a hospital. Other interested parties listed on the application will be formally invited by VCAT and they may choose to bring support people. Other people who may attend include service providers known to the older person, such as case managers and solicitors. VCAT will organise an appropriately trained interpreter to be present if the applicant has indicated that an interpreter is required on the application form. Hearings are open to the public; however the VCAT member may ask observers to leave if the matter is sensitive. VCAT can also order that hearings be closed to the public, and the applicant can request that VCAT consider this option. It is illegal to publicise any information of a proceeding unless VCAT orders otherwise.
Where hearings are held
Some hospitals in Victoria hold regular guardianship and administration hearings on site. In special circumstances hearings can be held at the older person’s bedside. Hearings can also take place at VCAT in Melbourne and at various local courts throughout Victoria. The applicant can nominate the preferred venue for the hearing, and should take into account the urgency of the matter and whether there might be a need for security to be on-call throughout the hearing. Hearings may also be held with some or all parties attending by phone or video-conference.
What to expect at the hearing
The formality of the hearing can vary depending on the venue and the VCAT member. The VCAT member will generally ask all present to introduce themselves and they will explain the purpose of the hearing. Sometimes the VCAT member may decide to adjourn the hearing if a particular person is not in attendance. They may also decide to refer the matter to OPA to investigate the issues and report back to them before the matter can be determined. The VCAT member may also adjourn a hearing part heard to enable OPA to gather new information or research issues which have arisen in the course of the hearing. Before deciding to appoint a guardian, the VCAT member must be satisfied that the proposed represented person:
- has a disability that is affecting their ability to make an informed decision
- that a decision needs to be made
- that all least restrictive options have been explored.
- encourage the represented person to participate as much as possible in the life of the community
- encourage and assist the represented person to become capable of caring for herself or himself and of making reasonable judgements about matters relating to her or his person
- protect the represented person from neglect, abuse or exploitation.
A guardian must also exercise their powers in a way which is least restrictive of the person’s freedom of decision and action.
The OPA website provides detailed information on the role and responsibilities of guardians. Guardians are not case managers, and when appointed they will rely on the treating team to source and implement least restrictive opportunities. It may take some time for the guardian to come to a decision for the older person in hospital, and as clinicians it is our role to support the older person and their family and carers throughout this process. It is also essential that we document continued attempts to trial least restrictive alternatives and work with our team to ensure the person’s ability to participate in everyday physical and cognitive tasks is encouraged and assisted.
The decision to lodge an application to VCAT for the appointment of a guardian of last resort should only be made if you and the treating team are satisfied that an older person has a disability that is impacting on their ability to make an informed decision, and when:
- a decision needs to be made
- there is a conflict about the nature of this decision
- you have trialled all least restrictive alternatives.
In many Victorian hospitals social workers are the 'applicant' and coordinate the application process. This includes:
- completing the application form and an accompanying report
- seeking advice from the OPA Advice Service
- discussing the decision to proceed with the application with the older person and their family and carers
- requesting reports from the treating doctor and other relevant clinicians.
Application forms can be completed and lodged on the VCAT website and downloaded as an alternative if required. As the applicant, it is essential that you provide the correct contact details for yourself and any interested parties, to ensure that the hearing is listed within the specified 30-day period and that the appointed guardian contacts the relevant parties as soon as possible.
Medical report
Use the medical report form provided on the VCAT website to describe:
- previous admissions to hospital
- nature of the decision-making disability
- how this is affecting the decision that needs to be made
- the trajectory of the admission, treatment provided, the person's ability to participate in their care routing and the level of support they require
- your recommendation.
Examples of the information required in the medical report is provided in Mrs Brown's case study.
Social work report
Each person’s situation will be unique. As the application form has minimal space to provide the VCAT member with the relevant context, you may need to provide a separate report to support the application. There is no universal template to guide this process; however, it would be helpful for the VCAT member if you provided as much relevant background information as possible, including the following:
- nature of the decision making disability.
- What is the trajectory of the admission, treatment provided, the person's ability to participate in their care routine and the level of support they require?
- What decision needs to be made?
- If the issue is long standing, describe the history and what attempts have been made to address the issue.
- Do they own their own home?
- Are there any relevant cultural, language preferences and values?
- Do they live by themselves or with others?
- Who is in their family/support network and what is their opinion of the reason for the application?
- Outline if the person has been receiving services.
- Determine if the person has an advance care plan or an advance statement.
- Is there a risk of harm?
- What level of supervision does the team believe the older person requires?
- Can these risks be minimised with formal services or informal supports?
- What least restrictive attempts have been made to mitigate the risks?
- Include physical therapy/retraining, education to the older person and their family/carers, psychological and emotional support that acknowledges and assists the older person and their family and carers with the process of adjustment.
- Has an occupational therapy home visit occurred? Have assistive devices been considered and trialled?
- Have you spoken to the OPA Advice Service? If so, document their advice.
- What will the appointment of a guardian achieve?
- Specify what decisions the team believe need to be made. This can include accommodation, access to services, access to the proposed represented person and medical, dental and other healthcare treatments.
- Why are you recommending that OPA be appointed as guardian of last resort?
An example of a social work report is provided in Mrs Brown's case study.
Mrs Brown: A sample case study
This is a fictitious case that has been designed for educative purposes.
Mrs Beryl Brown URN102030 20 Hume Road, Melbourne, 3000 DOB: 01/11/33
Date of application: 20 August 2019
Social work report: Background
Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke, which has left her with moderate weakness in her left arm and leg. A diagnosis of vascular dementia was also made, which is overlaid on a pre-existing diagnosis of Alzheimer’s disease (2016). Please refer to the attached medical report for further details.
Social work report: Social history
I understand that Mrs Brown has been residing in her own home, a two-story terrace house in Melbourne, for almost 60 years. She has lived alone since her husband died two years ago following a cardiac arrest. She has two daughters. The youngest daughter Jean has lived with her for the past year, after she lost her job. The eldest daughter Catherine lives on the Gold Coast with her family. Mrs Brown is a retired school teacher and she and both daughters describe her as a very private woman who has never enjoyed having visitors in her home. Mrs Brown took much encouragement to accept cleaning and shopping assistance once a week after her most recent admission; however, she does not agree to increase service provision. Jean has Enduring Power of Attorney (EPOA) paperwork that indicates that Mrs Brown appointed her under an EPOA two years ago. She does not appear to have appointed a medical treatment decision maker or any other decision-supporter.
I also understand from conversations with her daughters that Jean and Mrs Brown have always been very close and that there is a history of long-standing conflict between Catherine and Jean. This was exacerbated by the death of their father. Both daughters state they understand the impact of the stroke on their mother’s physical and cognitive functioning, but they do not agree on a discharge destination. Mrs Brown lacks insight into her care needs and says she will be fine once she gets back into her own home. Repeated attempts to discuss options with all parties in the same room have not resulted in a decision that is agreeable to all parties.
Social work report: Current function
Mrs Brown has a history of Alzheimer’s disease; type II diabetes – insulin dependent; hypertension; high cholesterol and osteoarthritis. She has had two recent admissions to hospital for a urinary tract infection and a fall in the context of low blood sugars. She is currently requiring one to two people to assist her into and out of bed and one person with managing tasks associated with post-toilet hygiene. She can walk slowly for short distances with a four-wheel frame with one person to supervise. She benefits from prompting to use her frame; she needs someone to cut her food and to set her up to eat and drink regularly and to manage her medication routine. She requires one person to assist her to manage her insulin twice daily.
The team believe that Mrs Brown’s capacity for functional improvement has plateaued in the last ten days. They recommend that it is in her best interests to be discharged to a residential care setting due to her need for one to two people to provide assistance with the core tasks associated with daily living. Mrs Brown is adamant that she wants to return home to live with Jean who she states can look after her. Jean, who has a history of chronic back pain, has required several admissions to hospital over the past five years, and states she wants to be able to care for her mother at home. Jean states she is reluctant to agree to extra services as her mother would not want this. Her sister Catherine is concerned that Jean has not been coping and states that given this is the third admission to hospital in a period of few months, believes it is now time for her mother to enter residential care. Catherine states that she is very opposed to her mother being discharged home.
Social work report: The current risks
Mrs Brown is at high risk of experiencing falls. She has reduced awareness of the left side of her body and her ability to plan and process information has been affected by her stroke. She is now requiring one to two people to assist with all her tasks of daily living and she lacks insight into these deficits. Mrs Brown is also at risk of further significant functional decline which may exacerbate Jean’s back pain. Jean has stated she is very worried about where she will live if her mother is to enter residential care.
Social work report: Attempts to trial least restrictive options
We have convened two family meetings with Mrs Brown, both her daughters and several members of the multi-disciplinary team. The outcome of the first meeting saw all parties agree for the ward to provide personalised carer training to Jean with the aim of trialling a discharge home. During this training Jean reported significant pain when transferring her mother from the bed and stated she would prefer to leave her mother in bed until she was well enough to get out with less support.
The team provided education to both Jean and Catherine about the progressive impact of their mother’s multiple conditions on her functioning. The occupational therapist completed a home visit and recommended that the downstairs shower be modified so that a commode can be placed in it safely and the existing dining room be converted into a bedroom for Mrs Brown. Mrs Brown stated she would not pay for these modifications and Jean stated she did not wish to go against her mother’s wishes. The team encouraged Mrs Brown to consider developing a back-up plan and explore residential care options close to her home so that Jean could visit often if the discharge home failed. Mrs Brown and Jean refused to consent to proceed with an Aged Care Assessment that would enable Catherine to waitlist her mother’s name at suitable aged care facilities. We proceeded with organising a trial overnight visit. Unfortunately, this visit was not successful as Jean and Catherine, who remained in Melbourne to provide assistance, found it very difficult to provide care without the use of an accessible bathroom. Mrs Brown remains adamant that she will remain at home. The team is continuing to work with the family to maximise Mrs Brown’s independence, but they believe that it is unlikely this will improve. I have spent time with Jean to explore her adjustment to the situation, and provided her with information on community support services and residential care services. I have provided her with information on the Transition Care Program which can assist families to work through all the logistics. I have provided her with more information on where she could access further counselling to explore her concerns. I have sought advice on the process and legislative requirements from the Office of the Public Advocate’s Advice Service. I discussed this process with the treating team and we decided that it was time to lodge an application for guardianship to VCAT.
Social work report: Recommendation
The treating team believe they have exhausted all least restrictive alternatives and that a guardianship order is required to make a decision on Mrs Brown’s discharge destination and access to services. The team recommend that the Public Advocate be appointed as Mrs Brown’s guardian of last resort. We believe that this is the most suitable arrangement as her daughters are not in agreement about what is in their mother’s best interests. We also believe that there is a potential conflict of interest as Jean has expressed significant concern that her mother’s relocation to residential care will have an impact on her own living arrangements.

Medical report: Background information
Mrs Brown’s medical history includes Alzheimer’s disease; type II diabetes; hypertension; high cholesterol and osteoarthritis. She was admitted to Hume Hospital on 3 March 2019 following a stroke that resulted in moderate left arm and leg weakness. This admission was the third hospital admission in the past year. Other admissions have been for a urinary tract infection, and a fall in the context hypoglycaemia (low blood sugars), both of which were complicated by episodes of delirium.
She was transferred to the subacute site under my care, a week post her admission, for slow-stream rehabilitation, cognitive assessment and discharge planning.
Mrs Brown was diagnosed with Alzheimer’s disease by Dr Joanne Winters, Geriatrician, in April 2016. At that time, Mrs Brown scored 21/30 on the Standardised Mini-Mental State Examination (SMMSE). During this admission, Mrs Brown scored 15/30. I have undertaken cognitive assessment and agree with the diagnosis; further cognitive decline has occurred in the context of the recent stroke. There are global cognitive deficits, but primarily affecting memory, attention and executive function (planning, problem solving, mental flexibility and abstract reasoning). The most recent CT-Brain scan shows generalised atrophy along with evidence of the new stroke affecting the right frontal lobe. My assessments suggest moderate to severe mixed Alzheimer’s and vascular dementia.
Medical report: Financial and legal affairs
While able to recall some key aspects of her financial affairs, including the general monetary value of her pension and regular expenses, Mrs Brown was unable to account for recent expenditure (for repairs to her home) or provide an estimate of its value, and had difficulty describing her investments. In addition, I consider that she would be unable to make complex financial decisions due to her level of cognitive impairment. Accordingly, I am of the view that Mrs Brown now lacks capacity to make financial decisions.
Mrs Brown states that she previously made an Enduring Power of Attorney (EPOA) but could no longer recall aspects of the EPOA, such as when it would commence and the nature of the attorney’s powers. Moreover, she confused the EPOA with her will. Her understanding of these matters did not improve with education, and therefore I consider that she no longer has capacity to execute or revoke an EPOA.
Medical report: General living circumstances
Mrs Brown acknowledges that she needs some assistance but lacks insight into the type of assistance that she requires, apart from home help for cleaning and shopping. She does not appreciate her risk of falling. She is unable to get in and out of bed without at least one person assisting her. She frequently forgets to use her gait aid when mobilising and is not able to describe how she would seek help in the event of falling. She is not able to identify or describe how she would manage her blood sugar levels, and this has not improved with education. Accordingly, I consider that she lacks capacity to make decisions about accommodation arrangements and services.
Mrs Brown does not agree with the treating team’s recommendation to move into residential care and maintains her preference to return home. This is in spite of a failed overnight trial at home with both her daughters assisting her. Unfortunately, she was unable to get out of bed to get to the toilet and required two people to assist her to do so in the morning. In light of these matters, and in the context of family disagreement regarding the matter, the team recommends that the Office of the Public Advocate be appointed as a guardian of last resort.
Reviewed 17 July 2024
- Print full document
Older people in hospital
- Hospital environment audit tool (HEAT)
- On the ward - limited resources
- On the ward
- Hospital environment audit tool - policy and procedure
- Hospital environment audit tool - facility audits
- Patient bedside orientation
- Assessment, communication and person-centred practice
- Person-centred practice
- Screening and assessment
- Communication and older people in hospital
- Communicating with older people
- Cognition - dementia, delirium and depression
- Differential diagnosis - depression, delirium and dementia
- Cognitive impairment screening
- Dementia in older people
- Managing dementia
- Continence in older people
- Falls, mobility and self-care
- Mobility and self-care
- Identifying frailty
- Nutrition and swallowing in older people
- Nutrition and hydration
- Pain in older people
- Palliative approach to caring for older people
- Managing needs of older people during palliative care
- Pressure injuries and skin tears
- Classifying and responding to pressure injuries and skin tears
- Identifying and preventing skin problems
- Supporting information for older people in hospital
- Guardianship and least restrictive practice in Victoria
- Least restrictive practice
- Decision making for older people
- Consumer information for older people in hospital
- Implementation case studies
- Clinical handover for older people in hospital
- Improving access
- Improving Care for Older People Program - Health service initiatives
Share this page
- Facebook , opens a new window
- X (formerly Twitter) , opens a new window
- LinkedIn , opens a new window
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
It’s a New Era for Mental Health at Work
- Kelly Greenwood

Research on how the past 18 months have affected U.S. employees — and how companies should respond.
In 2019, employers were just starting to grasp the prevalence of mental health challenges at work, the need to address stigma, and the emerging link to diversity, equity, and inclusion (DEI). One silver lining amid all the disruption and trauma over the last two years is the normalization of these challenges. In a follow-up study of their 2019 Mental Health at Work Report, Mind Share Partners’ 2021 Mental Health at Work Report, the authors offer a rare comparison of the state of mental health, stigma, and work culture in U.S. workplaces before and during the pandemic. They also present a summary of what they learned and their recommendations for what employers need to do to support their employees’ mental health.
When we published our research on workplace mental health in October 2019, we never could have predicted how much our lives would soon be upended by the Covid-19 pandemic. Then the murders of George Floyd and other Black Americans by the police; the rise in violence against Asian Americans and Pacific Islanders (AAPIs); wildfires; political unrest; and other major stressors unfolded in quick succession, compounding the damage to our collective mental health.
- Kelly Greenwood is the Founder and CEO of Mind Share Partners , a national nonprofit changing the culture of workplace mental health so both employees and organizations can thrive. Through movement building , custom training, and strategic advising, it normalizes mental health challenges and promotes sustainable ways of working to create a mentally healthy workforce. Follow her on LinkedIn and subscribe to her monthly newsletter.
- Julia Anas is the chief people officer at Qualtrics, the world’s #1 Experience Management (XM) provider and creator of the XM category. At Qualtrics, she is responsible for building a talented and diverse organization and driving employee development as well as organizational design, talent, and succession planning.
Partner Center
Recommended pages
- Undergraduate open days
- Postgraduate open days
- Accommodation
- Information for teachers
- Maps and directions
- Sport and fitness
Mental health practice case studies
Each of these short films presents a case study of a potentially difficult mental health situation that practitioners may need to deal with as part of their practice. Topics covered include appropriate listening skills, confidentiality, drug use, professional conduct, anger, social isolation, sexual advances and stereotyping. The aim of these films is to stimulate discussion and reflection about these particular situations and the issues that arise from them.
The following group of case studies form part of the Online Assessment Workbook.
See also Mental health case studies which were filmed as part of the SELF Project.
Return to film Index
- Find a Social Worker
About social work
Where social workers work
What social workers do
How social workers work
How to Find a Social Worker
Seeing a social worker
- Constitution & bylaws
Board of directors
AASW elections
Annual general meetings
Annual Reports
AASW structure
Strategic plan 24-27
Reconciliation action plan
Our history
- Practice & networking groups
Opportunities with AASW
Work with us
Volunteer with us
Employment partnerships
Sponsorships
Advertising
- Awards & grants
- Life Member
- AASW Fellow
Social Policy & Advocacy
Policy positions
Advocacy for the Profession
Registration of social work in Australia
Ethics and Standards
Code of ethics
Practice standards
Ethics consultation service
Making a complaint
Constitution & bylaws
Practice & networking groups
Awards & grants
Life member
AASW fellow
Become a member
- Membership FAQs
Credential Program
Renewal FAQs
Continuing professional development (CPD)
CPD overview
- Specialist learning programs & workshops
On Demand Learning
Live-online Webinars and Workshops
- Branch CPD & events
CPD Newsletter Subscription
Employer partnership program
Become an employer partner
Benefits to employers
Benefits to employees
Practice and careers
- Support & resources
Social work community
Mentoring program
AASW community hub
Credentials Program
- AASW credentials
Find CPD & Events
Specialist learning programs & workshops
Branch CPD & events
Support & resources
AASW Credentials
Higher education providers
Accredited Programs
Accreditation Process
Accreditation Roles
Additional Information
Migration & eligibility assessment (MEA)
Working Overseas
- Migration & eligibility assessment
International qualification recognition
New Zealand Mutual Recognition
International students studying an AASW accredited social work course in Australia
Temporary Graduate Visa Subclass 485
Renewals and reissue of Assessments
Optional migration assessments
Reassessment, internal review and external appeal
Horizon Career Centre
Mea online applications.
Migration & eligibility assessment
News and Media Releases
- News & media releases
- Information for the media
AASW in the media
Newsletters
Publications
Social Work Focus
Australian Social Work
News & media releases
Information for the Media
- Find a social worker
- AASW Accredited Mental Health Social Worker Application Criteria
- Credentials
- Mental Health
- Family Violence
- Child Protection
- Older Persons
In 2004, the Australian Government implemented the Enhanced Primary Care Program under which General Practitioners were able to refer patients with complex care requirements to a range of allied health services. Under this initiative social workers were recognised as one of the group of eligible mental health providers. In 2006, the Government introduced the ‘Better Access to Mental Health Care’ initiative, under which General Practitioners, Paediatricians and Private Psychiatrists could refer to suitably qualified and experienced allied health professionals namely: social workers; psychologists and occupational therapists for the provision of ‘Focussed Psychological Strategies’. This document explains the process which a social worker must undergo, should they wish to be considered by Medicare Australia as ‘suitably qualified and experienced allied health professional’.
Please refer to information below as to the 6 AMHSW criteria that must ALL be met to gain a successful outcome:
- Hold current eligible AASW membership
- Have at least 2 years’ full-time equivalent (FTE) post-qualifying social work experience* in a mental health setting within the last 5 years , totalling a minimum of 3,360 hours. The AASW recognises that full-time employment equates to 35 hours per week, for 48 weeks per year.
- Must be able to articulate your understanding and provide a case example on how your experience meets the AASW Practice Standards for Mental Health Social Workers 2014 . Where applicable, you must demonstrate the use of Focused Psychological Strategies (FPS), within your case example from your mental health practice position/s.
- Demonstrate at least 2 years’ full-time equivalent (FTE) post-qualifying supervision in a mental health setting/field within the last 5 years. You should be able to show that they have been formally supervised, in line with the AASW Supervision Standards . Generally, supervisors should have a higher level of practice experience than their supervisees and should have some training in supervision. For the purposes of this assessment, the supervisor does not necessarily need to have a social work background but should have provided the applicant/supervisee with appraisal and assessment in relation to practice in a mental health field (e.g. psychologist, medical practitioner or a mental health nurse).
- Have met the Continuing Professional Development requirements
- Demonstrate ability and knowledge of clinical Mental Health social work practice through Case study activities. Further information on the case study activity can be found on Case Study Activity
- Curriculum vitae: the CV or resume allows our assessor to get an overall picture of your social work experience. Please ensure the dates align with all the evidence you provide.
- Referee statement: You must provide the official AASW referee statement form completed, signed and dated by an employer or supervisor that validates your work and performance in a mental health setting/field using FPS. For the purposes of this credential, the referee must have appropriate qualifications and experience in mental health in order to provide appropriate assessment and appraisal of an applicants mental health practice and particularly your use of and competence in FPS. The form must also confirm the exact dates and hours per week of employment.
- Position description: an official agency position description on organisation letter head to confirm the key duties and responsibilities of the role.
Note for applicants who are self-employed in private practice
In addition to submitting a referee statement, you will need to provide a signed and declared statutory declaration outlining details of your roles and responsibilities in lieu of a position description. You will need to include the dates and approximate hours per week that you have worked in your private practice role, in particular, your clinical work with mental health clients, utilising FPS, and the percentage of time which is spent in this clinical mental health work.
Why be a member?
When you join the AASW you’ll become part of an active and vibrant community of more than 17,000 social work professionals. As the profession’s peak body, the AASW is committed to maintaining high standards, ethical practice and ongoing professional development.
Access on-demand content, live workshops and events at up to 50% discount as a member
National office
Level 7, 14-20 Blackwood St NORTH MELBOURNE 3051
PO Box 2008 Royal Melbourne Hospital VIC 3050
P: 03 9320 1000
Quick Links
Site information, get the latest cpd news & events, connect with us.
The AASW respectfully acknowledges Aboriginal and/or Torres Strait Islander peoples as the First Australians, and pay our respects to Elders past and present.
© 2023 - AASW Copyright

- Master of Social Work
- Paths of Study
Mental Health
- Mental health with adults: On-campus, Intensive Weekend, Online
- Mental health with children and adolescents: On-campus
Due to an increased awareness of compelling public health challenges, clinical social workers and therapists have moved to the forefront of identifying and advancing solutions to some of society’s most formidable public health challenges, including violence, trauma, suicide, and co-occurring substance abuse and mental health disorders.
The mental health specialization will prepare you for community‐based mental health practice in a variety of professional settings, such as hospitals, schools, child and family service agencies, substance abuse treatment programs and mental health centers.
The Mandel School’s mental health specialization faculty are advanced-level clinicians with extensive experience working in premiere mental health community treatment settings. In this specialization, you will integrate knowledge of biopsychosocial assessment and clinical practice theories with relevant content from rigorous evidence-based interventions. By graduation, you will have developed a solid foundation of practice skills, preparing you for clinical case manager and therapist positions.
Learn to incorporate strategies maximizing client and community strengths guided by recovery and resiliency philosophies, and think critically about how to leverage the myriad ways social and cultural diversity influences illness manifestations, wellness trajectories and treatment pathways.
Public mental health service provision requires a keen trauma-informed lens that accounts for the varied and complex clinical presentations encountered by therapists. At the Mandel School, you will become well-versed in trauma assessment as well as treatment approaches, allowing you to integrate trauma work within diverse clinical populations served through multiple human service sectors including health, behavioral health, education, child welfare, adult protective services, and juvenile and criminal justice.
From the Chair

"The Mandel School’s mental health specialization is ideally suited to integrate the resources of the school’s violence research and evidence-based practice training centers with advanced community mental health practice partners to educate the next generation of social work mental health and behavioral health clinicians.”
—David Hussey, PhD, associate professor, chair of the mental health specialization
Related Opportunities
- Advanced standing
- Certificates
- Combined graduate study (3+2 social work)
- Dual degrees
- Interprofessional education
- School social work
- Study abroad
Careers in Mental Health
- Case manager
- Care coordinator
- Child therapist
- Crisis response worker
- Family therapist
- Mental health counselor
- Program manager/director
- Psychotherapist

“One great memory of my time at the Mandel School was my second year field placement at Circle Health Services as a Behavioral Health Intern. I really enjoyed being in my role, the staff, the other interns, my clients and my supervisor who was an alum from the Mandel School.”
—Leah Adams, MSSA/MNO 2019
Sample Courses
- Mental Health Policy and Service Delivery
- Social Work in Child Abuse/Family Violence
- Social Work Practice in Mental Health: Adults
- Social work Practices in Mental Health: Children/Adolescents
Examples of Field Education Sites
- Catholic Charities
- Centers for Families and Children
- Cleveland Rape Crisis Center
- National Youth Advocate Program
Greater Good Science Center • Magazine • In Action • In Education
How Your Relationships Affect Your Health
All of us have heard guidelines about how to be physically healthy—eat well, exercise, wash your hands, get plenty of rest. But how many of us have thought seriously about our social lives—the strength of our relationships and our sense of belonging in a community—as key to staying healthy?
We may have some vague idea that relationships are important to our well-being. But we often don’t act like that’s the case, taking social connections for granted in the name of work or other pursuits.
Kasley Killam, author of the new book The Art and Science of Connection , sees this as a problem. Killam, a social scientist who’s been disseminating the science of social connection for more than a decade, argues that social health matters as much to our well-being as mental and physical health—and, in fact, is interrelated to each and necessary for keeping us fit. Through her book and her organization, Social Health Labs , she tries to encourage more people to prioritize their relationships with others.
“If you nourish your body and mind but neglect your relationships, your overall health may be compromised. In contrast, prioritizing your connection—in addition to habits that support your physical and mental health—can help you live longer, healthier, and happier,” she writes.
How social health affects everything else
What does Killam mean by “social health?” For her, it refers to “deeper connection, mutual support, and a good relationship with yourself” and “having the support you need and feeling cared for, understood, valued, and like you belong.”
This may seem like a strange marker of good health. But, as Killam argues, it’s a critical one—and researchers and health professionals, including the U.S. Surgeon General , are taking note.
For example, in one 1979 study of almost 7,000 adults, researchers found that people without social or community ties were more than twice as likely to die within nine years, regardless of their health habits (including smoking, drinking, or exercising regularly). Since then, decades of research have corroborated the connection between social ties and longevity, including a 2021 analysis of many prior studies.
Strong social connections also matter for disease prevention, Killam writes. For example, one study highlighted in the book found that people who had stronger relationships were much less likely to get cardiovascular disease or have a stroke. Another found that people who felt supported and received more hugs were less likely to develop a cold after being exposed to a virus. Something about our relationships not only makes us feel less vulnerable, but makes us literally less vulnerable, she says.
“When you spend time with family or friends, invite a coworker to lunch, or strike up a conversation with a neighbor, do you realize the interaction influences whether or not you —and they—will develop heart disease, diabetes, depression, or dementia?” she says. “Health is not only physical or mental. Health is also social.”
Of course, it’s hard with studies like these to prove cause and effect, and Killam recognizes that. But researchers can’t actually deprive people of social contact in an experiment to see what happens; they must rely on survey data. Still, the same is true of other potential health risks, like smoking, she argues; yet we accept that smoking causes cancer. Similarly, at least some researchers conclude that poor social connection causes poor physical health, making it an urgent matter for us all.
Killam is concerned that people don’t recognize how strong the link actually is—or they dismiss the importance of social ties as something relevant only to their emotional lives.
While social health is certainly important for mental health, she hopes that focusing more on how it affects physical health will elevate the issue in people’s minds.
“The wide-reaching significance of relationships is overlooked and underappreciated because it has been buried in the conversation on mental health. This is a huge problem,” she writes. “Human connection is so important, so influential for our overall health and longevity, that it deserves to rise from the shadows and stand tall in the spotlight.”
How to work on improving social health
To that end, much of Killam’s book is devoted to helping individuals improve their social health. But first, she believes people should assess the current health of their relationships and networks—just like you might do an assessment of your physical health.
To do that, she suggests looking closely at the relationships in your life—with loved ones, friends, work colleagues, neighbors, and your larger communities—as well as your individual needs for social contact (for example, if you’re more of an introvert or extrovert). By reflecting on the quality and quantity of relationships you currently have, you can decide if adjustments are needed (or not) and which of four basic strategies Killam outlines would be best for you.
1. “Stretch if the quantity is low.” If you have fewer social ties than you want, you may need to expand the places where you are looking to connect with people. For example, if you move to a new town and don’t know anyone, you may need to join a local club or introduce yourself to your neighbors. Even if you have been living in the same place for years, you could expand your circle by going to new places or just being friendlier with the people around you. Peripheral ties can lead to closer ties and are also valuable for well-being on their own merit, says Killam.
2. “Rest if the quantity is high.” Some people feel they have too many social ties and become overwhelmed by their social responsibilities—particularly if they are more introverted and need time alone to rejuvenate. If this is you, you may want to pull back some from your wider social network and focus more on the people closest to you—your near and dear friends—while saying “no” to multiple social events.
3. “Tone if the quality is low.” Sometimes we have lots of social connection, but we’re still lonely, because we don’t feel close to anyone. In this case, you may need to take more risks to increase intimacy with the people you already know, perhaps by sharing a personal struggle and asking for advice, or by expressing gratitude for that person, says Killam. She points to the importance of having meaningful connections in one’s life and to authors like Marisa Franco, whose book, Platonic , sheds light on how to increase intimacy within friendships.
4. “Flex if the quality is high.” When the quality of your relationships is high, you may not need to do much but general maintenance—continuing to do whatever is working in nurturing your relationships. “For social health, flex your social muscles to enjoy the benefits of mutual, meaningful connection in your life,” writes Killam.
Of course, we may need different strategies at different times. But Killam also encourages people to go beyond their comfort zones on occasion—especially when it comes to connecting with strangers. While you may be reluctant to do that, one study found that both introverts and extroverts benefitted in their daily lives from having more frequent and deeper conversations with other people, even though you might not expect that for introverts.
For those who want something more specific, Canadian researchers created numeric guidelines on how much socialization you need, based on mass surveys . Partly inspired by that, Killam gives her own shorthand “prescription” for social health: “First, connect with five different people every week. Second, maintain at least three close relationships in general. And, third, dedicate at least one hour each day to social interaction.”
Like other health guidelines, these don’t need to be followed to the letter. But aiming to follow them could result in better social health.
“Just like we’re told to walk 10,000 steps, get eight hours of sleep, or drink eight glasses of water per day, guidelines can be helpful,” she says.
What gets in the way of greater social health
Not everyone is at ease reaching out to others, perhaps fearing rejection or embarrassment. But maybe you’re being more cautious than you need to be, writes Killam, as research suggests people tend to enjoy social connection more than they think they will and underestimate how much others will like them or appreciate them if they reach out.
Some tips for connecting that Killam promotes include things like volunteering in your community, being vulnerable and self-disclosing (selectively) with others, expressing gratitude, or doing good deeds—all of which have been found to improve relationships. And, while many of these strategies will benefit you, they’ll also benefit the people around you, helping to create a warmer, more inviting social milieu for everyone.
Still, social health shouldn’t be left up to individuals alone, Killam argues. We need to make our neighborhoods, workplaces, urban spaces, and governments more conducive to inviting social interaction and connection. To that end, she describes projects happening around the world that are aimed at improving social health, from creating neighborhood gathering places (like public parks) to planning community events to supporting organizations that bring together people with shared hobbies to fostering intergenerational connection—and more.
While these programs may start as the brainchild of an individual, they are often supported by communities and government agencies that recognize the need for greater social interaction for all. And that, writes Killam, is good for everyone.
“Better access to gathering places is linked to more familiarity among neighbors, higher trust, and greater community cohesion—factors which serve society as a whole,” she writes. “And we know that all of these factors should improve social health—contributing to longer, healthier, and happier lives.”
About the Author

Jill Suttie
Jill Suttie, Psy.D. , is Greater Good ’s former book review editor and now serves as a staff writer and contributing editor for the magazine. She received her doctorate of psychology from the University of San Francisco in 1998 and was a psychologist in private practice before coming to Greater Good .
You May Also Enjoy

How Feeling Socially Connected Can Help With Chronic Pain

A Healthy Social Life Goes Beyond Friends and Family

Seven Guidelines for Healthy Social Connection

How Social Connections Keep Seniors Healthy

How Your Social Life Might Help You Live Longer

Why Relationships Are the Secret to Healthy Aging
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Social capital - a mixed blessing for women? A cross-sectional study of different forms of social relations and self-rated depression in Moscow
Affiliations.
- 1 Stockholm Centre for Health and Social Change (SCOHOST), Department of Sociology, School of Social Sciences, Södertörn University, 141 89, Huddinge, Sweden. [email protected].
- 2 Stockholm Centre for Health and Social Change (SCOHOST), Department of Sociology, School of Social Sciences, Södertörn University, 141 89, Huddinge, Sweden.
- 3 European Centre on Health of Societies in Transition (ECOHOST), London School of Hygiene and Tropical Medicine, London, UK.
- 4 Department of Human Ecology, Graduate School of Medicine, University of Tokyo, Tokyo, Japan.
- 5 Department of Quality of Life Measurement Problems at the Institute of Economics, Russian Academy of Sciences, Moscow, Russia.
- 6 Stockholm Centre for Health and Social Change (SCOHOST), Department of Social Work, School of Social Sciences, Södertörn University, Huddinge, Sweden.
- 7 Department of Sociology, Uppsala University, Uppsala, Sweden.
- PMID: 27449106
- PMCID: PMC4957323
- DOI: 10.1186/s40359-016-0144-1
- Erratum to: Social capital-a mixed blessing for women? A cross-sectional study of different forms of social relations and self-rated depression in Moscow. Ferlander S, Stickley A, Kislitsyna O, Jukkala T, Carlson P, Mäkinen IH. Ferlander S, et al. BMC Psychol. 2017 Jun 19;5(1):20. doi: 10.1186/s40359-017-0190-3. BMC Psychol. 2017. PMID: 28629402 Free PMC article. No abstract available.
Background: Depression is a major health problem worldwide, especially among women. The condition has been related to a number of factors, such as alcohol consumption, economic situation and, more recently, to social capital. However, there have been relatively few studies about the social capital-depression relationship in Eastern Europe. This paper aims to fill this gap by examining the association between different forms of social capital and self-rated depression in Moscow. Differences between men and women will also be examined, with a special focus on women.
Methods: Data was obtained from the Moscow Health Survey, which was conducted in 2004 with 1190 Muscovites aged 18 years or above. For depression, a single-item self-reported measure was used. Social capital was operationalised through five questions about different forms of social relations. Logistic regression analysis was undertaken to estimate the association between social capital and self-rated depression, separately for men and women.
Results: More women (48 %) than men (36 %) reported that they had felt depressed during the last year. An association was found between social capital and reported depression only among women. Women who were divorced or widowed or who had little contact with relatives had higher odds of reporting depression than those with more family contact. Women who regularly engaged with people from different age groups outside of their families were also more likely to report depression than those with less regular contact.
Conclusions: Social capital can be a mixed blessing for women. Different forms of social relations can lead to different health outcomes, both positive and negative. Although the family is important for women's mental health in Moscow, extra-familial relations across age groups can be mentally distressing. This suggests that even though social capital can be a valuable resource for mental health, some of its forms can be mentally deleterious to maintain, especially for women. More research is needed on both sides to social capital. A special focus should be placed on bridging social relations among women in order to better understand the complex association between social capital and depression in Russia and elsewhere.
PubMed Disclaimer
Similar articles
- Social capital, gender and self-rated health. Evidence from the Moscow Health Survey 2004. Ferlander S, Mäkinen IH. Ferlander S, et al. Soc Sci Med. 2009 Nov;69(9):1323-32. doi: 10.1016/j.socscimed.2009.08.009. Epub 2009 Sep 10. Soc Sci Med. 2009. PMID: 19748170
- Gender variations in the relationship between social capital and mental health outcomes among the Indigenous populations of Canada. Levesque A, Quesnel-Vallée A. Levesque A, et al. Int J Equity Health. 2019 Aug 14;18(1):124. doi: 10.1186/s12939-019-1028-9. Int J Equity Health. 2019. PMID: 31412891 Free PMC article.
- Group involvement and self-rated health among the Japanese elderly: an examination of bonding and bridging social capital. Kishimoto Y, Suzuki E, Iwase T, Doi H, Takao S. Kishimoto Y, et al. BMC Public Health. 2013 Dec 17;13:1189. doi: 10.1186/1471-2458-13-1189. BMC Public Health. 2013. PMID: 24341568 Free PMC article.
- Investigation into the metric properties of the workplace social capital questionnaire and its association with self-rated health and psychological distress amongst Greek-Cypriot registered nurses: cross-sectional descriptive study. Middleton N, Andreou P, Karanikola M, Kouta C, Kolokotroni O, Papastavrou E. Middleton N, et al. BMC Public Health. 2018 Aug 23;18(1):1061. doi: 10.1186/s12889-018-5959-7. BMC Public Health. 2018. PMID: 30139337 Free PMC article.
- Bonding, Bridging, and Linking Social Capital and Self-Rated Health among Chinese Adults: Use of the Anchoring Vignettes Technique. Chen H, Meng T. Chen H, et al. PLoS One. 2015 Nov 16;10(11):e0142300. doi: 10.1371/journal.pone.0142300. eCollection 2015. PLoS One. 2015. PMID: 26569107 Free PMC article.
- Factors related to the social network of core members of elderly care service social organizations: a cross-sectional study. Wang Z, Zhang X, Liu L, Tang L, Zhu Y, Bai Z, Chen R. Wang Z, et al. BMC Health Serv Res. 2022 Sep 10;22(1):1147. doi: 10.1186/s12913-022-08545-7. BMC Health Serv Res. 2022. PMID: 36088321 Free PMC article.
- The association between social capital indicators and psychological distress in Catalan adolescents. Carrillo-Alvarez E, Andrés A, Riera-Romaní J, Novak D, Rodriguez-Monforte M, Costa-Tutusaus L, Guerra-Balic M. Carrillo-Alvarez E, et al. Front Psychol. 2022 Aug 17;13:964689. doi: 10.3389/fpsyg.2022.964689. eCollection 2022. Front Psychol. 2022. PMID: 36059788 Free PMC article.
- Exploring the Social Networks of Women Bereaved by Stillbirth: A Descriptive Qualitative Study. Popoola T, Skinner J, Woods M. Popoola T, et al. J Pers Med. 2021 Oct 21;11(11):1056. doi: 10.3390/jpm11111056. J Pers Med. 2021. PMID: 34834407 Free PMC article.
- Socio-demographic, behavioural and psycho-social factors associated with depression in two Russian cities. Cook S, Saburova L, Bobrova N, Avdeeva E, Malyutina S, Kudryavtsev AV, Leon DA. Cook S, et al. J Affect Disord. 2021 Jul 1;290:202-210. doi: 10.1016/j.jad.2021.04.093. Epub 2021 May 4. J Affect Disord. 2021. PMID: 34004402 Free PMC article.
- Associations of Social Capital with Mental Disorder Prevalence, Severity, and Comorbidity among U.S. Adolescents. Hirota T, Paksarian D, He JP, Inoue S, Stapp EK, Van Meter A, Merikangas KR. Hirota T, et al. J Clin Child Adolesc Psychol. 2022 Nov-Dec;51(6):970-981. doi: 10.1080/15374416.2021.1875326. Epub 2021 Mar 3. J Clin Child Adolesc Psychol. 2022. PMID: 33656940 Free PMC article.
- WHO. Website of WHO. http://www.who.int/topics/depression/en/ . Accessed 17 Jul 2016.
- WHO . The global burden of disease: 2004 update. Geneva: W.H.O; 2008.
- Hopcroft RL, Bradley DB. The sex difference in depression across 29 countries. Soc Forces. 2007;85:1483–507. doi: 10.1353/sof.2007.0071. - DOI
- Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med. 2010;71:305–13. doi: 10.1016/j.socscimed.2010.03.035. - DOI - PubMed
- Zhan W, Shaboltas AV, Skochilov RV, Kozlov AP, Krasnoselskikh TV, Abdala N. Depressive symptoms and unprotected sex in St. Petersburg, Russia. J Psychosom Res. 2012;72:371–5. doi: 10.1016/j.jpsychores.2012.01.015. - DOI - PMC - PubMed
- Search in MeSH
LinkOut - more resources
Full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
Other Literature Sources
- scite Smart Citations
- Genetic Alliance
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Children and Mental Health: Is This Just a Stage?

- Download PDF
- Order a free hardcopy
All children are sad, anxious, irritable, or aggressive at times, and many find it occasionally challenging to sit still, pay attention, or interact with others. In most cases, these are just typical developmental phases. However, such behaviors may also indicate a more serious problem in some children.
What mental disorders can affect children?
Many mental disorders can begin in childhood. Examples include anxiety disorders, attention-deficit/hyperactivity disorder (ADHD), depression and other mood disorders, eating disorders, and post-traumatic stress disorder (PTSD). Early treatment can help children manage their symptoms and support their social and emotional well-being. Many adults reflect on how mental disorders affected their childhood and wish they had received help sooner.
What are the signs of mental health conditions in children?
Distinguishing between challenging behaviors and emotions that are a part of normal development and those that may be cause for concern can be hard. Consider seeking help if your child’s behavior or emotions last for weeks or longer, cause distress for your child or your family, or interfere with your child’s functioning at school, at home, or with friends. If your child’s behavior is unsafe, or if your child talks about wanting to hurt themselves or someone else, seek help immediately . Learn more about warning signs .
When might children benefit from an evaluation?
|
|
Get Immediate Help
If you, your child, or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911 .
Where should I start if I’m concerned about my child’s mental health?
Being proactive and aware of your child’s mental health is an important first step. If you have concerns about your child’s mental health, start by talking with others who frequently interact with your child. For example, ask their teacher about your child’s behavior in school, at daycare, or on the playground.
You can talk with your child’s pediatrician or health care provider and describe your child's behavior and what you have observed and learned from talking with others. You can also ask the health care provider for a referral to a mental health professional with experience and expertise in evaluating and treating children. Learn about ways to get help and how to find a health care provider or access treatment.
How is children’s mental health assessed?
An evaluation by a mental health professional can help understand and clarify your child's emotions, behavior, and current situation. Based on this information, the mental health professional can decide if your child would benefit from an intervention and what intervention might work best.
A comprehensive evaluation of a child’s mental health usually involves:
- A parent interview to discuss the child’s developmental history, temperament, relationships with friends and family, medical history, interests, abilities, and any prior treatment
- Information gathering from the child’s school, such as standardized test scores and reports on behavior, capabilities, and difficulties
- If needed, an interview with the child for testing and behavioral observations
Asking questions and providing information to your child’s health care provider can improve your child’s care. Talking with the health care provider builds trust and leads to better results, quality, safety, and satisfaction with care.
Here are some questions you can ask when meeting with prospective treatment providers.
- Do you use treatment approaches that are supported by research?
- Do you involve parents in the treatment? If so, how are parents involved?
- Will there be “homework” between sessions?
- How will progress be evaluated?
- How soon can we expect to see progress?
- How long should treatment last?
Find tips for talking with a health care provider to improve your child’s care and get the most out of your visit.
How are childhood mental health disorders treated?
The mental health professional will review the evaluation results to help determine if a child’s emotions and behavior are related to changes or stresses at home or school or if they may indicate a disorder for which they would recommend treatment.
There are several treatment options the mental health professional may recommend.
- Parent involvement in the treatment
- Teaching the child skills to practice at home or school (between-session “homework assignments”)
- Measures of progress (such as rating scales and improvements on “homework assignments”) that are tracked over time
- Medications , which will depend on the diagnosis and may include antidepressants, stimulants, mood stabilizers, or other medications. Medications are often used in combination with psychotherapy. If multiple health care providers or specialists are involved, treatment information should be shared and coordinated between providers to achieve the best results.
- Family counseling , which includes family members to help them understand how a child’s challenges may affect relationships with parents and siblings.
- Support for parents , such as individual or group sessions that include training and the opportunity to talk with other parents. Parental support can provide new strategies for helping a child manage difficult emotions and behavior in a positive way. The therapist can also coach parents on how to work with schools to receive classroom accommodations.
Learn more about treatment options for specific disorders.
How can the school support my child’s mental health?
Children who have behavioral or emotional challenges that interfere with success in school may benefit from plans or accommodations provided under laws that prevent discrimination against children with disabilities. Your child’s health care providers can help you communicate with the school.
A first step may be to ask the school whether accommodations such as an individualized education program (IEP) are appropriate for your child. Accommodations might include providing a child with a tape recorder for taking notes, allowing more time for tests, or adjusting seating in the classroom to reduce distraction.
The U.S. Department of Education offers information and resources on what schools can and, in some cases, must provide for children who would benefit from accommodations and how parents can request evaluation and services for their child.
- The Office for Civil Rights provides information on federal laws that prohibit discrimination based on disability in public programs, such as schools.
- The Center for Parent Information and Resources lists Parent Training and Information Centers and Community Parent Resource Centers in each state
Many organizations listed in the More information and resources section also offer information on working with schools and more general information on disorders affecting children.
More information and resources
Information on specific disorders is available on NIMH's Mental Health Information webpage .
The following organizations and agencies have information on symptoms, treatments, and support for childhood mental disorders. Some offer guidance for working with schools and finding mental health professionals. Participating in support groups can provide an avenue for connecting with other parents dealing with similar issues.
Note: This resource list is provided for informational purposes only. It is not comprehensive and does not constitute an endorsement by NIMH.
- American Academy of Child and Adolescent Psychiatry, Facts For Families Guide
- Anxiety and Depression Association of America
- Association for Behavioral and Cognitive Therapies
- Centers for Disease Control and Prevention, Children’s Mental Health
- Child Mind Institute
- Mental Health America
- National Alliance on Mental Illness
- National Federation of Families
- Society of Clinical Child and Adolescent Psychology, Effective Child Therapy
- StopBullying.gov
What research is being done on disorders affecting children?
NIMH conducts and supports research to help find new and improved ways to diagnose and treat mental disorders that occur in childhood. This research includes studies of risk factors—including genetics, experience, and the environment—which may provide clues to how these disorders develop and how to identify them early.
NIMH also supports efforts to develop and test new interventions, including behavioral, psychotherapeutic, and medication treatments, and ways to improve existing treatments and make them more available in communities, doctor's offices, and schools. Researchers are also exploring whether the benefits of treatment in childhood last into adolescence and adulthood.
What are clinical trials and why are they important?
Children are not little adults, yet they are often given medications and treatments that have been tested only in adults. Research shows that, compared to adults, children respond differently to medications and treatments, both physically and mentally. The way to get the best treatments for children is through research designed specifically for them.
Clinical trials are research studies that look at ways to prevent, detect, or treat diseases and conditions. These studies help show whether a treatment is safe and effective in people. Some people join clinical trials to help doctors and researchers learn more about a disease and improve health care. Other people, such as those with health conditions, join to try treatments that aren’t widely available.
NIMH supports clinical trials across the United States. Talk to a health care provider about clinical trials and whether one is right for your child. Learn more about participating in clinical trials .
For more information
Learn more about mental health disorders and topics . For information about various health topics, visit the National Library of Medicine’s MedlinePlus .
The information in this publication is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health NIH Publication No. 24-MH-8085 Revised 2024

IMAGES
VIDEO
COMMENTS
Grand Challenges Faculty Development Institute: Eradicate Social Isolation CSWE, Dallas, TX, Oct. 19, 2017. 1. Case Studies. The following case studies were included to highlight different ways that social workers can assess and intervene with issues of social isolation. These cases are free to you to use, modify, and incorporate into your ...
2. Significant impairment in social, occupational, or other important areas of functioning. C. The stress-related disturbance does not meet the criteria for another mental disorder and is not merely an exacerbation of a preexisting mental disorder. D. The symptoms do not represent normal bereavement.
At Tracking Happiness, we're dedicated to helping others around the world overcome struggles of mental health. In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year. 25% of people don't feel comfortable sharing their struggles with anyone, not even their ...
Her more recent episodes related to her parents' marital problems and her academic/social difficulties at school. She was treated using cognitive-behavioral therapy (CBT). Chafey, M.I.J., Bernal, G., & Rossello, J. (2009). Clinical Case Study: CBT for Depression in A Puerto Rican Adolescent. Challenges and Variability in Treatment Response.
Summary. Download the whole case study as a PDF file. Josef is 16 and lives with his mother, Dorota, who was diagnosed with Bipolar disorder seven years ago. Josef was born in England. His parents are Polish and his father sees him infrequently. This case study looks at the impact of caring for someone with a mental health problem and of being ...
3: 978--13-517190-5PrefaceMental Health in Social Work: A Casebook on Diagnosis and Strengths-Based Assessment is a graduate level textbook that will help students and professionals learn to understand clients holistically as they proceed with the assessm. nt and intervention process. A major purpose of Mental Health in Social Work is to ...
The role of social workers in community mental health is embedded in the broader relationship of people to social institutions. Social work's concern with the quality of life is sanctioned by the social system and involves, of necessity, some commitment to the institutions that organize and govern secular life.
The social workers at the health centers were contacted by a mental health social worker and a case manager nurse working at an urban health center. Both professionals were responsible for providing the health and social care workers with information about the study. ... Ellem K.A., Wilson J. Life story work and social work practice: A case ...
her professionals have encountered around engagement. There were still concerns and risk but hol. ing and working with risk is fundamental to this role.A day in the life of a mental health social worker involves being aware of statutory action that can be taken but also, the need to develop and maintain trusting working relationships so that ...
This case study portrays issues raised by social work students following a workshop with MHWLE as part of their graduate-level training. A workshop with MHWLE was designed for 24 social work graduate students during a mental health seminar. Following the workshop, a focus group was held.
Mental health and work injuries. ... involving a worldwide sample of more than 1.4 million participants across 147 studies conducted ... psychological and social health through prevention rather ...
Working in multidisciplinary community mental health teams: The impact on social workers and health professionals of integrated mental health care. British Journal of Social Work , 33, 1081-1103. Crossref
The scope begins with the notion that social support plays a substantial role in attaining and maintaining good mental health, in the prevention of and recovery from mental health problems (Topor et al. 2011; UN 2020; Wang et al. 2018) and have a potential in reducing inequalities in health (Stoltenberg 2015 ).
In a study of 151 community mental health workers in Northern California, Webster and Hackett ... (e.g, psychosocial rehabilitation workers or staff of an intensive case management team; see studies in (Leiter & Harvie, 1996; ... burnout and somatic symptoms among social workers. Community Mental Health Journal. 2010; 46 (6):591-600.
Social work report: Background. Mrs Beryl Brown (01/11/33) is an 85 year old woman who was admitted to the Hume Hospital by ambulance after being found by her youngest daughter lying in front of her toilet. Her daughter estimates that she may have been on the ground overnight. On admission, Mrs Brown was diagnosed with a right sided stroke ...
Summary. In 2019, employers were just starting to grasp the prevalence of mental health challenges at work, the need to address stigma, and the emerging link to diversity, equity, and inclusion (DEI).
Lyndsey case study: Self-harm; sexual assault. Nicki and Gina case study: Poor interview / listening skills. Mr Singh case study: Poor listening skills. Ronnie case study: Social isolation, psychosis, suicide risk. Steve case study: Psychosis, drug and alcohol use. Sue case study: Confidentiality. Holly and Chris case study: Confidentiality and ...
Will and Nikki have lived experience of mental health problems. In this video, they talk about when the influence and participation process wasn't too successful. Overcoming challenges 2. In this film, Sarah-Jane and Charlotte from Mind discuss some of the problems and challenges of lived experience work.
Have at least 2 years' full-time equivalent (FTE) post-qualifying social work experience* in a mental health setting within the last 5 years, totalling a minimum of 3,360 hours. The AASW recognises that full-time employment equates to 35 hours per week, for 48 weeks per year. Must be able to articulate your understanding and provide a case ...
Formats. Mental health with adults: On-campus, Intensive Weekend, Online; Mental health with children and adolescents: On-campus; Due to an increased awareness of compelling public health challenges, clinical social workers and therapists have moved to the forefront of identifying and advancing solutions to some of society's most formidable public health challenges, including violence ...
Social anxiety disorder is a common type of anxiety disorder. A person with social anxiety disorder feels symptoms of anxiety or fear in situations where they may be scrutinized, evaluated, or judged by others, such as speaking in public, meeting new people, dating, being on a job interview, answering a question in class, or having to talk to a cashier in a store.
The present case study discusses the burden and determination of a caregiver for an individual with schizophrenia over thirty years. It was a single-subject research design. ... (CHW) and the District Mental Health Program (DMHP) social worker. The researcher made a home visit along with the CHW and DMHP social worker. During the home visit, it ...
This mixed-methods study uses Maslow's hierarchy as a theoretical lens to investigate the experiences of 63 newly enrolled clients of housing first and traditional programs for adults with serious mental illness who have experienced homelessness. Quantitative findings suggests that identifying self-actualization goals is associated with not having one's basic needs met rather than from the ...
focuses specifically on Massachusetts and evaluates the nature of this interrelationship.2 The. study found that "7.26% of the male inmate population identified as having serious mental. illness [and] 24% of men in prison have open mental health cases."3 The statistics are even.
To bridge this gap, this scoping review will synthesise and map the current literature on social work leadership competencies in health and mental healthcare. Methods and analysis: Arksey and O'Malley's five-stage framework for scoping reviews will guide our search of six academic databases including: PsycINFO, OVID Social Work Abstracts, OVID ...
How to work on improving social health. To that end, much of Killam's book is devoted to helping individuals improve their social health. But first, she believes people should assess the current health of their relationships and networks—just like you might do an assessment of your physical health.
The aim of the current vignette study was to examine how social workers assess adolescents with substance misuse problems, criminal behaviour and mental health difficulties, and how they make decisions about treatment interventions to reduce these problems. Earlier research has shown lack of knowledge concerning factors and processes that ...
A case study of the community mental health work force in Nebraska over a seven-year period beginning in 1981 examined changes in the professional makeup, overall staffing levels, extent of professional training, and number of medical staff in both metropolitan and nonmetropolitan agencies. The stud …
Social capital can be a mixed blessing for women. Different forms of social relations can lead to different health outcomes, both positive and negative. Although the family is important for women's mental health in Moscow, extra-familial relations across age groups can be mentally distressing. This …
This fact sheet presents information on children's mental health including assessing your child's behavior, when to seek help, first steps for parents, treatment options, and factors to consider when choosing a mental health professional. It also provides guidance on how to work with your child's school, a list of resources, and information about clinical trials.