Case Study of a 44-Year-Old Patient with a Moderate Recurrent Depressive Disorder (ICD-10 F 33.1) from Psychodynamic Point of View
- First Online: 04 May 2021

Cite this chapter

- Christos Charis 3
1013 Accesses
Mrs. X is a 44-year-old divorced mother of one (daughter) who presented with a major depression of moderate intensity which was already chronic as she came to me for therapy (09/17). The onset of the depression was present when Mrs. X was 34 years old. She decided to rent a flat with her boyfriend who she loved. She developed severe panic attacks at that moment and became very depressed. Again, Mrs. X became severely depressed at the age of 41. The patient had a course of electroconvulsive therapy (ECT, 22 electroshocks) and after that behaviour therapy for 1 year. All those treatments helped her to feel better, but she felt exhausted every day and had a low mood. The psychodynamic analysis showed two conflicts, a narcissistic conflict and an autonomous-dependent conflict, as they are defined in the Operationalized Psychodynamic Diagnosis-2 (OPD-2). These conflicts are due to the treatment of Mrs. X by her parents and because of her disappointing experiences when she had to escape from her own country when she was 13 years old. She had to act against her own will. We can analyse the psychodynamics of Mrs. X with regard to the concept of Sidney Blatt, a psychoanalyst (Blatt and Blass, Development and vulnerabilities on close relationships, 1996; Blatt et al., Psyche, 59(9–10), 864–891, 2005). Blatt investigated areas that concern the everyday experiences of depressive people. The first core theme is “loneliness, weakness, helplessness and abandonment. Desires to be cared for, loved and protected”. This factor was called “dependency” or “anaclitic”. The second factor is preoccupation with self-definitional areas (“introjective”: harsh self-criticism; perfectionism). Introjective depression is characterized by a tendency towards self-criticism and self-evaluation. Our patient did not learn to trust other people because of her very disappointing experiences with her parents. This led to a very weak self-consciousness and an excessively perfectionistic ego ideal. These traits have played an important role for the onset of chronic depression of Mrs. X. The depressive symptoms of Mrs. X have been relieved even more in a psychodynamic treatment which is ongoing. (Until July 2020, 90 sessions have taken place.) She has succeeded in partially reducing her demands on herself.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Arbeitskreis, O. P. D. (2006). Operationalisierte Psychodynamische Diagnostik OPD-2. Das Manual für Diagnostik und Therapieplanung . Bern: Huber.
Google Scholar
Arieti, S., & Bemporad, J. R. (1980). The psychological organization of depression. The American Journal of Psychiatry, 137 (11), 1360–1365.
Beck, A. T. (1983). Cognitive therapy of depression. New perspectives. In P. J. Clayton & J. M. Barrett (Eds.), Treatment of depression: Old controversies and new approaches (pp. 265–290). New York, NY: Raven.
Beutel, M. E., Wiltink, J., Hafner, C., Reiner, I., Bleichner, F., & Blatt, S. (2004). Abhängigkeit und Selbstkritik als psychologische Dimensionen der Depression-Validierung der deutschsprachigen Version des Depressive Experience Questionnaire (DEQ). Zeitschrift für Klinische Psychologie, Psychiatrie und Psychotherapie, 1 , 1–14.
Bibring, E. (1952). Das problem der depression. Psyche, 6 (2), 81–101.
Blatt, S. J. (1998). Contributions of psychoanalysis to the understanding and treatment of depression. Journal of the American Psychoanalytic Association, 46 (3), 723–752.
Blatt, S. J. (2004). Experiences of depression: Theoretical clinical and research perspectives . Washington, DC: American Psychological Association.
Blatt, S. J. (2005). A dialectic model of personality development and psychopathology: Recent contributions to understanding and treating depression. In J. Corveleyn, P. Luyten, & S. J. Blatt (Eds.), The theory and treatment of depression: Towards a dynamic interactionism model (pp. 137–162). Hillsdale, NJ: Lawrence Erlbaum Associates.
Blatt, S. J., & Blass, R. B. (1996). Relatedness and self-definition: A dialectic model of personality development. In G. G. Noam & K. W. Fischer (Eds.), Development and vulnerabilities on close relationships (pp. 309–338). Hillsdale, NJ: Lawrence Erlbaum Associates.
Blatt, S. J., D’Afflitti, J. P., & Quinlan, D. M. (1976). Experiences of depression in normal young adults. Journal of Abnormal Psychology, 85 (4), 383.
Blatt, S. J., Luyten, P., & Corveleyn, J. (2005). Zur Entwicklung eines dynamischen Interaktionsmodells der Depression und ihrer Behandlung. Psyche, 59 (9–10), 864–891.
Blatt, S. J., & Maroudas, C. (1992). Convergences among psychoanalytic and cognitive-behavioral theories of depression. Psychoanalytic Psychology, 9 (2), 157–190.
Cohen, M. B., Blake, C. M., Grace, B., Cohen, R. A., Fromm-Reichmann, F., & Weigert, E. V. (1954). An intensive study of twelve cases of manic-depressive psychosis. Psychiatry, 17 (2), 103–137.
Enns, M. W., Cox, B. J., & Clara, I. (2002). Adaptive and maladaptive perfectionism: Developmental origins and association with depression proneness. Personality and Individual Differences, 33 (6), 921–935.
Freud, S. (1916–1917). Trauer und Melacholie. Gesammelte Werke Band X . London: Imago Publishing Co., Ltd..
Luyten, P. (2002). Normbesef en depressie: Aanzet tot een integraitef theoratisch kader en een empirisch onderzoek aan de hand van de depressietheorie van S. J. Blatt . Unpublished doctoral dissertation, University Leuven, Belgium.
Reis, S., & Grenyer, B. F. (2002). Pathways to anaclitic and introjective depression. Psychology and Psychotherapy: Theory, Research and Practice, 75 (4), 445–459.
Shahar, G., & Mayes, L. C. (2017). Sidney Blatt’s psychoanalytic legacy: An introduction. Journal of the American Psychoanalytic Association, 65 (3), 453–456.
Download references
Author information
Authors and affiliations.
Private Practice, Dillenburg, Germany
Christos Charis
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Department of Psychology and Center of Applied Neuroscience, University of Cyprus, Nicosia, Cyprus
Georgia Panayiotou
Rights and permissions
Reprints and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Charis, C. (2021). Case Study of a 44-Year-Old Patient with a Moderate Recurrent Depressive Disorder (ICD-10 F 33.1) from Psychodynamic Point of View. In: Charis, C., Panayiotou, G. (eds) Depression Conceptualization and Treatment. Springer, Cham. https://doi.org/10.1007/978-3-030-68932-2_6
Download citation
DOI : https://doi.org/10.1007/978-3-030-68932-2_6
Published : 04 May 2021
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-68931-5
Online ISBN : 978-3-030-68932-2
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Case Report
- Open access
- Published: 21 December 2012
A case of cola dependency in a woman with recurrent depression
- Charles Boy Kromann 1 &
- Connie Thuroee Nielsen 1
BMC Research Notes volume 5 , Article number: 692 ( 2012 ) Cite this article
8307 Accesses
8 Citations
62 Altmetric
Metrics details
Cola is an extremely popular caffeinated soft drink. The media have recently cited a poll in which 16% of the respondents considered themselves to be addicted to cola soft drinks. We find the contrast between the apparent prevalence of cola addiction and the lack of scientific literature on the subject remarkable. To our knowledge, this is the first case of cola dependency described in the scientific literature.
Case presentation
The patient is a 40-year-old woman, who when feeling down used cola to give her an energy boost and feel better about herself. During the past seven years her symptoms increased, and she was prescribed antidepressant medication by her family doctor. Due to worsening of symptoms she was hospitalised and later referred to a specialised outpatient clinic for affective disorders. At entry to the clinic she suffered from constant tiredness, lack of energy, failing concentration, problems falling asleep as well as interrupted sleep. She drank about three litres of cola daily, and she had developed a metabolic syndrome.
The patient fulfilled the ICD-10 criteria for dependency, and on the Yale Food Addiction Scale (YFAS) she scored 40 points. Her clinical mental status was at baseline assessed by the Major Depression Inventory (MDI) = 41, Hamilton Depression - 17 item Scale (HAMD-17) = 14, Young Mania Rating Scale (YMRS) = 2 and the Global Assessment of Functioning (GAF) Scale = 45.
During cognitive therapy sessions she was guided to stop drinking cola and was able to moderate her use to an average daily consumption of 200 ml of cola. Her concentration improved and she felt mentally and physically better. At discharge one year after entry her YFAS was zero. She was mentally stable (MDI =1, HAMD-17 = 0, YMRS = 0 and GAF = 85) and without antidepressant medication. She had lost 7.2 kg, her waistline was reduced by 13 cm and the metabolic syndrome disappeared.
This case serves as an example of how the overconsumption of a caffeinated soft drink likely was causing or accentuating the patient’s symptoms of mental disorder. When diagnosing and treating depression, health professionals should pay attention to potential overuse of cola or other caffeinated beverages.
The mental disorder recurrent depression or depressive episode is in ICD-10 [ 1 ] characterised by the following core symptoms: depressed mood, lack of energy and decreased interest. Accompanying symptoms include decreased appetite, problems with concentration and sleep disturbance [ 1 ]. Untreated, the condition will often result in improper diurnal rhythm, disturbances in eating habits and for some increased use of tobacco [ 2 ], alcohol or other stimulants [ 3 ], e.g. caffeine. This self-medicating behaviour can be seen as both comfort-seeking and as a compensation for lack of energy [ 4 ].
Cola is an extremely popular caffeinated soft drink. Some brands have secret recipes. The most popular brand has a declared sugar content of 106 g/L [ 5 ] and a caffeine concentration of about 100 mg/L [ 6 ]. Lately, the media have presented articles about cola-addicts, and recently one Danish radio station cited a poll in which 16% of 1006 respondents considered themselves to be addicted to cola [ 7 ]. A search on the internet revealed that there was a surprisingly large number of private practice rehab therapists offering their services to cola addicts [ 8 ].
Psychiatric patients often have addictive behaviours, and a study by O’Farrell states that 90% of all hospitalised psychiatric patients show signs of addictive behaviour [ 9 ]. The scientific literature on addictive behaviour related to intake of cola is to our knowledge non-existing. Various searches in the scientific literature as well as more general open literature using PubMed, Google Scholar on “cola” and “dependency” or “addiction” yield no papers on addiction to cola, although some papers on addiction to caffeine mention cola as a caffeine source. Caffeine itself is a well-described substance of abuse and ICD-10 contains definitions for both dependence and withdrawal symptoms [ 1 , 10 ].
It is good clinical practice to consider abuse of alcohol and drugs when treating psychiatric patients, but patients are rarely asked about consumption of soft drinks containing caffeine.
We find the contrast between the belief that cola addiction exists and the apparent lack of scientific literature on the subject interesting and present the case of a 40-year-old woman with recurrent depression, who considered herself addicted to cola and whose daily consumption of cola increased during depressive episodes. To the best of our knowledge, this is the first case of cola dependency described in the scientific literature.
The patient is a 40-year-old woman, who never drank coffee, rarely drank alcohol, but smoked 20 cigarettes per day. She worked as a waitress from the age of 21 years and had unlimited access to cola. During long work shifts she frequently used cola to boost her energy. When she later became a mother, she, as a role model, tried to cut down on cola consumption. However, when she felt down she often used cola to give her an energy boost and thus feel better about herself. Apart from her self-reported addiction to cola and cigarettes she had never used or been addicted to other substances.
The patient had been taking antidepressant medication for seven years. Her family doctor had treated her the first two years with citalopram and with duloxetine, 120 mg, for the last five years. Due to worsening of symptoms (suicidal intentions, lack of energy and sleep disturbances) she was hospitalised for four weeks. She was subsequently discharged with the antidepressant duloxetine, 120 mg, and additional medication (quetiapine, 75 mg and zopiclone, 10 mg) and referred to a specialised outpatient clinic for affective disorders. On admission she still suffered from constant tiredness, lack of energy and failing concentration, and could hardly get her children to school. She had also had a constant feeling of restlessness and difficulties falling asleep, as well as interrupted sleep. Asked about eating habits, she revealed that she drank about three litres of a specific cola brand daily. She had over the years tried other cola brands, but these brands could not give her the same kick of energy feeling. She explained that after a cola intake her tiredness would shortly disappear. Her craving for cola was so pronounced that she fulfilled the ICD-10 criteria for dependency [ 1 ], and on the Danish translation of the Yale Food Addiction-scale (YFAS) [ 11 ] she scored 40 points.
Her clinical mental status was at baseline assessed by the Major Depression Inventory (MDI) =41, Hamilton Depression - 17 item Scale (HAMD-17) =14, Young Mania Rating Scale (YRMS) =2, Global assessment of functioning (GAF) =45 and the physical status by waist circumference =101 cm, weight= 72.9 kg, blood pressure=108/75 mmHg. Laboratory test: Fasting blood glucose: 5.9 mmol/l, HDL: 1.17 mmol/l, triglycerides: 0.75 mmol/l. She fulfilled the criteria for metabolic syndrome according to the International Federation of Diabetes (IDF) [ 12 ].
She was offered cognitive therapy according to the guidelines for recurrent depression. The lack of energy and the feeling of guilt in relation to her parenthood were some of the themes in her case formulation. During sessions she was informed that her excessive consumption of cola could “negatively affect her brain”. She decided to stop drinking cola completely. However, shortly after, she was obsessing over cola and had craving for the soft drink. She was then guided to reduce the consumption and dilute the cola with ice cubes. The following six months she was able to reduce her use to an average daily consumption of 200 ml of cola. During these six months her concentration skills improved, and she felt mentally as well as physically better, so in collaboration with her psychiatrist at the clinic she decided to reduce her psychopharmacological medication.
Treatment outcome
At discharge from the outpatient clinic a year after entry she still had an average daily intake of 200 ml cola but her YFAS-score was now zero. She was not taking any medication and she was mentally stable and assessed by MDI=1, HAM-17=0, YMRS=0, GCI=2 and GAF=85. Due to the reduced consumption of soft drinks she lost weight to 65.7 kg, her waist circumference was reduced to 88 cm, and her blood pressure was approximately the same, 109/77 mmHg. Laboratory test: Fasting blood glucose was reduced to 4.3 mmol/l, HDL: 1.13 mmol/l, triglycerides: 0.78 mmol/l, and she no longer fulfilled the criteria for metabolic syndrome according to IDF.
We have presented a case of cola dependency in a woman with recurrent depression. As part of the treatment for her mental disorder her cola dependency was addressed and treated, with good effect on both her mental and physical health. The fact that her dependence on cola existed ahead of her recurrent depression, and that she could not reduce her consumption of cola by herself, is not sufficient to conclude that her dependence on cola was the primary cause of her recurrent depressions. It is, however, remarkable that both her dependence on cola and her depressive symptoms were reduced simultaneously, when she was treated with a recommended therapeutic method.
Caffeine is the world’s most widely consumed psychoactive substance and has associated psychiatric syndromes such as caffeine-induced sleep disorder, caffeine-induced anxiety disorder and caffeine dependency with withdrawal symptoms that are all well described and documented in the literature [ 13 ].
A daily caffeine intake as low as 100 mg caffeine (1 cup of coffee or one litre of cola may result in caffeine dependency and subsequently withdrawal symptoms such as headaches, drowsiness, dysphoric mood, depression and concentration difficulties [ 13 ].
It is straightforward to consider the patients symptoms solely to be related to caffeine dependency, but several aspects of the case point to a concept of cola dependency separate from the previously described caffeine dependency.
The patient had a distinct preference for a specific band of cola. Although she repeatedly tried, she could not find a satisfactory replacement for her preferred drink, not even among other caffeinated cola-flavoured soft drinks. Caffeine dependency is shown to be associated with taste preferences in the withdrawal phase, but only in acute caffeine abstinence [ 14 ]. The patient slowly reduced her consumption to 200 ml of cola equivalent to 25 mg of caffeine, but was unable to substitute the cola or stop the use completely.
It is very plausible that there is a synergistic effect of caffeine and sugar in drinks, as most energy drinks boast this combination. This effect could add to the addictiveness of cola as sugar is also attributed an addictive potential [ 15 ].
The most interesting aspect of the argumentation for the concept of a separate cola addiction is the common belief in cola dependency among lay people. More than every seventh person in Denmark consider themselves addicted to cola [ 7 ], some to such an extent that they are willing to pay for treatment in order to reduce their consumption.
Whilst the aforementioned poll with self-evaluated dependency is statistically sound, it is probably not scientifically valid. However, the large number of people who consider themselves addicted is still a relevant indication that a potential problem exists.
Cola and other caffeinated soft drinks are not associated with immediate health-threatening effects. They may, however, be related to prolonged and extensive consumption, mainly due to the high sugar content and thus the risk of obesity-related diseases. With regard to dependence on cola there is a discrepancy between the public perception and the official perception among health professionals. This may result in patients having problems with addiction to cola not getting attention in relation to their symptoms, or proper preventive or therapeutic treatment in relation to reduction of their consumption. Individual counseling on this matter could therefore be lacking. This lost opportunity for individual counseling could have negative consequences for patients, who are not reachable through health campaigns.
A case report is no proof of the existence of a specific cola addiction, and more research must be carried out in this field, in order to shed light on the apparent discrepancy between popular belief and the official more reluctant perception among health professionals. Studies examining the potential soft drink addiction are needed.
This case also serves as an example, where the overconsumption of a caffeinated soft drink most probably caused or accentuated the patient’s symptoms of mental disorder. When diagnosing and treating depression, health professionals should pay attention to potential overuse of cola or other caffeinated beverages.
Written and informed consent from the patient was obtained for the publication of this case report.
World Health Organization: The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. 1993, Geneva: World Health Organization
Google Scholar
Mendelsohn C: Smoking and depression–a review. Aust Fam Physician. 2012, 41: 304-307.
PubMed Google Scholar
Boden JM, Fergusson DM: Alcohol and depression. Addiction. 2011, 106: 906-914. 10.1111/j.1360-0443.2010.03351.x.
Article PubMed Google Scholar
Parylak SL, Koob GF, Zorrilla EP: The dark side of food addiction. Physiol Behav. 2011, 104: 149-156. 10.1016/j.physbeh.2011.04.063.
Article PubMed CAS PubMed Central Google Scholar
Coca-Cola® - Coca-Cola®. http://www.coca-cola.dk/nordic-corp/da_DK/pages/products/cocacola.html?cat=cc ,
Barone JJ, Roberts HR: Caffeine consumption. Food Chem Toxicol. 1996, 34: 119-129. 10.1016/0278-6915(95)00093-3.
Article PubMed CAS Google Scholar
[Every seventh person in Denmark is addicted to cola] In Danish. Hver syvende dansker afhængig af cola - dr.dk/P3/P3Nyheder. http://www.dr.dk/P3/P3Nyheder/2009/01/06/112539.htm ,
[Cola addicts want to be cured with hypnosis] In Danish. Colanarkomaner vil afvænnes med hypnose - dr.dk/Nyheder/Indland. http://www.dr.dk/Nyheder/Indland/2010/02/21/231153.htm ,
O'Farrell TJ, Connors GJ, Upper D: Addictive behaviors among hospitalized psychiatric patients. Addict Behav. 1983, 8: 329-333. 10.1016/0306-4603(83)90032-1.
Juliano LM, Griffiths RR: A critical review of caffeine withdrawal: empirical validation of symptoms and signs, incidence, severity, and associated features. Psychopharmacology. 2004, 176: 1-29. 10.1007/s00213-004-2000-x.
Gearhardt AN, Corbin WR, Brownell KD: Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009, 52: 430-436. 10.1016/j.appet.2008.12.003.
Alberti KGMM, Zimmet P, Shaw J: Metabolic syndrome-a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006, 23: 469-480.
Griffiths RR, Reissig CJ: Substance Abuse: Caffeine Use Disorders. Psychiatry. Edited by: Tasman A, Kay J, Lieberman JA, First MB, Maj M. 2008, Chichester: John Wiley & Sons, Ltd, 1019-1040. 3
Chapter Google Scholar
Tinley EM, Yeomans MR, Durlach PJ: Caffeine reinforces flavour preference in caffeine-dependent, but not long-term withdrawn, caffeine consumers. Psychopharmacology. 2003, 166: 416-423.
PubMed CAS Google Scholar
Avena NM, Rada P, Hoebel BG: Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008, 32: 20-39. 10.1016/j.neubiorev.2007.04.019.
Download references
Acknowledgements
We would like to thank Nurse Mona Tranberg Henningsen for her great work with data collection.
Author information
Authors and affiliations.
Mental Health Services, Region of Southern Denmark, Esbjerg- Ribe, Gl. Vardevej 101, DK-6715, Esbjerg N, Denmark
Charles Boy Kromann & Connie Thuroee Nielsen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Connie Thuroee Nielsen .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
CBK conducted the literature review and was a major contributor in the writing of the manuscript. CTN supervised data collection and was a major contributor in the writing of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Kromann, C.B., Nielsen, C.T. A case of cola dependency in a woman with recurrent depression. BMC Res Notes 5 , 692 (2012). https://doi.org/10.1186/1756-0500-5-692
Download citation
Received : 20 September 2012
Accepted : 19 December 2012
Published : 21 December 2012
DOI : https://doi.org/10.1186/1756-0500-5-692
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cola caffeinated soft drink
- Metabolic syndrome
BMC Research Notes
ISSN: 1756-0500
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Recurrent Brief Mixed Depression
This case study of a 21-year-old woman-referred by a relative because of long-standing severe interpersonal, academic, and occupational impairment-illustrates the importance of screening patients with brief episodes of depression for mixed features.
Jane, who is 21 years old, was referred by her mother because of long-standing severe interpersonal, academic, and occupational impairment. She was euthymic on the day she presented.
Jane had a history of unstable relationships and impulsive, self-destructive behavior. She failed to achieve educational objectives and to maintain stable employment. From early adolescence, she was defiant. When she was 15 years old, her parents became so frustrated with her that they sent her to a residential treatment facility for troubled girls.
In the years before presentation, she abused alcohol and experimented with a number of substances, but had not done so for more than a year before the evaluation. She had 3 first-degree relatives, none of whom were known to have a mood disorder.
Jane had been assessed by mental health professionals, including psychiatrists, over the years. Information about previously rendered diagnoses was not available. She had received psychotherapy but not a somatic treatment.
When interviewed, Jane was asked whether she had ever had episodes of depressed, irritable, or elevated mood, or some combination of these, lasting a week or longer. She did not recall this being the case. She was then asked whether she had ever had 2- to 3-day episodes characterized by some combination of these mood states. She said she had brief episodes of affective disturbance since early adolescence. These episodes occurred every 1 to 2 weeks, lasted about 2 days, and were marked predominantly by depressed and irritable mood. On these days, Jane had particularly low self-esteem, slept about 3 hours more than usual, ate excessively, and had a low level of energy and psychomotor slowing in the morning and restlessness late in the day and at night.
During some of these brief periods of depression, there were times throughout the day when Jane had brief bursts of strangely elevated mood, had hypertalkativeness but not frank pressured speech, was distractible, and had racing and crowded thoughts. She had never had a hypomanic episode or psychotic features. Jane's presentation most closely conformed to the criteria for “recurrent brief depression,” as specified in Appendix B of DSM-IV-TR. She was viewed by her physician as having “recurrent mixed depression.”
Although Jane was euthymic, a decision was made to use a pharmacological intervention aimed at interrupting the cyclical process. She was treated with lamotrigine rather than lithium because of its tolerability. She was instructed to take morning doses as follows: 25 mg for 14 days, then 50 mg for 14 days, followed by 100 mg for 7 days, and then 200 mg thereafter. Jane tolerated the medication well. She had 1- or 2-day periods of mixed depression weekly through the fifth week of treatment. However, from that point onward, she was free of symptoms.
After 9 months of treatment, Jane stopped taking lamotrigine. She became very depressed on the second day. Her mother called Jane's psychiatrist asking for guidance; he recommended that Jane restart her medication, since she had missed only 2 doses. Within a day, she felt well and did not cycle into an episode until 6 months later, when she decided to stop taking the medication. Two days later, Jane was in crisis and her mother called the psychiatrist. He recommended she resume taking lamotrigine. The symptoms remitted within 1 to 2 days. The cyclical process did not recur during the following 2 months, at which point she was lost to follow-up.
Recurrent brief depression is defined as a phenomenon marked by the presence of impairing depressive episodes of at least 2 days’ duration that meet all criteria for MDD (except for the duration criterion) and that occur at least once a month for 12 consecutive months and are not associated with the menstrual cycle. 1-5
Recurrent brief depression was included in Appendix B of DSM-IV and is now included in the main body of DSM-5. Mixed depression was not included in DSM-IV, but it is part of the chapter on MDD in DSM-5.
Mixed depression was first described by Kraepelin, 6 but the concept was ignored until quite recently. 7 The diagnosis of mixed depression, as described in the literature in recent years, focuses on the admixture of subthreshold symptoms of hypomania in the context of DSM-IV–defined MDD. By this standard, Jane did not have mixed depression because she never had an episode lasting at least 2 weeks. However, she did meet the criteria for recurrent brief depression and had significant mixed features during these episodes.
Angst and colleagues 8,9 have proposed validated changes in the criteria for hypomania that apply to this case. Their data suggest that hypomania is reasonably defined without reference to duration and includes symptoms of overactivity, euphoria, or irritability along with any 3 DSM-IV–specified symptoms of hypomania that lead to subjective or social impairment. By this standard, Jane would be viewed as having recurrent brief mixed hypomania.
Jane was euthymic when she presented, yet a psychotropic was prescribed for the purpose of aborting a cyclical process. Lithium would have been a reasonable option. 10 One might have also used divalproex. However, owing to its tolerability, lamotrigine was selected. Jane did well but had symptom relapse within 2 days on both occasions she stopped the medication; with resumption of treatment, she had prolonged asymptomatic periods. This strongly suggests that lamotrigine was causal in interrupting the cyclical process.
This case illustrates the value of assessing patients with histories of stormy interpersonal relationships, impulsive behavior, and low social function for the presence of brief, episodic affective disturbance. It also illustrates the importance of screening patients with brief episodes of depression for mixed features. The use of an antidepressant in an effort to abort the cyclical process might have further destabilized mood and worsened the course of illness.
Disclosures:
Dr Dilsaver is former Professor of Psychiatry and Behavioral Health at the University of Texas, Houston. He is currently at the Imperial County Behavioral Health Services in El Centro, Calif. He is an author of more than 150 publications in the fields of child, adolescent, and adult psychiatry. His focus of attention is the phenomenology of affective illness. He reports no conflicts of interest concerning the subject matter of this case.
References:
1. Angst J, Merikangas K, Scheidegger P, Wicki W. Recurrent brief depression: a new subtype of affective disorder. J Affect Disord . 1990;19:87-98.
2. Angst J. The history of the concept of recurrent brief depression. Eur Arch Psychiatry Clin Neurosci . 1994;244:171-173.
3. Carta MG, Altamura AC, Hardoy MC, et al. Is recurrent brief depression an expression of mood spectrum disorders in young people? Results of a large community sample. Eur Arch Psychiatry Clin Neurosci. 2003;253:149-153.
4. Pezawas L, Wittchen HU, Pfister H, et al. Recurrent brief depressive disorder reinvestigated: a community sample of adolescents and young adults. Psychol Med . 2003;33: 407-418.
5. Lövdahl H, Andersson S, Hynnekleiv T, Malt UF. The phenomenology of recurrent brief depression with and without hypomanic features. J Affect Disord. 2009;112:151-164.
6. Kraepelin E. Manic-Depressive Insanity and Paranoia . Edinburgh: E &S Livingstone; 1921.
7. Benazzi F. Bipolar disorder-focus on bipolar II disorder and mixed depression. Lancet . 2007;369:935-945.
8. Angst J, Gamma A, Benazzi F, et al. Toward re-definition of subthreshold bipolarity: epidemiology and proposed criteria for bipolar-II, minor bipolar disorders and hypomania. J Affect Disord . 2003;73:133-146.
9. Angst J, Gamma A. A new bipolar spectrum concept: a brief review. Bipolar Disord. 2002;4(suppl 1):11-14. 10. Conominas A, Bonet P, Nieto E. Recurrent brief depression treated with lithium. Biol Psychiatry . 1998;44:927-929.

An Update on GLP-1 Receptor Agonists as Pharmacotherapies for AUD

Here's to a Psychedelic Revolution

Post Hoc Analysis Explores Risk-Benefit Profile of KarXT

Blue Light Blockers: A Behavior Therapy for Mania

Evaluating the Efficacy of Lumateperone for MDD and Bipolar Depression With Mixed Features

Nonpharmacological Interventions for MDD and Their Effects on Neuroplasticity
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Migraine in recurrent depression: case-control study
Affiliation.
- 1 McMaster University, Department of Psychiatry and Behavioural Neurosciences, Mood Disorders Program, Centre for Mountain Health Services, St Joseph's Healthcare, Hamilton, Ontario L8N 3K7, Canada. [email protected]
- PMID: 19336787
- DOI: 10.1192/bjp.bp.108.054049
Background: An association between depression and headache is well established, but the specificity to migraine is unclear.
Aims: To investigate the specificity of the association of depression and migraine.
Method: People with recurrent depression (n=1259) were compared with psychiatrically healthy controls (n=851) to investigate headache defined according to International Headache Society criteria in each group.
Results: All headache types were more prevalent in the case group than in the controls. However, the strongest association was between depression and migraine with aura (OR=5.6). Among participants with recurrent headaches, migraine with aura (but not other forms of headache) was highly significantly associated with depression.
Conclusions: The data suggest that not only is there a general relationship between headache and depression but also that among people with recurrent headache there is a specific association between depression and migraine with aura. The association is likely to be explained by overlapping aetiological risk factors.
Publication types
- Comparative Study
- Multicenter Study
- Research Support, Non-U.S. Gov't
- Aged, 80 and over
- Case-Control Studies
- Depressive Disorder / complications*
- Depressive Disorder / epidemiology
- Middle Aged
- Migraine Disorders / epidemiology
- Migraine Disorders / etiology*
- United Kingdom / epidemiology
- Young Adult
Grants and funding
- G0701003/MRC_/Medical Research Council/United Kingdom
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Leanne: A Case Study in Major Depressive Disorder, Recurrent

Related Papers
American Journal of Psychiatry
John Markowitz
The Journal of psychotherapy practice and research
Child and Adolescent Psychiatric Clinics of North America
Nick Midgley , Carol Hughes , M. Rustin
Brian Kiluk
The two major forms of treatment for drug abuse, psychosocial treatments and pharmacologic treatments, have a number of differences in terms of their mode of action, time to effect, target symptoms, durability, and applicability across drugs of abuse. While each has specific indications and strengths, no psychotherapy or pharmacotherapy is universally effective, and both forms of treatment have some limitations, particularly when used alone. Several recent examples of the benefits of combined treatments for drug abusers are reviewed. These suggest that for many substance use disorders, outcomes can be broadened, enhanced, and extended by combining our most effective forms of psychotherapy and pharmacotherapy.
Pijar Senjakala Marthesa
MUKIIBI Cabrine
Journal of affective disorders
H. Schauenburg , Falk Leichsenring
There is evidence that psychotherapy is helpful in depressive disorders, with no significant differences between psychotherapies. For psychodynamic therapy (PDT) various models prove to be efficacious. Thus, the evidence for PDT is "scattered" between different forms of PDT, also implying problems in training of psychotherapy and in transferring research to clinical practice. A unified protocol based on empirically-supported methods of PDT in depression may contribute to solve these problems Systematic search for randomized controlled trials fulfilling the following criteria: (a) individual psychodynamic therapy (PDT) of depressive disorders, (b) treatment manuals or manual-like guidelines, (c) PDT proved to be efficacious compared to control conditions, (d) reliable measures for diagnosis and outcome, and (f) adult patients. Fourteen RCTs fulfilled the inclusion criteria. By a systematic review of the applied methods of PDT seven treatment components were identified. A hi...
Lindsay Michele
This study tested the relationships between Young’s (1990, 2003) model of EarlyMaladaptive Schemas (EMSs), negative life events occurring over the past 4 months,depressive symptoms, and anxious symptoms. We also replicated a design testing the ability of EMSs, negative life events, and their interaction to predict depressive and anxious symptoms and extended the design to include specific categories of negative life events (interpersonal and achievement). Results of this study showed that EMSs are predictive of depressive and anxious symptoms, but that negative life events account for a greater prediction. The EMS model was just as highly associated with and predictive of anxious symptoms as it was with depressive symptoms. The study was the first to examine specific types of negative life events and their relationships with EMSs. EMSs may be more highly associated with negative achievement than with negative interpersonal events but the EMSs appear to be vulnerable to global life stress in general
Professional Psychology: Research and Practice
Ellen Poleshuck , Luis Rosario-mccabe
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Warning Signs and Symptoms
- Mental Health Conditions
- Common with Mental Illness
- Mental Health By the Numbers
- Individuals with Mental Illness
- Family Members and Caregivers
- Kids, Teens and Young Adults
- Maternal & New Parent Mental Health
- Veterans & Active Duty
- Identity and Cultural Dimensions
- Frontline Professionals
- Mental Health Education
- Support Groups
- NAMI HelpLine
- Publications & Reports
- Podcasts and Webinars
- Video Resource Library
- Justice Library
- Find Your Local NAMI
- Find a NAMIWalks
- Attend the NAMI National Convention
- Fundraise Your Way
- Create a Memorial Fundraiser
- Pledge to Be StigmaFree
- Awareness Events
- Share Your Story
- Partner with Us
- Advocate for Change
- Policy Priorities
- NAMI Advocacy Actions
- Policy Platform
- Crisis Intervention
- State Fact Sheets
- Public Policy Reports
- About Mental Illness
Depressive disorder, frequently referred to simply as depression, is more than just feeling sad or going through a rough patch. It’s a serious mental health condition that requires understanding and medical care. Left untreated, depression can be devastating for those who have it and their families. Fortunately, with early detection, diagnosis and a treatment plan consisting of medication, psychotherapy and healthy lifestyle choices, many people can and do get better.
Some will only experience one depressive episode in a lifetime, but for most, depressive disorder recurs. Without treatment, episodes may last a few months to several years.
About 21 million U.S. adults— 8.4% of the population—had at least one major depressive episode in 2020. People of all ages and all racial, ethnic and socioeconomic backgrounds experience depression, but it does affect some groups more than others.
Personal Perspectives On Major Depressive Disorder
In this 2-part podcast series, NAMI Chief Medical Officer Dr. Ken Duckworth guides discussions on major depressive disorder that offer insights from individuals, family members and mental health professionals. Read the transcript . Note: Content includes discussions on topics such as suicide attempts and may be triggering.
Depression can present different symptoms, depending on the person. But for most people, depressive disorder changes how they function day-to-day, and typically for more than two weeks. Common symptoms include:
- Changes in sleep
- Changes in appetite
- Lack of concentration
- Loss of energy
- Lack of interest in activities
- Hopelessness or guilty thoughts
- Changes in movement (less activity or agitation)
- Physical aches and pains
- Suicidal thoughts
Depression does not have a single cause. It can be triggered by a life crisis, physical illness or something else—but it can also occur spontaneously. Scientists believe several factors can contribute to depression:
- Trauma . When people experience trauma at an early age, it can cause long-term changes in how their brains respond to fear and stress. These changes may lead to depression.
- Genetics . Mood disorders, such as depression, tend to run in families.
- Life circumstances . Marital status, relationship changes, financial standing and where a person lives influence whether a person develops depression.
- Brain changes . Imaging studies have shown that the frontal lobe of the brain becomes less active when a person is depressed. Depression is also associated with changes in how the pituitary gland and hypothalamus respond to hormone stimulation.
- Other medical conditions . People who have a history of sleep disturbances, medical illness, chronic pain, anxiety and attention-deficit hyperactivity disorder (ADHD) are more likely to develop depression. Some medical syndromes (like hypothyroidism) can mimic depressive disorder. Some medications can also cause symptoms of depression.
- Drug and alcohol misuse . Adults with a substance use disorder are at significantly higher risk for experiencing a major depressive episode. Co-occurring disorders require coordinated treatment for both conditions, as alcohol can worsen depressive symptoms.
To be diagnosed with depressive disorder, a person must have experienced a depressive episode lasting longer than two weeks. The symptoms of a depressive episode include:
- Loss of interest or loss of pleasure in all activities
- Change in appetite or weight
- Sleep disturbances
- Feeling agitated or feeling slowed down
- Feelings of low self-worth, guilt or shortcomings
- Difficulty concentrating or making decisions
- Suicidal thoughts or intentions
Although depressive disorder can be a devastating illness, it often responds to treatment. The key is to get a specific evaluation and treatment plan. Safety planning is important for individuals who have suicidal thoughts. After an assessment rules out medical and other possible causes, a patient-centered treatment plans can include any or a combination of the following:
- Psychotherapy including cognitive behavioral therapy, family-focused therapy and interpersonal therapy.
- Medications including antidepressants, mood stabilizers and antipsychotic medications.
- Exercise can help with prevention and mild-to-moderate symptoms.
- Brain stimulation therapies can be tried if psychotherapy and/or medication are not effective. These include electroconvulsive therapy (ECT) for depressive disorder with psychosis or repetitive transcranial magnetic stimulation (rTMS) for severe depression.
- Light therapy , which uses a light box to expose a person to full spectrum light in an effort to regulate the hormone melatonin.
- Alternative approaches including acupuncture, meditation, faith and nutrition can be part of a comprehensive treatment plan.
Reviewed August 2017
Many treatment options are available for depression, but how well treatment works depends on the type of depression and its severity. For most people, psychotherapy and medications give better results together than either alone, but this is something to review with your mental health care provider.
Psychotherapy
Psychotherapy (or talk therapy) has an excellent track record of helping people with depressive disorder. While some psychotherapies have been researched more than others, many types can be helpful and effective. A good relationship with a therapist can help improve outcomes.
Many clinicians are trained in more than one kind of psychotherapy, so ask your clinician what kind of psychotherapy they practice and how it can help you. A few examples include:
- Cognitive behavioral therapy (CBT) has a strong research base to show it helps with symptoms of depression. This therapy helps assess and change negative thinking patterns associated with depression. The goal of this structured therapy is to recognize negative thoughts and to teach coping strategies. CBT is often time-limited and may be limited to 8–16 sessions in some instances.
- Interpersonal therapy (IPT) focuses on improving problems in personal relationships and other changes in life that may be contributing to depressive disorder. Therapists teach individuals to evaluate their interactions and to improve how they relate to others. IPT is often time-limited like CBT.
- Psychodynamic therapy is a therapeutic approach rooted in recognizing and understanding negative patterns of behavior and feelings that are rooted in past experiences and working to resolve them. Looking at a person’s unconscious processes is another component of this psychotherapy. It can be done in short-term or longer-term modes.
Psychoeducation And Support Groups
Psychoeducation involves teaching individuals about their illness, how to treat it and how to recognize signs of relapse. Family psychoeducation is also helpful for family members who want to understand what their loved one is experiencing.
Support groups, meanwhile, provide participants an opportunity to share experiences and coping strategies. Support groups may be for the person with the mental health condition, for family/friends or a combination of both. Mental health professionals lead some support groups, but groups can also be peer-led.
Explore NAMI’s nationwide offerings of free educational programs and support groups that provide outstanding education, skills training and support.
Medications
For some people, antidepressant medications may help reduce or control symptoms. Antidepressants often take 2-4 weeks to begin having an effect and up to 12 weeks to reach full effect. Most people will have to try various doses or medications to find what works for them. Here are some antidepressants commonly used to treat depression:
Selective serotonin reuptake inhibitors (SSRIs) act on serotonin, a brain chemical. They are the most common medications prescribed for depression.
- Fluoxetine (Prozac)
- Sertraline (Zoloft)
- Paroxetine (Paxil)
- Citalopram (Celexa)
- Escitalopram (Lexapro)
Serotonin and norepinephrine reuptake inhibitors (SNRIs) are the second most common antidepressants. These medications increase serotonin and norepinephrine.
- Venlafaxine (Effexor)
- Desvenlafazine (Pristiq)
- Duloxetine (Cymbalta)
Norepinephrine-dopamine reuptake inhibitors (NDRIs) increase dopamine and norepinephrine. Bupropion (Wellbutrin) is a popular NDRI medication, which causes fewer (and different) side effects than other antidepressants. For some people, bupropion causes anxiety symptoms, but for others it is an effective treatment for anxiety.
Mirtazapine (Remeron) targets specific serotonin and norepinephrine receptors in the brain, thus indirectly increasing the activity of several brain circuits. Mirtazapine is used less often than newer antidepressants (SSRIs, SNRIs and bupropion) because it is associated with more weight gain, sedation and sleepiness. However, it appears to be less likely to result in insomnia, sexual side effects and nausea than the SSRIs and SNRIs.
- Bupropion (Wellbutrin)
- Mirtazapine (Remeron)
Second-generation antipsychotics (SGAs) , or “atypical antipsychotics,” treat schizophrenia, acute mania, bipolar disorder and bipolar mania and other mental illnesses. SGAs can be used for treatment-resistant depression.
- Aripiprazole (Abilify)
- Quetiapine (Seroquel)
Tricyclic antidepressants (TCAs) are older medications, seldom used today as initial treatment for depression. They work similarly to SNRIs but have more side effects. They are sometimes used when other antidepressants have not worked. TCAs may also ease chronic pain.
- Amitriptyline (Elavil)
- Desipramine (Norpramin)
- Doxepin (Sinequan)
- Imipramine (Tofranil)
- Nortriptyline (Pamelor, Avantyl)
- Protriptyline (Vivactil)
Monoamine oxidase inhibitors (MAOIs) are less used today because newer, more effective medications with fewer side effects have been found. These medications can never be used in combination with SSRIs. MAOIs can sometimes be effective for people who do not respond to other medications.
- Phenelzine (Nardil)
- Isocarboxazid (Marplan)
- Tranylcypromine Sulfate (Parnate)
- Selegiline patch (Emsam)
Brain Stimulation Therapies
For some, brain stimulation therapies may be effective, typically after other treatments have not been effective.
- Electroconvulsive Therapy (ECT) involves transmitting short electrical impulses into the brain. ECT does cause some side effects, including memory loss. Individuals should understand the risks and benefits of this intervention before beginning a treatment trial.
- Repetitive Transcranial Magnetic Stimulation (rTMS) is a relatively new type of brain stimulation that uses a magnet instead of an electrical current to activate the brain. It is not effective as a maintenance treatment.
- Vagus Nerve Stimulation (VNS) has a complex history. For a fuller understanding of this treatment, read the NIMH summary of this and other brain stimulation interventions.
Complementary And Alternative Medicine (CAM)
Relying solely on CAM methods is not enough to treat depression, but they may be useful when combined with psychotherapy and medication. Discuss your ideas of CAM interventions with your health care professional to be sure they will not cause side effects or adverse reactions.
The National Center for Complementary and Integrative Health reviews research on complementary treatments. You can search for each intervention on their website .
- Exercise. Studies show that aerobic exercise can help treat mild depression because it increases endorphins and stimulates norepinephrine, which can improve a person’s mood.
- Folate . Some studies have shown that when people with depression lack folate (also called folic acid or vitamin B9), they may not be receiving the full benefit from any antidepressants they may be taking. Studies suggest that in some situations taking L-methylfolate (an active form of folate) can be an additional treatment with other psychiatric medications.
- St John’s Wort. This supplement has similar chemical properties to some SSRIs. Risks of combining St John’s Wort with SSRIs and other medications are well-known and substantial.
Experimental Treatments
These following treatments are not FDA-approved but are being researched:
- Ketamine. Ketamine, which may offer a new model in treating depression, may have potentially quick and short-term impact on depression and suicidal thoughts. Ketamine is an anesthetic with a street value (special K) that has not been studied for long-term use. It can make psychosis worse and is not an ideal choice for people with substance use disorders.
- Deep Brain Stimulation . This treatment has been used to treat Parkinson’s disease. See the NIMH page on brain stimulation for more information .
- I Think I Might Be Gay
Coping with depression isn’t easy, but if you, a family member or a friend is struggling, there is help. NAMI is there to provide support and resources for you and your family.
Helping Yourself
Leading a balanced lifestyle can help you manage symptoms of depression. Here are some suggestions from people who have lived experience with depression:
Learn all you can . Learn about the many treatment options available. Connect with other people experiencing depression in support groups or meetings. Attend local conferences and conventions. Build a personal library of useful websites and helpful books.
Recognize early symptoms . Identify possible warning signs and triggers that may aggravate your depression symptoms. With this knowledge, you can recognize an emerging episode and get the help you need as soon as possible. Don’t be afraid to ask your friends and family for help—they can help you monitor your symptoms and behavior.
Partner with your health care providers . Give your health care provider all the information he or she needs to help you recover—including any reactions to medications, your symptoms or any triggers you notice. Develop trust and communicate openly.
Know what to do in a crisis . Be familiar with your community’s crisis hotline or emergency walk-in center. Know how to contact them and keep the information handy.
Find emotional support from others who experience depression . Share your story , thoughts, fears and questions with other people who have the same condition. Connect through online message boards or peer-education programs like NAMI Peer-to-Peer or support groups like NAMI Connection .
Avoid drugs and alcohol . These substances can disturb emotional balance and interact with medications. You may think using alcohol or drugs will help you feel better, but using them can hinder your recovery or make symptoms worse.
Get physically healthy . Eat well and exercise. To relieve stress, try activities like meditation, yoga or Tai Chi.
Helping A Family Member Or Friend
When someone you love and care about experiences the symptoms of mental illness, you face unique challenges yourself, including complex family dynamics, social isolation and often unpredictable behavior. Getting support for yourself is essential for you to be able to be helpful for the person you care about.
Learn more about your loved one’s condition . Learning about the condition your loved one experiences will help you better understand and support them. Read personal accounts of lived experience, full of tips and advice on the NAMI Blog :
- Depression is an Illness, Not a Weakness
- Living with Depression: How to Keep Working
Recognize early symptoms . Depression often has warning signs, such as a low mood, feeling fatigued or having trouble sleeping. Discuss your friend or family member’s past episodes with them to help them improve their ability to recognize the signs early.
Communicate . Speak honestly and kindly . Don’t scold or blame people with depression or urge them to “try harder” to “just be happy.” Instead, make specific offers of help and follow through with those offers. Tell the person you care about them. Ask them how they feel and truly listen.
React calmly and rationally . Even if your family member or friend is in a crisis, it’s important to remain calm. Listen to their concerns and make them feel understood—then take the next step toward getting help.
Find emotional support from others . Share your thoughts, fears and questions with other people who have loved ones with similar conditions. Connect with others through online message boards or NAMI peer-education programs .

Know the warning signs of mental illness

Learn more about common mental health conditions
NAMI HelpLine is available M-F, 10 a.m. – 10 p.m. ET. Call 800-950-6264 , text “helpline” to 62640 , or chat online. In a crisis, call or text 988 (24/7).
- Case report
- Open access
- Published: 27 April 2017
A case of recurrent depressive disorder presenting with Alice in Wonderland syndrome: psychopathology and pre- and post-treatment FDG-PET findings
- Tatsushi Yokoyama 1 ,
- Tsuyoshi Okamura 1 ,
- Miwako Takahashi 2 ,
- Toshimitsu Momose 2 &
- Shinsuke Kondo 1
BMC Psychiatry volume 17 , Article number: 150 ( 2017 ) Cite this article
6606 Accesses
15 Citations
13 Altmetric
Metrics details
Alice in Wonderland syndrome (AIWS) is a rare neuropsychiatric syndrome that typically manifests in distortion of extrapersonal visual image, altered perception of one’s body image, and a disturbed sense of the passage of distance and time. Several conditions have been reported to contribute to AIWS, although its biological basis is still unknown. Here, we present the first case demonstrating a clear concurrence of recurrent depressive disorder and AIWS. The clinical manifestations and pre- and post-treatment fluorodeoxyglucose positron-emission tomographic (FDG-PET) images provide insights into the psychopathological and biological basis of AIWS.
Case presentation
We describe a 63-year-old Japanese male who developed two distinct episodes of major depression concurrent with AIWS. In addition to typical AIWS perceptual symptoms, he complained of losing the ability to intuitively grasp the seriousness of news and the value of money, which implies disturbance of high-order cognition related to estimating magnitude and worth. Both depression and AIWS remitted after treatment in each episode. Pre-treatment FDG-PET images showed significant hypometabolism in the frontal cortex and hypermetabolism in the occipital and parietal cortex. Post-treatment images showed improvement of these abnormalities.
Conclusions
The clinical co-occurrence of depressive episodes and presentation of AIWS can be interpreted to mean that they have certain functional disturbances in common. In view of incapacity, indifference, devitalization, altered perception of one’s body image, and disturbed sense of time and space, the features of AIWS analogous to those of psychotic depression imply a common psychopathological basis. These high-order brain dysfunctions are possibly associated with the metabolic abnormalities in visual and parietotemporal association cortices that we observed on the pre- and post-treatment FDG-PET images in this case, while the hypometabolism in the frontal cortex is probably associated with depressive symptoms.
Peer Review reports
Alice in Wonderland syndrome (AIWS) is a rare neuropsychiatric syndrome, which Todd [ 1 ] named after the character created by Lewis Carroll. Collective manifestations of AIWS include distortion of extrapersonal visual image (micropsia, macropsia, metamorphopsia, teleopsia, and pelopsia), altered perception of one’s body image, and a disturbed sense of the passage of distance and time [ 2 ].
Many conditions have been reported to contribute to AIWS, and Lanska et al. [ 2 ] indicates that viral infection and migraine are the two most commonly identified causes, occurring preferentially in young individuals. To the best of our knowledge, only two reports to date have associated AIWS with a depressive disorder [ 3 , 4 ], neither of which clearly showed the concurrent nature of major depressive episodes and AIWS.
Evidence from a number of studies using fluorodeoxyglucose positron emission tomography (FDG-PET) indicates that specific cortical regions, primarily in the frontal cortex, are related to mood disorders. However, the results from imaging studies have not yielded a clear story, and many conflict with each other [ 5 , 6 , 7 ]. One of the more consistent findings with regard to depression, is that hypometabolism in the frontal cortex is characteristic in patients with depressive episodes, and can be partially reversed by successful treatment. In contrast, the biological basis of AIWS is even less clear, although a few studies have made attempts studying it using functional brain imaging [ 8 , 9 , 10 , 11 ].
Here, we present a case of an older patient whose recurrent depressive episodes and AIWS emerged and remitted simultaneously with successful treatment with antidepressants, antipsychotics, and electroconvulsive therapy (ECT). This is the first report showing the concurrent and recurrent nature of, depressive episodes and AIWS, and the strong association between the two. The clinical manifestations and pre- and post-treatment FDG-PET images provide insights into the psychopathological and biological basis of AIWS.
Here, we report the case of a 63-year-old Japanese man with no medical or psychiatric history, except for type-2 diabetes mellitus and essential hypertension. He had no previous history of psychotropic drug use, including antidepressants and antipsychotics. Additionally, he had no developmental abnormalities or neurodevelopmental disorders. He held a steady job from college graduation until retirement age, and his wife described his premorbid personality as dependable, sociable, and patient. He had no family history of psychiatric disorders, migraine, or epilepsy.
One year before his first admission to an inpatient psychiatric unit, he started experiencing mild depressive moods and fatigue that did not disrupt his day-to-day functioning. Two months before the first hospital admission, he began complaining about typical AIWS symptoms, including micropsia, altered perception of his body image, and a disturbed sense of the passage of distance and time. All sorts of objects in his environment, such as buildings and cars, looked extremely small to him. He gave up driving because cars looked so small that he lost his sense of speed and distance in relation to the cars around him. Nearby objects also looked very small, with the single exception of pill strips that he had difficulty opening. Moreover, even though he knew it was not possible, he felt as if he could ‘step over’ long distances in a flash, such as the 50 km from his suburban town to the center of Tokyo. Additionally, he felt that days passed extremely quickly, as if in a single moment. He also sometimes felt his body was slightly enlarged or shrunken compared with normal. These AIWS symptoms persisted all day long during the depressive episodes.
In addition to the typical AIWS symptoms described above, he also complained of disturbances in high-order cognition. For instance, he said, “I cannot sense how important the news is. For example, when I see news about a serial murder on television, I can understand intellectually how sad it is, but I cannot realize it emotionally”. Similarly, he said, “I cannot appreciate the value of money. Even if there were a ¥10,000 bill in front of me, I wouldn’t care about it because I can’t realize how much value it would have”. Although his bowel movements and urination were normal, he complained of a decreased urge to defecate and urinate.
The depressed mood, loss of interest and pleasure, psychomotor retardation, fatigue, and reduced concentration gradually worsened. He was referred to a neurologist. Organic causes were ruled out as follows: his blood-sugar level and blood pressure were well controlled with insulin injections and oral medications; he was a non-drinker, had no history of head trauma, and took no medications associated with adverse reactions that could mimic depression, such as beta-blockers and cimetidine. Neurological examinations and laboratory tests including endocrine evaluations and an HIV test, electroencephalography, and brain magnetic resonance imaging (MRI) detected no abnormalities. He was then referred to a psychiatrist. After confirming that he was not experiencing a manic episode, was not using illicit drugs, and had not experienced any recent stressful life events, he was diagnosed as having a severe depressive episode with AIWS. His condition worsened to the degree that he could not continue working despite taking paroxetine, and he was hospitalized for the first time.
At this first admission, he was bed-ridden all day because of severe depressive symptoms. Administration of amitriptyline (75 mg/day) and perphenazine (6 mg/day) induced gradual improvement of depressive and AIWS symptoms. He was discharged on day 47 after he had remitted almost completely from the depressive episode, with the exception of easily becoming fatigued and waking at night. At that time, he was also completely remitted from AIWS. His day-to-day functioning returned to normal, and his work and life continued as they had before the episode began.
Three years after discharge, he relapsed into another major depressive episode, again simultaneously presenting with AIWS. The symptoms worsened despite the use of amitriptyline (50 mg/day) and aripiprazole (6 mg/day) in the outpatient clinic. The Visual Perception Test for Agnosia detected nothing abnormal. His thoughts became stunted and he became very inactive, lying in bed all day. He continuously refused inpatient treatment because he delusionally believed he was too poor. Upon the strong recommendation from his family, 8 months after this recurrence, he was admitted to the hospital with recurrent severe depressive symptoms and AIWS at the age of 67 years.
At this second admission, he was alert and oriented, but had prolonged speech latency and spoke in a slow and quiet manner without making eye contact. His face was unshaven and he did not smile. Dementia was ruled out as a plausible cause of his symptoms for the following reasons: 1) his Mini-Mental State Examination (MMSE) score was 28/30 during this depressive episode, 2) he made a complete recovery from the observed reduction in concentration and processing speed after treatment of the first episode, 3) he exhibited no other signs of recognizable cognitive decline such as impaired executive function, learning, memory, language, or social recognition, and 4) he did not exhibit any typical symptoms of common dementia subtypes, such as amnesia, fluctuating cognition, visual hallucinations, extrapyramidal symptoms, or behavioral symptoms. Evidence of depressive symptoms and AIWS was comparable between the first and second episodes. He scored 30/63 on the Beck Depression Inventory-II (BDI-II), indicating severe depression. An ophthalmologist confirmed no eye/visual abnormalities with the exception of bilateral cataracts. Pre-therapy FDG-PET was performed as described below. After 2 weeks of maprotiline (75 mg/day) had no effect, twice-weekly ECT, duloxetine (60 mg/day) and mirtazapine (45 mg/day) were administered. He remitted completely from AIWS and almost completely from the depressive episode after 12 ECT sessions, except for a mild reduction in concentration. He scored 12/63 on the BDI-II, which also indicated significant recovery from depression. He was discharged after 75 days, just after post-therapeutic FDG-PET was performed.
FDG-PET acquisition, visual inspection, and statistical analysis
We obtained the pre- and post-treatment FDG-PET images of the brain during the second admission. The patient was kept at rest in supine posture with a blinder in a quiet and dim room from 10 min before each PET examination until the end of the scan. Scans were recorded with a PET scanner (Advance NXi; GE Medical Systems, Milwaukee, WI, USA) 45 min after the injection of 296 MBq FDG.
Upon visual inspection, the pre-treatment FDG-PET images depicted moderate hypometabolism in the frontal cortex and relative hypermetabolism in the occipital and parietal cortices (Fig. 1a ). These abnormalities improved slightly after treatment (Fig. 1b ).
Axial pre- and post-treatment brain FDG-PET images. The color scale ranges from zero to the maximum value within the brain. a Pre-treatment images show hypometabolism in the bilateral frontal cortex ( white arrows ) and relative hypermetabolism in the bilateral occipital and parietal cortex ( red arrows ). b Post-treatment images show slight normalization of these abnormalities
Statistical analysis was performed in the following steps: (1) morphological co-registration between pre-and post-treatment FDG-PET; (2) normalization of voxel values to the global mean voxel counts using proportional scaling; (3) subtraction of pre-treatment from post-treatment images to obtain pre-post difference images; (4) mean and standard deviations of voxel values were calculated for the difference images; and (5) identification of area with statistically significant difference, using a cutoff value of z > 2 and extent threshold k > 200. These methods are part of the standard process for subtracting ictal single photon emission computed tomography (SPECT) coregistered to MRI (SISCOM), which is generally used for comparing ictal and interictal SPECT images in epileptic patients [ 12 ]. The statistical analysis showed that metabolism decreased after treatment in the posterior half of the cerebral cortex, including the posterior part of the bilateral temporal cortex, the occipital cortex, the inferior part of parietal cortex, precuneus, and posterior cingulate cortex (Fig. 2 ). No area showed statistically significant increases in metabolism after treatment.
Within-subject comparison between pre- and post-treatment in our patient. The colored areas indicate significant decreases in metabolism from pre- to post-treatment, with the color scale (z score) ranging from 2 to 5
Synchronicity of depressive episodes and AIWS
In this case study, we described an older patient presenting with two distinct major depressive episodes, both of which occurred simultaneously with episodes of AIWS. Both sets of symptoms remitted completely after standard treatment for psychotic depression (i.e., an antidepressant plus an antipsychotic, or ECT), and we excluded the potential influence of dementia and other organic causes. This is the first report that clearly shows a link between recurrent depressive disorder and AIWS. The clinical co-occurrence of depressive episodes and AIWS can be interpreted as arising from common functional disturbances. Below we elaborate on the relationship between AIWS and severe depression from the viewpoints of psychopathology and of neuroimaging.
AIWS presenting in the course of psychotic depression
Lanska et al. reported that a variety of conditions contribute to AIWS, including infection, migraine, toxic encephalopathy, major depression, epileptic seizures, medications, and stroke [ 2 ]. However, to date, only two case reports have shown an association between depressive episodes and AIWS [ 3 , 4 ]. Mizuno et al. reported a 54-year-old man who exhibited depressive symptoms with AIWS (metamorphopsia, disturbed sense of passage of time, and distortion of body image). In that case, AIWS disappeared 2 days after admission despite no improvement in depressive symptoms [ 3 ]. Bui et al. reported a 74-year-old man who showed severe depressive symptoms with persecutory and somatic delusions (his stools being contaminated) and AIWS (he thought his hands and feet were shorter than usual), all of which remitted completely with ECT [ 4 ]. Importantly, both cases presented with psychotic depression during the clinical course. In Mizuno et al., the patient developed a delusion of culpability and in Bui et al., the patient developed persecutory and somatic delusions. Our patient also transiently developed delusions (he believed he was poor) during the depressive episode. The clinical presentation of these three cases indicates an association between AIWS and psychotic depression in particular.
Psychopathological similarities between AIWS and psychotic depression
Patients with psychotic depression tend to regard themselves as being useless, or consider everything meaningless. They also claim to lose a grasp on proper emotions and visceral sensations. Stanghellini et al. extensively reviewed the psychopathology of depression and described the qualitative features of experience in patients with psychotic depression to include incapacity, indifference, timelessness, and bodily devitalization [ 13 ]. Failure to sense the significance or magnitude of external facts or objects, such as the difficulty with news and money seen in our patient, can be viewed as being part of the incapacity or indifference categories. Being unable to estimate or sense one’s own urge to urinate or make bowel movements can also be explained by indifference or devitalization. According to Stanghellini et al. constriction of time and body experiences, as well as shrinking and extension of space, occur in major depression. Perceptual alterations in space, time, and body seem to be notably analogous to that of AIWS. Thus, we argue that comorbidity of AIWS and psychotic depression in our case was not by chance, but occurred because of a common underlying brain dysfunction.
Interpretation of FDG-PET results
The frontal cortex hypometabolism in our case was probably related to the depressive symptoms (Fig. 1 ). Hosokawa et al. reported that euthymic patients exhibited fewer areas with significantly low metabolism than did depressed patients in the cross-sectional study [ 5 ]. In our case, the decreased metabolism of bilateral frontal cortex and anterior cingulate cortex during the second depressive episode improved after treatment, although these alterations were not statistically significant. These results are consistent with many studies demonstrating that metabolism in the frontal cortex decreases in patients with depressive episodes and can be partially reversed by treatment [ 5 , 6 ].
The significant metabolic abnormalities and alterations in the posterior half of the cerebral cortex are the main characteristics of our case (Figs. 1 , 2 ). These regions include the primary visual cortex, precuneus, posterior cingulate, and temporal, parietal, and extrastriate cortices. The abnormalities in these association cortices possibly correspond to positive symptoms in our case, such as delusions of poverty or experiencing alterations in space, time, and body, which are not simply perceptual, but also include high-order cognitive disturbances. The parieto-occipital hypermetabolism in our case might also be associated with a common underlying abnormality that occurs in both psychotic depression and AIWS, although this should be explored in future studies.
We present the first case demonstrating a clear relationship between recurrent depressive disorder and AIWS. The co-occurrence and similarities in clinical manifestations between AIWS and psychotic depression imply a common psychopathological basis. The metabolic abnormalities seen in high-order brain regions on FDG-PET images suggest a biological basis of AIWS and psychotic symptoms of depression. Careful analysis of psychiatric symptoms comparing with metabolic changes using FDG-PET provides new insights into higher-order involvements, not only primary visual perception, in AIWS and psychotic depression.
Abbreviations
- Alice in Wonderland syndrome
Beck Depression Inventory-II
Electroconvulsive therapy
- Fluorodeoxyglucose positron emission tomography
Mini-Mental State Examination
Magnetic resonance imaging
Subtraction ictal SPECT coregistered to MRI
Single photon emission computed tomography
Todd J. The syndrome of Alice in Wonderland. Can Med Assoc J. 1955;73:701–4.
CAS PubMed PubMed Central Google Scholar
Lanska JR, Lanska DJ. Alice in Wonderland syndrome: somesthetic vs visual perceptual disturbance. Neurology. 2013;80:1262–4.
Article PubMed Google Scholar
Mizuno M, Kashima H, Chiba H, Murakami M, Asai M. Alice in Wonderland’ syndrome as a precursor of depressive disorder. Psychopathology. 1998;31:85–9.
Article CAS PubMed Google Scholar
Bui E, Chatagner A, Schmitt L. Alice in Wonderland syndrome in major depressive disorder. J Neuropsychiatry Clin Neurosci. 2010;22:e16.
Article Google Scholar
Hosokawa T, Momose T, Kasai K. Brain glucose metabolism difference between bipolar and unipolar mood disorders in depressed and euthymic states. Prog Neuro-Psychopharmacol Biol Psychiatry. 2009;33:243–50.
Article CAS Google Scholar
Chen Q, Liu W, Li H, Zhang H, Tian M. Molecular imaging in patients with mood disorders: a review of PET findings. Eur J Nucl Med Mol Imaging. 2011;38:1367–80.
Kennedy SH, Evans KR, Krüger S, Mayberg HS, Meyer JH, McCann S, et al. Changes in regional brain glucose metabolism measured with positron emission tomography after paroxetine treatment of major depression. Am J Psychiatry. 2001;158:899–905.
Morland D, Wolff V, Dietemann JL, Marescaux C, Namer IJ. Robin Hood caught in Wonderland: brain SPECT findings. Clin Nucl Med. 2013;38:979–81.
Kuo YT, Chiu NC, Shen EY, Ho CS, Wu MC. Cerebral perfusion in children with Alice in Wonderland syndrome. Pediatr Neurol. 1998;19:105–8.
Gencoglu EA, Alehan F, Erol I, Koyuncu A, Aras M. Brain SPECT findings in a patient with Alice in Wonderland syndrome. Clin Nucl Med. 2005;30:758–9.
Brumm K, Walenski M, Haist F, Robbins SL, Granet DB, Love T. Functional magnetic resonance imaging of a child with Alice in Wonderland syndrome during an episode of micropsia. J AAPOS. 2010;14:317–22.
Article PubMed PubMed Central Google Scholar
Matsuda H, Matsuda K, Nakamura F, Kameyama S, Masuda H, Otsuki T, et al. Contribution of subtraction ictal SPECT coregistered to MRI to epilepsy surgery: a multicenter study. Ann Nucl Med. 2009;23:283–91.
Stanghellini G, Raballo A. Differential typology of delusions in major depression and schizophrenia. A critique to the unitary concept of ‘psychosis’. J Affect Disord. 2015;171:171–8.
Download references
Acknowledgments
The authors are grateful to the patient and his family for their help and support in writing this case report. The authors thank Dr. Kiyoto Kasai for his general support. The authors also wish to express their deepest gratitude to Dr. Atsushi Iwata, Dr. Toshihiro Hayashi, Dr. Toji Miyagawa, and Dr. Kazuyuki Sugishita (Memory clinic of Tokyo University Hospital) for their support.
Availability of data materials
The data sets supporting the results of this article are included within the article.
Authors’ contributions
TY, TO, and SK were responsible for the clinical decisions outlined in this report. TY, MT, and SK drafted the manuscript. TO conceived the report and helped to draft the manuscript. MT performed the FDG-PET analysis. TM supported with the FDG-PET analysis. SK was critically involved in the theoretical discussion and writing the manuscript. All authors contributed to the literature review and manuscript preparation and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent for the publication of the case report was obtained from the patient.
Ethics approval and consent to participate
Approval by the University of Tokyo Hospital ethics committee was obtained (3349-(4)).
Author information
Authors and affiliations.
Department of Neuropsychiatry, Graduate School of Medicine, University of Tokyo, 7-3-1 Hongo, Bunkyo-ku, Tokyo, 113-8655, Japan
Tatsushi Yokoyama, Tsuyoshi Okamura & Shinsuke Kondo
Department of Radiology, Graduate School of Medicine, University of Tokyo, 7-3-1Hongo, Bunkyo-ku, Tokyo, 113-8655, Japan
Miwako Takahashi & Toshimitsu Momose
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Shinsuke Kondo .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Yokoyama, T., Okamura, T., Takahashi, M. et al. A case of recurrent depressive disorder presenting with Alice in Wonderland syndrome: psychopathology and pre- and post-treatment FDG-PET findings. BMC Psychiatry 17 , 150 (2017). https://doi.org/10.1186/s12888-017-1314-2
Download citation
Received : 19 April 2016
Accepted : 17 April 2017
Published : 27 April 2017
DOI : https://doi.org/10.1186/s12888-017-1314-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Recurrent depressive disorder
- Psychotic depression
- High-order brain function
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Malays Fam Physician
- v.17(1); 2022 Mar 28
Case scenario: Management of major depressive disorder in primary care based on the updated Malaysian clinical practice guidelines
Uma visvalingam.
MBBS (MAHE), Master of Medicine (Psychiatry) (UKM), Department of Psychiatry and Mental Health, Hospital Putrajaya, Putrajaya, Malaysia
Umi Adzlin Silim
MD (UKM), M. Med (Psychiatry) (UKM), Department of Psychiatry and Mental Health, Hospital Serdang, Serdang, Selangor, Malaysia
Ahmad Zahari Muhammad Muhsin
MB., BCh., BAO (UCD, Ireland), M. Psych Med (Malaya), Department of Psychological Medicine, Faculty of Medicine Universiti Malaya, Kuala Lumpur, Malaysia
Firdaus Abdul Gani
MBBS (Malaya) M.Med (Psy) (USM) CMIA (NIOSH), Department of Psychiatry and Mental Health, Hospital Sultan Haji Ahmad Shah, Temerloh, Pahang, Malaysia
Noormazita Mislan
MB, BCh, BAO (Ireland), M Med. (Psychiatry) (UKM), Department of Psychiatry and Mental Health, Hospital Tuanku Ja'afar, Seremban, Negeri Sembilan, Malaysia
Noor Izuana Redzuan
MBBS (Malaya), Dr in Psychiatry (UKM), Department of Psychiatry and Mental Health, Hospital Raja Permaisuri Bainun, Ipoh, Perak, Malaysia
Peter Kuan Hoe Low
MB, BCh, BAO (Ireland), M.Psych Med (UM), Department of Psychiatry and Mental Health, Hospital Kuala Lumpur, Kuala Lumpur, Malaysia
Sing Yee Tan
MBBS (Malaya), M.Med (Family Med) (UM), Klinik Kesihatan Jenjarom, Jenjarom Selangor, Malaysia
Masseni Abd Aziz
MD (USM) M Med (Fammed) USM, Klinik Kesihatan Umbai, Merlimau, Melaka, Malaysia
Aida Syarinaz Ahmad Adlan
MBBS (Malaya), M. Psych Med (UM), PostGrad. Dip. (Dynamic Psychotherapy) (Mcgill University), Department of Psychological Medicine, Faculty of Medicine, Universiti Malaya Kuala, Lumpur, Malaysia
Suzaily Wahab
MD (UKM), MMed Psych (UKM), Hospital Canselor Tuanku Muhriz UKM, Kuala Lumpur, Malaysia

Aida Farhana Suhaimi
B. Psych (Adelaide), M. Psych (Clin. Psych) (Tasmania), PhD (Psychological Medicine) (UPM), Department of Psychiatry and Mental Health, Hospital Putrajaya, Putrajaya, Malaysia
Nurul Syakilah Embok Raub
BPharm (Hons) (CUCMS), MPH (Malaya), Pharmacy Enforcement Branch, Selangor Health State Department, Shah Alam, Selangor, Malaysia
Siti Mariam Mohtar
BPharm (UniSA), Malaysian Health Technology Assessment Section (MaHTAS), Ministry of Health Malaysia, Putrajaya, Malaysia
Mohd Aminuddin Mohd Yusof
MD (UKM), MPH (Epidemiology) (Malaya), Malaysian Health Technology Assessment Section (MaHTAS), Ministry of Health Malaysia, Putrajaya, Malaysia, Email: moc.oohay@rd2ma
Major depressive disorder (MDD) is a common but complex illness that is frequently presented in the primary care setting. Managing this disorder in primary care can be difficult, and many patients are underdiagnosed and/or undertreated. The Malaysian Clinical Practice Guidelines (CPG) on the Management of Major Depressive Disorder (MDD) (2nd ed.), published in 2019, covers screening, diagnosis, treatment and referral (which frequently pose a challenge in the primary care setting) while minimising variation in clinical practice.
Introduction
MDD is one of the most common mental illnesses encountered in primary care. It presents with a combination of symptoms that may complicate its management.
This mental disorder requires specific treatment approaches and is projected to be the leading cause of the disease burden in 2030. 1 Patients experiencing this ailment are at elevated risk for early mortality from physical disorders and suicide. 2 In Malaysia in particular, MDD contributes to 6.9% of total Years Living with Disability. 3
Ensuring full functional recovery and prevention of relapse makes remission the targeted outcome for treatment of MDD. In contrast, nonremission of depressive symptoms in MDD can impact functionality 4 and subsequently amplify the economic burden that the illness imposes.
About the new edition
The highlights of the updated CPG MDD (2nd ed.) are as follows:
- emphasis on psychosocial and psychological interventions, particularly for mild to moderate MDD
- inclusion of all second-generation antidepressants as the first-line pharmacotherapy
- introduction of new emerging treatments, ie. intravenous ketamine for acute phase and intranasal esketamine for next-step treatment/treatment-resistant MDD
- improvement in pre-treatment screening and monitoring of treatment
- integration of mental health into other health services with emphasis on collaborative care
- addition of 2 new chapters on special populations (pregnancy and postpartum, chronic medical illness) and table on safety profile of pharmacotherapy in pregnancy and breastfeeding
- comprehensive, holistic biopsychosocial-spiritual approaches addressing psychospirituality
Details of the evidence supporting the above statements can be found in Clinical Practice Guidelines on the Management of Major Depressive Disorder (2nd ed.) 2019, available on the following websites: http://www.moh.gov.my (Ministry of Health Malaysia) and http://www.acadmed.org.my (Academy of Medicine). Corresponding organisation: CPG Secretariat, Health Technology Assessment Section, Medical Development Division, Ministry of Health Malaysia; contactable at ym.vog.hom@aisyalamath .
Statement of intent
This is a support tool for implementation of CPG Management of Major Depressive Disorder (2nd ed.).
Healthcare providers are advised of their responsibility to implement this evidence-based CPG in their local context. Such implementation will lead to capacity building to ensure better accessibility of psychosocial and psychological services. More options in pharmacotherapy facilitate flexibility in prescribing antidepressants among clinicians. Further integration of mental health into other health services, upscaling of mental health service development in perinatal and medical services, and enhancement of collaborative care will incorporate holistic approaches into care.
Case Scenario
Tini is a female college student aged 24 years old. She comes to the health clinic accompanied by a friend and complains of several symptoms that she has experienced over the past 4 weeks. She reports:
- difficulty falling asleep, feeling tired after waking up in the morning and experiencing headaches
- difficulty staying focused during classes. These symptoms have led to deterioration in her study and prompted her to seek advice from the doctor.
Will you screen her for depression?
Yes, because the patient presents with multiple vague symptoms and sleep disturbance. 5 (Refer to Subchapter 2.1, page 3 in CPG.)
What tools are used to screen for depression?
Screening tools for depression are:
- Beck Depression Inventory (BDI)
- Depression Anxiety and Stress Scale (DASS)
- Patient Health Questionnaire-9 (PHQ-9)
- Hospital Anxiety and Depression Scale (HADS)
- Whooley Questions
Screening for depression using Whooley Questions in primary care may be considered in people at risk. 5
( Refer to Subchapter 2.1, pages 3 and 4 in CPG. )
- “During the past month, have you often been bothered by feeling down, depressed or hopeless?”
- “During the past month, have you often been bothered by having little interest or pleasure in doing things?
The doctor decides to use Whooley Questions, and Tini answers “yes” to both questions.
How would you proceed from here to further assess for depression?
Assessment of depression consists of:
- detailed history taking (Refer to Subchapter 2.2, page 4 in CPG.)
- mental state examination (MSE), including evaluation of symptom severity, presence of psychotic symptoms and risk of harm to self and others
- physical examination to rule out organic causes
- investigations where indicated — biological and psychosocial investigations
Upon further assessment, Tini reveals that she feels overwhelmingly sad. She is frequently tearful and reports feeling excessively guilty, blaming herself for not performing well enough in her studies. Her postings on social media have been revolving around themes of self-defeat. Despite feeling low, she still strives to attend classes and complete her assignments. However, her academic performance has exhibited a marked deterioration. There is no history to suggest hypomanic, manic or psychotic symptoms. She denies using any illicit substances or alcohol. Her menstrual cycle is normal and does not correspond to her mood changes.
MSE reveals a young lady who appears to be in distress. Rapport is easily established, but her eyes are downcast. Her speech is relevant, with low tone. She describes her mood as sad; she is tearful while talking about her poor results, with appropriate affect. She harbours multiple unhelpful thoughts, eg. “I’m a failure” and “I’m useless”. She exhibits no suicidal ideations, delusions or hallucinations. Her concentration is poor, and insight is partial.
Physical examination reveals no recent selfharm scars, and examination of other systems is unremarkable. Biological investigations such as full blood count and thyroid function test are within normal range. Corroborative history is taken from accompanying person to verify the symptoms.
How would you arrive at the diagnosis and severity?
Diagnosis of depression can be made using the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) or the 10th revision of the International Statistical Classification of Disease and Related Health Problems (ICD-10). 5 (Refer to Appendix 3 and 4, pages 73-76 in CPG.) 6 , 7
In the last 2 weeks, Tini has been experiencing:
- poor concentration
- excessive guilt
These symptoms have caused marked impairment in her academic functioning. Thus, she is diagnosed as having MDD with mild to moderate severity in acute phase and can be treated in primary care.
Severity according to DSM-5
- Five or more symptoms are present, which cause distress but are manageable
- Result in minor impairment in social or occupational functioning
- Symptom presentation and functional impairment between 2 severities
- Most of the symptoms are present with marked impairment in functioning
What can be offered to this patient?
Psychosocial interventions and psychotherapy with or without pharmacotherapy. 5 (Refer to Algorithm 1. Treatment of Major Depressive Disorder, page xii in CPG)
ALGORITHM 1. TREATMENT OF MAJOR DEPRESSIVE DISORDER

Psychosocial interventions include the following:
- symptoms and course of depression
- biopsychosocial model of aetiology
- pharmacotherapy for acute phase and maintenance
- drug side effects and complications
- importance of medication adherence
- early signs of recurrence
- management of relapse and recurrence
- counselling/non-directive supportive therapy - aims to guide the person in decision-making and allow to ventilate their emotions
- relaxation - a method to help a person attain a state of calmness, eg. breathing exercise, progressive muscle relaxation, relaxation imagery
- peer intervention - eg. peer support group
- exercise - activity of 45-60 minutes per session, up to 3 times per week, and prescribed for 10-12 weeks
(Refer to subchapter 4.1.1, pages 9-12 in CPG.)
However, the doctor may choose to start antidepressant medication as an initial measure in some situations, for example:
- past history of moderate to severe depression
- patient’s preference
- previous response to antidepressants
- lack of response to non-pharmacotherapy interventions
What are the types of psychotherapy that can be offered in mild to moderate MDD, and what factors should be considered before starting psychotherapy?
Psychotherapy for the treatment of MDD has been shown to reduce psychological distress and improve recovery through the therapeutic relationship between the therapist and the patient.
In mild to moderate MDD, psychosocial intervention and psychotherapy should be offered, based on resource availability, and may include but are not restricted to the following 5 :
- Cognitive behavioural therapy (CBT)
- Interpersonal therapy
- Problem-solving therapy
- Behavioural therapy
- Internet-based CBT
The type of psychotherapy offered to the patient will depend on various factors, including 5 :
- patient preference and attitude
- nature of depression
- availability of trained therapist
- therapeutic alliance
- availability of therapy
(Refer to Subchapter 4.1.1, page 17 in CPG.)
After shared-decision making, Tini receives psychosocial intervention, that includes:
- psychoeducation
- non-directive supportive therapy
- lifestyle modification, e.g. restoring healthy sleep hygiene and adopting healthy eating habits
- relaxation, e.g. progressive muscle relaxation, imagery and breathing technique
Tini will benefit from CBT due to her multiple unhelpful thoughts, for example, “I’m a failure” and “I’m useless”.
CBT helps improve understanding of the impact of a person’s unhelpful thoughts on current behaviour and functioning through cognitive restructuring and a behavioural approach. By learning to correctly identify these negative thinking patterns, Tini can then challenge such thoughts repeatedly to replace disordered thinking with more rational, balanced and healthy thinking. However, she is not able to commit to regular sessions of CBT due to a demanding academic schedule and upcoming final examination. After further discussion, Tini opts for pharmacotherapy.
What are the options for pharmacotherapy?
The choice of antidepressant medication will depend on various factors, including efficacy and tolerability, patient profile and comorbidities, concomitant medications and drug-drug interactions, cost and availability, as well as the patient’s preference. Taking into account efficacy and side effect profiles, most second-generation antidepressants, namely selective serotonin reuptake inhibitors (SSRIs), serotonin noradrenaline reuptake inhibitors (SNRIs), noradrenergic and specific serotonergic antidepressants (NaSSAs), melatonergic agonist and serotonergic antagonist, noradrenaline/dopamine-reuptake inhibitors (NDRIs) and a multimodal antidepressants may be considered as the initial treatment medication, while the older antidepressants such as tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) may be subsequently considered for a later choice. 5 (Refer to Subchapter 4.1.2, page 18 in CPG.)
Since Tini is being seen at a health clinic, the widely available SSRIs are sertraline and fluvoxamine. Sertraline has fewer gastrointestinal side effects and drug interactions compared with fluvoxamine. TCAs are not the treatment of choice due to prominent side effects. Tini is put on tablet sertraline 50 mg daily and educated on the anticipated onset of response and possible side effects. Short-term and low dose benzodiazepine, eg. alprazolam or lorazepam, may be offered as an adjunct to treat her insomnia. (Refer to Subchapter 4.1.2, page 24 in CPG.) Tini is given tablet lorazepam 0.5 mg at night for 2 weeks. She is asked to come in for a follow-up.
What is her follow-up and monitoring plan?
The following should be done:
(Refer to Appendix 8, page 81 in CPG.)
- Titrate up by 50 mg within 1-2 weeks (but may be done earlier based on clinical judgement)
- Monitor biological parameters if indicated (Refer to Table 5. Ongoing monitoring during treatment of MDD, page 57 in CPG.)
During follow-up at 2 weeks, she is noted to show partial response despite being compliant with good tolerability. She is not experienceing nausea, diarrhoea, headache, constipation, dry mouth or somnolence. She reports being less tearful. Her sleep and ability to focus have improved. Tini has started engaging in regular exercise and practises relaxation, especially before sleep. Tablet sertraline is optimised to 100 mg daily, while tablet lorazepam is reduced to 0.5 mg PRN.
Tini is reviewed again within 4 weeks; during this subsequent follow-up, she achieves full remission. Tablet lorazepam is stopped. She is then advised to continue tablet sertraline for at least 6-9 months in maintenance phase. The aim in this phase is to prevent relapse and recurrence of MDD. In view of her young age, no comorbidities and good tolerability, repeated electrolyte monitoring is not indicated.
(Refer to Algorithm 2. Pharmacotherapy for Major Depressive Disorder, page xiii in CPG.)
ALGORITHM 2. PHARMACOTHERAPY FOR MAJOR DEPRESSIVE DISORDER

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 June 2024
Psychiatric adverse events following COVID-19 vaccination: a population-based cohort study in Seoul, South Korea
- Hong Jin Kim ORCID: orcid.org/0000-0002-8162-9585 1 ,
- Min-Ho Kim ORCID: orcid.org/0000-0003-4909-2308 2 ,
- Myeong Geun Choi 3 &
- Eun Mi Chun ORCID: orcid.org/0000-0001-9616-2722 3
Molecular Psychiatry ( 2024 ) Cite this article
23 Altmetric
Metrics details
- Bipolar disorder
- Schizophrenia
Evidence has suggested an increased risk of psychiatric manifestations following viral infections including coronavirus disease-2019 (COVID-19). However, psychiatric adverse events (AEs) after COVID-19 vaccination, which were documented in case reports and case series, remain unclear. This study is aimed to investigate the psychiatric AEs after COVID-19 vaccination from a large population-based cohort in Seoul, South Korea. We recruited 50% of the Seoul-resident population randomly selected from the Korean National Health Insurance Service (KNHIS) claims database on 1, January, 2021. The included participants ( n = 2,027,353) from the Korean National Health Insurance Service claims database were divided into two groups according to COVID-19 vaccination. The cumulative incidences per 10,000 of psychiatric AEs were assessed on one week, two weeks, one month, and three months after COVID-19 vaccination. Hazard ratios (HRs) and 95% Confidence interval (CIs) of psychiatric AEs were measured for the vaccinated population. The cumulative incidence of depression, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders at three months following COVID-19 vaccination were higher in the vaccination group than no vaccination group. However, schizophrenia and bipolar disorders showed lower cumulative incidence in the vaccination group than in the non-vaccinated group. Depression (HR [95% CI] = 1.683 [1.520–1.863]), anxiety, dissociative, stress-related, and somatoform disorders (HR [95% CI] = 1.439 [1.322–1.568]), and sleep disorders (HR [95% CI] = 1.934 [1.738–2.152]) showed increased risks after COVID-19 vaccination, whereas the risks of schizophrenia (HR [95% CI] = 0.231 [0.164–0.326]) and bipolar disorder (HR [95% CI] = 0.672 [0.470–0.962]). COVID-19 vaccination increased the risks of depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders while reducing the risk of schizophrenia and bipolar disorder. Therefore, special cautions are necessary for administering additional COVID-19 vaccinations to populations vulnerable to psychiatric AEs.
Similar content being viewed by others
Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population

Association of preexisting psychiatric disorders with post-COVID-19 prevalence: a cross-sectional study
COVID-19 and severe mental illness in Israel: testing, infection, hospitalization, mortality and vaccination rates in a countrywide study
Introduction.
In the unprecedented era of coronavirus disease-2019 (COVID-19), the global outbreak of COVID-19 has had an unpredictable and heterogeneous impact on the healthcare system worldwide [ 1 , 2 ]. Especially in mental illness, COVID-19 showed an increased risk of mental health problems together with lockdown, social distancing, and uncertain causes [ 3 , 4 ]. There have been growing concerns that the COVID-19 pandemic has increasingly had a detrimental effect on long-term mental health at an early stage in the development of vaccines [ 5 , 6 ].
The rapid development of COVID-19 vaccines, ranging from mRNA-based vaccines (BNT162b2, mRNA-1273) to viral vector vaccines (cDNA-based vaccines; AZD1222, JNJ-78436735), has contributed to overcoming the COVID-19 pandemic in the view of severity and mortality [ 1 , 7 ]. However, it has also given rise to new issues such as post-COVID-19 sequelae and vaccine-related adverse events (AEs) [ 2 , 5 , 6 , 7 , 8 , 9 , 10 ]. With their issues, mental health is still an unsolved concern in the post-COVID-19 era [ 4 , 6 ]. Many studies have focused on the correlation between mental health and COVID-19 breakthrough [ 11 ]. However, mental illness as a result of the COVID-19 vaccine itself, specifically post-vaccination psychiatric AEs was not well-studied, with scant evidence in the literature, which was documented primarily in the form of case reports and case series [ 12 , 13 , 14 , 15 ].
In this study, we investigated the psychiatric AEs including schizophrenia, depression, bipolar disorder, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders after COVID-19 vaccination from a population-based cohort using the Korean National Health Insurance Service (KNHIS) claims database in Seoul, South Korea.
Materials and methods
The concept and protocol of this study were approved by the Institutional Review Board (IRB) of our institute, which waived the requirement for informed consent because data analyses were performed retrospectively using anonymized data derived from the South Korean NHIS database.
Data source
We used the KNHIS claims database to recruit a randomly selected 50% of the population residing in Seoul on 1 January 2021 with their diagnostic records up to 31 December 2021. The process of selecting a random 50% of the population in Seoul was carried out by the KNHIS system. After authorization by KNHIS, the data collection was performed in November 2022. The psychiatric AEs included schizophrenia, mood disorders (depression, and bipolar disorder), anxiety, dissociative, stress-related, and somatoform disorders (anxiety disorders, obsessive-compulsive disorder, reacting to severe stress, and adjustment disorders, conversion disorders, somatoform disorders, and other neurotic disorders), sleep disorders, eating disorders, and sexual disorders using the International Classification of Diseases (ICD) Tenth Revision codes after the index date. This population-based cohort study was also conducted by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [ 16 ].
Study population
A total of 4,348,412 individuals living in Seoul, South Korea, constituting 50% of the population, were included and investigated as of January 1, 2021. Individuals under 20 years (n = 144,525) were excluded, leaving 4,203,887 individuals for analysis. We initially divided into two groups based on COVID-19 vaccination and defined as vaccinated group as individuals who received two doses of the COVID-19 vaccine. For the 3,839,014 vaccinated population, we excluded 1,684,625 individuals who did not receive a second dose by 1, October 2021. For 364,873 unvaccinated population, we excluded 13,890 individuals who died on 1, October 2021. The diagnostic records for the year preceding the index date were traced to investigate the causal relationship between vaccine administration and AEs. The occurrence of the target psychiatric disorders was defined as receiving a primary diagnosis of the disease from the day following the index date. Individuals who had received a primary or secondary diagnosis of any target disease for a year prior to index date were excluded from the study. We finally included the participants defined by two groups in this study: the vaccinated group (n = 1,718,999) and the non-vaccinated group (n = 308,354) (Fig. 1 ).
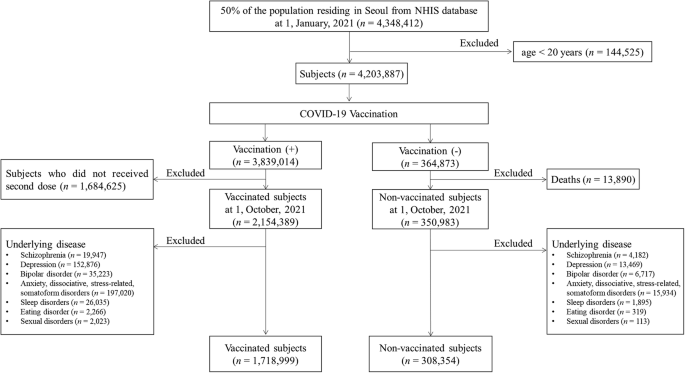
Flowchart of this study.
Outcome measurements
The primary outcome measure was the cumulative incidence of psychiatric AEs per 10,000 population at one week, two weeks, one month, and three months between two groups. The secondary outcome measures were risks of psychiatric target AEs for COVID-19 vaccination using the odd ratios (ORs) and hazard ratios (HRs). Furthermore, subgroup analyses were also conducted based on gender, age, the number of COVID-19 vaccine doses, the vaccine type (mRNA vaccine, cDNA vaccine, and heterologous vaccination), health insurance level, presence of diabetes mellitus (DM), hypertension (HTN), hyperlipidemia, and chronic obstructive pulmonary disease (COPD). Age, gender, insurance level, Charlson’s comorbidity index (CCI), presence of DM, HTN, hyperlipidemia, and COPD, and prior COVID-19 infection history were extracted using their ICD-19 codes, which were suggested by Sundararajan et al. [ 17 ]. The presence of comorbid diseases (i.e., DM, HTN, hyperlipidemia, and COPD), categories of CCI, and the prior COVID-19 infection history were determined based on receiving a primary or secondary diagnosis at least twice within one year before the index date. The National Health Insurance (NHI) premium was used as a proxy for income, as it is proportional to monthly income, encompassing both earnings and capital gains. The income quantiles of the enrolled participants were subdivided into three groups (low-, middle- and high-income groups in medical aid enrollees and the 0–33, 34–66, and 67–100 centiles of NHI enrollees). Detailed information for ICD-10 codes used for analysis is presented in Supplementary Table 1 .
Statistical analysis
Statistical analysis was performed using the SAS Enterprise Guide (version 8.3., SAS Institute, Cary, NC, USA). A normal distribution was confirmed with the Kolmogorov–Smirnov test. Baseline patient characteristics and comorbidities were reported as means ± standard deviation for continuous variables and ratio for categorical variables. Student’s t test was performed for continuous variables and the chi-square test for categorical variables. The cumulative incidence was calculated per 10,000 populations. To identify the association between COVID-19 vaccination and psychiatric AEs, a multiple logistic regression model was used for ORs, corresponding to 95% CIs. Cox proportional hazards regression was used to estimate the HRs and 95% CIs. Two-sided p values of 0.05 or less were considered to indicate statistical significance.
The participants’ characteristics
In total, 2,027,353 subjects were included in this study. Among them, 308,354 (15.21%) had not received the COVID-19 vaccine (i.e., non-vaccinated subjects, no vaccination group in this study), whereas 1,718,999 (84.79%) were vaccinated against COVID-19 (i.e., vaccinated subjects, the vaccinated group in this study). The baseline characteristics of the vaccinated and non-vaccinated groups are presented in Table 1 .
The cumulative incidences per 10,000 of psychiatric AEs following the COVID-19 vaccination
The cumulative incidence of the psychiatric AEs at three months was 0.51 (95% CI, 0.40–0.62) vs 1.98 (95% CI, 1.48–2.47) for schizophrenia, 18.30 (95% CI, 17.66-18.93) vs 14.24 (95% CI, 12.91–15.57) for depression, 0.79 (95% CI, 0.66–0.92) vs 1.39 (95% CI, 0.98–1.81) for bipolar disorder, 28.41 (95% CI, 27.62–29.21) vs 20.27 (95% CI, 18.68–21.86) for anxiety, dissociative, stress-related, and somatoform disorders, 0.30 (95% CI, 0.22–0.38) vs 0.32 (95% CI, 0.12–0.53) for eating disorder, 28.85 (95% CI, 28.05–29.96) vs 12.19 (95% CI, 10.96–13.43) for sleep disorders, 0.27 (95% CI, 0.19–0.34) vs 0.03 (95% CI, 0.00–0.10) for sexual disorders between the vaccinated group and non-vaccinated group. Therefore, the cumulative incidences of schizophrenia ( p < 0.001) and bipolar disorder ( p = 0.002) were significantly lower in the vaccinated group than in the non-vaccinated group. Meanwhile, depression ( p < 0.001), anxiety, dissociative, stress-related, and somatoform disorders ( p < 0.001), sleep disorders ( p < 0.001), and sexual disorders ( p = 0.007) showed significantly higher cumulative incidence in the vaccinated group than in the non-vaccinated group. There was no statistical difference in the cumulative incidence of eating disorders at three months between the two groups ( p = 0.724). Detailed information of cumulative incidence was presented in Table 2 .
The cumulative incidences per 10,000 of psychiatric AEs according to vaccine types
Our data was also stratified by vaccine type including vaccination using mRNA-based vaccine only (only mRNA vaccine), vaccination using cDNA-based vaccine only (only cDNA vaccine), and heterologous vaccination, which were compared by non-vaccinated group. For decreased incidences of schizophrenia and bipolar disorder following COVID-19 vaccination, schizophrenia showed the lowest cumulative incidence at three months in the case of heterologous vaccination (0.42; 95% CI, 0.05–0.79) compared to other vaccine types with statistical significances ( p < 0.001). The lowest cumulative incidence of bipolar disorder at three months was observed in the case of vaccination using only cDNA vaccine (0.39; 95% CI, 0.23-0.55) with a statistical difference ( p < 0.001). For increased incidences of depression, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders following COVID-19 vaccination, the highest cumulative incidence of depression at three months was significantly observed in heterologous vaccination (23.31; 95% CI, 20.56–26.05) compared to other vaccine types ( p < 0.001). However, the cumulative incidence of depression at three months was lower in the case of vaccination using only cDNA vaccine (12.26; 95% CI, 11.37–13.15) than in the non-vaccinated group (14.24; 95% CI, 12.91–15.57) with statistical differences ( p = 0.014). The incidence of anxiety, dissociative, stress-related, and somatoform disorders was significantly observed to be highest in the case of heterologous vaccination (31.75; 95% CI, 28.55–34.95), followed by only mRNA vaccination (29.13; 95% CI, 28.08–30.18) and only cDNA vaccination (26.53; 95% CI, 25.22–27.83) ( p < 0.001). The incidence of sleep disorders at three months was significantly observed to be high level in both cases of only cDNA vaccination (34.78; 95% CI, 33.28–36.28), and heterologous vaccination (32.09; 95% CI, 28.87–35.31), followed by only mRNA vaccination (24.98; 95% CI, 24.00–25.96) ( p < 0.001). The cumulative incidences of sexual disorders showed no statistical differences up to one month ( p > 0.05). At three months, the sexual disorder showed differences in cumulative incidence according to vaccine types ( p = 0.04). There was no statistical difference in the cumulative incidence of eating disorders at three months ( p = 0.785) according to vaccine types. The cumulative incidences of psychiatric AEs according to vaccine type are presented in Fig. 2 and Supplementary Table 2 .
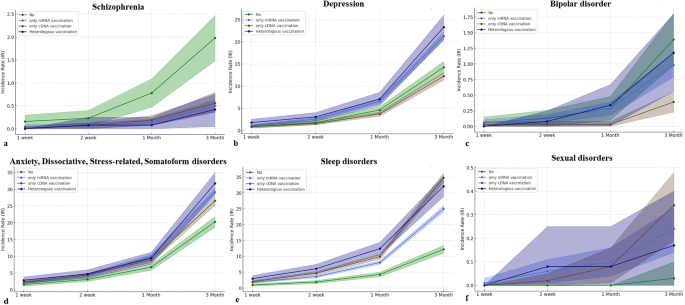
a Schizophrenia. b Depression. c Bipolar disorder. d Anxiety, dissociative, stress-related, and somatoform disorders. e Sleep disorder. f Sexual disorders.
The risks of psychiatric AEs following the COVID-19 vaccination
In the Cox proportional hazard model in this study, the HR for COVID-19 vaccination was 0.231 (95% CI, 0.164–0.326) for schizophrenia, 1.683 (95% CI, 1.520–1.863) for depression, 0.672 (95% CI, 0.470–0.962) for bipolar disorder, 1.439 (95% CI, 1.322–1.568) for anxiety, dissociative, stress-related, and somatoform disorders, 0.796 (95% CI, 0.395–1.604) for eating disorders, 1.934 (95% CI, 1.738–2.152) for sleep disorders, and 6.556 (95% CI, 0.890–48.296) for sexual disorders. Therefore, COVID-19 vaccination significantly decreased the risks of occurrence for schizophrenia and bipolar disorder, while significantly increasing the risks for depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders. There was no effect of COVID-19 vaccination on the occurrence of eating disorders and sexual disorders (Fig. 3a ).
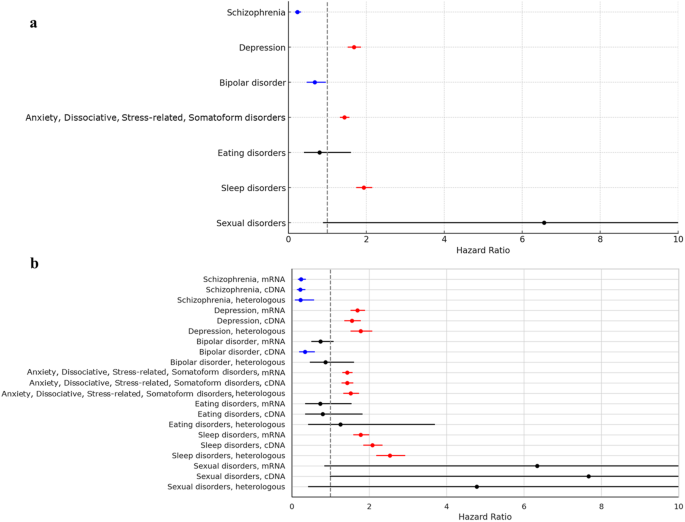
a The risks of psychiatric adverse events (AEs) according to COVID-19 vaccination. b The risks of psychiatric adverse events according to the COVID-19 vaccine types.
In the multivariate logistic model in this study, the ORs of target psychiatric AEs, except for bipolar disorder at one week, two weeks, and one month showed statistical significance, indicating similar patterns for HRs in the Cox proportional hazard model. For bipolar disorder, the OR showed 1.166 (95% CI, 0.240–5.670; p = 0.849) at one week, 0.946 (95% CI, 0.304–2.949; p = 0.924) at two weeks, 0.982 (95% CI, 0.463–2.079; p = 0.962) at one month, and 0.674 (95% CI, 0.471–0.964; p = 0.031). The detailed information for ORs of target psychiatric AEs was described in Supplementary Table 3 .
The risks of psychiatric AEs according to the COVID-19 vaccine type
We further assessed the risks of target psychiatric AEs according to the COVID-19 vaccine. For schizophrenia and bipolar disorder which were observed to have lower occurrences following COVID-19 vaccination, the HRs of schizophrenia were 0.239 (95% CI, 0.163–0.352) in only mRNA vaccination, 0.218 (95% CI, 0.138–0.343) in only cDNA vaccination, and 0.227 (95% CI, 0.091–0.566) in heterologous vaccination with statistical significances. On the other hand, the HR of bipolar disorder was statistically significant only in the case of only cDNA vaccination (0.339; 95% CI, 0.196–0.587). For depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders which were observed to have higher occurrences following COVID-19 vaccination, the HRs of depression (1.777; 95% CI, 1.527–2.067), anxiety, dissociative, stress-related, and somatoform disorders (1.521; 95% CI, 1.338–1.729), and sleep disorders (2.080; 95% CI, 1.855–2.332) showed the highest levels in the case of heterologous vaccination with statistical significances, respectively. There were no statistical differences in risks of eating disorders and sexual disorders according to vaccine types (Fig. 3b ).
The ORs of target psychiatric AEs, except for bipolar disorder at one week, two weeks, and one month also showed statistical significance, indicating similar patterns for HRs in the Cox proportional hazard model. For bipolar disorder, the OR for only cDNA vaccination showed 1.581 (95% CI, 0.172–14.496; p = 0.685) at one week, 0.459 (95% CI, 0.073–2.893; p = 0.407) at two weeks, 0.191 (95% CI, 0.039–0.939; p = 0.042) at one month, and 0.340 (95% CI, 0.197–0.589; p < 0.001). The detailed information for ORs of target psychiatric AEs according to vaccine types was described in Supplementary Table 3 .
Subgroup analysis for psychiatric AEs based on gender, age, insurance level, and CCI
As age increases, the risks of schizophrenia (HR, 1.027; 95% CI, 1.016–1.039) and sleep disorders (HR, 1.014; 95% CI, 1.012–1.016) significantly increase and the risks of depression (HR, 0.969; 95% CI, 0.966–0.971), bipolar disorder (HR, 0.982; 95% CI, 0.971–0.993), anxiety, dissociative, stress-related, somatoform disorders (HR, 0.988; 95% CI, 0.986–0.990) significantly decrease. Considering the HR values, age does not seem to largely affect the risk of psychiatric AEs. For the insurance level, the HR of schizophrenia at the high insurance level was 0.593 ( p = 0.007) with statistical differences compared to the low insurance level. The HRs of depression at the high insurance level and middle insurance level were respectively 0.904 ( p = 0.014) and 0.824 ( p < 0.001) with statistical differences. There were no statistical differences in other psychiatric disorders for the insurance levels. For CCI, a higher score of CCI more than 2 significantly increased the risks of depression (HR, 1.393; 95% CI, 1.217–1.596), anxiety, dissociative, stress-related, somatoform disorders (HR, 1.440; 95% CI, 1.306–1.587), and sleep disorders (HR, 1.315; 95% CI, 1.198–1.444) than zero score of CCI. Based on these results, women are mostly susceptible to psychiatric AEs (except for sexual disorders) compared to men. Detailed information for Cox proportional hazard model for psychiatric AEs was presented in Supplementary Table 4 .
The post-sequelae of COVID-19 and vaccine-related AEs have globally been concerns for mental illness, ranging from mild signs of mental symptoms to psychiatric disorders [ 18 ]. During the prolonged COVID-19 pandemic, there has been an emerging trend in complications of COVID-19 infection and vaccination, intensifying the psychosocial burdens [ 5 , 18 , 19 ]. Despite the considerable clinical benefits of the COVID-19 vaccination, it paradoxically made managing psychiatric disorders more challenging due to the contradictory outcomes associated with COVID-19 vaccination [ 11 , 13 , 14 , 15 , 18 , 19 , 20 , 21 ]. Here, we conducted a population-based retrospective cohort study for psychiatric AEs after COVID-19 vaccination in Seoul, South Korea. From our cohort between 1,718,999 vaccinated subjects and 308,354 non-vaccinated subjects, we found that the vaccinated subjects showed a significantly higher incidence of depression, anxiety, dissociative, stress-related, and somatoform disorders, sleep disorders, and sexual disorders and a significantly lower incidence of schizophrenia and bipolar disorder than the non-vaccinated subjects. Furthermore, COVID-19 vaccination increased risks of depression, anxiety, dissociative, stress-related, and somatoform disorders and sleep disorders but reduced risks of schizophrenia and bipolar disorder.
Some evidence between COVID-19 and mental illness has gradually grown since the most common symptoms of the long-COVID-19 pandemic were depression/anxiety, psychotic disorder, and cognitive impairment (called brain fog) experienced by 22% of patients within 6 months after COVID-19 infections [ 4 , 14 ]. However, there have been contradictory reports between mental illness and COVID-19 vaccinations. Chaudhuri et al. reported that vaccination significantly alleviated psychological distress measured by the General Health Questionnaire in the UK Household Longitudinal cohort study [ 18 ]. Meanwhile, Balasubramanian et al. reviewed the reports of psychiatric AEs to COVID-19 vaccines, which illustrated 14 cases of psychiatric reactions including psychosis, depression, and anxiety, dissociative, stress-related, and somatoform disorders [ 15 ]. To our knowledge, there are scarce studies on the association between vaccines and psychiatric AEs. Therefore, our population-based cohort study provides robust evidence for the psychiatric AEs after COVID-19 vaccinations. Furthermore, our study provided risks of psychiatric AEs according to vaccine type, revealing that the psychiatric disorders (depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders) with increased risks due to COVID-19 vaccination showed the highest risk in the case of heterogeneous vaccination. Meanwhile, occurrences of schizophrenia consistently decreased risks according to vaccine type but bipolar disorder showed significantly decreased risks from only cDNA vaccination.
Two representative mood disorders, depression, and bipolar disorders, showed contrasting trends for COVID-19 vaccination. The serotonin theory is that depression is caused by an alternation of the hypothalamic-pituitary-adrenal (HPA) axis, particularly serotonin (5-hydroxytryptamine or 5-HT) [ 22 , 23 , 24 ]. Along with this theory, the selective serotonin reuptake inhibitor is currently the main drug to treat depression [ 22 ]. Serotonin, known as a neurotransmitter, is important to immune systems as the regulator of immune responses and inflammatory processes by central and peripheral mechanisms [ 22 , 24 ]. For reports of COVID-19 vaccines, the association between adrenal crisis and COVID-19 vaccination has been suggested with the possible risk of heterologous vaccination [ 25 , 26 ] Therefore, COVID-19 may alternate the HPA axis, which can potentially increase the risk of depression from our study. In our study, HR for bipolar disorder was found to be 0.672 (95% CI, 0.470–0.962) in association with COVID-19 vaccination. However, this result was primarily caused by only cDNA vaccination with a notable lower HR of 0.339 (95% CI, 0.196–0.587). Interestingly, other types of COVID-19 vaccinations did not demonstrate a significant impact on the occurrences of bipolar disorder. These distinctive findings suggested that the differential effects along with vaccine types may be underestimated in mental illness, particularly bipolar disorder [ 12 , 27 ].
The immune response mediated by COVID-19 vaccination manifests in a variety of ways across different sites in our body [ 28 ]. Trougakos et al. described that the AEs following COVID-19 vaccination may related to the proinflammatory action of the lipid nanoparticles or the delivered mRNA and proinflammatory effects of the produced antigens-spike protein and/or its peptides fragments [ 29 ]. The COVID-19 vaccination activated proinflammatory cytokines such as interleukin (IL)-1, IL-6, and tumor necrosis factor-α mediated by CD4 + T cells [ 28 ]. Many immune-related factors have been suggested for the expression of psychosis [ 13 ]. The hyperinflammatory status can increase dopamine with N-inhibition of methyl-d-aspartate receptor (NMDAR), which leads to psychosis [ 30 ]. Furthermore, an autoimmune response caused by the spike protein and encoded viral protein in the vaccine can be a potential factor in the manifestation of schizophrenia [ 31 , 32 ]. Of many vaccination methods, Lee et al. described that the heterologous vaccination enhanced B cells and CD4 + T cell responses [ 33 ]. Proinflammatory effects can be exacerbated by preexisting inflammatory conditions after administration of mRNA lipid nanoparticles [ 29 ]. This heightened immune response may influence the occurrence of schizophrenia, as presented in our study. However, the profound pathophysiological mechanisms should be performed in future translational research [ 27 ].
Anxiety and stress-related disorders are the main concerns for COVID-19 infection and vaccination, which were widely studied from fear to vaccine hesitancy [ 34 ]. Conversion disorders, characterized by paralysis, sensory disturbances, and seizures are associated with alternation of brain function networks [ 35 ]. Our study showed increased risks of anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders, which were heightened by heterologous vaccination. Most patients who were infected with COVID-19 experienced chronic fatigue with mild cognitive impairment (i.e., brain fog) [ 21 , 35 , 36 ]. Abel et al. described that COVID-19 infection increased the risks of fatigue and sleep disorders from the UK primary care data [ 21 ]. The mechanism is thought to be caused by a decrease in cerebral blood flow, and it is similar to neuropsychiatric disorders affected by inflammatory processes and immune responses [ 37 ]. Since COVID-19 vaccination is also associated with immune responses, both clinicians and vaccinated subjects should be cautious of these manifestations, especially anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders that can also be affected by COVID-19 vaccination in our study. Therefore, the COVID-19 vaccination increases the manifestation of neurosis-related disorders but decreases that of psychosis-related disorders.
With the increasing evidence of extrapulmonary manifestations including neurological and psychiatric symptoms, COVID-19 infection as well as vaccination may affect the central and peripheral nervous system with profound cellular and molecular mechanisms [ 6 , 38 , 39 ]. The spike protein, especially brain-infiltrating SARS-CoV-2 spike protein has been suggested as an important target for the development of neurological and psychiatric disorders. Several mechanisms involved in spike protein have been proposed at the mice level such as TLR2-mediated depression, TLR4-mediated cognitive dysfunction, and anxiety mediated by non-cell autonomous hippocampal neuronal cell deaths by inducing IL-1β from glial cells [ 40 ]. Importantly, a recent study suggested that mRNA vaccines have slippery sequences inducing +1 ribosomal frameshifting products after vaccinations as a consequence of N 1 -methylpseudouridine-induced ribosome stalling [ 41 ]. Although the pathogenesis remains unclear, our study suggests that neuroinflammation caused by spike proteins may contribute to occurrences of some psychiatric AEs such as depression and anxiety, dissociative, stress-related, and somatoform disorders. Therefore, future translational research may provide the pathophysiological differences between psychosis and neurosis from the COVID-19 vaccination.
To supplement our hypothesis regarding the mechanism of action after COVID-19 vaccination, we tried further study using the gene sets enrichment analysis (Supplementary Table 5 ). We found that schizophrenia-related genes share the enrichment pathway for bile acid metabolism. Bile acids prevent the binding of spike protein with angiotensin-converting enzyme II (ACE2) and modulate the expression of ACE2, suggesting the protective role [ 42 ]. Our study also showed that COVID-19 vaccination reduced risks of schizophrenia. For depression, as an increased risk after COVID-19 vaccination, the results were shown for the deep interaction of spike protein-related factors such as NLRP3 inflammasome [ 40 ]. This supports that the presence of the spike protein plays a crucial role in the manifestation of diseases after COVID-19 vaccination. Regarding the neurosis, the Rap1 signaling was observed as an enrichment pathway in the genes of neuroticisms. It regulates MAPK pathways that are important for SARS-CoV-2 virus replication [ 43 , 44 ]. However, these findings will have to be validated by future experimental studies.
This study has several limitations. First, we collected the claims data based on ICD-19 codes, which led to potential errors regarding mismatching or misclassification could have occurred. Second, previous studies have suggested the impact of poverty rates on mental disorders but there are differences in the baseline characteristics between the two groups in this study [ 45 , 46 ]. Although propensity score matching could be a statistical option to overcome this limitation, the real-world data is scarce on the psychiatric AEs following the COVID-19 vaccination so future studies through the process of propensity score matching should be addressed for COVID-19 vaccine-related psychiatric AEs. Meanwhile, both schizophrenia and bipolar disorders often manifest at a young age (under 20 years old) [ 47 ]. However, our study protocol didn’t include the adolescent population group because our study protocol has been approved by our IRB to analyze adults more than 20 years old. Furthermore, the COVID-19 vaccination for adolescents in South Korea has been authorized since October 2021, which made it impossible to collect COVID-19 vaccine-related AEs of the population under 20 years old in our study protocol. Thus, future studies for adolescents considering the manifestation of psychiatric disorders will be needed on COVID-19 vaccine-related AEs. Third, we measured psychiatric AEs up to three months following COVID-19 vaccination. This study did not contain the long-term follow-up COVID-19 vaccine-associated AEs. Last, despite being a population-based study targeting the population in Seoul, South Korea, it cannot be generalized to the entire population, globally since psychiatric disorders could be related to ethnic and genetic backgrounds. Therefore, a global-scale real-world study for adverse events of COVID-19 vaccination will be important in the future.
In conclusion, this population-based cohort study revealed that COVID-19 vaccination differentially affects occurrences of psychiatric disorders. It increased the risks of depression, anxiety, dissociative, stress-related, and somatoform disorders, and sleep disorders while reducing the incidence and risk of schizophrenia and bipolar disorder. Our findings suggested that the relationship between COVID-19 vaccination and mental illness may be underestimated along with the complexity of its impact on mental health. Thus, close observation and special caution are necessary for administering additional COVID-19 vaccinations to populations vulnerable to psychiatric AEs.
Data availability
The datasets analyzed during the current study are available through an application to the National Health Insurance Service, South Korea. This protects the confidentiality of the data and ensures that Information Governance is robust.
Lundberg-Morris L, Leach S, Xu Y, Martikainen J, Santosa A, Gisslén M, et al. Covid-19 vaccine effectiveness against post-covid-19 condition among 589 722 individuals in Sweden: population based cohort study. Bmj. 2023;383:e076990.
Article PubMed PubMed Central Google Scholar
Lee DS, Kim JW, Lee KL, Jung YJ, Kang HW. Adverse events following COVID-19 vaccination in South Korea between February 28 and August 21, 2021: a nationwide observational study. Int J Infect Dis. 2022;118:173–82.
Article CAS PubMed PubMed Central Google Scholar
Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–24.
Jefsen OH, Kolbaek P, Gil Y, Speed M, Dinesen PT, Sonderskov KM, et al. COVID-19 vaccine willingness amongst patients with mental illness compared with the general population. Acta Neuropsychiatr. 2021;33:273–6.
Article PubMed Google Scholar
Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27:601–15.
Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26:1017–32.
Article CAS PubMed Google Scholar
Barouch DH. Covid-19 vaccines - immunity, variants, boosters. N Engl J Med. 2022;387:1011–20.
Wang W, Wang CY, Wang SI, Wei JC. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: a retrospective cohort study from the TriNetX US collaborative networks. EClinicalMedicine. 2022;53:101619.
Patone M, Handunnetthi L, Saatci D, Pan J, Katikireddi SV, Razvi S, et al. Neurological complications after first dose of COVID-19 vaccines and SARS-CoV-2 infection. Nat Med. 2021;27:2144–53.
Buchan SA, Seo CY, Johnson C, Alley S, Kwong JC, Nasreen S, et al. Epidemiology of Myocarditis and Pericarditis Following mRNA vaccination by vaccine product, schedule, and interdose interval among adolescents and adults in Ontario, Canada. JAMA Netw Open. 2022;5:e2218505.
Sun HL, Zhao YJ, Sha S, Li XH, Si TL, Liu YF, et al. Depression and anxiety among caregivers of psychiatric patients during the late stage of the COVID-19 pandemic: a perspective from network analysis. J Affect Disord. 2024;344:33–40.
Kita A, Fuyuno Y, Matsuura H, Yamaguchi Y, Okuhira K, Kimoto S. Psychiatric adverse reaction to COVID-19 vaccine booster presenting as first-episode acute mania with psychotic features: A case report. Psychiatry Res Case Rep. 2023;2:100143.
Google Scholar
Grover S, Rani S, Kohat K, Kathiravan S, Patel G, Sahoo S, et al. First episode psychosis following r eceipt of first dose of COVID-19 vaccine: a case report. Schizophr Res. 2022;241:70–1.
Harrison PJ, Taquet M. Neuropsychiatric disorders following SARS-CoV-2 infection. Brain. 2023;146:2241–7.
Balasubramanian I, Faheem A, Padhy SK, Menon V. Psychiatric adverse reactions to COVID-19 vaccines: a rapid review of published case reports. Asian J Psychiatr. 2022;71:103129.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bmj. 2007;335:806–8.
Article Google Scholar
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57:1288–94.
Chaudhuri K, Howley P. The impact of COVID-19 vaccination for mental well-being. Eur Econ Rev. 2022;150:104293.
Penninx B, Benros ME, Klein RS, Vinkers CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. 2022;28:2027–37.
Nishimi K, Neylan TC, Bertenthal D, Seal KH, O’Donovan A. Association of psychiatric disorders with incidence of SARS-CoV-2 breakthrough infection among vaccinated adults. JAMA Netw Open. 2022;5:e227287.
Abel KM, Carr MJ, Ashcroft DM, Chalder T, Chew-Graham CA, Hope H, et al. Association of SARS-CoV-2 Infection With Psychological distress, psychotropic prescribing, fatigue, and sleep problems among UK primary care patients. JAMA Netw Open. 2021;4:e2134803.
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, et al. Major depressive disorder. Nat Rev Dis Primers. 2016;2:16065.
Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Primers. 2018;4:18008.
Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry. 2023;28:3243–56.
Maguire D, McLaren DS, Rasool I, Shah PM, Lynch J, Murray RD. ChAdOx1 SARS-CoV-2 vaccination: a putative precipitant of adrenal crises. Clin Endocrinol. 2023;99:470–3.
Article CAS Google Scholar
Markovic N, Faizan A, Boradia C, Nambi S. Adrenal crisis secondary to COVID-19 vaccination in a patient with hypopituitarism. AACE Clin Case Rep. 2022;8:171–3.
Cozzolino A, Hasenmajer V, Newell-Price J, Isidori AM. COVID-19 pandemic and adrenals: deep insights and implications in patients with glucocorticoid disorders. Endocrine. 2023;82:1–14.
Li C, Lee A, Grigoryan L, Arunachalam PS, Scott MKD, Trisal M, et al. Mechanisms of innate and adaptive immunity to the Pfizer-BioNTech BNT162b2 vaccine. Nat Immunol. 2022;23:543–55.
Trougakos IP, Terpos E, Alexopoulos H, Politou M, Paraskevis D, Scorilas A, et al. Adverse effects of COVID-19 mRNA vaccines: the spike hypothesis. Trends Mol Med. 2022;28:542–54.
Tang SW, Helmeste D, Leonard B. Inflammatory neuropsychiatric disorders and COVID-19 neuroinflammation. Acta Neuropsychiatrica. 2021;33:165–77.
Yonker LM, Swank Z, Bartsch YC, Burns MD, Kane A, Boribong BP, et al. Circulating spike protein detected in Post-COVID-19 mRNA vaccine myocarditis. Circulation. 2023;147:867–76.
Yesilkaya UH, Sen M, Tasdemir BG. A novel adverse effect of the BNT162b2 mRNA vaccine: first episode of acute mania with psychotic features. Brain Behav Immun Health. 2021;18:100363.
Lee HK, Go J, Sung H, Kim SW, Walter M, Knabl L, et al. Heterologous ChAdOx1-BNT162b2 vaccination in Korean cohort induces robust immune and antibody responses that includes Omicron. iScience. 2022;25:104473.
McNeil A, Purdon C. Anxiety disorders, COVID-19 fear, and vaccine hesitancy. J Anxiety Disord. 2022;90:102598.
Espay AJ, Aybek S, Carson A, Edwards MJ, Goldstein LH, Hallett M, et al. Current concepts in diagnosis and treatment of functional neurological disorders. JAMA Neurol. 2018;75:1132–41.
Morin CM, Drake CL, Harvey AG, Krystal AD, Manber R, Riemann D, et al. Insomnia disorder. Nat Rev Dis Primers. 2015;1:15026.
Theoharides TC, Stewart JM, Hatziagelaki E, Kolaitis G. Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front Neurosci. 2015;9:225.
Khayat-Khoei M, Bhattacharyya S, Katz J, Harrison D, Tauhid S, Bruso P, et al. COVID-19 mRNA vaccination leading to CNS inflammation: a case series. J Neurol. 2022;269:1093–106.
Theoharides TC. Could SARS-CoV-2 spike protein be responsible for long-COVID syndrome? Mol Neurobiol. 2022;59:1850–61.
Fontes-Dantas FL, Fernandes GG, Gutman EG, De Lima EV, Antonio LS, Hammerle MB, et al. SARS-CoV-2 Spike protein induces TLR4-mediated long-term cognitive dysfunction recapitulating post-COVID-19 syndrome in mice. Cell Rep. 2023;42:112189.
Mulroney TE, Pöyry T, Yam-Puc JC, Rust M, Harvey RF, Kalmar L, et al. N 1 -methylpseudouridylation of mRNA causes +1 ribosomal frameshifting. Nature. 2024;625:189–94.
Fiorucci S, Urbani G, Biagioli M, Sepe V, Distrutti E, Zampella A. Bile acids and bile acid activated receptors in the treatment of Covid-19. Biochem Pharmacol. 2023;115983. https://doi.org/10.1016/j.bcp.2023.115983 .
Zhang YL, Wang RC, Cheng K, Ring BZ, Su L. Roles of Rap1 signaling in tumor cell migration and invasion. Cancer Biol Med. 2017;14:90–9.
Hadzega D, Babisova K, Hyblova M, Janostiakova N, Sabaka P, Janega P, et al. Analysis of transcriptomics data from COVID-19 patients: a pilot research. Folia Microbiol. 2024;69:155–64.
Das-Munshi J, Chang CK, Bakolis I, Broadbent M, Dregan A, Hotopf M, et al. All-cause and cause-specific mortality in people with mental disorders and intellectual disabilities, before and during the COVID-19 pandemic: cohort study. Lancet Reg Health Eur. 2021;11:100228.
Bennett JE, Pearson-Stuttard J, Kontis V, Capewell S, Wolfe I, Ezzati M. Contributions of diseases and injuries to widening life expectancy inequalities in England from 2001 to 2016: a population-based analysis of vital registration data. Lancet Public Health. 2018;3:e586–97.
Ortiz-Orendain J, Gardea-Resendez M, Castiello-de Obeso S, Golebiowski R, Coombes B, Gruhlke PM, et al. Antecedents to first episode psychosis and mania: comparing the initial prodromes of schizophrenia and bipolar disorder in a retrospective population cohort. J Affect Disord. 2023;340:25–32.
Download references
Author information
Authors and affiliations.
Department of Orthopedic Surgery, Inje University Sanggye Paik Hospital, College of Medicine, Inje University, Seoul, Republic of Korea
Hong Jin Kim
Informatization Department, Ewha Womans University Seoul Hospital, Seoul, Republic of Korea
Division of Pulmonology and Critical Care Medicine, Department of Internal Medicine, School of Medicine, Ewha Womans University, Seoul, Republic of Korea
Myeong Geun Choi & Eun Mi Chun
You can also search for this author in PubMed Google Scholar
Contributions
EMC conceptualized the study. HJK, M-HK, and EMC designed the study. HJK, M-HK, and EMC analyzed and interpreted the data. M-HK acquired the data. HJK and EMC drafted the manuscript. HJK, M-HK, MGC, and EMC critically reviewed the work. MGC verified the data in the study. All authors had full access to all the data and had final responsibility for the decision to submit for publication.
Corresponding author
Correspondence to Eun Mi Chun .
Ethics declarations
Competing interests.
The authors declare no competing interests.
The study protocol was approved by the Institutional Review Board of our institute (IRB No.: EUMC 2022-07-003), which waived the requirement for informed consent because data analyses were performed retrospectively using anonymized data derived from the South Korean NHIS database.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary tables, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Kim, H.J., Kim, MH., Choi, M.G. et al. Psychiatric adverse events following COVID-19 vaccination: a population-based cohort study in Seoul, South Korea. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02627-0
Download citation
Received : 09 January 2024
Revised : 22 May 2024
Accepted : 24 May 2024
Published : 04 June 2024
DOI : https://doi.org/10.1038/s41380-024-02627-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 2
- Recovery from recurrent depression with mindfulness-based cognitive therapy and antidepressants: a qualitative study with illustrative case studies
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Alice Tickell 1 ,
- Richard Byng 2 ,
- Catherine Crane 1 ,
- Felix Gradinger 2 ,
- Rachel Hayes 1 ,
- James Robson 3 ,
- Jessica Cardy 1 ,
- Alice Weaver 1 ,
- http://orcid.org/0000-0003-4022-8133 Nicola Morant 4 ,
- http://orcid.org/0000-0002-8596-5252 Willem Kuyken 1
- 1 Department of Psychiatry , University of Oxford , Oxford , UK
- 2 Peninsula Medical School, Faculty of Health , University of Plymouth , Plymouth , UK
- 3 Department of Education , University of Oxford , Oxford , UK
- 4 Department of Psychiatry , University College London , London , UK
- Correspondence to Dr Willem Kuyken; willem.kuyken{at}psych.ox.ac.uk
Objectives This study aimed to describe the recovery journeys of people with a history of recurrent depression who took part in a psychosocial programme designed to teach skills to prevent depressive relapse (mindfulness-based cognitive therapy (MBCT)), alongside maintenance antidepressant medication (ADM).
Design A qualitative study embedded within a multicentre, single blind, randomised controlled trial (the PREVENT trial).
Setting Primary care urban and rural settings in the UK.
Participants 42 people who participated in the MBCT arm of the parent trial were purposively sampled to represent a range of recovery journeys.
Interventions MBCT involves eight weekly group sessions, with four refresher sessions offered in the year following the end of the programme. It was adapted to offer bespoke support around ADM tapering and discontinuation.
Methods Written feedback and structured in-depth interviews were collected in the 2 years after participants undertook MBCT. Data were analysed using thematic analysis and case studies constructed to illustrate the findings.
Results People with recurrent depression have unique recovery journeys that shape and are shaped by their pharmacological and psychological treatment choices. Their journeys typically include several over-arching themes: (1) beliefs about the causes of depression, both biological and psychosocial; (2) personal agency, including expectations about their role in recovery and treatment; (3) acceptance, both of depression itself and the recovery journey; (4) quality of life; (5) experiences and perspectives on ADM and ADM tapering-discontinuation; and (6) the role of general practitioners, both positive and negative.
Conclusions People with recurrent depression describe unique, complex recovery journeys shaped by their experiences of depression, treatment and interactions with health professionals. Understanding how several themes coalesce for each individual can both support their recovery and treatment choices as well as health professionals in providing more accessible, collaborative, individualised and empowering care.
Trial registration number Clinical trial number ISRCTN26666654 ; post results.
- depression & mood disorders
- psychological therapy
- antidepressants
This is an open access article distributed in accordance with the Creative Commons Attribution 4.0 Unported (CC BY 4.0) license, which permits others to copy, redistribute, remix, transform and build upon this work for any purpose, provided the original work is properly cited, a link to the licence is given, and indication of whether changes were made. See: https://creativecommons.org/licenses/by/4.0/ .
https://doi.org/10.1136/bmjopen-2019-033892
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
Recurrent depression is a leading cause of disability adjusted life years and antidepressant medication (ADM) is the mainstay approach to treatment; this study is the first to describe people’s experiences of recovery with an ADM alongside a psychosocial approach designed to support recovery (mindfulness-based cognitive therapy (MBCT)).
The sample was relatively large and purposively sampled to illustrate a range of recovery journeys and outcomes.
Participants experiences in the 2 years following MBCT were sampled, using an innovative approach to supporting participants’ to describe the richness of their experiences of recovery and treatment.
The sampling necessarily meant that we did not include people with a history of recurrent depression who had decided against ADM, tapering and discontinuing their ADM and/or a psychological approach.
Depression is a major public health problem. Globally more than 264 million people suffer from depression, and lifetime prevalence rates are estimated to be between 6% and 20%. 1 2 Furthermore, depression can be a relapsing and recurring condition, and on average people who experience one episode of depression have seven or eight episodes over their lifetime. 3 Clinical guidance typically recommends that people with recurrent depression should take maintenance antidepressant medications (ADMs) after remission or engage in preventive psychological interventions to maintain recovery. 4 For people with recurrent depression, their recovery journey is shaped by their experiences of depression, ‘illness model’, interactions with mental health professionals, treatments that have and have not worked and expectations about what recovery will entail. 5 For many, ADMs are an important part of their recovery. Reasons for long-term ADM use include positive experiences of ADMs, fear of relapse, perceived lack of alternatives and concerns about withdrawal effects. 6 On the other hand, people also describe a number of reasons for wanting to discontinue ADMs, including feeling better and wanting to test whether depression has gone away, ambivalence and uncertainty about the role of ADMs in recovery, side effects outweighing benefits, questioning whether the self on ADMs is the ‘real self’, and wanting to assert control over their well-being. 7
Research and clinical guidelines suggests that psychological therapies, such as mindfulness-based cognitive therapy (MBCT) and cognitive-behavioural therapy (CBT), can support recovery from depression as well as support discontinuing ADMs. 4 8–10 A significant proportion of people express a preference for psychological therapies, so they can learn strategies that support recovery without the need for long-term reliance on ADMs. 11 But psychological therapies can be difficult to access, involve significant investment of time and energy and are not effective for everyone. 12
While studies have examined people’s experiences of ADM and MBCT in recovery, none have focused primarily on how they operate alongside one another. This study explores how people with a history of recurrent depression describe their experience of using MBCT and ADM to support their recovery, drawing on both written feedback booklets and more in-depth interviews. It was embedded within a randomised controlled trial (RCT) comparing MBCT with support to taper and discontinue ADMs (henceforth MBCT-TS) and maintenance antidepressants over a 2-year period. 13 These findings could inform decision-making between general practitioners (GPs) and patients about the journey of management and recovery from recurrent depression.
Study context
This qualitative process evaluation was embedded within a randomized controlled trial comparing mindfulness-based cognitive therapy with maintenance anti-depressant treatment in the prevention of depressive relapse/recurrence (the PREVENT trial). This was a multicentre, single blind, parallel RCT, which investigated whether MBCT-TS (n=212) was superior to maintenance ADMs (n=212) for the prevention of depressive relapse or recurrence over 24 months (trial design is described by Kuyken et al ). 13–16 The trial found that MBCT-TS was not superior to maintenance ADM in preventing depressive relapse over 2 years; however, a subsequent individual patient data meta-analysis which included this data suggests MBCT as an alternative to maintenance ADMs. 8 We present a statement concerning reflexivity in the online supplementary materials, which outlines the experience and background of the authors, to acknowledge our theoretical positions and values in relation to this study (see online supplementary 1 ). 17 We also include the consolidated criteria for reporting qualitative research (COREQ) checklist to match our procedures against standard criteria for qualitative research (see online supplementary 2 ).
Supplemental material
Participants.
Participants in the PREVENT trial were recruited from 95 general practices in urban and rural settings in four UK centres, in addition to self-referral. 13 Inclusion criteria were a diagnosis of recurrent major depressive disorder in full or partial remission according to the Diagnostic and Statistical Manual of Mental Disorders-IV 18 ; three or more previous major depressive episodes; age 18 years or older; and on a therapeutic dose of maintenance antidepressant drugs in line with the British National Formulary and NICE (National Institute for Health and Care Excellence) guidance. 4 Exclusion criteria were a current major depressive episode, comorbid diagnoses of current substance misuse; organic brain damage; current or past psychosis, including bipolar disorder; persistent antisocial behaviour; persistent self-injury needing clinical management or therapy; and formal concurrent psychotherapy. All participants gave informed consent before participating in the trial. The full process of recruitment for the PREVENT trial is described in Kuyken et al. 16
This study examined a sub-group of participants from the PREVENT trial (n=42) allocated to the MBCT-TS arm of the trial. Of the 212 participants allocated to receive MBCT-TS, 176 received an adequate dose of treatment (attended four or more group sessions of therapy). 13 The researchers purposively sampled a sub-group of these participants (n=46) to represent a spread of characteristics and experiences with respect to: whether they reported their childhood as having higher or lower levels of abuse, treatment response (relapse/no relapse to a major depressive episode), and ADM discontinuation profile across the 24-month follow-up period (discontinued ADMs, discontinued ADMs but subsequently resumed them, tapered ADMs but never fully discontinued, never tapered or discontinued ADMs). 13 Of the 46 people invited to interview, 42 agreed, which comprised the final sample. Of the four who declined, two had moved away from the area, one was not interested in participating and one participant had changed their contact details and could not be reached. Interviewees did not differ in either baseline characteristics or trial outcomes from the broader study sample (see table 1 ).
- View inline
Characteristics of the sample
MBCT-TS intervention
MBCT-TS comprised MBCT delivered in line with the published treatment manual, 19 but adapted to include a greater focus on developing a relapse/recurrence signature and response plan that explicitly included participants’ reduction/discontinuation of ADM (see Kuyken et al 16 for more detail). The programme involved eight 2¼-hour group sessions, normally over consecutive weeks, with up to four refresher sessions offered in the year following the end of the 8-week programme. Researchers encouraged participants in the MBCT-TS arm to taper and discontinue their maintenance ADMs at several points from the middle of the MBCT-TS course onwards, and provided information to GPs and participants about typical tapering/discontinuation regimes and possible withdrawal effects. If participants experienced a relapse/recurrence during the course of the trial, researchers encouraged them to discuss the most appropriate treatment with their GP and made no further requests that they consider tapering/discontinuing their ADMs.
Qualitative data collection
We used both written feedback booklets (collected at two time points, soon after MBCT and then at study end) and interviews (at study end) to gather participants’ more in-depth experiences of recovery. We combined each participant’s interview and written feedback booklet data to form a single account of their experiences. This formed the study’s data corpus.
Written feedback booklets
One month after completing MBCT-TS all trial participants were invited to complete a feedback booklet addressing attitudes towards, and experiences of, taking and reducing antidepressant medication; experiences of taking part in MBCT-TS and MBCT-TS practices; and the impact of MBCT. In addition to the earlier points, participants received a further feedback booklet 24 months later, which asked the same questions as the first booklet but also included questions focused on participants’ experiences in the follow-up period and basic data on the amount and type of mindfulness practice. The booklets are provided in the online supplementary materials (see online supplementary 3 and 4 ).
Interviews were semi-structured and normally conducted face-to-face by trained researchers, approximately 24 months after MBCT-TS. They lasted between 45 min and 1 hour and explored experiences during the follow-up period, with questions addressing times of wellness, early signs of potential depressive relapse and relapses. Questions explored the use and perceived value of mindfulness techniques, use of ADMs and their combination. We tailored interviews to the specific profile of each participant using a ‘timeline’ prepared in advance and amended by the participant at the interview, which summarised each participant’s ADM use, relapses and significant life events, as reported to the research team during the trial. The interview schedule was deliberately broad in focus (see online supplementary 5 ). Interviews were recorded and transcribed for analysis.
Public and patient involvement
The PREVENT trial benefited from the expertise of many people with lived experience of mental health difficulties including a number of members of a locally organised voluntary group called the lived experience group (LEG). The LEG assisted the PREVENT trial at every stage of its development including both the interview schedule and written feedback booklets. There were reviewed and then trialled by several members of the LEG who suggested a number of fundamental changes. A member of the LEG also provided specific training to the research staff on conducting interviews.
Data analyses
We used thematic analysis as our analytic approach. 17 First, we selected eight participants with a range of ADM discontinuation journeys during the trial period: two who had discontinued ADMs and remained ADM-free; two who had discontinued ADMs and subsequently resumed; two who had never tapered or discontinued ADMs; and two who had tapered but never discontinued ADMs. Four researchers (AT, CC, JR and WK) independently analysed the interview transcripts and accompanying 1-month and 24-month feedback booklets for each participant. In this phase, we conducted inductive analysis, with each researcher developing a preliminary coding frame. These frames were then integrated through discussion to remove redundancies and ensure breadth. This collaboratively produced, inductive coding frame was then combined with deductive codes developed from key literature on participant experiences of MBCT, 20 21 and ADM use, 7 22 to establish a working coding frame.
The lead researcher (AT) then analysed the 42 interviews and accompanying booklets against this coding frame, using NVivo V.11 software. AT, CC and JR met at regular intervals to discuss additional emerging codes and arising themes and, if deemed appropriate, integrated these into the coding frame. Midway through coding, AT sought peer feedback on emerging themes from co-authors, at an internal research meeting and at a symposium focused on antidepressant tapering at an international conference (Tickell, 2018). Feedback from these presentations helped clarify which themes were particularly important, and in particular helped the researchers reflect on those that related specifically to participants’ experiences of ADM alongside MBCT-TS. Once the data were fully coded, the researchers reviewed the themes in the light of the core research question. These were discussed with the wider authorship group, whose input was used to reduce redundancy across themes, and highlight their interactions. Peer review of an earlier version of this manuscript also led to further refining the questions and themes. Finally, we identified cases that illustrated the unique stories of recovery and the ways the common themes coalesced in different ways in illustrative case studies.
The thematic analysis yielded six over-arching themes, each with a number of constituent sub-themes. We provide a summary ( table 2 ) and narrative account of each theme and its constituent sub-themes, illustrating these with extracts from participants’ accounts. While each person’s experience of MBCT and ADMs was unique, these themes converged in complex ways within individual case. Five case examples illustrate these different recovery journeys ( box 1 ).
Themes and sub-themes
Case examples
Mandy . Mandy, aged 57, experienced nine episodes of depression, beginning when she was 32. Following the mindfulness-based cognitive therapy with support to taper and discontinue ADMs (MBCT-TS) course Mandy successfully discontinued her antidepressant medication (ADM) treatment. She did not experience a relapse over the 24-month follow-up period .
Mandy recalled how ADMs had helped her to function well. In the past, she had tried tapering, but had always relapsed, so assumed that ADMs would be a part of her life forever. At first, Mandy was nervous, but was willing to try tapering ADMs gradually and with the support of MBCT-TS ( Personal Agency: Control Over Depression ). Mandy’s GP was supportive, but reassured her that it was ultimately her decision ( Interactions with GP: Presence and Support ). During the MBCT-TS course, Mandy said that she learned a different model of depression and developed a better understanding of ‘how the mind works’ ( Beliefs about the Causes of Depression: Learning a Psychological Model ). She felt more confident about tapering, and said that this time it was ‘so easy, knowing that I have been given tools to help me through it if needed’, and found the course ‘totally liberating’ as it gave her the chance to take control of her depression, rather than the other way round ( Personal Agency: Responsibility ). She also found it helpful to learn about the possible symptoms of withdrawal, which included mood swings. Mandy realised that the relapses she had experienced when she had tried to taper her ADMs in the past might have been withdrawal symptoms, as opposed to ‘real relapses’ ( ADM Tapering / Discontinuation: Managing Withdrawal Effects ). At the time of interview, having discontinued ADMs, Mandy still practised what she learned in MBCT-TS and made it part of her daily routine. She accepted that if she ever relapsed, she could use ADMs, but it would only ever be a short-term solution, because she has the MBCT-TS skills as a ‘weapon’ to help her manage ( Acceptance: Self-Care ).
Greta . Greta, aged 72, had experienced three episodes of depression, beginning when she was 33. Following the MBCT-TS course she discontinued her ADMs but then resumed following a deterioration in mood .
Greta was very optimistic about the course because she hated being on ADMs, which gave her unpleasant side effects that interfered with her quality of life ( Personal Agency: Control over Depression ). At first, Greta said the course made an ‘immense difference’ to her, and she described learning how to combat the negative thoughts and feelings she was having ( Beliefs about the Causes of Depression: Learning a Psychological Model ). The programme left Greta feeling ‘so well and positive’ that she decided to taper her ADMs very quickly ( ADM Tapering/Discontinuation: Pace of Reduction ), but began to feel her mood dipping. Greta thought this must be a sign that the programme was not working, because she should not feel depressed ( Acceptance: Perspectives on Relapse ). Greta went to her GP, who did not seem interested in the programme and told her to resume ADMs immediately ( Interactions with GP: Presence and Support ). She was disappointed and felt ‘guilty’ that she was not able to use these new skills to keep herself well ( Personal Agency: Responsibility ). She stopped practising mindfulness, although the programme made her remember to appreciate the high points in her day and experience more joy ( Quality of Life: From Coping to Enjoying Life ).
Annie . Annie, aged 48, had experienced five episodes of depression, beginning when she was 23. Following the MBCT-TS programme, she discontinued her ADMs but then resumed them later .
Annie felt that ADMs had a positive impact on her life, allowing her to cope day-to-day as a full-time carer for her husband who had a disability. At first, she was very reluctant to try discontinuing ADMs because she believed she might have low levels of serotonin ( Beliefs about the Causes of Depression: Neurochemical Disruption ). However, the programme taught her a new model of understanding depression ( Beliefs about the Causes of Depression: Learning a Psychological Model ), which made her feel empowered to practice the psychological techniques ( Personal Agency: Responsibility ). She started to taper off ADMs, but then her mother died and her husband’s health deteriorated, so it was difficult to find time to practice mindfulness. Her GP advised her it was probably not a good time to discontinue ( Interactions with GP: Presence and Support ), so she resumed ADMs. However, Annie still incorporated the mindfulness exercises into her everyday life, which brought her more joy ( Quality of Life: Experiencing Emotions More Fully ). She also recognised that it is not her fault when she felt depressed, given how challenging her life was ( Acceptance: Resolving Shame ). Annie felt that the best way to manage her depression was to combine ADMs with mindfulness practices, which gave her more skills to look after herself during difficult times ( Acceptance: Self-Care ). She felt hopeful that 1 day she would discontinue ADMs, when her life circumstances were more stable.
George . George, aged 37, had experienced ten episodes of depression, beginning when he was 16. Following the MBCT-TS programme he discontinued his ADMs. He experienced a relapse to depression during the 24-month follow-up .
George was very optimistic about trying an alternative to ADMs, because they made him feel like a ‘zombie’. Having experienced substance misuse issues in the past George had the goal of being totally ‘chemical free’. Before the course, George felt he had no control over his depression symptoms, and his mood would deteriorate suddenly without warning ( Personal Agency: Control ). Through practising the mindfulness skills, he described developing more awareness of his emotions and felt he would have the skills to manage them ( Personal Agency: Responsibility ). George said that the best part of taking part in MBCT-TS was meeting other people with depression, which made him feel more accepting of himself ( Acceptance: Resolving Shame ). He felt that ADMs had masked his symptoms, whereas MBCT-TS allowed him to explore the problems in his life that were contributing to depression and work through them to make long-term changes ( Personal Agency: Responsibility ). When George relapsed shortly after discontinuing ADMs, he carried on practising MBCT-TS and said that the skills he learned were enough to pull him out of that period of low mood ( Acceptance: Perspectives on Relapse ).
Claire . Claire, aged 49, had experienced four episodes of depression, beginning when she was 17. Following the MBCT-TS programme, Claire discontinued her ADMs. She relapsed and resumed medication, but subsequently tapered and discontinued again, and was not using ADMs at the time of her follow-up interview .
At first, Claire was very sceptical about the MBCT-TS programme and thought it might all be ‘mumbo jumbo’. However, she was very keen to come off ADMs, so she approached the programme with an open mind and wanted to give it her all ( Personal Agency: Control ). As the course progressed, Claire changed her mind and began to ‘believe more and more that this might help me’. MBCT-TS gave her new ways to cope with her feelings, which shocked her because she ‘had never took control of my depression before’ ( Personal Agency: Responsibility ). She became very excited and tapered off her medication ‘too quickly’ and ‘hit a brick wall in a short amount of time. Went straight back in to a deep depression’ ( ADM Tapering/Discontinuation: Pace of Reduction ). Her doctor was very understanding, and did not push her to do anything, but advised her to go back on ADMs and try to taper off again when she was feeling better ( Interactions with GP: Presence and Support ). He said that she should try tapering them more slowly next time even though she ‘wanted to get off them as soon as possible’. This time, she did ‘exactly as she was told’ and did not experience a relapse ( Interactions with GP: Following Advice ). Claire was very pleased because she said they had always felt that ADMs had ‘suppressed’ her and that the person she was when taking ADMs ‘wasn’t really me’ ( Quality of Life: Experiencing Emotions More Fully ).
Beliefs about the causes and treatment of depression
This over-arching theme describes participants’ beliefs about the causes of depression and how these beliefs influence their treatment decisions. This theme comprises three sub-themes.
Neurochemical disruption
Many participants described entering the study believing that their recurrent depression was due to a neurochemical disruption in their brain, often citing specifically a deficiency or imbalance of the neurotransmitter serotonin. Participants viewed medication as a way to correct this issue and made parallels to biomedical disorders, viewing ADMs as a ‘physiological need’ in the same way that ‘diabetics require insulin’ because ‘there is some chemical missing ’ (2102; Written feedback, Never tapered or discontinued ). For instance, Annie explained that she went on ADMs because her doctor told her that she had lower levels of serotonin than other people (see box 1 ). This belief appeared to influence expectations about psychological therapy, as some participants stated that they did not understand how ‘mindfulness would be able to counteract depression […] if it’s generated by a chemical imbalance’ (1031, Interview, Never tapered or discontinued ). Other people said that they had not given much thought to why they were depressed or how ADMs worked: ‘Happy pills […] I've never really given it a great deal of thought exactly what they do to be honest. […] I just know I don't feel so bad with them’ (2123, Interview, Tapered but never discontinued ).
Learning a psychological model
Participants described how their views on the causes of depression evolved during and following the MBCT-TS programme. Despite some of the initial reservations described earlier, participants described an open mind as key to engaging with the new psychological model, in which their thoughts, behaviours and emotions played a role in depressive relapses and recurrences: ‘in the first sessions […] I switched from being highly sceptical to very interested very quickly’ (1203, Interview, Discontinued ). Some participants articulated a move away from ‘treating depression as a disease, like if you had a toothache, so you took pills’, and were surprised because they ‘hadn’t thought that there was an alternative’ (1069, Interview, Discontinued ). They began to feel confident to discontinue ADMs with the support of psychological therapy. In addition, people described how the programme gave them more awareness of how external factors, such as relationships or financial situations, could trigger or exacerbate depressive relapses and recurrences. On the other hand, some participants found it more difficult to engage in the programme and found themselves ‘rebelling against it’ because they did not have ‘intellectual confidence in the process’ (3105; Written feedback, Never tapered or discontinued ). People described how their initial treatment experiences influenced their attitudes: those who felt that the techniques were helping them to manage depressive relapse/recurrence often endorsed the psychological model. On the other hand, others who experienced deterioration in mood or relapse sometimes reported that they had reconsidered bio-medical explanations, and decided to resume or remain on ADMs: ‘I really thought depression was a psychosomatic problem, but I am not so sure now. I did give it my best shot, using the mindful techniques, but I still fell into the pit of despair […] I feel that my depression is caused by a chemical imbalance in my body which, at present, is only helped by taking medication’ (2200; Written feedback, Tapered but never discontinued ).
Integrating models
Although some participants viewed depression as either biomedical or psychological, many did not see the two models as distinct and found ways to integrate them. For instance, they conceptualised that ‘antidepressants hold onto the chemical in your body ‘cause you’re not making enough of it yourself’, while MBCT-TS allows you to ‘focus your mind onto how to make your own’ (1139, Interview, Never tapered or discontinued ). It seemed that participants who viewed these models as compatible were more open to using ADMs and using psychological techniques as an additional way to support their recovery, rather than viewing them as competing treatments. Furthermore, when participants observed the diversity of other people’s experiences on the programme, some formed the opinion that there are ‘all sorts of depressions’ underpinned by different causes ‘just as there are colds and flu's and viruses’ (3105, Interview, Never tapered or discontinued ). As such, some reasoned that different people would require different treatment decisions to support recovery: ‘My depression is not necessarily the same as other people’s […] The right combination of changing lifestyle, specific therapies, medication whatever else it takes – that seems to be different for different people’ (3109, Interview, Never tapered or discontinued ).
Personal agency
This over-arching theme describes people’s personal agency in their recovery and consequently their treatment choices. People described entering the study fearful about ADM discontinuation, but were hopeful that a psychological programme could support them. During MBCT-TS, people spoke about feeling better able to manage their vulnerability to depressive relapse, by using the skills and techniques they learned on the programme. While these enhanced feelings of personal agency were largely viewed as a positive and increased many people’s confidence to taper and discontinue ADMs, this was not always the case. For some having more responsibility to manage their condition created a sense of unhelpful pressure. This theme comprises two sub-themes.
Control over depression
People described how their treatment choices affected their sense of control over depression. Some felt that taking ADMs provided a sense of control, as it kept their mood on an even keel. However, this sense of control was contingent on taking ADMs, so many participants recalled how before the trial they would not consider discontinuing because they were afraid that depression would return. Through MBCT, some participants described a change in their sense of personal agency in their recovery, describing a shift from being a ‘helpless victim of circumstance’, to having more ‘control of my feelings and my life’ (1123; Written feedback, Tapered but never discontinued ). They reported increased awareness to recognise the early warning signs of depressive relapse and take steps to respond by applying mindfulness or cognitive-behavioural techniques from a ‘toolbox’, including things like meditation, activity scheduling or enlisting social support: ‘Before the trial, I didn’t have the tools to recognise what was happening. […] I didn’t even know I was getting depressed. [Now] if things are difficult I can do something about it’ (1203, Interview, Discontinued ). Learning these new skills reduced many people’s fears about coming off ADMs, because they felt they had the capacity to prevent or contain depressive relapses. For instance, George said that before the course, he would fall into depressive episodes very suddenly and without warning, whereas the skills learned in MBCT-TS gave him more awareness and control to act and prevent relapses before they occurred (see box 1 ).
Responsibility
Participants also articulated that learning how they could have more agency over their thoughts, feelings, and behaviours led to an increased sense of responsibility to manage their well-being. Most participants viewed this as positive, especially if they were able to use the techniques to manage relapse/recurrence. Some people said they preferred MBCT-TS to taking ADMs because it made recovery feel more like a personal achievement: ‘Once I’ve fallen and I realise that I am depressed, I take myself off and say, do 3 or 4 meditations a day. […] Which to me is better than taking a pill, because I know I’ve worked to get myself well’ (2016, Interview; Written feedback, Discontinued ).
However, not all participants viewed having more agency and responsibility over their well-being positively. In particular, some participants described how this made them feel like it was their fault if they relapsed or felt they had to resume ADMs: ‘I feel sad and disappointed that stopping [ADMs] made me feel low again. […] It makes me feel I'm not right in the head compared to others. I also feel annoyed with myself for not utilising MBCT skills learnt better’ (2123; Written feedback, Discontinued and resumed ). Furthermore, a substantial number of participants expressed the challenge of finding the time, motivation or self-discipline to keep up a regular mindfulness practice outside of the group sessions. Therefore, the sense of control did not always feel stable, as it was contingent on finding time to practice and ‘do it religiously, otherwise I would be fearful of it not being enough’ (2102; Written feedback, Never tapered or discontinued ). Some were disappointed when they realised that psychological therapy was not an ‘all-encompassing cure’ (1222, Interview, Discontinued and resumed ) and would involve an active and ongoing process of engagement with the techniques learned.
This over-arching theme describes people’s feelings of acceptance towards their history of recurrent depression and ongoing need to manage risk of relapse and recurrence. People reported feeling a sense of shame around long-term reliance on ADMs before the trial, feeling it labelled them as an ill person even if feeling well. After the trial, people described an increased sense of acceptance regarding their vulnerability to depression and an increased motivation to engage in self-care to support their recovery. This self-management included either ADMs and/or the psychological techniques for different people. This theme comprises three sub-themes.
Resolving shame
Many participants recalled that before the trial they had felt ‘inadequate’ or unable to cope with life compared with other people because of their recurrent depression treating it as a ‘guilty secret’ (1123; Interview, Tapered but never discontinued ). Taking ADMs had helped some people by reducing the symptoms and allowing them to return to feeling like a ‘normal contributing person in society’ (2200; Interview, Tapered but never discontinued ). However, others said that having to take ADMs on an ongoing basis gave them an underlying feeling that they were still ‘not a well person’ (2102; Interviews, Never tapered or discontinued ), even when the symptoms of depression were absent. For these reasons, some people recalled how before the trial, they found it difficult to name their depression, and ‘couldn’t even or wouldn’t even admit to that’ (1031, Interview, Never tapered or discontinued ). Through MBCT-TS, some participants described how they felt able to name their condition as depression for the first time. They discussed how meeting other people in the programme had made them realise that depression was not a negative aspect of their own self-identity, but an aspect of human experience: ‘You realise it is part of the human condition rather than you’ (1128; Interview, Never tapered or discontinued ), and it ‘confirmed that I am a human, worthwhile person’ (2176; Written feedback, Discontinued and resumed ). This led to increased feelings of acceptance towards depression, because participants experienced a shift away from viewing themselves as abnormal, to seeing depression as a more acceptable response to life’s difficulties: ‘Giving yourself credit […] ‘cause at the end of the day […] our human brain is quite a complex thing, isn’t it? […] There’s nothing wrong in feeling like it’ (2140; Interview, Discontinued and resumed ).
Participants described how developing more acceptance towards their condition improved their attitudes towards self-care. They said that accepting their vulnerability to depression allowed them to ‘look at solutions’ and that they finally had ‘consent to actually do something about it’ (1031, Interview, Never tapered or discontinued ). People described how they increasingly accepted that they needed to take care of themselves, and explained how the programme had taught them legitimate ways to do this such as using mindfulness practices: ‘Previously was a mindset […] that I wasn’t allowed to help myself feel better. […] Whereas this felt a way that I could do it without mollycoddling myself’ (1031, Interview, Never tapered or discontinued ). Participants also described how the programme had reframed self-care not as something ‘fluffy’, but as ‘practical’ and a necessary part of their ongoing recovery: ‘It doesn’t make you any less male of course. [Chuckles] Or any less powerful’ (1203, Interview, Discontinued ). In some cases, this new attitude towards self-care caused a shift such that people felt more acceptance towards taking ADMs: ‘I don't feel any more when I take my pill every morning that there's something wrong with me’ as they recognised it was important to do ‘everything in my power to help myself’ (1177, Interview, Tapered but never discontinued ). Some participants also described how originally they had taken ADMs unwillingly, whereas after MBCT-TS they decided to take ADMs as an act of effective self-management: ‘I used to hate taking them [ADMs] I accept [now] it’s all about looking after yourself isn't it?’ (3103; Interview, Discontinued and resumed ).
Perspectives on relapse
One dimension of acceptance was people’s perspectives on mood fluctuations and relapse itself. Some people favoured ADMs as an approach to relapse prevention, because it guaranteed them stability in their mood. For instance, when Greta experienced a deterioration in mood, she interpreted this as a sign that the MBCT-TS programme had been a ‘failure’ and she resumed taking ADMs (see box 1 ). However, this was not always the case, and many people described how participating in MBCT-TS changed their attitude towards relapse/recurrence. In particular, some people felt more able to accept mood fluctuations and even periods of depression. They described approaching them in a different way, ‘thinking it was a phase that one was going through and sort of accepting, okay this is how you're feeling today’ (1159; Interview, Discontinued and resumed ). Some people reported that they no longer wanted to ‘blank out their negative emotions’, and so did not resume ADMs, even if they relapsed: ‘it’s definitely helped me to realise that they [negative emotions] are a part of me as well’ (4057, Interview, Discontinued ).
Quality of life
People reflected on the ways in which treatment choices influenced their quality of life, specifically moving them from a place of coping, to a position where they could enjoy and appreciate their lives. This theme comprises two sub-themes.
Experiencing emotions more fully
On reflecting on their experiences with ADMs, some participants said that while ADMs lessened their low mood, at the same time they ‘dampen all other emotions’, for instance, they could not feel ‘blissfully happy, couldn’t get angry, and in hindsight feel I was sedated’ (4057, Written feedback, Discontinued ). In the context of depression, some people viewed this numbing effect as helpful, and reflected that while ADMs ‘take away the euphoria that you would get when you've done something really, really, really good’, this was ‘a small price to pay really for not having the really dark times’ (2200; Interviews, Tapered but never discontinued ). However, many people thought that this had negatively affected their quality of life, especially in cases where they found it hard to experience positive emotions. This appeared to influence people’s decision to taper or discontinue ADMs, because they said that restoring their emotional range was an important part of their long-term vision of recovery: both George and Claire described this as a key motivator to discontinue their ADMs (see box 1 ). Indeed, people described how their emotional capacity increased after coming off ADMs: ‘I am more alive: my emotions aren't “levelled out” anymore. I can be happy, sad, angry or calm instead of just bland’ (4057, Written feedback, Discontinued ). Despite this, some people found it a bit of a ‘shock’ at first, when faced with ‘very extreme emotions and feelings’ again ( 1212; Feedback booklets, Discontinued ). Therefore, people found it helpful that the programme taught them techniques to help manage this transition: ‘I definitely used mindfulness during coming off the tablets to […] be aware what’s going on inside and […] calm myself down, to have those little islands of tranquillity’ (4057, Written feedback, Discontinued ). On the other hand, some participants said that despite not tapering or discontinuing ADMs, the programme had helped them to cultivate more positive emotions, and appeared to increase their quality of life on ADMs: ‘I suppose the mindfulness in that respect has helped because […] by slowing yourself down you can […] capture some of that […] joy of life that possibly I would have lost’ (2200; Interviews, Tapered but never discontinued ).
From coping to enjoying life
Many people reflected that in their recovery journey they had been grateful for the periods of time where they were simply able to function. However, some participants said that the programme had helped them to move beyond that mind-set, and to develop more well-being and appreciate life: ‘What has changed? I think my outlook on life, I love life, I really do […] People said to me […] before you used to skulk into the room, now you light up the room. […] I do enjoy life now, where I didn’t before’ (2016, Interview, Discontinued ). They valued the fact that the programme had an active focus on positive functioning, and encouraged them to take part in activities that brought happiness and joy into their life. Participants described this as an active process, facilitated by a sense of having more control and autonomy over making positive decisions in their life: ‘I rearranged my life so that the things I do now are things that I enjoy and want to do’ (1203, Interviews, Discontinued) ; ‘ I am now making bigger future plans to make my life better and introducing new ventures’ (1031, Written feedback, Never tapered or discontinued ).
ADM tapering/discontinuation
The study’s focus included people’s experiences of tapering and discontinuing ADMs in the context of the MBCT-TS programme. This theme describes participants’ views of what helped or hindered the process of discontinuation. It comprises two sub-themes.
Reflecting on the right time to engage with different treatments, many participants felt that ADMs were helpful when they first became depressed: ‘they got me out of my initial depression so that I could cope more with just everyday life’ (4007, Interview, Never tapered or discontinued ). However, many did not envisage being on ADMs indefinitely, and they described an increasing need for insight and self-management of depression as time went on. They thought that the MBCT-TS techniques required more effort, but supported a longer-term vision of recovery, to ‘recognise what makes you depressed and to give you a way to cope with your depression throughout your life for the long-term, and a way that you can come off [ADMs]’ (4007, Interview, Never reduced or discontinued ). As illustrated by this quotation, some participants viewed the MBCT-TS skills as part of a longer-term solution to ADM discontinuation, which extended beyond the 2-year follow-up period. Some participants reflected on how they thought the two treatments could be used in combination to support people at different parts of their journey, from depression through to recovery: ‘I think you need that initial boost of antidepressant to perhaps get you back into a more rational level, and then once you’ve reached that, then bring in the MBCT, until you get back then you know, be weaned off. I can see that working very well really’ (1108, Interview, Never reduced or discontinued ).
Participants discussed the pace at which they tapered ADMs, and how they perceived this to have influenced their outcomes. Some people who were worried about coming off ADMs shared that they exercised caution, testing out the psychological techniques for a set period and tapering slowly. They said this was helpful as it gave them time to learn to use the psychological techniques before giving up the support of their ADMs, ‘by doing it slowly, you are learning those skills and you are finding out how you can use it. [Then] you can start dropping it [ADMs] at your own pace’ (1075; Interviews, Discontinued ). In comparison, those who were keen to come off ADMs and were less fearful of the consequences described tapering more quickly. Although the programme had included explicit guidance to taper gradually, participants’ reports suggested that many people had gone against this advice, and were looking for a ‘quick fix’ to ‘get off the pills as quick as possible’ (2131, Interview, Tapered but never discontinued ). However, on reflection many people thought, ‘perhaps that wasn't the answer perhaps the thing ought to be graded on over a longer period’ (2131, Interviews, Tapered but never discontinued ). Some of these participants reflected that in retrospect they should have been more cautious, and tapering too quickly had led to poorer outcomes: ‘I reduced my tablets too quick and paid the price by having to get straight back to the full dose’ (2016, Interview; Written feedback, Discontinued ). However, some people, like Claire, who did not successfully discontinue on their first attempt reported how they had then tried again, tapering more gradually and with more success (see box 1 ).
Managing withdrawal effects
People said that the programme had helped them to cope with withdrawal effects during and after tapering/discontinuing ADMs. They described how the group and the meditation techniques provided ongoing support to manage this period: ‘I used meditation techniques […] tried to treat myself with pleasurable experiences and told myself that this would pass over. […] I had a network of fellow participants and a trustworthy instructor. All of this put me in a position of confidence that it would work this time’ (4057, Written feedback, Discontinued ). In addition, people said that they were better able to differentiate the side effects of ADM withdrawal from a depressive relapse. For instance, Mandy said that in the past, withdrawal effects had been the biggest hindrance to tapering ADMs, because she had always mistaken them for a depressive relapse and resumed her medication. On the programme, she learned how to differentiate between these effects and ‘real relapses’, and said that tapering was relatively ‘easy’ this time around (see box 1 ). Indeed, some people recalled attempting to discontinue ADMs before the trial and their withdrawal symptoms being ‘misdiagnosed’ ‘as recurring depression’, whereas this time they ‘knew what was coming’ (4057, Written feedback, Discontinued ).
Interactions with GP
Participants’ described their interactions with their GPs as being important in their recovery, in both positive and negative ways. This theme comprises two sub-themes.
Presence and support
Participants described having a GP who was easy to access throughout the process of discontinuation as supportive: ‘Knowing that I could ring the doctor and say, “I need to make an appointment, I need to come and see you.” There was always that net underneath me to catch me if I was falling and I couldn't stop it’ (2090, Interview, Discontinued ), whereas some participants said they found it ‘very difficult’ to access their GPs, and so felt ‘unsupported’ (1123, Written feedback, Tapered but never discontinued ). Participants reported a more positive attitude to the programme if their GP had endorsed it, and some said they had only been convinced to take part in the trial because their GPs said they had themselves done a mindfulness course. When GPs encouraged their patients to use the mindfulness practices, this appeared to be associated with better engagement and subsequent success in ADM tapering and discontinuation: ‘I did reach a stage where I went to see my G.P. as the depression was returning. […] We decided that I should try the exercises before trying pills. I did not need to go back on them yet […] My GP is a great help’ (2090, Written feedback, Discontinued ).
Following advice
Participants differed in the extent to which they sought and followed the advice of their GPs. For instance, some participants described that they remained on their ADMs at their GP’s suggestion: ‘My GP would not allow me to come off my antidepressant or reduce it because I had been on them so long term. [I am] relieved but also a bit disappointed’ (1108; Written feedback, Never tapered or discontinued ). This adherence to medical advice seemed to be greater for participants who had more concerns about discontinuation. For instance, Claire, who relapsed the first time that she had attempted tapering and discontinuation, was much more receptive to her GP’s advice the second time around, because she was afraid of relapsing again (see box 1 ). On the other hand, where people were confident that they had learned the skills to self-manage their depression without ADMs, they more often reported that they could manage the process independently, and placed less value on their GP’s advice: ‘I went along to the doctors because I was polite to ask him if I could stop taking it. And he said, “Well yeah maybe in a few months time you can taper it- ease it off a bit.” But really I had decided (laughs) I was going to stop. So I was just there out of politeness’ (1203; Interview, Discontinued ).
Statement of principal findings
This study explored the recovery journeys of people with recurrent depression who followed a programme (MBCT-TS), designed to teach psychological skills to prevent depressive relapse while providing advice to encourage tapering and discontinuation of maintenance ADMs. 13 Thematic analysis suggested people have unique recovery journeys, but tend to be characterised by six common themes. Five illustrative stories are represented in case studies ( box 1 ). The over-arching themes in participants’ accounts were: beliefs about the causes of depression, personal agency, acceptance, quality of life, ADM tapering/discontinuation and interactions with GP ( table 2 ). Together, these findings have the potential to facilitate discussions between clinicians and patients about the depression recovery journey. The findings also provide a starting point for more research into which treatments for recurrent depression, or combination of treatments, work best for whom and when.
Strengths and weaknesses of this study
This study had a number of methodological strengths. We had a relatively large sample and purposively sampled the population for whom this research is relevant—people with a history of recurrent depression, stable on maintenance ADMs who were open to both a psychological and pharmacological approach to recovery. The study’s time frame enabled participants to reflect on their journey with MBCT-TS and ADMs over 2 years. To support participants’ recollection we developed prompts about the course of their depression and ADM use over the 2-year period based on information we had collected as part of the parent RCT.
Alongside these strengths, it is important to consider the context within which the study took place and its implications for interpretation of the findings. First, the trial was pragmatic in that it recruited participants from a particular population. 16 However, it did not include people either unwilling to consider a psychological therapy or unwilling to consider tapering/discontinuing their medication. Second, the parent trial included monitoring participants’ use of ADM, and if people following MBCT-TS were not tapering/discontinuing they were invited to discuss this with their GPs. Some participants reported feeling pressured to discontinue ADMs and it is reasonable to assume that some participants may have made different decisions in a more naturalistic setting. Third, our purposive sampling means this study does not speak to a larger population of people with a history of depression who are not interested in a psychological approach and tapering/discontinuing their ADMs, or indeed prefer not to use ADM. Fourth, the questions in our feedback booklets and interviews had a particular framing, and it is possible that if the questions were framed differently the answers too may have been different. Finally, for pragmatic reasons we did not ask participants’ feedback on the themes as is sometimes done in qualitative research.
Implications of our findings
Several RCTs have demonstrated that psychological therapies such as CBT and MBCT can support ADM discontinuation, 8–10 but to our knowledge, no qualitative studies have examined people’s experiences of this process. This study adds to the body of literature suggesting that people’s journey involves choices among different treatments, shaped by their prior beliefs, expectations, experiences and interactions with their GPs. In both MBCT and CBT people learn new skills to manage depressive symptoms, gaining new perspectives drawn from both the psychological model and peer-to-peer learning, and develop an increased sense of agency concerning ADM discontinuation. 11 20 21 In this study participants described learning attitudes towards self-care that were participatory and empowering, which facilitated a sense of agency around ADM use, tapering and discontinuation. On the other hand, some people’s biological beliefs about depression, positive experiences of ADM, and/or negative experiences of psychological therapies meant they were happy to use ADM as their primary approach to recovery.
People also emphasised the importance of a GP who is accessible and able to provide support that is collaborative, individualised and empowering, with careful monitoring over time. Moreover, they described how GPs had powerfully shared their models of depression, expectations of treatment and treatment choices. The implication for GPs is to provide accessible, collaborative, individualised and empowering care. Moreover GPs should provide people with explanatory models of depression that are bio-psycho-social alongside appropriate pharmacological and psychological treatment choices. Our findings alongside others 21–23 also suggest GPs should not offer an overly simplistic biological model, for example, ‘your serotonin levels are low’, followed by a (repeat) prescription of ADM.
ADMs are currently the mainstay treatment approach to recurrent depression. Kendrick has argued that many people remain on ADMs without clinical need and could benefit from support and guidance on how to discontinue, especially regarding how to deal with initial withdrawal symptoms. 23 Our findings underscore this. Moreover, participants spoke of the importance of feeling that they had acquired from alternative skills in MBCT-TS to support their recovery generally by being able to manage their depression, but also ADM tapering and discontinuation specifically. For example, where life circumstances were challenging some people felt that the time was not right for them to discontinue ADMs; they made an informed decision to continue with their medication. Even so, the majority of participants who remained on ADMs reported that the MBCT-TS treatment had increased their quality of life on ADMs, and improved their confidence in future discontinuation when circumstances were more favourable. Our analysis also outlines participants’ views on the appropriate timing of different treatments, which provide ideas for when it might be an appropriate time to initiate conversations about ADM and MBCT treatment choices.
People described how their expectations of both MBCT and ADM influenced their treatment choices. Although it is widely assumed that positive expectations predict greater benefit in psychological therapy, in our sample both unrealistically positive expectations (eg, expecting MBCT-TS to be an ‘all-encompassing cure-all’) and very negative expectations (having ‘no intellectual confidence in the process’) appeared to act as a barrier to engagement. These findings are consistent with those of Malpass et al 7 and suggest that openly discussing expectations at key junctures is likely to be key in preventing disappointment or disengagement from what is an effortful process of change. Likewise, in line with Maund et al ’s findings, 6 people’s causal models of depression also appeared to influence their expectations and engagement with psychological therapy. Moreover, they were subject to change during and beyond the therapy process, as their experiences either confirmed or disconfirmed their expectations and working model of depression and its treatment. People who suffer from depression frequently endorse biomedical explanations, 24 and this was evident in our sample. A number of people reported that they derived these models from discussions with their GPs as a rationale for taking ADMs. Previous research suggests that conceiving depression as a biomedical illness can absolve people of personal responsibility and thus challenge stereotypes of depression resulting from personal weakness. 7 However, our findings suggest that strongly held biomedical beliefs appeared to increase feelings of dependency on ADMs, and contribute to negative expectations and lack of engagement with psychological therapy. On the other hand, while learning a psychological model of depression empowered people towards more self-management of depression and feelings of mastery over their emotional well-being, in some cases, when people developed a psychological understanding and then went on to relapse, they blamed themselves. In some cases, practical life circumstances also made it very difficult for people to engage in an approach that required time and effort. Together, this suggests that polarised beliefs about the causes of depression can either compromise self-efficacy or promote self-blame. Many participants found it helpful to bridge biomedical and psychological theories, with parallels to a ‘biopsychosocial’ framework, 25 rather than viewing separate theories as competing, which seemed to foster more flexibility, self-compassion and open-mindedness towards trying different treatment options at different times in their journey of managing recurrent depression. This highlights the importance of recognising that a myriad of factors, including genetic vulnerability and challenging social circumstances, can influence depression.
People sometimes describe ADMs as sedating or numbing. 26 In these interviews participants said this could influence their decision-making about ADM use. For example, in the instance of numbing, some people viewed this as helpful as it reduced their feelings of depression, whereas other people said that ADMs numbed all of their emotions, including positive feelings, and this contributed towards a desire to discontinue them. These findings add to ongoing discussion about the psychoactive effects of ADMs, including their potential benefits and costs, how these effects impact people’s experience of recovery from depression and how participating in psychological therapy can interact with these experiences.
Finally, descriptions of the role of the GP in supporting ADM discontinuation varied markedly, and this appeared to result both from differences between patients in their preferred level of guidance and support, and the availability of their GPs to provide this. For example, some people adhered to their GP’s advice although this was in conflict with their own desired approach, some described informing their GP of their intentions as an act of courtesy, and some did not involve their GP at all. In some of these latter cases, participants felt that they would have benefited from more support, but their GP, for a range of reasons, was unable to provide this. People also described needing more understanding and support over time as they took more responsibility for managing their depression. This is in line with findings from Malpass et al , 7 who suggested that people vary in the extent to which they want to be involved in treatment decision-making, and their preferences for involvement are dynamic, not static. Archer has described different ‘modes of reflexivity’ noting the varying degrees to which people act autonomously or rely on endorsement from others. 27 Moreover, recovery meant different things to different people, and overall, the outcome most important to patients appeared to be their day-to-day functioning and quality of life. It is likely that when GPs are able to recognise their patients’ preferred mode of engagement, and complex, dynamic views of recovery and adapt their approach accordingly, this will facilitate patient–GP consultations about ADM and psychological therapies treatment choices.
Unanswered questions and future research
This work adds to the emerging literature on people’s experiences of recovery from depression with ADM and psychological therapies. Applied research asking how patients and health professionals communicate about their respective models of depression, and understand how this affects treatment decisions, compliance, outcomes and a broader conceptualisation of recovery would be valuable. Extending this to the broader population of people who suffer depression would not only provide an interesting and important alternate perspective but also will be important to consider with respect to recovery journeys and treatment choices.
Our work took a qualitative approach. An obvious next question asks how these process variables affect outcomes. That is to say, what works for who, how, when, to affect treatment outcomes? Finally, such research should prioritise the outcome that is most meaningful to patients: their day-to-day functioning and quality of life.
Dissemination declaration
The trial results were disseminated in workshops and via a flyer to all participants who requested this feedback. The findings of this study will be disseminated to relevant audiences through University of Oxford communications.
Acknowledgments
We would like to thank Trish Bartley for her input to mindfulness-based cognitive therapy (MBCT) therapist training and MBCT fidelity checks. We are grateful to members of our trial steering committee (Chris Leach, Richard Moore and Glenys Parry) and data monitoring committee (Paul Ewings, Andy Field and Joanne MacKenzie) for their valuable advice and support during the project. We acknowledge the additional support provided by the Mental Health and Primary Care Research Networks. We also acknowledge the support provided by the Department of Health and local Primary Care Trusts, in meeting the excess treatment and service support costs associated with the trial. Thanks go to the research team, who facilitated wider qualitative work in the trial, including Aaron Causley, Anna Hunt, Pooja Shah, Holly Sugg, Harry Sutton and Matthew Williams. Above all, we are grateful to the participants for their time in taking part in this trial.
- Kessler RC ,
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators
- Kruijshaar ME ,
- Barendregt J ,
- Vos T , et al
- National Institute of Health and Care Excellence (NICE)
- Bosman RC ,
- Huijbregts KM ,
- Verhaak PFM , et al
- Dewar-Haggart R ,
- Williams S , et al
- Malpass A ,
- Sharp D , et al
- Warren FC ,
- Taylor RS , et al
- Moore M , et al
- Bockting C ,
- Elgersma HJ , et al
- Cuijpers P ,
- Dowrick C , et al
- Bockting CL ,
- Hollon SD ,
- Jarrett RB , et al
- Barrett B , et al
- Byng R , et al
- American Psychiatric Association
- Williams JMG ,
- Teasdale JD
- Bromley A ,
- Kuyken W , et al
- Ridd M , et al
- Kokanovic R ,
- Broom A , et al
- Brewin CR ,
- Power MJ , et al
- Moncrieff J ,
Twitter @WillemKuyken
Contributors WK, RB and NM were responsible for the PREVENT trial protocol (A randomized controlled trial comparing mindfulness-based cognitive therapy with maintenance anti-depressant treatment in the prevention of depressive relapse/recurrence) and secured the study funding. NM designed the over-arching qualitative process study to elicit service users’ experiences of treatment, with input from RB, FG, RH, JC and WK. Interviews were conducted by FG and AW, supervised by NM. CC, WK, JR and AT developed the analytical strategy and protocol for the study reported here, and AT conducted the bulk of the analysis, with input from other members of the analytical team. AT, CC and WK drafted the manuscript. All other authors read the manuscript, revised it for significant intellectual content and approved the final manuscript. As chief investigator, WK had overall responsibility for the parent trial within which this study was embedded. The University of Exeter held responsibility for the parent trial and this work. WK is guarantor and corresponding author for the study.
Funding The PREVENT trial was funded by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme (08/56/01) and was published in full in Health Technology Assessment. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HTA programme, NIHR, National Health Service or the Department of Health and Social Care. A trial steering committee, data and ethics monitoring committee, the UK Mental Health Research Network, the Primary Care Research Network, and the Comprehensive Local Research Network all provided support to the project. WK, CC and AT are supported by the Wellcome Trust (107496/Z/15/Z). RB received funding from NIHR Collaboration for Leadership in Applied Health Research and Care South West Peninsula.
Disclaimer The funders had no role in the design of the study, in the collection, analysis and interpretation of the data, in the writing of the report or in the decision to submit the article for publication. All authors are independent of the funders, had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests None declared.
Patient consent for publication Not required.
Ethics approval The South West Research Ethics Committee approved the trial (09/H0206/43), which was registered with the International Standard Randomised Controlled Trial Register ( ISRCTN26666654 ) and the Medicines and Healthcare products Regulatory Agency (2009-012428-10).
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available. We will not be making the data publicly available due to its highly confidential and identifiable nature.
Read the full text or download the PDF:

IMAGES
VIDEO
COMMENTS
Recurrent Major Depressive Disorder of a Young Woman. This exercise is designed to test your comprehension of material relevant to this issue of Focus as well as your ability to evaluate, diagnose, and manage clinical problems. Answer the questions below to the best of your ability with the information provided, making your decisions as if the ...
In a study of 239 outpatients diagnosed with major depressive disorder in a NIMH. 16-week multi-center clinical trial, participants were assigned to interpersonal therapy, CBT, imipramine with clinical management, or placebo with clinical management. One. hundred sixty-two patients completed the trial.
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
This study explored the recovery journeys of people with recurrent depression who followed a programme (MBCT-TS), designed to teach psychological skills to prevent depressive relapse while providing advice to encourage tapering and discontinuation of maintenance ADMs. 13 Thematic analysis suggested people have unique recovery journeys, but tend ...
Case Study of a 44-Year-Old Patient with a Moderate Recurrent Depressive Disorder (ICD-10 F 33.1) from Psychodynamic Point of View. In: Charis, C., Panayiotou, G. (eds) Depression Conceptualization and Treatment.
The role of electroconvulsive therapy (ECT) in depression has been an area of ongoing debate. There has been a reduction in use of what has been historically a highly effective treatment and there is a move to decrease use to last resort only. This case illustrates the utility of ECT in recurrent depressive disorder over a lifespan.
Major depressive disorder is one of the most common forms of psychopathology, one that will affect approximately one in six men and one in four women in their lifetimes (Kessler et al., 1994).It is also usually highly recurrent, with at least 50% of those who recover from a first episode of depression having one or more additional episodes in their lifetime, and approximately 80% of those with ...
The European "Group for the Study of Resistant Depression" (GSRD) multi-site study found that age at first treatment (i.e., early-onset and early treatment), age, timespan between first and ...
Objectives: This study aimed to describe the recovery journeys of people with a history of recurrent depression who took part in a psychosocial programme designed to teach skills to prevent depressive relapse (mindfulness-based cognitive therapy (MBCT)), alongside maintenance antidepressant medication (ADM). Design: A qualitative study embedded within a multicentre, single blind, randomised ...
There were 1259 persons with recurrent depression recruited to the genetic case-control study, all of whom fulfilled ICD-10 and/or DSM-IV criteria for recurrent major depressive disorder. The mean age of this group was 47.3 years (s.d.=12.5, range 19-85).
The ECT minimum data-set for the UK for 2016-2017 Reference Buley, Copland and Hodge 22 reported that across the 76% of centres that supplied data, there were 141 patients undergoing maintenance ECT for recurrent symptoms of depression. This represents about 8% of those undergoing ECT in total, and so is a relatively uncommon use of ECT.
The mental disorder recurrent depression or depressive episode is in ICD-10 [] characterised by the following core symptoms: depressed mood, lack of energy and decreased interest.Accompanying symptoms include decreased appetite, problems with concentration and sleep disturbance [].Untreated, the condition will often result in improper diurnal rhythm, disturbances in eating habits and for some ...
The study used recurrent major depression, the type of depression that has been shown to be most heritable (4, 8), with collection of cases in the U.K. by the same clinical team giving a homogeneous clinical sample. As depression is common in the general population, excluding cases of lifetime depression from the comparison sample can ...
diagnoses as part of a genetic case-control association study of recurrent depression, the Depression Case-Control (DeCC) study.3 Participants who had experienced two or more episodes of major depression of at least moderate severity were recruited from psychiatric clinics and hospitals (26%) and general practices (46%), and through self ...
In this case study, we described an older patient presenting with two distinct major depressive episodes, both of which occurred simultaneously with episodes of AIWS. Both sets of symptoms remitted completely after standard treatment for psychotic depression (i.e., an antidepressant plus an antipsychotic, or ECT), and we excluded the potential ...
This case study of a 21-year-old woman-referred by a relative because of long-standing severe interpersonal, academic, and occupational impairment-illustrates the importance of screening patients with brief episodes of depression for mixed features. ... Recurrent brief depression is defined as a phenomenon marked by the presence of impairing ...
current issue. current issue; browse recently published; browse full issue index; learning/cme
Method: People with recurrent depression (n=1259) were compared with psychiatrically healthy controls (n=851) to investigate headache defined according to International Headache Society criteria in each group. Results: All headache types were more prevalent in the case group than in the controls. However, the strongest association was between ...
Leanne: A Case Study in Major Depressive Disorder, Recurrent Leanne came to the office because she stated that her depression had worsened in recent months and that she was feeling nervous and panicky almost daily. She is 31 years old. Leanne described her home situation as "less than ideal."
RECURRENT DEPRESSION - CASE STUDY Patricia Luciana RUNCAN Faculty of Sociology and Psychology, West University of Timisoara, Romania ABSTRACT. In the following writing we have decided to offer a partial outlook above the social and psychological factors which caused the depression of Ms. C.E., aged 62 years.
Depressive disorder, frequently referred to simply as depression, is more than just feeling sad or going through a rough patch. ... Marital status, relationship changes, financial standing and where a person lives influence whether a person develops depression. Brain changes. Imaging studies have shown that the frontal lobe of the brain becomes ...
Rumination is an established transdiagnostic factor in mental illness, but there remains a significant gap in understanding the subjective experiences of those affected by it. This study explored the lived experiences of depressive rumination in early adulthood, a population notably susceptible to its effects. We interviewed 20 participants aged between 18 and 35 years using a semistructured ...
In this case study, we described an older patient presenting with two distinct major depressive episodes, both of which occurred simultaneously with episodes of AIWS. Both sets of symptoms remitted completely after standard treatment for psychotic depression (i.e., an antidepressant plus an antipsychotic, or ECT), and we excluded the potential ...
1 INTRODUCTION. Intranasal esketamine has recently been approved as a novel treatment option for Major Depressive Disorder (MDD) and its use is increasing worldwide. 1-3 Esketamine is a non-selective, non-competitive antagonist of the glutamatergic N-methyl-D Aspartate (NMDA) receptor and has robust antidepressant and anti-suicidal effects. 4 In the Netherlands, intranasal esketamine is only ...
Diagnosis of depression can be made using the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) or the 10th revision of the International Statistical Classification of Disease and Related Health Problems (ICD-10). 5 (Refer to Appendix 3 and 4, pages 73-76 in CPG.) 6,7
Evidence has suggested an increased risk of psychiatric manifestations following viral infections including coronavirus disease-2019 (COVID-19). However, psychiatric adverse events (AEs) after ...
Objectives This study aimed to describe the recovery journeys of people with a history of recurrent depression who took part in a psychosocial programme designed to teach skills to prevent depressive relapse (mindfulness-based cognitive therapy (MBCT)), alongside maintenance antidepressant medication (ADM). Design A qualitative study embedded within a multicentre, single blind, randomised ...
Case Study Five: Research on Accessibility of Urban Parks for People with Disabilities: The Case Study of Birlik Park, Konya-Turkey, 2016. ... Depression: a mood disorder characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities; ... This recurrent shape of the design is present in the main layout of the ...
Background/Objectives: Particle beam therapy (PBT) was approved in April 2018 for head and neck malignancies and has since been introduced as a radical therapy for parotid malignancies. However, its prevalence and effectiveness in relation to surgical treatment have not been investigated. Methods: In this study, we evaluated 36 patients with parotid malignancy who underwent surgery (n = 26) or ...