- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


2: Acute Otitis Media
Aimee Dassner; Jennifer E. Girotto
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Patient presentation.
- Full Chapter
- Supplementary Content
Chief Complaint
“Increased irritability and right ear pain.”
History of Present Illness
JL is a 22-month-old female who presents to her primary care provider (PCP) with a 2-day history of rhinorrhea and a 1-day history of increased irritability, fever (to 101.5°F per Mom), and right-ear tugging. Mom denies that JL has had any nausea, vomiting, or diarrhea.
Past Medical History
Full-term birth via spontaneous vaginal delivery. Hospitalized at 9 months of age for respiratory syncytial virus–associated bronchiolitis. Two episodes of acute otitis media (AOM), with last episode about 6 months earlier.
Surgical History
Social history.
Lives with mother, father, and her 5-year-old brother who attends kindergarten. JL attends daycare 2 d/wk, and stays at home with maternal grandmother 3 d/wk.
No known drug allergies
Immunizations
|
|
Hepatitis B | Birth |
DTap/Hep B/IPV | 2 mo, 4 mo, 6 mo |
Hib | 2 mo, 4 mo, 6 mo, 15 mo |
PCV13 | 2 mo, 4 mo, 6 mo, 12 mo |
Influenza | 6 mo, 8 mo, 18 mo |
MMR | 12 mo |
Varicella | 12 mo |
Home Medications
Vitamin D drops 600 IU/d
Physical Examination
Vital signs (while crying).
Temp 100.7°F, P 140 bpm, RR 35, BP 100/57 mm Hg, Ht 81 cm, Wt 23.7 kg
Fussy, but consolable by Mom; well-appearing
Normocephalic, atraumatic, moist mucous membranes, normal conjunctiva, clear rhinorrhea, moderate bulging and erythema of right tympanic membrane with middle-ear effusion
Good air movement throughout, clear breath sounds bilaterally
Cardiovascular
Normal rate and rhythm, no murmur, rub or gallop
Soft, non-distended, non-tender, active bowel sounds
Genitourinary
Normal female genitalia, no dysuria or hematuria
Alert and appropriate for age
Extremities
1. Which of the following clinical criteria is not part of the diagnostic evaluation or staging of acute otitis media (AOM) for this patient?
A. Rhinorrhea
D. Contour of the tympanic membrane
Get Free Access Through Your Institution
Pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMJ Case Rep

Case Report
The connection between acute otitis media and the acute abdomen, imran masood.
Touro University California, Vallejo, California, USA
Tami Hendriksz
A female aged 9 years with a recent episode of acute otitis media (AOM) presented to her primary care physician with complaints of severe abdominal pain with right lower quadrant rebound tenderness, suggestive of an acute surgical abdomen. Neurological examination was normal on presentation. She was transferred to the local children’s hospital for workup of appendicitis, during which she began exhibiting ataxia and slurred speech. Further evaluation revealed mastoiditis, venous sinus thrombosis and subdural empyema. Appendicitis was ruled out. We describe the first documented case of neurological complications of AOM presenting as an acute surgical abdomen without initial neurological findings.
Our case highlights many important lessons that primary care physicians will encounter. First, we present an example of when prematurely focusing on one diagnosis may distract the clinician from the true diagnosis and lead to diagnostic delay. Moreover, we illustrate an example of the interplay between distant body systems; connecting abdominal pain to a neurological infection. We believe that this case provides a fund of knowledge for other primary care physicians.
Complications of acute otitis media (AOM) are varied and can result in significant harm. Of these, most notable are intracranial disease such as venous sinus thrombosis (VST) and cerebral abscess, and extracranial disease such as mastoiditis. VSTs among children most commonly present as isolated, gradual-onset, localised headaches. 1 Although less likely, ‘thunderclap’ and migraine-type headaches may occur. 2–5 Focal neurological findings, encephalopathy and seizures are possible findings as well. Intracranial abscesses are associated with the classic triad of headache, fever and focal neurological findings; however, less than half of cases present with this triad. 6 Common findings for intracranial abscesses also include lethargy, nausea and vomiting. 7 Mastoiditis is characterised by postauricular tenderness, erythema, fluctuance, auricular displacement or protrusion and ear pain. 7 8
In the case of our patient, she presented with a primary concern of acute onset abdominal pain in the setting of an episode of AOM. Her presentation has never been reported in the literature as the presenting complaint for VST, mastoiditis or subdural empyema.
Case presentation
Our patient is a female aged 9 years with no significant past medical history who presented to her primary care provider on 21 January 2016 with the complaint of 5 days of fever, bilateral ear pain, anorexia, non-bloody and non-bilious emesis and 2 days of generalised abdominal pain. Two days prior to presentation, she was seen at an outside emergency department for AOM. Because of a penicillin allergy, she was given azithromycin 500 mg for 1 day, followed by 250 mg for 4 more days. However, after the first dose, she began to vomit, and did not complete her antibiotic therapy. The remaining review of systems were negative. On arriving to the primary care paediatrician, initial physical examination revealed that she was tired and ill-appearing with purulent drainage from her left ear and acute tenderness in the right lower quadrant of her abdomen. She exhibited rebound and guarding. Her urinalysis in the outpatient clinic was negative, and due to concern for acute abdomen and serious bacterial infection she was sent to the emergency department of the local Children’s Hospital.
Investigations
Initial labs at the emergency department showed a white blood cell count of 23 x 10 3 /µL and a C reactive protein of 28.6 mg/L. Chemistry was within normal limits. Her left ear was again noted to have purulent drainage, and her abdomen continued to be very tender to palpation with guarding. She was initially admitted to the surgical service given concern for appendicitis. On her first day of admission, she received a limited abdominal ultrasound, which was negative for appendicitis. During the ultrasound, the patient was noted to have slurred speech and right-sided weakness. Neurology was then consulted, and felt that her symptoms were more consistent with a seizure disorder, therefore, they recommended an electroencephalogram (EEG) which showed focal left paracentral slowing. After receiving the results of the EEG, neurology recommended a brain MRI and magnetic resonance venography (MRV). These studies were done the same day, and they revealed meningeal enhancement of the frontal and parietal lobes consistent with meningitis, as well as left venous sinus thrombosis and left mastoiditis. Haematology was then consulted. They recommended a hypercoagulable workup, which was negative. Due in part to her persistent right-sided weakness, a subsequent brain MRI was obtained, 6 days after the first, which showed a subdural empyema. The patient’s venous sinus thrombosis, subdural empyema, meningitis and cerebritis were attributed to a complicated otitis media and mastoiditis. Blood culture drawn at the time of admission grew coagulase-negative staphylococcus at 24 hours, which was thought to likely be a contaminant. A lumbar puncture revealed cerebral spinal fluid (CSF) with a white blood cell count of 153 cells/µL, with 59% neutrophils and 41% monocytes. The CSF protein level was 71 mg/dL and glucose 67 mg/dL. CSF culture had no growth. CSF was positive for Streptococcus pneumoniae by PCR (negative PCR for Neisseria meningitides and Haemophilus influenzae type b). Subdural empyemic fluid culture had no growth, and culture of her ear drainage grew scant coagulase-negative staphylococcus.
Studies completed during this hospitalisation:
Hospital day 1—ultrasound abdomen limited
Hospital day 1—EEG
Hospital day 1—MRI and MRV brain with contrast
Hospital day 3—CT orbit, ear, temporal bone with and without contrast
Hospital day 3—CT neck with contrast
Differential diagnosis
- Mesenteric adenitis (working diagnosis).
- Lemierre’s syndrome with otogenic variant.
- Mesenteric ischaemia and cavernous sinus thrombosis secondary to hypercoagulable state induced by serum inflammation.
- Primary otitis media with spread to adjacent tissues causing central nervous system infection with secondary bacteraemia/fungaemia, leading to hematogenous spread to the abdomen.
- Abdominal pain secondary to recurrent vomiting in the setting of elevated intracranial pressure.
The patient was started on vancomycin and ceftriaxone empirically on admission. Infectious disease consultants recommended adding metronidazole on day 2 of hospitalisation given the unclear aetiology of her infection and her persistent fevers. She was treated with intravenous ceftriaxone and metronidazole for 2 weeks inpatient, followed by an additional 4 weeks outpatient (via a peripherally-inserted central catheter (PICC) line). On discovery of the venous sinus thrombosis, the patient was started on a heparin drip and later in her hospital course transitioned to enoxaparin and heparin XA (low molecular weight heparin). She also underwent tympanostomy tube placement and left mastoidectomy on day 2 of hospitalisation, followed by burr hole irrigation of the subdural empyema 5 days later. The patient was followed by neurology, haematology, neurosurgery, otolaryngology, infectious disease and physical therapy during the course of her stay.
Procedures completed during this hospitalisation:
Hospital day 2—bilateral myringotomy tubes, and mastoidectomy with wash out
Hospital day 4—single lumen PICC line placement in left brachial vein
Hospital day 7—burr hole irrigation of subdural empyema
Outcome and follow-up
The patient’s abdominal pain resolved within the first 2 days of her hospital stay. Patient was discharged from the hospital after 22 days. Follow-up brain MRI 3 weeks after hospital discharge showed resolution of the subdural empyema and the venous sinus thrombosis, with resolving cerebritis, and evolving postsurgical changes of the left mastoid process. Her antibiotics were discontinued at that time, and her PICC line was removed the following day. By her follow-up appointment with haematology 7 weeks after discharge, patient had ‘returned to her baseline normal activity without any evidence of ongoing infection’ or sequelae.
On recent follow-up, now 11 months after initial presentation, the patient exhibits a full recovery. She has graduated from physical therapy, and is back to practicing competitive gymnastics. Our patient is no longer on any medications, and has been discharged from the haematology, infectious disease, neurosurgical and neurology specialists. She does continue to see the otolaryngologist and audiologist for follow-up care while her tympanostomy tube remains in place.
We present the case of a female aged 9 years with multiple sequelae of AOM demonstrating an atypical clinical presentation. VSTs are considered exceptionally rare, with the incidence reported at 0.67/100 000 in children. 9 Studies also show that VSTs are more common in neonates and infants, rather than children or adolescents. 9 Furthermore, while mastoiditis is more common than VSTs, the incidence of mastoiditis is exceedingly rare in a child aged 9 years. Various studies have demonstrated that mastoiditis occurs most often in children <2 years of age, with one report of a median age of 48 months. 10–12 Moreover, as mentioned above, the clinical presentation for these particular sequelae largely present with neurological findings. Our patient did not initially exhibit any of the aforementioned neurological findings.
Demographically, statistically and clinically, our patient exists as an anomaly to the current literature. Our case highlights the essential nature of acknowledging the connection between distinct organ systems. Additionally, focusing on the possibility of an acute emergency can be a distraction from investigating its aetiology, and may lead to diagnostic delay.
In an attempt to connect otitis media with abdominal pain, we propose the diagnosis of mesenteric adenitis. Mesenteric adenitis is associated with group A streptococcal (Streptococcus pyogenes) pharyngitis, which is also present in cases of AOM. 13 14 Mesenteric adenitis has been shown to present very similarly to appendicitis. 14 A potential cause of our patient’s severe abdominal pain with rebound and guarding may have been her S. pneumoniae otitis media contributing to the development of mesenteric adenitis. It is possible that the mesenteric lymph node enlargement was missed on the limited abdominal ultrasound, as the ultrasound focused primarily on the appendix. Along with this theory, we also postulate that a primary otitis media may have occurred, with spread into contiguous tissues causing mastoiditis, subdural empyema and venous sinus thrombosis. This infection may have then become haematologically disseminated, with resultant seeding of the infection in the abdomen, which prompted the need for intravenous antibiotics. Interestingly, her ear fluid culture grew coagulase-negative staphylococcus, an organism also found in her blood culture, which correlates this theory. However, this was considered to be a contaminant, and not a true infection. This theory is less likely considering the bacteria that was isolated in her CSF was S. pneumoniae , and that her blood cultures were presumably negative. Furthermore, we considered the link between elevated intracranial pressure and repetitive vomiting to be a potential explanation for her abdominal pain. However, abdominal pain due to vomiting would not typically present as severe right lower quadrant pain with rebound tenderness and guarding.
Another potential explanation to connect these symptoms include the otogenic variant of Lemierre’s syndrome. Lemierre’s syndrome is a suppurative thrombophlebitis involving the internal jugular veins, most often caused by Fusobacterium necrophorum . Thrombosis of the jugular veins occur, followed by septic emboli to the lungs. 15 A case reported by Masterson et al revealed an otogenic variant of Lemierre’s syndrome, in which a young girl suffered bilateral mastoiditis with subsequent internal jugular vein thrombosis. 16 While this explanation is plausible, it is weakened by the fact that she did not present with pulmonary symptoms, which is a classic finding in Lemierre’s syndrome. Chest X-ray was not performed during the course of this illness.
Moreover, considering her elevated CRP suggesting serum inflammation, she may have been in a hypercoagulable state. This hypercoagulable state could have presented with two separate infarctions, one being her documented venous sinus thrombosis, and the other being a thrombus in a mesenteric vessel. This theory is supported by her improvement while on anticoagulants and decreased abdominal pain with bowel rest (a hallmark aspect of managing mesenteric ischaemia). However, considering her otitis media, mastoiditis and subdural empyema, it is more likely that the thrombus in her cerebral sinus was due to contiguous spread of infection with vascular insult, rather than primary vascular thrombosis.
Unfortunately, due to the high morbidity associated with appendicitis, it is likely that the clinician will narrowly focus on this diagnosis, at the expense of a broad diagnostic workup. In this scenario, focusing on the diagnosis of appendicitis resulted in a distraction away from the patient’s ear infection and its potential sequelae. Had neurological symptoms not developed, she may have suffered from a higher morbidity, due to delayed diagnosis. Luckily she had been admitted to a Children’s Hospital, under the care of multiple specialists, where she was able to have an EEG and then subsequent brain MRI with MRV with little time delay. It is interesting to note that this patient had an EEG performed prior to any imaging of her brain. At the time, the patient had been admitted to the surgical service for a likely appendicitis, and the recommendation to obtain an EEG by the consulting neurology team had been followed without consideration of prior emergent brain imaging. Also interesting to note is that no further workup (beyond the initial limited ultrasound) or discussion regarding the cause of her acute abdominal pain is apparent in review of her medical records. There appears to have been a somewhat myopic focus on the symptom that was most severe at a given time (initially abdominal pain, later the neurological symptoms), without much effort to search for connections or provide more holistic care.
In conclusion, our unique case provides important teaching points for any physician treating patients in the ambulatory clinic. We found in this case, that prematurely focusing on one diagnosis led to diagnostic delay. Furthermore, we highlighted that distant body systems may be unsuspectingly related, requiring a ‘whole-body’ approach for accurate diagnosis. An important lesson to be taken away from this case is that one unifying diagnosis is more likely than two separate, unrelated diseases. Fortunately, our patient is healing appropriately and remains well overall.
Learning points
- Prematurely locking onto a diagnosis may distract a clinician from the true diagnosis.
- Distant body systems may be unsuspectingly related, therefore, clinicians should always exercise a ‘whole-body’ approach.
- For a set of signs and symptoms, one unifying diagnosis is more likely than two separate aetiologies.
- There is a potential connection between abdominal pain and neurological infections that is not well-defined by our current literature. Mesenteric adenitis may be one possible explanation.
Contributors: This manuscript has not been published previously and is not under consideration for publication elsewhere. Both authors participated in the concept and design, analysis and interpretation of the data, drafting and revising of the manuscript and have approved the manuscript as submitted. The authors have no conflicts of interest to disclose.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.

Case Challenge: Acute Otitis Media in Children--Best Management Strategies
Gordon h. sun, md, ms.
March 28, 2018
Toddler Ear Tugging
A 2-year-old girl was seen by a pediatric nurse practitioner in the ambulatory clinic. The girl's mother reported that her daughter had been fussing and pulling on her right ear for the past 2 days but had no fevers or lethargy. There were no recent sick contacts. The patient had no history of ear surgery. She was not taking any medications and had no known drug allergies.
The patient demonstrated normal vital signs. She appeared nontoxic and was breathing comfortably. She was awake, active, and tugging on her right ear. There was no erythema or edema of the right auricle or mastoid. Otoscopic exam of the right ear demonstrated a normal-appearing external auditory canal and an inflamed and bulging tympanic membrane. The tympanic membrane was immobile on pneumatic insufflation . No otorrhea was seen in the canal. The remainder of the physical exam, including left ear otoscopy, was unremarkable.

Medscape Family Medicine © 2018 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Case Challenge: Acute Otitis Media in Children--Best Management Strategies - Medscape - Mar 28, 2018.
Authors and Disclosures
Medical Director of Inpatient Services; Chief, Division of Otolaryngology and Ophthalmology, Rancho Los Amigos National Rehabilitation Center, Downey, California; Adjunct Clinical Associate Professor of Otolaryngology, University of Southern California, Los Angeles, California Disclosure: Gordon H. Sun, MD, MS, has disclosed the following relevant financial relationship: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Partnership for Health Analytic Research, LLC
You have already selected for My Alerts
- Add Other Topics
Click the topic below to receive emails when new articles are available.
You've successfully added to your alerts. You will receive email when new content is published.
- Perspective
- Drugs & Diseases
- Global Coverage
- Additional Resources

- Social Media a 'Powerful' Way to Talk to Teens About Obesity
- Prescription for Caution: Can Social Media Posts Jeopardize Your Next Job?

- 2001/viewarticle/sleep-and-social-media-impact-youth-brain-development-2024a1000ag1 news Sleep and Social Media Impact Youth Brain Development
- 2001/viewarticle/surgeon-generals-push-social-media-warning-label-explained-2024a1000c3g news The Surgeon General's Push for Social Media Warning Label Explained
- 2001/viewarticle/social-media-powerful-way-talk-teens-about-obesity-2024a10009lo news Social Media a 'Powerful' Way to Talk to Teens About Obesity
- 2001/viewarticle/prescription-caution-can-social-media-posts-jeopardize-your-2024a10001ne news Prescription for Caution: Can Social Media Posts Jeopardize Your Next Job?
- Otitis Media
- Otitis Media With Effusion
- Acute Otitis Media
- Complications of Otitis Media
- Chronic Suppurative Otitis Media
- Emergent Management of Acute Otitis Media

- Sleep and Social Media Impact Youth Brain Development
- The Surgeon General's Push for Social Media Warning Label Explained
- Managing Common Ear Complaints: An ENT's Advice
- Bell's Palsy: What to Know in Primary Care
- Erosive Esophagitis: 5 Things to Know

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection

Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed, acute otitis media, affiliations.
- 1 Midwestern University
- 2 Kingman Regional Medical Center
- PMID: 29262176
- Bookshelf ID: NBK470332
Acute otitis media is defined as an infection of the middle ear space. It is a spectrum of diseases that includes acute otitis media (AOM), chronic suppurative otitis media (CSOM), and otitis media with effusion (OME). Acute otitis media is the second most common pediatric diagnosis in the emergency department, following upper respiratory infections. Although otitis media can occur at any age, it is most commonly seen between the ages of 6 to 24 months.
Infection of the middle ear can be viral, bacterial, or coinfection. The most common bacterial organisms causing otitis media are Streptococcus pneumoniae , followed by non-typeable Haemophilus influenzae (NTHi) and Moraxella catarrhalis . Following the introduction of the conjugate pneumococcal vaccines, the pneumococcal organisms have evolved to non-vaccine serotypes. The most common viral pathogens of otitis media include the respiratory syncytial virus (RSV), coronaviruses, influenza viruses, adenoviruses, human metapneumovirus, and picornaviruses.
Otitis media is diagnosed clinically via objective findings on physical exam (otoscopy) combined with the patient's history and presenting signs and symptoms. Several diagnostic tools are available such as a pneumatic otoscope, tympanometry, and acoustic reflectometry, to aid in the diagnosis of otitis media. Pneumatic otoscopy is the most reliable and has a higher sensitivity and specificity as compared to plain otoscopy, though tympanometry and other modalities can facilitate diagnosis if pneumatic otoscopy is unavailable.
Treatment of otitis media with antibiotics is controversial and directly related to the subtype of otitis media in question. Without proper treatment, suppurative fluid from the middle ear can extend to the adjacent anatomical locations and result in complications such as tympanic membrane (TM) perforation, mastoiditis, labyrinthitis, petrositis, meningitis, brain abscess, hearing loss, lateral and cavernous sinus thrombosis, and others. This has led to the development of specific guidelines for the treatment of OM. In the United States, the mainstay of treatment for an established diagnosis of AOM is high-dose amoxicillin, and this has been found to be most effective in children under two years of age. Treatment in countries like the Netherlands is initially watchful waiting, and if unresolved, antibiotics are warranted. However, the concept of watchful waiting has not gained full acceptance in the United States and other countries due to the risk of prolonged middle ear fluid and its effect on hearing and speech, as well as the risks of complications discussed earlier. Analgesics such as non-steroidal anti-inflammatory medications such as ibuprofen can be used alone or in combination to achieve effective pain control in patients with otitis media.
Copyright © 2024, StatPearls Publishing LLC.
PubMed Disclaimer
Conflict of interest statement
Disclosure: Amina Danishyar declares no relevant financial relationships with ineligible companies.
Disclosure: John Ashurst declares no relevant financial relationships with ineligible companies.
- Continuing Education Activity
- Introduction
- Epidemiology
- Pathophysiology
- Histopathology
- History and Physical
- Treatment / Management
- Differential Diagnosis
- Complications
- Consultations
- Deterrence and Patient Education
- Enhancing Healthcare Team Outcomes
- Review Questions
Similar articles
- Otitis media outcomes of a combined 10-valent pneumococcal Haemophilus influenzae protein D conjugate vaccine and 13-valent pneumococcal conjugate vaccine schedule at 1-2-4-6 months: PREVIX_COMBO, a 3-arm randomised controlled trial. Leach AJ, Mulholland EK, Santosham M, Torzillo PJ, McIntyre P, Smith-Vaughan H, Wilson N, Arrowsmith B, Beissbarth J, Chatfield MD, Oguoma VM, Morris PS. Leach AJ, et al. BMC Pediatr. 2021 Mar 8;21(1):117. doi: 10.1186/s12887-021-02552-z. BMC Pediatr. 2021. PMID: 33685411 Free PMC article. Clinical Trial.
- Otitis media. Schilder AG, Chonmaitree T, Cripps AW, Rosenfeld RM, Casselbrant ML, Haggard MP, Venekamp RP. Schilder AG, et al. Nat Rev Dis Primers. 2016 Sep 8;2(1):16063. doi: 10.1038/nrdp.2016.63. Nat Rev Dis Primers. 2016. PMID: 27604644 Free PMC article. Review.
- General health, otitis media, nasopharyngeal carriage and middle ear microbiology in Northern Territory Aboriginal children vaccinated during consecutive periods of 10-valent or 13-valent pneumococcal conjugate vaccines. Leach AJ, Wigger C, Beissbarth J, Woltring D, Andrews R, Chatfield MD, Smith-Vaughan H, Morris PS. Leach AJ, et al. Int J Pediatr Otorhinolaryngol. 2016 Jul;86:224-32. doi: 10.1016/j.ijporl.2016.05.011. Epub 2016 May 11. Int J Pediatr Otorhinolaryngol. 2016. PMID: 27260611
- Diagnosis and treatment of otitis media. Ramakrishnan K, Sparks RA, Berryhill WE. Ramakrishnan K, et al. Am Fam Physician. 2007 Dec 1;76(11):1650-8. Am Fam Physician. 2007. PMID: 18092706 Review.
- What is new in otitis media? Corbeel L. Corbeel L. Eur J Pediatr. 2007 Jun;166(6):511-9. doi: 10.1007/s00431-007-0461-8. Epub 2007 Mar 16. Eur J Pediatr. 2007. PMID: 17364173 Free PMC article. Review.
- Meherali S, Campbell A, Hartling L, Scott S. Understanding Parents' Experiences and Information Needs on Pediatric Acute Otitis Media: A Qualitative Study. J Patient Exp. 2019 Mar;6(1):53-61. - PMC - PubMed
- Ubukata K, Morozumi M, Sakuma M, Takata M, Mokuno E, Tajima T, Iwata S, AOM Surveillance Study Group Etiology of Acute Otitis Media and Characterization of Pneumococcal Isolates After Introduction of 13-Valent Pneumococcal Conjugate Vaccine in Japanese Children. Pediatr Infect Dis J. 2018 Jun;37(6):598-604. - PubMed
- Ubukata K, Morozumi M, Sakuma M, Adachi Y, Mokuno E, Tajima T, Iwata S, AOM Surveillance Study Group Genetic characteristics and antibiotic resistance of Haemophilus influenzae isolates from pediatric patients with acute otitis media after introduction of 13-valent pneumococcal conjugate vaccine in Japan. J Infect Chemother. 2019 Sep;25(9):720-726. - PubMed
- Protasova IN, Per'yanova OV, Podgrushnaya TS. [Acute otitis media in the children: etiology and the problems of antibacterial therapy]. Vestn Otorinolaringol. 2017;82(2):84-89. - PubMed
- García Carretero R. Cerebellar abscesses, infective endocarditis and bacteraemia due to a rare pathogen: Streptococcus constellatus. BMJ Case Rep. 2017 Sep 01;2017 - PMC - PubMed
Publication types
- Search in PubMed
- Search in MeSH
- Add to Search
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- NCBI Bookshelf

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
The website will be down for maintenance from 6:00 a.m. to noon CDT on Sunday, June 30.

HEIDI L. GADDEY, MD, MATTHEW THOMAS WRIGHT, DO, AND TRACY N. NELSON, MD
Am Fam Physician. 2019;100(6):350-356
Author disclosure: No relevant financial affiliations.
Acute otitis media (AOM) is the most common diagnosis in childhood acute sick visits. By three years of age, 50% to 85% of children will have at least one episode of AOM. Symptoms may include ear pain (rubbing, tugging, or holding the ear may be a sign of pain), fever, irritability, otorrhea, anorexia, and sometimes vomiting or lethargy. AOM is diagnosed in symptomatic children with moderate to severe bulging of the tympanic membrane or new-onset otorrhea not caused by acute otitis externa, and in children with mild bulging and either recent-onset ear pain (less than 48 hours) or intense erythema of the tympanic membrane. Treatment includes pain management plus observation or antibiotics, depending on the patient's age, severity of symptoms, and whether the AOM is unilateral or bilateral. When antibiotics are used, high-dose amoxicillin (80 to 90 mg per kg per day in two divided doses) is first-line therapy unless the patient has taken amoxicillin for AOM in the previous 30 days or has concomitant purulent conjunctivitis; amoxicillin/clavulanate is typically used in this case. Cefdinir or azithromycin should be the first-line antibiotic in those with penicillin allergy based on risk of cephalosporin allergy. Tympanostomy tubes should be considered in children with three or more episodes of AOM within six months or four episodes within one year with one episode in the preceding six months. Pneumococcal and influenza vaccines and exclusive breastfeeding until at least six months of age can reduce the risk of AOM.
Acute otitis media (AOM) is commonly diagnosed in children in primary care offices. It is also a leading contributor to antibiotic prescriptions and medical costs in children. 1 This article provides a summary and review of the best, most recent evidence to guide the diagnosis and treatment of AOM.
| Practice guideline from the AAP, which is based on consistent evidence from observational studies | ||
| , | Expert opinion and practice guideline from the AAP, which is based on consistent evidence from observational studies | |
| Practice guideline from the AAP, which is based on consistent evidence from observational studies | ||
| , | Practice guideline from the AAP, which is based on consistent evidence from observational studies; Cochrane review on antibiotics for acute otitis media in children | |
| Practice guideline from the AAP, which is based on consistent evidence from observational studies |
| Do not prescribe antibiotics for otitis media in children two to 12 years of age with nonsevere symptoms if the observation option is reasonable. | American Academy of Family Physicians |
Epidemiology
AOM is the most common diagnosis in childhood acute sick visits, accounting for 13.6 million office visits among children annually. 1
The incidence of AOM peaks between six and 15 months of age. 2
AOM is marginally more common in boys than in girls. 2
By three years of age, 50% to 85% of children experience at least one episode of AOM. However, after 24 months of age, the risk decreases with increasing age. 2 , 3
Risk factors for AOM are shown in Table 1 . 2 , 4 The most common causative bacterial species are Streptococcus pneumoniae , Haemophilus influenzae , and Moraxella catarrhalis . 5 , 6
| Age younger than five years |
| Craniofacial abnormalities |
| Family history of ear infections |
| Low birth weight (less than 2.5 kg [5 lb, 8 oz]) |
| Male sex |
| Premature birth (before 37 weeks of gestation) |
| Prior ear infections |
| Recent viral upper respiratory tract infection |
| White ethnicity |
| Exposure to tobacco smoke or environmental air pollution |
| Factors increasing crowded living conditions (e.g., cold seasons, low socioeconomic level, day care/school) |
| Gastroesophageal reflux |
| Lack of breastfeeding |
| Pacifier use after six months of age |
| Supine bottle feeding (bottle propping) |
In addition to ear pain, AOM is commonly associated with fever, irritability, otorrhea, anorexia, and sometimes vomiting or lethargy. 2
The diagnosis is made clinically using common symptoms and findings on examination of the tympanic membrane. 7
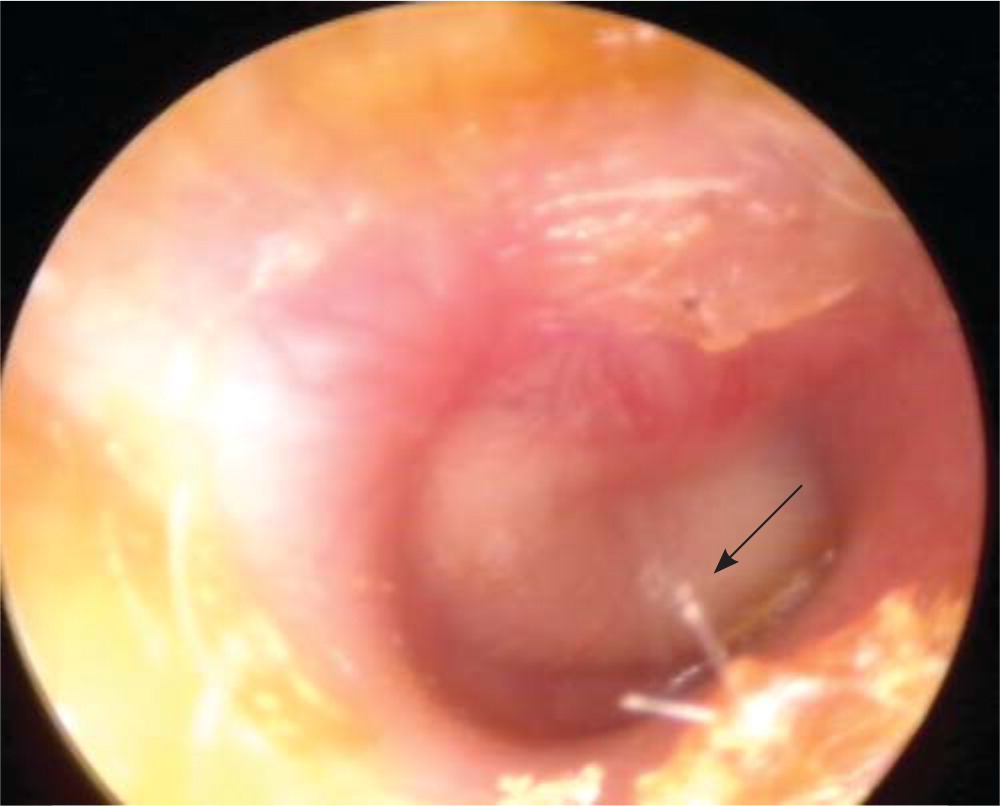
AOM should be diagnosed in symptomatic children with moderate to severe bulging of the tympanic membrane ( Figure 1 4 ) or new-onset otorrhea not caused by otitis externa. 7 It can also be diagnosed in children with mild bulging and either recent-onset ear pain (less than 48 hours) or intense erythema of the tympanic membrane. Ear pain can be assumed in fussy, nonverbal children who hold, tug, or rub the ear. 7
AOM should not be diagnosed without evidence of middle ear effusion on pneumatic otoscopy or tympanometry. 7
Otitis media with effusion is often misdiagnosed as AOM. Otitis media with effusion can be distinguished on physical examination by a neutral or retracted (not bulging) tympanic membrane with an amber or blue (not white or pale yellow) hue. Air fluid levels, however, may be present in both conditions. 8
Pneumatic otoscopy should be used for the assessment of the tympanic membrane . 4 , 7 Pneumatic otoscopy is up to 94% sensitive and 90% specific for identifying middle ear effusion. 4 , 9
Tympanometry can be used as an adjunct to pneumatic otoscopy. Tympanometry is also 70% to 94% sensitive and 90% specific for identifying middle ear effusion. 4 , 9
Tympanocentesis is the diagnostic standard for identifying the causative bacteria in the middle ear fluid. However, this procedure is impractical in a primary care clinic, and it rarely changes initial management because the common bacterial pathogens are predictable. 5 However, tympanocentesis may be considered to guide treatment in children with ongoing severe symptoms despite treatment with multiple antibiotics by identifying the offending pathogen and its antibiotic susceptibility. 7
Table 2 lists treatment strategies based on age, symptoms, and physical examination findings. 7
| AOM with otorrhea | Antibiotic therapy |
| AOM with severe symptoms or if follow-up cannot be guaranteed | Antibiotic therapy |
| Bilateral AOM without otorrhea | Six months to two years of age: antibiotic therapy |
| Two years and older: antibiotic therapy or observation without initial antibiotic treatment | |
| Unilateral AOM without otorrhea | Antibiotic therapy or observation without initial antibiotic treatment† |
ANTIBIOTIC THERAPY
The resolution rate of AOM in children is 81% without antibiotic treatment vs. 93% with antibiotic treatment. 1 Thus, antibiotics have limited benefits compared with the potential adverse effects, such as rash, vomiting, or diarrhea. 10
Antibiotic treatment of AOM in children does not decrease early pain (before 24 hours), hearing loss at three months, or recurrence within 30 days. 10
Antibiotic treatment has some beneficial effect on pain after 24 hours (up to 12 days), number of tympanic membrane perforations, and contralateral otitis media. 10 Children younger than two years with bilateral otitis media or otitis media with otorrhea benefit most from antibiotics. 10
If antibiotics are used for AOM, high-dose amoxicillin (80 to 90 mg per kg per day in two divided doses) is first-line therapy , unless the child has taken antibiotics for AOM in the previous 30 days, has purulent conjunctivitis, or has a penicillin allergy. 7
Observation for 48 to 72 hours with deferment of antibiotics should be considered in lower-risk children with AOM. 7 , 10
Amoxicillin/clavulanate (Augmentin) should be the initial antibiotic for children who have taken amoxicillin for AOM in the previous 30 days or who have purulent conjunctivitis. 7
Single-dose intramuscular ceftriaxone is as effective as amoxicillin for isolated episodes of AOM. However, ceftriaxone should not be used as a first-line treatment, because there are limited options if treatment fails. 7
Cefdinir or azithromycin (Zithromax) should be the first-line antibiotic in those with penicillin allergy based on risk of cephalosporin allergy.
Antibiotic treatment failure is defined as diagnosis of AOM in the 30 days following treatment initiation or severe symptoms that do not resolve within 48 to 72 hours of treatment initiation and unimproved findings on tympanic membrane examination. 7
Lack of resolution of AOM is likely secondary to beta-lactamase–producing H. influenzae or M. catarrhalis ; amoxicillin/clavulanate should be used for treatment if amoxicillin fails. 7
Duration of therapy is based on patient age and severity of symptoms. A 10-day course of antibiotics is recommended if the child is younger than two years or has severe symptoms. A five- to seven-day course is effective if the child is two years or older and does not have severe symptoms. 7
Figure 2 is an algorithm for the treatment of AOM in children requiring antibiotics. 7
PAIN MANAGEMENT
Pain should be treated as needed in children with AOM . 7 Monotherapy with oral ibuprofen or acetaminophen provides short-term (less than 48 hours) relief of ear pain secondary to AOM. Evidence is insufficient to establish that one of these medications is superior to the other or that combined therapy provides better pain relief. 11 Caregivers should be counseled on appropriate use of these pain medications. 7
Topical anesthetic eardrops and naturopathic eardrops have been found to decrease pain in some small studies, but overall evidence is insufficient to recommend routine use. 12 , 13 They should be avoided if there is any concern for tympanic membrane perforation. 7
There is limited evidence for the benefit of home remedies, such as distraction, external application of heat or cold, and oil drops into the external auditory canal. 7
For children younger than two years, follow-up of AOM can typically occur at the next scheduled wellness visit or three months after completing treatment to ensure resolution of middle ear fluid. For children two years and older without an upcoming visit or children with recurrent AOM, reevaluation within three months of completing treatment should be considered to ensure resolution of middle ear effusion. 14
Susceptibility to AOM is complex and not well understood, and it likely includes a combination of genetic, anatomic, and environmental factors. 2
The previous heptavalent pneumococcal vaccine reduced the relative risk of AOM by 5% to 6% in high-risk children and up to 6% in low-risk children. For AOM caused specifically by pneumococcus, the relative risk reduction was 20% to 25%. It is difficult to assess the effect of the current 13-valent pneumococcal conjugate vaccine (Prevnar 13) on prevention of AOM, but a recent study showed that the extra six serotypes result in an 86% risk reduction of pneumococcal-specific AOM in middle ear fluid compared with the heptavalent vaccine. 16 All children should receive pneumococcal vaccination according to guidelines from the Advisory Committee on Immunization Practices. 17
AOM often follows a viral upper respiratory tract infection. Influenza vaccination leads to a 4% absolute reduction in AOM episodes and a 30% to 55% reduction in AOM during the respiratory illness season. 7 , 18 Children older than six months should receive annual influenza vaccination. 19
Breastfeeding reduces the risk of AOM. Longer duration of breastfeeding provides greater protection for children younger than two years. 20 Exclusive breastfeeding until six months of age reduces the risk by 43%. 7 , 20
Xylitol (chewing gum, lozenges, or syrup) reduces the occurrence of AOM in children attending day care by 25%. Evidence for the benefit of xylitol in children prone to otitis media or in children with an acute respiratory infection is inconclusive. Adverse effects of xylitol include abdominal pain and rash. 21 Xylitol must be used multiple times per day for the entire respiratory illness season to be effective, leading to poor compliance. 22
Evidence is mixed on the benefit of zinc supplementation for the prevention of AOM in healthy children younger than five years. 23
Weak evidence exists for eliminating tobacco smoke exposure, avoiding supine bottle feeding (bottle propping), and reducing or eliminating pacifier use after six months of age in the prevention of AOM and AOM recurrences. However, given the risk of tobacco smoke exposure on overall health, avoidance is recommended. 7 , 24
Recurrent AOM
Referral to an otolaryngologist for possible tympanostomy tube placement should be considered in children with three or more episodes of AOM within six months or four episodes within one year with one episode in the preceding six months. 7
Tympanostomy tubes should not be placed in children with recurrent AOM if no middle ear effusion is noted at the time of otolaryngologist evaluation. 25
Possible long-term sequelae of tympanostomy tubes include structural changes to the tympanic membrane, such as focal atrophy, tympanosclerosis, retraction pockets, and chronic perforation; cholesteatoma; and chronic otorrhea. 26 These risks should be weighed against the risks associated with chronic otitis media with effusion, including decreased academic performance, vestibular problems, behavioral issues, and overall decreased quality of life. 25
Prophylactic antibiotics should not be prescribed to reduce the frequency of AOM episodes in children with recurrent AOM. They have not been shown to be effective and increase rates of microbial resistance. 7
Special Considerations for Infants
Infants eight weeks and younger are at greater risk of severe sequelae from AOM, including sepsis, meningitis, and mastoiditis. 4
Group B streptococci, gram-negative enteric bacteria, and Chlamydia trachomatis are common pathogens found in the middle ear fluid of neonates younger than two weeks, and a full sepsis workup should be completed for any neonate younger than two weeks with fever and apparent AOM. 26 , 27 Antibiotics should be initiated for sepsis as indicated. Amoxicillin is the first-line antibiotic for neonates older than two weeks. 26 , 27
Special Considerations for Adults
Treatment of AOM in adults is largely extrapolated from studies of treatment in children, with amoxicillin as the recommended first-line antibiotic.
There are no data on observation instead of treatment in adults with AOM. Therefore, adults should be treated with antibiotics at initial presentation to prevent complications.
Adults with recurrent AOM (more than two episodes per year) or otitis media with effusion that persists for more than six weeks should be referred to an otolaryngologist to be evaluated for mechanical eustachian tube obstruction. 4
Practical Considerations
To allow visualization of the tympanic membrane, attempts should be made to safely remove cerumen obstruction/impaction using ceruminolytics, irrigation, or manual removal. No one ceruminolytic has been shown to be superior. 28 If visualization remains difficult, cerumen removal should be attempted again the next day or the patient should be referred to an otolaryngologist. 29 Cerumen impaction was covered previously in American Family Physician . 30
Tympanometry can be difficult in young children. If adequate readings cannot be obtained, cerumen should be removed and proper fit of the device tip should be ensured, then tympanometry reattempted. If this fails, visualized insufflation may be attempted to look for movement of the tympanic membrane.
Other causes of ear pain and erythema of the tympanic membranes, including vascular engorgement from crying, viral and hemorrhagic myringitis, and aberrant tympanic membrane vessels, should be considered before diagnosing AOM. 31
Parents should be counseled that fever and ear pain may persist for 48 to 72 hours after initiation of antibiotics. However, parents should seek care immediately if the child is vomiting or has a high fever, headaches, or pain behind the ear.
This article updates previous articles on this topic by Harmes, et al. 4 ; Ramakrishnan, et al. 32 ; and Pichichero . 33
Data Sources: A PubMed search was completed in Clinical Queries using the key terms pediatric, children, acute otitis media, evaluation, treatment, and antibiotic management. We reviewed the updated Agency for Healthcare Research and Quality Evidence Report on the management of acute otitis media, which included a systematic review of the literature through October 2018. Also searched were Essential Evidence Plus, Clinical Evidence, Google Scholar, and the Cochrane database. Reference lists of retrieved articles were also searched. Search dates: September to October 2018 and May 2019.
The views expressed in this material are those of the authors and do not reflect the official policy or position of the U.S. government, Department of Defense, or Department of the Air Force.
Coco AS. Cost-effectiveness analysis of treatment options for acute otitis media. Ann Fam Med. 2007;5(1):29-38.
Qureishi A, Lee Y, Belfield K, et al. Update on otitis media - prevention and treatment. Infect Drug Resist. 2014;7:15-24.
Klein JO. Epidemiology of otitis media. Pediatr Infect Dis J. 1989;8(1 suppl):S9.
Harmes KM, Blackwood RA, Burrows HL, et al. Otitis media: diagnosis and treatment [published correction appears in Am Fam Physician . 2014;89(5):318]. Am Fam Physician. 2013;88(7):435-440. Accessed July 17, 2019. https://www.aafp.org/afp/2013/1001/p435.html
Pumarola F, Marès J, Losada I, et al. Microbiology of bacteria causing recurrent acute otitis media (AOM) and AOM treatment failure in young children in Spain: shifting pathogens in the post-pneumococcal conjugate vaccination era. Int J Pediatr Otorhinolaryngol. 2013;77(8):1231-1236.
Chen YJ, Hsieh YC, Huang YC, et al. Clinical manifestations and microbiology of acute otitis media with spontaneous otorrhea in children. J Microbiol Immunol Infect. 2013;46(5):382-388.
Lieberthal AS, Carroll AE, Chonmaitree T, et al. The diagnosis and management of acute otitis media [published correction appears in Pediatrics . 2014;133(2):346]. Pediatrics. 2013;131(3):e964-e999.
Shaikh N, Hoberman A, Rockette HE, et al. Development of an algorithm for the diagnosis of otitis media. Acad Pediatr. 2012;12(3):214-218.
Rovers MM, Schilder AG, Zielhuis GA, et al. Otitis media [published correction appears in Lancet . 2004;363(9414):1080]. Lancet. 2004;363(9407):465-473.
Venekamp RP, Sanders SL, Glasziou PP, et al. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2015(6):CD000219.
Sjoukes A, Venekamp RP, van de Pol AC, et al. Paracetamol (acetaminophen) or non-steroidal anti-inflammatory drugs, alone or combined, for pain relief in acute otitis media in children. Cochrane Database Syst Rev. 2016(12):CD011534.
Bolt P, Barnett P, Babl FE, et al. Topical lignocaine for pain relief in acute otitis media: results of a double-blind placebo-controlled randomised trial. Arch Dis Child. 2008;93(1):40-44.
Foxlee R, Johansson A, Wejfalk J, et al. Topical analgesia for acute otitis media. Cochrane Database Syst Rev. 2006(3):CD005657.
Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical practice guideline: otitis media with effusion executive summary (update). Otolaryngol Head Neck Surg. 2016;154(2):201-214.
Fortanier AC, Venekamp RP, Boonacker CW, et al. Pneumococcal conjugate vaccines for preventing acute otitis media in children. Cochrane Database Syst Rev. 2019(5):CD001480.
Pichichero M, Kaur R, Scott DA, et al. Effectiveness of 13-valent pneumococcal conjugate vaccination for protection against acute otitis media caused by Streptococcus pneumoniae in healthy young children: a prospective observational study. Lancet Child Adolesc Health. 2018;2(8):561-568.
Centers for Disease Control and Prevention. Pneumococcal vaccine recommendations. Accessed May 15, 2019. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/recommendations.html
Norhayati MN, Ho JJ, Azman MY. Influenza vaccines for preventing acute otitis media in infants and children. Cochrane Database Syst Rev. 2017(10):CD010089.
Centers for Disease Control and Prevention. Flu (influenza). Accessed May 15, 2019. https://www.cdc.gov/vaccines/vpd/flu/index.html
Bowatte G, Tham R, Allen KJ, et al. Breastfeeding and childhood acute otitis media: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):85-95.
Azarpazhooh A, Lawrence HP, Shah PS. Xylitol for preventing acute otitis media in children up to 12 years of age. Cochrane Database Syst Rev. 2016(8):CD007095.
Danhauer JL, Johnson CE, Baker JA, et al. Will parents participate in and comply with programs and regimens using xylitol for preventing acute otitis media in their children?. Lang Speech Hear Serv Sch. 2015;46(2):127-140.
Gulani A, Sachdev HS. Zinc supplements for preventing otitis media. Cochrane Database Syst Rev. 2014(6):CD006639.
Salah M, Abdel-Aziz M, Al-Farok A, et al. Recurrent acute otitis media in infants: analysis of risk factors. Int J Pediatr Otorhinolaryngol. 2013;77(10):1665-1669.
Rosenfeld RM, Schwartz SR, Pynnonen MA, et al. Clinical practice guideline: tympanostomy tubes in children. Otolaryngol Head Neck Surg. 2013;149(1 suppl):S1-S35.
Nozicka CA, Hanly JG, Beste DJ, et al. Otitis media in infants aged 0–8 weeks: frequency of associated serious bacterial disease. Pediatr Emerg Care. 1999;15(4):252-254.
Turner D, Leibovitz E, Aran A, et al. Acute otitis media in infants younger than two months of age: microbiology, clinical presentation and therapeutic approach. Pediatr Infect Dis J. 2002;21(7):669-674.
Michaudet C, Malaty J. Cerumen impaction: diagnosis and management. Am Fam Physician. 2018;98(8):525-529. Accessed July 17, 2019. https://www.aafp.org/afp/2018/1015/p525.html
Rettig E, Tunkel DE. Contemporary concepts in management of acute otitis media in children. Otolaryngol Clin North Am. 2014;47(5):651-672.
Michaudet C, Malaty J. Cerumen impaction: diagnosis and management. Am Fam Physician. 2018;98(8):525-529. Accessed June 18, 2019. https://www.aafp.org/afp/2018/1015/p525.html
Earwood JS, Rogers TS, Rathjen NA. Ear pain: diagnosing common and uncommon causes. Am Fam Physician. 2018;97(1):20-27. Accessed July 17, 2019. https://www.aafp.org/afp/2018/0101/p20.html
Ramakrishnan K, Sparks RA, Berryhill WE. Diagnosis and treatment of otitis media [published correction appears in Am Fam Physician . 2008;78(1):30]. Am Fam Physician. 2007;76(11):1650-1658. Accessed July 18, 2019. https://www.aafp.org/afp/2007/1201/p1650.html
Pichichero ME. Acute otitis media: part I. Improving diagnostic accuracy. Am Fam Physician. 2000;61(7):2051-2056. Accessed July 18, 2019. https://www.aafp.org/afp/2000/0401/p2051.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

Acute otitis media
Citation, doi, disclosures and case data.
At the time the case was submitted for publication Bálint Botz had no recorded disclosures.
Presentation
Purulent right ear discharge with headache, nausea, and vertigo. Prior history of operated cholesteatoma on the right. Intracranial abscess?
Patient Data
Bilateral mastoid air cell hypoplasia and opacification. On the symptomatic right side the middle ear is also opacified, but as much as it can be appreciated on a standard head CT the ossicular chain appears normal. No pathological enhancement after iv. contrast, incidental right frontal DVA noted.
Altogether findings are highly suggestive of otitis media on the right.
Follow-up MRI after antibiotic therapy to differentiate potential underlying cholesteatoma.
Partial fluid signal filling the right tympanic cavity and mastoid air cells but no findings indicative of cholesteatoma.
Case Discussion
The case demonstrates that otitis media can present with minimal morphological changes on imaging, and that these have to be correlated clinically to provide a correct interpretation.
2 public playlists include this case
- InteGrated Head & Neck by Marsel N L
- Enfektif by Yasin Aydın
Related Radiopaedia articles
- Developmental venous anomaly
- Otitis media
Promoted articles (advertising)
How to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers


IMAGES
VIDEO
COMMENTS
Case study 91 Acute otitis media 1. Which five characteristics/functions are assessed in determining an Apgar score for a newborn infant? The five characteristics assessed are heart rate, muscle tone, respiratory effort, skin color, and
In a prospective Finnish cohort study, earache was about 7 times more likely to be elicited from a child with AOM than from a child who did not have AOM (LR, 7.3). 26 However, a more important finding is that 40% (48/121) of the children with AOM in this study had no apparent earache (LR for no earache, 0.4).
View Case Study 91- Acute Otitis Media.docx from NUR 3125 at Palm Beach State College. Case Study 91: Acute Otitis Media 1. Which 5 characteristics/functions are assessed in determining an APGAR
Acute otitis media is defined as an infection of the middle ear space. It is a spectrum of diseases that includes acute otitis media (AOM), chronic suppurative otitis media (CSOM), and otitis media with effusion (OME). Acute otitis media is the second most common pediatric diagnosis in the emergency department, following upper respiratory infections. Although otitis media can occur at any age ...
Read chapter 2 of Infectious Diseases: A Case Study Approach online now, exclusively on AccessPharmacy. AccessPharmacy is a subscription-based resource from McGraw Hill that features trusted pharmacy content from the best minds in the field. ... Acute Otitis Media. In: Cho JC. Cho J.C.(Ed.), Ed. Jonathan C. Cho. eds. Infectious Diseases: A Case ...
A female aged 9 years with a recent episode of acute otitis media (AOM) presented to her primary care physician with complaints of severe abdominal pain with right lower quadrant rebound tenderness, suggestive of an acute surgical abdomen. Neurological examination was normal on presentation. She was transferred to the local children's ...
Acute otitis media is extremely common in children. In fact, it is one of the most common diagnosis in children who are seen in outpatient settings, and is one of the most common reasons for antibiotic therapy. The peak incidence of AOM is between 6 months and 2 years of age. Three out of four children will experience at least one ear infection ...
View Case study 91 Acute otitis media and 95.docx from NUR 3125 at Palm Beach State College. Case study 91 Acute otitis media, page 438 answer all 14 questions 1. Which five characteristics/functions
Case Challenge: Acute Otitis Media in Children--Best Management Strategies. Gordon H. Sun, MD, MS. Disclosures. March 28, 2018. ... Acute Otitis Media in Young Children Today; 2001.
Acute Otitis Media Case Study - p. Pathophysiology: This is an infection in the middle ear. The course of infection is associated with a preceding respiratory infection, inflammation, and accumulation of secretions produced by the middle ear mucosa. Features involved: middle ear Risk factors: having a respiratory infection Discriminating features: Acute ear pain, enlarged periauricular lymph ...
Acute otitis media is the second most common pediatric diagnosis in the emergency department, following upper respiratory infections. Although otitis media can occur at any age, it is most commonly seen between the ages of 6 to 24 months. Infection of the middle ear can be viral, bacterial, or coinfection. The most common bacterial organisms ...
Continue Reading. Acute otitis media (AOM) is the most common diagnosis in childhood acute sick visits. By three years of age, 50% to 85% of children will have at least one episode of AOM ...
View Acute Otis Media.doc from BIOLOGY 2116 at Trinidad State Junior College. Case Study 91: Acute Otitis Media History of present illness K.J. is a 17-month-old Winnebago Indian female who is
Documentation Tips. Reporting otitis media in ICD-10 allows for the differentiation between an acute episode versus an acute episode of a recurrent infection. Guidelines of otitis media coding state that if there is a smoking or smoking exposure history in the patient environment, and additional code should be used to indicate that exposure.
Patient Case Question 5. Identify seven risk factors that are consistent with a diagnosis of acute otitis media in this patient. Seven risk factors that are consistent with a diagnosis of acute otitis media in this patient are: 1. exposure to secondhand smoke by her father, 2. recent upper respiratory infection, 3. attending daycare, 4. being around other children who are sick, 5. supplemental ...
The case demonstrates that otitis media can present with minimal morphological changes on imaging, and that these have to be correlated clinically to provide a correct interpretation. 2 public playlists include this case
Acute Otitis Media Case Study - p. 1. Provide a definition of the pathophysiology to the cellular level and link to the most common signs and symptoms. Explain the pathophysiologic and anatomic features involved. a middle ear infection that comes on quickly. It mostly happens to kids, but it can happen to people of any age.
Various epidemiologic studies report the prevalence rate of acute otitis media to be 17-20% within the first two years of life. One-third of children experience six or more episodes of otitis media by age 7 years. Peak prevalence of otitis media in both sexes occurs in children aged 6 to 18 months
View Case study 91 Acute otitis media and 95.docx from NUR 3125 at Palm Beach State Col... group case study (RF).docx. Mercyhurst University. BIO 254. Streptococcus pyogenes. Rheumatic fever. group case study (RF).docx. View group case study (RF).docx from BIO 254 at Mercyhurst University. 1. List 16 clini...
Case study 91 Acute otitis media 1. Which five characteristics/functions are assessed in determining an Apgar score for a newborn infant? The five characteristics assessed are heart rate, muscle tone, respiratory effort, skin color, and reflex irritability. 2. Why is Prevnar an important vaccine for this patient?
CASE PRESENTATION- ACUTE OTITS MEDIA - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Obstruction of the eustachian tube due to upper respiratory tract infections is a key factor in the development of acute otitis media (AOM). Viruses commonly cause the initial infection in the nasopharynx, leading to inflammation ...
Enhanced Document Preview: Case Study 91: Acute Otitis Media Patient Case Question 1. Which five characteristics/functions are assessed in determining an Apgar score for a newborn infant? Five characteristics that are assessed to determine an Apgar score are appearance, which is the skin color, pulse, grimace, which is reflex irritability, activity, which is muscle tone, and respiration.
View Case Study 95,91 .docx from NUR 3125 at Palm Beach State College. Ivelisa Castrejon Romero NUR 3125 Professor Sirota Case Study #91,95 Case study 91 Acute otitis media, 1. APGAR score assesses