

Inter-Rater Reliability Testing For Utilization Management Staff
- Full text of this article is available in PDF
Introduction
Recent regulatory pressures and certification requirements have heightened the need for payer organizations to abide by specific standards regarding medical management operations. Payer organizations that are making medical-necessity determinations regarding reimbursement for health care services, as well as risk-bearing provider groups to whom some of these functions have been delegated, must insure consistency and appropriateness in their determinations. The most powerful accreditation body for health care payers, the National Committee for Quality Assurance (NCQA), requires that payer organizations carry out periodic inter-rater reliability assessments to insure consistency in medical management decision making.
An inter-rater reliability assessment or study is a performance-measurement tool involving a comparison of responses for a control group (i.e., the “raters”) with a standard. Inter-rater reliability (also called inter-observer reliability) traditionally refers to how well two or more raters agree and is derived from the correlation of different raters’ judgments. For the purposes of this paper, inter-rater reliability is a measurement of how well raters agree with a standard, which is more of an assessment of the validity of the responses. The purpose of the study is to determine whether the raters have been consistently trained and are applying that training in a consistent fashion. The analysis is intended to gauge the raters’ observations and reactions resulting from a specific situation. The principles discussed herein would apply to any set of utilization management guidelines.
An inter-rater reliability assessment can be used to measure the level of consistency among a plan or provider group’s utilization management staff and adherence to organizational medical management criteria or standards. Reasons for conducting an inter-rater reliability study within an organization include:
- Minimizing variation in the application of clinical guidelines;
- Evaluating staff’s ability to identify potentially avoidable utilization;
- Evaluating staff’s ability to identify quality-of-care issues;
- Targeting specific areas most in need of improvement;
- Targeting staff needing additional training; and
- Avoiding litigation due to inconsistently applied guidelines.
NCQA requires that health plans develop and implement an inter-rater reliability process for Health Plan Employer Data and Information Set (HEDIS) compliance. NCQA is an independent review organization dedicated to evaluating and reporting on the quality of managed care organizations. HEDIS is a set of standardized performance measures developed by NCQA with assistance from managed care organizations and employers concerned with quality health care. The performance indicators in HEDIS are continually developing, but most involve measuring access to care, health plan service, provider qualifications, activities that assist people to recover from illness, and management of chronic illness. The combination of these measures is intended to provide a tool for performance comparison of different health plans.
An inter-rater reliability study can provide measurement of many of these quality indicators. It can most readily be used to measure access, as NCQA looks for “fair and consistent health plan decisions about medical treatments and services provided to plan members.” It also can be used to measure service, as NCQA looks for “actual improvements that the plan has made in care and service” (“What NCQA Looks for in a Health Plan,” «http://www.ncqa.org»). This latter indicator can be measured by reviewing the results of the inter-rater reliability study from year to year.
An inter-rater reliability assessment can be a useful tool for a health plan or provider organization. However, as with any benchmarking exercise, it cannot in and of itself enhance performance. To improve outcomes, the assessment must be followed up by analysis of the results and, most importantly, by action.
Medical management clinical guidelines, whether developed internally or purchased and then adjusted to meet specified objectives and local practice standards, are an extension of the organization’s overall philosophies and goals. It is essential to the future viability of the plan or provider organization, the welfare of members and corporate partners, and the organization’s standing in the community that they be applied appropriately and in a uniform fashion. Periodic benchmarking of clinical guideline application via an inter-rater reliability study is one way for an organization to insure its intentions for utilization management are met.
This paper will examine several elements that health plans or provider groups with utilization management responsibilities should consider when designing and implementing an inter-rater reliability study. The example presented illustrates some aspects of the process. The example, although fairly simple, demonstrates how easily an inter-rater reliability study can be performed. However, inter-rater reliability is a complex concept, and a much more detailed analysis is possible. End users of any inter-rater reliability analysis should be advised of the method and depth of the analysis to avoid confusion or misunderstandings.
- Link to full text of this article in PDF

Paul Lendner ist ein praktizierender Experte im Bereich Gesundheit, Medizin und Fitness. Er schreibt bereits seit über 5 Jahren für das Managed Care Mag. Mit seinen Artikeln, die einen einzigartigen Expertenstatus nachweisen, liefert er unseren Lesern nicht nur Mehrwert, sondern auch Hilfestellung bei ihren Problemen.
Header Text Here...
On-demand informed webinar series, how loma linda university health uses irr to reduce denials.
Please note : This webinar does not offer continuing education credit.
In this webinar, you'll hear how Loma Linda University Health uses Interrater Reliability (IRR) , a module inside the MCG Learning Management System (LMS), to evaluate, test, and develop staff skills for proper guideline use. By integrating denial prevention strategies tied to proper guideline use, Loma Linda has significantly reduced denials. Learn practical tips for using IRR, as well as how to optimize the use of MCG’s LMS to provide a comprehensive training program and develop staff competencies.
Highlights include:
- How IRR is used to evaluate proper guideline use
- How IRR can be set up to target the most-denied types of cases
- How the LMS can be set up to personalize targeted improvement plans for staff
- Ideas you can apply for successfully delivering education to staff
WHO SHOULD VIEW THIS WEBINAR
Directors, managers, staff and physician advisors involved in case management, utilization management, clinical quality and improvement, nursing, denials management, medical informatics, and more will benefit from viewing this webinar.
OTHER WEBINARS
Please visit our Webinars page to see more MCG webinars.

Jump to content

OptumHealth Education
- Create account
Bookmark/Search this post

You are here
Mcg 27th edition ambulatory care interrater reliability.
- Faculty and planners
- Accreditation
- Register/Continue
Activity description
MCG (formerly referred to as Milliman Care Guidelines) is a tool that is used to help clinicians complete case reviews and make clinical decisions. The MCG 27th Edition Interrater Reliability (IRR) consists of scenarios that allow users to demonstrate their ability to use the tool correctly by applying the most appropriate ambulatory care evidence-based guideline to each case review.
Course last reviewed: 3/31/2023
Provided by This activity is provided by Optum Health Education and Optum Care.
Commercial support No commercial support was received for this activity.
Hardware/Software Requirements Please ensure you are using the web-browser Chrome and disable any pop-up blocking software. Click here for information on how to enable pop-ups.
Target Audience
This activity is designed to meet the educational needs of nurses, physicians and pharmacists.
Learning Objectives
At the end of this educational activity, participants should be able to:
- Analyze ambulatory care scenarios, and
- Identify and apply the most appropriate 27th Edition Ambulatory Care evidence-based guideline to inform care decisions.
- 0.50 ACPE - Pharmacists
- 0.50 AMA - Physicians
- 0.50 ANCC - Nurses
- 0.50 Attendance - General Attendance
Faculty/Planners Rebecca Gleason, RN, CCM Clinical Planner OptumHealth Education
Katherine Dittmer BSN, RN Associate Director Clinical Adherence and Remediation Clinical Consistency and Safety Clinical Performance Optum
Jennifer Every BSN, RN, CCM Training Consultant Clinical Adherence and Remediation Clinical Consistency and Safety Clinical Performance Optum
Katie Shelton MSN, RN, CCM Training Consultant Clinical Adherence and Remediation Clinical Consistency and Safety Clinical Performance Optum
Brian J Kennedy, MD MBA Senior Medical Director Clinical Performance Optum
Disclosures of relevant financial relationships In accordance with the Accreditation Council for Continuing Medical Education's (ACCME) Standards for Integrity and Independence in Accredited Continuing Education, Optum Health Education (OHE) requires all those in control of educational content to disclose their financial relationships with ineligible companies within the prior 24 months. Ineligible companies are defined by the ACCME as companies whose primary business is producing, marketing, selling, re-selling, or distributing health care products used by or on patients. Individuals must disclose all financial relationships, regardless of the amount, with ineligible companies and regardless of their view of the relevance of the relationship to the education. OHE ensures that the content is independent of commercial bias.
The activity faculty/planners have no financial relationships to disclose.
Method for calculating CE credit CE credit was calculated by the complexity of content.
Credit Designation Statements
Nurses The participant will be awarded up to 0.50 contact hour(s) of credit for attendance and completion of supplemental materials.
Nurse practitioners The American Academy of Nurse Practitioners Certification Program (AANPCP) accepts credit from organizations accredited by the ACCME and ANCC.
Pharmacists/Pharmacy technicians This activity is approved for 0.50 contact hours ([0.05] CEU) in states that recognize ACPE. Attending the full program will earn 0.50 contact hours. Unique Activity Number(s): JA0007123-9999-23-078-H01-P
Physicians Optum Health Education designates this enduring activity for a maximum of 0.50 AMA PRA Category 1 Credit ™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
PAs The American Academy of Physician Assistants (AAPA) accepts credit from organizations accredited by the ACCME.
Attendance A certificate of attendance will be provided to learners upon completion of activity requirements, enabling participants to register with licensing boards or associations that have not been pre-approved for credits. To apply for credit types not listed above, participants should use the procedure established by the specific organization with which they wish to obtain credit.
Available Credit
Prior to beginning this activity, please ensure you are using the web-browser Chrome and disable any pop-up blocking software. Click here for information on how to enable pop-ups.
You must be logged into your account to participate in this activity. Get started by clicking “Continue” and taking the module “MCG Interrater Reliability”; then follow the prompts at the bottom of the screen. At the end of the activity, you will be able to view, save or print your certificate of participation. A complete listing of all of your activities can be found under “My Account”, “My Activities.”
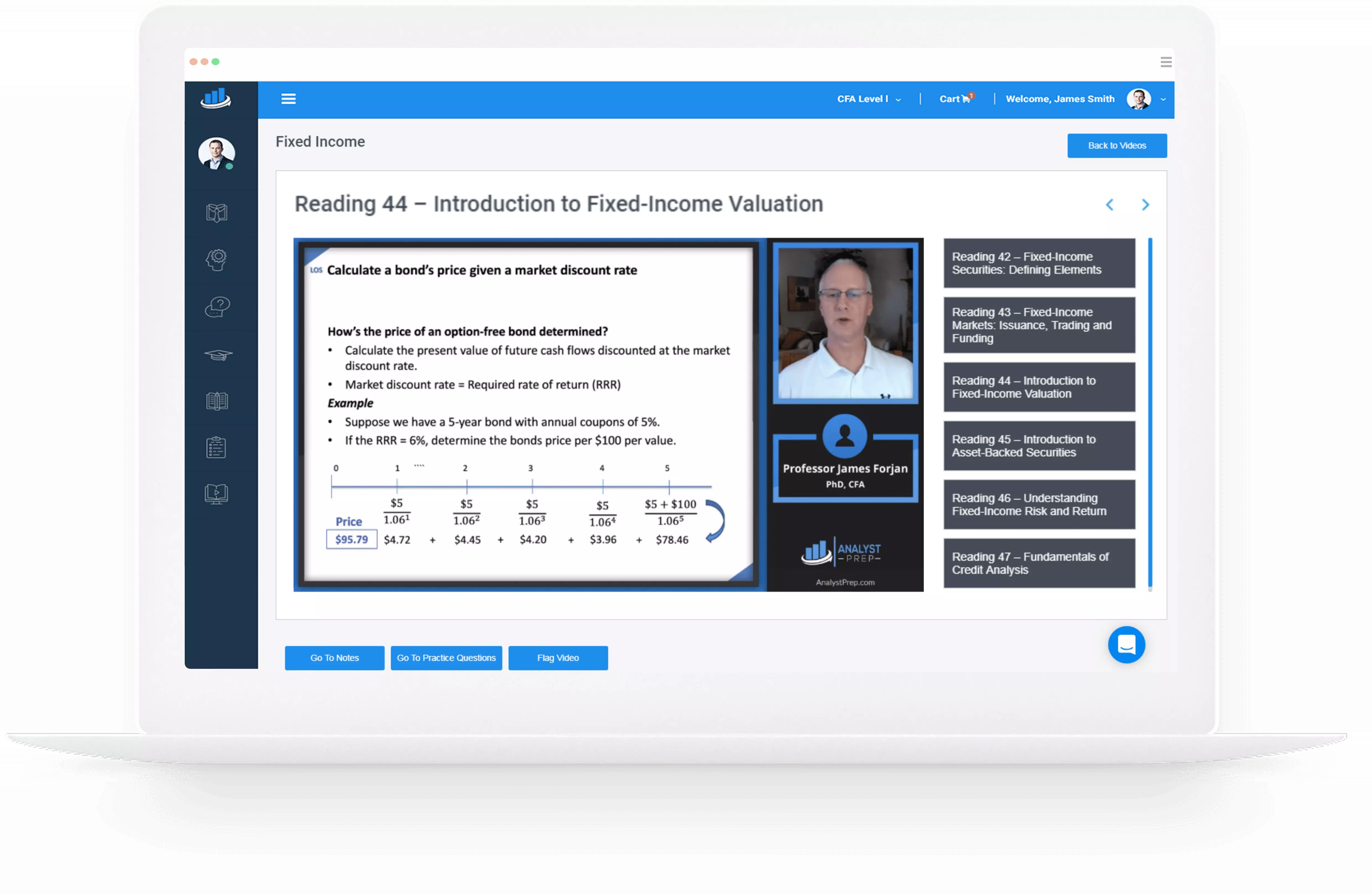
Save 10% on All AnalystPrep 2024 Study Packages with Coupon Code BLOG10 .
- Payment Plans
- Product List
- Partnerships

- Try Free Trial
- Study Packages
- Levels I, II & III Lifetime Package
- Video Lessons
- Study Notes
- Practice Questions
- Levels II & III Lifetime Package
- About the Exam
- About your Instructor
- Part I Study Packages
- Part I & Part II Lifetime Package
- Part II Study Packages
- Exams P & FM Lifetime Package
- Quantitative Questions
- Verbal Questions
- Data Insight Questions
- Live Tutoring
- About your Instructors
- EA Practice Questions
- Data Sufficiency Questions
- Integrated Reasoning Questions


The Internal Rate of Return
The internal rate of return is the discount rate that sets the present value of all cash inflows of a project equal to the present value of all cash outflows of the same project. In other words, it is the effective rate of return that makes a project have a net present value of zero. Thus:
NPV = 0 if r = IRR, for any given project.
PV outgo = PV income when r = IRR
The internal rate of return method of project appraisal assumes that all proceeds from the project can be re-invested immediately, and in projects offering returns equal to the IRR, until maturity. A higher IRR indicates a more “profitable” project.
Interpreting the Internal rate of Return
You should note that the IRR need not be positive – It can be zero or even negative. A positive return indicates that the project makes money for the investor. A zero return indicates that the investor is neither profitable nor loss-making. Lastly, if the IRR is negative, the investor loses money. However, if the IRR is less than -1, it means the yield or rather the return is undefined.
The internal rate of return is usually compared to the cost of capital, usually the weighted average cost of capital, WACC. A project whose IRR is above its WACC increases the shareholders’ wealth. Otherwise, it would be unwise to borrow cash at an interest rate, say, 10% and then invest the money in a project with a rate of return less than 10%. The borrower would be unable to service the loan.
Usually, candidates cannot solve questions involving IRR directly and you may need to carry out linear extrapolation. Working with a spreadsheet or calculator is also a better, easier approach. However, you should aim to understand the manual approach first. It will then be easier to use a calculator.
Question Suppose we have a project with the following cash flows; Outgo: $150,000 at t = 0, $250,000 at t = 1, and some more $250,000 at t = 2 Income: $1 million at t = 3 Find the IRR of the project. A. 25.2% B. 0% C. 23% Solution The correct answer is A. We need to find the rate r such that: $$ -150,000 – 250,000(1 + r)^{-1} – 250,000(1 + r)^{-2} + 1000,000( 1 + r )^{-3} = 0 $$ $$ \text{At } 20\%, -150,000 – 250,000 * 1.2^{-1} – 250,000 * 1.2^{-2} + 1000,000 * 1.2^{-3} = 46,800 $$ $$ \text{At } 25\%, -150,000 – 250,000 * 1.2^{-1} – 250,000 * 1.2^{-2} + 1000,000 * 1.2^{-3} = 2,000 $$ We can approximate r by linear extrapolation using the two values: $$ r = 20\% + \cfrac {(0 – 46,800)}{(2 – 46,800)} * (25\% – 20\%) = 25.2\%$$ Suppose the WACC is 20% in the example above. What would be your advice to investors? Since WACC (20%) is less than IRR (25.2%), the project is economically viable and would increase the investors’ wealth. Conclusion : A capital project should be accepted if its IRR is greater than the cost of capital.
Reading 7 LOS 7a (Part 2)
Calculate and interpret the net present value (NPV) and the internal rate of return (IRR) of an investment.
Quantitative Methods – Learning Sessions
Offered by AnalystPrep
Categories of Valuation Model
Describe the business cycle and its phases, measures of dispersion.
Measures of dispersion are used to describe the variability or spread in a... Read More
Time-series Data vs. Cross-sectional D ...
Cumulative distribution function (cdf).
A cumulative distribution function, \(F(x)\), gives the probability that the random variable \(X\)... Read More
Discrete Random Variables and Outcomes
A discrete random variable can take on a finite or countable number of... Read More
Moving patients toward health proactively and efficiently.
MCG provides unbiased clinical guidance that gives healthcare organizations confidence in their patient-centered care decisions. MCG solutions support clinical decisions that help patients get the right level of care and the appropriate care activities for the right amount of time.
See the Difference
Sign up to receive our newsletter and stay on top of the latest news.

Helping healthcare organizations confidently provide informed, collaborative, and effective care.
MCG’s transparent assessment of the latest research and scholarly articles, along with our own data analysis, gives patients, providers and payers the vetted information they need to feel confident in every care decision, as well as providing a means to have collaborative discussions about care.
MCG helps payer organizations optimally balance the needs of their members, their provider networks, and the bottom line.
With a majority of the largest health plans and thousands of hospitals using our solutions, MCG helps providers align clinical decisions with a common language shared by providers and payers. Providers can lower denial rates and improve patient care.
MCG has more than three decades of experience working with State, Regional, and Federal Government Healthcare Agencies and Government Contractors.
Strategic Partners
MCG works with many healthcare software vendors. Integration allows users to access MCG care guidelines from the electronic health record or within a utilization management workflow.
MCG care guidelines can help patients feel equipped to have a more meaningful conversation with their care team about what is right for them.
Solutions that enable efficient and effective care management
MCG solutions provide the tools that support doing the right thing for the patient throughout the healthcare journey, from the inpatient decision through post-release care.
MCG CARE GUIDELINES
Evidenced-based research compiled annually to present the most effective courses of treatment based on available data.
A web-based software suite developed for payers giving transparency into how care is provided and which strategies provide the best quality care for a member.
A web-based software suite delivering evidence-based care guidelines for aligning care delivery and clinical documentation.


IMAGES
VIDEO
COMMENTS
Enhanced Document Preview: Interrater Reliability Case Study #25-96 Behavioral Health Condition Clinical History - Presenting Status A 50-year-old female presented to the emergency department (ED) with a 4-week history of flashbacks, nightmares, and severe anxiety about her past experiences during the World Trade Center (WTC) terrorist attacks. Past Medical History: Diagnosed with ...
Family / Social History. Engaged to be married. Lives with partner in a 2-bedroom apartment with cat. No children. Denies alcohol or illicit drug use. Patient has good family and friend support system. Both patient and partner work from home as authors. Interrater Reliability Case Study #RMHP-MCaid-2021. Transgender Condition.
Interrater Reliability supports your efforts in meeting URAC and NCQA requirements by documenting the consistent and appropriate use of nationally recognized guidelines, testing your staff's ability to find the right guideline sections and apply them appropriately to a clinician-written case study. Automated grading and record-keeping track ...
Interrater reliability (IRR) is one of the four main types of reliability. It refers to the extent of consistency in scoring (measurement) between two or more raters, observers, judges, or scorers ...
The MCG Interrater Reliability (IRR) consists of scenarios that allow users to demonstrate their ability to use the tool correctly by applying the most appropriate inpatient and surgical care evidence-based guideline to each case review. Course last reviewed: 7/1/2022. This activity is provided by Optum Health Education and Optum.
An inter-rater reliability assessment can be used to measure the level of consistency among a plan or provider group's utilization management staff and adherence to organizational medical management criteria or standards. Reasons for conducting an inter-rater reliability study within an organization include: Minimizing variation in the ...
list of case study tests, test answer keys and a detailed administrator guide to manage system use and report on Interrater Reliability ... MCG - part of the Hearst Health network 901 Fifth Avenue, Suite 2000, Seattle, WA 98164 | 888 464 4746 | www.mcg.com IRR-001 12/16 Care Guidelines Covered: The Interrater Reliability Module offers test ...
IRR has helped MCG clients to achieve measurable improvements in care guideline usage. By consistently using IRR over the course of three years, St. Joseph Health System increased their appropriate guideline-selection rate from 72% all the way up to 89%. Topping that impressive gain, a regional hospital system that attended our 2019 Client ...
why the MCG developed Interrater Reliability or (IRR). IRR is a training tool built to help our clients improve the accuracy and consistency of using their guides. It aims to measure the skills necessary to select and use the guiding(s) that best suit the patient's condition and needs. Tests in the IRR solution include case
Procedure: The IRR process consists of the following: Staff are assigned a minimum of (2) IRR test scenarios based on the types of clinical reviews they perform in Utilization Management (Inpatient, Outpatient, etc.) BSC utilizes MCG's IRR developed tests as they support compliance with federal and state parity mandates as well as URAC and ...
The use of inter-rater reliability (IRR) methods may provide an opportunity to improve the transparency and consistency of qualitative case study data analysis in terms of the rigor of how codes and constructs have been developed from the raw data. Few articles on qualitative research methods in the literature conduct IRR assessments or neglect ...
By integrating denial prevention strategies tied to proper guideline use, Loma Linda has significantly reduced denials. Learn practical tips for using IRR, as well as how to optimize the use of MCG's LMS to provide a comprehensive training program and develop staff competencies. Highlights include: How IRR is used to evaluate proper guideline ...
Study with Quizlet and memorize flashcards containing terms like • Benefit plans vary in coverage and some plans may not provide coverage for certain services discussed in the customized guidelines. Coverage decisions are subject to all terms and conditions of the applicable benefit plan, including specific exclusions and limitations, as well as applicable state and/or federal law. The ...
Boost your workflows: mcg irr case study answers 2021 with airSlate. There's no better way to interrater reliability certification answers 2021 than with airSlate. The automation solution helps you remove tedious and repetitive activities. Using our service, you can concentrate on increasing your effectiveness and developing a more robust ...
Mcg Irr Case Study Answers 2023 WebMCG customers have used IRR to determine the need in the necessary, length of stay, temporary risk, extended stay, and consyent consideration—just to name a few people. For example, ... 2021-07-30 by guest content on immunization and vaccine information for … WebMcg Irr Case Study Answers 2023 The
Currently, MCG care guidelines are licensed by nine of the largest U.S. health plans and over 2,200 hospitals, making them a rare common ground between the payer and provider communities. On March 18, 2021, MCG will offer a free webinar to all MCG clients who wish to learn more about the changes in the 25 th edition.
The MCG 27th Edition Interrater Reliability (IRR) consists of scenarios that allow users to demonstrate their ability to use the tool correctly by applying the most appropriate ambulatory care evidence-based guideline to each case review. Course last reviewed: 3/31/2023. This activity is provided by Optum Health Education and Optum Care.
Lastly, if the IRR is negative, the investor loses money. However, if the IRR is less than -1, it means the yield or rather the return is undefined. The internal rate of return is usually compared to the cost of capital, usually the weighted average cost of capital, WACC. A project whose IRR is above its WACC increases the shareholders' wealth.
Electronic Prior Authorization: The Future of Care Coordination. View the real world case studies of payers and providers who have achieved improvement through use of the healthcare management solutions we provide.
Mcg Irr Case Study Answers 2022 3 3 crisis lies at the intersection of two public health challenges: reducing the burden of suffering from pain and containing the rising toll of the harms that can arise from the use of opioid medications. Chronic pain and opioid use disorder both represent complex human conditions affecting millions of ...
Web"Mcg Irr Case Study Answers 2022," a mesmerizing literary creation penned with a celebrated wordsmith, readers attempt an enlightening odyssey, unraveling the intricate significance of language and its enduring affect our lives. In this appraisal, we shall explore the book is central themes, evaluate its distinctive WebMcg Irr Case Study ...
Case Study. The Future of Case Management: Navigating the Impacts of New Technology. 5/7/2024 Cynthia Young, MBA, BSN, RN, ... For the recently released 28th edition of MCG Inpatient & Surgical Care, there have been more than the usual number of changes to the Goal Length of Stay (GLOS) for both medical and surgical (procedural) Optimal ...
Moving patients toward health proactively and efficiently. MCG provides unbiased clinical guidance that gives healthcare organizations confidence in their patient-centered care decisions. MCG solutions support clinical decisions that help patients get the right level of care and the appropriate care activities for the right amount of time.