- Brain & Nervous System

What to Know About Speech Impairment

A speech impairment affects people who have problems speaking in a regular tone of voice or tempo. Speech impairments make it hard for people to communicate properly, and they can happen in both children and adults.
These disorders can cause frustration and embarrassment to the person suffering from them.
What is Speech Impairment?
People who have speech impairments have a hard time pronouncing different speech sounds. They might distort the sounds of some words and leave other sounds out completely.
There are three general categories of speech impairment:
- Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production.
- Voice disorder. A voice disorder means you have an atypical tone of voice. It could be an unusual pitch, quality, resonance, or volume.
- Articulation disorder. If you have an articulation disorder, you might distort certain sounds. You could also fully omit sounds.
Stuttering , or stammering, is a common fluency disorder that affects about 3 million Americans. It usually affects young children who are just learning to speak, but it can continue on into adulthood.
Speech and language impairments are two words that are often used interchangeably, but they are two very different types of problems.
Speech means talking. It uses the jaw muscles, tongue, lips, and vocal chords. Language is a set of words and symbols made to communicate a message. Language and speech disorders can affect you separately, or both can happen at the same time.
Types of Speech Impairments
Speech impairments can begin in childhood and carry on through your adult years. Others can happen due to trauma, or after a medical event like a stroke.
The types of speech impairments are:
- Childhood apraxia of speech. This can happen to children when it’s time for them to start talking. The brain’s signals don’t communicate with the mouth, so the child can’t move their lips and tongue in the way they’re mean to.
- Dysarthria. This type of speech impairment happens when the muscles you use to talk are too weak, and can’t form words properly.
- Orofacial myofunctional disorders (OMD). OMDs are characterized by an abnormal pattern of facial muscle use. OMD interferes with how the facial muscles, including the tongue, are used. People who suffer from OMD might also struggle to breathe through their nose.
- Speech sound disorders. It’s normal for children to struggle to pronounce certain sounds as they learn to talk. But after ages four or five, constant mispronunciation might signal a problem. It can continue into adulthood, or some people get it after a stroke.
- Stuttering. Stuttering can mean repeating words or sounds like “uh” and “um” (disfluencies) involuntarily. Stuttering can be intensified by strong emotions or stress.
- Voice. A voice disorder can mean you “lost” your voice because you stressed it too much. It can also mean a chronic cough or paralysis of the vocal cords, among others.
Health Issues That Affect Speech Impairment
Other than childhood speech impairments, there are a range of reasons you could get one in your adult years. They can happen due to a traumatic event, illness, or surgery.
Dysarthria , aphasia, and voice disturbances can happen in adulthood, and are usually due to these medical events.
Aphasia. Aphasia is the loss of ability to understand words, spoken or written. There are many types of aphasia . It can happen after a stroke or if a tumor reaches the part of the brain where language is processed.
Medical issues that can cause aphasia:
- Head trauma
- Transient ischemic attack (TIA)
- Brain tumor
- Alzheimer’s disease
Dysarthria. Dysarthria is usually caused by a nerve problem. The person suffering from it loses the ability to make certain sounds or might have poor pronunciation. It can also affect your ability to control the tongue, larynx, lips, and vocal chords.
Medical issues that can cause dysarthria:
- Facial trauma
- Diseases that affect your nervous system
- Side effects of certain medication
- Alcoholic intoxication
- Dentures that don’t fit properly
- Transient ischemic attack (TIA)
Voice disturbances. Traumatic events or extreme stress placed on the vocal cords can cause you to “lose” your voice or have a vocal disturbance. Disease can also affect the way your voice sounds.
Cancerous or noncancerous growths or nodules on the vocal cords can make your voice sound different.
Understanding Speech Impairments
Having a speech impairment can be a very frustrating and embarrassing experience for the person experiencing it. It’s important to be patient and understanding when communicating.
Try the following tips to improve communication and foster an accepting environment with someone who has a speech impairment:
- Speak slowly and use hand gestures
- Keep a pen and paper handy in case it’s needed to communicate
- Maintain a calm environment free of stimulating sounds
- Use simple phrases when you speak
- Use your normal tone of voice
Consulting with a mental health care provider can help with feelings of anger and depression that can accompany speech impairments.
Top doctors in ,
Find more top doctors on, related links.
- Brain & Nervous System News & Features
- Brain & Nervous System Reference
- Brain & Nervous System Slideshows
- Brain & Nervous System Quizzes
- Brain & Nervous System Videos
- Find a Neurologist
- Living Better With MS
- Alzheimer's Disease
- Creutzfeldt-Jakob Disease
- Guillain-Barré Syndrome
- Lou Gehrig’s Disease (ALS)
- Multiple Sclerosis
- Parkinson's Disease
- Restless Legs Syndrome
- Spinal Muscular Atrophy
- More Related Topics
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Types of Speech Impediments
Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
:max_bytes(150000):strip_icc():format(webp)/SanjanaGupta-d217a6bfa3094955b3361e021f77fcca.jpg)
Steven Gans, MD is board-certified in psychiatry and is an active supervisor, teacher, and mentor at Massachusetts General Hospital.
:max_bytes(150000):strip_icc():format(webp)/steven-gans-1000-51582b7f23b6462f8713961deb74959f.jpg)
Phynart Studio / Getty Images
Articulation Errors
Ankyloglossia, treating speech disorders.
A speech impediment, also known as a speech disorder , is a condition that can affect a person’s ability to form sounds and words, making their speech difficult to understand.
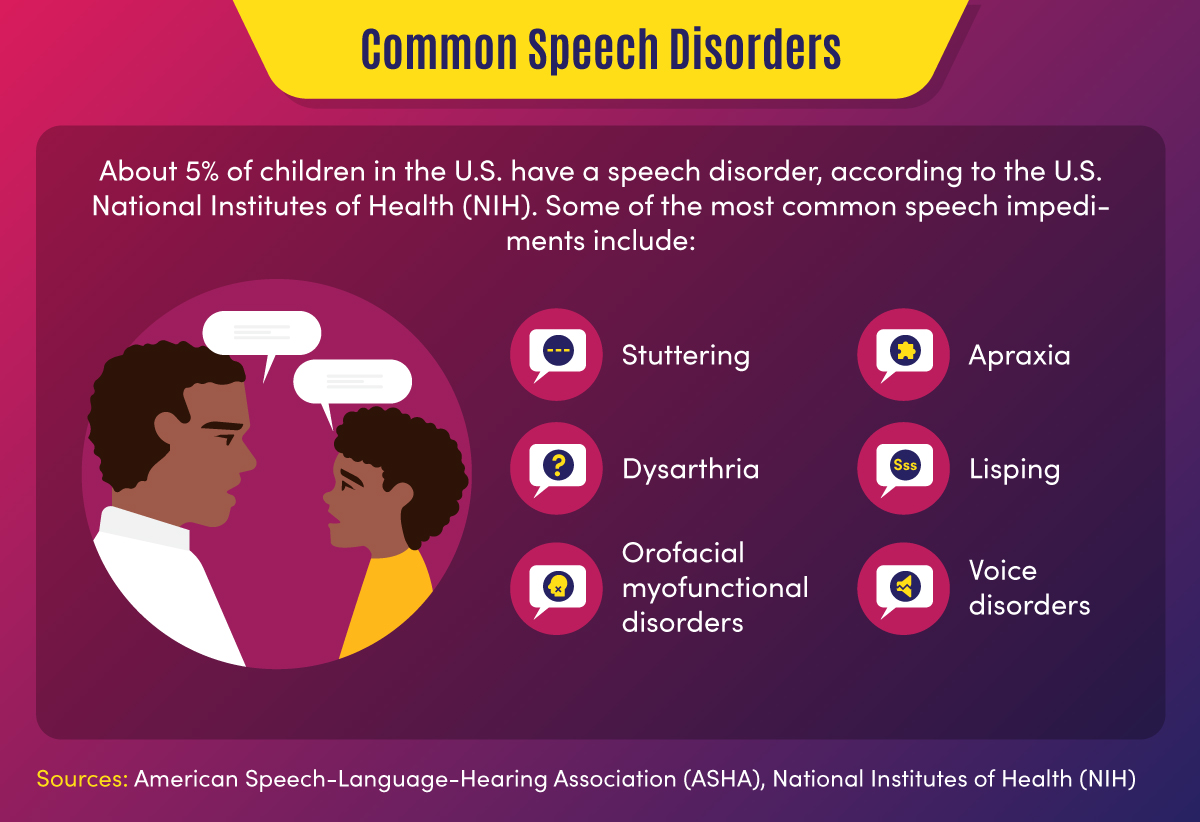
Speech disorders generally become evident in early childhood, as children start speaking and learning language. While many children initially have trouble with certain sounds and words, most are able to speak easily by the time they are five years old. However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders.
There are many different types of speech impediments, including:
- Articulation errors
This article explores the causes, symptoms, and treatment of the different types of speech disorders.
Speech impediments that break the flow of speech are known as disfluencies. Stuttering is the most common form of disfluency, however there are other types as well.
Symptoms and Characteristics of Disfluencies
These are some of the characteristics of disfluencies:
- Repeating certain phrases, words, or sounds after the age of 4 (For example: “O…orange,” “I like…like orange juice,” “I want…I want orange juice”)
- Adding in extra sounds or words into sentences (For example: “We…uh…went to buy…um…orange juice”)
- Elongating words (For example: Saying “orange joooose” instead of "orange juice")
- Replacing words (For example: “What…Where is the orange juice?”)
- Hesitating while speaking (For example: A long pause while thinking)
- Pausing mid-speech (For example: Stopping abruptly mid-speech, due to lack of airflow, causing no sounds to come out, leading to a tense pause)
In addition, someone with disfluencies may also experience the following symptoms while speaking:
- Vocal tension and strain
- Head jerking
- Eye blinking
- Lip trembling
Causes of Disfluencies
People with disfluencies tend to have neurological differences in areas of the brain that control language processing and coordinate speech, which may be caused by:
- Genetic factors
- Trauma or infection to the brain
- Environmental stressors that cause anxiety or emotional distress
- Neurodevelopmental conditions like attention-deficit hyperactivity disorder (ADHD)
Articulation disorders occur when a person has trouble placing their tongue in the correct position to form certain speech sounds. Lisping is the most common type of articulation disorder.
Symptoms and Characteristics of Articulation Errors
These are some of the characteristics of articulation disorders:
- Substituting one sound for another . People typically have trouble with ‘r’ and ‘l’ sounds. (For example: Being unable to say “rabbit” and saying “wabbit” instead)
- Lisping , which refers specifically to difficulty with ‘s’ and ‘z’ sounds. (For example: Saying “thugar” instead of “sugar” or producing a whistling sound while trying to pronounce these letters)
- Omitting sounds (For example: Saying “coo” instead of “school”)
- Adding sounds (For example: Saying “pinanio” instead of “piano”)
- Making other speech errors that can make it difficult to decipher what the person is saying. For instance, only family members may be able to understand what they’re trying to say.
Causes of Articulation Errors
Articulation errors may be caused by:
- Genetic factors, as it can run in families
- Hearing loss , as mishearing sounds can affect the person’s ability to reproduce the sound
- Changes in the bones or muscles that are needed for speech, including a cleft palate (a hole in the roof of the mouth) and tooth problems
- Damage to the nerves or parts of the brain that coordinate speech, caused by conditions such as cerebral palsy , for instance
Ankyloglossia, also known as tongue-tie, is a condition where the person’s tongue is attached to the bottom of their mouth. This can restrict the tongue’s movement and make it hard for the person to move their tongue.
Symptoms and Characteristics of Ankyloglossia
Ankyloglossia is characterized by difficulty pronouncing ‘d,’ ‘n,’ ‘s,’ ‘t,’ ‘th,’ and ‘z’ sounds that require the person’s tongue to touch the roof of their mouth or their upper teeth, as their tongue may not be able to reach there.
Apart from speech impediments, people with ankyloglossia may also experience other symptoms as a result of their tongue-tie. These symptoms include:
- Difficulty breastfeeding in newborns
- Trouble swallowing
- Limited ability to move the tongue from side to side or stick it out
- Difficulty with activities like playing wind instruments, licking ice cream, or kissing
- Mouth breathing
Causes of Ankyloglossia
Ankyloglossia is a congenital condition, which means it is present from birth. A tissue known as the lingual frenulum attaches the tongue to the base of the mouth. People with ankyloglossia have a shorter lingual frenulum, or it is attached further along their tongue than most people’s.
Dysarthria is a condition where people slur their words because they cannot control the muscles that are required for speech, due to brain, nerve, or organ damage.
Symptoms and Characteristics of Dysarthria
Dysarthria is characterized by:
- Slurred, choppy, or robotic speech
- Rapid, slow, or soft speech
- Breathy, hoarse, or nasal voice
Additionally, someone with dysarthria may also have other symptoms such as difficulty swallowing and inability to move their tongue, lips, or jaw easily.
Causes of Dysarthria
Dysarthria is caused by paralysis or weakness of the speech muscles. The causes of the weakness can vary depending on the type of dysarthria the person has:
- Central dysarthria is caused by brain damage. It may be the result of neuromuscular diseases, such as cerebral palsy, Huntington’s disease, multiple sclerosis, muscular dystrophy, Huntington’s disease, Parkinson’s disease, or Lou Gehrig’s disease. Central dysarthria may also be caused by injuries or illnesses that damage the brain, such as dementia, stroke, brain tumor, or traumatic brain injury .
- Peripheral dysarthria is caused by damage to the organs involved in speech. It may be caused by congenital structural problems, trauma to the mouth or face, or surgery to the tongue, mouth, head, neck, or voice box.
Apraxia, also known as dyspraxia, verbal apraxia, or apraxia of speech, is a neurological condition that can cause a person to have trouble moving the muscles they need to create sounds or words. The person’s brain knows what they want to say, but is unable to plan and sequence the words accordingly.
Symptoms and Characteristics of Apraxia
These are some of the characteristics of apraxia:
- Distorting sounds: The person may have trouble pronouncing certain sounds, particularly vowels, because they may be unable to move their tongue or jaw in the manner required to produce the right sound. Longer or more complex words may be especially harder to manage.
- Being inconsistent in their speech: For instance, the person may be able to pronounce a word correctly once, but may not be able to repeat it. Or, they may pronounce it correctly today and differently on another day.
- Grasping for words: The person may appear to be searching for the right word or sound, or attempt the pronunciation several times before getting it right.
- Making errors with the rhythm or tone of speech: The person may struggle with using tone and inflection to communicate meaning. For instance, they may not stress any of the words in a sentence, have trouble going from one syllable in a word to another, or pause at an inappropriate part of a sentence.
Causes of Apraxia
Apraxia occurs when nerve pathways in the brain are interrupted, which can make it difficult for the brain to send messages to the organs involved in speaking. The causes of these neurological disturbances can vary depending on the type of apraxia the person has:
- Childhood apraxia of speech (CAS): This condition is present from birth and is often hereditary. A person may be more likely to have it if a biological relative has a learning disability or communication disorder.
- Acquired apraxia of speech (AOS): This condition can occur in adults, due to brain damage as a result of a tumor, head injury , stroke, or other illness that affects the parts of the brain involved in speech.
If you have a speech impediment, or suspect your child might have one, it can be helpful to visit your healthcare provider. Your primary care physician can refer you to a speech-language pathologist, who can evaluate speech, diagnose speech disorders, and recommend treatment options.
The diagnostic process may involve a physical examination as well as psychological, neurological, or hearing tests, in order to confirm the diagnosis and rule out other causes.
Treatment for speech disorders often involves speech therapy, which can help you learn how to move your muscles and position your tongue correctly in order to create specific sounds. It can be quite effective in improving your speech.
Children often grow out of milder speech disorders; however, special education and speech therapy can help with more serious ones.
For ankyloglossia, or tongue-tie, a minor surgery known as a frenectomy can help detach the tongue from the bottom of the mouth.
A Word From Verywell
A speech impediment can make it difficult to pronounce certain sounds, speak clearly, or communicate fluently.
Living with a speech disorder can be frustrating because people may cut you off while you’re speaking, try to finish your sentences, or treat you differently. It can be helpful to talk to your healthcare providers about how to cope with these situations.
You may also benefit from joining a support group, where you can connect with others living with speech disorders.
National Library of Medicine. Speech disorders . Medline Plus.
Centers for Disease Control and Prevention. Language and speech disorders .
Cincinnati Children's Hospital. Stuttering .
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, and language .
Cleveland Clinic. Speech impediment .
Lee H, Sim H, Lee E, Choi D. Disfluency characteristics of children with attention-deficit/hyperactivity disorder symptoms . J Commun Disord . 2017;65:54-64. doi:10.1016/j.jcomdis.2016.12.001
Nemours Foundation. Speech problems .
Penn Medicine. Speech and language disorders .
Cleveland Clinic. Tongue-tie .
University of Rochester Medical Center. Ankyloglossia .
Cleveland Clinic. Dysarthria .
National Institute on Deafness and Other Communication Disorders. Apraxia of speech .
Cleveland Clinic. Childhood apraxia of speech .
Stanford Children’s Hospital. Speech sound disorders in children .
Abbastabar H, Alizadeh A, Darparesh M, Mohseni S, Roozbeh N. Spatial distribution and the prevalence of speech disorders in the provinces of Iran . J Med Life . 2015;8(Spec Iss 2):99-104.
By Sanjana Gupta Sanjana is a health writer and editor. Her work spans various health-related topics, including mental health, fitness, nutrition, and wellness.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Overcoming Speech Impediment: Symptoms to Treatment
There are many causes and solutions for impaired speech
- Types and Symptoms
- Speech Therapy
- Building Confidence
Speech impediments are conditions that can cause a variety of symptoms, such as an inability to understand language or speak with a stable sense of tone, speed, or fluidity. There are many different types of speech impediments, and they can begin during childhood or develop during adulthood.
Common causes include physical trauma, neurological disorders, or anxiety. If you or your child is experiencing signs of a speech impediment, you need to know that these conditions can be diagnosed and treated with professional speech therapy.
This article will discuss what you can do if you are concerned about a speech impediment and what you can expect during your diagnostic process and therapy.
FG Trade / Getty Images
Types and Symptoms of Speech Impediment
People can have speech problems due to developmental conditions that begin to show symptoms during early childhood or as a result of conditions that may occur during adulthood.
The main classifications of speech impairment are aphasia (difficulty understanding or producing the correct words or phrases) or dysarthria (difficulty enunciating words).
Often, speech problems can be part of neurological or neurodevelopmental disorders that also cause other symptoms, such as multiple sclerosis (MS) or autism spectrum disorder .
There are several different symptoms of speech impediments, and you may experience one or more.
Can Symptoms Worsen?
Most speech disorders cause persistent symptoms and can temporarily get worse when you are tired, anxious, or sick.
Symptoms of dysarthria can include:
- Slurred speech
- Slow speech
- Choppy speech
- Hesitant speech
- Inability to control the volume of your speech
- Shaking or tremulous speech pattern
- Inability to pronounce certain sounds
Symptoms of aphasia may involve:
- Speech apraxia (difficulty coordinating speech)
- Difficulty understanding the meaning of what other people are saying
- Inability to use the correct words
- Inability to repeat words or phases
- Speech that has an irregular rhythm
You can have one or more of these speech patterns as part of your speech impediment, and their combination and frequency will help determine the type and cause of your speech problem.
Causes of Speech Impediment
The conditions that cause speech impediments can include developmental problems that are present from birth, neurological diseases such as Parkinson’s disease , or sudden neurological events, such as a stroke .
Some people can also experience temporary speech impairment due to anxiety, intoxication, medication side effects, postictal state (the time immediately after a seizure), or a change of consciousness.
Speech Impairment in Children
Children can have speech disorders associated with neurodevelopmental problems, which can interfere with speech development. Some childhood neurological or neurodevelopmental disorders may cause a regression (backsliding) of speech skills.
Common causes of childhood speech impediments include:
- Autism spectrum disorder : A neurodevelopmental disorder that affects social and interactive development
- Cerebral palsy : A congenital (from birth) disorder that affects learning and control of physical movement
- Hearing loss : Can affect the way children hear and imitate speech
- Rett syndrome : A genetic neurodevelopmental condition that causes regression of physical and social skills beginning during the early school-age years.
- Adrenoleukodystrophy : A genetic disorder that causes a decline in motor and cognitive skills beginning during early childhood
- Childhood metabolic disorders : A group of conditions that affects the way children break down nutrients, often resulting in toxic damage to organs
- Brain tumor : A growth that may damage areas of the brain, including those that control speech or language
- Encephalitis : Brain inflammation or infection that may affect the way regions in the brain function
- Hydrocephalus : Excess fluid within the skull, which may develop after brain surgery and can cause brain damage
Do Childhood Speech Disorders Persist?
Speech disorders during childhood can have persistent effects throughout life. Therapy can often help improve speech skills.
Speech Impairment in Adulthood
Adult speech disorders develop due to conditions that damage the speech areas of the brain.
Common causes of adult speech impairment include:
- Head trauma
- Nerve injury
- Throat tumor
- Stroke
- Parkinson’s disease
- Essential tremor
- Brain tumor
- Brain infection
Additionally, people may develop changes in speech with advancing age, even without a specific neurological cause. This can happen due to presbyphonia , which is a change in the volume and control of speech due to declining hormone levels and reduced elasticity and movement of the vocal cords.
Do Speech Disorders Resolve on Their Own?
Children and adults who have persistent speech disorders are unlikely to experience spontaneous improvement without therapy and should seek professional attention.
Steps to Treating Speech Impediment
If you or your child has a speech impediment, your healthcare providers will work to diagnose the type of speech impediment as well as the underlying condition that caused it. Defining the cause and type of speech impediment will help determine your prognosis and treatment plan.
Sometimes the cause is known before symptoms begin, as is the case with trauma or MS. Impaired speech may first be a symptom of a condition, such as a stroke that causes aphasia as the primary symptom.
The diagnosis will include a comprehensive medical history, physical examination, and a thorough evaluation of speech and language. Diagnostic testing is directed by the medical history and clinical evaluation.
Diagnostic testing may include:
- Brain imaging , such as brain computerized tomography (CT) or magnetic residence imaging (MRI), if there’s concern about a disease process in the brain
- Swallowing evaluation if there’s concern about dysfunction of the muscles in the throat
- Electromyography (EMG) and nerve conduction studies (aka nerve conduction velocity, or NCV) if there’s concern about nerve and muscle damage
- Blood tests, which can help in diagnosing inflammatory disorders or infections
Your diagnostic tests will help pinpoint the cause of your speech problem. Your treatment will include specific therapy to help improve your speech, as well as medication or other interventions to treat the underlying disorder.
For example, if you are diagnosed with MS, you would likely receive disease-modifying therapy to help prevent MS progression. And if you are diagnosed with a brain tumor, you may need surgery, chemotherapy, or radiation to treat the tumor.
Therapy to Address Speech Impediment
Therapy for speech impairment is interactive and directed by a specialist who is experienced in treating speech problems . Sometimes, children receive speech therapy as part of a specialized learning program at school.
The duration and frequency of your speech therapy program depend on the underlying cause of your impediment, your improvement, and approval from your health insurance.
If you or your child has a serious speech problem, you may qualify for speech therapy. Working with your therapist can help you build confidence, particularly as you begin to see improvement.
Exercises during speech therapy may include:
- Pronouncing individual sounds, such as la la la or da da da
- Practicing pronunciation of words that you have trouble pronouncing
- Adjusting the rate or volume of your speech
- Mouth exercises
- Practicing language skills by naming objects or repeating what the therapist is saying
These therapies are meant to help achieve more fluent and understandable speech as well as an increased comfort level with speech and language.
Building Confidence With Speech Problems
Some types of speech impairment might not qualify for therapy. If you have speech difficulties due to anxiety or a social phobia or if you don’t have access to therapy, you might benefit from activities that can help you practice your speech.
You might consider one or more of the following for you or your child:
- Joining a local theater group
- Volunteering in a school or community activity that involves interaction with the public
- Signing up for a class that requires a significant amount of class participation
- Joining a support group for people who have problems with speech
Activities that you do on your own to improve your confidence with speaking can be most beneficial when you are in a non-judgmental and safe space.
Many different types of speech problems can affect children and adults. Some of these are congenital (present from birth), while others are acquired due to health conditions, medication side effects, substances, or mood and anxiety disorders. Because there are so many different types of speech problems, seeking a medical diagnosis so you can get the right therapy for your specific disorder is crucial.
Centers for Disease Control and Prevention. Language and speech disorders in children .
Han C, Tang J, Tang B, et al. The effectiveness and safety of noninvasive brain stimulation technology combined with speech training on aphasia after stroke: a systematic review and meta-analysis . Medicine (Baltimore). 2024;103(2):e36880. doi:10.1097/MD.0000000000036880
National Institute on Deafness and Other Communication Disorders. Quick statistics about voice, speech, language .
Mackey J, McCulloch H, Scheiner G, et al. Speech pathologists' perspectives on the use of augmentative and alternative communication devices with people with acquired brain injury and reflections from lived experience . Brain Impair. 2023;24(2):168-184. doi:10.1017/BrImp.2023.9
Allison KM, Doherty KM. Relation of speech-language profile and communication modality to participation of children with cerebral palsy . Am J Speech Lang Pathol . 2024:1-11. doi:10.1044/2023_AJSLP-23-00267
Saccente-Kennedy B, Gillies F, Desjardins M, et al. A systematic review of speech-language pathology interventions for presbyphonia using the rehabilitation treatment specification system . J Voice. 2024:S0892-1997(23)00396-X. doi:10.1016/j.jvoice.2023.12.010
By Heidi Moawad, MD Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.
- Second Opinion
Speech Sound Disorders in Children
What are speech sound disorders in children?
It’s normal for young children learning language skills to have some trouble saying words the right way. That’s part of the learning process. Their speech skills develop over time. They master certain sounds and words at each age. By age 8, most children have learned how to master all word sounds.
But some children have speech sound disorders. This means they have trouble saying certain sounds and words past the expected age. This can make it hard to understand what a child is trying to say.
Speech sound problems include articulation disorder and phonological process disorder.
Articulation disorder is a problem with making certain sounds, such as “sh.”
Phonological process disorder is a pattern of sound mistakes. This includes not pronouncing certain letters.
What causes speech sound disorders in a child?
Often, a speech sound disorder has no known cause. But some speech sound errors may be caused by:
Injury to the brain
Thinking or development disability
Problems with hearing or hearing loss, such as past ear infections
Physical problems that affect speech, such cleft palate or cleft lip
Disorders affecting the nerves involved in speech
Which children are at risk for speech sound disorders?
The cause often is not known, but children at risk for a speech sound disorder include those with:
Developmental disorders such as autism
Genetic disorders such as Down syndrome
Hearing loss
Nervous system disorders such as cerebral palsy
Illnesses such as frequent ear infections
Physical problems such as a cleft lip or palate
Too much thumb-sucking or pacifier use
Low education level of the parent
Lack of support for learning in the home
What are the symptoms of speech sound disorders in a child?
Your child’s symptoms depend on what type of speech sound disorder your child has. He or she may have trouble forming some word sounds correctly past a certain age. This is called articulation disorder. Your child may drop, add, distort, or swap word sounds. Keep in mind that some sound changes may be part of an accent. They are not speech errors. Signs of this problem can include:
Leaving off sounds from words (example: saying “coo” instead of “school”)
Adding sounds to words (example: saying “puhlay” instead of “play”)
Distorting sounds in words (example: saying “thith” instead of “this”)
Swapping sounds in words (example: saying “wadio” instead of “radio”)
If your child often makes certain word speech mistakes, he or she may have phonological process disorder. The mistakes may be common in young children learning speech skills. But when they last past a certain age, it may be a disorder. Signs of this problem are:
Saying only 1 syllable in a word (example: “bay” instead of “baby”)
Simplifying a word by repeating 2 syllables (example: “baba” instead of “bottle”)
Leaving out a consonant sound (example: “at” or “ba” instead of “bat”)
Changing certain consonant sounds (example: “tat” instead of “cat”)
How are speech sound disorders diagnosed in a child?
First, your child’s healthcare provider will check his or her hearing. This is to make sure that your child isn’t simply hearing words and sounds incorrectly.
If your child’s healthcare provider rules out hearing loss, you may want to talk with a speech-language pathologist. This is a speech expert who evaluates and treats children who are having problems with speech-language and communication.
By watching and listening to your child speak, a speech-language pathologist can determine whether your child has a speech sound disorder. The pathologist will evaluate your child’s speech and language skills. He or she will keep in mind accents and dialect. He or she can also find out if a physical problem in the mouth is affecting your child’s ability to speak. Finding the problem and getting help early are important to treat speech sound disorders.
How are speech sound disorders treated in a child?
The speech-language pathologist can put together a therapy plan to help your child with his or her disorder. These healthcare providers work with children to help them:
Notice and fix sounds that they are making wrong
Learn how to correctly form their problem sound
Practice saying certain words and making certain sounds
The pathologist can also give you activities and strategies to help your child practice at home. If your child has a physical problem in the mouth, the pathologist can refer your child to an ear, nose, throat healthcare provider or orthodontist if needed.
Spotting a speech sound disorder early can help your child overcome any speech problems. He or she can learn how to speak well and comfortably.
How can I help my child live with a speech sound disorder?
You can do things to take care of your child with a speech sound disorder:
Keep all appointments with your child’s healthcare provider.
Talk with your healthcare provider about other providers who will be involved in your child’s care. Your child may get care from a team that may include experts such as speech-language pathologists and counselors. Your child’s care team will depend on your child’s needs and the severity of the speech sound disorder.
Tell others of your child’s disorder. Work with your child’s healthcare provider and schools to develop a treatment plan.
Reach out for support from local community services. Being in touch with other parents who have a child with a speech sound disorder may be helpful.
When should I call my child’s healthcare provider?
Call your child’s healthcare provider if your child has:
Symptoms that don’t get better, or get worse
New symptoms
Key points about speech sound disorders in children
A speech sound disorder means a child has trouble saying certain sounds and words past the expected age.
A child with an articulation disorder has problems making certain sounds the right way.
A child with phonological process disorder regularly makes certain word speech mistakes.
The cause of this problem is often unknown.
A speech-language pathologist can help diagnose and treat a speech sound disorder.
Tips to help you get the most from a visit to your child’s healthcare provider:
Know the reason for the visit and what you want to happen.
Before your visit, write down questions you want answered.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
Ask if your child’s condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if your child does not take the medicine or have the test or procedure.
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Fluency Disorder
- Age-Appropriate Speech and Language Milestones
- Communication Disorders in Children
Related Topics
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health

- Games & Quizzes
- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
Prevalence of speech disorders
Classification of speech disorders, treatment and rehabilitation, development of speech correction.
- Voice disorders
- Disorders of language development
- Stuttering, or stammering
- Dysphasia and aphasia
- Shaking palsy
- Intellectual disability
- Language and mental disorder
- Speech of the hard of hearing
- Loss of tongue
- Nasal speech
- Cleft palate speech

speech disorder
Our editors will review what you’ve submitted and determine whether to revise the article.
- Table Of Contents

Recent News
speech disorder , any of the disorders that impair human speech .
Human communication relies largely on the faculty of speech, supplemented by the production of certain sounds, each of which is unique in meaning. Human speech is extraordinarily complex, consisting of sound waves of a diverse range of frequencies, intensities, and amplitudes that convey specific information. The production and reception of these sounds require a properly functioning ear and auditory system, as well as intact and healthy vocal and sound-generating structures, including the larynx , the tongue, and the lips.
Vocal communication can be rendered difficult or impossible by deformities in the physical structures used in speech and sound production or by disorders affecting areas of the brain that process speech and sound.
The study of speech disorders
In the United States , statistics from the early 21st century compiled by the National Institute on Deafness and Other Communication Disorders revealed that approximately 5 percent of American children had detectable speech disorders by age six or seven. About 7.5 million Americans were found to be unable to use their voice normally. Disorders of articulation among young children were frequent.

Studies in Germany, Austria, and other central European countries suggest that the incidence and prevalence of speech disorders in these countries follow patterns similar to those observed among other Western countries. There are, however, deviations from these trends. For example, the incidence of cleft palate is very high among Native Americans, while it is much lower among blacks than in whites. Studies of stuttering that have focused on specific populations, including Americans, Europeans, and Africans, have indicated that the prevalence of the disorder among these populations is highly variable. However, generalization of the data suggests that roughly 2.5 percent of children under age five are affected by stuttering . For some speech disorders, reliable data on global prevalence and distribution are lacking.
In accordance with physiological considerations, disorders of communication are first classified into disorders of voice and phonic respiration, disorders of articulated speech, and disorders of language . It has been known for a long time that the majority of communication disorders are not caused by local lesions of the teeth, tongue, vocal cords, or regulating brain centres. Since these predominant disorders of voice and speech develop from derangements of the underlying physiological functions of breathing, use of the voice, speaking habits, or emotional disorders, this group has been labeled as functional. The remainder of the communication disorders with clearly recognizable structural abnormalities in the total speech mechanism has been labeled organic.
While this empirical grouping has certain implications for the selection of the appropriate treatment, it is not satisfactory because organic structure and living function can never be separated. Certain functional disorders of the voice caused by its habitual abuse may very well lead to secondary structural changes, such as the growths (polyps and nodules) of the vocal cords, which develop as a result of vocal abuse. On the other hand, all the obviously organic and structural lesions, such as loss of the tongue from accident or surgery, will almost inevitably be followed by emotional and other psychological reactions. In this case, the functional components are of a secondary nature but to a great extent will influence the total picture of disturbance, including the patient’s ability to adjust to the limitation , to relearn a new mode of appropriate function, and to make the best of his or her condition.
Within these major groups, the various types of communication disorders have for a long time, and in most parts of the world, been described by the listener’s perceptual impression. Most languages employ specific words for the various types of abnormal speech, such as stuttering, stammering, cluttering, mumbling, lisping, whispering, and many others. The problem with such subjective and symptomatic labels is the fact that they try to define the final, audible result, the recognizable phenomenon, and not by any means the underlying basis. This general human tendency to describe disorders of communication by what the listener hears is analogous to the attempts of early medicine to classify diseases by the patient’s symptoms that the diagnosing physician could see or hear or feel or perhaps smell. Before the great discoveries of the 19th century had erected a logical basis for medical pathology , the various diseases were classified as numerous types of fevers, congestions, and dyscrasias. Thus, malaria was originally thought to be caused by the evil emanations (miasma) of the bad air ( mal aria ) near swamps until it was recognized to be caused by a blood parasite transmitted by the mosquito.
The various approaches of medical, psychiatric, psychological, educational, behavioral, and other schools of speech pathology have made great advances in the recent past and better systems of classification continue to be proposed. They aim at grouping the observable symptoms of speech disorders according to the underlying origins instead of the listener’s subjective impressions. While this is relatively easy in the case of language loss from, for example, a brain stroke because the destroyed brain areas can be identified at autopsy, it is more difficult in the case of the large group of so-called functional speech disorders for two reasons: first, they are definitely not caused by gross, easily visible organic lesions, and, second, many functional disorders are outgrown through maturation or appropriate learning (laboratory study of the involved tissues in such cases would reveal no detectable lesions). It is hoped that refined methods of study in the areas of both “functional” psychology and “organic” neurophysiology will eventually reveal the structural bases for the prevalent disorders of voice and speech.
The selection of methods in the medical treatment or educational rehabilitation of communication disorders depends primarily on the underlying basis for the disturbance. Any case of chronic hoarseness should be evaluated first by a laryngologist to establish a precise diagnosis . This is particularly important in the older age groups in which an incipient laryngeal cancer is often overlooked because the patient does not pay attention to his or her deteriorating voice. The prognosis of all cancers becomes rapidly poorer the longer the disease remains unrecognized. As soon as disease of the larynx is excluded as a cause of the vocal complaint, vocal rehabilitation by a competent speech pathologist should be considered.
Malformations, diseases, or injuries of the peripheral speech mechanism are treated by appropriate specialists. The plastic surgeon repairs a cleft of the palate. The neurologist and internist treat the stroke patient until he or she has recovered sufficiently to be referred for reeducation of language abilities. The pediatrician treats the child with intellectual disability , while the geneticist counsels the family regarding the possible inheritance of the disorder and its future avoidance. Deafness or severe hearing loss in early childhood is a typical cause for severe delay of language development and should be promptly recognized through appropriate examination by the ear surgeon (otologist) and hearing specialist (audiologist). Cases of childhood autism (withdrawal, severe eccentricities) or early schizophrenia are recognized with increasing frequency by speech pathologists, child psychiatrists, pediatricians, and clinical psychologists. This multitude of various professional interests in the recognition and rehabilitation of such exceptional children is well served by the coordination of these efforts in the modern team approach. But again, the largest group of disorders of voice and speech has causes other than these grossly organic lesions. They belong within the province of speech rehabilitation by experts in speech pathology and other functional practitioners.
In the 21st century, researchers from diverse fields, including neuroscience, bioengineering, and linguistics, worked to develop state-of-the-art devices capable of generating a synthetic voice controlled by activity in the speech centres of a person’s brain. Part of this research entailed mapping sound produced by the voice of healthy individuals to movements of the vocal tract, which allowed for the subsequent development of algorithms that associate brain activity generated during speech with specific vocal tract movements. Those movements could then be used to produce a synthetic version of an individual’s voice. In an early trial, one such neural decoder successfully generated understandable sentences that had been silently mimed by a person with intact speech.
That humankind has been troubled by speech afflictions since the beginning of recorded history can be gleaned from numerous remarks in the books of the Bible. Further, many scientific and medical writers from the time of antiquity to the Middle Ages reported observations of speech and voice disorders. The recommended remedies merely reflected the inadequacies of the philosophical or empirical notions of their times. Scientifically oriented speech pathology originated in Germany during the latter part of the 19th century, following closely the development of otolaryngology. Three names stand out in this respect: Carl Ludwig Merkel ( Anthropophonik ; 1857), Adolph Kussmaul ( The Disorders of Speech ; 1877), and Hermann Gutzmann, Sr., who became the first professor of speech pathology at the University of Berlin Medical School around 1900.
During the same time, the new science of experimental phonetics was developed by Jean-Pierre Rousselot in Paris, who promptly recognized the great contributions that experimental phonetics could make to the study of normal and disturbed speech. This close collaboration of medical speech pathology with experimental phonetics has remained typical for the European continent where speech correction is customarily carried out under the direction of physicians in the ear, nose, and throat departments of the university hospitals. The designation of speech and voice pathology as logopedics and phoniatrics with its medical orientation subsequently reached many other civilized nations, notably in Japan and on the South American continent. The national organizations in most of these areas are now represented in the International Association of Logopedics and Phoniatrics, which was founded in Vienna in 1924.
The evolution of speech correction in the Anglo-Saxon countries followed a different trend. Although the United Kingdom has had a long tradition in general and experimental phonetics, its College of Speech Therapists was organized as an examining and supervisory body in 1945. Similar organizations followed in other areas of the British Commonwealth.
American speech pathology elected a different way. The American Speech-Language-Hearing Association (ASHA), founded in 1925 in New York City as the American Academy of Speech Correction, became the organizing, examining, and supervisory body for a rapidly growing membership, which surpassed 130,000 by 2008. Many colleges and universities in the United States are accredited by ASHA and offer degrees in speech pathology and audiology , some including work at the doctoral level. The large majority of ASHA members work as speech clinicians. A smaller number with master’s degrees and a still smaller number with doctoral degrees staff clinics that deal with communication disorders and that are usually affiliated with hospitals, colleges, universities, and occasionally with civic organizations.
Russian speech correction originally followed the developments of European logopedics and phoniatrics. One facet of early speech pathology research in Russia was its emphasis on Pavlovian theory ( conditioning and retraining) and intensive use of neuropsychiatric methods, including pharmacology, sleep therapy, and other intensive treatment programs during hospitalization. Similar trends operate in the eastern European countries, such as in the Czech Republic , where the first independent medical department of logopedics and phoniatrics was organized at the Faculty of Medicine of Charles University in Prague.
American Speech-Language-Hearing Association
- Certification
- Publications
- Continuing Education
- Practice Management
- Audiologists
- Speech-Language Pathologists
- Academic & Faculty
- Audiology & SLP Assistants
Speech Sound Disorders
On this page:
About Speech Sound Disorders
Signs and symptoms of speech sound disorders, causes of speech sound disorders, seeing a professional, other resources.
Children may say some sounds the wrong way as they learn to talk. They learn some sounds earlier, like p, m, or w. Other sounds take longer to learn, like z, v, or th. Most children can say almost all speech sounds correctly by 4 years old. A child who does not say sounds by the expected ages may have a speech sound disorder. You may hear the terms "articulation disorder" and "phonological disorder" to describe speech sound disorders like this.
To learn more about what you should expect your child to be able to say, see these two resources:
- ASHA's Communication and Feeding Milestones: Birth to 5 Years
- Your Child's Communication Development: Kindergarten Through Fifth Grade
Adults can also have speech sound disorders. Some adults have problems that started when they were children. Others may have speech problems after a stroke or traumatic brain injury . To learn more about adult speech disorders after a stroke or traumatic brain injury, see apraxia of speech in adults and dysarthria .
Your child may substitute one sound for another, leave sounds out, add sounds, or change a sound. It can be hard for others to understand them.
It is normal for young children to say the wrong sounds sometimes. For example, your child may make a "w" sound for an "r" and say "wabbit" for "rabbit." They may leave sounds out of words, such as "nana" for "banana." This is okay when they are young. It may be a problem if they keep making these mistakes as they get older.
You and your child may also sound different because you have an accent or dialect. This is not a speech sound disorder.
The chart below shows the ages when most English-speaking children develop sounds. Children learning more than one language may develop some sounds earlier or later.
| Makes cooing sounds | |
| Laughs and makes playful sounds | |
| Makes speech-like babbling sounds like | |
| Babbles longer strings of sounds like | |
| Says and in words Familiar people understand the child's speech | |
| Says and in words May still make mistakes on the and sounds Most people understand the child’s speech |
Many children learn to say speech sounds over time, but some do not. You may not know why your child has problems speaking.
Some children have speech problems because the brain has trouble sending messages to the speech muscles telling them how and when to move. This is called apraxia. Childhood apraxia of speech is not common but will cause speech problems.
Some children have speech problems because the muscles needed to make speech sounds are weak. This is called dysarthria .
Your child may have speech problems if he has
- a developmental disorder, like autism;
- a genetic syndrome, like Down syndrome;
- hearing loss, from ear infections or other causes; or
- brain damage, like cerebral palsy or a head injury.
Adults can also have speech sound disorders. Some adults have problems that started when they were children. Others may develop speech problems after a stroke or traumatic brain injury , or other trauma. To learn more about adult speech disorders, see apraxia of speech in adults , dysarthria , laryngeal cancer , and oral cancer .
Testing for Speech Sound Disorders
A speech-language pathologist, or SLP, can test your child's speech. The SLP will listen to your child to hear how they say sounds. The SLP also will look at how your child moves their lips, jaw, and tongue. The SLP may also test your child’s language skills. Many children with speech sound disorders also have language disorders. For example, your child may have trouble following directions or telling stories.
It is important to have your child’s hearing checked to make sure they do not have a hearing loss. A child with a hearing loss may have more trouble learning to talk.
The SLP can also help decide if you have a speech problem or speak with an accent. An accent is the unique way that groups of people sound. Accents are NOT a speech or language disorder.
Treatment for Speech Sound Disorders
SLPs can help you or your child say sounds correctly and clearly. Treatment may include the following:
- Learning the correct way to make sounds
- Learning to tell when sounds are right or wrong
- Practicing sounds in different words
- Practicing sounds in longer sentences
See ASHA information for professionals on the Practice Portal’s Speech Sound Disorders page.
- Identify the Signs
- Typical Speech and Language Development
In the Public Section
- Hearing & Balance
- Speech, Language & Swallowing
- About Health Insurance
- Adding Speech & Hearing Benefits
- Advocacy & Outreach
- Find a Professional
- Advertising Disclaimer
- Advertise with us
ASHA Corporate Partners
- Become A Corporate Partner

The American Speech-Language-Hearing Association (ASHA) is the national professional, scientific, and credentialing association for 234,000 members, certificate holders, and affiliates who are audiologists; speech-language pathologists; speech, language, and hearing scientists; audiology and speech-language pathology assistants; and students.
- All ASHA Websites
- Work at ASHA
- Marketing Solutions
Information For
Get involved.
- ASHA Community
- Become a Mentor
- Become a Volunteer
- Special Interest Groups (SIGs)
Connect With ASHA
American Speech-Language-Hearing Association 2200 Research Blvd., Rockville, MD 20850 Members: 800-498-2071 Non-Member: 800-638-8255
MORE WAYS TO CONNECT
Media Resources
- Press Queries
Site Help | A–Z Topic Index | Privacy Statement | Terms of Use © 1997- American Speech-Language-Hearing Association

- Bachelor’s Degrees
- Master’s Degrees
- Doctorate Degrees
- Certificate Programs
- Nursing Degrees
- Cybersecurity
- Human Services
- Science & Mathematics
- Communication
- Liberal Arts
- Social Sciences
- Computer Science
- Admissions Overview
- Tuition and Financial Aid
- Incoming Freshman and Graduate Students
- Transfer Students
- Military Students
- International Students
- Early Access Program
- About Maryville
- Our Faculty
- Our Approach
- Our History
- Accreditation
- Tales of the Brave
- Student Support Overview
- Online Learning Tools
- Infographics
Home / Blog
Speech Impediment Guide: Definition, Causes, and Resources
December 8, 2020

Tables of Contents
What Is a Speech Impediment?
Types of speech disorders, speech impediment causes, how to fix a speech impediment, making a difference in speech disorders.
Communication is a cornerstone of human relationships. When an individual struggles to verbalize information, thoughts, and feelings, it can cause major barriers in personal, learning, and business interactions.
Speech impediments, or speech disorders, can lead to feelings of insecurity and frustration. They can also cause worry for family members and friends who don’t know how to help their loved ones express themselves.
Fortunately, there are a number of ways that speech disorders can be treated, and in many cases, cured. Health professionals in fields including speech-language pathology and audiology can work with patients to overcome communication disorders, and individuals and families can learn techniques to help.

Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual’s ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
Some 7.7% of U.S. children — or 1 in 12 youths between the ages of 3 and 17 — have speech, voice, language, or swallowing disorders, according to the National Institute on Deafness and Other Communication Disorders (NIDCD). About 70 million people worldwide, including some 3 million Americans, experience stuttering difficulties, according to the Stuttering Foundation.
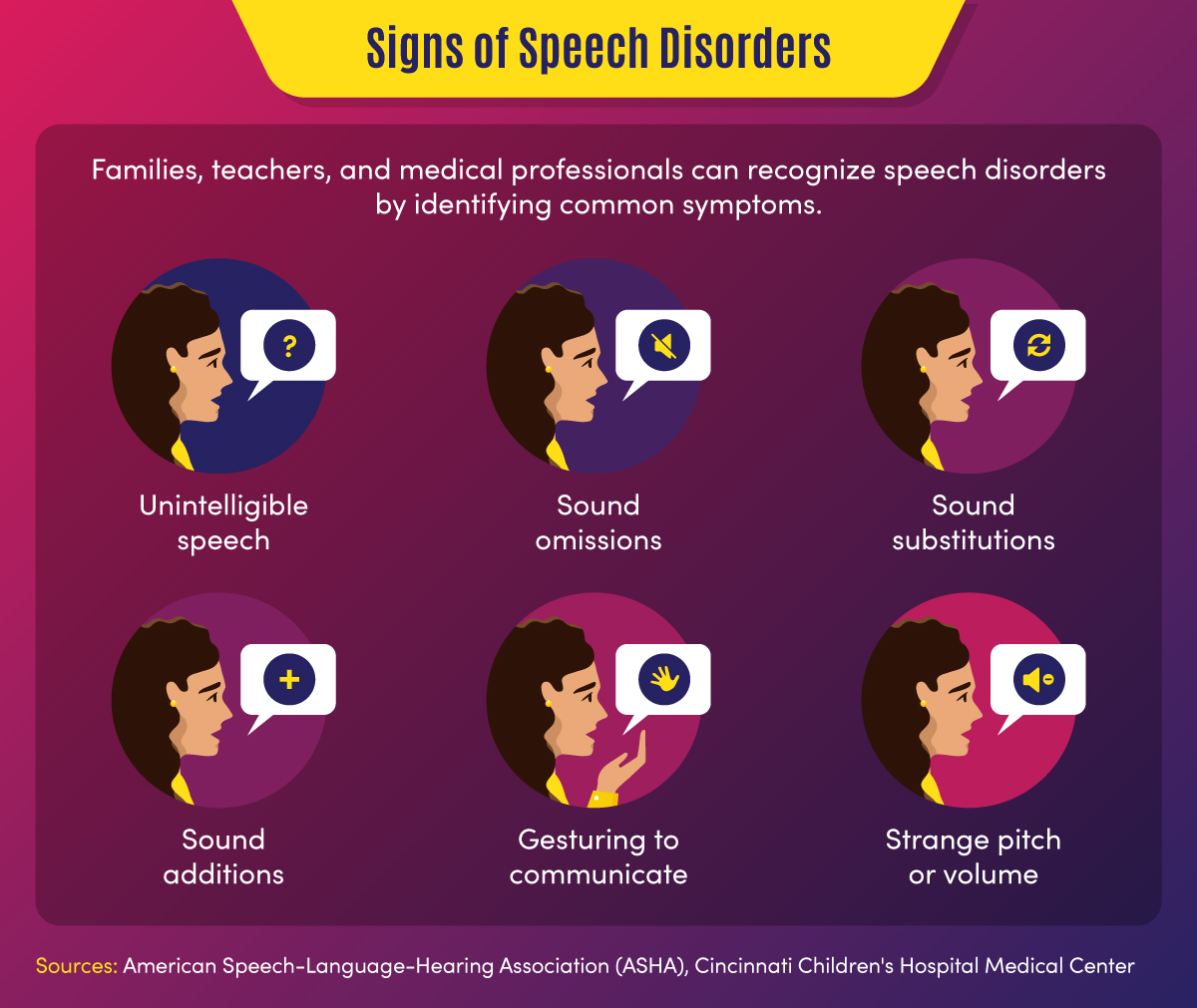
Common signs of a speech disorder
There are several symptoms and indicators that can point to a speech disorder.
- Unintelligible speech — A speech disorder may be present when others have difficulty understanding a person’s verbalizations.
- Omitted sounds — This symptom can include the omission of part of a word, such as saying “bo” instead of “boat,” and may include omission of consonants or syllables.
- Added sounds — This can involve adding extra sounds in a word, such as “buhlack” instead of “black,” or repeating sounds like “b-b-b-ball.”
- Substituted sounds — When sounds are substituted or distorted, such as saying “wabbit” instead of “rabbit,” it may indicate a speech disorder.
- Use of gestures — When individuals use gestures to communicate instead of words, a speech impediment may be the cause.
- Inappropriate pitch — This symptom is characterized by speaking with a strange pitch or volume.
In children, signs might also include a lack of babbling or making limited sounds. Symptoms may also include the incorrect use of specific sounds in words, according to the American Speech-Language-Hearing Association (ASHA). This may include the sounds p, m, b, w, and h among children aged 1-2, and k, f, g, d, n, and t for children aged 2-3.
Back To Top
Categories of Speech Impediments
Speech impediments can range from speech sound disorders (articulation and phonological disorders) to voice disorders. Speech sound disorders may be organic — resulting from a motor or sensory cause — or may be functional with no known cause. Voice disorders deal with physical problems that limit speech. The main categories of speech impediments include the following:
Fluency disorders occur when a patient has trouble with speech timing or rhythms. This can lead to hesitations, repetitions, or prolonged sounds. Fluency disorders include stuttering (repetition of sounds) or (rapid or irregular rate of speech).
Resonance disorders are related to voice quality that is impacted by the shape of the nose, throat, and/or mouth. Examples of resonance disorders include hyponasality and cul-de-sac resonance.
Articulation disorders occur when a patient has difficulty producing speech sounds. These disorders may stem from physical or anatomical limitations such as muscular, neuromuscular, or skeletal support. Examples of articulation speech impairments include sound omissions, substitutions, and distortions.
Phonological disorders result in the misuse of certain speech sounds to form words. Conditions include fronting, stopping, and the omission of final consonants.
Voice disorders are the result of problems in the larynx that harm the quality or use of an individual’s voice. This can impact pitch, resonance, and loudness.
Impact of Speech Disorders
Some speech disorders have little impact on socialization and daily activities, but other conditions can make some tasks difficult for individuals. Following are a few of the impacts of speech impediments.
- Poor communication — Children may be unable to participate in certain learning activities, such as answering questions or reading out loud, due to communication difficulties. Adults may avoid work or social activities such as giving speeches or attending parties.
- Mental health and confidence — Speech disorders may cause children or adults to feel different from peers, leading to a lack of self-confidence and, potentially, self-isolation.
Resources on Speech Disorders
The following resources may help those who are seeking more information about speech impediments.
Health Information : Information and statistics on common voice and speech disorders from the NIDCD
Speech Disorders : Information on childhood speech disorders from Cincinnati Children’s Hospital Medical Center
Speech, Language, and Swallowing : Resources about speech and language development from the ASHA
Children and adults can suffer from a variety of speech impairments that may have mild to severe impacts on their ability to communicate. The following 10 conditions are examples of specific types of speech disorders and voice disorders.
1. Stuttering
This condition is one of the most common speech disorders. Stuttering is the repetition of syllables or words, interruptions in speech, or prolonged use of a sound.
This organic speech disorder is a result of damage to the neural pathways that connect the brain to speech-producing muscles. This results in a person knowing what they want to say, but being unable to speak the words.
This consists of the lost ability to speak, understand, or write languages. It is common in stroke, brain tumor, or traumatic brain injury patients.
4. Dysarthria
This condition is an organic speech sound disorder that involves difficulty expressing certain noises. This may involve slurring, or poor pronunciation, and rhythm differences related to nerve or brain disorders.
The condition of lisping is the replacing of sounds in words, including “th” for “s.” Lisping is a functional speech impediment.
6. Hyponasality
This condition is a resonance disorder related to limited sound coming through the nose, causing a “stopped up” quality to speech.
7. Cul-de-sac resonance
This speech disorder is the result of blockage in the mouth, throat, or nose that results in quiet or muffled speech.
8. Orofacial myofunctional disorders
These conditions involve abnormal patterns of mouth and face movement. Conditions include tongue thrusting (fronting), where individuals push out their tongue while eating or talking.
9. Spasmodic Dysphonia
This condition is a voice disorder in which spasms in the vocal cords produce speech that is hoarse, strained, or jittery.
10. Other voice disorders
These conditions can include having a voice that sounds breathy, hoarse, or scratchy. Some disorders deal with vocal folds closing when they should open (paradoxical vocal fold movement) or the presence of polyps or nodules in the vocal folds.
Speech Disorders vs. Language Disorders
Speech disorders deal with difficulty in creating sounds due to articulation, fluency, phonology, and voice problems. These problems are typically related to physical, motor, sensory, neurological, or mental health issues.
Language disorders, on the other hand, occur when individuals have difficulty communicating the meaning of what they want to express. Common in children, these disorders may result in low vocabulary and difficulty saying complex sentences. Such a disorder may reflect difficulty in comprehending school lessons or adopting new words, or it may be related to a learning disability such as dyslexia. Language disorders can also involve receptive language difficulties, where individuals have trouble understanding the messages that others are trying to convey.
Resources on Types of Speech Disorders
The following resources may provide additional information on the types of speech impediments.
Common Speech Disorders: A guide to the most common speech impediments from GreatSpeech
Speech impairment in adults: Descriptions of common adult speech issues from MedlinePlus
Stuttering Facts: Information on stuttering indications and causes from the Stuttering Foundation
Speech disorders may be caused by a variety of factors related to physical features, neurological ailments, or mental health conditions. In children, they may be related to developmental issues or unknown causes and may go away naturally over time.
Physical and neurological issues. Speech impediment causes related to physical characteristics may include:
- Brain damage
- Nervous system damage
- Respiratory system damage
- Hearing difficulties
- Cancerous or noncancerous growths
- Muscle and bone problems such as dental issues or cleft palate
Mental health issues. Some speech disorders are related to clinical conditions such as:
- Autism spectrum disorder
- Down syndrome or other genetic syndromes
- Cerebral palsy or other neurological disorders
- Multiple sclerosis
Some speech impairments may also have to do with family history, such as when parents or siblings have experienced language or speech difficulties. Other causes may include premature birth, pregnancy complications, or delivery difficulties. Voice overuse and chronic coughs can also cause speech issues.
The most common way that speech disorders are treated involves seeking professional help. If patients and families feel that symptoms warrant therapy, health professionals can help determine how to fix a speech impediment. Early treatment is best to curb speech disorders, but impairments can also be treated later in life.
Professionals in the speech therapy field include speech-language pathologists (SLPs) . These practitioners assess, diagnose, and treat communication disorders including speech, language, social, cognitive, and swallowing disorders in both adults and children. They may have an SLP assistant to help with diagnostic and therapy activities.
Speech-language pathologists may also share a practice with audiologists and audiology assistants. Audiologists help identify and treat hearing, balance, and other auditory disorders.

How Are Speech Disorders Diagnosed?
Typically, a pediatrician, social worker, teacher, or other concerned party will recognize the symptoms of a speech disorder in children. These individuals, who frequently deal with speech and language conditions and are more familiar with symptoms, will recommend that parents have their child evaluated. Adults who struggle with speech problems may seek direct guidance from a physician or speech evaluation specialist.
When evaluating a patient for a potential speech impediment, a physician will:
- Conduct hearing and vision tests
- Evaluate patient records
- Observe patient symptoms
A speech-language pathologist will conduct an initial screening that might include:
- An evaluation of speech sounds in words and sentences
- An evaluation of oral motor function
- An orofacial examination
- An assessment of language comprehension
The initial screening might result in no action if speech symptoms are determined to be developmentally appropriate. If a disorder is suspected, the initial screening might result in a referral for a comprehensive speech sound assessment, comprehensive language assessment, audiology evaluation, or other medical services.
Initial assessments and more in-depth screenings might occur in a private speech therapy practice, rehabilitation center, school, childcare program, or early intervention center. For older adults, skilled nursing centers and nursing homes may assess patients for speech, hearing, and language disorders.
How Are Speech Impediments Treated?
Once an evaluation determines precisely what type of speech sound disorder is present, patients can begin treatment. Speech-language pathologists use a combination of therapy, exercise, and assistive devices to treat speech disorders.
Speech therapy might focus on motor production (articulation) or linguistic (phonological or language-based) elements of speech, according to ASHA. There are various types of speech therapy available to patients.
Contextual Utilization — This therapeutic approach teaches methods for producing sounds consistently in different syllable-based contexts, such as phonemic or phonetic contexts. These methods are helpful for patients who produce sounds inconsistently.
Phonological Contrast — This approach focuses on improving speech through emphasis of phonemic contrasts that serve to differentiate words. Examples might include minimal opposition words (pot vs. spot) or maximal oppositions (mall vs. call). These therapy methods can help patients who use phonological error patterns.
Distinctive Feature — In this category of therapy, SLPs focus on elements that are missing in speech, such as articulation or nasality. This helps patients who substitute sounds by teaching them to distinguish target sounds from substituted sounds.
Core Vocabulary — This therapeutic approach involves practicing whole words that are commonly used in a specific patient’s communications. It is effective for patients with inconsistent sound production.
Metaphon — In this type of therapy, patients are taught to identify phonological language structures. The technique focuses on contrasting sound elements, such as loud vs. quiet, and helps patients with unintelligible speech issues.
Oral-Motor — This approach uses non-speech exercises to supplement sound therapies. This helps patients gain oral-motor strength and control to improve articulation.
Other methods professionals may use to help fix speech impediments include relaxation, breathing, muscle strengthening, and voice exercises. They may also recommend assistive devices, which may include:
- Radio transmission systems
- Personal amplifiers
- Picture boards
- Touch screens
- Text displays
- Speech-generating devices
- Hearing aids
- Cochlear implants
Resources for Professionals on How to Fix a Speech Impediment
The following resources provide information for speech therapists and other health professionals.
Assistive Devices: Information on hearing and speech aids from the NIDCD
Information for Audiologists: Publications, news, and practice aids for audiologists from ASHA
Information for Speech-Language Pathologists: Publications, news, and practice aids for SLPs from ASHA
Speech Disorder Tips for Families
For parents who are concerned that their child might have a speech disorder — or who want to prevent the development of a disorder — there are a number of activities that can help. The following are tasks that parents can engage in on a regular basis to develop literacy and speech skills.
- Introducing new vocabulary words
- Reading picture and story books with various sounds and patterns
- Talking to children about objects and events
- Answering children’s questions during routine activities
- Encouraging drawing and scribbling
- Pointing to words while reading books
- Pointing out words and sentences in objects and signs
Parents can take the following steps to make sure that potential speech impediments are identified early on.
- Discussing concerns with physicians
- Asking for hearing, vision, and speech screenings from doctors
- Requesting special education assessments from school officials
- Requesting a referral to a speech-language pathologist, audiologist, or other specialist
When a child is engaged in speech therapy, speech-language pathologists will typically establish collaborative relationships with families, sharing information and encouraging parents to participate in therapy decisions and practices.
SLPs will work with patients and their families to set goals for therapy outcomes. In addition to therapy sessions, they may develop activities and exercises for families to work on at home. It is important that caregivers are encouraging and patient with children during therapy.
Resources for Parents on How to Fix a Speech Impediment
The following resources provide additional information on treatment options for speech disorders.
Speech, Language, and Swallowing Disorders Groups: Listing of self-help groups from ASHA
ProFind: Search tool for finding certified SLPs and audiologists from ASHA
Baby’s Hearing and Communication Development Checklist: Listing of milestones that children should meet by certain ages from the NIDCD
If identified during childhood, speech disorders can be corrected efficiently, giving children greater communication opportunities. If left untreated, speech impediments can cause a variety of problems in adulthood, and may be more difficult to diagnose and treat.
Parents, teachers, doctors, speech and language professionals, and other concerned parties all have unique responsibilities in recognizing and treating speech disorders. Through professional therapy, family engagement, positive encouragement and a strong support network, individuals with speech impediments can overcome their challenges and develop essential communication skills.
Additional Sources
American Speech-Language-Hearing Association, Speech Sound Disorders
Identify the Signs, Signs of Speech and Language Disorders
Intermountain Healthcare, Phonological Disorders
MedlinePlus, Speech disorders – children
National Institutes of Health, National Institutes on Deafness and Other Communication Disorders, “Quick Statistics About Voice, Speech, Language”
Bring us your ambition and we’ll guide you along a personalized path to a quality education that’s designed to change your life.
Take Your Next Brave Step
Receive information about the benefits of our programs, the courses you'll take, and what you need to apply.

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

Speech Disorder
Speech Disorder: any defect or abnormality that prevents an individual from communicating by means of spoken words. Speech disorders may develop from nerve injury to the brain, muscular paralysis, structural defects, hysteria, or mental retardation.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Speech disorders - children
A speech disorder is a condition in which a person has problems creating or forming the speech sounds needed to communicate with others. This can make the person's speech difficult to understand.
Common speech disorders are:
- Articulation disorders
- Phonological disorders
- Voice disorders or resonance disorders
Speech disorders are different from language disorders in children . Language disorders refer to someone having difficulty with:
- Getting their meaning or message across to others (expressive language)
- Understanding the message coming from others (receptive language)
Speech is one of the main ways in which we communicate with those around us. It develops naturally, along with other signs of normal growth and development . Disorders of speech and language are common in preschool age children.
Disfluencies are disorders in which a person repeats a sound, word, or phrase. Stuttering may be the most serious disfluency. It may be caused by:
- Genetic abnormalities
- Emotional stress
- Any trauma to the brain or infection
Articulation and phonological disorders may occur in other family members. Other causes include:
- Problems or changes in the structure or shape of the muscles and bones used to make speech sounds. These changes may include cleft palate and tooth problems.
- Damage to parts of the brain or the nerves (such as from cerebral palsy ) that control how the muscles work together to create speech.
- Hearing loss.
Voice disorders are caused by problems when air passes from the lungs, through the vocal cords, and then through the throat, nose, mouth, and lips. A voice disorder may be due to:
- Acid from the stomach moving upward ( GERD )
- Cancer of the throat
- Cleft palate or other problems with the palate
- Conditions that damage the nerves that supply the muscles of the vocal cords
- Laryngeal webs or clefts (a birth defect in which a thin layer of tissue is between the vocal cords)
- Noncancerous growths (polyps, nodules, cysts, granulomas, papillomas, or ulcers) on the vocal cords
- Overuse of the vocal cords from screaming, constantly clearing the throat, or singing
- Hearing loss
Stuttering is the most common type of disfluency.
Symptoms of disfluency can include:
- Repetition of sounds, words, or parts of words or phrases after age 4 (I want...I want my doll. I...I see you.)
- Putting in (interjecting) extra sounds or words (We went to the...uh...store.)
- Making words longer (I am Boooobbby Jones.)
- Pausing during a sentence or words, often with the lips together
- Tension in the voice or sounds
- Frustration with attempts to communicate
- Head jerking while talking
- Eye blinking while talking
- Embarrassment with speech
ARTICULATION DISORDER
The child is not able to produce speech sounds clearly, such as saying "coo" instead of "school."
- Certain sounds (like "r", "l", or "s") may be consistently distorted or changed (such as making the 's' sound with a whistle).
- Errors may make it hard for people to understand the person (only family members may be able to understand a child).
PHONOLOGICAL DISORDER
The child does not use some or all of the speech sounds to form words as expected for their age.
- The last or first sound of words (most often consonants) may be left out or changed.
- The child may have no problem pronouncing the same sound in other words (a child may say "boo" for "book" and "pi" for "pig", but may have no problem saying "key" or "go").
VOICE DISORDERS
Other speech problems include:
- Hoarseness or raspiness to the voice
- Voice may break in or out
- Pitch of the voice may change suddenly
- Voice may be too loud or too soft
- Person may run out of air during a sentence
- Speech may sound odd because too much air is escaping through the nose (hypernasality) or too little air is coming out through the nose (hyponasality)
Exams and Tests
Your health care provider will ask about your child's developmental and family history. The provider will do some neurological screening and check for:
- Fluency of speech
- Any emotional stress
- Any underlying condition
- Effect of speech disorder on daily life
Some other evaluation tools used to identify and diagnose speech disorders are:
- Denver Articulation Screening Examination.
- Leiter International Performance scale-3.
- Goldman-Fristoe Test of Articulation 3 (GFTA-3).
- Arizona Articulation and Phonology Scale 4th Revision (Arizona-4).
- Prosody-voice screening profile.
A hearing test may also be done to check for hearing loss as a cause of the speech disorder.
Children may outgrow milder forms of speech disorders. The type of treatment will depend on the severity of the speech disorder and its cause.
Speech therapy may help with more severe symptoms or any speech problems that do not improve.
In therapy, the therapist may teach your child how to use their tongue to create certain sounds.
If a child has a speech disorder, parents are encouraged to:
- Avoid expressing too much concern about the problem, which can make matters worse by making the child more self-conscious.
- Avoid stressful social situations whenever possible.
- Listen patiently to the child, make eye contact, don't interrupt, and show love and acceptance. Avoid finishing sentences for them.
- Set aside time for talking.
Support Groups
More information and support for people with stuttering and their families can be found at:
- American Institute for Stuttering -- stutteringtreatment.org
- American Speech-Language-Hearing Association (ASHA) -- www.asha.org/
- The Stuttering Foundation -- www.stutteringhelp.org
- National Stuttering Association (NSA) -- westutter.org
Outlook (Prognosis)
The outlook depends on the cause of the disorder. Speech can often be improved with speech therapy. Early treatment is likely to have better results.
Possible Complications
Speech disorders may lead to challenges with social interactions due to difficulty communicating.
When to Contact a Medical Professional
Contact your provider if:
- Your child's speech is not developing according to normal milestones.
- You think your child is in a high-risk group.
- Your child is showing signs of a speech disorder.
Hearing loss is a risk factor for speech disorders. At-risk infants should be referred to an audiologist for a hearing test. Hearing and speech therapy can then be started, if necessary.
As young children begin to speak, some disfluency is common, and most of the time, it goes away without treatment. If you place too much attention on the disfluency, a stuttering pattern may develop.
Alternative Names
Articulation deficiency; Articulation disorder; Phonological disorder; Voice disorders; Vocal disorders; Disfluency; Communication disorder - speech disorder; Speech disorder - stuttering; Cluttering; Stammering; Childhood onset fluency disorder
American Speech-Language-Hearing Association website. Voice disorders. www.asha.org/Practice-Portal/Clinical-Topics/Voice-Disorders/ . Accessed February 22, 2024.
Driver LE, Nelson ME. Pediatric speech disorders. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery . 7th ed. Philadelphia, PA: Elsevier; 2021:chap 183.
Simms MD. Language development and communication disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics . 21st ed. Philadelphia, PA: Elsevier; 2020:chap 52.
Trauner DA, Nass RD. Developmental language disorders. In: Swaiman KF, Ashwal S, Ferriero DM, et al, eds. Swaiman's Pediatric Neurology: Principles and Practice . 6th ed. Philadelphia, PA: Elsevier; 2017:chap 53.
Zajac DJ. Evaluation and management of speech disorders for the patient with cleft palate. In: Fonseca RJ, ed. Oral and Maxillofacial Surgery . 3rd ed. St Louis, MO: Elsevier; 2018:chap 32.
Review Date 2/17/2024
Updated by: Charles I. Schwartz, MD, FAAP, Clinical Assistant Professor of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, General Pediatrician at PennCare for Kids, Phoenixville, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Related MedlinePlus Health Topics
- Speech and Language Problems in Children
- To save this word, you'll need to log in. Log In
speech defect
Definition of speech defect
Love words.
You must — there are over 200,000 words in our free online dictionary, but you are looking for one that’s only in the Merriam-Webster Unabridged Dictionary.
Start your free trial today and get unlimited access to America's largest dictionary, with:
- More than 250,000 words that aren't in our free dictionary
- Expanded definitions, etymologies, and usage notes
- Advanced search features
Dictionary Entries Near speech defect
speech form
Cite this Entry
“Speech defect.” Merriam-Webster.com Dictionary , Merriam-Webster, https://www.merriam-webster.com/dictionary/speech%20defect. Accessed 10 Jun. 2024.
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
What's the difference between 'fascism' and 'socialism', more commonly misspelled words, commonly misspelled words, how to use em dashes (—), en dashes (–) , and hyphens (-), absent letters that are heard anyway, popular in wordplay, the words of the week - june 7, 8 words for lesser-known musical instruments, 9 superb owl words, 10 words for lesser-known games and sports, your favorite band is in the dictionary, games & quizzes.


10 Most Common Speech-Language Disorders & Impediments
As you get to know more about the field of speech-language pathology you’ll increasingly realize why SLPs are required to earn at least a master’s degree . This stuff is serious – and there’s nothing easy about it.
In 2016 the National Institute on Deafness and Other Communication Disorders reported that 7.7% of American children have been diagnosed with a speech or swallowing disorder. That comes out to nearly one in 12 children, and gets even bigger if you factor in adults.
Whether rooted in psycho-speech behavioral issues, muscular disorders, or brain damage, nearly all the diagnoses SLPs make fall within just 10 common categories…
Types of Speech Disorders & Impediments
Apraxia of speech (aos).
Apraxia of Speech (AOS) happens when the neural pathway between the brain and a person’s speech function (speech muscles) is lost or obscured. The person knows what they want to say – they can even write what they want to say on paper – however the brain is unable to send the correct messages so that speech muscles can articulate what they want to say, even though the speech muscles themselves work just fine. Many SLPs specialize in the treatment of Apraxia .
There are different levels of severity of AOS, ranging from mostly functional, to speech that is incoherent. And right now we know for certain it can be caused by brain damage, such as in an adult who has a stroke. This is called Acquired AOS.
However the scientific and medical community has been unable to detect brain damage – or even differences – in children who are born with this disorder, making the causes of Childhood AOS somewhat of a mystery. There is often a correlation present, with close family members suffering from learning or communication disorders, suggesting there may be a genetic link.
Mild cases might be harder to diagnose, especially in children where multiple unknown speech disorders may be present. Symptoms of mild forms of AOS are shared by a range of different speech disorders, and include mispronunciation of words and irregularities in tone, rhythm, or emphasis (prosody).
Stuttering – Stammering
Stuttering, also referred to as stammering, is so common that everyone knows what it sounds like and can easily recognize it. Everyone has probably had moments of stuttering at least once in their life. The National Institute on Deafness and Other Communication Disorders estimates that three million Americans stutter, and reports that of the up-to-10-percent of children who do stutter, three-quarters of them will outgrow it. It should not be confused with cluttering.
Most people don’t know that stuttering can also include non-verbal involuntary or semi-voluntary actions like blinking or abdominal tensing (tics). Speech language pathologists are trained to look for all the symptoms of stuttering , especially the non-verbal ones, and that is why an SLP is qualified to make a stuttering diagnosis.
The earliest this fluency disorder can become apparent is when a child is learning to talk. It may also surface later during childhood. Rarely if ever has it developed in adults, although many adults have kept a stutter from childhood.
Stuttering only becomes a problem when it has an impact on daily activities, or when it causes concern to parents or the child suffering from it. In some people, a stutter is triggered by certain events like talking on the phone. When people start to avoid specific activities so as not to trigger their stutter, this is a sure sign that the stutter has reached the level of a speech disorder.
The causes of stuttering are mostly a mystery. There is a correlation with family history indicating a genetic link. Another theory is that a stutter is a form of involuntary or semi-voluntary tic. Most studies of stuttering agree there are many factors involved.
Dysarthria is a symptom of nerve or muscle damage. It manifests itself as slurred speech, slowed speech, limited tongue, jaw, or lip movement, abnormal rhythm and pitch when speaking, changes in voice quality, difficulty articulating, labored speech, and other related symptoms.
It is caused by muscle damage, or nerve damage to the muscles involved in the process of speaking such as the diaphragm, lips, tongue, and vocal chords.
Because it is a symptom of nerve and/or muscle damage it can be caused by a wide range of phenomena that affect people of all ages. This can start during development in the womb or shortly after birth as a result of conditions like muscular dystrophy and cerebral palsy. In adults some of the most common causes of dysarthria are stroke, tumors, and MS.
A lay term, lisping can be recognized by anyone and is very common.
Speech language pathologists provide an extra level of expertise when treating patients with lisping disorders . They can make sure that a lisp is not being confused with another type of disorder such as apraxia, aphasia, impaired development of expressive language, or a speech impediment caused by hearing loss.
SLPs are also important in distinguishing between the five different types of lisps. Most laypersons can usually pick out the most common type, the interdental/dentalised lisp. This is when a speaker makes a “th” sound when trying to make the “s” sound. It is caused by the tongue reaching past or touching the front teeth.
Because lisps are functional speech disorders, SLPs can play a huge role in correcting these with results often being a complete elimination of the lisp. Treatment is particularly effective when implemented early, although adults can also benefit.
Experts recommend professional SLP intervention if a child has reached the age of four and still has an interdental/dentalised lisp. SLP intervention is recommended as soon as possible for all other types of lisps. Treatment includes pronunciation and annunciation coaching, re-teaching how a sound or word is supposed to be pronounced, practice in front of a mirror, and speech-muscle strengthening that can be as simple as drinking out of a straw.
Spasmodic Dysphonia
Spasmodic Dysphonia (SD) is a chronic long-term disorder that affects the voice. It is characterized by a spasming of the vocal chords when a person attempts to speak and results in a voice that can be described as shaky, hoarse, groaning, tight, or jittery. It can cause the emphasis of speech to vary considerably. Many SLPs specialize in the treatment of Spasmodic Dysphonia .
SLPs will most often encounter this disorder in adults, with the first symptoms usually occurring between the ages of 30 and 50. It can be caused by a range of things mostly related to aging, such as nervous system changes and muscle tone disorders.
It’s difficult to isolate vocal chord spasms as being responsible for a shaky or trembly voice, so diagnosing SD is a team effort for SLPs that also involves an ear, nose, and throat doctor (otolaryngologist) and a neurologist.
Have you ever heard people talking about how they are smart but also nervous in large groups of people, and then self-diagnose themselves as having Asperger’s? You might have heard a similar lay diagnosis for cluttering. This is an indication of how common this disorder is as well as how crucial SLPs are in making a proper cluttering diagnosis .
A fluency disorder, cluttering is characterized by a person’s speech being too rapid, too jerky, or both. To qualify as cluttering, the person’s speech must also have excessive amounts of “well,” “um,” “like,” “hmm,” or “so,” (speech disfluencies), an excessive exclusion or collapsing of syllables, or abnormal syllable stresses or rhythms.
The first symptoms of this disorder appear in childhood. Like other fluency disorders, SLPs can have a huge impact on improving or eliminating cluttering. Intervention is most effective early on in life, however adults can also benefit from working with an SLP.
Muteness – Selective Mutism
There are different kinds of mutism, and here we are talking about selective mutism. This used to be called elective mutism to emphasize its difference from disorders that caused mutism through damage to, or irregularities in, the speech process.
Selective mutism is when a person does not speak in some or most situations, however that person is physically capable of speaking. It most often occurs in children, and is commonly exemplified by a child speaking at home but not at school.
Selective mutism is related to psychology. It appears in children who are very shy, who have an anxiety disorder, or who are going through a period of social withdrawal or isolation. These psychological factors have their own origins and should be dealt with through counseling or another type of psychological intervention.
Diagnosing selective mutism involves a team of professionals including SLPs, pediatricians, psychologists, and psychiatrists. SLPs play an important role in this process because there are speech language disorders that can have the same effect as selective muteness – stuttering, aphasia, apraxia of speech, or dysarthria – and it’s important to eliminate these as possibilities.
And just because selective mutism is primarily a psychological phenomenon, that doesn’t mean SLPs can’t do anything. Quite the contrary.
The National Institute on Neurological Disorders and Stroke estimates that one million Americans have some form of aphasia.
Aphasia is a communication disorder caused by damage to the brain’s language capabilities. Aphasia differs from apraxia of speech and dysarthria in that it solely pertains to the brain’s speech and language center.
As such anyone can suffer from aphasia because brain damage can be caused by a number of factors. However SLPs are most likely to encounter aphasia in adults, especially those who have had a stroke. Other common causes of aphasia are brain tumors, traumatic brain injuries, and degenerative brain diseases.
In addition to neurologists, speech language pathologists have an important role in diagnosing aphasia. As an SLP you’ll assess factors such as a person’s reading and writing, functional communication, auditory comprehension, and verbal expression.
Speech Delay – Alalia
A speech delay, known to professionals as alalia, refers to the phenomenon when a child is not making normal attempts to verbally communicate. There can be a number of factors causing this to happen, and that’s why it’s critical for a speech language pathologist to be involved.
The are many potential reasons why a child would not be using age-appropriate communication. These can range anywhere from the child being a “late bloomer” – the child just takes a bit longer than average to speak – to the child having brain damage. It is the role of an SLP to go through a process of elimination, evaluating each possibility that could cause a speech delay, until an explanation is found.
Approaching a child with a speech delay starts by distinguishing among the two main categories an SLP will evaluate: speech and language.
Speech has a lot to do with the organs of speech – the tongue, mouth, and vocal chords – as well as the muscles and nerves that connect them with the brain. Disorders like apraxia of speech and dysarthria are two examples that affect the nerve connections and organs of speech. Other examples in this category could include a cleft palette or even hearing loss.
The other major category SLPs will evaluate is language. This relates more to the brain and can be affected by brain damage or developmental disorders like autism. There are many different types of brain damage that each manifest themselves differently, as well as developmental disorders, and the SLP will make evaluations for everything.
Issues Related to Autism
While the autism spectrum itself isn’t a speech disorder, it makes this list because the two go hand-in-hand more often than not.
The Centers for Disease Control and Prevention (CDC) reports that one out of every 68 children in our country have an autism spectrum disorder. And by definition, all children who have autism also have social communication problems.
Speech-language pathologists are often a critical voice on a team of professionals – also including pediatricians, occupational therapists, neurologists, developmental specialists, and physical therapists – who make an autism spectrum diagnosis .
In fact, the American Speech-Language Hearing Association reports that problems with communication are the first detectable signs of autism. That is why language disorders – specifically disordered verbal and nonverbal communication – are one of the primary diagnostic criteria for autism.
So what kinds of SLP disorders are you likely to encounter with someone on the autism spectrum?
A big one is apraxia of speech. A study that came out of Penn State in 2015 found that 64 percent of children who were diagnosed with autism also had childhood apraxia of speech.
This basic primer on the most common speech disorders offers little more than an interesting glimpse into the kind of issues that SLPs work with patients to resolve. But even knowing everything there is to know about communication science and speech disorders doesn’t tell the whole story of what this profession is all about. With every client in every therapy session, the goal is always to have the folks that come to you for help leave with a little more confidence than when they walked in the door that day. As a trusted SLP, you will build on those gains with every session, helping clients experience the joy and freedom that comes with the ability to express themselves freely. At the end of the day, this is what being an SLP is all about.
Ready to make a difference in speech pathology? Learn how to become a Speech-Language Pathologist today
- Emerson College - Master's in Speech-Language Pathology online - Prepare to become an SLP in as few as 20 months. No GRE required. Scholarships available.
- NYU Steinhardt - NYU Steinhardt's Master of Science in Communicative Sciences and Disorders online - ASHA-accredited. Bachelor's degree required. Graduate prepared to pursue licensure.
- Arizona State University - Online - Online Bachelor of Science in Speech and Hearing Science - Designed to prepare graduates to work in behavioral health settings or transition to graduate programs in speech-language pathology and audiology.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Medscape J Med
- v.10(6); 2008
Speech-Language Impairment: How to Identify the Most Common and Least Diagnosed Disability of Childhood
Patricia a. prelock.
Department of Communication Sciences, University of Vermont, Burlington, Vermont
Tiffany Hutchins
Frances p. glascoe.
Department of Pediatrics, Vanderbilt University, Nashville, Tennessee
Disclosure: Tiffany Hutchins, PhD, has disclosed no relevant financial relationships in addition to her employment.
Disclosure: Frances P. Glascoe, PhD, has disclosed no relevant financial relationships in addition to her employment.
Abstract and Introduction
Speech-language problems are the most common disability of childhood yet they are the least well detected, particularly in primary care settings. The goal of this article is to: (1) define the nature of speech-language problems, their causes, and consequences; (2) facilitate early recognition by healthcare providers via accurate screening and surveillance measures suitable for busy clinics; and (3) describe the referral and intervention process.
Introduction
Speech-language deficits are the most common of childhood disabilities and affect about 1 in 12 children or 5% to 8% of preschool children. [1] The consequences of untreated speech-language problems are significant and lead to behavioral challenges, mental health problems, reading difficulties, [2] and academic failure including in-grade retention and high school dropout. [3] Yet, such problems are ones that are least well detected in primary care, [4] even though intervention is available and plentiful.
Speech-language impairments embrace a wide range of conditions that have, at their core, challenges in effective communication. As the term implies, they include speech disorders which refer to impairment in the articulation of speech sounds, fluency, and voice as well as language disorders which refer to impairments in the use of the spoken (or signed or written) system and may involve the form of language (grammar and phonology), the content of language (semantics), and the function of language (pragmatics). [5] These may also be described more generally as communication disorders which are typically classified by their impact on a child's receptive skills (ie, the ability to understand what is said or to decode, integrate, and organize what is heard) and expressive skills (ie, the ability to articulate sounds, use appropriate rate and rhythm during speech, exhibit appropriate vocal tone and resonance, and use sounds, words, and sentences in meaningful contexts). There are common conditions in infants, toddlers, and preschoolers that are associated with receptive and expressive communication challenges as presented in Table 1 . [6 – 17]
Disorders in Young Children Commonly Associated With Receptive and Expressive Communication Problems
| Condition & Cause | Receptive Communication Problems | Expressive Communication Problems |
|---|---|---|
| Psychosocial risk, abuse and neglect | Less talkative and fewer conversational skills than expected; seldom volunteer ideas or discuss feelings; utterances shorter than peers | |
| Autism spectrum disorder | Difficulty analyzing, integrating, and processing information; misinterpretation of social cues | Variability in speech production from functionally nonverbal to echolalic speech to nearly typical speech; use of language in social situations is more challenging than producing language forms (eg, articulating speech sounds, using sentence structure) ; tendency to use verbal scripts; difficulty selecting the right words to represent intended meaning; often mechanical voice quality |
| Brain injury | Difficulty making connections, inferences and using information to solve problems; challenges in attention and memory which affect linguistic processing; challenges in understanding figurative language and multiple meaning words | Greatest difficulty is commonly inpragmatics – using language appropriately across contexts, especially narratives and conversations |
| Cerebral palsy | Speech sound discrimination, information processing and attention can be areas of challenge; language comprehension is affected by cognitive status | Dysarthric speech – slower rate, with shorter phrases or prolonged pauses; articulation is often imprecise with distorted vowel productions; voice quality can be breathy or harsh, hypernasal with a low or monotone pitch; apraxic speech – sound substitutions that can be inconsistent, groping for sound production and nonfluent volitional speech with more fluent automatic speech ; language production is affected by breath support as well as cognitive status |
| Fetal drug or alcohol exposure | Difficulty comprehending verbal information, especially understanding abstract concepts, multiple word meanings, and words indicating time and space | Fewer vocalizations in infancy, poor use of gestures and delays in oral language ; poor word retrieval, shorter sentences, and less well-developed conversational skills |
| Fluency disorders | Difficulty with the rate and rhythm of speech; false starts; repetitions of sounds, syllables and words; may or may not be accompanied by atypical physical behaviors (eg, grimacing, head bobbing) | |
| Hearing impairment | Difficulty with sound perception and discrimination, voice recognition, and understanding of speech, especially under adverse hearing conditions | Sound productions made until about 6 months; limited oral output depending on degree of hearing loss; for oral communicators, vocal resonance, speech sound accuracy, and syntactic structure often affected |
| Intellectual Disability | Comprehension of language is often below cognitive ability ; difficulty organizing and categorizing information heard for later retrieval; difficulty with abstract concepts; difficulty interpreting information presented auditorily | Production is often below cognitive ability ; similar but slower developmental path than typical peers; tendency to use more immature language forms; tendency to produce shorter and less elaborated utterances |
| Specific language impairment | Slower and less efficient information processing , ; limited capacity for understanding language , | Shorter, less elaborated sentences than typical peers; difficulty in rule formulation for speech sound, word, and sentence productions ; ineffective use of language forms in social contexts sometimes leading to inappropriate utterances ; poorly developed vocabulary |
It is important to distinguish speech and language impairment from language delay and language difference. Language delay is characterized by the emergence of language that is relatively late albeit typical in its pattern of development. In contrast to an impairment or a delay, a language difference is associated with systematic variation in vocabulary, grammar, or sound structures. Such variation is “used by a group of individuals [and] reflects and is determined by shared regional, social, or cultural and ethnic factors” and is not considered a disorder. [18]
Unfortunately, non-native speakers of English, speakers of various dialects (whose language also varies within dialect), and bilingual or multilingual speakers are frequently classified as language delayed or disordered when, in fact, they are language different [18 , 19] –although problems of underidentification also occur. This is particularly important in an increasingly pluralistic society such as ours in which 1 of 4 people identify as other than white non-Hispanic, approximately 17% of the population is bilingual (mostly speaking Spanish and English), and where minorities represent more than 50% of the population in several cities and counties. [20]
The overidentification of culturally and linguistically diverse populations commonly occurs when a mismatch is observed and incorrectly interpreted between a language used in a particular community and that of the majority culture. This may be seen most clearly in the improper use of formal tests of speech and language to assess the competencies of speakers who are dissimilar to the sample upon which the test was normed and developed. [21] Similar errors also occur during informal evaluations of language and literacy as when the sound structure of the language influences the spelling or grammatical conventions used in written discourse. [22] With regard to bilingualism, it is commonly assumed that children's acquisition of 1 or both languages is delayed; however, the effects of bilingualism are more complex and differ with the age of the child, the nature of the linguistic input, and the manner and timing of language acquisition. What is clear is that equivalent proficiency in each language should not be expected or assumed as this has the potential to lead to misidentification of a speech and language impairment. (For more information on the effects of bilingualism on language learning, see http://asha.org/public/speech/development/BilingualChildren.htm and http://asha.org/public/speech/development/second.htm ) In the case of culturally and linguistically diverse individuals, decisions to intervene and bring language use in line with that of the majority culture or promote proficiency in the dominant language are not inappropriate; however, such decisions must be seen as separate from the language difference vs disorder question.
In your experience, which of the following is the most important barrier to the effective assessment of speech and language impairment in young children? (Select only 1 answer.)
- ○ Variability in the development of speech and language in young children
- ○ Lack of effective screening tools that discriminate children with and without speech and language impairment
- ○ Lack of accurate parent interview tools that identify clear concerns in speech and language development
- ○ Insufficient time with young children in the clinical setting to observe speech and language skills
- ○ Inadequate understanding of milestones for speech and language development
How confident are you that you are up-to-date in the diagnosis and management of speech and language impairment in young children? (Select only 1 answer.)
- ○ Not at all confident
- ○ Somewhat confident
- ○ Confident
- ○ Very confident
All of the following statements about young children with speech and language impairment are true except :
- ○ Young children tend to produce words with sounds that are consistent with the words they already know
- ○ Young children are able to communicate intent before speaking their first words
- ○ Disfluency is a common occurrence in a young child's early speech
- ○ Children usually begin to put 2 words together at 30 months
Answer: Children usually begin to put 2 words together at 30 months. Children usually begin to put 2 words together at 18 months.
Etiology, Neurobiology, and Prevalence of Speech-Language Impairments
The etiology of most cases of speech-language impairments is unknown but diverse causes are suspected. The range of causes or origins includes anatomical abnormalities, cognitive deficits, faulty learning, genetic differences, hearing impairments, neurologic impairments, or physiologic abnormalities. [6] As noted above, language differences as revealed in the communication output associated with diverse cultural, ethnic, regional or social dialects are not considered disorders. [5] Speech and language impairments may be acquired (ie, result from illness, injury or environmental factors) or congenital (ie, present at birth).
Children with speech and language impairment are an under-representation of the broader occurrence of communication disorders, [23] especially considering the co-occurrence of communication disorders with other disabilities (eg, learning disabilities). Approximately 8% to 12% of preschool populations exhibit language impairments. [6] Among children enrolled in early intervention programs, 46% have communication impairments while 26% have developmental delays in multiple areas, usually including language skills. [24] These findings indicate that the most common presentation of disability in preschoolers involves problems with language.
In a family with a child with a speech and language impairment, which of the following would be clinically appropriate?
- ○ Reassure the parents that the child is just a late talker and will catch up
- ○ Urge the parents to have their child undergo genetic testing
- ○ Discourage the child's parents and sibling(s) from talking for the child as this may be a primary cause of a speech and language impairment
- ○ Advise the parent to have the child's hearing tested
Answer: Advise the parent to have the child's hearing tested. This is appropriate because hearing would be the first condition to rule out as a potential cause of a speech and language delay.
Course and Prognosis
Speech-language impairment sometimes emerges during infancy with challenges in response to sound, atypical birth cries, or limited response to others and progresses through the toddler and preschool age with limited comprehension of spoken language and difficult interactions with peers and others as well as delays in producing first words and word combinations. Speech and language difficulties often persist in school age with difficulties following directions, attending and comprehending oral and written language, and problems producing narratives and using language appropriately in social contexts. Parents are often the first to notice difficulties as they encounter other children with more advanced speech-language skills and thus often wonder if their child is behind. [25] Although many parents raise concerns to primary care providers, many do not. In turn, primary care providers who do not use quality screening tools often dismiss parental concerns with panaceas such as, “He's a boy. Boys talk later.” Or, “Let's give this some time and see if it continues.” Yet, parental concerns about speech and language are associated with developmental disabilities [26] and, thus, careful screening with accurate tools is the requisite response. [27]
The use of a “wait and see” approach underscores the difficulty in distinguishing children who are language delayed from those who have a speech and language impairment. Although most children who have aspeech and language impairment have a history of language delay, only one quarter to one half of late-talkers are eventually diagnosed with a language disorder. [19] In advocating for a more aggressive response for late-talking children, some have argued for careful scrutiny of other risk factors that may guide decisions to refer and intervene. [19] Predictors of a true speech and language impairment that should be considered include poor receptive language skills, [28] limited expressive language skills (eg, small vocabulary, few verbs), and limited development in the sound structure of a language (eg, limited number of consonants, limited variety in babbling structure, vowel errors). [26] Additional predictors include nonspeech (eg, behavioral problems, few gestures, little imitation or symbolic play), environmental (eg, low socioeconomic status, parental use of a directive rather than sensitive and responsive interactional style), and hereditary factors (eg, family history). [26] As a general recommendation, professionals are urged to consider a larger number of risk factors with greater concern. [26]
Often speech-language impairments can be difficult to distinguish from what is considered typical variations in speech and language. For example, disfluencies in speech may be either normal or abnormal. In the nonstuttering child, the most common disfluencies include 1-unit word repetitions (eg, “I… I want that”), interjections (eg, “I saw a… um… picture”), and revisions (eg, “I don't know where… Mommy, help me find my doll”) and, when combined, comprise no more than 10% of words spoken. [29] In the stuttering child, the fluency disorder typically emerges between the ages of 2 and 5 years, is more common among males than females, and is characterized by more than 10% disfluencies in speech, multi-unit syllable (eg, “s-s-s-s-s-September”) and word (eg, “That's my-my-my ball”) repetitions, and may be accompanied by secondary behaviors such as eye-blinking, head-bobbing, or grimacing, as well as feelings of frustration or embarrassment surrounding the stuttering event. [29]
Identification of speech and language impairments is further complicated by the fact that they often masquerade as other diagnostic conditions. For example, children with a diagnosis of attention-deficit/hyperactivity disorder (ADHD) may in fact have an underlying language disorder. Differential diagnosis is challenged by the diagnostic criteria shared between the 2 conditions. Specifically, the diagnostic criteria for ADHD share several characteristics with language disorders including difficulty listening when spoken to, following instructions, talking excessively, blurting out answers, interrupting, and waiting for turns in conversation. [30] Similarly, 50% of preschoolers presenting for psychiatric services were found in several studies to have undiagnosed language impairment. [31 , 32]
The diagnostic criteria for speech-language impairments are defined both by the Diagnostic and Statistical Manual of Mental Disorders , 4th edition (DSM-IV) [33 , 34] and by the Individuals with Disabilities Education Act (IDEA) through the US Department of Education. Table 2 specifies the criteria for communication disorders as described in the DSM-IV. As an example of eligibility criteria for speech-language impairment in response to IDEA guidelines, Vermont indicates that children must demonstrate significant deficits greater than 2 standard deviations below the mean in listening comprehension (eg, measures of auditory (language) processing or comprehension of connected speech including semantics, syntax, phonology, recalling information, following directions and pragmatics) and/or oral expression (eg, measures of oral discourse-syntax, semantics, phonology and pragmatics; voice; fluency; articulation) to qualify as speech or language impaired. [35]
Characteristics of Communication Disorders as Described in the DSM-IV [33 , 34]
| Characteristics | Expressive Language Disorder | Mixed Receptive-Expressive Language Disorder |
|---|---|---|
| Standardized tests indicate skill area is substantially below what is expected considering chronological age (CA), IQ, and education | Expressive language development (eg, vocabulary, tense errors, word recall, sentence length, and complexity) is below nonverbal IQ and receptive language | Battery of measures of receptive and expressive languagedevelopment (eg, understanding words, sentences, or specific word types-spatial terms) is below nonverbal IQ |
| Difficulties interfere with academic or occupational achievement or with social communication | X | X |
| If mental retardation, environmental deprivation, sensory or speech motor deficit is present, difficulties are greater than what is expected | X | X |
| Criteria not met for mixed receptive-expressive language disorder | X | |
| Criteria not met for pervasive developmental disorder | X | X |
Distinguishing children with speech-language deficits from those with other disabilities is often a challenging task as several disabilities share characteristics and have similar diagnostic criteria. For example, an intellectual disability is one in which a child's performance falls at or below 1.5 standard deviations from the mean on a test of intellectual ability with concurrent deficits in adaptive behavior. Children with intellectual disabilities, however, often have significant challenges in receptive and expressive communication as is typical of children with speech and language impairments. Children with learning disabilities have deficits in 1 or more basic skill areas including oral expression and listening comprehension, challenges characteristic of children with speech-language impairments. Children with pervasive developmental disorders/autism exhibit marked impairments in communication and social interaction and restricted and repetitive stereotyped patterns of behavior. Although social impairment is a defining feature of autism, communication impairments are similar to those with a speech-language impairment.
Which of the following is not true of speech-language impairment?
- ○ Early intervention is critical as speech-language impairments place children at risk for later academic difficulties
- ○ Most children with speech-language impairments have intellectual deficits
- ○ Communication disorders may manifest themselves at different stages of life
- ○ Children with learning disabilities are likely to have speech and language impairments
Answer: Most children with speech-language impairments have intellectual deficits. Although many children who have mental retardation have speech-language impairments, most children with specific speech-language impairments have nonverbal intelligence within normal limits.
Screening and Early Assessment of Speech-Language Disorders
The American Academy of Pediatrics recommends ongoing surveillance and periodic use of broad-band screening measures at all well-visits. Table 3 provides information on a number of tools that have high levels of accuracy in detecting speech-language problems and other disabilities. All included measures were standardized on national samples, proven to be reliable, and validated against a range of measures. When used, referral rates to early intervention programs rise to meet prevalence. [36] In the absence of accurate measures, most providers rely on informal milestone checklists. These lack criteria and are probably the leading reason why only about 1 in 4 children with disabilities of any kind are referred for needed assistance.
Accurate Developmental, Mental Health/Behavioral, and Academic Screens Suitable for Primary Care *
| Developmental-Behavioral Screens for Young Children | Age Range | Description | Scoring | Accuracy | Time Frame/Costs |
|---|---|---|---|---|---|
| (2002), Ellsworth & Vandermeer Press, Ltd., 1013 Austin Court, Nolensville TN 37135; phone: 615-776-4121 fax: 615-776-4119; ($30.00)PEDS is also available online together with the Modified Checklist of Autism in Toddlers for electronic records: contact. | Birth to 8 years | 10 questions eliciting parents' concerns in English, Spanish, Vietnamese, Somali, Arabic, and many other languages. Written at the 5th grade level. Determines when to refer, provide a second screen, provide patient education, or monitor development, behavior/emotional, and academic progress. Provides longitudinal surveillance and triage. | Identifies children as low, moderate, or high risk for various kinds of disabilities and delays | Sensitivity ranges from 74% to 79% and specificity ranges from 70% to 80% across age levels | About 2 minutes (if interview needed) Print materials = ∼$0.31 Admin. = ∼$0.88 Total = ∼$1.19 |
| (formerly Infant Monitoring System) (2004), Paul H. Brookes Publishing, Inc., PO Box 10624, Baltimore, MD 21285; phone: 1-800-638-3775 ($199) For screening mental/health/behavioral problems, there is also the , which works like the ASQ. | 4–60 months | Parents indicate children's developmental skills on 25–35 items (4–5 pages) using a different form for each well visit. Reading level varies across items from 3rd to 12th grade. Can be used in mass mail-outs for child-find programs. Available in English, Spanish, French, and Korean. | Single pass/fail score for developmental status | Sensitivity ranges from 70% to 90% at all ages except the 4-month level. Specificity ranges from 76% to 91% | About 15 minutes (if interview needed) Materials = ∼$0.40 Admin. = ∼$4.20 Total = ∼$4.60 |
| (1998). Paul H. Brookes Publishing, Inc., P.O. Box 10624, Baltimore, MD, 21285; phone 1-800-638-3775. (Part of CSBS-DP, ) ($99.95 w/CD-ROM) | 6–24 months | Parents complete the Checklist's 24 multiple-choice questions in English. Reading level is 6th grade. Based on screening for delays in language development as the first evident symptom that a child is not developing typically. Does not screen for motor milestones. The Checklist is copyrighted but remains free for use at the Brookes Web site although the factor scoring system is complicated and requires purchase of the CD-ROM. | Manual table of cut-off scores at 1.25 standard deviations below the mean O0052, an optional scoring CD-ROM | Sensitivity is 78%; specificity is 84%. | About 5 to 10 minutes Materials = ∼$0.20 Admin. = ∼$3.40 Total = ∼$3.60 |
| (2007), Ellsworth & Vandermeer Press, Ltd., 1013 Austin Court, Nolensville TN 37135; phone: 615-776-4121; fax: 615-776-4119 ($275) | 0–8 years | PEDS-DM consists of 6–8 items at each age level (spanning the well visit schedule). Each item taps a different domain (fine/gross motor, self-help, academics, expressive/receptive language, social-emotional). Items are administered by parents or professionals. Forms are laminated and marked with a grease pencil. It can be used to complement PEDS or stand alone. Administered by parent report or directly. Written at the 2nd grade level. A longitudinal score form tracks performance. Supplemental measures also include the M-CHAT, Family Psychosocial Screen, PSC-17, the SWILS, the Vanderbilt, and a measure of parent-child interactions. An Assessment Level version is available for NICU follow-up and early intervention programs. | Cutoffs tied to performance above and below the 16th percentile for each item and its domain. On the Assessment Level, age equivalent scores are produced and enable users to compute percentage of delays. | Sensitivity ranges from 75% to 87%; specificity ranges from 71% to 88% for performance in each domain. Sensitivity ranges from 70% to 94%; specificity ranges from 77% to 93% across age levels. | About 3–5 minutes Materials = ∼.$0.02 Admin. = ∼$1.00 Total = ∼$1.02 |
| . Jellinek MS, Murphy JM, Robinson J, et al. Pediatric Symptom Checklist: Screening school age children for academic and psychosocial dysfunction. , 1988;112:201-209 (the test is included in the article). Also can be freely downloaded at or with factor scores at . The Pictorial PSC, useful with low-income Spanish speaking families, is included in PEDS: Developmental Milestones ( ). | 4–16 years | 35 short statements of problem behaviors including both externalizing (conduct) and internalizing (depression, anxiety, adjustment, etc.) Ratings of never, sometimes, or often are assigned a value of 0,1, or 2. Scores totaling 28 or more suggest referrals. Factor scores identify attentional, internalizing, and externalizing problems. Factor scoring is available for download at: | Single refer/nonrefer score | All but one study showed high sensitivity (80% to 95%) but somewhat scattered specificity (68% – 100%). | About 7 minutes (if interview needed) Materials = ∼$0.10 Admin. = ∼$2.38 Total = ∼$2.48 |
| Glascoe FP. , 2002. Items courtesy of Curriculum Associates, Inc. The SWILS can be freely downloaded at: and is included in PEDS: Developmental Milestones | 6–14 years | Children are asked to read 29 common safety words (eg, High Voltage, Wait, Poison) aloud. The number of correctly read words is compared to a cutoff score. Results predict performance in math, written language, and a range of reading skills. Test content may serve as a springboard to injury prevention counseling. | Single cutoff score indicating the need for a referral | 78% to 84% sensitivity and specificity across all ages | About 7 minutes (if interview needed) Materials = ∼$0.30 Admin. = ∼$2.38 Total = ∼$2.68 |
| Kemper KJ, Kelleher KJ. Family psychosocial screening: instruments and techniques. . 1996;4:325-339. The measures are included in the article and downloadable at (included in the PEDS: Developmental Milestones). | Screens parents and best used along with the above screens | A 2-page clinic intake form that identifies psychosocial risk factors associated with developmental problems including: a 4-item measure of parental history of physical abuse as a child; (2) a 6-item measure of parental substance abuse; and (3) a 3-item measure of maternal depression. | Refer/nonrefer scores for each risk factor. Also has guides to referring and resource lists. | All studies showed sensitivity and specificity to larger inventories greater than 90% | About 15 minutes (if interview needed) Materials = ∼$0.20 Admin. = ∼$4.20 Total = ∼$4.40 |
© 2007, Glascoe FP. PEDS: Developmental Milestones Professionals Manual. Nashville, Tennessee: Ellsworth & Vandermeer Press, Ltd. Permission is given to reproduce this table.
The first column in Table 3 provides publication information and the cost of purchasing a specimen set. The “Description” column provides information on alternative ways, if available, to administer measures (eg, waiting rooms). The “Accuracy” column shows the percentage of patients with and without problems identified correctly. The “Time Frame/Costs” column shows the costs of materials per visit along with the costs of professional time (using an average salary of $50 per hour) needed to administer and interpret each measure. Time/cost estimates do not include expenses associated with referring. For parent report tools, administration time reflects not only scoring of test results, but also the relationship between each test's reading level and the percentage of parents with less than a high school education (who may or may not be able to complete measures in waiting rooms due to literacy problems and will need interview administrations).
Even when screens are deployed, it is nevertheless helpful to complement these brief measures with clinical observation. The brevity of screens useful for primary care means that some skills may not be captured. For example, at any given age range, a brief screen may not present articulation items, measure ability to repeat a story, describe daily events, ask questions, or engage in conversation, etc. The value in routinely administering validated, accurate screening tools, however, is essential to improving currently problematic and extremely low rates of early detection on the part of primary healthcare providers.
Table 4 describes some major language developmental milestones in the prelinguistic (birth to 1 year) and linguistic period (1 year and beyond). [37 , 38] It is important to note that there are wide variations in the speed (and style) with which typically developing children acquire language skills.
Average Age and Range of Ages for Achievement for Important Language Developmental Milestones * [37 , 38]
| Prelinguistic Period (birth – 1 year) | Language Precursors |
|---|---|
| 2–4 months | |
| 6–7 months | |
| 9–10 months | |
| 12–14 months | |
| 15–24 months (average = 18 months) | |
| 18–24 months | |
| 18–27 months | |
| 27–36 months | |
| 30–48 months |
Providers are reminded that these indicators are an aid to early detection but do not substitute for quality measurement. See Table 3 for a list of screening measures with proven accuracy.
Screening for Other Potential Contributors to Speech-Language Deficits
Another critical avenue for exploration into possible contributors to speech-language deficits is psychosocial risk. Parents who are depressed and/or have housing or food instability have children more likely to have language problems, perhaps because parents lack the energy and freedom from preoccupations to engage in the kinds of language-mediated social interactions known to support optimal child language development. Some parents are not aware of positive parenting practices that promote development, especially language skills (eg, talking with and reading to their child, creating opportunities for sustained dialogue, responding contingently to a child's initiations). Detecting and intervening when psychosocial risk factors, including abuse and neglect, are present has the potential to prevent language problems from developing. Screens for psychosocial risk factors including depression and parent-child interactions are widely available and include the Family Psychosocial Screen and the Brigance Parent-Child Interactions Scale . Both are included in PEDS: Developmental Milestones [39] as supplementary measures helpful for surveillance and offer evidence-based compliance with recommendations in early detection from the American Academy of Pediatrics. [40] , Many other screens, such as the Ages and Stages Questionnaire , include a background information questionnaire that captures common psychosocial risk factors. [41]
Screening Older Children
With school-age children, obtaining and reviewing group achievement test scores can help reveal undiagnosed language deficits. Such children typically have weaknesses in general information (eg, science, social studies knowledge), problems with reading comprehension, and sometimes also problems with math concepts. Table 3 also includes screens suitable for primary care professionals working with children aged 8 years and older.
For both preschoolers and school-age children, broad-band screens (or review of group achievement test results) should be deployed first and serve as a guide to the selection of narrow-band instruments. For example, attentional deficits can be due to a range of conditions such as language impairment, learning disabilities, and mental health problems such as depression. The optimal approach is to administer a broad developmental or academic screen along with a measure such as the Pediatric Symptom Checklist (which discriminates mental health from attentional difficulties). Only afterward and as suggested by the results of broad-band measures should a narrowly focused tool such as the Vanderbilt ADHD Diagnostic Rating Scale be administered. Making sure that other conditions are treated first or at least concomitantly with ADHD is essential.
Billing and Coding for Screening
Primary care providers can use the – 25 modifier to their preventive service code (to indicate that stand-alone services were offered and then use 96110 times the number of screens administered, eg, 96110 X 2. For insurers not accepting units, the distinct procedural service of each screen is best represented with the – 59 modifier appended to each additional unit of 96110.
In 2005, the Centers for Medicare and Medicaid Services published a total relative value unit (RVU) of 0.36 for 96110, which amounts to a Medicare payment of $13.64. None of this can guarantee that a valid claim will be accepted, so the American Academy of Pediatrics is willing to help with denied claims via their Coding Hotline: 800-433-9016, x4022, or at .gro.paa@eniltohgnidocpaa RVUs do not cover physician time, so making use of office staff and parent-report tools is essential.
Referrals and Other Interventions
Once suspicion exists that a child may have a speech-language impairment, referral to early intervention or to the public schools (depending on age) is the first step. These programs offer intervention by speech-language pathologists. If sufficient quantity is not available, referrals can also be made to private therapy services, which may be covered by the patients' insurance. If there appear to be underlying medical conditions, assessment by other disciplines, such as developmental-behavioral or neurodevelopmental pediatrics, is important.
For families with psychosocial risk factors, developmental promotion is essential as is careful monitoring of progress. If brief advice and information handouts are not effective and particularly if children have delays not sufficiently great as to qualify for services, then parent training, quality day care, Head Start, after-school tutoring, and private speech-language therapy should be recommended. Table 5 shows a list of professional development and referral resources. Table 6 provides a list of resources and information for parents.
Professional Development and Referral Resources
| Links to State, regional, and local early intervention and testing services provided without charge to families whose children have known or suspected disabilities through the Individuals with Disabilities Act (IDEA) | |
| Provides help finding Head Start programs | |
| , | Provides assistance locating quality preschool and day care programs |
| Supplies information about parent training classes | |
| Official Web site of The American Academy of Pediatrics' Section on Developmental and Behavioral Pediatrics. The site offers tutorials in early detection and information on the management of children with a range of conditions. | |
| Provides training slide shows on early detection and offers an early detection discussion list focused on primary care | |
Resources and Information for Parents
| ASHA Websites | Content |
|---|---|
| Typical speech and language development | |
| What is language? What is speech? | |
| How does your child hear and talk? | |
| Communication Development: Kindergarten-5th grade | |
| Reading and writing (literacy) | |
| Social language use (pragmatics) | |
| Learning more than 1 language | |
| Late blooming or language problem? | |
| Apel K, Masterson J (2001). . American Speech and Language Association. | This book is designed to answer parents' questions about their child's speech and language development and describes speech and language development during infancy and the toddler and preschool years. |
Components of a Diagnostic Evaluation of Speech-Language Impairment and the Nature of Interventions
Although screening tools for speech-language often identify those children who have speech-language impairments, a screening is not a diagnostic evaluation and only suggests a child requires a more comprehensive assessment. There are several goals in a diagnostic assessment, including verifying that a speech-language impairment exists, describing the strengths and challenges of the child's speech and language, evaluating the severity of the problem, ascertaining the etiology, determining recommendations for a treatment plan, and providing a prognosis. [6] Assessment requires obtaining a sample of communication skills across settings through a number of procedures. It is critical to collect information not only from standardized, formal tools but also to gather more authentic, real-life information to facilitate meaningful and accurate decisions. Typically, case history information, parent interviews, checklists from other providers, systematic observation, hearing screening, and examination of the speech mechanism is included. [6] Formal norm-referenced tests are used to assess articulation, phonology, grammatical understanding and production, and pragmatic language use. The collection of data from the authentic assessment tools and the formal measures provide a comprehensive picture of the speech-language needs of a young child with a communication impairment.
All of the following are true in the assessment of a young child with speech-language impairments except :
- ○ Obtaining information from multiple sources across settings is necessary to specify communication strengths and challenges
- ○ Speech-language pathologists (SLPs) make diagnoses of specific speech-language impairment, identify probable causes, determine severity, describe the likely prognosis, and provide recommendations
- ○ Clinical judgment is most appropriate for determining the severity of a child's speech-language impairment
- ○ During assessment, speech, language, hearing, and processing abilities should be probed
Answer: Clinical judgment is most appropriate for determining the severity of a child's speech-language impairment. Objective criteria are important to ensure consistency in the assessment of severity.
To determine the prognosis for a young child with a speech-language impairment, which of the following is true?
- ○ A clinician should avoid providing prognostic information, as questions like “Will my son outgrow his speech-language impairment?” cannot be answered
- ○ Trial therapy during an assessment period is an appropriate strategy to inform prognosis
- ○ Families and clinicians have little difficulty making decisions about whether or not a young child with early expressive language delay will benefit from therapy
- ○ Single evaluation measures can be used to determine the severity of a young child's speech-language impairment and the prognosis for successful outcomes
Answer: Trial therapy during an assessment period is an appropriate strategy to inform prognosis. Clinicians often probe a child's response to intervention strategies to determine responsiveness to treatment and to inform the development of the treatment plan.
Intervention Approaches and Outcomes
The complexity of impairments in speech and language requires a variety of intervention approaches that can address deficits in language form (syntax, phonology, morphology), language content (semantics), and language use (pragmatics) as well as speech and voice production. Further, intervention for young children may involve not just the speech-language pathologist but also care providers and peers.
The ultimate goal of intervention is to increase a child's success in using language to communicate his or her intent, respond to the intent of others, and participate in reciprocal interactions. The speech and language targets vary for each child depending on the context and aspects of communication affected. Targets may or may not follow a strict developmental approach. Sometimes a more functional approach is appropriate, supporting communication at the point of frustration and breakdown. [6] Intervention targets should consider the family's desired outcomes for their child's communication. Targets should be developmentally appropriate and meaningful to the child.
Several teaching methods are used to support the speech and language of children. Modeling is a typical intervention strategy that provides focused stimulation on the speech or language targets selected for an individual child. Cueing is another frequently used technique that includes direct and indirect verbal cues (eg, asking a child to imitate a sound, word, or utterance) or nonverbal cues (eg, giving a child a jar with a desired item that can't be opened without help). In addition, responding to a child's communication efforts through reinforcement or corrective feedback (eg, “Remember to say the ending sound /t/ so we know you mean the word ‘boat’”) is frequently used to facilitate effective communication. [6]
Case Studies
Bobby [pseudonym] is a 7-year-old boy whom you have seen in your office for a number of years. He comes to you today for his annual check-up. Bobby is enrolled in the second grade. His mother is concerned because Bobby's teachers have noted difficulties in his ability to learn to read. Specifically, Bobby's teachers say that he has difficulties with word recognition and reading comprehension. Bobby's mother indicates that this is consistent with her own observations that he seems to have trouble with understanding what is being said (eg, directions, questions) and storytelling. Moreover, she suspects that Bobby's vocabulary is less well developed compared with his peers. She also describes frequent errors in how he formulates sentences such as omitting possessives (eg, “Sam dog” instead of “Sam's dog”) and verbs (eg, “He cooking” instead of “He is cooking”) that she fears are atypical. Bobby's nonverbal IQ is in the typical range.
The difficulties described above are most consistent with a possible diagnosis of:
- ○ Autism spectrum disorder
- ○ Intellectual disability
- ○ Specific language impairment
- ○ Language delay
Answer: Specific language impairment.
Darius [pseudonym] is a 5-year-old African American boy whom you are meeting today for the first time. He and his mother have recently moved to your area and she has brought him to you because he seems to be developing a nasty cough. When talking with Darius, you notice that he is extremely difficult to understand. Darius is a speaker of African American English; however, even with young speakers of this dialect, you have never had such difficulty understanding and communicating effectively. You learn that he and his parents have just moved from an impoverished community in South Carolina where he attended an age-appropriate class in a school in which approximately 85% of his classmates were black, to a school district in your area that almost entirely comprises white administrators, staff, and students. His mother further reports that Darius's new teachers have expressed concerns about his language. They say he is hard to understand, has a limited vocabulary, cannot master letter-sound correspondences, and has trouble listening to and understanding others.
Which of the following additional patient characteristics obtained from the mother would increase your suspicion of a diagnosis of speech and language impairment? (Select all that apply.)
- ▪ Darius's mother reports that he has always talked differently compared with his parents, siblings, and peers
- ▪ Darius's scores on a test of articulation of standard English are in the 10th percentile
- ▪ Darius becomes frustrated when you ask him to repeat himself
- ▪ Even though they are consistent with the sound structure of African American English, errors in Darius's spelling are quite common (eg, he writes "nes" instead of “nest”)
Answer: Darius's mother reports that he has always talked differently compared with his parents, siblings, and peers.
Which of the following additional patient or parent characteristics would increase your suspicion that Darius is exhibiting a language difference as opposed to a speech and language impairment? (Select all that apply.)
- ▪ Not only do you find Darius difficult to understand, but his mother is equally difficult to understand; both seem to be using a variation of African American English dialect that, although not commonly heard in your area, is characteristic of their native community
- ▪ Darius's scores on a test of vocabulary standardized on a cross-section of North American native English speakers are in the 35th percentile
- ▪ Darius's mother has no trouble understanding him
- ▪ Darius's mother does not share these concerns and considers him competent in all aspects of his language development
Answer: Not only do you find Darius difficult to understand, but his mother is equally difficult to understand; both seem to be using a variation of African American English dialect that, although not commonly heard in your area, is characteristic of their native community. Darius's mother does not share these concerns and considers him competent in all aspects of his language development.
You have been Sam's [pseudonym] primary care physician since he was born. He is now 18 months old and comes to you for his annual flu shot. During this visit, his mother expresses concerns about his speech and language development. More specifically, she reports he is “not talking like other kids his age” and uses repeated vocalizations (eg, “eh eh eh eh” while pointing) to communicate. Very recently, Sam has begun to use some words which are often paired with a gesture (eg, “Daddy” while pointing or “up” while raising hands to be picked up). You notice during your visit that Sam is a social and attentive child. He looks at other people and follows their eye gaze to distal objects. He also seems to understand the speech that his mother directs to him and he can easily carry out 2-step commands (eg, “Pick up the cup and sit next to me, please”). Sam's mother is aware of no immediate or extended family members who have ever had a speech or language impairment. Sam has no history of ear infection, and a recent hearing screen indicated hearing in the normal range.
- ▪ Limited imitation
- ▪ Limited pretend play
- ▪ Limited facial expressiveness
- ▪ Excessive use of nonverbal communicative gestures (eg, reaching, pointing, looking)
Answer: Limited imitation. Limited pretend play.
What should the mother expect with time if her child does not have a speech and language impairment but is rather a late-talker? (Select all that apply.)
- ▪ The child will begin to engage in unusual repetitive behaviors
- ▪ The child will steadily albeit slowly add new words and begin to combine them into 2-word utterances
- ▪ Any new words that the child utters are likely to be distorted and difficult to understand
- ▪ The child may develop aggressive behaviors to cope with his inability to communicate effectively
Answer: The child will steadily albeit slowly add new words and begin to combine them into 2-word utterances.
Theresa [pseudonym] is a 3-year-old female whom you have seen in your office regularly since her birth. She comes to you today for her annual check-up. During her visit, you observe that Theresa is precocious in her language development. Indeed, her mother reports that she has always been a “great talker” and that she began to speak in well-formed utterances at age 18 months. During this visit, you notice a number of disfluencies in Theresa's speech. At one point, she repeats a word 3 times before getting the rest of the sentence out (ie, “I see… see… see a book with a clown”). Theresa's mother states that these kinds of disfluencies began about 1 month ago and, although she characterizes them as relatively infrequent, she has questions about whether this kind of speech is normal.
Which of the following additional patient characteristics obtained from your observation of Theresa would increase your suspicion of a diagnosis of a fluency disorder? (Select all that apply.)
- ▪ Theresa seems aware of and perturbed by her disfluencies
- ▪ Theresa sometimes jerks her head when hesitating to utter her next word
- ▪ Approximately 20% of Theresa's words appear to constitute disfluencies
- ▪ Theresa produces multi-unit syllable repetitions (eg, “t-t-t-time”)
- ▪ All of the above
Answer: All of the above.
Reader Comments on: Speech-Language Impairment: How to Identify the Most Common and Least Diagnosed Disability of Childhood See reader comments on this article and provide your own.
Readers are encouraged to respond to the author at [email protected] or to George Lundberg, MD, Editor in Chief of The Medscape Journal of Medicine , for the editor's eyes only or for possible publication as an actual Letter in the Medscape Journal via email: ten.epacsdem@grebdnulg
Contributor Information
Patricia A. Prelock, Department of Communication Sciences, University of Vermont, Burlington, Vermont.
Tiffany Hutchins, Department of Communication Sciences, University of Vermont, Burlington, Vermont.
Frances P. Glascoe, Department of Pediatrics, Vanderbilt University, Nashville, Tennessee.
Look up a word, learn it forever.
Speech defect.
Other forms: speech defects
- noun a disorder of oral speech synonyms: defect of speech , speech disorder see more see less types: show 10 types... hide 10 types... anarthria partial or total loss of articulate speech resulting from lesions of the central nervous system aphonia , voicelessness a disorder of the vocal organs that results in the loss of voice cataphasia a speech disorder in which the same word is repeated several times in succession dysarthria impaired articulatory ability resulting from defects in the peripheral motor nerves or in the speech musculature dyslogia impaired ability to express ideas verbally; usually resulting from difficulties of reasoning (as in feeblemindedness or certain psychoses) dysphonia speech disorder attributable to a disorder of phonation lallation defective articulation of the `l' phoneme or the phoneme `r' is pronounced as `l' lambdacism speech defect involving excessive use or unusual pronunciation of the phoneme `l' lisp a speech defect that involves pronouncing `s' like voiceless `th' and `z' like voiced `th' stammer , stutter a speech disorder involving hesitations and involuntary repetitions of certain sounds type of: disorder , upset a physical condition in which there is a disturbance of normal functioning
Sign up now (it’s free!)
Whether you’re a teacher or a learner, vocabulary.com can put you or your class on the path to systematic vocabulary improvement..
Psychology Discussion
Speech defects in children: meaning, causes and forms.
ADVERTISEMENTS:
In this article we will discuss about ‘Speech Defects in Children’. After reading this article you will learn about: 1. Meaning of Speech Defects 2. Causes of Speech Defects 3. Forms.
Meaning of Speech Defects:
Speech defects and disorders develop more prominently when the baby is just learning to speak. Speech disorders, even baby talks are serious handicaps to social adjustment of the child. Particularly when he grows up, mixes, and communicates with people, he feels inferior, anxious and withdraws from the group, society and friends.
He becomes imaginative and lives in day dream, suffers from frustration. All these lead to frustration and maladjustment in every child who has speech defects. Though he is talented, he is scared to talk to people in groups, give speeches in meetings and communicates in social gatherings.
Further a child having speech defects deviates significantly from the general standard that other children of his age show and he commits more errors. Commonly defects in speech means defects in pronounciation. But in a wider sense, it may refer to any type of speech that is incorrect.
Speech defects can be divided under three sub types:
(a) Defects in word meaning
(b) Defects in pronounciation
(c) Defects in sentence structure.
Speech disorders refer to serious defect in pronounciation in that they are caused by some defect or malformation of vocal organs or by persistent emotional tensions. Speech disorders cannot be rectified or cured by learning correct pronounciation. The real cause of speech disorder must be diagnosed and removed.
Causes of Speech Defects :
1. Malformation of speech organs, defects due to tongue tied conditions, deformed teeth or lips or jaw may be the physical causes of speech disorders.
2. Slow maturation, inadequate learning, poor environmental conditions, etc. may lead to emotional tensions or other forms of emotional maladjustments which may produce speech defects or difficulty in articulation.
3. Poor and faulty child rearing practices, one or both the parents having neurotic tendencies, poor parent child relationship, lack of congenial and warm relationship between parents, aggressive, dominant, possessive and demanding mother with high aspirations for the child, may lead to speech disorder in the child.
4. Lack of proper adjustment with family, friends and peers because of the above factors may produce speech disorders.
5. Conflict and tension in day to day life, threatening and severe punishment by parents and teachers may also produce speech disorders in children.
6. Dependency, destructiveness and aggressiveness, tempertantrum timidity and allied psychological problems are related to speech disorder.
Thus, it is clear that speech disorders are largely due to adjustmental problems and emotional instabilities because of faulty environmental feed backs.
Forms of Speech Defects and Disorder:
Some of the Common forms of speech defects and disorders are discussed below:
(i) Difficulty in Pronounciation :
Incorrect and unintelligible speech habits may be developed due to inadequate environment stimulations. Childish errors may be caused due to ommission of letters by the child and no one to correct it. Inability to pronounce a word correctly may also be due to malnutrition and physical weakness.
If the small child is exposed to incorrect grammar in the home by family members or baby seaters or neighbours, he may continue to use incorrectly the pronoun forms “I” and ‘me’ or “who” and “whom”.
Baby talk by parents either to get pleasure or because they think the child cannot understand their language leads to faulty pronounciation like when a mother or family member speaks ‘Babbal’ for chappal (shoe) ‘Pai’ for Pani (water) ‘Taibu’ for Khaibu (eating) etc.
The child is encouraged to speak like that and continue it till adulthood. Experience shows that the child is capable enough to say chappal, pani and khaibu or the correct pronounciations if encouraged to say so. Hence it is the fault of the parents and family members and adults for which the child develops wrong pronounciations.
Similarly when a woman in charge of the child constantly speaks “Suibu instead of Soibu (sleep) or Daibi instead of Basibi (sit) the child learns to pronounce the word in the same way. These faulty speech habits developed during preschool years can be rectified by consistent and constant correction in the early stage.
Speech disorders usually develop during preschool year though they may develop at any time during one’s life. During preschool years, the child’s mind is very malleable and he is just learning to speak. Speech habits are yet to be formed.
So what be hears he imitates. Once a set of pronounciations have been clearly and distinctly developed, it is difficult to give it up. At a stage when he is learning to speak, any serious emotional trouble is most likely to disturb this speech habits and pronounciations. Most of the speech disorders therefore develop during the preschool years.
Thus speech errors occur primarily due to faulty learning, baby talk by parents and others. If not corrected in due time they may persist and cause trouble in adjustment during later life. According to Mccarthy (1960) mostly the errors in pronounciation excepting those due to organic causes, occurs due to the neuroticism of parents, unhappy parent-child, father-mother relationship.
(ii) Lisping :
It is the most common defect in the preschool children. The lisper appears to find it difficult to utter certain letters correctly, particularly the letter’s. He pronounces ‘this’ as thilh or simple as thimple.
This disorder may have its origin in baby talks or due to the deformity of teeth, lip or jaw gaps caused by falling of baby tooth may cause lisping. During the beginning stage it may be cured by training. Otherwise the child requires the help of speech specialist; speech therapist for acquiring new and correct speech pattern.
If it is not due to physical defect the child can gradually be trained to overcome it. He can learn to give up baby talks and infantile speech. If adults instead of diswading the child enjoy it he is encouraged and more motivated to continue the same. So adults should be very careful about infantile speech and discourage their children from developing it.
Thus, in lisping due to some reasons stated above, children substitute ‘the’ for’s’ Z, w for ‘r’ etc. Lisping may also disappear or decrease after permanent teeth appears. If still the problem persists, the speech specialist should be consulted.
(iii) Slurring :
When the child is not able to pronounce any word clearly it is called slurring. Thus, slurring results from running words together, sometimes in the form of mumbling jorgon and indistinctiveness, slurring usually occurs in the preschool age. Slurring may occur due to several reasons.
Due to inactivity of lips, paralysis of vocal cords, fear, excitement, stage frightness, fear for strangers, the speech of the child becomes indistinct. A shy, introvert, withdrawal type of child may feel very nervous and tongue tied in the presence of strangers. He might be very interested to talk, he might be knowing the correct reply but he finds difficult to say whatever he wants to say, so he speaks rapidly.
Rapidity of speech interferes with clear and distinct pronunciation as he cannot give adequate time and space to all the letters. A normal child may slur when emotionally upset, excited or anxious. Because when the tries to rush through the letters/words, they loose their clarity.
Unless it is due to paralysis of the vocal cord or any other physical reason, slurring can be managed to be corrected by asking the child to open his mouth and give emphasis to each word he utters, to speak slowly but distinctly. It the child opens his mouth while speaking so that sounds can came out, slurring can be rectified by means so speech therapy and continuous practice to speak slowly, but distinctly.
Unless there is any organic difficulty, slurring can also be removed if the children learn to control the slurring tendency by perseverance and determination. Parents should take extra care to speak clearly, slowly and fluently and they should also advise the child to imitate them.
(iv) Stuttering and Stammering :
Among all the speech disorders stuttering and stammering are most serious type. Stuttering is a type of hesitant repetitive speech, defects in articulation caused by emotional problems anxiety, frustration, fear for authority, insecurity, fear for failure, over protection, during early childhood. Stuttering and stammering occur because of failure of coordination of speech muscles, spasms of throat muscles and disphragme.
In stammering there is a check in speech, then no speech, then sudden speech and then again no speech. It creates the inability to produce sound. Between age 22 to 3 years stuttering may occur due to talk of coordination between thought and language. He has a lot to speak, but has not the capacity for the same. So he tries to speak as fast as possible and suffers from stuttering.
While stuttering the child is under serious mental and emotional strain. Parents should not give over attention to it and consider it a serious problem so that it would disappear automatically.
But if parents make it an issue and try to correct him when he stutters or rebuke and ridicule him it may aggravate stuttering. By suitable social and home adjustment stuttering also decreases. Sometimes stuttering is accompanied by a dead locking of speech and temporary inability to produce sound.
Stammering is also a type of stuttering. When the opening letter of a word is prolonged it refers to stammering like eeee—error-c-c-c-cat. Stammering occurs when a child cannot get a word out. There appears difficulty in producing any spcech sound.
The stammerer gasps, hesitates, gasps again and then mouths the word with spasmodic movements and facial grimaces efforts to articulate. Some children stammer only with certain consonants and not others. Stuttering and stammering may differ from place to place in the same person and also from person to person.
In one situation he may stutter & stammer while in another situation he may not. He may stammer while trying to utter some and not in others.
However, for the cure of stuttering and stammering the underlying emotional causes are to be brought to the sources and released, although stammering does not cause any handicap for use of intellectual capacities and many stammerers have reached high position in life. Studies show that primitive uncivilized people do not stutter.
Some say the causes are hereditary and run in families. Stammering and stuttering may also occur because of defective speech muscles. In a study, West and others examined 204 stammers and 204 normal children (without stammering) and found lat this disorder may be due to hereditary factors. Johnson opined that children start stammering when they are called stammerer.
Moncur found that if parents overprotect their children, criticise them, take excessive care and have high aspirations about their children, put a lot of pressure on them to excel in every sphere from early childhood, they stammer.
Psychoanalysts opine that fixation of the libidinal energy in the oral stage of psychosexual development lead to stammering and stuttering. Davis was of view that when a small child is not able to integrate his speech properly, he starts stuttering. When he becomes habituated in speaking it disappears. Hence the stammer should speak as much as possible.
Sometimes when the child becomes conscious while speaking, becomes highly excited after observing his own behaviour and tries to catch attention of others, he starts stammering. Most people say that stammering is a learned behaviour psychological in origin resulting from environmental pressures.
Nervousness, emotional instability, anxiety, confusion, fearfulness, over-protection, anxiety, are common causes. Perfectionistic, dominating, over anxious parents pressure on the child to learn two languages at a time leading to stuttering. Besides other techniques and precautions mentioned above, stutters and stammers should be treated by specialists and speech therapists for all the best.
(v) Cluttering :
Cluttering is otherwise known as rapid, jumpled, mistaken and confused type speech. Cluttering is caused due to delayed motor control and speech developments. Children whose speech development is delayed they usually show this speech disorder. Cluttering is more or less similar to stuttering.
It creates more errors in speech. Speech errors made by normal people are exaggerated by the clutterers in their speech. The speech of clutterers can be improved by concentration, attention and by becoming cautious and aware before speaking. Sufficient love and understanding, warm relationship with the child can prevent their speech disorders and defects.
Almost all speech defects and disorders are due to emotional disturbances excepting those having I physical causes. Proper handling of the child by parents and due attention during his language development period is extremely urgent to avoid future complication in language development.
Related Articles:
- Writing and Reading Disorders Seen among Children
- 4 Main Types of Exceptional Children | Psychology
- Communication: Meaning, Components and Forms
- Emotions in Children: Meaning, Effects and Hints | Term Paper | Psychology
What does 'From the river to the sea, Palestine will be free' mean?
Here is what palestinian and jewish groups have to say about the slogan.

Social Sharing
"From the river to the sea, Palestine will be free" has been a popular refrain in pro-Palestinian protests and online discussion across North America in the wake of the Israel-Hamas war.
It has also been the subject of criticism and, in some cases, institutional backlash.
Hamilton MPP Sarah Jama was recently criticized for using the slogan at a pro-Palestinian rally, two weeks after she was kicked out of the NDP caucus after calling for a ceasefire , characterizing the Israeli occupation as "apartheid" and taking what the party called "unilateral actions" that "contributed to unsafe work environments for staff."
In the U.S., Democratic Rep. Rashida Tlaib — the only Palestinian member of Congress — was censured for using the phrase in a video on social media, while in the U.K., senior Labour MP Andy McDonald was suspended from the party after echoing a version of the slogan at a rally.
In Calgary, a protester was arrested after using the slogan, although charges against him have since been stayed.

Israel advocacy groups in Canada and the U.S., such as the Anti-Defamation League, the Centre for Israel and Jewish Affairs and B'nai Brith, say the slogan is an antisemitic call for the ethnic cleansing of Jewish people.
"When someone says from the river to the sea, Palestine will be free, I question, 'Where do you see the Jews going?'" said Yair Szlak, president and CEO of Montreal-based Federation CJA. "That is hate speech, right, because it is into the sea that they seek to send the Jews."
Meanwhile, Palestinians and some Jewish academics say the slogan is not inherently threatening or hateful.
Yousef Munayyer, head of the Palestine-Israel program at the Arab Center Washington D.C., has written extensively about the meaning of the slogan before and since Hamas's attacks on Oct. 7, which led to Israel's current bombardment of the Gaza Strip.
Munayyer says today, the phrase is used to reference the lack of freedoms Palestinians have in the territory between the Jordan River and the Mediterranean Sea, which includes the state of Israel as well as the Gaza Strip and the occupied territories of the West Bank and East Jerusalem.
"That's what has to change. That doesn't mean that there should be any violence against Israelis," Munayyer said.
- Questions raised after arrest of Calgary protester on hate-motivated disturbance charge
- Charges stayed against Calgary protester accused of causing hate-motivated disturbance
Hamas's Oct. 7 assault, which killed an estimated 1,200 people in Israel, according to Israeli authorities, and included the kidnapping of an additional 240 people, has been followed by a month-long Israeli siege and ground offensive that has killed more than 12,000 Palestinians, according to health officials in Gaza, which is controlled by Hamas.
A call for Palestinian freedom
Dov Waxman, a professor and director of the Nazarian Center for Israel Studies at the University of California, Los Angeles, does not perceive the slogan to be "inherently threatening" and believes that is not what many Palestinians and their supporters mean when repeating it.
"It's an expression of Palestinian nationalism and it's an expression of a demand for Palestinian freedom or self-determination," said Waxman. "I think Palestinian self-determination need not come at the expense of Jewish self-determination. Nor do I think Palestinian freedom has to be considered a threat to Jewish rights."
According to Waxman, many Jewish people hear the chant as a call for "the violent destruction of Israel," which is how Hamas and its supporters use the phrase.
Waxman said that "From the river to the sea, Palestine will be free" originated in the 1960s as an expression of Palestinian nationalism and has been co-opted by various groups over time, including Hamas when the group formed in 1987.
He noted that Israeli Prime Minister Benjamin Netanyahu and his Likud Party believe that "Jews had the rightful claim to this entire territory."
"They still would like to have Jewish sovereignty, essentially, from the river to the sea," Waxman said.
Some Palestinians say the slogan refers to a single state within which Palestinians and Israelis could live together. Some Jewish groups and Palestinian extremists see the slogan as a call to remove Israelis from the region in order to form a single Palestinian state.
- Ontario NDP kicks Hamilton MPP Sarah Jama from caucus after controversial Gaza comments
- Rashida Tlaib, only Palestinian-American member of Congress, censured for controversial war statements
Waxman says the idea of a state in which Palestinians and Israelis live harmoniously is "unrealistic" but not "inherently problematic."
The alternative is a two-state solution, which would create separate states of Israel and Palestine, an idea that originated in 1947. U.S. President Joe Biden has been touting it in recent weeks, and in a statement on Monday evening, so did Canadian Foreign Minister Mélanie Joly.
"Canada continues to recognize the Palestinian right to self-determination and remains committed to the goal of a comprehensive, just and lasting peace in the region, of a two-state solution, including the creation of an independent, viable Palestinian state living side by side in peace and security with Israel," reads the statement from Joly's office .
'75 years of occupation'
Rama Al Malah, an organizer with the Palestinian Youth Movement in Canada, said the chant has been repeated over the past six weeks as a call for Palestinian "liberation from 75 years of occupation."
"My great-grandmother on my mom's side was kicked out of Haifa in 1948," Al Malah said, referring to the Nakba, or catastrophe, in which hundreds of thousands of Palestinians were driven from their homes or fled during the war over the creation of Israel .
Al Malah says the chant also calls for "the return of refugees who have been kicked out of their homes from 1948 till now."
WATCH | What 'From the river to the sea, Palestine will be free' means to different people:

What ‘from the river to the sea’ chant means to different people
According to the United Nations Relief and Works Agency for Palestine Refugees, there are currently 5.9 million Palestinian refugees, a third of whom live in refugee camps across Gaza, West Bank, Jordan, Syria and Lebanon. Various human rights groups and the United Nations have documented that Palestinians in the Gaza Strip and the West Bank "continue to be deprived of their freedom, dignity and rights by Israel."
Al Malah said the slogan is a response to this situation and doesn't call "for the killing of Jewish people at all. It's basically a way for us to say that we want freedom," she said.
The lack of freedoms for Palestinians is well documented by human rights groups, said Sheryl Nestel, a retired University of Toronto professor and member of advocacy group Independent Jewish Voices Canada.
"Palestinians both under occupation and living inside Israel face enormous discrimination, enormous differences in the rights that they enjoy, and the infrastructure that they live under," said Nestel, who lived in Israel for 15 years, where she said she advocated against illegal Jewish settlements in the West Bank.
- Canada calls on Israel to reverse thousands of West Bank settlement approvals
- Analysis A generation gap in attitudes could be undermining support for Israel in the West
For Nestel, criticism of the slogan is tantamount to anti-Palestinian racism.
"One of the problems with the criticism of the slogan is that it imputes genocidal intent to Palestinians, and there's no evidence that the majority of Palestinians want to eliminate Jews from historical Palestine," Nestel said.
Different characterizations of the slogan
For Munayyer, the backlash against the use of the chant "From the river to the sea, Palestine will be free" is comparable to those who objected to the slogan "Black lives matter" during the protests sparked by the police killing of George Floyd in 2020.
"People were saying Black Lives Matter, not because they didn't think white lives mattered, but because they were objecting to a set of policies and practices that [meant] for many Black people that their lives didn't matter as much," he said. "There were some people who thought that it was racist against white people to say that Black lives matter."
Waxman said that "From the river to the sea…" has different meanings depending on the context in which it is used.
"If it's invoked by supporters of Hamas, for example, [the chant] has a very different meaning, and I would understand that as much more threatening than if it was advocated by, say, Rashida Tlaib," Waxman said.
Waxman says the vision of a single state in which Israeli and Palestinian people live with equal rights is "utopian," but "I don't think we should necessarily see [the slogan] as a call for ethnic cleansing or genocide, which is how many Jews do hear it."
- Amid on-campus tensions brought on by Israel-Hamas war, experts worry about free expression
According to Waxman, the backlash against the slogan is a result of an "effort to essentially insist that any form of anti-Zionism, any opposition to Israel's continued existence as a Jewish state, is inherently antisemitic, so even when that statement is now [said] by a college student who might favour just granting of equal rights [to] Palestinians in the West Bank, in Gaza, there are those who want to insist that that is inherently antisemitic."

For Munayyer, Islamophobia is also a factor.
"There is a deep history of racism and Islamophobia in the West towards Palestinians and Arabs and Muslims more broadly, which always throws upon them the worst of intentions and interpretations of their words," Munayyer said.
"The way that they are increasingly responding to protests against this is by trying to criminalize [the slogan] and shut it down."
Clarifications
- The deck of the story has been updated to reflect the points of view cited in the article. Nov 21, 2023 3:47 PM ET
Corrections
- A previous version of this article stated that charges against a Calgary protester had been dropped. In fact, they have been stayed. The previous version also said Ontario MPP Sarah Jama was kicked out of the NDP caucus after using the phrase "From the river to the sea, Palestine will be free." In fact, she was criticized for using the phrase, but her dismissal from caucus was linked to a statement that characterized the Israeli occupation as "apartheid" and to what the party called "unilateral actions" that "contributed to unsafe work environments for staff." Nov 21, 2023 10:59 AM ET
ABOUT THE AUTHOR

Senior writer
Brishti Basu is a senior writer with CBCNews.ca. Before joining CBC, her in-depth coverage of health care, housing and sexual violence at Capital Daily was nominated for several national and provincial journalism awards. She was deputy editor at New Canadian Media and has been a freelance journalist for numerous publications including National Geographic, VICE, The Tyee, and The Narwhal. Send story tips to [email protected].
With files from CBC's Thomas Daigle
- Share full article
Advertisement
Supported by
U.C. Berkeley’s Leader, a Free Speech Champion, Has Advice for Today’s Students: Tone It Down
“Just because you have the right to say something doesn’t mean it’s right to say,” said Carol Christ, who is retiring as chancellor at the end of this month.

By Kurt Streeter
Reporting from the University of California, Berkeley.
Waves of boos, angry chants and the steady rhythm of feet pounding on metal seats were upending the graduation ceremony at the University of California, Berkeley.
“Viva, viva Palestina!” students sang out. “Hey, hey, ho, ho, Israel’s apartheid has got to go!”
It was the soundtrack of this year’s antiwar protest, voiced on the morning of May 11 by hundreds of cap-and-gowned graduates, loud enough to nearly drown out the ceremony’s official speakers — and force the event to halt.
One minute passed.
Two minutes.
It looked like Berkeley’s 2024 commencement was about to be canceled midstream.
Then, suddenly, surprisingly, the ceremony resumed.
Once it was over and most had left the school’s low-slung football stadium, Berkeley’s chancellor, Carol Christ, sat near the podium in a folding chair. She is silver-haired and soft-spoken, a soon-to-retire 80-year-old former English professor with an unusual background for the modern college president: Her views on free speech first crystallized during her years as a student protester in the turbulent 1960s.
When the demonstrators forced the pause, had she considered ending the event?
“Absolutely not,” Dr. Christ said. This is Berkeley, she said. “We were always going to power through. Protest is part of our core.”
Dr. Christ (her name rhymes with “wrist”) plans to retire at the end of June. The first woman appointed to the job, she leaves as the oldest chancellor in Berkeley history, and one of the oldest leaders of an elite college campus in America.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Election latest: Farage says poll shows Reform 'now the challengers to Labour'
The Liberal Democrats have kicked off a vital stage of the election campaign by launching their manifesto to "save the NHS". Reform UK haven't gone that far yet, but are seeking to explain their tax-cutting plans. Meanwhile, Rishi Sunak has insisted he's not considered resigning as PM.
Monday 10 June 2024 12:39, UK
- General Election 2024
Please use Chrome browser for a more accessible video player
Election news
- Reform UK outlining economic plans - watch live above
- Lib Dems launch manifesto to 'save the NHS'
- Davey pays tribute to carers | Will Lib Dems take UK back into EU?
- Reform outlines tax cut plan | Farage says UK at 'tipping point'
- PM insists he didn't consider quitting after D-Day fallout
- Douglas Ross to quit as Scottish Tory leader
- Live reporting by Tim Baker and Ollie Cooper
Expert analysis
- Sam Coates: Lib Dems falling victim to tonal whiplash
- Connor Gillies: Big moment for Scottish politics
- Rob Powell: Sunak struggles to change weather after bad two weeks
Election essentials
- Battle For No 10: PM and Starmer taking part in Sky News special
- Campaign Heritage: Memorable moments from elections gone by
- Trackers: Who's leading polls? | Is PM keeping promises?
- Follow Sky's politics podcasts: Electoral Dysfunction | Politics At Jack And Sam's
- Read more: Who is standing down? | Key seats to watch | How to register to vote | What counts as voter ID? | Check if your constituency is changing | Your essential guide to election lingo | Sky's election night plans
Sir Ed Davey, the leader of the Liberal Democrats, has launched the party's 114-page, "fully costed" manifesto.
We updated this post with the key pledges as they were announced:
- It is branded a "manifesto to save the NHS";
- Everyone will have a right to see a GP with seven days - or 24 hours if it's urgent;
- Improved access to dentists and pharmacists;
- Guaranteed cancer treatment within two months;
- New mental health hubs for young people, and mental health professional in all schools;
- There will be NHS-style free social care;
- A new higher minimum wage will be offered to care workers;
- Establishing a new Royal College of Care Workers;
- Restoring "proper" bereavement support for parents who lose a partner;
- A plan to stop raw sewage being dumped into rivers and onto beaches, and hold water companies to account;
- Policies to solve the cost of living crisis for "the long term";
- An emergency home energy upgrade scheme;
- Restoring community policing;
- "Fixing" the "broken relationship" with Europe;
- Ending first past the post and replacing it with proportional representation;
- Getting "big money out of politics" with a cap on donations to parties;
- Shifting power out of the centre to the communities they affect.
You can read the Lib Dem manifesto in full here .
Sky political correspondent Gurpreet Narwan asks the Reform leadership more about their policy to change how the Bank of England pays interest on the debt it holds.
As a reminder - this is the money, about £800bn worth, that the Bank has printed since 2008 to keep the UK economy healthy by lending it to the government.
In late 2022, it started to sell the debt off, but this process will take years to complete.
Nigel Farage and Richard Tice want to see an end to interest being paid on the figure, as they say it means billions is going from the taxpayer to high street banks through the Bank of England.
Mr Farage singles out Rishi Sunak for his acts as chancellor during COVID, in which the Bank lent £400bn of the money.
He says the then-chancellor should have locked in the interest rate at which the money was borrowed by the government. The base rate stood at 0.1% at the time, and is now above 5%.
He says it was "financial mismanagement on a gargantuan scale" and is costing tens of billions.
The pair say they want to see the Bank pay zero interest on the debts.
Nigel Farage has on stage been hyping up Reform's chances of doing well at next month's election.
"We may be just a bit closer to a tipping point than many realise," he claims.
He says by removing London and Scotland from a YouGov poll last week that had Reform at 17% , just two points behind the Tories, "you get a very interesting picture".
Reform was ahead of the Tories in the North East, the North West, Yorkshire and the Humber, the East Midlands, and the West Midlands.
The party's also ahead with male voters and Brexit voters.
"We're quite a long way behind" in London and Scotland, he admits, but in "significant parts of the country we are now the challengers to Labour".
Richard Tice, the Reform UK chairman, is giving a speech in London about his party's economic policy.
He says he wants to get more people into work, as it will reduce the burden on the exchequer.
People in the UK are "literally suffocating" because of tax, he says.
His party wants to raise the threshold for paying income tax to £20,000, up from which he says will cost £40bn.
Mr Tice claims it will be paid for by overhauling the Bank of England.
He specifically singles out the interest paid on the £800bn of debt held by the Bank following quantitative easing.
The interest payments on this debt have soared since the base rate went up as the Bank tries to return inflation to 2%.
'Great British tax cut'
It is money taken off the taxpayer and paid on "institutions" in the city, among others.
The money would be used for a "great British tax cut".
Mr Tice says he also wants to raise the VAT threshold for small businesses to £150,000 from £90,000.
Other pledges include abolishing IR35, or off-payroll working, saying we can't "tax our way out of a crisis".
Party leader Nigel Farage takes over, and says the government may have difficulties issuing gilts if the current system of borrowing continues.
The Liberal Democrats have wrapped up their manifesto launch event, and you can scroll back through the Politics Hub to read more on their announcements and leader Sir Ed Davey's answers to the media.
We'll have more reaction and analysis to the manifesto throughout the afternoon.
Shortly we'll have live coverage of a Reform UK event with party leader Nigel Farage, where he and predecessor Richard Tice will be outlining their economic policies.
Stay with us for updates.
Speaking to broadcasters at the Dog and Bacon pub in Horsham, West Sussex, Mr Sunak is asked if contemplated stepping aside.
It is the first time he has answered on-camera questions since Friday, when he apologised for leaving last week's D-Day commemorations at Normandy before they had finished.
He says: "No, of course not.
"I'm energised about the vision that we're putting forward for the country.
"This campaign is not even halfway through yet, and I'm finding an enormous amount of support for the policies that we're putting on the table."
He says lots of people are saying the election is a "foregone conclusion" - and have been saying so since he took over.
But the PM says he is "not going to stop going - I'm not going to stop fighting for people's votes".
Reacting to the outlining of the Liberal Democrats' election manifesto, our deputy political editor Sam Coates says the party seem confused.
"A party leader desperate, it seems, to show how serious he is about British politics says he's come up with a manifesto to save the health service, a series of tax rises and proposals that he insists are fully costed," Sam says.
"He (Sir Ed Davey) wants the Liberal Democrats to be taken seriously, but then in the next breath, he says: 'I'm off to go on a rollercoaster'."
A bit of tonal whiplash, to say the least.
The Lib Dem battle bus is heading to Thorpe Park this afternoon.
Sir Ed spent much of today asking the public to "take a chance" on a serious party in the Lib Dems, but much of his campaigning has been focused on social media stunts - and he opened his speech by joking he'd become "a meme".
"I think that kind of encapsulates a bit of where we are with the Liberal Democrats at the moment," Sam says.
Politico asks the Lib Dem leader about the fallout from the party's coalition government with the Tories.
Sir Ed - who was a minister at the time - says the party "fought the Conservatives every day, but we didn't win everything - and we paid a price for that".
He points to how he lost his parliamentary seat, and the three "bad" general election results the Lib Dems have endured since.
Sir Ed says that when he became leader he said people "needed to wake up and smell the coffee".
He said he instilled "iron discipline" in the party and people have "seen the disaster of the Conservatives".
Times Radio asks the Liberal Democrat leader how he will pay for specific policies in the manifesto.
They list ending the two-child benefit limit, doubling statutory maternity and paternity pay and paying compensation to Waspi women.
Sir Ed says the manifesto has been costed, and there is a policy costing document online that goes through the figures.
We'll be hearing more about that later from our economics and data editor Ed Conway .
Back to the politics, and Sir Ed says taxes will be put up on big banks, oil and gas companies, social media giants and the wealthiest people in the UK.
He adds that, in his view, some parties "are not really telling the truth about the funding of their policies".
The Lib Dems' costings document can be found here .
Sky deputy political editor Sam Coates asks Sir Ed Davey what success looks like to the Liberal Democrats.
He says that in the first instance, success is "lots of liberal MPs getting elected".
Sir Ed says he wants people to "take a chance on us" - and see the Lib Dems have "got great ideas, great candidates".
"And the more of us they vote for, the more we can get real change because we are the party offering change - whether it's on the political system or health and care".
He says his policy on health is "the most ambitious" of any party.
Sir Ed later tells GB News that in many seats, the Lib Dems are the only party who can beat the Tories.
Continuing to take questions from journalists, Sir Ed Davey is now asked about the Liberal Democrat's long-standing ambition of getting the UK to the "heart of Europe".
He's asked specifically on when he would want to see the UK back in Europe.
"We've made clear time and again that we are a pro-European party who believe that our country's interests are best served by working with other countries in mutual benefit.
"We believe in the long term."
"But we're being really clear that we're not going to pretend that's going to be easy," he adds, adding that the Tories damaging the UK's reputation so badly has made it harder.
"There are lots of things set out in the manifesto about how we could begin to rebuild that relationship... but it's going to take time."
Asked what he makes of the European elections across the weekend may mean for those plans, he says: "[People] want change and we want change, too, because we're unhappy."
You can follow the fallout from those polls, which led to Emmanuel Macron calling a snap election in France after major gains for the far right, in our dedicated live blog:
Be the first to get Breaking News
Install the Sky News app for free


IMAGES
VIDEO
COMMENTS
A speech-language pathologist (SLP) is a healthcare professional who specializes in speech and language disorders. An SLP will evaluate a person for groups of symptoms that indicate one type of ...
A speech impediment, or speech disorder, is a condition that makes it hard for you to communicate. There are many types of speech impediments, and anyone can develop one. In some cases, children are born with conditions that affect speech. Other times, people have conditions or injuries that affect speech. Speech therapy can help.
Speech disorders affect roughly 11.5% of the US population, and 5% of the primary school population. Speech is a complex process that requires precise timing, nerve and muscle control, and as a result is susceptible to impairments. A person who has a stroke, an accident or birth defect may have speech and language problems.
There are three general categories of speech impairment: Fluency disorder. This type can be described as continuity, smoothness, rate, and effort in speech production. Voice disorder. A voice ...
Definition. A speech disorder is a condition in which a person has problems creating or forming the speech sounds needed to communicate with others. This can make the child's speech difficult to understand. ... Laryngeal webs or clefts (a birth defect in which a thin layer of tissue is between the vocal cords) Noncancerous growths (polyps ...
However, some speech disorders persist. Approximately 5% of children aged three to 17 in the United States experience speech disorders. There are many different types of speech impediments, including: Disfluency. Articulation errors. Ankyloglossia. Dysarthria. Apraxia. This article explores the causes, symptoms, and treatment of the different ...
Common causes of childhood speech impediments include: Autism spectrum disorder: A neurodevelopmental disorder that affects social and interactive development. Cerebral palsy: A congenital (from birth) disorder that affects learning and control of physical movement. Hearing loss: Can affect the way children hear and imitate speech.
Key points about speech sound disorders in children. A speech sound disorder means a child has trouble saying certain sounds and words past the expected age. A child with an articulation disorder has problems making certain sounds the right way. A child with phonological process disorder regularly makes certain word speech mistakes.
speech disorder, any of the disorders that impair human speech.. Human communication relies largely on the faculty of speech, supplemented by the production of certain sounds, each of which is unique in meaning. Human speech is extraordinarily complex, consisting of sound waves of a diverse range of frequencies, intensities, and amplitudes that convey specific information.
hearing loss, from ear infections or other causes; or. brain damage, like cerebral palsy or a head injury. Adults can also have speech sound disorders. Some adults have problems that started when they were children. Others may develop speech problems after a stroke or traumatic brain injury, or other trauma.
Commonly referred to as a speech disorder, a speech impediment is a condition that impacts an individual's ability to speak fluently, correctly, or with clear resonance or tone. Individuals with speech disorders have problems creating understandable sounds or forming words, leading to communication difficulties.
Speech Disorder: any defect or abnormality that prevents an individual from communicating by means of spoken words. Speech disorders may develop from nerve injury to the brain, muscular paralysis, structural defects, hysteria, or mental retardation.
Disorders of speech and language are common in preschool age children. Disfluencies are disorders in which a person repeats a sound, word, or phrase. Stuttering may be the most serious disfluency. It may be caused by: Genetic abnormalities. Emotional stress. Any trauma to the brain or infection.
Certain birth defects, such as a cleft palate, can interfere with someone's ability to produce speech. People with a cleft palate have a hole in the roof of the mouth (which affects the movement of air through the oral and nasal passages), and also might have problems with other structures needed for speech, including the lips, teeth, and jaw.
speech defect: [noun] a defect in oral speech (such as lisping or stuttering).
Dysarthria (pronounced "dis-AR-three-uh") is a motor speech disorder that makes it difficult to form and pronounce words. Motor speech disorders occur when damage to your nervous system prevents you from fully controlling parts of your body that control speech, like your tongue, voice box (larynx) and jaw. Dysarthria makes it challenging to ...
Spasmodic Dysphonia (SD) is a chronic long-term disorder that affects the voice. It is characterized by a spasming of the vocal chords when a person attempts to speak and results in a voice that can be described as shaky, hoarse, groaning, tight, or jittery. It can cause the emphasis of speech to vary considerably.
Introduction. Speech-language deficits are the most common of childhood disabilities and affect about 1 in 12 children or 5% to 8% of preschool children. The consequences of untreated speech-language problems are significant and lead to behavioral challenges, mental health problems, reading difficulties, and academic failure including in-grade retention and high school dropout.
speech defect: 1 n a disorder of oral speech Synonyms: defect of speech , speech disorder Types: show 10 types... hide 10 types... anarthria partial or total loss of articulate speech resulting from lesions of the central nervous system aphonia , voicelessness a disorder of the vocal organs that results in the loss of voice cataphasia a speech ...
Meaning of Speech Defects: Speech defects and disorders develop more prominently when the baby is just learning to speak. Speech disorders, even baby talks are serious handicaps to social adjustment of the child. Particularly when he grows up, mixes, and communicates with people, he feels inferior, anxious and withdraws from the group, society ...
A disorder of speech.... Click for English pronunciations, examples sentences, video.
Machine learning definition. Machine learning is a subfield of artificial intelligence (AI) that uses algorithms trained on data sets to create self-learning models that are capable of predicting outcomes and classifying information without human intervention. Machine learning is used today for a wide range of commercial purposes, including ...
Israel advocacy groups in Canada and the U.S., such as the Anti-Defamation League, the Centre for Israel and Jewish Affairs and B'nai Brith, say the slogan is an antisemitic call for the ethnic ...
Natural language processing (NLP) is a subset of artificial intelligence, computer science, and linguistics focused on making human communication, such as speech and text, comprehensible to computers. NLP is used in a wide variety of everyday products and services. Some of the most common ways NLP is used are through voice-activated digital ...
A Free Speech Champion's Advice: U.C. Berkeley's leader, Carol Christ, has spent the last several months asking students to consider the way speech and protest affect the entire campus community.
It's a new week in the election campaign - and over the next four days parties will launch their manifestos. Today is the turn of the Liberal Democrats, who have pledged £9bn for the NHS.