Compliance and documentation
How to write progress notes.
Progress notes are the core piece of documentation a mental health care provider should write after each session with a client, but it’s more than just a record of what happened in the session.
Progress notes are aptly named: It’s a documentation of each session with your client where you share the progress you’re making on your treatment goals. Specifically, the treatment goals you aligned on in your treatment plan .
Simple, right? Not always, when you’re navigating insurer requirements and billing standards.
“I often hear from providers I work with that the concept of progress notes is ‘easy,’ but writing them in a compliant way is the hard part,” says Innocent Turner, Clinical Strategy and Quality Manager at Headway.
If the “rules” for writing compliant progress notes are confusing and vague, that’s because they’re left open for you to step in as the expert.
Other than following the advice in this article (or using a great template), Innocent recommends a quick gut check.
Read your progress notes back to yourself and reflect: Does this accurately portray what happened? Or is there an element of treatment that didn’t make it onto the page? If you feel like you’ve forgotten something, you probably did, but you can always figure out a way to include it.
This guide will help you understand the purpose of progress notes, what to include in your session documentation, and helpful templates and examples to get you started.

Use Headway’s free progress notes feature
When you’re a Headway provider, you get complimentary access to built-in documentation templates designed to make your note-taking fast, easy, and compliant.
Learn more about Headway’s EHR features and enhanced rates today; and start seeing insurance clients in less than 30 days.
What are progress notes?
Progress notes are the core piece of documentation a mental health care provider should write after each session with a client, but it’s more than just a record of what happened in the session. Progress notes keep a record of the client's progress and the care you provide.
“When someone reads a note, they need to understand how your patient presented, what's going on with them right now, how you helped them, and how they received that help,” says Innocent Turner, LCSW and Headway’s Clinical Strategy Lead. “And if those questions are answered for the most part, you’re good.”
It’s also important that clear continuity of care is documented: While each note should lead into the next, each note should also stand alone, demonstrating a clear and comprehensive story of the client's progress through treatment.
You don’t need to include everything your client said in your progress notes, only what pertains to their treatment. If they spend the first 5 minutes complaining about their in-laws, don’t worry about capturing that in your documentation.
3 essential types of clinical documentation
A complete patient chart contains three core pieces of clinical documentation : an intake assessment, treatment plan, and progress notes.
Think of these as the “golden thread” : Your intake note should inform your treatment plan, and your treatment plan goals and objectives should be reflected in each progress note.
Here are the key details of the different types of documentation:
- An intake assessment (intake note) should be created when initiating a treatment relationship with a client, and serve to document their current state and past experiences with mental healthcare.
- A treatment plan establishes objectives and monitors progress. The plan includes a diagnosis and clearly establishes medical necessity for treatment.
- Progress notes should demonstrate a clear and comprehensive story of the client’s progress through treatment. Clear continuity of care is important — each note should lead into the next but also stand alone.
Clinical documentation is a staple of any mental healthcare practice — it’s used to clarify the purpose of your sessions, justify the billing code used, and demonstrate a good picture of the patient’s current mental state.
These standards are outlined by the American Medical Association (AMA), Centers for Medicare and Medicaid Services (CMS), National Committee for Quality Assurance (NCQA), commercial insurers, and other regulatory agencies.
Your license or a particular insurer may have even stricter requirements than those set forth here.
6 progress notes requirements
Your progress notes need to contain the following details in order to effectively capture the progress you’re making with the client towards their goals.
1. Session details
These easy-to-note facts are required for all documentation, including your progress notes:
- Start and stop time
- Place of service: For telehealth sessions, include the client's location (for example: “home” or “office,” as well as a statement that the session was conducted via a HIPAA-compliance audio/visual platform)
- Date of service
- Patient name and a second unique identifier, such as their date of birth or an assigned ID number
- Provider name and credentials
2. Person-centered details
Person-centered details are session-specific information that paints a helpful picture of the client's mental state and feelings, in their own words. Infusing specificity into your notes — such as the use of quotations from your client — helps insurers verify that the session was unique and veritable, and that you didn’t simply copy and paste from a previous session.
3. Patient-centered observations
Your notes should reflect a clinical assessment of your client’s current mental state in order to portray the full picture of their symptoms, diagnosis, and treatment. As a guide, each progress note should include at least three components of the mental status exam, such as descriptions of the patient’s appearance, behavior, alertness, reasoning, or mood.
4. Progress towards goal(s)
Make sure you identify progress towards the goal(s) outlined in your treatment plan, including whether the client made progress, regressed, or stayed about the same. Insurers review this item frequently; it's one of the most commonly missed. If you need to update the treatment plan, say that too. This will support the CPT code you're using and offer clarity if treatment goals change frequently (as they sometimes do).
5. Risk assessment
Because this is a sensitive area, it's especially important to clearly and completely document any risks in your progress note — it must also be unique to each session. Documentation of risk can be simple such as "client denies all areas of risk." That said, if you identify a risk, you are required to identify the client's risk level and create and document a safety plan. In these cases, you don't need to document the safety plan in the progress note itself, but you do need to include a note that the safety plan was created and the client agreed to it. For example, you might write "safety plan was discussed and reviewed with client."
6. Clinical path forward
Progress notes should outline the evidence-based practice used in the session, and comment on any changes in modality. You might also include any skills that may be helpful for clients to practice to help manage or reduce their symptoms, and why it would be helpful in reducing their symptoms.
Templates for progress notes
Because progress notes are required for every session through insurance, it’s helpful to leverage a template to help you complete your notes quickly and comprehensively.
Three of the most common progress note templates include:
- SOAP notes : Subjective, Objective, Assessment, Plan. This format allows the provider to document their observations of the client and the session, and how they’re approaching the care plan. This is a popular type of template for talk therapy, especially used by licensed clinical social workers.
- DAP notes : Data, Assessment, and Plan. These are similar to SOAP notes, but condense the subjective and objective sections into a single reflection of “data.”
- BIRP notes : Behavior, Intervention, Response, and Plan. These notes help the provider reflect on the specific problem, or behavior, that’s being addressed in the session, then document what they tried and how it was received by the client.
Progress note example: SOAP note
Here’s an example of a progress note that meets most insurance carriers’ expectations for this type of clinical documentation. It follows the SOAP note template :
- Subjective: A provider's own observations as well as the client's stated reasons for seeking care. Can include general references to the client's likely emotional state and the provider's summary of presenting problems.
- Objective: References to specific and measurable elements from the session, such as physical appearance and the client's progress toward goals and modalities used during the session.
- Assessment: A set of conclusions based on the provider's professional synthesis of both subjective and objective observations.
- Plan: Next steps for the client, based on the provider's assessment, such as when the next session will take place, and what updates may be needed for the treatment plan.
Notice how it contains all 6 of the primary requirements for a compliant note.
Client Full Name: Katie Client Client Date of Birth: 9/9/1999
Date of Service: 3/08/2023 Exact start time and end time: 10:23 am – 11:20 am: 57 mins
Session Location: Telehealth, patient provided consent to telehealth, service performed on HIPAA compliant software
Subjective notes: Katie presents today’s session feeling “depressed.” She states that her mood has been “getting worse.” She reports that she has been struggling to get out of the house to enjoy social events that she is actually interested in, then becomes more frustrated with herself. She describes an increase in sleep issues, both difficulty falling asleep and staying asleep. Katie says that she “just wants to be better.” Katie continues to endorse low energy, loss of interest in activities, difficulty sleeping, and feelings of guilt, although she is not able to express the source of her guilt.
Objective notes: Therapist helped Katie process her feelings, provided in depth psychoeducation on guilt and how it relates to depression. Katie’s mood throughout the session was low, flat affect, her speech is low volume and soft. Therapist used the CBT triangle in session to assess Katie’s ability to identify patterns in behavior and thoughts. Katie required extensive guidance to understand the concept of the thought triangle. Therapist explored her feelings of guilt at length, and used socratic questioning to fully engage with past experiences that may be triggering guilt/shame. Therapist helped Katie process how her feelings influence her behavior (CBT triangle) and discussed in depth behavioral patterns that potentially are increasing her depressive symptoms.
Assessment: Katie continues to struggle with depressive symptoms, primarily guilt, making it difficult to engage with her surroundings as she desires. She lacks insight into her diagnosis, often saying things like “if I don’t want to be depressed then why am I depressed.” She required extensive socratic questioning to help her gain a little more insight into her diagnosis and feelings of guilt/shame. She denies SI/HI/AVH. She is struggling to make progress toward her goal of identifying triggers or past experiences that contribute to her feelings of guilt and worthlessness, as she requires redirection to provide relevant examples and/or to clarify her comments.
Plan: Therapist will continue to use CBT informed treatment to help Katie learn coping skills to manage depression symptoms and specifically guilt. For the next week, therapist asks Katie to consider her core beliefs and the source of her core beliefs. She was provided a worksheet to help clarify what core beliefs are and some potential sources. Therapist recommends meeting in one week, Katie will schedule the next session.
Client Signature and Date: Katie Client, 3/8/23
Clinician Signature and Date: Olivia Wells, LMFT, 3/8/2023
This document is intended for educational purposes only. Examples are for purposes of illustration only. It is designed to facilitate compliance with payer requirements and applicable law, but please note that the applicable laws and requirements vary from payer to payer and state to state. Please check with your legal counsel or state licensing board for specific requirements.
Are progress notes just for insurance?
Progress notes are a requirement for billing sessions with insurance, but they also simply provide a written record of the care you delivered.
Even therapists who operate their practices through self pay should document progress notes. There may be times when thorough mental health care documentation becomes important, such as if your client transitions to a new provider or ends up in a health crisis or legal proceeding.
“If your patient is in some type of crisis — not even a mental health crisis but something like a car accident — they may end up in a hospital telling their care team, ‘yeah I see a therapist’,” says Turner. “Their care team might need to know what’s been going on in your care, so they can provide consistent care — like not giving medication that might cause issues.”
How to bill and code progress notes
It’s important to choose the medically appropriate billing code for the correct service delivered, and ensure your documentation supports and substantiates the service.
For talk therapists:
- CPT code 90834: 45 minutes of psychotherapy, where the total time spent with the patient is 38–52 minutes
- CPT code 90837: 60 minutes of psychotherapy, where the total time spent with the patient is 53–60 minutes
For psychiatrists and nurse practitioners:
- CPT code 99204: 45-minute new patient outpatient visit, where the total time spent with the patient is 45–59 minutes
- CPT code 99205: 60-minute new patient outpatient visit, where the total time spent with the patient is 60–74 minutes
Notes associated with 45-minute sessions should include a connection to the client’s diagnosis, symptoms, and plan, as well as details about how the session impacted their symptoms.
A 60-minute session note should include all the same details, as well as notes relating to medical necessity of why extra time was needed for more intensive treatment. This doesn’t have to be extensive – it just needs to be directly acknowledged. (You can find examples of medical necessity statements to help you craft your notes.)
It’s important to use the code that most accurately reflects the time you spent with the patient to treat their condition, and ensure that documentation for the session supports the chosen code.
Documentation of relevant aspects of client care, including documentation of medical necessity, should ideally be completed within 24 hours of visit, and no later than 72 hours.
Compliance— a Headway Guide
Navigating compliance can be time-consuming and stressful. We’re committed to changing that.
What are therapy intake assessments?
The intake assessment is your chance to get a deep understanding of your patient — and maybe connect some elements from their journey that they wouldn’t connect themselves.

How to write a mental health treatment plan
Whenever you want to change the goal of your therapy care, or the path you want to take with the client to reach that goal, you’ll want to document a treatment plan.
866-847-3590
Log in classic, log in plus.

How to Write Progress Notes
As a therapist, progress notes are necessary for you to track your patient's progress and ensure they are receiving effective treatment options. Progress notes contain critical information about an individual, couple, or group therapy session you can reference to adjust or modify your methods as needed.
However, if your notes are often illegible, confusing, unorganized, or not detailed enough, it can be difficult to translate them later and may cause you frustration and wasted time. To provide effective and efficient care, it's critical to keep your progress notes organized, specific, relevant, and concise. Below, we'll examine the differences between progress and psychotherapy notes, documentation styles you can use, and how implementing EHR software can enhance your note-writing processes.
Table of Contents
- How Progress Notes Differ From Psychotherapy Notes
Examples of What Makes Up Progress Notes
Documentation Styles
- How to Write Effective Progress Notes
- Common Terminology and Interventions to Reference
Best Practices for Writing Progress Notes
- Why You Should Consider Using EHR Software for Progress Notes
Writing Better, Writing Faster
Get Instant Access to Our Guide to Efficient Clinical Notes in Behavioral Health.
How Progress Notes Differ from Psychotherapy Notes
Though you may have heard progress notes and psychotherapy notes used interchangeably, they have a few significant differences in their purpose, formatting and who has access to them. For starters, psychotherapy notes are generally for a therapist or other mental health professional alone to view and reference to help remember patient encounters. These are your personal notes to use as needed in individual, couple, or group counseling sessions which may contain your unique interpretations and impressions of patients.
The Health Insurance Portability and Accountability Act (HIPAA) regulates psychotherapy notes . These notes may not be included in any other documentation about your clients, such as billing or medical information, and cannot be shared with anyone else, including the client, unless in some cases where you may need their permission to share them. Psychotherapy notes should never contain information about your patient:
- Results of clinical tests
- Treatment plan details
Progress notes, on the other hand, have a much more formal structure and include your client's medical and treatment plan details. These notes help therapists and other treating practitioners stay updated on their work with a patient and help inform insurance companies of the efficiency of your methods.
You may have to write your progress notes according to specifications by the insurance company, but these notes can also protect you if questions arise about your quality of care. Other behavioral health providers working with your client, the client themselves, and their family members are generally allowed to view your progress notes.
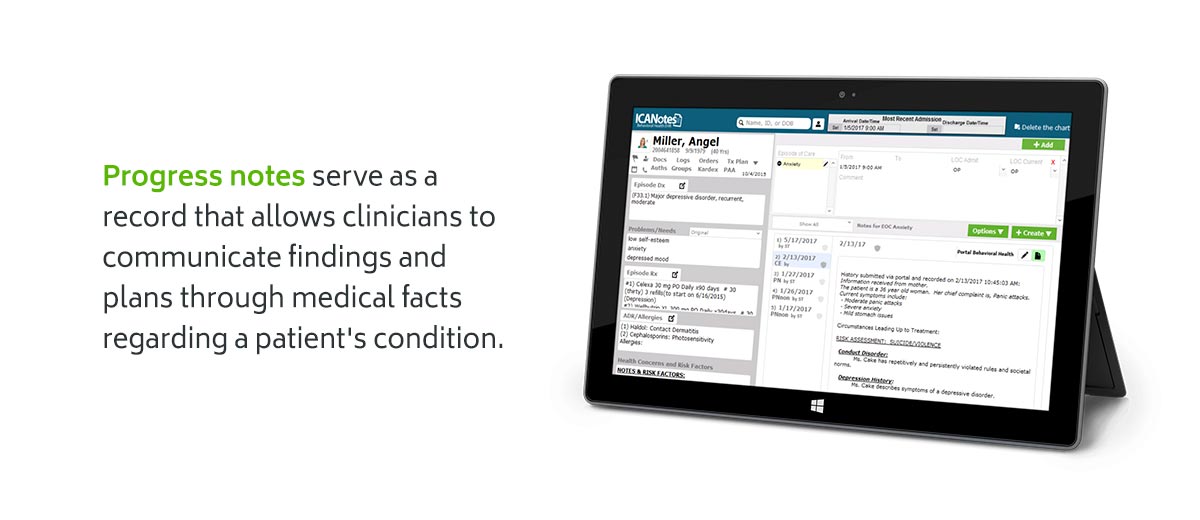
Progress notes serve as a communication tool between you and other clinical staff about your patient's overall care and treatment plan. With consistent, updated notes, you can focus more easily on your patient's progression and streamline your billing and reimbursement processes. These notes are also protected under the HIPAA Privacy Rule , so it's important to know what information is protected, like individual identifiers.
Though we briefly mentioned the general structure of progress and psychotherapy notes above, let's look at more specific progress note examples and what therapists and other behavioral health professionals must document.
Progress notes serve as a record that allows clinicians to communicate findings and plans through medical facts regarding a patient's condition. The specific elements you must include in your progress notes may depend on the insurance company, your state requirements, your licensing board, or your professional organization or practice. It's critical to check with these channels and confirm your note formats and templates are compliant.
In general, all progress notes should include a variation of the following:
- Demographic information: You may include your client's name, date of birth, start and end times of each session, and your signature.
- Description of client behavior: Describe your client's behavior, appearance, mood, symptoms, diagnosis, changes to medications, and a safety assessment. You can also use a mental health status checklist to help consolidate this area of your notes.
- Treatment plans: List the treatment modalities, recommendations, coping skills, and assignments you used during the session. You should also include your client's response and progress toward their established goals and what you plan to work on in the following session. Note any referrals you've made for the client or if you've collaborated with other mental health professionals regarding your client.
Your progress notes should never include anything that cannot be validated or justified through clinical evidence and investigation, so there should be no references to your subjective opinion, judgments, feelings, or hypotheses. Your progress notes should only contain precisely what you observe through your professional opinion and what was discussed between you and your client during your session. In some cases, you may need to make an exception in your notes, such as if your client brings up a critical incident, significant changes, or risk of harm to themselves or others.
Here's an example of patient symptoms/behaviors in a progress note:
"Jane denied having suicidal thoughts in the past week. She reported feeling anxious and sad most of the time. She received a write-up at work this week. She expressed frustration with her management. Jane was tearful as she talked about feeling incompetent at her job and not understanding how she can progress. She noted that after speaking to her manager about the write-up using a recommended therapeutic exercise, he was more understanding and offered to help improve her training".
Because there are many different ways you can conduct your notes to meet your needs, let's look at four different documentation styles therapists commonly use to keep their progress notes organized, relevant and concise. While you can use these documentation formats for other types of notes, we'll focus on structuring them to fit progress note criteria.
In DAP notes, you will construct your progress notes in a Data, Assessment, and Plan format. These notes should include:
- Data: Include descriptions of major events or topics discussed and interventions you provide. Collect objective and relevant information, including behaviors, actions, and descriptions from the patient that may affect their treatment methods.
- Assessment: Your observations of your client's status and functioning, including risk status, are considered the assessment. Analyze the data you've collected and include your client's response to the methods you use during the session.
- Plan: List any plans for the future or changes to your client's treatment plan, such as recommendations, alternative treatments, homework assigned, and additional resources.
DAP notes may also sometimes be referred to as DARP notes, which include the acronym for Response. In these notes, you will fill out the Data, Assessment, and Plan section as usual, but include a “Response” section after your Assessment. This section will include your clinical rationale and reasoning for providing specific treatment based on your most recent interactions with your client.
The four sections of the SOAP method include:
- Subjective data: Though progress notes should remain free of your unsourced personal opinions and judgments , such as describing a client as “hysterical," you may be able to list a patient's direct quotes, experiences, feelings, thoughts, or observations.
- Objective data: Note your patient's general and mental health status and other relevant details from your therapy appointment. List your descriptions as if you were performing a physical exam of your client, including their body language or other facts.
- Assessment information: After collecting your subjective and objective details, provide your professional interpretation and a summary of your patient's diagnosis. Include your conclusion about the interventions and goals you addressed during the session.
- Plan: List any details regarding the next steps or adjustments to your patient's treatment plan. Note any follow-up information, referrals, lab orders, review of medications, and your plan for your next therapy session.
Like SOAP notes, BIRP notes involve four different sections to help therapists and mental health professionals document patient progression and treatment. However, BIRP notes focus more on patient behavior . The four sections of BIRP notes should include:
- Behavior: Document the chief complaint or primary problem the patient presents, including their actions, willingness to participate, and observations of their behavior.
- Intervention: Provide a detailed account of the methods you used to intervene and help your patient reach their treatment goals, such as the questions you asked and decisions you made to adjust treatment or techniques.
- Response: Describe your patient's response and reaction to your intervention techniques and treatment methods. Record what they said, the questions they asked, and whether they changed their minds about therapy.
- Plan: Create a plan for your next session with the patient and note the time and date when you will meet again. Note what you plan to discuss in the next appointment and whether you assigned any exercises for your patient to complete before their next session.
How to Write Effective Progress Notes
Here is a step-by-step guide for progress notes that can help ensure you have all the important details and information needed to create more effective documentation:
- Note header: Write a brief review of session information, such as the practitioner and patient name, the time and date of the appointment, and relevant service or billing codes.
- Diagnosis: Include any DSM-5 or ICD-10 codes if you have diagnosed your patient with a mental health condition.
- Patient Appearance: Provide an objective description of how your patient appears, including their behavior or cognitive functioning.
- Safety concerns: Note any critical information regarding your patient's safety and well-being, including risks.
- Medications: Psychiatrists may only need to use this section, but as a therapist, you can list a patient's medications and their relationship with them, such as if they feel they're effective.
- Symptom description report: Include direct quotes and reports about your patient's status, such as how they're feeling, their opinions on their treatment plan, and how they view their progress.
- Relevant information: Describe any valuable, objective data such as therapy notes, documents, and test results to help keep your progress notes updated.
- Interventions: Document the treatment modalities and interventions you applied during the session, such as relaxation techniques, cognitive restructuring, or mindfulness training.
9. Treatment plan progress: With each progress note during each session, you should mention whether you and your patient are successful at achieving their treatment plan objectives.
10. Signature: You must always include your signature on your progress note documents to keep them compliant. You may also need to include your credentials.
As part of the overall therapy treatment for your client, you may also have an admission and discharge/dismissal note, which are important to keep in your records:
- Admission note: Following the initial assessment session with your client, your admission progress note will include the presenting problem, the participants in the session, your observations, acknowledgment of informed consent and patient rights, and your recommendations.
- Discharge/dismissal note: Following termination with your patient, corresponding with your final session, your discharge note will include a summary of the treatment provided, the level of progress achieved through the treatment plan, the reason for termination, and your recovery plan recommendations.
Common Terminology and Interventions to Reference
When documenting progress notes, it can be helpful to refer to common terminology and different interventions you can use to keep your notes professional and objective.
Some examples of common terminology used in progress notes to describe a patient's appearance and health include:
- Affect, Mood, or Disposition: Depressed, dejected, lighthearted, disheartened, carefree, listless
- Attitude: Disagreeable, apathetic, inert, quarrelsome, absence of effect
- Behavior: Lethargic, spontaneous, immediate, over-cautious, sluggish
You may also include descriptions of a patient's cognition, orientation, or work habits from their direct quotes or your observations.
Here's a list of frequently used interventions you can reference to help you and other practitioners understand different treatments a patient might be undergoing with other specialists:
- Behavior reinforcement
- Collaborative problem-solving
- Anger management
- Communication skills development
- Cognitive restructuring
- Mindfulness
- Progress or objective review
- Coping strategies development
- Stress management
- Problem-solving skills development
- Eye movement desensitization and reprocessing
- Identifying triggers
Since you need to update your progress notes after each session with every client, here are some tips to keep in mind that can help boost efficiency in your note-writing process:
- Read your progress notes before meeting with your patient to refresh your memory and know what to discuss.
- Ensure your notes always mention the time and date of entry, the duration of your sessions, and your signature.
- Refer to your previous progress note entries for continuity.
- Document your notes as soon as possible after each session so you don't forget any important details.
- Avoid using acronyms, abbreviations, and jargon in your notes, because it can be difficult for you and other practitioners to understand later.
- If you make a mistake, cross it out and continue. Don't tamper with your entries.
- Write down all relevant information or details about your sessions you think can be useful for developing or adjusting your treatment plan. Remember, if you don't write it down, it didn't happen.
- Keep in mind, your progress notes contain confidential information and must always be kept in a secure location and only accessed by you, your patient, or other authorized behavioral health staff.
Why You Should Use EHR Software for Progress Notes
Depending on how many patients you see and how frequently, you can end up spending several hours every day writing your progress notes . Not to mention, hand-written, paper progress notes can present many issues, such as getting lost or damaged. Paper progress notes will also take you much longer to complete than electronic notes, such as those within electronic health record (EHR) software .
Research shows that clinical documentation contributes heavily to staff burnout because it takes significant time that therapists and other mental health professionals could instead spend with patients. One study found that clinicians welcome a serious redesign of documentation processes to restore autonomy, eliminate the number of actions that do not add value and return time to staff for more essential care activities.
By introducing EHR software, you can lift the burden of documentation with these benefits:
- Making your notes legible, easy and quick to read
- Reducing documentation errors or missing information
- Preventing lost revenue due to under-coded notes or claims being rejected
- Reducing time spent on documentation and record-keeping
- Using client progress note samples and other templates for various types of therapy
- Increasing your peace of mind that your notes will pass regulations
- Simplifying and minimizing the expense and turnaround time of transcribing clinical dictation
ICANotes Can Help You Write Your Progress Notes
As a mental health therapist or practitioner, improving your note-writing processes can help you create more effective, useful, and legible progress notes that make it easier to communicate with other professionals about your patients. With ICANotes, you can access several charting and note templates for quick, comprehensive documentation.
Our behavioral health EHR contains many specialized features designed to help you reduce your documentation time, comply with regulatory requirements, get paid faster, and spend more time with your clients. To learn more about our service and features, contact us today or start your free trial to see how our software can enhance your progress notes.
Start Your Free Trial Today
Therapist Shame and Documentation: How the Shame Spiral Keeps You Behind on Notes and Hating Documentation
Top 8 Things to Include in Your Substance Abuse Counseling Notes

How to Write DAP Notes

How to Write Couples Therapy Notes
Types of Therapy Notes

6 Reasons Why You Should Avoid Medical Transcribing Services

EMDR Therapy Note-Writing Tips
Biggest Myths About Clinical Notes
How Much Time Are You Spending Writing Mental Health Notes?
- Psychiatric Nurse Practitioners
- Psychiatric Hospital Records
- Certified Drug & Alcohol Abuse Counselors
- Social Work Case Management Software
- Family Therapists
- Group Therapy
- EHRs for Integrated Care
- Sample Notes
- Appointment Reminders
- Document Management
- Patient Portal
- Telehealth Platforms for Mental Health
- Billing Software for Mental Health Professionals
- Clearinghouses
- Health Information Exchange Integration
- Interoperability
- Lab Integration
- PDMP Integration
- Mobile Medication Management
- Automatic Coding
- ONC-ATCB Certification
- CARF Compliance
- Joint Commission
- Meaningful Use
- Medicaid-Compliant EHR Software
- Assessment Tools
- Behavioral Health EHR
- Sample Treatment Plans
- Note Writing Tips
- Treatment Planning
- Practice Management
- Mental Health Care Trends
- All Blog Categories
- Our Leadership Team
- Customer Reviews
- Quote Request
- Remote Support
- Access ICANotes
- Knowledge Base
- Support Portal
- User Guides and Documentation
5 Perfect Nursing Progress Notes Examples + How to Write

If you are a nurse, you know one of the most important parts of our jobs is to document about our patient’s status, the care they receive, and their response to any treatments. There are many types of documentation nurses and other healthcare professionals use. One type of documentation is a nursing progress note. If you are new to nursing or unsure about the different types of documentation, you may wonder, “What is a nursing progress note?” In this article, I will tell you about nursing progress notes, what they are, their purpose, and the advantages and disadvantages of using them. I will also share 5 perfect nursing progress notes examples + how to write them. At the end of this article, I will answer some frequently asked questions about nursing progress notes to give you more insight into these important documents.
WHAT IS A NURSING PROGRESS NOTE?
What is the purpose of writing a nursing progress note, is a nursing progress note the same as a nursing progress chart, 3 advantages of nursing progress notes, advantage #1: nursing progress notes keep patient information accessible, advantage #2: you can use nursing progress notes to promote positive patient outcomes, advantage #3: nursing progress notes create a legal record of the care you provide, 2 disadvantages of nursing progress notes, disadvantage #1: it is time-consuming to create nursing progress notes, disadvantage #2: it is easy for the nursing progress note to become repetitious, what elements should be included in a nursing progress note, 1. subjective data:, 2. objective data:, 3. nursing assessment findings:, 4. planned nursing interventions:, 5. patient response to interventions:, what elements should not be included in a nursing progress note, 1. jargon or meaningless phrases should not be included:, 2. avoid providing unnecessary information:, 3. another nurse’s opinion or statement about a patient:, 4. unapproved medical abbreviations should be avoided:, 5. care not yet given should never be documented:, how to write a perfect nursing progress note, step #1: begin the nursing progress note with relevant information, step #2: provide a general description of the patient and the reason for their visit/encounter, step #3: perform a patient interview to obtain subjective information, step #4: gather essential objective data and record your findings., step #5: describe proposed treatment plan, step #6: document nursing interventions, step #7: document the patient’s response to care or treatment provided, what are the perfect examples of nursing progress notes, bonus 7 most common mistakes to avoid while writing nursing progress notes, mistake #1: adding irrelevant or unnecessary information, about the mistake:, how to avoid:, mistake #2: making assumptions, mistake #3: using incorrect or unapproved abbreviations, mistake #4: writing sloppy notes, mistake #5: waiting too long to write your note & forgetting important facts, mistake #6: not reviewing progress notes from previous shifts, mistake #7: not documenting care or interventions, my final thoughts, frequently asked questions answered by our expert, 1. who can write a nursing progress note, 2. when to write a nursing progress note, 3. do nurses write progress notes every shift, 4. ideally, how long should nursing progress notes be, 5. what’s the most important part of a nursing progress note, 6. what are the 5 legal requirements of nursing progress notes.
• Documentation must be centered around the nursing assessment and nursing interventions that should occur. • The note should document previous conditions and responses to treatments as well as changes in the patient’s health condition and any new interventions to be implemented. • The nursing progress note must reflect the extent of care needed, such as continuous care, the patient’s needs, and any interventions initiated to provide that care. • HIPPA Privacy Rules must always be upheld. • The nursing progress note must be clear, legible, and contain accurate information.
7. Can I Use Abbreviations In A Nursing Progress Note?
8. what tense do i write a nursing progress note, 9. are nursing progress notes handwritten or printed, 10. how to sign off nursing progress notes, 11. what happens if i forget to write a progress note on the time it should have been written, 12. can a nursing student write a nursing progress note.

How to Write Patient Progress Notes [+ Example]
Table of contents.
Nurses are with the patient more than any other provider on the healthcare team, so you carry a big burden as a nurse to keep close watch over your patients and document every single detail of their care — no pressure though!
Below, I’m sharing what goes into good patient progress notes, from what they are to how to write them.
What Are Patient Progress Notes?
Patient progress notes are used to keep a record of a patient’s care when they are staying at a hospital. Nurses, doctors, physical therapists, and all other members of the healthcare team who provide care to the patient will document notes in the patient’s chart. All progress notes can be accessed by the members of the healthcare team in order to keep everyone aware of what is going on with the patient’s condition and care.
As a nurse, you will spend a lot of time reading patient progress notes as well as writing your own. Many nurses start their shift by reading through progress notes to get an idea of what’s going on with the patient and to prepare for their day of caring for them.
How to Properly Write Patient Progress Notes
Even though you won’t be the only healthcare provider writing patient progress notes, your notes as a nurse are some of the most important because you’ll be spending more time with the patient than any of the other providers. Here are some tips to follow to help you write effective patient progress notes.
Include essential information
There are essential pieces of information that should be included in every patient’s progress note.
Every patient progress note should include:
- Date and time
- Name of the patient
- Identification of the nurse who is writing the note
- An overview or general description of the patient
- Clinical assessment
- Any incidents that occurred
- Any changes noticed by the nurse (such as changes in the behavior, well-being, or emotional state)
- Any changes in the care (such as shift change to a new nurse or new orders placed by a doctor)
- Recommendations for further care
Use subjective and objective data
You should use subjective and objective data to craft a nursing note. Subjective data include information that the patient has provided, such as their pain level and their perspective. Objective data are what you have observed or gathered as the nurse, such as the patient’s visible state, their vital signs, or other clinical markers of their condition.
Make sure to distinguish between these two things when documenting. You can write things like “the patient states their pain level is a 10 and that they feel nauseous”. To gather subjective data prior to writing a nursing note, ask the patient questions about how they are feeling.
Use the nursing process as a guide
Whether you’ve just started nursing school or you’ve graduated, you’re likely familiar with the nursing process. I personally remember having this concept drilled into me as a brand new nursing student.
The nursing process is as follows:
- Diagnosis (nursing diagnosis)
- Intervention
The nursing process is a great guide for progress notes because it covers all bases. Remember, nurses can’t diagnose in the same way that doctors can, so you can discuss nursing diagnoses (such as pain or risk of infection) or you can note what the doctor has stated as the diagnosis.
Types of Nursing Documentation
Students and new graduates are often confused by all the different forms of nursing documentation. Here are some examples to help you distinguish them.
1. Charting
If you haven’t already, you’ll soon realize that charting is a big part of being a nurse. Charting includes all documentation of the patient’s care that is documented in the patient’s computerized chart. When charting patient assessments, you’ll use a computer-based spreadsheet to go through each body system and plug in information such as the patient’s pain level, how their lungs sounded, what their pulse felt like, etc. Progress notes are one aspect of charting.
2. Progress notes
Progress notes are the written notes that you’ll add to your patient’s chart when any changes occur. If the patient’s condition starts to decline or there are any changes in the patient’s care, then you will want to put a note in the chart so that it is documented. Progress notes are not only written by the nurse but by all of the providers who see the patient.
3. Handwritten notes
As a nurse, you will likely also keep some handwritten notes ( I know I did). Handwritten notes are a helpful way to jot down information as it’s happening if you’re not able to get to a computer right away.
4. Verbal communication at shift change
Another form of important communication as a nurse is the handoff report that you will give and receive at the end and start of each shift. This is an overview of each patient that is shared between nurses when a shift is changing. You’ll likely use your handwritten notes when giving your handoff report to the next nurse.
Why Is Documentation Important for Nurses?
Documentation is crucial for nurses because it helps to ensure proper patient care.
Nurses use patient progress notes to learn about new patients and their conditions, then they use progress notes to keep track of a patient’s care throughout their hospitalization. Progress notes are used by all members of the healthcare team to get an idea of how a patient is progressing throughout their hospitalization.
If for some reason a patient’s condition declines, documentation can be used to look back and determine whether any of the healthcare providers are at fault. In the rare case that a patient or their family decides to sue the hospital because of medical negligence, the nurses’ notes are some of the main documentation that will be used and looked at to determine what happened in the patient’s case. Many nurses use progress notes as a method to “cover themselves” in the case of a lawsuit. If you clearly documented every aspect of the patient’s care that you were involved in, you’re less likely to be blamed for whatever went wrong.
When Should You Write Progress Notes?
Every hospital will be a little different when it comes to how they prefer to have charting and progress notes performed. Some nurses enter progress notes at shift change, some write them with each patient assessment – it just varies. Ask your supervisor or the other nurses on your unit about how they prefer progress notes be written. If you have any issues with your patient, such as a decline in their condition or a transfer to a more critical unit, this would be a time when you should include a progress note.
Tips for Writing Effective Progress Notes
Writing strong patient progress notes is a skill that you will develop with time and experience as a nurse. In the meantime, you can follow some of these tips to help ensure that your progress notes are effective and informative.
Follow your workplace’s protocol
Asking your supervisor and other nurses on your unit can help you determine whether there is a specific format that you’re supposed to follow when writing patient progress notes. Every hospital will be a little different in what they prefer.
Use the facts
Try to be as objective as possible when writing patient progress notes. Include the facts and observations that are essential to help a person understand the situation at hand. Objective information ensures accuracy and understanding for anyone who reads the notes.
Keep it concise
Try to avoid including unnecessary information in your progress notes, despite possibly wanting to include it (such as stating that the patient called you a name or was rude to you). Adding anecdotal information to a progress note waters down the actual purpose of the note and pulls the attention of whoever reads it away from the important information. Not to mention, it is unprofessional!
Review the notes of other nurses
If you’re new to nursing (or still in nursing school) take some time to review examples of other nurses’ progress notes for their patients to get an idea of what a strong progress note looks like.
Example of a Patient Progress Note
Here is an example of a patient progress note that includes all the necessary information:
Date: 02/15/2023
This RN (Sophia) found the patient slumped over in bed. Upon assessment, the patient was found to be cold and sweaty. This nurse was able to wake the patient by tapping them on the arm and stating their name, but the patient remained in a disoriented, drowsy state. The patient’s speech was slurred and their eyes were glazed over. Vitals were taken. Blood pressure 125/45; Pulse 65; Blood glucose 50. This RN notified the physician, orders were given. Glucagon administered. Blood glucose rechecked and found to have increased to 100. The patient began to become more lucid and awake, speech became clearer. Will continue to monitor.
Final Thoughts
Writing strong patient progress notes is an essential part of being a nurse, but just like with any other nursing skill, it will take time and practice to get good at writing them. Do your best to be clear and concise and include all of the pertinent information when writing patient progress notes.

My name is Sophia. I am a Registered Nurse with experience working as a floor nurse on a Renal Care Unit and Hematology/Oncology Unit.
Further Reading

How to Practice Clinical Skills at Home
The Hardest Class in Nursing School

Writing Notes for Studying in Nursing School
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
User Reviews
Get premium to test your knowledge.
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.
Unlocking Client Progress: The Essential Guide to Therapy Progress Notes
The importance of therapy progress notes.
Therapy progress notes play a vital role in the therapeutic process, providing a comprehensive record of a client’s journey. These notes serve as a valuable resource for therapists, coaches, and practitioners to track and evaluate progress, ensure continuity of care, and enhance treatment outcomes.
What Are Therapy Progress Notes?
Therapy progress notes are written documents that capture essential information about each therapy session. They serve as a record of the client’s progress, interventions used, treatment goals, and any observations made during the session. These notes are typically written by the therapist or practitioner and are considered an integral part of the therapy documentation process.
Why Are Therapy Progress Notes Important?
Therapy progress notes are of utmost importance for several reasons:
- Continuity of Care : Progress notes facilitate continuity of care by providing a detailed account of each session. They allow therapists to track the client’s progress over time, identify patterns or trends, and make informed treatment decisions. In the event of a transition between therapists or when collaborating with other healthcare providers, progress notes ensure that everyone involved is informed about the client’s treatment.
- Evaluation and Assessment : Progress notes enable therapists to assess the effectiveness of their interventions and treatment plans. By documenting the client’s progress, therapists can evaluate the impact of different techniques, adjust strategies as needed, and tailor the therapy to meet the client’s evolving needs.
- Legal and Ethical Compliance : Therapy progress notes are essential for legal and ethical compliance. They serve as a record of the therapist’s adherence to professional standards, documenting the scope of therapy, interventions used, and the client’s responses. Progress notes also protect both the therapist and the client by providing a legal record of the treatment provided.
- Communication and Collaboration : Progress notes facilitate communication and collaboration between therapists and other professionals involved in the client’s care. These notes provide a concise summary of the client’s treatment history, allowing for effective communication and seamless collaboration across healthcare settings.
To ensure effective therapy progress note documentation, it is important to follow best practices and maintain a systematic approach. This includes using clear and objective language, maintaining client confidentiality, including relevant details, and organizing notes in a consistent and accessible manner. For more information on best practices and tips for writing therapy progress notes, check out our article on therapy documentation .
By recognizing the importance of therapy progress notes and committing to thorough and accurate documentation, therapists and practitioners can unlock valuable insights, enhance client progress, and provide high-quality care.
Components of Effective Therapy Progress Notes
When it comes to documenting therapy sessions, effective therapy progress notes are essential for maintaining accurate records and tracking client progress. These notes serve as a valuable resource for therapists, coaches, and practitioners to reference during treatment and collaborate with other healthcare professionals. The key components of effective therapy progress notes include:
Client Information
Begin each therapy progress note by including relevant client information . This may include the client’s name, age, gender, contact information, and any other details necessary for identification. By providing this information at the start of each note, you ensure clarity and accuracy in your documentation.
Session Details and Observations
Next, document session details and observations . Include the date, time, and duration of the session. Note any significant observations during the session, such as the client’s mood, behavior, or any notable incidents that occurred. This section helps create a comprehensive record of each therapy session and provides valuable context for future reference.
Treatment Plan and Goals
Outline the treatment plan and goals that have been established for the client. This includes the therapeutic approaches, techniques, and interventions that are being used to address the client’s concerns. Clearly define the goals the client is working towards and outline the strategies being employed to achieve those goals. This section helps track progress and ensures that therapy sessions remain focused and purposeful.
Interventions and Techniques Used
Document the interventions and techniques employed during the session. This may include specific therapeutic techniques, exercises, or activities that were utilized to help the client work through their challenges. By noting the interventions and techniques used, you create a comprehensive record of the strategies employed and can refer back to them in future sessions or when collaborating with other professionals.
Progress and Outcomes
Record client progress and outcomes in each therapy progress note. This section highlights the client’s growth, achievements, and challenges faced during the treatment process. It is important to document both positive and negative outcomes to accurately reflect the client’s journey. Utilize clear and objective language to describe the progress made and any setbacks encountered.
Future Recommendations
End each therapy progress note with future recommendations for the client’s treatment. This may include suggestions for further interventions, strategies to address specific challenges, or recommendations for additional support or resources. By providing future recommendations, you ensure continuity of care and support the client’s ongoing progress.
By including these key components in your therapy progress notes, you create a comprehensive and useful record of each client’s journey. Remember to maintain client confidentiality throughout the documentation process and ensure that your notes are clear, objective, and organized. For more information on therapy progress notes and best practices for documentation, check out our article on therapy notes .
Best Practices for Writing Therapy Progress Notes
Writing effective and comprehensive therapy progress notes is essential for maintaining accurate records of client sessions. Here are some best practices to keep in mind when documenting therapy progress notes:
Use Clear and Objective Language
When writing therapy progress notes, it is important to use clear and objective language. Avoid subjective interpretations or judgments, and instead focus on describing the client’s behavior, responses, and progress in an unbiased manner. Using precise and specific language helps ensure that the notes accurately reflect the client’s experiences and progress.
Maintain Client Confidentiality
Maintaining client confidentiality is of utmost importance when writing therapy progress notes. Ensure that you are following all legal and ethical guidelines regarding client privacy and confidentiality. Avoid using any personally identifiable information in the notes, and consider using client initials or a unique identifier instead. For more information on maintaining client confidentiality, refer to our article on therapy note confidentiality .
Include Relevant Details
To create comprehensive therapy progress notes, it is crucial to include relevant details about the session. Document important topics discussed, interventions used, progress made, and any challenges encountered. Include information about the client’s emotional state, their response to treatment, and any notable changes or developments. This level of detail provides a complete picture of the session and helps track the client’s progress over time.
Be Timely and Consistent
Timeliness and consistency in documenting therapy progress notes are essential. Make it a practice to write your notes immediately after each session while the details are still fresh in your mind. This ensures accuracy and prevents important information from being forgotten. Consistently maintaining progress notes also helps track the client’s journey effectively and allows for meaningful review and analysis.
Keep Notes Organized and Accessible
Keeping therapy progress notes organized and easily accessible is crucial for efficient record-keeping. Use a structured format or template to ensure consistency and ease of retrieval. Consider using therapy note software or electronic platforms to store and organize your notes securely. This not only streamlines the documentation process but also provides a secure and centralized location for all your therapy notes. For more information on therapy note organization, refer to our article on therapy note organization .
By following these best practices, therapists can ensure that their therapy progress notes are thorough, accurate, and compliant with ethical and legal standards. Effective progress note documentation plays a vital role in tracking client progress, informing treatment decisions, and facilitating collaboration with other healthcare professionals.
Tips for Efficient and Effective Progress Note Documentation
To ensure efficient and effective progress note documentation, therapists can follow these essential tips:
Develop a Note-Taking System
Developing a personal note-taking system can greatly enhance your efficiency and organization when documenting progress notes. Create a template or structure that works best for you, allowing for a systematic approach to recording important information. Consider using electronic therapy note software to streamline the process and improve accessibility. For more information on therapy note systems, check out our article on therapy note systems .
Simplify Your Note-Taking Process
Simplify your note-taking process by using clear and concise language. Avoid unnecessary jargon or complex terminology that may hinder readability. Focus on capturing the essential details of the session, such as key interventions, client responses, and progress towards treatment goals. For additional guidance, explore our article on therapy note abbreviations to help streamline your documentation.
Prioritize Key Information
When documenting progress notes, prioritize key information that is relevant to the client’s treatment and progress. Include vital session details, interventions used, client responses, and any notable changes or outcomes. By focusing on the most critical aspects, you can ensure the note remains concise and informative.
Use Templates or Forms
Utilize therapy note templates or forms to maintain consistency and structure in your progress notes. Templates can help guide your documentation process, ensuring that you capture all the necessary information in a standardized format. These templates can be customized to suit your specific needs and the requirements of your practice. Check out our article on therapy note templates for more information.
Review and Reflect on Your Notes
Regularly review and reflect on your progress notes to assess the effectiveness of your interventions and treatment approach. This process allows you to evaluate the progress made by the client and make any necessary adjustments to the treatment plan. By reviewing your notes, you can identify patterns, strengths, and areas for improvement in your therapeutic work. For additional insights, explore our articles on therapy note review , therapy note assessment , and therapy note evaluation .
By implementing these tips, therapists can optimize their progress note documentation process, ensuring efficiency, accuracy, and enhanced client care. Remember to always prioritize client confidentiality and adhere to professional and legal guidelines when documenting progress notes.

Download free guide (PDF)
Discover how to engage your clients on autopilot while radically scaling your coaching practice.
Coach, This Changes Everything (Free PDF)
- Search Menu
- Sign in through your institution
- Advance Articles
- Editors Choice
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- Author Resources
- Read & Publish
- Reasons to Publish With Us
- About Postgraduate Medical Journal
- About the Fellowship of Postgraduate Medicine
- Editorial Board
- Advertising & Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- Introduction
- Conclusions
- Acknowledgements
- Contributors
- Competing interests
- Provenance and peer review
- Supplemental material
- Ethics statements
- < Previous
Your note, your way: how to write an inpatient progress note accurately and efficiently as an intern
- Article contents
- Figures & tables
- Supplementary Data
Miao Wei, Efrain Salgado, Christine E Girard, Jonathan D Santoro, Natasha Lepore, Your note, your way: how to write an inpatient progress note accurately and efficiently as an intern, Postgraduate Medical Journal , Volume 99, Issue 1171, May 2023, Pages 492–497, https://doi.org/10.1136/postgradmedj-2022-141834
- Permissions Icon Permissions
A physician’s progress note is an essential piece of documentation regarding key events and the daily status of patients during their hospital stay. It serves not only as a communication tool between care team members, but also chronicles clinical status and pertinent updates to their medical care. Despite the importance of these documents, little literature exists on how to help residents to improve the quality of their daily progress notes. A narrative literature review of English language literature was performed and summated to provide recommendations on how to write an inpatient progress note more accurately and efficiently. In addition, the authors will also introduce a method to build a personal template with the goal of extracting relevant data automatically to reduce clicks for an inpatient progress note in the electronic medical record system.

Email alerts
Citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1469-0756
- Print ISSN 0032-5473
- Copyright © 2024 Fellowship of Postgraduate Medicine
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
15 Actionable Tips to Write Professional Progress Notes (2024)

By Katherine Ellison on Apr 04, 2024.
Fact Checked by Nate Lacson.

How to write a good progress note
In clinical documentation, the cornerstone is often the progress note . These brief yet comprehensive records encapsulate a client's behavior journey, offering key details and objective data that shape the care narrative. But how does one write a progress note that captures the essence of a client's journey and adheres to best practices in healthcare documentation?
An effective progress note begins with understanding the balance between subjective opinion and objective observation. While the former offers valuable insights, anchoring observations in concrete data and body language cues is crucial. This ensures that the note remains a reliable record of the client's progress, free from bias or interpretation.
A well-structured progress note should include relevant information that aligns with the clinical progress notes template . This ensures consistency and provides a comprehensive overview for fellow healthcare providers. Whether it's a daily progress note template or one tailored for specific settings like aged care, adherence to these templates streamlines the documentation process while ensuring all pertinent details are captured.
In the following sections, we'll delve deeper into the nuances of progress note writing, offering practical tips and insights to help you navigate this essential aspect of clinical practice. From understanding the anatomy of a progress note to mastering the art of concise yet informative documentation, this guide will equip you with the tools needed to write progress notes that genuinely make a difference.
Why are progress notes so important?
In the fast-paced world of healthcare, progress notes stand as indispensable pillars, serving multiple crucial functions.
- Legal documents: First and foremost, progress notes serve as legal documents, meticulously documenting the patient's journey and the therapeutic interventions provided. These notes, often HIPAA Compliant , ensure compliance with legal standards and safeguard both patients and practitioners in case of disputes or legal proceedings.
- Means of communication: Furthermore, progress notes are vital for communication among healthcare professionals. They provide a comprehensive overview of the patient's status, treatment plan, and response to interventions. This fosters seamless collaboration and ensures continuity of care, particularly in settings involving multiple clinicians.
- A contract between clients and clinicians: Moreover, progress notes are a contract between clients and clinicians, reflecting the agreed-upon treatment goals and strategies. Documenting in-session interventions and cognitive restructuring techniques demonstrates the therapist's commitment to the client's well-being and provides a roadmap for further exploration in subsequent sessions.
In essence, progress notes serve as electronic footprints of the therapeutic journey, capturing the nuances of each session while upholding the highest standards of professionalism and accountability.
What format do I use?
Adopting a structured format for progress notes enhances communication, supports HIPAA Compliant documentation, and ensures consistency in clinical practice. Here are the common formats for writing progress notes:
SOAP format
The SOAP (Subjective, Objective, Assessment, Plan) format is a widely used framework in healthcare documentation. It allows for a systematic approach to recording patient information. The Subjective section captures the patient's self-reported symptoms and concerns. Objective data, such as vital signs or observations, is documented in the Objective section. The Assessment section contains the clinician's evaluation and diagnosis, while the Plan outlines the proposed interventions and follow-up steps.
The DAP (Data, Assessment, Plan) format is another structured approach to progress notes. Data encompasses subjective and objective information gathered during the session in this format. Assessment involves the clinician's data analysis and diagnosis or treatment plan formulation. The Plan outlines specific interventions or actions to address the patient's needs.
BIRP (Behavior, Intervention, Response, Plan) notes are commonly used in mental health settings. They focus on documenting observable behaviors, interventions employed by the clinician, the patient's response to those interventions, and plans. This format emphasizes the therapeutic process and facilitates continuity of care by highlighting effective strategies and areas for further exploration.
SIRP format
SIRP (Subjective, Intervention, Response, Plan) notes follow a similar structure to BIRP notes but emphasize the patient's subjective experience more. This format encourages clinicians to explore clients' thoughts, feelings, and perceptions, providing valuable insights into their mental health and well-being.
Essential components of a good progress note
In mental health, crafting a thorough and insightful progress note is paramount to effective treatment and continuity of care. Here are the essential components that every progress note should encompass:
- Subjective and objective sections : A well-rounded soap note begins with a clear delineation between subjective information provided by the client and objective observations made by the mental health professional. This distinction ensures a holistic understanding of the client's experience.
- Mental status exam : Including a mental status exam provides an objective assessment of the client's cognitive, emotional, and behavioral functioning during the session. This helps track changes over time and informs treatment planning.
- Treatment goals : Clearly articulated treatment goals guide the therapeutic process and serve as benchmarks for assessing client progress. These goals should be specific, measurable, achievable, relevant, and time-bound (SMART).
- Treatment plan : The progress note should outline the treatment plan, detailing the therapeutic interventions employed to address the client's concerns. This may include psychotherapy techniques, medication management, or referral to other healthcare professionals.
- Client progress : Documenting the client's progress towards treatment goals provides valuable feedback on the effectiveness of interventions and informs adjustments to the treatment plan as needed.
- Client's response : Recording the client's response to interventions and therapeutic techniques allows for ongoing evaluation of treatment efficacy and helps tailor future sessions to meet the client's needs.
- Important details : Including relevant information such as changes in symptoms, significant life events, or insights gained during the session enriches the progress note and provides context for understanding the client's progress.
- Safety plan : In cases of safety concerns, a safety plan should be documented in the progress note to mitigate risk and ensure the client's well-being.
- Next session plans : Anticipating the focus of the next session and outlining any homework assignments or follow-up tasks fosters continuity of care and client engagement.
- Documentation of telehealth sessions : For telehealth sessions, it's important to note the mode of communication used, any technical issues encountered, and the client's comfort level with the format.
By incorporating these essential components into therapy progress notes , mental health professionals can create comprehensive and insightful records that support effective treatment, collaboration with other professionals, and communication with insurance companies or professional organizations.
15 Actionable Tips to Write Professional Progress Notes
These tips are the best guides on how to write a progress note. Each tip will help improve comprehensive progress notes that specify all the sections needed for clinical documentation:
1. Use clear and concise language
When writing progress notes, prioritize clarity and brevity. Use language that is easily understood by fellow healthcare professionals and avoid unnecessary jargon or technical terms.
2. Follow a structured format
To ensure consistency and organization in your progress notes, adhere to a standardized format such as SOAP notes (Subjective, Objective, Assessment, Plan) or DAP notes (Data, Assessment, Plan).
3. Include objective observations
Incorporate objective observations of the client's behavior, demeanor, and physical appearance. This adds depth to your notes and provides valuable context for understanding the client's progress.
4. Document treatment methods and modalities
Detail the specific treatment methods and modalities utilized during the therapy session. This provides a comprehensive overview of the client's treatment plan and progress.
5. Assess safety and risk
Conduct a thorough safety assessment and document any safety concerns or risk factors. This ensures the client's well-being and supports informed decision-making regarding their care.
6. Focus on critical information
Prioritize the essential inclusion of information relevant to the client's treatment and progress. This may include changes in symptoms, responses to interventions, or significant developments since the previous session.
7. Review and reference previous sessions
Referencing previous progress notes provides continuity of care and allows for tracking of the client's progress over time. Reviewing past sessions ensures that treatment plans are informed by the client's history and ongoing needs.
8. Incorporate coping skills and relaxation techniques
Document the client's utilization of coping skills and relaxation techniques during the session. This highlights their ability to manage stressors and contributes to developing effective coping strategies.
9. Avoid personal opinion
Maintain objectivity in your progress notes by refraining from including personal opinions or judgments. Focus on factual observations and professional assessments to ensure accuracy and impartiality.
10. Ensure compliance with insurance requirements
Be mindful of insurance company guidelines and requirements when documenting progress notes. Accurate and detailed documentation is essential for reimbursement and legal purposes.
11. Utilize electronic notes efficiently
Using electronic notes, take advantage of features such as templates and autofill to streamline the documentation process. This saves time and ensures consistency in formatting.
12. Collaborate with colleagues
Collaborate with other healthcare professionals involved in the client's care to ensure comprehensive documentation and coordination of treatment efforts.
13. Tailor notes to the therapy session
Customize progress notes to reflect the content and focus of the therapy session. This ensures that notes accurately capture the client's experience and progress towards treatment goals.
14. Conduct a physical exam if necessary
Incorporate relevant findings from a physical exam if conducted during the therapy session. This provides additional insight into the client's health status and informs treatment planning.
15. Continuously update the client's treatment plan
Regularly review and update the patient's treatment plan based on their progress and evolving needs. This ensures that therapy goals remain relevant and achievable throughout treatment.
Good vs. bad progress notes
Crafting effective progress notes is not just a routine task in healthcare; it's critical to providing quality patient care and maintaining professional integrity. Here's a profound comparison between good and bad progress notes:
Good progress notes
In good progress notes, each entry reflects a commitment to accuracy, collaboration, and adherence to professional standards. Here are some examples:
- Objective observations: "The client arrived punctually, exhibiting a relaxed demeanor and actively engaged in therapeutic dialogue."
In a good progress note, objective observations are specific, detailed, and relevant to the client's condition. This helps paint a clear picture of the client's presentation and behavior during the session, aiding in accurate assessment and treatment planning.
- Clear treatment plan: "Utilized evidence-based cognitive-behavioral therapy techniques to address specific anxiety symptoms identified in collaboration with the client."
A good progress note includes a clearly defined treatment plan that outlines the interventions implemented during the session. This demonstrates a proactive approach to addressing the client's needs and ensures transparency in the therapeutic process.
- Assessment of progress: "Noted significant improvement in the client's ability to implement coping mechanisms, resulting in reduced anxiety levels compared to the previous session."
It should assess the client's progress objectively and quantifiably. By noting specific improvements and comparing them to previous sessions, it provides evidence of the interventions' effectiveness and helps guide future treatment decisions.
- Collaborative language: "In consultation with the client, agreed upon and implemented adjustments to the treatment plan to enhance efficacy and meet evolving therapeutic goals."
Language in the good progress note is collaborative, indicating active involvement and agreement between the client and the healthcare provider. This fosters a therapeutic alliance and empowers the client in their treatment journey.
- Compliance with guidelines: "This progress note adheres meticulously to SOAP format, ensuring comprehensive documentation consistent with professional standards."
The good progress note follows professional documentation standards, such as the SOAP format. This ensures consistency, clarity, and completeness in the documentation, facilitating communication and continuity of care among healthcare providers.
Bad progress notes
Bad progress notes lack specificity, fail to outline a comprehensive treatment plan, omit critical progress assessments, use non-collaborative language, and disregard formatting guidelines. Here are things you should avoid:
- Vague observations: "Client's demeanor was normal."
Observations lacking specificity and detail make assessing the client's condition and progress challenging. Vague observations undermine the credibility of the documentation and may lead to misinterpretation or oversight of crucial clinical information.
- Lack of treatment plan: "Discussed various issues during the session."
Without a clear treatment plan, the bad progress note fails to provide insight into the therapeutic interventions implemented during the session. This hinders continuity of care and leaves the client and other healthcare providers uninformed about the direction of treatment.
- No assessment of progress: "Client talked about things."
Without evidence of progress, it's challenging to evaluate the client's response to treatment and make informed decisions about their care.
- Non-collaborative language: "Client needs to improve."
Directive and non-collaborative language suggest a lack of client involvement in the treatment process. This undermines the therapeutic relationship and may contribute to feelings of disempowerment or alienation on the part of the client.
- Non-compliance with guidelines: "Progress note lacks detail and structure, making it challenging to ascertain the client's progress."
Failure to adhere to professional documentation standards, lacking structure, detail, and organization. This compromises the clarity and accuracy of the documentation, potentially leading to confusion or errors in clinical decision-making.
Common terminologies and interventions used in progress notes
In progress notes, several common terminologies and interventions are frequently utilized to effectively communicate a client's condition, progress, and treatment plan. Here are some of the critical terms and interventions commonly found in progress notes:
- Therapy techniques: Utilizing evidence-based therapies like Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT) to address symptoms and promote coping skills.
- Medication management: Monitoring medication adherence, dosage adjustments, and side effects to ensure optimal treatment outcomes.
- Behavioral interventions: Implementing strategies to modify maladaptive behaviors and reinforce positive ones, promoting healthier habits.
- Skill building: Providing guidance and education to help clients develop practical skills for managing stress, communication, problem-solving, and emotional regulation.
- Supportive counseling: Offering empathetic listening, validation of experiences, and emotional support to help clients navigate challenges and promote well-being.
- Psychoeducation: Educating clients about their diagnosis, treatment options, and self-care strategies to enhance understanding and empower active participation in treatment.
- Referrals: Facilitating connections to other healthcare professionals or community resources for specialized services or additional support beyond the scope of current treatment.
- Crisis intervention: Providing immediate support and safety planning in acute distress or crisis, ensuring the client's well-being and access to appropriate care.
- Collaboration: Working closely with other healthcare providers, such as psychiatrists, primary care physicians, or occupational therapists, to coordinate care and ensure holistic support for the client.
- Goal setting: Collaboratively setting realistic and measurable treatment goals with the client, regularly monitoring progress, and adjusting interventions to achieve desired outcomes.
Other common words:
- Subjective complaints
- Objective findings
- Treatment plan
- Interventions
- Client progress
- Follow-up plan
- Goal setting
- Therapeutic techniques
- Coping strategies
- Symptom management
- Client engagement
Psychoeducation
- Symptom severity
Key takeaways
Building a solid foundation for effective client care requires a multifaceted approach. Here are key takeaways to consider:
- Holistic interventions: Explore various therapies, medication management, and other strategies to comprehensively address each client's unique needs.
- Client-centered care: Prioritize collaborative goal setting and tailor interventions to align with each client's specific situation and desired outcomes.
- Detailed documentation: Maintain accurate and thorough progress notes on interventions delivered to ensure clear communication and continuity of care.
- Interdisciplinary collaboration: Recognize the value of working alongside other healthcare professionals and make referrals when necessary to provide holistic support for your clients' multifaceted needs.
- Continuous improvement: Regularly assess client progress, adjust interventions as needed, and adhere to ethical and regulatory standards to optimize client outcomes and deliver the highest quality care.
Incorporating these fundamental principles into your practice ensures that your clients receive comprehensive, effective, and ethical care.
.png)
Related Articles
Types of Therapy Interfering Behaviors & How to Address Them
Learn how to effectively address various therapy-interfering behaviors in healthcare settings to optimize patient care and treatment outcomes

Counseling Microskills: Types, Benefits, and Use Cases
Unlock deeper client connections! Counseling microskills are powerful tools for therapists. Learn the types, benefits & how to use them in different therapies.

AI Speech Therapy: Addressing Communicative and Cognitive Impairments
Discover how AI speech therapy transforms the treatment of communicative and cognitive impairments, enhancing patient outcomes.

Physical Therapy Burnout: Causes and Tips for Prevention
Learn the causes of physical therapy burnout and learn effective tips for prevention to maintain a healthy, productive work environment.
Ethical Dilemmas in Counseling
Explore vital ethical dilemmas in counseling and learn how Carepatron's software ensures compliance and enhances decision-making in our comprehensive guide.
Clinical Words to Use in Progress Notes
Explore a comprehensive guide to expand your clinical vocabulary and create effective progress notes.

Artificial Intelligence in Physical Therapy
Explore how AI transforms physical therapy with enhanced diagnostics, personalized treatments, and innovative technologies for better patient outcomes.
When to Stop Therapy
Explore key indicators for healthcare professionals on when to conclude therapy, ensuring effective patient management and therapeutic outcomes.
Empower patients with knowledge! Carepatron's guide explores psychoeducation in therapy & its benefits for mental health professionals.
Bowen Family Therapy
Explore Bowen Family Therapy with Carepatron! Our secure platform & features empower therapists to guide families & promote emotional well-being. Read here.
AI in Psychiatry
Explore the role of AI in psychiatry and its impact on diagnosing, treating, and managing mental health issues effectively. Learn more at Carepatron.
AI and Psychology
Explore how to maximize the power of AI in clinical practice while remaining ethical and effective.
How to Write an Email to a Patient: Tips for Success
Learn essential tips on how to craft effective patient emails that enhance communication and trust in healthcare. Try out our email templates here.

Physical Therapy Billing Units
Discover the importance of Physical Therapy Billing Units for successful healthcare reimbursement. Learn more now!

DBT Journal Prompts
Gain some inspiration to guide clients in practicing journaling and incorporating principles of DBT into their daily lives.
Art Therapy Group Activities
Explore art therapy & its benefits for healthcare professionals. Learn how Carepatron software empowers art therapists.
Physical Therapy CPT Codes
Learn about Physical Therapy CPT codes, including their significance, purpose, and utilization in inpatient billing.

When Can a Therapist Break Confidentiality?
Discover the crucial scenarios in which therapists may need to break confidentiality to ensure client safety and well-being. Learn more here.
Join 10,000+ teams using Carepatron to be more productive
01.06 How to Write A Nursing Progress Note
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
- Assessments
- Care & Treatments
- Chronological report
- Includes responses, changes and issues
- Legal evidence
- Reimbursement
- Quality assurance
- Physical assessment
- Patient interview
- NANDA nursing diagnosis
- Prioritize care
- Set goals/outcomes
- Interventions
- Determine outcomes
- Determine effectiveness of interventions
- Make changes as needed
- Patient condition
- Diagnostic procedures
- Other interventions
- Patient response to interventions
- Care & teaching provided
- Complaints/other issues during care
- Separate notes for each team member
- Most popular
- What the patient says
- Why is the patient here?
- Onset of symptoms
- Location of symptoms
- Duration of symptoms
- Character of symptoms
- What relieves or makes it worse?
- Does it stay in one place or move?
- Is it worse at a certain time of day?
- Scale of 1-10
- Things we observe
- Uses nursing diagnosis
- Nursing diagnosis
- Care/treatment provided
- Did the intervention work?
- Highlights specific problem, condition changes, concerns or events
- Be consistent
- Never chart in advance
- Always notate date and time written
- Familiar to other medical personnel
- Approved by agency/facility
- Avoid opinion/personal feelings
- Note all communication
- Sign all notes with credentials
- Write legibly
- Use black ink
- No white out
- Sign/initial error
- Date and time with initials
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Today we’re going to be talking about how to write a nursing progress note.
In this lesson, we will cover the types of progress notes you can write, what information actually goes into a progress note, and what you absolutely must know before you begin writing one.
Let’s start by addressing what a progress note is. Nursing progress notes document our patient’s medical status. We document any assessments, care and treatments we’ve performed on our shift, and the patient’s progress and response to those actions. The goal of the progress note is to write a chronological narrative of the shift including any issues you may have come across. For instance, you can write a note after you complete your initial assessment. It may look a little something like this: (date/time: Physical assessment completed. VS WNL. Pt A&Ox3, no complaints of pain at this time. RN signature). If there’s anything abnormal about your assessment, it would go here as well along with any interventions you may have had. Remember that nursing progress notes are legal documents and can be used in court proceedings, for insurance reimbursement and for quality assurance purposes.
The nursing process is something that will never go away. It shapes the way we work as nurses! With that said, it’s important to show you how it affects the way we write our progress notes as well. So our assessment is anything we found in the physical assessment or in the patient interview. You’ll want to include that information in your note, particularly for those findings that aren’t normal. NANDA diagnoses are used dependent on your facility policy, but you may want to use it to determine what your central focus is for your patient. It will help shape your plan of care. As I’m mentioning plan, this is where we are prioritizing our care. This is why I say you can use the NANDA diagnosis. In the process of prioritizing, you should be setting goals for your patient to achieve on the short term. Maybe you want them to achieve something before the end of your shift, or before discharge. Interventions are the implement stage of the process. These are those treatments and any other care we are providing during the shift. Finally, we have the evaluate stage. This is where we are looking for the response to interventions and making changes to the plan as needed. Why did I bring this up? We all know ADPIE at this point but what you may not know is you can always refer back to it if you get stuck on what to write in your notes.
What do we put in a progress note? Remember, we are creating a narrative description of what happened with the patient during the shift. So we want to include the patient’s condition and any abnormal lab values or diagnostic results. Any tests that the patient had completed or ordered should also be included even if we don’t have the results back. Medications and treatments, as well as the patient’s response to them are very important to include. This includes any patient concerns, complaints or other issues as well as the care or any teaching we have provided during the course of the shift. We want to know if they tolerated the treatment or if a change has been made or is warranted. Were there any new med orders made? We also talk about any follow up care or consults that may be required. When you hear it in a list like this it sounds like a lot. But think about what you’re expected to do on your shift as a nurse. The most important take-away here is that you want to document the things that happened, because if you don’t, it didn’t.
There’s a lot of different ways to write a progress note, however, we will discuss the ones you may see most frequently. These are the SOAP note, the PIE note, and the DAR note. Let’s explore each of these individually.
SOAP notes are the most popular progress note for nurses. They fall into the category of problem oriented notes, which means we are focused on the reason for seeing the patient. It lays out exactly what we need to include. Subjective information is what comes from the patient. We take this information in the History & Physical most often and it includes not only why they are here with us, but also the details of their symptoms. Objective information is what we observe, usually from the physical assessment we perform. Bear in mind there can be times where S and O don’t necessarily add up, but make note of it all anyway. Then we have the assessment and the plan. Again, we take that from the nursing process. Find the problem and make a plan to fix it. So let’s say we have a patient who just had abdominal surgery 2 days ago. The SOAP note may look something like this: S – Pt reports pain and itching around surgical site. Pt states the pain is 4/10 and throbbing. O – Pt A&Ox3, calm and cooperative. VS WNL. No edema to extremities. Lungs clear. OOB to chair with assistance. Positive bowel sounds in all 4 quadrants. Redness and swelling around surgical site. Tenderness noted in LUQ. No drainage or bleeding present. Dressing CDI. Pain medication given per order for mild to moderate pain. Call light in reach. A – Pt pain level decreased to 2/10 after pain medication. Pt has some SOB after ambulation to chair and c/o mild fatigue. P – Will continue to assist with activity as tolerated. Continue pain medications, skin care and dressing changes as ordered. Assess surgical site throughout shift. Report any other issues to physician.
PIE notes are another problem oriented note, but these rely on the use of the nursing diagnosis to identify and document the problem, discuss the care or treatment provided, and then whether or not the intervention actually worked. PIE notes are a little more clear cut and to the point, but don’t allow for as much detail as SOAP notes. Let’s use the same patient we just discussed. The PIE note may look like this: P – Acute pain r/t surgery as evidenced by reports of pain 4/10. I – Administered pain medication as ordered for mild to moderate pain. Assistance provided for OOB activity. Call light placed in reach. E – Pain decreased to 2/10. Pt uses call light when in need of assistance. We said the same thing as we did in the SOAP note, just more concise and we focused on a central issue, in this case, the patient’s pain. If there are other issues, you can write on those as well.
DAR notes are in a different category than SOAP and PIE notes. These notes are called focus notes, which highlight a specific problem, condition changes, concerns or events. When you think of it that way, it’s easy to determine what each piece is for, but I’ll explain anyway. Our data comes from the assessment findings. So this is likely both subjective and objective information if you think of it in terms of SOAP notes. Action and response are exactly that. What did we do to address the problem we’ve identified, and did it work. Let’s revisit our post op patient again. The DAR note may be this: D – Pt is 2 days post op abdominal surgery. Pt c/o pain 4/10 around surgical site. Some redness, swelling and tenderness noted at the site. A – Tylenol 325mg 2 tabs PO administered as ordered for mild to moderate pain. R – Pt reports pain decreased to 2/10 after medication administration.
So we’ve arrived at the rules for writing progress notes. Remember, we said earlier that progress notes are a legal document. If you are ever called to testify in court, your notes can be used as evidence so you want to be sure that you are consistent, concise and timely with your notes. Never write notes in advance. Anything can happen and more importantly, if you’re writing ahead of time, do you really have true knowledge of the situation? We love to use short-hand in the medical field. It’s okay to do this, just be mindful that the abbreviations you use are standard and approved before doing so. Make sure that what you are using is familiar to everyone reading. No one wants to have to track you down to clarify what you meant. Include any and all communication you’ve had regarding your patient and ensure that you use quotations so it is clear that what you are writing was a statement made by the person you are referring to. This includes family members, visitors, and medical personnel. This is important, because once it’s written down, it can’t be denied or changed. Above all else, you earned your credentials. You worked hard for them. So make sure you are using them when you sign off on your notes. It’s a standard you will get used to.
A final note for those who still create hand-written notes. Make sure you write legibly in black ink only. This is a legal requirement, I’ve always been told. Also correcting errors is a really big thing for legal reasons. We all make mistakes and it’s okay to as long as you find it and correct it. When you do make an error, know that white out is not permitted. You should put one line through the error, and initial with date and time.
Let’s talk some key points. Remember progress notes are legal documents. They can be used in court or for insurance to pay your facility. Be mindful of what you write. If you ever get stuck on what to include in your progress notes, it’s okay. You can always come back home to the nursing process! A goal in writing progress notes is to stay objective! It is not the place to air your grievances and should stay judgment free. Document ONLY the facts! Most important, always remember, If it’s not documented, it didn’t happen. Make sure you hit everything you want the reader to know.
That’s all! We love you guys! Go out and be your best self today! And as always, Happy Nursing!
View the FULL Transcript
Documentation.

Documentation can be hard! This course will take you through the daily charting and documentation that is necessary for your patients. In this course, you will also understand documenting phone calls, the legalities of charting, and how the electronic medical record (EMR) works.
0 – Documentation Course Introduction
1 – documentation basics for the new nurse, 2 – legal responsibilities.
DARP Note Template
DARP notes are a widely used method for documenting therapy sessions and clinical progress notes. Similar to the popular SOAP notes format , DARP (sometimes DAP) stands for:
Our template is designed to assist you in writing progress notes, with fillable fields for each section of a DARP note, ensuring quick and efficient documentation.
Download this free PDF for easy access whenever you need. If you're unsure about using DARP notes in your practice or if you're looking for examples to guide you, check out our article all about DARP notes for inspiration and best practices.
Published on
Wednesday, May 22, 2024
Professional Toolbox
We offer easy and centralized access to various documents, tools and resources for both work and intervention.

Agreement for the Transfer or Temporary Custody of Professional Records

Authorization for Collection and Use of Personal Information

Authorisation to Disclose Information - 15-Day Delay
Focus on the essentials: your customers.

Our clinical notes take a lot of time to write. Is it time well spent?
SARINA SCHRAGER, MD, MS
Fam Pract Manag. 2022;29(4):3-4
Clinical office notes communicate what happens within the examination room. The progress note is a tool for clinicians to convey information to each other to optimize the care of our patients. I read notes from specialists to help my patients navigate their care. These notes explain to me why a certain medication was prescribed or a specific test was ordered during the visit. I can also determine whether the patient understood what the consultant or one of my partners told them in another office visit. I rely on my own notes to remind myself what I was thinking during the patient's previous visit, especially if it was a long time ago. Why did I order that test? What was I thinking when I made that diagnosis? A well-written note is essential to patient-centered care.
It is no surprise to any clinician that these notes take a lot of time to write. A recent study showed that the average physician spends a mean of 1.77 hours daily on documentation outside of normal office hours. 1 EHRs have not improved the efficiency of writing notes; they have actually made completing documentation more cumbersome. In their classic 2017 paper, Arndt and colleagues described the burden of EHR documentation on primary care clinicians. 2 In this study, for each hour of direct patient care, clinicians spent two hours interacting with the EHR. Excess documentation for billing purposes only increases the administrative burden.
Many of us worked during a time when handwritten notes were the norm. They were shorter and did not include problem lists, medication lists, or extensive reviews of systems. The documentation was limited to the story (history or subjective), exam (objective), assessment, and plan. Note templates in the EHR, on the other hand, often include extensive supplemental data, much of which exists elsewhere in the record.
Recent studies have evaluated how notes are read. A 2015 cognitive task analysis of 16 primary care physicians found that the assessment and plan sections of office progress notes were reviewed first and were rated as the most important components of the note. 3 Some organizations have recommended a change from the traditional SOAP notes (subjective, objective, assessment, and plan) to APSO notes (assessment, plan, subjective, and objective), which may save clinicians time and improve the usability of the EHR. 4 Preliminary data demonstrates clinician satisfaction with the APSO note format in both outpatient and inpatient arenas. 5 , 6
OpenNotes is an initiative in the recently implemented 21st Century Cures Act. It provides patients with access to all notes written by their physicians, other medical providers, and care teams. The ability for patients to access notes may be beneficial. With more complete information, patients can engage more fully in their care. Initial data suggests that most patients find it helpful to read their notes. 7 , 8 On the other hand, a small study documented that more than 10% of patients were offended or felt judged by something the clinician wrote. 9 The use of stigmatizing and judgmental language in notes is not unusual 10 and may be more common in notes written about people of color. 11 One study looking at history and physical notes from an emergency department found that negative language was included in charts of Black patients 2.55 times as much as White patients. 11
As note writing in medicine evolves, we must continue to focus on tools that enhance its efficiency in primary care. The 2021 Medicare guidelines relieved clinicians of some of the burden of note writing by decreasing billing requirements. We need to continue looking for ways to reduce the amount of time clinicians spend writing notes, while at the same time paying attention to implicit bias in our notes.

Gaffney A, Woolhandler S, Cai C, et al. Medical documentation burden among U.S. office-based physicians in 2019: a national study. JAMA Intern Med . 2022;182(5):564-566.
Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med . 2017;15(5):419-426.
Koopman RJ, Steege LMB, Moore JL, et al. Physician information needs and electronic health records (EHRs): time to reengineer the clinic note. J Am Board Fam Med . 2015;28(3):316-323.
Belden JL, Koopman RJ, Patil SJ, Lowrance NJ, Petroski GF, Smith JB. Dynamic electronic health record note prototype: seeing more by showing less. J Am Board Fam Med . 2017;30(6):691-700.
Lin CT, McKenzie M, Pell J, Caplan L. Health care provider satisfaction with a new electronic progress note format: SOAP vs. APSO format. JAMA Intern Med . 2013;173(2):160-162.
Sieja A, Pell J, Markley K, Johnston C, Peskind R, Lin CT. Successful implementation of APSO notes across a major health system. Am J Accountable Care . 2017;5(1):29-34.
Walker J, Leveille S, Bell S, et al. OpenNotes after seven years: patient experiences with ongoing access to their clinicians' outpatient visit notes. J Med Internet Res . 2019;21(5):e13876. 2020;22(4):e18639.
Chimowitz H, Fernandez L. Sharing visit notes: getting patients and physicians on the same page. Fam Pract Manag . 2016;23(6):10-13.
Fernandez L, Fossa A, Dong Z, et al. Words matter: what do patients find judgmental or offensive in outpatient notes?. J Gen Intern Med . 2021;36(9):2571-2578.
Park J, Saha S, Chee B, Taylor J, Beach MC. Physician use of stigmatizing language in patient medical records. JAMA Netw Open . 2021;4(7):e2117052.
Sun M, Oliwa T, Peek ME, Tung EL. Negative patient descriptors: documenting racial bias in the electronic health record. Health Aff (Millwood) . 2022;41(2):203-211.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2022 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Internet Res
- v.23(10); 2021 Oct

Writing Practices Associated With Electronic Progress Notes and the Preferences of Those Who Read Them: Descriptive Study
Thomas h payne.
1 Department of Medicine, University of Washington School of Medicine, Seattle, WA, United States
Carolyn Keller
Pallavi arora, allison brusati, jesse levin, monica salgaonkar.
2 University of Southern California, Los Angeles, CA, United States
Jennifer Zech
3 Columbia University, New York, NY, United States
A Fischer Lees
Hospital progress notes can serve as an important communication tool. However, they are criticized for their length, preserved content, and for the time physicians spend writing them.
We aimed to describe hospital progress note content, writing and reading practices, and the preferences of those who create and read them prior to the implementation of a new electronic health record system.
Using a sample of hospital progress notes from 1000 randomly selected admissions, we measured note length, similarity of content in successive daily notes for the same patient, the time notes were signed and read, and who read them. We conducted focus group sessions with note writers, readers, and clinical leaders to understand their preferences.
We analyzed 4938 inpatient progress notes from 418 authors. The average length was 886 words, and most were in the Assessment & Plan note section. A total of 29% of notes (n=1432) were signed after 4 PM. Notes signed later in the day were read less often. Notes were highly similar from one day to the next, and 26% (23/88) had clinical risk associated with the preserved content. Note content of the highest value varied according to the reader’s professional role.
Conclusions
Progress note length varied widely. Notes were often signed late in the day when they were read less often and were highly similar to the note from the previous day. Measuring note length, signing time, when and by whom notes are read, and the amount and safety of preserved content will be useful metrics for measuring how the new electronic health record system is used, and can aid improvements.
Introduction
Inpatient progress notes can serve as an important communication tool across the physician team, nurses, therapists, consultants, and the patient. Because safety problems that occur in hospitals can be traced to communication lapses [ 1 ], progress notes are vital to achieve safer care. However, some feel that few read progress notes, and that they therefore no longer serve the purpose of communication and are now primarily billing documents [ 2 ]. Many physicians feel they spend too much time writing progress notes [ 3 , 4 ] and employ methods to shorten writing time. These include copy-paste [ 5 - 8 ] and extensive templating with “note bloat,” which can introduce error [ 9 - 11 ], harm patients [ 12 ], and make it difficult for note readers to separate current from outdated content [ 13 ].
We have used our current electronic health record (EHR) system at the University of Washington (UW) Medical Center and the Harborview Medical Center for 17 years with little change in the format of the inpatient progress note used in the Medicine service. In preparation for the transition to a new inpatient EHR system, we conducted this analysis of progress notes on inpatient medical services to take stock of current practices. The purpose of this study was to describe current hospital progress note writing and reading practices, as well as the preferences of those who create progress notes and those who read them.
This work retrieved its data from the inpatient general medicine services at the UW Medical Center and the Harborview Medical Center, which are major teaching hospitals of the UW with approximately 35,000 combined admissions annually. The EHR system was installed in 2003, and the transition from paper to electronic notes occurred in 2006 using Cerner Millennium (Cerner Corp). Nearly all progress notes pertaining to these inpatient services are typed using the Clinical Notes Editor, based on templates that automatically import patient-specific data such as medication lists, vital signs, and laboratory results [ 14 ]. Daily progress notes are required by hospital bylaws and are mostly written by residents (usually interns) and attending hospitalists.
Selection of Notes
We randomly selected 1000 patient admissions to the general Medicine service of UW Medical Center and the Harborview Medical Center between July 1, 2016, and June 30, 2017. The Medicine services at both facilities share the same progress note template. We excluded patients admitted to subspecialty services with unique progress note templates (oncology, cardiology, and geriatrics). For each admission, we extracted the data for all daily progress notes as shown in Textbox 1 from the analytical data repository (Enterprise Data Warehouse, Caradigm), which contains a subset of EHR data extracted for research. Progress notes were identified by the title “Medicine - Inpt Record,” the note type used within our system for Medicine service daily progress notes. Given that this study was focused on practices around the use of progress notes by those who create and those who read them, we excluded all notes other than progress notes (admission notes, procedure notes, consult notes, interim summaries, discharge summaries, and other notes).
Metadata obtained for each progress note.
Full text of the note and other data listed were gathered for each note. Authenticators are supervising physicians whose note cosignature finalizes the note.
Metadata obtained:
- Note date and time
- Note authors and authenticators
- Note identifier
- Note action log (provided by the electronic health record system), which includes the following:
- Action (eg, perform, transcribe, modify, sign and CC/review, verify)
- Performed by (name)
- Performed date and time
- Action status
- Proxy personnel
- Requested by (name)
Note Analysis
We deidentified each note using published methods [ 15 ] and stored them securely. Using Python scripts written for this project, we determined the total number of words in each note and in each note section (Identification/Chief Concern, Interim History, etc) ( Textbox 2 ). We also determined when notes were signed; before progress notes are signed, they cannot be viewed except by the author.
Progress note sections.
Sections are automatically created using the template used to create Medicine progress notes.
HOSPITAL DAY
IDENTIFICATION/CHIEF CONCERN
INTERVAL HISTORY
INPATIENT PROBLEM LIST
SCHEDULED MEDICATIONS
PRN MEDICATIONS
PHYSICAL EXAM
ASSESSMENT & PLAN
- Fluids/electrolytes/nutrition
- Prophylaxis
- Tubes/lines
- Disposition
- Code status
ATTENDING STATEMENT
- Additional diagnoses
Copy-Paste Analysis
We identified the sequence of daily notes written for each patient during their hospital stay and then determined the percentage of text within each and in the note as a whole that overlapped with the note written on that same patient the previous day using natural language processing methods [ 16 , 17 ].
To determine the clinical implications of copy-paste, we used methods described by Hammond et al [ 18 ] to highlight shared content across progress notes from one day compared to the previous day for the same patient. We then used the same 6-point scale as in that paper to rank the clinical importance of copy-paste. Since this required time-consuming manual review by clinicians, we performed this for a subset of notes.
Measuring Note Readership
Note reading practices were analyzed by extracting a note-viewing record using auditing software (P2Sentinel, Cerner Corporation). Each time a note was viewed, the username, user role (resident physician, attending physician, registered nurse, etc), and timestamp were recorded in the auditing database. To determine views within the same hospital day—which have unique potential to communicate the patient’s current clinical state and today’s plan—we assessed note views within 12 hours after the note was signed. Usernames were used to identify members of the patient’s primary team. Views by physicians on the patient’s primary team were assumed to be related to the note writing process, and were excluded from the note-reading analysis. Statistical testing was performed using Stata/IC 13 (StataCorp LLC).
Focus Groups
To understand different perspectives on the current use of progress notes, we conducted 3 sets of focus groups: note authors (Medicine interns and hospitalists), note consumers (nurses, therapists, and consultants who view Medicine progress notes that others had written), and leaders (hospital service leaders who form documentation policies and standards). Each focus group was led by a coinvestigator who followed a script and showed PowerPoint slides of the results of the note analysis and the copy-paste analyses. The 5 focus group sessions were recorded, and transcripts were made for all but one of the focus groups.
The UW Institutional Review Board approved this work and designated it as “minimal risk.”
From 1000 randomly selected hospital admissions to the Medicine service, we obtained 4938 inpatient progress notes written by 418 authors, an average of 4.9 daily progress notes per patient admission.
The results of the note analysis are summarized in Figures 1 - -4. 4 . The average note length was 886 words (median 827), and most of the length (~500 words) was in the Assessment & Plan section, which comprised on average two-thirds of the note. There was marked variation in note length—some notes contained over 2000 words in the Assessment & Plan section alone. The Interval History and Physical Exam sections were among the shortest sections. These findings reflect the common practice of copying one day’s Assessment & Plan into the next day’s note and appending each day’s assessment to those of the previous days. (While the History and Physical sections are also frequently copied, the lack of appending new information to old information prevents these sections from lengthening over the hospital course.)

The time at which progress notes were signed by the author.

Display of note readership data for 7 notes. Each colored dot indicates who (role) read the note and when over several days. Different colors indicate different roles. Each column of dots shows the readership of one progress note. QI: quality improvement, ARNP: advanced registered nurse practitioner, PA: physician assistant, RN: registered nurse, MD: medical doctor.
Progress note authors signed their notes at various times of the day as shown in Figure 1 . A total of 29% (n=1432) of notes were signed after 4 PM, and some were signed as late as 10 PM.

Distribution of note length in words (the programming code used to calculate note length is available from the authors).
Notes had high levels of similarity to the prior day’s note on the same patient. The median note similarity was 66% using the methods described above. While note similarity was high for all author types ( Figures 5 and and6), 6 ), it was higher for trainees than attendings ( P <.001), and higher when both notes were written by the same author rather than by different authors ( P <.001) ( Figure 6 ).

Similarity by author training level. Box and whisker plots of the similarity of notes calculated using natural language processing methods [ 16 , 17 ] are shown. Box shows IQR.

Similarity by original authorship. Box and whisker plots of the similarity of notes calculated using natural language processing methods [ 16 , 17 ] are shown. Box shows IQR.
We conducted manual reviews of note pairs to assess the clinical importance of note similarity. Preserved content from one day to the next was visually highlighted, using the CopyFind program [ 18 ]. Physician reviewers then assessed the preserved content for risk using the Hammond scale [ 18 ] ( Textbox 3 ). The results showed that 26% (23/88) of the pairs were assessed to have minimal or some risk because of human copying; a second set of reviews found 17% (5/29) of the pairs had minimal or some risk in the preserved content. In this sample then, about 1 in 5 notes had clinical risk associated with preserved content, which was very likely the result of copy-paste practices. An example of copying assessed to be of minimal risk (code 4) was including the phrase “Gen Surg to take to the OR today” when this happened the day before. An example of copying regarded to be of some risk (code 5) was when the History section was completely copied from the day before, incurring a legal risk of fraud. In the Plan section of the same note was the phrase “will obtain MRI” copied forward, but the MRI (magnetic resonance imaging) was obtained the day before as evidenced by the results of the MRI appearing elsewhere in the note.
Risk scale for duplicated material appearing in notes.
The scale below is used to assess the risk associated with duplicated note text, derived from Hammond et al [ 18 ] ( Figure 7 ).

Copy-paste risk, assessed using the Hammond risk scale [ 18 ]. Colors represent judgment of risk assigned by the 2 physicians who analyzed a sample of note pairs. One physician assigned scores to 100 note pairs (blue) and one assigned scores to 25 note pairs (green).
Code risk description:
- 1 = Artifact, not misleading, no risk
- 2 = Artifact, minimally misleading, minimal risk
- 3 = Human, not misleading, no risk
- 4 = Human, minimally misleading, minimal risk
- 5 = Human, misleading, some risk
- 6 = Human, clinically misleading, major risk
Note-reading practices were analyzed on a random subset of 250 notes (limited by auditing time constraints). The 250 notes in this sample were similar to the overall progress note library: the authors who wrote them were representative of the pool of authors in the larger library, and because they were randomly sampled, other note characteristics (eg, time written, length) were similar to the overall note library. This sample had 4036 note views, an average of 16.1 views per note, which includes many types of professionals beyond bedside nurses and physicians. Figures 8 A and 8B describe note readership by note sign time. Notes signed before noon were read more than notes signed between noon and 4 PM ( P =.002), and those signed between noon and 4PM were read more than those between 4 PM and 8 PM ( P =.05), with successively fewer reads for notes signed between 4 PM and 8 PM. Analysis of note reading by role revealed that more notes were read by providers (physicians, nurse practitioners, physician assistants, medical students) when published before noon (ie, early in the day) ( P =.003). Nursing readership was not correlated with the time the notes were signed ( P =.95).

Note reads by published time. Plots show the cumulative number of all staff (A) and providers (B) who read notes as a function of the time since the note was viewable (signed).
Note Authors
We learned that note authors vary widely in how they use progress notes (ie, section of note reviewed, such as Labs, Scheduled Medications, etc), and in the purposes for which they use them, such as regarding them to be a billing document, as a “note to self” to remember important items from one day to the next, and as a communication tool to colleagues. Note authors mentioned this as one reason there is so much heterogeneity in the length and content of inpatient progress notes.
Note Consumers
Nursing and other ancillary service staff said they value medical progress notes and prefer detailed notes. They regarded them to be an important communication tool that helps them understand what is going on with patients and the plan for the day and for the hospital stay. They frequently used the progress note to assist their communication with families. They reported wanting to see more details regarding the disposition plan and preferred to have the Labs and Radiology sections deleted.
Leaders believed the collective memory in notes to be important to prevent “reinventing the wheel.” They believed that the primary focus of a note should be communication and patient safety, but that we should also make trainees aware of future billing pressures when they finish training and are able to bill. They felt, as a group, that the medication list is important to include in progress notes.
Figure 3 shows that notes are read by authorized users from a wide range of disciplines, including registered nurses, physicians, and administrators.

Length of note sections. Box and whisker plots of the number of words in each note section is shown. Box shows IQR. ID: identification.
Our analysis of a large set of randomly selected hospital progress notes found that notes were often long and highly similar to the prior day’s note. Additionally, notes that were signed later were read less frequently; about one-third were signed after 4 PM when their value as a communication tool for other providers is diminished. Given the vast quantity of physician hours spent on their creation, inpatient progress notes have been relatively neglected as an area of study. Limitations in duty hours, increased patient complexity, and decline in physician morale suggest a need to re-evaluate our note-writing practices.
We found broad variation in note-writing and reading practices. Some notes in our sample were over 2000 words (approximately half the length of this paper); this may reflect the common practice of copying one day’s assessment into the next day’s note and adding each day’s findings to those of the previous days. The progress notes often become a running summary of the hospitalization.
Our analysis showed a high degree of similarity between notes on the same patient on successive days. Though methods for measuring note content similarity vary across studies [ 19 ], it is interesting that others also noted this [ 20 , 21 ]. Note similarity could occur from either note templating or from copy-paste; we believe that the high similarity in our sample was mainly due to copy-paste, as the most heavily templated sections of our progress note (Allergies, Medications, and Labs) make up just 22% of the average note length. Our focus group with note authors provided further evidence that this was the case.
Note similarity was high across training levels, and while trainee notes had more similarity than attending notes, attending notes were still over 50% similar to the prior day’s note. Perhaps equally concerning was a high degree of similarity between notes with distinct authors. While our Medicine community sees the progress note as more of a living, communal document (where the practice of copy-paste is not viewed as flagrant plagiarism), this practice nevertheless is a clear setup for miscommunication and medical error [ 22 , 23 ]. Indeed, manual review revealed that 1 in 5 notes had clinical risk associated with preserved content, which was very likely the result of copy-paste practices. Reassuringly, this was primarily in the minimal-risk category with no examples of major human risk captured in the small sample we reviewed. This may suggest that careful use of copy-paste with a diligent review (defined as a review sufficient to assure that the note is accurate on the day it is written) of the information that is carried forward is not associated with a major risk of error.
Progress notes in our sample were read frequently by nonprimary team members. Readership of timely clinical data (within 12 hours of note signing) was highly sensitive to the time of day the note was signed, with significantly more notes read if signed before noon. This was especially true of physicians, who tend to have day schedules on the acute care services and are thus unlikely to view a note that is published late in the evening (as many notes are). Nurse views were not sensitive to note-signing time, likely reflecting the presence of night-shift nurses, who also want to use the progress note as a means to communicate the plan of care. (However, if a night-shift nurse reads a note, the content from the morning rounds is over 12 hours old.)
In the focus groups, we heard many and different reasons nurses and physicians value progress notes. Some nurses read them soon after they were created even if it was late in the day and appreciated the detail of Medicine progress notes compared with other services. For nurses, these notes served as an important communication tool to help them understand the Medicine team’s plan. Most expressed interest in more information tailored to their needs. Note authors—largely house staff and hospitalists—also valued notes, though what they valued differed by group. House staff are charged with tracking details, critical and minor, and used their notes for their “future selves”—as a way to remind them of what is to be done and for the collective memory of what has occurred. For hospitalists, there was wide variation in the attitude toward progress note writing, with some hospitalists favoring a more succinct note that concisely summarizes why the patient remains hospitalized and focuses on changes in patient status and plan for that day, while others (especially those who also worked nights) also focused on the importance of a note as a communication tool. Ultimately, the use of the note as a repository or collective memory of hospital course was a hotly contested topic among the hospitalists depending on their attitude toward and group practice with regards to interim summary writing. This suggests a need for direction from leadership regarding the use and role of medical inpatient progress notes versus interim summaries as collective memory of a patient’s hospital course.
Recent literature offers additional perspectives and hopes for progress notes. We know that attendings and house staff physicians differ in their perception of note quality but agree that communication is an important purpose for them [ 24 ]. Some senior authors advocated restoring the story to clinical notes [ 25 , 26 ]. If this is an objective, using voice to create notes could fit this into the workflow because it may be faster than typing a more narrative note. Creating a wiki-style note, broadly adopting the APSO (Assessment, Plan, Subjective, Objective) format, utilizing vendor tools to create an ongoing hospital course, or drastically shortening notes were not explored in this study but may be embraced by a segment of physicians.
These results have implications for those who develop electronic documentation systems used in EHRs. Documentation methods that facilitate the completion of notes sooner in the day may result in greater readership, fulfilling an important communication objective for electronic notes. However, the opportunity cost of earlier documentation may be diverting physician hours away from other time-sensitive tasks, such as contacting specialists or meeting with families. Permitting the simple creation of a summary of the hospital course, outside of the progress note itself, could result in more succinct notes that convey what progress occurred that day, and would be simpler to read. Developing note-writing tools that permit more rapid note creation, tailored to the aptitudes of the note author, such as use of voice [ 27 , 28 ] or scribes, could permit the notes to be signed earlier in the day, resulting in increased readership, which is an important objective of the daily progress note.
Templates can also speed note writing but is done so at the risk of retaining content of the history or physical exam, which is included in some templates. Many clinicians who read notes are most interested in what the note author has to say rather than what is within the template text. Every change to note-writing approaches has potential for side-effects. For example, methods that reduce the time to create notes and that permit them to be completed earlier in the day may also decrease note quality.
There is an important role for hospital leaders in setting the direction for this critical part of clinical care and training [ 29 ]. As a result of this work, our community has expressed agreement on increasing the communication value of progress notes, in part by making it possible for them to be completed earlier, and to reduce the time devoted to writing them.
Acknowledgments
We greatly appreciate the assistance of Xi Li, who performed the note content analysis, and of Jacki DeNonno and Johnathan Bubalo, Cerner Corporation, for obtaining the data on note readership.
This work was funded by a University of Washington Department of Medicine Accelerator Grant.
Abbreviations
Conflicts of Interest: None declared.
- History, Facts & Figures
- YSM Dean & Deputy Deans
- YSM Administration
- Department Chairs
- YSM Executive Group
- YSM Board of Permanent Officers
- FAC Documents
- Current FAC Members
- Appointments & Promotions Committees
- Ad Hoc Committees and Working Groups
- Chair Searches
- Leadership Searches
- Organization Charts
- Faculty Demographic Data
- Professionalism Reporting Data
- 2022 Diversity Engagement Survey
- State of the School Archive
- Faculty Climate Survey: YSM Results
- Strategic Planning
- Mission Statement & Process
- Beyond Sterling Hall
- COVID-19 Series Workshops
- Previous Workshops
- Departments & Centers
- Find People
- Biomedical Data Science
- Health Equity
- Inflammation
- Neuroscience
- Global Health
- Diabetes and Metabolism
- Policies & Procedures
- Media Relations
- A to Z YSM Lab Websites
- A-Z Faculty List
- A-Z Staff List
- A to Z Abbreviations
- Dept. Diversity Vice Chairs & Champions
- Dean’s Advisory Council on Lesbian, Gay, Bisexual, Transgender, Queer and Intersex Affairs Website
- Minority Organization for Retention and Expansion Website
- Office for Women in Medicine and Science
- Committee on the Status of Women in Medicine Website
- Director of Scientist Diversity and Inclusion
- Diversity Supplements
- Frequently Asked Questions
- Recruitment
- By Department & Program
- News & Events
- Executive Committee
- Aperture: Women in Medicine
- Self-Reflection
- Portraits of Strength
- Mindful: Mental Health Through Art
- Event Photo Galleries
- Additional Support
- MD-PhD Program
- PA Online Program
- Joint MD Programs
- How to Apply
- Advanced Health Sciences Research
- Clinical Informatics & Data Science
- Clinical Investigation
- Medical Education
- Visiting Student Programs
- Special Programs & Student Opportunities
- Residency & Fellowship Programs
- Center for Med Ed
- Organizational Chart
- Leadership & Staff
- Committee Procedural Info (Login Required)
- Faculty Affairs Department Teams
- Recent Appointments & Promotions
- Academic Clinician Track
- Clinician Educator-Scholar Track
- Clinican-Scientist Track
- Investigator Track
- Traditional Track
- Research Ranks
- Instructor/Lecturer
- Social Work Ranks
- Voluntary Ranks
- Adjunct Ranks
- Other Appt Types
- Appointments
- Reappointments
- Transfer of Track
- Term Extensions
- Timeline for A&P Processes
- Interfolio Faculty Search
- Interfolio A&P Processes
- Yale CV Part 1 (CV1)
- Yale CV Part 2 (CV2)
- Samples of Scholarship
- Teaching Evaluations
- Letters of Evaluation
- Dept A&P Narrative
- A&P Voting
- Faculty Affairs Staff Pages
- OAPD Faculty Workshops
- Leadership & Development Seminars
- List of Faculty Mentors
- Incoming Faculty Orientation
- Faculty Onboarding
- Past YSM Award Recipients
- Past PA Award Recipients
- Past YM Award Recipients
- International Award Recipients
- Nominations Calendar
- OAPD Newsletter
- Fostering a Shared Vision of Professionalism
- Academic Integrity
- Addressing Professionalism Concerns
- Consultation Support for Chairs & Section Chiefs
- Policies & Codes of Conduct
- First Fridays
- Fund for Physician-Scientist Mentorship
- Grant Library
- Grant Writing Course
- Mock Study Section
- Research Paper Writing
- Establishing a Thriving Research Program
- Funding Opportunities
- Join Our Voluntary Faculty
- Child Mental Health: Fostering Wellness in Children
- Faculty Resources
- Research by Keyword
- Research by Department
- Research by Global Location
- Translational Research
- Research Cores & Services
- Program for the Promotion of Interdisciplinary Team Science (POINTS)
- CEnR Steering Committee
- Experiential Learning Subcommittee
- Goals & Objectives
- Issues List
- Print Magazine PDFs
- Print Newsletter PDFs
- YSM Events Newsletter
- Social Media
- Patient Care
INFORMATION FOR
- Residents & Fellows
- Researchers
Progress Notes
Hi everyone:
Most of you spend countless hours writing progress notes, so you should use this time well.
We write progress notes for two main reasons: to track a patient’s course and to communicate. Patients are complicated, and for consultants and cross-covering physicians, clear, concise notes are priceless.
Sadly, many notes are a mess of unfiltered, outdated, and irrelevant factoids. Let’s do better. Here are some precepts:
- Copying and pasting: As I wrote last week, copying and pasting can crater your credibility. If you do copy and paste, ensure your notes are accurate and up to date.
- Hospital summaries: Brief summaries at the top of the note can be helpful, but please synthesize. If Ms. Johnson was admitted three days ago with chills, fever, productive cough, and a right upper lobe infiltrate, just say she was admitted with pneumonia.
- Focused physical exams: I’m skeptical that anyone is doing head-to-toe physicals on every patient every day, though some notes imply this. After admission, focus your exams. You don’t need to check pupillary responses every morning in patients with cellulitis (assuming they’re awake and talking), but you should update your skin exam, comparing your findings to the previous day (pictures are a bonus).
- Targeted data: Don’t clog your note with reams of test results, especially radiology studies. Any reader can look them up, and no one relies on your notes to find the results of old head CTs. Show new tests and delete the rest.
- Assessments: Don’t use assessments to reiterate raw data. Show your thinking. Tell readers if the patient is making progress or not (that’s why it’s called a “progress note”). For example: “Mr. Jones is a middle-aged man with a history of IV drug use, being treated with oxacillin for mitral valve endocarditis due to MSSA, now afebrile with negative blood cultures.” Or, if the diagnosis is uncertain, you might say “Mr. Jones has ongoing fevers despite antibiotics. Given that all cultures and imaging to date are negative, we’ve begun to suspect a non-infectious cause of fever.”
- Follow up blood cultures
- Start piperacillin-tazobactam, pending cultures
- Everything in its place: Whether you use problem-based lists (on the floor) or system-based lists (in the ICU), organize your assessments and plans. For patients with diabetic foot ulcers, separate ulcer management (wound care) from diabetes treatment (insulin). For patients intubated with multilobar pneumonia, discuss ventilator management under “respiratory” and antibiotics under “ID.”
- Be concise: Be brief . If your notes are too long, important information will get lost. Be thorough, but as with so much in medicine , less is more.
Writing effective progress notes will distinguish you as an internist. Good notes minimize the risk of dropped handoffs, they help consultants know what’s being asked of them, and they’re essential during emergencies. As a bonus, well-crafted notes save time, both for readers and for you.
Enjoy your Sunday, everyone. We flew in from Europe last night, and I look forward to seeing you again soon. Today, I’m driving down to New Jersey to visit my mom.
PS Pictures from Italy and Slovenia:
Featured in this article
- Mark David Siegel, MD Professor of Medicine (Pulmonary); Program Director, Internal Medicine Traditional Residency Program

The Do’s and Don’ts of Progress Notes
Progress notes are crucial components of clinical documentation utilized by social workers to talk with members of the medical treatment team and insurance companies about the client’s progress and setbacks. This documentation may also be reviewed by the patient or their family, so the notes should be detailed enough to allow reviewers to understand the situation but not so private as to eliminate the confidentiality that protects it. It can be overwhelming at times to determine what should and should not be included in a note, as there is so much that goes on in one 45 minute session. Below will go over the basics of note writing as well as recommendations as to what to include as well as what to avoid when documenting client sessions.

What to include in a progress note
In any given mental health progress note, there are certain elements that should be included in order to provide an accurate and complete picture of the client’s current status. First and foremost, the date and time of the session should be noted. This is followed by a brief description of the client’s presenting problem or reason for seeking services. This includes describing the nature of the problem, how long the client has been experiencing it, and any relevant background information. Additionally, it is important to document what progress the client has made since beginning treatment. This can include any positive changes in symptoms or functioning, as well as any setbacks or plateaus. If a setback of plateau occurs, it is usually best practice to identify why this is happening (if the reason is known).
The next section should include a summary of the therapist-client interaction during the session. This can include anything from how the client was feeling during the session to what topics were discussed. Be sure to note how the client responded to the interventions. Finally, the progress note should end with a brief conclusion or summary of the session as well as any goals or plans for future sessions.
For additional details on how to write a progress note, read my earlier post: How Social Workers Can Write and Effective Progress Note.
What not to include in a progress note
A mental health progress note is a tool used by clinicians to document and communicate a client’s progress in therapy. While there is no one “right” way to write a progress note, there are some things that should be avoided. Here are three things to avoid when writing mental health progress notes:
1. Avoid using heavy amounts of clinical jargon : Jargon can be confusing and off-putting for clients. Instead, use clear and concise language that can be easily understood by the client. If you are going to use a clinical term, be sure that you are using it correctly and a way that can be understood with relative ease by a non-clinical person as they read through the note. Often times insurance reviewers do not have a clinical mental health degree, therefore if too much jargon is used and the note it not understandable, there is a higher risk for an insurance denial or audit.
2. Avoid making assumptions about the client: Every client is unique and should be treated as such. Progress notes should reflect this by avoiding generalizations and stereotypes. Stick to the facts only. Any personal assumptions or theories should be kept in a psychotherapy note and not within the medical documentation of a progress note.
3 . Avoid sounding judgmental: It is important to remain objective when documenting a client’s progress. Judgmental language can be interpreted as bias and undermine the relationship between clinician and client.

How to format a progress note
I personally enjoy using a SOAP note format for my progress notes. To read more about how to write a great SOAP note read my latest post here.
For a SOAP note template, go to the products page of this website.
The benefits of using progress notes
In my clinical practice, I have found that using mental health progress notes is an extremely beneficial way to document treatment. Not only does it provide a detailed record of what has been discussed and accomplished during each session, but it can also be used to help track a client’s progress over time.
I often find myself referring back to old progress notes when meeting with a client for follow-up appointments. It’s helpful to be able to see how far they’ve come and what issues they may still be struggling with. Additionally, progress notes can be useful in identifying any patterns or trends in a client’s behavior or symptoms.
Overall, I believe that mental health progress notes are an invaluable tool for social workers and other mental health professionals. They provide us with a way to accurately document our work with clients and track their progress over time.
The importance of accuracy in progress notes
As a social worker, progress notes are an important way to document interactions with clients and track their progress. Accuracy is essential in order to provide the best possible care for clients and to ensure continuity of care if another social worker takes over their case.
Progress notes can be used in a variety of ways, including to assess whether goals are being met, to document changes in a client’s condition, or to provide justification for continued services. Inaccurate progress notes can lead to false assumptions about a client’s progress and may even result in them not receiving the services they need.
If a client’s sessions are reimbursed by insurance and there is inaccurate data, the insurance reserves the right to deny payment and may even file the claim as insurance fraud. Even if the intentions are good and an honest mistake was made, accuracy errors can leave a practitioner open to legal recourse and malpractice.
It is therefore essential that social workers take the time to write accurate and detailed progress notes. This may require some extra time initially, but it will pay off in the long run by providing better care for clients and avoiding any potential problems that could arise from inaccurate documentation.

In conclusion, writing a mental health progress note is important for treatment as it helps to document changes in a client’s condition. It is important to be accurate and objective when writing progress notes, as this information can be used to make decisions about a client’s treatment.
Want an easy way to write your clinical documentation?
My masterclass: Mastering Clinical Documentation With Speed and Efficiency breaks it down in template form so you no longer have to do any guess work as to what to include in order to get reimbursed for your hard work. Access it here to get started!
NEXT STEPS…
Are you tired of spending hours every week writing case notes and updating client records?
Do you struggle to keep track of all the information you need for accurate diagnosis and treatment planning?
If so, it’s time to invest in your clinical documentation skills.
Register for my Mastering Clinical Documentation with Speed & Efficiency (Includes Templates)
During this 90 minute instant access masterclass, you will get…

Buy today and access forever! All registered guests get immediate access to a ThriveCart Learn student portal where they will have lifetime access to the documentation templates, masterclass recording, and in-depth videos on how to use each template.
Register here: https://www.stresslesstherapist.com/documentation-course
Similar Posts

Want To Book New Clients in 30 Days? Avoid These Rookie Mistakes
Hands up if you want to attract new clients to your therapy practice. Do you want it like yesterday? Of course, you do. You may have even signed up for an expensive directory that promises to be a “game changer” for your business. But… are still hearing crickets instead of phone calls. In this post,…

Shedding Light On The 5 Factors That Shape Therapist Salary
Ever thought about what determines a therapist salary? The therapy field offers not only the opportunity to heal using empathy and compassion, but also the opportunity for financial stability. If you are a prospective therapist, especially someone who is interested in starting a private practice, it is important to consider various factors that can influence…
![writing progress notes How I Built Passive Income as Private Practice Owner [Show Notes]](https://i0.wp.com/www.stresslesstherapist.com/wp-content/uploads/2023/10/Most-Attractive-Youtube-Thumbnail-1.png?fit=768%2C432&ssl=1)
How I Built Passive Income as Private Practice Owner [Show Notes]
Discover the top side hustles for therapists! Learn how I built passive income as a private practice owner and boost your earnings today.

The 4 Steps How to Get More Clients To Your Private Practice – No Ads Needed!
Are you an independent practitioner looking for ways to grow your private practice? Discover 4 simple steps I recommend for getting started in digital marketing without ads to attract more clients.

Discharge Note Template–Perfect for Therapy
Create professional therapy documentation quickly and easily with this discharge note template. Perfect for therapists, it ensures you provide detailed, accurate information for all your patients.

How to Start a Business As A Therapist: 3 Things You Can Do Today That Cost You Nothing
As a business coach, the most common question I hear from mental health professionals is “How to Start a Business? More specifically, how to start their private practice with a little overhead as possible. In today’s fast-paced, technology-driven world, the demand for virtual therapy services has skyrocketed. As more people seek mental health support from…
More From Forbes
Students aren’t writing well anymore. can ai help.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
A group of students begins an in-class writing test. According to new data analysis, half of U.S. ... [+] eighth graders have difficulty with long-form writing on tests and classwork that involves reading.
Fifty percent. That’s the approximate number of students in eighth grade who struggle with long-form writing on tests and classwork that involves reading.
A colleague of mine, L Burleigh, studying reading data collected in 2022 from the National Assessment of Educational Progress (NAEP) found that fewer than half of eighth graders write “long answers to questions on tests or assignments that involve reading.”
While people may put a premium on the notion of short and sweet when it comes to writing and reading – doing so at formative ages means that young learners will not build the skills they need to convey and explain ideas and information.
Writing Frequency Matters
Frequency of practice is a common theme cited by both researchers and teachers in assessing causes for declining K-12 student writing skills. Middle and high schoolers simply are not engaging in and practicing writing enough. The reasons for this are myriad but overburdened teachers without the time or support to grade more frequent writing assignments is a significant factor.
In a survey I did with some colleagues a few years ago, a key challenge was workload. More than 70 percent of educators say they are overwhelmed with grading, providing feedback, and other administrative tasks. Additionally, according to our report, educators in low-income schools are almost 20 percent more likely than teachers in other schools to report being overburdened by routine duties like grading essays.
In short, kids are not writing as much as frequency in writing education falls victim to staffing, time, and resource shortages.
Highlighting this point is NAEP reading data for eighth graders collected by L that included the following question to students about their writing habits: “How often have you been asked to write long answers to questions on tests or assignments that involved reading?” The results: Never - 2%; Once - 3%; Two or Three Times - 22%; Four or Five Times - 25%; More than Five Times - 48 percent.
Why Is Chief Boden Leaving ‘Chicago Fire?’ Eamonn Walker’s Exit Explained
Nvidia are splitting 10 for 1 here s what it means and how to profit, massive dota 2 7 36 patch notes add innate abilities and facets, using ai to aid writing gains.
There’s lots that can be done to fix this problem: Improved teacher professional development, greater emphasis on writing across the curriculum, etc. For my part, I’m optimistic that AI will be a deep help to students, given recent advances in the technology, and many are exploring new avenues to support students in boosting their long-form writing ability.
For instance, the team at ThinkCirca is working on a formative assessment and feedback tool to enhance student writing. This tool focuses on argumentative essays and identifies key elements within the text as students write. By highlighting these elements, the tool provides real-time assessment and feedback, creating mini-instructional moments that guide students in improving their arguments during the writing process.
Large language models can help, too. Indeed, just asking ChatGPT provides helpful feedback. But for more targeted support, researchers have found that fine-tuning is necessary. For instance, when researchers looked at holistic scoring using ChatGPT (version 4), they found the technology could provide human-level performance.
However, when asking the chatbot to focus on more granular, discourse-level evaluation, ChatGPT began to struggle. More specifically, it had a hard time identifying the distinct elements of argumentative writing (e.g., claim, counterclaim, rebuttal, supporting evidence). Additionally, ChatGPT was a more generous grader than humans when focused on smaller writing segments, like discourse elements, rating them at a higher effectiveness level than a human would.
This finding makes sense because chatbots are usually trained to create text using thousands of example essays. However, chatbots don't see many examples of labeled essay parts during their training compared to tasks like summarizing a text or analyzing the emotion of an essay. So, while ChatGPT is not as reliable for evaluating the structure of an essay due to its lack of training, it is extensively taught on what forms a strong long-form essay and its ability to generate essays is an area of greater concern for educators.
Some worry certain LLM technologies could help students cheat by doing their long-form writing for them, although recent research from Stanford and others indicates this is not occurring as frequently as initially feared. The potential benefit of incorporating technology to help students strengthen their writing skills may far outweigh any risks posed by introducing AI solutions – especially since researchers point out that declines in student writing can be traced to how often students are engaging in long-form writing.
Even as AI carves out its place in improving student writing, staying true to some hallmark tenets is recommended to help young learners build on the writing skills and abilities deemed indispensable in the workforce.
Whether gains on this front are realized through AI or teacher interaction, the ultimate goal is to make the essential communication and job skill of writing something that students can navigate naturally and with confidence that will carry them successfully through college and the workforce.

- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.

IMAGES
VIDEO
COMMENTS
Learn the purpose, requirements, and tips for writing compliant progress notes for mental health care. Find templates, examples, and a free EHR feature to help you document each session with your client.
Learn the differences between progress and psychotherapy notes, documentation styles, and best practices for writing effective progress notes. Find out how EHR software can help you streamline your note-writing processes and improve your care quality.
10 Steps For Writing Effective Progress Notes. Following a template is an easy way to ensure all important details and information are included in your therapy progress notes. Many treatment software solutions offer this functionality, with a variety of formats and outlines for different healthcare subsectors ...
Learn how to write therapy progress notes to document the details of every session. Download our free therapy progress notes templates.
The next step in writing a perfect nursing progress note is to ensure you obtain objective data. Objective data include your patient's vital signs, laboratory or diagnostic test results, and any observable symptoms.For example, "Vital signs for Mr. Smith are B/P 150/98, P 90, R 20, Temp 101.4.
A Good Nursing Progress Notes Example. There's nothing like reading an example to help you grasp a concept, so let's take a look at a sample nurse's progress note: 08.07.2022 — 10:30 am. Patient: Anne Example. The patient reported dizzy spells lasting up to 10 minutes once or twice a day over the last week.
Patient progress notes are used to keep a record of a patient's care when they are staying at a hospital. Nurses, doctors, physical therapists, and all other members of the healthcare team who provide care to the patient will document notes in the patient's chart. All progress notes can be accessed by the members of the healthcare team in ...
When writing therapy progress notes, it is important to use clear and objective language. Avoid subjective interpretations or judgments, and instead focus on describing the client's behavior, responses, and progress in an unbiased manner. Using precise and specific language helps ensure that the notes accurately reflect the client's ...
Here are four EHR features that can make your workflow move faster: Progress note templates: Have the most common mental status exams ready to paste or include into your notes. You can also create templates for assessments and plans for common diagnoses. This is particularly helpful if you have a homogenous patient population.
Writing progress notes is an essential part of every physician and trainee's daily responsibility. The problem-oriented structure of a note has its long history as part of Dr. Lawrence Weed's problem-oriented medical record framework in the 1960s . Each progress note should consist of subjective information, objective information ...
Here are some of them: 1. Progress notes are a contract between the client and the clinician. They are where treatment goals and plans can be discussed and decided on before they are put into a document to track the treatment progression. 2. Progress notes provide communication within and between care teams.
Tips for writing good progress notes. Several strategies are essential to produce highly effective progress notes. First, maintain objectivity within the notes. Although some subjectivity is necessary to reflect the practitioner's professional opinions on the patient's presentation, evidence should always support these. Avoid using language ...
These tips are the best guides on how to write a progress note. Each tip will help improve comprehensive progress notes that specify all the sections needed for clinical documentation: 1. Use clear and concise language. When writing progress notes, prioritize clarity and brevity.
None of the trademark holders are endorsed by nor affiliated with Osmosis or this website. Writing a good progress note Videos, Flashcards, High Yield Notes, & Practice Questions. Learn and reinforce your understanding of Writing a good progress note.
There are a lot of different formal approaches to taking progress notes, but the three main types are SOAP notes, BIRP notes, and DAP notes: 1. SOAP notes: SOAP notes are the most common type, containing four separate types of information in four distinct rows: S = Subjective information, such as quotes from the client, or paraphrased ...
The goal of the progress note is to write a chronological narrative of the shift including any issues you may have come across. For instance, you can write a note after you complete your initial assessment. It may look a little something like this: (date/time: Physical assessment completed. VS WNL.
DARP notes are a widely used method for documenting therapy sessions and clinical progress notes. Similar to the popular SOAP notes format, DARP (sometimes DAP) stands for: Our template is designed to assist you in writing progress notes, with fillable fields for each section of a DARP note, ensuring quick and efficient documentation.
Clinical office notes communicate what happens within the examination room. The progress note is a tool for clinicians to convey information to each other to optimize the care of our patients. I ...
Developing note-writing tools that permit more rapid note creation, tailored to the aptitudes of the note author, such as use of voice [27,28] or scribes, could permit the notes to be signed earlier in the day, resulting in increased readership, which is an important objective of the daily progress note.
Here's a list of steps to follow in order to write a nursing progress note using the SOAPI method: 1. Gather subjective evidence. After you record the date, time and both you and your patient's name, begin your nursing progress note by requesting information from the patient. This information is likely subjective and limited to the patient's ...
7 Practise writing objective progress notes Learners demonstrate that they can write objective progress notes Writing and discussion Pairs Whole group Workbook p6 5 Guidelines for writing objectively Learners understand that progress notes: Need to be factual Can report on things that are heard, but need to identify this
Progress Notes. August 21, 2022. Hi everyone: Most of you spend countless hours writing progress notes, so you should use this time well. We write progress notes for two main reasons: to track a patient's course and to communicate. Patients are complicated, and for consultants and cross-covering physicians, clear, concise notes are priceless.
Complete Guide to Progress Notes in Disability & Aged Care. Rob Scott. Written on 8 August, 2023. Progress notes are created by support workers at the end of a shift. This guide includes valuable tips on how to write progress notes to a high professional standard for the Disability and Home Care industry. Progress notes are a vital part of a ...
A mental health progress note is a tool used by clinicians to document and communicate a client's progress in therapy. While there is no one "right" way to write a progress note, there are some things that should be avoided. Here are three things to avoid when writing mental health progress notes: 1.
This tool focuses on argumentative essays and identifies key elements within the text as students write. By highlighting these elements, the tool provides real-time assessment and feedback ...
The course is open to any writer with previous workshop experience and a book in progress, including traditional or experimental novels and novels-in-stories. We will read novels by Jessica Au and Joan Silber, to see how they create memorable characters and meaningful predicaments, and use in-class writing exercises to practice new techniques ...