Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center


Autism Spectrum Disorder: A case study of Mikey
This paper describes Autism Spectrum Disorder (ASD) including diagnostic criteria, suspected causes, prevalence, comorbidities, and influences on client factors. A hypothetical case study is presented to give readers an illustration of what someone with ASD might look like. Possible treatment based on evidence and selected frame of references will be given for the hypothetical client. This paper is not all inclusive of the role of occupational therapy in the treatment of Autism Spectrum Disorder, but gives an illustrative example.
Related Papers
Jennelyn Pondang
Autism Spectrum Disorder - Recent Advances
IOSR Journals
This article aims to observe all the manifestations of the behavior of a child with Autism Spectrum Disorder (ASD), which shows deficits mainly in the communication sector. Also, the child shows repetitive and stereotypical behaviors throughout the lesson (Stasinos, 2016). Initially the paper describes the methodology followed. It then describes the child's cognitive profile and the deficits he presents. He then analyzes the intervention that was applied in order to improve the difficulties he faces and to further strengthen the skills he has already acquired. Finally, the paper presents the main conclusions as they emerged from the intervention.
Function and Disability Journal
Seyed Hassan Saneii
Melissa Vandiver Phelan
American Journal of Occupational Therapy
Renee Watling
Occupational therapy has much to offer to families of people with autism spectrum disorder (ASD). However, people outside the profession may be unaware of occupational therapy’s breadth and scope. It is our responsibility and our duty to express the full range of occupational therapy services through research, clinical practice, advocacy, and consumer education. This special issue of the American Journal of Occupational Therapy, with its focus on autism, embarks on this endeavor by highlighting research and theoretical articles that address the various aspects of occupational therapy practice that can help to fully meet the needs of people with ASD and their families.
IP International Journal of Medical Paediatrics and Oncology
Autism spectrum disorder encompasses a wide range of neurodevelopment disabilities which affect children and their families across all sections of the society both in rural and urban settings. The prevalence of autism is rising irrespective of the socioeconomic background of the children. Hence every health worker has to be aware of ways to suspect and diagnose this condition and decide the appropriate treatment. Earliest intervention in autism spectrum disorder gives better results due to neuroplasticity. This article is targeted to help Medical officers, auxiliary nurse midwifes, anganwadi workers and other peripheral health workers by providing information on basics of ASD, normal speech development, simple ways for diagnosis and treatment for the same.
The American Journal of Occupational Therapy
Objective. The purpose of this study was to examine the current practice patterns of occupational therapists experienced in working with children with autism spectrum disorders. Method. Occupational therapists experienced in providing services to 2-year-old to 12-year-old children with autism completed a mail questionnaire describing practice patterns, theoretical approaches, intervention techniques, and preferred methods of preparation for work with children with autism. Results. Of those contacted, 72 occupational therapists met the study criteria and returned completed questionnaires. Practice patterns included frequent collaboration with other professionals during assessment and intervention. Intervention services were typically provided in a one-to-one format with the most common techniques being sensory integration (99%) and positive reinforcement (93%). Theoretical approaches included sensory integration (99%), developmental (88%), and behavioral (73%). Evaluations relied hea...
The American journal of occupational therapy : official publication of the American Occupational Therapy Association
Kristie P Koenig
Evidence Connection articles provide a clinical application of systematic reviews developed in conjunction with the American Occupational Therapy Association's (AOTA's) Evidence-Based Practice Project. In this Evidence Connection article, we describe a case report of an adolescent with autism spectrum disorder. The occupational therapy assessment and treatment processes for school, home, community, and transition settings are described. Findings from the systematic reviews on this topic were published in the September/October 2015 issue of the American Journal of Occupational Therapy and in AOTA's Occupational Therapy Practice Guidelines for Individuals With Autism Spectrum Disorder. Each article in this series summarizes the evidence from the published reviews on a given topic and presents an application of the evidence to a related clinical case. Evidence Connection articles illustrate how the research evidence from the reviews can be used to inform and guide clinical ...
Javiera Poblete
Autism spectrum disorder is a term used to describe a constellation of early-appearing social communication deficits and repetitive sensory-motor behaviours associated with a strong genetic component as well as other causes. The outlook for many individuals with autism spectrum disorder today is brighter than it was 50 years ago; more people with the condition are able to speak, read, and live in the community rather than in institutions, and some will be largely free from symptoms of the disorder by adulthood. Nevertheless, most individuals will not work full-time or live independently. Genetics and neuroscience have identified intriguing patterns of risk, but without much practical benefit yet. Considerable work is still needed to understand how and when behavioural and medical treatments can be effective, and for which children, including those with substantial comorbidities. It is also important to implement what we already know and develop services for adults with autism spectrum disorder. Clinicians can make a difference by providing timely and individualised help to families navigating referrals and access to community support systems, by providing accurate information despite often unfiltered media input, and by anticipating transitions such as family changes and school entry and leaving.
RELATED PAPERS
Drew Kershen
Bernard Baum
richard morante
Russian Journal of Physical Chemistry A
Olga Maksimenko
Revista Brasileira de Coloproctologia
Francisco simão Ndulo paulo
BMC Veterinary Research
Ezio Bianchi
Bolema: Boletim de Educação Matemática
Rosa Elena Durán González
Ananda putri
Cretaceous Research
Ladislav Fucek
International advanced research journal in science, engineering and technology
Anjali Krishna
Advanced Information Systems
Volodymyr Lysechko
IVAN SALAZAR
This is an extract from the article “The People vs. Hegel: The Mystifying Transcendence of Time and the Immanence of Radical Democracy” by Ricardo Sanín-Restrepo published in the book “Decrypting Power” 2018. Rowman and Littlefield Int. London
Ricardo Sanín-Restrepo
Coral Reefs and Associated Marine Fauna around the Arabian Peninsula
John A Burt
Economic Jurisprudence Studies (EJS)
فصلنامه علمی مطالعات فقه اقتصادی ایران
The New York Times
Joseph Fuzaylov
Advances in Fuzzy Systems
Journal of Interactive Advertising
Sally J McMillan
Emmatul Afifah
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
To read this content please select one of the options below:
Please note you do not have access to teaching notes, being diagnosed with autism in adulthood: a personal case study.
Advances in Autism
ISSN : 2056-3868
Article publication date: 19 June 2020
Issue publication date: 11 August 2021
This paper aims to report the personal experiences of an adult male diagnosed with autism at the age of 48 years.
Design/methodology/approach
A personal case study methodology was used to illustrate the journey to autism diagnosis, the experience of diagnosis and post-diagnosis support.
This case study illustrates how stress and mental health difficulties can precede autism diagnosis in adults. The personal experiences detailed highlight how an adult autism diagnosis can bring about positive change, prompting increased self-knowledge and coping skills, improved relationships and. Furthermore, it highlights how a supportive employer can make reasonable adjustments in the workplace to improve productivity of an autistic employee.
Research limitations/implications
This case study has implications for various practice issues, including post-diagnosis counselling and access to support for autistic adults nationally.
Originality/value
This paper provides an original case study highlighting the personal experiences of an adult diagnosed with autism.
- Mental health
- Autism spectrum condition
- Mental disorder
Henley, R. (2021), "Being diagnosed with autism in adulthood: a personal case study", Advances in Autism , Vol. 7 No. 3, pp. 256-261. https://doi.org/10.1108/AIA-03-2020-0018
Emerald Publishing Limited
Copyright © 2020, Emerald Publishing Limited
Related articles
We’re listening — tell us what you think, something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 25: Case Study: Autism Spectrum Disorder
Karen Tartick
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Introduction.
- Motor Delays and Deficits
- Examination: Age 6 Years, 22 Days
- Plan of Care
- Intervention
- Conclusion of Care
- Examination: Age 7 Years, 9 Months
- Termination of Episodes
- Recommended Resources
- Full Chapter
- Supplementary Content
A utism spectrum disorder (ASD) is a neurodevelopmental disorder estimated to affect up to 1.7% of children in the United States, according to the Centers for Disease Control and Prevention (CDC) ( Maenner et al., 2020 ), and 3% of children age 4 years in the United States ( Christensen et al., 2019 ). Children with ASD have impairments in social and communication interactions and restrictive/repetitive behaviors that affect their functional abilities. ASD is one of the fastest growing pediatric disorders and affects boys four times more often than girls ( Maenner et al., 2020 ). The prevalence of ASD has risen dramatically in recent years, with estimates from 1:150 children in the year 2000 to 1:54 children in 2020 (1:34 boys, 1:144 girls) an increase of 175% since 2000 ( Maenner et al., 2020 ). Autism affects all ethnic and socioeconomic groups; prevalence estimates are approximately identical for children who identify as non-Hispanic white, non-Hispanic black, and Asian/Pacific Islander (18.5, 18.3, and 17.9, respectively) but lower for children who identify as Hispanic (15.4) ( Maenner et al., 2020 ). Co-occurring conditions are common in children with ASD, including sleep disorders and seizures; other developmental or behavioral diagnoses, such as attention deficit-hyperactivity disorder (ADHD), anxiety, and mood disorders; and behavioral disorders, such as food refusal, self-injury, and aggression ( Coury, 2010 ; Hossain et al., 2020 ). Both fine and gross motor skills may be delayed in preschool-age children with ASD ( Lloyd, MacDonald, & Lord, 2013 ). Children with ASD are more likely to have delays in gross motor skills and coordination compared with children in the general population and may meet DSM-5 criteria (see next paragraph) for developmental coordination disorder (DCD) in addition to ASD ( Bhat, 2020 ; Dewey, Cantell, & Crawford, 2007 ).
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Prev Med Rep
- v.36; 2023 Dec
- PMC10728454
Global burden and inequality of autism spectrum disorders: Based on data from the 2019 Global Burden of Disease study
a Clinical Medical College & Affiliated Hospital of Chengdu University, Chengdu, Sichuan, China
b School of Basic Medicine and Nursing, Chengdu University, Chengdu, Sichuan, China
c College of Pharmacy, Zunyi Medical University, Zunyi, Guizhou, China
Huiqing Wang
d Department of Pediatrics, West China Second University Hospital, Sichuan University, Sichuan, China
Associated Data
Data will be made available on request.
It is unclear whether the health equity of autism spectrum disorders (ASDs) has changed in different years, regions, and gender. The aims of this study were to provide a comprehensive description of the ASDs burden and provide evidence for improvement in health policies regarding ASDs inequality. This study is a population-based cross-sectional study based on the Global Burden of Disease datasets 1990–2019. We collected detailed information on ASDs between 1990 and 2019 in 204 countries worldwide, derived from the Global Burden of Disease study in 2019. Burden was calculated in terms of the incidence, prevalence and years lived with disability (YLDs). Concentration curves and concentration indices were used to summarize the degree of income-related inequality in the burden of ASDs. The overall age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR) and age-standardized YLDs rate (ASYR) of ASDs was 9.3 (95 %UI 7.7–11.1), 369.4 (95 %UI 305.9–441.2), 56.3 (95 %UI 36.8–81.5) per 100,000 people, respectively. The ASIR, ASPR and ASYR of ASDs affected three times as many males as females. The changing trends of age-standardized rates of ASDs showed that the ASIR of ASDs a slow growing trend globally. However, the ASPR and ASYR of ASDs showed a slow decreasing trend globally. All the concentration curves were below the line of equality and statistically significant. There was no significant difference in the age-standardized rate for different years in socio-demographic index-related inequality happened over 29 years (p > 0.05). The global burden of ASDs has remained higher in males and pro-rich, the income-related inequality tended not to change between 1990 and 2019.
1. Introduction
According to 2019 Global Burden of Disease (GBD) Mental Disorder Collaborators, mental disorders remain one of the top ten major causes of burden worldwide, with years lived with disability (YLDs) being the cause of the majority of the burden on mental disorders, with 125.3 million YLDs (95% uncertainty interval, UI 93.0–163.2), and the proportion of global YLDs attributed to mental disorders was 14.6% [12.2–16.8] in 2019 ( Collaborators“ GMD, 2022 ). In the mental disorders, it should be noted that autism spectrum disorders (ASDs) are persistent disabling neurodevelopmental disorders characterized by neuropsychological and behavioral deficits clinically evident from early childhood ( Baxter et al., 2015 ). ASDs was first described in 1943 and since then, a large increase in the incidence of ASDs worldwide ( Baj et al., 2021 ). ASDs is one of the fastest growing disabilities, accounting for substantial health loss across the lifespan ( Bhat et al., 2014 ). Epidemiological data reveal that there were an estimated 52 million cases of ASDs, equating to a prevalence of 7.6 per 1000 or one in 132 persons in 2010 ( Baxter et al., 2015 ). For 2016, across all 11 sites, ASDs prevalence was 18.5 per 1,000 (one in 54) children aged 8 years in the United States, the prevalence of ASDs was higher than previous estimates over the years ( Maenner et al., 2020 ). In 3/4 patients with ASDs, the disorder is accompanied by mental retardation. In addition, it is boys who are four times more likely to suffer from ASDs than girls. To date, the etiology of the disease has not been explained, although it is believed that it is most likely the result of gene and environmental factors interactions ( Baj et al., 2021 ). Understanding the burden of ASDs is essential for effective policy making. Previous research has shown that age, gender, and country of study were associated with heterogeneity in estimated prevalence of ASDs ( Lai et al., 2019 ). Because of the great personal and sociological cost of ASDs (estimated to be $2 million/patient/year ( Buescher et al., 2014 )), the epidemiological description of ASDs is needed to inform public health policy and to plan for education, housing, and financial support services. In addition, improved incidence, prevalence, and YLDs estimates and identification of moderators are needed to enhance recognition and care, and to guide future research.
Though some recent studies of ASDs have carried out ( Li et al., 2022 , Solmi et al., 2022 , Kang et al., 2023 , Li et al., 2022 ), they only focused on the global epidemiology of ASDs. However, it is unclear whether the health equity of ASD has changed in different years, regions, and gender. In our study, we aimed to evaluate the global burden of ASDs, focusing on the incidence prevalence, and YLDs of ASDs in different years, regions, and gender. The concentration index was calculated to assess the equities in global burden of ASDs. Our findings will provide a comprehensive description of the ASDs burden and provide evidence for improvement in health policies regarding ASDs inequality.
2.1. Study design
This study is a population-based cross-sectional study based on the Global Burden of Disease datasets 1990–2019.
2.2. Study data
The data come from the 2019 Global Burden of Disease (GBD) study ( https://vizhub.healthdata.org/gbd-results/ ). The official GBD website provides a detailed instruction on the general methods applied for GBD 2019 ( https://www.healthdata.org/gbd/2019 ). According to specific research objectives, various indices such as “cause”, “location”, and “year” can be selected in data source query tool (Global Health Data Exchange, GBDx). In this study, we obtained the annual case number of ASDs in all age groups and their corresponding age-standardized rates (ASRs), including incidence, prevalence, and YLDs and the 95% uncertainty interval from 1990 to 2019. GBD world population age standard was used as age-standardized population ( Global burden of 369 diseases and injuries in 204 countries and territories, 2019 ). A Bayesian meta-regression modelling tool, DisMod-MR 2.1, was used to ensure consistency between incidence, prevalence for most causes. Prevalence estimates were multiplied by disability weights for mutually exclusive sequelae of diseases and injuries to calculate YLDs. For administrative and data analysis purposes, the world has been divided into 21 GBD regions based on epidemiological similarity and geographic proximity. The socio-demographic index (SDI) is a composite indicator of income per capita in the 2019 GBD study, the calculation of SDI combined three main indicators: the average education level of individuals aged 15 and older, fertility rate in females under 25 years old, and the lag-distributed income per capita ( Global burden of 369 diseases and injuries in 204 countries and territories, 2019 , Wang et al., 2022 ). The SDI levels range from 0 (low SDI) to 100 (high SDI): the quintile is used to describe SDI levels, including low, medium low, medium, high, and high SDI ( Global burden of 369 diseases and injuries in 204 countries and territories, 2019 ), the SDI levels measures the socio-demographic development of a region, with higher values indicating better socio-economic conditions. In our study, the SDI levels were used as a proxy measure for concentration curves, which can be used to show the distribution of ASD burden of disease across regions with different economic development status. Our analysis was done in accordance with the GBD protocol. All data from GBDx can be shared and modified by non commercial users through an open data sharing attribution license.
2.3. Statistical analysis
The general methods for the GBD 2019 and the methods for estimations of disease burden have been detailed in previous studies ( Collaborators“ GMD, 2022 , Baxter et al., 2015 ). Briefly, we downloaded dataset including the incidence, prevalence and YLDs of ASDs. These data are open source and available for download from the GBD Results Tool. Detailed descriptions of the methods and approach used for the GBD estimation have been previously described ( Global burden of 369 diseases and injuries in 204 countries and territories, 2019 ). The age-standardized incidence rate (ASIR), the age-standardized prevalence rate (ASPR), the age-standardized YLDs rate (ASYR) (per 100,000 population) and estimated annual percentage change (EAPC) was calculated as previously described ( Liu et al., 2019 ). ASIR, ASPR and ASYR were calculated by summing up the products of the age-specific rate ( α i , where i is the i th age group) and the number of persons ( w i ) in the same age subgroup i of the selected reference standard population, i.e. , ASR = ∑ i = 1 A α i w i ∑ i = 1 A w i × 100,000, y = α + βx + ε , where x is year, y = In(ASR), EAPC = 100 × (exp(β) − 1) and its 95% confidence interval (CI) can also be obtained from the linear regression model. The ASR was in an increasing trend if the lower boundary of EAPC’s 95% CI was greater than 0, or, conversely, the ASR was in a decreasing trend if the upper boundary of EAPC’s 95% CI was less than 0. In other cases, the ASR was stable over time. Additionally, the influential factors and the change trend for ASIR, ASPR and ASYR explored by using scatter plot and line graph. Concentration curves and concentration indices ( Liu et al., 2012 ) were used to summarize the degree of income-related inequality in the burden of ASDs. A concentration curve plots the cumulative percentage of the outcome variable (age-standardized rate in incidence, prevalence and YLDs in this study) on the y-axis against the cumulative percentage of countries or regions ranked by socioeconomic status based on the SDI levels (from the lowest SDI levels to highest SDI levels) on the x-axis.
If the concentration curve is above the line of equality (the 45-degree line), it indicates that the ASDs-induced disease burden is higher among low-SDI countries; otherwise, the disease burden is higher among high-SDI countries. We computed the concentration index based on the concentration curve.
The covariance method was used to calculate the concentration index ( Peng et al., 2023 ).
In the above calculation formula, C represents the concentration index, cov means the covariance, r indicates the ranking of region i in the socio-economic distribution (from poorest to wealthiest), and h represents the health outcomes, μ considered as an average health outcome ( Peng et al., 2023 ).
Concentration index = 0 indicates that the health outcomes have a complete equal distribution, and the concentration curve is consistent with the equal distribution line. The concentration index < 0 means that the adverse health outcomes (disease burden) are concentrated in poor (low SDI levels) countries, with the concentration curve above the equality line, and vice versa.
A positive value indicates that the age-standardized rate is higher for the richer people. All statistics were performed using the STATA (Version Stata/MP 14.0), R program (Version 4.1.3) and RStudio 2022.02.1 Build 461. A p value of less than 0.05 was considered statistically significant.
2.4. Ethics statement
Our study was based on publicly available anonymized databases, and thus exempt from ethical compliance.
3.1. The global burden and changing trends of ASDs
From 1990 to 2019, the global incident cases of ASDs rose from 6.03 × 10 5 to 6.04 × 10 5 , increasing by 1.5‰, the ASIR of ASDs was ranged from 9.2 per 100,000 persons in 1990 to 9.3 per 100,000 persons in 2019. The results revealed that, overall, a growing trend of ASIR was observed from 1990 to 2019 (EAPC = 0.06; 95% CI 0.04 to 0.07). In 2019, the global incident cases of ASDs were 459,492.9 (95% UI 384,472.4 to 544,405.9) in males, which was 3.2-folds more than those in females (144,297.0; 95% UI 115,510.3 to 174,371.1). Moreover, a high ASIR of ASDs was recorded in under 5 years subgroup, in high SDI subgroup and in High-income North America subgroup, respectively. ( Table 1 and Fig. 1 ).
The incidence of autism spectrum disorders, and its changing trends from 1990 to 2019.
ASIR, age-standardized incidence rate; EAPC, estimated annual percentage change; UI, uncertainty interval; CI, confidence interval.

The global incidence burden and changing trends of ASDs between 1990 and 2019 in 204 countries and territories. (A) The ASIR of autistic spectrum disorders in 2019. (B) The relative change in incident cases of autistic spectrum disorders between 1990 and 2019. (C) The EAPC in ASIR of autistic spectrum disorders from 1990 to 2019. ASIR, age-standardized incidence rate; CIC, change in cases; EAPC, estimated annual percentage change.
As shown in STable 1 , from 1990 to 2019, the global number of prevalent ASDs rose from 2.03 × 10 7 to 2.83 × 10 7 , increasing by 39.3%. However, the ASPR of ASDs decreased from 372.8 per 100,000 persons to 369.4 per 100,000 persons over 29 years. The results revealed that, overall, a downtrend of ASPR was observed between 1990 and 2019 (EAPC = -0.02; 95% CI −0.03 to −0.01). In 2019, the global number of prevalent ASDs were 21,633,775.9 (95% UI 17,978,516.1 to 25,761,347.6) in males, which was 3.2-folds more than those in females (6,691,162.7; 95% UI 5,436,261.6 to 8,153,529.4). Moreover, a high ASPR of ASDs was recorded in under 5 years subgroup, in high SDI subgroup and in High-income North America subgroup, respectively ( STable 1 and SFig 1 ).
As shown in STable 2 , the years lived with ASDs were 4,306,615.4 (95% UI 2,821,511.9 to 6,232,360.5) in 2019, which was 1.39-folds higher than those in 1990 (3,105,909.1; 95% UI 2,025,303.0 to 4,514,467.3). However, the ASYR of ASDs decreased from 56.7 per 100,000 persons to 56.3 per 100,000 persons over 29 years. The results revealed that, overall, a downtrend of ASYR was observed between 1990 and 2019 (EAPC = -0.02; 95% CI −0.03 to −0.01). In 2019, the years lived with ASDs were 3,294,467.6 (95% UI: 2,152,733.3 to 4,769,102.9) in males, which was 3.3-folds more than those in females (1,012,147.8, 95% UI: 663,237–1,477,449.8). Moreover, a a high ASYR of ASDs was recorded in under 5 years subgroup, in high SDI subgroup and in High-income Asia Pacific subgroup, respectively ( STable 2 and SFig 2 ).
3.2. The influential factors for the burden of ASDs
The Scatter plot showed that the countries in which the SDI was approximately 0.6 had the lowest ASIR, ASPR and ASYR of ASDs, while those with SDI near 1.0 presented a high ASIR, ASPR and ASYR ( Fig. 2 ). In males, an obvious growing trend of ASIR, ASPR and ASYP was observed between 1990 and 2019 in high SDI subgroup, but in other SDI subgroups, the ASIR, ASPR and ASYR of ASDs remained stable over 29 years. However, in females, the ASIR, ASPR and ASYR of ASDs remained stable over 29 years in all SDI subgroups ( Fig. 3 ).

The association between age standardized rate of autistic spectrum disorders and SDI between 1990 and 2019 in 204 countries and territories. (A) ASIR and SDI. (B) ASPR and SDI. (C) ASYR and SDI. ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASYR, age-standardized YLDs rate; YLDs, years lived with disability; SDI, socio-demographic index.

The change trends of age-standardized rate of autistic spectrum disorders among SDI groups and gender from 1990 to 2019 (A) ASIR. (B) ASPR. (C) ASYR. ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASYR, age-standardized YLDs rate; YLDs, years lived with disability; SDI, socio-demographic index.
3.3. Health equity of ASDs between 1990 and 2019
The concentration curves and concentration indices for age-standardized rate of ASDs from 1990 to 2019 presented in Fig. 4 and Table 2 . All the curves were below the line of equality and statistically significant, suggesting that the ASIR, ASPR and ASYP of ASDs were more concentrated among the higher SDI between 1990 and 2019. There was no significant difference in the age-standardized rate for different years meant there was no significant changes in SDI-related inequality happened over 29 years (p > 0.05).

Concentration curves for age standardized rate of autistic spectrum disorders between 1990 and 2019 (A) ASIR. (B) ASPR. (C) ASYR. ASIR, age-standardized incidence rate; ASPR, age-standardized prevalence rate; ASYR, age-standardized YLDs rate; YLDs, years lived with disability; SDI, socio-demographic index.
Concentration indices for age-standardized rate of autism spectrum disorders from 1990 to 2019.
The concentration index for age-standardized rate in incidence, prevalence and YLDs ranked by SDI. ASIR, age-standardized incidence rate; ASPR, the age-standardized prevalence rate; ASYR, the age-standardized YLDs rate.
* This method checks up the value of the age-standardized rate is zero by hypothesis testing. p-value < 0.05 means the age-standardized rate is not equal to 0, otherwise, the age-standardized rate is equal to 0.
# Check of variance was used among different year groups. p-value < 0.05 means there is significant difference in the age-standardized rate for different years, otherwise, no significant difference.
The regression equation between concentration indices for age-standardized rate of ASDs and its influence factors is educed ( Table 3 ). The regression analysis showed that influencing factors SDI levels (Low SDI, Low-middle SDI, Middle SDI, High-middle SDI, High SDI) and sex (male, female) statistically correlated with ASIR, ASPR and ASYR of ASDs, respectively (P < 0.05). Analysis of contribution rate on effect factors of concentration indices, the results showed sex contributed 91.81%, 88.83%, and 88.57% to concentration indices of ASIR, ASPR and ASYR of ASDs, respectively.
The regression equation between concentration indices for age-standardized rate of ASDs and its influence factors.
§ Contribution rate, the contribution proportion of each factor to concentration indices of age-standardized rate in R-squared for the regression equation.
* This method checks up the coefficient is zero by hypothesis testing. p-value < 0.05 means the coefficient has statistical significance, the coefficient is not equal 0, otherwise, has no statistical significance.
# p-value < 0.05 means the regression equation is of significance and applicable, otherwise, has no statistical significance.
4. Discussion
Having sufficient information on factors affecting the burden of ASDs and its inequalities could help to prevent and decrease the risk of ASDs. This study examined the global burden of ASDs and socioeconomic-related inequality. In our study, the overall ASIR, ASPR and ASYR of ASDs was 9.3 (95 %UI 7.7–11.1), 369.4 (95 %UI 305.9–441.2), 56.3 (95 %UI 36.8–81.5) per 100,000 people, respectively. It was different between males and females, and ASIR, ASPR and ASYR of ASDs among males were about three times higher than those in females. The results were consistent with previous studies ( Lai and Baron-Cohen, 2015 , Constantino et al., 2010 , Kim et al., 2011 , Zwaigenbaum et al., 2012 ). However, it is worth noting that the risk of undiagnosed ASD in women is much higher than in men ( Bargiela et al., 2016 ). This gender bias has a serious impact on the health of girls and women with ASD, and it has been identified by the ASD academic circles as a key issue that needs to be studied and solved by research ( Pellicano et al., 2014 ). The changing trends of age-standardized rates of ASDs showed that the ASIR of ASDs a slow growing trend globally. However, the ASPR and ASYR of ASDs showed a slow decreasing trend globally. Furthermore, when SDI was greater than 0.6, the ASIR, ASPR and ASYR of ASDs were increasing with SDI growth. The increase global burden of ASDs was attributed to a varies of efforts. First, heightened awareness and enhanced diagnostic methods have contributed to identifying more cases ( Kim et al., 2011 ). Second, environmental factors are increasingly recognized as contributing to the rising incidence of ASDs ( Modabbernia et al., 2017 ). Lastly, societal and demographic changes, more parents are choosing to have children at an older age, and the older age of the parents also influences the increased prevalence of ASDs ( Wu et al., 2017 ). The global burden of ASDs has remained pro-rich, the income-related inequality tended not to change between 1990 and 2019. This may be due to the fact that high SDI countries have better access to health care facilities, and the higher ASIR, ASPR, and ASYR reported in these countries may reflect the better level of diagnosis rather than higher ASIR, ASPR, and ASYR of ASDs. On the other hand, some low SDI countries have limited health care resources and may not have enough epidemiological data on ASDs, leading to inaccuracies ( Samms-Vaughan, 2014 ). These results will improve the latest incidence, prevalence, and YLDs estimates and identify of the important contributing factors of burden and changing trends of ASDs. These findings will enhance recognition and care of ASDs, and to guide future research.
Previous research has shown that there was limited clinical or epidemiological evidence in ASDs ( Baxter et al., 2015 ). Immense challenges remained and progress was uneven in estimating the incidence, prevalence, and YLDs of ASDs. ASDs were difficult to screen and diagnose in very young (non-verbal) children ( Baxter et al., 2015 ). Our results revealed that the ASDs burden in the incident cases, prevalent cases, and YLDs increased worldwide. The overall number of the incident cases, prevalent cases, and YLDs increased by 1.5‰, 39.3% and 38.6%, respectively. This growth is expected to continue due to population growth and the ability of clinicians to understand and deal with ASDs increased accordingly ( Collaborators“ GMD, 2022 ). However, the age-standardized rates of prevalence and YLDs for ASDs showed a slow decreasing trend globally. The most likely explanation is that the effective intervention programs for ASDs have the potential to alleviate the severity of symptoms and reduce the risk of YLDs. However, the substantial burden of ASDs in lifespan has important public health and policy implications. Thus, support and interventions for patients with ASDs and their families need to extend beyond pediatric health and early education to primary health care providers at the community level, additional skills training and vocational support ( Baxter et al., 2015 ).
However, overall, a high ASIR, ASPR and ASYR of ASDs was recorded in high SDI subgroup. A big surprise in our study is that the countries in which the SDI was approximately 0.6 had the lowest ASIR, ASPR and ASYR of ASDs. When SDI was greater than 0.6, the association between age-standardized rates of ASDs and SDI in 2019 are shown that the ASIR, ASPR and ASYR of ASDs were increasing with SDI growth. Additionally, the patients of ASDs were more in males than in females worldwide. Further study showed that the changing trend of ASIR, ASPR and ASYP showed a significant growing trend in males in high SDI subgroup from 1990 to 2019, but in other SDI subgroups, the ASIR, ASPR and ASYR of ASDs remained stable in males at the same time. However, in females, the ASIR, ASPR and ASYR of ASDs remained stable over 29 years in all SDI subgroups. These results highlight some managerial implications for further research into the effect of differential exposures to possible risk factors.
Several strengths and limitations in our study should be considered. The strengths of our study include the using of concentration curves and concentration indices to measure health inequality, which is sensitive to changes in population distribution among different socio-economic groups and can reflect the socio-economic dimensions of health inequality ( Wagstaff et al., 1991 ). Additionally, our in-depth data mining and analysis of GBD data could fill the gap where the actual data on ASDs burden are sparse or unavailable. These results can effectively guide medical policy decision-making. At the same time, the present study has some limitations. First, the data coming from the GBD study uses the WHO world standard population. Although this ensures consistent comparisons between studies, it may not accurately capture the unique age distribution of specific regions or countries, which may lead to bias in age specific calculations. Second, when evaluating the severity of health losses caused by diseases, the GBD uses disability weights. These weights are derived from comprehensive surveys and research. However, they may not always be consistent with the different cultural and social beliefs of the studied disease ( Salomon et al., 2015 ). Third, our research is conducted at the global and national levels. In order to provide evidence within a specific country, it is necessary to conduct research within that country. Fourth, the GBD uses modeling techniques such as cross-walking to address data gaps. However, these methods come with fundamental assumptions that may affect the final estimate ( Haagsma et al., 2013 ). Especially, there might be more uncertainty in the estimated value in some low SDI countries. The absence of data from developing countries, the limited information for adults and the lack of studies reporting population-representative estimates for incidence, prevalence, and YLDs meant that generalized hypothesis had to be made to build a comprehensive model for the distribution of ASDs. To move from estimations and assumptions toward certainties, future studies should set up special databases. In particular, the data of the ASDs routine surveillance and sentinel surveillance and special survey in developing countries are urgently required.
5. Conclusions
The global burden of ASDs has remained higher in males and pro-rich, the income-related inequality tended not to change between 1990 and 2019.
CRediT authorship contribution statement
Lijun Yang: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. Feng Chen: Data curation, Project administration, Supervision, Writing – original draft, Writing – review & editing. Xingyu He: Writing – original draft, Writing – review & editing. Yu Tong: Writing – original draft, Writing – review & editing. QingYun Li: Writing – original draft, Writing – review & editing. Ting Yang: Writing – original draft, Writing – review & editing. Rong Peng: Funding acquisition, Project administration, Writing – review & editing. Huiqing Wang: Funding acquisition, Project administration, Writing – review & editing. Zheng Shi: Funding acquisition, Project administration, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank the GBD dataset for sharing the valuable data.
Funding statement
The study was supported by Innovation team project of Clinical Medical college & Affiliated hospital of Chengdu University (Award Number: CDFYCX202202, CDFYCX202204, CDFYCX202205, CDFYCX202208), the Project of Chengdu Municipal Health Commission (Award Number: 2023073, Recipient: Rong Peng; 2021345), Sichuan Provincial Science and Technology Foundation (Award Number: 22NZZH0031, Recipient: Zheng Shi; Award Number: 2023JDKP0037, Recipient: Huiqing Wang), program for Excellent Talents in Clinical Medical college & Affiliated hospital of Chengdu University (Recipient: Rong Peng), the program of Sichuan Provincial Nursing Association (Award Number: H21003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Patient consent statement
Not applicable.
Appendix A Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102511 .
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Supplementary figure 1

Supplementary figure 2

Data availability
- Baj J., Flieger W., Flieger M., Forma A., Sitarz E., Skórzyńska-Dziduszko K., et al. Autism spectrum disorder: Trace elements imbalances and the pathogenesis and severity of autistic symptoms. Neurosci. Biobehav. Rev. 2021; 129 :117–132. [ PubMed ] [ Google Scholar ]
- Bargiela S., Steward R., Mandy W. The experiences of late-diagnosed women with autism spectrum conditions: an investigation of the female autism phenotype. J. Autism Dev. Disord. 2016; 46 (10):3281–3294. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Baxter A.J., Brugha T.S., Erskine H.E., Scheurer R.W., Vos T., Scott J.G. The epidemiology and global burden of autism spectrum disorders. Psychol. Med. 2015; 45 (3):601–613. [ PubMed ] [ Google Scholar ]
- Bhat S., Acharya U.R., Adeli H., Bairy G.M., Adeli A. Autism: cause factors, early diagnosis and therapies. Rev. Neurosci. 2014; 25 (6):841–850. [ PubMed ] [ Google Scholar ]
- Buescher A.V., Cidav Z., Knapp M., Mandell D.S. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014; 168 (8):721–728. [ PubMed ] [ Google Scholar ]
- Collaborators“ GMD Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022; 9 (2):137–150. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Constantino J.N., Zhang Y., Frazier T., Abbacchi A.M., Law P. Sibling recurrence and the genetic epidemiology of autism. Am. J. Psychiatry. 2010; 167 (11):1349–1356. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. 2020. Lancet 396(10258): 1204-1222. [ PMC free article ] [ PubMed ]
- Haagsma J.A., Polinder S., Stein C.E., Havelaar A.H. Systematic review of foodborne burden of disease studies: quality assessment of data and methodology. Int. J. Food Microbiol. 2013; 166 (1):34–47. [ PubMed ] [ Google Scholar ]
- Kang L., Liu J., Liu Y., Liang W., Yang F., Liu M. Global, regional, and national disease burden of autism spectrum disorder among children under 5 years from 1990 to 2019: An analysis for the Global Burden of Disease 2019 Study. Asian J. Psychiatr. 2023; 79 [ PubMed ] [ Google Scholar ]
- Kim Y.S., Leventhal B.L., Koh Y.J., Fombonne E., Laska E., Lim E.C., et al. Prevalence of autism spectrum disorders in a total population sample. Am. J. Psychiatry. 2011; 168 (9):904–912. [ PubMed ] [ Google Scholar ]
- Lai M.C., Baron-Cohen S. Identifying the lost generation of adults with autism spectrum conditions. Lancet Psychiatry. 2015; 2 (11):1013–1027. [ PubMed ] [ Google Scholar ]
- Lai M.C., Kassee C., Besney R., Bonato S., Hull L., Mandy W., et al. Prevalence of co-occurring mental health diagnoses in the autism population: a systematic review and meta-analysis. Lancet Psychiatry. 2019; 6 (10):819–829. [ PubMed ] [ Google Scholar ]
- Li Y.A., Chen Z.J., Li X.D., Gu M.H., Xia N., Gong C., et al. Epidemiology of autism spectrum disorders: Global burden of disease 2019 and bibliometric analysis of risk factors. Front. Pediatr. 2022; 10 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li Z., Yang L., Chen H., Fang Y., Zhang T., Yin X., et al. Global, regional and national burden of autism spectrum disorder from 1990 to 2019: results from the Global Burden of Disease Study 2019. Epidemiol. Psychiatr. Sci. 2022; 31 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liu Z., Jiang Y., Yuan H., Fang Q., Cai N., Suo C., et al. The trends in incidence of primary liver cancer caused by specific etiologies: Results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J. Hepatol. 2019; 70 (4):674–683. [ PubMed ] [ Google Scholar ]
- Liu J., Shi L., Meng Q., Khan M.M. Income-related inequality in health insurance coverage: analysis of China Health and Nutrition Survey of 2006 and 2009. Int. J. Equity Health. 2012; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Maenner M.J., Shaw K.A., Baio J., Washington A., Patrick M., DiRienzo M., et al. Prevalence of autism spectrum disorder among children aged 8 years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. MMWR Surveill. Summ. 2020; 69 (4):1–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Modabbernia A., Velthorst E., Reichenberg A. Environmental risk factors for autism: an evidence-based review of systematic reviews and meta-analyses. Mol Autism. 2017; 8 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pellicano E., Dinsmore A., Charman T. What should autism research focus upon? Community views and priorities from the United Kingdom. Autism. 2014; 18 (7):756–770. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peng R., Tong Y., Yang M., Wang J., Yang L., Zhu J., et al. Global burden and inequality of maternal and neonatal disorders: Based on data from the 2019 Global Burden of Disease study. QJM. 2023 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Salomon J.A., Haagsma J.A., Davis A., de Noordhout C.M., Polinder S., Havelaar A.H., et al. Disability weights for the Global Burden of Disease 2013 study. Lancet Glob. Health. 2015; 3 (11):e712–e723. [ PubMed ] [ Google Scholar ]
- Samms-Vaughan M.E. The status of early identification and early intervention in autism spectrum disorders in lower- and middle-income countries. Int. J. Speech Lang. Pathol. 2014; 16 (1):30–35. [ PubMed ] [ Google Scholar ]
- Solmi M., Song M., Yon D.K., Lee S.W., Fombonne E., Kim M.S., et al. Incidence, prevalence, and global burden of autism spectrum disorder from 1990 to 2019 across 204 countries. Mol. Psychiatry. 2022; 27 (10):4172–4180. [ PubMed ] [ Google Scholar ]
- Wagstaff A., Paci P., van Doorslaer E. On the measurement of inequalities in health. Soc. Sci. Med. 1991; 33 (5):545–557. [ PubMed ] [ Google Scholar ]
- Wang M., Gao H., Wang J., Cao C., Ying X., Wei Y., et al. Global burden and inequality of iron deficiency: findings from the Global Burden of Disease datasets 1990–2017. Nutr. J. 2022; 21 (1):16. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wu S., Wu F., Ding Y., Hou J., Bi J., Zhang Z. Advanced parental age and autism risk in children: a systematic review and meta-analysis. Acta Psychiatr. Scand. 2017; 135 (1):29–41. [ PubMed ] [ Google Scholar ]
- Zwaigenbaum L., Bryson S.E., Szatmari P., Brian J., Smith I.M., Roberts W., et al. Sex differences in children with autism spectrum disorder identified within a high-risk infant cohort. J. Autism Dev. Disord. 2012; 42 (12):2585–2596. [ PubMed ] [ Google Scholar ]
It is More Anxiousness than Role-playing: Social Camouflaging Conceptualization Among Adults on the Autism Spectrum Compared to Persons with Social Anxiety Disorder
- Original Article
- Open access
- Published: 06 June 2024
Cite this article
You have full access to this open access article

- Anna Pyszkowska ORCID: orcid.org/0000-0002-5041-7475 1
Purpose. Autistic individuals consider social camouflaging, e.g., masking autistic traits or social skills compensation, as exhausting and effortful, often leading to diminished well-being or burnout, as well as adaptive for satisfying social interactions. Developing camouflaging may result in isolation, social avoidance, increased self-stigmatization, and misdiagnosis, including social anxiety disorder. The study’s objective was to explore and conceptualize social camouflaging, with a particular focus on social anxiety symptoms, autistic burnout, and public stigma, among autistic individuals, with two comparative samples: with social anxiety disorder (SAD) and dual diagnoses (SAD + ASD). Methods. 254 individuals participated in the study (including 186 females, 148 with ASD diagnosis). CAT-Q, AQ-10, AASPIRE’s Autistic Burnout Scale, LSAS-SR, The Perceived Public Stigma Scale were used. Results. The findings suggest differences in the interrelation dynamics between the samples studied, with autistic burnout and social anxiety symptoms of essential significance in camouflaging strategies, and autistic traits being of secondary importance. Structural equation models showed that the proposed conceptualization, with camouflaging and autistic burnout as the outcome variables, exhibited acceptable fit, implying that this strategy is costly and may result in exhaustion. Conclusion. The total score of camouflaging did not differ between the groups studied, suggesting that a tendency to camouflage is rather transdiagnostic, deriving from anxiousness and negative self-perception, not being autistic per se.
Similar content being viewed by others
“putting on my best normal”: social camouflaging in adults with autism spectrum conditions.

Is social camouflaging associated with anxiety and depression in autistic adults?
Understanding the Reasons, Contexts and Costs of Camouflaging for Autistic Adults
Avoid common mistakes on your manuscript.

Introduction
Autism spectrum disorder (ASD) is considered a heterogeneous phenomenon, and it has been suggested that it might share a common etiopathological root with other psychiatric disorders and be the risk factor for developing mental health issues (Dell’Osso et al., 2019 ). Despite several studies proving that autistic traits are associated with higher anxiety, stress, (Hull et al., 2021b ), suicidal ideations, and trauma-related experiences, these are not caused directly by autistic features (e.g., limited social skills, sensory sensitivity, and diminished executive functions) but are a reaction to the lack of ability to adapt to a non-autistic, often maladjusted, environment (Raymaker et al., 2020 ). In turn, the autism spectrum is associated with an increased prevalence of psychiatric disorders (Rosen et al., 2018 ), with overlapping diagnoses of 70% in this population. Therefore, a differentiation diagnosis between ASD and other disorders is challenging and yet to be fully understood, resulting in misdiagnoses, such as personality disorders (Iversen & Kildahl, 2022 ), social anxiety (Gesi et al., 2021 ), psychotic disorders (Demetriou et al., 2020 ), or delayed diagnosis in adulthood. Females are more likely to receive a delayed diagnosis or a misdiagnosis, with an average time lapse between first contact with mental health care and proper ASD diagnosis being eight-ten years (Gesi et al., 2021 ).
One of the potential reasons for a misdiagnosis is social camouflaging. The current literature depicts camouflaging in various behavioral contexts, characterizing it as a combination of (1) masking of autistic traits (e.g., refraining from self-stimulation), (2) social skills compensation (e.g., employing scripts for different social scenarios), and (3) assimilation to social situations (e.g., forcing oneself to develop a small-talk) (Hull et al., 2017 ). Livingston and Happe ( 2017 ) point out that compensation may be exhibited in deep or shallow form. The former is based on one’s executive functions and is more intuitive (e.g., based on one’s good memory), when the latter is more rigid and unintuitive (e.g., mimicking others’ behaviors without understanding the context). Research implies that females more often develop camouflaging, obtaining this strategy across more situations and for more of the time than males (Cassidy et al., 2018 ), affecting the diagnosis ratio. However, it does not mean that fewer females meet the diagnostic criteria; instead, they may elude traditional diagnostic methods that do not consider camouflage (Rynkiewicz et al., 2016 ).
Autistic individuals consider camouflaging as exhausting and effortful, often leading to diminished well-being (Cook et al., 2021 ) or burnout (Hull et al., 2017 ; Raymaker et al., 2020 ), and adaptive for developing satisfying social interactions (Miller et al., 2021 ; Bradley et al., 2021 ). A recurrent theme in camouflaging-related reports is inauthenticity, described as performing or playing a role (Livingston et al., 2019 ), which often results in the inability to meet (or acknowledge) other autistic people and, in turn, disallows for normalization of one’s experiences (Cook et al., 2022 ). In sum, camouflaging’s impact on well-being and self-perception depends on various contexts and motivations (Hull et al., 2021b ). It is rather dialectic than dichotomic: persons on the spectrum implement strategies to navigate social contexts and blend into the environment, also mask their autistic traits due to stigma experiences or fear of exclusion (Petrolini et al., 2023 ). Researchers highlight that as the autistic spectrum is broad and heterogeneous, so is camouflaging. Therefore, not all autistic individuals experience camouflaging as unfavorable, e.g., those who face more visible autistic traits and thus are not in the position to hide or engage in deep compensation moves (Petrolini et al., 2023 ).
Perry et al. ( 2021 ) propose interpreting camouflaging through the lens of the “passing” phenomenon. Passing is a sociology-based construct referring to a person’s ability to be regarded as a member of an identity group or category different from their own (Goffman, 1963 ). A motivation to “pass” as non-autistic may derive from negative experiences from the past, acceptance seeking, or internalized stigma (treating negative stereotypes about autism as truth and incorporating them as beliefs about oneself). Given that persons on the autism spectrum often present self-stigmatizing beliefs (e.g., “Being autistic means I am worse than others”), camouflaging would be a consequence of negative self-perception and act as its behavioral manifestation (e.g., “I should be less autistic to be liked/accepted” would lead to camouflaging). Perry et al. ( 2021 ) propose considering camouflaging in this population via a Social Identity Framework (SIT; Tajfel & Turner, 2004 ), which suggests that group members seek to regain a positive identity through individualistic and collective strategies when a group is stigmatized. This proposition aligns with findings that masking autistic traits were associated with increased internalized stigmatization and discrimination (Botha & Frost, 2020 ); high autistic identification and open disclosure of one’s diagnosis are reported to be associated with reduced camouflaging strategies (Cage & Troxell-Whitman, 2020 ). Of note, self-stigmatization may comprise public stigma, including stereotypical beliefs and prejudicial attitudes endorsed by a sizable group in society toward a discredited subgroup (Corrigan & Watson, 2002 ).
Social camouflaging may result in isolation and social avoidance (Cook et al., 2021 ), maintaining a widespread misconception regarding autistic people’s preference for solitude and needlessness for social relationships (Maddox & White, 2015 ). It is suggested that social isolation experienced by many autistic individuals may be mainly due to a lack of interpersonal skills (Maddox & White, 2015 ) or discrimination experiences (Perry et al., 2021 ) rather than a lack of desire for relationships. Therefore, a growing body of research reports co-occurrence between autism spectrum and social anxiety disorder (SAD) (Espelöer et al., 2021 ). SAD is characterized in DSM-5 as “a persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or possible scrutiny by others. The individual fears that they will act in a way that will be embarrassing and humiliating” (APA, 2013). SAD is often misdiagnosed for ASD: autistic persons fulfill some of the SAD criteria as they tend to avoid social situations due to fear of negative evaluation and experience physiological symptoms in social situations (e.g., blushing, trembling; Espelöer et al., 2021 ). However, according to DSM-5 and cognitive-behavioral models (Clark & Wells, 1995 ), SAD occurs when a person experiences the symptoms excessively and inadequately to the real risk of embarrassment – which in the case of autistic people is debatable as they are at factual risk of discrimination. Spain et al.’s ( 2018 ) meta-analysis showed that a handful of studies displayed a significant overlap between social anxiety and low social competencies, including verbal competencies or social context understanding, with people with a diagnosis of SAD (without ASD) showed lower social competences than people with ASD (without SAD). It may suggest that it is the issue of competence, and not the diagnosis itself, that is crucial for fear expression. Therefore, in differential diagnosis, it is fundamental to determine whether the fear is adequate or justified (e.g., due to prior experiences of discrimination; Botha & Frost, 2020 ), results from a lack of social skills (deriving from autistic traits, not SAD; Spain et al., 2018 ), or from the fear of social evaluation and self-embarrassment (which would indicate the presence of SAD; Hull et al., 2021b ). A scarce body of literature regarding camouflaging and SAD symptoms reports mixed results, as some (Hull et al., 2019 , 2021b ) point to significant relationships, while others (Shuck et al., 2019; Lai et al., 2017 ) report contrary.
Based on prior literature and clinical research, the focus of the current study was to present a hypothetical conceptualization model of social camouflaging. It is proposed to conceptualize social camouflaging as the behavioral effect of interactions between specific autism spectrum traits, one’s negative social experiences, and self-perception (e.g., negative self-esteem, fear of social failure). Therefore, social camouflaging may derive from negative experiences (including discrimination), diminished social skills (poor theory of mind, reactions considered inadequate by non-autistic peers), and self-esteem (e.g., self-criticism and self-stigma) that lead to social avoidance and social anxiety symptoms (e.g., fear of failure, anxiousness around other people). Notably, social anxiety is associated with social perfectionism, exhibiting inaccurate or impossible to achieve social goals regarding one’s reaction or perception by others (Clark & Wells, 1995 ). As persons on the autism spectrum display high rates of perfectionism and control demand (Dupuis et al., 2022 ), this specific aspect of social anxiety may play a significant role in developing a specific need to match with the environment and analyzing what behavior is expected (and rewarded) by others. In turn, avoidance backfires on diminished social skills, while anxiety increases feelings of incompetence and self-criticism. Additionally, social camouflaging, requiring constant social observation and responding in an unintuitive, non-autistic manner, may develop exhaustion and sensory burnout (autistic burnout, Raymaker et al., 2020 ), causing yet another decline in social skills resulting from overload. In this case, camouflaging would not be described solely as a compensation strategy as it is motivated by negative experiences and self-perception, not by thriving for self-development or a sense of belonging (Perry et al., 2021 ; Petrolini et al., 2023 ). A hypothesized model explaining relationships that result in social camouflaging is presented below [Fig. 1 ].
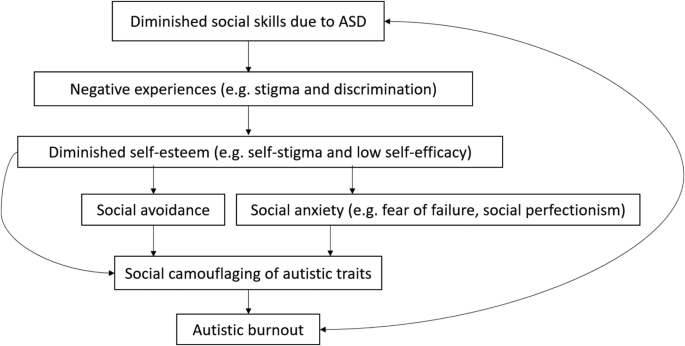
Proposed camouflaging conceptualization
The Current Study
The study’s main objective was to explore and conceptualize the psychological mechanisms explaining social camouflaging in persons on the autism spectrum, with a particular focus on social anxiety symptoms. As social camouflaging derives from social discomfort and fear of exclusion (Cook et al., 2021 ), it was decided to frame an additional, comparative group consisting of individuals with social anxiety disorder diagnosis. Due to common comorbidity (Rosen et al., 2018 ), a third group of persons with both diagnoses was also devised. Two research goals were formulated. First, to establish differences in social camouflaging features (masking, assimilation, compensation), autistic traits, autistic burnout, social anxiety symptoms (anxiety and avoidance), and social contexts (public stigma) among adult individuals on the autism spectrum, with SAD, or both diagnoses (ASD + SAD). Second, to evaluate associations and determinants of camouflaging based on symptomatology and social contexts, rather than mere diagnosis, (a) a structural equation modeling, and (b) network analysis were designed to shape possible interactions between camouflaging traits and autistic and/or social anxiety factors. As the network approach focuses on studying the dynamics and structure of behavioral systems (Kobourov, 2012 ), it was hypothesized that it would be more accurate for establishing links between variables in the current study’s question.
Participants
The inclusion criteria for the study were: (1) a declaration of a formal diagnosis of autism spectrum disorder (ASD), or social anxiety disorder (SAD), or both (ASD + SAD); (2) being without an intellectual disability (IQ < 70); (3) being fluent in the Polish language. Due to the high comorbidity of ASD and SAD with other mental health issues (Rosen et al., 2018 ), the participants were asked to provide additional information in that matter. Persons declaring a self-diagnosis were excluded from the sample. Participants were recruited online through groups and societies aimed at autistic individuals, and stationary mental health facilities in Silesia, Poland (psychiatric and psychotherapeutic offices, outpatient departments). Participants interested in the project filled out an online form via LimeSurvey. The recruitment took place in autumn 2022. All participants provided written informed consent before enrolment in the study. The study was voluntary and unpaid, although all participants were eligible to leave their contact address through a non-affiliated and anonymous link to participate in further paid qualitative studies from this area.
The autism community was involved in the theoretical background of the camouflaging conceptualization, including examples of camouflaging’s effects on exhaustion, social avoidance, and burnout.
Two hundred fifty-four persons participated in the study, including 186 female. One hundred forty-eight participants were on the autism spectrum, declaring having an autism spectrum disorder (ASD) diagnosis, 65 had a SAD diagnosis, and 45 declared ASD + SAD diagnoses. The summary of group characteristics is presented in Table 1 .
Due to the sociocultural context and population homogeneity, as the research was conducted in Poland among Polish participants, data on race/ethnicity status was not recorded.
Measurements
Camouflaging. The Camouflaging Autistic Traits Questionnaire (CAT-Q, Hull et al., 2019 ) was used. It consists of 25 items (e.g., “In social situations, I feel like I’m “performing” rather than being myself”), rated on a 1 (definitely disagree) to 7 (definitely agree) scale, regarding three subtypes of camouflaging: compensation, masking, assimilation. The reliability rates for the current study were: (a) total score α = 0.70, ώ=0.70, (b) compensation α = 0.81, ώ=0.82, (c) masking α = 0.74, ώ=0.75, (d) assimilation α = 0.81, ώ=0.82.
Autistic traits. The Autism Quotient-10 (AQ-10, Allison et al., 2012 ) was used. The scale consists of 10 items (“I find it difficult to work out people’s intentions”); in the current study, a four-point response scale was used (Bertrams, 2021 ). The reliability rates for the current study were: α = 0.68, ώ=0.70, in line with previous works regarding AQ-10 internal reliability and homogeneity (Bertrams, 2021 ; Taylor et al., 2020 ).
Autistic burnout. The AASPIRE’s Autistic Burnout Scale (Raymaker et al., unpublished, Polish version by Pyszkowska) was used. The scale consists of 27 items (e.g., “In the past three months, I’ve had a harder time tolerating sensory input than I usually do”), rated from 0 (strongly disagree) to 4 (strongly agree). It has been assessed and used by Arnold et al. ( 2023 ) to conceptualize autistic burnout in an adult autistic population. The reliability rates for the current study were: α = 0.95, ώ=0.95.
Social anxiety features. The Liebowitz Social Anxiety Scale (LSAS-SR; Liebowitz, 1987 ) was used, consisting of examples of 24 social situations (e.g., working while being observed) that are each rated for level of fear from 0 (none) to 3 (severe) and avoidance from 0 (none) to 3 (usually) for the past week. The reliability rates for the current study were: (a) social fear α = 0.86, ώ=0.86, (b) social avoidance α = 0.84, ώ=0.84. The LSAS-SR was previously used in the autistic population, proving satisfactory reliability scores (Bejerot et al., 2014 ).
Public stigma. The Perceived Public Stigma Scale (PPSS; Chan & Lam, 2017 , Polish translation by Pyszkowska, Rożnawski, & Farny, 2021 ). The Scale contained eight items (e.g., “Most people feel that having an ASD is a sign of personal failure”) adapted from Green’s (2001) study. The items were rated on a six-point Likert scale ranging from 0 (strongly disagree) to 5 (strongly agree). To the author’s knowledge, the scale has not been used in the autistic population before (although it was used in the population of parents of children with ASD, e.g., Pyszkowska et al., 2021; Chan & Lam, 2017 ). The reliability rates for the current study were: α = 0.70, ώ=0.70.
Data Analysis
Correlations were conducted using Kendall’s tau b (Shober et al., 2018). Analysis of variance (ANOVA) was applied to compare differences between three groups (ASD, SAD, ASD + SAD) regarding variables studied, using mean square and F (variation between sample means / variation within the samples) values. Post-hoc Bonferroni corrections were used for significant differences using the bootstrap method for 10,000 samples.
Structural equation modeling (SEM) was designed to establish the significance of models predicting camouflaging and autistic burnout, as mentioned in the conceptualization model above. In this case, only data from persons with ASD or ASD + SAD samples was used. It was decided to perform variance-based SEM (VB-SEM) in partial least squares structural equation modeling (PLS-SEM, Hair et al., 2019 ). The current study’s design encountered circumstances predisposing to VB-SEM: (1) relatively small sample, (2) exploratory design, (3) correct model specification cannot be ensured (Wong, 2010 ). PLS-SEM estimates partial model structures by combining principal components analysis with ordinary least squares regressions (Mateos-Aparicio, 2011 ). Latent variables are composed of items (“indicators”), with the indicator’s satisfactory reliability being > 0.70 or higher (in exploratory research, it is > 0.40, e.g., Hulland, 1999 ), and convergent validity (average variance extracted, AVE) being higher than 0.50 (Bagozzi & Yi, 1988). Standardized Root Mean Square Residual (SRMR) was the indicator of the model’s fit, with values less than 0.10 or 0.08 (in a more conservative version; Hu & Bentler, 1998 ) considered a good fit. To assess collinearity issues of the inner model, Variance Inflation Factor (VIF) values were obtained, with VIF values being 5 or lower to avoid the collinearity problem (Hair et al., 2010). Two PLS-SEM models were performed: (1) factors predicting camouflaging with a total score, (2) factors predicting three features of camouflaging: masking, compensation, assimilation. Variables standardization and the bootstrap method with 10,000 samples were applied.
To perform network analysis, signed weighted concentration (partial correlation) networks were created using the Qgraph package of JASP software with an EBICglasso estimator. Regularized Gaussian graphical models (GGMs, cf. Costantini et al., 2015 ) were used in the analysis, assuming no common latent variables. GGMs focus on the interplay between observable components (the network) and their role in shifting behavior. In this approach, “nodes” are the independent variables, and “edges” are partial correlation coefficients between the variables, indicating conditional dependence (potential causality) between the nodes they connect (Kobourov, 2012 ). Three nodes were selected for the current study: (1) camouflaging factors (masking, assimilation, compensation), (2) autistic factors (AQ total score, autistic burnout), and (3) social anxiety factors (anxiety, avoidance). Qgraph’s “spring” layout was used to render networks. Thinner edges represented weaker coefficients while thicker – stronger ones (Kobourov, 2012 ). The bootstrap method for 10,000 samples was also applied.
Calculations were made using the JASP 0.12.2.0 statistical package (University of Amsterdam, Amsterdam, The Netherlands, 2018); for the PLS-SEM, SmartPLS 4.0.8.5. version was used. An α level of 0.05 was considered statistically significant for all statistical tests.
First, Kendall’s tau b correlation analysis was conducted on a total sample. The results are presented in Table 2 , including a normality test result ( W Shapiro-Wilk’s normality test).
The total score of camouflaging correlated moderately and significantly with autistic burnout ( tau = 0.30, p < .001), and both factors of social anxiety (anxiety symptoms tau = 0.29, p < .001, avoidance symptoms tau = 0.30, p < .001); weak associations were established with autistic traits ( tau = 0.16, p < .001) and public stigma ( tau = 0.19, p < .001). The compensation feature of camouflaging was the strongest correlate of autistic traits ( tau = 0.25, p < .001); the assimilation feature showed moderate associations with both symptoms of social anxiety (anxiety tau = 0.38, p < .001; avoidance tau = 0.37, p < .001). Public stigma was associated with assimilation ( tau = 0.20, p < .001) and both features of SAD (anxiety tau = 0.21, p < .001; avoidance tau = 0.20, p < .001) but exhibited an insignificant ( p > .05) relationship with autistic traits.
Then, a comparison of three subgroups was performed using an ANOVA analysis. The results are summarized in Table 3 .
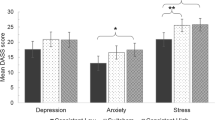
The total score of camouflaging and pubic stigma did not differentiate the subgroups. The compensation feature of camouflaging was significantly higher in persons on the autism spectrum, regardless of SAD. The masking feature was significantly higher among persons with only SAD. The assimilation feature was significantly higher among all persons with SAD, regardless of autism. Autistic traits, assessed by the AQ total score, were significantly higher among persons on the autism spectrum, and even higher for those who also had SAD. Autistic burnout was significantly higher in persons with both autism and SAD when compared to persons with either alone. When compared to autism alone, both social anxiety disorder factors were significantly higher among persons with SAD and highest among those with both SAD and autism.
In the next step, partial least squares structural equation modeling (PLS-SEM) was applied to verify the fitness of two models predicting camouflaging. The models were designed based on the proposed camouflaging and autistic burnout conceptualization presented in the Introduction section, therefore only ASD and ASD + SAD subgroups were used in this calculation ( N = 193). In both models, autistic traits, public stigma, social anxiety and social avoidance were predictors of camouflaging and autistic burnout. Model a used a total score of CAT-Q, and model b used scores of three camouflaging features (masking, assimilation, compensation). Fig. 2 (model a ) and Fig. 3 (model b ) show the PLS path modeling estimations.

Partial least squares structural equation modeling results for model a

Partial least squares structural equation modeling results for model b
For model a , the results showed that the model tested explained 11.5% of camouflaging total score and 10.7% of autistic burnout. The model showed acceptable fit with Standardized Root Mean Square Residual (SRMR) factor = 0.087. Indicators’ reliability and validity were obtained. Most outer loadings scored higher than 0.70 with five two below (PSS4 = 0.671, CAT-Q3 = 0.638, LSAS21 for social avoidance = 0.653, AQ9 = 0.408), and AVE scores being higher than 0.50. Public stigma predicted both social anxiety ( β = 0.284, p < .05) and social avoidance ( β = 0.220, p < .05). The strongest predictors of camouflaging were public stigma, with β = 0.192 ( p < .05), and social avoidance, with β = 0.177 ( p < .05). Camouflaging showed a substantial effect on autistic burnout ( β = 0.327, p < .05). Autistic traits showed little effect on public stigma, with β =-0.041 ( p > .05).
In model b ’s case, the results showed that the model tested explained 15.6% of masking, 9.1% of compensation, 25.4% of assimilation, and 15.8% of autistic burnout. The model showed acceptable fit with Standardized Root Mean Square Residual (SRMR) factor = 0.090. Indicators’ reliability and validity were obtained. Most outer loadings scored higher than 0.70 with nine below (AQ6 = 0.408, LSAS24 for social anxiety = 0.679, PSS4 = 0.684, LSAS24 for social avoidance = 0.665, CAT-Q3 = 0.612, CAT-Q4 = 0.698, CAT-Q9 = 0.673, CAT-Q10 = 0.628), and AVE scores being higher than 0.50. Social avoidance most strongly predicted masking ( β = 0.255, p < .05). In contrast, social anxiety showed the highest effect on assimilation ( β = 0.286, p < .05). Public stigma showed similar effects on all camouflaging’s features ( β s range from 0.119 in compensation to 0.151 in assimilation, p s < 0.05). Assimilation showed the strongest effect on autistic burnout ( β = 0.289, p < .05). Similarly to model a , autistic traits showed little effect on public stigma, with β = − 0.040 ( p > .05).
To outline possible interactions between significant variables (camouflaging, autistic traits, autistic burnout, social anxiety factors), network analyses were applied for three subgroups: (1) autism spectrum, (2) social anxiety disorder, (3) both diagnoses. Pink nodes represented camouflaging factors (1. compensation, 2. masking, 3. assimilation), green nodes autistic factors (4. autistic traits, 5. autistic burnout), and blue nodes – anxiety factors (6. avoidance symptoms, 7. anxiety symptoms). Fig. 4 presents network plots, and Fig. 5 centrality plots for the three groups studied.

Network plots

Centrality plots
In the autism spectrum network, autistic traits scored the highest expected influence ( EI =-1.753), while in the SAD network, it was the masking feature of camouflaging ( EI =-1.423); in a network of ASD + SAD’s highest expected influence was affective (anxiety) factor of social anxiety ( EI = 1.693). The autism spectrum (sparsity = 0.238) and SAD (sparsity = 0.238) networks showed 16 non-zero edges, while the ASD + SAD diagnoses network showed only 2 (sparsity = 0.905). Each of the camouflaging factors was connected with autistic burnout and autistic traits on a similar level (0.25-0.28), with masking presenting a negative relation with autism quotient score (-0.25). No connections with social anxiety affective (anxiety) factor were obtained. In contrast, the social anxiety avoidance factor was related to the assimilation feature of camouflaging (0.22). Similar results were obtained in a SAD network. However, with differences in relations between social anxiety affective (anxiety symptoms) factor being associated with compensation (0.17) and assimilation (0.06), avoidance factor of SAD being related to autistic burnout symptoms (0.13), and affective factor with autistic traits (0.14). In a network consisting of persons with both diagnoses, the only relation was between social anxiety affective (anxiety) factor and assimilation (0.13).
The present study’s objective was to explore and conceptualize links between social camouflaging and social anxiety symptoms in adults on the autism spectrum compared to persons with social anxiety disorders. The total score of camouflaging did not differ between the groups studied (although ASD + SAD sample scored significantly higher in masking and assimilation), suggesting that a tendency to camouflage is rather transdiagnostic, deriving from anxiousness and negative self-perception, not from being autistic per se. Additionally, the findings suggest that autistic burnout and social anxiety symptoms are significant in camouflaging strategies, with autistic traits being of secondary importance. The path analysis exhibited an acceptable fit in the conceptualization model proposed, with autistic burnout being an outcome variable predicted by public stigma, social anxiety symptoms, and camouflaging. These results allow for clinical implications and future research directions, limitations are also discussed.
Differences Between ASD, SAD, and ASD + SAD Samples
Masking and assimilation features of camouflaging were significantly higher among persons with social anxiety disorder and dual diagnoses (ASD + SAD). It is worth noting that both of these factors are associated with behavioral outcomes and specific strategies (e.g., social observations and appropriate social responses in assimilation, holding back from stimming, etc.). On the other hand, compensation was significantly higher in the ASD group as it is represented by behavioral modifications made by autistic individuals to blend into social situations. These comparative analyses seem to align with Espelöer et al.’s ( 2021 ) research reporting that social anxiety symptoms in individuals with ASD are primarily based on deficits in social competence, and the symptoms associated with both diagnoses run like a vicious circle. In this light, another finding in the current study seems understandable, as persons with ASD + SAD scored significantly highest in social anxiety symptoms and autistic traits.
Although it was marginally significant ( p = .052), autistic burnout was highest in persons with ASD + SAD, acting as a constant predictor and correlate of camouflaging, showing significance in relationships with all its features. Interestingly, it was not associated with the AQ score through network analysis in the ASD sample (with weak association in the SAD sample), although it was linked with camouflaging and anxiety (in an ASD sample) and avoidance (in the SAD sample) symptoms. Therefore, these results support a hypothesis that the burnout experienced by persons in the ASD population may be due to personal and environmental demands (including stigma and discrimination), diminished well-being, and mental strain (including anxiousness and distress), being in accordance with Mantzalas et al.’s (2022) conceptual model for autistic burnout. In that model, “personal demands” include masking or camouflaging, sensory sensitiveness, and autistic traits – all factors were interrelated in the current study, proving that these dynamics may affect each other. Additionally, these results suggest that a measurement of “autistic burnout” (e.g., AASPIRE’s Autistic Burnout Scale used in this study) may be, in fact, a measure of sensory or cognitive overload that may appear in different contexts and psychopathologies (e.g., SAD). Therefore, further studies should focus on more specific aspects of the “autistic” aspects of burnout experienced in the result of social exhaustion (Arnold et al., 2023 ).
Conceptualization Model Verification
Structural equation models showed that the proposed conceptualization, with camouflaging and autistic burnout as the outcome variables, exhibited an acceptable fit. However, it must be highlighted that it was on the verge of acceptability (0.09-0.08, cf. Hu & Bentler 1998 ). Autistic traits exhibited minimal prediction of public stigma (less than 1%), yet public stigma predicted 8% of social anxiety and 4% of social avoidance. The effects of public stigma and SAD features varied in terms of the camouflaging total score and individual camouflaging features: assimilation was predicted most strongly (25%) and compensation least strongly (9%) by the model tested, with a combined CAT-Q score being predicted by 11%. These results suggest that camouflaging should be considered a complex behavioral strategy with a specific function of its features, consistent with previous works by Jorgenson et al. ( 2020 ) or Bernardin et al. ( 2021 ). Furthermore, in both models tested, camouflaging resulted significantly in autistic burnout, implying that this strategy (or each of the strategies presented in camouflaging) is costly and may result in exhaustion. The models did not point to the importance of autistic traits in either camouflaging or public stigma, which – according to previous research (e.g. Botha & Frost, 2020 ; Perry et al., 2021 ) – shows that negative self-perception and strategies to “pass” as non-autistic most significantly derives from environmental factors, not “autistic traits”.
In line with previous works, a masking feature of camouflaging exhibited negative associations with autistic traits (Wiskerke et al., 2018 ). As masking is related to the suppression of autism-related behaviors (e.g., motor stereotypies) and/or intentionally exhibiting neurotypical behaviors (e.g., maintaining eye contact), persons who use masking may appear as “non-autistic”. Of note, masking was positively associated with autistic burnout, highlighting that it requires cognitive and behavioral effort, resulting in exhaustion. No anxiety symptoms were significant in relationships with masking, perhaps due to being related to social demands of “passing” as non-autistic and coming as a natural social reaction for many autistic individuals (Raymaker et al., 2020 ; Hull et al., 2017 ). Further research in this area is needed. With autistic traits showing the highest negative expected influence in the ASD sample, it can be hypothesized that the dynamics between camouflaging, social anxiety, and autistic burnout vary in terms of autistic symptoms’ intensification – as proposed by Petrolini et al. ( 2023 ) or Kapp et al. ( 2019 ) who highlight that the engagement in camouflaging strategies may be affected by one’s social skills or executive functions.
Assimilation was the feature strongest predicted by social anxiety. These results may imply that assimilation – understood as putting one’s effort into fitting in and not being recognized as “different” (Hull et al., 2019 ) – derives from the fear of standing out and behaviors obtained in this strategy may be used to “pass” as a neurotypical (Perry et al., 2021 ). However, while actions such as forcing oneself to talk to a stranger or attending a crowded party enable one to pass as non-autistic (or less autistic) and partially improve social interactions, it can be dissonant and unauthentic (ego-dystonic) and motivated by fear (of rejection, stigmatization, etc.), not harmonious to one’s values and needs (ego-syntonic). Therefore, it can be sensory and cognitively exhausting, and – according to prior research in line with the current study – results in diminished well-being and overload (Cook et al., 2021 ; Raymaker et al., 2020 ). However, it should be noted that these outcomes do not contradict the fact that autistic individuals long for connection and sense of belonging, engaging in socializing and assimilating to their social environment (Cage & Troxell-Whitman, 2020 ) – even if it may result in overstimulation or masking.
The results partially confirm the assumptions regarding the relationships between social camouflaging, public stigma, social anxiety symptoms, and autistic burnout. Consistently with a hypothesized conceptualization, camouflaging exhibited higher associations with autistic burnout than autistic traits. Similarly, a total camouflaging score correlated more with social anxiety symptoms (fear and avoidance) and public stigma than the AQ-10 total score. Public stigma displayed no significance in relationship with autistic traits. However, it was correlated with autistic burnout, all features of camouflaging, and both aspects of SAD symptoms being of particular importance in predicting assimilation camouflaging. Additionally, the total score of camouflaging did not differ between the groups studied, while masking and assimilation tendencies were higher among persons with a SAD diagnosis, with compensation being significantly higher among individuals with the ASD diagnosis. These results may suggest that the presence of the autistic traits (or ASD diagnosis) may be less relevant for engaging in a camouflaging strategy and result from a combination of sensory overload, social anxiety symptoms, and negative self-concept (Raymaker et al., 2020 ; Hull et al., 2021b ), not being a part of the autistic phenotype itself. Further research regarding camouflaging should be conducted on various non-autistic populations to compare these strategies.
Limitations
Despite its strengths, the current study had its limitations. First, due to the study’s exploratory nature and cross-sectional design, the results cannot be generalized, and the hypothesized camouflaging conceptualization cannot be approved or declined based on the current research. However, the outcomes seem promising and prepare the ground for further examinations, especially in the experimental design. Second, the sample was unbalanced and homogenous, comprised of mostly white, employed or student-enrolled adults living in Poland, dominated by females. Although camouflaging appears more often in women (Cook et al., 2021 ), it seems necessary to further understand male and non-binary perspectives as they seem highly underrepresented in the current camouflaging literature. The sample’s diagnoses were also unbalanced, with a dominance of the ASD group. The population studied experienced public stigma in a Polish context (e.g., low social awareness about the autism spectrum or mental health; common beliefs that one cannot stand out; diminished tolerance for any differences, cf. Pisula et al., 2024 ) and further research needs to focus on how it manifests in different countries or cultures. However, it needs to be highlighted that vast majority of previous research in this area was conducted in the Anglo-Saxon context hence the current study significantly adds to the existing knowledge in this area. Another issue that needs to be addressed is the small number of measurements aimed at different symptoms or factors of ASD/SAD, which disallows for a deeper understanding of specific aspects significant for developing camouflaging strategies (e.g., empathizing vs. systemizing, social perfectionism, fear of failure, etc.). In that context, the use of the AQ-10, a standard measure of autistic traits in research, was understandable but posed difficulties in terms of unsatisfactory reliability rates (α = 0.68, ώ=0.70), which was in line with previous works regarding internal reliability and homogeneity issues (Bertrams, 2021 ). Additionally, AQ-10 was used in all three samples, with the average score of each group was more than 6 (in a SAD sample it was M = 6.27) indicating that the cut-off point of the scale was exceeded. It is consistent with Taylor et al.’s ( 2020 ) work that highlighted that AQ-10 is not a psychometrically robust measure when used in non-autistic samples.
Clinical Implications and Future Research Directions
The abovementioned findings and limitations allow for distinguishing clinical implications and future research directions. Given that camouflaging was exhibited by all samples studied, this issue should be addressed in working with persons experiencing social anxiety or other social difficulties. Additionally, a context of camouflaging strategy used by autistic individuals should be conceptualized by mental health professionals: whether it is driven by anxiety and fear of rejection or stigma, compensation for social skills, or a way to achieve one’s social or professional goals. Based on that context camouflaging can be assessed as beneficial or maintaining one’s suffering. Furthermore, psycho-education regarding potential advantages (e.g., assimilating to environment, social acceptance) as well as costs (e.g., burnout, risks of developing negative self-image, including self-stigma) of camouflaging should be discussed while working with autistic individuals. In sum, the context and function of camouflaging should always be defined, especially that it can vary in different circumstances and fulfill various needs (or cause symptoms and distress to persist). Considering that autistic burnout was an outcome of camouflaging, additional interventions aimed at emotional regulation and sensory overload-related self-care should be applied (e.g., dialectical-behavioral therapy, DBT, Ritschel et al., 2022 ).
As camouflaging is a multifaceted behavioral strategy, it must be observed through experimental, not only cross-sectional, lenses: an additional research area should be addressed, focusing on therapeutic approaches to develop self-acceptance, social skills, self-regulation, and sensory overload-related regulation. In turn, further observations should be focused on whether these abilities would affect camouflaging strategies in both ASD and SAD populations. Additionally, as camouflaging is mainly associated with females, it should be considered to develop a further understanding of males’ and non-binary functioning in this area. As the total score of camouflaging did not differ between the ASD and SAD samples, it is suggested to broaden the focus on this strategy among persons with social anxiety. Lastly, as the concept of “camouflaging” is not heterogenous and its features vary in terms of dynamics with different psychological variables, future research should aim at specific aspects of camouflaging to verify the pros and cons of applying this strategy among individuals with difficulties with social interactions.
Allison, C., Auyeung, B., & Baron-Cohen, S. (2012). Toward brief red flags for autism screening: The short autism spectrum quotient and quantitative checklist in 1,000 cases and 3,000 controls. Journal of the American Academy of Child and Adolescent Psychiatry , 51 , 202–212e7. https://doi.org/10.1016/j.jaac.2011.11.003 .
Article PubMed Google Scholar
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.) https://doi.org/10.1176/appi.books.9780890425596 .
Arnold, S. R., Higgins, J. M., Weise, J., Desai, A., Pellicano, E., & Trollor, J. N. (2023). Towards the measurement of autistic burnout. Autism , 27 (7), 1933–1948. https://doi.org/10.1177/13623613221147401 .
Bejerot, S., Eriksson, J. M., & Mörtberg, E. (2014). Social anxiety in adult autism spectrum disorder. Psychiatry Research , 220 (1–2), 705–707. https://doi.org/10.1016/j.psychres.2014.08.030 .
Bernardin, C. J., Mason, E., Lewis, T., et al. (2021). You must become a Chameleon to survive: Adolescent experiences of camouflaging. Journal of Autism and Developmental Disorders , 51 , 4422–4435.
Bertrams, A. (2021). Internal reliability, homogeneity, and factor structure of the ten-item autism-spectrum quotient (AQ-10) with two additional response categories. Experimental Results , 2 , E3. https://doi.org/10.1017/exp.2020.70 .
Article Google Scholar
Botha, M., & Frost, D. M. (2020). Extending the minority stress model to understand mental health problems experienced by the autistic population. Society and Mental Health , 10 (1), 20–34. https://doi.org/10.1177/2156869318804297 .
Bradley, L., Shaw, R., Baron-Cohen, S., & Cassidy, S. (2021). Autistic adults’ experiences of camouflaging and its perceived impact on mental health. Autism in Adulthood , 3 (4), 320–329.
Article PubMed PubMed Central Google Scholar
Cage, E., & Troxell-Whitman, Z. (2020). Understanding the relationships between autistic identity, disclosure, and camouflaging. Autism in Adulthood , 2 (4), 334–338. https://doi.org/10.1089/aut.2020.0016 .
Cassidy, S., Bradley, L., Shaw, R. (2018). Risk markers for suicidality in autistic adults. Molecular Autism, 9 , 42 (2018). https://doi.org/10.1186/s13229-018-0226-4 .
Chan, K. K. S., & Lam, C. B. (2017). Trait Mindfulness attenuates the adverse psychological impact of Stigma on parents of children with Autism Spectrum Disorder. Mindfulness , 8 , 984–994. https://doi.org/10.1007/s12671-016-0675-9 .
Clark, D. M., & Wells, A. A. (1995). Cognitive model of Social Phobia . Guilford Press.
Cook, J., Crane, L., Hull, L., Bourne, L., & Mandy, W. (2022). Self-reported camouflaging behaviours used by autistic adults during everyday social interactions. Autism, 26 (2), 406–421. https://doi.org/10.1177/13623613211026754
Cook, J., Hull, L., Crane, L., & Mandy, W. (2021). Camouflaging in autism: A systematic review. Clinical Psychology Review , 89 , 102080. https://doi.org/10.1016/j.cpr.2021.102080 .
Corrigan, P. W., & Watson, A. C. (2002). The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice , 9 (1), 35–53. https://doi.org/10.1093/clipsy.9.1.35 .
Costantini, G., Epskamp, S., Borsboom, D., Perugini, M., Mõttus, R., Waldorp, L. J., & Cramer, A. O. J. (2015). State of the aRt personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality , 54 , 13–29. https://doi.org/10.1016/j.jrp.2014.07.003 .
Dell’Osso, L., Carpita, B., Muti, D., Morelli, V., Salarpi, G., Salerni, A., Scotto, J., Massimetti, G., Gesi, C., Ballerio, M., et al. (2019). Mood symptoms and suicidality across the autism spectrum. Compehensive Psychiatry , 91 , 34–38.
Demetriou, E. A., Park, S. H., Ho, N., Pepper, K. L., Song, Y. J. C., Naismith, S. L., Thomas, E. E., Hickie, I. B., & Guastella, A. J. (2020). Machine learning for Differential diagnosis between clinical conditions with Social Difficulty: Autism Spectrum Disorder, early psychosis, and social anxiety disorder. Frontiers in Psychiatry , 11 , 545. https://doi.org/10.3389/fpsyt.2020.00545 .
Dupuis, A., Mudiyanselage, P., Burton, C. L., Arnold, P. D., Crosbie, J., & Schachar, R. J. (2022). Hyperfocus or flow? Attentional strengths in autism spectrum disorder. Frontiers in Psychiatry , 13 , 886692. https://doi.org/10.3389/fpsyt.2022.886692 .
Espelöer, J., Hellmich, M., Vogeley, K., & Falter-Wagner, C. M. (2021). Brief report: Social anxiety in Autism Spectrum Disorder is based on deficits in social competence. Journal of Autism and Developmental Disorders , 51 (1), 315–322. https://doi.org/10.1007/s10803-020-04529-w .
Gesi, C., Migliarese, G., Torriero, S., Capellazzi, M., Omboni, A. C., Cerveri, G., & Mencacci, C. (2021). Gender Differences in Misdiagnosis and Delayed Diagnosis among Adults with Autism Spectrum Disorder with No Language or Intellectual Disability. Brain Sciences, 11(7) , 912. MDPI AG. Retrieved from https://doi.org/10.3390/brainsci11070912 .
Goffman, E. (1963). Stigma. Notes on the management of Spoiled Identity . Penguin Books.
Hair, J. F., Risher, J. J., Sarstedt, M., & Ringle, C. M. (2019). When to use and how to report the results of PLS-SEM. European Business Review , 31 (1), 2–24. https://doi.org/10.1108/EBR-11-2018-0203 .
Hu, L., & Bentler, P. M. (1998). Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods , 3 (4), 424–453.
Hulland, J. (1999). Use of partial least squares (PLS) in strategic management research: A review of four recent studies. Strategic Management Journal , 20 (2), 195–204.
Hull, L., Levy, L., Lai, M. C., Petrides, K. V., Baron-Cohen, S., Allison, C., Smith, P., & Mandy, W. (2021b). Is social camouflaging associated with anxiety and depression in autistic adults? Molecular Autism , 12 (1). https://doi.org/10.1186/s13229-021-00421-1 . Article 13.
Hull, L., Mandy, W., Lai, M. C., Baron-Cohen, S., Allison, C., Smith, P., & Petrides, K. V. (2019). Development and validation of the camouflaging autistic traits questionnaire (CAT-Q). Journal of Autism and Developmental Disorders , 49 (3), 819–833. https://doi.org/10.1007/s10803-018-3792-6 .
Hull, L., Petrides, K. V., Allison, C., Smith, P., Baron-Cohen, S., Lai, M. C., & Mandy, W. (2017). Putting on my best normal: Social camouflaging in adults with autism spectrum conditions. Journal of Autism and Developmental Disorders , 47 (8), 2519–2534. https://doi.org/10.1007/s10803-017-3166-5 .
Hull, L., Petrides, K. V., & Mandy, W. (2021). Cognitive predictors of self-reported camouflaging in autistic adolescents. Autism Research , 14 (3), 523–532. https://doi.org/10.1002/aur.2407 .
Iversen, S., & Kildahl, A. N. (2022). Case Report: Mechanisms in misdiagnosis of Autism as Borderline personality disorder. Frontiers in Psychology , 13 , 735205. https://doi.org/10.3389/fpsyg.2022.735205 .
Jorgenson, C., Lewis, T., Rose, C., et al. (2020). Social Camouflaging in autistic and neurotypical adolescents: A pilot study of differences by sex and diagnosis. Journal of Autism and Developmental Disorders , 50 , 4344–4355.
Kapp, S. K., Steward, R., Crane, L., Elliott, D., Elphick, C., Pellicano, E., & Russell, G. (2019). People should be allowed to do what they like’: Autistic adults’ views and experiences of stimming. Autism , 23 (7), 1782–1792. https://doi.org/10.1177/1362361319 .
Kobourov, S. G. (2012). Spring embedders and force directed graph drawing algorithms. https://doi.org/10.48550/arXiv.1201.301 .
Lai, M. C., Lombardo, M. V., Ruigrok, A. N., Chakrabarti, B., Auyeung, B., Szatmari, P., Happe, F., Baron-Cohen, S., & Consortium, M. A. (2017). Quantifying and exploring camouflaging in men and women with autism. Autism , 21 (6), 690–702. https://doi.org/10.1177/1362361316671012 .
Liebowitz, M. R. (1987). Social phobia. Modern Problems in Pharmacopsychiatry , 22 , 141–173.
Livingston, L. A., & Happé, F. (2017). Conceptualising compensation in neurodevelopmental disorders: Reflections from autism spectrum disorder. Neuroscience and Biobehavioral Reviews , 80 , 729–742. https://doi.org/10.1016/j.neubiorev.2017.06.005 .
Livingston, L. A., Shah, P., & Happé, F. (2019). Compensatory strategies below the behavioural surface in autism: a qualitative study. The Lancet Psychiatry, 6 (9), 766–777. https://doi.org/10.1016/S2215-0366(19)30224-X
Maddox, B. B., & White, S. W. (2015). Comorbid Social Anxiety Disorder in adults with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders , 45 (12), 3949–3960. https://doi.org/10.1007/s10803-015-2531-5 .
Mateos-Aparicio, G. (2011). Partial least squares (PLS) methods: Origins, evolution, and application to social sciences. Communications in Statistics - Theory and Methods , 40 (13), 2305–2317.
Miller, D., Rees, J., & Pearson, A. (2021). Masking is life: Experiences of masking in autistic and nonautistic adults. Autism in Adulthood , 3 (4), 330–338.
Perry, E., Mandy, W., Hull, L., & Cage, E. (2021). Understanding camouflaging as a response to autism-related stigma: A social identity theory approach. Journal of Autism and Developmental Disorders . https://doi.org/10.1007/s10803-021-04987-w .
Petrolini, V., Rodríguez-Armendariz, E., & Vicente, A. (2023). Autistic camouflaging across the spectrum. New Ideas in Psychology , 68 , 1–9. https://doi.org/10.1016/j.newideapsych.2022.100992 .
Pisula, E., Płatos, M., Banasiak, A., Danielewicz, D., Gosztyła, T., Podgórska-Jachnik, D., Pyszkowska, A. M., Rumińska, A. E., & Winczura, B. (2024). Neuroróżnorodność na polskich uczelniach. Doświadczenia osób studiujących: w spektrum autyzmu, z ADHD i z dysleksją Oficyna Wydawnicza Impuls. https://doi.org/10.62634/9788382943139 .
Pyszkowska, A., Rożnawski, K., & Farny, Z. (2021). Self-stigma and cognitive fusion in parents of children with autism spectrum disorder. The moderating role of self-compassion. PeerJ, 9 , e12591. https://doi.org/10.7717/peerj.12591
Raymaker, D. M., Teo, A. R., Steckler, N. A., Lentz, B., Scharer, M., Delos Santos, A., Kapp, S. K., Hunter, M., Joyce, A., & Nicolaides, C. (2020). Having all of your internal resources exhausted beyond measure and being left with no clean-up crew: Defining autistic burnout. Autism in Adulthood , 2 (2), 1–12. https://doi.org/10.1089/aut.2019.0079 .
Ritschel, L. A., Guy, L., & Maddox, B. B. (2022). A pilot study of dialectical behaviour therapy skills training for autistic adults. Behavioural and Cognitive Psychotherapy , 50 (2), 187–202. https://doi.org/10.1017/S1352465821000370 .
Rosen, T. E., Mazefsky, C. A., Vasa, R. A., & Lerner, M. D. (2018). Co-occurring psychiatric conditions in autism spectrum disorder. International Review of Psychiatry , 30 , 40–61. https://doi.org/10.1080/09540261.2018.1450229 .
Rynkiewicz, A., Schuller, B., Marchi, E., Piana, S., Camurri, A., Lassalle, A., & Baron-Cohen, S. (2016). An investigation of the ‘female camouflage effect’ in autism using a computerized ADOS-2 and a test of sex/gender differences. Molecular Autism , 7 , 10. https://doi.org/10.1186/s13229-016-0073-0 .
Spain, D., Sin, J., Linder, K. B., McMahon, J., & Happe, F. (2018). Social anxiety in autism spectrum disorder: A systematic review. Research in Autism Spectrum Disorders , 52 , 51–68.
Tajfel, H., & Turner, J. C. (2004). The Social Identity Theory of Intergroup Behavior. In J. T. Jost & J. Sidanius (Eds.), Political psychology: Key readings (pp. 276–293). Psychology Press. https://doi.org/10.4324/9780203505984-16 .
Taylor, E., Livingston, L., Clutterbuck, R., & Shah, P. (2020). Psychometric concerns with the 10-item autism-spectrum quotient (AQ10) as a measure of trait autism in the general population. Experimental Results , 1 , e3. https://doi.org/10.1017/exp.2019.3.CrossRefGoogleScholar .
Wiskerke, J., Stern, H., & Igelström, K. (2018). Camouflaging of repetitive movements in autistic female and transgender adults . https://doi.org/10.1101/412619 .
Wong, K. K. (2010). Handling small survey sample size and skewed dataset with partial least square path modelling . Vue: The Magazine of the Marketing Research and Intelligence Association.
Download references
This work was supported by the National Science Centre, Poland, grant’s MINITATURA 6 (2022/06/X/HS6/00530).
Author information
Authors and affiliations.
University of Silesia in Katowice, Grażyńskiego 53, Katowice, 40-007, Poland
Anna Pyszkowska
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Anna Pyszkowska .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the University of Silesia in Katowice, Poland (approval no.: KEUS KEUS283/10.2022). All participants provided written consent.
Community Involvement
The author consulted the theoretical background of the camouflaging and aims of the study at the autism society group at the University of Silesia in Katowice.
Conflict of Interest
The Author declares no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Pyszkowska, A. It is More Anxiousness than Role-playing: Social Camouflaging Conceptualization Among Adults on the Autism Spectrum Compared to Persons with Social Anxiety Disorder. J Autism Dev Disord (2024). https://doi.org/10.1007/s10803-024-06416-0
Download citation
Accepted : 20 May 2024
Published : 06 June 2024
DOI : https://doi.org/10.1007/s10803-024-06416-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Camouflaging
- Autistic burnout
- Public stigma
- Social anxiety
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 07 June 2024
Sleep disturbances are associated with greater healthcare utilization in children with autism spectrum disorder
- Shirley Solomon 1 ,
- Leena Elbedour 1 , 2 ,
- Gal Meiri 1 , 3 ,
- Analya Michaelovski 1 , 4 ,
- Yair Sadaka 1 , 5 ,
- Michal Ilan 1 , 3 ,
- Michal Faroy 1 , 3 ,
- Ilan Dinstein 1 , 6 , 7 , 8 &
- Idan Menashe ORCID: orcid.org/0000-0003-1961-1461 1 , 2 , 8
Journal of Neurodevelopmental Disorders volume 16 , Article number: 29 ( 2024 ) Cite this article
Metrics details
Sleep disturbances are frequently reported in children with autism spectrum disorder (ASD) and are associated with the severity of co-occurring symptoms. This study’s aim was to examine the extent of healthcare utilization and clinical outcomes associated with sleep disturbances in children with ASD.
Study design
A retrospective, cross-sectional study of 541 children with ASD from the Azrieli National Center for Autism and Neurodevelopment Research (ANCAN) whose parents completed the Children’s Sleep Habits Questionnaire (CSHQ). Children with a total CSHQ score ≥ 48 were defined as having sleep disturbances. Sociodemographic characteristics, ASD diagnostic measures, chronic co-occurring conditions, medication usage, hospitalizations, visits to the emergency room (ER), and visits to specialists were compared in ASD children with and without sleep disturbances. Multivariate logistic regression models were then used to assess the independent association of sleep disturbances with clinical characteristics and healthcare utilization.
Of the 541 children with ASD, 257 (47.5%) had sleep disturbances. Children with sleep disturbances exhibited higher rates of multiple (≥ 3) co-occurring conditions (19.1% vs. 12.7%; p = 0.0414) and prescribed medications (45.5% vs. 32.7%; p = 0.0031) than other children. Finally, ASD children with sleep disturbances were 1.72 and 2.71 times more likely to visit the ER and be hospitalized than their counterparts (aOR = 1.72; 99%CI = 1.01–2.95; and aOR = 2.71; 99%CI = 1.10–6.67, respectively).
Conclusions
Our findings suggest that sleep disturbances are associated with greater healthcare utilization among children with ASD. Further studies could examine whether treating sleep disturbances in children with ASD yields additional clinical benefits beyond improvements in sleep.
Adequate sleep is essential for normal brain development in children [ 1 ] and reduces the risk of mental health disorders [ 2 ], hypertension [ 3 ], obesity [ 3 ], and type-2 diabetes [ 4 ] in childhood and adolescence. In contrast, difficulties in initiating or maintaining sleep over a sustained period are associated with higher usage of medications, more frequent physician visits, and twice as many hospitalizations in the general population [ 5 ], as well as an increased risk of having at least one psychiatric or medical comorbidity [ 6 ].
Sleep disturbances, identified using parent reports, are reported in 40–80% of children with autism spectrum disorder (ASD) [ 7 , 8 , 9 ] in contrast to approximately 25% in typically developing children [ 10 ]. The Children’s Sleep Habits Questionnaire (CSHQ) [ 12 ] is a parent questionnaire that has been used widely to identify children with clinically meaningful sleep disturbances in typically developing and ASD children [ 13 , 14 ]. The types of sleep disturbances reported in children with ASD include, but are not limited to, prolonged sleep onset, restless sleep, frequent awakenings, and a reduction in total sleep time [ 11 , 12 ]. Higher rates of sleep disturbances in children with ASD relative to controls have been identified as early as 30 months of age and continue into adolescence [ 16 ].
Sleep disturbances have been associated with the severity of additional behavioral symptoms in children with ASD. For example, several studies reported that children with ASD and sleep disturbances also displayed higher sensory sensitivities [ 13 , 14 , 15 ] and more challenging behaviors, including irritability, hyperactivity, inattention, and hostility [ 16 , 17 ]. Shorter sleep duration has also been associated with higher social communication difficulties and increased restricted and repetitive behaviors (RRBs) [ 18 ]. This has led to the suggestion that sleep disturbances may exacerbate the severity of core and secondary ASD symptoms [ 24 , 25 ]. Thus, behavioral and pharmacological treatments for sleep disturbances in ASD may alleviate multiple symptoms [ 19 ]. Indeed, one recent study has reported that treatment with prolonged release of melatonin improved total sleep time and reduced hyperactivity in children with ASD [ 20 ].
Children with ASD are known to exhibit multiple co-occurring conditions and use healthcare services more frequently than controls. Specifically, it has been reported that children with ASD have a higher prevalence of gastrointestinal issues [ 21 ], seizures [ 22 ], epilepsy [ 23 ], and psychiatric conditions [ 24 ]. Furthermore, children with ASD utilize primary care (pediatric visits), specialty care (psychiatric, neurology visits), acute care (emergency room [ER] visits), outpatient care, and hospitalizations more frequently than controls [ 25 , 26 ]. This increased healthcare may be attributable to the behavioral and developmental needs of children with ASD [ 33 ]. However, it may also be due to higher prevalence of co-occurring conditions [ 27 ]. For example, one study indicated that 13% of ER visits among children with ASD were psychiatric-related, compared to only 2% among children without ASD [ 28 ].
Given the higher rates of co-occurring conditions and healthcare utilization reported in children with ASD as well as the higher rates of sleep disturbances in these children, we aimed to examine the association between sleep disturbances and healthcare utilization in children with ASD registered in the database of the Azrieli National Center for Autism and Neurodevelopment Research (ANCAN).
Participants
We conducted a retrospective, cross-sectional study of 541 children with ASD between the ages of 1 and 10 years who were registered at the ANCAN database [ 29 , 30 ] between 2015 and 2021. Children were included in the current study if they were members of Clalit Health Services (CHS) and their parents had completed the Children’s Sleep Habits Questionnaire (CSHQ). CHS is the largest health maintenance organization (HMO) in Israel, which insures 70% of the population in the south of Israel. We focused solely on members of CHS because the children’s electronic patient records from this HMO were available to us through the Soroka University Medical Center’s (SUMC) medical database. The study was approved by the SUMC Helsinki committee.
Evaluation of sleep disturbances
Sleep disturbances were evaluated using the CSHQ, a 33-item parent questionnaire that asks parents to rate the frequency of specific sleep disturbances (e.g., difficulty to fall asleep) within the last week. The CSHQ was shown to exhibit high sensitivity and specificity in identifying children with clinical sleep disorders [ 12 ]. The CSHQ yields scores in eight subscales relating to common sleep disturbances: bedtime resistance, sleep onset delay, sleep duration, anxiety around bedtime, parasomnias, night wakening, sleep-disordered breathing, and daytime sleepiness. All items are summed to create a final total score ranging between 33 and 99, with higher scores indicating greater severity. We used a conservative threshold for identifying children with sleep disturbances using a CSHQ total score of ≥ 48 as suggested before [ 31 ]. The CSHQ has been used in research studies to assess children aged 4 to 10 years but has also shown to be clinically useful for screening sleep problems in younger children [ 32 ].
Diagnosis and evaluation of core and secondary ASD symptoms
ASD diagnosis for all study participants was determined by a child psychiatrist or a pediatric neurologist according to the DSM-5 criteria following behavioral and cognitive assessments, as described previously [ 30 ]. Core ASD symptom severity was evaluated in all children using the Autism Diagnostic Observation Schedule, 2nd edition (ADOS-2) calibrated severity score (CSS). The ADOS-CSS, computed from ADOS-2 raw scores, allows comparison of ADOS-2 total scores across ages and modules [ 33 ]. We also compared symptom severity using the DSM-5 levels of required support (“Requiring support,” “Requiring substantial support,” “Requiring very substantial support”) in social communication (category A) and restricted, repetitive behaviors (RRB; category B) domains [ 34 ]. In addition, cognitive assessment scores from either the Bayley Scales of Infant and Toddler Development [ 35 ] or the Wechsler Preschool and Primary Scale of Intelligence (WPPSI) [ 36 ] were available for most ( n = 445, 82%) of the children included in the final study sample.
Evaluation of health services utilization and medication use
Health records were obtained from the CHS electronic patient record system for all participating children, as described before [ 27 ]. Co-occurring chronic conditions were obtained from the Ofek database that houses all medical data for every patient insured by CHS. This database documents, among other things, all chronic diagnoses that were recorded by primary care and specialist physicians. We extracted all co-occurring chronic conditions, which were coded according to the International Classification of Diseases, Ninth Revision (ICD-9) format, and grouped them into broader disease categories (excluding complications of pregnancy, childbirth, and the puerperium [630–676] and conditions originating in the perinatal period [760–799]). Codes 780–799, which are grouped as “symptoms, signs, and ill-defined conditions” according to the ICD-9, consist of symptoms, abnormal laboratory results or investigative procedures. This group includes labels such as “undiagnosed cardiac murmurs” and “respiratory abnormality, unspecified” and can otherwise be designated as “unknown etiology” [ 37 ]. Records of medication usage were obtained and grouped based on primary clinical use (Supplementary Table S1 ). In addition, hospitalizations, visits to the ER, and visits to specialists during a time period corresponding to one year before and after completion of the CSHQ were also gathered from the electronic records.
Statistical analyses
Standard univariate tests were used to examine differences in various demographic and clinical characteristics between ASD children with and without sleep disturbances. Co-occurring chronic conditions and medication classes with a prevalence of less than 1% were excluded from the analyses. Chi-square or Fisher-exact tests were used to assess for differences in categorical variables, Mann–Whitney U‐test for continuous variables, and linear-by-linear association tests for ordinal variables. Differences with a p-value of < 0.05 were considered statically significant. Finally, the independent association between sleep disturbances and co-occurring chronic conditions, medication use, and healthcare utilization was assessed via multiple logistic regression models, each sequentially adjusting for potential confounders as follows. The initial analysis included only the sleep disturbances status (crude model). Basic sociodemographic and clinical covariates (e.g., age, sex, ethnicity, and DSM-V B required level of support) were then added to the model, followed by the addition of the presence of co-occurring conditions and medication use. The adjusted odds ratios of these associations were reported with stringent 99% confidence intervals. The statistical analyses were performed using R studio, version 1.4.1717 (R Foundation for Statistical Computing version).
Of the 1,108 children with ASD in the ANCAN database as of August 2021, 541 children (48.9%) fulfilled the study inclusion criteria. Children included in the sample were 3.25 (± 1.33) years old, on average, 79.1% of the children were of Jewish ethnicity, and their male-to-female ratio was 4:1. This sample did not differ significantly from the entire sample in the ANCAN database in these characteristics or in their cognitive scores, and ADOS-2 calibrated severity scores (Table 1 ). However, children in the study sample required more support than children who were not included in the study sample, as estimated by the diagnosing physician according to the DSM-5 levels of required support. This difference may reflect a tendency of parents of children who require more support to complete the CSHQ questionnaire.
Overall, participating children had a broad distribution of CSHQ scores ranging from 33 to 81, with 257 (47.5%) exhibiting CSHQ scores ≥ 48, which were indicative of sleep disturbances (Fig. 1 ). There were no significant differences in sex ratio, cognitive scores, or ADOS-2 calibrated severity scores across children with and without sleep disturbances (Table 2 ). However, more children of Bedouin origin were observed in the sleep disturbances group (24.6% vs. 14.2%; p = 0.01), and the mean age of the children in the sleep disturbances group was slightly higher (4.34 vs. 4.03 years; p = 0.039). In addition, children with sleep disturbances required more support according to the DSM-V criteria, with significant differences observed in the B criteria describing disturbances in RRB symptoms ( p = 0.027).

Distribution of CSHQ scores in the study sample. A histogram of the frequency of CSHQ scores (X-axis) of children with ASD in the study sample. Overall, 257 children had CSHQ scores ≥ 48 and were defined as having insomnia. Abbreviations: Children’s Sleep Habits Questionnaire (CSHQ)
Co-occurring chronic conditions
Differences in co-occurring chronic conditions are depicted in Table 3 . There was a small but non-significant difference in number of ASD children who had any co-occurring chronic condition (49.8% vs. 45.8%; p = 0.3947) between the study groups. However, more ASD children with sleep disturbances had three or more co-occurring conditions compared to children without sleep disturbances (19.1% vs. 12.7%; p = 0.0414). In addition, ASD children with sleep disturbances had significantly more co-occurring conditions in the symptoms, signs, and ill-defined conditions classification than ASD children without sleep disturbances (21.0% vs. 13.7%, p = 0.0334). There were no significant differences in other examined categories of co-occurring chronic conditions.
- Medication use
The use of medication for the management of chronic conditions (as listed in Supplementary Table S1 ) for both groups is presented in Table 4 . Children with sleep disturbances were more likely to be prescribed medications than those without (45.5% vs. 32.7%, p = 0.0031). This difference was partially due to medication prescriptions for sleep disturbances (e.g., Melatonin and Promethazine) that were almost twice as frequent in the sleep disturbances group (15.2% vs. 8.1%, p = 0.0145). Nevertheless, the number of prescribed medications for children with ASD and sleep disturbances was still significantly higher after excluding medications that treat sleep disturbances (37.0% vs. 28.2%, p = 0.0364), demonstrating their higher use of medications unrelated to sleep disturbances. Specifically, prescriptions for medications in the treatment of mental or mood conditions were significantly more frequent in the sleep disturbances group (9.7% vs. 4.9%, p = 0.0468).
Health services utilization
Children with ASD and sleep disturbances utilized more health services than children without sleep disturbances (Fig. 2 ), including 50% more visits to the ER (mean[SD] = 0.63[1.19] vs. 0.42[1.01]; p = 0.0153) and a 2.7 times higher rate of hospitalization (mean[SD] = 0.19[0.60] vs. 0.07[1.30]; p = 0.0042). Moreover, children with sleep disturbances were hospitalized for twice the number of days compared to children without sleep disturbances (mean[SD] = 0.32[1.08] vs. 0.16[1.06] days per child, respectively; p = 0.004). These findings suggest that the cost of ER visits and hospitalization is significantly higher for children with sleep disturbances. No significant differences were found in the total number of outpatient visits, including visits to primary care physicians (mean [SD] = 16.7 [14.7] vs. 16.9 [13.2] visits per child, respectively; p = 0.7492) and specialists (mean[SD] = 0.95[1.81] vs. 0.80[1.51] visits per child, respectively; p = 0.5206).

Percentage of health services utilization during a period of one year before and after completion of the CSHQ. A. Number of hospitalizations. B. Days hospitalized. C. Number of visits to a specialist. D . Number of visits to a primary care physician. E . Number of visits to the ER. Note that percentages presented in panels A, C, and E sum to 13.6%, 42.4%, and 34.6% of ASD children with insomnia and 6.4%, 58.5%, and 25.3% of children without insomnia who were hospitalized, visited specialists, and visited the ER, respectively. P-values from Mann-Whitney U tests are for the differences between children with and without insomnia. Abbreviations: Children’s Sleep Habits Questionnaire (CSHQ), ER (ER)
Factors associated with sleep disturbances
Finally, we used multivariable logistic regression models to quantify the independent association of sleep disturbances with co-occurring chronic conditions, medication use, and healthcare utilization in our sample while controlling for potential confounders (Table 5 ). Sleep disturbances in children with ASD were associated with higher odds of having co-occurring chronic conditions and medication use. However, these associations were not statistically significant in the fully adjusted models (Table 5 ). Nevertheless, children with sleep disturbances were 1.72 more likely to visit the ER (≥ 1 visits during the study period) (aOR = 1.72; 99% CI = 1.01, 2.95), and 2.71 more likely to be hospitalized (≥ 1 hospitalizations during the study period) (aOR = 2.71; 99% CI = 1.10, 6.67), even after adjusting for sociodemographic characteristics, presence of co-occurring chronic conditions and medication use.
The results demonstrate that sleep disturbances are present in nearly 50% of children with ASD. These children have a higher number of co-occurring chronic conditions, use more medications, and are more likely to visit the ER and be hospitalized compared to ASD children without sleep disturbances.
These findings from children with ASD are in line with previous studies that have reported positive associations between sleep disturbances and a diverse range of co-occurring chronic conditions within the general adult population. These include associations between sleep disturbances and anxiety and depression [ 38 ], gastrointestinal disorders [ 39 ], psychopathy symptoms [ 40 ], and even a 45% increased risk of mortality from cardiovascular disease [ 41 ]. The mechanism underlying the associations between sleep disturbances and co-occurring chronic conditions remains unknown. It is possible that the symptoms associated with co-occurring conditions (e.g. anxiety or gastrointestinal disorders) cause sleep disturbances. Alternatively, sleep disturbances could increase the risk of developing or exacerbating co-occurring chronic conditions. A third option is that alterations in biological mechanisms such as circadian rhythm misalignment [ 42 ], low-grade inflammatory state [ 43 ], elevation of cortisol [ 44 ], and metabolic or endocrine changes [ 45 ] could contribute to both sleep disturbances and co-occurring chronic conditions. Some of these mechanisms were also suggested to be involved in ASD etiology [ 46 , 47 ], thus highlighting potential mechanistic links between ASD and sleep disturbances.
The association of sleep disturbances with greater use of health services in this study is also consistent with previous reports of increased utilization of health services with sleep disturbances in the general adult population, including more frequent ER visits and hospitalizations, but no significant increases in the number of physician visits [ 5 , 48 , 49 ]. Moreover, in our study, sleep disturbances were independently associated with healthcare utilization in ASD children even after controlling for medication use and chronic co-occurring chronic conditions. In a previous study we reported that children with ASD are referred to the ER and admitted to the hospital more frequently than children without ASD [ 27 ]. It is possible that the higher prevalence of sleep disturbances in children with ASD compared to controls contributed to this observation. Furthermore, the association between sleep disturbances and healthcare utilization was also demonstrated in other studies with an adult population, where the association between sleep disturbances and increased hospitalizations and ER visits remained significant even after accounting for medical or mental health conditions [ 50 , 51 ]. A possible explanation for the association between sleep disturbances and hospitalizations and ER visits, but not with outpatient or specialist visits, may be due to the nature of ER visits. Sleep disturbances have been shown to increase the amount of challenging behaviors including hyperactivity, irritability and hostility [ 16 , 17 ], potentially increasing the risk for injuries that may require a visit to the ER. Unfortunately, we could not test this hypothesis due to the lack of information regarding the reason for ER admission in the medical records used in this study.
Finally, ASD children with sleep disturbances were more likely to consume more medications for sleep as well as other medications than ASD children without sleep disturbances. These findings are consistent with similar differences between good and bad sleepers in the general population [ 53 , 54 ]. Notably, in the current study, the association between medication use and sleep disturbances was statistically significant only in the unadjusted regression model, and this association, although it remained positive, lost its statistical significance in the fully adjusted model. This finding is expected given that ASD children with sleep disturbances display more challenging behaviors [ 16 , 17 ], and antipsychotics, including risperidone and aripiprazole (the two most common medications prescribed in this study sample under the mental and mood conditions classification), are prescribed to reduce challenging behaviors, particularly irritability and aggression in children with ASD [ 55 , 56 ].
The results reported in this study should be interpreted in the context of the following limitations. First, information on the child’s sleep behavior was gathered via parental reports using the CSHQ. This method may be biased as it relies on parents’ perception and their subjective ability to recall their child’s sleep disturbances accurately. Alternative methods such as daily sleep diaries or direct measures such as actigraphy and polysomnography may offer less biased estimates of sleep disturbances; however, these measures are often difficult to acquire from children with ASD due to sensory sensitivities and lack of cooperation [ 58 ]. Second, this study used a retrospective, cross-sectional design. Thus, it was impossible to determine the causality or directionality of the association between the emergence of sleep disturbances and the utilization of health services and/or clinical outcomes. It is unknown whether sleep disturbances directly increase the risk of these factors or if adverse health outcomes produce sleep disturbances, as a temporal relationship was not established. It is also possible that sleep disturbances and health outcomes are caused by a shared underlying biological mechanisms. Third, data was obtained solely from the electronic records, which included only clinical data, and no information regarding use of over-the-counter medications, including melatonin. Furthermore, no information was provided regarding the nature of ER visits. Fourth, despite a large sample size, the rarity of some co-occurring chronic conditions and prescribed medication classes limited our ability to find a significant association between sleep disturbances and these variables. Indeed, a post-hoc power analysis indicated that the observed differences between the study groups in the rates of each of the co-occurring chronic conditions and medication classes only had a 40% statistical power to declare these differences as statistically significant within our sample size. Finaly, data collection was derived from children living in southern Israel and enrolled in a single HMO, which may have limited the generalizability of the study findings to other populations.
Our findings suggest that sleep disturbances are associated with greater healthcare utilization among children with ASD. Future studies should validate our findings and further investigate the underlying mechanisms of these associations. Furthermore, it would be interesting to examine whether treatments for sleep disturbances reduce the utilization of health services in a manner associated with the amelioration of sleep problems in children with ASD.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to ethical reasons. The anonymized data could be obtained from the corresponding author on reasonable request.
Abbreviations
Autism Spectrum Disorder
Azrieli National Center for Autism and Neurodevelopment Research
Children’s Sleep Habits Questionnaire
Repetitive Behavior
Emergency Room
Clalit Health Services
Health Maintenance Organization
Soroka University Medical Center’s
Ednick M, Cohen AP, McPhail GL, Beebe D, Simakajornboon N, Amin RS. A review of the effects of Sleep during the First Year of Life on Cognitive, Psychomotor, and temperament development. Sleep. 2009;32:1449–58.
Article PubMed PubMed Central Google Scholar
Samanta P, Mishra DP, Panigrahi A, Mishra J, Senapati LK, Ravan JR. Sleep disturbances and associated factors among 2-6-year-old male children with autism in Bhubaneswar, India. Sleep Med. 2020;67:77–82.
Article PubMed Google Scholar
Grandner M, Mullington JM, Hashmi SD, Redeker NS, Watson NF, Morgenthaler TI. Sleep duration and hypertension: analysis of > 700,000 adults by age and sex. J Clin Sleep Med. 2018;14:1031–9.
Reutrakul S, Van Cauter E, Metabolism. W.B. Saunders; 2018. 56–66.
Léger D, Guilleminault C, Bader G, Lévy E, Paillard M. Medical and Socio-Professional Impact of Insomnia. Sleep. 2002;25:621–5.
Article Google Scholar
Sarsour K, Morin CM, Foley K, Kalsekar A, Walsh JK. Association of Insomnia severity and comorbid medical and psychiatric disorders in a health plan-based sample: Insomnia severity and comorbidities. Sleep Med. 2010;11:69–74.
Bianca B, Silvia G, Elisa F, Deny M, Giovanni V, Lino N et al. Insomnia in children with Autism Spectrum disorder: a cross-sectional study on clinical correlates and parental stress. J Autism Dev Disord. 2022.
Leung MHB, Ngan STJ, Cheng PWC, Chan FCG, Chang WC, Cheung HK, et al. Sleep problems in children with autism spectrum disorder in Hong Kong: a cross-sectional study. Front Psychiatry. 2023;14:1088209.
Saletin JM, Koopman-Verhoeff ME, Han G, Barker DH, Carskadon MA, Anders TF et al. Sleep problems and autism impairments in a large community sample of children and adolescents. Child Psychiatry Hum Dev. 2022.
Veeravigrom M, Chonchaiya W, Insomnia. Focus on children. Sleep Med Clin. 2022;17:67–76.
Carmassi C, Palagini L, Caruso D, Masci I, Nobili L, Vita A et al. Systematic review of Sleep disturbances and Circadian Sleep Desynchronization in Autism Spectrum Disorder: toward an integrative model of a self-reinforcing Loop. Front Psychiatry. 2019;10.
Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S. Atypical behaviors in children with autism and children with a history of language impairment. Res Dev Disabil. 2007;28:145–62.
Cortesi F, Giannotti F, Ivanenko A, Johnson K. Sleep in children with autistic spectrum disorder. Sleep Med. 2010;11:659–64.
Manelis-Baram L, Meiri G, Ilan M, Faroy M, Michaelovski A, Flusser H et al. Sleep disturbances and sensory sensitivities Co-vary in a longitudinal manner in Pre-school Children with Autism Spectrum disorders. J Autism Dev Disord. 2021.
Tzischinsky O, Meiri G, Manelis L, Bar-Sinai A, Flusser H, Michaelovski A, et al. Sleep disturbances are associated with specific sensory sensitivities in children with autism. Mol Autism. 2018;9:1–10.
Hollway JA, Aman MG, Butter E. Correlates and risk markers for sleep disturbance in participants of the autism treatment network. J Autism Dev Disord. 2013;43:2830–43.
Mazurek MO, Sohl K. Sleep and behavioral problems in children with Autism Spectrum Disorder. J Autism Dev Disord. 2016;46:1906–15.
Veatch OJ, Sutcliffe JS, Warren ZE, Keenan BT, Potter MH, Malow BA. Shorter sleep duration is associated with social impairment and comorbidities in ASD. Autism Res. 2017;10:1221–38.
Lord C. Taking sleep difficulties seriously in Children with Neurodevelopmental disorders and ASD. Pediatrics. 2019;143.
Schroder CM, Malow BA, Maras A, Melmed RD, Findling RL, Breddy J, et al. Pediatric prolonged-release melatonin for Sleep in Children with Autism Spectrum Disorder: Impact on Child Behavior and Caregiver’s quality of life. J Autism Dev Disord. 2019;49:3218–30.
Holingue C, Newill C, Lee L-C, Pasricha PJ, Daniele Fallin M. Gastrointestinal symptoms in autism spectrum disorder: a review of the literature on ascertainment and prevalence. Autism Res. 2018;11:24–36.
Tuchman R. What is the relationship between Autism Spectrum disorders and Epilepsy? Semin Pediatr Neurol. 2017;24:292–300.
Lukmanji S, Manji SA, Kadhim S, Sauro KM, Wirrell EC, Kwon C-S, et al. The co-occurrence of epilepsy and autism: a systematic review. Epilepsy Behav. 2019;98:238–48.
Mutluer T, Aslan Genç H, Özcan Morey A, Yapici Eser H, Ertinmaz B, Can M et al. Population-Based Psychiatric Comorbidity in Children and adolescents with Autism Spectrum disorder: a Meta-analysis. Front Psychiatry. 2022;13.
Cummings JR, Lynch FL, Rust KC, Coleman KJ, Madden JM, Owen-Smith AA, et al. Health services utilization among children with and without Autism Spectrum disorders. J Autism Dev Disord. 2016;46:910–20.
Liu G, Pearl AM, Kong L, Leslie DL, Murray MJ. A Profile on Emergency Department utilization in adolescents and young adults with Autism Spectrum disorders. J Autism Dev Disord. 2017;47:347–58.
Dizitzer Y, Meiri G, Flusser H, Michaelovski A, Dinstein I, Menashe I. Comorbidity and health services’ usage in children with autism spectrum disorder: a nested case–control study. Epidemiol Psychiatr Sci. 2020;29:e95.
Kalb LG, Stuart EA, Freedman B, Zablotsky B, Vasa R. Psychiatric-Related Emergency Department visits among children with an Autism Spectrum Disorder. Pediatr Emerg Care. 2012;28:1269–76.
Dinstein I, Arazi A, Golan HM, Koller J, Elliott E, Gozes I, et al. The National Autism Database of Israel: a resource for studying autism risk factors, biomarkers, outcome measures, and treatment efficacy. Journal of Molecular Neuroscience. Humana Press Inc.; 2020. pp. 1303–12.
Meiri G, Dinstein I, Michaelowski A, Flusser H, Ilan M, Faroy M, et al. Brief report: the Negev Hospital-University-based (HUB) autism database. J Autism Dev Disord. 2017;47:2918–26.
Reynolds AM, Soke GN, Sabourin KR, Hepburn S, Katz T, Wiggins LD et al. Sleep problems in 2-to 5-year-olds with autism spectrum disorder and other developmental delays. Pediatrics. 2019;143.
Goodlin-Jones BL, Sitnick SL, Tang K, Liu J, Anders TF. The children’s Sleep habits Questionnaire in toddlers and Preschool Children. J Dev Behav Pediatr. 2008;29:82–8.
Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in Autism Spectrum disorders. J Autism Dev Disord. 2009;39:693–705.
American Psychiatric Association. Task Force D-5. Diagnostic and statistical Manual of Mental disorders (DSM-5®). American Psychiatric Publishing; 2013.
Bayley N, Bayley, -III. Bayley Scales of infant and toddler development. 3rd ed. San Antonio, TX: Pearson; 2006.
Google Scholar
Wechsler D. Wechsler Preschool and Primary Scale of Intelligence. New York, NY: Psychological Corp; 1967.
Williams MA, Martin MY. Symptoms, signs, and ill-defined conditions. Handbook of clinical health psychology: volume 1 Medical disorders and behavioral applications. Washington: American Psychological Association; 2002. pp. 533–53.
Book Google Scholar
Sørensen L, Jensen MSA, Rathleff MS, Holden S. Comorbid Insomnia, psychological symptoms and widespread pain among patients suffering from musculoskeletal pain in general practice: a cross-sectional study. BMJ Open. 2019;9.
Balikji S, Mackus M, Brookhuis K, Garssen J, Kraneveld A, Roth T, et al. The Association of Insomnia, Perceived Immune Functioning, and irritable bowel syndrome complaints. J Clin Med. 2018;7:238.
Akram U, Allen S, McCarty K, Gardani M, Tan A, Villarreal D, et al. The relationship between insomnia symptoms and the dark triad personality traits. Pers Individ Dif. 2018;131:212–5.
Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. 2014;21:57–64.
Nobre B, Rocha I, Morin CM, Meira e Cruz M. Insomnia and circadian misalignment: An underexplored interaction towards cardiometabolic risk. Sleep Science. Brazilian Association of Sleep and Latin American Federation of Sleep Societies; 2021. pp. 55–63.
Friedman EM. Sleep quality, social well-being, gender, and inflammation: an integrative analysis in a national sample. Ann N Y Acad Sci. 2011;1231:23–34.
Vargas I, Vgontzas AN, Abelson JL, Faghih RT, Morales KH, Perlis ML. Altered ultradian cortisol rhythmicity as a potential neurobiologic substrate for chronic insomnia. Sleep Med Rev. 2018;41:234–43.
Copinschi G. Metabolic and endocrine effects of sleep deprivation. Essent Psychopharmacol. 2005;6.
Abdul F, Sreenivas N, Kommu JVS, Banerjee M, Berk M, Maes M, et al. Disruption of circadian rhythm and risk of autism spectrum disorder: role of immune-inflammatory, oxidative stress, metabolic and neurotransmitter pathways. Rev Neurosci. 2022;33:93–109.
Article CAS PubMed Google Scholar
Geoffray M-M, Nicolas A, Speranza M, Georgieff N. Are circadian rhythms new pathways to understand Autism Spectrum Disorder? J Physiology-Paris. 2016;110:434–8.
Skaer TL, Sclar DA. Economic implications of Sleep disorders. PharmacoEconomics. 2010;28:1015–23.
Wickwire EM, Vadlamani A, Tom SE, Johnson AM, Scharf SM, Albrecht JS. Economic aspects of insomnia medication treatment among Medicare beneficiaries. Sleep. 2020;43.
Tzuang M, Owusu JT, Huang J, Sheehan OC, Rebok GW, Paudel ML et al. Associations of Insomnia symptoms with subsequent health services use among community-dwelling U.S. older adults. Sleep. 2021;44.
Amari DT, Juday T, Frech FH, Wang W, Wu Z, Atkins N, et al. Falls, healthcare resources and costs in older adults with insomnia treated with zolpidem, trazodone, or benzodiazepines. BMC Geriatr. 2022;22:484.
Brossoit RM, Crain TL, Leslie JJ, Hammer LB, Truxillo DM, Bodner TE. The effects of sleep on workplace cognitive failure and safety. J Occup Health Psychol. 2019;24:411–22.
Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J, Baillargeon L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10:427–38.
Sivertsen B, Krokstad S, Mykletun A, Øverland S. Insomnia Symptoms and Use of Health Care Services and medications: the HUNT-2 study. Behav Sleep Med. 2009;7:210–22.
Ching H, Pringsheim T. Aripiprazole for autism spectrum disorders (ASD). In: Pringsheim T, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2012.
Loy JH, Merry SN, Hetrick SE, Stasiak K. Atypical antipsychotics for disruptive behaviour disorders in children and youths. Cochrane Database of Systematic Reviews. 2017;2017.
Miller BJ, McCall WV. Insomnia and suicide as reported adverse effects of second-generation antipsychotics and mood stabilizers. J Clin Sleep Med. 2022;18:517–22.
Goldman SE, Surdyka K, Cuevas R, Adkins K, Wang L, Malow BA. Defining the Sleep phenotype in Children with Autism. Dev Neuropsychol. 2009;34:560–73.
Download references
Acknowledgements
We thank the families who participated in this research.
This study was funded by Neurim Pharmaceuticals Ltd.
Author information
Authors and affiliations.
Azrieli National Centre for Autism and Neurodevelopment Research, Ben-Gurion University of the Negev, Beer-Sheva, Israel
Shirley Solomon, Leena Elbedour, Gal Meiri, Analya Michaelovski, Yair Sadaka, Michal Ilan, Michal Faroy, Ilan Dinstein & Idan Menashe
Department of Epidemiology, Biostatistics, and Community Health Sciences, Ben-Gurion University of the Negev, P.O. Box 653, Beer-Sheva, 84105, Israel
Leena Elbedour & Idan Menashe
Preschool Psychiatric Unit, Soroka University Medical Center, Beer-Sheva, Israel
Gal Meiri, Michal Ilan & Michal Faroy
Child Development Center, Soroka University Medical Center, Beer-Sheva, Israel
Analya Michaelovski
Child Development Center, Ministry of Health, Beer-Sheva, Israel
Yair Sadaka
Psychology Department, Ben-Gurion University of the Negev, Beer-Sheva, Israel
Ilan Dinstein
Cognition and Brain Sciences Department, Ben-Gurion University of the Negev, Beer-Sheva, Israel
Zlotowski Center for Neurosciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel
Ilan Dinstein & Idan Menashe
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: ID, IM; Data curation: SS; Formal analysis: SS; Funding acquisition: GM, ID, IM; Investigation: GM, AM, YS, MI, MF; Methodology: IM; Project administration: ID, IM; Resources: GM, AM, YS, MI, MF, ID, IM; Supervision: IM; Validation: LE; Visualization: LE; Writing – original draft: SS; Writing – review and editing: LE, IM.
Corresponding author
Correspondence to Idan Menashe .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the ethics committee of SUMC. The study was conducted on retrospective data from medical records of patients. Therefore, no participant’s consent was needed.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Solomon, S., Elbedour, L., Meiri, G. et al. Sleep disturbances are associated with greater healthcare utilization in children with autism spectrum disorder. J Neurodevelop Disord 16 , 29 (2024). https://doi.org/10.1186/s11689-024-09550-z
Download citation
Received : 24 January 2024
Accepted : 28 May 2024
Published : 07 June 2024
DOI : https://doi.org/10.1186/s11689-024-09550-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Autism spectrum disorder (ASD)
- Sleep disturbances
- Healthcare utilization
- Co-occurring conditions
Journal of Neurodevelopmental Disorders
ISSN: 1866-1955
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Making an Autism Spectrum Disorder Diagnosis Autism Case Training: A Developmental-Behavioral Pediatrics Curriculum 4 Distribute Case Study Part I Slide 3 Case Study Part I Billy is a 3 ½ -year-old boy you are seeing for the first time in your resident practice. He was born full term following a normal pregnancy and delivery. His newborn ...
CASE STUDY EXAMPLE effective instructional strategy and parents of children with ASD have used this strategy to successfully teach requesting. Additionally, naturalistic intervention is designed to be conducted within natural routines. Next, Mrs. Dell creates a data collection system that is succinct and easy to implement
Abstract. This article aims to observe all the manifestations of the behavior of a child with Autism Spectrum Disorder (ASD), which shows deficits mainly in the communication sector. Also, the ...
Autism spectrum as a communication disorder: A case study Mayada Senouci1, Hussein Obeidat2* and Rabha Ghaouti3 1Djillali Liabes University of Sidi Bel Abbes, Algeria. 2Yarmouk University, Irbid, Jordan. 3Djillali Liabes University of Sidi Bel Abbes, Algeria. Accepted 4 July, 2021 ABSTRACT Communication is a vital social phenomenon; therefore, its study must be related to theories of social
The following case studies present three different children with ASD and describe the SLP's strategies to enhance communication and quality of life. The three case studies demonstrate various options in AAC intervention that can be used by children of different ages. —Ann-Mari Pierotti, MS, CCC-SLP. Case Study 1: Anderson | Case Study 2 ...
Clinical case scenarios: Autism: recognition, referral and diagnosis. September 2011 Page 5 of 60 Clinical case scenarios for professionals working with children and young people Case scenario 1: Howard - recognition, referral and diagnosis Presentation Howard is 7 years old and presents at his GP with his mother as she is
Western Michigan University Abstract. This paper describes Autism Spectrum Disorder (ASD) including diagnostic criteria, suspected. causes, prevalence, comorbidities, and influences on client factors. A hypothetical case study is. presented to give readers an illustration of what someone with ASD might look like.
April 25, 202 1. Autism spectrum disorder is considered in broad neurodevelopmen tal. disorder, experience in roughly 1 in 68 children globally ( Autism and. Developmental Disabilities Monitoring ...
Autism spectrum disorder (ASD) is a congenital or early-acquired complex neurodevelopmental disorder characterised by difficulties in social interaction, impaired social communication and restricted behavioural patterns (Association, Citation 2013; Wing & Gould, Citation 1979).The symptoms must be present in the early developmental period, typically before age of three, and usually persist ...
Autism Spectrum Disorder: A Case Study on Students Attainments Anthi Maneta Pre-school Teacher, Email: [email protected] Article Received: 30 August 2018 Article Accepted: 29 December 2018 Article Published: 28 February 2019 INTRODUCTION Autism is a chronic developmental disorder that influences all aspects of social interaction and ...
The Communication Symbolic and Behavior Scales Developmental Profile (CSBS DP; Wetherby & Prizant, 1993) was used to determine communicative competence. This norm-referenced instrument for children 6-24 months old is characterized by outstanding psychometric data (i.e., sensitivity=89.4%- 94.4%; specificity=89.4%).
Autism or ASD is a "neurodevelopmental disorder". The worldwide prevalence is about one in 59 children. and India being the second most populated country. accounts for about one in 1000 ...
Autism spectrum disorder (ASD) is a neurological and developmental disorder that afects how people interact with others, communicate, learn, and behave. Although autism can be diagnosed at any age, it is described as a "developmental disorder" because symptoms generally appear in the first two years of life. Autism is known as a "spectrum ...
The following literature review and case study highlight the need for improved training among allied health and educational professionals with the diagnosis of Autism Spectrum Disorder (ASD). A brief review of the literature will demonstrate the need for better staff training for professionals who work with children regarding the early ...
Citation: Sang Yeon Lee, Hyunjun Ahn, Won-ju Jung, Jihye Ahn, Kye Ho Lee (2020) A Case Study on Autism Spectrum Disorder Treatment Using Allogenic Mesenchymal Stem Cells Derived from the Human Umbilical Cord. Case Reports: Open Access 5: 1-7. Received Date: October 25, 2020 Accepted Date: November 26, 2020 Published Date: November 28, 2020
Gabrielle Lober. 2015. This paper describes Autism Spectrum Disorder (ASD) including diagnostic criteria, suspected causes, prevalence, comorbidities, and influences on client factors. A hypothetical case study is presented to give readers an illustration of what someone with ASD might look like. Possible treatment based on evidence and ...
This case study illustrates how stress and mental health difficulties can precede autism diagnosis in adults. The personal experiences detailed highlight how an adult autism diagnosis can bring about positive change, prompting increased self-knowledge and coping skills, improved relationships and. Furthermore, it highlights how a supportive ...
Open PDF in Browser. Add Paper to My Library. Share: Permalink. Using these links will ensure access to this page indefinitely. ... Maneta, Anthi, Autism Spectrum Disorder: A Case Study on Students Attainments (February 9, 2019). Mediterranean Journal of Basic and Applied Sciences (MJBAS), Volume 3, Issue 1, Pages 25-36, (2019), ...
Autism spectrum disorder (ASD) is a neurodevelopmental disorder estimated to affect up to 1.7% of children in the United States, according to the Centers for Disease Control and Prevention (CDC) (Maenner et al., 2020), and 3% of children age 4 years in the United States (Christensen et al., 2019).Children with ASD have impairments in social and communication interactions and restrictive ...
Abstract. Autism Spectrum Disorders (ASDs) are a group of neurodevelopmental disorders characterised by impairments in 3 domains: communication, social interaction and repetitive behaviour. It is ...
Making an Autism Spectrum Disorder Diagnosis. Autism Case Training: A Developmental-Behavioral Pediatrics Curriculum 4. Distribute Case Study Part I. Slide 3. Case Study Part I. Billy is a 3 ½ -year-old boy you are seeing for the first time in your resident practice. He was born full term following a normal pregnancy and delivery. His newborn ...
1. Introduction. According to 2019 Global Burden of Disease (GBD) Mental Disorder Collaborators, mental disorders remain one of the top ten major causes of burden worldwide, with years lived with disability (YLDs) being the cause of the majority of the burden on mental disorders, with 125.3 million YLDs (95% uncertainty interval, UI 93.0-163.2), and the proportion of global YLDs attributed ...
Both GDD and autism spectrum disorder are common and yet clinically and genetically heterogeneous disorders. Despite their high prevalence and the advent of sequencing detection methods, the genomic etiology of GDD and autism spectrum disorder in most patients is largely unknown. CASE REPORT In this study, we describe a 6-year-old girl with GDD ...
Autism spectrum disorder (ASD) is considered a heterogeneous phenomenon, and it has been suggested that it might share a common etiopathological root with other psychiatric disorders and be the risk factor for developing mental health issues (Dell'Osso et al., 2019).Despite several studies proving that autistic traits are associated with higher anxiety, stress, (Hull et al., 2021b), suicidal ...
The purpose of this paper is to provide a brief overview of a case involving a child on the Autism Spectrum and how it affects their social life. For this purpose, the first episode of the series ...
Sleep disturbances are frequently reported in children with autism spectrum disorder (ASD) and are associated with the severity of co-occurring symptoms. This study's aim was to examine the extent of healthcare utilization and clinical outcomes associated with sleep disturbances in children with ASD. A retrospective, cross-sectional study of 541 children with ASD from the Azrieli National ...
This study elucidation of Lebanese ASD patient characteristics and comparison to the same in different populations is elucidation of Lebanese ASD patient characteristics and comparison to the same in different populations. Background: Autism Spectrum Disorder (ASD) is a group of neurodevelopmental disorders with delays in communication, restricted interests and repetitive behaviors.
Autism Spectrum Disorder: A Case Study on Students Attainments. Anthi Maneta. Pre-school Teacher, Email: amaneta@amcst udent.edu.gr. Article Received: 30 August 2018 Article Accepted: 29 December ...
Background: Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by impairments in social interaction and restricted and repetitive behaviors. Oxidative stress may be a critical link between mitochondrial dysfunction and ASD as reactive oxygen species (ROS) generated from pro-oxidant environmental toxicants and activated immune cells can result in mitochondrial failure ...