Home Care/ Home Health Case Studies
Home » Home Care/ Home Health Case Studies
A listing of Home Care/Home Health Case Studies .
- T elehealth Helps Great Plains Health Patients Manage Their Conditions Confidently in the Comfort of Their Home to Improve Outcomes : In this case study, Great Plains Health chose a Tailored Ambulatory Care platform and Remote Patient Monitoring Program for Transitional Care from LeadingAge Silver Partner and CAST Supporter Philips to scale up their tailored ambulatory program. The effort produced 98% patient satisfaction scores and reduced hospital readmissions. The technology also improved the team’s ability to educate patients to care for themselves, to coordinate care, and to help patients reconcile their medications. Patients also enjoyed the security of monitoring.
- Evaluation of Selfhelp Community Services’ Virtual Senior Center : This case study explores how CAST Patron Selfhelp Community Services established a technology-driven program called the Virtual Senior Center (VSC) to enrich quality of life for socially isolated homebound older adults.
- Reducing Blood Pressure among Engaged Participants through Multi-User Telehealth, Gamification, and Engagement Platform : This case study shows how technology company higi SH llc examined the relationship between ambulatory blood pressure (ABP) and patient engagement with a nationwide ABP kiosk platform deployed in pharmacies, grocery stores, and other community centers. Results showed a statistically significant relationship between frequency of engagement and lowering of systolic blood pressure. This study is applicable to the broader senior living market, as ABP kiosks provide an accessible, affordable, convenient and accurate means for individuals who cannot afford home BP devices to monitor their BP.
- Targeting the ‘Superusers’ of Healthcare With Telehealth : This case study describes how Banner Health monitored 135 clients who had at least 5 chronic health conditions. The project used a range of biometric sensors from LeadingAge Silver Partner and CAST Supporter Philips, and the Philips Lifeline personal emergency response system with automatic fall detection. In addition, program participants were matched with a multidisciplinary care team that included health coaches, nurses, social workers, pharmacists, and primary care “intensivists.” Outcomes included a 27% reduction in cost of care, a 32% reduction in acute and long-term care costs, and a 45% reduction in hospitalizations.
- Supporting Independence of Seniors through Remote Activity and Adherence Monitoring : Recover Healthcare had first-hand experience with some of the healthcare trends impacting their business and the long-term care industry as a whole, and were interested in leveraging technology to help address some of these challenges. Having already partnered with PointClickCare for over five years for their senior care facilities, Recover Healthcare saw an opportunity with PointClickCare’s acquisition of TouchStream Solutions and the possibilities of in-home remote monitoring.
- 2016 Shared Care Planning and Coordination Case Studies: 5 case studies highlight how providers went about implementing these technologies, the impacts they experienced, lessons they learned and pitfalls to avoid.
- Integrating Innovative Technology in the Home to Provide Enhanced Continuity of Care and Decreased Healthcare Costs for Older Adults : Element Care’s PACE (Program of All-Inclusive Care for the Elderly) program in Massachusetts North Shore, the Merrimack Valley and northeast region of Middlesex County implemented a Digital Avatar with Voice Activated Assistant Technology and Captioning to provide enhanced continuity of care in the home. The technology was provided by Care.Coach.
- Using Technology to Reduce Social Isolation and Depression in Homebound Older Adults : Nonprofit Care at Home New Jersey (CAHNJ) has reduced social isolation and depression among study participants who used a touchscreen Telikin computer to communicate with family, friends, and CAHNJ personnel.
- Improving Medication Compliance, Quality of Life, and Peace of Mind through Voice Assistant Technology : Libertana Home Health in Sherman Oaks, CA implemented a voice assistance technology to improve medication compliance, quality of life, and peace of mind. The voice assistance technology was provided by Orbita.
- Senior Patient Engagement:Using Telehealth to Support Chronic Disease Self-Management : This case study explores how the “On4Care Mobile” solution from CAST Supporter Panasonic was used to monitor the health of 22 older adults who were clients of Pleasantville Senior Center in Pleasantville, NY.
- How telehealth is helping a provider to position itself as a partner to hospitals on avoiding readmission : This case study shows how Jewish Home Lifecare uses technology in all of its service lines and in all components of its Community Service Division. It is currently in the process of rolling out technology-enabled services in its sub-acute unit.
- Reduction of Hospital Readmissions through Telehealth among High-Risk Cardiac Patients : A new case study explores how Rockford Memorial Hospital in Rockford, IL, implemented a Heart & Vascular RPM program that helped reduce its readmission rates from 28% to 14% over 2 years.
- I mproving Medication Compliance, Quality of Life, and Peace of Mind through Voice Assistant Technology: Libertana Home Health in Sherman Oaks, CA implemented a voice assistance technology to improve medication compliance, quality of life, and peace of mind. The voice assistance technology was provided by Orbita.
- TELEHEALTH AND REMOTE PATIENT MONITORING (RPM) – Provider Case Studies 2014: Provider Case Studies 2014 was compiled to help a variety of organizations become familiar with real-life examples of telehealth implementation. The case studies also explore the impacts experienced by users of these technologies and the potential revenue streams and business models that support them
- CAST Case Study: Evangelical Homes of Michigan: In July 2013, CAST Patron and LeadingAge Member Evangelical Homes of Michigan (EHM) learned about a newly formed, physician-based accountable care organization (ACO) called Northwest Ohio ACO during its conversations with Ohio Presbyterian Retirement Services (OPRS), a LeadingAge member in Columbus, OH.
- Medication Management Technologies PROVIDER CASE STUDIES 2015 : A set of 4 new case studies provides real-life examples of how providers implemented medication management technologies. One document in the collection summarizes the lessons learned from all the case studies.

Most Recommended
May 22, 2024
Nursing Home Staffing Mandates: What You Need to Know
May 08, 2024, summer recess for congress means advocacy opportunity for members, may 13, 2024, apply for aws imagine grants for nonprofit technology.
May 20, 2024
HOTMA: New Rules for Housing
Recently added.

May 23, 2024
HUD Announces New Funding Awards for Energy Efficiency and Climate Resilience

Colleagues on the Move, May 22, 2024

CAST Members in the News
CAST Updates Social Connectedness Technology Tool
Login | 1(877) 307-8573 | Contact Us
The page you're looking for has a new home.
We’re bringing things together! The knowingmore.com website has merged with homecarepulse.com and you’ve been redirected. Welcome to the new site!
Need to log into eLearning? You can log in here .

Case Studies
Learn from other agency’s success.

How A Long Term Companion Used HCP to Hire 51.5% More Employees and Build an Employer Brand That Resulted in an Indeed Click Through Rate Over 10x the Site Average
Caring for an aging parent or loved one can feel overwhelming. At A Long Term Companion, our compassionate, professional caregivers have been providing one-on-one support to our clients for over a decade.

How BrightStar Care Tinley Park Uses HCP Experience Management to Retain 85% of Caregivers For Their First Six Months
In an industry where the median turnover rate has exceeded 60% for over five years now, any agency with sub-30% turnover has a story to tell.

How Angels On Call Used Home Care Pulse to Build a Reputation that Increased Caregiver Applicants 26% Year-Over-Year
Increasing caregiver applicants is no small feat. See how one agency managed to do it amongst a caregiver shortage.

How Arosa Boston Managed Their Employment Brand to Hire 62% of New Caregivers Through Google Reviews
See how online reviews help this agency stand out amongst competitors.

How Third-Party Surveys Helped Visiting Angels of Carlisle Achieve Their Top Growth Quarter in Company History
A skeptic became an advocate, and his agency is prospering.

How Norwood Seniors Network Keeps Their Annual Caregiver Turnover Under 30%

LIFETIME Care At Home Secures Referral Partnerships Using Satisfaction Data
Referral sources, especially in healthcare, look for consistency and quality. Here's how one agency owner uses satisfaction data to speak their language in a way that his competition isn't.
LIFETIME Care At Home Uses Client/Caregiver Satisfaction to Motivate Office Staff to Do Their Best Work
Motivating staff to do their best can be difficult. Here's one agency owner rallies his staff to get them all rowing in the same direction.
Visiting Angels of Carlisle Says Satisfaction Data is a ‘Game-Changer’ in Referral Partnerships
Read one marketer's experience of how showing client satisfaction data turned a competitor into a referral partner.

Request a Live Demo
See our integrations in action on a zero-pressure Zoom call.

© 2024 Home Care Pulse, LLC | Terms of Service | Privacy Policy
Case Studies
Multiple studies have validated the cost savings and population health benefits associated with Home-Based Primary Care.
This New York City visiting doctors program, in operation for more than 15 years, allows for aging in place by providing in-home health care and chronic disease management for 1,100 elders. The program consistently demonstrates success, including:
- 66% reduction in hospitalizations
This house call program has been providing chronic disease management and advanced illness management for high-cost elders in the Bronx area of New York City for more than five years. For its roster of 400 patients, outcomes include:
- 42% reduction in hospitalizations
- 33% reduction in total costs
This house call program provides home-based medical care services and chronic disease management for an active roster of more than 700 Washington, DC-area patients, each with three or more chronic diseases. Data from the program has evidenced:
- Better patient care
- More primary care visits (house calls), more home health and more hospice
- 25% reduction in hospital length of stay
- 75% reduction in end-of-life hospitalizations
As compared to 2,161 matched controls, the program generated:
- 17% lower Medicare costs, which resulted in $8,477 savings per beneficiary
- 9% reduction in hospitalizations
- 10% reduction in ED visits
- 27% decrease in skilled nursing home days
Two-year savings came to $6.1 million.
Reference: De Jonge, E., Jamshed, N., Gilden, D., Kubisiak, J., Bruce, S., & Taler, G. (2014). Effects of Home-Based Primary Care on Medicare Costs in High-Risk Elders. Journal of the American Geriatrics Society, 1825-1831.
A study of patients with congestive heart failure discharged from the hospital and receiving transitional care via nurse practitioner house calls found:
- 50% reduction in 90 day readmissions
- 50% reduction in costs
Reference: Naylor, M., Brooten, D., Campbell, R., Maislin, G., McCauley , K., & Schwartz, J. (2004). Transitional Care of Older Adults Hospitalized with Heart Failure: A Randomized, Controlled Trial. Journal of the American Geriatrics Society, 675-684.
Launched in 1972, this house call program currently serves 30,000 veterans. The program has generated significant cost savings and reduction in resource utilization, including:
- 63% hospital cost savings
- 87% nursing home cost savings
- Total savings over $103 million
- 59% reduction in hospital days, 89% reduction in nursing home days and 21% reduction in 30-day readmissions (2006 data)Patients dually enrolled in VA and Medicare demonstrated additional benefits:
Patients dually enrolled in VA and Medicare demonstrated additional benefits:
- 7% VA cost savings and
- 8% Medicare cost savings
- $9,132 overall savings per veteran across 11,334 veterans served
- 25% reduction in hospitalizations
- Highest patient satisfaction of any VA program
Reference: Edes, T., Kinosian, B., Vukovic, N., Nichols, L., Becker, M., & Hossain, M. (2014). Better Access, Quality, and Cost for Clinically Complex Veterans with Home-Based Primary Care. Journal of the American Geriatrics Society, 1954-1964.
- Study protocol
- Open access
- Published: 12 June 2020
Home care clients: a research protocol for studying their pathways
- Janice M. Keefe ORCID: orcid.org/0000-0003-3073-8535 1 ,
- Laura Funk 2 ,
- Lucy Knight 3 ,
- Michelle Lobchuk 4 ,
- Marilyn Macdonald 5 ,
- Lori Mitchell 6 ,
- Julie Rempel 7 ,
- Grace Warner 8 &
- Susan Stevens 9
BMC Health Services Research volume 20 , Article number: 535 ( 2020 ) Cite this article
3839 Accesses
5 Citations
1 Altmetric
Metrics details
Enhancing non-clinical home care supports and services for older adults to live well is a strategic priority in developed countries, including Canada. Underpinning these supports and services are structures of care that are reflected in home care policies, programs and practices within jurisdictions. These approaches to care exist at multiple levels and inform interactions, perceptions, and care assessment, planning and provision, ultimately shaping the supports that are delivered. Jurisdictional differences in approaches to care mean that pathways through home care systems may differ, depending on where one lives. The goal of this study is to understand how approaches to care shape the pathways of older adult home care clients with chronic and long term conditions in two Canadian health jurisdictions.
This longitudinal mixed-methods study has three interrelated research streams informed by aspects of the socio-ecological framework. We will examine client pathways using a retrospective analysis of home care assessment data (Resident Assessment Instrument- Home Care) in two health authorities (Client/Service Data Stream). We will analyze interview data from older adult home care clients and a cluster of each client’s family or friend caregiver(s), home support worker(s), care/case coordinator(s) and potentially other professionals at up to three points over 18 months using a prospective qualitative comparative case study design (Constellation Data Stream). We will review home care policies relevant to both health authorities and interview key informants regarding the creation and implementation of policies (Policy Stream). Our study will apply an integrated knowledge translation (iKT) approach that engages knowledge users in research design, analysis and interpretation to facilitate relevancy of results.
Applying a mixed-method research design to understand approaches to care within and between two jurisdictions will contribute to the evidence base on older adult home care client pathways. Study results will identify how potential differences are experienced by clients and their families. An understanding of the policies will help to contextualize these findings. The iKT model will ensure that findings are useful for strategic planning and decision-making, and supporting changes in care practice.
Peer Review reports
Health and social care systems in Canada and other countries are struggling to meet the demand for care from older adults as a result of population aging [ 1 ]. In this context, home care and community supports are increasingly viewed as having an integral role in health care systems, and in facilitating ‘aging in place,’ across the globe. Older adults generally prefer to receive care in their own homes [ 2 , 3 ]. Governments also increasingly look to home care as a sustainable approach with the potential to reduce public-payer costs by easing the pressure on waitlists for residential long term care, supporting earlier hospital discharge [ 3 , 4 ] and promoting reablement. Evidence suggests that home care services can delay but not necessarily prevent institutionalization [ 5 ]. A recent report by the Canadian Institutes of Health Information found subpopulations of older adults in residential care who may not have required placement if appropriate community-based supports had been available [ 6 ]. This finding signals the need for ongoing attention to identifying unmet needs for supportive home care or service, and a nuanced understanding of service pathways and factors that influence service delivery in meeting client needs along the care path.
There is some concern, however, that increasing attention in home care to supporting short-term medical and complex care needs (e.g., post-acute, multi-morbidity) will lead to the erosion of preventive, non-medical and supportive functions of home care [ 7 , 8 ]. This “quick fix” approach in home care moves away from attention to the prevention or maintenance of health and wellness to mitigate health and functional breakdown, and eventually institutionalization [ 9 ]. This can disadvantage older adult clients with chronic and long term care needs for supportive home care [ 10 , 11 ], including personal care (e.g., bathing, shampooing, and dressing), housekeeping, meal preparation, transportation, and caregiver respite– otherwise known as non-clinical supportive home care, and the health system overall. Support with housework services, personal care and assistance, and meal preparation reduce the risk for institutional care [ 12 , 13 , 14 ]. Overall, evidence indicates that non-clinical supports can sustain functioning and independent living.
Although access to non-clinical supportive home care helps older adults to stay in their homes longer, certain factors may impact client trajectories or pathways within, and potentially out of, the home care system, with implications for clients, their family and friend caregivers, home support workers [ 15 , 16 , 17 ], and the system [ 8 , 18 ]. For instance, clients’ use of home care services might maintain, decline or cease over time due to system-level approaches to care, that can restrict the availability of home care supports and services and client eligibility [ 19 ], creating barriers to access and utilization. Clients and families might also react to inconsistencies in care, high staff turnover [ 20 ] and perceptions of insufficient resources, inadequate and depersonalized care [ 21 , 22 ] by reducing, ceasing or refusing their service use. Safety issues can also arise related to security, cleanliness and maintenance of homes, family and friend caregiver knowledge and skills [ 23 ], home support worker competencies, reassessments, and responsiveness in adapting care to changes in client and carer needs [ 18 , 24 , 25 , 26 ]. When clients do not access appropriate home support services at critical points, and when family and friend caregivers are not adequately supported, service trajectories [ 27 , 28 ] and outcomes are negatively impacted [ 28 , 29 , 30 ] and some can experience a potentially avoidable entry into long term residential care [ 31 ].
A few studies offer insights into family and friend caregiver experiences [ 32 , 33 , 34 , 35 ], including their interactions with the health and/or long term care system [ 36 , 37 ], helping us to start to comprehend older adult care pathways over time. While medical care is most commonly delivered by professionals, family and friend caregivers provide many other necessary supports including transportation, help with domestic tasks and home maintenance duties, and emotional support [ 2 , 38 ]. Recent research confirms that caregiver inability to continue is one predictor of increased likelihood of entering residential care [ 18 ], yet the recognition of the importance of supporting their role varies within the home care system [ 39 , 40 ].
In Canada, where home care is not an insured service under the Canada Health Act, provinces, territories and geographic jurisdictions set their own parameters on the level and type of publicly funded home and community care that is provided. Due to differences in definitions, services and data collection and reporting measures, there is limited comparative information about home and community care across jurisdictions [ 3 , 41 ]. Yet the availability of home and community based supports and services varies in different locations depending on jurisdictionally specific contextual factors, such as varying eligibility to receive care, public coverage of services, residency requirements, and access to services [ 42 ]. To date, no known studies have explored and compared how jurisdictional differences in approaches to care influence client and family and friend caregiver pathways through the home care system. By combining quantitative and qualitative research components, this study will generate evidence to address this gap and inform future home care policy and practice.
Study goal and research questions
The overall goal of this study is to enhance understanding of home care client pathways of older adults with chronic and long term conditions through home care. Specifically, we will examine how approaches to care in two jurisdictions in Canada shape pathways through the home care system, from client and family and friend caregiver, provider and system level perspectives. Our overarching research question is: How do approaches to care shape older adult home care client pathways through the home care system in two health authorities in Canada? Three inter-related research streams (Client/Service Data Stream, Constellation Data Stream, Policy Stream) will address this research question (see fig. 1 ).

Research question and interrelated research streams
Approaches to care
Approaches to care, as defined in this study, encompass the philosophies and structures of care, as reflected and manifested in home care policies, programs and practices, within and across jurisdictions. Approaches to care inform client and care worker interactions, perceptions of family and friend caregivers, assessment and reassessment, care planning, care coordination, and care provision. Approaches to care at multiple levels (provincial, regional, office or agency) shape the kinds of supports and services that are either delivered publicly or purchased privately. These approaches influence who receives what level of services and for how long, the human resources and organizations needed to deliver and maintain standards of care, the expected contribution of family and friend caregivers, and the public and/or private costs associated with this care.
We will examine approaches to care by examining the home care pathways of older adult clients with chronic and long term conditions at two study sites in Canada. These sites are the Winnipeg Regional Health Authority (WRHA, one of five health authorities in the province of Manitoba) and the Nova Scotia Health Authority (NSHA, Nova Scotia’s single health authority). Nova Scotia (NS) and Manitoba (MB) have distinct geographic and cultural compositions, yet both are experiencing population aging and increased demand for home care services [ 43 , 44 , 45 , 46 ]. However, the home care systems have notably different staffing and delivery models. NS has a single health authority model in which agencies are funded by the Department of Health and Wellness (DHW) and contracted by the NSHA to deliver home care services to NSHA clients, which is distinct from the public provider model in MB in which health authority employees directly manage and, in most cases, deliver home care, through five health authorities. However, home care in both sites is embedded in a similar governance structure, whereby policy is set at the provincial health ministry level. Therefore, the case comparison of the sites will involve understanding relevant provincial policy and strategic direction.
The Home Care Pathways study is a longitudinal, two province, mixed-methods study involving a retrospective analysis of administrative data, alongside a prospective qualitative comparative case study of interview data and policy documents to identify when, where and how approaches to care influence home care client pathways (see figs. 1 and 2 ). We adopt a partnered Integrated Knowledge Translation (iKT) approach which is operationalized in the study’s structure ensuring partners are contributing to both knowledge discovery and application [ 47 ]. The study includes partners representing academic, decision-maker (provincial health ministry and health authority) perspectives and representatives from provider agencies on each stream-level working group. As well, the study’s management group, which includes academic and knowledge user members, share in the decisions regarding overall direction of the study.
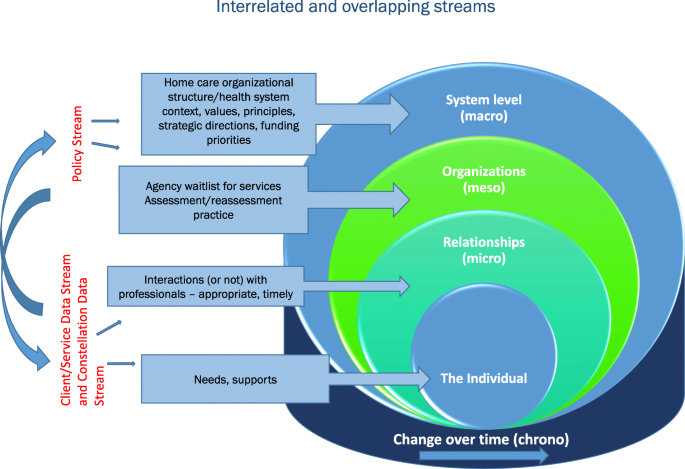
Guiding framework: Socio-ecological Model
Guiding framework: a socio-ecological framework
The Socio-ecological Model is a systems framework, that informs this research design to help guide the examination of interlocking spheres of influence (e.g., chrono, macro, meso, micro systems) to illustrate how client pathways shape and are shaped by individual circumstances, social interactions and organizational and system-level approaches to care (see Figure 2 ) [ 48 , 49 ].
Using a socio-ecological framework to inform all three research streams draws attention to the dynamic and reciprocal interplay of individual, family, community and organizational factors and the intersection of time throughout the analysis process. For example, our interpretation of individual circumstances as understood through the Client/Service Data Stream and Constellation Data Stream will be enhanced by recognizing that these circumstances are influenced by meso factors (e.g., a home care agency’s waitlist for services) which may influence resource allocation decisions (e.g., budget priorities at a funder level).
Research activities will occur over a three-year period, and are detailed below for each Stream.
Research question # 1. What are the common pathways of older adult home care clients through the home care system? (client/service data stream)
The goal of the Client/Service Data Stream is to identify and examine person and health service-level factors related to an older client’s pathway – their clinical status and trajectory of care after admission to publicly funded home care. Our objectives are to: a) describe and understand the client population at admission to home care and over time; b) review quality of care, patterns of health service utilization after admission, and outcomes of home care clients; and c) compare and contrast clients’ clinical status and trajectory of home care between two provinces.
The Client/Service Data Stream involves a population-based retrospective cohort study that will use several MB and NS health data sources linked to a cohort of older adult home care clients. Clients admitted to home care will be followed for up to four years after their admission date to review change in clinical status and health system use over time. Client characteristics including health status, will be identified through the clinical assessment used by both the WRHA and NSHA, the interRAI assessment for Home Care (HC) (Resident Assessment Instrument RAI-HC). RAI-HC data from admission and follow up assessments will capture any change in client clinical status (improvement or decline) or maintenance in status over time. The RAI-HC initial assessment dates for the home care client cohort will be used to examine health service utilization in the following four years. Services examined will include amount and types of home care, emergency department visits, hospital stays, physician visits, and long term care admission.
Study cohort
The cohort will consist of all clients age 60 years and older at the time of admission to home care, who received non-clinical home care supports after admission. Older clients admitted to home care between January 1, 2011 to December 31, 2013, and who have at least one other assessment by the end of 2017, will form the study cohort. The cohort is estimated to be approximately 5500 individual home care clients in each study site, enabling techniques to be employed to detect relationships or difference.
Data analysis for this study includes two phases. The first phase entails descriptive analysis to characterize the study cohort and changes in clinical status they experience over time based on the RAI-HC data. Home care assessment patterns and service allocation will be described along with other health service utilization. Retrospective analysis of clinical and health service utilization data will provide empirical data on actual interactions within the formal system and client patterns of utilization. The clients’ status at the end of the four-year follow-up will be reported – whether they remain in community, are admitted to long term care, or have some other disposition. The second phase of analysis will involve longitudinal analysis and multivariate modelling to estimate home care client trajectories. A number of variables will be examined for their potential effect on trajectories, such as changes in client health status, family caregiver involvement, and home care service levels, as well as home care assessment frequency and occurrence of other health service use.
The data linkage and analyses undertaken in this study will allow us to examine the various pathways of clients within the home care system and what factors are related to these pathways. Comparison of results between MB (WRHA) and NS (NSHA) will establish similarities and differences in client pathways between the two jurisdictions.
Challenges and mitigation strategies
Home care client data are protected by privacy legislation and accessible only by request to data custodians and ethics boards in each province. Timely data access and data linkage challenges will be mitigated by direct participation of health authorities and provincial health ministries. Contracting analysis of data at each site (WRHA and NSHA) to a single individual will promote replicability and consistency across the sites.
Research question #2. How are service pathways shaped by (and in turn shape) the experiences of home care recipients, family and friend caregivers, home support workers and health care professionals? (constellation data stream)
The goal of the Constellation Data Stream is to explore individual experiences of clients, their family and friend caregivers (where available), and providers and coordinators of home care supports and services to understand how complex factors shape client service pathways in each study site, including identifying similarities and differences across urban and rural areas.
A prospective qualitative comparative case study design will be used, drawing on data from individual interviews conducted with members of 12 pre-defined care constellations (six in each study site). Interview questions will be initially retrospective to understand impetus for accessing home care service, and will include probes for specific experiences and examples of changes in care (as well as reasons for these changes). Care/Case coordinators and home support workers will be asked to comment on the client’s care plan but also more generally about policies shaping their work, as well as clients’ service use over time and decision making around service allocation and case management. Constellations will be followed over 18 months at three points in time every six months to observe potential changes in chronic care conditions of study participants and services provided. Findings will enhance understanding of contextual factors affecting client pathways (e.g., changes in cognition, resources), and the pathways preferred by clients.
Care constellations will be identified and theoretically sampled based on pathway typologies used in the Client/Service Data Stream: improve, maintain, decline . Each care constellation will include no less than three people, including a home care client aged 60 years or older residing in the community (with a Cognitive Performance Scale [CPS] score of 0–1), their care/case coordinator, and their home support worker. When available, that client’s family or friend caregiver will be included. Other professionals might be included depending on the care structure in respective jurisdictions; for instance, in NSHA, where care is delivered through contracted agencies, an agency supervisor will be included in the constellation.
It is estimated that between 42 and 54 individuals affiliated with 12 care constellations will be interviewed. This design maximizes the depth of data obtained for any particular care constellation and provides confidence that data saturation can be achieved. Specifically, the sample size will allow sufficient breadth and depth of data to identify patterns and build theory [ 50 , 51 ].
Transcribed interview data will be analyzed through complementary cross-sectional (thematic) [ 52 ] and temporal analyses – the latter to ascertain changes in experience of pathways over time [ 53 ]. Moreover, these cross-sectional and temporal analyses will attend to both within-constellation and between-constellation variation. This case study comparison approach [ 54 ] will be informed by the socio-ecological framework and findings from the policy review (Policy Stream described below).
Team members from the two study sites will inform and support recruitment. Client recruitment will draw on expertise and experience of case/care coordinators to identify clients who fit the study criteria. In Nova Scotia, agreement will be obtained from four agencies to support their staff to participate. Strategies to address potential client attrition include recruiting clients at Time 1 with CPS scores of 0–1, and conducting exit interviews with other members of a constellation if a client dies. Team members have experience in the ethical engagement of research participants who may have cognitive impairment (e.g., recruitment, informed consent).
Research question #3. How do policy contexts inform approaches to care and shape client pathways? (policy stream)
The goal of the Policy Stream is to contribute to understanding how the structure of home care in the two study sites can shape client pathways, through an analysis of the policy context of home care programs in NS and MB.
A policy document analysis [ 55 , 56 ] and comparative case study design (where the province/jurisdiction is the case) will be used to review key policy documents that guide or structure how care is delivered. Key informant interviews will be conducted in each province to contextualize this analysis, which will also be informed by emerging findings or policy-related questions arising from the Client/Service Data Stream and Constellation Data Stream. Interview questions will focus on the intent/goal of the home care program, its values, and challenges and opportunities. Knowledge user team members will assist in the identification of relevant documents and key informants.
Documentation will include policies, guidelines, manuals, and other materials (including strategic documentation and website content) used by the provincial health ministries and health authorities (NSHA and WRHA) to guide home care. Key informant interviews will be conducted with approximately 10 senior decision-makers in each province, at health department, health authority, and agency (in NS) level to provide further insight into the development, operationalization and interpretation of the policies. This number of key informant participants is considered sufficient, given that the study has only two jurisdictions and the role of key informant interviews is to provide a secondary source of information to validate and/or enhance understanding and interpretation of information collected from the policy document analysis.
A content analysis will be undertaken to describe the home care policy context in each jurisdiction (e.g., legislation, oversight, program delivery, caregiver support, scope of practice). Results from this analysis will provide the framework for better understanding the approach to care in each jurisdiction. These insights will enhance interpretation of other Streams’ findings into individual and family and friend caregiver experiences of home care, and service access and delivery considerations. Analysis of key informant interviews will contextualize findings from the streams and will help to identify policy actions and inactions that shape client pathways within and across the study sites, and the structural and contextual constraints and enablers in each jurisdiction.
Home care services and approaches to care are multidimensional and complex [ 28 , 44 ] emerging from the intersection of varying policies. Not all policies may be well known, or formalized, and those that are formalized may in fact have very little influence on operational aspects of home care service delivery. They may also be implemented in different and unintended ways. The iKT model and engaged knowledge users from health ministries and health authorities will guide our interpretation of the policy context and the implementation process, as will the information collected from key informants, and participants interviewed in the Constellation Data Stream.
Ethics approval for the Client/Service Data Stream and Constellation Data Stream was obtained using a two-site model, with oversight at Mount Saint Vincent University. For the Client/Service Data Stream, the WRHA study site ethics was approved by the University of Manitoba Health Research Ethics Board (HS22118) and the NSHA study site ethics by the Nova Scotia Health Authority Research Ethics Board. For the Constellation Data Stream, the MB study site ethics was approved by the University of Manitoba Psychology/Sociology Research Ethics Board (HS22462) and by the WRHA Research Access and Approval Committee (2019–003) and the NSHA study site ethics by the Nova Scotia Health Authority Research Ethics Board. For the Policy Stream, ethics approval for key informant interviews was obtained by the Mount Saint Vincent University Research Ethics Board. All site/stream level clearances received by ethics boards external to Mount Saint Vincent University obtained expedited review and clearance by the Mount Saint Vincent University Research Ethics Board, as the home institution for the Nominated Principal Applicant (NPA) and institution responsible for administering grant funds. Informed consent will be obtained from all interview participants (Constellation Data Stream and Policy Stream). For the Constellation Data Stream, consent will be ongoing and reviewed at each of the time points for the interview participants. While mild to moderate cognitive impairment of home care clients is not an eliminating factor, screening will occur as follows to ensure that cognitive impairment is minimal: care/case coordinators will be asked to select potential client participants with a CPS of 0–1; additional screening (in the form of questions confirming their comprehension of study information) will occur with clients at the time of informed consent [ 57 ].
Implementing a multi-dimensional study of this kind is complex. In a two-site model, in two jurisdictional contexts, timelines may diverge. With three streams, continued emphasis on the linkages between each stream’s research and the overall research question is important. However, the iKT model, together with a governance structure that includes high-level representation from each site, are strengths. This study’s findings stand to uniquely contribute to the evidence base on older adult home care client pathways over time. In addition to adding to what is known about home care in less studied jurisdictions of Canada (a gap identified by Johnson and colleagues) [ 58 ], the study will make the following contributions to scientific literature.
First, our study will take a longitudinal approach to comprehend care pathways through both a retrospective analysis of client pathways, and a prospective case study of care constellation member experiences over 18 months (while incorporating some retrospective data, for clients and families, on experiences over the last few years before Time 1). An understanding of home care policies in place during the time span covered by the service utilization data (2011–2017), as well as current policies will help to contextualize the research findings from the first two streams.
Second, our study outcomes will reflect unique cross-jurisdictional knowledge of approaches to care for older clients. For instance, many provincial publicly funded home and community-based programs and services claim to be organized by client-centered approaches to care [ 59 ]. However, it is not always clear how approaches to care are defined, translated into practice and policy, and how outcomes are evaluated. This makes it difficult to evaluate the influence of home supports and services on client pathways, and to assess the ability of the home care system to adapt and respond to changes in client care needs. Study results will identify potential differences between approaches to care as defined by the home care programs and how these are experienced by clients and their families. Comparing results from the two study sites will be a unique contribution that provides a nuanced understanding of the complexity of client pathways and provides an opportunity to analyze any commonalities or differences in experiences within the context of each jurisdiction’s distinct home care delivery model.
Third, the direct involvement of knowledge users from study conception to team composition and research design will facilitate timely access to client data (Client/Service Data Stream) and study research participants (Constellation Data Stream) and will guide our interpretation of the policy context (Policy Stream). Our knowledge users will aid in ensuring that findings are used to address knowledge gaps within the continuing care sector, and challenges can be better foreseen and addressed. Inclusion of knowledge users helps ensure that knowledge products will be relevant for provincial health ministries and regional health authorities, caregiver organizations and home care agencies.
Home care and non-clinical support services provided to older adults and family and friend caregivers in the community can vary highly across jurisdictions in Canada. By combining a novel longitudinal, mixed-methods design informed by the socio-ecological model and an integrated knowledge translation approach, this study will generate evidence to inform decision making and practice in home care specifically for two Canadian health authorities, and be of interest to other jurisdictions as well. This study uniquely incorporates clinical data and experimentation data from clients, family and friend caregivers, and those coordinating and providing care, about factors that shape care pathways as embedded in the policy landscapes of two provincial home care programs. We will produce knowledge products that identify, specify and characterize the types of care pathways, and delineate the approaches to care that shape them. Through our partnership of researchers and knowledge users, outcomes will be used to project utilization, inform strategic planning and decision-making, and support changes in care practice.
Availability of data and materials
Not applicable.
Abbreviations
Cognitive Performance Scale
Department of Health and Wellness (Nova Scotia)
Integrated Knowledge Translation
Nova Scotia
Nova Scotia Health Authority
Nominated Principal Applicant
Resident Assessment Instrument – Home Care
Winnipeg Regional Health Authority
National Institute on Ageing. Enabling the future provision of long-term care in Canada. Toronto: National Institute on Ageing; 2019. p. 161. Available from: https://cnpea.ca/images/futureoflong-termcare_v7_final-09-09-2019.pdf .
Sinha M, Bleakney A. Receiving care at home. Ottawa: Statistics Canada; 2014. p. 18. Catalogue no. 89–652-X – No.002. Available from: https://www150.statcan.gc.ca/n1/pub/89-652-x/89-652-x2014002-eng.htm .
Canadian Healthcare Association. Home care in Canada: From the margins to the mainstream. Ottawa: Canadian Healthcare Association; 2009. p. 152. Available from: https://www.healthcarecan.ca/wp-content/themes/camyno/assets/document/PolicyDocs/2009/External/EN/HomeCareCanada_MarginsMainstream_EN.pdf .
Health Council of Canada. Seniors in need, caregivers in distress: What are the home care priorities for seniors in Canada? Ottawa: Health Council of Canada; 2012. p. 68. https://healthcouncilcanada.ca/files/HCC_HomeCare_FA.pdf .
Kane R, Lum T, Kane R, Homyak P, Parashuram S. Does home- and community- based care affect nursing home use? J Aging Soc Policy. 2013;25(2):146–60. https://doi.org/10.1080/08959420.2013.766069 .
Canadian Institute for Health Information. Seniors in transition: exploring pathways across the care continuum. Ottawa: Canadian Institute for Health Information; 2017. p. 45. Available from: https://www.cihi.ca/sites/default/files/document/seniors-in-transition-report-2017-en.pdf .
Chappell N. Population aging and the evolving needs of older Canadians: An overview of the policy challenges . Montreal: Institute for Research on Public Policy; 2011. 31 p. Study No. 21.
Toews R. Future of home care services in Manitoba. Winnipeg: Minister of Health, Seniors and Active Living (MB); 2016. p. 99. Available from: https://www.gov.mb.ca/health/homecare/future_homecare.pdf .
Martin-Matthews A, Sims-Gould J, Tong CE. Canada’s complex and fractionalized home care context: Perspectives of workers, elderly clients, family carers, and home care managers. Canadian Review of Social Policy. 2013;(68/69):55–74.
Neysmith S. Caring and aging: examining policy inequities. In: Westhues A, Wharf B, editors. Canadian social policy: issues and perspectives. Waterloo (ON): Wilfrid Laurier Press; 2013. p. 297–314.
Google Scholar
Weeks LE, Keefe J, MacDonald DJ. Factors predicting relocation among older adults. J Hous Elderly. 2012;26(4):355–71. https://doi.org/10.1080/02763893.2011.653099 .
Chen YM, Berkowitz B. Older adults’ home- and community-based care service use and residential transitions: a longitudinal study. BMC Geriatr. 2012;12(44):1–12. https://doi.org/10.1186/1471-2318-12-44 .
Chen YM, Adams Thompson E, Berkowitz B, Ward D. Factors and home- and community-based services (HCBS) that predict older adults’ residential transitions. J Serv Sci Manag. 2011;4(3):368–79. https://doi.org/10.4236/jssm.2011.43043 .
Xu H, Weiner M, Paul S, Thomas J, Craig, B, Roseman M. et al. Volume of home and community-based Medicaid waiver services and risk of hospital admissions. J Am Geriatr Soc. 2010;58(1):109–15. https://doi.org/10.1111/j.1532-5415.2009.02614.x .
Panagiotoglou D, Keefe J, Fancey P, Martin-Matthews A. Job satisfaction and the context of care work by home support workers: Insights from three Canadian jurisdictions. Can J Aging. 2017;(36)1:1–14. https://doi.org/10.1017/S0714980816000726 .
Denton M, Zeytinoglu IU, Davis S. Working in clients’ homes: the impact on the mental health and well-being of visiting home care workers. Home Health Care Serv Q. 2002;21(1):1–27.
Article Google Scholar
Sims-Gould J, Byrne K, Craven C, Martin-Matthews A, Keefe J. Why I became a home support worker: recruitment in the home health sector. Home Health Care Serv Q. 2010;29(4):171–94. https://doi.org/10.1080/01621424.2010.534047 .
Doran DM, Hirdes JP, Blais R, Baker GR, Poss JW, Li X, McIsaac C. Adverse events associated with hospitalization or detected through RAI-HC assessment among Canadian home care clients. Healthc Policy. 2013;9(1):76–88.
PubMed PubMed Central Google Scholar
Fancey P, Keefe J. Home to nursing homes: Understanding factors that impact the path seniors take. 2014. Report contracted by the Nova Scotia Department of Health and Wellness, Continuing Care Branch.
Dill DM, Keefe J, McGrath DS. The influence of intrinsic and extrinsic job values on turnover intention among continuing care assistants in Nova Scotia. Home Health Care Serv Q. 2012;31(2):111–29. https://doi.org/10.1080/01621424.2012.681526 .
Aronson J. Elderly people’s accounts of home care rationing: missing voices in long-term care policy debates. Aging & Society. 2002;22(4):399–418. https://doi.org/10.1017/S0144686X02008759 .
Funk LM, Stajduhar KI, Cloutier-Fisher D. Exploring family caregivers’ rationales for nonuse of formal home health services when caring for a dying family member. Home Health Care Manag Pract. 2011;23(5):318–28. https://doi.org/10.1177/1084822310384920 .
Urbanik C, Lobchuk M. Encouraging family caregivers to “step inside the patient’s shoes”. Home Healthc Nurse. 2009;27(4):213–8. https://doi.org/10.1097/01.NHH.0000349906.89989.d1 .
Lang A, Macdonald M, Storch J, Stevenson L, Mitchell L, Barber T, et al. Researching triads in home care: perceptions of safety from home care clients, their caregivers, and providers. Home Health Care Manag Pract. 2014;26(2):59–71. https://doi.org/10.1177/1084822313501077 .
Lang A, MacDonald M, Storch J, Elliott K, Stevenson L, Lacroix H, et al. Home care safety perspectives from clients, family members, caregivers and paid providers. Healthcare Q. 2009;12:97–101. https://doi.org/10.12927/hcq.2009.20720 .
MacDonald M, Lang A, Storch J, Stevenson L, Barber T, Laboni K, et al. Examining markers of safety in homecare using the international classification for patient safety. BMC Health Serv Res. 2013;13:191–201. https://doi.org/10.1186/1472-6963-13-191 .
Turcotte M. Canadians with unmet home care needs. Ottawa: Statistics Canada; 2014. p. 14. Catalogue no. 75–006-X. Available from: https://www150.statcan.gc.ca/n1/en/pub/75-006-x/2014001/article/14042-eng.pdf?st=5JpmlbSf .
Robison J, Shugrue N, Porter M, Fortinsky RH, Curry LA. Transition from home care to nursing home: unmet needs in a home- and community-based program for older adults. J Aging Soc Policy. 2012;24(3):251–70. https://doi.org/10.1080/08959420.2012.676315 .
Canadian Institute for Health Information. Supporting informal caregivers – The heart of home care. Canadian Institute for Health Information; 2010. p. 22. Available from: https://secure.cihi.ca/free_products/Caregiver_Distress_AIB_2010_EN.pdf .
Gaugler J, Kane R, Kane R, Newcomer R. Unmet care needs and key outcomes in dementia. J Am Geriatr Soc. 2005;53(12):2098–105.
Sarma S, Hawley G, Basu K. Transitions in living arrangements of Canadian seniors: findings from the NPHS longitudinal data. Soc Sci Med. 2009;68(6):1106–13.
Cloutier DS, Penning MJ. Janus at the crossroads: perspectives on long-term care trajectories for older women with dementia in a Canadian context. Gerontologist. 2017;57(1):68–81. https://doi.org/10.1093/geront/gnw158 .
Turpin L. Ward-Griffin C. The meaning of a positive client-nurse relationship for senior home care clients with chronic disease. Can J Aging. 2012;31(4):457–69. https://doi.org/10.1017/S0714980812000311 .
Fraser K, Nissen C. Uncovering the meaning of home care using an arts-based and qualitative approach. Can J Aging. 2014;33(3):246–58. https://doi.org/10.1017/S0714980814000191 .
St-Amant O, Hall J. Making decisions in home-based dementia care: why context matters. Can J Aging. 2012;31(4):423–34. https://doi.org/10.1017/S0714980812000396 .
Gruneir A, Fung K, Fischer HD, Bronskill SE, Panjwani D, Bell CM, et al. Care setting and 30-day hospital readmissions among older adults: a population-based cohort study. CMAJ. 2018;24(190):E1124–33. https://doi.org/10.1503/cmaj.180290 . .
Penning MJ, Cloutier DS, Nuernberger K, MacDonald SWS, Taylor D. Long-term care trajectories in Canadian context: patterns and predictors of publicly funded care. J Gerontol B Psychol Sci Soc Sci. 2016;73(6):1077–87. https://doi.org/10.1093/geronb/gbw104 .
Sims-Gould J, Martin-Matthews A. We share the care: family caregivers' experiences of their older relative receiving home support services. Health Soc Care Community. 2010;8(4):415–23. https://doi.org/10.1111/j.1365-2524.2010.00913.x .
Guberman N, Keefe J, Fancey P, Barylak L. ‘Not another form!’: Lessons for implementing carer assessment in health and social service agencies. Health Soc Care Community. 2007;15(6):577–87. https://doi.org/10.1111/j.1365-2524.2007.00718.x .
Guberman N, Lavoie JP, Pepin J, Lauzon S, Montejo ME. Formal service practitioners’ views of family caregivers’ responsibilities and difficulties. Can J Aging. 2006;25(1):43–53. https://doi.org/10.1353/cja.2006.0024 .
Hermus G, Stonebridge C, Thériault L, Bounajm F. Home and community care in Canada: an economic footprint. The Conference Board of Canada. 2012;23:1–66. Available from http://www.conferenceboard.ca/temp/65572e9a-c2b1-470e-81b1-651b35a01d36/12-306_homeandcommunitycare_prt.pdf .
Williams PA, Lum J, Deber R, Montgomery R, Kuluski K, Peckham A, Zhu L. Aging at home: integrating community-based care for older persons. Healthcare Papers: New Models for the New Healthcare. 2009;10(1):8–21.
Health Association Nova Scotia. Rising to the challenge: Responding to increasing demands in home care. Bedford (NS): Health Association Nova Scotia; 2014. p. 56. Available from https://www.healthassociation.ns.ca/res/base/documents/library/research%20and%20policy/6%20home%20support%20-%20responding%20to%20increased%20demands%20-%20%20final20july207%202014.pdf .
Ricard N. Manitoba home care program. Winnipeg (MB): Office of the Auditor General; 2015. p. 49. Available from: http://www.oag.mb.ca/wp-content/uploads/2015/08/Manitoba-Home-Care-Program-Report-Web-Version.pdf .
Mitchell L, Roos NP, Shapiro E. Patterns in home care use in Manitoba. Can J Aging. 2005;24(Suppl 1):59–68. https://doi.org/10.1353/cja.2005.0053 .
Manitoba Health. Advancing continuing care: a blueprint to support system change. Manitoba: Health, Seniors and Active Living; 2014. p. 12. Available from: https://www.gov.mb.ca/health/documents/blueprint.pdf .
Canadian Institutes of Health Research. Guide to knowledge translation planning at CIHR: Integrated and end-of-grant approaches. Ottawa: Canadian Institutes of Health Research; 2015. p. 34. Available from http://www.cihr-irsc.gc.ca/e/45321.html .
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77. https://doi.org/10.1177/109019818801500401 .
Andrew MK, Keefe JM. Social vulnerability from a social ecology perspective: a cohort study of older adults from the National Population Health Survey of Canada. BMC Geriatr. 2014;14:90. https://doi.org/10.1186/1471-2318-14-90 .
Morse JM. Determining sample size. Qual Health Res. 2000;10(1):3–5.
Morse JM. The significance of saturation. Qual Health Res. 1995;5(2):147–9.
Braun V, Clark V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. https://doi.org/10.1191/1478088706qp063oa .
Thomson R, Holland J. Hindsight, foresight and insight: the challenges of longitudinal qualitative research. Int J Soc Res Methodol. 2013;6(3):233–44. https://doi.org/10.1080/1364557032000091833 .
Flyvbjerg B. Five misunderstandings about case-study research. Qual Inq. 2016;12(2):219–45. https://doi.org/10.1177/1077800405284363 .
Yanow D. Conducting interpretive policy analysis. Thousand oaks. CA: SAGE.
Cheung KK, Mirzael M, Leeder S. Health policy analysis: a tool to evaluate in policy documents the alignment between policy statements and intended outcomes. Aust Health Rev. 2010;34(4):405–13. https://doi.org/10.1071/AH09767 .
Palmer BW, Dunn LB, Appelbaum PS, Mudaliar S, Thai L, Henry R, et al. Assessment of capacity to consent to research among older persons with schizophrenia, Alzheimer disease, or diabetes mellitus: comparison of a 3-item questionnaire with a comprehensive standardized capacity instrument. Arch Gen Psychiatry. 2005;62(7):726–33. https://doi.org/10.1001/archpsyc.62.7.726 .
Johnson S, Bacsu J, Abeykoon H, McIntosh T, Jeffrey B, Novik N. No place like home: a systematic review of home care for older adults in Canada. Can J Aging. 2018;37(4):400–19. https://doi.org/10.1017/S0714980818000375 .
Veteran’s Affairs Canada [Internet]. Client-centred approach. Government of Canada; 2015. Available from: http://www.veterans.gc.ca/eng/services/transition/case-management/approach#implement .
Download references
Acknowledgements
We thank Pamela Fancey of the Nova Scotia Centre on Aging, Mount Saint Vincent University for support with coordinating the production of this manuscript.
This study is funded by the Canadian Institutes of Health Research (CIHR) (funding reference number 155950) and was independently peer-reviewed by the funder. CIHR has not been involved in the design of the study or in writing of this manuscript, nor will CIHR be involved in data collection, analysis or interpretation of data.
Author information
Authors and affiliations.
Department of Family Studies and Gerontology and Nova Scotia Centre on Aging, Mount Saint Vincent University, Halifax, Nova Scotia, B3M 2J6, Canada
Janice M. Keefe
Department of Sociology, University of Manitoba, Winnipeg, Manitoba, Canada
Nova Scotia Centre on Aging, Mount Saint Vincent University, Halifax, Nova Scotia, Canada
Lucy Knight
Helen Glass Centre for Nursing, University of Manitoba, Winnipeg, Manitoba, Canada
Michelle Lobchuk
Faculty of Nursing, Dalhousie University, Halifax, Nova Scotia, Canada
Marilyn Macdonald
Home Care Program, Winnipeg Regional Health Authority, Winnipeg, Manitoba, Canada
Lori Mitchell
Julie Rempel
School of Occupational Therapy, Dalhousie University, Halifax, Nova Scotia, Canada
Grace Warner
Continuing Care, Nova Scotia Health Authority, Halifax, Nova Scotia, Canada
Susan Stevens
You can also search for this author in PubMed Google Scholar
Contributions
JK, LF, ML, MM, LM, GW and SS made substantial contributions to the conception and design of this study. JK maintains overall responsibility for the study in consultation with ML (Manitoba site lead) and SS (lead Knowledge User). LM is lead of the Client/Service Data Stream. LF is lead of the Constellation Data Stream. JK is lead of the Policy Stream. All authors (JK, LF, LK, ML, MM, LM, JR, GW, SS) were involved in drafting and critically revising the manuscript. All authors (JK, LF, LK, ML, MM, LM, JR, GW, SS) read and approved the final manuscript.
Corresponding author
Correspondence to Janice M. Keefe .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained using a two-site model, with site-specific clearances received for the Client/Service Data Stream and the Constellation Data Stream, and secondary clearances received from the study lead’s institutional research ethics board at Mount Saint Vincent University. Client/Service Data Stream: Primary ethics approval for the WRHA (Manitoba) study site was obtained from the University of Manitoba Health Research Ethics Board (Ethics # HS22118[H2018:349]). Primary ethics approval for the NSHA (Nova Scotia) study site was obtained from the Nova Scotia Health Authority Research Ethics Board (File # 1024323). Secondary approvals for each study site were obtained from Mount Saint Vincent University Research Ethics Board (File # 2018–087[Manitoba]; File # 2018–202[Nova Scotia]). Constellation Data Stream: Primary ethics approval for the WRHA (Manitoba) study site was obtained from the University of Manitoba Psychology/Sociology Research Ethics Board (Protocol # P2018:146 [HS22462]) and by the WRHA Research Access and Approval Committee (Reference no. RAAC 2019–003). Primary ethics approval for the NSHA (Nova Scotia) study site was obtained from the Nova Scotia Health Authority Research Ethics Board (File # 1024409). Secondary approvals for each study site were obtained from Mount Saint Vincent University Research Ethics Board (File # 2018–117[Manitoba]; File # 2018–209[Nova Scotia]). Policy Stream: Ethics approval for the study lead to conduct key informant interviews was approved by the Mount Saint Vincent University Research Ethics Board (File # 2019–187).
Processes to obtain informed consent have been approved, where required, by respective research boards. Constellation Data Stream: An informed consent form will be mailed or emailed to each participant approximately one week in advance of their interview, to allow the participant an opportunity to review the form and raise any questions. Written informed consent will then be obtained by the person conducting the interview, during an informed consent discussion prior to the interview commencing. Policy Stream: An informed consent form will be emailed to each participant in advance of their interview. Participants will be asked to sign and return the consent form prior to the interview. However, past experience interviewing key informants over the phone in their professional capacities suggests that signed consent forms may not always be returned by the time of the interview. If the form has not been returned prior to the interview, ethics approval is obtained to allow verbal consent to be given, and for the signed form to be emailed to research staff afterwards. Client/Service Data Stream: This stream uses data that is not personally identifiable. Approval to waive informed consent was obtained by the respective ethics boards.
Consent for publication
Competing interests.
SS is the Senior Director of Continuing Care with the Nova Scotia Health Authority, one of the partners of this research and a study site. LM is employed as a researcher on home care with the Winnipeg Regional Health Authority, the other study site.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Keefe, J.M., Funk, L., Knight, L. et al. Home care clients: a research protocol for studying their pathways. BMC Health Serv Res 20 , 535 (2020). https://doi.org/10.1186/s12913-020-05363-7
Download citation
Received : 01 May 2020
Accepted : 25 May 2020
Published : 12 June 2020
DOI : https://doi.org/10.1186/s12913-020-05363-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Home care policy
- Community health service needs
- Longitudinal analyses
- Mixed methods
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Search Menu
- Sign in through your institution
- Advance Articles
- Special Issues
- Supplements
- Virtual Collection
- Online Only Articles
- International Spotlight
- Free Editor's Choice
- Free Feature Articles
- Author Guidelines
- Submission Site
- Calls for Papers
- Why Submit to the GSA Portfolio?
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Journals Career Network
- About The Gerontologist
- About The Gerontological Society of America
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- GSA Journals
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Conflict of interest.
- < Previous
Care Home Life and Identity: A Qualitative Case Study
- Article contents
- Figures & tables
- Supplementary Data
Katie Paddock, Christine Brown Wilson, Catherine Walshe, Chris Todd, Care Home Life and Identity: A Qualitative Case Study, The Gerontologist , Volume 59, Issue 4, August 2019, Pages 655–664, https://doi.org/10.1093/geront/gny090
- Permissions Icon Permissions
The transition to a care home can involve multiple changes and losses that can affect an older person’s well-being and identity. It is not clear how older people perceive and manage their identity within a care home over time. This study explores how living in a care home affects the identities of residents and how they address this in their daily lives.
A multiple qualitative case study approach incorporated interview and observational data. Eighteen semistructured interviews and 260 hr of observations were conducted over 1 year with care home residents, relatives, and staff across three care homes within Greater Manchester, UK. Data were analyzed using framework analysis, drawing on the social identity perspective as an interpretive lens.
Four themes were identified: (a) changing with age, (b) independence and autonomy, (c) bounded identity, and (d) social comparison. The impact of aging that initially altered residents’ identities was exacerbated by the care home environment. Institutional restrictions jeopardized independence and autonomy, provoking residents to redefine this within the allowances of the care home. Strict routines and resource constraints of well-meaning staff resulted in the bounded expression of personalities. Consequently, to forge a positive identity, residents without dementia engaged in social comparison with residents with dementia, emphasizing their superior cognitive and physical abilities.
Social comparison as an adaptive strategy has previously been unidentified in care home literature. Residents need more support to express their identities, which may reduce the necessity of social comparison, and improve interrelationships and well-being.
Moving to long-term residential and/or nursing care facilities (hereafter referred to as “care homes”) involves a series of changes that can affect an older person’s sense of identity ( Froggatt, Davies, & Meyer, 2009 ; Næss, Fjær, & Vabø, 2016 ; Tajfel & Turner, 1979 ). Residents can become disconnected from facets or symbols of their identity, including social networks, familiar routines, recreational activities, and meaningful belongings. This disconnect can result in poor well-being or depression ( NCHR&D, 2006 ; Tester, Hubbard, Downs, MacDonald, & Murphy, 2004 ). In addition, the transition to a care home often occurs at the nadir of physical and/or cognitive abilities ( Kingston et al., 2017 ), thereby limiting residents’ functional abilities to adapt to this new context and increasing their reliance on care staff to facilitate identity maintenance. In England, supporting identities is a quality standard for care homes, but variations in care quality, limited resources, and poor workforce morale can impede such aims ( Alzheimer’s Society, 2013 ; Care Quality Commission, 2016 ; Lievesley, Crosby, Bowman, & Midwinter, 2011 ). To improve residents’ sense of identity in care homes, we must understand how it is negotiated within this complex context.
Few studies have explored the daily impact of life within care homes on identity, particularly from the perspectives of relevant stakeholders; residents, their significant others, and care home staff. In this article, we address this gap. We use the social identity perspective (SIP) as a theoretical lens to explore the strategies that residents use to adapt to life in a care home over time, and the daily contributions of others in the co-construction of residents’ identities.
SIP holds that individuals’ overall sense of identity is a composite of memberships to meaningful social groups (social identity) and idiosyncratic personal attributes (personal identity). Identity maintenance is an inherently social process that occurs across the life course, where different identities come to the fore within different salient contexts ( Hogg & Abrams, 1988 ; Oakes, Haslam, & Turner, 1994 ; Turner, 1982 ). Major life events, such as the transition to a care home, can disrupt connections to social groups and idiosyncratic attributes ( Hockey & James, 2003 ; NCHR&D, 2006 ; Kroger, Martinussen, & Marcia, 2010 ; Tajfel & Turner, 1979 ). Maintaining social relationships or establishing new connections buffers against negative outcomes ( A. Haslam, Jetten, Postmes, & Haslam, 2009 ; Jetten & Pachana, 2012 ), but studies have shown physical and interpersonal barriers to this ( Abbott, Bangerter, Humes, Klumpp, & Van Haitsma, 2017 ; Hubbard, Tester, & Downs, 2003 ), limiting opportunities to bolster identities within this new context.
Social groups are also judged by others as being of a higher or lower status, and the positivity of one’s identity is derived from the internalization of these evaluations ( Tajfel & Turner, 1979 ). Adaptive strategies can be used to maintain a positive identity when associated with a negatively perceived group ( Reicher, Spears, & Haslam, 2010 ; Tajfel, 1981 ; Tajfel & Turner, 1979 ). These include (a) social mobility: physically or psychologically leave the group and adopt a different identity; (b) social creativity: reframing the negativity as something positive, changing comparator dimensions to something more positive, or changing the comparison group to an even more negatively perceived group; and (c) social competition: direct competition with the outgroup. The use of these strategies will depend on the perceived permeability of the boundaries between groups. SIP, therefore, emphasizes the social- and context-dependent nature of identity.
SIP has been used in other social care areas ( Black et al., 2018 ; Iyer, Jetten, Tsivrikos, Postmes, & Haslam, 2009 ; Jetten & Pachana, 2012 ; Knight, Haslam, & Haslam, 2010 ), but it has been used much less frequently in care homes ( C. Haslam et al., 2014 ) and with little focus on the social- and context-dependent nature of identity from multiple perspectives. In this study, we use SIP to explore identity management within the care home context and incorporate the perspectives of residents, their relatives, and staff members. This will help inform approaches for supporting residents to maintain a positive sense of self and improve well-being, and improve their experiences of long-term care.
Study Design
This study used a multiple qualitative case study approach. Case study methodology facilitates the triangulation of multiple methods and sources of evidence to explore complex, context-dependent phenomena ( Walshe, Caress, Chew-Graham, & Todd, 2004 ; Yin, 2009 ), which is congruent with the inherently social and complex, context-dependent nature of identity management in SIP. Cases were defined as individual care homes. Within each case, data were collected using interview and observation methods (see below) to explore how daily life in a care home influences identity from multiple stakeholders’ perspectives.
The following theoretical propositions ( Yin, 2009 ), based on SIP and care home literature, were used to guide data collection and analysis:
Residents will renegotiate their identities within the context of the care home in light of new social relationships and interactions;
Maintaining links with previous social networks and habits (e.g., daily routines, personal décor) will be important for residents to maintain a sense of self; and
The care home environment will have the potential to accommodate a multitude of identities with adequate support from individuals and appropriate resources.
Within- and Cross-Case Sampling and Recruitment
Care homes in Greater Manchester, UK, were recruited through local research networks and via gatekeepers. Cases were purposefully sampled to vary in size (number of beds), location (high- or low-income areas), and building type (converted house or purpose-built facility). This aimed to acquire a broad range of experiences, and theoretical replication, where differing variables across cases are anticipated to yield contrasting results ( Yin, 2009 , 2010). The intended case sample was small to encourage rich, contextualized data, to understand the phenomenon under study ( Cleary, Horsfall, & Hayter, 2014 ; Geertz, 1973 ). Twenty-three care homes were approached to participate, and three care homes agreed. Table 1 illustrates basic information about the care homes.
Features of Participating Care Homes
Care home residents, family and friends, and staff, who met the following inclusion criteria, were eligible to participate: Residents aged 65 years or older, who had capacity to consent; all staff who had regular contact with residents, including managerial and nursing staff; all visitors who were a relative or long-term acquaintance of a resident (collectively termed “relatives” for ease). Staff identified residents with capacity to consent. Only individuals who could speak English were included, although only one resident was excluded by this constraint.
Prior to study commencement, the first author (K. Paddock) spent an introductory period within each care home. She introduced herself and the study, and engaged in informal conversations, to ensure that potential participants were comfortable with her presence and identified her as a researcher, not a visitor or staff member.
Convenience and purposeful techniques were used to sample residents, their relatives, and staff for interview. These included if residents/relatives had particularly positive or negative experiences of the move to a care home and subsequent adjustment or staff who were involved in daily decision making in the care homes or care of residents. Informed consent was obtained prior to recording of interviews. It was not possible to obtain written consent prior to observations due to the busy, often transient nature of care homes, and the risk of disrupting daily care or altering the dynamic of any event being observed. Information about the study and observations were displayed in each care home, and before each observation, individuals were verbally made aware of the researcher’s presence. Individuals could opt-out of observations via the researcher, members of staff, or opt-out form, and any field notes would then be excluded from analysis, an approach used elsewhere ( Conroy, 2017 ; Newnham, McKellar, & Pincombe, 2017 ). No individuals opted out.
Within-Case Methods: Data Collection
Semistructured topic guides were designed to provoke discussion of perceptions of the residents’ identity over their life course, their transition to the care home, and subsequent adjustment. Staff were asked for their perspectives on their roles in promoting identities within the care home, on perceived barriers and facilitators, and on residents’ adjustment over time. Questions included “Tell me about your move to the care home,” “What would you consider to be a ‘good’ day for you?” (Residents), “How would you describe [the resident]?”, “What would you consider to be meaningful activities for him/her?” (Relatives), “Tell me about a time a resident moved here,” “How do you incorporate individuality within the care home?” (Staff). Questions were developed iteratively to reflect emerging topics and themes.
Observations
All residents, staff, and relatives were eligible for inclusion in observations. Observations were exploratory and guided by SIP’s assertion that identities are influenced by social interactions and can be expressed externally, such as via hobbies and possessions. Observations and field notes focused on daily events in the care homes, including organized activities, daily care, and interactions between residents, staff, and visitors. Field notes also included conversations between participants and the first author. Residents without capacity to consent or opt-out were included in field notes for contextual purposes if they were central to observations involving other participants. Observations were a mixture of participatory and nonparticipatory: At times, the researcher remained a passive observer, but where possible she contributed informally to the daily life of the care homes by helping to serve meals and make drinks. This facilitated immersion in each care home and being allowed to witness personal care, such as dressing, an approach used in a similar context ( Næss et al., 2016 ). Observations occurred on different days and times of day, including evenings and weekends, to reduce the possibility that data were focused around particular activities or participants.
Data collection ceased once data saturation was reached, where no new findings emerge in subsequent data collection, within or across cases ( O’Reilly & Parker, 2012 ).
Data Analysis, Rigor, and Validity
Transcripts of recorded interviews and field notes were managed using NVivo and analyzed, within and cross-case, using framework analysis ( Ritchie & Spencer, 1994 ). This is a systematic and rigorous approach consisting of five interrelated stages (see Box 1 ), whereby iterative data collection and analysis of multiple data sources produce a transparent audit trail, so findings and interpretations are grounded in the data ( Gale, Heath, Cameron, Rashid, & Redwood, 2013 ; Ward, Furber, Tierney, & Swallow, 2013 ). The theoretical propositions derived from SIP (section Study Design) informed the preliminary coding framework, which was continuously reviewed in light of emergent data-driven codes and themes. Pattern-matching of data against a priori propositions reconciles the diverse perspectives of a phenomenon within and across cases ( Almutairi, Gardner, & McCarthy, 2014 ). Analysis generated a final analytic framework of 62 codes, grouped, and charted into four themes.
Familiarization
Immersion in the data. Read complete transcripts and field notes.
Identify a thematic framework
Initial development of a coding framework developed through a priori issues and familiarization stage.
The process of systematically applying the thematic framework to data. Changes made as necessary to reflect the data.
Using headings from thematic framework to create charts of data.
Mapping and interpretation
Searching for patterns and explanations in the data.
All data were collected by the first author (K. Paddock), who has prior experience working and researching in social care settings, but is not a clinician. She led data analysis, and regularly discussed emerging findings and experiences with the other three authors, two of whom (C. Brown Wilson and C. Walshe) are registered nurses with experience of working and researching in residential and social care.
Rigor and validity were ensured through the triangulation of multiple modes of data collection and sources of evidence across multiple cases, conducted over time. For respondent validation, the first author provided oral summaries of data and interpretations to participants, and invited comments.
To ensure reflexivity, the first author kept a reflexive diary alongside field notes to record her possible biases and role in shaping encounters. Developing a reflexive, iterative process between data collection and analysis continuously connected the data with emerging insights, leading to a more refined, and credible, understanding of identity ( Lincoln & Guba, 1985 ; Shenton, 2004 ; Srivastava & Hopwood, 2009 ).
Research Ethics Committee approval was obtained from the University of Manchester and Northampton NRES committee (reference number 12/EM/0431). All names have been changed to pseudonyms to protect anonymity. Permission was only granted by the ethics committees to interview residents with capacity to consent.
Semistructured interviews were conducted with 18 participants, and over 260 hr of observations were conducted over a 12-month period across the three cases (see Table 2 ). Interviews lasted between 18 min and 1.5 hr. The majority of residents across the care homes had severe dementia, so could not be interviewed. Some participants were intimidated by a recorded interview, and many staff were too busy, so preferred discussions to be included as field notes (see Table 2 ). Residents also received very few visitors during the data collection period.
Interview Sample and Observational Data Across Care Homes
Within-case analysis generated substantially similar experiences and themes in each care home, and thus, results from a cross-case analysis are presented, with any divergent themes discussed. The four interrelated themes are as follows:
Changing with age, and how this predated a move into a care home;
Bounded identity;
Independence and autonomy; and
Social comparisons.
Changing With Age
Prior to the relocation to a care home, residents and relatives acknowledged that increased frailty impeded residents’ abilities to perform everyday tasks and meaningful activities, which influenced their self-perception.
Ageing is a terrible thing . . . You can’t do what you used to do . . . (Hayley [resident], interview, Care Home 03)
Social networks and interactions gradually receded due to bereavements or family and friends moving away, which made residents feel disconnected and unable to be themselves:
I miss my people. Where are my people? They know who I am . . . (Philippa [resident], field notes, Care Home 02)
Residents adapted their homes, hobbies, and activities to accommodate these changes. For instance, Ruth (resident, Care Home 02) connected with her family and friends by knitting items for them, but her arthritis restricted her ability to hold knitting needles, so she began crocheting, which uses a different type of needles. This enabled Ruth to continue to make gifts and maintain a feeling of connectedness to important social networks.
The aging process had affected residents’ sense of self, but some had been able to employ strategies to help mitigate its impact. The care home further impeded their established identities and restricted residents’ abilities to adjust in a manner most acceptable to themselves.
Bounded Identity
Residents’ own homes served as a benchmark for the expression of their personal identities, particularly through possessions, clothing, and activities, but the care home environment largely restricted this.
Possessions
All participants agreed that personal possessions helped residents to express their personal and social identities and served as anchors to important memories.
When they wake up ‘til they go to sleep they have that sense of belonging. That this is my room now . . . I know that I bought that clock at such and such a place . . . and that picture there of my husband, that’s a reminder of me and my husband when I was younger . . . (Charlotte [staff, manager], interview, Care Home 02)
Staff emphasized that rooms could be personalized with furniture from home, but there was limited scope to do so because of the small size of most bedrooms. Residents had to relinquish many personal possessions, which upset them and their families, as this was associated with loss of important memories and symbols of identity. Julia (Care Home 01) had been a seamstress, her sewing machine a symbol of her independence, and an anchor for memories of her deceased husband. It was too large for the care home, and its loss signified the loss of important identities and memories:
. . . I’ll never operate the sewing machine again. It’s just the fact that [it’s in storage, not with her]. And it’s my past. (Julia [resident], interview, Care Home 01)
Residents across the care homes had little opportunity to acquire new possessions because there were infrequent visitors to support procurement. Staff typically focused on the occasional acquisition of practical items, such as underwear or toiletries. However, staff also stated that the minimal involvement of relatives made it difficult for them to learn about the preferences of residents with less communicative ability. There were anomalous instances where staff purchased meaningful items for residents, such as a stereo for a resident who loved music (Care Home 01), and jewelry in the color of a resident’s favorite football team (Care Home 02).
Residents and relatives often mentioned the importance of personal aesthetic. Residents admitted to the care home as an emergency had little input into which belongings they kept or relied on clothing borrowed from other residents or purchased by staff. Clothing was occasionally lost or mixed-up between residents, which upset residents and their relatives, who felt that an element of themselves had been stolen. This was particularly pertinent for relatives of residents with dementia, as they felt it highlighted their increased depersonalization and powerlessness:
It was like she was wearing part of me mum. (Amanda [relative], field notes, Care Home 02)
As care needs increased, staff in Care Homes 01 and 02 in particular tended to dress residents in looser-fitting, easy-to-change and easy-to-clean clothes, or “babywear” ( Twigg and Buse, 2013 : 330), regardless of the individual’s personal aesthetic. However, there were notable examples across each care home of staff making an effort to incorporate residents’ preferences in their daily care, typically in relation to colors, or whether someone was a “skirt person” or a “trouser person”:
. . . Joanna [staff], said that it’s ‘a bit of a faff’ getting them in and out of trousers, “but it’s what they prefer” . . . (Field notes, Care Home 03)
Residents derived a sense of self through their hobbies and activities. Staff in each care home initially claimed to incorporate residents’ preferences, but during observations, this rarely occurred. Staff felt constrained by understaffing and limited resources and unable to support residents’ identities and individuality. Consequently, there were few activities overall, and observed activities were based on generalizations to please the most people and did not account for nuanced preferences. These included a music-themed reminiscence group, tai chi (Care Home 01), bingo, and a “memory man” who discussed local history (Care Home 02):
. . . let’s say someone’s gay, and like to go to gay bars, and would like to meet gay people, erm, for example. Um, or let’s say someone’s Caribbean and they like to go to Caribbean clubs . . . I find they kind of take the headline title [of residents’ preferences] and that’s about it. (Adam [staff], interview, Care Home 01)
This approach did not satisfy most residents and relatives, who complained about a lack of stimulation and false promises of individualized activities.
I mean, Tracey [manager] said that they did lots of things in the afternoon, and I’ve never been convinced they’ve done as many as Tracey said they did. (Daniel [relative], interview, Care Home 01)
Residents and relatives acknowledged the financial constraints of many care homes, but felt more could be done to improve daily life. Staff also highlighted difficulties of organizing activities for residents with physical and cognitive impairments:
. . . It’s hard to think of where they can go really. You got to think about where they’re going to go to the toilet and everything—so there’s loads to think about before you even take them out. (Laura [staff], interview, Care Home 02)
Participants in Care Home 03 mentioned plans of a daytrip, but none occurred during the data collection period. However, in Care Home 03, some residents attended a weekly church fete unchaperoned; a luxury they valued. Across all three care homes, television was the most common activity observed. There were limited opportunities for residents to suggest ad hoc activities beyond the immediate resources of the care homes.
Independence and Autonomy
Residents and their relatives frequently emphasized the importance of independence as an element of residents’ identities throughout their life course, and evidenced this in a variety of ways. For instance, Carrie (Care Home 02) was an international fashion buyer; Mary (Care Home 02) attended football matches “with the boys,” which was considered unusual at the time; Richard (Care Home 03) was a freelance photographer.
Repeated reflections on their independence highlighted its absence in the care home. Residents missed the freedom to set their own agendas for the day. The care homes all adopted similar routines: set times for waking residents and putting them to bed, for food and drink, and any activities. Staff discouraged deviations from these routines as it jeopardized the smooth running of the care home. Residents felt that minor changes to routines were occasionally catered for, but at a compromise; Louis (resident, Care Home 03) had requested to sleep in one day, but was then allegedly denied his breakfast as the allotted breakfast time had passed and staff were busy elsewhere. Participants’ perceptions of how successful these allowances and compromises were in practice differed:
Well Ruth (resident) likes to get up really early—Ruth likes to get up at like quarter to seven. . . . So—like when they first come [to the care home], you ask them, like what they like to do . . . (Laura [staff], interview, Care Home 02) I like to get up early. But I have to wait for the nurse [to get me up]. (Ruth [resident], interview, Care Home 02)
Strict health and safety policies and organizational efficiency meant risk-averse staff tended to complete minor tasks themselves, such as making hot drinks, which undermined residents’ independence. The role of staff as carers seemed at odds with the expectation that they should also facilitate independence, particularly because of limited resources:
. . . It’s all well and good saying they want to remain independent, but if you can’t walk, you can’t walk . . . It is our job at the end of the day—to keep them well . . . (Edna [staff], field notes, Care Home 02)
To counter the negative perceptions of aging and increased dependency, many residents amended their definitions of independence and autonomy to emphasize minor daily tasks and accomplishments. Autonomy within the care home was limited to small day-to-day decisions, such as choosing a meal from the available selection, requesting an alternative meal where possible, or deciding when to go to bed if they were physically able to do so unaided. Physical independence to perform certain small tasks such as setting tables at mealtimes, usually authorized by staff, helped residents to feel as though they had retained an important element of their personal identities:
Catherine . . . helped to place the cutlery on the tables . . . and added “I know I’m not completely independent anymore. But it’s something” . . . (Catherine [resident], field notes, Care Home 01)
Each care home had members of staff who made a conscious effort to accommodate residents’ autonomous decision making and individual preferences. A notable example involved Edna’s (staff, Care Home 02) determination to allow a resident a “duvet day,” who uncharacteristically wanted to stay in bed. These infrequent instances encouraged residents to express their individuality, and made them feel more in control of their surroundings and their care. With residents’ new perceptions of independence and autonomy largely based on physical capabilities, this enabled them to use levels of cognition as a source of comparison against other residents who experienced dementia or mental health problems.
Social Comparison
Residents without dementia accepted that moving to a care home was necessary because of their care needs, but felt their positive sense of identity was jeopardized because of the association of care homes with severe cognitive and physical impairment. Residents with dementia represented these negative stereotypes, and symbolized the worst aspects of aging. Consequently, residents without dementia distanced themselves from residents with dementia by engaging in social comparison. They regularly pointed out those with dementia and emphasized their own perceived cognitive superiority, while also expressing sympathy and frustration over the often repetitive or disruptive behaviors associated with severe dementia. Such downward social comparisons serve to enhance self-image and in turn improve well-being ( Gibbons & Gerrard, 1991 ):
[Philippa] was looking at the row of residents sat asleep against the wall . . . “Most of these have lost their minds, you know . . . I can still think for myself. I haven’t gone yet” . . . (Philippa [resident], field notes, Care Home 02)
Residents without dementia typically vocalized their comparisons with members of staff, visitors, or the researcher; not with one another. Only two residents in Care Homes 01 and 03 indicated that they were friends and regularly conversed. Most residents suggested they were lonely, but did not converse with others beyond mealtimes. Although residents stated they were unable to hold meaningful social interactions with residents with dementia, it was difficult to determine why residents without dementia did not engage more with one another. Some participants, particularly staff, suggested residents may not wish to invest in making connections with others because they are acutely aware of their own mortality. When asked, residents said that they simply did not like the other residents, or that it was a lot of effort, especially if they were at risk of developing dementia.
I asked Elizabeth why she didn’t chat to Carrie more . . . after they seemed to have a nice time the other day . . . Elizabeth pulled a face and after a pause said “she’ll probably end up like the rest of ‘em in here . . .” (Field notes, Care Home 02)
The purpose of this study was to explore how life in a care home affects on the identities of care homes residents. The use of SIP offers a broad approach to identity that highlights the importance of context-bound social interactions for the development and maintenance of identity within the unique context of a care home. At the outset of the study, we proposed three theoretical propositions. In relation to these propositions, our findings reveal that (a) residents renegotiate their identities within the context of the care home, but use social interactions to facilitate social comparison with more impaired individuals, while largely failing to establish new relationships; (b) care homes have the potential to accommodate a multitude of identities by facilitating links with previous social networks or symbols that are necessary to maintain a sense of self, (c) but lack adequate support or appropriate resources to achieve this. We now discuss these findings in detail, followed by their implications.
Findings confirm the role of activities, possessions, and clothing, in symbolizing identities, particularly in light of personal and physical loss. Continued identification with such meaningful symbols help to bolster identity, even for individuals with limited expressive capacity, and can be maintained through adapted ways of living ( Black et al., 2018 ; Cohen-Mansfield, Marx, Thein, & Dakheel-Ali, 2010 ; Lloyd, Calnan, Cameron, Seymour, & Smith, 2014 ). But for participants in the present study, the care home environment undermined their abilities to adapt, disrupting connections to many important symbols, and resulting in a limited, bounded expression of residents’ identities.
Institutional restrictions, standardized routines, and strict risk management also threatened residents’ independence and autonomy, as perceived staff shortages and limited resources necessitated the precedence of organizational efficiency over individual needs. It has been established that a failure to satisfy needs for independence and autonomy is related to depressive symptoms and poor well-being and also hinders individuality and the expression of personalities ( Custers, Westerhof, Kuin, Gerritsen, & Riksen-Walraven, 2012 ; Goffman, 1961 ; A. Haslam et al., 2009 ; Knight et al., 2010 ; Wiersma & Dupuis, 2010 ; Kloos, Trompetter, Bohlmeijer, & Westerhof, 2018 ). Consistent with other studies ( Falk, Wijk, Persson, & Falk, 2013 ; Golander, 1995 ; Wiersma & Dupuis, 2010 ), participants in the present study reported an “emotional limbo” between the awareness of residents’ increased care needs and dependency on staff, and the importance of independence to residents’ identities. Our findings show that this motivates residents to emphasize their physical abilities to perform small tasks, to reconcile their established identities within a new, more constrained context.
Maintaining links with social networks or establishing new identity-relevant connections is also necessary to reinforce a sense of self and to buffer against a threatened identity or well-being ( Cohen-Mansfield, Golander, & Arnheim, 2000 ; A. Haslam et al., 2009 ; Surr, 2006 ). Relatives have the potential to support residents’ identity and improve resident outcomes by maintaining relationships with them and with staff ( Davies & Nolan, 2006 ; Roberts & Ishler, 2017 ), but most residents in the present study had little contact anyone outside of the care home and thus were unable to maintain identity-affirming connections. However, residents did not appear to value the opportunity to develop friendships with one another, as has been described elsewhere ( Surr, 2006 ; Tester et al., 2004 ). Rather, our findings resonate with those of Abbott and colleagues (2017) , where residents cited various barriers to social interactions with others, but participants in the present study focused on cognitive impairment as the fundamental obstacle. The fact that most older people residing in the care homes of the present study had a diagnosis of dementia reflects the national statistics of the United Kingdom on levels of impairment in care homes ( Alzheimer’s Society, 2014 ). But the belief among unimpaired residents that residents with dementia, particularly those who also had severe physical impairments, were not viable companions and should be avoided, reflects a more complex issue relating to threatened identities.
According to SIP, psychological strategies such as social competition, social creativity, and social mobility can be used to protect a threatened identity ( Reicher et al., 2010 ; Tajfel, 1981 ; Tajfel & Turner, 1979 ). The present study has shown that by highlighting the impairments of others and emphasizing their own abilities, residents without dementia used social creativity, specifically social comparison, as a means of cognitive adaptation. With little consistent opportunity to buffer identities through other means, social comparison and the motivation to distance oneself from impairment may have also served to alienate residents from one another who could have formed meaningful relationships, whether cognitively impaired or otherwise.
Implications
Although global policy states that care provision should enable self-expression and identity, the ability to make choices, and to maintain connections with social networks ( World Health Organisation, 2015 ), our findings suggest that such goals are difficult to achieve in the care home setting. Few visitors and opportunities to maintain connections outside of the care home place greater pressure on staff to perform identity work. To move forward, we need to understand how guidelines or training on identity is implemented in care homes and how this may be improved. In addition, further research on how residents can maintain connections outside of the care home is needed.
Staffing and resource constraints cannot be easily rectified, but care homes could facilitate residents’ needs within the allowances of their means. This study has demonstrated the value of seemingly minor, but meaningful, interactions between stakeholders, small changes to routines, and supported independence and autonomy. Evidence suggests that interventions to facilitate group-based decision making among care home residents regarding the refurbishment of communal areas created a shared identification, increased social engagement, and improved cognitive function and life satisfaction ( C. Haslam et al., 2014 ). Future interventions could support residents to make collective decisions in other, smaller areas of care home life, such as weekly activities or menu choices. This can promote positive social interaction among stakeholders and improve feelings of independence and autonomy, thereby minimizing the necessity for some residents to distance themselves from others. An assessment of such interventions versus standard practice, focusing on the cost implications and impact on staff workload, can help to determine their feasibility in under-resourced facilities.
Strengths and Limitations
This study is the only U.K.-based study to date that has used observational and interview methods across care homes with SIP. A key strength is the volume of data collected: Over 260 hr of observations across 1 year, combined with iterative interviews, facilitated in-depth exploration of context-bound data to understand the phenomenon of identity management over time. SIP has contributed to other social care areas, and its use in the care home setting helped to uncover and explore psychological strategies used by residents to cope and maintain a positive sense of self.
We only interviewed residents who had capacity to consent, which limits the generalizability of the findings. Future observational studies are needed that includes the perspectives of all care home residents. Furthermore, recruitment of care homes proved difficult. Managers were concerned with the potential distraction for staff or suggested the study had duplicitous aims in light of contemporaneous negative media representations of care homes. Although sampling was purposeful, no purpose-built care homes agreed to participate. There were also very few visitors across each care home, resulting in a small sample of relatives interviewed. Although this may limit generalizability, it is nonetheless an artifact of each case and serves to highlight the contemporaneous issues of maintaining relationships, and in turn identity, in care homes.
This study explored how life in a care home affects residents’ identities. The use of SIP within a multiple case study design, with interview and observational methods, is unique in care home research. Although moving to a care home initially emphasized age-related changes, institutional restrictions and limited social networks further undermined residents’ identities over time. The use of social comparison by residents without dementia served to buffer against daily threats to identity, in particular, the threat of being considered severely cognitively impaired and lacking independence. Resource constraints can make it difficult to adequately support diverse identities, yet even small changes to routines and daily care can help. Adequate resources and support within care homes can facilitate the expression of positive identities. This may reduce the need for staunch social comparison and create a more constructive environment for all residents, which may in turn improve well-being.
This study was funded by Medical Research Council doctoral studentship award for K. Paddock. Grant reference MR/J500410/1.
None reported.
Abbott , K. M. , Bangerter , L. R. , Humes , S. , Klumpp , R. , & Van Haitsma , K . ( 2017 ). “It’s important, but…”: Perceived barriers and situational dependencies to social contact preferences of nursing home residents . The Gerontologist , 00, 1–10. doi: 10.1093/geront/gnx109
Google Scholar
Almutairi , A. F. , Gardner , G. E. , & McCarthy , A . ( 2014 ). Practical guidance for the use of a pattern-matching technique in case-study research: A case presentation . Nursing & Health Sciences , 16 , 239 – 244 . doi: 10.1111/nhs.12096
Alzheimer’s Society . ( 2013 ). Low expectations: Attitudes on choice, care and community for people with dementia in care homes . London : Author .
Alzheimer’s Society . ( 2014 ). What is dementia? (Factsheet 400LP. The Information Standard). Retrieved from www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=106
Black , H. K. , Rubinstein , R. L. , Frankowski , A. C. , Hrybyk , G. , Nemec , M. , & Tucker , G. G . ( 2018 ). Identity, semiotics, and use of symbols in adult day services . The Gerontologist , 58, 730–738. doi: 10.1093/geront/gnx074
Care Quality Commission . ( 2016 ). The state of health care and adult social care in England 2015/16 . Retrieved from http://www.cqc.org.uk/content/state-of-care
Cleary , M. , Horsfall , J. , & Hayter , M . ( 2014 ). Data collection and sampling in qualitative research: Does size matter ? Journal of Advanced Nursing , 70 , 473 – 475 . doi: 10.1111/jan.12163
Cohen-Mansfield , J. , Golander , H. , & Arnheim , G . ( 2000 ). Self-identity in older persons suffering from dementia: Preliminary results . Social Science & Medicine , 51 , 381 – 394 . doi: 10.1016/S0277-9536(99)00471-2
Cohen-Mansfield , J. , Marx , M. S. , Thein , K. , & Dakheel-Ali , M . ( 2010 ). The impact of past and present preferences on stimulus engagement in nursing home residents with dementia . Aging & Mental Health , 14 , 67 – 73 . doi: 10.1080/13607860902845574
Conroy , T . ( 2017 ). A beginner’s guide to ethnographic observation in nursing research . Nurse Researcher , 24 , 10 – 14 . doi: 10.7748/nr.2017.e1472
Custers , A. F. , Westerhof , G. J. , Kuin , Y. , Gerritsen , D. L. , & Riksen-Walraven , J. M . ( 2012 ). Relatedness, autonomy, and competence in the caring relationship: The perspective of nursing home residents . Journal of Aging Studies , 26 , 319 – 326 . doi: 10.1016/j.jaging.2012.02.005
Davies , S. , & Nolan , M . ( 2006 ). ‘Making it better’: Self-perceived roles of family caregivers of older people living in care homes: A qualitative study . International Journal of Nursing Studies , 43 , 281 – 291 . doi: 10.1016/j.ijnurstu.2005.04.009
Falk , H. , Wijk , H. , Persson , L. O. , & Falk , K . ( 2013 ). A sense of home in residential care . Scandinavian Journal of Caring Sciences , 27 , 999 – 1009 . doi: 10.1111/scs.12011
Froggatt , K. , Davies , S. , & Meyer , J . ( 2009 ). Understanding care homes: A research and development perspective . Jessica Kingsley Publishers .
Gale , N. K. , Heath , G. , Cameron , E. , Rashid , S. , & Redwood , S . ( 2013 ). Using the framework method for the analysis of qualitative data in multi-disciplinary health research . BMC Medical Research Methodology , 13 , 117 . doi: 10.1186/1471-2288-13-117
Geertz , C . ( 1973 ). Thick description: Toward an interpretive theory of culture . In C. Geertz (Ed.), The interpretation of cultures: Selected essays (pp. 3 – 30 ). New York : Basic Books, Inc., Publishers .
Google Preview
Gibbons , F. X. , & Gerrard , M . ( 1991 ). Downward social comparison and coping with threat . In J. M. Suls & T. A. Wills (Eds.), Social comparison: Theory and research (pp. 317 – 345 ). Hillside, NJ : Lawrence Erlbaum .
Goffman , E . ( 1961 ). Asylums: Essays on the social situation of mental patients and other inmates . London : Penguin .
Golander , H . ( 1995 ). Chronically ill, old, and institutionalized: Being a nursing home resident . Family & Community Health , 17 , 63 – 79 . doi: 10.1097/00003727-199501000-00008
Haslam , C. , Alexander Haslam , S. , Knight , C. , Gleibs , I. , Ysseldyk , R. , & McCloskey , L. G . ( 2014 ). We can work it out: Group decision-making builds social identity and enhances the cognitive performance of care residents . British Journal of Psychology , 105 , 17 – 34 . doi: 10.1111/bjop.12012
Haslam , A. , Jetten , J. , Postmes , T. , & Haslam , C . ( 2009 ). Social identity, health, and well-being: An emerging agenda for applied psychology . Applied Psychology , 58 , 1 – 23 . doi: 10.1111/j.1464-0597.2008.00379.x
Hockey , J. , & James , A . ( 2003 ). Social identities across the life course . Basingstoke : Palgrave Macmillan .
Hogg , M. , & Abrams , D . ( 1988 ). Social identifications: A social psychology of intergroup relations and group processes . London : Routledge .
Hubbard , G. , Tester , S. , & Downs , M. G . ( 2003 ). Meaningful social interactions between older people in institutional care settings . Ageing and Society , 23 , 99 – 114 . doi: 10.1017/S0144686X02008991
Iyer , A. , Jetten , J. , Tsivrikos , D. , Postmes , T. , & Haslam , S. A . ( 2009 ). The more (and the more compatible) the merrier: Multiple group memberships and identity compatibility as predictors of adjustment after life transitions . The British Journal of Social Psychology , 48 ( Pt. 4 ), 707 – 733 . doi: 10.1348/014466608X397628
Jetten , J. , & Pachana , N. A . ( 2012 ). Not wanting to grow old: A social identity model of identity change (SIMIC) analysis of driving cessation among older adults . In J. Jetten , C. Haslam , & A. S. Haslam (Eds.), The social cure: Identity, health and well-being . East Sussex, UK : Psychology Press .
Kingston , A. , Wohland , P. , Wittenberg , R. , Robinson , L. , Brayne , C. , Matthews , F. E. , … Jagger , C .; Cognitive Function and Ageing Studies Collaboration . ( 2017 ). Is late-life dependency increasing or not? A comparison of the Cognitive Function and Ageing Studies (CFAS) . The Lancet , 390 , 1676 – 1684 . doi: 10.1016/S0140-6736(17)31575-1
Kloos , N. , Trompetter , H. R. , Bohlmeijer , E. T. , & Westerhof , G. J . ( 2018 ). Longitudinal associations of autonomy, relatedness, and competence with the well-being of nursing home residents . The Gerontologist , 00, 1–9. doi: 10.1093/geront/gny005
Knight , C. , Haslam , A. , & Haslam , C . ( 2010 ). In home or at home? How collective decision making in a new care facility enhances social interaction and wellbeing amongst older adults . Ageing & Society , 30 , 1393 – 1418 . doi: 10.1017/S0144686X10000656
Kroger , J. , Martinussen , M. , & Marcia , J. E . ( 2010 ). Identity status change during adolescence and young adulthood: A meta-analysis . Journal of Adolescence , 33 , 683 – 698 . doi: 10.1016/j.adolescence.2009.11.002
Lievesley , N. , Crosby , G. , Bowman , C. , & Midwinter , E . ( 2011 ). The changing role of care homes . BUPA and Centre for Policy on Ageing. Retrieved from http://www.cpa.org.uk/information/reviews/changingroleofcarehomes.pdf (accessed December 20, 2015).
Lincoln , Y. S. , & Guba , E. G . ( 1985 ). Naturalistic inquiry . Newbury Park, CA : Sage .
Lloyd , L. , Calnan , M. , Cameron , A. , Seymour , J. , & Smith , R . ( 2014 ). Identity in the fourth age: Perseverance, adaptation and maintaining dignity . Ageing & Society , 34 , 1 – 19 . doi: 10.1017/S0144686X12000761
Næss , A. , Fjær , E. G. , & Vabø , M . ( 2016 ). The assisted presentations of self in nursing home life . Social Science & Medicine , 150 ( Suppl. C ), 153 – 159 . doi: 10.1016/j.socscimed.2015.12.027
NCHR&D . ( 2006 ). My home life: Quality of life in care homes . Retrieved from http://myhomelife.org.uk/wp-content/uploads/ 2014/11/mhl_report.pdf
Newnham , E. C. , McKellar , L. V. , & Pincombe , J. I . ( 2017 ). Paradox of the institution: Findings from a hospital labour ward ethnography . BMC Pregnancy and Childbirth , 17 , 2 . doi: 10.1186/s12884-016-1193-4
Oakes , P. J. , Haslam , A. , & Turner , J. C . ( 1994 ). Stereotyping and social reality . Oxford, England : Blackwell .
O’Reilly , M. , & Parker , N . ( 2012 ). ‘Unsatisfactory Saturation’: A critical exploration of the notion of saturated sample sizes in qualitative research . Qualitative Research , 13 , 190 – 197 . doi: 10.1177/1468794112446106
Reicher , S. D. , Spears , R. , & Haslam , A . ( 2010 ). The social identity approach in social psychology . In M. Wetherell & C. T. Mohanty (Eds.), Sage identities handbook (pp. 45–62). London : Sage .
Ritchie , J. , & Spencer , L . ( 1994 ). Qualitative data analysis for applied policy research . In A. Bryman & R. G. Burgess (Eds.), Analyzing qualitative data (pp. 173 – 194 ). London : Routledge .
Roberts , A. R. , & Ishler , K. J . ( 2017 ). Family involvement in the nursing home and perceived resident quality of life . The Gerontologist , 00, 1–11. doi: 10.1093/geront/gnx108
Shenton , A . ( 2004 ). Strategies for ensuring trustworthiness in qualitative research projects . Education for Information , 22 , 63 – 75 . doi: 10.3233/EFI-2004-22201
Srivastava , P. , & Hopwood , N . ( 2009 ). A practical iterative framework for qualitative data analysis . International Journal of Qualitative Methods , 8 , 76 – 84 . doi: 10.1177/160940690900800107
Surr , C. A . ( 2006 ). Preservation of self in people with dementia living in residential care: A socio-biographical approach . Social Science & Medicine , 62 , 1720 – 1730 . doi: 10.1016/j.socscimed.2005.08.025
Tajfel , H . ( 1981 ). Human groups and social categories: Studies in social psychology . Cambridge : Cambridge University Press .
Tajfel , H. , & Turner , J . ( 1979 ). An integrative theory of intergroup conflict . In W. G. Austin & S. Worchel (Eds.), The social psychology of intergroup relations (pp. 33–37). Monterey, CA : Brooks-Cole .
Tester , S. , Hubbard , G. , Downs , M. , MacDonald , C. , & Murphy , J . ( 2004 ). What does quality of life mean for frail residents ? Nursing and Residential Care , 6 , 89 – 92 . doi: 10.12968/nrec.2004.6.2.12052
Turner , J. C . ( 1982 ). Towards a cognitive redefinition of the social group . In H. Tajfel (Ed.), Social identity and intergroup relations (Vol. 1 , pp. 15 – 40 ). Cambridge : Cambridge University Press .
Twigg , J. , & Buse , C. E . ( 2013 ). Dress, dementia and the embodiment of identity . Dementia , 12 , 326 – 336 . doi: 10.1177/1471301213476504
Walshe , C. E. , Caress , A. L. , Chew-Graham , C. , & Todd , C. J . ( 2004 ). Case studies: A research strategy appropriate for palliative care ? Palliative Medicine , 18 , 677 – 684 . doi: 10.1191/0269216304pm962ra
Ward , D. J. , Furber , C. , Tierney , S. , & Swallow , V . ( 2013 ). Using Framework Analysis in nursing research: A worked example . Journal of Advanced Nursing , 69 , 2423 – 2431 . doi: 10.1111/jan.12127
Wiersma , E. , & Dupuis , S. L . ( 2010 ). Becoming institutional bodies: Socialization into a long-term care home . Journal of Aging Studies , 24 , 278 – 291 . doi: 10.1016/j.jaging.2010.08.003
World Health Organisation . ( 2015 ). World report on ageing and health . Retrieved from http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1
Yin , R. K . ( 2009 ). Case study research: Design and methods (Vol. 5 ). London : Sage .
Yin , R. K . ( 2010 ). Qualitative research from start to finish . New York : Guilford Press .
- internship and residency
- personal satisfaction
- social identification
- medical residencies
Email alerts
Citing articles via, looking for your next opportunity.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1758-5341
- Copyright © 2024 The Gerontological Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Home care and technology: a case study
Affiliation.
- 1 University of Alberta, Edmonton, Canada. [email protected]
- PMID: 23138089
Health care aides (HCAs) are the backbone of the home care system and provide a range of services to people who, for various reasons related to chronic conditions and aging, are not able to take care of themselves independently. The demand for HCA services will increase and the current HCA supply will likely not keep up with this increasing demand without fundamental changes in the current environment. Information and communication technology (ICT) can address some of the workflow challenges HCAs face. In this project, we conducted an ethnographic study to document and analyse HCAs' workflows and team interactions. Based on our findings, we designed an ICT tool suite, integrating easily available existing and newly developed (by our team) technologies to address these issues. Finally, we simulated the deployment of our technologies, to assess the potential impact of these technological solutions on the workflow and productivity of HCAs, their healthcare teams and client care.
Publication types
- Research Support, Non-U.S. Gov't
- Appointments and Schedules
- Cell Phone*
- Continuity of Patient Care / organization & administration
- Electronic Health Records / instrumentation
- Electronic Health Records / organization & administration*
- Home Health Aides / organization & administration*
- Information Systems / instrumentation
- Information Systems / organization & administration
- Monitoring, Ambulatory / instrumentation
- Monitoring, Ambulatory / methods*
- Organizational Case Studies
- Patient Care Team / organization & administration
- Telecommunications / instrumentation
- Telecommunications / organization & administration
- Telemedicine / instrumentation
- Telemedicine / organization & administration*

We help keep seniors safe at home

208.892.4584 [email protected]

Our Facebook Page
In Home Dementia/Alzheimer’s Care: Living with dementia, happily
We provide in home care for seniors with dementia/Alzheimer’s in the Moscow, Idaho area , using person-centered care and strength-based dementia techniques (see the DAWN Method® of dementia care ). We can help you keep your loved one at home longer, lowering costs and greatly improving their quality of life. Our case manager and dementia care specialists work with you to design supportive and safe care at home—giving you an alternative to assisted living and Alzheimer’s care in care facilities. For more about the value of strength-based dementia care, see Judy Cornish’s TEDx Talk, “The Dawn of Dementia Care.”
Reviews from Palouse Dementia Care clients

PDC Family Portal
Palouse Dementia Care, LLC

Home hospital care brings ‘phenomenal’ benefits to patients and providers, study finds
A growing number of patients and providers are heralding the benefits of bringing hospital care into private homes — but a lack of permanent federal funding could put such programs at risk.
The shift to in-home care began with the onset of COVID in March 2020, when the Centers for Medicare and Medicaid Services (CMS) launched its Acute Hospital Care at Home waiver program in response to a shortage of beds.
The program enables hospitals to receive the same reimbursement for home care as they would for patients who are treated in actual facilities.
SOME NURSES EXPERIENCE VIOLENT ATTACKS AT SEATTLE CHILDREN’S HOSPITAL, SAY THEY WANT PROTECTION, SUPPORT
Since the program’s launch, hundreds of hospitals in 37 states have implemented home care for thousands of patients.
One of those is the Mass General Brigham (MGB) network in downtown Boston, which launched its Healthcare at Home program in 2016.
READ ON THE FOX NEWS APP
MGB’s Home Hospital is one of the largest in the country, serving 66 neighborhoods from five of its facilities.
Since its launch, the program has had over 2,400 home hospital admissions, translating to more than 12,700 acute care bed days saved, according to a press release from the hospital.
Dr. Stephen Dorner, chief clinical and innovation officer at MGB Healthcare at Home, talked to Fox News Digital about the program’s growth and goals, as well as the benefits for patients and providers.
TEXAS DOCTOR GOES VIRAL ON TIKTOK FOR SKATING THROUGH THE HOSPITAL HALLS TO CELEBRATE HIS RETIREMENT
"In January 2022, we had an average census of nine patients — today, we have an average census of 36 patients with an overall capacity for 40," he said in a Zoom interview.
"We will continue to grow that in the months and years ahead until we ultimately shift at least 10% of current inpatient volume out of hospitals and into patients' homes."
Dorner sees home-based care as a viable solution for the "massive capacity crisis" facing the nation’s hospitals.
"Health care just costs too much money," he said. "And especially as we look at the aging baby boomer generation and the amount of care they're going to need — particularly as longevity increases — we have to find new, lower-cost ways to do things."
The ability to deliver acute inpatient care in people’s homes is a "phenomenal" way to improve overall access to care and reduce medical costs, Dorner noted.
While home hospital care isn’t for everyone, many patients are more than willing to receive it.
"The patients who are most willing to accept home hospital care are those who are most in tune and aware of what their medical needs are," Dorner told Fox News Digital.
That typically includes patients with chronic conditions that may lead to frequent hospitalizations, such as heart failure or chronic obstructive pulmonary disease, he noted.
"They're more willing to accept home hospital care because they spend so much time dealing with their chronic illness and they'd like to be able to spend more time at home," the doctor said.
MGB has also had "great success" in admitting patients with new, acute issues that they've never dealt with before, such as cellulitis, kidney infection or pneumonia, Dorner added.
"Folks want to have the creature comforts of being in their own bed, eating their own food, petting their dog as they're recovering, being able to have loved ones come and visit, and not having to trek into the city and pay for parking and all of those things," he said.
Patients enjoy the personalized nature of in-home care, Dorner also said.
GOOGLE REVEALS THE TOP 10 HEALTH SEARCHES OF 2023 — AND EXPERTS ANSWER THEM
"About 60% to 70% of our visits are actually conducted in the home, not virtually," he said. "So we’re sending physicians, nurse practitioners and physician assistants into the homes of our patients to be able to see them firsthand, which gives them a unique vantage point of understanding the patients’ home environment."
He added, "Many of the patients tell us they never want to receive hospital-based care again. They want to know how they can get all of their care from the comfort of their own home."
The program also has the potential to alleviate provider burnout.
"We've heard from our clinicians that the time they spend in home hospital care delivery is among the most meaningful encounters they've had in their entire careers," Dorner said.
That doesn’t mean that all care can be brought into the home, however.
"We’re not building ICUs in the home, and we're not looking to conduct surgeries in anybody's living room," Dorner said.
"But in the right conditions, we'd like to be able to build a complement in the home-based environment."
Dr. Shana Johnson, a physical medicine and rehabilitation physician in Scottsdale, Arizona , also voiced her support of the home hospital model.
"With appropriate patient selection, acute hospital care at home is an important care model to continue," said Johnson, who is not involved with MGB’s program or research.
"For certain medical conditions, the quality of care and outcomes appear equal to or better than in-hospital care," she added.
"In particular, some studies have found fewer complications from inactivity, such as pressure sores, reduced need for skilled nursing facilities, and lower hospital readmission rates."
To measure the outcomes of its Home Hospital program, MGB researchers recently conducted a study that was published in Annals of Internal Medicine.
The team analyzed the outcomes of 5,858 U.S. patients who received home hospital care between July 1, 2022, and June 30, 2023.
MOST SENIORS IN AMERICA CAN’T AFFORD NURSING HOMES OR ASSISTED LIVING, STUDY FINDS
The patients in the study had "medically complex conditions," including 42.5% with heart failure, 43.3% with chronic obstructive pulmonary disease, 22.1% with cancer and 16.1% with dementia, the researchers noted.
The five most common discharge diagnoses were heart failure, respiratory infection (including COVID), sepsis, kidney/urinary tract infections and cellulitis.
The researchers found that the patients who received home care had low rates of mortality (0.5% during hospitalization and 3.2% at 30 days). Only 62.2% of them were "escalated" to the hospital.
Within 30 days of discharge, 2.6% used a skilled nursing facility and 15.6% were readmitted, numbers the researchers described as lower than expected.
"Home Hospital is serving very complex and acutely ill patients — these are not ‘cherry-picked’ patients," study co-author David Michael Levine, M.D., clinical director for research and development for MGB’s Healthcare at Home, told Fox News Digital.
"This is the first time we’ve been able to show the true complexity and acuity of patients cared for in this model on a national basis."
The researchers also concluded that Home Hospital delivers "equitable care across traditionally underserved populations," Levine said.
AS PHYSICAL THERAPIST PRACTICES IN AMERICA FACE STAFFING SHORTAGES, KIDS ARE 'SUFFERING,' SAY EXPERTS
"We know that traditional hospital care has large disparities in outcomes across underserved groups, and we don't see that with Home Hospital."
Johnson, who reviewed the findings of MGB’s study, said she found them to be consistent with previous research .
"This study of acute hospital care at home showed low rates of mortality, hospital escalation and skilled nursing facility use," she told Fox News Digital. "These positive outcomes were seen for socially vulnerable patients as well."
The study was limited, however, as it was based on observational data and did not have the capability to compare the numbers to in-hospital patients.
"Comparing home hospital patients to traditional hospital patients takes a lot of additional research," said Levine. "We wouldn’t want to compare home hospital patients to, say, surgical patients or labor and delivery patients."
He added, "If you simply look at all hospitalizations, yes, these numbers are better — but that is not a worthwhile comparison. We are currently undertaking this more advanced analysis."
Providers are concerned that the Acute Hospital Care at Home program is still a temporary payment mechanism.
The waiver is set to expire in Dec. 2024 unless Congress takes action to extend it or make it permanent.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"A permanent payment mechanism is critical in order for more people to have access to Home Hospital care," Levine told Fox News Digital.
"We wanted to conduct this national analysis so there would be more data for policymakers and clinicians to make an informed decision about extending or even permanently approving the waiver to extend opportunities for patients to receive care in the comfort of home."
When contacted for comment, the American Hospital Association (AHA) provided a statement.
"Emerging evidence suggests hospital care at home is safe, effective and useful to many patients. The AHA supported last year’s congressional extension of the regulatory flexibilities that have enabled hospitals to continue their hospital at home programs, and is working to ensure this innovative model of care remains available to patients and communities."
Fox News Digital reached out to the Centers for Medicare and Medicaid Services (CMS) requesting comment on the potential extension of the Acute Hospital Care at Home waiver program.
For more Health articles, visit www.foxnews.com/health .
Original article source: Home hospital care brings ‘phenomenal’ benefits to patients and providers, study finds

Strategies for Building a Sustainable Nursing Workforce

Nursing and staffing shortages continue to be a pain point for leaders facing the increasing demand for care at home. While there is no one-size-fits-all solution to address these challenges, a panel of industry leaders shared pathways to sustain the nursing workforce at the 2024 Axxess, Growth, Innovation and Leadership Experience (AGILE) .
Marcylle Combs, President and Owner of MAC Legacy, moderated the session with panelists Marcia B. Proto, Executive Director of The Connecticut Center for Nursing Workforce, Inc; Kayla Davis, Research Specialist for Texas Center of Nursing Workforce Studies; Clark Ruttinger, Director of Health Workforce Consulting and Life Sciences Consulting at Global Data; and Kathy Driscoll, Chief Nursing Officer at Humana.
The panel discussed the growth surrounding the care at home industry and strategies leaders should focus on to attract and retain nurses to meet the increased demand.
Spotlight on Data
The panelists highlighted the importance of understanding data when discussing staffing challenges and ways to accommodate the growing care at home market.
“Looking at nurses in home health, they’re almost two times, 1.8 times, more likely to leave employment in home health than in hospitals,” Ruttinger said. “They’re also 2.1 times more likely to leave the workforce altogether than a hospital nurse.”
Leaders are also encouraged to analyze the data to better understand movement trends among nurses seeking new opportunities.
“When you’re looking to get nurses into home health, you’re four times more likely to have a nurse come from residential care than a hospital,” Ruttinger said. “We have to consider, you know, increase in demand because of elderly populations, but also competition between not just industries, but also settings within the healthcare industry itself as we look at what’s going on into the future.”
Davis drew attention to the data on the length of time it is taking organizations to fill nursing positions.
“91-plus days, that’s how long it was taking to fill positions by nurse type,” Davis said.
Proto emphasized that organizations need to collaborate with state entities to identify and accurately report the challenges nurses are facing, some of which hinder them from entering or staying in the care at home industry.
“We learned more information about [the reasoning], everything from not on a bus route, as well as the hours of work, as well as how do I get to the different home locations if I don’t have transportation,” Proto said. “So, we were really excluding a lot of very good people from the world of home care.”
Sustaining Your Workforce
The panelists encouraged leaders to first focus on listening to the needs of nurses to support their well-being and ultimately retain them and meet the growing home care demand.
“For our organization, the first thing that we really needed to do was make sure we are listening to our nurses,” Driscoll said. “We can all think we know what nurses are feeling, what they value.”
Organizations should also take a strong look at the career and professional development programs offered and tailor them to meet evolving needs of their workforce.
“We relooked at our educational benefit; we had a very traditional tuition reimbursement benefit,” Driscoll said. “We found that people weren’t going for the degree they wanted because they couldn’t afford to put the money out to get reimbursed, or it just was too much toll on their family situation or their life situation at the moment. So, people wanted to be reimbursed for certifications. They wanted opportunities for microlearning.”
The panelists discussed building partnerships, encouraging leaders to focus on partnering with more than just nursing schools. Leaders need to emphasize that nurses are needed in more than just hospitals.
“We really focused on partnering with schools and thinking [about] what those schools needed, just to expose student nurses, our future nurses, to home health and to the community as a setting that they could really enjoy, thrive in, make a difference,” Driscoll said. “We made an investment, with Emory University, in building a simulation lab that was a home. It’s an apartment. What we found was that they really didn’t have the curricula that reflected what home health is like, what care in the home really is like.”
The panelists concluded the session by encouraging organizations to look at the leadership structure of the business, making sure that the right clinicians are being put into leadership positions and building policy around those needs.
“There’s an assumption that because you’re a good clinician, you’re going to be a good leader,” Driscoll said. “Well, that’s kind of rolling the dice there.”
Davis added, “We want good leadership. People stay for leadership.”
With more than 350 attendees, more than 50 sponsors and countless connections made, AGILE 2024 was a massive success for everyone. Check out this recap video .

- Axxess (133)
- Clinical (142)
- Financial (71)
- Home Care (351)
- Home Health (341)
- Hospice (378)
- Operational (220)
- Palliative Care (130)
- Patient Engagement (68)
- Regulatory (191)
- Revenue Cycle Management (41)
- Staffing (46)
You're in Good Company
See why 9,000+ organizations trust Axxess.

Industry Insights
For healthcare at home.
Get the latest news and business insights affecting home health, hospice and home care providers.
Be the First to Know
Tell us which insights you want to help grow your business and make lives better.
By clicking the button above, you are agreeing to our Privacy Policy.
Thank You For Subscribing To Our Email List
- Hispanoamérica
- Work at ArchDaily
- Terms of Use
- Privacy Policy
- Cookie Policy
Dogchitecture: WE Architecture Designs a Center That Challenges Traditional Animal Shelters

- Written by Ella Comberg
Copenhagen firm WE Architecture has completed a proposal for a “Dog Center” in Moscow that challenges traditional notions of animal shelters. Nestled in the countryside, the one-story pavilion will rely on a series of courtyards divided by pergolas that disappear into the landscape. The firm notes that the courtyards, which provide enclosed outdoor space for the dogs , allow the center “to avoid the 'jail-like' fencing which is often associated with dog shelters."

WE, in collaboration with MASU Planning , hopes to create a “healthy and inspiring environment for sheltered dogs and for the different people who will visit and work at the Center.” The project accomplishes its atmospheric goals by complimenting steel pillars with wooden rafters. The rafters extend to create an exterior overhang which functions as “a sun screen in summer time and as an exterior cover/hallway on rainy days.” As visitors approach the building, the green roof , which sits atop the wooden rafters, is meant to serve as a “fifth facade” that can blend in easily with its wooded surroundings. Extensive outdoor seating space bleeds into greenery, inviting both human and animal recreation.

Design Team
Project year, photographs.
News via: WE Architecture
Project gallery

Materials and Tags
- Sustainability
世界上最受欢迎的建筑网站现已推出你的母语版本!
想浏览archdaily中国吗, you've started following your first account, did you know.
You'll now receive updates based on what you follow! Personalize your stream and start following your favorite authors, offices and users.
I cared for my dad under ‘hospital at home’ in his final weeks. The program is missing one big piece

I cared for my father 24/7 in the last years of his life. A lot of that care happened through the hospital-at-home program. While he received high-quality care, the support provided to his primary caregiver, me, fell short.
Innovation in health care delivery increasingly keeps patients out of the hospital by providing medical care in the home. As a result, care is being pushed into the home much earlier in the patient journey than ever before. One major evolution—starting in the last decade but gaining momentum since COVID—has been the popular hospital-at-home program. It’s widely supported across the nation, with support from the Centers for Medicare and Medicaid Services through the “ Acute Hospital Care at Home ” waiver. The program ends later this year, and it’s up for debate how the federal agency should make such models permanent moving forward. A bill now being considered by Congress would extend the program.
Health care at home
Either way, the trend is clear: Health care providers have made the growth of the hospital-at-home program a major priority for the coming year. Mass General Brigham , for example—one of the largest health care systems in the U.S.—has indicated it would like to move 10% of its medical patients to home care. A McKinsey & Company study predicts that health care will continue to be delivered at home, to the tune of $265 billion by 2025 . But while it’s embraced by both health care systems and patients, the hospital-at-home program overlooks a key piece of the puzzle: the family caregivers who do so much of the work, often with little warning and no training.
Family caregivers have long been a part of the care ecosystem. They cover over $470 billion worth of unpaid care every year, and our health care system is reliant on family caregivers to provide over 80% of community-based long-term care. According to the National Alliance for Caregiving, over 65 million Americans serve as family caregivers for a disabled or ill relative. On average, caregivers shoulder 37.4 hours of care per week , a trend that will only intensify with the momentum of aging-in-place and hospital-at-home models. Despite the growing reliance on them, family caregivers have been left out of the equation. But as hospital-at-home and its ilk gain popularity, the care taking place at home is becoming more acute and complex.
As the primary family caregiver to both of my parents for eight years, I intimately understand the emotional and logistical toll caregiving can take, both in clinical settings and in the home. My mom had pancreatic cancer for seven years and moved in with my family. I cared for her until she passed away in my home six years ago. My dad had been living with us since then and experienced a major health decline from congestive heart failure. Last year, we became participants in a hospital-at-home program upon his discharge after a hospital stay to treat complications from congestive heart failure.
At that time, I didn’t know what the program was until I found myself sitting in my living room with my recently discharged dad, a doctor, and a nurse. They brought the monitoring equipment and took his vitals. The whole time they were talking to him as the patient—and didn’t ask me any questions about the living situation, care coverage, or daily care needs. Once their 20-minute visit ended, I was left to figure out all the extra care he needed after a six-day hospital stay. I had to cancel a work trip that week because my dad needed extra assistance for his daily care. The monitoring equipment was impressive, but the many moments he walked a few inches beyond the 13-foot coverage, I was being called by their 24/7 monitoring line asking to check on him.
Having experienced this program firsthand while also being a health-tech leader in the industry, I want to emphasize that the positives abound for health care systems, which can discharge patients from an acute care setting, and for patients, most of whom prefer to be cared for in their homes. However, hospital-at-home will not reach its full potential until the family caregivers are integrated into the process with the appropriate onboarding and support.

Supporting family caregivers
A few key steps should be taken. First, be intentional with the onboarding process and education provided to family caregivers. Clearly explain the program in a way that sets the caregiver’s role and expectations. Lay out how long it’s intended to last, ask the caregiver about the home care environment, and assess where needs may arise. Provide a thorough overview of any resources and support that are available, and incorporate the family caregiver as part of the care team. Caregivers in this situation are not just players sitting by the bedside, as in a hospital setting. They are playing the roles of health aides, social workers, food service, and 24/7 monitoring beyond key vitals. Consider the care in the home environment, where daily life distractions and obligations occur.
In my case, caring for my father at home coincided with my work at ianacare, a caregiving tech company that I cofounded to help bridge the gaps in home-based care. I have learned that the important thing, as we make this critical shift of transitioning care into the home, is to start by acknowledging the importance of family caregivers. The hardest part, after all, falls to them.
Clinical evidence demonstrates the key role they play. The goals of the provider align with the outcome of well-supported caregivers, with a 25% reduction in hospital readmission when a family caregiver is involved. Meanwhile, patients whose caregivers are burned out, stressed, or fatigued experience a 73% increase in emergency department utilization .
I recently spoke with a health care system as they began the process of implementing hospital-at-home, and they mentioned that caregiver support was important to them—but that they were more concerned about getting the program up and running for the patients first. Unfortunately, this is the prevalent mindset within health care systems, and the unintended consequence is the large amount of stress and pressure placed on family caregivers.
While hospital-at-home is designed to deliver clinical support and professional care, the reality is that informal unpaid caregivers do much of the work in the home. We’re caring for our loved ones and ensuring that they get the best standard of care in the process. The moments between in-home and virtual visits quickly become critical—and that is where family caregivers, who are often thrust into that role with little warning and no training, come in. It’s the last mile of the patient’s care.
These caregivers need far more attention. Proper training and support for them will not only reduce burnout, but ultimately lead to better patient outcomes and lowered costs. Hospital-at-home is the start of other initiatives pushing care in the home, so we need to get this right—starting now.
Jessica Kim is cofounder and executive chairman of ianacare . She is a graduate of Brown University and holds an MBA from Northwestern University’s Kellogg School of Management.
The opinions expressed in Fortune.com commentary pieces are solely the views of their authors and do not necessarily reflect the opinions and beliefs of Fortune .
Latest in Commentary

Biden’s tariffs on Chinese EVs make sense—but only for a while

Ask Andy: How do I choose the right cofounder for my startup?

Big Tech employees missed out on $5.1 billion in 401(k) gains over the last decade because of fossil fuels, new research finds

Bipartisan support of cryptocurrency is resurging in Congress. Here’s why

America’s productivity growth is recovering to pre-Great Financial Crisis rates. Europe has more work to do

Most Popular

Jerome Powell’s Fed is beginning to think its interest rate hikes ‘may be having smaller effects than in the past’

The CEO of Crunch Fitness doesn’t think there’s such a thing as work-life balance: ‘That’s for somebody who’s not fully committed’

The starting salary for a new American Airlines flight attendant is low enough to qualify for food stamps in some states

The new quiet luxury is burgers and fries: Over 60% of Americans are buying less fast food because it’s just too expensive, survey finds

Chinese, Iranian, and Russian gangs are attacking U.S. drinking water and officials are alarmed

Amazon CEO Andy Jassy: An ‘embarrassing’ amount of your success in your 20s depends on your attitude
- Open access
- Published: 14 May 2024
Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study
- Jocelyn Schroeder 1 ,
- Barbara Pesut 1 , 2 ,
- Lise Olsen 2 ,
- Nelly D. Oelke 2 &
- Helen Sharp 2
BMC Nursing volume 23 , Article number: 326 ( 2024 ) Cite this article
204 Accesses
Metrics details
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada’s legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses’ (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education; and bereavement care for family. Nurses have a right under the law to conscientious objection to participating in MAiD. Therefore, it is essential to prepare nurses in their entry-level education for the practice implications and moral complexities inherent in this practice. Knowing what nursing students think about MAiD is a critical first step. Therefore, the purpose of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context.
The design was a mixed-method, modified e-Delphi method that entailed item generation from the literature, item refinement through a 2 round survey of an expert faculty panel, and item validation through a cognitive focus group interview with nursing students. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
During phase 1, a 56-item survey was developed from existing literature that included demographic items and items designed to measure experience with death and dying (including MAiD), education and preparation, attitudes and beliefs, influences on those beliefs, and anticipated future involvement. During phase 2, an expert faculty panel reviewed, modified, and prioritized the items yielding 51 items. During phase 3, a sample of nursing students further evaluated and modified the language in the survey to aid readability and comprehension. The final survey consists of 45 items including 4 case studies.
Systematic evaluation of knowledge-to-date coupled with stakeholder perspectives supports robust survey design. This study yielded a survey to assess nursing students’ attitudes toward MAiD in a Canadian context.
The survey is appropriate for use in education and research to measure knowledge and attitudes about MAiD among nurse trainees and can be a helpful step in preparing nursing students for entry-level practice.
Peer Review reports
Medical Assistance in Dying (MAiD) is permitted under an amendment to Canada’s Criminal Code which was passed in 2016 [ 1 ]. MAiD is defined in the legislation as both self-administered and clinician-administered medication for the purpose of causing death. In the 2016 Bill C-14 legislation one of the eligibility criteria was that an applicant for MAiD must have a reasonably foreseeable natural death although this term was not defined. It was left to the clinical judgement of MAiD assessors and providers to determine the time frame that constitutes reasonably foreseeable [ 2 ]. However, in 2021 under Bill C-7, the eligibility criteria for MAiD were changed to allow individuals with irreversible medical conditions, declining health, and suffering, but whose natural death was not reasonably foreseeable, to receive MAiD [ 3 ]. This population of MAiD applicants are referred to as Track 2 MAiD (those whose natural death is foreseeable are referred to as Track 1). Track 2 applicants are subject to additional safeguards under the 2021 C-7 legislation.
Three additional proposed changes to the legislation have been extensively studied by Canadian Expert Panels (Council of Canadian Academics [CCA]) [ 4 , 5 , 6 ] First, under the legislation that defines Track 2, individuals with mental disease as their sole underlying medical condition may apply for MAiD, but implementation of this practice is embargoed until March 2027 [ 4 ]. Second, there is consideration of allowing MAiD to be implemented through advanced consent. This would make it possible for persons living with dementia to receive MAID after they have lost the capacity to consent to the procedure [ 5 ]. Third, there is consideration of extending MAiD to mature minors. A mature minor is defined as “a person under the age of majority…and who has the capacity to understand and appreciate the nature and consequences of a decision” ([ 6 ] p. 5). In summary, since the legalization of MAiD in 2016 the eligibility criteria and safeguards have evolved significantly with consequent implications for nurses and nursing care. Further, the number of Canadians who access MAiD shows steady increases since 2016 [ 7 ] and it is expected that these increases will continue in the foreseeable future.
Nurses have been integral to MAiD care in the Canadian context. While other countries such as Belgium and the Netherlands also permit euthanasia, Canada is the first country to allow Nurse Practitioners (Registered Nurses with additional preparation typically achieved at the graduate level) to act independently as assessors and providers of MAiD [ 1 ]. Although the role of Registered Nurses (RNs) in MAiD is not defined in federal legislation, it has been addressed at the provincial/territorial-level with variability in scope of practice by region [ 8 , 9 ]. For example, there are differences with respect to the obligation of the nurse to provide information to patients about MAiD, and to the degree that nurses are expected to ensure that patient eligibility criteria and safeguards are met prior to their participation [ 10 ]. Studies conducted in the Canadian context indicate that RNs perform essential roles in MAiD care coordination; client and family teaching and support; MAiD procedural quality; healthcare provider and public education; and bereavement care for family [ 9 , 11 ]. Nurse practitioners and RNs are integral to a robust MAiD care system in Canada and hence need to be well-prepared for their role [ 12 ].
Previous studies have found that end of life care, and MAiD specifically, raise complex moral and ethical issues for nurses [ 13 , 14 , 15 , 16 ]. The knowledge, attitudes, and beliefs of nurses are important across practice settings because nurses have consistent, ongoing, and direct contact with patients who experience chronic or life-limiting health conditions. Canadian studies exploring nurses’ moral and ethical decision-making in relation to MAiD reveal that although some nurses are clear in their support for, or opposition to, MAiD, others are unclear on what they believe to be good and right [ 14 ]. Empirical findings suggest that nurses go through a period of moral sense-making that is often informed by their family, peers, and initial experiences with MAID [ 17 , 18 ]. Canadian legislation and policy specifies that nurses are not required to participate in MAiD and may recuse themselves as conscientious objectors with appropriate steps to ensure ongoing and safe care of patients [ 1 , 19 ]. However, with so many nurses having to reflect on and make sense of their moral position, it is essential that they are given adequate time and preparation to make an informed and thoughtful decision before they participate in a MAID death [ 20 , 21 ].
It is well established that nursing students receive inconsistent exposure to end of life care issues [ 22 ] and little or no training related to MAiD [ 23 ]. Without such education and reflection time in pre-entry nursing preparation, nurses are at significant risk for moral harm. An important first step in providing this preparation is to be able to assess the knowledge, values, and beliefs of nursing students regarding MAID and end of life care. As demand for MAiD increases along with the complexities of MAiD, it is critical to understand the knowledge, attitudes, and likelihood of engagement with MAiD among nursing students as a baseline upon which to build curriculum and as a means to track these variables over time.
Aim, design, and setting
The aim of this study was to develop a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in MAiD in the Canadian context. We sought to explore both their willingness to be involved in the registered nursing role and in the nurse practitioner role should they chose to prepare themselves to that level of education. The design was a mixed-method, modified e-Delphi method that entailed item generation, item refinement through an expert faculty panel [ 24 , 25 , 26 ], and initial item validation through a cognitive focus group interview with nursing students [ 27 ]. The settings were a University located in an urban area and a College located in a rural area in Western Canada.
Participants
A panel of 10 faculty from the two nursing education programs were recruited for Phase 2 of the e-Delphi. To be included, faculty were required to have a minimum of three years of experience in nurse education, be employed as nursing faculty, and self-identify as having experience with MAiD. A convenience sample of 5 fourth-year nursing students were recruited to participate in Phase 3. Students had to be in good standing in the nursing program and be willing to share their experiences of the survey in an online group interview format.
The modified e-Delphi was conducted in 3 phases: Phase 1 entailed item generation through literature and existing survey review. Phase 2 entailed item refinement through a faculty expert panel review with focus on content validity, prioritization, and revision of item wording [ 25 ]. Phase 3 entailed an assessment of face validity through focus group-based cognitive interview with nursing students.
Phase I. Item generation through literature review
The goal of phase 1 was to develop a bank of survey items that would represent the variables of interest and which could be provided to expert faculty in Phase 2. Initial survey items were generated through a literature review of similar surveys designed to assess knowledge and attitudes toward MAiD/euthanasia in healthcare providers; Canadian empirical studies on nurses’ roles and/or experiences with MAiD; and legislative and expert panel documents that outlined proposed changes to the legislative eligibility criteria and safeguards. The literature review was conducted in three online databases: CINAHL, PsycINFO, and Medline. Key words for the search included nurses , nursing students , medical students , NPs, MAiD , euthanasia , assisted death , and end-of-life care . Only articles written in English were reviewed. The legalization and legislation of MAiD is new in many countries; therefore, studies that were greater than twenty years old were excluded, no further exclusion criteria set for country.
Items from surveys designed to measure similar variables in other health care providers and geographic contexts were placed in a table and similar items were collated and revised into a single item. Then key variables were identified from the empirical literature on nurses and MAiD in Canada and checked against the items derived from the surveys to ensure that each of the key variables were represented. For example, conscientious objection has figured prominently in the Canadian literature, but there were few items that assessed knowledge of conscientious objection in other surveys and so items were added [ 15 , 21 , 28 , 29 ]. Finally, four case studies were added to the survey to address the anticipated changes to the Canadian legislation. The case studies were based upon the inclusion of mature minors, advanced consent, and mental disorder as the sole underlying medical condition. The intention was to assess nurses’ beliefs and comfort with these potential legislative changes.
Phase 2. Item refinement through expert panel review
The goal of phase 2 was to refine and prioritize the proposed survey items identified in phase 1 using a modified e-Delphi approach to achieve consensus among an expert panel [ 26 ]. Items from phase 1 were presented to an expert faculty panel using a Qualtrics (Provo, UT) online survey. Panel members were asked to review each item to determine if it should be: included, excluded or adapted for the survey. When adapted was selected faculty experts were asked to provide rationale and suggestions for adaptation through the use of an open text box. Items that reached a level of 75% consensus for either inclusion or adaptation were retained [ 25 , 26 ]. New items were categorized and added, and a revised survey was presented to the panel of experts in round 2. Panel members were again asked to review items, including new items, to determine if it should be: included, excluded, or adapted for the survey. Round 2 of the modified e-Delphi approach also included an item prioritization activity, where participants were then asked to rate the importance of each item, based on a 5-point Likert scale (low to high importance), which De Vaus [ 30 ] states is helpful for increasing the reliability of responses. Items that reached a 75% consensus on inclusion were then considered in relation to the importance it was given by the expert panel. Quantitative data were managed using SPSS (IBM Corp).
Phase 3. Face validity through cognitive interviews with nursing students
The goal of phase 3 was to obtain initial face validity of the proposed survey using a sample of nursing student informants. More specifically, student participants were asked to discuss how items were interpreted, to identify confusing wording or other problematic construction of items, and to provide feedback about the survey as a whole including readability and organization [ 31 , 32 , 33 ]. The focus group was held online and audio recorded. A semi-structured interview guide was developed for this study that focused on clarity, meaning, order and wording of questions; emotions evoked by the questions; and overall survey cohesion and length was used to obtain data (see Supplementary Material 2 for the interview guide). A prompt to “think aloud” was used to limit interviewer-imposed bias and encourage participants to describe their thoughts and response to a given item as they reviewed survey items [ 27 ]. Where needed, verbal probes such as “could you expand on that” were used to encourage participants to expand on their responses [ 27 ]. Student participants’ feedback was collated verbatim and presented to the research team where potential survey modifications were negotiated and finalized among team members. Conventional content analysis [ 34 ] of focus group data was conducted to identify key themes that emerged through discussion with students. Themes were derived from the data by grouping common responses and then using those common responses to modify survey items.
Ten nursing faculty participated in the expert panel. Eight of the 10 faculty self-identified as female. No faculty panel members reported conscientious objector status and ninety percent reported general agreement with MAiD with one respondent who indicated their view as “unsure.” Six of the 10 faculty experts had 16 years of experience or more working as a nurse educator.
Five nursing students participated in the cognitive interview focus group. The duration of the focus group was 2.5 h. All participants identified that they were born in Canada, self-identified as female (one preferred not to say) and reported having received some instruction about MAiD as part of their nursing curriculum. See Tables 1 and 2 for the demographic descriptors of the study sample. Study results will be reported in accordance with the study phases. See Fig. 1 for an overview of the results from each phase.
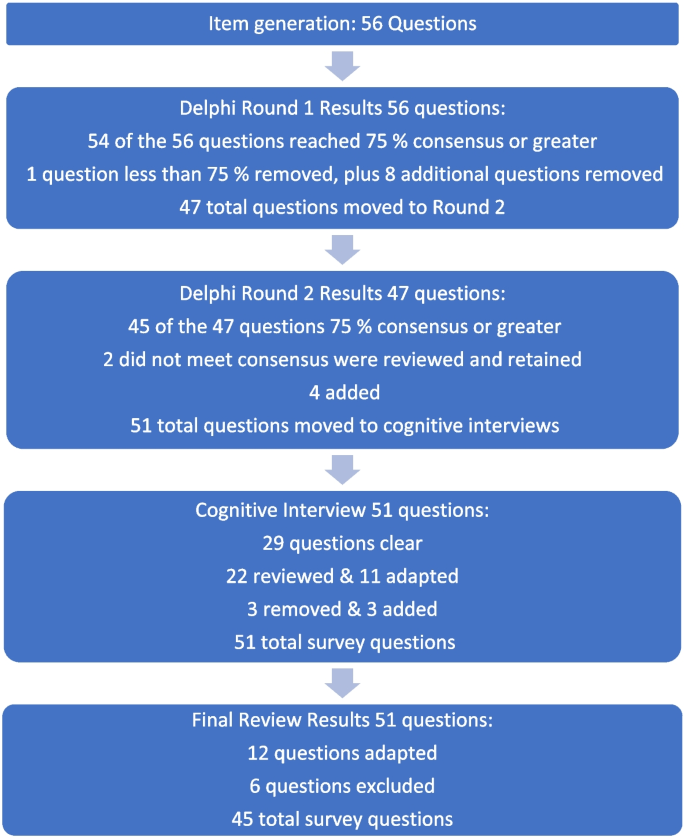
Fig. 1 Overview of survey development findings
Phase 1: survey item generation
Review of the literature identified that no existing survey was available for use with nursing students in the Canadian context. However, an analysis of themes across qualitative and quantitative studies of physicians, medical students, nurses, and nursing students provided sufficient data to develop a preliminary set of items suitable for adaptation to a population of nursing students.
Four major themes and factors that influence knowledge, attitudes, and beliefs about MAiD were evident from the literature: (i) endogenous or individual factors such as age, gender, personally held values, religion, religiosity, and/or spirituality [ 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], (ii) experience with death and dying in personal and/or professional life [ 35 , 40 , 41 , 43 , 44 , 45 ], (iii) training including curricular instruction about clinical role, scope of practice, or the law [ 23 , 36 , 39 ], and (iv) exogenous or social factors such as the influence of key leaders, colleagues, friends and/or family, professional and licensure organizations, support within professional settings, and/or engagement in MAiD in an interdisciplinary team context [ 9 , 35 , 46 ].
Studies of nursing students also suggest overlap across these categories. For example, value for patient autonomy [ 23 ] and the moral complexity of decision-making [ 37 ] are important factors that contribute to attitudes about MAiD and may stem from a blend of personally held values coupled with curricular content, professional training and norms, and clinical exposure. For example, students report that participation in end of life care allows for personal growth, shifts in perception, and opportunities to build therapeutic relationships with their clients [ 44 , 47 , 48 ].
Preliminary items generated from the literature resulted in 56 questions from 11 published sources (See Table 3 ). These items were constructed across four main categories: (i) socio-demographic questions; (ii) end of life care questions; (iii) knowledge about MAiD; or (iv) comfort and willingness to participate in MAiD. Knowledge questions were refined to reflect current MAiD legislation, policies, and regulatory frameworks. Falconer [ 39 ] and Freeman [ 45 ] studies were foundational sources for item selection. Additionally, four case studies were written to reflect the most recent anticipated changes to MAiD legislation and all used the same open-ended core questions to address respondents’ perspectives about the patient’s right to make the decision, comfort in assisting a physician or NP to administer MAiD in that scenario, and hypothesized comfort about serving as a primary provider if qualified as an NP in future. Response options for the survey were also constructed during this stage and included: open text, categorical, yes/no , and Likert scales.
Phase 2: faculty expert panel review
Of the 56 items presented to the faculty panel, 54 questions reached 75% consensus. However, based upon the qualitative responses 9 items were removed largely because they were felt to be repetitive. Items that generated the most controversy were related to measuring religion and spirituality in the Canadian context, defining end of life care when there is no agreed upon time frames (e.g., last days, months, or years), and predicting willingness to be involved in a future events – thus predicting their future selves. Phase 2, round 1 resulted in an initial set of 47 items which were then presented back to the faculty panel in round 2.
Of the 47 initial questions presented to the panel in round 2, 45 reached a level of consensus of 75% or greater, and 34 of these questions reached a level of 100% consensus [ 27 ] of which all participants chose to include without any adaptations) For each question, level of importance was determined based on a 5-point Likert scale (1 = very unimportant, 2 = somewhat unimportant, 3 = neutral, 4 = somewhat important, and 5 = very important). Figure 2 provides an overview of the level of importance assigned to each item.
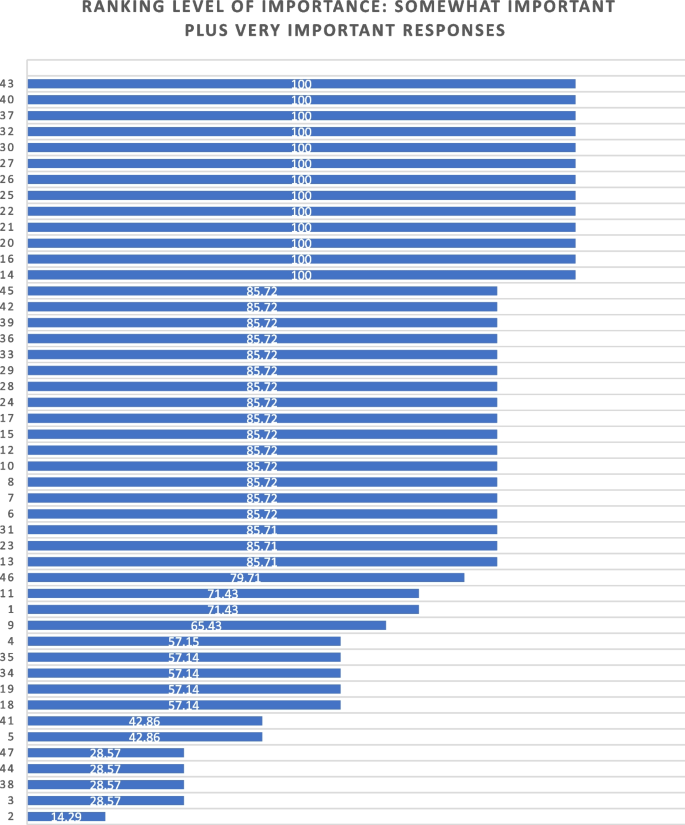
Ranking level of importance for survey items
After round 2, a careful analysis of participant comments and level of importance was completed by the research team. While the main method of survey item development came from participants’ response to the first round of Delphi consensus ratings, level of importance was used to assist in the decision of whether to keep or modify questions that created controversy, or that rated lower in the include/exclude/adapt portion of the Delphi. Survey items that rated low in level of importance included questions about future roles, sex and gender, and religion/spirituality. After deliberation by the research committee, these questions were retained in the survey based upon the importance of these variables in the scientific literature.
Of the 47 questions remaining from Phase 2, round 2, four were revised. In addition, the two questions that did not meet the 75% cut off level for consensus were reviewed by the research team. The first question reviewed was What is your comfort level with providing a MAiD death in the future if you were a qualified NP ? Based on a review of participant comments, it was decided to retain this question for the cognitive interviews with students in the final phase of testing. The second question asked about impacts on respondents’ views of MAiD and was changed from one item with 4 subcategories into 4 separate items, resulting in a final total of 51 items for phase 3. The revised survey was then brought forward to the cognitive interviews with student participants in Phase 3. (see Supplementary Material 1 for a complete description of item modification during round 2).
Phase 3. Outcomes of cognitive interview focus group
Of the 51 items reviewed by student participants, 29 were identified as clear with little or no discussion. Participant comments for the remaining 22 questions were noted and verified against the audio recording. Following content analysis of the comments, four key themes emerged through the student discussion: unclear or ambiguous wording; difficult to answer questions; need for additional response options; and emotional response evoked by questions. An example of unclear or ambiguous wording was a request for clarity in the use of the word “sufficient” in the context of assessing an item that read “My nursing education has provided sufficient content about the nursing role in MAiD.” “Sufficient” was viewed as subjective and “laden with…complexity that distracted me from the question.” The group recommended rewording the item to read “My nursing education has provided enough content for me to care for a patient considering or requesting MAiD.”
An example of having difficulty answering questions related to limited knowledge related to terms used in the legislation such as such as safeguards , mature minor , eligibility criteria , and conscientious objection. Students were unclear about what these words meant relative to the legislation and indicated that this lack of clarity would hamper appropriate responses to the survey. To ensure that respondents are able to answer relevant questions, student participants recommended that the final survey include explanation of key terms such as mature minor and conscientious objection and an overview of current legislation.
Response options were also a point of discussion. Participants noted a lack of distinction between response options of unsure and unable to say . Additionally, scaling of attitudes was noted as important since perspectives about MAiD are dynamic and not dichotomous “agree or disagree” responses. Although the faculty expert panel recommended the integration of the demographic variables of religious and/or spiritual remain as a single item, the student group stated a preference to have religion and spirituality appear as separate items. The student focus group also took issue with separate items for the variables of sex and gender, specifically that non-binary respondents might feel othered or “outed” particularly when asked to identify their sex. These variables had been created based upon best practices in health research but students did not feel they were appropriate in this context [ 49 ]. Finally, students agreed with the faculty expert panel in terms of the complexity of projecting their future involvement as a Nurse Practitioner. One participant stated: “I certainly had to like, whoa, whoa, whoa. Now let me finish this degree first, please.” Another stated, “I'm still imagining myself, my future career as an RN.”
Finally, student participants acknowledged the array of emotions that some of the items produced for them. For example, one student described positive feelings when interacting with the survey. “Brought me a little bit of feeling of joy. Like it reminded me that this is the last piece of independence that people grab on to.” Another participant, described the freedom that the idea of an advance request gave her. “The advance request gives the most comfort for me, just with early onset Alzheimer’s and knowing what it can do.” But other participants described less positive feelings. For example, the mature minor case study yielded a comment: “This whole scenario just made my heart hurt with the idea of a child requesting that.”
Based on the data gathered from the cognitive interview focus group of nursing students, revisions were made to 11 closed-ended questions (see Table 4 ) and 3 items were excluded. In the four case studies, the open-ended question related to a respondents’ hypothesized actions in a future role as NP were removed. The final survey consists of 45 items including 4 case studies (see Supplementary Material 3 ).
The aim of this study was to develop and validate a survey that can be used to track the growth of knowledge about MAiD among nursing students over time, inform training programs about curricular needs, and evaluate attitudes and willingness to participate in MAiD at time-points during training or across nursing programs over time.
The faculty expert panel and student participants in the cognitive interview focus group identified a need to establish core knowledge of the terminology and legislative rules related to MAiD. For example, within the cognitive interview group of student participants, several acknowledged lack of clear understanding of specific terms such as “conscientious objector” and “safeguards.” Participants acknowledged discomfort with the uncertainty of not knowing and their inclination to look up these terms to assist with answering the questions. This survey can be administered to nursing or pre-nursing students at any phase of their training within a program or across training programs. However, in doing so it is important to acknowledge that their baseline knowledge of MAiD will vary. A response option of “not sure” is important and provides a means for respondents to convey uncertainty. If this survey is used to inform curricular needs, respondents should be given explicit instructions not to conduct online searches to inform their responses, but rather to provide an honest appraisal of their current knowledge and these instructions are included in the survey (see Supplementary Material 3 ).
Some provincial regulatory bodies have established core competencies for entry-level nurses that include MAiD. For example, the BC College of Nurses and Midwives (BCCNM) requires “knowledge about ethical, legal, and regulatory implications of medical assistance in dying (MAiD) when providing nursing care.” (10 p. 6) However, across Canada curricular content and coverage related to end of life care and MAiD is variable [ 23 ]. Given the dynamic nature of the legislation that includes portions of the law that are embargoed until 2024, it is important to ensure that respondents are guided by current and accurate information. As the law changes, nursing curricula, and public attitudes continue to evolve, inclusion of core knowledge and content is essential and relevant for investigators to be able to interpret the portions of the survey focused on attitudes and beliefs about MAiD. Content knowledge portions of the survey may need to be modified over time as legislation and training change and to meet the specific purposes of the investigator.
Given the sensitive nature of the topic, it is strongly recommended that surveys be conducted anonymously and that students be provided with an opportunity to discuss their responses to the survey. A majority of feedback from both the expert panel of faculty and from student participants related to the wording and inclusion of demographic variables, in particular religion, religiosity, gender identity, and sex assigned at birth. These and other demographic variables have the potential to be highly identifying in small samples. In any instance in which the survey could be expected to yield demographic group sizes less than 5, users should eliminate the demographic variables from the survey. For example, the profession of nursing is highly dominated by females with over 90% of nurses who identify as female [ 50 ]. Thus, a survey within a single class of students or even across classes in a single institution is likely to yield a small number of male respondents and/or respondents who report a difference between sex assigned at birth and gender identity. When variables that serve to identify respondents are included, respondents are less likely to complete or submit the survey, to obscure their responses so as not to be identifiable, or to be influenced by social desirability bias in their responses rather than to convey their attitudes accurately [ 51 ]. Further, small samples do not allow for conclusive analyses or interpretation of apparent group differences. Although these variables are often included in surveys, such demographics should be included only when anonymity can be sustained. In small and/or known samples, highly identifying variables should be omitted.
There are several limitations associated with the development of this survey. The expert panel was comprised of faculty who teach nursing students and are knowledgeable about MAiD and curricular content, however none identified as a conscientious objector to MAiD. Ideally, our expert panel would have included one or more conscientious objectors to MAiD to provide a broader perspective. Review by practitioners who participate in MAiD, those who are neutral or undecided, and practitioners who are conscientious objectors would ensure broad applicability of the survey. This study included one student cognitive interview focus group with 5 self-selected participants. All student participants had held discussions about end of life care with at least one patient, 4 of 5 participants had worked with a patient who requested MAiD, and one had been present for a MAiD death. It is not clear that these participants are representative of nursing students demographically or by experience with end of life care. It is possible that the students who elected to participate hold perspectives and reflections on patient care and MAiD that differ from students with little or no exposure to end of life care and/or MAiD. However, previous studies find that most nursing students have been involved with end of life care including meaningful discussions about patients’ preferences and care needs during their education [ 40 , 44 , 47 , 48 , 52 ]. Data collection with additional student focus groups with students early in their training and drawn from other training contexts would contribute to further validation of survey items.
Future studies should incorporate pilot testing with small sample of nursing students followed by a larger cross-program sample to allow evaluation of the psychometric properties of specific items and further refinement of the survey tool. Consistent with literature about the importance of leadership in the context of MAiD [ 12 , 53 , 54 ], a study of faculty knowledge, beliefs, and attitudes toward MAiD would provide context for understanding student perspectives within and across programs. Additional research is also needed to understand the timing and content coverage of MAiD across Canadian nurse training programs’ curricula.
The implementation of MAiD is complex and requires understanding of the perspectives of multiple stakeholders. Within the field of nursing this includes clinical providers, educators, and students who will deliver clinical care. A survey to assess nursing students’ attitudes toward and willingness to participate in MAiD in the Canadian context is timely, due to the legislation enacted in 2016 and subsequent modifications to the law in 2021 with portions of the law to be enacted in 2027. Further development of this survey could be undertaken to allow for use in settings with practicing nurses or to allow longitudinal follow up with students as they enter practice. As the Canadian landscape changes, ongoing assessment of the perspectives and needs of health professionals and students in the health professions is needed to inform policy makers, leaders in practice, curricular needs, and to monitor changes in attitudes and practice patterns over time.
Availability of data and materials
The datasets used and/or analysed during the current study are not publicly available due to small sample sizes, but are available from the corresponding author on reasonable request.
Abbreviations
British Columbia College of Nurses and Midwives
Medical assistance in dying
Nurse practitioner
Registered nurse
University of British Columbia Okanagan
Nicol J, Tiedemann M. Legislative Summary: Bill C-14: An Act to amend the Criminal Code and to make related amendments to other Acts (medical assistance in dying). Available from: https://lop.parl.ca/staticfiles/PublicWebsite/Home/ResearchPublications/LegislativeSummaries/PDF/42-1/c14-e.pdf .
Downie J, Scallion K. Foreseeably unclear. The meaning of the “reasonably foreseeable” criterion for access to medical assistance in dying in Canada. Dalhousie Law J. 2018;41(1):23–57.
Nicol J, Tiedeman M. Legislative summary of Bill C-7: an act to amend the criminal code (medical assistance in dying). Ottawa: Government of Canada; 2021.
Google Scholar
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf .
Council of Canadian Academies. The state of knowledge on advance requests for medical assistance in dying. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2019/02/The-State-of-Knowledge-on-Advance-Requests-for-Medical-Assistance-in-Dying.pdf .
Council of Canadian Academies. The state of knowledge on medical assistance in dying for mature minors. Ottawa; 2018. Available from: https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-for-Mature-Minors.pdf .
Health Canada. Third annual report on medical assistance in dying in Canada 2021. Ottawa; 2022. [cited 2023 Oct 23]. Available from: https://www.canada.ca/en/health-canada/services/medical-assistance-dying/annual-report-2021.html .
Banner D, Schiller CJ, Freeman S. Medical assistance in dying: a political issue for nurses and nursing in Canada. Nurs Philos. 2019;20(4): e12281.
Article PubMed Google Scholar
Pesut B, Thorne S, Stager ML, Schiller CJ, Penney C, Hoffman C, et al. Medical assistance in dying: a review of Canadian nursing regulatory documents. Policy Polit Nurs Pract. 2019;20(3):113–30.
Article PubMed PubMed Central Google Scholar
College of Registered Nurses of British Columbia. Scope of practice for registered nurses [Internet]. Vancouver; 2018. Available from: https://www.bccnm.ca/Documents/standards_practice/rn/RN_ScopeofPractice.pdf .
Pesut B, Thorne S, Schiller C, Greig M, Roussel J, Tishelman C. Constructing good nursing practice for medical assistance in dying in Canada: an interpretive descriptive study. Global Qual Nurs Res. 2020;7:2333393620938686. https://doi.org/10.1177/2333393620938686 .
Article Google Scholar
Pesut B, Thorne S, Schiller CJ, Greig M, Roussel J. The rocks and hard places of MAiD: a qualitative study of nursing practice in the context of legislated assisted death. BMC Nurs. 2020;19:12. https://doi.org/10.1186/s12912-020-0404-5 .
Pesut B, Greig M, Thorne S, Burgess M, Storch JL, Tishelman C, et al. Nursing and euthanasia: a narrative review of the nursing ethics literature. Nurs Ethics. 2020;27(1):152–67.
Pesut B, Thorne S, Storch J, Chambaere K, Greig M, Burgess M. Riding an elephant: a qualitative study of nurses’ moral journeys in the context of Medical Assistance in Dying (MAiD). Journal Clin Nurs. 2020;29(19–20):3870–81.
Lamb C, Babenko-Mould Y, Evans M, Wong CA, Kirkwood KW. Conscientious objection and nurses: results of an interpretive phenomenological study. Nurs Ethics. 2018;26(5):1337–49.
Wright DK, Chan LS, Fishman JR, Macdonald ME. “Reflection and soul searching:” Negotiating nursing identity at the fault lines of palliative care and medical assistance in dying. Social Sci & Med. 2021;289: 114366.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;54(4):511–20.
Bruce A, Beuthin R. Medically assisted dying in Canada: "Beautiful Death" is transforming nurses' experiences of suffering. The Canadian J Nurs Res | Revue Canadienne de Recherche en Sci Infirmieres. 2020;52(4):268–77. https://doi.org/10.1177/0844562119856234 .
Canadian Nurses Association. Code of ethics for registered nurses. Ottawa; 2017. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-ethics .
Canadian Nurses Association. National nursing framework on Medical Assistance in Dying in Canada. Ottawa: 2017. Available from: https://www.virtualhospice.ca/Assets/cna-national-nursing-framework-on-maidEng_20170216155827.pdf .
Pesut B, Thorne S, Greig M. Shades of gray: conscientious objection in medical assistance in dying. Nursing Inq. 2020;27(1): e12308.
Durojaiye A, Ryan R, Doody O. Student nurse education and preparation for palliative care: a scoping review. PLoS ONE. 2023. https://doi.org/10.1371/journal.pone.0286678 .
McMechan C, Bruce A, Beuthin R. Canadian nursing students’ experiences with medical assistance in dying | Les expériences d’étudiantes en sciences infirmières au regard de l’aide médicale à mourir. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2019;5(1). https://doi.org/10.17483/2368-6669.1179 .
Adler M, Ziglio E. Gazing into the oracle. The Delphi method and its application to social policy and public health. London: Jessica Kingsley Publishers; 1996
Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–12.
Keeney S, Hasson F, McKenna H. The Delphi technique in nursing and health research. 1st ed. City: Wiley; 2011.
Willis GB. Cognitive interviewing: a tool for improving questionnaire design. 1st ed. Thousand Oaks, Calif: Sage; 2005. ISBN: 9780761928041
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood EW. Conscience, conscientious objection, and nursing: a concept analysis. Nurs Ethics. 2017;26(1):37–49.
Lamb C, Evans M, Babenko-Mould Y, Wong CA, Kirkwood K. Nurses’ use of conscientious objection and the implications of conscience. J Adv Nurs. 2018;75(3):594–602.
de Vaus D. Surveys in social research. 6th ed. Abingdon, Oxon: Routledge; 2014.
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: A primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2018.00149 .
Puchta C, Potter J. Focus group practice. 1st ed. London: Sage; 2004.
Book Google Scholar
Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. Oxford: Oxford University Press; 2015.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Adesina O, DeBellis A, Zannettino L. Third-year Australian nursing students’ attitudes, experiences, knowledge, and education concerning end-of-life care. Int J of Palliative Nurs. 2014;20(8):395–401.
Bator EX, Philpott B, Costa AP. This moral coil: a cross-sectional survey of Canadian medical student attitudes toward medical assistance in dying. BMC Med Ethics. 2017;18(1):58.
Beuthin R, Bruce A, Scaia M. Medical assistance in dying (MAiD): Canadian nurses’ experiences. Nurs Forum. 2018;53(4):511–20.
Brown J, Goodridge D, Thorpe L, Crizzle A. What is right for me, is not necessarily right for you: the endogenous factors influencing nonparticipation in medical assistance in dying. Qual Health Res. 2021;31(10):1786–1800.
Falconer J, Couture F, Demir KK, Lang M, Shefman Z, Woo M. Perceptions and intentions toward medical assistance in dying among Canadian medical students. BMC Med Ethics. 2019;20(1):22.
Green G, Reicher S, Herman M, Raspaolo A, Spero T, Blau A. Attitudes toward euthanasia—dual view: Nursing students and nurses. Death Stud. 2022;46(1):124–31.
Hosseinzadeh K, Rafiei H. Nursing student attitudes toward euthanasia: a cross-sectional study. Nurs Ethics. 2019;26(2):496–503.
Ozcelik H, Tekir O, Samancioglu S, Fadiloglu C, Ozkara E. Nursing students’ approaches toward euthanasia. Omega (Westport). 2014;69(1):93–103.
Canning SE, Drew C. Canadian nursing students’ understanding, and comfort levels related to medical assistance in dying. Qual Adv Nurs Educ - Avancées en Formation Infirmière. 2022;8(2). https://doi.org/10.17483/2368-6669.1326 .
Edo-Gual M, Tomás-Sábado J, Bardallo-Porras D, Monforte-Royo C. The impact of death and dying on nursing students: an explanatory model. J Clin Nurs. 2014;23(23–24):3501–12.
Freeman LA, Pfaff KA, Kopchek L, Liebman J. Investigating palliative care nurse attitudes towards medical assistance in dying: an exploratory cross-sectional study. J Adv Nurs. 2020;76(2):535–45.
Brown J, Goodridge D, Thorpe L, Crizzle A. “I am okay with it, but I am not going to do it:” the exogenous factors influencing non-participation in medical assistance in dying. Qual Health Res. 2021;31(12):2274–89.
Dimoula M, Kotronoulas G, Katsaragakis S, Christou M, Sgourou S, Patiraki E. Undergraduate nursing students’ knowledge about palliative care and attitudes towards end-of-life care: A three-cohort, cross-sectional survey. Nurs Educ Today. 2019;74:7–14.
Matchim Y, Raetong P. Thai nursing students’ experiences of caring for patients at the end of life: a phenomenological study. Int J Palliative Nurs. 2018;24(5):220–9.
Canadian Institute for Health Research. Sex and gender in health research [Internet]. Ottawa: CIHR; 2021 [cited 2023 Oct 23]. Available from: https://cihr-irsc.gc.ca/e/50833.html .
Canadian Nurses’ Association. Nursing statistics. Ottawa: CNA; 2023 [cited 2023 Oct 23]. Available from: https://www.cna-aiic.ca/en/nursing/regulated-nursing-in-canada/nursing-statistics .
Krumpal I. Determinants of social desirability bias in sensitive surveys: a literature review. Qual Quant. 2013;47(4):2025–47. https://doi.org/10.1007/s11135-011-9640-9 .
Ferri P, Di Lorenzo R, Stifani S, Morotti E, Vagnini M, Jiménez Herrera MF, et al. Nursing student attitudes toward dying patient care: a European multicenter cross-sectional study. Acta Bio Medica Atenei Parmensis. 2021;92(S2): e2021018.
PubMed PubMed Central Google Scholar
Beuthin R, Bruce A. Medical assistance in dying (MAiD): Ten things leaders need to know. Nurs Leadership. 2018;31(4):74–81.
Thiele T, Dunsford J. Nurse leaders’ role in medical assistance in dying: a relational ethics approach. Nurs Ethics. 2019;26(4):993–9.
Download references
Acknowledgements
We would like to acknowledge the faculty and students who generously contributed their time to this work.
JS received a student traineeship through the Principal Research Chairs program at the University of British Columbia Okanagan.
Author information
Authors and affiliations.
School of Health and Human Services, Selkirk College, Castlegar, BC, Canada
Jocelyn Schroeder & Barbara Pesut
School of Nursing, University of British Columbia Okanagan, Kelowna, BC, Canada
Barbara Pesut, Lise Olsen, Nelly D. Oelke & Helen Sharp
You can also search for this author in PubMed Google Scholar
Contributions
JS made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. JS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. BP made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and drafting and substantively revising the work. BP has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. LO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. LO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. NDO made substantial contributions to the conception of the work; data acquisition, analysis, and interpretation; and substantively revising the work. NDO has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HS made substantial contributions to drafting and substantively revising the work. HS has approved the submitted version and agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
JS conducted this study as part of their graduate requirements in the School of Nursing, University of British Columbia Okanagan.
Corresponding author
Correspondence to Barbara Pesut .
Ethics declarations
Ethics approval and consent to participate.
The research was approved by the Selkirk College Research Ethics Board (REB) ID # 2021–011 and the University of British Columbia Behavioral Research Ethics Board ID # H21-01181.
All participants provided written and informed consent through approved consent processes. Research was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schroeder, J., Pesut, B., Olsen, L. et al. Developing a survey to measure nursing students’ knowledge, attitudes and beliefs, influences, and willingness to be involved in Medical Assistance in Dying (MAiD): a mixed method modified e-Delphi study. BMC Nurs 23 , 326 (2024). https://doi.org/10.1186/s12912-024-01984-z
Download citation
Received : 24 October 2023
Accepted : 28 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s12912-024-01984-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical assistance in dying (MAiD)
- End of life care
- Student nurses
- Nursing education
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Gerontologist

Care Home Life and Identity: A Qualitative Case Study
Katie paddock.
1 School of Health Sciences, Faculty of Biology, Medicine and Health, Division of Nursing, Midwifery and Social Work, University of Manchester, UK
2 Manchester Academic Health Science Centre, UK
6 Psychological Sciences, Institute of Psychology, Health, and Society, University of Liverpool, Liverpool, UK
Christine Brown Wilson
3 School of Nursing and Midwifery, Queen’s University, Belfast, UK
Catherine Walshe
4 International Observatory on End of Life Care, Division of Health Research, Furness Building, Lancaster University, UK
5 Manchester University Foundation NHS Foundation Trust, UK
Background and Objectives
The transition to a care home can involve multiple changes and losses that can affect an older person’s well-being and identity. It is not clear how older people perceive and manage their identity within a care home over time. This study explores how living in a care home affects the identities of residents and how they address this in their daily lives.
Research Design and Methods
A multiple qualitative case study approach incorporated interview and observational data. Eighteen semistructured interviews and 260 hr of observations were conducted over 1 year with care home residents, relatives, and staff across three care homes within Greater Manchester, UK. Data were analyzed using framework analysis, drawing on the social identity perspective as an interpretive lens.
Four themes were identified: (a) changing with age, (b) independence and autonomy, (c) bounded identity, and (d) social comparison. The impact of aging that initially altered residents’ identities was exacerbated by the care home environment. Institutional restrictions jeopardized independence and autonomy, provoking residents to redefine this within the allowances of the care home. Strict routines and resource constraints of well-meaning staff resulted in the bounded expression of personalities. Consequently, to forge a positive identity, residents without dementia engaged in social comparison with residents with dementia, emphasizing their superior cognitive and physical abilities.
Discussion and Implications
Social comparison as an adaptive strategy has previously been unidentified in care home literature. Residents need more support to express their identities, which may reduce the necessity of social comparison, and improve interrelationships and well-being.
Moving to long-term residential and/or nursing care facilities (hereafter referred to as “care homes”) involves a series of changes that can affect an older person’s sense of identity ( Froggatt, Davies, & Meyer, 2009 ; Næss, Fjær, & Vabø, 2016 ; Tajfel & Turner, 1979 ). Residents can become disconnected from facets or symbols of their identity, including social networks, familiar routines, recreational activities, and meaningful belongings. This disconnect can result in poor well-being or depression ( NCHR&D, 2006 ; Tester, Hubbard, Downs, MacDonald, & Murphy, 2004 ). In addition, the transition to a care home often occurs at the nadir of physical and/or cognitive abilities ( Kingston et al., 2017 ), thereby limiting residents’ functional abilities to adapt to this new context and increasing their reliance on care staff to facilitate identity maintenance. In England, supporting identities is a quality standard for care homes, but variations in care quality, limited resources, and poor workforce morale can impede such aims ( Alzheimer’s Society, 2013 ; Care Quality Commission, 2016 ; Lievesley, Crosby, Bowman, & Midwinter, 2011 ). To improve residents’ sense of identity in care homes, we must understand how it is negotiated within this complex context.
Few studies have explored the daily impact of life within care homes on identity, particularly from the perspectives of relevant stakeholders; residents, their significant others, and care home staff. In this article, we address this gap. We use the social identity perspective (SIP) as a theoretical lens to explore the strategies that residents use to adapt to life in a care home over time, and the daily contributions of others in the co-construction of residents’ identities.
SIP holds that individuals’ overall sense of identity is a composite of memberships to meaningful social groups (social identity) and idiosyncratic personal attributes (personal identity). Identity maintenance is an inherently social process that occurs across the life course, where different identities come to the fore within different salient contexts ( Hogg & Abrams, 1988 ; Oakes, Haslam, & Turner, 1994 ; Turner, 1982 ). Major life events, such as the transition to a care home, can disrupt connections to social groups and idiosyncratic attributes ( Hockey & James, 2003 ; NCHR&D, 2006 ; Kroger, Martinussen, & Marcia, 2010 ; Tajfel & Turner, 1979 ). Maintaining social relationships or establishing new connections buffers against negative outcomes ( A. Haslam, Jetten, Postmes, & Haslam, 2009 ; Jetten & Pachana, 2012 ), but studies have shown physical and interpersonal barriers to this ( Abbott, Bangerter, Humes, Klumpp, & Van Haitsma, 2017 ; Hubbard, Tester, & Downs, 2003 ), limiting opportunities to bolster identities within this new context.
Social groups are also judged by others as being of a higher or lower status, and the positivity of one’s identity is derived from the internalization of these evaluations ( Tajfel & Turner, 1979 ). Adaptive strategies can be used to maintain a positive identity when associated with a negatively perceived group ( Reicher, Spears, & Haslam, 2010 ; Tajfel, 1981 ; Tajfel & Turner, 1979 ). These include (a) social mobility: physically or psychologically leave the group and adopt a different identity; (b) social creativity: reframing the negativity as something positive, changing comparator dimensions to something more positive, or changing the comparison group to an even more negatively perceived group; and (c) social competition: direct competition with the outgroup. The use of these strategies will depend on the perceived permeability of the boundaries between groups. SIP, therefore, emphasizes the social- and context-dependent nature of identity.
SIP has been used in other social care areas ( Black et al., 2018 ; Iyer, Jetten, Tsivrikos, Postmes, & Haslam, 2009 ; Jetten & Pachana, 2012 ; Knight, Haslam, & Haslam, 2010 ), but it has been used much less frequently in care homes ( C. Haslam et al., 2014 ) and with little focus on the social- and context-dependent nature of identity from multiple perspectives. In this study, we use SIP to explore identity management within the care home context and incorporate the perspectives of residents, their relatives, and staff members. This will help inform approaches for supporting residents to maintain a positive sense of self and improve well-being, and improve their experiences of long-term care.
Study Design
This study used a multiple qualitative case study approach. Case study methodology facilitates the triangulation of multiple methods and sources of evidence to explore complex, context-dependent phenomena ( Walshe, Caress, Chew-Graham, & Todd, 2004 ; Yin, 2009 ), which is congruent with the inherently social and complex, context-dependent nature of identity management in SIP. Cases were defined as individual care homes. Within each case, data were collected using interview and observation methods (see below) to explore how daily life in a care home influences identity from multiple stakeholders’ perspectives.
The following theoretical propositions ( Yin, 2009 ), based on SIP and care home literature, were used to guide data collection and analysis:
- Residents will renegotiate their identities within the context of the care home in light of new social relationships and interactions;
- Maintaining links with previous social networks and habits (e.g., daily routines, personal décor) will be important for residents to maintain a sense of self; and
- The care home environment will have the potential to accommodate a multitude of identities with adequate support from individuals and appropriate resources.
Within- and Cross-Case Sampling and Recruitment
Care homes in Greater Manchester, UK, were recruited through local research networks and via gatekeepers. Cases were purposefully sampled to vary in size (number of beds), location (high- or low-income areas), and building type (converted house or purpose-built facility). This aimed to acquire a broad range of experiences, and theoretical replication, where differing variables across cases are anticipated to yield contrasting results ( Yin, 2009 , 2010). The intended case sample was small to encourage rich, contextualized data, to understand the phenomenon under study ( Cleary, Horsfall, & Hayter, 2014 ; Geertz, 1973 ). Twenty-three care homes were approached to participate, and three care homes agreed. Table 1 illustrates basic information about the care homes.
Features of Participating Care Homes
Care home residents, family and friends, and staff, who met the following inclusion criteria, were eligible to participate: Residents aged 65 years or older, who had capacity to consent; all staff who had regular contact with residents, including managerial and nursing staff; all visitors who were a relative or long-term acquaintance of a resident (collectively termed “relatives” for ease). Staff identified residents with capacity to consent. Only individuals who could speak English were included, although only one resident was excluded by this constraint.
Prior to study commencement, the first author (K. Paddock) spent an introductory period within each care home. She introduced herself and the study, and engaged in informal conversations, to ensure that potential participants were comfortable with her presence and identified her as a researcher, not a visitor or staff member.
Convenience and purposeful techniques were used to sample residents, their relatives, and staff for interview. These included if residents/relatives had particularly positive or negative experiences of the move to a care home and subsequent adjustment or staff who were involved in daily decision making in the care homes or care of residents. Informed consent was obtained prior to recording of interviews. It was not possible to obtain written consent prior to observations due to the busy, often transient nature of care homes, and the risk of disrupting daily care or altering the dynamic of any event being observed. Information about the study and observations were displayed in each care home, and before each observation, individuals were verbally made aware of the researcher’s presence. Individuals could opt-out of observations via the researcher, members of staff, or opt-out form, and any field notes would then be excluded from analysis, an approach used elsewhere ( Conroy, 2017 ; Newnham, McKellar, & Pincombe, 2017 ). No individuals opted out.
Within-Case Methods: Data Collection
Semistructured topic guides were designed to provoke discussion of perceptions of the residents’ identity over their life course, their transition to the care home, and subsequent adjustment. Staff were asked for their perspectives on their roles in promoting identities within the care home, on perceived barriers and facilitators, and on residents’ adjustment over time. Questions included “Tell me about your move to the care home,” “What would you consider to be a ‘good’ day for you?” (Residents), “How would you describe [the resident]?”, “What would you consider to be meaningful activities for him/her?” (Relatives), “Tell me about a time a resident moved here,” “How do you incorporate individuality within the care home?” (Staff). Questions were developed iteratively to reflect emerging topics and themes.
Observations
All residents, staff, and relatives were eligible for inclusion in observations. Observations were exploratory and guided by SIP’s assertion that identities are influenced by social interactions and can be expressed externally, such as via hobbies and possessions. Observations and field notes focused on daily events in the care homes, including organized activities, daily care, and interactions between residents, staff, and visitors. Field notes also included conversations between participants and the first author. Residents without capacity to consent or opt-out were included in field notes for contextual purposes if they were central to observations involving other participants. Observations were a mixture of participatory and nonparticipatory: At times, the researcher remained a passive observer, but where possible she contributed informally to the daily life of the care homes by helping to serve meals and make drinks. This facilitated immersion in each care home and being allowed to witness personal care, such as dressing, an approach used in a similar context ( Næss et al., 2016 ). Observations occurred on different days and times of day, including evenings and weekends, to reduce the possibility that data were focused around particular activities or participants.
Data collection ceased once data saturation was reached, where no new findings emerge in subsequent data collection, within or across cases ( O’Reilly & Parker, 2012 ).
Data Analysis, Rigor, and Validity
Transcripts of recorded interviews and field notes were managed using NVivo and analyzed, within and cross-case, using framework analysis ( Ritchie & Spencer, 1994 ). This is a systematic and rigorous approach consisting of five interrelated stages (see Box 1 ), whereby iterative data collection and analysis of multiple data sources produce a transparent audit trail, so findings and interpretations are grounded in the data ( Gale, Heath, Cameron, Rashid, & Redwood, 2013 ; Ward, Furber, Tierney, & Swallow, 2013 ). The theoretical propositions derived from SIP (section Study Design) informed the preliminary coding framework, which was continuously reviewed in light of emergent data-driven codes and themes. Pattern-matching of data against a priori propositions reconciles the diverse perspectives of a phenomenon within and across cases ( Almutairi, Gardner, & McCarthy, 2014 ). Analysis generated a final analytic framework of 62 codes, grouped, and charted into four themes.
Box 1. Stages of Framework Analysis
Immersion in the data. Read complete transcripts and field notes.
Initial development of a coding framework developed through a priori issues and familiarization stage.
The process of systematically applying the thematic framework to data. Changes made as necessary to reflect the data.
Using headings from thematic framework to create charts of data.
Searching for patterns and explanations in the data.
All data were collected by the first author (K. Paddock), who has prior experience working and researching in social care settings, but is not a clinician. She led data analysis, and regularly discussed emerging findings and experiences with the other three authors, two of whom (C. Brown Wilson and C. Walshe) are registered nurses with experience of working and researching in residential and social care.
Rigor and validity were ensured through the triangulation of multiple modes of data collection and sources of evidence across multiple cases, conducted over time. For respondent validation, the first author provided oral summaries of data and interpretations to participants, and invited comments.
To ensure reflexivity, the first author kept a reflexive diary alongside field notes to record her possible biases and role in shaping encounters. Developing a reflexive, iterative process between data collection and analysis continuously connected the data with emerging insights, leading to a more refined, and credible, understanding of identity ( Lincoln & Guba, 1985 ; Shenton, 2004 ; Srivastava & Hopwood, 2009 ).
Research Ethics Committee approval was obtained from the University of Manchester and Northampton NRES committee (reference number 12/EM/0431). All names have been changed to pseudonyms to protect anonymity. Permission was only granted by the ethics committees to interview residents with capacity to consent.
Semistructured interviews were conducted with 18 participants, and over 260 hr of observations were conducted over a 12-month period across the three cases (see Table 2 ). Interviews lasted between 18 min and 1.5 hr. The majority of residents across the care homes had severe dementia, so could not be interviewed. Some participants were intimidated by a recorded interview, and many staff were too busy, so preferred discussions to be included as field notes (see Table 2 ). Residents also received very few visitors during the data collection period.
Interview Sample and Observational Data Across Care Homes
Within-case analysis generated substantially similar experiences and themes in each care home, and thus, results from a cross-case analysis are presented, with any divergent themes discussed. The four interrelated themes are as follows:
- Changing with age, and how this predated a move into a care home;
- Bounded identity;
- Independence and autonomy; and
- Social comparisons.
Changing With Age
Prior to the relocation to a care home, residents and relatives acknowledged that increased frailty impeded residents’ abilities to perform everyday tasks and meaningful activities, which influenced their self-perception.
Ageing is a terrible thing . . . You can’t do what you used to do . . . (Hayley [resident], interview, Care Home 03)
Social networks and interactions gradually receded due to bereavements or family and friends moving away, which made residents feel disconnected and unable to be themselves:
I miss my people. Where are my people? They know who I am . . . (Philippa [resident], field notes, Care Home 02)
Residents adapted their homes, hobbies, and activities to accommodate these changes. For instance, Ruth (resident, Care Home 02) connected with her family and friends by knitting items for them, but her arthritis restricted her ability to hold knitting needles, so she began crocheting, which uses a different type of needles. This enabled Ruth to continue to make gifts and maintain a feeling of connectedness to important social networks.
The aging process had affected residents’ sense of self, but some had been able to employ strategies to help mitigate its impact. The care home further impeded their established identities and restricted residents’ abilities to adjust in a manner most acceptable to themselves.
Bounded Identity
Residents’ own homes served as a benchmark for the expression of their personal identities, particularly through possessions, clothing, and activities, but the care home environment largely restricted this.
Possessions
All participants agreed that personal possessions helped residents to express their personal and social identities and served as anchors to important memories.
When they wake up ‘til they go to sleep they have that sense of belonging. That this is my room now . . . I know that I bought that clock at such and such a place . . . and that picture there of my husband, that’s a reminder of me and my husband when I was younger . . . (Charlotte [staff, manager], interview, Care Home 02)
Staff emphasized that rooms could be personalized with furniture from home, but there was limited scope to do so because of the small size of most bedrooms. Residents had to relinquish many personal possessions, which upset them and their families, as this was associated with loss of important memories and symbols of identity. Julia (Care Home 01) had been a seamstress, her sewing machine a symbol of her independence, and an anchor for memories of her deceased husband. It was too large for the care home, and its loss signified the loss of important identities and memories:
. . . I’ll never operate the sewing machine again. It’s just the fact that [it’s in storage, not with her]. And it’s my past. (Julia [resident], interview, Care Home 01)
Residents across the care homes had little opportunity to acquire new possessions because there were infrequent visitors to support procurement. Staff typically focused on the occasional acquisition of practical items, such as underwear or toiletries. However, staff also stated that the minimal involvement of relatives made it difficult for them to learn about the preferences of residents with less communicative ability. There were anomalous instances where staff purchased meaningful items for residents, such as a stereo for a resident who loved music (Care Home 01), and jewelry in the color of a resident’s favorite football team (Care Home 02).
Residents and relatives often mentioned the importance of personal aesthetic. Residents admitted to the care home as an emergency had little input into which belongings they kept or relied on clothing borrowed from other residents or purchased by staff. Clothing was occasionally lost or mixed-up between residents, which upset residents and their relatives, who felt that an element of themselves had been stolen. This was particularly pertinent for relatives of residents with dementia, as they felt it highlighted their increased depersonalization and powerlessness:
It was like she was wearing part of me mum. (Amanda [relative], field notes, Care Home 02)
As care needs increased, staff in Care Homes 01 and 02 in particular tended to dress residents in looser-fitting, easy-to-change and easy-to-clean clothes, or “babywear” ( Twigg and Buse, 2013 : 330), regardless of the individual’s personal aesthetic. However, there were notable examples across each care home of staff making an effort to incorporate residents’ preferences in their daily care, typically in relation to colors, or whether someone was a “skirt person” or a “trouser person”:
. . . Joanna [staff], said that it’s ‘a bit of a faff’ getting them in and out of trousers, “but it’s what they prefer” . . . (Field notes, Care Home 03)
Residents derived a sense of self through their hobbies and activities. Staff in each care home initially claimed to incorporate residents’ preferences, but during observations, this rarely occurred. Staff felt constrained by understaffing and limited resources and unable to support residents’ identities and individuality. Consequently, there were few activities overall, and observed activities were based on generalizations to please the most people and did not account for nuanced preferences. These included a music-themed reminiscence group, tai chi (Care Home 01), bingo, and a “memory man” who discussed local history (Care Home 02):
. . . let’s say someone’s gay, and like to go to gay bars, and would like to meet gay people, erm, for example. Um, or let’s say someone’s Caribbean and they like to go to Caribbean clubs . . . I find they kind of take the headline title [of residents’ preferences] and that’s about it. (Adam [staff], interview, Care Home 01)
This approach did not satisfy most residents and relatives, who complained about a lack of stimulation and false promises of individualized activities.
I mean, Tracey [manager] said that they did lots of things in the afternoon, and I’ve never been convinced they’ve done as many as Tracey said they did. (Daniel [relative], interview, Care Home 01)
Residents and relatives acknowledged the financial constraints of many care homes, but felt more could be done to improve daily life. Staff also highlighted difficulties of organizing activities for residents with physical and cognitive impairments:
. . . It’s hard to think of where they can go really. You got to think about where they’re going to go to the toilet and everything—so there’s loads to think about before you even take them out. (Laura [staff], interview, Care Home 02)
Participants in Care Home 03 mentioned plans of a daytrip, but none occurred during the data collection period. However, in Care Home 03, some residents attended a weekly church fete unchaperoned; a luxury they valued. Across all three care homes, television was the most common activity observed. There were limited opportunities for residents to suggest ad hoc activities beyond the immediate resources of the care homes.
Independence and Autonomy
Residents and their relatives frequently emphasized the importance of independence as an element of residents’ identities throughout their life course, and evidenced this in a variety of ways. For instance, Carrie (Care Home 02) was an international fashion buyer; Mary (Care Home 02) attended football matches “with the boys,” which was considered unusual at the time; Richard (Care Home 03) was a freelance photographer.
Repeated reflections on their independence highlighted its absence in the care home. Residents missed the freedom to set their own agendas for the day. The care homes all adopted similar routines: set times for waking residents and putting them to bed, for food and drink, and any activities. Staff discouraged deviations from these routines as it jeopardized the smooth running of the care home. Residents felt that minor changes to routines were occasionally catered for, but at a compromise; Louis (resident, Care Home 03) had requested to sleep in one day, but was then allegedly denied his breakfast as the allotted breakfast time had passed and staff were busy elsewhere. Participants’ perceptions of how successful these allowances and compromises were in practice differed:
Well Ruth (resident) likes to get up really early—Ruth likes to get up at like quarter to seven. . . . So—like when they first come [to the care home], you ask them, like what they like to do . . . (Laura [staff], interview, Care Home 02) I like to get up early. But I have to wait for the nurse [to get me up]. (Ruth [resident], interview, Care Home 02)
Strict health and safety policies and organizational efficiency meant risk-averse staff tended to complete minor tasks themselves, such as making hot drinks, which undermined residents’ independence. The role of staff as carers seemed at odds with the expectation that they should also facilitate independence, particularly because of limited resources:
. . . It’s all well and good saying they want to remain independent, but if you can’t walk, you can’t walk . . . It is our job at the end of the day—to keep them well . . . (Edna [staff], field notes, Care Home 02)
To counter the negative perceptions of aging and increased dependency, many residents amended their definitions of independence and autonomy to emphasize minor daily tasks and accomplishments. Autonomy within the care home was limited to small day-to-day decisions, such as choosing a meal from the available selection, requesting an alternative meal where possible, or deciding when to go to bed if they were physically able to do so unaided. Physical independence to perform certain small tasks such as setting tables at mealtimes, usually authorized by staff, helped residents to feel as though they had retained an important element of their personal identities:
Catherine . . . helped to place the cutlery on the tables . . . and added “I know I’m not completely independent anymore. But it’s something” . . . (Catherine [resident], field notes, Care Home 01)
Each care home had members of staff who made a conscious effort to accommodate residents’ autonomous decision making and individual preferences. A notable example involved Edna’s (staff, Care Home 02) determination to allow a resident a “duvet day,” who uncharacteristically wanted to stay in bed. These infrequent instances encouraged residents to express their individuality, and made them feel more in control of their surroundings and their care. With residents’ new perceptions of independence and autonomy largely based on physical capabilities, this enabled them to use levels of cognition as a source of comparison against other residents who experienced dementia or mental health problems.
Social Comparison
Residents without dementia accepted that moving to a care home was necessary because of their care needs, but felt their positive sense of identity was jeopardized because of the association of care homes with severe cognitive and physical impairment. Residents with dementia represented these negative stereotypes, and symbolized the worst aspects of aging. Consequently, residents without dementia distanced themselves from residents with dementia by engaging in social comparison. They regularly pointed out those with dementia and emphasized their own perceived cognitive superiority, while also expressing sympathy and frustration over the often repetitive or disruptive behaviors associated with severe dementia. Such downward social comparisons serve to enhance self-image and in turn improve well-being ( Gibbons & Gerrard, 1991 ):
[Philippa] was looking at the row of residents sat asleep against the wall . . . “Most of these have lost their minds, you know . . . I can still think for myself. I haven’t gone yet” . . . (Philippa [resident], field notes, Care Home 02)
Residents without dementia typically vocalized their comparisons with members of staff, visitors, or the researcher; not with one another. Only two residents in Care Homes 01 and 03 indicated that they were friends and regularly conversed. Most residents suggested they were lonely, but did not converse with others beyond mealtimes. Although residents stated they were unable to hold meaningful social interactions with residents with dementia, it was difficult to determine why residents without dementia did not engage more with one another. Some participants, particularly staff, suggested residents may not wish to invest in making connections with others because they are acutely aware of their own mortality. When asked, residents said that they simply did not like the other residents, or that it was a lot of effort, especially if they were at risk of developing dementia.
I asked Elizabeth why she didn’t chat to Carrie more . . . after they seemed to have a nice time the other day . . . Elizabeth pulled a face and after a pause said “she’ll probably end up like the rest of ‘em in here . . .” (Field notes, Care Home 02)
The purpose of this study was to explore how life in a care home affects on the identities of care homes residents. The use of SIP offers a broad approach to identity that highlights the importance of context-bound social interactions for the development and maintenance of identity within the unique context of a care home. At the outset of the study, we proposed three theoretical propositions. In relation to these propositions, our findings reveal that (a) residents renegotiate their identities within the context of the care home, but use social interactions to facilitate social comparison with more impaired individuals, while largely failing to establish new relationships; (b) care homes have the potential to accommodate a multitude of identities by facilitating links with previous social networks or symbols that are necessary to maintain a sense of self, (c) but lack adequate support or appropriate resources to achieve this. We now discuss these findings in detail, followed by their implications.
Findings confirm the role of activities, possessions, and clothing, in symbolizing identities, particularly in light of personal and physical loss. Continued identification with such meaningful symbols help to bolster identity, even for individuals with limited expressive capacity, and can be maintained through adapted ways of living ( Black et al., 2018 ; Cohen-Mansfield, Marx, Thein, & Dakheel-Ali, 2010 ; Lloyd, Calnan, Cameron, Seymour, & Smith, 2014 ). But for participants in the present study, the care home environment undermined their abilities to adapt, disrupting connections to many important symbols, and resulting in a limited, bounded expression of residents’ identities.
Institutional restrictions, standardized routines, and strict risk management also threatened residents’ independence and autonomy, as perceived staff shortages and limited resources necessitated the precedence of organizational efficiency over individual needs. It has been established that a failure to satisfy needs for independence and autonomy is related to depressive symptoms and poor well-being and also hinders individuality and the expression of personalities ( Custers, Westerhof, Kuin, Gerritsen, & Riksen-Walraven, 2012 ; Goffman, 1961 ; A. Haslam et al., 2009 ; Knight et al., 2010 ; Wiersma & Dupuis, 2010 ; Kloos, Trompetter, Bohlmeijer, & Westerhof, 2018 ). Consistent with other studies ( Falk, Wijk, Persson, & Falk, 2013 ; Golander, 1995 ; Wiersma & Dupuis, 2010 ), participants in the present study reported an “emotional limbo” between the awareness of residents’ increased care needs and dependency on staff, and the importance of independence to residents’ identities. Our findings show that this motivates residents to emphasize their physical abilities to perform small tasks, to reconcile their established identities within a new, more constrained context.
Maintaining links with social networks or establishing new identity-relevant connections is also necessary to reinforce a sense of self and to buffer against a threatened identity or well-being ( Cohen-Mansfield, Golander, & Arnheim, 2000 ; A. Haslam et al., 2009 ; Surr, 2006 ). Relatives have the potential to support residents’ identity and improve resident outcomes by maintaining relationships with them and with staff ( Davies & Nolan, 2006 ; Roberts & Ishler, 2017 ), but most residents in the present study had little contact anyone outside of the care home and thus were unable to maintain identity-affirming connections. However, residents did not appear to value the opportunity to develop friendships with one another, as has been described elsewhere ( Surr, 2006 ; Tester et al., 2004 ). Rather, our findings resonate with those of Abbott and colleagues (2017) , where residents cited various barriers to social interactions with others, but participants in the present study focused on cognitive impairment as the fundamental obstacle. The fact that most older people residing in the care homes of the present study had a diagnosis of dementia reflects the national statistics of the United Kingdom on levels of impairment in care homes ( Alzheimer’s Society, 2014 ). But the belief among unimpaired residents that residents with dementia, particularly those who also had severe physical impairments, were not viable companions and should be avoided, reflects a more complex issue relating to threatened identities.
According to SIP, psychological strategies such as social competition, social creativity, and social mobility can be used to protect a threatened identity ( Reicher et al., 2010 ; Tajfel, 1981 ; Tajfel & Turner, 1979 ). The present study has shown that by highlighting the impairments of others and emphasizing their own abilities, residents without dementia used social creativity, specifically social comparison, as a means of cognitive adaptation. With little consistent opportunity to buffer identities through other means, social comparison and the motivation to distance oneself from impairment may have also served to alienate residents from one another who could have formed meaningful relationships, whether cognitively impaired or otherwise.
Implications
Although global policy states that care provision should enable self-expression and identity, the ability to make choices, and to maintain connections with social networks ( World Health Organisation, 2015 ), our findings suggest that such goals are difficult to achieve in the care home setting. Few visitors and opportunities to maintain connections outside of the care home place greater pressure on staff to perform identity work. To move forward, we need to understand how guidelines or training on identity is implemented in care homes and how this may be improved. In addition, further research on how residents can maintain connections outside of the care home is needed.
Staffing and resource constraints cannot be easily rectified, but care homes could facilitate residents’ needs within the allowances of their means. This study has demonstrated the value of seemingly minor, but meaningful, interactions between stakeholders, small changes to routines, and supported independence and autonomy. Evidence suggests that interventions to facilitate group-based decision making among care home residents regarding the refurbishment of communal areas created a shared identification, increased social engagement, and improved cognitive function and life satisfaction ( C. Haslam et al., 2014 ). Future interventions could support residents to make collective decisions in other, smaller areas of care home life, such as weekly activities or menu choices. This can promote positive social interaction among stakeholders and improve feelings of independence and autonomy, thereby minimizing the necessity for some residents to distance themselves from others. An assessment of such interventions versus standard practice, focusing on the cost implications and impact on staff workload, can help to determine their feasibility in under-resourced facilities.
Strengths and Limitations
This study is the only U.K.-based study to date that has used observational and interview methods across care homes with SIP. A key strength is the volume of data collected: Over 260 hr of observations across 1 year, combined with iterative interviews, facilitated in-depth exploration of context-bound data to understand the phenomenon of identity management over time. SIP has contributed to other social care areas, and its use in the care home setting helped to uncover and explore psychological strategies used by residents to cope and maintain a positive sense of self.
We only interviewed residents who had capacity to consent, which limits the generalizability of the findings. Future observational studies are needed that includes the perspectives of all care home residents. Furthermore, recruitment of care homes proved difficult. Managers were concerned with the potential distraction for staff or suggested the study had duplicitous aims in light of contemporaneous negative media representations of care homes. Although sampling was purposeful, no purpose-built care homes agreed to participate. There were also very few visitors across each care home, resulting in a small sample of relatives interviewed. Although this may limit generalizability, it is nonetheless an artifact of each case and serves to highlight the contemporaneous issues of maintaining relationships, and in turn identity, in care homes.
This study explored how life in a care home affects residents’ identities. The use of SIP within a multiple case study design, with interview and observational methods, is unique in care home research. Although moving to a care home initially emphasized age-related changes, institutional restrictions and limited social networks further undermined residents’ identities over time. The use of social comparison by residents without dementia served to buffer against daily threats to identity, in particular, the threat of being considered severely cognitively impaired and lacking independence. Resource constraints can make it difficult to adequately support diverse identities, yet even small changes to routines and daily care can help. Adequate resources and support within care homes can facilitate the expression of positive identities. This may reduce the need for staunch social comparison and create a more constructive environment for all residents, which may in turn improve well-being.
This study was funded by Medical Research Council doctoral studentship award for K. Paddock. Grant reference MR/J500410/1.
Conflict of Interest
None reported.
- Abbott K. M., Bangerter L. R., Humes S., Klumpp R., & Van Haitsma K (2017). “It’s important, but…”: Perceived barriers and situational dependencies to social contact preferences of nursing home residents . The Gerontologist , 00, 1–10. doi: 10.1093/geront/gnx109 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Almutairi A. F., Gardner G. E., & McCarthy A (2014). Practical guidance for the use of a pattern-matching technique in case-study research: A case presentation . Nursing & Health Sciences , 16 , 239–244. doi: 10.1111/nhs.12096 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alzheimer’s Society.(2013). Low expectations: Attitudes on choice, care and community for people with dementia in care homes London: Author. [ Google Scholar ]
- Alzheimer’s Society.(2014). What is dementia? (Factsheet 400LP. The Information Standard). Retrieved from www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=106
- Black H. K., Rubinstein R. L., Frankowski A. C., Hrybyk G., Nemec M., & Tucker G. G (2018). Identity, semiotics, and use of symbols in adult day services . The Gerontologist , 58, 730–738. doi: 10.1093/geront/gnx074 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Care Quality Commission.(2016). The state of health care and adult social care in England 2015/16 Retrieved from http://www.cqc.org.uk/content/state-of-care
- Cleary M., Horsfall J., & Hayter M (2014). Data collection and sampling in qualitative research: Does size matter ? Journal of Advanced Nursing , 70 , 473–475. doi: 10.1111/jan.12163 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen-Mansfield J., Golander H. & Arnheim G (2000). Self-identity in older persons suffering from dementia: Preliminary results . Social Science & Medicine , 51 , 381–394. doi: 10.1016/S0277-9536(99)00471-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cohen-Mansfield J., Marx M. S., Thein K., & Dakheel-Ali M (2010). The impact of past and present preferences on stimulus engagement in nursing home residents with dementia . Aging & Mental Health , 14 , 67–73. doi: 10.1080/13607860902845574 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Conroy T. (2017). A beginner’s guide to ethnographic observation in nursing research . Nurse Researcher , 24 , 10–14. doi: 10.7748/nr.2017.e1472 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Custers A. F., Westerhof G. J., Kuin Y., Gerritsen D. L., & Riksen-Walraven J. M (2012). Relatedness, autonomy, and competence in the caring relationship: The perspective of nursing home residents . Journal of Aging Studies , 26 , 319–326. doi: 10.1016/j.jaging.2012.02.005 [ CrossRef ] [ Google Scholar ]
- Davies S., & Nolan M (2006). ‘Making it better’: Self-perceived roles of family caregivers of older people living in care homes: A qualitative study . International Journal of Nursing Studies , 43 , 281–291. doi: 10.1016/j.ijnurstu.2005.04.009 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Falk H. Wijk H. Persson L. O. & Falk K (2013). A sense of home in residential care . Scandinavian Journal of Caring Sciences , 27 , 999–1009. doi: 10.1111/scs.12011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Froggatt K., Davies S., & Meyer J (2009). Understanding care homes: A research and development perspective . Jessica Kingsley Publishers . [ Google Scholar ]
- Gale N. K. Heath G. Cameron E. Rashid S. & Redwood S (2013). Using the framework method for the analysis of qualitative data in multi-disciplinary health research . BMC Medical Research Methodology , 13 , 117. doi: 10.1186/1471-2288-13-117 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Geertz C. (1973). Thick description: Toward an interpretive theory of culture . In C. Geertz (Ed.), The interpretation of cultures: Selected essays (pp. 3–30). New York: Basic Books, Inc., Publishers. [ Google Scholar ]
- Gibbons F. X., & Gerrard M (1991). Downward social comparison and coping with threat . In Suls J. M. & Wills T. A. (Eds.), Social comparison: Theory and research (pp. 317–345). Hillside, NJ: Lawrence Erlbaum. [ Google Scholar ]
- Goffman E. (1961). Asylums: Essays on the social situation of mental patients and other inmates . London: Penguin. [ Google Scholar ]
- Golander H. (1995). Chronically ill, old, and institutionalized: Being a nursing home resident . Family & Community Health , 17 , 63–79. doi: 10.1097/00003727-199501000-00008 [ CrossRef ] [ Google Scholar ]
- Haslam C. Alexander Haslam S. Knight C. Gleibs I. Ysseldyk R., & McCloskey L. G (2014). We can work it out: Group decision-making builds social identity and enhances the cognitive performance of care residents . British Journal of Psychology , 105 , 17–34. doi: 10.1111/bjop.12012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haslam A., Jetten J., Postmes T., & Haslam C (2009). Social identity, health, and well-being: An emerging agenda for applied psychology . Applied Psychology , 58 , 1–23. doi: 10.1111/j.1464-0597.2008.00379.x [ CrossRef ] [ Google Scholar ]
- Hockey J., & James A (2003). Social identities across the life course . Basingstoke: Palgrave Macmillan. [ Google Scholar ]
- Hogg M., & Abrams D (1988). Social identifications: A social psychology of intergroup relations and group processes . London: Routledge. [ Google Scholar ]
- Hubbard G., Tester S., & Downs M. G (2003). Meaningful social interactions between older people in institutional care settings . Ageing and Society , 23 , 99–114. doi: 10.1017/S0144686X02008991 [ CrossRef ] [ Google Scholar ]
- Iyer A. Jetten J. Tsivrikos D. Postmes T. & Haslam S. A (2009). The more (and the more compatible) the merrier: Multiple group memberships and identity compatibility as predictors of adjustment after life transitions . The British Journal of Social Psychology , 48 ( Pt. 4 ), 707–733. doi: 10.1348/014466608X397628 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jetten J., & Pachana N. A (2012). Not wanting to grow old: A social identity model of identity change (SIMIC) analysis of driving cessation among older adults . In Jetten J., Haslam C., & Haslam A. S. (Eds.), The social cure: Identity, health and well-being . East Sussex, UK: Psychology Press. [ Google Scholar ]
- Kingston A. Wohland P. Wittenberg R. Robinson L. Brayne C. Matthews F. E., … Jagger C; Cognitive Function and Ageing Studies Collaboration (2017). Is late-life dependency increasing or not? A comparison of the Cognitive Function and Ageing Studies (CFAS) . The Lancet , 390 , 1676–1684. doi: 10.1016/S0140-6736(17)31575-1 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kloos N., Trompetter H. R., Bohlmeijer E. T., & Westerhof G. J (2018). Longitudinal associations of autonomy, relatedness, and competence with the well-being of nursing home residents . The Gerontologist , 00, 1–9. doi: 10.1093/geront/gny005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Knight C., Haslam A., & Haslam C (2010). In home or at home? How collective decision making in a new care facility enhances social interaction and wellbeing amongst older adults . Ageing & Society , 30 , 1393–1418. doi: 10.1017/S0144686X10000656 [ CrossRef ] [ Google Scholar ]
- Kroger J., Martinussen M. & Marcia J. E (2010). Identity status change during adolescence and young adulthood: A meta-analysis . Journal of Adolescence , 33 , 683–698. doi: 10.1016/j.adolescence.2009.11.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lievesley N., Crosby G., Bowman C., & Midwinter E (2011). The changing role of care homes . BUPA and Centre for Policy on Ageing. Retrieved from http://www.cpa.org.uk/information/reviews/changingroleofcarehomes.pdf (accessed December 20, 2015). [ Google Scholar ]
- Lincoln Y. S., & Guba E. G (1985). Naturalistic inquiry . Newbury Park, CA: Sage. [ Google Scholar ]
- Lloyd L., Calnan M., Cameron A., Seymour J., & Smith R (2014). Identity in the fourth age: Perseverance, adaptation and maintaining dignity . Ageing & Society , 34 , 1–19. doi: 10.1017/S0144686X12000761 [ CrossRef ] [ Google Scholar ]
- Næss A., Fjær E. G., & Vabø M (2016). The assisted presentations of self in nursing home life . Social Science & Medicine , 150 ( Suppl. C ), 153–159. doi: 10.1016/j.socscimed.2015.12.027 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- NCHR&D.(2006). My home life: Quality of life in care homes Retrieved from http://myhomelife.org.uk/wp-content/uploads/ 2014/11/mhl_report.pdf
- Newnham E. C. McKellar L. V. & Pincombe J. I (2017). Paradox of the institution: Findings from a hospital labour ward ethnography . BMC Pregnancy and Childbirth , 17 , 2. doi: 10.1186/s12884-016-1193-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oakes P. J., Haslam A., & Turner J. C (1994). Stereotyping and social reality . Oxford, England: Blackwell. [ Google Scholar ]
- O’Reilly M., & Parker N (2012). ‘Unsatisfactory Saturation’: A critical exploration of the notion of saturated sample sizes in qualitative research . Qualitative Research , 13 , 190–197. doi: 10.1177/1468794112446106 [ CrossRef ] [ Google Scholar ]
- Reicher S. D., Spears R., & Haslam A (2010). The social identity approach in social psychology . In Wetherell M. & Mohanty C. T. (Eds.), Sage identities handbook (pp. 45–62). London: Sage. [ Google Scholar ]
- Ritchie J., & Spencer L (1994). Qualitative data analysis for applied policy research . In Bryman A. & Burgess R. G. (Eds.), Analyzing qualitative data (pp. 173–194). London: Routledge. [ Google Scholar ]
- Roberts A. R., & Ishler K. J (2017). Family involvement in the nursing home and perceived resident quality of life . The Gerontologist , 00, 1–11. doi: 10.1093/geront/gnx108 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shenton A. (2004). Strategies for ensuring trustworthiness in qualitative research projects . Education for Information , 22 , 63–75. doi: 10.3233/EFI-2004-22201 [ CrossRef ] [ Google Scholar ]
- Srivastava P., & Hopwood N (2009). A practical iterative framework for qualitative data analysis . International Journal of Qualitative Methods , 8 , 76–84. doi: 10.1177/160940690900800107 [ CrossRef ] [ Google Scholar ]
- Surr C. A. (2006). Preservation of self in people with dementia living in residential care: A socio-biographical approach . Social Science & Medicine , 62 , 1720–1730. doi: 10.1016/j.socscimed.2005.08.025 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tajfel H. (1981). Human groups and social categories: Studies in social psychology . Cambridge: Cambridge University Press. [ Google Scholar ]
- Tajfel H., & Turner J (1979). An integrative theory of intergroup conflict . In Austin W. G. & Worchel S. (Eds.), The social psychology of intergroup relations (pp. 33–37). Monterey, CA: Brooks-Cole. [ Google Scholar ]
- Tester S., Hubbard G., Downs M., MacDonald C., & Murphy J (2004). What does quality of life mean for frail residents ? Nursing and Residential Care , 6 , 89–92. doi: 10.12968/nrec.2004.6.2.12052 [ CrossRef ] [ Google Scholar ]
- Turner J. C. (1982). Towards a cognitive redefinition of the social group . In Tajfel H. (Ed.), Social identity and intergroup relations (Vol. 1 , pp. 15–40). Cambridge: Cambridge University Press. [ Google Scholar ]
- Twigg J. & Buse C. E (2013). Dress, dementia and the embodiment of identity . Dementia , 12 , 326–336. doi: 10.1177/1471301213476504 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Walshe C. E. Caress A. L. Chew-Graham C. & Todd C. J (2004). Case studies: A research strategy appropriate for palliative care ? Palliative Medicine , 18 , 677–684. doi: 10.1191/0269216304pm962ra [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ward D. J. Furber C. Tierney S. & Swallow V (2013). Using Framework Analysis in nursing research: A worked example . Journal of Advanced Nursing , 69 , 2423–2431. doi: 10.1111/jan.12127 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wiersma E., & Dupuis S. L (2010). Becoming institutional bodies: Socialization into a long-term care home . Journal of Aging Studies , 24 , 278–291. doi: 10.1016/j.jaging.2010.08.003 [ CrossRef ] [ Google Scholar ]
- World Health Organisation.(2015). World report on ageing and health Retrieved from http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1
- Yin R. K. (2009). Case study research: Design and methods (Vol. 5 ). London: Sage. [ Google Scholar ]
- Yin R. K. (2010). Qualitative research from start to finish . New York: Guilford Press. [ Google Scholar ]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Adverse Childhood Experiences
- Risk and Protective Factors
- Program: Essentials for Childhood: Preventing Adverse Childhood Experiences through Data to Action
- Adverse childhood experiences can have long-term impacts on health, opportunity and well-being.
- Adverse childhood experiences are common and some groups experience them more than others.

What are adverse childhood experiences?
Adverse childhood experiences, or ACEs, are potentially traumatic events that occur in childhood (0-17 years). Examples include: 1
- Experiencing violence, abuse, or neglect.
- Witnessing violence in the home or community.
- Having a family member attempt or die by suicide.
Also included are aspects of the child’s environment that can undermine their sense of safety, stability, and bonding. Examples can include growing up in a household with: 1
- Substance use problems.
- Mental health problems.
- Instability due to parental separation.
- Instability due to household members being in jail or prison.
The examples above are not a complete list of adverse experiences. Many other traumatic experiences could impact health and well-being. This can include not having enough food to eat, experiencing homelessness or unstable housing, or experiencing discrimination. 2 3 4 5 6
Quick facts and stats
ACEs are common. About 64% of adults in the United States reported they had experienced at least one type of ACE before age 18. Nearly one in six (17.3%) adults reported they had experienced four or more types of ACEs. 7
Preventing ACEs could potentially reduce many health conditions. Estimates show up to 1.9 million heart disease cases and 21 million depression cases potentially could have been avoided by preventing ACEs. 1
Some people are at greater risk of experiencing one or more ACEs than others. While all children are at risk of ACEs, numerous studies show inequities in such experiences. These inequalities are linked to the historical, social, and economic environments in which some families live. 5 6 ACEs were highest among females, non-Hispanic American Indian or Alaska Native adults, and adults who are unemployed or unable to work. 7
ACEs are costly. ACEs-related health consequences cost an estimated economic burden of $748 billion annually in Bermuda, Canada, and the United States. 8
ACEs can have lasting effects on health and well-being in childhood and life opportunities well into adulthood. 9 Life opportunities include things like education and job potential. These experiences can increase the risks of injury, sexually transmitted infections, and involvement in sex trafficking. They can also increase risks for maternal and child health problems including teen pregnancy, pregnancy complications, and fetal death. Also included are a range of chronic diseases and leading causes of death, such as cancer, diabetes, heart disease, and suicide. 1 10 11 12 13 14 15 16 17
ACEs and associated social determinants of health, such as living in under-resourced or racially segregated neighborhoods, can cause toxic stress. Toxic stress, or extended or prolonged stress, from ACEs can negatively affect children’s brain development, immune systems, and stress-response systems. These changes can affect children’s attention, decision-making, and learning. 18
Children growing up with toxic stress may have difficulty forming healthy and stable relationships. They may also have unstable work histories as adults and struggle with finances, jobs, and depression throughout life. 18 These effects can also be passed on to their own children. 19 20 21 Some children may face further exposure to toxic stress from historical and ongoing traumas. These historical and ongoing traumas refer to experiences of racial discrimination or the impacts of poverty resulting from limited educational and economic opportunities. 1 6
Adverse childhood experiences can be prevented. Certain factors may increase or decrease the risk of experiencing adverse childhood experiences.
Preventing adverse childhood experiences requires understanding and addressing the factors that put people at risk for or protect them from violence.
Creating safe, stable, nurturing relationships and environments for all children can prevent ACEs and help all children reach their full potential. We all have a role to play.
- Merrick MT, Ford DC, Ports KA, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019;68:999-1005. DOI: http://dx.doi.org/10.15585/mmwr.mm6844e1 .
- Cain KS, Meyer SC, Cummer E, Patel KK, Casacchia NJ, Montez K, Palakshappa D, Brown CL. Association of Food Insecurity with Mental Health Outcomes in Parents and Children. Science Direct. 2022; 22:7; 1105-1114. DOI: https://doi.org/10.1016/j.acap.2022.04.010 .
- Smith-Grant J, Kilmer G, Brener N, Robin L, Underwood M. Risk Behaviors and Experiences Among Youth Experiencing Homelessness—Youth Risk Behavior Survey, 23 U.S. States and 11 Local School Districts. Journal of Community Health. 2022; 47: 324-333.
- Experiencing discrimination: Early Childhood Adversity, Toxic Stress, and the Impacts of Racism on the Foundations of Health | Annual Review of Public Health https://doi.org/10.1146/annurev-publhealth-090419-101940 .
- Sedlak A, Mettenburg J, Basena M, et al. Fourth national incidence study of child abuse and neglect (NIS-4): Report to Congress. Executive Summary. Washington, DC: U.S. Department of Health an Human Services, Administration for Children and Families.; 2010.
- Font S, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse Negl. 2016;51:390-399.
- Swedo EA, Aslam MV, Dahlberg LL, et al. Prevalence of Adverse Childhood Experiences Among U.S. Adults — Behavioral Risk Factor Surveillance System, 2011–2020. MMWR Morb Mortal Wkly Rep 2023;72:707–715. DOI: http://dx.doi.org/10.15585/mmwr.mm7226a2 .
- Bellis, MA, et al. Life Course Health Consequences and Associated Annual Costs of Adverse Childhood Experiences Across Europe and North America: A Systematic Review and Meta-Analysis. Lancet Public Health 2019.
- Adverse Childhood Experiences During the COVID-19 Pandemic and Associations with Poor Mental Health and Suicidal Behaviors Among High School Students — Adolescent Behaviors and Experiences Survey, United States, January–June 2021 | MMWR
- Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004 Feb;113(2):320-7.
- Miller ES, Fleming O, Ekpe EE, Grobman WA, Heard-Garris N. Association Between Adverse Childhood Experiences and Adverse Pregnancy Outcomes. Obstetrics & Gynecology . 2021;138(5):770-776. https://doi.org/10.1097/AOG.0000000000004570 .
- Sulaiman S, Premji SS, Tavangar F, et al. Total Adverse Childhood Experiences and Preterm Birth: A Systematic Review. Matern Child Health J . 2021;25(10):1581-1594. https://doi.org/10.1007/s10995-021-03176-6 .
- Ciciolla L, Shreffler KM, Tiemeyer S. Maternal Childhood Adversity as a Risk for Perinatal Complications and NICU Hospitalization. Journal of Pediatric Psychology . 2021;46(7):801-813. https://doi.org/10.1093/jpepsy/jsab027 .
- Mersky JP, Lee CP. Adverse childhood experiences and poor birth outcomes in a diverse, low-income sample. BMC pregnancy and childbirth. 2019;19(1). https://doi.org/10.1186/s12884-019-2560-8 .
- Reid JA, Baglivio MT, Piquero AR, Greenwald MA, Epps N. No youth left behind to human trafficking: Exploring profiles of risk. American journal of orthopsychiatry. 2019;89(6):704.
- Diamond-Welch B, Kosloski AE. Adverse childhood experiences and propensity to participate in the commercialized sex market. Child Abuse & Neglect. 2020 Jun 1;104:104468.
- Shonkoff, J. P., Garner, A. S., Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. https://doi.org/10.1542/peds.2011-2663
- Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsych. 2017;87(1):3. https://doi.org/10.1037/ort0000133 .
- Schofield TJ, Donnellan MB, Merrick MT, Ports KA, Klevens J, Leeb R. Intergenerational continuity in adverse childhood experiences and rural community environments. Am J Public Health. 2018;108(9):1148-1152. https://doi.org/10.2105/AJPH.2018.304598 .
- Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. J Adolesc Health. 2013;53(4 Suppl):S32-38. https://doi.org/10.1016/j.jadohealth.2013.05.004 .
Adverse Childhood Experiences (ACEs)
ACEs can have a tremendous impact on lifelong health and opportunity. CDC works to understand ACEs and prevent them.
- Skip to main content
- Keyboard shortcuts for audio player
Weekend Edition Sunday
- Latest Show
Sunday Puzzle
- Corrections
Listen to the lead story from this episode.
Politics chat: Biden and Trump pin their hopes on debate to give them an edge
by Tamara Keith , Mara Liasson
Meet the woman who escaped two conflicts — as a Palestinian refugee, then in Ukraine
by Tamara Keith , Eleana Tworek
Biden will address the commencement ceremony at Morehouse College. Protests are expected
by Tamara Keith , Stephen Fowler

These teens were missing too much school. Here's what it took to get them back
by Leigh Paterson , Elizabeth Miller
Plant-based restaurants are adding beef. Does the climate math add up?
by Tamara Keith , Julia Simon
An iconic chocolate factory shuts shop in Chicago
by Michael Puente

Sunday Puzzle NPR hide caption
Sunday Puzzle: Complete the compound with these animal connections!
by Will Shortz
Tree seeds that flew around the moon are now being planted across the U.S.
by William Joseph Hudson
Music Interviews
Sudanese musician sinkane on his new album 'we belong'.
by Tamara Keith
The Supreme Court ruled to protect the CFPB. Here's why it matters for your money
Middle east, anger at netanyahu cuts through a somber tel aviv rally to bring home the hostages.
by Hadeel Al-Shalchi
Trump addresses NRA's annual meeting, urges them to vote
by Tamara Keith , Caroline Love
A London court will rule on Julian Assange's extradition to the U.S.
by Tamara Keith , Willem Marx
Rock icon or a victim of exploitation? Examining Amy Winehouse's legacy
by Tamara Keith , Stephen Thompson
Scientists at Berkeley develop a tool to help cities measure carbon emissions
by Kevin Stark / KQED
Furiosa makes a splash at the 2024 Cannes Film Festival
Environment, on a trail in the adirondack mountains, runners appreciate the spring season.
by Emily Russell, NCPR

Author Interviews
Hold on to your wishes — there's a 'spider in the well'.
by Tamara Keith , Samantha Balaban , Melissa Gray
Searching for a song you heard between stories? We've retired music buttons on these pages. Learn more here.

IMAGES
VIDEO
COMMENTS
2016 Shared Care Planning and Coordination Case Studies: 5 case studies highlight how providers went about implementing these technologies, the impacts they experienced, lessons they learned and pitfalls to avoid. Integrating Innovative Technology in the Home to Provide Enhanced Continuity of Care and Decreased Healthcare Costs for Older Adults ...
How A Long Term Companion Used HCP to Hire 51.5% More Employees and Build an Employer Brand That Resulted in an Indeed Click Through Rate Over 10x the Site Average. Caring for an aging parent or loved one can feel overwhelming. At A Long Term Companion, our compassionate, professional caregivers have been providing one-on-one support to our ...
BENEFITS Excluding physician fees, the average cost of caring for patients at home rather than the hospital is 19 percent lower. Clinical outcomes are comparable or better, while patient satisfaction is higher. CHALLENGES A sufficient and predictable number of enrolled patients is needed to develop economies of scale and justify the investment ...
An instrumental case study was used to achieve the research objectives . The transitional care team from the central RHS was the case of interest, named herein as 'Case D'. This team formed a diverse case, offering a different insight to the roles of nurses providing care in a home environment . Nurses in specially developed programmes to ...
Remote research technique: phone interviews. This COVID-19 study was part of a formative qualitative phase of the larger intervention study of the safe Home care Project to improve the safety of HC workers and clients [].All study protocols and materials were approved by the University of Massachusetts Lowell Institutional Review Board (IRB), approval number 19-112-QUI-XPD.
This COVID-19 study was part of a formative qualitative phase of the larger intervention study of the safe Home care Project to improve the safety of HC workers and clients . All study protocols and materials were approved by the University of Massachusetts Lowell Institutional Review Board (IRB), approval number 19-112-QUI-XPD.
goals for home care, 369 home visit, 368-369 interdisciplinary care plan, 373-375 Neal Theory implications, 370 orders for home care, 368 rehabilitation needs, 368 reimbursement considerations, 367 CLTC (community long term care), 65, 67 Coach, health care, 29-30 Colostomy care, in hospice case study, 447-457 Commission on Chronic ...
Home health care is an important aspect of community health and a growing area of healthcare services. Clinical Case Studies in Home Health Care uses a case-based approach to provide home healthcare professionals, educators, and students with a useful tool for thoughtful, holistic care. The book begins with a thorough and accessible introduction to the principles of home health care, including ...
Home health care is an important aspect of community health and a growing area of healthcare services. Clinical Case Studies in Home Health Care uses a case-based approach to provide home healthcare professionals, educators, and students with a useful tool for thoughtful, holistic care. The book begins with a thorough and accessible introduction to the principles of home health care, including ...
Multiple studies have validated the cost savings and population health benefits associated with Home-Based Primary Care. Mount Sinai Visiting Doctors This New York City visiting doctors program, in operation for more than 15 years, allows for aging in place by providing in-home health care and chronic disease management for 1,100 elders.
The definitions in "Case Study Terms" are provided so readers can quickly clarify points and apply them to their own practice. Home Healthcare Nurse: The Journal for the Home Care and Hospice Professional 23(10):p 636-638, October 2005.
The Home Care Pathways study is a longitudinal, two province, mixed-methods study involving a retrospective analysis of administrative data, alongside a prospective qualitative comparative case study of interview data and policy documents to identify when, where and how approaches to care influence home care client pathways (see figs. 1 and 2).We adopt a partnered Integrated Knowledge ...
This case study is one in a series examining programs that aim to improve outcomes and reduce costs of care for patients with complex needs, who account for a large share of U.S. health care spending. Also read case studies about: Care Management Plus, CareMore, Commonwealth Care Alliance, Guided Care, Hennepin Health, MedStar Washington, PACE ...
This case study illustrates the characteristics of, and challenges for, a woman in the United States with multiple health problems. DATA SOURCES. Data were obtained through the authors' experience and knowledge of community health nursing and from published literature. DATA SYNTHESIS.
Table 1 shows each case's characteristics based on the following: (a) living location (urban or rural area); (b) older person's gender; (c) main caregiver referring to the type of carer and gender; (d) older person's dependency level - measured through the Barthel index (Wade and Collin, 1988); (e) distance from home to care home ...
The use of SIP within a multiple case study design, with interview and observational methods, is unique in care home research. Although moving to a care home initially emphasized age-related changes, institutional restrictions and limited social networks further undermined residents' identities over time.
Case history. A 78-year-old suffered a work injury. Because the worker was a quadriplegic, they needed wound care for a pressure ulcer on the right plantar heel. Until Paradigm started working on the file, the patient was being transported three times a week to the wound care clinic, and weekly to their physician appointments.
Health care aides (HCAs) are the backbone of the home care system and provide a range of services to people who, for various reasons related to chronic conditions and aging, are not able to take care of themselves independently. ... Home care and technology: a case study Stud Health Technol Inform. 2012;182:142-52. Authors Eleni Stroulia 1 ...
Our case manager and dementia care specialists work with you to design supportive and safe care at home—giving you an alternative to assisted living and Alzheimer's care in care facilities. For more about the value of strength-based dementia care, see Judy Cornish's TEDx Talk, "The Dawn of Dementia Care."
To measure the outcomes of its Home Hospital program, MGB researchers recently conducted a study that was published in Annals of Internal Medicine. The team analyzed the outcomes of 5,858 U.S ...
Date: May 22, 2024. Nursing and staffing shortages continue to be a pain point for leaders facing the increasing demand for care at home. While there is no one-size-fits-all solution to address these challenges, a panel of industry leaders shared pathways to sustain the nursing workforce at the 2024 Axxess, Growth, Innovation and Leadership ...
In the project life cycle phase, the project's life cycle begins. There are five steps during this phase: (1) feasibility, (2) business studies, (3) functional model itera-tion, (4) design and build iteration, and (5) implementation. In steps one and two, the feasibility and business studies are completed.
Case Managers use a comprehensive evaluation that: Assesses our physical, psychological and social needs. Considers available family members and friends who are able to assist us before looking at other available paid options. Is used to build a supportive services plan. Case Managers continue to oversee our progress until we are able to manage ...
Equitable Care: Help foster a culture and environment that ensures that this patient population receives equal attention and resources; work to decrease biases. Physical Environment: Be aware of defined spaces for safe and private evaluation and ongoing treatment. Patient and Staff Safety: Regularly assess and communicate patient risk; know ...
Copenhagen firm WE Architecture has completed a proposal for a "Dog Center" in Moscow that challenges traditional notions of animal shelters. Nestled in the countryside, the one-story pavilion ...
According to the National Alliance for Caregiving, over 65 million Americans serve as family caregivers for a disabled or ill relative. On average, caregivers shoulder 37.4 hours of care per week ...
Medical Assistance in Dying (MAiD) was legalized in Canada in 2016. Canada's legislation is the first to permit Nurse Practitioners (NP) to serve as independent MAiD assessors and providers. Registered Nurses' (RN) also have important roles in MAiD that include MAiD care coordination; client and family teaching and support, MAiD procedural quality; healthcare provider and public education ...
Research Design and Methods. A multiple qualitative case study approach incorporated interview and observational data. Eighteen semistructured interviews and 260 hr of observations were conducted over 1 year with care home residents, relatives, and staff across three care homes within Greater Manchester, UK.
Toxic stress, or extended or prolonged stress, from ACEs can negatively affect children's brain development, immune systems, and stress-response systems. These changes can affect children's attention, decision-making, and learning. 18. Children growing up with toxic stress may have difficulty forming healthy and stable relationships.
Meet the woman who escaped two conflicts — as a Palestinian refugee, then in Ukraine. by Tamara Keith, Eleana Tworek. 6 min.